Please set your exam date
Mood Disorders
Study Questions
Practice Exercise 1
A nurse is developing a care plan for a client diagnosed with bipolar disorder. The inclusion of the nursing diagnosis Risk for imbalanced nutrition demonstrates that the nurse understands that clients diagnosed with bipolar disorder:
Explanation
Bipolar disorder is a chronic psychiatric condition marked by alternating episodes of mania and depression, often accompanied by impaired judgment, impulsivity, and disrupted routines. During manic phases, individuals may neglect basic physiological needs, including nutrition and sleep, while depressive episodes can reduce appetite and motivation. These fluctuations contribute to inconsistent dietary intake and increased risk for nutritional deficiencies. Additionally, comorbidities such as substance use and gastrointestinal disturbances may further impair nutritional status.
Rationale for correct answer
2. Individuals with bipolar disorder frequently experience disorganized routines and impaired self-care during mood episodes, leading to skipped meals, poor food choices, and inadequate nutrient intake. This pattern contributes to malnutrition and supports the nursing diagnosis of Risk for imbalanced nutrition.
Rationale for incorrect answers
1. The term compulsive eating is more commonly associated with binge eating disorder or bulimia nervosa. While some individuals with bipolar disorder may overeat during manic episodes, this behavior is not consistent or diagnostic of the condition. Impulsivity may lead to erratic eating, but not compulsive patterns.
3. Although certain medications used in bipolar disorder, such as atypical antipsychotics, can contribute to weight gain, the diagnosis of Risk for imbalanced nutrition focuses on inadequate intake rather than excess. Obesity risk is a separate concern and not the primary rationale for this nursing diagnosis.
4. While some medications like stimulants or mood stabilizers may cause anorexia, this is not a universal effect and does not represent the predominant nutritional risk in bipolar disorder. The broader concern is inconsistent intake due to mood instability rather than pharmacologic weight loss.
Take Home Points
- Bipolar disorder disrupts daily routines, often leading to poor nutritional intake and self-care deficits.
- Nutritional risk is highest during manic and depressive episodes due to impaired judgment and motivation.
- Risk for imbalanced nutrition is based on inadequate intake, not compulsive eating or medication-induced weight changes.
- Differentiating bipolar-related nutritional issues from eating disorders or medication side effects is essential for accurate nursing diagnosis.
A nurse assesses a client who reports feeling full of energy in spite of being awake for the past 48 hours. Which diagnosis is the nurse likely to find documented in the client’s medical record?
Explanation
Bipolar disorder is a chronic psychiatric illness characterized by alternating episodes of mania and depression, with manic phases marked by elevated mood, reduced need for sleep, and hyperactivity. During mania, individuals may exhibit pressured speech, impulsive behavior, grandiosity, and severely impaired judgment. Sleep deprivation without fatigue is a hallmark feature. The condition is often diagnosed in adolescence or early adulthood and requires long-term pharmacologic and psychotherapeutic management.
Rationale for correct answer
2. The presence of elevated energy despite 48 hours of wakefulness is a classic indicator of a manic episode. Mania includes decreased need for sleep, heightened activity, and impaired insight, aligning with bipolar I disorder.
Rationale for incorrect answers
1. Obsessive-compulsive disorder involves intrusive thoughts and repetitive behaviors aimed at reducing anxiety. It does not present with decreased need for sleep or elevated energy levels, which are core features of mania.
3. Bipolar disorder/mixed type includes simultaneous symptoms of mania and depression, such as irritability with hopelessness. The absence of depressive features in the scenario makes this diagnosis less likely.
4. Korsakoff’s psychosis is a chronic memory disorder due to thiamine deficiency, often seen in alcohol use disorder. It presents with confabulation and amnesia, not elevated energy or reduced sleep need.
Take Home Points
- Bipolar I disorder is diagnosed after at least one manic episode, often with reduced sleep and heightened energy.
- Mania differs from hypomania by its severity and impact on functioning, including psychotic features.
- Mixed episodes involve concurrent depressive and manic symptoms, requiring careful differentiation.
- Korsakoff’s psychosis is a neurocognitive disorder unrelated to mood elevation or sleep disruption.
A nurse observes that a client diagnosed with major depressive disorder who recently started on an antidepressant is acting differently. Two days ago, the client appeared sad and remained in bed. Now the client is awake at 4 a.m. and planning a unit party. What is the most likely explanation for the change in behavior?
Explanation
Bipolar disorder is a mood disorder characterized by alternating episodes of depression and mania, often misdiagnosed as major depressive disorder due to symptom overlap. Manic episodes include elevated mood, decreased need for sleep, impulsivity, and grandiosity. Antidepressants given without mood stabilizers can precipitate manic symptoms in undiagnosed bipolar patients, leading to behavioral shifts such as excessive energy, early morning wakefulness, and socially inappropriate planning.
Rationale for correct answer
2. The sudden shift from depressive withdrawal to elevated activity and early morning wakefulness suggests a manic episode, likely triggered by antidepressant initiation. This pattern is consistent with bipolar disorder, not unipolar depression.
Rationale for incorrect answers
1. A positive response to antidepressants typically involves gradual mood improvement and restored functioning, not abrupt hyperactivity or insomnia. The client's behavior reflects mood destabilization rather than therapeutic progress.
3. Familiarity with the unit may increase comfort, but it does not explain the dramatic behavioral change. Planning a party at 4 a.m. indicates disinhibition and elevated mood, not mere self-expression.
4. Anticipation of discharge may cause relief, but it does not account for manic-like symptoms such as insomnia and excessive social planning. The timing and intensity of the behavior suggest a mood episode.
Take Home Points
- Bipolar disorder is frequently misdiagnosed as major depressive disorder due to overlapping depressive symptoms.
- Antidepressants can trigger mania in bipolar patients if not paired with mood stabilizers.
- Sudden behavioral activation, insomnia, and grandiosity are hallmark signs of mania.
- Differentiating bipolar disorder from unipolar depression is critical for safe and effective treatment.
A nurse is assessing the mental status of a client diagnosed with bipolar disorder. Which client behavior is the nurse most likely to assess during a manic episode?
Explanation
Mania is a distinct phase of bipolar disorder characterized by elevated mood, excessive energy, and cognitive acceleration. During manic episodes, individuals often exhibit rapid speech, impulsivity, and racing thoughts. One hallmark feature is “flight of ideas,” where the person jumps quickly from one topic to another, often with tenuous or illogical connections. This symptom reflects disorganized thinking and heightened psychomotor activity, and is frequently observed during psychiatric assessments of manic states.
Rationale for correct answer
3. The presence of flight of ideas reflects accelerated thought processes and disorganized speech, both of which are core features of mania. This symptom is often accompanied by pressured speech and distractibility, indicating cognitive dysregulation.
Rationale for incorrect answers
1. Social withdrawal is more characteristic of depressive episodes, where individuals isolate due to low energy, hopelessness, or anhedonia. It is not typical of manic behavior, which tends to be socially intrusive or overly engaging.
2. Somatic-type delusions are more common in psychotic disorders or severe depression with psychotic features. While mania can include grandiose delusions, somatic delusions are not a hallmark of manic episodes.
4. Trembling or shaking is a physical symptom more often associated with anxiety, withdrawal syndromes, or neurological conditions. It is not a diagnostic feature of mania and does not reflect the elevated mood or thought disturbances typical of bipolar disorder.
Take Home Points
- Flight of ideas is a hallmark cognitive symptom of mania in bipolar disorder.
- Mania presents with elevated mood, decreased need for sleep, and rapid, disorganized thinking.
- Social withdrawal and somatic delusions are more consistent with depressive or psychotic states.
- Physical symptoms like trembling are not diagnostic of manic episodes and suggest alternative etiologies.
The most common comorbid condition in children with bipolar disorder is:
Explanation
Attention-deficit/hyperactivity disorder (ADHD) is the most frequent comorbid condition in children diagnosed with bipolar disorder, often complicating diagnosis and treatment. Both conditions share overlapping features such as impulsivity, distractibility, and emotional dysregulation. ADHD typically presents earlier in childhood, while bipolar symptoms may emerge later, making early differentiation challenging. The presence of ADHD can intensify mood instability and impair executive functioning, requiring integrated pharmacologic and behavioral interventions.
Rationale for correct answer
4. ADHD is highly comorbid with pediatric bipolar disorder, with shared features like hyperactivity and poor impulse control. Its early onset and symptom overlap often mask or exacerbate bipolar presentations, making it the most prevalent co-occurring diagnosis.
Rationale for incorrect answers
1. Schizophrenia is rare in children and typically has a later onset than bipolar disorder. While psychotic features may occur in severe pediatric bipolar cases, schizophrenia is not a common comorbidity.
2. Substance disorders are more prevalent in adolescents and adults with bipolar disorder. In children, these are less common due to limited access and developmental factors, making them an unlikely primary comorbidity.
3. Oppositional defiant disorder involves defiance and argumentative behavior, which may co-occur but is less consistently linked to bipolar disorder than ADHD. Its behavioral nature does not share the neurobiological overlap seen with ADHD.
Take Home Points
- ADHD is the most common comorbid condition in pediatric bipolar disorder due to overlapping symptoms and early onset.
- Differentiating ADHD from bipolar disorder is essential for accurate diagnosis and treatment planning.
- Substance use disorders are more relevant in adolescent and adult bipolar populations.
- Schizophrenia and oppositional defiant disorder are less frequently comorbid with pediatric bipolar disorder.
A child with bipolar disorder also has attention-deficit/hyperactivity disorder (ADHD). How would these comorbid conditions most likely be treated?
Explanation
Comorbid bipolar disorder and ADHD in children presents a complex clinical challenge due to overlapping symptoms such as impulsivity, emotional dysregulation, and hyperactivity. Treating ADHD with stimulants before stabilizing mood can precipitate manic episodes or worsen mood instability. Therefore, clinical guidelines recommend prioritizing mood stabilization using mood stabilizers or atypical antipsychotics before initiating ADHD-specific pharmacotherapy. This sequence minimizes the risk of treatment-induced mania and ensures safer symptom control.
Rationale for correct answer
3. Stabilizing mood symptoms first is essential to prevent stimulant-induced manic episodes. Once bipolar symptoms are controlled, ADHD can be safely treated with non-stimulant or carefully monitored stimulant options.
Rationale for incorrect answers
1. Withholding medication for both conditions neglects the functional impairment caused by untreated mood and attention symptoms. Evidence-based practice supports pharmacologic intervention tailored to symptom severity and safety.
2. Simultaneous treatment risks manic activation, especially if stimulants are introduced before mood stabilization. This approach lacks safety prioritization and may exacerbate bipolar symptoms.
4. Treating ADHD first can trigger mania, especially with stimulant use. Bipolar disorder must be addressed initially to reduce the risk of destabilization and ensure therapeutic safety.
Take Home Points
- Bipolar disorder must be stabilized before initiating ADHD treatment to prevent manic exacerbation.
- Stimulants can worsen mood symptoms if used prematurely in bipolar-ADHD comorbidity.
- Non-stimulant ADHD options may be considered after mood stabilization.
- Integrated treatment planning is essential for managing overlapping symptoms in pediatric populations.
Which situation supports the biological theory of the development of bipolar affective disorder?
Explanation
Biological theory of bipolar disorder emphasizes neurochemical, genetic, and brain structure abnormalities as underlying causes. Dysregulation of neurotransmitters such as serotonin, dopamine, and norepinephrine contributes to mood instability. Genetic predisposition plays a significant role, with heritability estimates reaching up to 85%. Neuroimaging studies show structural and functional changes in regions like the prefrontal cortex and amygdala. Pharmacologic triggers, such as antidepressants, can unmask latent bipolar tendencies by altering neurotransmitter balance, supporting the biological basis of the disorder.
Rationale for correct answer
1. The emergence of manic symptoms—impulsivity, expansive mood, and flight of ideas—after SSRI initiation reflects a pharmacologically induced shift in neurotransmitter activity, supporting the biological theory of bipolar disorder development.
Rationale for incorrect answers
2. High energy demands from multiple jobs reflect behavioral adaptation, not a biologically driven mood disorder. This scenario lacks evidence of mood dysregulation or neurochemical involvement.
3. Fluctuating self-image and grandiosity may suggest personality traits or coping mechanisms, but without neurochemical or genetic indicators, it does not support the biological theory.
4. A chaotic household environment aligns with psychosocial theories, not biological. Environmental stressors may influence expression but do not constitute biological causation.
Take Home Points
- Biological theory of bipolar disorder centers on neurotransmitter imbalance, genetic predisposition, and brain structure abnormalities.
- SSRIs can trigger manic episodes in predisposed individuals, revealing underlying bipolar disorder.
- Environmental and behavioral factors may influence symptom expression but do not confirm biological causation.
- Differentiating biological from psychosocial models is essential for accurate diagnosis and treatment planning.
A nursing instructor is teaching about the criteria for the diagnosis of bipolar II disorder. Which student statement indicates that learning has occurred?
Explanation
Bipolar II disorder is a subtype of bipolar spectrum disorders characterized by recurrent depression and episodes of hypomania, which are less severe than full mania. Hypomanic episodes involve elevated mood, increased energy, and impulsivity but do not cause marked impairment or require hospitalization. The depressive episodes are often more debilitating and longer-lasting. Diagnosis requires at least one major depressive episode and one hypomanic episode, with no history of full manic episodes.
Rationale for correct answer
4. This statement accurately reflects the diagnostic criteria for bipolar II disorder, which includes episodic hypomania and recurrent depressive episodes. It demonstrates understanding of the distinction between bipolar I and II.
Rationale for incorrect answers
1. Bipolar II disorder does not include mania; that is a defining feature of bipolar I. The presence of full manic episodes excludes a diagnosis of bipolar II.
2. Hypomania and dysthymia are not the diagnostic criteria for bipolar II. Dysthymia refers to persistent depressive disorder, which is distinct from the episodic depression seen in bipolar II.
3. Mood disturbances due to substances fall under substance/medication-induced bipolar and related disorders, not bipolar II. This reflects a misunderstanding of etiology and diagnostic classification.
Take Home Points
- Bipolar II disorder requires at least one hypomanic and one major depressive episode, without any history of mania.
- Hypomania is less severe than mania and does not cause significant functional impairment.
- Substance-induced mood disorders are classified separately from bipolar I and II.
- Persistent depressive disorder (dysthymia) is distinct from the episodic depression seen in bipolar II.
Practice Exercise 2
A nurse is admitting a client with a history of bipolar disorder. The nurse determines that the client is in the manic phase. Which signs and symptoms contribute to the nurse’s conclusion? Select all that apply.
Explanation
Manic episode is a phase of bipolar disorder marked by elevated mood, increased energy, and disinhibition. Individuals often display impulsivity, reduced need for sleep, and excessive goal-directed activity. Cognitive symptoms include racing thoughts, distractibility, and rapid speech. Behavioral signs such as grandiosity and irritability are common, and psychotic features may emerge in severe cases. The presentation is typically abrupt and may impair social, occupational, or interpersonal functioning.
Rationale for correct answers
1. Irritability is a frequent mood manifestation in mania, often replacing or accompanying euphoria. It reflects heightened emotional reactivity and poor frustration tolerance, especially when goals are obstructed.
