Please set your exam date
Research And Evidence Based Practice In Nursing
Study Questions
Practice Exercise 1
Which of the following is the lowest level of “best evidence” for evidence-based practice?
Explanation
Evidence-based practice (EBP) uses a hierarchy of evidence to guide clinical decision-making. This hierarchy ranks sources of knowledge from the most reliable (such as systematic reviews of randomized controlled trials) to the least reliable.
Rationale for correct answer:
D. Trial and error: This is not considered valid evidence in evidence-based practice because it lacks systematic methodology, reproducibility, and scientific rigor. Decisions based on trial and error are often anecdotal and not grounded in validated research.
Rationale for incorrect answers:
A. Clinical experiences: While personal clinical experiences are important, they are still grounded in observation and practice. They may be biased, but they are often more applicable than trial and error.
B. Opinions of experts: Expert opinion is valuable, but it lacks the rigorous testing and validation of research. It’s based on experience rather than systematic investigation.
C. Client values and preferences: While subjective, client values are essential in shared decision-making. They do not rank in the evidence hierarchy itself but are considered alongside best evidence.
Take-home points:
- The strongest evidence comes from well-designed research, but patient values and clinical judgment remain essential in applying it.
A quantitative research approach is most appropriate for which study?
Explanation
Quantitative research focuses on measurable variables and numerical data to establish patterns, relationships, and cause-effect links. It is particularly useful when researchers want to test hypotheses or determine the impact of an intervention.
Rationale for correct answer:
A. A study measuring the effects of sleep deprivation on wound healing: This involves measurable outcomes (e.g., wound size, healing time) and seeks statistical analysis, making it ideal for quantitative research.
Rationale for incorrect answers:
B. A study examining the bereavement process in spouses of clients with terminal cancer: This involves exploring personal experiences, emotions, and meanings, which fits qualitative research.
C. A study exploring factors influencing weight control behavior: While some parts could be measured, “exploring factors” often implies a qualitative approach to understand motivations and barriers.
D. A study examining a client’s feelings before and after a bone marrow aspiration: This involves subjective feelings and personal perception, which are typically analyzed using qualitative methods.
Take home points:
- Quantitative research answers “how much” or “how many” using numbers and measurable outcomes.
- Qualitative research explores meanings, experiences, and perceptions, often without statistical measurement.
A nurse proposes that the hospital apply the findings from a recent research study that shows that clients appreciate classical orchestra music and playing it frequently lowers clients’ blood pressure. Which aspect of research suggests that it may not be appropriate to implement this as evidence-based practice?
Explanation
Evidence-based practice (EBP) integrates the best available research evidence with clinical expertise and patient preferences. However, the adoption of findings into practice requires critical appraisal of research quality, replication of results, and applicability to a specific patient population.
Rationale for correct answer:
C. One study would not be sufficient to show that all clients would find orchestral music pleasing: Evidence-based practice typically requires consistent findings from multiple high-quality studies to ensure that the results are reliable and applicable to diverse populations.
Rationale for correct answer:
A. All research is flawed: While no study is perfect, this statement is overly broad and does not specifically address why one study alone may be insufficient to guide practice.
B. The research would not have taken into consideration the cost of acquiring and playing the music in a hospital: Cost analysis is relevant to feasibility but is not the primary research limitation in this scenario; the main concern is generalizability from only one study.
D. Research cannot demonstrate clients’ appreciation of music since research is only appropriate for physiological problems: Research can absolutely study psychological, emotional, and satisfaction-related variables; it is not limited to physiological outcomes.
Take home points
- Always look for replication of results across multiple well-designed studies before recommending widespread implementation of a practice.
- Evidence-based practice considers not only the presence of a positive finding but also its generalizability to different patient populations.
A nurse is formulating a clinical question in PICO format. Which of the following is represented by the letter P?
Explanation
PICO is a mnemonic used to build focused clinical questions for evidence-based practice: Patient/Population/Problem, Intervention, Comparison, Outcome.
Rationale for correct answer:
D. Explicit descriptions of population of interest: P refers to the patient group or problem (e.g., adults with type 2 diabetes, postoperative hip fracture patients).
