Please set your exam date
Drugs Used for Anxiety Disorders
Study Questions
Practice Exericise 1
Which of the following best describes anxiety?
Explanation
Anxiety is a common psychological and physiological response nurses assess when clients exhibit symptoms such as restlessness, tension, or worry. Understanding the nature of anxiety helps nurses differentiate it from fear or other mental health conditions, allowing for appropriate interventions and patient education.
Rationale for correct answer:
3. A normal response involving apprehension of danger:
This best describes anxiety. It is a normal, adaptive response that becomes problematic only when excessive or interfering with functioning. It involves physical, cognitive, and emotional components.
Rationale for incorrect answers:
1. A real emotional response to an immediate threat:
This describes fear, which is an emotional reaction to a known or definite threat. Anxiety, in contrast, is more diffuse and often related to unknown or potential danger.
2. An unpleasant feeling caused by actual danger only:
Anxiety can occur in the absence of actual danger. It is more commonly associated with anticipation of potential harm rather than a direct, present threat.
4. A state that always requires medical treatment:
While some forms of anxiety may require treatment, not all anxiety warrants medical intervention. Mild or situational anxiety is part of the normal human experience and often resolves without clinical support.
What distinguishes a panic attack from generalized anxiety disorder (GAD)?
Explanation
Understanding the difference between panic disorder and generalized anxiety disorder (GAD) is essential in nursing assessments and mental health interventions. While both fall under anxiety disorders, they differ significantly in onset, duration, symptom patterns, and intensity.
Rationale for correct answer:
2. Panic attacks involve an abrupt surge of intense fear:
This defines a panic attack accurately. It involves rapid onset, intense physical symptoms (e.g., palpitations, chest pain, shortness of breath), and peaks within 10 minutes.
Rationale for incorrect answers:
1. GAD has a sudden onset of symptoms:
GAD is characterized by persistent, excessive worry lasting for 6 months or more, not a sudden onset. Its symptoms develop gradually and are often chronic.
3. Panic attacks are caused by daily stressors:
While stress may trigger a panic attack, they often occur unexpectedly and are not always linked to specific daily events.
4. GAD causes more physical symptoms than panic disorder:
Panic attacks typically involve more acute physical symptoms, such as trembling, sweating, and chest discomfort, compared to the chronic muscle tension and fatigue in GAD.
Take-home points:
- Panic attacks involve a sudden surge of overwhelming fear with intense physical symptoms, peaking within minutes.
- GAD features long-term, excessive worry across various domains of life, with more chronic and less intense symptoms.
- Nurses should distinguish between episodic panic attacks and persistent anxiety to implement effective treatment strategies.
What is a hallmark feature of Generalized Anxiety Disorder (GAD)?
Explanation
Generalized Anxiety Disorder (GAD) is one of the most commonly encountered anxiety disorders in clinical practice. It is defined by persistent, uncontrollable worry that spans various aspects of daily life, such as health, work, finances, and relationships. Identifying this hallmark pattern of excessive worry lasting for at least 6 months helps nurses screen, refer, and support clients with chronic anxiety symptoms.
Rationale for correct answer:
3. Excessive worry for more than 6 months:
GAD is defined by chronic, excessive, and difficult-to-control worry about various life areas. The anxiety persists most days for at least 6 months, often accompanied by symptoms like restlessness, fatigue, and muscle tension.
Rationale for incorrect answers:
1. Avoidance of specific objects:
This describes phobias, where anxiety is focused on a specific object or situation (e.g., snakes, heights), not the generalized worry seen in GAD.
2. Obsessions and compulsions:
These are hallmark features of Obsessive-Compulsive Disorder (OCD), not GAD. Obsessions are intrusive thoughts, and compulsions are repetitive behaviors aimed at reducing anxiety.
4. Fear triggered by social exposure:
This describes Social Anxiety Disorder, where individuals experience significant fear of being judged or embarrassed in social situations.
Take-home points:
- GAD is marked by ongoing, excessive worry about everyday events lasting 6 months or more.
- Nurses should differentiate GAD from phobias, OCD, and social anxiety based on the focus and duration of worry.
- Early identification of GAD improves patient outcomes through timely mental health referral and intervention.
Which of the following best defines an obsession in OCD?
Explanation
In Obsessive-Compulsive Disorder (OCD), clients experience a cycle of obsessions and compulsions. Obsessions are persistent, intrusive thoughts or images that cause significant anxiety, while compulsions are behaviors intended to neutralize or reduce the distress. Nurses must recognize how clients with OCD often understand that their obsessions are irrational, yet still feel unable to control them.
Rationale for correct answers:
2. An unwanted, intrusive thought:
This is the hallmark of an obsession. These thoughts are distressing, often irrational, and difficult to suppress, even when the person knows they’re unreasonable.
Rationale for incorrect answers:
1. A repetitive behavior that reduces anxiety:
This defines a compulsion, not an obsession. Compulsions include rituals like handwashing or checking that temporarily relieve anxiety caused by obsessions.
3. A pleasant idea that brings relief:
Obsessions are usually disturbing, not pleasant. They trigger anxiety and lead to compulsive behaviors for temporary relief.
4. A response to a real danger:
Obsessions are not based on real external threats. They are internal, persistent thoughts that are perceived as intrusive or disturbing by the client.
Take-home points:
- Obsessions in OCD are unwanted, intrusive thoughts that cause anxiety despite being recognized as irrational.
- Compulsions are the behaviors or rituals performed to relieve anxiety triggered by obsessions.
- Understanding the difference between obsessions and compulsions is critical for appropriate nursing assessment and intervention.
Which anxiety disorder is most strongly associated with a genetic link?
Explanation
Nurses must understand the biological and genetic underpinnings of anxiety disorders to anticipate risks and provide holistic care. Among all anxiety disorders, panic disorder shows the strongest genetic association, often running in families and linked with neurochemical imbalances involving serotonin and norepinephrine.
Rationale for correct answers:
2. Panic disorder:
This disorder has a notable hereditary pattern, with studies showing that first-degree relatives are significantly more likely to develop it. It is closely tied to genetic vulnerability and neurochemical dysregulation.
Rationale for incorrect answers:
1. Simple phobia:
While phobias may be influenced by learned behavior or trauma, they have weaker genetic connections compared to panic disorder.
3. Generalized anxiety disorder:
Although there may be some familial tendency, the genetic component is less robust than in panic disorder.
4. Social anxiety disorder:
This may also run in families, but it is often more influenced by environmental and developmental factors, such as early childhood experiences or social modeling.
Take-home points:
- Panic disorder has the strongest evidence of genetic linkage among anxiety disorders.
- Understanding familial trends in mental health helps in assessing patient risk and planning early interventions.
- Nurses should consider both biological and psychosocial factors when evaluating patients with anxiety.
Practice Exercise 2
Which of the following assessment findings should prompt the nurse to hold a dose of lorazepam?
Explanation
Benzodiazepines like lorazepam are central nervous system depressants used for anxiety and sedation. Nurses must prioritize respiratory status when administering these drugs, as respiratory depression is a potentially life-threatening adverse effect. A low respiratory rate warrants immediate action, including holding the dose and notifying the provider.
Rationale for correct answer:
2. Respiratory rate of 10 breaths per minute:
A respiratory rate below 12 breaths per minute is a red flag for respiratory depression in patients taking CNS depressants. Lorazepam should be withheld, and the provider notified.
Rationale for incorrect answers:
1. Blood pressure 120/80 mmHg:
This is a normal blood pressure reading and does not contraindicate lorazepam administration.
3. Patient reports headache:
While a headache can occur with anxiety or medication use, it is not an immediate contraindication to administering lorazepam.
4. Temperature of 37.2°C (98.9°F):
This is within normal limits and does not influence lorazepam safety or effectiveness.
Take-home points:
- Monitor respiratory rate closely before administering benzodiazepines.
- Hold lorazepam if the respiratory rate falls below 12/min to prevent respiratory compromise.
- Prioritize assessment of vital signs in clients on CNS depressants
Which drug is best suited for immediate relief of an acute panic attack?
Explanation
In acute psychiatric emergencies such as panic attacks, nurses must administer medications that act rapidly to alleviate severe anxiety symptoms. Benzodiazepines like diazepam are effective due to their fast onset of action, making them ideal for immediate symptom relief. In contrast, other anxiolytics require longer periods to reach therapeutic levels.
Rationale for correct answers:
4. Diazepam:
A benzodiazepine with rapid onset, diazepam quickly reduces symptoms of acute anxiety and can abort a panic attack within minutes, making it the most appropriate choice.
Rationale for incorrect answers:
1. Sertraline:
This is a selective serotonin reuptake inhibitor (SSRI) used for long-term management of anxiety disorders, but it takes several weeks to become effective and is not appropriate for acute relief.
2. Buspirone:
Although buspirone treats chronic anxiety, it has a delayed onset (typically 1–2 weeks) and lacks sedative properties, so it's not suitable for acute panic situations.