2. Grandiosity involves exaggerated self-esteem or unrealistic beliefs about one’s abilities, often seen in manic states. It reflects impaired insight and contributes to risky decision-making and interpersonal conflict.
3. Pressured speech is a hallmark of mania, characterized by rapid, loud, and difficult-to-interrupt verbal output. It reflects accelerated thought processes and heightened psychomotor activity.
Rationale for incorrect answers
4. Thought blocking is more typical of schizophrenia or severe depression, where cognitive flow is interrupted. It is not a feature of mania, which is marked by racing thoughts rather than halted ones.
5. Psychomotor retardation is a classic sign of major depressive episodes, involving slowed movement and speech. Mania presents with the opposite—psychomotor acceleration and hyperactivity.
Take Home Points
- Mania presents with elevated mood, irritability, grandiosity, and pressured speech.
- Thought blocking and psychomotor retardation are inconsistent with manic episodes.
- Differentiating manic symptoms from depressive and psychotic features is essential for accurate diagnosis.
- Behavioral and cognitive acceleration are central to identifying manic states in bipolar disorder.
The nurse assesses a client with the diagnosis of bipolar disorder, manic episode. Which clinical findings support this diagnosis? Select all that apply.
Explanation
Manic episode in bipolar disorder is defined by a distinct period of abnormally and persistently elevated, expansive, or irritable mood, lasting at least one week and accompanied by increased energy or activity. Core features include inflated self-esteem, decreased need for sleep, pressured speech, racing thoughts, distractibility, and excessive involvement in risky behaviors. These symptoms reflect heightened psychomotor and cognitive activation, often impairing social and occupational functioning.
Rationale for correct answers
4. Grandiosity reflects inflated self-esteem and unrealistic beliefs about one’s abilities, a classic symptom of mania. It contributes to poor judgment and risky decision-making during manic episodes.
5. Talkativeness, especially when excessive and difficult to interrupt, is a manifestation of pressured speech. It indicates accelerated thought processes and heightened verbal output, common in mania.
6. Distractibility arises from impaired attention and racing thoughts. Individuals in a manic state often shift topics rapidly and struggle to maintain focus, reflecting cognitive disorganization.
Rationale for incorrect answers
1. Passivity is more consistent with depressive states, where motivation and initiative are diminished. Mania typically presents with assertiveness or overactivity, not passivity.
2. Dysphoria, or a state of unease or dissatisfaction, may occur in mixed episodes but is not a hallmark of pure mania. Mania is more often associated with euphoria or irritability.
3. Anhedonia, the inability to feel pleasure, is a defining feature of depression. It contrasts with the heightened pleasure-seeking and goal-directed behavior seen in manic episodes.
Take Home Points
- Mania is characterized by elevated mood, grandiosity, distractibility, and pressured speech.
- Depressive symptoms like anhedonia and passivity are not consistent with manic presentations.
- Dysphoria may appear in mixed states but is not central to manic episodes.
- Accurate symptom recognition is essential for differentiating mood phases in bipolar disorder.
A client diagnosed with bipolar disorder states, “My mom has a history of depression.” While teaching about predisposing factors, using a biological theory, which client statement indicates that teaching has been successful?
Explanation
Biological theory of bipolar disorder emphasizes genetic predisposition, neurochemical imbalances, and brain structure abnormalities as key contributors to its development. Family history, especially among first-degree relatives, significantly increases the risk of bipolar disorder. While no single gene causes the condition, multiple genetic variants interact with environmental factors to influence susceptibility.
Rationale for correct answer
1. This statement reflects an understanding of hereditary risk and the client’s thoughtful consideration of genetic transmission. It shows insight into the biological basis of bipolar disorder and responsible decision-making.
Rationale for incorrect answers
2. Negative thoughts are more aligned with cognitive theories of mood disorders. While they may exacerbate symptoms, they do not explain the biological etiology of bipolar disorder.
3. Blaming a parent reflects misunderstanding of genetic predisposition. Biological theory emphasizes inherited risk, not fault or intentional transmission.
4. Learning through family interactions aligns with behavioral or social learning theories. It does not demonstrate understanding of the biological mechanisms underlying bipolar disorder.
Take Home Points
- Biological theory attributes bipolar disorder to genetic, neurochemical, and structural brain factors.
- Family history increases risk but does not imply blame or certainty of inheritance.
- Cognitive and behavioral models explain symptom maintenance, not biological origin.
- Educating clients on genetic risk supports informed decisions and reduces stigma.
A nurse working with a client diagnosed with bipolar I disorder attempts to recognize the motivation behind the client’s use of grandiosity. Which is the rationale for this nurse’s action?
Explanation
Grandiosity in bipolar I disorder is a symptom of mania, characterized by inflated self-esteem, unrealistic beliefs about abilities, and impaired insight. It often serves as a psychological defense against feelings of vulnerability, shame, or inadequacy. Understanding the underlying emotional drivers of grandiosity allows clinicians to approach the client with empathy and therapeutic intent, rather than reacting to the surface-level behavior. This insight fosters rapport and supports individualized care planning.
Rationale for correct answer
1. Recognizing the emotional motivation behind grandiosity helps the nurse separate the client’s identity from symptomatic behavior. This promotes therapeutic alliance and allows for compassionate, nonjudgmental engagement.
Rationale for incorrect answers
2. While accountability is important, insisting on responsibility before understanding the behavior may hinder rapport. Insight and change often follow empathetic exploration, not confrontation.
3. Increasing self-esteem may reduce manipulative behaviors, but this statement oversimplifies the complex psychological function of grandiosity. It does not address the nurse’s role in understanding motivation.
4. Reinforcement strategies are useful in behavior modification but do not directly address the emotional or cognitive roots of grandiosity. This approach is more applicable to structured behavioral interventions.
Take Home Points
- Grandiosity in mania often masks underlying emotional vulnerability and impaired insight.
- Understanding the motivation behind symptoms fosters therapeutic connection and individualized care.
- Accountability and behavior change follow empathetic engagement, not precede it.
- Behavioral strategies alone may not address the psychological drivers of manic symptoms.
A nursing instructor is teaching about the psychosocial theory related to the development of bipolar disorder. Which student statement would indicate that learning has occurred?
Explanation
Psychosocial theory of bipolar disorder suggests that environmental stressors, early life experiences, and interpersonal dynamics interact with biological vulnerabilities to influence the onset and course of the illness. Factors such as trauma, disrupted attachment, and maladaptive coping mechanisms may shape emotional regulation and behavioral responses. While genetic and neurochemical components are central, psychosocial influences contribute to symptom expression, relapse risk, and treatment outcomes. The theory supports a multifactorial model of etiology.
Rationale for correct answer
4. This statement reflects an accurate understanding of the multidimensional nature of bipolar disorder. It acknowledges both biological and psychosocial contributions, aligning with current integrative models of psychiatric illness.
Rationale for incorrect answers
1. While psychosocial theories offer valuable insights, their credibility has not necessarily “strengthened” in isolation. Modern understanding favors integrative models rather than elevating psychosocial theory alone.
2. Describing bipolar disorder as purely genetic oversimplifies its etiology. Although heritability is high, environmental and psychological factors significantly influence onset and progression.
3. Manic episodes following substance use reflect substance/medication-induced mood disorders, not psychosocial theory. This explanation aligns more with pharmacologic or biological models.
Take Home Points
- Bipolar disorder arises from a complex interplay of genetic, neurochemical, and psychosocial factors.
- Psychosocial theory emphasizes environmental stressors, early experiences, and interpersonal influences.
- Substance-induced mania is classified separately from primary bipolar disorder.
- Integrative models best explain the multifactorial etiology of mood disorders.
Which statement about the development of bipolar disorder is from a biochemical perspective?
Explanation
Biochemical perspective of bipolar disorder focuses on cellular and molecular abnormalities, particularly involving electrolyte regulation, neurotransmitter dynamics, and intracellular signaling. Research has shown that individuals with bipolar disorder may exhibit altered ion channel function, leading to elevated intracellular calcium and sodium levels. These disruptions affect neuronal excitability, synaptic transmission, and mood regulation. Lithium and other mood stabilizers target these pathways, further supporting the biochemical basis of the disorder.
Rationale for correct answer
2. This statement reflects a core biochemical mechanism in bipolar disorder—altered ion transport across cell membranes. Elevated intracellular calcium and sodium disrupt neuronal signaling and mood stability, consistent with biochemical pathogenesis.
Rationale for incorrect answers
1. Family studies demonstrate genetic risk, not biochemical changes. While heritability is important, this statement aligns with genetic theory rather than biochemical mechanisms.
3. MRI findings indicate structural brain changes, such as ventricular enlargement and white matter abnormalities. These support neuroanatomical theories, not biochemical ones.
4. Twin studies highlight genetic concordance, showing heritable patterns of bipolar disorder. This evidence supports genetic predisposition, not biochemical dysfunction.
Take Home Points
- Biochemical theory emphasizes ion dysregulation, neurotransmitter imbalance, and intracellular signaling abnormalities.
- Elevated intracellular calcium and sodium are linked to mood instability in bipolar disorder.
- Genetic and neuroanatomical findings support other etiological models but are distinct from biochemical theory.
- Understanding biochemical mechanisms informs pharmacologic treatment strategies like mood stabilizers.
The brother of a client admitted to the hospital in an acute manic phase questions the nurse about why the psychiatrist would discuss electroconvulsive therapy (ECT) as a potential treatment modality with the family. Which response best answers the family member’s question?
Explanation
Electroconvulsive therapy (ECT) is a somatic treatment modality used in severe psychiatric conditions, including bipolar disorder, particularly when symptoms are refractory to pharmacologic interventions. ECT induces controlled seizures under anesthesia, leading to neurochemical changes that can rapidly stabilize mood. It is especially considered in cases of acute mania, severe depression, or catatonia when medications are ineffective, contraindicated, or poorly tolerated. ECT has demonstrated efficacy in reducing manic symptoms and improving functional outcomes in treatment-resistant cases.
Rationale for correct answer
2. ECT is indicated when clients with bipolar disorder cannot tolerate or fail to respond to mood stabilizers or antipsychotics. It offers a rapid and effective alternative for symptom control, especially in acute manic phases or life-threatening presentations.
Rationale for incorrect answers
1. ECT is not primarily used to prevent depressive episodes. While it can treat bipolar depression, its role is therapeutic rather than prophylactic. Preventive strategies typically involve long-term pharmacologic maintenance.
3. ECT may be used in schizophrenia, but chronic undifferentiated schizophrenia is not a common dual indication with bipolar disorder. This statement inaccurately generalizes ECT use across unrelated diagnoses.
4. Disordered eating is not a primary indication for ECT. While mania may involve poor impulse control, ECT is reserved for severe mood symptoms, not behavioral patterns like eating disturbances.
Take Home Points
- ECT is a safe and effective option for bipolar disorder when medications are ineffective or poorly tolerated.
- It is used to treat acute manic or depressive episodes, not to prevent future mood cycles.
- ECT is not indicated for behavioral symptoms like disordered eating unless tied to severe mood dysregulation.
- Understanding ECT’s role helps families support informed treatment decisions during acute psychiatric episodes.
A nursing assistant comments to the nurse about a recently admitted client. “I think the new admission is just faking being sick. Yesterday we couldn’t get a word out of the client and today the client is talking nonstop.” Which response by the nurse is most appropriate in reflecting empathy for the client?
Explanation
Rapid-cycle bipolar disorder is a subtype of bipolar disorder characterized by frequent mood shifts, including episodes of mania, hypomania, and depression occurring four or more times within a 12-month period. These fluctuations can happen over days or even hours, making the clinical presentation appear inconsistent or confusing to observers. The rapid transitions are not under voluntary control and reflect underlying neurochemical dysregulation, not manipulation or attention-seeking behavior. Empathetic responses from healthcare staff are essential to reduce stigma and support therapeutic engagement.
Rationale for correct answer
3. This response educates the assistant about the clinical nature of rapid mood changes in bipolar disorder. It reflects empathy by validating the client’s experience and reframing the behavior as part of a legitimate psychiatric condition.
Rationale for incorrect answers
1. Suggesting the client is seeking attention reinforces stigma and dismisses the seriousness of the illness. It lacks empathy and undermines the therapeutic environment.
2. While promoting respectful language is important, this response does not address the misunderstanding about the client’s behavior or provide insight into the condition.
4. Saying the client has the “right” to be difficult to assess is vague and non-informative. It neither educates nor fosters empathy, and may confuse the assistant further.
Take Home Points
- Rapid cycling bipolar disorder involves frequent, unpredictable mood shifts that may appear inconsistent to others.
- Educating staff about psychiatric conditions fosters empathy and reduces stigma.
- Dismissing symptoms as attention-seeking undermines therapeutic care and client dignity.
- Clear, informative responses help staff understand and support clients with complex mental health needs.
Practice Exercise 3
The emergency department (ED) is calling to report on a patient who will be admitted to your acute psychiatric unit. He has a history of bipolar disorder and was in an altercation that resulted in the death of another. He has contusions, abrasions, and minor lacerations. What is the priority question that you should ask?
Explanation
Acute mania in bipolar disorder can present with extreme agitation, impulsivity, and poor judgment, often escalating to aggressive or dangerous behavior. When admitting a client with recent violent involvement, the priority is to assess current mental status, including mood, behavior, and risk factors such as psychosis, suicidality, or homicidality. This guides immediate safety planning, medication needs, and level of observation. Physical injuries are secondary to psychiatric stabilization in this context, especially when the client is medically cleared.
Rationale for correct answer
4. Determining the client’s current mood and behavioral presentation is essential for psychiatric triage. It informs risk assessment, safety measures, and initial treatment planning, especially in the context of recent violence and bipolar history.
Rationale for incorrect answers
1. While transfer timing is operationally relevant, it does not address clinical urgency. Psychiatric units must first prepare for the client’s behavioral presentation and safety needs.
2. Police presence may be necessary depending on legal status, but asking this first overlooks clinical priorities. Risk assessment should precede logistical or custodial concerns.
3. The client’s physical injuries are minor and medically cleared, making psychiatric admission appropriate. Questioning trauma unit placement diverts focus from psychiatric stabilization.
Take Home Points
- Psychiatric triage prioritizes mental status and behavioral risk over logistical or custodial details.
- Acute mania may involve aggression, requiring immediate assessment of mood and safety risk.
- Physical injuries are managed medically before psychiatric admission; they do not override psychiatric needs.
- Understanding current behavior guides observation level, medication initiation, and staff safety planning.
A client who is in a manic phase of bipolar disorder threatens staff and clients on an acute psychiatric unit. Place the following interventions in priority order from the least restrictive to the most restrictive.
Explanation
Manic phase of bipolar disorder is marked by elevated mood, impulsivity, and agitation, which can escalate into threatening or aggressive behavior. Management follows a least-to-most restrictive approach to preserve autonomy while ensuring safety. Initial strategies focus on redirecting energy and setting boundaries. If these fail, pharmacologic intervention is used to reduce symptoms. Physical containment measures like seclusion and restraints are reserved for imminent risk when other interventions are ineffective.
