Please set your exam date
Pathophysiology of the respiratory system
Study Questions
Tuberculosis
Explanation
A) Incorrect. TB is not primarily transmitted through contaminated food and water; it is mainly an airborne disease.
B) Correct. TB is primarily an airborne disease, and the bacteria can be transmitted through respiratory droplets when an infected person coughs, sneezes, or talks.
C) Incorrect. TB is not primarily transmitted through sexual contact.
D) Incorrect. TB is not primarily transmitted through contact with skin lesions. It primarily affects the lungs and is transmitted through the respiratory route.
Explanation
A) Incorrect. Joint pain and swelling are not typical symptoms of pulmonary TB.
B) Incorrect. Skin rash and itching are not common symptoms of pulmonary TB.
C) Correct. Persistent cough and sputum production are common symptoms of pulmonary TB, as the disease primarily affects the lungs.
D) Incorrect. Blurred vision and eye pain are not typical symptoms of TB, although TB can affect other parts of the body in addition to the lungs.
Explanation
A) Correct. LTBI is not contagious, as the bacteria are dormant and not actively causing illness. Active TB disease, on the other hand, is contagious and can be transmitted to others through respiratory droplets.
B) Incorrect. LTBI is not contagious, whereas active TB disease is contagious.
C) Incorrect. LTBI and active TB disease have different symptoms and treatment approaches. LTBI has no symptoms, while active TB disease presents with symptoms and requires treatment to prevent progression.
D) Incorrect. LTBI does not always progress to active TB disease. In fact, many individuals with LTBI do not develop active disease, but they are at risk, especially if their immune system becomes compromised.
Explanation
A) Correct. Isolation in a negative-pressure room is the standard precaution for preventing the transmission of TB in healthcare settings, as it helps contain airborne pathogens.
B) Incorrect. While handwashing is important for general infection control, it is not the primary measure for preventing TB transmission.
C) Incorrect. Wearing a surgical mask at all times is not sufficient to prevent TB transmission, especially in a healthcare setting.
D) Incorrect. Avoiding close contact with the client is not a practical measure for healthcare professionals providing care to TB patients. Proper isolation measures are more effective.
Explanation
A) Correct. Using multiple drugs to treat TB reduces the risk of drug resistance development, as it targets the bacteria from different angles and makes it harder for them to become resistant to one or more drugs.
B) Incorrect. While using multiple drugs may help manage side effects by spreading the burden of treatment, the primary purpose is to prevent drug resistance.
C) Incorrect. Shortening the treatment duration is a goal, but it is not the primary purpose of using multiple drugs.
D) Incorrect. Although improving patient compliance is important, the primary purpose of using multiple drugs is to reduce drug resistance.
QUESTIONS
Explanation
A) Incorrect. Living in well-ventilated areas with good air circulation actually reduces the risk of TB transmission, as TB is an airborne disease.
B) Incorrect. Having a strong immune system can help protect against TB infection, as a compromised immune system increases the risk of developing active TB disease from latent TB infection.
C) Correct. Close contact with someone who has active TB disease is a significant risk factor for TB transmission, as the bacteria can be transmitted through respiratory droplets.
D) Incorrect. While cleanliness and hygiene are important, excessive handwashing alone is not sufficient to prevent TB transmission, as the bacteria are primarily transmitted through the air.
Explanation
A) Correct. During latent TB infection, TB bacteria are in a dormant state and do not actively replicate or cause symptoms. They can become active and multiply if the immune system weakens.
B) Incorrect. While the immune system can control TB bacteria during latency, it does not immediately eliminate them.
C) Incorrect. Latent TB infection can occur in various parts of the body, not just the lungs, and it typically does not cause symptoms.
D) Incorrect. TB bacteria in latent infection are in a dormant state and do not actively multiply, although they remain viable.
Explanation
A) Correct. Using multiple drugs to treat TB reduces the risk of drug resistance development, as it targets the bacteria from different angles and makes it harder for them to become resistant to one or more drugs.
B) Incorrect. While using multiple drugs may help manage side effects by spreading the burden of treatment, the primary purpose is to prevent drug resistance.
C) Incorrect. Shortening the treatment duration is a goal, but it is not the primary purpose of using multiple drugs.
D) Incorrect. Although improving patient compliance is important, the primary purpose of using multiple drugs is to reduce drug resistance.
Explanation
A) Incorrect. LTBI does not always progress to active TB disease. Many individuals with LTBI do not develop active disease, especially if they have a strong immune system.
B) Incorrect. While the risk of progression is highest in the first two years after LTBI, it can occur at any time, and some individuals may progress years or even decades later.
C) Correct. LTBI rarely progresses to active TB, especially in individuals with a strong immune system. Most people with LTBI do not develop active disease.
D) Incorrect. LTBI carries a risk of progressing to active TB disease, although the risk is relatively low in many individuals.
Explanation
A) Correct. Granulomas are structures formed by the immune system in an attempt to encapsulate and contain TB bacteria, preventing their spread and aiding in their destruction.
B) Incorrect. Granulomas are not clusters of active TB bacteria; they are the body's response to containing the bacteria.
C) Incorrect. TB bacteria interact with the immune system within granulomas, leading to the formation of these structures.
D) Incorrect. Granulomas are not the primary site of TB bacteria replication; instead, they are formed to limit bacterial replication and spread.
Explanation
A) Incorrect. TB is primarily transmitted through the inhalation of respiratory droplets from an infected person and is not related to contaminated water or food sources.
B) Incorrect. Having a family history of TB can increase the risk, as there may be genetic factors that affect susceptibility to the disease.
C) Correct. Crowded and poorly ventilated settings increase the risk of TB transmission, as the bacteria can be easily spread in close quarters.
D) Incorrect. Underlying health conditions like HIV, diabetes, and immunosuppression can indeed increase the risk of TB due to compromised immune function.
Explanation
A) Incorrect. LTBI can progress to active TB disease if the immune system weakens or is compromised.
B) Incorrect. The risk of progression from LTBI to active TB is higher in individuals with weakened immune systems, not those with strong immune systems.
C) Correct. LTBI can remain dormant for years, and the risk of progression to active TB disease is higher when the immune system becomes compromised.
D) Incorrect. LTBI and active TB disease are distinct conditions, and LTBI does not always require immediate treatment. Treatment may be recommended for individuals at higher risk of progression to active disease.
Explanation
A) Incorrect. While multiple antibiotics may lead to symptom relief, the primary goal is to prevent drug resistance.
B) Correct. Combination therapy with multiple antibiotics is used to reduce the risk of drug-resistant TB, as it makes it more difficult for the bacteria to develop resistance to all drugs simultaneously.
C) Incorrect. Multiple antibiotics are used to target different aspects of TB treatment, not different types of TB bacteria.
D) Incorrect. While using multiple antibiotics can help manage side effects, the primary reason is to prevent drug resistance.
Explanation
A) Incorrect. Avoiding close contact alone may not be sufficient, as TB is primarily transmitted through the inhalation of respiratory droplets.
B) Incorrect. While wearing a surgical mask may offer some protection, it is not foolproof, especially in high-burden areas.
C) Incorrect. The BCG vaccine provides some protection against severe forms of TB in children but is not considered highly effective for preventing TB in adults.
D) Correct. Following good respiratory hygiene and avoiding crowded, poorly ventilated areas are essential measures to reduce the risk of TB transmission in high-burden areas.
Explanation
A) Incorrect. LTBI can be treated on an outpatient basis and typically does not require hospitalization.
B) Incorrect. While multiple antibiotics may be used, the duration of LTBI treatment is usually several months.
C) Incorrect. Treatment for LTBI is recommended to prevent progression to active TB, especially in individuals at higher risk.
D) Correct. Completing the recommended treatment course for LTBI is essential to reduce the risk of developing active TB disease.
Explanation
A) Incorrect. Joint pain and swelling are not typical symptoms of pulmonary TB.
B) Incorrect. Skin rash and itching are not common symptoms of pulmonary TB.
C) Correct. Persistent cough and sputum production are common symptoms of pulmonary TB, as the disease primarily affects the lungs.
D) Incorrect. Confusion and memory loss are not typical symptoms of pulmonary TB; they may occur in cases of disseminated or extrapulmonary TB.
Explanation
A) Incorrect. The symptoms described are more indicative of active TB disease rather than latent TB infection.
B) Correct. Night sweats, fatigue, and unexplained weight loss are classic symptoms of active TB disease.
C) Incorrect. TB exposure without infection typically does not present with these symptoms.
D) Incorrect. Atypical pneumonia may have different symptoms, and it is not the most likely diagnosis based on the symptoms provided.
Explanation
A) Incorrect. While coughing up blood can occur in TB, it should not be considered common and should always be evaluated.
B) Incorrect. Coughing up blood should prompt evaluation and treatment but does not necessarily require immediate hospitalization.
C) Incorrect. Coughing up blood is a concerning symptom that should not be dismissed as unrelated to TB.
D) Correct. Coughing up blood (hemoptysis) is a possible symptom of TB and should be reported to a healthcare provider for further assessment and management.
Explanation
A) Incorrect. Cervical lymphadenopathy is not specific to active pulmonary TB and can occur in extrapulmonary TB as well.
B) Incorrect. Allergic reactions typically do not result in cervical lymphadenopathy.
C) Correct. Cervical lymphadenopathy is often associated with extrapulmonary TB, as TB can affect various parts of the body, including lymph nodes.
D) Incorrect. Cervical lymphadenopathy is not necessarily indicative of a secondary bacterial infection.
Explanation
A) Incorrect. GERD may cause chest discomfort, but it is not typically described as pleuritic chest pain.
B) Incorrect. Muscular strain or injury is a possibility, but pleuritic chest pain suggests inflammation of the pleura.
C) Correct. Pleuritic chest pain is a symptom of pleurisy or pleural inflammation, which can occur in TB.
D) Incorrect. While anxiety or panic attacks can cause chest discomfort, pleuritic chest pain is more likely related to a physical condition, such as pleural inflammation.
Explanation
A) Incorrect. Chest X-rays are often used to assess lung involvement in TB but are not a primary screening test for TB infection.
B) Incorrect. Sputum culture is used to confirm the presence of TB bacteria in individuals with suspected active TB disease.
C) Correct. The Mantoux TST is a common screening test for TB infection. A small amount of PPD is injected under the skin, and the reaction is assessed after 48-72 hours.
D) Incorrect. CT scans may be used in TB diagnosis but are not typically used for initial screening of TB infection.
Explanation
A) Incorrect. A complete blood count (CBC) may reveal abnormalities associated with TB, but it does not directly confirm the presence of Mycobacterium tuberculosis in sputum samples.
B) Correct. Polymerase chain reaction (PCR) is a molecular test that can detect the genetic material of Mycobacterium tuberculosis in sputum samples, providing a confirmatory diagnosis.
C) Incorrect. The tuberculin skin test (TST) is a screening test for TB infection, not a test for confirming active disease in sputum samples.
D) Incorrect. Gram stain is a laboratory technique used to visualize the characteristics of bacterial cells but is not specific for Mycobacterium tuberculosis.
Explanation
A) Incorrect. Chest X-rays do not confirm the presence of TB bacteria but can indicate lung abnormalities associated with TB disease.
B) Correct. Chest X-rays are valuable in assessing the extent of lung involvement, the presence of cavities, and other abnormalities related to TB. This information helps guide treatment decisions.
C) Incorrect. Chest X-rays are not primarily used to detect TB infection in the blood; they focus on lung and chest abnormalities.
D) Incorrect. Chest X-rays are routinely used in the diagnosis and management of TB, especially for assessing lung involvement.
Explanation
A) Correct. Sputum samples are often most concentrated with TB bacteria when collected in the morning, as they have had time to accumulate overnight.
B) Incorrect. Rinsing the mouth before collecting sputum may dilute the sample and reduce its accuracy.
C) Incorrect. Deep coughing is encouraged to obtain samples from the lower respiratory tract, where TB bacteria are more likely to be present.
D) Incorrect. Sputum samples should be collected in specific containers designed for this purpose to maintain sample integrity and avoid contamination.
Explanation
A) Incorrect. A CT scan does not directly confirm the presence of TB bacteria but provides detailed images of the chest.
B) Incorrect. A CT scan is not used as a primary screening tool for TB infection in the bloodstream.
C) Correct. Chest CT scans are valuable for assessing the extent of lung involvement, detecting complications such as cavities or pleural effusions, and guiding treatment decisions in TB cases.
D) Incorrect. CT scans are commonly used in the evaluation and management of TB, especially for assessing lung abnormalities.
Explanation
A) Incorrect. It is not recommended to skip doses, but if the client experiences side effects, they should inform their healthcare provider rather than discontinuing treatment without guidance.
B) Incorrect. TB treatment must be completed in its entirety, even if the client starts to feel better. Stopping treatment prematurely can lead to drug resistance and a relapse of the disease.
C) Correct. Taking medications consistently and for the full duration of treatment is crucial to cure TB and prevent drug resistance.
D) Incorrect. Medications for TB should not be shared with family members or others, as they need individualized treatment and evaluation.
Explanation
A) Incorrect. While multiple medications may lead to symptom relief, the primary goal is to prevent drug resistance.
B) Incorrect. The duration of TB treatment is determined by the specific regimen and is not solely related to the number of medications.
C) Incorrect. Multiple medications in TB treatment may target different aspects of TB bacteria, but the primary purpose is to reduce the risk of drug resistance.
D) Correct. Using multiple medications in combination therapy makes it more difficult for TB bacteria to develop resistance to all drugs simultaneously, helping to prevent drug-resistant TB.
Explanation
A) Incorrect. Prompt reporting of side effects is important, even if they are not severe, as they may indicate the need for treatment adjustments.
B) Correct. Reporting side effects promptly allows the healthcare provider to assess and address any issues, potentially preventing treatment interruptions or complications.
C) Incorrect. While some side effects are expected, not all are normal, and reporting is necessary to ensure safe and effective treatment.
D) Incorrect. Waiting until the next appointment may lead to prolonged side effects and potential treatment complications.
Explanation
A) Incorrect. Completing treatment does not guarantee that the client will not develop TB again in the future, but it reduces the risk of a relapse.
B) Incorrect. Stopping treatment early does not reduce the risk of side effects; it increases the risk of drug resistance and a relapse.
C) Correct. Completing the full course of treatment is essential to prevent the development of drug-resistant TB and ensure effective treatment.
D) Incorrect. TB treatment should be completed as prescribed, regardless of the absence of symptoms, to prevent drug resistance and relapse.
Explanation
A) Incorrect. While it is essential to minimize close contact, isolation from family members is not typically necessary. Effective treatment and infection control measures can reduce the risk of transmission.
B) Incorrect. Wearing a mask at all times at home may not be necessary, but it is important to follow respiratory hygiene practices, especially when close to others.
C) Correct. Good hand hygiene and proper respiratory etiquette, such as covering the mouth when coughing, can help reduce the risk of TB transmission within the household.
D) Incorrect. TB can be transmitted in close household settings, so infection control measures are important to prevent transmission to family members.
Explanation
A) Incorrect. Skipping doses, even when feeling better, can lead to drug resistance and treatment failure.
B) Correct. Taking all medications as prescribed is essential to prevent the development of drug-resistant TB.
C) Incorrect. TB treatment should be completed in its entirety, even if symptoms improve before the regimen is finished.
D) Incorrect. TB medications should be taken as prescribed, not solely based on symptom severity.
Explanation
A) Incorrect. Isolating from family members and avoiding close contact is not typically necessary for clients with active TB who are on appropriate treatment.
B) Incorrect. While medication adherence is crucial, isolation is not a requirement for clients with active TB on treatment.
C) Correct. Clients with active TB who are on appropriate treatment and have had a reduction in infectiousness can generally return to their normal activities and interactions without isolation.
D) Incorrect. Isolation is not typically needed during TB treatment, as clients can resume their normal activities once their infectiousness has decreased.
Explanation
A) Incorrect. Covering the mouth when coughing is important, as it helps prevent the spread of respiratory droplets to others.
B) Correct. Coughing and sneezing into a tissue or the elbow helps contain respiratory droplets and reduces the risk of transmission.
C) Incorrect. Wearing a mask when coughing can be beneficial to prevent the spread of respiratory droplets, especially in crowded settings.
D) Incorrect. Ventilating living spaces by keeping windows and doors open, not closed, helps reduce the concentration of infectious particles in the air.
Explanation
A) Incorrect. One month is not typically sufficient for TB treatment; it usually lasts much longer.
B) Correct. The standard treatment duration for TB is at least six months to ensure complete eradication of the bacteria.
C) Incorrect. Two weeks is not an adequate duration for TB treatment; it is a prolonged treatment course.
D) Incorrect. While treatment duration can vary based on individual factors, the minimum duration is typically six months for active TB.
Explanation
A) Incorrect. Follow-up appointments are essential for monitoring progress and should not be limited to addressing side effects only.
B) Correct. Regular follow-up appointments are crucial for monitoring the client's response to treatment, ensuring medication adherence, and assessing for any complications.
C) Incorrect. Follow-up appointments should not be skipped, as they are important for assessing treatment effectiveness and making any necessary adjustments.
D) Incorrect. Follow-up appointments are typically not optional; they are a standard part of TB care to ensure successful treatment and minimize the risk of relapse.
Pneumonia
Explanation
A) Incorrect. Pneumonia is primarily a respiratory infection, not a gastrointestinal one.
B) Incorrect. Pneumonia primarily affects the lungs and is not related to joints and muscles.
C) Correct. Pneumonia is characterized by inflammation in the lungs and is often caused by infection.
D) Incorrect. Pneumonia is not an autoimmune disorder and does not primarily affect the skin.
Explanation
A) Incorrect. Pneumonia is typically an acute condition, and it does not lead to permanent scarring of the airways.
B) Incorrect. Pneumonia is not a genetic condition related to lung development.
C) Correct. Pneumonia is an acute respiratory infection characterized by inflammation in the lungs.
D) Incorrect. Pneumonia is a respiratory condition and does not primarily affect the cardiovascular system.
Explanation
A) Incorrect. Pneumonia is not a skin condition and does not cause itchy rashes.
B) Incorrect. Pneumonia is typically an acute condition, not a chronic one that slowly reduces lung function.
C) Correct. Pneumonia is characterized by sudden and acute infection and inflammation of the air sacs in the lungs.
D) Incorrect. Pneumonia primarily affects the respiratory system, not the digestive system.
Explanation
A) Incorrect. Pneumonia is not rare; it is a relatively common respiratory infection.
B) Incorrect. Pneumonia primarily affects the lungs, not the brain.
C) Correct. Pneumonia is a common respiratory infection that can affect the lungs.
D) Incorrect. Pneumonia does not lead to scarring of the vocal cords; it primarily affects the lungs.
Explanation
A) Incorrect. Pneumonia is not primarily caused by excessive heat and sunlight.
B) Incorrect. Pneumonia can affect individuals of all age groups, not just children.
C) Correct. Pneumonia can be caused by various microorganisms, including bacteria and viruses.
D) Incorrect. While smoking can increase the risk of respiratory infections, pneumonia can result from various causes, not solely from smoking.
Explanation
A) Incorrect. Pneumonia is not primarily caused by exposure to environmental conditions like cold and wet environments.
B) Incorrect. While viruses can cause pneumonia, it is not solely due to direct viral damage to lung tissue.
C) Correct. Pneumonia is characterized by inflammation and infection of the air sacs (alveoli) in the lungs.
D) Incorrect. Allergic reactions can lead to respiratory symptoms, but they are not the primary cause of pneumonia.
Explanation
A) Incorrect. Narrowing of the bronchial tubes is more characteristic of conditions like asthma, not pneumonia.
B) Incorrect. Inflammation of the pleura is known as pleuritis or pleurisy, and it is different from pneumonia.
C) Correct. Pneumonia typically involves the infection and inflammation of the alveoli, the small air sacs in the lungs where gas exchange occurs.
D) Incorrect. Blood clots in the lung arteries are associated with pulmonary embolism, not pneumonia.
Explanation
A) Incorrect. Pneumonia primarily affects the respiratory system, not the heart's ability to pump blood.
B) Incorrect. Narrowing of the airways is not the primary feature of pneumonia; it is more characteristic of conditions like asthma.
C) Incorrect. While mucus production can increase in response to infection, it is not the primary cause of pneumonia.
D) Correct. In pneumonia, infection and inflammation of the air sacs (alveoli) in the lungs are key features of the pathophysiology.
Explanation
A) Incorrect. Pneumonia does not cause the air sacs to contract but can lead to their inflammation and reduced function.
B) Correct. Inflammation in pneumonia can disrupt the normal exchange of oxygen and carbon dioxide in the alveoli, leading to respiratory symptoms.
C) Incorrect. Pneumonia does not typically lead to an overproduction of surfactant; instead, it can affect the function of surfactant.
D) Incorrect. Pneumonia does impact the exchange of oxygen and carbon dioxide in the lungs, as it affects the function of the alveoli.
Explanation
A) Incorrect. Bacterial pneumonia is not primarily an overreaction of the
immune system but a result of bacterial infection.
B) Correct. Bacterial pneumonia involves direct damage to lung tissue and airways by invading bacteria.
C) Incorrect. While bacteria can enter the bloodstream and spread to the lungs, this is not the primary mechanism of bacterial pneumonia.
D) Incorrect. Inhalation of contaminated air can introduce bacteria to the respiratory tract, but it is not the sole cause of bacterial pneumonia.
Explanation
A) Incorrect. Pneumonia is not primarily caused by exposure to cold weather or low temperatures; infections are the main contributors.
B) Correct. Pneumonia can be caused by various infectious agents, including bacteria, viruses, and fungi.
C) Incorrect. While indoor air pollutants can contribute to respiratory issues, pneumonia is not exclusively caused by them.
D) Incorrect. Pneumonia is not solely a hereditary condition but is primarily caused by infectious agents.
Explanation
A) Incorrect. Good hand hygiene and avoiding contact with others can help prevent infections but are not the primary risk factors for pneumonia.
B) Incorrect. Chronic diseases, such as diabetes and heart disease, can increase the risk of pneumonia, especially when they weaken the immune system.
C) Incorrect. Age is a risk factor for pneumonia, but being young and healthy does not eliminate the risk, and other factors also play a role.
D) Correct. Smoking, chronic lung conditions (e.g., COPD), and a weakened immune system are significant risk factors for pneumonia.
Explanation
A) Incorrect. Vaccination can play a role in preventing pneumonia, especially certain types.
B) Incorrect. Vaccination can be effective against both bacterial and viral forms of pneumonia, depending on the vaccine.
C) Correct. Vaccination can help prevent specific types of bacterial pneumonia, such as those caused by Streptococcus pneumoniae.
D) Incorrect. While vaccination is a valuable prevention measure, other measures like good hygiene and infection control are also important.
Explanation
A) Incorrect. While genetics can play a role in susceptibility to some infections, it is not the only risk factor for pneumonia.
B) Incorrect. Being young and having strong immunity does not eliminate the risk of pneumonia, and other factors are also important.
C) Correct. Chronic conditions such as asthma and diabetes can weaken the immune system, making individuals more susceptible to pneumonia.
D) Incorrect. Smoking and alcohol use can increase the risk of pneumonia, especially when they weaken the respiratory and immune systems.
Explanation
A) Incorrect. Oral hygiene can influence pneumonia risk, especially in certain populations.
B) Correct. Maintaining good oral hygiene can reduce the risk of aspiration pneumonia, which is more common in older adults and individuals with swallowing difficulties.
C) Incorrect. While oral health is related to gastrointestinal and overall health, it can also affect the respiratory system and pneumonia risk.
D) Incorrect. Good oral hygiene is important in reducing the risk of pneumonia, but its impact can vary among different populations and risk factors.
Explanation
A) Incorrect. While chest pain can occur in pneumonia, it doesn't necessarily indicate severe lung damage. It is often due to inflammation of the pleura (lining around the lungs).
B) Incorrect. Chest pain in pneumonia can be related to the inflammatory process affecting the pleura.
C) Incorrect. Chest pain in pneumonia can occur without coughing and sputum production, especially if it's related to pleurisy.
D) Correct. Chest pain in pneumonia is often caused by pleurisy, which is inflammation of the pleural lining around the lungs.
Explanation
A) Incorrect. Hyperventilation typically leads to increased breath sounds, not decreased.
B) Correct. Decreased breath sounds in a specific area can be indicative of pneumonia affecting that lung region.
C) Incorrect. Decreased breath sounds are not a normal finding and should be further investigated, especially in the context of suspected pneumonia.
D) Incorrect. While a lung tumor can cause abnormal breath sounds, decreased breath sounds in the context of suspected pneumonia are more likely related to the infection.
Explanation
A) Incorrect. Fatigue can be related to pneumonia, especially due to the body's response to infection.
B) Correct. Pneumonia can lead to fatigue because the body's increased metabolic demands during infection can result in feeling weak and tired.
C) Incorrect. While coughing can disrupt sleep, fatigue in pneumonia is not solely due to lack of sleep.
D) Incorrect. Fatigue in pneumonia may persist until the infection is effectively treated and the body's energy levels are restored.
Explanation
A) Incorrect. A bluish tint to the skin and lips (cyanosis) is not a normal skin tone variation and should be assessed further.
B) Correct. Central cyanosis, indicated by bluish discoloration of the skin and lips, can be a sign of oxygen deprivation and should be reported to the healthcare provider.
C) Incorrect. While providing comfort measures is important, addressing cyanosis requires a medical evaluation.
D) Incorrect. Hydration is essential, but central cyanosis is more concerning and should be evaluated by a healthcare provider.
Explanation
A) Incorrect. Greenish-yellow sputum may indicate the presence of infection, but it does not necessarily indicate improvement.
B) Correct. Sputum color can provide clues about the type of bacteria or pathogens causing the infection, which can guide antibiotic treatment.
C) Incorrect. While a change in sputum color should be reported, it is not always an emergency. The significance depends on other clinical factors.
D) Incorrect. Sputum color can be significant in pneumonia diagnosis and treatment, as it may indicate the type of infection.
Explanation
A) Incorrect. While a chest X-ray is a valuable tool in diagnosing pneumonia, additional tests are often required for a comprehensive evaluation.
B) Correct. Blood tests, including a complete blood count (CBC), can provide important information to support the diagnosis of pneumonia, such as elevated white blood cell count.
C) Incorrect. A physical examination is essential, but it alone is not sufficient to diagnose pneumonia definitively.
D) Incorrect. A sputum culture is primarily used to identify the specific causative bacteria or pathogens in pneumonia, not to assess lung function.
Explanation
A) Incorrect. While a chest X-ray is valuable in diagnosing pneumonia, it does not typically identify the specific causative pathogen.
B) Correct. A chest X-ray is crucial for assessing the extent of lung involvement and detecting complications such as pleural effusion.
C) Incorrect. Chest X-rays primarily focus on lung and chest cavity assessment, not heart function.
D) Incorrect. A chest X-ray informs the diagnosis and management of pneumonia but does not determine antibiotic treatment.
Explanation
A) Incorrect. While sputum testing can provide information about the causative pathogen, it is not the primary purpose of collecting sputum in pneumonia diagnosis.
B) Incorrect. Sputum testing can help identify the causative pathogen, but its primary purpose is to confirm the presence of pneumonia and assess its severity.
C) Incorrect. Sputum samples are not primarily used to assess lung function but rather to detect the presence of infectious agents.
D) Correct. Collecting sputum helps confirm the diagnosis of pneumonia and provides information about the severity and causative pathogen.
Explanation
A) Incorrect. Oxygen saturation measurements do not determine the type of pneumonia but rather assess oxygen levels in the blood.
B) Incorrect. While low oxygen saturation can indicate severe pneumonia, it does not directly indicate the severity of pneumonia.
C) Incorrect. Oxygen saturation measurements are not typically used for the early diagnosis of pneumonia but rather for monitoring oxygenation during treatment.
D) Correct. Oxygen saturation measurements provide information about how effectively the lungs are oxygenating the blood, which is important in pneumonia management.
Explanation
A) Incorrect. While a sputum culture is part of pneumonia diagnosis, its primary purpose is to identify the causative bacteria or pathogen.
B) Incorrect. While a sputum culture can provide information about the specific causative pathogen, its primary role is to identify the pathogen itself.
C) Incorrect. Sputum cultures are not used to assess lung function but rather to detect infectious agents.
D) Correct. A sputum culture is essential for identifying the specific bacteria or pathogen causing pneumonia, which helps guide antibiotic treatment.
Explanation
A) Incorrect. Completing antibiotics is not primarily about treating symptoms faster but rather ensuring complete eradication of the infection.
B) Correct. Finishing all the antibiotics is crucial to prevent the development of antibiotic resistance and ensure the infection is completely treated.
C) Incorrect. Saving leftover antibiotics for future use is not recommended, as the full course may be needed for a future infection or a different strain of bacteria.
D) Incorrect. Stopping antibiotics early does not reduce the risk of side effects; it increases the risk of treatment failure and antibiotic resistance.
Explanation
A) Incorrect. Oxygen therapy does not directly kill bacteria but helps support the body's oxygen needs during infection.
B) Correct. Oxygen therapy is used to improve lung function and maintain proper oxygen levels in the blood, which can be compromised during pneumonia.
C) Incorrect. Oxygen therapy and antibiotic treatment serve different purposes, and oxygen therapy does not reduce the need for antibiotics.
D) Incorrect. While oxygen therapy can support recovery, it does not speed up the recovery process on its own.
Explanation
A) Incorrect. Returning to work immediately may not be advisable, and it's essential to consult with a healthcare provider for guidance.
B) Correct. Gradually resuming work as tolerated is a reasonable approach, but it's important to discuss with a healthcare provider to ensure it's safe and appropriate.
C) Incorrect. Avoiding work completely for a month is not necessary for all clients with pneumonia and should be determined based on individual circumstances.