Rationale for incorrect answers:
A. Comparison to another similar treatment: That describes C (Comparison), not P.
B. Clearly defined, focused literature review: A literature review is a research activity, not the P element of PICO.
C. Specific identification of the desired outcome: That is O (Outcome), not P.
Take home points:
- A research critique is a balanced appraisal of strengths and weaknesses that informs evidence-based decisions.
- Use the critique to determine trustworthiness and clinical applicability, not just to summarize the article
A new graduate nurse attends a hospital in-service training focused on evidence-based nursing. Which of the following best describes the foundation of research?
Explanation
In nursing practice, research provides the backbone of evidence-based care, which leads to improved patient outcomes, safer practices, and informed clinical decision-making.
Rationale for correct answer:
D. The scientific method is the core foundation of research. It provides a systematic, logical process that includes formulating a question, developing a hypothesis, collecting data, analyzing results, and drawing conclusions.
Rationale for incorrect answers:
A. Evidence: While evidence is the product or outcome of research, it is not the foundation. Evidence is gathered after a study has been conducted, analyzed, and interpreted using a structured approach.
B. Experience contributes to clinical judgment, but it is not the foundation of formal research. Relying solely on experience can introduce bias and inconsistencies. Research goes beyond individual experiences to test hypotheses under controlled and repeatable conditions.
C. Critical thinking is essential for interpreting and applying research findings, but it is not the foundational structure upon which research is conducted. It supports research utilization, not research development itself.
Take home points:
- The scientific method is the structured process that underpins all rigorous nursing research.
- Only the scientific method provides the systematic framework necessary to conduct high-quality research and generate evidence for clinical decision-making.
Practice Exercise 2
Which of the following are obstacles to moving research rapidly into client care?
Explanation
Evidence-based practice (EBP) is essential for improving patient outcomes and ensuring safe, effective nursing care. However, translating research findings into real-world clinical practice can be delayed due to a variety of barriers.
Rationale for correct answer:
A. Inadequate scientific base: Without a strong foundation of evidence, it's difficult to justify or implement new practices in client care.
B. Unfavorable organizational climates: Resistance to change, lack of leadership support, or rigid bureaucratic structures can slow down the adoption of research findings.
D. Limited communication and collaboration between researchers and practitioners: When researchers and clinicians operate in silos, valuable insights may not be shared or translated effectively into practice.
Rationale for incorrect answer:
C. Lack of access to a health care library: While access to resources is helpful, it's not typically considered a major systemic barrier compared to the others listed.
Take home points:
- Barriers to EBP include lack of evidence, organizational resistance, limited resources, and poor communication.
- Actively fostering collaboration, access to research, and supportive environments speeds up the integration of evidence into patient care.
A qualitative research approach is most appropriate for which study?
Explanation
Qualitative research is used to explore and understand human experiences, emotions, perceptions, and meanings. Unlike quantitative research, which focuses on numbers and measurable data, qualitative research investigates the "why" and "how" behind behaviors, feelings, and decisions.
Rationale for correct answer:
C. A study examining client reactions to stress after open heart surgery: This is qualitative because it focuses on subjective reactions, emotions, and coping strategies. Such data cannot be fully captured through numbers but require descriptive, narrative accounts.
Rationale for incorrect answers:
A. A study measuring nutrition and weight loss or gain in clients with cancer: This is quantitative research because it involves objective measurement of physical parameters (weight, nutrient intake) and statistical analysis, not subjective experiences.
B. A study examining oxygen levels after endotracheal suctioning: This also falls under quantitative research since oxygen levels are numerical, measurable values.
D. A study measuring differences in blood pressure before, during, and after a procedure: This is a quantitative study as it involves measurable physiologic data (blood pressure readings).
Take home points:
- Qualitative research = exploring lived experiences, perceptions, and emotions; quantitative research = measuring numerical variables.
- Research design must match the research question-subjective experiences that require qualitative methods.
A key function of a study’s methodology is to
Explanation
In research, the methodology is the structured plan that outlines how a study will be conducted. It details the research design, data collection methods, sampling, and analysis procedures.
Rationale for correct answer:
B. Exercise control over contaminating factors in the study environment: Methodology includes strategies to minimize bias and control extraneous variables to ensure that results are accurate and valid.
Rationale for incorrect answers:
A. Determine the hypotheses that will be tested in the study: Hypotheses are formulated before the methodology section is developed. The methodology tests the hypotheses, but determining them is part of the research question formulation stage.