Rationale for answer
4. Diversional activities are the least restrictive and aim to redirect excess energy into safe, structured outlets. They help reduce agitation and promote engagement without limiting freedom.
3. Limit setting involves establishing behavioral boundaries and expectations. It maintains safety while preserving the client’s autonomy and is essential in early behavioral de-escalation.
5. Medication administration is more restrictive as it involves pharmacologic intervention to manage symptoms. It is used when behavioral strategies are insufficient to control agitation or risk.
1. Seclusion removes the client from the environment to prevent harm. It is restrictive and used only when the client poses a danger to others and cannot be managed through verbal or pharmacologic means.
2. Restraints are the most restrictive, involving physical containment. They are used as a last resort when all other measures fail and there is an immediate threat to safety.
Take Home Points
- Managing mania requires a stepwise approach from behavioral redirection to physical containment.
- Diversional activities and limit setting preserve autonomy and reduce escalation.
- Medications are used when non-pharmacologic strategies fail to control symptoms.
- Seclusion and restraints are reserved for imminent risk and must follow strict legal and ethical protocols.
A provocatively dressed client diagnosed with bipolar I disorder is observed laughing loudly with peers in the milieu. Which nursing action is a priority in this situation?
Explanation
Milieu management in bipolar I disorder, particularly during manic episodes, focuses on maintaining safety, reducing stimulation, and promoting structured engagement. Clients in mania often display disinhibited behavior, excessive socialization, and poor boundaries. Provocative dress and loud laughter may reflect elevated mood and impaired judgment. The priority is to redirect the group to minimize reinforcement of inappropriate behavior and prevent escalation. Structured activities help channel energy and support behavioral containment without confrontation or pharmacologic intervention.
Rationale for correct answer
2. Redirecting to structured activities reduces environmental stimulation and reinforces appropriate social behavior. It protects the therapeutic milieu and helps manage manic symptoms through non-pharmacologic means.
Rationale for incorrect answers
1. Joining the milieu may increase attention to the behavior and inadvertently reinforce it. It does not address the need for behavioral redirection or environmental control.
3. Discussing dress privately may be appropriate later, but it does not address the immediate behavioral disruption. Priority lies in managing group dynamics and preventing escalation.
4. Administering PRN medication without first attempting behavioral interventions bypasses least-restrictive strategies. Medication is reserved for when redirection fails or risk escalates.
Take Home Points
- Structured activities are effective in managing manic behavior and preserving milieu safety.
- Behavioral redirection should precede medication in managing disinhibition and hyperactivity.
- Confrontation or attention may reinforce manic behaviors and disrupt group dynamics.
- Milieu therapy emphasizes environmental control and therapeutic engagement over immediate pharmacologic intervention.
A client diagnosed with bipolar I disorder has a nursing diagnosis of disturbed thought process related to biochemical alterations. Based on this diagnosis, which outcome would be appropriate?
Explanation
Disturbed thought process in bipolar I disorder is often linked to biochemical alterations affecting neurotransmitter systems such as dopamine, serotonin, and norepinephrine. During manic episodes, clients may experience delusions, flight of ideas, and impaired reality testing. These cognitive disruptions stem from neurochemical dysregulation and can be severe enough to interfere with judgment, perception, and social functioning. Treatment aims to restore neurochemical balance and improve insight, making reality orientation a central therapeutic goal.
Rationale for correct answer
4. The ability to distinguish reality from delusions directly addresses the disturbed thought process. It reflects improvement in cognitive clarity and insight, aligning with the biochemical basis of the diagnosis and expected therapeutic outcomes.
Rationale for incorrect answers
1. Preventing injury is a safety goal, not a cognitive one. While important, it does not specifically target the disturbed thought process or reflect progress in reality testing.
2. Appropriate interaction is a behavioral goal that may improve with cognitive clarity, but it does not directly measure resolution of delusional thinking or thought disturbance.
3. Medication compliance supports treatment but is a behavioral outcome. It does not confirm cognitive improvement or resolution of disturbed thought processes.
Take Home Points
- Disturbed thought process in bipolar I disorder involves impaired reality testing and delusional thinking.
- Neurochemical dysregulation underlies cognitive symptoms and guides pharmacologic intervention.
- Outcomes should reflect cognitive improvement, such as distinguishing reality from delusions.
- Behavioral goals like safety and compliance are supportive but not primary indicators of thought process resolution.
A client diagnosed with bipolar I disorder and experiencing a manic episode is newly admitted to the in-patient psychiatric unit. Which nursing diagnosis is a priority at this time?
Explanation
Bipolar I disorder is a chronic psychiatric condition marked by alternating episodes of mania and depression. During manic phases, clients exhibit elevated mood, hyperactivity, grandiosity, and poor impulse control. These episodes often impair judgment and increase risk-taking behaviors, including aggression, self-harm, and harm to others. The manic state may also include psychotic features such as hallucinations or delusions, but the most immediate concern is safety—especially when disinhibition and impulsivity escalate to violent behavior.
Rationale for correct answer
1. During acute mania, impulsivity and poor judgment heighten the risk of aggressive outbursts toward others. The client may misinterpret interactions or act on grandiose beliefs, making violence a priority concern for nursing safety interventions.
Rationale for incorrect answers
2. Although hallucinations may occur in manic episodes, they are not the most immediate threat unless they directly provoke harmful behavior. The priority is safety, not perceptual disturbances.
3. Manic clients are typically hyper-social and intrusive, not withdrawn. Isolation is more characteristic of depressive phases, making this diagnosis less relevant during acute mania.
4. Feelings of guilt and low self-esteem are more prominent in depressive episodes. During mania, clients often display inflated self-worth and lack insight into inappropriate behaviors.
Take Home Points
- In acute mania, safety risks due to impulsivity and aggression take precedence over other psychosocial concerns.
- Bipolar I disorder includes manic episodes that may escalate to psychosis or violence, requiring close monitoring.
- Differentiating manic symptoms from depressive or psychotic features is essential for accurate nursing diagnosis.
- Nursing priorities shift with phase of illness—mania demands safety-focused interventions, while depression may focus on mood and cognition.
Beldine, age 68, is diagnosed with bipolar I disorder, current episode manic. She is extremely hyperactive and has lost weight. One way to promote adequate nutritional intake for Beldine is to:
Explanation
Manic episodes in bipolar I disorder are marked by elevated mood, hyperactivity, and reduced need for sleep, often leading to poor nutritional intake and weight loss. Clients may be too distracted or restless to sit for meals, and their impulsivity can interfere with structured routines. Nutritional strategies must accommodate their erratic behavior while ensuring caloric sufficiency. High-calorie, nutrient-dense finger foods are ideal because they can be consumed quickly and frequently, even during periods of excessive movement or agitation.
Rationale for correct answer
3. Providing finger foods allows Beldine to maintain her hyperactive behavior while still consuming calories. These foods are portable, easy to eat, and can be offered frequently, supporting nutritional intake without requiring her to sit still.
Rationale for incorrect answers
1. Sitting with Beldine may not be effective due to her restlessness. She may resist structured meal times or leave the table prematurely, making this approach impractical during a manic phase.
2. While familiar foods may be comforting, relying on a family member to bring meals does not address the need for accessibility and caloric density. It also lacks consistency and clinical oversight.
4. Room restriction is punitive and may escalate agitation or noncompliance. It does not address the underlying issue of poor intake and may worsen behavioral symptoms during mania.
Take Home Points
- Clients in manic episodes often require flexible, high-calorie nutrition strategies due to hyperactivity and distractibility.
- Finger foods and snacks are more effective than structured meals for promoting intake during mania.
- Punitive measures like room restriction are contraindicated and may exacerbate agitation or noncompliance.
- Nutritional interventions should be tailored to behavioral presentation, especially in psychiatric conditions with fluctuating energy and attention.
Margaret, a 68-year-old widow, is brought to the emergency department by her sister-in-law. Margaret has a history of bipolar disorder and has been maintained on medication for many years. Her sister-in-law reports that Margaret quit taking her medication a few months ago, thinking she did not need it anymore. She is agitated, pacing, demanding, and speaking very loudly. Her sister-in-law reports that Margaret eats very little, is losing weight, and almost never sleeps. “I am afraid she is going to just collapse!” Margaret is admitted to the psychiatric unit. The priority nursing diagnosis for Margaret is:
Explanation
Manic episodes in bipolar I disorder are characterized by elevated mood, hyperactivity, and impaired judgment, often resulting in risk-taking behaviors and physical exhaustion. Clients may exhibit pressured speech, pacing, and agitation, which significantly increase the risk of injury due to falls, collisions, or physical depletion. The priority in acute mania is to ensure safety, as the combination of psychomotor agitation and poor insight can lead to accidental harm or collapse from exhaustion. Nutritional and sleep deficits are important but secondary to immediate physical risk.
Rationale for correct answer
2. Margaret’s extreme hyperactivity and agitation place her at high risk for physical harm. Her inability to rest, combined with poor nutritional intake, increases the likelihood of injury from collapse, falls, or overexertion.
Rationale for incorrect answers
1. While Margaret’s poor intake is concerning, nutrition is not the most immediate threat. The physical consequences of hyperactivity, such as collapse or injury, take precedence in acute care.
3. Sleep disturbance is a hallmark of mania, but agitation and hyperactivity pose more immediate safety risks. Sleep can be addressed once Margaret is stabilized and safe.
4. Denial of illness is common in bipolar disorder, but coping strategies are not the priority during acute manic episodes. Immediate physiological safety concerns override psychosocial considerations.
Take Home Points
- In acute mania, physical safety risks due to hyperactivity and exhaustion are the top nursing priority.
- Nutritional and sleep deficits are important but secondary to injury prevention during manic episodes.
- Bipolar clients often lack insight into their condition, requiring structured interventions to ensure safety.
- Nursing diagnoses must prioritize physiological needs first, especially when behaviors threaten immediate harm.
A client diagnosed with bipolar disorder is in an acute manic state. The nursing staff is unable to verbally de-escalate the situation, and a physician orders a stat dose of aripiprazole (Abilify®) intramuscularly. Which client behavior indicates that the medication has been effective?
Explanation
Aripiprazole is a second-generation antipsychotic used in the management of acute mania in bipolar I disorder. It acts as a partial agonist at dopamine D2 and serotonin 5-HT1A receptors, and antagonist at 5-HT2A receptors. Its pharmacologic profile allows it to stabilize mood and reduce excitability without excessive sedation. When administered intramuscularly in acute settings, it rapidly targets agitation and hyperactivity, making it suitable for de-escalation. Unlike sedatives, its goal is behavioral control rather than sedation, and it does not immediately equalize mood swings.
Rationale for correct answer
2. Aripiprazole’s primary effect in acute mania is reducing excitability and agitation. Its dopaminergic modulation calms hyperactive behavior without causing oversedation, allowing for safer interaction and stabilization.
Rationale for incorrect answers
1. Sedation is not the therapeutic goal of aripiprazole. While some calming may occur, excessive sedation suggests overmedication or use of a different pharmacologic class like benzodiazepines.
3. Although aripiprazole can reduce psychotic symptoms over time, its immediate IM use in acute mania targets agitation and excitability first. Psychotic symptom relief is not the primary indicator of short-term effectiveness.
4. Mood stabilization is a long-term goal in bipolar management. Acute IM administration does not equalize mood swings immediately; it primarily addresses behavioral dysregulation.
Take Home Points
- Aripiprazole IM is used for rapid control of agitation and excitability in acute manic episodes.
- Sedation is not the intended outcome; behavioral calming without oversedation is preferred.
- Psychotic symptom relief and mood stabilization are longer-term therapeutic goals.
- In acute psychiatric emergencies, medication effectiveness is judged by reduction in dangerous or disruptive behaviors.
Comprehensive Questions
A client is admitted to the facility in the manic phase of bipolar disorder. When placing a diet order for the client, which foods are most appropriate?
Explanation
Manic phase of bipolar disorder is marked by elevated mood, hyperactivity, and distractibility, often leading to poor nutritional intake. Clients may be unable to sit through full meals, making finger foods essential for maintaining caloric intake. Nutritional strategies must accommodate erratic behavior and ensure energy-dense, portable options that can be consumed quickly. Foods should be easy to handle, require minimal utensils, and be appealing enough to encourage spontaneous eating during periods of agitation or pacing.
Rationale for correct answer
2. This option provides nutritious, high-calorie finger foods that can be eaten while moving. The sandwich, carrot sticks, grapes, and cookies are portable and require no utensils, supporting adequate intake during hyperactivity.
Rationale for incorrect answers
1. Soup and peaches require utensils and sitting still, which is impractical during manic episodes. The liquid nature of soup also increases spill risk and may discourage consumption.
3. Roast chicken and mashed potatoes are difficult to eat without sitting and using utensils. These foods are less suitable for clients who are pacing or unable to focus on structured meals.
4. Although the tuna sandwich is portable, the ice cream and apple require more effort to consume and may not be appealing or practical during periods of agitation and distractibility.
Take Home Points
- Clients in manic states benefit from high-calorie, portable finger foods that accommodate hyperactivity and distractibility.
- Structured meals requiring utensils are often ineffective during acute mania.
- Nutritional interventions must prioritize accessibility and caloric density to prevent weight loss and exhaustion.
- Food choices should be tailored to behavioral presentation, not just nutritional value.
Margaret, a 68-year-old widow experiencing a manic episode, is admitted to the psychiatric unit after being brought to the emergency department by her sister-in-law. Margaret yells, “My sister-in-law is just jealous of me! She is trying to make it look like I am insane!” This behavior is an example of:
Explanation
Delusions are fixed, false beliefs that persist despite evidence to the contrary and are common in manic episodes of bipolar I disorder. These beliefs often reflect the client’s distorted interpretation of reality, driven by heightened dopaminergic activity and impaired insight. Among the various types, persecutory delusions involve the belief that one is being targeted, harmed, or conspired against. These are especially prevalent during manic states when grandiosity and paranoia co-occur, often escalating agitation and mistrust toward others.
Rationale for correct answer
2. Margaret’s belief that her sister-in-law is trying to make her “look insane” reflects a classic persecutory delusion. She perceives intentional harm or sabotage, which is a hallmark of paranoia in manic psychosis.
Rationale for incorrect answers
1. Delusions of grandeur involve inflated self-worth or identity, such as believing one is famous or has special powers. Margaret’s statement does not reflect exaggerated self-importance but rather suspicion of others.
3. Delusions of reference involve interpreting neutral events as having personal meaning, such as believing TV shows are sending messages. Margaret’s accusation is directed at a person, not an external event.
4. Delusions of control involve the belief that one’s thoughts or actions are being manipulated by external forces. Margaret’s statement does not suggest external control over her behavior or thoughts.
Take Home Points
- Persecutory delusions are common in manic episodes and involve beliefs of being targeted or harmed.
- Delusions of grandeur reflect inflated self-concept, not suspicion of others.
- Referential delusions misinterpret neutral events as personally significant.
- Delusions of control involve perceived manipulation of thoughts or actions by external forces.
The nurse observes that a client with bipolar disorder is pacing in the hall, talking loudly and rapidly, and using elaborate hand gestures. The nurse concludes that the client is demonstrating which of the following?