3. Hydroxyzine:
This antihistamine has anxiolytic and sedative effects, but its onset is slower and it is less reliable than benzodiazepines for rapidly stopping a panic attack.
Take-home points:
- Benzodiazepines like diazepam are first-line for acute panic attacks due to their rapid action.
- SSRIs and buspirone are used for chronic anxiety, not immediate symptom control.
- Always consider onset of action when choosing medications for acute versus long-term anxiety treatment.
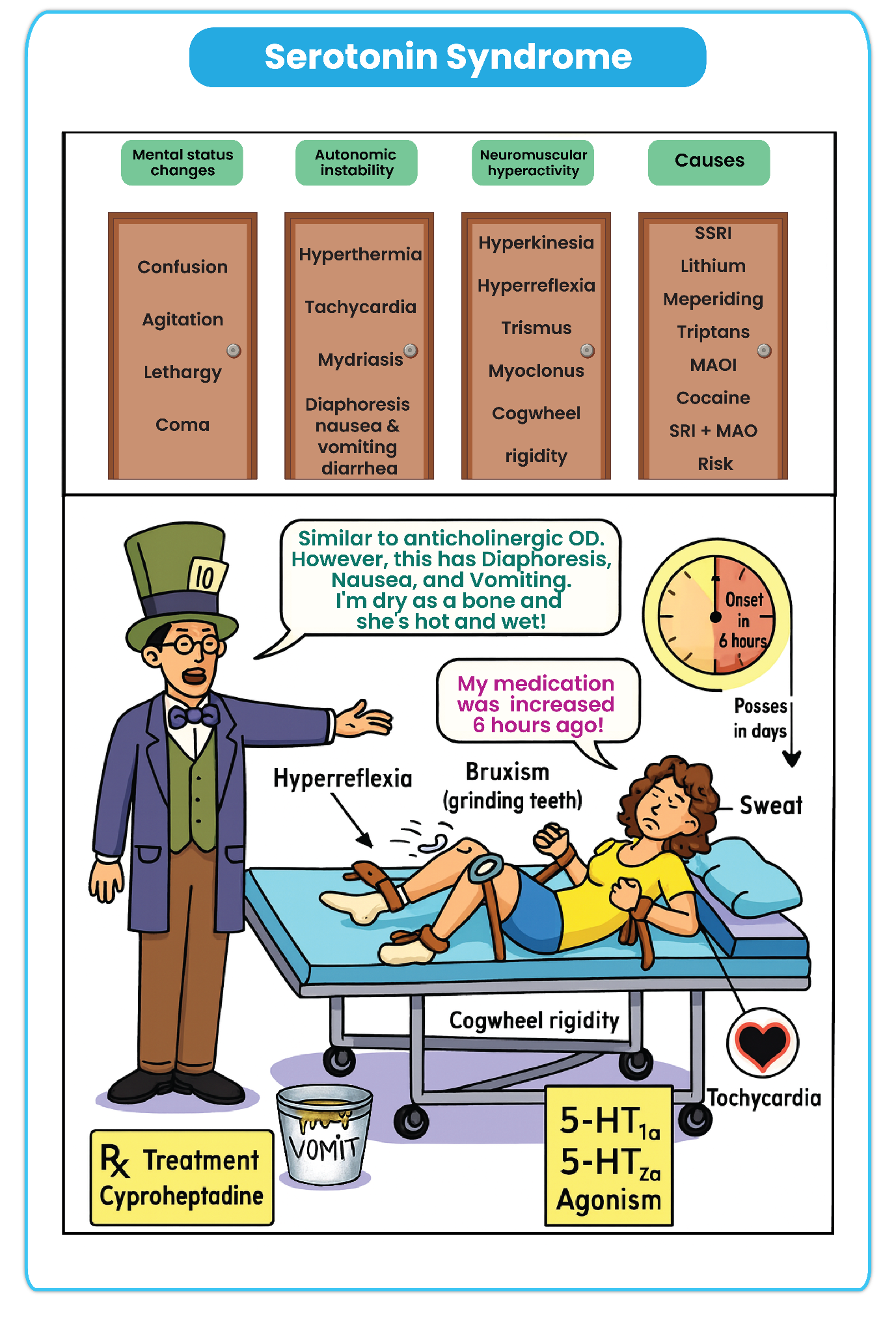
A client taking fluoxetine reports agitation, muscle twitching, fever, and confusion. What complication should the nurse suspect?
Explanation
Serotonin syndrome is a potentially life-threatening complication that can occur with excess serotonergic activity, often due to SSRI use like fluoxetine. Nurses must be alert to the triad of symptoms: neuromuscular abnormalities (e.g., twitching), autonomic instability (e.g., fever), and altered mental status (e.g., confusion).
Rationale for correct answers:
3. Serotonin syndrome:
Characterized by excessive serotonin activity, this syndrome presents with agitation, muscle twitching, hyperthermia, confusion, and may lead to seizures or coma. It is a known risk of fluoxetine, especially if combined with other serotonergic agents.
Rationale for incorrect answers:
1. Neuroleptic malignant syndrome:
This is associated with antipsychotic medications and presents with muscle rigidity, hyperthermia, and altered consciousness, but not typically with twitching or serotonergic drug use.
2. Discontinuation syndrome:
Occurs when SSRIs are abruptly stopped, leading to flu-like symptoms, insomnia, imbalance, and sensory disturbances, rather than fever, agitation, or twitching.
4. Anticholinergic toxicity:
Involves dry mouth, urinary retention, blurred vision, hyperthermia, and delirium, but does not usually include muscle twitching or relate to SSRI use.
Take-home points:
- Serotonin syndrome is a medical emergency linked to serotonergic medications like SSRIs.
- Key symptoms include mental status changes, autonomic instability, and neuromuscular hyperactivity.
- Early recognition and discontinuation of the offending drug are vital to prevent complications.
A nurse is educating a client prescribed fluoxetine. Which statement indicates a need for further teaching?
Explanation
When teaching patients about SSRIs such as fluoxetine, nurses must emphasize adherence, safety, and side effect expectations. Fluoxetine requires consistent, long-term use, often taking several weeks to reach full therapeutic effect.
Rationale for correct answers:
3. "I can stop taking the medication if I feel okay.":
This signals misunderstanding. Abruptly stopping fluoxetine can lead to withdrawal symptoms and risk relapse or serotonin imbalance. It should only be discontinued under medical supervision.
Rationale for incorrect answers:
1. "I should avoid alcohol while taking this medication.":
This reflects proper understanding. Alcohol can increase CNS depression and interfere with the medication’s therapeutic effects.
2. "It might take several weeks before I feel better.":
This is accurate. SSRIs like fluoxetine often take 2 to 4 weeks to show noticeable improvements in mood.
4. "I may experience nausea or insomnia at first.":
This is correct. Early side effects of SSRIs include GI upset and sleep disturbances, which often diminish over time.
Take-home points:
- Fluoxetine should not be discontinued without consulting a healthcare provider.
- Patient education should stress medication adherence and delayed onset of therapeutic effects.
- Early side effects like insomnia and nausea are common but often temporary
Which medication is contraindicated in a client with asthma and social anxiety?
Explanation
When selecting anxiolytic medications for patients with comorbid conditions, nurses must evaluate potential contraindications and respiratory risks. Beta-blockers like propranolol are sometimes used off-label for performance-related social anxiety, but their non-selective beta-blocking effect can exacerbate bronchospasm in patients with asthma.
Rationale for correct answers:
3. Propranolol:
Propranolol is contraindicated in asthma due to its non-selective beta-blocking activity, which may trigger bronchoconstriction and worsen asthma symptoms.
Rationale for incorrect answers:
1. Sertraline:
This SSRI is commonly used for social anxiety and does not pose a respiratory risk, making it a safe option for patients with asthma.
2. Buspirone:
Buspirone is non-sedating and lacks respiratory effects, making it suitable for anxiety in patients with asthma.
4. Hydroxyzine:
This antihistamine can be used for anxiety and may cause sedation, but it does not cause bronchospasm and is typically safer than beta-blockers in asthma patients.
Take-home points:
- Propranolol is contraindicated in patients with asthma due to risk of bronchospasm.
- Medication choice for anxiety must consider comorbid respiratory conditions.
- SSRIs and non-sedating anxiolytics like buspirone are safer alternatives in asthma
Practice Exercise 3
A client taking imipramine experiences blurred vision and constipation. These effects are best described as:
Explanation
When caring for patients prescribed tricyclic antidepressants (TCAs) such as imipramine, nurses must monitor for common anticholinergic effects that may appear during therapy. These include blurred vision, dry mouth, urinary retention, and constipation—all of which are predictable pharmacologic responses related to the anticholinergic properties of TCAs
Rationale for correct answers:
1. Expected anticholinergic side effects:
Imipramine, a TCA, often causes blurred vision and constipation due to its inhibition of acetylcholine, which reduces parasympathetic activity.