C. Identify grants and other funding sources for conducting the study: Securing funding is part of the research planning process, not the methodological framework.
D. Protect the rights of the study’s participants: Protecting participants’ rights is part of research ethics and is overseen by Institutional Review Boards (IRBs), not directly a function of the methodology section (though ethical procedures are described within it).
Take home points
- Methodology ensures control of variables and consistency in how research is carried out, which improves validity and reliability.
- While ethics and funding are important, methodology’s main role is to describe how the study is conducted to answer the research question accurately.
Which of the following is a nursing responsibility when reading published nursing research?
Explanation
When nurses read published research, their role is to critically appraise the study. That means evaluating the study’s quality, relevance to their patients, feasibility of applying the findings in their setting, and whether the evidence fits with patient values and resources.
Rationale for correct answer:
B. Evaluate whether the findings are applicable to the nurse’s specific clients: A key nursing responsibility is to determine external validity - are the study population, setting, interventions, and outcomes similar enough to your clients that the findings can be safely and effectively applied?
Rationale for incorrect answers:
A. Assume that the research was properly conducted since it has been published: Publication (even peer review) does not guarantee methodological rigor or applicability. Studies may have bias, small samples, conflicts of interest, or be published in low-quality journals.
C. Implement the research findings if at least two studies have shown the same results: Consistency across studies is important, but implementation requires assessing study quality, totality of evidence (systematic reviews/meta-analyses are stronger), clinical significance, feasibility, and patient preferences.
D. Request the raw data from the researchers so that the nurse can analyze the statistics again: Re-analyzing raw data is not a routine nursing responsibility and is often impractical (data access, time, statistical expertise, confidentiality). Nurses should critique methods and report analyses instead.
Take home points
- Always critically appraise research for validity and applicability before applying it to your patients.
- Relevance to your specific patient population and clinical setting is as important as the study’s reported results.
Practice Exercise 3
A client in the ICU experiences a sentinel event related to central line catheter care that resulted in serious injury. What performance improvement (PI) model should the unit use to identify errors that led to the sentinel event?
Explanation
Sentinel events are unexpected occurrences involving death or serious physical or psychological injury. When such events happen, healthcare teams must investigate what went wrong and why. Performance improvement (PI) models provide structured frameworks to analyze and improve healthcare processes.
Rationale for correct answer:
B. Root Cause Analysis (RCA) is the primary tool used after a sentinel event to investigate and understand the underlying system failures that led to the incident. It involves asking "why" repeatedly to drill down into the fundamental causes.
Rationale for incorrect answers:
A. Six Sigma is a data-driven quality improvement method used to reduce process variation and defects. While it is useful for process improvement over time, it is not the first-line tool used immediately after a sentinel event.
C. PDSA (Plan-Do-Study-Act) cycle is a quality improvement model used to test and implement changes in processes. While PDSA can follow RCA to address problems identified, it is not the ideal tool to investigate a serious sentinel event.
D. Balanced Scorecard is a strategic planning and management system used to align activities with organizational goals by monitoring performance metrics. It is not designed for root-cause investigation or immediate error analysis following a sentinel event.
Take home points:
- Root Cause Analysis (RCA) is the most appropriate model for investigating sentinel events.
- Choosing the right PI model is essential-use RCA for event investigation.
The nurse identifies which of the following as outcomes measurements? Select all that apply
Explanation
In nursing and healthcare quality improvement, outcome measurements are indicators used to evaluate the actual results or impact of an intervention or care process on client health and safety.
Rationale for correct answer:
C. A nursing unit adopts a set of strategies for reducing pressure injuries, and the UPC members use direct observation of the skin to measure incidence of pressure injuries. Measuring the incidence of pressure injuries is a true outcome measurement. It evaluates whether the implemented strategies had the desired clinical effect on patient outcomes.
D. A nursing unit implements a new fall prevention protocol and checks the monthly performance data for incidence of falls on the unit. The incidence of falls reflects the clinical outcome of the fall prevention strategy. This is a classic example of an outcome measurement because it focuses on the end result that matters to patient safety.
Rationale for incorrect answers:
A.A nurse teaches a client how to administer an injection and then watches the client do a return demonstration. This is a process evaluation, not an outcome measurement. The nurse is assessing whether the client can perform the procedure correctly, but it does not measure the end result.