Explanation
Psychomotor agitation is a behavioral manifestation of mental tension and internal restlessness, often seen in mood disorders like bipolar I disorder. It involves excessive, purposeless motor activity such as pacing, rapid speech, and exaggerated gestures. These movements are not goal-directed but serve as an outlet for emotional dysregulation. In manic episodes, psychomotor agitation reflects heightened arousal and poor impulse control, and may escalate to aggression if not addressed. It differs from anxiety or anger by its physical intensity and lack of clear emotional focus.
Rationale for correct answer
4. The client’s pacing, loud rapid speech, and elaborate gestures are hallmark signs of psychomotor agitation. These behaviors reflect restlessness and internal tension, commonly seen in manic phases of bipolar disorder.
Rationale for incorrect answers
1. Aggression involves intent to harm or confront others. The client’s behavior lacks hostility or directed threat, making this an inaccurate interpretation.
2. Anger is an emotional state often accompanied by verbal or physical aggression. The client’s actions are more consistent with restlessness than emotional expression.
3. Anxiety may cause restlessness, but psychomotor agitation is more intense and physically expressive. The client’s symptoms exceed typical anxious behavior.
Take Home Points
- Psychomotor agitation involves purposeless, excessive motor activity driven by internal tension.
- It is commonly seen in manic episodes of bipolar disorder and requires early intervention to prevent escalation.
- Differentiating agitation from aggression or anxiety is critical for accurate nursing assessment.
- Behavioral signs like pacing, rapid speech, and exaggerated gestures are key indicators of psychomotor agitation.
A major principle the nurse should observe when communicating with a patient experiencing elated mood is to:
Explanation
Elated mood in bipolar disorder, particularly during manic episodes, is marked by euphoria, distractibility, and pressured speech. Clients may exhibit flight of ideas, grandiosity, and reduced attention span, making it difficult to process complex or abstract information. Effective communication must be grounded in clarity, structure, and emotional containment. A calm, firm approach helps establish boundaries, reduce overstimulation, and maintain therapeutic rapport without escalating the client’s mood or behavior.
Rationale for correct answer
1. A calm, firm approach provides structure and containment, which are essential during manic episodes. It helps reduce overstimulation and maintains safety while preserving therapeutic engagement.
Rationale for incorrect answers
2. Expanded explanations overwhelm the client’s limited attention span during mania. They may increase confusion or trigger tangential thinking, making communication ineffective.
3. Abstract concepts are poorly processed during manic states due to cognitive disorganization. Concrete, simple language is more appropriate for maintaining clarity.
4. Lightheartedness and joking may reinforce grandiosity or escalate manic behavior. It undermines the seriousness of the situation and may compromise therapeutic boundaries.
Take Home Points
- Communication with manic clients should be calm, firm, and structured to reduce overstimulation.
- Avoid abstract or complex explanations; use simple, direct language.
- Humor and lightness may escalate symptoms and should be used cautiously.
- Therapeutic boundaries are essential to maintain safety and emotional regulation during elated mood states.
Nadia has been diagnosed with bipolar disorder. Which is an outcome for Nadia in the continuation of treatment phase of bipolar disorder?
Explanation
Continuation phase of bipolar disorder treatment follows acute symptom stabilization and focuses on relapse prevention, medication adherence, and psychosocial recovery. This phase typically spans 4 to 9 months and aims to consolidate gains made during the acute phase. The most critical goal is ensuring adherence to pharmacologic therapy, as discontinuation is a major predictor of relapse. Psychosocial education, monitoring for side effects, and gradual reintegration into daily routines are emphasized. Mood stabilization—not euphoria—is the therapeutic target, and weight management is monitored but not prioritized over psychiatric stability.
Rationale for correct answer
2. Adherence to the medication regimen is the cornerstone of the continuation phase. It prevents recurrence of mood episodes and supports long-term stability, making it the most appropriate outcome for this phase.
Rationale for incorrect answers
1. Avoiding self-help groups contradicts supportive care principles. Peer support enhances coping and reduces isolation, especially during recovery phases.
3. Euphoric mood is a symptom of mania, not a desired outcome. The goal is mood stabilization, not emotional elevation, which may signal relapse.
4. While maintaining weight is beneficial, it is not the primary objective in the continuation phase. Psychiatric stability and medication adherence take precedence.
Take Home Points
- The continuation phase focuses on preventing relapse and reinforcing medication adherence.
- Mood stabilization—not emotional highs—is the therapeutic goal in bipolar disorder.
- Support groups and psychosocial interventions enhance recovery and reduce isolation.
- Physical health monitoring is important but secondary to psychiatric stabilization during continuation treatment.
A client diagnosed with bipolar disorder has a nursing diagnosis of sleep pattern disturbance. Which intervention should the nurse implement initially?
Explanation
Sleep pattern disturbance in bipolar disorder is often linked to manic episodes, where clients experience reduced need for sleep, hyperactivity, and racing thoughts. Sleep disruption can exacerbate mood instability and impair recovery. Before implementing behavioral or environmental interventions, the nurse must first assess the client’s baseline sleep habits, triggers, and patterns. This foundational data guides individualized care planning and helps differentiate between chronic sleep issues and those specific to the current mood phase.
Rationale for correct answer
1. Assessing normal sleep patterns is the initial step in managing sleep disturbances. It provides essential data for tailoring interventions and identifying whether the disturbance is episodic or chronic, linked to mania or other factors.
Rationale for incorrect answers
2. Discouraging daytime naps may be appropriate later, but without understanding the client’s baseline, it risks worsening fatigue or agitation. Assessment must precede behavioral modification.
3. While caffeine and nicotine can impair sleep, this intervention is secondary. It assumes causality without first evaluating the client’s specific sleep behaviors and contributing factors.
4. Relaxation exercises are useful but not the first step. Without assessment, they may be mismatched to the client’s needs or ineffective due to manic energy levels.
Take Home Points
- Initial nursing interventions must begin with assessment to guide individualized care.
- Sleep disturbances in bipolar disorder often reflect underlying mood phase and require tailored strategies.
- Behavioral modifications like nap restriction or relaxation are secondary to understanding baseline patterns.
- Accurate assessment informs safe and effective sleep management in psychiatric care.
The nurse is reviewing expected outcomes for a client diagnosed with bipolar I disorder. Number the outcomes presented in the order in which the nurse would address them.
Explanation
Bipolar I disorder is a chronic psychiatric condition marked by alternating episodes of mania, depression, and periods of euthymia. Manic phases often present with impulsivity, poor judgment, and psychomotor agitation, increasing risk for injury and nutritional neglect. Prioritization of care must follow physiological stabilization before psychosocial rehabilitation.
Rationale for correct order
1. During acute mania, the client is at high risk for injury due to hyperactivity, poor impulse control, and impaired judgment. Immediate safety is the nurse’s top priority, aligning with physiological needs.
2. Nutritional intake is often compromised in manic states due to distractibility and hyperactivity. Finger foods support autonomy and minimize disruption, promoting caloric intake and hydration.
4. Once stabilized physically, the client can begin to engage in insight-oriented interventions. Accepting responsibility reflects progress in cognitive integration and readiness for therapeutic work.
3. Accessing outpatient resources is a long-term goal requiring insight, motivation, and stability. It is addressed after acute symptoms subside and the client demonstrates readiness for discharge planning.
Take Home Points
- Bipolar I disorder requires prioritization of physiological safety before psychosocial goals.
- Acute mania increases risk for injury and nutritional neglect due to hyperactivity and poor judgment.
- Insight and responsibility are addressed only after stabilization of physical and behavioral symptoms.
- Discharge planning and outpatient resource access are long-term goals contingent on clinical improvement.
A client diagnosed with bipolar II disorder has a nursing diagnosis of impaired social interactions related to egocentrism. Which short-term outcome is an appropriate expectation for this client problem?
Explanation
Bipolar II disorder is characterized by recurrent depressive episodes and at least one episode of hypomania, which is less severe than mania. Clients often experience egocentrism, social withdrawal, and impaired interpersonal functioning during depressive phases. Short-term goals must reflect realistic, measurable progress toward social engagement, beginning with internal motivation before observable behavior.
Rationale for correct answer
3. Verbalizing a desire to interact reflects emerging insight and motivation, which are foundational for behavioral change. It is a realistic short-term goal for someone with impaired social functioning due to egocentrism.
Rationale for incorrect answers
1. One-on-one interaction requires initiative, emotional regulation, and social reciprocity, which may be premature for a client still struggling with egocentrism and impaired interpersonal skills.
2. Exchanging personal information implies a level of trust and social comfort that is typically achieved in later stages of therapeutic progress, not within early short-term goals.
4. Initiating a social relationship demands judgment and sustained interpersonal effort, which exceeds the scope of a short-term outcome for a client with impaired social interaction.
Take Home Points
- Bipolar II disorder often presents with egocentrism and social withdrawal during depressive episodes.
- Short-term goals should focus on internal motivation before expecting observable social behaviors.
- Verbalizing desire to interact is a realistic and measurable early outcome.
A client diagnosed with bipolar I disorder in the manic phase is yelling at another peer in the milieu. Which nursing intervention takes priority?
Explanation
Bipolar I disorder in the manic phase presents with elevated mood, agitation, and impaired impulse control, often resulting in disruptive or aggressive behavior. Clients may exhibit poor judgment, pressured speech, and hyperactivity, which can escalate quickly in stimulating environments. Immediate nursing interventions must prioritize safety and de-escalation using the least restrictive measures first.
Rationale for correct answer
1. Calmly redirecting and removing the client from the milieu is the most appropriate initial response. It uses verbal de-escalation and environmental control to reduce stimulation and prevent escalation, aligning with least restrictive intervention principles.
Rationale for incorrect answers
2. Administering a PRN intramuscular injection is a chemical restraint, appropriate only after non-invasive methods fail. It is not the first-line intervention unless the client poses imminent danger.
3. Telling the client to lower their voice may provoke defensiveness or escalate agitation. It lacks therapeutic engagement and does not address the underlying behavioral dysregulation.
4. Seclusion is a restrictive intervention requiring justification and physician order. It is reserved for situations where the client poses a threat and other strategies have failed.
Take Home Points
- Manic episodes in bipolar I disorder often involve agitation, impulsivity, and poor judgment.
- Least restrictive interventions like verbal redirection and environmental modification are prioritized.
- Chemical and physical restraints are used only when safety is compromised and other methods fail.
- Effective nursing care requires rapid assessment and therapeutic communication to prevent escalation.
A client newly admitted with bipolar I disorder has a nursing diagnosis of risk for injury related to extreme hyperactivity. Which nursing intervention is appropriate?
Explanation
Bipolar I disorder during manic episodes presents with elevated mood, hyperactivity, and impaired judgment, often leading to risk-taking behaviors and physical exhaustion. Clients may exhibit distractibility, impulsivity, and psychomotor agitation, which significantly increase the risk for injury. Immediate interventions must target physiological stabilization and behavioral containment using pharmacologic and environmental strategies.
Rationale for correct answer
2. PRN antipsychotic medications help reduce agitation and stabilize mood by modulating dopamine activity. They are appropriate for acute symptom control when hyperactivity poses a risk for injury and non-pharmacologic methods are insufficient.
Rationale for incorrect answers
1. Placing the client with another symptomatic peer increases stimulation and risk of behavioral escalation. It compromises safety and violates principles of environmental control in psychiatric care.
3. Discussing consequences requires insight, which is impaired during acute mania. The client may be unable to process or retain such information, making this intervention ineffective in the short term.
4. Reinforcing coping skills assumes cognition and emotional regulation, which are compromised during manic episodes. The client is unlikely to engage meaningfully with learned strategies until stabilized.
Take Home Points
- Bipolar I disorder with hyperactivity requires immediate pharmacologic intervention to reduce risk of injury.
- Antipsychotics are effective in managing acute agitation and restoring behavioral control.
- Environmental stimulation must be minimized to prevent escalation of manic symptoms.
- Insight-based and cognitive interventions are deferred until the client achieves symptom stabilization.
A client diagnosed with bipolar I disorder experienced an acute manic episode and was admitted to the in-patient psychiatric unit. The client is now ready for discharge. Which of the following resource services should be included in discharge teaching? Select all that apply.
Explanation
Bipolar I disorder is a chronic psychiatric illness marked by alternating episodes of mania, depression, and periods of remission. Discharge planning must address both symptom management and psychosocial reintegration. Clients often face challenges in medication adherence, interpersonal relationships, and functional stability. A comprehensive support system is essential to reduce relapse risk and promote long-term recovery.
Rationale for correct answers
1. Financial and legal assistance supports clients with impaired judgment during manic episodes, which may result in debt, legal issues, or loss of employment. These services help stabilize external stressors that can trigger relapse.
2. Crisis hotlines provide immediate support during emotional distress or symptom recurrence. They are vital for early intervention and suicide prevention, especially during post-discharge adjustment.
3. Individual psychotherapy facilitates insight development, emotional regulation, and adherence to treatment plans. It is a cornerstone of long-term management for bipolar I disorder.
4. Support groups offer peer-based validation and shared coping strategies. They reduce isolation and promote accountability for treatment adherence and lifestyle adjustments.
5. Family education groups enhance understanding of the disorder, improve communication, and equip families to recognize early warning signs. This strengthens the client’s home support system and reduces hospitalization risk.
Take Home Points
- Discharge planning for bipolar I disorder must include clinical, emotional, and social support systems.
- Financial and legal services mitigate consequences of manic behaviors and promote stability.
- Crisis hotlines and psychotherapy provide immediate and ongoing emotional support.
- Family and peer-based interventions reduce isolation and improve treatment adherence.
A client who is being admitted to the mental health unit with bipolar disorder is depressed, avoids eye contact, responds in a very low voice, and is tearful. What is most therapeutic for a nurse to say during the assessment interview?
Explanation
Therapeutic communication in psychiatric nursing involves intentional, empathetic, and structured interaction that promotes trust, emotional safety, and client engagement. During depressive episodes in bipolar disorder, clients may exhibit psychomotor retardation, low self-worth, and withdrawal. The nurse’s role is to maintain a calm, nonjudgmental presence while respecting the client’s emotional state and cognitive limitations.
Rationale for correct answer
4. Acknowledging difficulty and offering a clear plan demonstrates empathy and structure. It respects the client’s emotional vulnerability while providing reassurance and predictability, which are essential during depressive states.
Rationale for incorrect answers
1. This statement implies pressure and conditional support, which may increase guilt or resistance. It lacks empathy and fails to validate the client’s current emotional experience.
2. Physical contact may be perceived as intrusive, especially when the client is withdrawn or tearful. It risks breaching boundaries and may not be appropriate without established rapport.
3. This approach is task-oriented and dismissive of the client’s emotional state. It prioritizes procedure over therapeutic engagement and may reinforce feelings of isolation.
Take Home Points
- Therapeutic communication must be empathetic, structured, and emotionally attuned to the client’s psychiatric presentation.
- Depressed clients benefit from validation, predictability, and gentle reassurance.
- Avoid statements that imply pressure, judgment, or conditional support.
- Physical contact should be used cautiously and only when rapport and consent are established.