Rationale for incorrect answers:
2. Signs of overdose toxicity:
TCA overdose typically causes cardiac arrhythmias, severe hypotension, or seizures, not isolated blurred vision and constipation.
3. Symptoms of serotonin syndrome:
This condition is characterized by agitation, hyperreflexia, fever, tremors, and diarrhea, not anticholinergic effects like dry mouth or blurred vision.
4. Hypersensitivity reactions:
Hypersensitivity involves rash, fever, and possibly anaphylaxis, which are immune-mediated—not anticholinergic effects.
What nursing instruction is essential for a client starting duloxetine for anxiety?
Explanation
Duloxetine, a serotonin-norepinephrine reuptake inhibitor (SNRI), is used to treat generalized anxiety disorder and depression. While it is generally well-tolerated, it may lead to increased blood pressure, especially at higher doses. Therefore, blood pressure monitoring is essential, particularly during the initial stages of therapy or dose adjustments.
Rationale for correct answers:
3. "Check your blood pressure regularly."
Duloxetine can cause dose-related hypertension due to norepinephrine reuptake inhibition, making blood pressure monitoring an important nursing instruction.
Rationale for incorrect answers:
1. "Expect effects within 1–2 days.
SNRIs like duloxetine typically take 2 to 4 weeks for full therapeutic effects, not within 1–2 days.
2. "Avoid operating heavy machinery due to sedation."
Sedation is less common with duloxetine than with benzodiazepines; this instruction is not routinely emphasized.
4. "You can take it PRN when feeling anxious."
Duloxetine must be taken on a regular schedule to maintain therapeutic levels. It is not effective as a PRN (as-needed) medication.
A nurse is caring for a client newly prescribed buspirone. Which of the following statements by the client indicates a need for further teaching?
Explanation
Buspirone is an anxiolytic used for the long-term management of generalized anxiety disorder (GAD). Unlike benzodiazepines, it does not cause sedation or dependency, and it is not effective for acute anxiety relief. It must be taken consistently on a scheduled basis, not as needed.
Rationale for correct answers:
2. “I can take this medication whenever I feel anxious.”
This reflects a misunderstanding. Buspirone must be taken regularly (not PRN) to maintain steady plasma levels for therapeutic benefit.
Rationale for incorrect answers:
1. “I know this medication may take a few weeks to start working.”
This statement is accurate. Buspirone typically takes 2 to 4 weeks to achieve full anxiolytic effects.
3. “I will avoid drinking grapefruit juice while on this medication.”
This is appropriate. Grapefruit juice may inhibit CYP3A4, increasing buspirone levels and the risk of side effects.
4. “This drug does not cause dependence like benzodiazepines.”
This is true. Buspirone has no abuse potential and is not associated with physical dependence or withdrawal.
A nurse is caring for a client starting escitalopram. What symptom should be reported immediately?
Explanation
Escitalopram, a selective serotonin reuptake inhibitor (SSRI), is commonly prescribed for anxiety and depression. While generally well tolerated, SSRIs can increase the risk of suicidal ideation, especially in children, adolescents, and young adults, particularly during the first few weeks of therapy.
Rationale for correct answer:
3. Suicidal thoughts
This is a priority finding that requires immediate intervention. Suicidal ideation can emerge or worsen when starting antidepressants and must be reported right away.
Rationale for incorrect answers:
1. Mild headache
A common and transient side effect of SSRIs, especially in the first week; usually resolves without intervention.
2. Increased anxiety
This may occur early in treatment before therapeutic effects are established. It is often temporary but should be monitored—not an emergency.
4. Sexual dysfunction
A known and common side effect of SSRIs, but not emergent. It should be addressed in follow-up visits if it persists.
Take-home points:
- Always assess for suicidal ideation when initiating SSRIs.
- Early side effects like anxiety or headache are common but should not be ignored if they worsen.
- Sexual side effects are common and dose-dependent, but not immediately dangerous.
Which client statement about quetiapine indicates proper understanding?
Explanation
Quetiapine, an atypical antipsychotic sometimes used off-label for generalized anxiety disorder or agitation, is associated with metabolic side effects, including weight gain, hyperglycemia, and dyslipidemia.
Rationale for correct answers:
1. "This drug might increase my blood sugar and weight."
This demonstrates accurate understanding. Quetiapine is known to cause metabolic syndrome, especially in long-term use, requiring monitoring of glucose and lipid levels.
Rationale for incorrect answers:
2. "This will give me energy and help with concentration."
Quetiapine is sedating, not stimulating. It may impair concentration and cause drowsiness, especially early in treatment.
3. "I should take this medication only when I feel anxious."
Quetiapine must be taken on a regular schedule as prescribed, not PRN. It is not a short-acting anxiolytic.
4. "It causes fewer side effects than other anxiety medications."
This is misleading. While it may be effective in treatment-resistant cases, it carries significant side effect risks including sedation, metabolic effects, and extrapyramidal symptoms.
Take-home points:
- Quetiapine may increase blood sugar and cause weight gain, requiring regular metabolic monitoring.
- It must be taken regularly, not as-needed; it is not meant for immediate anxiety relief.
- It is not free of side effects and may cause sedation, so patient education is essential.
Comprehensive Questions
A nurse working in an emergency department is caring for a client who has benzodiazepine toxicity due to an overdose. Which of the following is the priority nursing action?
Explanation
In cases of benzodiazepine overdose, the central nervous system can become significantly depressed, affecting airway, breathing, and consciousness. The nurse must follow the ABC (Airway, Breathing, Circulation) priority framework, which emphasizes assessment before intervention. Identifying the client’s neurological status is essential to determine the urgency of further treatment, including antidote use or advanced airway support.
Rationale for correct answer:
B. Identify the client’s level of orientation:
Assessing the client’s level of consciousness and orientation is the priority initial action because it provides critical information about the severity of CNS depression and airway risk. This assessment guides the urgency and type of interventions needed, including potential antidote administration or airway management.
Rationale for incorrect answers:
A. Administer flumazenil (Romazicon):
Flumazenil is the antidote for benzodiazepine toxicity, but it should not be given before assessing the client’s neurological status. It can precipitate seizures, especially in clients with long-term benzodiazepine use or co-ingestion of other substances.
C. Infuse IV fluids:
IV fluids may help support circulation, but they do not address the CNS depression caused by benzodiazepines. This action is supportive and not the first priority in a toxicity scenario unless hypotension or dehydration is present.
D. Prepare the client for gastric lavage:
Gastric lavage is rarely used and is most effective if performed within one hour of ingestion. It carries risks such as aspiration, especially in clients with depressed mental status, and should not precede a neurological and airway assessment.
Take-home points:
- Always assess before intervening, especially in overdose scenarios.
- Flumazenil is not routinely used in all benzodiazepine overdoses due to seizure risk.
- The priority is to assess airway and neurological status before initiating further treatment.
- Follow the ABC priority framework: Airway, Breathing, Circulation.
A nurse is caring for a client who is to begin taking escitalopram (Lexapro) for treatment of generalized anxiety disorder. Which of the following statements by the client indicates understanding of the use of this medication?
Explanation
Escitalopram (Lexapro), an SSRI, is frequently prescribed for generalized anxiety disorder (GAD). Client teaching should focus on medication adherence, delayed therapeutic effects, and the importance of gradual discontinuation. Sudden cessation can result in withdrawal symptoms, emphasizing the need for tapering under medical supervision.
Rationale for correct answer:
C. “I need to discontinue this medication slowly.”
This response shows accurate understanding of the medication. SSRIs should be tapered gradually to prevent discontinuation syndrome, which may cause dizziness, nausea, headache, irritability, or sensory disturbances if stopped abruptly.
Rationale for incorrect answers:
A. “I will take the medication at bedtime.”
Although escitalopram may cause drowsiness in some, it more commonly leads to insomnia or restlessness, particularly when therapy is initiated. Taking it in the morning helps avoid sleep disturbances.
B. “I will need to follow a low-sodium diet while taking this medication.”
There is no requirement for sodium restriction with escitalopram. While SSRIs may cause hyponatremia—especially in older adults—it is not managed through routine dietary sodium restriction unless clinically necessary.
D. “I probably won’t desire intimacy during the first days of treatment.”
While sexual dysfunction is a potential side effect of SSRIs, it usually develops after prolonged use, not within the initial days. The statement reflects a misunderstanding of the timing and nature of this adverse effect.
Take-home points:
- Taper SSRIs gradually to avoid withdrawal symptoms.
- Onset of action is delayed—symptom relief may take 1–4 weeks.
- Monitor for sexual side effects, though these typically appear after continued use.
A nurse is providing teaching to a client who has a new prescription to start buspirone (BuSpar) in place of diazepam (Valium). The client has a history of panic disorder and cirrhosis of the liver. The client asks why his provider is making the medication change. Which of the following statements is an appropriate response by the nurse?