B. A nurse implements a new pain-management protocol and checks clients’ charts to confirm whether interventions are being provided. This is process-focused-it checks compliance with the intervention, not whether the intervention improved the clients' pain levels (which would be an outcome).
E. A nursing unit implements a client rounding program, and the charge nurse watches the assistive personnel to see whether hourly rounding is being done on clients. This is another process measure-the nurse is checking whether the intervention was carried out, not whether it had the desired impact, such as fewer call lights or improved patient satisfaction.
Take home points:
- Outcome measurements evaluate the effectiveness of nursing interventions by focusing on changes in client health status.
- Distinguishing between process and outcome measures ensures that healthcare teams not only implement changes correctly.
The nurse is using the QSEN competency of evidence-based practice (EBP) when working with the unit council to initiate a change related to pain management. Which behaviors demonstrate that the nurse is practicing behaviors associated with EBP? Select all that apply
Explanation
The Quality and Safety Education for Nurses (QSEN) initiative outlines key competencies to prepare nurses with the knowledge, skills, and attitudes (KSAs) necessary to improve healthcare quality and safety. One of these competencies is Evidence-Based Practice (EBP), which involves integrating the best current evidence with clinical expertise and patient/family preferences for optimal care.
Rationale for correct answer:
B. Reading original research related to pain management: This is a core behavior of EBP-seeking and critically appraising current research to inform clinical decisions. Reading primary research articles is an essential part of integrating evidence into practice.
D. Valuing EBP as critical to the development of pain management guidelines for the unit: This reflects the attitudinal component of EBP-recognizing the importance of evidence in creating protocols. Valuing evidence is key to fostering a culture of inquiry and improvement.
E.Describing to the unit council reliable sources for locating clinical guidelines: This demonstrates knowledge of where and how to access reliable, evidence-based resources, which is an important behavior when participating in practice change through EBP.
Rationale for incorrect answers:
A. Initiating plan for self-development as a team member: This behavior is related to teamwork and collaboration or professional development, not specifically to the QSEN competency of EBP. While personal growth is valuable, it does not directly demonstrate evidence-based practice behavior.
C. Demonstrating effective use of strategies to reduce risk of harm to self or others: This reflects the QSEN competency of safety, not EBP. Although safety overlaps with evidence-based practice in some contexts, this behavior is more aligned with risk reduction and injury prevention.
F. Applying technology and information management tools to support safe processes of care: This behavior aligns more with the QSEN competency of informatics, not EBP. While technology may assist in EBP efforts, the focus here is on safe care processes, not evaluating or using evidence.
Take home points:
- EBP behaviors include actively seeking, appraising, and applying current research and clinical guidelines to improve patient care.
- QSEN competencies are distinct yet interconnected.
The nurses in a medical unit have seen an increase in the number of pressure injuries developing in their clients. The nurses decide to initiate a performance improvement (PI) project using the PDSA model. Which of the following is an example of “Plan” from that model?
Explanation
Performance Improvement (PI) models like the PDSA (Plan-Do-Study-Act) cycle to guide problem-solving and promote better outcomes. The PDSA model is a cyclical, four-step framework used to test and implement changes in clinical practice.
Rationale for correct answer:
D. Meeting with all disciplines to develop a multidisciplinary approach for reducing pressure injuries: This reflects the “Plan” phase of the PDSA cycle. The team is identifying the problem, engaging key stakeholders, and developing a collaborative strategy to address pressure injuries.
Rationale for incorrect answers:
A. Orienting clients to the unit’s practice of hourly rounding on clients: This is an action that occurs after a plan has been made. It falls under the “Do” phase, where interventions are implemented. It reflects putting a plan into practice, not the planning process itself.
B. Reviewing the incidence of pressure injuries on clients cared for using the protocol: This is an example of the “Study” phase, where data is analyzed to determine whether the intervention had the desired effect. It involves reviewing outcomes, not planning them.
C. Based on findings from clients who developed injuries, implementing an evidence-based skin care protocol on all units: This reflects part of the “Act” phase, where broader implementation of a successful intervention is carried out. It's a step beyond planning and testing; it represents full-scale application of what has been learned.
Take home points:
- The "Plan" stage of the PDSA cycle focuses on identifying a problem, collecting baseline data, and designing an initial intervention.
- Understanding each phase of the PDSA cycle (Plan, Do, Study, Act) ensures that quality improvement efforts are well-organized, data-driven.