A client with the diagnosis of bipolar disorder, depressive episode, has been hospitalized on a psychiatric unit for 1 week. What is the most appropriate activity for this client?
Explanation
Bipolar disorder, depressive episode is marked by persistent low mood, reduced energy, and impaired concentration. Clients often experience psychomotor retardation, social withdrawal, and difficulty initiating or sustaining activities. Therapeutic interventions must be paced to match the client’s cognitive and emotional capacity, emphasizing structured, supportive engagement over stimulation or solitary tasks.
Rationale for correct answer
3. Talking with the nurse several times daily provides consistent support and therapeutic presence. It encourages emotional expression, builds trust, and gently re-engages the client without overwhelming cognitive or social demands.
Rationale for incorrect answers
1. Completing a puzzle alone reinforces isolation and may be cognitively demanding for a client with impaired concentration. It lacks interpersonal engagement and therapeutic value at this stage.
2. Playing cards with several clients requires social energy and sustained attention, which may be too taxing during a depressive episode. It risks overstimulation and withdrawal if the client cannot keep up.
4. Ping-Pong involves coordination and physical exertion, which may exceed the client’s current energy level. It is more appropriate during recovery or euthymic phases, not early in depressive hospitalization.
Take Home Points
- Depressive episodes in bipolar disorder impair energy, concentration, and social engagement.
- Therapeutic communication with staff fosters emotional safety and gradual re-engagement.
- Activities must be low-demand, structured, and emotionally supportive during early recovery.
- Stimulating or solitary tasks may worsen withdrawal or overwhelm cognitive capacity.
What is the best nursing intervention when the language of a client in the manic phase of a bipolar disorder becomes vulgar and profane?
Explanation
Manic phase of bipolar disorder is characterized by elevated mood, disinhibition, and pressured speech, often resulting in inappropriate or profane language. Clients may lack insight and impulse control, making limit-setting essential. Therapeutic responses must balance recognition of the illness with behavioral boundaries to maintain safety and respect within the milieu.
Rationale for correct answer
3. Recognizing the behavior as part of the illness while setting limits maintains therapeutic boundaries and protects the dignity of all clients. It communicates that the nurse understands the psychiatric context but will not tolerate disruptive or offensive language.
Rationale for incorrect answers
1. This response is judgmental and lacks therapeutic value. It may escalate the client’s defensiveness and does not acknowledge the psychiatric basis of the behavior.
2. Ignoring vulgarity may reinforce inappropriate behavior and compromise the therapeutic environment. It fails to model boundaries or protect other clients from verbal aggression.
4. Withholding communication until the client complies is punitive and risks emotional withdrawal. It undermines rapport and may worsen manic symptoms due to perceived rejection.
Take Home Points
- Manic episodes often involve disinhibited speech and poor impulse control.
- Therapeutic limit-setting must acknowledge the illness while maintaining behavioral boundaries.
- Ignoring or punishing inappropriate language can escalate symptoms or damage rapport.
- Nurses must balance empathy with structure to preserve safety and therapeutic integrity.
A client with bipolar disorder, manic episode, has a superior, authoritative manner and constantly instructs other clients about how to dress, what to eat, and where to sit. The nurse should intervene because these behaviors eventually will cause the other clients to feel:
Explanation
Manic episodes in bipolar disorder are marked by elevated mood, grandiosity, and intrusive behavior, often leading to overbearing interactions with others. Clients may exhibit inflated self-esteem and a need to control their environment, which can disrupt group dynamics and provoke negative emotional responses from peers. These behaviors are not intentional acts of malice but stem from impaired impulse control and disinhibition.
Rationale for correct answer
1. Authoritative and intrusive behavior during mania often leads to resentment among peers. Other clients may feel their autonomy is being violated, resulting in frustration and anger, especially when repeatedly instructed or corrected by someone acting superior.
Rationale for incorrect answers
2. Clients are unlikely to become dependent on someone exhibiting manic control. Instead, they may resist or reject the behavior, as it undermines their independence and personal boundaries.
3. Feelings of inadequacy are more common in depressive contexts or when clients compare themselves to others in a passive way. In this scenario, the issue is not self-worth but interpersonal conflict.
4. Ambivalence implies mixed or uncertain feelings, which does not accurately reflect the typical reaction to persistent controlling behavior. The response is more likely to be direct irritation or anger.
Take Home Points
- Manic behavior often includes grandiosity and intrusive control over others.
- Such behaviors disrupt group cohesion and provoke anger in peers.
- Nurses must intervene to maintain therapeutic boundaries and protect client autonomy.
- Emotional reactions to manic intrusiveness are typically frustration, not dependency or ambivalence.
A client with the diagnosis of bipolar disorder, manic episode, is extremely active, talks constantly, and tends to badger the other clients, some of whom are now becoming agitated. What is the best strategy for a nurse to use with this client?
Explanation
Manic episode in bipolar disorder presents with elevated mood, hyperactivity, and excessive talkativeness, often accompanied by intrusive or disruptive behavior. Clients may lack insight and impulse control, leading to overstimulation of others in the milieu. Nursing strategies must focus on behavioral redirection using non-confrontational, therapeutic techniques that preserve safety and reduce agitation.
Rationale for correct answer
3. Distraction is a non-invasive method that redirects energy and attention without escalating conflict. It helps manage intrusive behavior by shifting focus to a neutral or structured activity, reducing stimulation and protecting group dynamics.
Rationale for incorrect answers
1. Humor may be perceived as mocking or dismissive, especially during mania. It risks escalating the client’s behavior or provoking agitation in others, undermining therapeutic rapport.
2. Sympathy may reinforce dependency or validate inappropriate behavior. It lacks structure and does not address the need for behavioral containment or environmental control.
4. Confrontation increases defensiveness and may escalate manic symptoms. It challenges the client’s impaired judgment and can provoke aggression or further disruption in the unit.
Take Home Points
- Manic episodes involve hyperactivity, pressured speech, and poor impulse control.
- Distraction is an effective strategy to redirect behavior without confrontation.
- Humor and sympathy may be misinterpreted and are not therapeutic in acute mania.
- Confrontation should be avoided as it escalates agitation and compromises safety.
What should the nurse include when developing a plan of care for a client in the manic phase of bipolar disorder?
Explanation
Manic phase of bipolar disorder is marked by elevated mood, hyperactivity, and impaired concentration, often accompanied by distractibility, impulsivity, and rapid speech. Clients may exhibit excessive goal-directed activity without completion, leading to exhaustion and interpersonal disruption. Nursing care must prioritize behavioral containment and energy redirection to reduce risk and promote functional engagement.
Rationale for correct answer
3. Redirecting excess energy into constructive channels helps manage agitation and prevents escalation. Structured activities like walking or folding laundry provide physical outlet while minimizing overstimulation and promoting behavioral regulation.
Rationale for incorrect answers
1. Focusing on reality may be ineffective due to grandiosity and poor insight during mania. The client may resist or misinterpret attempts to reorient, leading to frustration or confrontation.
2. Encouraging unrestricted talking reinforces pressured speech and disorganized thought. It may overwhelm others and increase manic intensity, compromising therapeutic boundaries.
4. Persuading task completion assumes attention and follow-through, which are impaired in mania. The client may become irritable or abandon tasks midway, making this approach ineffective.
Take Home Points
- Manic episodes involve hyperactivity, distractibility, and poor impulse control.
- Structured redirection of energy helps contain behavior and reduce agitation.
- Reality orientation and task completion are limited by impaired insight and attention.
- Unrestricted verbalization may escalate symptoms and disrupt the therapeutic environment.
A 25-year-old woman with the diagnosis of bipolar disorder, manic episode, is admitted to the psychiatric unit. A nurse on the unit reviews the admission information provided by the client’s husband and assesses the client. Based on the information, what is an appropriate nursing intervention?
Explanation
Manic episode in bipolar disorder is marked by elevated mood, hyperactivity, and impaired impulse control, often accompanied by distractibility, grandiosity, and intrusive behavior. Clients may overstimulate easily and disrupt group settings due to excessive energy and pressured speech. Nursing interventions must prioritize environmental control to reduce stimulation and promote behavioral containment.
Rationale for correct answer
1. Assigning the client to a private room minimizes stimulation and protects other clients from disruptive behavior. It allows for better behavioral monitoring and supports de-escalation in a controlled setting.
Rationale for incorrect answers
2. Playing cards with several clients increases arousal and social stimulation, which may exacerbate manic symptoms. The client may dominate the activity or provoke agitation in others.
3. Introspection requires insight, which is impaired during mania. The client may be unable to reflect meaningfully or engage in therapeutic self-examination until symptoms stabilize.
4. Communal dining may lead to disruption due to excessive talking or intrusive behavior. It risks overstimulation and conflict with peers, especially in early stages of admission.
Take Home Points
- Manic episodes require environmental control to reduce stimulation and prevent escalation.
- Private rooms support behavioral containment and minimize disruption to others.
- Insight-based interventions are deferred until the client achieves symptom stabilization.
- Group activities and communal settings may worsen manic symptoms and compromise safety.
A client in a mental health facility with the diagnosis of bipolar disorder, manic phase, is argumentative, domineering, and exhibitionistic. A visitor reports that this client is running down the hall scaring people. What should the nurse do first?
Explanation
Manic phase of bipolar disorder presents with elevated mood, disinhibition, and impaired judgment, often resulting in intrusive, aggressive, or exhibitionistic behavior. Clients may act impulsively and pose a risk to themselves or others. Immediate nursing actions must prioritize safety using structured, non-confrontational approaches that prevent escalation and maintain control of the environment.
Rationale for correct answer
2. Approaching the client with several staff members ensures containment and safety. It provides a calm but firm presence that can de-escalate behavior while minimizing risk to others. This strategy also reinforces therapeutic boundaries without confrontation.
Rationale for incorrect answers
1. Asking for reasons assumes insight, which is often absent during mania. The client may respond with defensiveness or further agitation, making this approach ineffective and potentially unsafe.
3. Nonthreatening assessment is appropriate once stabilized, but not as a first response when behavior is disruptive and frightening others. Immediate containment is required before therapeutic engagement.
4. Seclusion is a restrictive intervention requiring clinical justification and physician order. It is not the first-line response and should only be considered if less invasive methods fail to ensure safety.
Take Home Points
- Manic episodes may involve impulsive, disruptive, and exhibitionistic behavior requiring immediate containment.
- Safety is the nurse’s first priority, and structured staff intervention prevents escalation.
- Insight-based or therapeutic assessment follows only after behavioral control is achieved.
- Seclusion is reserved for extreme cases and must follow protocol after other strategies fail.
A nurse is caring for a newly admitted client who has been diagnosed with bipolar disorder and has a history of hyperactivity and combativeness. Later in the evening, a commotion is heard, and this client is found hitting another client. What are the legal implications of this situation?
Explanation
Legal implications in psychiatric care center on the nurse’s duty to provide reasonable care, prevent foreseeable harm, and uphold client rights. When a client has a documented history of aggression or hyperactivity, the standard of care requires proactive monitoring and intervention. Failure to do so may constitute negligence if harm occurs to others in the facility.
Rationale for correct answer
4. Close observation is a legally and ethically required precaution when a client has a known history of combativeness. It reflects anticipatory care and aligns with the nurse’s duty to protect both the client and others from foreseeable risk.
Rationale for incorrect answers
1. Restraints must be justified by imminent danger, not history alone. Using restraints preemptively violates legal standards and patient rights, and may be considered abusive or excessive.
2. Sedation without clinical indication or behavioral escalation is unlawful and unethical. It disregards the principle of least restrictive intervention and may lead to liability for chemical restraint.
3. Even if in contact with reality, a client with a history of aggression requires monitoring. Reality orientation does not eliminate risk, and failure to supervise may result in preventable harm and legal consequences.
Take Home Points
- Nurses must anticipate risk based on client history and implement appropriate observation.
- Legal standards require least restrictive interventions unless danger is imminent.
- Sedation and restraints must be clinically justified and documented.
- Failure to monitor a known combative client may result in negligence and liability.
A psychiatric social worker is conducting a community meeting. You are the co-leader. All patients are attending because there has been theft of personal items. Ms. M (manic phase bipolar disorder) continuously interrupts and loudly announces, “Ms. B (borderline personality) stole my lipstick. Look at her lips!” What is your best response to this situation?
Explanation
Manic phase bipolar disorder presents with elevated mood, impulsivity, and poor judgment, often resulting in loud, intrusive, and disruptive behavior. Clients may exhibit flight of ideas, pressured speech, and paranoia, which can destabilize group settings. In community meetings, the nurse must act swiftly to preserve safety, structure, and therapeutic integrity without escalating the situation.
Rationale for correct answer
1. Quietly escorting Ms. M out of the meeting uses non-confrontational redirection to remove the disruptive stimulus. It protects the group dynamic, prevents escalation, and allows for individualized de-escalation in a controlled setting.
Rationale for incorrect answers
2. Deferring responsibility undermines collaboration and delays intervention. As co-leader, the nurse shares accountability for maintaining structure and must act promptly to manage disruptive behavior.
3. Instructing Ms. B to respond invites conflict and emotional escalation. It risks reinforcing accusatory dynamics and compromising the psychological safety of both clients.
4. Telling Ms. M to stop and promising investigation may provoke defensiveness or further outbursts. It lacks therapeutic containment and may be perceived as invalidating or dismissive.
Take Home Points
- Manic behavior in group settings requires immediate, calm redirection to preserve safety.
- Nurses must act collaboratively and proactively to manage disruptive dynamics.
- Avoid escalating conflict by involving accused clients or making public statements.
- Individualized de-escalation outside the group setting is often the most therapeutic approach.
Exams on Mood Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
Upon completion of this topic, the nursing student will be able to:
- Define and differentiate between the concepts of mood and affect.
- Describe the diagnostic criteria for Bipolar I Disorder, Bipolar II Disorder, and Cyclothymic Disorder, as per the DSM-5.
- Distinguish between a manic episode and a hypomanic episode.
- Discuss the epidemiology and common comorbidities associated with bipolar disorders.
- Identify the major biological and psychosocial theories of etiology for bipolar disorders.
- Explain the primary pharmacological and non-pharmacological treatment modalities for bipolar disorders.
- Apply the nursing process to a patient experiencing a bipolar disorder, including performing a comprehensive assessment, formulating nursing diagnoses, establishing outcomes, planning interventions, and implementing care.
- Recognize the indications and procedures for the use of seclusion and restraints in the management of acute mania.
Introduction
- Mood disorders are a class of psychiatric illnesses defined by a pervasive and sustained disturbance of mood that causes significant functional impairment and distress.
- These disorders are characterized by either an elevation or a depression of mood, or a combination of both.
- Bipolar disorders, which are the focus of these notes, are a specific category of mood disorders characterized by alternating episodes of mania or hypomania and depression.
1.1. Mood and Affect Defined
- Mood: A pervasive and sustained emotion that colors an individual's perception of the world.
- It is a subjective experience, reported by the individual. Examples of mood descriptions include euphoric, dysphoric, irritable, anxious, or apathetic.
- A person's mood can be described in terms of its quality, pervasiveness, and stability.
- Affect: The external, observable expression of an individual's emotional state. It is an objective observation made by the nurse.