Explanation
When treating panic disorder, medication selection must balance efficacy, safety, and risk for dependence. Benzodiazepines like diazepam carry a high risk of tolerance, dependence, and sedation, especially in clients with liver impairment. Buspirone, a non-benzodiazepine anxiolytic, provides a safer long-term alternative with a lower risk of dependence, making it especially suitable for clients transitioning off chronic benzodiazepine therapy.
Rationale for correct answer:
D. “Buspirone has less risk for dependency than other treatment options.”
This is the most appropriate response. Buspirone is non-sedating, non-habit forming, and does not lead to dependence or withdrawal symptoms like benzodiazepines, making it an ideal choice for clients with a history of long-term anxiety treatment or liver concerns.
Rationale for incorrect answers:
A. “Diazepam can cause seizures as an adverse effect.”
Diazepam is actually used to prevent or treat seizures, particularly status epilepticus. While withdrawal from benzodiazepines can cause seizures, seizures are not an expected adverse effect during therapeutic use.
B. “Diazepam is not indicated for the treatment of panic disorder.”
Diazepam is indicated for short-term management of anxiety and panic symptoms. However, long-term use is discouraged due to risks of dependence, sedation, and tolerance, particularly problematic in clients with chronic anxiety disorders.
C. “Buspirone is a safe medication for clients who have liver dysfunction.”
Buspirone is metabolized in the liver, and caution is advised in clients with hepatic impairment. Although it is safer than benzodiazepines, it is not entirely risk-free for those with liver disease, and dosing may need adjustment.
- Buspirone is preferred for long-term use due to its low abuse and dependence potential.
- Benzodiazepines should be used cautiously in clients with liver disease due to impaired metabolism.
- Buspirone does not cause sedation or euphoria, reducing misuse potential.
A nurse working in a mental health clinic is caring for a client who has obsessive-compulsive disorder and recently started a new prescription for buspirone (BuSpar). The client tells the nurse that the medication has not helped him sleep and that he is still having obsessive compulsions. Which of the following statements is an appropriate response by the nurse?
Explanation
Buspirone (BuSpar) is a non-benzodiazepine anxiolytic used primarily for generalized anxiety disorder (GAD). It has a delayed onset of action, often taking 2 to 4 weeks to reach full therapeutic effect. Unlike benzodiazepines, it is not effective for acute symptoms or immediate relief and does not produce sedation, making client education about timing and expectations essential.
Rationale for correct answer:
A. “It may take several weeks before you feel like the medication is helping.”
This is the best response because buspirone has a gradual onset of action, and therapeutic effects are not immediate. Setting proper expectations helps improve adherence and prevents premature discontinuation.
Rationale for incorrect answers:
B. “Take the medication just before bedtime to promote sleep.”
Buspirone does not have sedative properties and is not prescribed as a sleep aid. Advising the client to take it at bedtime for sleep issues misrepresents its pharmacologic profile.
C. “You should take the medication on an as-needed basis when you experience obsessive urges.”
Buspirone must be taken on a scheduled, consistent basis, not PRN. It is not suitable for treating acute anxiety episodes or compulsive urges on demand.
D. “Your provider may need to increase your prescription due to developing tolerance.”
Buspirone does not cause tolerance or dependence like benzodiazepines. If a dose adjustment is needed, it is typically based on symptom control rather than tolerance development.
Take-home points:
- Buspirone requires daily, consistent use and takes 2–4 weeks to show effects.
- It is not effective for acute anxiety or compulsive episodes.
- Client education on delayed onset is crucial for adherence.
A nurse is caring for a client who takes paroxetine (Paxil) to treat posttraumatic stress disorder. The client states that he grinds his teeth during the night, which causes jaw pain. The nurse should identify which of the following as possible measures to manage the client’s bruxism? Select all that apply
Explanation
Paroxetine (Paxil), an SSRI, is commonly prescribed for posttraumatic stress disorder (PTSD). One potential side effect of SSRIs is bruxism (teeth grinding), which may result in jaw pain, tooth damage, or sleep disruption. Management involves evaluating pharmacologic adjustments and non-pharmacologic strategies to relieve symptoms while maintaining therapeutic benefits.
Rationale for correct answers:
A. Concurrent administration of buspirone:
Adding buspirone can help reduce bruxism caused by SSRIs, particularly when related to increased serotonin activity. It has anxiolytic effects without worsening bruxism and is often used as an augmenting agent.
C. Use of a mouth guard:
A mouth guard worn at night is a safe, non-pharmacologic option that protects teeth from damage and may reduce discomfort. It does not treat the underlying cause but can alleviate physical effects of bruxism.
D. Changing to a different class of antianxiety medication:
If bruxism is severe and unresponsive, switching to a different drug class such as an SNRI or atypical anxiolytic (e.g., buspirone, hydroxyzine) may be beneficial. This helps reduce side effects while still treating PTSD symptoms.
Rationale for incorrect answers:
B. Administration of a different SSRI:
Switching to another SSRI may not resolve the bruxism, as this side effect can occur with any drug in the same class. A different SSRI could potentially produce the same serotonergic effects contributing to the problem.
E. Increasing the dose of paroxetine:
Increasing the dose may worsen bruxism due to greater serotonergic activity. It does not address the side effect and may lead to more discomfort or complications.
Take-home points:
- SSRIs may cause bruxism, especially at night, due to increased serotonin activity.
- Buspirone can help alleviate SSRI-induced bruxism without reducing antidepressant effect.
- Mouth guards protect teeth and ease physical symptoms, especially during sleep.
The nurse should assess a client who is taking lorazepam (Ativan) for the development of which of these adverse effects?
Explanation
Lorazepam (Ativan) is a benzodiazepine used for anxiety, sedation, and seizure control. While effective, it can cause central nervous system depression, especially in older adults or with prolonged use. Nurses must assess for signs of impaired coordination, sedation, and potential overdose.
Rationale for correct answer:
C. Ataxia:
Ataxia—uncoordinated movement or difficulty with balance—is a known adverse effect of lorazepam due to CNS depression. It is especially common in older adults and can increase fall risk, making regular neurological assessments essential.
Rationale for incorrect answers:
A. Tachypnea:
Lorazepam depresses the central nervous system and is more likely to cause bradypnea than tachypnea. An increased respiratory rate is not typically associated with benzodiazepine use.
B. Astigmatism:
Astigmatism is a refractive error of the eye and is unrelated to benzodiazepine therapy. Lorazepam does not affect the eye in a way that would cause or worsen this condition.
D. Euphoria:
While euphoria may occur, especially with high doses or misuse, it is not as common or clinically significant as ataxia. Euphoria can signal misuse but is not typically monitored as a standard adverse effect during routine use.
Take-home points:
- Ataxia is a key adverse effect of benzodiazepines, especially in older adults.
- Monitor for impaired coordination, sedation, and fall risk.
- Lorazepam causes CNS depression, not stimulation—expect slowed respiratory and neurological activity.
A client is receiving temazepam (Restoril). Which of these responses should a nurse expect the client to have if the medication is achieving the desired effect?
Explanation
Temazepam (Restoril) is a benzodiazepine hypnotic prescribed primarily for short-term management of insomnia. The expected therapeutic effect is improved sleep duration and quality. Nurses must evaluate whether the client is experiencing restorative, uninterrupted sleep, which indicates the medication is working as intended.
Rationale for correct answer:
D. The client reports sleeping 7 hours without awakening:
This is the desired therapeutic response to temazepam. The medication is intended to promote uninterrupted sleep, allowing for rest and improved daytime functioning.
Rationale for incorrect answers:
A. The client sleeps in 3-hour intervals, awakens for a short time, and then falls back to sleep:
While better than complete insomnia, fragmented sleep does not reflect full therapeutic success. The goal of temazepam is to promote continuous, restful sleep throughout the night.
B. The client reports feeling less anxiety during activities of daily living:
Temazepam is not prescribed for generalized anxiety relief during daytime activities. While it has anxiolytic properties, its use is targeted at nighttime sleep, not ongoing anxiety management.
C. The client reports having fewer episodes of panic attacks when stressed:
Panic disorder is not an indication for temazepam. Other benzodiazepines or medications like SSRIs are more appropriate for managing panic attacks. Temazepam is not expected to reduce panic symptoms during the day.
Take-home points:
- Temazepam is used short-term for insomnia, not daytime anxiety or panic disorders.
- The desired effect is 6–8 hours of uninterrupted sleep.
- Assess sleep patterns to determine treatment effectiveness.
A 32-year-old female client has been taking lorazepam (Ativan) for her anxiety and is brought into the emergency department after taking 30 days’ worth at one time. What antagonist for benzodiazepines may be used in this case?
Explanation
Lorazepam (Ativan) is a benzodiazepine used for anxiety, but in overdose, it can cause profound central nervous system depression, including respiratory suppression, coma, or death. Flumazenil is the specific benzodiazepine receptor antagonist used in emergencies to reverse sedation or toxicity.