D) Incorrect. Complete bed rest and avoiding all physical activities are generally not recommended for pneumonia recovery but should be guided by healthcare provider recommendations.
Explanation
A) Incorrect. Alcohol can interact with antibiotics, and it's generally not recommended to consume them together.
B) Correct. Avoiding alcohol while taking antibiotics is a common recommendation to prevent potential interactions and reduce the risk of side effects.
C) Incorrect. Consuming alcohol with a meal may not eliminate potential interactions between alcohol and antibiotics.
D) Incorrect. Alcohol can interact with antibiotics, and it's advisable to avoid excessive alcohol consumption while on antibiotics.
Explanation
A) Incorrect. Antibiotic treatment for pneumonia is typically more extended than just a few days, but the duration varies based on individual factors.
B) Incorrect. While two weeks may be a standard duration for some cases, it varies depending on factors like pneumonia severity and the specific antibiotic regimen.
C) Correct. The duration of antibiotic treatment for pneumonia is individualized and depends on various factors, including the type and severity of pneumonia.
D) Incorrect. The duration of antibiotic treatment should be determined by the healthcare provider's instructions, not solely based on fever resolution.
Explanation
A) Incorrect. Antibiotics should be taken for the full prescribed course, even if symptoms improve before completion.
B) Correct. Completing the full course of antibiotics is essential to ensure that the infection is completely eradicated and to prevent recurrence or antibiotic resistance.
C) Incorrect. The duration of antibiotic treatment should be based on the healthcare provider's instructions, not solely on the resolution of fever.
D) Incorrect. Antibiotics should not be saved for future use or shared with others; they should be taken as prescribed and disposed of properly if not used.
Explanation
A) Incorrect. Alternating between acetaminophen and ibuprofen can be effective for fever control, but it's important to consult a healthcare provider for specific guidance.
B) Incorrect. Fever management may be necessary, especially if the fever is causing discomfort or other symptoms.
C) Correct. It is essential to consult a healthcare provider before combining or alternating medications, as there may be specific considerations based on the individual's health status and other medications they are taking.
D) Incorrect. Taking both medications simultaneously is not a recommended approach without guidance from a healthcare provider.
Explanation
A) Incorrect. Specific fluid requirements can vary among individuals, and an arbitrary amount may not be suitable for everyone.
B) Incorrect. Staying adequately hydrated is important during illness, especially when experiencing fever and respiratory symptoms.
C) Incorrect. While overhydration can be a concern, clients with pneumonia should drink enough to maintain proper hydration.
D) Correct. Monitoring urine color and aiming for pale yellow is a practical approach to ensuring adequate hydration.
Explanation
A) Correct. Frequent coughing and deep breathing exercises are essential to prevent complications such as pneumonia-associated atelectasis and maintain lung function. Clients should be encouraged to perform these exercises hourly, including during the night.
B) Incorrect. While performing exercises three times a day may be better than not doing them at all, more frequent exercises are recommended for clients with pneumonia.
C) Incorrect. Waiting until shortness of breath occurs may not provide adequate prevention of respiratory complications.
D) Incorrect. Coughing and deep breathing exercises are beneficial for maintaining lung function and preventing complications in clients with pneumonia.
Explanation
A) Incorrect. Resuming strenuous exercise immediately after pneumonia treatment may not be advisable, as the body needs time to recover.
B) Incorrect. Avoiding exercise completely is not necessary, but a gradual approach is recommended.
C) Correct. Gradually reintroducing exercise, starting with light activities and increasing intensity as tolerated, is a safe approach after recovering from pneumonia.
D) Incorrect. Exercising at the same intensity as before illness may be too strenuous for the body immediately after treatment and recovery.
Asthma
Explanation
A) Incorrect. Asthma is not contagious, and it is not caused by bacteria.
B) Correct. Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways.
C) Incorrect. Asthma is not a skin disorder and does not involve itchy rashes.
D) Incorrect. Asthma is not an autoimmune disorder and does not primarily affect the joints.
Explanation
A) Incorrect. Asthma can affect individuals of all age groups, not just the elderly.
B) Incorrect. Asthma primarily affects the respiratory system, not the digestive system.
C) Correct. Asthma is a chronic condition characterized by symptoms such as difficulty breathing and wheezing.
D) Incorrect. Asthma is a chronic condition, and while symptoms may improve with treatment, it does not typically resolve on its own within a few days.
Explanation
A) Incorrect. Asthma primarily affects the respiratory system, not the cardiovascular system.
B) Incorrect. While there can be a genetic predisposition to asthma, it is not solely a genetic condition.
C) Correct. Asthma is a chronic respiratory disease characterized by airway inflammation and narrowing, leading to difficulty breathing.
D) Incorrect. Asthma is not a bacterial infection but a chronic respiratory condition.
Explanation
A) Incorrect. Asthma is not rare; it is a relatively common chronic condition.
B) Incorrect. Asthma is not caused by a virus but is related to airway inflammation.
C) Incorrect. Asthma is not a skin condition and does not involve hives and itching.
D) Correct. Asthma is a common chronic respiratory condition characterized by airway inflammation and narrowing.
Explanation
A) Incorrect. Asthma primarily affects the respiratory system, not the joints and muscles.
B) Incorrect. Asthma is not an autoimmune disorder and does not primarily involve inflammation of the skin.
C) Incorrect. While asthma involves inflammation, it is not typically an acute respiratory infection.
Explanation
A) Incorrect. Asthma is not primarily caused by bacterial infections.
B) Incorrect. While excess mucus can contribute to asthma symptoms, it is not the primary mechanism.
C) Correct. Asthma is characterized by chronic inflammation of the airways and increased reactivity, leading to airway narrowing and symptoms.
D) Incorrect. Asthma primarily involves airway inflammation and narrowing, not a lack of oxygen in the bloodstream.
Explanation
A) Incorrect. Mast cells do not release hormones that relax airway muscles; they are involved in inflammation.
B) Correct. Mast cells release inflammatory substances in response to allergens, leading to bronchoconstriction and inflammation in asthma.
C) Incorrect. Mast cells are not primarily involved in clearing excess mucus from the airways.
D) Incorrect. Mast cells do not produce antibodies to protect against asthma attacks.
Explanation
A) Incorrect. Asthma leads to airway narrowing, not widening.
B) Incorrect. While chronic inflammation can lead to airway remodeling over time, it does not make the airway walls more rigid in the acute phase.
C) Correct. Asthma is characterized by inflammation and narrowing of the airways, which can lead to symptoms like wheezing and difficulty breathing.
D) Incorrect. Asthma does affect the structure of the airways, primarily through inflammation and airway remodeling in the long term.
Explanation
A) Incorrect. Eosinophils do not release hormones that relax airway muscles.
B) Incorrect. Eosinophils are not primarily involved in antibody production in asthma.
C) Incorrect. Eosinophils are not responsible for clearing excess mucus from the airways.
D) Correct. Eosinophils are white blood cells that contribute to inflammation and airway damage in asthma by releasing inflammatory substances.
Explanation
A) Incorrect. Bronchial smooth muscle is involved in asthma, particularly in airway constriction.
B) Correct. In asthma, bronchial smooth muscle contracts and narrows the airways, contributing to symptoms like wheezing and shortness of breath.
C) Incorrect. Bronchial smooth muscle's primary role in asthma is not to clear mucus from the airways.
D) Incorrect. Bronchial smooth muscle does not release antibodies to protect against asthma attacks.
Explanation
A) Incorrect. Bacterial infections are not the primary cause of asthma; it is more related to inflammation and airway hyperreactivity.
B) Incorrect. Genetics can indeed play a role in the development of asthma.
C) Correct. Environmental factors, including allergens and irritants, are significant contributors to asthma development and exacerbation.
D) Incorrect. While emotional stress and anxiety can exacerbate asthma symptoms, they are not the sole triggers of the condition.
Explanation
A) Incorrect. Being physically active and spending time outdoors can have positive effects on respiratory health, reducing the risk of asthma.
B) Correct. Exposure to secondhand smoke, especially during childhood, is a significant risk factor for asthma.
C) Incorrect. A diet rich in fruits and vegetables is generally associated with better overall health but is not a direct risk factor for asthma.
D) Incorrect. Avoiding all exercise is not necessary for asthma prevention and can lead to other health problems. Properly managed exercise can be beneficial for individuals with asthma.
Explanation
A) Incorrect. Exposure to certain allergens from pets can increase the risk of asthma, especially in individuals with allergic tendencies.
B) Incorrect. Living in an urban area with high levels of air pollution can contribute to the development and exacerbation of asthma.
C) Incorrect. A family history of asthma is a known risk factor for the condition.
D) Correct. Respiratory infections, especially during early childhood, can be a risk factor for the development of asthma.
Explanation
A) Incorrect. Allergies are related to the development and exacerbation of asthma in some cases.
B) Correct. Allergies, especially allergic rhinitis, are known risk factors for the development of asthma in susceptible individuals.
C) Incorrect. While allergies can have a protective effect against asthma in some cases (the hygiene hypothesis), this is not universally true.
D) Incorrect. Allergies are one of several potential factors that can contribute to asthma, but they are not the sole cause.
Explanation
A) Incorrect. Regular participation in outdoor activities can be beneficial for respiratory health and may reduce the risk of asthma in some cases.
B) Incorrect. A history of good respiratory health is not a risk factor for asthma.
C) Correct. Frequent respiratory infections, especially during childhood, can increase the risk of asthma.
D) Incorrect. Having a diet low in processed foods may be associated with better overall health but is not a direct risk factor for asthma.
Explanation
A) Incorrect. Severe coughing can occur during an asthma attack but is not typically considered an early warning sign.
B) Correct. Wheezing is often an early sign of airway constriction and can precede other symptoms of an asthma attack.
C) Incorrect. Chest pain and discomfort are not typical early warning signs of asthma.
D) Incorrect. Difficulty speaking in full sentences is a more advanced symptom that may occur during an asthma attack.
Explanation
A) Incorrect. A persistent low-grade fever is not a typical asthma symptom.
B) Incorrect. A sore throat and runny nose are more characteristic of upper respiratory infections or allergies, not asthma.
C) Incorrect. A sharp, stabbing pain in the chest is not a classic asthma symptom and should be evaluated by a healthcare provider.
D) Correct. Frequent coughing and the production of thick mucus can be indicative of asthma, especially during exacerbations.
Explanation
A) Incorrect. Intermittent shortness of breath during physical activity is common in asthma but does not necessarily indicate a severe attack.
B) Incorrect. Occasional coughing and wheezing at night can be part of asthma but do not necessarily signal a severe attack.
C) Correct. Persistent shortness of breath, especially when present at rest, is a potential indicator of a severe asthma attack and should be taken seriously.
D) Incorrect. Mild chest tightness after exposure to allergens is a common symptom of asthma but may not necessarily indicate a severe attack.
Explanation
A) Incorrect. Improvement of asthma symptoms when lying down is not typical, and nighttime symptoms often worsen in asthma.
B) Correct. Waking up in the middle of the night with a cough and difficulty breathing is a common symptom of nighttime worsening in asthma.
C) Incorrect. While some individuals with asthma may not experience nighttime symptoms, this is not typical.
D) Incorrect. Improved lung function and increased energy at night are not characteristic of asthma; in fact, asthma symptoms often worsen at night.
Explanation
A) Correct. Frequent use of a rescue inhaler is often an early sign that asthma symptoms are worsening and may precede an exacerbation.
B) Incorrect. Rarely experiencing chest tightness does not necessarily indicate the early stages of an asthma exacerbation.
C) Incorrect. The absence of wheezing or coughing is not an early indicator of worsening asthma symptoms; wheezing is a common asthma symptom.
D) Incorrect. Infrequent nighttime awakenings due to asthma may be a sign of well-controlled asthma but do not necessarily signal an exacerbation.
Explanation
A) Incorrect. An ECG is used to assess heart function, not lung function.
B) Incorrect. MRI is a diagnostic imaging technique used to visualize internal structures but is not typically used for asthma diagnosis.
C) Incorrect. Chest X-rays may be performed to rule out other conditions but are not a primary test for asthma diagnosis.
D) Correct. Spirometry is a common lung function test used to assess airflow and determine the presence and severity of asthma.
Explanation
A) Incorrect. Measuring oxygen levels in the blood is typically done using pulse oximetry or arterial blood gas tests, not a bronchial provocation test.
B) Correct. A bronchial provocation test evaluates how the airways respond to substances that can trigger bronchoconstriction, helping to diagnose asthma.
C) Incorrect. Visualizing airways using a special camera is usually done through bronchoscopy, not a bronchial provocation test.
D) Incorrect. Checking for specific antibodies related to asthma is not a primary diagnostic test for asthma; it is more commonly associated with allergies.
Explanation
A) Incorrect. Peak flow measurements are not primarily used to assess the response to allergy medications.
B) Incorrect. Assessing heart function is not the purpose of peak flow measurements; they focus on lung function.
C) Correct. Peak flow readings are a valuable tool in assessing lung function and the severity of asthma symptoms, helping guide treatment decisions.
D) Incorrect. Evaluating bone density and fracture risk is not related to peak flow monitoring.
Explanation
A) Correct. A CBC can detect elevated levels of white blood cells (eosinophils) associated with airway inflammation in asthma.
B) Incorrect. Serum cholesterol levels are not a primary diagnostic test for asthma.
C) Incorrect. Urinalysis is used to assess kidney function and detect abnormalities in the urine, not for asthma diagnosis.
D) Incorrect. ESR is a nonspecific test used to detect inflammation in the body but is not specific to asthma diagnosis.
Explanation
A) Incorrect. A blood test for specific IgE antibodies can detect allergen-specific antibodies but is not the same as a skin prick test.
B) Incorrect. A chest X-ray is used to visualize the lungs and is not a test for allergies.
C) Incorrect. A pulmonary function test (PFT) assesses lung function but does not test for allergies.
D) Correct. A skin prick test, also known as a skin allergy test or scratch test, involves applying small amounts of allergens to the skin and monitoring for allergic reactions, helping identify specific allergens triggering asthma symptoms.
Explanation
A) Incorrect. An asthma action plan primarily focuses on managing acute symptoms and exacerbations, not long-term treatment.
B) Incorrect. While asthma action plans may include recommendations for daily activities, their primary purpose is to address asthma exacerbations.
C) Correct. An asthma action plan is designed to help individuals manage asthma attacks by providing instructions on when and how to use rescue medications, as well as when to seek medical assistance.
D) Incorrect. While asthma action plans may mention triggers, their primary function is to guide actions during asthma attacks.
Explanation
A) Incorrect. Inhaled corticosteroids (ICS) are not typically used for quick relief during asthma attacks; they are primarily for long-term control.
B) Incorrect. Relaxing airway muscles is the function of bronchodilators, not ICS.
C) Correct. ICS medications are anti-inflammatory drugs that reduce airway inflammation, making them a cornerstone of asthma management for long-term control.
D) Incorrect. ICS are not used to treat acute allergic reactions; they are aimed at preventing asthma symptoms over time.
Explanation
A) Incorrect. A decrease in peak flow measurements typically indicates worsening asthma, not improved control.
B) Incorrect. While an increase in rescue inhaler use may be necessary during an exacerbation, it does not address the underlying issue of worsening asthma.
C) Correct. A decrease in peak flow measurements is a sign of declining lung function, suggesting that asthma may be worsening. Following the asthma action plan is essential in this situation.
D) Incorrect. Peak flow measurements are a valuable tool in asthma management and are related to monitoring and controlling asthma symptoms.
Explanation
A) Incorrect. Reducing airway inflammation is the primary function of inhaled corticosteroids, not bronchodilators.
B) Correct. Bronchodilators, such as beta-agonists, help relax the smooth muscles surrounding the airways, which can improve airflow and relieve bronchoconstriction in asthma.
C) Incorrect. Bronchodilators primarily provide quick relief during asthma attacks but do not prevent asthma symptoms over the long term.
D) Incorrect. Bronchodilators are not used to treat allergic reactions; they are used to relieve acute bronchoconstriction associated with asthma.
Explanation
A) Incorrect. Smoking is a significant asthma trigger, and even occasional smoking can worsen asthma symptoms.
B) Incorrect. Feather pillows may contain allergens that can exacerbate asthma in individuals sensitive to these allergens.
C) Incorrect. Frequent vacuuming can stir up dust and allergens, potentially worsening asthma symptoms, rather than improving indoor air quality.
D) Correct. Outdoor allergens like pollen can trigger asthma symptoms in many individuals, so avoiding exposure is an important part of asthma management.
Explanation
A) Incorrect. Scented candles and air fresheners can release irritants that may trigger asthma symptoms in some individuals, so they should be avoided.
B) Correct. Cold air is a known asthma trigger, and individuals with asthma should take precautions during cold weather to minimize exposure.
C) Incorrect. Dairy products can trigger asthma symptoms in some people who have dairy allergies or sensitivities.
D) Incorrect. Pet fur and dander can be potent asthma triggers, and regular cleaning and reducing exposure to these allergens are essential for asthma management.
Explanation
A) Incorrect. Breathing too forcefully into the peak flow meter can result in artificially high readings. The client should use a steady, controlled breath.
B) Incorrect. Exhaling forcefully can also lead to inaccurate readings. Gentle exhalation is recommended.
C) Incorrect. The peak flow meter should be exhaled into, not inhaled from.
D) Correct. The correct technique involves standing with feet together and exhaling gently but forcefully into the peak flow meter.
Explanation
A) Incorrect. A spacer does not increase the force of the medication but rather optimizes the delivery.
B) Incorrect. The purpose of a spacer is not related to portability; it's about enhancing the effectiveness of the inhaler.
C) Incorrect. Using a spacer does not allow for larger doses; it improves the distribution of the prescribed dose.
D) Correct. A spacer device helps ensure that more of the medication reaches the lungs by slowing down and dispersing the spray from the inhaler, making it easier to inhale effectively.
Explanation
A) Incorrect. Rescue inhalers are typically not used as a daily preventive measure but are reserved for acute symptom relief.
B) Incorrect. While exercise-induced asthma is a valid reason to use a rescue inhaler, it should also be used when experiencing other asthma symptoms.
C) Correct. Rescue inhalers are meant for quick relief during asthma symptoms or exacerbations, and their use should be guided by symptoms or healthcare provider instructions.
D) Incorrect. There is no specific benefit to using a rescue inhaler before bedtime unless asthma symptoms are present at that time.
Explanation
A) Incorrect. Spacers can be beneficial for both children and adults, depending on their ability to use the inhaler effectively.
B) Incorrect. A spacer does not deliver medication directly into the bloodstream but optimizes delivery to the lungs.
C) Correct. Using a spacer reduces the risk of side effects, such as oral thrush, associated with some inhaled medications by ensuring more targeted delivery to the lungs.
D) Incorrect. Spacers are designed to make inhalers easier to use correctly, not more challenging.
Chronic Obstructive Pulmonary Disease (COPD)
Explanation
A) Incorrect. The correct acronym is "COPD," and it stands for Chronic Obstructive Pulmonary Disease.
B) Correct. COPD is an abbreviation for Chronic Obstructive Pulmonary Disease, which includes chronic bronchitis and emphysema.
C) Incorrect. "Cardiovascular" is not part of the COPD acronym.
D) Incorrect. "Occupational" is not part of the COPD acronym.
Explanation
A) Incorrect. While smoking is a major risk factor, other factors can contribute to COPD development.
B) Incorrect. While allergies and air pollution may affect respiratory health, they are not primary risk factors for COPD.
C) Incorrect. Occupational exposure and genetics can play a role in COPD, but they are not the primary risk factors.
D) Correct. Smoking is a significant risk factor, but exposure to secondhand smoke and occupational dust can also increase the risk of developing COPD.
Explanation
A) Incorrect. Abdominal pain and nausea are not typical symptoms of COPD.
B) Correct. Common symptoms of COPD include a persistent cough, shortness of breath, and increased mucus production.
C) Incorrect. Skin rashes and joint swelling are not characteristic symptoms of COPD.
D) Incorrect. High fever and chest pain are not typical symptoms of COPD.
Explanation
A) Incorrect. COPD primarily affects the airways and lung parenchyma, not blood vessels.
B) Correct. The term "obstructive" in COPD refers to the narrowing and obstruction of the airways, which leads to airflow limitation.
C) Incorrect. COPD is characterized by a decrease in lung elasticity, not an increase.
D) Incorrect. The weakening of the diaphragm is not typically described as the "obstructive" aspect of COPD.
Explanation
A) Incorrect. While heart failure can occur in severe cases of COPD, it is not the primary reason for the progression of the condition.
B) Correct. The progressive nature of COPD is mainly attributed to the loss of lung elasticity and airflow limitation over time.
C) Incorrect. While infections can exacerbate COPD symptoms, they are not the primary cause of disease progression.
D) Incorrect. An increase in lung capacity is not a characteristic of COPD progression; it typically involves reduced lung function.
Explanation
A) Incorrect. While respiratory muscle weakness can contribute, loss of lung elasticity is a primary factor in COPD-related shortness of breath.
B) Incorrect. Overproduction of mucus can be a symptom of COPD, but it's not the primary cause of shortness of breath.
C) Correct. Loss of lung elasticity, along with airflow limitation, leads to difficulty in breathing in COPD.
D) Incorrect. Shortness of breath in COPD is primarily a physiological response to lung changes, not solely related to anxiety.
Explanation
A) Incorrect. In COPD, the airways become narrower, making it harder, not easier, to breathe.
B) Incorrect. COPD primarily involves changes in the airways and lung parenchyma, not just the lung tissue itself.
C) Incorrect. Chronic bronchitis in COPD is associated with increased mucus production and inflammation but not increased lung elasticity.
D) Correct. Emphysema, a subtype of COPD, is characterized by the destruction of the walls of the air sacs, leading to reduced elasticity and airflow limitation.
Explanation
A) Incorrect. In COPD, inflammation primarily affects the airways and lung tissue, not joints and bones.
B) Incorrect. Inflammation is a significant component of COPD, and it's not solely due to smoking.
C) Correct. Inflammation in COPD is primarily centered in the airways and lung parenchyma.
D) Incorrect. COPD-related inflammation is not related to the skin.
Explanation
A) Correct. Smoking is a major cause of COPD, and it damages the air sacs in the lungs, contributing to the development of the condition.
B) Incorrect. Smoking has widespread effects on the respiratory system, not just the throat and vocal cords.
C) Incorrect. Smoking is a leading cause of COPD, but it doesn't cause high blood pressure in the lungs (pulmonary hypertension).
D) Incorrect. While genetics can play a role, smoking is a significant factor in COPD development.
Explanation
A) Incorrect. While infections can exacerbate COPD symptoms, the chronic cough is primarily due
to narrowed airways and increased mucus production.
B) Correct. In COPD, narrowed airways, increased mucus production, and chronic inflammation contribute to a persistent cough.
C) Incorrect. COPD primarily affects the airways and lung tissue, not the vocal cords.
D) Incorrect. A chronic cough is a common symptom of COPD and is directly related to the condition.
Explanation
A) Correct. Smoking is the primary risk factor for COPD, and not smoking significantly reduces the risk.
B) Incorrect. Exposure to secondhand smoke can increase the risk of COPD.
C) Incorrect. Occupational exposure to dust and pollutants without protective measures can contribute to COPD development.
D) Incorrect. A family history of COPD can indeed increase the risk of the condition.
Explanation
A) Incorrect. While smoking is a major risk factor for COPD, air pollution can still exacerbate the condition.
B) Correct. Air pollution, including particulate matter and irritants, can aggravate COPD symptoms and lead to exacerbations.
C) Incorrect. Using an inhaler alone may not fully protect against the effects of air pollution on COPD.
D) Incorrect. Both outdoor and indoor air quality can impact COPD, but outdoor air pollution can also contribute to symptom exacerbation.
Explanation
A) Correct. A family history of COPD is a valid risk factor for the condition.
B) Correct. Smoking is indeed the leading cause of COPD.
C) Incorrect. Exposure to indoor pollutants like cooking fumes and indoor smoking can contribute to COPD.
D) Correct. Occupational exposure to dust and chemicals is a recognized risk factor for COPD.
Explanation
A) Incorrect. Genetics can play a role in COPD risk, but lifestyle choices, especially avoiding smoking, are still crucial in prevention.
B) Incorrect. A family history of COPD can increase the risk, so it is a relevant factor.
C) Correct. Genetics can contribute, but smoking cessation and lifestyle choices are essential in preventing COPD.
D) Incorrect. While genetics may have some influence, lifestyle choices, including smoking, can significantly impact COPD risk.
Explanation
A) Incorrect. Age can influence COPD risk, with an increased risk seen in older individuals.
B) Incorrect. COPD is more commonly diagnosed in middle-aged and older adults, not young adults.
C) Correct. COPD risk does increase with age, particularly after the age of 60.
D) Incorrect. While age is a factor, other factors such as smoking play significant roles in COPD development.
Explanation
A) Incorrect. While cough and sputum production are common in COPD, shortness of breath is the hallmark symptom.
B) Incorrect. Severe chest pain during deep breaths is not a hallmark symptom of COPD; it may suggest other conditions.
C) Correct. Shortness of breath, particularly during physical activity, is a characteristic symptom of COPD due to impaired lung function.
D) Incorrect. A high fever and chills are not typical symptoms of COPD but may be associated with other respiratory or infectious conditions.
Explanation
A) Incorrect. Mild wheezing can occur in stable COPD and may not necessarily indicate exacerbation.
B) Incorrect. Increased energy levels and activity tolerance would be positive signs but are not indicative of exacerbation.
C) Incorrect. Decreased shortness of breath during exertion would be a positive change, suggesting improved control of COPD.
D) Correct. Cyanosis (bluish discoloration) of the lips and fingertips is a sign of hypoxia and indicates exacerbation or worsening of COPD.
Explanation
A) Incorrect. Chest pain and tightness are not typically associated with chronic bronchitis but may occur in other conditions.
B) Incorrect. Wheezing and airway constriction are more characteristic of asthma than chronic bronchitis.
C) Correct. Chronic bronchitis is characterized by a persistent cough with sputum production, which is often referred to as a "productive cough."
D) Incorrect. Rapid, shallow breathing is a general respiratory symptom and not specific to chronic bronchitis.
Explanation
A) Correct. Dyspnea is the term used to describe a subjective sensation of difficulty or discomfort in breathing, commonly experienced by individuals with COPD.
B) Incorrect. Hemoptysis refers to coughing up blood, which is not the sensation described.
C) Incorrect. Orthopnea is the difficulty of breathing that occurs when lying flat and is typically associated with heart failure, not COPD.
D) Incorrect. Tachypnea refers to rapid breathing, not the sensation of not getting enough air.
Explanation
A) Incorrect. Bradycardia (slow heart rate) is not typically associated with increased work of breathing in COPD.
B) Correct. Pursed-lip breathing is a compensatory technique used by individuals with COPD to relieve air trapping and reduce the work of breathing.
C) Incorrect. Cyanosis of the extremities may occur with COPD but is not directly related to increased work of breathing.
D) Incorrect. Increased work of breathing typically leads to an increased respiratory rate, not a decreased rate.
Explanation
A) Incorrect. Chest X-rays can provide information about the lungs but are not the primary diagnostic tool for assessing lung function in COPD.
B) Incorrect. A complete blood count (CBC) may reveal signs of infection or anemia but does not assess lung function.
C) Correct. Pulmonary function tests (PFTs), such as spirometry, are the primary diagnostic tool for assessing lung function in COPD. They measure parameters like forced expiratory volume in one second (FEV1) and forced vital capacity (FVC).
D) Incorrect. An electrocardiogram (ECG) is used to assess the electrical activity of the heart and is not a primary tool for diagnosing COPD.
Explanation
A) Incorrect. A sputum culture and sensitivity test is not primarily used to diagnose lung cancer.
B) Incorrect. While the effectiveness of COPD medications may be assessed through other means, this test focuses on identifying bacteria or pathogens.
C) Correct. A sputum culture and sensitivity test helps identify specific bacteria or pathogens present in the sputum, which can guide antibiotic therapy if needed.
D) Incorrect. The test for measuring oxygen and carbon dioxide levels in the blood is typically done through arterial blood gases (ABG) rather than a sputum culture.
Explanation
A) Incorrect. Imaging studies, such as chest X-rays or CT scans, are not used to assess lung function or airflow; they provide structural information.
B) Incorrect. Identifying specific pathogens is typically done through sputum cultures or other microbiological tests, not imaging studies.
C) Correct. Imaging studies can be valuable in confirming or ruling out other lung conditions that may have similar symptoms to COPD, but they are not the primary diagnostic tool for COPD.
D) Incorrect. Imaging studies are not typically used to monitor the progression of COPD; pulmonary function tests (PFTs) are more suitable for this purpose.
Explanation
A) Incorrect. While ABG tests provide information about blood gases, they do not directly evaluate lung function and airflow.
B) Correct. Arterial blood gas (ABG) tests measure the levels of oxygen and carbon dioxide in the blood, which can help assess respiratory function and acid-base balance.
C) Incorrect. ABG tests do not directly assess for the presence of respiratory infections; they focus on blood gas parameters.
D) Incorrect. Identifying specific bacteria causing respiratory symptoms is typically done through sputum cultures and sensitivity tests, not ABG tests.
Explanation
A) Correct. While a chest X-ray cannot diagnose COPD directly, it can reveal structural abnormalities and rule out other lung conditions, helping to confirm the presence and severity of COPD.
B) Incorrect. Chest X-rays focus on providing structural information about the lungs and are not used to evaluate lung function or airflow.
C) Incorrect. Identifying specific pathogens causing respiratory symptoms is typically done through microbiological tests, not chest X-rays.
D) Incorrect. The test for measuring oxygen and carbon dioxide levels in the blood is typically done through arterial blood gas (ABG) analysis, not a chest X-ray.