- Affect can be described in terms of its range, intensity, and appropriateness.
- Range: The extent of emotional expression shown. Can be full range, constricted (limited variability), blunted (a significant reduction in emotional expression), or flat (virtually no emotional expression).
- Intensity: The strength of the emotional expression. Can be described as intense, moderate, or low.
- Appropriateness: The congruence between the emotional expression and the content of the conversation. Affect can be described as congruent or incongruent.
NURSING INSIGHTS
- The distinction between mood and affect is crucial for accurate assessment. A patient might report feeling "fine" (mood), but their facial expression and tone of voice are flat and monotone (affect).
- This incongruence is a significant clinical finding that requires further investigation.
Bipolar And Related Disorders
- Bipolar and related disorders are characterized by a fluctuation between manic/hypomanic episodes and major depressive episodes.
- The DSM-5 organizes these disorders based on the type and severity of these episodes.
1.1. Bipolar I Disorder
- Defined by at least one manic episode. A major depressive episode may or may not have occurred, but it is not a requirement for the diagnosis.
- The manic episode must be present for at least one week and present for most of the day, nearly every day, or any duration if hospitalization is necessary.
- The symptoms must cause marked impairment in social or occupational functioning or necessitate hospitalization to prevent harm to self or others, or there are psychotic features.
1.2. Bipolar II Disorder
- Defined by a history of at least one major depressive episode and at least one hypomanic episode.
- The individual has never experienced a full manic episode.
- The hypomanic episode must be present for at least four consecutive days and present for most of the day, nearly every day.
- The episode is not severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization.
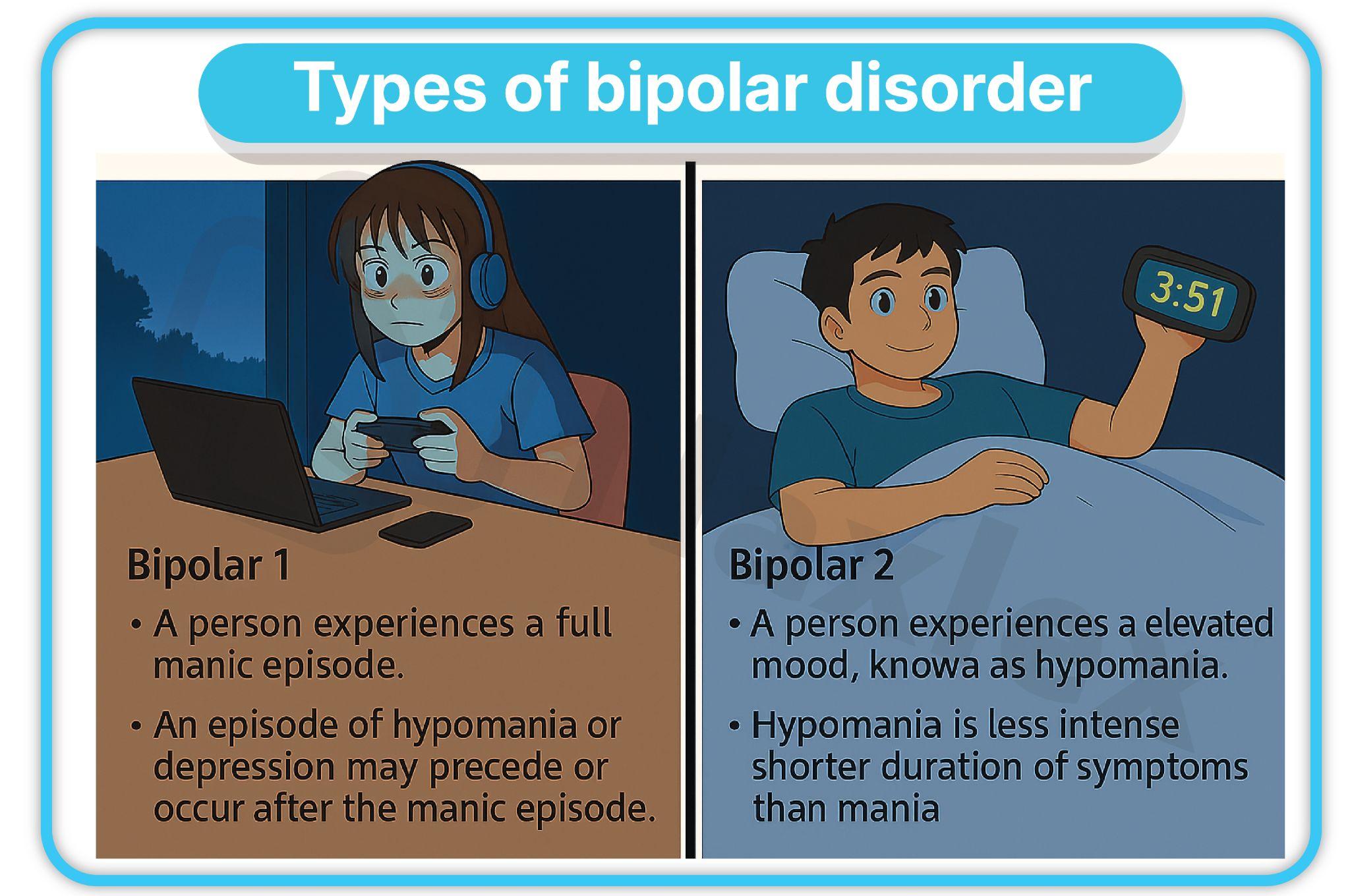
NURSING INSIGHTS
- Bipolar I is often considered more severe than Bipolar II due to the presence of a full manic episode, which can lead to significant functional impairment, hospitalization, and potential harm.
- However, the chronic nature of Bipolar II, characterized by frequent depressive episodes, can be equally debilitating and is often misdiagnosed as major depressive disorder.
- This is a critical point for the nurse to recognize, as treating Bipolar II with antidepressants alone can precipitate a hypomanic or manic episode.
1.3. Cyclothymic Disorder
- A chronic, fluctuating mood disturbance involving numerous periods of hypomanic symptoms and numerous periods of depressive symptoms.
- The symptoms are not severe enough or do not last long enough to meet the criteria for a hypomanic episode or a major depressive episode.
- The symptoms have been present for at least two years in adults (one year in children and adolescents).
- During this two-year period, the individual has not been without symptoms for more than two consecutive months.
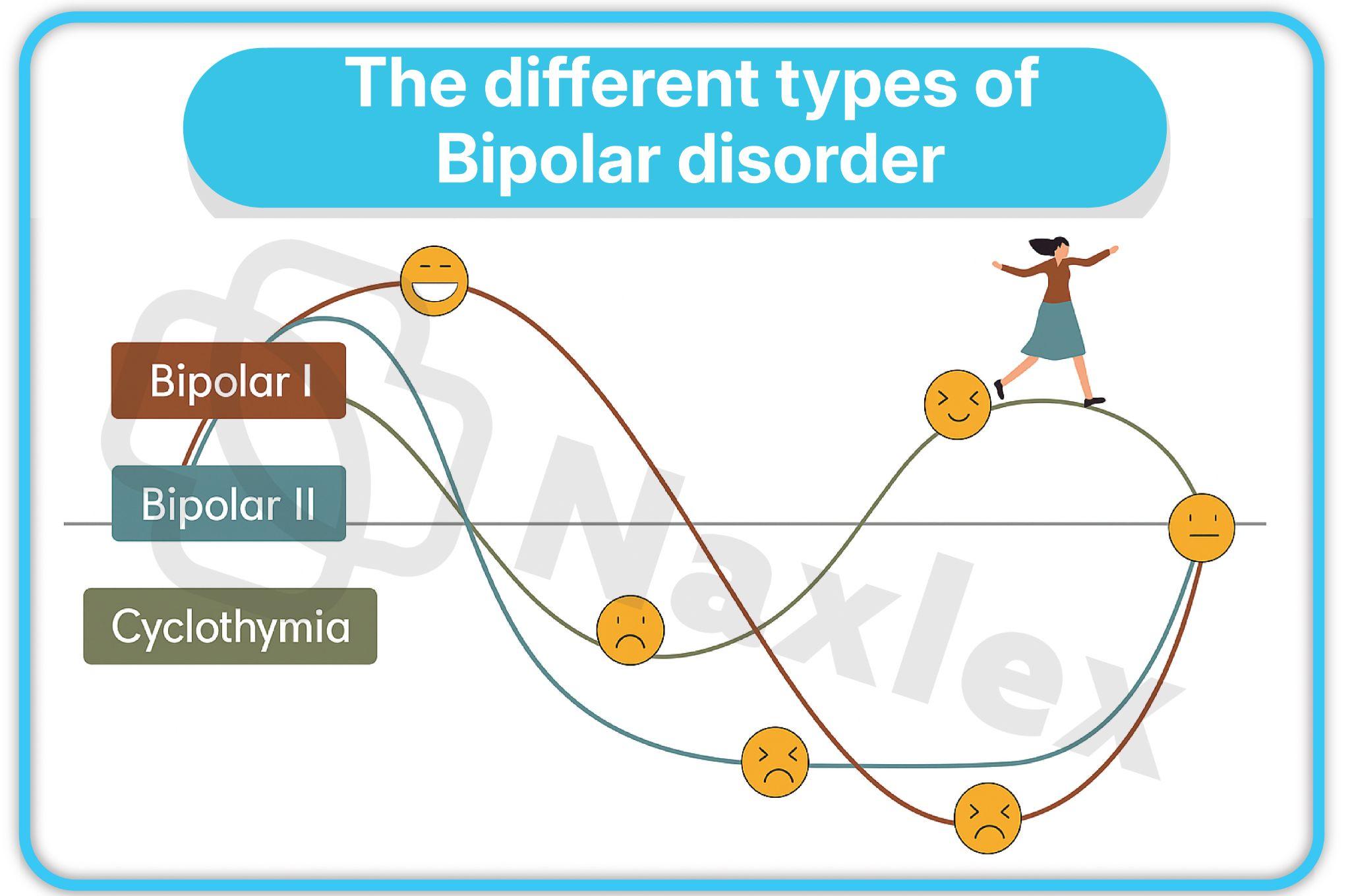
1.4. Manic Episodes
- A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least one week and present for most of the day, every day.
- During the period of mood disturbance and increased energy or activity, at least three of the following symptoms (four if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior:
- Grandiosity or inflated self-esteem: Exaggerated belief in one's own abilities, wealth, or power.
- Decreased need for sleep: Feeling rested after only a few hours of sleep.
- More talkative than usual or pressure to keep talking: Rapid, loud, and often difficult to interrupt speech.
- Flight of ideas or racing thoughts: A continuous flow of accelerated speech with abrupt changes from topic to topic.
- Distractibility: Attention is too easily drawn to unimportant or irrelevant external stimuli.
- Increase in goal-directed activity: May involve social, occupational, or sexual pursuits.
- Excessive involvement in activities that have a high potential for painful consequences: Examples include unrestrained spending sprees, sexual indiscretions, or foolish business investments.
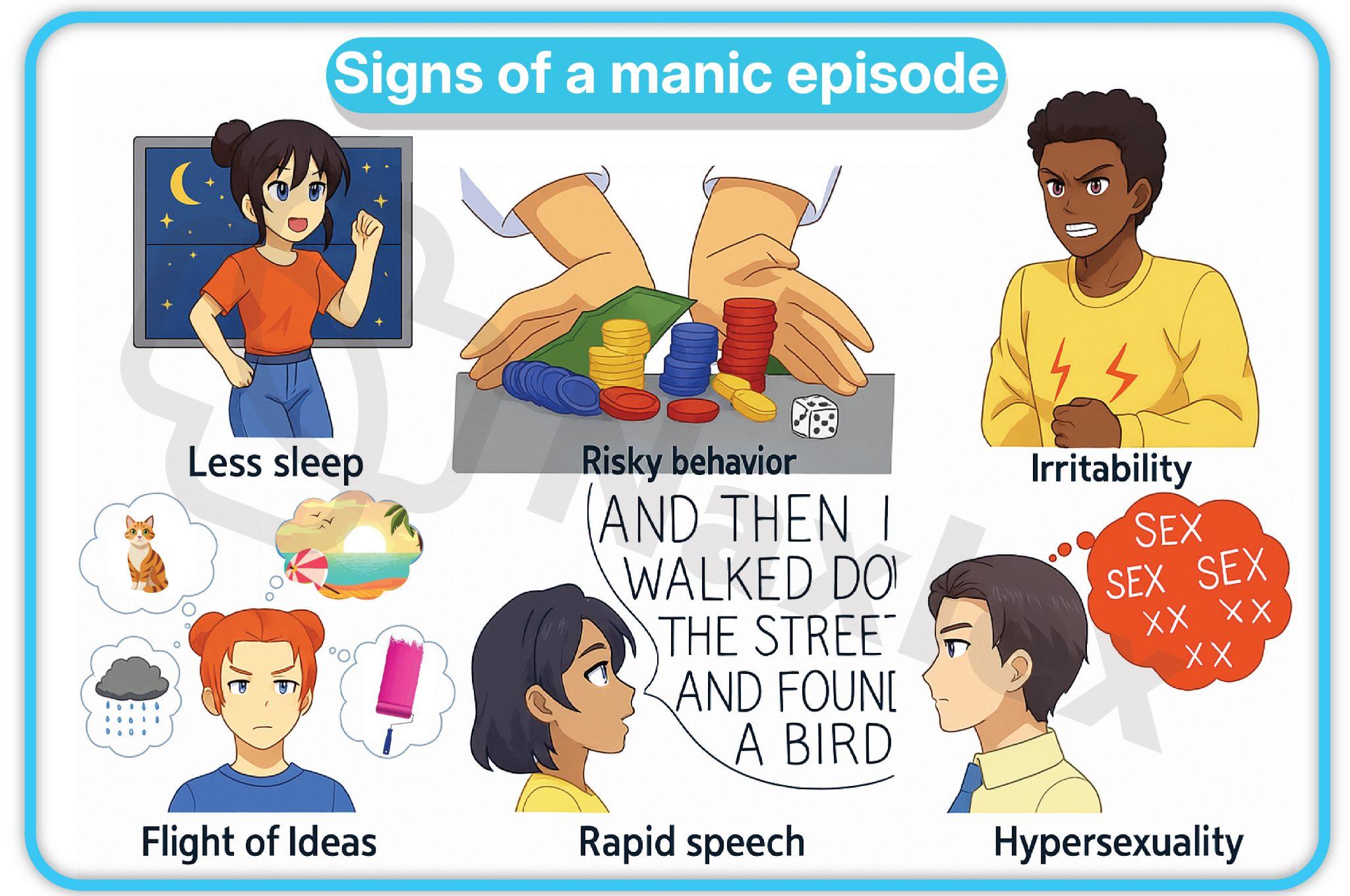
1.5. Hypomanic Episodes
- A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least four consecutive days and present for most of the day, every day.
- The same number of symptoms (at least three or four if irritable) from the list for a manic episode are present.