Rationale for correct answer:
C. Flumazenil:
Flumazenil is the only benzodiazepine antagonist that acts by competitively inhibiting GABA receptors where benzodiazepines bind. It may rapidly reverse sedation but must be used cautiously due to the risk of seizures, especially in chronic benzodiazepine users or mixed overdoses.
Rationale for incorrect answers:
A. Epinephrine:
Epinephrine is a vasopressor and bronchodilator used in anaphylaxis or cardiac arrest, not for reversing benzodiazepine effects. It has no role in managing CNS depression due to lorazepam.
B. Atropine:
Atropine is an anticholinergic used to treat bradycardia or reverse certain cholinergic poisonings. It does not interact with GABA receptors and won’t reverse lorazepam toxicity.
D. Naloxone:
Naloxone is an opioid antagonist used for reversing opioid overdoses. It has no effect on benzodiazepine receptors and won’t reverse lorazepam-induced sedation.
Take-home points:
- Flumazenil is the antidote for benzodiazepine overdose.
- Use flumazenil with caution due to seizure risk, especially in chronic users.
- Distinguish between antidotes for different drug classes: naloxone for opioids, flumazenil for benzodiazepines.
A 17-year-old client has been prescribed escitalopram (Lexapro) for increasing anxiety uncontrolled by other treatment measures. Because of this client’s age, the nurse will ensure that the client and parents are taught what important information?
Explanation
When prescribing escitalopram (Lexapro), an SSRI antidepressant, to adolescents, nurses must prioritize safety education due to the black box warning about increased risk of suicidal ideation in clients under 24 years of age, particularly in the early phases of treatment or after dose changes.
Rationale for correct answer:
B. Signs of increasing depression or thoughts of suicide should be reported immediately.
Adolescents taking SSRIs are at an increased risk of suicidal thoughts, especially in the first few weeks. Parents and clients must be educated to monitor for behavioral changes, agitation, and worsening mood. This is the most urgent and relevant teaching.
Rationale for incorrect answers:
A. Cigarette smoking will counteract the effects of the drug.
While smoking can affect the metabolism of some psychotropics, it does not significantly alter escitalopram efficacy. This is not the most crucial safety education point for this age group.
C. The drug causes dizziness and alternative schooling arrangements may be needed for the first two months of use.
Although dizziness may occur, it is usually mild and does not warrant a major life disruption like altering school arrangements. This advice would be excessive and not evidence-based.
D. Anxiety and excitability may increase during the first two weeks of use but then will have significant improvement.
Early activation symptoms can occur, but they are not guaranteed. More importantly, this option fails to address the critical safety priority—suicide risk—which must always be emphasized in adolescent clients on SSRIs.
Take-home points:
- SSRIs like escitalopram carry a black box warning for increased suicide risk in adolescents and young adults.
- Monitor for behavioral changes, especially during the first few weeks or after dosage changes.
- Safety education for the family is essential when initiating antidepressants in clients under 2D.
A client admitted to the mental health unit following a panic attack that lasted longer than 15 minutes was advised to come in for medication adjustment.
Identify the type of behavior the client may be exhibiting with each cue. Indicate with an X in the box that gives an example of the behavior.
Explanation
|
Counts the number of steps that it takes to walk to the car |
Excessive and unrealistic worry about grades as a student |
Declines getting into the MRI machine, feeling too confined |
Suddenly feeling lightheaded and seeing spots, then fainting during a course examination |
|
|
Phobic disorder |
X |
|||
|
Generalized anxiety disorder |
X |
|||
|
Obsessive-compulsive and related disorder |
X |
|||
|
Panic disorder |
X |
Anxiety disorders are a group of mental health conditions characterized by excessive fear, worry, or behavioral disturbances that impair daily functioning. Each type of anxiety disorder presents with specific behavioral patterns. Understanding these distinctions enables nurses to recognize symptoms, contribute to accurate diagnosis, and provide individualized care.
Rationale for correct answer:
The behaviors in this scenario reflect classic symptoms of different anxiety-related disorders:
- Obsessive-compulsive and related disorder (OCD): Counting steps repeatedly is a common compulsive behavior aimed at reducing anxiety from intrusive thoughts or obsessions.
- Generalized anxiety disorder (GAD): Excessive and persistent worry about everyday situations (such as academic performance) is a hallmark of GAD.
- Phobic disorder: Avoidance of specific triggers (e.g., small, enclosed spaces like an MRI machine) suggests a phobic response.
- Panic disorder: Sudden physical symptoms like dizziness, visual disturbances, and fainting without clear medical cause may reflect a panic attack, especially in anxiety-provoking settings (like an exam).
Take-home points:
- OCD involves repetitive behaviors (compulsions) such as counting or checking that serve to reduce anxiety from intrusive thoughts.
- GAD is marked by persistent and excessive worry about multiple aspects of life, often without a clear trigger.
- Phobic disorders feature irrational fears of specific objects or situations, leading to avoidance behavior (e.g., fear of enclosed spaces).
A nurse performing a baseline mental status assessment on the client in the scenario will include which of the following details? Select all that apply
Explanation
A baseline mental status assessment is a fundamental component of psychiatric nursing care. It provides objective data about the client’s cognitive function, behavior, emotional state, and thought processes, which guides treatment planning and ongoing evaluation.
Rationale for correct answer
A. General appearance and appropriateness of attire
This provides insight into the client’s self-care, hygiene, and possible psychomotor changes often seen in psychiatric conditions like depression, schizophrenia, or mania.
B. Clarity of thought
Assesses cognitive processes and coherence, helping to identify delusions, disorganized thinking, or confusion, which may occur in conditions like psychosis or delirium.
C. Mood and affect
Evaluating the client’s emotional state (mood) and observable expression (affect) is essential to understand their psychological status and match it with reported symptoms.
D. Obsessions or compulsions
These are part of the thought content assessment, important in clients with obsessive-compulsive disorder (OCD) or anxiety disorders, and must be documented during baseline evaluation.
Rationale for incorrect answer:
E. Job history
This is not part of the mental status exam, although it may be included in the psychosocial history. It does not directly assess mental or emotional functioning and is not a core element of a mental status exam.
Take-home points:
- Mental status assessments focus on appearance, behavior, speech, mood/affect, thought processes/content, cognition, and insight/judgment.
- Details like employment or educational history are documented in the psychosocial section but not in the mental status exam.
- Always assess for risk factors, including delusions, hallucinations, and compulsive behaviors, during initial evaluations.
The nurse will monitor which of these laboratory values to determine whether there are any adverse effects for the client in the scenario who is receiving a benzodiazepine for anxiety?
Explanation
Benzodiazepines, including drugs like lorazepam and diazepam, are commonly prescribed for anxiety. While generally safe when used short-term, these medications can lead to systemic effects, especially with prolonged use. Nurses must monitor key laboratory parameters to detect early signs of organ dysfunction or toxicity.
Rationale for correct answers:
A. Complete blood cell count with differential
Bone marrow suppression and blood dyscrasias, although rare, can occur with benzodiazepines. Monitoring CBC can help identify anemia, leukopenia, or thrombocytopenia.
E. Liver function
Many benzodiazepines are metabolized hepatically. Liver enzyme elevations may occur with long-term use. Monitoring liver function helps identify hepatotoxicity.
F. Renal function
Although renal metabolism is minimal for most benzodiazepines, renal impairment may alter drug clearance, especially in older adults. Renal function tests help assess potential accumulation and toxicity risk.
8. Electrolytes
Imbalances may occur with altered fluid status or when benzodiazepines are used concurrently with other medications. Electrolyte monitoring ensures safe physiological balance, particularly in vulnerable populations.
Rationale for incorrect answers:
B. Thyroid function
Benzodiazepines do not affect thyroid hormone synthesis or regulation, so routine thyroid testing is not required unless clinically indicated.
C. Lipid panel
There is no established link between benzodiazepines and lipid metabolism. A lipid panel is not used to assess benzodiazepine adverse effects.
D. Blood glucose
Benzodiazepines are not known to affect glucose metabolism significantly. Blood glucose monitoring is not a standard safety measure unless the client has diabetes or is on medications affecting glucose.
The nurse caring for the client in the scenario with an anxiety disorder knows that certain drugs can be used for treatment of anxiety disorders. Match the drug class used in the treatment of the specific anxiety disorder.
|
DRUG CLASS USED FOR ANXIETY |
ANXIETY DISORDERS |
|
Azaspirones |
GAD |
|
Selective serotonin reuptake inhibitors |
Panic disorders |
|
Benzodiazepines |
OCD |
|
|
Phobias |
No explanation
After discussing with the client and the family the drug management of lorazepam (Ativan) for anxiety, the nurse knows further teaching is needed after the client makes which statement?