Explanation
A) Incorrect. Low-tar cigarettes are not a safe alternative, and quitting smoking entirely is recommended.
B) Incorrect. Smoking cessation is essential even after a COPD diagnosis to prevent further lung damage and improve quality of life.
C) Correct. Smoking cessation is a key component of COPD management and can help slow the progression of the disease.
D) Incorrect. E-cigarettes are not a safe alternative to smoking and can still harm the lungs.
Explanation
A) Incorrect. Pursed-lip breathing is beneficial in various situations, not just during exercise.
B) Incorrect. While pursed-lip breathing can help with oxygenation, its primary purpose is to optimize breathing patterns.
C) Correct. Pursed-lip breathing is a technique that promotes more efficient breathing by slowing down the breath rate and enhancing oxygen exchange.
D) Incorrect. While it can have a calming effect, the primary purpose of pursed-lip breathing is to aid in respiratory function.
Explanation
A) Incorrect. Taking short, shallow breaths can lead to inadequate oxygenation and increased fatigue. Deep and controlled breaths are preferred.
B) Incorrect. Performing all activities at once can lead to excessive fatigue. Energy conservation involves pacing activities and taking rest breaks.
C) Incorrect. While assistive devices can be helpful, relying solely on them without considering energy conservation principles may not be effective.
D) Correct. Prioritizing activities and taking rest breaks as needed are key components of energy conservation for individuals with COPD.
Explanation
A) Incorrect. While oxygen therapy is generally safe when used as prescribed, it is not entirely risk-free.
B) Correct. Overuse of oxygen or using a higher flow rate than prescribed can lead to oxygen toxicity and lung damage. It's crucial to follow the prescribed flow rate.
C) Incorrect. Oxygen therapy is not known to increase the risk of developing COPD.
D) Incorrect. There are potential risks associated with oxygen therapy, especially if it is misused or overused.
Explanation
A) Incorrect. Bronchodilators are not primarily focused on reducing inflammation, although some may have anti-inflammatory properties.
B) Incorrect. Thinning mucus is typically achieved with mucolytic medications, not bronchodilators.
C) Correct. Bronchodilators are medications that relax and widen the airways, making it easier to breathe for individuals with COPD.
D) Incorrect. Bronchodilators do not prevent respiratory infections; they primarily address airway constriction and bronchoconstriction.
Explanation
A) Incorrect. Low-tar cigarettes are not a safe alternative, and quitting smoking entirely is recommended.
B) Incorrect. Smoking cessation is essential even after a COPD diagnosis to prevent further lung damage and improve quality of life.
C) Correct. Smoking cessation is a key component of COPD management and can help slow the progression of the disease.
D) Incorrect. E-cigarettes are not a safe alternative to smoking and can still harm the lungs.
Explanation
A) Incorrect. Pursed-lip breathing is beneficial in various situations, not just during exercise.
B) Incorrect. While pursed-lip breathing can help with oxygenation, its primary purpose is to optimize breathing patterns.
C) Correct. Pursed-lip breathing is a technique that promotes more efficient breathing by slowing down the breath rate and enhancing oxygen exchange.
D) Incorrect. While it can have a calming effect, the primary purpose of pursed-lip breathing is to aid in respiratory function.
Explanation
A) Incorrect. Taking short, shallow breaths can lead to inadequate oxygenation and increased fatigue. Deep and controlled breaths are preferred.
B) Incorrect. Performing all activities at once can lead to excessive fatigue. Energy conservation involves pacing activities and taking rest breaks.
C) Incorrect. While assistive devices can be helpful, relying solely on them without considering energy conservation principles may not be effective.
D) Correct. Prioritizing activities and taking rest breaks as needed are key components of energy conservation for individuals with COPD.
Explanation
A) Incorrect. While oxygen therapy is generally safe when used as prescribed, it is not entirely risk-free.
B) Correct. Overuse of oxygen or using a higher flow rate than prescribed can lead to oxygen toxicity and lung damage. It's crucial to follow the prescribed flow rate.
C) Incorrect. Oxygen therapy is not known to increase the risk of developing COPD.
D) Incorrect. There are potential risks associated with oxygen therapy, especially if it is misused or overused.
Explanation
A) Incorrect. Bronchodilators are not primarily focused on reducing inflammation, although some may have anti-inflammatory properties.
B) Incorrect. Thinning mucus is typically achieved with mucolytic medications, not bronchodilators.
C) Correct. Bronchodilators are medications that relax and widen the airways, making it easier to breathe for individuals with COPD.
D) Incorrect. Bronchodilators do not prevent respiratory infections; they primarily address airway constriction and bronchoconstriction.
Pulmonary Embolism
Explanation
A) Incorrect. This description is more related to coronary artery blockages, not pulmonary embolism.
B) Incorrect. This describes a different lung condition called pneumonia, not pulmonary embolism.
C) Correct. A pulmonary embolism is a blockage in the pulmonary arteries, typically caused by a blood clot traveling from elsewhere in the body.
D) Incorrect. This describes a characteristic of chronic obstructive pulmonary disease (COPD), not pulmonary embolism.
Explanation
A) Incorrect. Surgery does increase the risk of pulmonary embolism, especially when accompanied by immobility.
B) Correct. Prolonged immobility, birth control pills, and obesity are known risk factors for post-surgery pulmonary embolism.
C) Incorrect. While smoking and caffeine intake can impact lung health, they are not the primary risk factors for post-surgery pulmonary embolism.
D) Incorrect. While a family history of clotting disorders can contribute to the risk, it is not a common risk factor discussed in the context of post-surgery pulmonary embolism.
Explanation
A) Incorrect. While pulmonary embolism can strain the heart, it is primarily a result of disrupted blood flow to the lungs, not heart failure.
B) Incorrect. While pulmonary embolism can impact lung function, it does so through blocked blood flow rather than severe inflammation.
C) Correct. The most critical aspect of pulmonary embolism is the blockage of blood flow to the lungs, which can lead to severe oxygen deprivation and be fatal.
D) Incorrect. The collapse of bronchial tubes is not a characteristic of pulmonary embolism.
Explanation
A) Incorrect. High-intensity exercise may not necessarily reduce the risk and could potentially increase the risk if it leads to prolonged immobility afterward.
B) Correct. Maintaining a healthy weight, regular physical activity, and avoiding smoking are known lifestyle factors that can reduce the risk of pulmonary embolism.
C) Incorrect. Lifestyle changes, as mentioned, can play a role in prevention.
D) Incorrect. While stress reduction is beneficial for overall health, it is not specifically linked to the prevention of pulmonary embolism.
Explanation
A) Correct. Chest pain that worsens with deep breaths (pleuritic chest pain) is a common and concerning symptom of pulmonary embolism.
B) Incorrect. Persistent cough with yellow-green mucus production is not a typical symptom of pulmonary embolism.
C) Incorrect. Lightheadedness and dizziness can be associated with pulmonary embolism but are less specific symptoms.
D) Incorrect. Swelling and redness in the lower legs are more indicative of deep vein thrombosis (DVT), which can sometimes lead to pulmonary embolism but are not direct symptoms of pulmonary embolism.
Explanation
A) Incorrect. Prolonged sitting during travel, especially on long flights, can increase the risk of pulmonary embolism due to immobility.
B) Incorrect. Long-term anticoagulant therapy is often prescribed to reduce the risk of pulmonary embolism, not increase it.
C) Correct. Prolonged immobility, such as sitting for long hours or bed rest, is a significant risk factor for pulmonary embolism.
D) Incorrect. Recent surgery, trauma, or hospitalization can increase the risk of developing pulmonary embolism due to factors such as immobility and altered blood clotting.
Explanation
A) Incorrect. This description is more aligned with a lung infection, such as pneumonia, not pulmonary embolism.
B) Correct. Pulmonary embolism is typically caused by a blood clot that travels to the lungs and obstructs the pulmonary arteries.
C) Incorrect. Prolonged exposure to environmental toxins is not the primary cause of pulmonary embolism.
D) Incorrect. Chronic inflammation in the airways is characteristic of conditions like chronic obstructive pulmonary disease (COPD) but not pulmonary embolism.
Explanation
A) Incorrect. DVT and pulmonary embolism are related conditions, and they share risk factors.
B) Correct. Deep vein thrombosis (DVT) in the legs can lead to pulmonary embolism if a clot dislodges and travels to the lungs.
C) Incorrect. DVT and pulmonary embolism are distinct conditions, although they are closely related due to their connection through blood clots.
D) Incorrect. DVT is not a more severe form of pulmonary embolism; they are separate but related conditions.
Explanation
A) Incorrect. While surgical trauma can be a risk factor, it is not solely associated with incisions and scars.
B) Incorrect. The risk of pulmonary embolism after surgery is not low, and specific factors do contribute to the risk.
C) Correct. Prolonged immobility, surgical trauma, and changes in blood clotting are common risk factors for post-surgery pulmonary embolism.
D) Incorrect. Excessive fluid intake during recovery is not a primary risk factor for post-surgery pulmonary embolism.
Explanation
A) Incorrect. Pulmonary embolism does not directly affect the bronchial tubes or cause airway constriction.
B) Incorrect. While inflammation can occur as a response to pulmonary embolism, its primary impact is on blood flow, not the alveoli.
C) Correct. The main effect of pulmonary embolism is the disruption of blood flow to lung tissue, reducing oxygen supply.
D) Incorrect. Excessive mucus production is not a characteristic effect of pulmonary embolism.
Explanation
A) Correct. Prolonged immobility and a sedentary lifestyle are significant risk factors for pulmonary embolism.
B) Incorrect. Environmental pollutants and toxins are not primary causes of pulmonary embolism.
C) Incorrect. While healthy individuals can also develop pulmonary embolism, various factors contribute to its risk.
D) Incorrect. Lifestyle factors, as well as medical conditions, can contribute to the risk of pulmonary embolism.
Explanation
A) Incorrect. Surgery, especially major procedures, can increase the risk of pulmonary embolism.
B) Incorrect. The risk of pulmonary embolism is often higher after major surgeries, not limited to minor procedures.
C) Correct. Major surgeries and procedures carry a higher risk of pulmonary embolism due to factors like immobility and surgical trauma.
D) Incorrect. While genetics can play a role in clotting disorders, surgery remains a significant risk factor for pulmonary embolism.
Explanation
A) Incorrect. Age can influence the risk of pulmonary embolism, and it tends to increase with age.
B) Incorrect. While younger individuals can develop pulmonary embolism, the risk generally rises with age.
C) Correct. Pulmonary embolism risk is higher in older individuals, particularly those over 60.
D) Incorrect. Age is one of many factors that contribute to the risk of pulmonary embolism.
Explanation
A) Incorrect. Pregnancy can increase the risk of pulmonary embolism, especially during specific periods.
B) Correct. Pregnancy is a known risk factor for pulmonary embolism due to hormonal changes, increased clotting factors, and reduced mobility during pregnancy.
C) Incorrect. While the risk may be higher during the postpartum period, it can also occur during pregnancy.
D) Incorrect. While genetics can play a role, other factors associated with pregnancy contribute to the risk of pulmonary embolism.
Explanation
A) Incorrect. Smoking can influence the risk of pulmonary embolism, typically increasing it.
B) Incorrect. Smoking is generally associated with increased pulmonary embolism risk, not reduced risk.
C) Correct. Smoking can damage blood vessels and promote clot formation, contributing to the risk of
pulmonary embolism.
D) Incorrect. Both the duration and amount of smoking can impact pulmonary embolism risk.
Explanation
A) Incorrect. Fatigue and weakness can be nonspecific symptoms and are not specific to pulmonary embolism.
B) Incorrect. While cough and sore throat can be symptoms of respiratory conditions, they are not specific to pulmonary embolism.
C) Correct. Sharp, stabbing chest pain that worsens with deep breaths, known as pleuritic chest pain, is a classic symptom of pulmonary embolism.
D) Incorrect. Increased appetite and weight gain are not typically associated with pulmonary embolism and may suggest other conditions.
Explanation
A) Incorrect. Hemoptysis refers to coughing up blood, which is not described in the client's symptoms.
B) Incorrect. Orthopnea is the inability to breathe comfortably when lying flat and is not the best description of the client's symptoms.
C) Incorrect. Syncope refers to fainting or loss of consciousness, which is not the primary symptom described.
D) Correct. Dyspnea, or difficulty breathing, along with lightheadedness and rapid heart rate, is a common presentation of pulmonary embolism.
Explanation
A) Incorrect. Wheezing is a high-pitched whistling sound that occurs during expiration and is not associated with crackling sounds.
B) Incorrect. Rhonchi are continuous low-pitched sounds heard during both inspiration and expiration, usually due to airway obstruction.
C) Incorrect. Stridor is a high-pitched, crowing sound that occurs during inspiration and suggests upper airway obstruction.
D) Correct. Rales, also known as crackles, are crackling or popping sounds heard during inspiration and can be indicative of fluid or inflammation in the lungs, which can occur with pulmonary embolism.
Explanation
A) Incorrect. Anhedonia refers to the inability to experience pleasure and is not the best description of the client's symptom.
B) Incorrect. Euphoria is a state of intense happiness or elation, which is not consistent with the client's report.
C) Correct. The client's feeling of impending doom and restlessness is characteristic of anxiety, which can occur in response to a pulmonary embolism.
D) Incorrect. Apathy refers to a lack of interest or emotion and does not describe the client's state of restlessness and fear.
Explanation
A) Incorrect. Jaundice is a yellowing of the skin and sclera due to elevated bilirubin levels, which is not described in the client's symptoms.
B) Incorrect. Pallor refers to paleness of the skin, which is not consistent with the client's cyanosis.
C) Incorrect. Erythema refers to redness of the skin due to increased blood flow, which is not the best description of the client's symptoms.
D) Correct. Cyanosis is the bluish discoloration of the skin, lips, and nail beds due to decreased oxygen saturation in the blood, which is indicative of a severe oxygen deficit often seen in pulmonary embolism.
Explanation
A) Incorrect. Chest X-rays can show certain abnormalities but are not the primary diagnostic tool for pulmonary embolism.
B) Incorrect. Electrocardiograms (ECGs) are used to assess heart rhythm and electrical activity but are not used to diagnose pulmonary embolism.
C) Incorrect. Magnetic resonance imaging (MRI) may be used in some cases, but CTPA is the preferred test for diagnosing pulmonary embolism.
D) Correct. Computed tomography pulmonary angiography (CTPA) is the gold standard for diagnosing pulmonary embolism as it can visualize blood clots in the pulmonary arteries.
Explanation
A) Incorrect. A complete blood count (CBC) provides information about the composition of blood cells but is not specific to pulmonary embolism.
B) Incorrect. Arterial blood gas (ABG) analysis helps assess oxygen and carbon dioxide levels but is not a primary test for diagnosing pulmonary embolism.
C) Correct. The D-dimer assay measures a substance released when a blood clot breaks up. Elevated D-dimer levels can suggest the presence of a blood clot, but it is not specific to pulmonary embolism.
D) Incorrect. Creatine kinase (CK) levels are used to assess muscle damage and are not a primary test for diagnosing pulmonary embolism.
Explanation
A) Incorrect. Visualizing the heart's electrical activity is typically done with an electrocardiogram (ECG), not a V/Q scan.
B) Correct. A ventilation-perfusion (V/Q) scan is used to assess lung function and oxygenation and to detect areas of the lung where blood flow and air ventilation do not match, which can indicate a pulmonary embolism.
C) Incorrect. Measuring blood clotting time is typically done using coagulation tests such as prothrombin time (PT) or activated partial thromboplastin time (aPTT).
D) Incorrect. Evaluating kidney function is not the primary purpose of a V/Q scan.
Explanation
A) Incorrect. Pulmonary angiography involves the injection of contrast dye into the pulmonary arteries, not the insertion of a scope into the lungs.
B) Correct. Remaining still during the procedure is crucial to obtain clear images, and the client should be educated about the importance of cooperation.
C) Incorrect. Allergies to contrast dye can be a concern, and the client should inform the healthcare team of any allergies to prevent potential adverse reactions.
D) Incorrect. Mild discomfort and chest pain are not common during pulmonary angiography and should not be expected. The procedure is typically done under local anesthesia, and any discomfort should be reported to the healthcare team.
Explanation
A) Incorrect. An echocardiogram does not visualize blood clots in the pulmonary arteries; it focuses on assessing heart function and structure.
B) Correct. An echocardiogram provides valuable information about heart valve function and heart structure, helping assess the impact of a pulmonary embolism on the heart.
C) Incorrect. Measurement of arterial blood gases (ABGs) is typically performed through blood sampling, not with an echocardiogram.
D) Incorrect. Echocardiograms do not evaluate lung function and ventilation; they primarily assess cardiac function.
Explanation
A) Incorrect. Intravenous antibiotics are not typically used as the initial treatment for pulmonary embolism. Antibiotics are used to treat bacterial infections, not blood clots.
B) Correct. Anticoagulant therapy, such as heparin or low-molecular-weight heparin, is often the initial treatment for pulmonary embolism to prevent further clot formation and reduce the risk of complications.
C) Incorrect. Emergency surgical removal of the embolism is considered in severe cases but is not the common initial treatment approach.
D) Incorrect. Placement of a chest tube for drainage is not a standard treatment for pulmonary embolism; it is used for conditions involving pleural effusion or pneumothorax.
Explanation
A) Incorrect. Aspirin is an antiplatelet agent, not a long-term anticoagulant, and it is typically not used as the primary treatment for pulmonary embolism.
B) Correct. Warfarin (Coumadin) is commonly used for long-term anticoagulation in individuals with a history of recurrent pulmonary embolism. It helps prevent the formation of new blood clots.
C) Incorrect. Insulin is used to manage blood sugar levels in diabetes and is not a medication for anticoagulation.
D) Incorrect. Nitroglycerin is used to relieve chest pain (angina) related to heart conditions but is not an anticoagulant.
A nurse is caring for a client with a pulmonary embolism who is receiving tissue plasminogen activator (tP therapy. What is the primary purpose of tPA in this situation?
Explanation
A) Incorrect. tPA therapy is not primarily used for pain relief but rather for clot dissolution.
B) Incorrect. While improving lung function and oxygenation is a goal in treating pulmonary embolism, tPA's primary purpose is to dissolve existing blood clots.
C) Correct. tPA (tissue plasminogen activator) is a thrombolytic agent used to break down and dissolve existing blood clots in the pulmonary arteries, improving blood flow.
D) Incorrect. tPA is not used to prevent the formation of new blood clots but rather to treat existing clots.
Explanation
A) Incorrect. Oxygen therapy is not administered to increase heart rate but rather to improve oxygen delivery to tissues.
B) Incorrect. While oxygen therapy may help alleviate anxiety related to shortness of breath, its primary goal is to address oxygenation.
C) Correct. The primary goal of oxygen therapy in pulmonary embolism is to improve oxygen saturation and tissue oxygenation, as pulmonary embolism can lead to decreased oxygen levels in the blood.
D) Incorrect. Oxygen therapy is not used to lower blood pressure but rather to address oxygenation and tissue oxygen delivery.
Explanation
A) Correct. Smoking cessation is an important lifestyle modification to reduce the risk of recurrent pulmonary embolism. Smoking is a risk factor for blood clot formation.
B) Incorrect. Limiting physical activity is not recommended, as moderate physical activity can be beneficial. However, strenuous activity may need to be adjusted depending on the individual's condition and treatment.
C) Incorrect. A high-sodium diet is not recommended, as excessive sodium intake can contribute to hypertension, which is a risk factor for blood clots.
D) Incorrect. Avoiding vaccinations is not relevant to the prevention of pulmonary embolism. Vaccinations are essential for preventing certain infections.
Explanation
A) Incorrect. Mild shortness of breath during activities may not be unusual, but sudden or severe shortness of breath should be reported.
B) Correct. Chest pain that worsens with deep breathing or coughing may indicate a worsening of the pulmonary embolism and should be reported immediately.
C) Incorrect. Mild swelling in the ankles is not typically a sign of a pulmonary embolism. However, severe leg swelling or pain should be evaluated.
D) Incorrect. An occasional cough with clear sputum is not necessarily a sign of a pulmonary embolism. However, if the cough becomes severe or is associated with other symptoms, it should be reported.
Explanation
A) Incorrect. Avoiding all physical activity is not recommended. Clients should engage in appropriate physical activity, and the level of activity may be adjusted based on their condition.
B) Incorrect. A diet high in cholesterol is not a preventive measure for blood clots; in fact, it can contribute to cardiovascular risk factors.
C) Incorrect. While excessive caffeine and alcohol intake should be avoided, eliminating them completely is not a specific preventive measure for pulmonary embolism.
D) Correct. Following the healthcare provider's recommendations for anticoagulant therapy is crucial in preventing recurrent pulmonary embolism, especially in individuals with a history of the condition.
Explanation
A) Correct. Computed tomography angiography (CTA) is often used as an initial screening tool for pulmonary embolism, as it provides detailed images of the pulmonary arteries.
B) Incorrect. Magnetic resonance imaging (MRI) may be used in some cases but is less commonly employed as an initial screening tool for pulmonary embolism.
C) Incorrect. Chest X-ray is typically not sensitive enough to diagnose pulmonary embolism directly but may show other related findings, such as an enlarged heart or lung abnormalities.
D) Incorrect. Electrocardiogram (ECG) may help identify signs of right heart strain or dysfunction caused by a pulmonary embolism but is not a primary diagnostic tool for detecting emboli in the pulmonary arteries.
Explanation
A) Incorrect. An IVC filter is not used to administer anticoagulant medications but rather to prevent blood clots from reaching the pulmonary circulation.
B) Incorrect. IVC filters are not used to prevent airway obstruction.
C) Correct. The primary purpose of an IVC filter is to capture and prevent blood clots from reaching the pulmonary circulation, reducing the risk of pulmonary embolism.
D) Incorrect. IVC filters are not used to deliver oxygen directly to the lungs but rather to prevent emboli from reaching the lungs.
Explanation
A) Incorrect. While pain management is important, providing supplemental oxygen to address severe shortness of breath takes priority.
B) Incorrect. Initiating anticoagulant therapy is essential but may take some time to have an effect. Oxygen therapy should be provided immediately to address the client's oxygenation.
C) Correct. Providing supplemental oxygen is the priority intervention for a client with severe
shortness of breath to ensure adequate oxygenation.
D) Incorrect. Encouraging ambulation is not appropriate in a client with severe shortness of breath. Stabilizing the client's oxygenation and condition is the immediate concern.
Cystic Fibrosis
Explanation
A) Incorrect. CF is an autosomal recessive genetic disorder, meaning that both copies of the CFTR gene must carry a mutation for the condition to manifest.
B) Correct. CF is caused by the inheritance of two recessive genetic mutations, one from each parent, resulting in defective CFTR protein function.
C) Incorrect. CF is primarily a genetic disorder present from birth, not one caused by spontaneous mutations during a person's lifetime.
D) Incorrect. CF is primarily a genetic disorder with well-established genetic mutations associated with its development.
Explanation
A) Incorrect. Frequent nosebleeds are not a hallmark symptom of CF.
B) Correct. A chronic cough with thick, sticky mucus production is a hallmark feature of CF due to the accumulation of mucus in the respiratory tract.
C) Incorrect. Rapid weight gain is not a typical symptom of CF; in fact, individuals with CF often struggle with poor weight gain and malnutrition.
D) Incorrect. High blood pressure is not a characteristic symptom of CF.
Explanation
A) Incorrect. CF primarily affects the lower respiratory tract, particularly the bronchi and bronchioles, rather than the upper respiratory tract.
B) Correct. CF leads to thickened mucus in the airways, which can cause inflammation, recurrent infections, and progressive lung damage.
C) Incorrect. Enlarged tonsils and adenoids are not a typical manifestation of CF-related respiratory complications.
D) Incorrect. CF affects both the bronchial tubes and the entire respiratory system, often leading to chronic lung infections.
Explanation
A) Incorrect. CF primarily affects the pancreas and small intestine, not the stomach.
B) Incorrect. While liver complications can occur in some individuals with CF, such as liver disease or cirrhosis, it is not a primary manifestation of the disease.
C) Correct. CF often results in thickened mucus obstructing the pancreatic ducts, causing pancreatic insufficiency and malabsorption of essential nutrients.
D) Incorrect. CF primarily affects the pancreas and small intestine rather than the large intestine, and chronic constipation is not a typical symptom of CF.
Explanation
A) Incorrect. Both partners having a family history of CF increases the likelihood of carrying CF gene mutations, making it possible for their child to inherit the condition.
B) Incorrect. Having a single CF gene mutation (carrier status) does not guarantee that a child will develop CF; it requires inheriting two CF gene mutations, one from each parent.
C) Correct. CF is an autosomal recessive genetic disorder, which means that a child will have CF only if they inherit two copies of the CF gene mutation, one from each parent.
D) Incorrect. The risk of a child having CF is determined by both parents' genetic history, not solely the mother's.
Explanation
A) Incorrect. CF is an autosomal recessive genetic disorder, meaning that both copies of the CFTR gene must carry a mutation for the condition to manifest.
B) Incorrect. CF is not caused by dominant genetic mutations.
C) Correct. CF results from inheriting two recessive genetic mutations, one from each parent, leading to defective CFTR protein function.
D) Incorrect. CF is primarily a genetic disorder with well-established genetic mutations associated with its development.
Explanation
A) Incorrect. The CFTR protein primarily functions in the respiratory and digestive systems, not the kidneys.
B) Incorrect. While CFTR plays a role in chloride secretion, its primary role is related to mucus production and chloride ion movement in the respiratory and digestive systems.
C) Incorrect. The CFTR protein is not involved in the production of red blood cells.
D) Correct. The CFTR protein is responsible for regulating mucus consistency and chloride ion transport in the respiratory and digestive systems.
Explanation
A) Incorrect. CF is not caused by an extra chromosome; it is a genetic disorder resulting from mutations in specific genes.
B) Incorrect. CF is not characterized by a duplication of the CFTR gene but rather by various mutations in this gene.
C) Correct. CF is primarily caused by mutations in the CFTR (cystic fibrosis transmembrane conductance regulator) gene, leading to the production of dysfunctional chloride channels.
D) Incorrect. CF is not characterized by the absence of the CFTR gene; instead, it involves various mutations in this gene.
Explanation
A) Incorrect. The CFTR protein does not regulate blood sugar levels.
B) Incorrect. CFTR does not play a role in oxygen transport in the bloodstream.
C) Correct. The primary function of the CFTR protein is to regulate chloride ion and water movement across cell membranes, which is disrupted in individuals with CF.
D) Incorrect. The production of digestive enzymes in the pancreas is not a direct function of the CFTR protein.
Explanation
A) Incorrect. While inflammation can be a consequence of CF, it is not the primary cause of airway constriction.
B) Correct. In CF, thickened mucus accumulates in the airways, leading to chronic inflammation, recurrent infections, and progressive lung damage.
C) Incorrect. CF does not result in the overproduction of surfactant, which is a substance that helps reduce surface tension in the lungs.
D) Incorrect. The CFTR protein does not produce oxygen but rather regulates chloride ion and water transport in the lungs
Explanation
A) Correct. CF is primarily caused by mutations in a single gene, the CFTR gene, and it can be inherited from one parent, resulting in a carrier state, or from both parents for the disease to manifest.
B) Incorrect. While genetic factors are the primary cause of CF, environmental factors can exacerbate symptoms but are not the root cause.
C) Incorrect. CF is not an X-linked genetic disorder; it follows an autosomal recessive pattern of inheritance.
D) Incorrect. CF is not caused by exposure to respiratory pathogens during infancy; it is primarily a genetic disorder.
Explanation
A) Incorrect. CF occurs at a similar frequency in both males and females.
B) Incorrect. CF is not significantly associated with any specific ethnicity, and the risk is not influenced by being of African descent.
C) Correct. A family history of CF increases the risk because CF is an autosomal recessive genetic disorder, and having affected family members increases the likelihood of carrying CF gene mutations.
D) Incorrect. While CF can affect individuals from any ethnicity, it is primarily a genetic disorder, and family history plays a crucial role in the risk of inheritance.
Explanation
A) Incorrect. If both parents are carriers, their child's risk of having CF is 25%, not 50%.
B) Incorrect. While the risk is increased, having two carrier parents does not guarantee that a child will have CF.
C) Incorrect. If both parents are carriers, their child can inherit two normal genes (no CF), one normal and one CF gene (carrier status), or two CF genes (CF).
D) Correct. When both parents are carriers, there is a 25% chance that their child will inherit two CF genes and have CF, a 50% chance of being a carrier, and a 25% chance of inheriting two normal genes (no CF).
Explanation
A) Incorrect. Genetic testing for CF is important for individuals of all ages, not limited to infants.
B) Correct. Genetic testing is a crucial diagnostic tool for confirming the presence of CF gene mutations, regardless of the individual's age.
C) Incorrect. Genetic testing is primarily used for diagnosis, not for determining the severity of CF symptoms.
D) Incorrect. Genetic testing is not reserved solely for family members of individuals already diagnosed with CF; it is used for diagnostic purposes in suspected cases of CF.
Explanation
A) Incorrect. Wheezing and chest pain can occur in CF, but a chronic cough with thick mucus production is often one of the earliest respiratory symptoms.
B) Correct. A chronic cough with thick, sticky mucus is a hallmark symptom of CF due to the accumulation of mucus in the respiratory tract.
C) Incorrect. Blood in the urine is not a common early sign of CF; it may indicate other issues.
D) Incorrect. Digestive discomfort and diarrhea are more related to CF's impact on the gastrointestinal system, rather than being early respiratory symptoms.
Explanation
A) Incorrect. Frequent nosebleeds are not common gastrointestinal symptoms in CF.