- The episode is not severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization.
|
Feature |
Bipolar I |
Bipolar II |
Cyclothymia |
|
Key Episode |
Mania |
Hypomania + Depression |
Hypomanic + Depressive Symptoms (subthreshold) |
|
Severity |
Severe, often requires hospitalization |
Moderate impairment, no full mania |
Chronic, fluctuating |
|
Psychosis |
Common in mania |
Absent |
Absent |
|
Risk of Suicide |
High |
High |
Moderate |
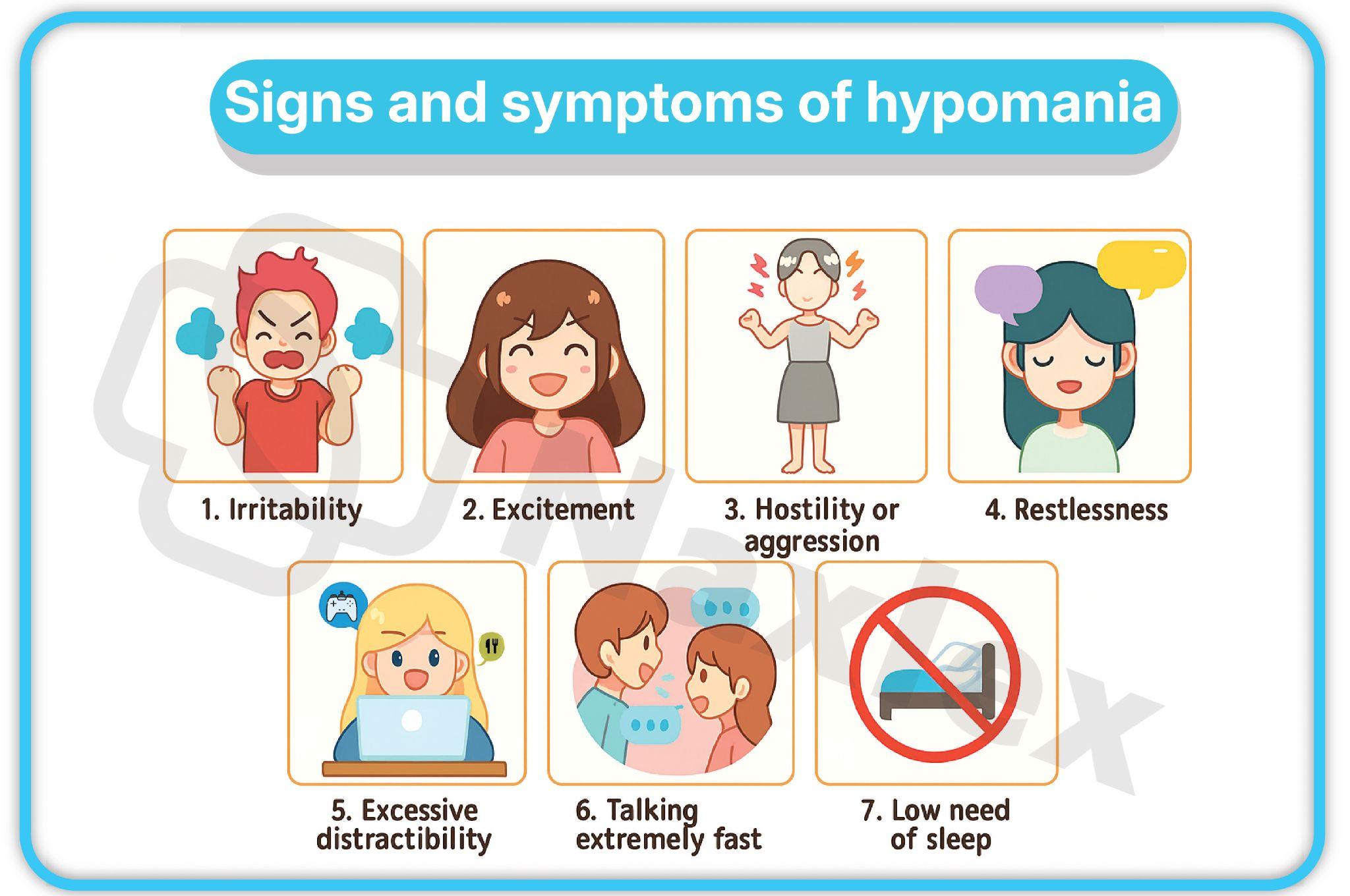
NURSING INSIGHTS
- The key difference between mania and hypomania lies in the severity and duration of the symptoms, and the degree of functional impairment.
- Mania is a medical emergency requiring immediate attention due to the high risk of harm to self and others. Hypomania, while still a clinical concern, does not involve the same level of functional impairment or risk.
1.6. Mixed Features
- Specifier for manic, hypomanic, or major depressive episodes.
- The individual experiences symptoms of both mania/hypomania and depression simultaneously.
- For example, during a manic episode, the individual may also experience feelings of sadness, worthlessness, or suicidal ideation. This can be a particularly dangerous state due to the high energy level combined with feelings of hopelessness, increasing the risk of suicide.
Epidemiology
- Bipolar disorder affects approximately 2.8% of the U.S. adult population in a given year, and the lifetime prevalence is around 4.4%.
- Bipolar I disorder affects men and women in roughly equal proportions, while Bipolar II is more common in women.
- The average age of onset is in the early 20s, but it can occur at any age, from childhood to older adulthood.
- Bipolar disorder is often misdiagnosed, leading to a significant delay (up to 10 years) in receiving appropriate treatment.
Comorbidity
- Comorbidity is a significant issue in bipolar disorders, complicating diagnosis and treatment.
- Substance Use Disorders: Are present in a high percentage of individuals with bipolar disorder (estimated 60%). Alcohol and cannabis use disorders are particularly common.
- Anxiety Disorders: Include panic disorder, social anxiety disorder, and obsessive-compulsive disorder (OCD). These disorders often precede the onset of bipolar symptoms.
- Eating Disorders: Anorexia nervosa and bulimia nervosa are frequently comorbid conditions.
- Attention-Deficit/Hyperactivity Disorder (ADHD): There is significant symptom overlap, and both are often present, especially in children and adolescents.
- Personality Disorders: Borderline personality disorder is a common comorbidity, with some research suggesting a shared genetic vulnerability.
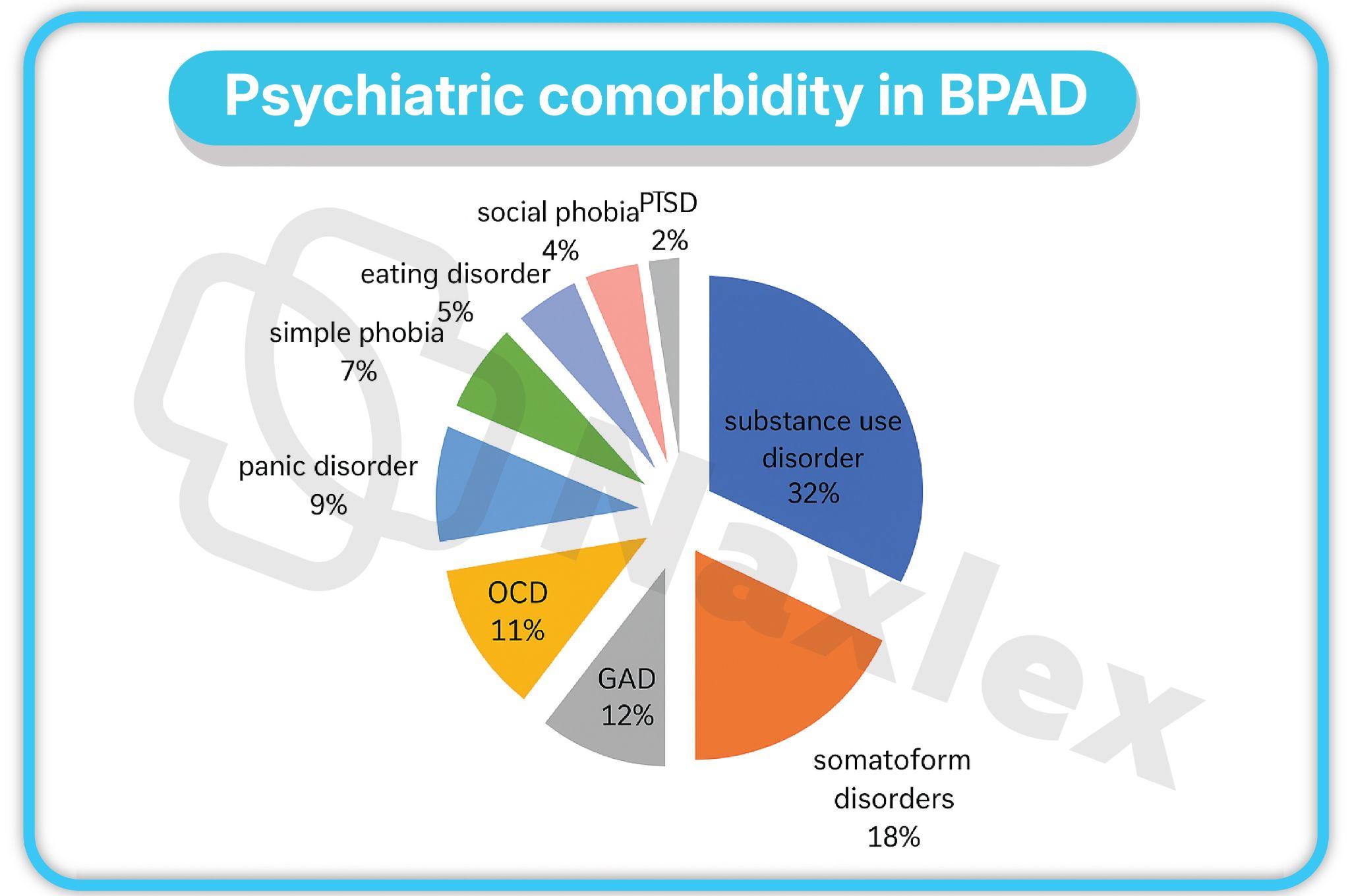
Etiology
- The etiology of bipolar disorder is complex and multifactorial, involving a combination of biological and psychosocial factors.
1.1. Biological Theories
1.1.1. Genetic Factors
- Bipolar disorder has a strong genetic component.
- The lifetime risk for developing bipolar disorder is significantly higher in first-degree relatives of individuals with the disorder.
- Concordance rates are much higher in monozygotic (identical) twins (60-80%) compared to dizygotic (fraternal) twins (10-20%).
- Multiple genes are likely involved, each contributing a small risk. Genome-wide association studies (GWAS) have identified several genes and chromosomal regions associated with the disorder, though no single "bipolar gene" has been found.
1.1.2. Neurobiological Factors
- Neurotransmitters:
- Norepinephrine: Excessive levels of norepinephrine are thought to be associated with mania, while a deficiency is linked to depression. This is known as the "monoamine hypothesis."
- Dopamine: Increased dopamine activity is implicated in mania, especially in symptoms like euphoria, grandiosity, and psychosis.
- Serotonin: A decrease in serotonin is associated with depression. Serotonin dysregulation is also thought to play a role in the mood instability and impulsivity seen in bipolar disorder.
- GABA (Gamma-aminobutyric acid): A major inhibitory neurotransmitter. Low levels of GABA are hypothesized to contribute to manic symptoms.
- Glutamate: The primary excitatory neurotransmitter. Dysregulation of glutamate has been implicated in the pathophysiology of bipolar disorder.
- Brain Structure and Function:
- Prefrontal Cortex: Responsible for executive functions, including decision-making, judgment, and emotional regulation. Abnormalities in the prefrontal cortex are consistently found in individuals with bipolar disorder, especially during manic episodes.
- Amygdala: The brain's "fear center," involved in emotional processing. The amygdala is often hyperactive in individuals with bipolar disorder, leading to heightened emotional reactivity and impulsivity.
- Hippocampus: Involved in memory and emotional regulation. Volume reductions in the hippocampus have been reported in individuals with bipolar disorder, particularly after repeated episodes.
- Basal Ganglia: Abnormalities in the basal ganglia, which are involved in motor control and motivation, are also observed.
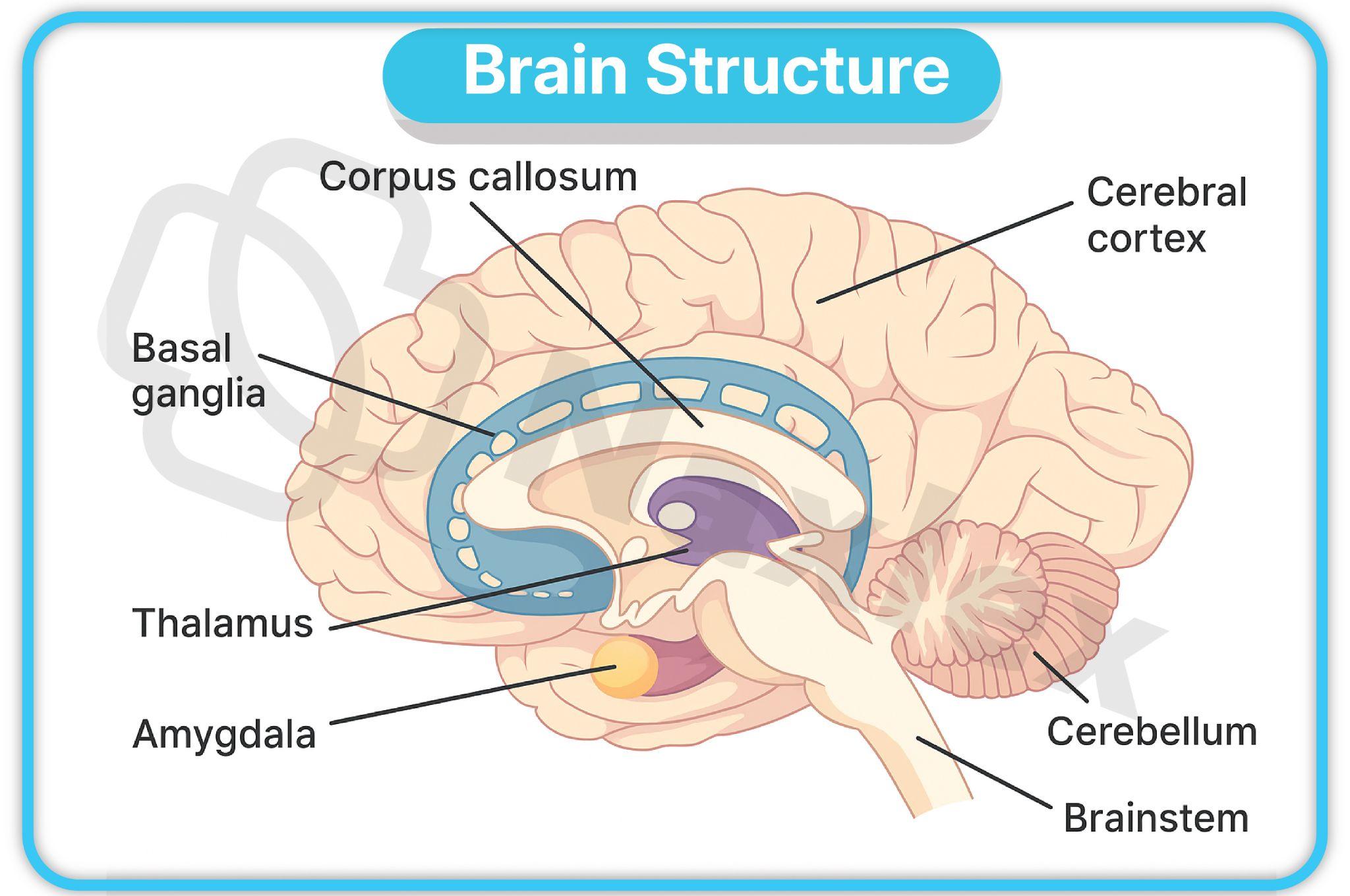
- Kindling Theory: Proposes that a person with a genetic predisposition to bipolar disorder becomes more neurologically sensitive to stressors with each successive episode. Each episode lowers the threshold for the next, leading to more frequent and severe episodes over time, even with a minimal trigger.