Explanation
Lorazepam (Ativan) is a short-acting benzodiazepine used for the management of anxiety disorders. It is associated with a risk for tolerance, dependence, and withdrawal symptoms. For this reason, clients should never discontinue the medication abruptly or without medical guidance. Patient and family education is essential to ensure safe use.
Rationale for correct answer:
C. “I understand that I can stop the drug at any time that I feel I do not need it anymore.”
This statement indicates a need for further teaching. Abrupt discontinuation can cause withdrawal symptoms such as tremors, agitation, insomnia, and even seizures. Tapering under medical supervision is required.
Rationale for incorrect answers:
A. “I know that I need to avoid drinking any alcohol while taking this Ativan.”
Alcohol is a central nervous system depressant, and its use with lorazepam can lead to profound sedation, respiratory depression, or death. Avoiding alcohol while on lorazepam is a correct and necessary precaution.
B. “I understand that this drug may make me drowsy during the day and I should not work around machinery while taking it.”
Lorazepam causes sedation and can impair coordination and reaction time. It is appropriate for the client to avoid operating machinery or driving until they understand how the drug affects them.
D. “I know that Ativan will start to work within a week.”
Although lorazepam has a rapid onset of action (typically within 20–60 minutes), clients may generalize it with other psychiatric medications like SSRIs that take a week or more to show effects. However, this minor misconception does not pose a serious safety risk compared to abrupt discontinuation.
Take-home points:
- Lorazepam must never be stopped abruptly; it requires tapering under supervision.
- Benzodiazepines have CNS depressant effects; avoid alcohol and hazardous activities.
- Nurses must clarify and correct misunderstandings that could lead to withdrawal or overdose.
A client is prescribed lorazepam (Ativan). What does the nurse know to be true regarding lorazepam?
Explanation
Lorazepam (Ativan) is a benzodiazepine that enhances the effect of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter in the central nervous system. While it is commonly used for anxiety, sedation, and insomnia, nurses must be aware of its neurological and behavioral side effects, especially when evaluating patient safety and medication teaching.
Rationale for correct answer
A. It may cause anterograde amnesia and sleep-related behaviors.
This is a known side effect of lorazepam and other benzodiazepines. Patients may perform complex behaviors such as sleepwalking, driving, or eating with no memory of the events afterward, increasing the risk for injury.
Rationale for incorrect answers:
B. It has a maximum adult dose of 25 mg/day.
This dosage exceeds the recommended range. The usual maximum dose for lorazepam is approximately 10 mg/day in divided doses for anxiety. Higher doses may be used in specific inpatient settings (e.g., status epilepticus), but not as a standard adult limit.
C. When combined with cimetidine, it causes plasma levels to be decreased.
Cimetidine inhibits the metabolism of several drugs, including benzodiazepines, thereby increasing, not decreasing, plasma levels of lorazepam, which may intensify its effects.
D. It interferes with the binding of dopamine receptors.
Lorazepam acts on GABA-A receptors, not dopamine receptors. This mechanism is distinct from antipsychotics, which block dopamine to reduce psychotic symptoms.
Take-home points:
- Lorazepam may cause anterograde amnesia and unusual sleep-related behaviors.
- Monitor for sedation, memory impairment, and fall risk, especially in older adults.
- Cimetidine increases lorazepam levels, raising the risk for excessive sedation.
Exams on Drugs Used for Anxiety Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
OBJECTIVES
- Define anxiety disorders and identify the main classes of drugs used in their pharmacologic treatment.
- Describe how SSRIs, SNRIs, benzodiazepines, and buspirone work to relieve anxiety symptoms.
- Distinguish between short-term and long-term pharmacologic treatments for anxiety disorders.
- Identify the major side effects, interactions, and precautions associated with anxiolytic drugs.
- Explain the role of beta-blockers, antihistamines, and antipsychotics in managing specific or resistant anxiety.
- Assess patients for baseline anxiety symptoms, risk factors, and response to prescribed medications.
- Educate patients on proper use, adherence, and lifestyle precautions related to anti-anxiety medications.
- Recognize signs of toxicity, serotonin syndrome, CNS depression, and withdrawal symptoms.
- Apply clinical judgment in selecting and adjusting pharmacologic interventions for different anxiety types.
- Use the nursing process to safely administer and evaluate the effectiveness of anxiety medications.
Introduction
Anxiety is a normal human emotion that is similar to fear.
It is an unpleasant feeling of apprehension or nervousness caused by the perception of potential or actual danger that threatens a person’s security, whereas fear is an emotional response to a real or perceived threat.
Mild anxiety is a state of heightened awareness of one’s surroundings and is seen in response to day-to-day circumstances.
This type of anxiety can be beneficial as a motivator for the individual to take action in a reasonable and adaptive manner. It is sometimes said that people find the inner strength to meet their challenges or “rise to the occasion.”
Anxiety is a primary symptom of many psychiatric disorders, including schizophrenia, mania, depression, dementia, and substance abuse.
Therefore, the evaluation of the anxious patient requires a thorough history and physical and psychiatric examinations to determine whether the anxiety is a primary condition or secondary to another illness.
Anxiety disorders are among the most common mental health conditions, characterized by excessive fear, worry, or apprehension that is out of proportion to actual situations.
These disorders often interfere with daily functioning, relationships, and quality of life.
Effective pharmacologic treatment can significantly improve patient outcomes, especially when combined with psychotherapy.
Anxiety disorders
3.1. Generalized Anxiety Disorder
Generalized anxiety disorder is described as excessive and unrealistic worry about two or more life circumstances (e.g., finances, illness, misfortune) for 6 months or more. Symptoms are both psychological (e.g., tension, fear, difficulty concentrating, apprehension) and physical (e.g., tachycardia, palpitations, tremor, sweating, gastrointestinal upset).
The disease has a gradual onset, usually among individuals in the 20- to 30-year-old age group, and it has twice the frequency among women as among men. This illness usually follows a chronic fluctuating course of exacerbations and remissions that are triggered by stressful events in the person’s life.
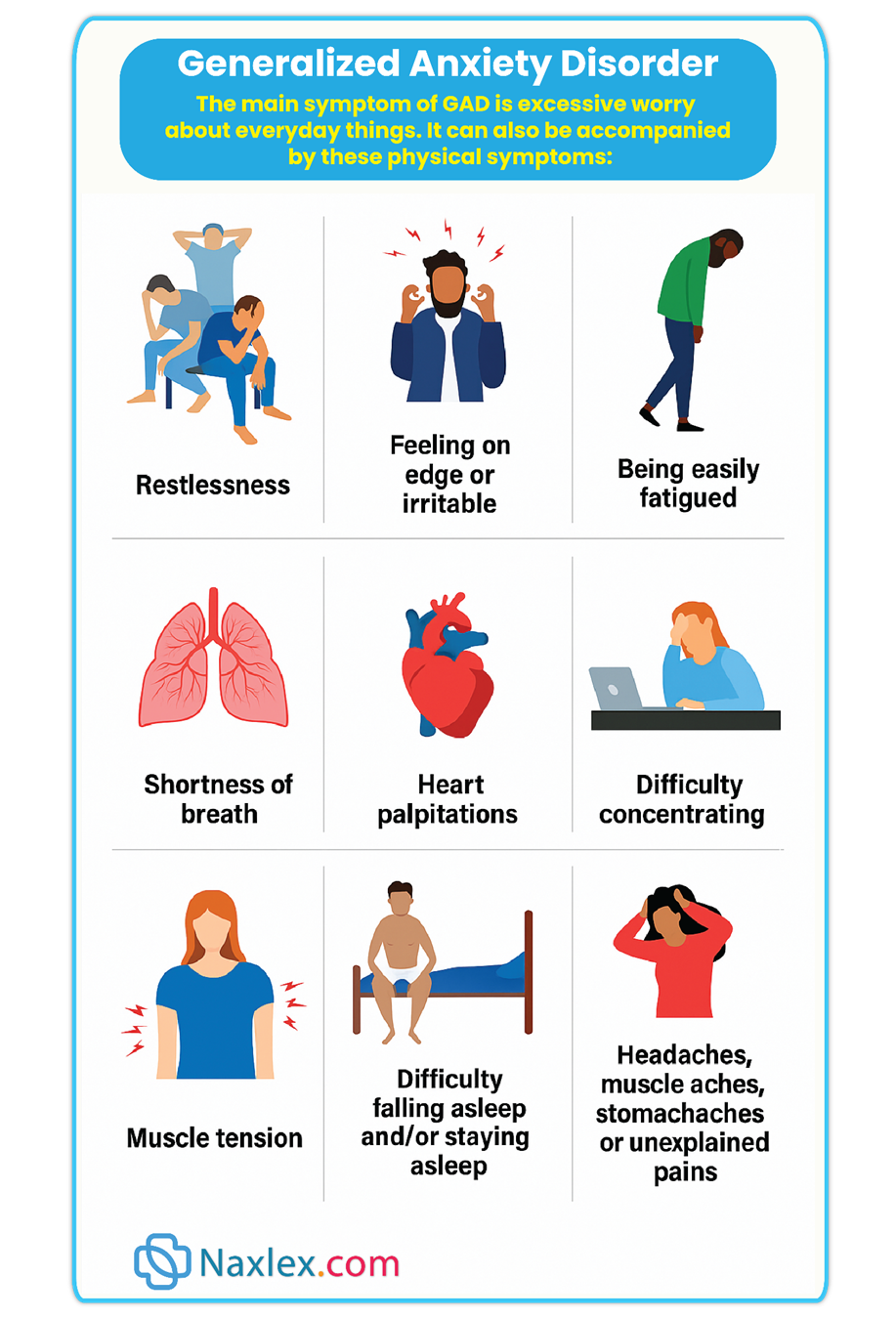
Persistent irrational anxiety or episodic anxiety generally requires medical and psychiatric treatment. Patients with generalized anxiety disorder often develop other psychiatric disorders (e.g., panic disorder, OCD, social anxiety disorder, major depression) at some time during their lives.