An 85-year-old client in a nursing home tells a nurse, “Because the doctor was so insistent, I signed the papers for that research study. Also, I was afraid he would not continue taking care of me.” Which client right is being violated?
Explanation
Informed consent is a fundamental component of ethical research involving human participants. It ensures that individuals voluntarily agree to participate after receiving full disclosure about the purpose, risks, benefits, and their rights.
Rationale for correct answer:
D. Right to self-determination: This right means individuals have the freedom to make their own choices-including the right to refuse participation in research-without pressure, coercion, or fear of losing care.
Rationale for incorrect answers:
A. Right not to be harmed: This right protects participants from physical, emotional, or psychological harm during a study. While the situation is ethically concerning, the client did not report harm from the research itself-only pressure to participate.
B. Right to full disclosure: Full disclosure involves providing complete and understandable information about the research, including its purpose, risks, benefits, and procedures.
C. Right to privacy and confidentiality: This right pertains to the handling of personal information-ensuring that any data collected is kept confidential and used appropriately. There's no indication in the scenario that the client’s private health information was mishandled.
Take home points:
- The right to self-determination is foundational in research ethics, requiring that all participation be voluntary and free of coercion.
- Pressure, manipulation, or fear of withdrawal of care invalidates informed consent.
A nurse implements an EBP change that teaches patients the importance of taking their diabetes medications correctly and regularly on time using videos streamed on the Internet. The nurse measures the patients’ behavioral outcome from the practice change by using which type of measurement?
Explanation
When you implement an intervention you must choose appropriate measures. Distinguish process measures (was the intervention delivered?), behavioral measures (did patients change what they do?), and clinical/physiologic outcomes (did health status change?).
Rationale for correct answer:
D. Checking patients’ blood sugars: Blood glucose (or A1c) is a clinical outcome closely tied to medication adherence for diabetes and therefore a meaningful measure of whether the educational intervention produced the desired behavioral effect.
Rationale for incorrect answers:
A. Measuring the patients’ weight: Weight may change from many factors and is not a direct indicator of diabetes medication adherence over a short timeframe.
B. Chart auditing teaching sessions: This is a process measure (documents that teaching occurred), not a measure of patients’ behavior or clinical response.
C. Observing patients viewing the videos: That shows exposure to the intervention (process), not whether they actually take medications correctly and on time.
Take home points:
- Match your measure to the outcome: process (was it done?), behavior (did patients change actions?), or clinical outcome (did health improve?).
- When direct behavioral measures aren’t available, use meaningful clinical proxies (e.g., blood sugars for diabetes adherence), but be aware they can be influenced by other factors.
Comprehensive Questions
A nurse is aware that, ‘‘The systematic collection of numerical information, often under conditions of considerable control, and the analysis of the information using statistical procedures’’ best defines:
Explanation
In nursing and healthcare research, understanding the different types of research methodologies is essential for evaluating and applying evidence to practice. Distinguishing between the various approaches helps nurses select appropriate studies, critically appraise findings, and contribute to improving care.
Rationale for correct answer:
A. Quantitative research: This type of research involves the systematic collection and statistical analysis of numerical data. It typically uses controlled conditions, large sample sizes, and measurable variables to test hypotheses and answer specific questions.
Rationale for incorrect answers:
B. Qualitative research focuses on exploring human experiences, emotions, and perceptions through non-numerical data such as interviews, observations, and thematic analysis. It is more subjective and descriptive.
C.Experimental research is a subcategory of quantitative research that includes manipulating variables and using control groups to determine cause-and-effect relationships.
D. Evidence-based practice (EBP) is the integration of the best research evidence with clinical expertise and patient values. It is a broader approach that uses research findings (from both quantitative and qualitative studies), but it is not a type of research itself.
Take home points:
- Quantitative research is defined by its use of numerical data, statistical analysis, and controlled conditions.
- Understanding the differences between research types helps nurses critically evaluate studies.
The nurse understands that informed consent requires the researcher to communicate which of the following to the participant? Select all that apply
Explanation
The nurse researcher plays a key role in ensuring that the consent process respects the client’s autonomy, confidentiality, and decision-making rights. Understanding what information must be included in the consent process helps ensure that participants are protected and ethical standards are upheld.