NURSING INSIGHTS:
- Understanding the neurobiological underpinnings of bipolar disorder is essential for the nurse to explain the rationale for pharmacological interventions.
- For example, a nurse can explain to a patient that mood stabilizers work by regulating the activity of neurotransmitters and stabilizing the electrical activity of the brain, which helps to prevent the extreme highs and lows of the disorder.
1.2. Psychosocial Theories
- Stressful Life Events: Psychological stress, such as major life changes, relationship conflicts, or financial difficulties, can act as a trigger for manic or depressive episodes in genetically vulnerable individuals.
- Psychosocial Rhythm and Zeitgebers: Disruptions to a person's routine or "zeitgebers" (external cues that regulate the body's circadian rhythm, such as sleep-wake cycles, mealtimes, and social routines) can precipitate an episode. For example, a person with bipolar disorder who experiences sleep deprivation due to a stressful event may be more likely to have a manic episode.
- Expressed Emotion (EE): High levels of expressed emotion within a family (criticism, hostility, and over-involvement) are associated with a higher rate of relapse in individuals with bipolar disorder.
Treatments For Bipolar Disorders
- Treatment for bipolar disorder is multifaceted and typically involves a combination of pharmacological and non-pharmacological interventions.
- The goal is to manage acute episodes, prevent future episodes, and improve overall quality of life.
1.1. Pharmacological Interventions
- Mood Stabilizers: The cornerstone of treatment for bipolar disorder.
- Lithium: The oldest and most studied mood stabilizer. It is highly effective in treating both mania and preventing future episodes.
- Mechanism of Action: Believed to modulate the activity of neurotransmitters (e.g., dopamine, norepinephrine, and serotonin) and to stabilize electrical activity in the brain.
- Nursing Considerations:
- Requires regular monitoring of blood lithium levels to prevent toxicity (therapeutic range: 0.6-1.2 mEq/L for maintenance, 0.8-1.5 mEq/L for acute mania).
- Patients should maintain consistent salt and fluid intake, as fluctuations can affect lithium levels. Dehydration can lead to lithium toxicity.
- Common side effects: Tremor, polyuria, polydipsia, weight gain, nausea.
- Signs of toxicity: Coarse tremor, severe diarrhea, ataxia, blurred vision, tinnitis.
- Anticonvulsants (Antiepileptic Drugs): Used as mood stabilizers, especially for rapid-cycling bipolar disorder.
- Valproate (Depakote):
- Mechanism of Action: Increases levels of GABA.
- Nursing Considerations: Monitor liver function tests and complete blood counts, as it can cause hepatotoxicity and thrombocytopenia.
- Carbamazepine (Tegretol):
- Mechanism of Action: Reduces nerve impulses.
- Nursing Considerations: Monitor for a rare but serious side effect of agranulocytosis (a decrease in white blood cells). Requires regular blood tests.
- Lamotrigine (Lamictal):
- Mechanism of Action: Thought to work by inhibiting glutamate release.
- Nursing Considerations: Monitor for a potentially life-threatening rash, Stevens-Johnson syndrome. Patients should be instructed to report any rash immediately.
- Valproate (Depakote):
- Lithium: The oldest and most studied mood stabilizer. It is highly effective in treating both mania and preventing future episodes.
- Atypical Antipsychotics: Often used in combination with mood stabilizers to manage acute manic or mixed episodes and to augment antidepressant therapy for bipolar depression.
- Examples: Olanzapine (Zyprexa), Quetiapine (Seroquel), Aripiprazole (Abilify), Risperidone (Risperdal).
- Nursing Considerations: Monitor for metabolic side effects, including weight gain, hyperglycemia, and dyslipidemia.
- Benzodiazepines: Used for short-term management of agitation, anxiety, and insomnia during acute manic episodes. Not a primary treatment.
|
Medication Class |
Examples |
Primary Use |
Monitoring Parameters |
|
Mood Stabilizers |
Lithium |
Mania prevention |
Serum levels, renal function, thyroid |
|
Anticonvulsants |
Valproate, Lamotrigine |
Acute mania, depression |
Liver enzymes, rash risk |
|
Atypicals |
Olanzapine, Risperidone |
Psychotic features |
Weight, glucose, lipids |
1.2. Psychotherapy
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing negative thought patterns and behaviors. It helps patients recognize triggers for episodes and develop coping strategies.
- Psychoeducation: Educating the patient and family about the illness, including symptoms, triggers, and the importance of medication adherence and a stable routine.
- Family-Focused Therapy: Aims to reduce expressed emotion in the family, improve communication, and help the family develop a plan to manage the illness.
- Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on stabilizing daily routines and improving interpersonal relationships to minimize disruptions to the circadian rhythm and prevent mood episodes.
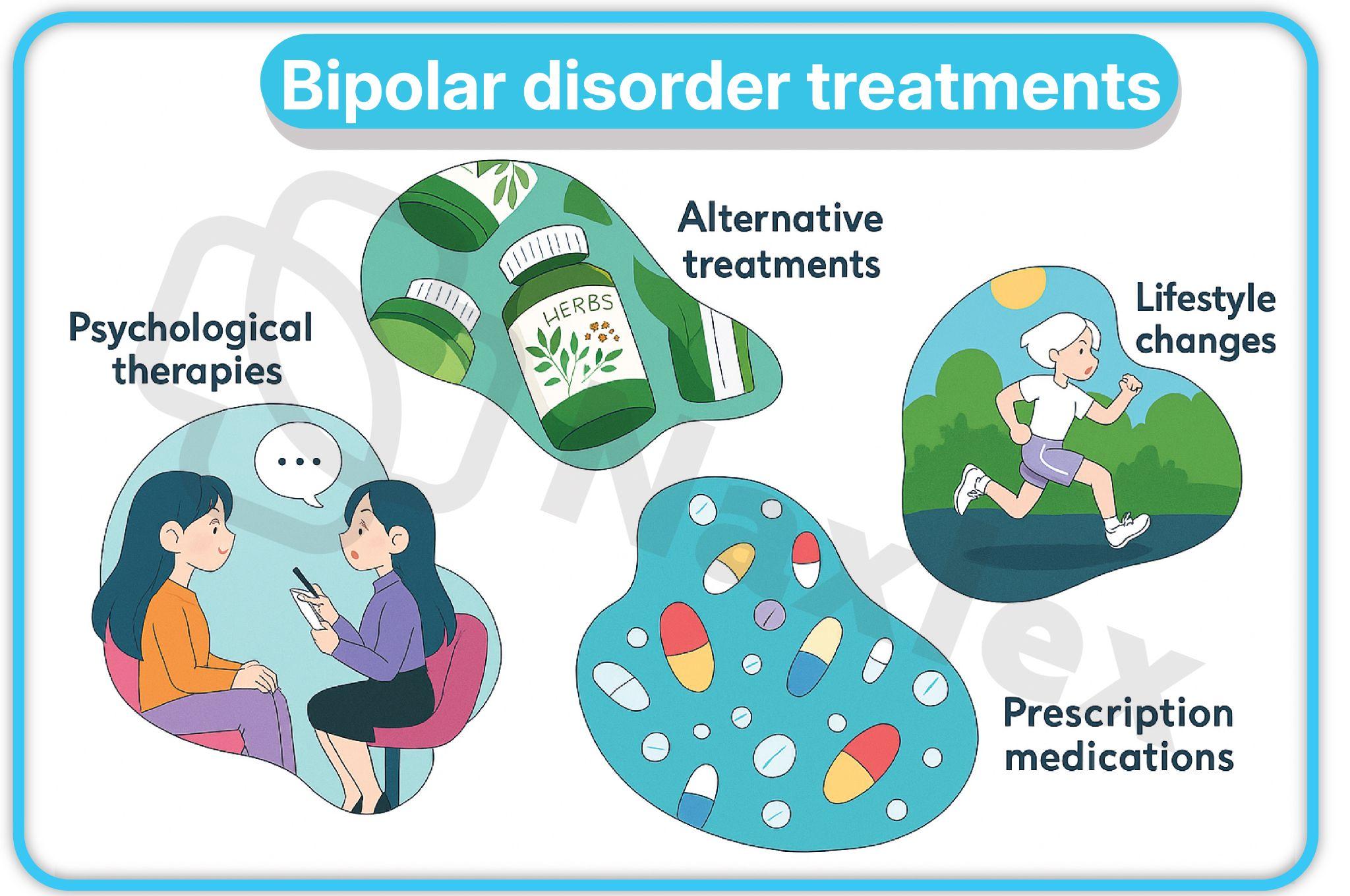
Applying The Nursing Process To Bipolar Disorders
1.1. Assessment
- Mental Status Examination (MSE): A systematic evaluation of a patient's current mental state.
- Appearance: Often flamboyant, disheveled, or inappropriate for the setting during a manic episode.
- Behavior/Activity: Hyperactive, agitated, and goal-directed. Pacing, hand-wringing, and an inability to sit still.
- Mood/Affect: Mood is often euphoric, irritable, or expansive. Affect is often labile and can change rapidly.
- Speech: Pressured speech, loud, rapid, and difficult to interrupt. May include rhyming or clang associations.
- Thought Process: Flight of ideas, racing thoughts, and distractibility.
- Thought Content: Grandiose or paranoid delusions may be present.
- Sensorium/Cognition: Oriented to person, place, and time, but memory and concentration may be impaired.
- Insight/Judgment: Often impaired, especially during a manic episode. The patient may not recognize their own illness or the consequences of their behavior.
- Screening Tools:
- Mood Disorder Questionnaire (MDQ): A self-report tool used to screen for bipolar disorder.
- Young Mania Rating Scale (YMRS): A clinician-administered scale used to assess the severity of manic symptoms.
- Comprehensive Assessment:
- History: Elicit a detailed history of the patient's mood episodes, including duration, severity, and triggers. Inquire about family history of mood disorders.
- Substance Use: Screen for current and past substance use, as it can complicate the clinical picture.
- Suicide/Homicide Risk: Always assess for suicidal or homicidal ideation, plans, or intent, especially in the context of a mixed episode or severe depression.
NURSING INSIGHTS:
- A thorough and non-judgmental assessment is the foundation of effective nursing care.
- It is crucial to gather information from both the patient and collateral sources, such as family members, who can provide valuable insights into the patient's baseline functioning and symptom changes.
1.2. Diagnoses
Based on the assessment data, the nurse formulates appropriate nursing diagnoses. Common diagnoses for a patient in a manic state include:
- Risk for Injury: Related to extreme hyperactivity, agitation, and impaired judgment.
- Ineffective Coping: Related to inability to manage stress and emotional lability.
- Imbalanced Nutrition: Less Than Body Requirements: Related to refusal to eat or inability to sit still long enough to eat.
- Sleep Deprivation: Related to manic hyperactivity and decreased need for sleep.
- Defensive Coping: Related to grandiose thinking and denial of problems.
1.3. Outcomes Identification
Outcomes should be specific, measurable, achievable, relevant, and time-bound (SMART). Examples include:
- The patient will remain free from injury throughout the shift.
- The patient will sleep for at least 4 hours per night by the end of the week.
- The patient will consume at least 75% of meals and maintain adequate hydration.
- The patient will verbalize a plan to seek help from staff when feeling agitated by the next day.
1.4. Planning Interventions
- Establish Therapeutic Relationship: Build a trusting and non-judgmental relationship. Be calm, firm, and consistent.
- Safety: Prioritize the patient's safety and the safety of others. Remove any potential weapons or dangerous objects from the environment.
- De-escalation: Use calm and simple language. Avoid power struggles.
- Environmental Management: Provide a quiet, low-stimulus environment. Reduce excessive lighting, noise, and social interaction.
1.5. Implementing Interventions for Mania
- Physical Needs:
- Nutrition: Provide frequent, high-calorie, and easy-to-carry finger foods and drinks to meet the patient's nutritional and hydration needs.
- Sleep: Encourage regular sleep-wake cycles. Discourage napping during the day.
- Hygiene: Remind and assist the patient with personal hygiene, as they may be too preoccupied to attend to it.
- Communication:
- Use brief, concise, and direct communication.
- Avoid complex sentences or abstract concepts.
- Do not get drawn into arguments or power struggles. Set clear limits.
- Structure and Routine:
- Provide a structured daily schedule with simple, non-competitive activities.
- Activities should be low-key and individual or in a small group.
- Medication Administration:
- Administer prescribed medications as ordered.
- Monitor for side effects and therapeutic effectiveness.
- Educate the patient and family about the purpose of the medication and the importance of adherence.
1.6. Seclusion or Restraints
- Purpose: Seclusion or restraints are a last resort for managing a patient in an acute manic state who poses an imminent risk of harm to self or others and less restrictive interventions have failed.
- Indications: Imminent danger, extreme agitation, and physical aggression.
- Procedure:
- Requires a physician's order.
- The nurse must continuously monitor the patient's safety, physical well-being (e.g., circulation, hydration, and elimination), and mental status.
- Document all observations, interventions, and the patient's response in detail.
- Review the order and assess the need for continued seclusion or restraint at regular, specified intervals.
- Debrief with the patient after the episode to help them understand the reason for the intervention and to plan for future crises.
Summary
- Mood disorders are a class of psychiatric illnesses defined by a pervasive disturbance in mood. Bipolar disorders are characterized by alternating episodes of mania/hypomania and depression.
- Bipolar I Disorder is defined by at least one manic episode, while Bipolar II Disorder requires at least one hypomanic episode and one major depressive episode. Cyclothymic disorder is a chronic, milder form.
- The etiology of bipolar disorder is multifactorial, including genetic, neurobiological, and psychosocial factors. Key neurobiological players include dysregulation of neurotransmitters like norepinephrine, dopamine, and serotonin.
- Treatment is comprehensive, involving pharmacological interventions (mood stabilizers, antipsychotics) and psychotherapy (CBT, psychoeducation, IPSRT).
- The nursing process for a patient with bipolar disorder begins with a thorough assessment, including a mental status examination and screening for comorbidity and risk.
- Nursing care focuses on ensuring patient safety, providing a structured and low-stimulus environment, managing physical needs, and providing consistent and therapeutic communication.
- Seclusion and restraints are extreme measures used only when a patient poses an imminent danger and all other de-escalation techniques have failed.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Mood Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