Panic disorder is recognized as a separate entity and not as a more severe form of chronic generalized anxiety disorder. A panic attack is an abrupt surge of intense fear or intense discomfort that reaches a peak within minutes.

During the attack, at least four of the following symptoms arise:
- Palpitations, tachycardia, or pounding heart
- Sweating
- Shaking or trembling
- Sensations of shortness of breath or smothering
- Feelings of choking
- Chest pain or discomfort
- Nausea or abdominal distress
- Feeling dizzy, unsteady, lightheaded, or faint
- Chills or heat sensations
- Numbness or tingling sensations
- Feelings of unreality or depersonalization
- Fear of losing control
- Fear of dying
The average age of onset is during the early 20s; the disorder is often relapsing and may require lifetime treatment. Panic disorder is estimated to affect 1% to 2% of Americans at some time during their lives. Women are affected two to three times more frequently than men.
Genetic factors appear to play a significant role in the disease; 15% to 20% of patients will have a close relative with a similar illness. Panic disorder begins as a series of acute or unprovoked anxiety (panic) attacks that involve an intense, terrifying fear. The attacks do not occur as a result of exposure to anxiety-causing situations, as phobias do.
Initially, the panic attacks are spontaneous, but later during the course of the illness, they may be associated with certain actions (e.g., driving a car, being in a crowded place). Patients with panic disorder often develop other psychiatric disorders (e.g., generalized anxiety disorder, personality disorders, substance abuse, OCD, social anxiety disorder, major depression) at some time during their lives.
Phobias are irrational fears of specific objects, activities, or situations. Unlike other anxiety disorders, the object or activity that creates the feeling of fear is recognized by the patient, who also realizes that the fear is unreasonable. The fear persists, however, and the patient seeks to avoid the situation.
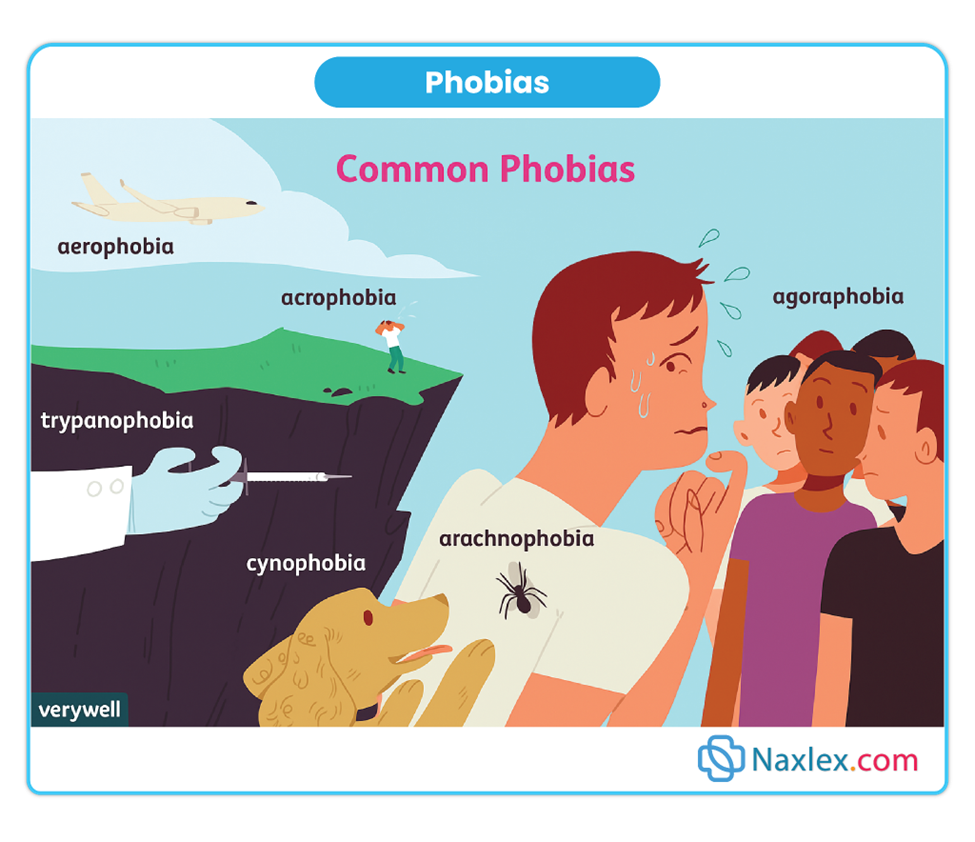
Social phobia is described as a fear of certain social situations in which the person is exposed to scrutiny by others and fears doing something embarrassing. A social phobia involving public speaking is fairly common, and the activity is usually avoided. If public speaking is unavoidable, it is done with intense anxiety. Social phobias are rarely incapacitating, but they do cause some interference with social or occupational functioning.
A simple phobia is an irrational fear of a specific object or situation, such as heights (acrophobia), closed spaces (claustrophobia), air travel, or driving. Phobias that involve animals such as spiders, snakes, and mice are particularly common. If the person with the phobia is exposed to the object, there is an immediate feeling of panic, sweating, and tachycardia. People are aware of their phobias, and they simply avoid the feared objects.
3.4. Obsessive-Compulsive Disorder (OCD)
OCD is not classified under anxiety disorders in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The DSM-5 added a new category of disorders called obsessive-compulsive and related disorders (OCRDs). The OCRDs category includes the familiar OCD.
Although anxiety remains a key feature in OCRDs, there are enough unique differences between anxiety disorders and OCRDs to justify a separate category.
The primary features of OCD are recurrent obsessions or compulsions that cause significant distress and interfere with normal occupational responsibilities, social activities, and relationships.
The average age of onset of the symptoms of OCD is during late adolescence to the early 20s. The condition occurs with twice the frequency in men as in women, and there also appears to be a genetic component to the disease. It is estimated that 2% to 8% of the general population suffers from OCD, making it one of the most common psychiatric disorders.
An obsession is an unwanted thought, idea, image, or urge that the patient recognizes as time-consuming and senseless but that repeatedly intrudes into that patient’s consciousness, despite their attempts to ignore, prevent, or counteract it.
Examples of obsessions are recurrent thoughts of dirt or germ contamination, a fear of losing things, a need to know or remember something, a need to count or check something, blasphemous thoughts, or concerns about something happening to the self or others. An obsession produces a tremendous sense of anxiety in the affected person.
A compulsion is a repetitive, intentional, purposeful behavior that must be performed to decrease the anxiety associated with an obsession. The act is done to prevent a vague dreaded event, but the person does not derive pleasure from the act. Common compulsions deal with cleanliness, grooming, and counting.
When patients are prevented from performing a compulsion, there is a sense of mounting anxiety. In some individuals, the compulsion can become the patient’s lifetime activity.
OCD is a complex condition that requires a highly individualized and integrated approach to treatment that includes pharmacologic, behavioral, and psychosocial components.
Drug therapy for anxiety disorders
Classes of Drugs Used to Treat Anxiety
The primary pharmacological classes used in treating anxiety disorders include:
- Benzodiazepines
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Buspirone
- Beta-blockers
- Antihistamines
- Atypical antipsychotics
Each class has unique mechanisms of action, indications, advantages, and drawbacks. The choice of agent is based on the type of anxiety disorder, patient history, response to previous treatments, and potential for side effects or abuse.
Examples: Diazepam, Lorazepam, Clonazepam, Alprazolam
Mechanism of Action: Benzodiazepines enhance the action of GABA, an inhibitory neurotransmitter, by binding to GABA-A receptors, promoting sedation, anxiolysis, muscle relaxation, and anticonvulsant activity. This results in calming effects by suppressing excessive neuronal activity.