B) Correct. Abdominal pain and bloating are common gastrointestinal symptoms in CF, often due to the impact of thickened mucus on the pancreas and intestines.
C) Incorrect. Rapid weight gain is not a typical gastrointestinal symptom in CF; individuals with CF often struggle with poor weight gain and malnutrition.
D) Incorrect. Muscle weakness is not a common gastrointestinal symptom in CF but may be associated with other complications.
Explanation
A) Incorrect. Clubbed fingers in CF can be more than a cosmetic concern and may indicate underlying medical issues.
B) Correct. Clubbing of the fingers can be associated with advanced lung disease or reduced oxygen levels in CF.
C) Incorrect. Clubbing is not related to excessive sodium intake in CF patients.
D) Incorrect. While CF can affect the digestive system, clubbing of the fingers is primarily associated with respiratory issues.
Explanation
A) Incorrect. In advanced CF-related lung disease, a chronic, productive cough with thick mucus production is more common than a dry, nonproductive cough.
B) Correct. Decreased breath sounds may occur in clients with advanced CF-related lung disease due to airway obstruction and lung damage.
C) Incorrect. Hematuria is not a typical respiratory symptom of CF.
D) Incorrect. Rapid weight gain is not associated with advanced CF-related lung disease; individuals with advanced CF often experience weight loss and malnutrition.
Explanation
A) Incorrect. Meconium ileus is a complication typically seen in newborns with CF, not in adults.
B) Incorrect. Failure to thrive is a concern in infants and young children with CF but not typically in adults.
C) Correct. Osteoporosis is a common complication in adults with CF due to malabsorption of calcium and vitamin D, chronic inflammation, and reduced physical activity.
D) Incorrect. Rapid growth and development are typically observed in adolescents, not as a complication but as a part of normal growth.
Explanation
A) Correct. The sweat chloride test is commonly used for newborn screening for CF. Elevated sweat chloride levels are indicative of CF.
B) Incorrect. Chest X-rays may be used to assess lung changes in individuals with CF but are not a primary diagnostic test, especially in newborns.
C) Incorrect. Pulmonary function tests are used to evaluate lung function but are not typically performed as part of newborn screening for CF.
D) Incorrect. A complete blood count (CBC) is a general blood test and is not specific for CF diagnosis.
Explanation
A) Incorrect. Genetic testing can confirm CF but is not typically the initial diagnostic test used in infants with symptoms suggestive of CF.
B) Correct. The sweat chloride test is often used as the initial diagnostic test to assess for CF in infants who exhibit symptoms.
C) Incorrect. Chest X-rays may be used to assess lung changes in individuals with CF but are not typically the initial diagnostic test in infants.
D) Incorrect. Pulmonary function tests are used to evaluate lung function but are not typically the initial diagnostic test for CF in infants.
Explanation
A) Incorrect. Genetic testing is used to confirm the presence of CF gene mutations but is not a measure of lung function.
B) Incorrect. The sweat chloride test is used for CF diagnosis and may not be performed regularly to monitor lung function.
C) Incorrect. Chest X-rays may be used to assess lung changes in individuals with CF, but they do not directly measure lung function.
D) Correct. Pulmonary function tests are commonly performed to assess lung function, monitor disease progression, and guide treatment in individuals with CF.
Explanation
A) Incorrect. The sweat chloride test is used for CF diagnosis, but it does not analyze genetic mutations.
B) Incorrect. Chest X-rays are used to assess lung changes but do not directly confirm CF by analyzing genetic mutations.
C) Incorrect. Pulmonary function tests assess lung function but do not confirm CF by analyzing genetic mutations.
D) Correct. Genetic testing is a diagnostic procedure commonly used to confirm CF by analyzing the specific CF gene mutations present in an individual.
Explanation
A) Incorrect. Genetic testing is used to confirm CF but does not directly measure chloride ion concentration in sweat.
B) Incorrect. Chest X-rays may be used to assess lung changes in individuals with CF but are not used to measure chloride ion concentration in sweat.
C) Incorrect. Pulmonary function tests assess lung function but do not directly measure chloride ion concentration in sweat.
D) Correct. The sweat chloride test measures the concentration of chloride ions in sweat and is commonly used to confirm CF. Elevated sweat chloride levels are indicative of CF.
Explanation
A) Incorrect. Postural drainage involves positioning the body to help drain mucus but does not use a mechanical device.
B) Incorrect. Autogenic drainage is a technique that involves controlled breathing and airflow, not a mechanical device.
C) Incorrect. PEP therapy uses a device to provide positive pressure during exhalation but is different from HFCWO.
D) Correct. High-frequency chest wall oscillation (HFCWO) involves using a mechanical device to deliver oscillations to the chest wall, helping to mobilize and clear mucus from the airways.
Explanation
A) Incorrect. While monitoring carbohydrate intake is important in CF, limiting carbohydrates is not the primary focus of nutrition management.
B) Incorrect. Increasing sodium intake is not a general recommendation for individuals with CF; it depends on the individual's needs.
C) Correct. Individuals with CF often require a high-calorie diet rich in fats and proteins to address malabsorption and maintain adequate nutrition.
D) Incorrect. Restricting fluid intake is not recommended for individuals with CF, as staying hydrated is important for preventing thickening of mucus.
Explanation
A) Incorrect. Long-term oxygen therapy is typically reserved for individuals with chronic hypoxemia and is not the primary treatment for a pulmonary exacerbation.
B) Correct. Bronchodilators and corticosteroids are commonly used to manage pulmonary exacerbations in CF by reducing airway inflammation and improving airflow.
C) Incorrect. Surgical lung transplantation is considered in severe cases of CF with irreversible lung damage but is not typically the first-line treatment for a pulmonary exacerbation.
D) Incorrect. Bed rest and minimal physical activity are not recommended as the primary treatment for pulmonary exacerbations; maintaining mobility and airway clearance techniques are important.
Explanation
A) Incorrect. While airway clearance techniques can help maintain lung function, their primary goal is not to improve lung capacity.
B) Incorrect. Preventing respiratory infections is an important aspect of CF care, but it is not the primary goal of airway clearance techniques.
C) Incorrect. Maintaining electrolyte balance is important in CF, but it is not the primary goal of airway clearance techniques.
D) Correct. The primary goal of airway clearance techniques in CF is to mobilize and clear mucus and secretions from the airways, improving breathing and reducing the risk of infection.
Explanation
A) Incorrect. PERT is not primarily used to control blood sugar levels; it is used to improve nutrient absorption.
B) Incorrect. While CF management aims to improve lung function, PERT is specifically used to address pancreatic insufficiency and digestive issues.
C) Correct. The primary purpose of PERT in CF management is to replace the missing digestive enzymes and aid in the digestion of fats and nutrients.
D) Incorrect. PERT does not increase mucus production in the airways; it is focused on the digestive system.
Explanation
A) Incorrect. Protein intake is important for growth and repair but should not be limited in CF. High-calorie intake is more critical.
B) Correct. CF can lead to malabsorption of fat-soluble vitamins and calories, so a high-fat diet is recommended to support weight gain and nutrient absorption.
C) Incorrect. Dairy products are a good source of calcium and calories, and they are generally well-tolerated by CF patients. Avoiding them is not necessary.
D) Incorrect. Increasing sugary snacks is not advisable for CF patients. They need a balanced diet to meet their nutritional needs.
Explanation
A) Correct. Postural drainage and chest percussion help mobilize and remove thick, sticky mucus from the airways, which is crucial in managing CF.
B) Incorrect. While bronchodilators may be used, they are not the primary therapy for managing CF. Airway clearance techniques like postural drainage are more important.
C) Incorrect. Oxygen therapy should be administered as needed, but it is not required around the clock for all CF patients.
D) Incorrect. Deep breathing exercises should be encouraged regularly, not just during illness, to maintain airway clearance and lung function.
Explanation
A) Incorrect. Hypertension is not typically associated with CF.
B) Incorrect. Hypoglycemia is not a common manifestation of CF.
C) Incorrect. Chronic diarrhea is not a common symptom of CF.
D) Correct. CF is characterized by thick, sticky mucus that can lead to chronic respiratory infections, making this a key clinical manifestation to monitor.
Explanation
A) Incorrect. While coughing is important, huff coughing is a more effective and less strenuous airway clearance technique for CF patients.
B) Incorrect. Controlled breathing exercises may help with relaxation but are not the primary airway clearance technique.
C) Correct. Huff coughing is a technique where the client takes a deep breath and forcefully exhales in short bursts, helping to move mucus from the airways.
D) Incorrect. Vigorous exercise is beneficial for CF patients but should not replace specific airway clearance techniques.
Explanation
A) Correct. Staying well-hydrated is important for CF patients to help keep mucus thin and easier to clear.
B) Correct. It's important to administer all prescribed medications as directed to manage the condition effectively.
C) Incorrect. While infection control is important, it is not necessary for the child to avoid close contact with other children. Common-sense hygiene measures should be followed.
D) Correct. Regular follow-up appointments with the CF care team are crucial to monitor the child's health and adjust the treatment plan as needed.
Pulmonary Edema
Explanation
A) Incorrect. Pulmonary edema is not a bacterial lung infection.
B) Incorrect. Pleuritis (inflammation of the pleura) is a different condition unrelated to pulmonary edema.
C) Correct. Pulmonary edema is characterized by the accumulation of excess fluid in the lungs, often in the alveoli and interstitial spaces.
D) Incorrect. A blockage in the coronary arteries is related to myocardial infarction (heart attack) and is not the primary characteristic of pulmonary edema.
Explanation
A) Correct. Pink, frothy sputum is often referred to as hemoptysis and is a common presentation in pulmonary edema.
B) Incorrect. Orthopnea refers to difficulty breathing when lying flat and is associated with heart failure but is not specifically related to pink, frothy sputum.
C) Incorrect. Paroxysmal nocturnal dyspnea (PND) is another symptom of heart failure but does not involve the coughing up of pink, frothy sputum.
D) Incorrect. Crepitus is a term used to describe a crackling or popping sound and is not directly related to the sputum seen in pulmonary edema.
Explanation
A) Incorrect. Routine physical activity does not typically precipitate the development of pulmonary edema.
B) Incorrect. Recent vaccination is not a common precipitating factor for pulmonary edema.
C) Correct. Severe hypertension can increase the workload of the heart, leading to left ventricular failure, which is a common precipitating event for pulmonary edema.
D) Incorrect. Controlled diabetes is not a precipitating factor for pulmonary edema; uncontrolled diabetes can have cardiovascular implications but is not directly related to this condition.
Explanation
A) Incorrect. Increased lung compliance would not contribute to pulmonary edema; in fact, it might reduce the risk of fluid accumulation in the lungs.
B) Correct. Impaired alveolar fluid clearance, often due to altered pulmonary capillary permeability, is a key factor in the pathophysiology of pulmonary edema.
C) Incorrect. Constricted pulmonary blood vessels (vasoconstriction) would reduce blood flow to the lungs and are not a primary factor in pulmonary edema.
D) Incorrect. Enhanced left ventricular contractility, while beneficial for cardiac function, is not directly related to the development of pulmonary edema.
Explanation
A) Correct. Increased hydrostatic pressure in pulmonary capillaries, often due to left ventricular failure, leads to the filtration of fluid from the capillaries into the alveoli and interstitial spaces, causing pulmonary edema.
B) Incorrect. Decreased capillary permeability is not typically a primary factor in the development of pulmonary edema.
C) Incorrect. Enhanced lymphatic drainage from the lungs is not a primary mechanism responsible for the accumulation of fluid in pulmonary edema.
D) Incorrect. Elevated colloid osmotic pressure in pulmonary vessels would oppose fluid accumulation in the alveoli and is not a primary cause of pulmonary edema.
Explanation
A) Incorrect. Atrial contraction contributes to ventricular filling but is not typically the primary site of impairment in heart failure leading to pulmonary edema.
B) Incorrect. Ventricular relaxation (diastole) is necessary for ventricular filling, but the impaired contraction during systole is a more common issue in heart failure.
C) Correct. Impaired ventricular contraction (systole) in heart failure results in reduced forward flow of blood and leads to fluid backup in the lungs, contributing to pulmonary edema.
D) Incorrect. Electrical conduction in the heart may affect heart rhythm but is not directly related to the development of pulmonary edema.
Explanation
A) Incorrect. The primary role of the lymphatic system in the lungs is not gas exchange but rather fluid removal.
B) Incorrect. While the lymphatic system plays a role in overall fluid balance, it is not primarily responsible for regulating blood pressure.
C) Correct. The lymphatic system helps remove excess interstitial fluid from the lungs, preventing fluid accumulation and contributing to fluid balance.
D) Incorrect. Surfactant production is primarily related to maintaining lung compliance and preventing alveolar collapse but is not a primary function of the lymphatic system.
A client with a history of myocardial infarction (MI) develops pulmonary edema. Which pathophysiological process is likely occurring in this client, leading to fluid accumulation in the lungs?
Explanation
A) Incorrect. Increased myocardial contractility would not typically lead to left ventricular remodeling but might improve cardiac function.
B) Incorrect. Reduced afterload on the heart may be beneficial, but it is not a primary factor in left ventricular remodeling.
C) Correct. Left ventricular remodeling, often occurring after a myocardial infarction, involves changes in the size and shape of the ventricle, which can impair cardiac function and lead to pulmonary edema.
D) Incorrect. Enhanced pulmonary vasodilation is not a primary cause of left ventricular remodeling or pulmonary edema.
Explanation
A) Incorrect. Regular physical exercise is generally a healthy behavior and is not a risk factor for pulmonary edema.
B) Incorrect. Low blood pressure (hypotension) is not a risk factor for pulmonary edema; in fact, high blood pressure (hypertension) is a more common risk factor.
C) Incorrect. Adequate fluid intake is important for overall health but is not a direct risk factor for pulmonary edema.
D) Correct. Chronic kidney disease can lead to fluid and electrolyte imbalances, which can contribute to the development of pulmonary edema.
Explanation
A) Correct. Atrial fibrillation is a cardiac arrhythmia that can lead to heart failure, which is a common etiological factor for pulmonary edema.
B) Incorrect. Hypothyroidism is not typically a direct cause of pulmonary edema.
C) Incorrect. While COPD can lead to respiratory-related symptoms, it is not a direct cause of pulmonary edema.
D) Incorrect. Rheumatoid arthritis is not a known cause of pulmonary edema.
Explanation
A) Incorrect. Regular exercise is generally beneficial for heart health and would not increase the risk of pulmonary edema.
B) Incorrect. Smoking cessation is a positive health behavior and does not increase the risk of pulmonary edema.
C) Incorrect. Hypertension control is important for reducing the risk of heart-related complications and pulmonary edema.
D) Correct. Prior heart muscle damage, such as from a myocardial infarction (MI), increases the risk of heart failure and subsequently pulmonary edema.
Explanation
A) Incorrect. Caffeine, when consumed in moderation, is not a known risk factor for pulmonary edema.
B) Correct. Excessive alcohol consumption can lead to heart-related issues, including alcoholic cardiomyopathy, which can increase the risk of pulmonary edema.
C) Incorrect. While nicotine is harmful to the cardiovascular system, it is not a direct cause of pulmonary edema.
D) Incorrect. While marijuana use can have various health effects, it is not a known direct risk factor for pulmonary edema.
Explanation
A) Correct. Hypertension is a significant risk factor for the development of heart failure, which can lead to pulmonary edema.
B) Incorrect. Diabetes, while a chronic condition, is not a direct risk factor for pulmonary edema.
C) Incorrect. Hypercholesterolemia (high cholesterol) can contribute to atherosclerosis and cardiovascular disease but is not a direct cause of pulmonary edema.
D) Incorrect. Osteoarthritis is a musculoskeletal condition and is not directly related to the development of pulmonary edema.
Explanation
A) Incorrect. A persistent dry cough is not a typical symptom of acute pulmonary edema.
B) Incorrect. Productive cough with green sputum is more suggestive of a respiratory infection than acute pulmonary edema.
C) Correct. Sudden-onset severe shortness of breath, often described as "air hunger," is a hallmark symptom of acute pulmonary edema.
D) Incorrect. Sharp, stabbing chest pain is not a primary symptom of acute pulmonary edema but may be present in some cases.
Explanation
A) Incorrect. A decreased respiratory rate is not typically associated with pulmonary edema, which often leads to increased respiratory effort.
B) Correct. Inspiratory crackles in the lung bases are indicative of fluid accumulation in the alveoli and are a common physical finding in pulmonary edema.
C) Incorrect. Increased breath sounds are not typically associated with pulmonary edema; instead, crackles or wheezing may be heard.
D) Incorrect. Diminished heart sounds are not a characteristic finding in pulmonary edema.
Explanation
A) Incorrect. Nausea and vomiting are not typically associated with pulmonary edema.
B) Correct. Orthopnea, or difficulty breathing when lying flat, is a common symptom of pulmonary edema related to heart failure.
C) Incorrect. While sweating and diaphoresis can occur in response to respiratory distress, they are not specific to pulmonary edema.
D) Incorrect. Sharp, stabbing chest pain is not a common manifestation of pulmonary edema but may occur with other cardiac or respiratory conditions.
Explanation
A) Correct. Pink, frothy sputum, often described as "pink froth," is indicative of severe pulmonary edema with the presence of blood-tinged fluid in the alveoli.
B) Incorrect. A low-grade fever is not a typical sign of pulmonary edema and may indicate another underlying condition.
C) Incorrect. Clear breath sounds throughout the lung fields are not indicative of severe pulmonary edema, which often presents with crackles.
D) Incorrect. The absence of peripheral edema does not necessarily reflect the severity of pulmonary edema; it may be related to factors other than heart failure.
Explanation
A) Incorrect. Hyperventilation leading to respiratory alkalosis may occur in response to respiratory distress but is not the primary cause of the sensation of "suffocation."
B) Incorrect. Reduced cardiac output may be a consequence of pulmonary edema, but it does not typically result in bradycardia, nor is it the primary cause of the sensation described.
C) Correct. In pulmonary edema, fluid accumulation in the alveoli impairs oxygen diffusion, leading to hypoxemia, which contributes to the sensation of "suffocation."
D) Incorrect. Elevated blood pressure and hypertension can be associated with heart failure but are not the primary factors contributing to the sensation of "suffocation" in pulmonary edema.
Explanation
A) Incorrect. While a complete blood count (CBC) may provide some information, it is not the primary diagnostic test for pulmonary edema.
B) Incorrect. An electrocardiogram (ECG) may be used to evaluate cardiac function but does not directly assess pulmonary edema.
C) Correct. A chest X-ray is a key diagnostic tool for assessing the presence, severity, and underlying causes of pulmonary edema by visualizing lung and heart structures.
D) Incorrect. Urinalysis is not a primary diagnostic test for pulmonary edema; it is used to assess kidney function and screen for urinary tract infections.
Explanation
A) Correct. Serum creatinine levels can be elevated in cases of heart failure-related pulmonary edema, indicating impaired kidney function due to reduced cardiac output.
B) Incorrect. Blood glucose levels may be elevated in some individuals with diabetes but are not directly related to pulmonary edema.
C) Incorrect. Hemoglobin levels are not typically used to diagnose pulmonary edema; they are more related to oxygen-carrying capacity in the blood.
D) Incorrect. Serum potassium levels may be influenced by various factors but are not a primary indicator of pulmonary edema.
Explanation
A) Correct. Pulmonary edema can lead to impaired gas exchange, resulting in respiratory acidosis, characterized by a decreased pH on ABG analysis.
B) Incorrect. Pulmonary edema typically leads to decreased oxygenation, so an elevated PaO2 would not be consistent with this condition.
C) Incorrect. A decreased PaCO2 is more commonly associated with respiratory alkalosis and is not a primary finding in pulmonary edema.
D) Incorrect. Increased bicarbonate (HCO3-) levels are more indicative of metabolic alkalosis and are not typically associated with pulmonary edema.
Explanation
A) Incorrect. Oxygen saturation levels are typically assessed using pulse oximetry and are not provided by an echocardiogram.
B) Incorrect. Blood pressure measurements are not directly assessed through an echocardiogram.
C) Correct. An echocardiogram provides valuable information about the structure and function of the heart, which can help diagnose the underlying cause of pulmonary edema, such as heart failure.
D) Incorrect. A white blood cell count is not part of an echocardiogram and is not used to diagnose pulmonary edema.
Explanation
A) Correct. A CT scan can help identify the presence of fluid in the alveoli and interstitial spaces of the lungs, making it a valuable tool in diagnosing pulmonary edema.
B) Incorrect. MRI is not typically used to diagnose pulmonary edema, as it may not provide as clear an image of lung tissue as a CT scan.
C) Incorrect. PET scans are more commonly used in oncology to detect metabolic activity and are not typically used for pulmonary edema diagnosis.
D) Incorrect. While ultrasound can be useful in assessing pleural effusions, it may not provide the same level of detail as a CT scan for diagnosing pulmonary edema.
Explanation
A) Incorrect. Intravenous antibiotics may be necessary for certain pulmonary infections, but they do not address the immediate oxygenation needs in acute pulmonary edema.
B) Correct. Providing supplemental oxygen helps increase the client's oxygen levels, improving oxygenation in acute pulmonary edema.
C) Incorrect. While deep breathing exercises are beneficial for overall lung health, they may not be sufficient to address the immediate oxygenation issue in acute pulmonary edema.
D) Incorrect. Antipyretic medications are used to reduce fever and do not directly improve oxygenation in pulmonary edema.
Explanation
A) Incorrect. Sudden onset of severe chest pain is not a typical finding in chronic pulmonary edema.
B) Incorrect. Profuse hemoptysis is not a common symptom of chronic pulmonary edema.
C) Correct. Bilateral pitting edema in the lower extremities is a common sign of fluid retention in chronic pulmonary edema.
D) Incorrect. While an increased heart rate may be present, palpitations are not a typical finding in chronic pulmonary edema.
Explanation
A) Correct. Diuretics are commonly used in the management of pulmonary edema to reduce fluid volume, preload, and afterload on the heart.
B) Incorrect. Antibiotics are used to treat bacterial infections and are not typically used as a primary treatment for pulmonary edema.
C) Incorrect. Bronchodilators are used to relieve airway constriction and are not the primary treatment for pulmonary edema.
D) Incorrect. Anticoagulants are used to prevent blood clot formation and are not the primary treatment for pulmonary edema.
Explanation
A) Incorrect. The supine position with legs elevated is not recommended for clients with pulmonary edema, as it can worsen fluid retention.
B) Correct. High Fowler's position allows for optimal lung expansion and improved gas exchange in clients with pulmonary edema.
C) Incorrect. The left lateral recumbent position may be used in some cases, but it is not the primary position for managing pulmonary edema.
D) Incorrect. The prone position is not typically recommended for clients with pulmonary edema.
Explanation
A) Incorrect. Limiting fluid intake should be based on the client's specific medical recommendations and should not be a general guideline.
B) Incorrect. Avoiding all physical activity is not necessary and can lead to deconditioning. Clients should engage in appropriate physical activity as advised by their healthcare provider.
C) Incorrect. Blood pressure should be regularly monitored as directed by the healthcare provider, not only when symptoms worsen.
D) Correct. Taking prescribed medications as directed, especially diuretics and medications to manage underlying conditions, is crucial in preventing recurrence of pulmonary edema.
Explanation
A) Correct. Skin temperature and color can provide important clues about tissue perfusion and oxygenation, which are critical in pulmonary edema.
B) Incorrect. While urinary output is important, it is not the primary focus when monitoring respiratory status in pulmonary edema.
C) Incorrect. Bowel sounds are unrelated to pulmonary edema and should not be the priority assessment.
D) Incorrect. Peripheral edema may be a sign of fluid retention, but skin color and temperature are more directly related to respiratory status.
Explanation
A) Incorrect. Diuretics typically reduce blood pressure, so increased blood pressure is an unlikely side effect.
B) Incorrect. Hyperglycemia is not a common side effect of diuretics.
C) Correct. Diuretics can lead to the loss of potassium, resulting in hypokalemia.
D) Incorrect. Bradycardia is not typically associated with diuretic therapy.
Explanation
A) Incorrect. Elevated body temperature is not a typical manifestation of pulmonary edema.
B) Incorrect. Bradycardia is not a common finding in pulmonary edema.
C) Correct. Crackles in the lung fields are a hallmark sign of pulmonary edema due to the accumulation of fluid in the alveoli.
D) Incorrect. Hypertension is not a typical finding in pulmonary edema; it is more commonly associated with conditions like heart failure.
Explanation
A) Incorrect. A high-sodium diet is not recommended for clients with pulmonary edema, as it can exacerbate fluid retention.
B) Incorrect. Low-potassium diets are not typically recommended for clients with pulmonary edema, as potassium is important for heart and muscle function.
C) Correct. A low-sodium diet is essential to reduce fluid retention and manage pulmonary edema.
D) Incorrect. While adequate protein intake is important for overall health, it is not the primary dietary concern in pulmonary edema.
Explanation
A) Incorrect. Urinary output is important but does not directly assess the client's oxygenation status.
B) Correct. Monitoring the respiratory rate and effort is essential to ensure the client is adequately oxygenated and not in respiratory distress.
C) Incorrect. Skin turgor is unrelated to oxygenation and pulmonary edema.
D) Incorrect. Bowel sounds do not provide information about the client's oxygenation status.
Lung Cancer
Explanation
A) Incorrect. While exposure to secondhand smoke is a risk factor, it is not the primary cause of lung cancer.
B) Incorrect. Genetics can play a role, but it is not the most significant factor in the development of lung cancer.
C) Incorrect. Avoiding tobacco smoke is important, but other factors can also contribute to the risk of lung cancer.
D) Correct. Smoking is the leading cause of lung cancer, but exposure to radon and occupational carcinogens is also significant in the development of the disease.
Explanation
A) Incorrect. There are multiple types of lung cancer, not just one.
B) Correct. The two main types of lung cancer are non-small cell lung cancer and small cell lung cancer.
C) Incorrect. While lung cancer can occur in different parts of the lungs, it is primarily classified into non-small cell and small cell types.
D) Incorrect. Although these are common subtypes of non-small cell lung cancer, there are only two main categories: non-small cell and small cell.
Explanation
A) While family history can be a risk factor, it is not the most strongly associated factor for lung cancer.
B) Correct. Exposure to asbestos is a significant risk factor for lung cancer, particularly in occupational settings.
C) Occasional exposure to secondhand smoke can contribute to the risk, but it is not the most strongly associated factor.
D) Consumption of high-fat foods is not a primary risk factor for lung cancer.
Explanation
A) Incorrect. While some symptoms of lung cancer can include coughing up blood and chest pain, they are not always obvious and may not occur in the early stages.
B) Correct. Early-stage lung cancer can be asymptomatic, but as it advances, symptoms like a persistent cough, shortness of breath, and chest pain may develop.
C) Weight loss can be a symptom, but it is not the most common or specific one associated with lung cancer.
D) Lung cancer primarily affects the lungs and respiratory system, and skin changes like new moles or rashes are not typical symptoms.
Explanation
A) Mammography is a screening method for breast cancer, not lung cancer.
B) The PSA test is used to screen for prostate cancer, not lung cancer.
C) Colonoscopy is a screening method for colorectal cancer, not lung cancer.
D) Correct. Low-dose computed tomography (LDCT) scans are commonly recommended for individuals at high risk of lung cancer to detect the disease at an early stage when it may be more treatable.
Explanation
A) Incorrect. While lifestyle factors like smoking are significant, genetic mutations can also play a role in lung cancer.
B) Correct. Mutations in certain genes, especially in non-smokers, can increase the risk of developing lung cancer.
C) Incorrect. Genetic mutations can be associated with various types of lung cancer, not just small cell lung cancer.
D) Incorrect. Lung cancer is influenced by both genetic mutations and environmental factors like smoking.
Explanation
A) Incorrect. Metastasis involves the spread of malignant (cancerous) cells, not benign tumors.
B) Correct. Metastasis is the process by which cancer cells from the primary lung tumor can travel to other parts of the body and form secondary tumors.
C) Incorrect. Metastasis can occur at various stages of lung cancer, not just in advanced stages.
D) Incorrect. Metastasis is not the process of early cancer development but rather the spread of cancer cells.
Explanation
A) Incorrect. SCLC is generally more aggressive and grows rapidly compared to NSCLC.
B) Correct. NSCLC is more common, and treatment outcomes are generally better when compared to SCLC.
C) Incorrect. NSCLC and SCLC have distinct characteristics and treatment approaches.
D) Incorrect. Both NSCLC and SCLC are associated with smoking, although SCLC is more strongly linked to smoking.
Explanation
A) Incorrect. EGFR mutations can occur in both smokers and non-smokers with NSCLC.
B) Incorrect. EGFR mutations are primarily associated with NSCLC, not SCLC.
C) Correct. EGFR mutations are relevant to NSCLC and can influence treatment choices, including the use of targeted therapies.
D) Incorrect. EGFR mutations are relevant in NSCLC and can impact treatment decisions.
Explanation
A) Incorrect. Angiogenesis is not related to the spread of cancer cells but rather to the blood vessel development around tumors.
B) Correct. Angiogenesis is the process by which tumors stimulate the growth of new blood vessels to provide nutrients and oxygen, supporting tumor growth.
C) Incorrect. Angiogenesis is not a genetic mutation but a biological process.
D) Incorrect. Angiogenesis does not involve the surgical removal of tumors but rather the blood vessel development around them.
Explanation
A) Incorrect. While a diet high in fruits and vegetables is beneficial for overall health, it is not a primary risk factor for lung cancer.
B) Correct. Occupational exposure to asbestos is a significant risk factor for lung cancer development.
C) Incorrect. While regular physical exercise is essential for health, it is not a primary risk factor for lung cancer.
D) Incorrect. Drinking alcohol in moderation may have health implications, but it is not a primary risk factor for lung cancer.
Explanation
A) Incorrect. Smoking is strongly associated with the development of lung cancer.
B) Incorrect. Both heavy and light smokers are at an increased risk of developing lung cancer.
C) Correct. Smoking is the primary cause of lung cancer, accounting for the majority of cases.
D) Incorrect. Passive smoking or exposure to secondhand smoke can increase the risk of lung cancer in non-smokers.
Explanation
A) Incorrect. Radon exposure is associated with an increased risk of lung cancer.
B) Incorrect. Radon exposure can be a risk factor in both urban and rural areas.
C) Correct. Radon is a radioactive gas that can accumulate in homes and is a known risk factor for lung cancer.
D) Incorrect. Radon exposure can increase the risk of lung cancer in both smokers and non-smokers.
Explanation
A) Incorrect. Family history can influence the risk of developing lung cancer.
B) Incorrect. While lung cancer is not purely hereditary, family history can still play a role.
C) Correct. A family history of lung cancer, particularly in first-degree relatives, can increase the individual's risk.
D) Incorrect. A family history of lung cancer itself is relevant to lung cancer risk.
Explanation
A) Incorrect. Air pollution, especially fine particulate matter, can increase lung cancer risk.
B) Incorrect. While smoking is a major risk factor, air pollution remains a significant contributor to lung cancer risk.
C) Correct. Exposure to air pollution, including fine particulate matter, is associated with an increased risk of lung cancer.
D) Incorrect. Air pollution is linked to lung cancer risk, not primarily to skin cancer.
Explanation
A) Incorrect. Lung cancers are primarily categorized as malignant, but the classification is based on the type of malignant cells.
B) Correct. The main types of lung cancer are adenocarcinoma, squamous cell carcinoma, and small cell lung cancer.
C) Incorrect. The classification mentioned includes some types of lung cancer, but it is not comprehensive.
D) Incorrect. While staging is crucial, lung cancers are classified based on their histological type.
Explanation
A) Incorrect. Adenocarcinoma is not necessarily linked to smoking, and it is not the most aggressive type of lung cancer.
B) Correct. Adenocarcinoma is the most common type of lung cancer and often originates from the cells lining the airways.
C) Incorrect. Adenocarcinoma primarily affects the outer parts of the lungs and can have various symptoms.
D) Incorrect. Adenocarcinoma may have different growth rates, and treatment effectiveness depends on multiple factors.
Explanation
A) Incorrect. Small cell lung cancer is known for its rapid growth and is generally harder to cure.
B) Incorrect. Small cell lung cancer is considered aggressive due to its rapid proliferation.
C) Correct. Small cell lung cancer is characterized by rapidly growing cancer cells and is strongly associated with smoking.
D) Incorrect. Small cell lung cancer has a high tendency to spread to other parts of the body.
Explanation
A) Incorrect. Squamous cell carcinoma is not the rarest type of lung cancer.
B) Correct. Squamous cell carcinoma often originates in the central airways of the lungs.
C) Incorrect. Squamous cell carcinoma is commonly associated with smoking.
D) Incorrect. Squamous cell carcinoma is not linked to the formation of fluid-filled sacs in the lungs.
Explanation
A) Incorrect. Large cell carcinoma is not typically slow-growing and does not have the best prognosis.
B) Incorrect. Large cell carcinoma is a distinct type of lung cancer and not a subtype of adenocarcinoma.
C) Correct. Large cell carcinoma is a non-small cell lung cancer known for its aggressive and rapid growth.
D) Incorrect. Large cell carcinoma can metastasize to other parts of the body.
Explanation
A) Incorrect. Fever and chills are not typical symptoms of lung cancer.
B) Incorrect. Weight gain is not commonly associated with lung cancer.
C) Correct. Loss of appetite and unexplained weight loss are common symptoms of lung cancer, often due to the metabolic changes caused by the cancer.
D) Incorrect. Skin rash is not a typical symptom of lung cancer.
Explanation
A) Incorrect. While lung infections can cause various respiratory symptoms, they are not typically associated with hoarseness and difficulty swallowing.
B) Incorrect. Bronchitis primarily affects the airways and does not directly lead to hoarseness and difficulty swallowing.
C) Correct. Tumor compression of the esophagus can result in hoarseness and difficulty swallowing due to the physical obstruction.
D) Incorrect. Allergic reactions to medication may cause various symptoms but are not typically associated with these specific symptoms.
Explanation
A) Incorrect. Chest pain in lung cancer is often related to the disease itself and its effects on nearby tissues.
B) Incorrect. Chest pain in lung cancer is not typically due to an allergic reaction to chemotherapy.
C) Correct. As lung cancer advances, it can invade nearby structures, leading to chest pain.
D) Incorrect. While radiation therapy can have side effects, chest pain is not a normal side effect of radiation for lung cancer.
Explanation
A) Incorrect. Dysphagia refers to difficulty swallowing, not coughing up blood-tinged sputum.
B) Correct. Hemoptysis is the medical term for coughing up blood or blood-tinged sputum, which can occur in lung cancer.
C) Incorrect. Orthopnea is the inability to breathe comfortably while lying flat and is not related to coughing up blood.
D) Incorrect. Tachypnea is rapid breathing and is not related to coughing up blood.
Explanation
A) Incorrect. Arthritis may cause joint pain but is not typically associated with worsening bone pain in the context of lung cancer.
B) Incorrect. Muscular strain can cause localized pain but does not explain worsening bone pain.
C) Correct. Bone metastases occur when cancer spreads to the bones, leading to bone pain and increased risk of fractures.
D) Incorrect. Peripheral neuropathy is characterized by nerve-related symptoms and is not a typical cause of bone pain associated with lung cancer.
Explanation
A) Incorrect. An electrocardiogram (ECG) is used to assess heart function and electrical activity, not to visualize the lungs.
B) Correct. A CT scan is commonly used to visualize the lungs and identify suspicious masses or nodules, making it an important diagnostic tool for lung cancer.
C) Incorrect. Urinalysis is a test of urine composition and is not used to diagnose lung cancer.
D) Incorrect. Colonoscopy is a procedure used to examine the colon and rectum, not the lungs.
Explanation
A) Incorrect. A bone marrow biopsy is not used to diagnose lung cancer.
B) Incorrect. Fine-needle aspiration (FNA) biopsy typically involves the removal of cells from a suspicious mass or nodule, not lung tissue.
C) Correct. Bronchoscopy involves the insertion of a thin, flexible tube into the airways to visualize and obtain a tissue sample from the lungs.
D) Incorrect. An excisional biopsy involves the removal of an entire mass or lesion, and it is not typically used for lung cancer diagnosis.
Explanation
A) Incorrect. Mammography is a breast cancer screening test, not a lung cancer screening test.
B) Incorrect. A Pap smear is used to detect cervical cancer, not lung cancer.
C) Correct. Lung cancer screening with low-dose computed tomography (LDCT) is a screening test recommended for high-risk individuals, such as current or former smokers, to detect lung cancer at an early, more treatable stage.
D) Incorrect. The prostate-specific antigen (PSA) test is used to screen for prostate cancer, not lung cancer.
Explanation
A) Incorrect. A PET scan does not assess blood pressure.
B) Incorrect. Bone density is not the primary focus of a PET scan.
C) Correct. A PET scan primarily assesses cellular metabolism and activity, which can help identify areas of increased metabolic activity, often seen in cancer cells.
D) Incorrect. While lung function is important in lung cancer, a PET scan does not directly assess lung function.
Explanation
A) Incorrect. Fasting for 24 hours before a bronchoscopy is not typically required. However, the client may be asked to avoid food and liquids for a specific period before the procedure.
B) Incorrect. Removal of all jewelry and clothing is not a standard requirement for a bronchoscopy.
C) Incorrect. While a consent form may be required, it is not specifically related to anesthesia for a bronchoscopy.
D) Correct. NPO (nothing by mouth) status for a specified period before the procedure is typically necessary to reduce the risk of aspiration during the bronchoscopy.
Explanation
A) Incorrect. Chemotherapy is typically used for advanced stages of NSCLC or as adjuvant therapy after surgery.
B) Incorrect. Radiation therapy may be used as a primary treatment for NSCLC or in combination with other modalities, but it is not the primary treatment for early-stage disease.
C) Incorrect. Targeted therapy is often used for specific genetic mutations in NSCLC, but it is not the primary treatment for early-stage disease.
D) Correct. Surgical resection involves the removal of the tumor and surrounding tissue and is a common treatment for early-stage NSCLC.
Explanation
A) Correct. Cisplatin and vinorelbine are commonly used as a first-line chemotherapy regimen for SCLC.
B) Incorrect. Erlotinib is a targeted therapy primarily used for non-small cell lung cancer (NSCLC).
C) Incorrect. Pembrolizumab is an immunotherapy drug used in the treatment of NSCLC, particularly in cases with specific genetic mutations.
D) Incorrect. Bevacizumab is a targeted therapy used in combination with chemotherapy for certain cases of NSCLC, but it is not typically used in SCLC.
Explanation
A) Incorrect. Palliative care is not focused on curing cancer but on managing symptoms and improving the patient's overall well-being.
B) Incorrect. While palliative care may extend a patient's life by managing symptoms and side effects, its primary goal is to enhance the quality of life rather than focusing solely on life expectancy.
C) Correct. The primary goal of palliative care is to provide relief from symptoms, alleviate suffering, and enhance the overall quality of life for individuals with serious illnesses, such as advanced lung cancer.
D) Incorrect. Palliative care is a complementary approach to cancer treatment and does not replace other forms of treatment but works alongside them.
Explanation
A) Incorrect. While physical activity can help combat fatigue in some cases, it may not be advisable during radiation therapy. Rest and moderate activity are often recommended.
B) Correct. Applying lotion to the treatment area can help soothe skin changes and alleviate discomfort caused by radiation therapy.
C) Incorrect. Using a heating pad on the treatment area can exacerbate skin irritation and is not recommended during radiation therapy.
D) Incorrect. It is important for clients to stay hydrated during cancer treatment. Avoiding fluids is not advisable.
Explanation
A) Incorrect. While tobacco smoke exposure is a risk factor for lung cancer, it is not a direct cause of pneumonitis.
B) Incorrect. Viral infections can cause respiratory symptoms, but pneumonitis typically results from factors such as radiation therapy or certain medications.
C) Correct. Radiation therapy to the lung is a known cause of pneumonitis, which is inflammation of the lung tissue.
D) Incorrect. Chemotherapy-induced hair loss is a side effect of chemotherapy but is not related to pneumonitis.
Explanation
A) Incorrect. Open communication with friends and family is important for emotional support and should not be avoided.
B) Correct. Support groups provide a safe space for individuals with cancer to share their experiences, express their feelings, and receive support from others facing similar challenges.
C) Incorrect. While staying engaged in activities can be helpful, distraction alone may not effectively address anxiety and fear related to a cancer diagnosis.
D) Incorrect. Ignoring physical symptoms is not advisable, as early symptom recognition and management are important in cancer care.
Explanation
A) Incorrect. Radiation therapy side effects can vary in severity and may not always be immediate or severe.
B) Incorrect. While radiation therapy is targeted to the tumor site, it can affect surrounding tissues and organs.
C) Incorrect. Radiation therapy can be used in combination with chemotherapy, depending on the treatment plan.
D) Correct. Radiation therapy can cause both immediate side effects (such as fatigue and skin changes) and delayed side effects (such as lung inflammation).
Explanation
A) Incorrect. A lobectomy typically involves the removal of a portion of the lung (a lobe) rather than the entire lung.
B) Correct. A lobectomy removes the affected lobe of the lung while preserving the remaining lung tissue and function.
C) Incorrect. Removing lymph nodes in the chest is not the primary purpose of a lobectomy.
D) Incorrect. A lobectomy is a therapeutic procedure, not a diagnostic one.
Explanation
A) Incorrect. The chest tube should only be removed by a healthcare provider, and drainage cessation is not the sole indicator for removal.
B) Incorrect. Encouraging deep breathing and coughing exercises is essential to prevent complications such as pneumonia.
C) Correct. Monitoring and reporting changes in drainage or signs of infection are critical for early detection of complications.
D) Incorrect. It is not advisable to shower with the chest tube in place, as moisture can affect the integrity of the dressing and tubing connections.
Explanation
A) Incorrect. The chest tube should only be removed by a healthcare provider, and drainage cessation is not the sole indicator for removal.
B) Incorrect. Encouraging deep breathing and coughing exercises is essential to prevent complications such as pneumonia.
C) Correct. Monitoring and reporting changes in drainage or signs of infection are critical for early detection of complications.
D) Incorrect. It is not advisable to shower with the chest tube in place, as moisture can affect the integrity of the dressing and tubing connections.
Exams on Pathophysiology of the respiratory system
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Develop more effective diagnostic tools for early detection of tuberculosis.
- Enhance public awareness and education about pneumonia prevention strategies.
- Implement widespread asthma management programs to improve quality of life for affected individuals.
- Identify therapies that improve the prognosis of Chronic Obstructive Pulmonary Disease (COPD) patients.
- Promote smoking cessation and awareness campaigns to reduce COPD-related cases.
- Investigate targeted therapies for specific subtypes of Pulmonary Embolism.
- Enhance education on preventive measures for Pulmonary Embolism, particularly for high-risk groups.
- Identify the interventions and technologies that improve the management of Pulmonary Edema in clinical settings.
- Implement comprehensive screening programs for early detection of lung cancer in high-risk populations.
- Promote smoking cessation initiatives and educate on environmental factors contributing to lung cancer risk.
Tuberculosis
Introduction to tuberculosis
- Tuberculosis (TB) is an infectious disease caused by the bacteria Mycobacterium tuberculosis.
- It mainly affects the lungs, but can also affect other organs such as the brain, kidneys, bones, and lymph nodes.
- TB is spread through the air when a person with active pulmonary TB coughs, sneezes, or speaks.
- People who breathe in the bacteria can become infected, but not everyone who is infected develops active TB.
- Some people have latent TB infection, which means they have no symptoms and cannot transmit the disease, but they may develop active TB in the future if their immune system weakens.
- TB is a global health problem that kills about 1.4 million people each year.
- It is more common in low- and middle-income countries, especially in Africa and Asia, where there are high rates of poverty, malnutrition, HIV/AIDS, and poor access to health care.
- However, TB can affect anyone, regardless of age, gender, race, or socioeconomic status.
- TB can be prevented by avoiding close contact with people who have active TB, wearing a mask or respirator if working in high-risk settings, and getting vaccinated with the Bacille Calmette-Guérin (BCG) vaccine in countries where TB is endemic.
- TB can be cured by taking a combination of antibiotics for at least six months.
- However, some strains of TB are resistant to one or more of the standard drugs, making treatment more difficult and costlier.
- Therefore, it is important to diagnose TB early, complete the full course of treatment, and monitor for any signs of drug resistance.
Pathophysiology
- Tuberculosis (TB) is a chronic infectious disease caused by the bacterium Mycobacterium tuberculosis. TB mainly affects the lungs, but can also spread to other organs through the bloodstream or lymphatic system.
- TB is transmitted through airborne droplets that are expelled when a person with active pulmonary TB coughs, sneezes, speaks, or sings.
- These droplets contain M. tuberculosis and can remain suspended in the air for several hours.
- People who inhale these droplets may become infected with TB.
- When M. tuberculosis enters the lungs, it reaches the alveoli, where it encounters macrophages, which are immune cells that try to engulf and destroy the bacteria.
- However, some bacteria survive and multiply within the macrophages, forming granulomas, which are clusters of infected cells surrounded by other immune cells.
- Granulomas can prevent the bacteria from spreading further, but they can also damage the lung tissue and cause scarring or cavities.
- Most people who are infected with TB do not develop active TB disease, but remain in a latent state, where the bacteria are dormant and do not cause any symptoms. This is called latent TB infection (LTBI).
- People with LTBI are not contagious and cannot spread TB to others.
- However, they have a 5-10% lifetime risk of developing active TB disease, especially if their immune system is weakened by factors such as HIV infection, diabetes mellitus, malnutrition, corticosteroid use, or aging.
- Active TB disease occurs when the bacteria become active and multiply rapidly, causing symptoms such as persistent cough, hemoptysis (coughing up blood), chest pain, night sweats, weight loss, fatigue, and fever.
- Active TB disease can be pulmonary (affecting the lungs) or extrapulmonary (affecting other organs such as the lymph nodes, bones, kidneys, brain, or spine).
- Active TB disease is contagious and can spread TB to others through respiratory droplets.
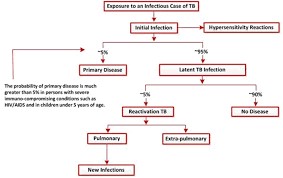
Etiology and risk factors
- The etiology of TB is the infection by Mycobacterium tuberculosis, a rod-shaped bacterium that belongs to the Mycobacteriaceae family.
- The bacteria can survive in harsh environments and can remain dormant for long periods of time inside the human body.
- The bacteria can also mutate and develop resistance to antibiotics over time.
- The risk factors for TB include:
- Close contact with someone who has active pulmonary TB
- Living or working in crowded and poorly ventilated places
- Having a weakened immune system due to HIV/AIDS, diabetes, cancer, malnutrition, or other chronic conditions
- Having a history of previous or incomplete treatment for TB
- Traveling to or living in countries where TB is endemic or prevalent
- Being a health care worker or working in other high-risk occupations such as mining, prison, or military
- Smoking or using tobacco products
- Alcohol or substance abuse
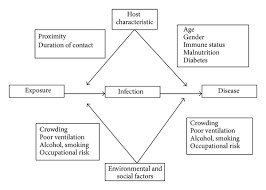
Clinical manifestations and symptoms
- The clinical manifestations and symptoms of TB depend on the site and extent of infection, the immune status of the person, and the presence of any complications.
- The most common symptoms of pulmonary TB are:
- Cough that lasts for more than two weeks, sometimes with blood-stained sputum
- Chest pain or discomfort
- Fever and night sweats
- Weight loss or loss of appetite
- Fatigue or weakness
- Other symptoms may include:
- Shortness of breath or difficulty breathing
- Wheezes or crackles in the lungs
- Enlarged lymph nodes in the neck or armpits
- Hoarseness or loss of voice
- If TB spreads to other organs, it can cause additional symptoms such as:
- Headache or confusion
- Seizures or coma
- Neck stiffness or meningitis
- Vision loss or blindness
- Hearing loss or deafness
- Abdominal pain or swelling
- Diarrhea or constipation
- Nausea or vomiting
- Jaundice or liver failure
- Bone pain or fractures
- Joint pain or arthritis
- Skin rash or ulcers
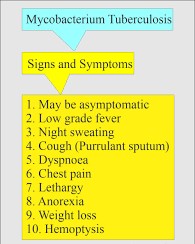
Diagnostic Evaluation
- The diagnostic evaluation for TB involves a combination of history taking, physical examination, laboratory tests, imaging studies, and microbiological confirmation.
- The main methods for diagnosing TB are:
- Tuberculin skin test (TST) or Mantoux test: This is a simple and inexpensive test that involves injecting a small amount of purified protein derivative (PPD) into the forearm and measuring the size of the induration (hardened area) after 48 to 72 hours. A positive result indicates that the person has been exposed to TB bacteria at some point in their life, but does not necessarily mean that they have active TB. A negative result does not rule out TB infection, especially if the person has a weakened immune system or has received the BCG vaccine.
- Interferon-gamma release assay (IGRA): This is a blood test that measures the release of interferon-gamma by white blood cells when they are exposed to antigens from TB bacteria. A positive result indicates that the person has been infected with TB bacteria, but does not necessarily mean that they have active TB. A negative result does not rule out TB infection, especially if the person has a weakened immune system or has received the BCG vaccine.
- Sputum smear microscopy: This is a test that involves examining a sample of sputum (mucus from the lungs) under a microscope for the presence of acid-fast bacilli (AFB), which are characteristic of TB bacteria. A positive result indicates that the person has active pulmonary TB and is infectious. A negative result does not rule out TB infection, as the bacteria may be present in low numbers or in other parts of the body.
- Sputum culture: This is a test that involves growing a sample of sputum in a special medium for several weeks to isolate and identify the type and strain of TB bacteria. A positive result confirms that the person has active TB and allows for testing the sensitivity of the bacteria to different antibiotics. A negative result does not rule out TB infection, as the bacteria may be present in low numbers or in other parts of the body.
- Chest X-ray: This is an imaging study that involves taking a picture of the chest to look for any abnormalities in the lungs or pleura (the membrane that covers the lungs). A chest X-ray can show signs of TB such as cavities, nodules, infiltrates, calcifications, or pleural effusion (fluid around the lungs). However, a chest X-ray cannot distinguish between TB and other lung diseases, and it may be normal in some cases of TB.
- Other tests: Depending on the symptoms and suspected site of infection, other tests may be performed to diagnose TB, such as:
- Biopsy: This is a procedure that involves taking a small sample of tissue from the affected organ and examining it under a microscope for the presence of granulomas (inflammatory lesions) or AFB.
- Lumbar puncture: This is a procedure that involves inserting a needle into the lower back and collecting cerebrospinal fluid (CSF) from the spinal canal. The CSF is then analyzed for signs of meningitis, such as increased pressure, protein, glucose, white blood cells, or AFB.
- Urine analysis: This is a test that involves checking the urine for signs of kidney involvement, such as proteinuria (protein in the urine), hematuria (blood in the urine), or pyuria (pus in the urine).
- Blood tests: These are tests that involve checking the blood for signs of systemic infection, such as anemia (low red blood cell count), leukocytosis (high white blood cell count), thrombocytopenia (low platelet count), or elevated liver enzymes.

Management and Treatment
- The management and treatment of TB aim to eradicate the infection, prevent transmission, and minimize complications.
- The mainstay of TB treatment is a combination of anti-TB drugs that are taken for at least six months. The most commonly used drugs are isoniazid, rifampin, ethambutol, and pyrazinamide.
- The choice and duration of drug therapy depend on factors such as the type and extent of TB, the drug susceptibility of the bacteria, the patient's adherence, and the presence of co-morbidities.
- Some patients may require longer or more intensive treatment, such as those with multidrug-resistant TB (MDR-TB) or extensively drug-resistant TB (XDR-TB), which are resistant to some or most of the first-line drugs. These patients may need second-line drugs, such as fluoroquinolones, injectable agents, and newer drugs like bedaquiline and delamanid. However, these drugs have more side effects and are less effective than the first-line drugs. Therefore, it is essential to ensure proper diagnosis, drug susceptibility testing, and monitoring of treatment response to optimize outcomes and prevent further resistance.
- The management of TB also involves supportive measures, such as:
- nutritional supplementation- Patients with TB should be advised to eat a balanced diet that provides adequate calories, protein, vitamins, and minerals to support healing and immune function. They should also drink plenty of fluids to prevent dehydration and help clear secretions.
- symptom relief- Patients may need analgesics, antipyretics, or anti-inflammatory drugs to relieve pain, fever, or inflammation caused by TB or its treatment.
- psychosocial support- Patients with TB may experience emotional distress, stigma, isolation, or depression due to their condition. They should be offered counseling, peer support, or referral to mental health services as needed.
- patient education- Patients should also be educated about the nature, transmission, prevention, and treatment of TB. They should be encouraged to adhere to their medication regimen, report any adverse effects or signs of treatment failure, and complete their course of therapy. They should also be taught how to prevent spreading the infection to others by covering their mouth and nose when coughing or sneezing, disposing of tissues properly, washing their hands frequently, and avoiding close contact with others until they are no longer infectious.
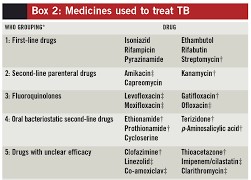
Nursing care and patient education
- Nursing care for patients with TB involves assessing their physical, psychological, social, and educational needs; planning and implementing interventions to meet those needs; and evaluating the outcomes of care.
- Some of the nursing interventions for patients with TB are:
- Assessing the patient's history, symptoms, risk factors, diagnostic tests, drug regimen, adherence level, and response to treatment.
- Monitoring the patient's vital signs, weight, oxygen saturation, chest x-ray findings, sputum smear or culture results, liver function tests, and other laboratory tests as indicated.
- Administering anti-TB drugs as prescribed and observing for any adverse effects or drug interactions.
- Providing nutritional support and advising the patient to eat a balanced diet that meets their caloric and nutritional needs.
- Providing symptom relief and advising the patient to take analgesics, antipyretics, or anti-inflammatory drugs as needed.
- Providing psychosocial support and referring the patient to counseling or mental health services as needed.
- Educating the patient about TB infection control measures such as covering their mouth and nose when coughing or sneezing; disposing of tissues properly; washing their hands frequently; avoiding close contact with others until they are no longer infectious; wearing a mask in public places if advised by their health care provider; and notifying their contacts about their diagnosis and the need for screening.
- Educating the patient about TB prevention measures such as completing their course of therapy; adhering to their medication regimen; reporting any adverse effects or signs of treatment failure; avoiding alcohol or tobacco use; getting adequate rest and exercise; avoiding exposure to other respiratory infections; getting vaccinated for influenza or pneumococcal disease if recommended by their health care provider; and undergoing regular follow-up visits and tests.
- Evaluating the patient's progress toward achieving their goals of care such as curing the infection; preventing transmission; minimizing complications; improving quality of life; enhancing knowledge; increasing self-efficacy; reducing stigma; and increasing satisfaction.
Summary
- Tuberculosis is a chronic infectious disease caused by Mycobacterium tuberculosis that mainly affects the lungs.
- It can be transmitted through respiratory droplets from an infected person who is coughing or sneezing. The symptoms of TB include cough, weight loss or anorexia, fever, night sweats, hemoptysis, chest pain, and fatigue.
- The diagnosis of TB is based on history, physical examination, chest x-ray, sputum smear or culture, and other tests as indicated.
- The treatment of TB involves a combination of anti-TB drugs that are taken for at least six months.
- The choice and duration of drug therapy depend on factors such as the type and extent of TB, the drug susceptibility of the bacteria, the patient's adherence, and the presence of comorbidities.
- The management of TB also involves supportive measures, such as nutritional supplementation, symptom relief, psychosocial support, and patient education.
- Nursing care for patients with TB involves assessing their needs; planning and implementing interventions to meet those needs; and evaluating the outcomes of care.
Conclusion
- Tuberculosis is a serious public health problem that requires prompt diagnosis, effective treatment, and comprehensive care.
- Nurses play a vital role in providing care for patients with TB by:
- administering anti-TB drugs
- monitoring their response to treatment
- providing nutritional, symptomatic, and psychosocial support
- educating them about TB infection control and prevention measures
- evaluating their progress toward achieving their goals of care
- By doing so, nurses can help patients with TB to overcome their infection, prevent transmission, and improve their quality of life.
Pneumonia
Introduction
- Pneumonia is an inflammation of the alveoli, the tiny air sacs in the lungs where gas exchange occurs.
- Pneumonia is a common and potentially serious respiratory infection that affects millions of people worldwide each year.
- Pneumonia can be caused by bacteria, viruses, fungi, or other microorganisms.
- Pneumonia can affect one or both lungs, and can range from mild to severe.
- Pneumonia is a serious health problem that can lead to complications such as respiratory failure, sepsis, and death.
- It is a leading cause of illness and mortality, particularly among vulnerable populations such as young children, the elderly, and individuals with compromised immune systems.
- Pneumonia presents a diverse clinical spectrum, ranging from mild, self-limiting cases to severe, life-threatening illnesses.
- It is a dynamic disease that can develop suddenly or progress gradually, often with symptoms such as fever, cough, chest pain, and difficulty breathing.
- Due to its variable clinical presentation and the multitude of causative agents, accurate diagnosis and appropriate treatment are essential for ensuring optimal patient outcomes.
- The impact of pneumonia extends beyond individual health, affecting healthcare systems and societies as a whole.
- It places a significant burden on healthcare resources, leading to hospital admissions, increased healthcare costs, and lost productivity.
- Furthermore, pneumonia remains a global public health concern, particularly in resource-limited regions, where access to healthcare and vaccinations may be limited, contributing to higher rates of morbidity and mortality.

Pathophysiology
- The pathophysiology of pneumonia involves a series of events initiated by the inhalation of infectious agents, such as bacteria, viruses, fungi, or less commonly, parasites as outlined below:
- Inhalation of Pathogens: Pneumonia typically begins when infectious microorganisms are inhaled into the respiratory tract. These pathogens may be present in the environment or as part of the individual's normal respiratory flora.
- Alveolar Invasion: Once inside the lungs, the pathogens reach the alveoli, where they encounter the host's immune defenses. The alveoli are the primary sites for gas exchange, and their infection disrupts this crucial function.
- Immune Response: The host's immune system, including alveolar macrophages and neutrophils, responds to the invading pathogens. These immune cells attempt to engulf and neutralize the microbes through phagocytosis. Additionally, the immune system activates an inflammatory response.
- Inflammatory Response: The activation of immune cells and the release of pro-inflammatory cytokines, such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), result in the characteristic signs of pneumonia, including fever, localized chest pain, and an increase in white blood cells.
- Exudate Formation: The inflammatory response leads to the accumulation of exudate in the alveoli. This exudate consists of fluid, dead immune cells, and debris, impairing the normal exchange of oxygen and carbon dioxide. This is often referred to as consolidation.
- Impaired Gas Exchange: As the infection progresses, the exudate and inflammation cause the alveoli to become less compliant and filled with fluid, reducing their ability to participate in gas exchange. This results in hypoxemia, which can lead to respiratory distress and increased work of breathing.
- Consolidation and Alveolar Collapse: In severe cases, the alveolar walls may collapse, leading to a condition known as atelectasis. This further impairs gas exchange and can cause areas of the lung to become nonfunctional.