Therapeutic Uses:
- Short-term treatment of acute anxiety
- Panic attacks
- Preoperative sedation
- Alcohol withdrawal
Pharmacokinetics:
- Rapid onset of action (especially diazepam and alprazolam)
- Metabolized in the liver, with varying half-lives
- Lipid-soluble; crosses blood-brain barrier quickly
Nursing Insight:
- Assess for sedation, respiratory depression, and hypotension
- Monitor for signs of dependence or tolerance
- Use short-term only to minimize risk of addiction
- Avoid alcohol or other CNS depressants
Patient Education:
- Avoid driving or hazardous activities
- Do not abruptly stop the medication (risk of withdrawal seizures)
- Use only as prescribed; risk of physical and psychological dependence
Adverse Effects:
- Drowsiness, confusion, ataxia, and memory impairment
- Paradoxical agitation in some older adults
- Long-term use increases risk for tolerance and dependence
Drug Interactions:
- Potentiates effects of alcohol, opioids, and other sedatives
- Metabolized via CYP450 enzymes, caution with enzyme inhibitors or inducers
5.2. SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs)
Examples: Paroxetine, Sertraline, Escitalopram, Fluoxetine
Mechanism of Action: SSRIs block the reuptake of serotonin (5-HT) at the synaptic cleft, increasing its availability. This improves mood and reduces symptoms of anxiety over time.
Therapeutic Uses:
- First-line treatment for generalized anxiety disorder (GAD)
- Panic disorder, OCD, PTSD, and social anxiety
- Effective for long-term control of anxiety symptoms
Pharmacokinetics:
- Onset of therapeutic action: 2–4 weeks
- Metabolized by liver; most have long half-lives
Nursing Insight:
- Monitor for serotonin syndrome, especially when combined with other serotonergic agents
- Assess for increased anxiety during early treatment phase
- Evaluate suicidal ideation, particularly in young adults
Patient Education:
- Takes weeks to feel full effect; continue taking even if no immediate change
- Do not stop abruptly (risk of discontinuation syndrome)
- Report symptoms of agitation, confusion, muscle twitching, fever (serotonin syndrome)
Adverse Effects:
- Nausea, sexual dysfunction, insomnia, weight gain, headache
- Initial increased anxiety before improvement begins
5.3. SEROTONIN-NOREPINEPHRINE REUPTAKE INHIBITORS (SNRIs)
Examples: Venlafaxine, Duloxetine, Desvenlafaxine
Mechanism of Action: SNRIs inhibit the reuptake of both serotonin and norepinephrine, enhancing neurotransmission involved in mood and arousal.
Therapeutic Uses:
- Second-line treatment for GAD, panic disorder, and PTSD
- May be effective when SSRIs are inadequate
Nursing Insight:
- Monitor blood pressure (especially with venlafaxine)
- Monitor for insomnia, restlessness, and nausea
Patient Education:
- May take 2–4 weeks to see effects
- Avoid alcohol and other CNS stimulants
Adverse Effects:
- Hypertension, headache, insomnia, dry mouth, sexual dysfunction
Mechanism of Action: Buspirone is a partial agonist at serotonin (5-HT1A) receptors. It modulates serotonin activity without sedative effects. Unlike benzodiazepines, it does not affect GABA.
Therapeutic Uses:
- Management of generalized anxiety disorder (GAD)
- Long-term control, not useful for acute anxiety or panic
Key Advantages:
- Non-sedating, non-habit forming
- Minimal abuse potential
- Does not cause tolerance or withdrawal
Nursing Insight:
- Takes 1–2 weeks for onset; 3–6 weeks for full effect
- Monitor for dizziness, nausea, and headaches
Patient Education:
- Take medication consistently, not PRN
- Avoid grapefruit juice (inhibits metabolism)
Adverse Effects:
- Dizziness, nausea, nervousness, lightheadedness
- Fewer cognitive side effects compared to benzodiazepines
5.5. TRICYCLIC ANTIDEPRESSANTS (TCAs)
Examples: Imipramine, Clomipramine, Amitriptyline, Nortriptyline
Mechanism of Action: TCAs inhibit the reuptake of both serotonin and norepinephrine, increasing their levels at synapses. They also block other receptors (muscarinic, histaminergic, alpha-adrenergic), contributing to side effects.
Therapeutic Uses:
- Second or third-line option for anxiety disorders
- Effective in panic disorder and OCD (especially clomipramine)
Adverse Effects:
- Anticholinergic effects: dry mouth, blurred vision, constipation, urinary retention
- Orthostatic hypotension, sedation, weight gain, cardiac arrhythmias
Nursing Insight:
- Baseline ECG may be needed before starting
- Use caution in older adults and cardiac patients
- Monitor for toxicity, especially in overdose (narrow therapeutic index)
5.6. MONOAMINE OXIDASE INHIBITORS (MAOIs)
Examples: Phenelzine, Tranylcypromine, Isocarboxazid
Mechanism of Action: MAOIs inhibit the enzyme monoamine oxidase, which breaks down serotonin, norepinephrine, and dopamine. This results in increased availability of these neurotransmitters.
Therapeutic Uses:
- Reserved for treatment-resistant anxiety and depression
- Rarely used due to dietary restrictions and risk of serious side effects
Dietary Restrictions:
- Avoid tyramine-rich foods (aged cheese, cured meats, wine) to prevent hypertensive crisis
Drug Interactions:
- Severe interaction with SSRIs, SNRIs, TCAs, meperidine → Serotonin syndrome
Nursing Insight:
- Monitor BP regularly
- Educate on dietary restrictions and drug interaction risks
Examples: Propranolol, Atenolol
Mechanism of Action: Beta blockers block beta-adrenergic receptors, reducing the physical symptoms of anxiety such as tachycardia, tremors, and sweating.
Therapeutic Uses:
- Performance anxiety (e.g., public speaking)
- Short-term situational anxiety
Nursing Insight:
- Monitor HR and BP
- Use cautiously in patients with asthma or diabetes
Adverse Effects:
- Bradycardia, hypotension, fatigue, sexual dysfunction
5.8. ANTIHISTAMINES (Hydroxyzine)
Mechanism of Action: Hydroxyzine blocks histamine (H1) receptors, leading to sedative and anxiolytic effects. It has some anticholinergic properties as well.
Therapeutic Uses:
- Short-term relief of anxiety
- Often used when benzodiazepines are contraindicated
Advantages:
- Non-habit forming
- Quick onset
Adverse Effects:
- Drowsiness, dry mouth, dizziness, blurred vision
5.9. ATYPICAL ANTIPSYCHOTICS
Examples: Quetiapine, Olanzapine, Risperidone (used off-label)
Mechanism of Action: Block dopamine and serotonin receptors; anxiolytic effects result from serotonin receptor antagonism.
Therapeutic Uses:
- Treatment-resistant anxiety
- Often as adjuncts to antidepressants
Adverse Effects:
- Weight gain, sedation, metabolic syndrome, EPS, increased prolactin
Summary
Anxiety is a normal emotional response to perceived threats, distinguished from fear, which is a reaction to a real danger.
Common Types of Anxiety Disorders
- Generalized Anxiety Disorder (GAD): Chronic worry over multiple life issues for 6+ months.
- Panic Disorder: Recurrent, unexpected panic attacks with intense physical and psychological symptoms.
- Phobias: Irrational fear of specific objects or situations (e.g., social, simple phobias).
- Obsessive-Compulsive Disorder (OCD): Characterized by persistent obsessions and compulsions, now classified under OCRDs in DSM-5.
Thorough assessment including medical, psychiatric history, and physical examination is crucial to distinguish primary anxiety from symptoms secondary to other conditions (e.g., depression, schizophrenia, substance abuse).
Benzodiazepines provide rapid relief of anxiety but carry risks of tolerance, dependence, and withdrawal.
Lorazepam, alprazolam, and diazepam are commonly prescribed benzodiazepines for short-term use.
SSRIs (e.g., sertraline, escitalopram) are first-line drugs for generalized anxiety, panic disorder, and social anxiety.
SSRIs may cause initial increased anxiety, GI upset, or sexual dysfunction during early treatment.
SNRIs such as venlafaxine and duloxetine treat anxiety by increasing serotonin and norepinephrine levels.
Buspirone is a long-term anxiety treatment with no risk of sedation or dependence but has delayed onset.
Beta-blockers, especially propranolol, are used to manage physical symptoms like tachycardia and tremors.
TCAs (e.g., amitriptyline) are older antidepressants used when SSRIs fail, but they cause anticholinergic side effects.
MAOIs are effective but rarely used due to dietary restrictions and serious drug interactions.
Hydroxyzine, an antihistamine, is a non-habit-forming option for acute anxiety relief.
Atypical antipsychotics like quetiapine may be added for treatment-resistant anxiety disorders.
Nurses should assess CNS depression, fall risk, and suicidal ideation, especially with sedating drugs.
Patient education includes avoiding alcohol, tapering benzodiazepines, and reporting worsening symptoms.
Nurses must collaborate with providers and monitor therapeutic response, adherence, and side effects regularly.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Anxiety Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