- Systemic Effects: Pneumonia can have systemic effects on the body. The release of pro-inflammatory cytokines and the presence of bacterial toxins in the bloodstream can lead to sepsis, a potentially life-threatening condition characterized by widespread inflammation, organ dysfunction, and shock.
- Resolution or Progression: The outcome of pneumonia can vary widely. In some cases, the immune system effectively clears the infection, and the lung tissue gradually heals. In others, the infection can progress, leading to complications such as lung abscesses, pleural effusion, or dissemination of the pathogen to other organs.
- Chronic Pneumonia: Chronic pneumonia may develop in cases where the initial infection is not adequately treated or in individuals with underlying lung conditions. Chronic pneumonia can lead to structural lung damage and fibrosis
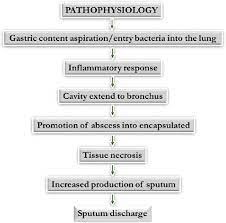
Etiology and risk factors
- Pneumonia can be classified into different types based on the causative agent, the location of infection, and the mode of acquisition.
- The most common types of pneumonia are:
- Community-acquired pneumonia (CAP): Pneumonia that occurs in people who have not been hospitalized or in contact with health care facilities in the past 14 days. The most common causes of CAP are Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, Mycoplasma pneumoniae, and respiratory viruses.
- Hospital-acquired pneumonia (HAP): Pneumonia that occurs 48 hours or more after admission to a hospital or health care facility. The most common causes of HAP are Staphylococcus aureus (including methicillin-resistant S. aureus or MRSA), Pseudomonas aeruginosa, Klebsiella pneumoniae, and Escherichia coli.
- Ventilator-associated pneumonia (VAP): Pneumonia that occurs 48 hours or more after intubation and mechanical ventilation. The most common causes of VAP are similar to HAP, but also include Acinetobacter baumannii and Enterobacter species.
- Aspiration pneumonia: Pneumonia that occurs when foreign material, such as food, saliva, or gastric contents, is inhaled into the lungs. The most common causes of aspiration pneumonia are anaerobic bacteria, such as Bacteroides, Fusobacterium, and Peptostreptococcus.
- Fungal pneumonia: Pneumonia that occurs when fungi infect the lungs. The most common causes of fungal pneumonia are Candida albicans, Aspergillus fumigatus, Cryptococcus neoformans, Histoplasma capsulatum, and Pneumocystis jirovecii.
- Some of the risk factors for developing pneumonia are:
- Age: Older adults and young children are more susceptible to pneumonia due to weaker immune systems and lower lung capacity.
- Smoking: Smoking damages the cilia, the hair-like structures that help clear mucus and debris from the lungs. Smoking also increases the risk of chronic obstructive pulmonary disease (COPD), which predisposes to pneumonia.
- Chronic lung diseases: Conditions such as asthma, COPD, cystic fibrosis, bronchiectasis, and pulmonary fibrosis impair lung function and increase the risk of pneumonia.
- Immunocompromised states: Conditions such as HIV/AIDS, cancer, organ transplantation, diabetes mellitus, chronic kidney disease, liver disease,
- and autoimmune disorders weaken the immune system and increase the risk of pneumonia.
- Medications: Certain medications such as corticosteroids, chemotherapy drugs,
- immunosuppressants, proton pump inhibitors (PPIs), and antacids reduce the body's ability to fight infections and increase the risk of pneumonia.
- Other factors that can also increase the risk of pneumonia include:
- Malnutrition
- dehydration
- alcohol abuse
- poor oral hygiene
- influenza
- allergies
- exposure to air pollution
- dust
- chemicals

Clinical manifestations and symptoms
- The signs and symptoms of pneumonia vary depending on the type, severity, and underlying conditions of the patient.
- Some of the common signs and symptoms are:
- Fever
- Chills
- Cough
- Sputum production
- Dyspnea
- Tachypnea
- Chest pain
- Pleural effusion
- Crackles
- Wheezes
- Rhonchi
- Decreased breath sounds
- Cyanosis
- Hypoxemia
- Confusion
- Fatigue
- Anorexia
- Nausea
- Vomiting
- Diarrhea
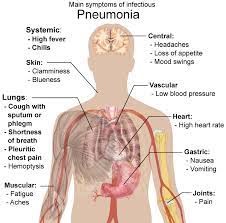
Diagnostic Evaluation
- The diagnosis of pneumonia is based on the history, physical examination, and laboratory and imaging tests.
- Some of the tests that are used to diagnose pneumonia are:
- Chest X-ray: A chest X-ray can show the presence and extent of lung consolidation, infiltrates, cavities, or pleural effusion. A chest X-ray can also help differentiate between bacterial and viral pneumonia, as bacterial pneumonia tends to cause lobar or segmental consolidation, while viral pneumonia tends to cause interstitial or diffuse infiltrates.
- Sputum culture and Gram stain: A sputum culture and Gram stain can help identify the causative organism and guide antibiotic therapy. A sputum sample should be obtained before starting antibiotics, if possible, and should be collected by expectoration, suctioning, or bronchoscopy.
- Blood culture: A blood culture can help detect bacteremia or sepsis, which are serious complications of pneumonia. A blood culture should be obtained before starting antibiotics, if possible, and should be collected from two different sites.
- Complete blood count (CBC): A CBC can show the presence of leukocytosis, leukopenia, neutrophilia, neutropenia, lymphocytosis, lymphopenia, eosinophilia, or eosinopenia, which can indicate the type and severity of infection. A CBC can also show the presence of anemia or thrombocytopenia, which can indicate complications such as hemolysis or disseminated intravascular coagulation (DIC).
- C-reactive protein (CRP): A CRP is a nonspecific marker of inflammation that can help monitor the response to treatment and the prognosis of pneumonia. A CRP level can also help differentiate between bacterial and viral pneumonia, as bacterial pneumonia tends to cause a higher CRP level than viral pneumonia.
- Procalcitonin (PCT): A PCT is a biomarker of bacterial infection that can help guide antibiotic therapy and the prognosis of pneumonia. A PCT level can also help differentiate between bacterial and viral pneumonia, as bacterial pneumonia tends to cause a higher PCT level than viral pneumonia.
- Arterial blood gas (ABG): An ABG can measure the pH, partial pressure of oxygen (PaO2), partial pressure of carbon dioxide (PaCO2), bicarbonate (HCO3), and oxygen saturation (SaO2) of the blood. An ABG can help assess the severity of hypoxia, hypercapnia, and acidosis, which are indicators of respiratory failure.
- Pulse oximetry: Pulse oximetry can measure the percentage of hemoglobin that is saturated with oxygen (SpO2) in the peripheral blood. Pulse oximetry can help monitor the oxygenation status of the patient and the need for supplemental oxygen therapy.
- Other tests: Other tests that may be used to diagnose pneumonia include:
- urine antigen tests
- serology tests
- polymerase chain reaction (PCR) tests
- bronchoalveolar lavage (BAL)
- thoracentesis
- lung biopsy
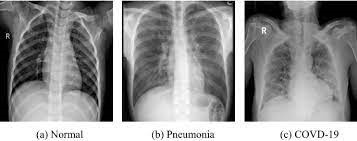
Management and Treatment
- The management and treatment of pneumonia depend on the type, severity, and causative agent of the infection.
- The main goals are to eradicate the infection, relieve the symptoms, prevent complications, and restore lung function.
- The following are some of the common interventions for pneumonia:
- Antibiotics are the mainstay of treatment for bacterial pneumonia. The choice of antibiotic depends on the suspected organism, local resistance patterns, patient's allergies, and clinical response. Some examples of antibiotics used for pneumonia are penicillin, amoxicillin, azithromycin, clarithromycin, doxycycline, levofloxacin, and ceftriaxone.
- Antiviral drugs are used for viral pneumonia, such as influenza or COVID-19. These drugs may reduce the duration and severity of symptoms, but they are not effective for all types of viruses. Some examples of antiviral drugs are oseltamivir, zanamivir, baloxavir, remdesivir, and monoclonal antibodies.
- Antifungal drugs are used for fungal pneumonia, such as Pneumocystis jirovecii or Aspergillus. These drugs may be given orally or intravenously, depending on the type and extent of the infection. Some examples of antifungal drugs are trimethoprim-sulfamethoxazole, pentamidine, voriconazole, caspofungin, and amphotericin B.
- Oxygen therapy is indicated for patients with hypoxemia (low blood oxygen level) or respiratory distress. Oxygen can be delivered via nasal cannula, face mask, or mechanical ventilation. The goal is to maintain oxygen saturation above 90% or partial pressure of oxygen above 60 mmHg.
- Bronchodilators are used to relax the smooth muscles of the airways and improve airflow. They may be given by inhalation or nebulization. They are especially helpful for patients with underlying asthma or chronic obstructive pulmonary disease (COPD). Some examples of bronchodilators are albuterol, ipratropium, salmeterol, and tiotropium.
- Corticosteroids are used to reduce inflammation and edema in the lungs. They may be given orally or intravenously. They are usually reserved for patients with severe pneumonia or those who do not respond to antibiotics. Some examples of corticosteroids are prednisone, methylprednisolone, and dexamethasone.
- Analgesics are used to relieve pain and discomfort caused by coughing or chest wall inflammation. They may be given orally or intravenously. They should be used with caution in patients with respiratory depression or impaired liver function. Some examples of analgesics are acetaminophen, ibuprofen, naproxen, and morphine.
- Antipyretics are used to lower fever and reduce metabolic demand. They may be given orally or intravenously. They should be used with caution in patients with liver dysfunction or bleeding disorders. Some examples of antipyretics are acetaminophen, ibuprofen, naproxen, and aspirin.
Nursing care and patient education
- Nursing care for patients with pneumonia involves:
- monitoring vital signs
- oxygen saturation
- respiratory rate and pattern
- breath sounds
- sputum production and characteristics
- level of consciousness
- fluid and electrolyte balance
- nutritional status
- response to treatment
- The following are some of the nursing interventions for pneumonia:
- Maintain a patent airway by suctioning secretions as needed, positioning the patient in semi-Fowler's or high-Fowler's position (unless contraindicated), encouraging coughing and deep breathing exercises every 2 hours (or as tolerated), providing humidified oxygen as prescribed (or as needed), and administering bronchodilators as ordered.
- Promote effective gas exchange by monitoring arterial blood gas (ABG) results (or pulse oximetry readings), adjusting oxygen flow rate as needed (or as ordered), assessing for signs of hypoxemia (such as cyanosis, confusion, restlessness) or hypercapnia (such as headache, drowsiness), and notifying the physician if any abnormalities occur.
- Prevent infection transmission by following standard precautions (or droplet precautions if indicated), washing hands before and after contact with the patient (or using alcohol-based hand sanitizer), wearing personal protective equipment (such as gloves, mask) as appropriate (or as required), isolating the patient if necessary (or as advised), educating the patient and family about the mode of transmission and prevention measures (such as covering mouth and nose when coughing or sneezing, disposing tissues properly), and ensuring adequate ventilation in the room (or in the environment).
- Relieve pain and discomfort by administering analgesics as prescribed (or as needed), assessing the effectiveness and side effects of the medication, applying warm or cold compresses to the chest wall (or as preferred by the patient), providing comfort measures (such as massage, music, distraction), and encouraging the patient to express feelings and concerns.
- Maintain fluid and electrolyte balance by monitoring intake and output, daily weight, and serum electrolyte levels, encouraging oral fluid intake (unless contraindicated), providing intravenous fluids as ordered (or as needed), assessing for signs of dehydration (such as dry mucous membranes, poor skin turgor) or fluid overload (such as edema, crackles), and notifying the physician if any imbalances occur.
- Promote optimal nutrition by assessing the patient's nutritional status, dietary preferences, and swallowing ability, providing a high-calorie, high-protein diet (unless contraindicated), offering small, frequent meals (or as tolerated by the patient), supplementing with oral or enteral nutrition as ordered (or as needed), assisting with feeding as necessary (or as requested by the patient), and monitoring for signs of malnutrition (such as weight loss, muscle wasting) or aspiration (such as coughing, choking).
- Enhance activity tolerance by assessing the patient's baseline activity level, physical condition, and fatigue level, providing rest periods between activities (or as needed by the patient), assisting with activities of daily living as necessary (or as desired by the patient), encouraging gradual increase in physical activity (as tolerated by the patient), and monitoring for signs of exertion (such as dyspnea, tachycardia).
- Patient education is an essential part of nursing care for patients with pneumonia.
- The following are some of the topics that should be covered with the patient and family:
- The nature, cause, and course of pneumonia
- The signs and symptoms of pneumonia and when to seek medical attention
- The treatment regimen and possible side effects
- The importance of compliance with medication therapy and follow-up appointments
- The prevention measures to avoid recurrence or complications of pneumonia
- The lifestyle modifications to promote recovery and prevent further lung damage
- The available resources and support groups for patients with pneumonia
Summary
- Pneumonia is a common respiratory infection that causes inflammation of the lung parenchyma.
- It can be classified into four types: community-acquired pneumonia, health care–associated pneumonia, pneumonia in the immunocompromised host, and aspiration pneumonia.
- The management and treatment of pneumonia depend on the type, severity, and causative agent of the infection.
- The main goals are to eradicate the infection, relieve the symptoms, prevent complications, and restore lung function.
- Nursing care for patients with pneumonia involves monitoring vital signs, oxygen saturation, respiratory rate and pattern, breath sounds, sputum production and characteristics, level of consciousness, fluid and electrolyte balance, nutritional status, and response to treatment.
- Nursing interventions include maintaining a patent airway, promoting effective gas exchange, preventing infection transmission, relieving pain and discomfort, maintaining fluid and electrolyte balance, promoting optimal nutrition, and enhancing activity tolerance.
- Patient education is an essential part of nursing care for patients with pneumonia.
- It covers topics such as the nature, cause, and course of pneumonia; the signs and symptoms of pneumonia and when to seek medical attention; the treatment regimen and possible side effects; the importance of compliance with medication therapy and follow-up appointments; the prevention measures to avoid recurrence or complications of pneumonia; the lifestyle modifications to promote recovery and prevent further lung damage; and the available resources and support groups for patients with pneumonia.
Conclusion
- Pneumonia is a serious respiratory infection that can affect anyone at any age.
- It requires prompt diagnosis and treatment to prevent life-threatening complications.
- Nurses play a vital role in providing holistic care for patients with pneumonia.
- They assess the patient's condition, implement appropriate interventions, evaluate the outcomes, educate the patient and family, and collaborate with other health care professionals.
- By doing so, they can help improve the quality of life and prognosis of patients with pneumonia.
Asthma
Introduction
- Asthma is a chronic inflammatory disease of the airways that causes airway hyperresponsiveness, mucosal edema, and mucus production.
- Asthma affects people of different ages and can lead to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing.
- Asthma can be triggered by various factors such as allergens, irritants, exercise, stress, medications, and infections.
- Asthma can be classified as intermittent, mild persistent, moderate persistent, or severe persistent based on the frequency and severity of symptoms.
- Asthma can also be classified as allergic or non-allergic based on the presence or absence of immunoglobulin E (IgE) mediated response to specific allergens.
- Asthma is a common and potentially serious condition that requires proper diagnosis, management, and education to prevent complications and improve quality of life.
Pathophysiology
- The underlying pathophysiology of asthma is reversible and diffuse airway inflammation that leads to airway narrowing and obstruction.
- The inflammation is mediated by various cells and molecules such as mast cells, eosinophils, basophils, neutrophils, lymphocytes, macrophages, cytokines, chemokines, leukotrienes, prostaglandins, histamine, and nitric oxide.
- The inflammation results in two main processes:
- Bronchoconstriction
- airway remodeling
- Bronchoconstriction is the acute contraction of the smooth muscle in the bronchial walls that reduces the diameter of the airways and increases the resistance to airflow.
- Bronchoconstriction can be triggered by exposure to allergens, irritants, cold air, exercise, or emotional stress.
- Bronchoconstriction can be reversed by bronchodilators such as beta2-agonists that relax the smooth muscle.
- Airway remodeling is the chronic structural change in the airways that occurs due to prolonged inflammation and tissue damage.
- Airway remodeling can include subepithelial fibrosis, increased smooth muscle mass, mucus hypersecretion, goblet cell hyperplasia, epithelial cell shedding, angiogenesis, and edema. Airway remodeling can lead to irreversible airflow limitation and reduced responsiveness to bronchodilators.
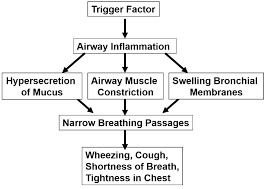
Etiology and risk factors
- The etiology of asthma is multifactorial and involves genetic and environmental factors that interact to influence the development and expression of the disease.
- Some of the factors that influence the development of asthma are:
- Allergy: Allergy is the strongest predisposing factor for asthma. About 80% of children and 50% of adults with asthma have allergic sensitization to one or more allergens such as dust mites, animal dander, pollen, mold, cockroaches, or food.
- Family history: Asthma has a strong familial aggregation and heritability. Having a parent or sibling with asthma increases the risk of developing asthma by two to six times.
- Atopy: Atopy is the genetic tendency to produce IgE antibodies in response to exposure to common environmental allergens. Atopy is associated with increased risk of developing asthma and other allergic diseases such as allergic rhinitis and eczema.
- Gender: Asthma is more prevalent in boys than girls before puberty but more prevalent in women than men after puberty. The reasons for this gender difference are not fully understood but may involve hormonal, immunological, anatomical, or behavioral factors.
- Obesity: Obesity is associated with increased risk of developing asthma and worse asthma control. Obesity may affect asthma by increasing inflammation, reducing lung volume, impairing respiratory mechanics, or altering immune response.
- Smoking: Smoking is a major risk factor for developing asthma and worsening asthma outcomes. Smoking can cause direct damage to the airways.
- Respiratory infections: Viral respiratory infections, especially during early childhood, are known to be a risk factor for the development of asthma. Respiratory syncytial virus (RSV) and rhinovirus infections, in particular, have been associated with an increased risk of asthma in children.
- Environmental exposures: Exposure to certain environmental factors, such as secondhand smoke, air pollution, and occupational exposures to allergens or irritants, can contribute to the development or exacerbation of asthma. Prolonged exposure to indoor and outdoor air pollutants can irritate the airways and increase the risk of asthma symptoms.
- Early life exposures: Early life factors, including exposure to allergens, infections, and diet during infancy, can influence the risk of developing asthma. For example, exposure to allergens like dust mites or pet allergens in the home during infancy may increase the likelihood of developing allergies and asthma later in life.
- Socioeconomic factors: Socioeconomic status can play a role in asthma risk. Individuals from lower socioeconomic backgrounds may face increased exposure to environmental triggers, have limited access to healthcare, and experience disparities in asthma management and control.
- Psychological factors: Stress and psychological factors can impact asthma symptoms and control. High levels of stress or anxiety may exacerbate asthma symptoms, although the exact mechanisms are complex and not fully understood.
- Airway hyperresponsiveness: Individuals with airway hyperresponsiveness have overly sensitive airways that are more likely to constrict in response to various triggers. This hyperresponsiveness is a risk factor for asthma and can be measured through lung function tests.
- Occupational exposures: Certain occupational exposures to allergens or irritants, such as dust, fumes, or chemicals, can lead to occupational asthma. This type of asthma is specifically triggered by workplace conditions and is a recognized risk for individuals in certain occupations.
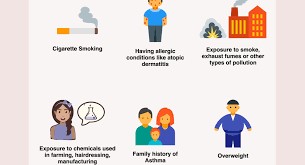
Clinical manifestations and symptoms
- The signs and symptoms of asthma vary from person to person and may include:
- Coughing
- Wheezing
- chest tightness
- dyspnea
- tachypnea
- use of accessory muscles
- prolonged expiration
- decreased breath sounds
- hypoxemia
- Asthma symptoms can be intermittent or persistent, mild or severe, and may be triggered by various factors.
- Patients with asthma may experience symptom-free periods alternating with acute exacerbations that last from minutes to hours or days.
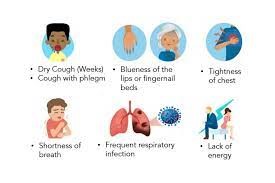
Diagnostic Evaluation
- The diagnosis of asthma is based on a combination of:
- History
- physical examination
- spirometry
- peak expiratory flow (PEF) measurement
- chest X-ray (CXR)
- allergy testing
- Spirometry is used to measure the forced expiratory volume in 1 second (FEV1) and the forced vital capacity (FVC), which are reduced in asthma due to airway obstruction.
- PEF measurement is used to monitor the severity and variability of asthma.
- CXR is used to rule out other causes of respiratory symptoms.
- Allergy testing is used to identify specific allergens that trigger asthma.

Management and Treatment
- The goals of asthma management are to achieve good symptom control, maintain normal lung function, prevent exacerbations, minimize the need for rescue medications, and avoid adverse effects from therapy.
- Asthma management involves pharmacologic therapy, peak flow monitoring, avoidance of triggers, patient education, and self-management skills.
- Pharmacologic therapy includes two types of medications: controllers and relievers.
- Controllers are long-term medications that prevent or reduce inflammation and bronchoconstriction, such as inhaled corticosteroids (ICS), long-acting beta2-agonists (LABA), leukotriene receptor antagonists (LTRA), and biologic agents.
- Relievers are short-term medications that provide quick relief of bronchospasm and symptoms, such as short-acting beta2-agonists (SABA), anticholinergics, and oral corticosteroids (OCS).
- Peak flow monitoring is used to assess the degree of airflow limitation and adjust the treatment accordingly.
- Avoidance of triggers is important to prevent or reduce exposure to allergens and irritants that worsen asthma.
- Patient education and self-management skills are essential to empower patients to recognize and manage their asthma symptoms, adhere to their treatment plan, use their inhaler devices correctly, and seek medical help when needed.
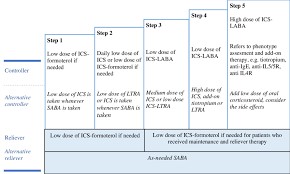
Nursing care and patient education
- Nursing care for patients with asthma involves assessing the patient's respiratory status, administering medications, monitoring peak flow, providing oxygen therapy, and teaching the patient how to manage their condition.
- Some of the nursing interventions for asthma are:
- Assess the patient's respiratory rate, rhythm, depth, and effort. Note any signs of respiratory distress, such as wheezes, cough, dyspnea, use of accessory muscles, or cyanosis.
- Administer bronchodilators and anti-inflammatory medications as prescribed. These include short-acting beta2-agonists (SABAs), long-acting beta2-agonists (LABAs), inhaled corticosteroids (ICS), leukotriene receptor antagonists (LTRAs), and biologic therapy for severe asthma.
- Monitor the patient's peak expiratory flow (PEF) using a peak flow meter. This is a device that measures how fast the patient can exhale. The patient should record their personal best PEF and use it as a reference for their asthma action plan.
- Provide oxygen therapy as needed to maintain adequate oxygen saturation. Use a pulse oximeter to monitor the patient's oxygen level. Adjust the oxygen flow rate according to the patient's condition and response.
- Teach the patient how to recognize and avoid asthma triggers, such as allergens, irritants, exercise, stress, medications, or infections. Advise the patient to keep their environment clean and free of dust, mold, smoke, or pet dander.
- Teach the patient how to use their inhalers and spacers correctly. Demonstrate the proper technique and have the patient return the demonstration. Instruct the patient to rinse their mouth after using ICS to prevent oral candidiasis.
- Teach the patient how to follow their asthma action plan. This is a written document that tells the patient how to adjust their medications and when to seek medical help based on their symptoms and PEF readings. The action plan should include three zones: green (good control), yellow (caution), and red (emergency).
- Teach the patient how to manage acute asthma exacerbations. This includes using their SABA inhaler as needed, increasing their fluid intake, resting in a comfortable position, and seeking emergency care if their symptoms do not improve or worsen.
Summary
- Asthma is a chronic inflammatory disease of the airways that causes airway hyperresponsiveness, mucosal edema, and mucus production.
- Asthma can cause recurrent episodes of wheezing, coughing, chest tightness, and dyspnea.
- Asthma can be triggered by various factors, such as allergens, irritants, exercise, stress, medications, or infections.
- Asthma can be diagnosed by history, physical examination, spirometry, peak flow monitoring, chest X-ray, and allergy testing.
- Asthma can be treated by pharmacologic therapy, which includes bronchodilators and anti-inflammatory agents; and non-pharmacologic therapy, which includes avoiding triggers, using peak flow meters, following an asthma action plan, and receiving education.
Conclusion
- Asthma is a common but serious respiratory condition that requires ongoing management and monitoring.
- Nurses play a vital role in providing care and education for patients with asthma.
- Nurses should assess the patient's respiratory status, administer medications, monitor peak flow, provide oxygen therapy, and teach the patient how to manage their condition.
- By doing so, nurses can help patients with asthma achieve better control of their symptoms and improve their quality of life.
Chronic Obstructive Pulmonary Disease (COPD)
Introduction
- Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable, and treatable disease.
- It is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities, usually caused by significant exposure to noxious particles or gases.
- COPD is a heterogeneous lung condition that includes chronic bronchitis and emphysema, which are associated with chronic inflammation and abnormal inflammatory responses in the lungs.
- COPD is a major cause of morbidity and mortality worldwide, and it poses a significant burden on the health care system and the quality of life of patients and their families.
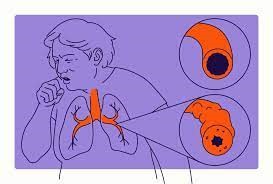
Pathophysiology
- COPD is a progressive disease that affects the lungs and leads to narrowing of the airways and changes in lung parenchyma and pulmonary vasculature.
- In the airways, there are increased mucus production, thickening of the airway wall, and overall narrowing.
- In the lung parenchyma, alveolar wall destruction and loss of elastic recoil occur.
- Imbalances of substances in the lung, such as proteinases, can further contribute to airflow limitation.
- These changes can be influenced by factors like chronic inflammation, environmental exposures, and genetic factors like alpha1-antitrypsin deficiency.
- The airflow limitation in COPD results in reduced expiratory flow rate, increased residual volume, hyperinflation, ventilation-perfusion mismatch, hypoxemia, hypercapnia, and respiratory acidosis.
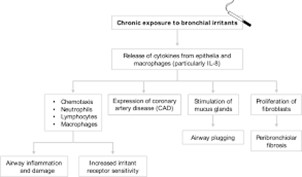
Etiology and risk factors
- The main risk factor for COPD is cigarette smoking, which accounts for about 80% of cases.
- Other risk factors include:
- exposure to biomass fuels
- occupational dusts and chemicals
- air pollution
- recurrent respiratory infections
- asthma
- bronchiectasis
- tuberculosis
- HIV infection
- Malnutrition
- Genetic factors such as alpha1-antitrypsin deficiency can also predispose to COPD, especially in young patients with severe emphysema.
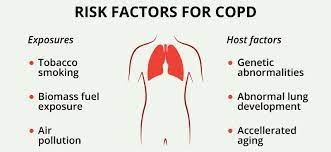
Clinical manifestations and symptoms
- The main symptoms of COPD are:
- Dyspnea
- chronic cough
- sputum production
- wheezes
- These symptoms may vary in severity and frequency depending on the stage of the disease, the presence of exacerbations, and the coexistence of other comorbidities.
- Dyspnea is usually progressive and worsens with exertion or emotional stress.
- Chronic cough may be productive or nonproductive and may be worse in the morning or at night.
- Sputum production may be clear, white, yellow, or green depending on the degree of infection or inflammation.
- Wheezes are caused by airway narrowing and may be audible or detected by auscultation.
- Other signs and symptoms of COPD may include:
- chest tightness
- fatigue
- weight loss
- anorexia
- cyanosis
- barrel chest
- pursed-lip breathing
- use of accessory muscles
- tripod position
- decreased breath sounds
- crackles
- rhonchi
- prolonged expiratory phase
- cor pulmonale (right-sided heart failure)
- peripheral edema
- jugular venous distension (JVD)
- hepatomegaly (enlarged liver)
- ascites (fluid accumulation in abdomen)
- polycythemia (increased red blood cells)
- pulmonary hypertension (high blood pressure in lungs)
- respiratory failure
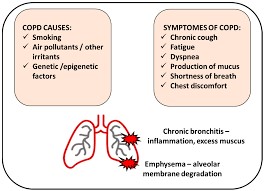
Diagnostic Evaluation
- The diagnosis of COPD is based on clinical history, physical examination, and spirometry.
- Spirometry is the gold standard for measuring airflow limitation and assessing the severity of COPD. It involves measuring the forced expiratory volume in one second (FEV1) and the forced vital capacity (FVC) of the lungs.
- ratio of FEV1/FVC is used to determine the presence and degree of airflow obstruction. A ratio of less than 0.7 indicates airflow limitation consistent with COPD.
- The severity of COPD is classified according to the GOLD (Global Initiative for Chronic Obstructive Lung Disease) criteria, which are based on the post-bronchodilator FEV1 as a percentage of the predicted normal value. The four stages are:
- Stage I: Mild COPD (FEV1 ≥ 80% predicted)
- Stage II: Moderate COPD (FEV1 50-79% predicted)
- Stage III: Severe COPD (FEV1 30-49% predicted)
- Stage IV: Very severe COPD (FEV1 < 30% predicted or FEV1 < 50% predicted with chronic respiratory failure or right heart failure)
- Other diagnostic tests that may be performed include:
- chest x-ray
- arterial blood gas analysis
- pulse oximetry
- sputum culture
- alpha1-antitrypsin level
- electrocardiogram
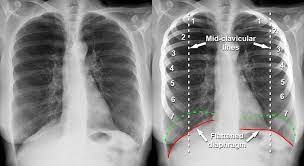
Management and Treatment
- The main goals of management and treatment of COPD are to reduce symptoms, improve quality of life, prevent exacerbations, and reduce mortality.
- The main components of management and treatment are:
- Smoking cessation is the most effective intervention to slow the progression of COPD and reduce mortality. It should be offered to all patients with COPD who smoke, using a combination of behavioral support and pharmacotherapy (such as nicotine replacement therapy, bupropion, or varenicline).
- Pharmacotherapy for COPD includes bronchodilators, corticosteroids, mucolytics, antibiotics, and oxygen therapy.
- Bronchodilators are the mainstay of pharmacotherapy and can be classified into short-acting (SABA) or long-acting (LABA) beta2-agonists, short-acting (SAMA) or long-acting (LAMA) anticholinergics, and methylxanthines. They work by relaxing the smooth muscle of the airways and improving airflow.
- Corticosteroids have anti-inflammatory effects and can be administered orally or inhaled. They are usually reserved for patients with severe or very severe COPD or frequent exacerbations.
- Mucolytics help to thin and clear the mucus from the airways and may reduce exacerbations.
- Antibiotics are used to treat bacterial infections that may trigger or worsen exacerbations. Oxygen therapy is indicated for patients with chronic hypoxemia (PaO2 < 55 mmHg or SaO2 < 88%) or signs of tissue hypoxia (such as cor pulmonale or polycythemia). It can be delivered via nasal cannula, face mask, or transtracheal catheter.
- Non-pharmacological interventions for COPD include:
- Pulmonary rehabilitation- is a comprehensive program that involves education, exercise training, nutritional counseling, psychosocial support, and self-management skills. It aims to improve physical function, reduce symptoms, enhance quality of life, and reduce hospitalizations.
- Nutrition counseling- is important to maintain a healthy weight and prevent malnutrition or obesity
- Immunization- Immunization against influenza and pneumococcal infection can prevent respiratory infections that may worsen COPD.
- Exercise training- can improve muscle strength, endurance, and oxygen utilization.
- breathing techniques- such as pursed-lip breathing and diaphragmatic breathing can reduce dyspnea and improve ventilation.
- Energy conservation strategies- can help patients cope with daily activities without excessive fatigue.
- Psychosocial support can address the emotional and social aspects of living with COPD.
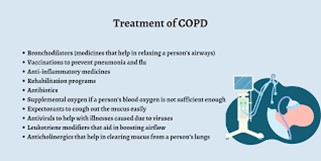
Nursing care and patient education
- Nursing care for patients with COPD involves:
- assessing their respiratory status
- monitoring their vital signs and oxygen saturation
- administering medications and oxygen therapy as prescribed
- providing comfort measures such as positioning and humidification
- promoting infection control measures such as hand hygiene and isolation precautions
- assisting with activities of daily living as needed
- encouraging smoking cessation and adherence to treatment regimen
- providing emotional support and coping strategies
- educating them about their disease process, management options, self-care skills,
- and when to seek medical attention.
- Patient education for COPD should include the following topics:
- The nature and causes of COPD and how it affects the lungs and other organs
- The signs and symptoms of COPD and how to monitor them
- The goals and components of treatment and how to use medications and devices correctly
- The importance of smoking cessation and how to access resources and support for quitting
- The benefits of pulmonary rehabilitation and exercise training and how to participate in them
- The role of nutrition and hydration in maintaining health and preventing complications
- The prevention and management of exacerbations and how to recognize and report them
- The indications and benefits of oxygen therapy and how to use it safely and effectively
- The breathing techniques and energy conservation strategies that can reduce dyspnea and fatigue
- The psychosocial impact of COPD and how to cope with stress, anxiety, depression, and social isolation
- The available resources and support groups for patients with COPD and their caregivers
Summary
- COPD is a chronic respiratory disease that causes airflow limitation, dyspnea, cough, sputum production, and exacerbations.
- COPD is diagnosed by spirometry and classified by the severity of airflow obstruction according to the GOLD criteria.
- COPD is managed by smoking cessation, pharmacotherapy, non-pharmacological interventions, and management of exacerbations.
- Nursing care for COPD involves assessing, monitoring, administering, providing, promoting, encouraging, supporting, and educating patients with COPD.
Conclusion
- COPD is a common, preventable, and treatable disease that affects millions of people worldwide.
- COPD can have a significant impact on the physical, psychological, social, and economic aspects of patients' lives.
- Nurses play a vital role in providing holistic care for patients with COPD and empowering them to manage their condition effectively.
- COPD is a preventable and treatable disease, but it requires a comprehensive, patient-centered approach that addresses not only the physical but also the psychological and social aspects of the condition.
- It is essential for individuals at risk, healthcare providers, and policymakers to work together to reduce risk factors, raise awareness, and improve access to care for those affected by COPD.
- Innovations in research and treatment options continue to provide hope for better outcomes and a brighter future for individuals living with COPD.
- Education, early intervention, and ongoing support are key elements in the battle against this chronic lung disease, ultimately aiming to enhance the lives of those impacted by COPD and reduce its global burden.
Pulmonary Embolism
Introduction
- Pulmonary embolism (PE) is a serious and potentially life-threatening condition that occurs when a blood clot (thrombus) blocks one or more arteries in the lungs.
- The clot usually originates from the deep veins of the legs or pelvis, a condition known as deep vein thrombosis (DVT).
- PE can impair gas exchange, increase pulmonary vascular resistance, and cause right ventricular failure, shock, and death.
- PE requires prompt diagnosis and treatment to prevent complications and improve outcomes.
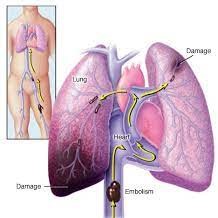
Pathophysiology
- When a thrombus breaks off from the deep veins and travels to the lungs, it obstructs the blood flow to the affected lung segments.
- This causes ventilation-perfusion mismatch, meaning that some areas of the lungs receive air but not blood, while others receive blood but not air.
- This results in hypoxemia (low oxygen level in the blood) and hypercapnia (high carbon dioxide level in the blood).
- The obstruction also triggers the release of vasoconstrictors, such as serotonin and thromboxane, that cause the pulmonary arteries to constrict.
- This increases the pulmonary artery pressure and the workload of the right ventricle, which pumps blood to the lungs.
- If the right ventricle cannot overcome the increased resistance, it may fail and reduce the cardiac output, leading to hypotension (low blood pressure), shock, and organ damage.
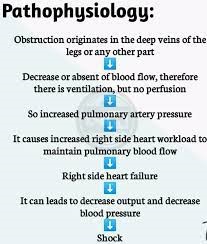
Etiology and risk factors
- The most common cause of PE is DVT, which can be triggered by various factors that affect blood coagulation, such as:
- Immobility or prolonged bed rest
- Surgery or trauma
- Cancer or chemotherapy
- Pregnancy or oral contraceptives
- Smoking or obesity
- Genetic or acquired clotting disorders
- Other less common causes of PE include:
- Fat emboli from bone fractures or liposuction
- Air emboli from intravenous injections or diving accidents
- Amniotic fluid emboli from childbirth complications
- Septic emboli from bacterial infections
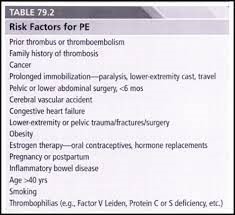
Clinical manifestations and symptoms
- The signs and symptoms of PE depend on:
- the size and location of the clot
- the extent of lung involvement
- the presence of underlying heart or lung disease
- Some common manifestations include:
- Dyspnea (difficulty breathing) or tachypnea (rapid breathing)
- Chest pain that is sharp, pleuritic (worsens with breathing), or anginal (similar to a heart attack)
- Cough or hemoptysis (coughing up blood)
- Tachycardia (rapid heart rate) or palpitations
- Syncope (fainting) or dizziness
- Anxiety or restlessness
- Cyanosis (bluish skin color) or diaphoresis (sweating)
- Fever or hypothermia
Diagnostic Evaluation
- The diagnosis of PE is based on clinical suspicion, risk assessment, and imaging tests.
- Some common diagnostic tools include:
- D-dimer test: a blood test that measures a protein fragment that is released when a clot dissolve. A high level of D-dimer suggests the presence of a clot, but it is not specific for PE.
- Chest X-ray: a radiographic image that shows the lungs and the heart. It can rule out other causes of chest pain or dyspnea, such as pneumonia or pneumothorax, but it cannot confirm PE.
- Electrocardiogram (ECG): a recording of the electrical activity of the heart. It can detect signs of right ventricular strain or ischemia, such as sinus tachycardia, right axis deviation, or S1Q3T3 pattern, but it is not specific for PE.
- Echocardiogram: an ultrasound image that shows the structure and function of the heart. It can measure the pulmonary artery pressure and evaluate the right ventricular function. It can also detect signs of right ventricular dilation or dysfunction, such as McConnell's sign (hypokinesis of the right ventricular free wall with preserved apical contraction), but it is not specific for PE.
- Computed tomography pulmonary angiography (CTPA): a scan that uses contrast dye and X-rays to visualize the pulmonary arteries. It is considered the gold standard for diagnosing PE, as it can directly identify the location and size of the clot.
- Ventilation-perfusion scan (V/Q scan): a scan that uses radioactive tracers to measure the airflow and blood flow in the lungs. It can detect areas of mismatch between ventilation and perfusion, indicating possible PE. However, it is less sensitive and specific than CTPA, and it can be affected by other lung conditions.
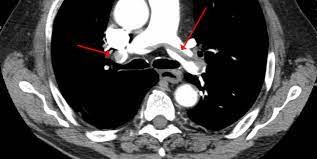
Management and Treatment
- The main goals of treatment for PE are to prevent further clot formation, dissolve the existing clot, and prevent complications.
- The treatment options depend on the severity and stability of the patient, and may include:
- Anticoagulation: the use of drugs that inhibit the clotting cascade and prevent the growth or recurrence of clots. Examples include heparin, low molecular weight heparin (LMWH), fondaparinux, or direct oral anticoagulants (DOACs). Anticoagulation is usually started as soon as PE is suspected and continued for at least 3 months or longer depending on the risk factors and bleeding risk of the patient.
- Thrombolysis: the use of drugs that break down the clot and restore blood flow. Examples include alteplase, reteplase, or tenecteplase. Thrombolysis is reserved for patients with massive or submassive PE who have hemodynamic instability or right ventricular dysfunction, as it carries a high risk of bleeding complications.
- Mechanical thrombectomy: the use of devices that remove the clot from the pulmonary artery. Examples include catheter-directed thrombolysis, suction embolectomy, or rotational thrombectomy. Mechanical thrombectomy is an alternative or adjunct to thrombolysis for patients with massive or submassive PE who have contraindications or failed response to thrombolysis, or who have access to specialized centers.
- Inferior vena cava (IVC) filter: the placement of a device that traps clots from the lower extremities and prevents them from reaching the lungs. IVC filters are indicated for patients with contraindications or complications from anticoagulation, recurrent PE despite adequate anticoagulation, or large free-floating clots in the iliac or femoral veins.
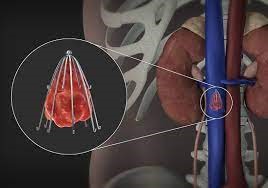
Nursing care and patient education
- Nurses play a vital role in the care and education of patients with PE.
- Some of the nursing interventions and responsibilities include:
- Monitoring vital signs, oxygen saturation, cardiac rhythm, urine output, and mental status
- Administering oxygen therapy, medications, fluids, and blood products as ordered
- Assessing for signs of bleeding, such as hematuria, hematemesis, melena, epistaxis, ecchymosis, or petechiae
- Evaluating the effectiveness and side effects of treatment, such as improvement in symptoms, resolution of clot, or occurrence of hemorrhage
- Providing comfort measures, such as pain relief, positioning, relaxation techniques, and emotional support
- Educating patients about the signs and symptoms of PE and DVT, the importance of medication adherence and follow-up, the prevention of clot formation (such as avoiding prolonged immobility, wearing compression stockings, staying hydrated), and the management of risk factors (such as smoking cessation, weight control, exercise)

Summary
- PE is a serious condition that can cause significant morbidity and mortality.
- It is caused by a blood clot that blocks one or more arteries in the lungs.
- It can impair gas exchange, increase pulmonary vascular resistance, and cause right ventricular failure.
- It requires prompt diagnosis and treatment to prevent complications and improve outcomes.
- The diagnosis is based on clinical suspicion, risk assessment, and imaging tests.
- The treatment options depend on the severity and stability of the patient, and may include anticoagulation, thrombolysis, mechanical thrombectomy, or IVC filter.
- Nurses play a vital role in the care and education of patients with PE.
Conclusion
- PE is a complex and time-sensitive condition that requires a multidisciplinary approach to provide effective care for patients.
- PE can manifest with a range of symptoms, from mild breathlessness and chest pain to severe respiratory distress and hemodynamic instability.
- Timely diagnosis is crucial, and it relies on a combination of clinical assessment, imaging studies, and laboratory tests.
- Treatment options include anticoagulation therapy to prevent further clot formation and measures to stabilize the patient's condition, such as oxygen supplementation or, in severe cases, thrombolytic therapy or surgical intervention.
- Nurses should be familiar with the pathophysiology, etiology, clinical manifestations, diagnostic evaluation, management options, nursing interventions, and patient education for PE.
- Preventing PE is a key aspect of managing this condition, and strategies involve addressing risk factors, such as immobility, surgery, prolonged travel, and certain medical conditions, which can predispose individuals to clot formation.
- Prophylactic measures, including the use of anticoagulants, compression stockings, and early ambulation after surgery, play a vital role in reducing the risk of PE.
- Advances in medical research and healthcare practices continue to refine our understanding and management of this condition, offering hope for improved outcomes and quality of life for those affected by pulmonary embolism.
Cystic Fibrosis
Introduction
- Cystic Fibrosis (CF) is a genetic disorder that affects the exocrine glands, which produce mucus, sweat, and digestive enzymes.
- CF causes these secretions to become thick and sticky, leading to blockage of the airways, lungs, pancreas, liver, and other organs.
- CF can cause chronic respiratory infections, malnutrition, diabetes, infertility, and other complications.
- CF is inherited in an autosomal recessive pattern, meaning that both parents must carry a mutated copy of the CFTR gene for their child to have the disease.
- There is no cure for CF, but treatments can help manage the symptoms and improve the quality of life of people with CF.
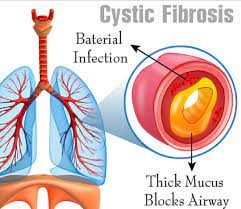
Pathophysiology
- The pathophysiology of CF is related to the defective function of the cystic fibrosis transmembrane conductance regulator (CFTR) protein, which is encoded by the CFTR gene.
- The CFTR protein is a chloride channel that regulates the movement of chloride ions and water across the cell membrane of epithelial cells.
- In people with CF, the CFTR protein is either absent or dysfunctional, resulting in reduced or abnormal chloride transport and water balance in the affected tissues.
- This leads to dehydration and increased viscosity of the mucus, sweat, and digestive secretions.
- The consequences of this defect vary depending on the organ system involved:
- Respiratory system: The thick and sticky mucus in the airways obstructs the normal airflow and traps bacteria, causing chronic inflammation, infection, and damage to the lung tissue. The mucus also impairs the function of the cilia, which are hair-like structures that help clear the airways of foreign particles and microorganisms. The accumulation of mucus and bacteria in the lungs leads to recurrent episodes of pneumonia, bronchitis, bronchiectasis (abnormal dilation of the bronchi), hemoptysis (coughing up blood), atelectasis (collapse of lung segments), and respiratory failure.
- Gastrointestinal system: The thick and sticky mucus in the pancreas blocks the ducts that carry digestive enzymes to the small intestine. This results in pancreatic insufficiency, which means that the body cannot digest and absorb fats especially the fat-soluble vitamins (A, D, E, K), proteins, and some vitamins properly. This leads to malabsorption, malnutrition, weight loss, steatorrhea (fatty stools), abdominal pain, bloating, gas, and constipation. The mucus can also cause inflammation and scarring of the pancreas, leading to pancreatitis (inflammation of the pancreas) or diabetes mellitus (high blood sugar levels). The thick and sticky mucus in the liver can obstruct the bile ducts that carry bile to the small intestine. This can cause liver damage, cirrhosis (scarring of the liver), portal hypertension (high blood pressure in the portal vein), varices (enlarged veins in the esophagus or stomach), and bleeding. The thick and sticky mucus in the intestines can cause intestinal obstruction, especially in newborns with meconium ileus (blockage of the intestine by meconium, which is the first stool of a baby). This can cause bowel perforation (tearing of the bowel wall), peritonitis (inflammation of the lining of the abdomen), or death.
- Reproductive system: The thick and sticky mucus in the reproductive organs can cause infertility or reduced fertility in both males and females with CF. In males with CF, the vas deferens (the tube that carries sperm from the testes to the penis) is either absent or blocked by mucus. This prevents sperm from reaching the ejaculatory duct and, consequently, from being present in the ejaculate. Therefore, males with CF often have a condition called congenital bilateral absence of the vas deferens (CBAVD). This condition does not affect the production of sperm in the testes, but it does affect their ability to father children naturally. However, with the help of assisted reproductive techniques such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI), some men with CF can still father children. In females with CF, the thickened mucus can affect the cervical mucus, making it more viscous and difficult for sperm to swim through. This can hinder natural conception. Additionally, the overall impact of CF on a woman's reproductive health can vary, with some women experiencing reduced fertility, while others may have a relatively normal reproductive function.
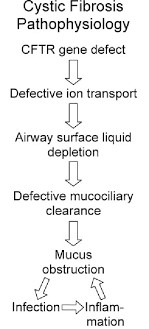
Etiology and risk factors
- The etiology of CF is genetic, involving mutations in the CFTR gene located on chromosome 7.
- There are more than 2,000 different mutations that can cause CF, but the most common one is called delta F508, which accounts for about 70% of cases.
- The risk factors for inheriting CF are having parents who are carriers of the mutated gene or having a family history of CF.
- The incidence of CF varies by ethnicity and geographic region.
- The highest incidence is among Caucasians of Northern European descent (about 1 in 2,500 births), followed by Hispanics (about 1 in 8,000 births), African Americans (about 1 in 15,000 births), and Asians (about 1 in 31,000 births).
Clinical manifestations and symptoms
- The clinical manifestations and symptoms of CF depend on the severity of the disease and the organs involved.
- The most common signs and symptoms include:
- Respiratory: persistent cough with thick sputum production, wheezes, crackles, dyspnea, chest pain, recurrent respiratory infections (especially with Pseudomonas aeruginosa), bronchiectasis (dilation and destruction of bronchial walls), hemoptysis (coughing up blood), nasal polyps (growths in the nose), sinusitis (inflammation of the sinuses), hypoxia (low oxygen levels in the blood), cyanosis (bluish discoloration of the skin and mucous membranes), clubbing (enlargement of the fingertips), pulmonary hypertension (high blood pressure in the lungs), cor pulmonale (right-sided heart failure due to lung disease), respiratory failure.
- Gastrointestinal: steatorrhea (foul-smelling stools with high fat content), abdominal pain, bloating, flatulence, constipation or diarrhea, weight loss or failure to thrive (poor growth), anorexia (loss of appetite), vitamin deficiencies (especially A, D, E, K), anemia (low red blood cell count), hypoproteinemia (low protein levels in the blood), edema (swelling due to fluid retention), osteoporosis (bone loss), osteopenia (low bone density), meconium ileus (blockage of the intestines by thick meconium in newborns), distal intestinal obstruction syndrome (DIOS) or meconium ileus equivalent (partial or complete blockage of the intestines by thick stool in older children and adults), rectal prolapse (protrusion of the rectum through the anus), intussusception (telescoping of one part of the intestine into another), volvulus (twisting of the intestine), appendicitis (inflammation of the appendix).
- Pancreatic: pancreatic insufficiency (inability to produce enough digestive enzymes), pancreatic enzyme replacement therapy (PERT) with oral capsules containing lipase, protease, and amylase enzymes to aid digestion and absorption of nutrients, diabetes mellitus (high blood sugar levels due to insufficient insulin production or resistance), pancreatic fibrosis (scarring of the pancreas), pancreatitis (inflammation of the pancreas), pancreatic pseudocysts (fluidfilled sacs in the pancreas), pancreatic cancer.
- Hepatobiliary: liver disease (cirrhosis, portal hypertension, varices, ascites, hepatic encephalopathy, liver failure), gallstones (cholelithiasis), cholecystitis (inflammation of the gallbladder), cholangitis (inflammation of the bile ducts), biliary cirrhosis (scarring of the bile ducts).
- Reproductive: infertility (inability to conceive or father a child) due to absence or obstruction of the vas deferens in males or thick cervical mucus in females, decreased libido (sexual desire), erectile dysfunction (impotence) in males, menstrual irregularities, amenorrhea (absence of periods), or dysmenorrhea (painful periods) in females, pregnancy complications (preterm labor, low birth weight, gestational diabetes, preeclampsia, fetal distress, stillbirth).
- Sweat glands: salty tasting skin or sweat due to high sodium and chloride levels in the sweat, dehydration, electrolyte imbalance, heat exhaustion, heat stroke.
Diagnostic Evaluation
- The diagnostic evaluation of CF includes:
- Newborn screening: a blood test that measures the level of immunoreactive trypsinogen (IRT), a pancreatic enzyme that is elevated in most infants with CF. A positive result is followed by a confirmatory test for CFTR gene mutations or a sweat test.
- Sweat test: a test that measures the amount of chloride in the sweat. A high level (>60 mmol/L) is diagnostic of CF. The test is performed by applying a chemical that stimulates sweating on the arm or leg and collecting the sweat on a filter paper or pad. The test is repeated on a different day or site to confirm the result.
- Genetic testing: a test that identifies the specific mutations in the CFTR gene. The test can be done on blood, saliva, or tissue samples. The test can be used for prenatal diagnosis, carrier screening, or confirmation of CF diagnosis.
- Pulmonary function tests (PFTs): tests that measure the lung capacity, volume, flow rate, and gas exchange. The tests include spirometry (measuring how much and how fast air can be exhaled), lung volumes (measuring how much air remains in the lungs after exhaling), diffusion capacity (measuring how well oxygen passes from the lungs to the blood), and arterial blood gas analysis (measuring the oxygen and carbon dioxide levels in the blood). The tests show reduced lung function and impaired gas exchange in CF patients.
- Chest x-ray: an imaging test that shows the condition of the lungs and chest cavity. The test may reveal hyperinflation (overexpansion) of the lungs, atelectasis (collapse) of lung segments or lobes, bronchial wall thickening, mucus plugging, consolidation (solidification) of lung tissue due to infection or inflammation, bronchiectasis, pulmonary fibrosis, pneumothorax (air in the pleural space), pleural effusion (fluid in the pleural space), pulmonary hypertension, or cor pulmonale.
- Sputum culture and sensitivity: a laboratory test that identifies the type and antibiotic susceptibility of bacteria present in the sputum. The test helps guide antibiotic therapy for pulmonary infections. The most common bacteria isolated from CF patients are Staphylococcus aureus, Haemophilus influenzae, Pseudomonas aeruginosa, Burkholderia cepacia complex, Stenotrophomonas maltophilia, Achromobacter xylosoxidans, and nontuberculous mycobacteria.
- Fecal fat analysis: a laboratory test that measures the amount of fat in the stool. A high level (>7 g/day) indicates malabsorption due to pancreatic insufficiency. The test requires collecting stool samples for 72 hours and following a diet containing 100 g of fat per day.
- Fecal elastase: a laboratory test that measures the level of elastase, a pancreatic enzyme that digests proteins, in the stool. A low level (<200 μg/g) indicates pancreatic insufficiency. The test requires collecting one stool sample and does not require any dietary modification.
- Vitamin levels: blood tests that measure the levels of fat-soluble vitamins (A, D, E, K) and other vitamins (B12, C, folate) in CF patients. Low levels indicate malabsorption due to pancreatic insufficiency or dietary deficiency. The tests help guide vitamin supplementation therapy.
- Glucose tolerance test: a blood test that measures the glucose level before and after ingesting a glucose solution. The test diagnoses diabetes mellitus if the glucose level is higher than normal at 2 hours after ingestion (>200 mg/dL). The test requires fasting for 8 hours before ingestion and avoiding caffeine.
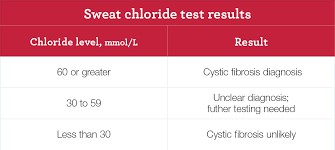
Management and Treatment
- The management and treatment of cystic fibrosis (CF) aim to prevent and control pulmonary infections, promote clearance of mucus, manage gastrointestinal problems, and provide nutritional and psychosocial support.
- The treatment plan is individualized according to the patient's needs and preferences, and may include the following:
- Antibiotics: These are used to treat acute and chronic bacterial infections in the lungs, such as Pseudomonas aeruginosa, Staphylococcus aureus, and Burkholderia cepacia. Antibiotics may be given orally, intravenously, or by inhalation. Some examples are azithromycin, ciprofloxacin, tobramycin, and ceftazidime.
- Bronchodilators: These are used to relax the smooth muscles of the airways and improve airflow. They may be given by inhalation or orally. Some examples are albuterol, salmeterol, and theophylline.
- Mucolytics: These are used to thin the thick and sticky mucus in the lungs and facilitate its removal. They may be given by inhalation or orally. Some examples are dornase alfa, hypertonic saline, and N-acetylcysteine.
- Chest physiotherapy: This is a technique that involves manual or mechanical percussion, vibration, postural drainage, and breathing exercises to loosen and mobilize the mucus in the lungs. It is usually done twice a day or more, depending on the patient's condition.
- Airway clearance devices: These are devices that help the patient clear the mucus from the lungs by creating positive or negative pressure, oscillating airflow, or high-frequency chest wall oscillation. Some examples are flutter valve, acapella device, vest therapy, and intrapulmonary percussive ventilation.
- Oxygen therapy: This is used to supplement oxygen in patients with hypoxemia (low blood oxygen level). It may be given by nasal cannula, face mask, or transtracheal catheter. The oxygen flow rate and duration are adjusted according to the patient's needs and tolerance.
- Lung transplantation: This is a surgical procedure that involves replacing one or both diseased lungs with healthy donor lungs. It is considered as a last resort for patients with end-stage lung disease who have failed other treatments. It has many risks and complications, such as rejection, infection, bleeding, and organ failure.
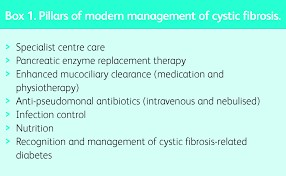
Nursing care and patient education
- The nursing care of patients with CF focuses on providing holistic care that addresses the physical, emotional, social, and spiritual needs of the patient and the family.
- The nursing care plan may include the following:
- Assessing the patient's respiratory status, including breath sounds, respiratory rate, oxygen saturation, sputum production, cough, dyspnea, chest pain, and signs of infection or exacerbation.
- Administering medications as prescribed and monitoring their effects and side effects.
- Assisting with chest physiotherapy and airway clearance devices as ordered and teaching the patient and the family how to perform them correctly and safely at home.
- Providing oxygen therapy as ordered and monitoring its effects and complications.
- Encouraging fluid intake to hydrate the mucus membranes and thin the secretions.
- Providing a high-calorie, high-protein diet that is supplemented with vitamins A, D, E, K, and pancreatic enzymes to prevent malnutrition and malabsorption.
- Monitoring the patient's weight, height, body mass index (BMI), and growth charts regularly.
- Assessing the patient's gastrointestinal status, including bowel sounds, abdominal pain, distension, nausea, vomiting, diarrhea, constipation, and signs of intestinal obstruction or perforation.
- Administering laxatives, stool softeners, or enemas as needed to prevent or relieve constipation.
- Assessing the patient's skin integrity, especially in areas prone to pressure ulcers, such as sacrum, heels, and elbows.
- Applying moisturizers, barrier creams, or dressings as needed to prevent or treat skin breakdown.
- Assessing the patient's psychosocial status, including mood, coping skills, self-esteem, body image, social support, and quality of life.
- Providing emotional support and counseling to the patient and the family and referring them to appropriate resources such as support groups, social workers, psychologists, or chaplains as needed.
- Educating the patient and the family about CF and its management and treatment options.
- Teaching them how to recognize and report signs and symptoms of complications or worsening condition such as fever, increased sputum production, change in sputum color or consistency, hemoptysis, increased dyspnea, chest pain, cyanosis, clubbing, weight loss, anorexia, jaundice, ascites, edema, or bleeding.
- Teaching them how to prevent and control infections by practicing good hand hygiene, avoiding contact with sick people, getting vaccinated, and taking prophylactic antibiotics as prescribed.
- Teaching them how to adhere to the medication regimen and the importance of taking the medications as prescribed and not skipping or altering doses without consulting the health care provider.
- Teaching them how to use and care for the inhalers, nebulizers, airway clearance devices, oxygen equipment, and other devices as prescribed.
- Teaching them how to monitor and record their vital signs, oxygen saturation, peak expiratory flow rate (PEFR), sputum characteristics, weight, and dietary intake at home.
- Teaching them how to plan and modify their daily activities according to their energy level and tolerance and how to balance rest and exercise.
- Teaching them how to cope with stress and anxiety by using relaxation techniques, distraction methods, positive thinking, or humor.
- Teaching them how to maintain a positive outlook and a hopeful attitude toward the future.
Summary
- Cystic fibrosis (CF) is a genetic disorder that affects the exocrine glands and causes thick and sticky mucus to build up in the lungs, pancreas, and other organs.
- It leads to chronic lung infections, respiratory failure, malnutrition, diabetes, liver disease, and infertility.
- The management and treatment of CF aim to prevent and control pulmonary infections, promote clearance of mucus, manage gastrointestinal problems, and provide nutritional and psychosocial support.
- The nursing care of patients with CF focuses on providing holistic care that addresses the physical, emotional, social, and spiritual needs of the patient and the family.
- The nursing care plan may include:
- assessing the patient's respiratory and gastrointestinal status
- administering medications and oxygen therapy
- assisting with chest physiotherapy and airway clearance devices
- providing a high-calorie, high-protein diet
- monitoring the patient's weight and growth
- providing emotional support and counseling
- educating the patient and the family about CF and its management and treatment options
- teaching them how to prevent and control infections
- adhere to the medication regimen
- use and care for the devices
- monitor and record their condition at home
- plan and modify their daily activities
- cope with stress and anxiety
- maintain a positive outlook and a hopeful attitude toward the future
Conclusion
- Cystic fibrosis (CF) is a challenging and complex disease that requires lifelong care and management.
- Nurses play a vital role in providing effective care for patients with CF by applying evidence-based practice, collaborating with other health care professionals, advocating for the patient's rights and preferences, and empowering the patient and the family to participate in decision making and self-care.
- Nurses can also contribute to research and education on CF by staying updated on the latest developments, sharing their knowledge and experience with others, and participating in clinical trials and studies.
- By doing so, nurses can help improve the quality of life and outcomes for patients with CF and their families.
Pulmonary Edema
Introduction
- Pulmonary edema is a condition in which excess fluid accumulates in the lungs, impairing gas exchange and causing respiratory distress.
- It can be a life-threatening emergency that requires prompt diagnosis and treatment.
- Pulmonary edema can be classified as cardiogenic or non-cardiogenic, depending on the underlying cause of the fluid accumulation.
- Cardiogenic pulmonary edema is caused by increased pressure in the left side of the heart, which forces fluid into the pulmonary capillaries.
- Non-cardiogenic pulmonary edema is caused by injury or inflammation of the lung tissue, which increases the permeability of the alveolar-capillary membrane and allows fluid to leak into the alveoli.
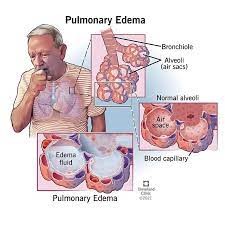
Pathophysiology
- The pathophysiology of pulmonary edema involves a disruption of the Starling forces that regulate the movement of fluid across the alveolar-capillary membrane.
- Normally, the hydrostatic pressure in the capillaries is balanced by the oncotic pressure in the plasma, which prevents fluid from leaving the vascular space.
- However, when the hydrostatic pressure exceeds the oncotic pressure, fluid shifts from the capillaries to the interstitial space and then to the alveoli, resulting in pulmonary edema.
- can occur due to increased capillary pressure (as in cardiogenic pulmonary edema) or decreased plasma oncotic pressure (as in hypoalbuminemia or nephrotic syndrome).
- Alternatively, when the alveolar-capillary membrane is damaged or inflamed, it becomes more permeable to fluid and proteins, which also causes fluid to move into the alveoli (as in non-cardiogenic pulmonary edema).
- This can occur due to various lung injuries or infections (such as acute respiratory distress syndrome, pneumonia, aspiration, inhalation of toxic substances, etc.).
Etiology and risk factors
- The etiology and risk factors of pulmonary edema depend on whether it is cardiogenic or non-cardiogenic.
- Cardiogenic pulmonary edema is most commonly caused by left ventricular failure, which can result from:
- myocardial infarction
- ischemic heart disease
- valvular heart disease
- hypertensive crisis
- arrhythmias
- cardiomyopathies
- Other causes include: mitral stenosis, aortic stenosis, pulmonary embolism, or fluid overload.
- Risk factors for cardiogenic pulmonary edema include:
- Age
- Hypertension
- diabetes mellitus
- smoking
- obesity
- dyslipidemia
- family history of cardiovascular disease
- Non-cardiogenic pulmonary edema can be caused by various lung injuries or infections that damage or inflame the alveolar-capillary membrane.
- These include:
- acute respiratory distress syndrome (ARDS)
- pneumonia aspiration of gastric contents or foreign bodies inhalation of toxic substances (such as smoke chlorine gas ammonia etc.)
- high altitude pulmonary edema (HAPE)
- neurogenic pulmonary edema (due to increased intracranial pressure)
- re-expansion pulmonary edema (after rapid removal of pleural effusion or pneumothorax) transfusion-related acute lung injury (TRALI)
- drug-induced lung injury (such as heroin overdose)
- Risk factors for non-cardiogenic pulmonary edema include:
- sepsis
- trauma
- surgery
- burns
- pancreatitis
- anaphylaxis
- blood transfusion
- mechanical ventilation with high positive end-expiratory pressure (PEEP)
- exposure to high altitude or toxic substances
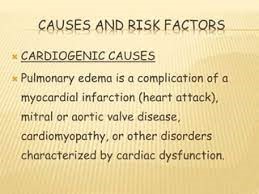
Clinical manifestations and symptoms
- The clinical manifestations and symptoms of pulmonary edema vary depending on the severity and acuity of the condition.
- The main symptom is dyspnea (shortness of breath), which may be accompanied by:
- orthopnea (difficulty breathing when lying down)
- paroxysmal nocturnal dyspnea (sudden awakening from sleep with breathlessness)
- cough (which may produce frothy pink sputum)
- Other symptoms include:
- chest pain or discomfort (especially if cardiac ischemia is present)
- palpitations or irregular heartbeat (due to arrhythmias)
- anxiety or restlessness (due to hypoxia)
- fatigue or weakness (due to reduced cardiac output)
- confusion or altered mental status (due to cerebral hypoperfusion)
- The physical examination may reveal signs of respiratory distress such as:
- tachypnea (rapid breathing)
- cyanosis (bluish discoloration of skin and mucous membranes)
- use of accessory muscles of respiration, intercostal retractions, or nasal flaring
- Auscultation of the lungs may reveal crackles (rales) or wheezes due to fluid accumulation in the airways.
- Auscultation of the heart may reveal gallop rhythms (S3 or S4 sounds) due to ventricular dysfunction, murmurs due to valvular abnormalities, or pericardial friction rub due to pericarditis.
- Jugular venous distension may indicate increased right atrial pressure due to right ventricular failure or pulmonary hypertension.
- Peripheral edema may indicate systemic venous congestion due to left ventricular failure or fluid overload.
- Hepatomegaly or splenomegaly may indicate hepatic or splenic congestion due to portal hypertension.
- Ascites may indicate abdominal fluid accumulation due to low albumin levels or portal hypertension.
Diagnostic Evaluation
- The diagnostic evaluation of pulmonary edema aims to identify the underlying cause, assess the severity and extent of the condition, and guide the management and treatment.
- The initial tests include:
- Chest X-ray can show signs of pulmonary congestion such as increased vascular markings, interstitial or alveolar infiltrates, Kerley B lines, or pleural effusions.
- ECG can show signs of cardiac ischemia such as ST-segment elevation or depression, T-wave inversion, or Q waves. It can also show signs of ventricular hypertrophy, arrhythmias, or conduction abnormalities.
- ABG analysis can show signs of hypoxemia (low oxygen level in the blood), hypercapnia (high carbon dioxide level in the blood), or acidosis (low pH in the blood).
- CBC can show signs of infection such as leukocytosis (high white blood cell count) or anemia (low red blood cell count or hemoglobin level).
- Serum electrolytes can show signs of fluid imbalance such as hyponatremia (low sodium level), hyperkalemia (high potassium level), or hypocalcemia (low calcium level). BUN and creatinine can show signs of renal impairment due to reduced renal perfusion or acute kidney injury.
- Liver function tests can show signs of hepatic impairment due to reduced hepatic perfusion or hepatic congestion.
- Cardiac biomarkers can show signs of myocardial injury or stress due to cardiac ischemia or ventricular dysfunction.
- Other tests that may be performed include:
- Echocardiography can assess the structure and function of the heart, such as the size and shape of the chambers and valves, the ejection fraction and cardiac output, the presence and severity of valvular regurgitation or stenosis, the presence and extent of wall motion abnormalities, the presence and degree of pulmonary hypertension, and the presence and size of pericardial effusion.
- Pulmonary artery catheterization can measure the hemodynamic parameters such as the pulmonary artery pressure, pulmonary capillary wedge pressure, cardiac output, systemic vascular resistance, and pulmonary vascular resistance. It can also help differentiate between cardiogenic and non-cardiogenic pulmonary edema by comparing the pulmonary capillary wedge pressure (which reflects the left atrial pressure) and the pulmonary artery occlusion pressure (which reflects the alveolar pressure). If the pulmonary capillary wedge pressure is higher than the pulmonary artery occlusion pressure, it indicates cardiogenic pulmonary edema. If they are equal or reversed, it indicates non-cardiogenic pulmonary edema.
- CT scan can provide detailed images of the lungs and chest cavity, showing the distribution and extent of pulmonary edema, as well as other possible causes such as pulmonary embolism, pneumonia, lung cancer, or pneumothorax.
- MRI can provide similar information as CT scan but with better resolution and without radiation exposure. However, it is more expensive and time-consuming and may not be available in emergency situations.
- Bronchoscopy can allow direct visualization of the airways and sampling of bronchoalveolar lavage fluid for cytology, culture, or analysis. It can help diagnose infections such as pneumonia or tuberculosis, as well as other causes such as aspiration, inhalation injury, or lung cancer.
- Lung biopsy can obtain tissue samples from the lungs for histopathological examination. It can help diagnose inflammatory conditions such as ARDS, sarcoidosis, or interstitial lung disease, as well as neoplastic conditions such as lung cancer or lymphoma.
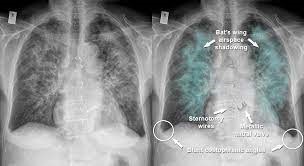
Management and Treatment
- The management and treatment of pulmonary edema depend on the underlying cause and the severity of the condition.
- The main goals are to improve oxygenation, reduce fluid overload, and treat the underlying cause.
- Some of the common interventions include:
- Oxygen therapy: To increase the oxygen saturation and relieve hypoxemia. Oxygen can be delivered by nasal cannula, face mask, or noninvasive ventilation (NIV) such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP). In severe cases, intubation and mechanical ventilation may be required.
- Diuretics: To reduce the fluid volume in the lungs and decrease the pressure in the pulmonary capillaries. Furosemide is the most commonly used diuretic for pulmonary edema. It also has a vasodilatory effect that reduces the preload and afterload of the heart.
- Vasodilators: To dilate the blood vessels and lower the blood pressure. This can reduce the workload of the heart and decrease the fluid leakage into the lungs. Nitroglycerin and nitroprusside are examples of vasodilators used for pulmonary edema.
- Morphine: To relieve dyspnea, anxiety, and pain. Morphine also has a vasodilatory effect that reduces the preload and afterload of the heart. However, morphine should be used with caution as it can cause respiratory depression, hypotension, and nausea.
- Inotropic agents: To increase the contractility and output of the heart. This can improve the perfusion of vital organs and reduce the congestion in the lungs. Dobutamine and milrinone are examples of inotropic agents used for pulmonary edema.
- Anticoagulants: To prevent or treat thromboembolism that may cause or worsen pulmonary edema. Heparin and warfarin are examples of anticoagulants used for pulmonary edema.
- Antibiotics: To treat infections that may cause or complicate pulmonary edema. The choice of antibiotics depends on the type and severity of the infection.
- Steroids: To reduce inflammation and edema in the lungs. Steroids are mainly used for noncardiogenic pulmonary edema caused by conditions such as ARDS, pneumonia, or inhalation injuries.
Nursing care and patient education
- The nursing care for patients with pulmonary edema involves monitoring, supporting, and educating them.
- Some of the nursing interventions include:
- Monitor vital signs, oxygen saturation, respiratory rate and pattern, breath sounds, chest X-ray, ECG, ABGs, electrolytes, BNP, urine output, weight, and edema.
- Administer oxygen therapy, medications, and fluids as ordered. Adjust the oxygen flow rate and medication doses according to the patient's condition and response.
- Position the patient in high Fowler's position or semi-Fowler's position to facilitate breathing and lung expansion.
- Assist with intubation and mechanical ventilation if indicated. Monitor the ventilator settings, airway pressure, tidal volume, and oxygenation. Suction the airway as needed to remove secretions.
- Provide comfort measures such as mouth care, skin care, pain relief, relaxation techniques, and emotional support.
- Educate the patient about the causes, signs and symptoms, treatment, and prevention of pulmonary edema. Teach them how to monitor their weight, fluid intake and output, blood pressure, and edema at home. Instruct them to take their medications as prescribed and to report any adverse effects or worsening symptoms to their health care provider.
- Encourage lifestyle modifications such as smoking cessation, salt restriction, fluid restriction, weight management, exercise, stress management, and adherence to follow-up appointments.
Summary
- Pulmonary edema is a condition characterized by fluid accumulation in the lungs that impairs gas exchange and causes hypoxemia.
- This condition can develop acutely or chronically and is often associated with underlying cardiovascular or respiratory disorders.
- The consequences of pulmonary edema can be life-threatening, as it severely impairs the ability of the lungs to oxygenate the blood and eliminate carbon dioxide.
- It can be classified into cardiogenic or noncardiogenic depending on the cause.
- The management and treatment of pulmonary edema aim to improve oxygenation, reduce fluid overload, and treat the underlying cause.
- The nursing care for patients with pulmonary edema involves monitoring, supporting, and educating them.
Conclusion
- Pulmonary edema is a serious condition that requires prompt diagnosis and intervention.
- Nurses play a vital role in providing holistic care for patients with pulmonary edema and helping them achieve optimal outcomes.
- Treatment approaches for pulmonary edema encompass a combination of interventions aimed at reducing fluid overload, improving cardiac function, and enhancing oxygenation.
- These may include oxygen therapy, diuretics, positive pressure ventilation (e.g., CPAP or mechanical ventilation), and medications to manage the underlying condition.
- Preventing and managing pulmonary edema require a multidisciplinary approach involving healthcare providers, including cardiologists, pulmonologists, and critical care specialists.
- Patient education, lifestyle modifications, and adherence to treatment plans are key components of long-term management, particularly in cases of chronic heart failure or lung disease.
Conclusion
- Pulmonary edema is a serious condition that requires prompt diagnosis and intervention.
- Nurses play a vital role in providing holistic care for patients with pulmonary edema and helping them achieve optimal outcomes.
- Treatment approaches for pulmonary edema encompass a combination of interventions aimed at reducing fluid overload, improving cardiac function, and enhancing oxygenation.
- These may include oxygen therapy, diuretics, positive pressure ventilation (e.g., CPAP or mechanical ventilation), and medications to manage the underlying condition.
- Preventing and managing pulmonary edema require a multidisciplinary approach involving healthcare providers, including cardiologists, pulmonologists, and critical care specialists.
- Patient education, lifestyle modifications, and adherence to treatment plans are key components of long-term management, particularly in cases of chronic heart failure or lung disease.
Lung Cancer
Introduction
- Lung cancer is a type of malignancy or carcinoma that develops in the lungs.
- It is usually characterized by the uncontrolled proliferation of lung tissues.
- Lung cancer is the second most common cancer and the leading cause of cancer death in both men and women in the United States.
- Lung cancer can be classified into two types:
- small cell lung cancer (SCLC)
- non-small cell lung cancer (NSCLC).
- The type of lung cancer determines the treatment options and prognosis.

Pathophysiology
- Lung cancer is a disease process that begins when an abnormal cell is transformed by the genetic mutation of the cellular DNA.
- The mutated cell then escapes the normal mechanisms of cellular control and regulation, and starts to grow and divide rapidly.
- The abnormal cells form a mass or tumor that invades the surrounding tissues and organs.
- Lung cancer can also spread to other parts of the body through the bloodstream or lymphatic system, a process called metastasis.
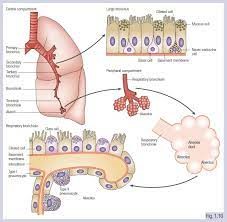
Etiology and risk factors
- The majority of lung cancers are caused by smoking or exposure to second-hand smoke.
- Smoking damages the lungs by introducing carcinogens that alter the DNA of the cells.
- The risk of lung cancer increases with the duration and intensity of smoking, and decreases with quitting smoking.
- Other risk factors for lung cancer include:
- Exposure to radon, a radioactive gas that can accumulate in homes and buildings
- Exposure to asbestos, a mineral fiber that can cause lung scarring and inflammation
- Exposure to other occupational or environmental carcinogens, such as arsenic, chromium, nickel, uranium, cadmium, etc.
- Family history or genetic predisposition to lung cancer
- Previous radiation therapy to the chest or other organs
- Underlying lung diseases, such as chronic obstructive pulmonary disease (COPD), tuberculosis, or pulmonary fibrosis
- Age, as lung cancer is more common in older adults
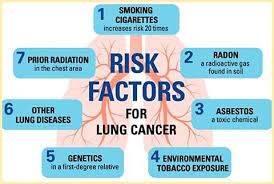
Classification of Lung Cancers
- Lung cancers are classified into two main types based on their histology or appearance under the microscope: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC).
- SCLC accounts for about 10-15% of all lung cancers. It is more common in heavy smokers and tends to grow and spread quickly. SCLC is also called oat cell carcinoma because of its small and round shape.
- NSCLC accounts for about 85-90% of all lung cancers. It is a broad term that encompasses several subtypes, such as adenocarcinoma, squamous cell carcinoma, large cell carcinoma, etc. NSCLC tends to grow and spread more slowly than SCLC.
Clinical manifestations and symptoms
- Lung cancer may not cause any symptoms in its early stages.
- As the tumor grows and invades the surrounding tissues, it may cause symptoms such as:
- Chronic cough that does not go away or worsens over time
- Hemoptysis or coughing up blood
- Dyspnea or difficulty breathing
- Wheezing or whistling sound when breathing
- Chest pain or discomfort that worsens with breathing or coughing
- Hoarseness or changes in voice
- Dysphagia or difficulty swallowing
- Weight loss or loss of appetite
- Fatigue or weakness
- Recurrent infections, such as bronchitis or pneumonia
- Lung cancer may also cause symptoms related to its metastasis to other organs, such as:
- Bone pain or fractures
- Headache, dizziness, seizures, or changes in mental status
- Jaundice or yellowing of the skin and eyes
- Lymphadenopathy or enlarged lymph nodes
- Horner syndrome, which is a combination of drooping eyelid, miosis (small pupil), anhidrosis (lack of sweating), and enophthalmos (sunken eye) on one side of the face
- Paraneoplastic syndrome, which is a group of symptoms caused by substances secreted by the tumor cells that affect other organs or systems
Diagnostic Evaluation
- The diagnosis of lung cancer is based on a combination of clinical history, physical examination, imaging tests, laboratory tests, and biopsy.
- Imaging tests are used to visualize the lungs and other organs for signs of tumor or metastasis. The most common imaging tests for lung cancer are:
- Chest X-ray: A simple and inexpensive test that can show abnormal masses, nodules, or infiltrates in the lungs.
- Computed tomography (CT) scan: A more detailed test that can show the size, shape, location, and extent of the tumor and its involvement with other structures.
- Magnetic resonance imaging (MRI) scan: A test that uses magnetic fields to create images of soft tissues and organs. It can be useful to detect brain metastases or spinal cord compression.
- Positron emission tomography (PET) scan: A test that uses a radioactive substance (tracer) that is injected into the bloodstream and accumulates in areas of high metabolic activity, such as cancer cells. It can help to identify the primary tumor and its spread to other organs.
- Bone scan: A test that uses a radioactive substance that is injected into the bloodstream and accumulates in areas of bone damage, such as fractures or metastases. It can help to detect bone involvement by lung cancer.
- Laboratory tests are used to measure the levels of certain substances in the blood or other body fluids that may indicate the presence or activity of lung cancer.
- The most common laboratory tests for lung cancer are:
- Complete blood count (CBC): A test that measures the number and quality of red blood cells, white blood cells, and platelets. It can show anemia, infection, or bleeding disorders that may be related to lung cancer.
- Blood chemistry: A test that measures the levels of electrolytes, glucose, liver enzymes, kidney function, and other substances in the blood. It can show organ dysfunction or metabolic abnormalities that may be related to lung cancer or its treatment.
- Tumor markers: A test that measures the levels of certain proteins or antigens that are produced by tumor cells or released into the bloodstream. They can help to diagnose, monitor, or predict the response to treatment of lung cancer. Some examples of tumor markers for lung cancer are carcinoembryonic antigen (CEA), neuron-specific enolase (NSE), cytokeratin 19 fragment (CYFRA 21-1), and squamous cell carcinoma antigen (SCC).
- Biopsy is the definitive test to confirm the diagnosis of lung cancer and to determine its type and grade. Biopsy involves taking a sample of tissue from the suspected tumor and examining it under a microscope. Biopsy can be done by different methods, such as:
- Bronchoscopy: A procedure that uses a flexible tube with a light and a camera (bronchoscope) that is inserted through the mouth or nose into the airways. It can allow the doctor to see inside the lungs and take samples of tissue or fluid using forceps, brushes, needles, or catheters.
- Transthoracic needle biopsy: A procedure that uses a long needle that is inserted through the chest wall into the lung tissue under the guidance of imaging tests. It can allow the doctor to obtain samples of tissue from peripheral lung lesions that are not accessible by bronchoscopy.
- Thoracentesis: A procedure that uses a needle that is inserted through the chest wall into the pleural space (the area between the lungs and the chest wall) to drain excess fluid (pleural effusion) that may accumulate due to lung cancer. The fluid can then be analyzed for the presence of cancer cells.
- Mediastinoscopy: A procedure that uses a small incision in the neck and a thin tube with a light and a camera (mediastinoscope) that is inserted into the mediastinum (the area between the lungs) to examine and take samples of lymph nodes or other structures that may be affected by lung cancer.
- Thoracotomy: A surgical procedure that uses a large incision in the chest wall to open up the chest cavity and allow direct access to the lungs and other organs. It can allow the doctor to remove part or all of a lung tumor, lymph nodes, or other tissues for biopsy or treatment.
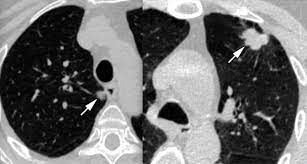
Management and Treatment
- The treatment of lung cancer depends on several factors, such as:
- The type and stage of lung cancer
- The location and size of the tumor
- The presence or absence of metastasis
- The patient's overall health and preferences
- The availability and effectiveness of different treatment options
- The main treatment options for lung cancer are:
- Surgery: The removal of part or all of a lung tumor along with some surrounding normal tissue and lymph nodes. Surgery can be done by different techniques, such as lobectomy (removal of a lobe of the lung), pneumonectomy (removal of an entire lung), segmentectomy (removal of a segment of a lobe), wedge resection (removal of a wedge-shaped piece of tissue), or sleeve resection (removal of a part of an airway along with some surrounding tissue). Surgery can be curative for early-stage NSCLC, but it is rarely used for SCLC due to its rapid spread.
- Radiation therapy: The use of high-energy rays or particles to kill cancer cells or shrink tumors. Radiation therapy can be delivered from outside the body (external beam radiation therapy) or from inside the body (brachytherapy). Radiation therapy can be used alone or in combination with other treatments, such as surgery, chemotherapy, or targeted therapy. Radiation therapy can be palliative for advanced-stage lung cancer or curative for limited-stage SCLC.
- Chemotherapy: Chemotherapy uses drugs that kill cancer cells or stop them from dividing. It can be used as a primary treatment for patients with advanced NSCLC or small cell lung cancer (SCLC), as an adjuvant treatment after surgery or radiation therapy to reduce the risk of recurrence, as a neoadjuvant treatment before surgery to shrink the tumor and make it easier to remove, or as a palliative treatment to improve quality of life and survival. Chemotherapy can be given intravenously or orally, and usually involves a combination of two or more drugs.
- Targeted therapy: Targeted therapy uses drugs that target specific molecules or pathways that are involved in the growth and survival of cancer cells. It can be used as a primary treatment for patients with advanced NSCLC who have certain genetic mutations or biomarkers that make them eligible for these drugs, such as EGFR, ALK, ROS1, BRAF, NTRK, MET, RET, or HER2. Targeted therapy can be given intravenously or orally, and usually involves one or more drugs that are specific for each mutation or biomarker.
- Immunotherapy: Immunotherapy uses drugs that stimulate the immune system to recognize and attack cancer cells. It can be used as a primary treatment for patients with advanced NSCLC who have high levels of PD-L1 expression on their tumor cells or who have MSI-H or dMMR status, which indicate a high level of genetic instability. Immunotherapy can also be used in combination with chemotherapy or targeted therapy for some patients. Immunotherapy can be given intravenously or subcutaneously, and usually involves one or more drugs that block the interaction between PD-1 and PD-L1 or CTLA-4.
- Palliative care: Palliative care is a specialized form of care that focuses on improving the quality of life and relieving the symptoms and stress of patients with serious illnesses such as lung cancer. Palliative care can be provided at any stage of the disease and along with any other treatments. Palliative care involves a multidisciplinary team of health professionals who address the physical, emotional, social, spiritual, and practical needs of the patient and their family. Palliative care may include pain management, symptom control, psychosocial support, advance care planning, hospice care, and bereavement care.
Nursing care and patient education
- The nursing care and patient education for lung cancer patients depend on the type, stage, and location of the tumor, as well as the treatments received and the symptoms experienced by the patient.
- The general goals of nursing care and patient education are to:
- Assess the patient's condition and monitor their vital signs, oxygen saturation, respiratory status, pain level, nutritional status, mental status, skin integrity, wound healing, and potential complications.
- Administer medications as prescribed and monitor their effects and side effects.
- Provide comfort measures such as positioning, massage, relaxation techniques, distraction techniques, music therapy, aromatherapy, etc.
- Educate the patient about their diagnosis, prognosis, treatment options, benefits and risks, expected outcomes, possible side effects, and follow-up care.
- Teach the patient how to manage their symptoms such as cough, dyspnea, hemoptysis, fatigue, anorexia, nausea, vomiting, diarrhea, constipation, mucositis, skin reactions, hair loss, infection, bleeding, etc.
- Teach the patient how to perform self-care activities such as oral hygiene, skin care, wound care, catheter care, ostomy care, etc.
- Teach the patient how to use assistive devices such as oxygen therapy, inhalers, nebulizers, suction machines, chest tubes, drains, etc.
- Teach the patient how to prevent complications such as infection, pneumonia, atelectasis, pulmonary embolism, deep vein thrombosis, superior vena cava syndrome, spinal cord compression, etc.
- Teach the patient how to cope with the emotional and psychological impact of lung cancer such as anxiety, depression, fear, anger, guilt, grief, loss of control, etc.
- Teach the patient how to access support resources such as support groups, counseling services, social workers, financial assistance, legal assistance, spiritual care, etc.
- Encourage the patient to quit smoking and avoid exposure to second-hand smoke and other environmental carcinogens.
- Encourage the patient to maintain a healthy lifestyle such as eating a balanced diet, drinking enough fluids, exercising regularly, getting enough rest and sleep, managing stress, etc.
- Encourage the patient to participate in shared decision making and express their preferences and values regarding their care.
- Encourage the patient to communicate with their health care team and family members and ask questions and voice concerns.
Summary
- Lung cancer is a type of malignancy or carcinoma that develops in the lungs.
- It is usually characterized by the uncontrolled proliferation of lung tissues.
- Lung cancer can be classified into two types: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC).
- Lung cancer can be staged according to the TNM system or the AJCC system.
- The main causes of lung cancer are smoking and exposure to radon and other carcinogens. The main risk factors for lung cancer are family history, smoking or exposure to second-hand smoke, previous radiation treatment, exposure to carcinogens (occupational or environmental), and underlying diseases such as tuberculosis.
- The main signs and symptoms of lung cancer are:
- chronic cough,
- hemoptysis,
- dysphagia,
- dyspnea,
- wheezing,
- generalized weakness and fatigue,
- weight loss,
- anorexia,
- recurrent respiratory infections (e.g., bronchitis, pneumonia),
- headaches,
- changes in mentation,
- changes in body temperature,
- The main modalities of treatment for lung cancer are surgery,
- radiation therapy,
- chemotherapy,
- targeted therapy,
- immunotherapy,
- palliative care
- The nursing care and patient education for lung cancer patients depend on the type, stage, and location of the tumor, as well as the treatments received and the symptoms experienced by the patient.
- The general goals of nursing care and patient education are to assess the patient's condition and monitor their vital signs and potential complications;
- administer medications as prescribed and monitor their effects and side effects;
- provide comfort measures;
- educate the patient about their diagnosis, prognosis, treatment options,
- expected outcomes,
- possible side effects,
- and follow-up care;
- teach the patient how to manage their symptoms;
- teach the patient how to perform self-care activities;
- teach the patient how to use assistive devices;
- teach the patient how to prevent complications;
- teach the patient how to cope with the emotional and psychological impact of lung cancer;
- teach the patient how to access support resources;
- encourage the patient to quit smoking and avoid exposure to second-hand smoke and other environmental carcinogens;
- encourage the patient to maintain a healthy lifestyle;
- encourage the patient to participate in shared decision making and express their preferences and values regarding their care; and encourage the patient to communicate with their health care team and family members.
Conclusion
- Lung cancer is a serious disease that affects millions of people worldwide.
- It is caused by various factors such as smoking and exposure to radon and other carcinogens.
- It can be classified into two types: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC).
- It can be staged according to the TNM system or the AJCC system.
- It can be treated with various modalities such as surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy, and palliative care.
- The nursing care and patient education for lung cancer patients are essential components of providing quality care and improving outcomes.
- Nurses play a vital role in assessing the patient's condition and monitoring their vital signs and potential complications; administering medications as prescribed and monitoring their effects and side effects; providing comfort measures; educating the patient about their diagnosis, prognosis, treatment options, expected outcomes.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Pathophysiology of the respiratory system
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