Rationale for correct answers:
A. The nature of the study: Participants must be clearly informed about what the study involves, including its purpose, procedures, and overall design. This ensures transparency and informed decision-making.
B. The subject’s right to refuse participation: A core component of informed consent is that participation must be voluntary, and participants have the right to refuse or withdraw at any time without penalty or impact on their care.
D.The expected outcomes, risks, and benefits of the study: Participants must be made aware of potential risks, benefits, and possible outcomes of participation so they can make an informed decision about whether or not to enroll.
Rationale for incorrect answers:
C.That the data will be shared with all health care providers: Informed consent emphasizes confidentiality and data protection. Data should only be shared as outlined in the consent form, often limited to the research team.
E. That the family and the prescribing practitioner determine the client’s rights to participate: The right to participate in research lies with the individual client, assuming they have capacity. Family or providers cannot override or control a capable individual's right to consent or refuse participation.
F. That the agency has the right to use the data freely: Participants must be told how their data will be used, stored, and shared, and data use must align with what they consent to. Agencies do not have unrestricted rights to use participant data unless explicitly stated and agreed upon.
Take home points:
Informed consent protects participants' autonomy and requires that they receive clear, complete, and truthful information.
Nurses involved in research must ensure that:
- confidentiality is maintained
- consent is voluntary
- participants understand they can withdraw without consequences
A nurse is conducting a staff education about evidence-based practice. Number the following steps of evidence-based reports in the appropriate order.
Explanation
Evidence-Based Practice (EBP) is a structured process that integrates the best available research evidence with clinical expertise and patient preferences to improve outcomes. To effectively implement EBP, nurses must follow a systematic approach that begins with asking the right question and ends with making evidence-informed recommendations.
Rationale for correct answer:
Step 1: Ask the clinical question
The EBP process begins with formulating a focused, answerable question-often using the PICO format. This step guides the literature search and ensures that the review is relevant to the clinical issue at hand.
Step 2: Analysis of scientific data
Once relevant research is gathered, it must be analyzed critically to determine what the studies found. This includes evaluating results, statistical significance, and how the findings apply to the clinical setting.
Step 3: Level of evidence
After analyzing the data, the quality and strength of the evidence are determined. This step involves grading the studies based on the hierarchy of evidence, with systematic reviews and randomized controlled trials ranked highest.
Step 4: Recommendations for practice
Based on the strength and applicability of the evidence, the final step is to formulate recommendations that can be implemented in clinical practice to improve outcomes.
Take home points:
- Following a structured sequence in EBP ensures clinical decisions are grounded in solid evidence.
- The first and most important step in EBP is asking a clear clinical question.
A nurse is attending a staff training on evidence-based practice. Match the components of PICO using the question “Does the use of guided imagery compared with standard care affect the postoperative pain in hospitalized adolescents?
Explanation
The PICO format is a framework used in evidence-based practice (EBP) to help clinicians formulate well-structured, answerable clinical questions and guide effective literature searches. PICO stands for Population/Problem, Intervention, Comparison, and Outcome.
Correct answers:
P) Patient/Population → 3. Hospitalized adolescents
This identifies the population being studied-the group affected by the clinical problem.
(I) Intervention → 4. Guided imagery
This is the new or experimental treatment being evaluated.
(C) Comparison → 1. Adolescents receiving standard care
This represents the control or usual care group against which the intervention is compared.
(O) Outcome → 2. Postoperative pain
This is the measurable effect or result being examined to determine the intervention's impact.
Take home points:
- The PICO format helps structure clinical questions clearly and concisely, guiding effective literature searches and research evaluation.
- Accurately identifying each component improves the nurse's ability to integrate evidence into clinical decision-making.
A nurse is educating student nurses about the PICO format. In the PICO format for phrasing research questions and identifying key terms for a literature search, what does the “P” stand for?
Explanation
The PICO format is a framework used in evidence-based practice (EBP) to help clinicians formulate well-structured, answerable clinical questions and guide effective literature searches. PICO stands for Population/Problem, Intervention, Comparison, and Outcome.
Rationale for correct answer:
B. Population: "P" in the PICO format stands for Population (or sometimes Patient/Problem). It defines who the question is about-including patient demographics (age, gender, condition, setting).
Rationale for incorrect answers:
A. Patterns: While recognizing clinical patterns can be useful in practice, "Patterns" is not part of the PICO framework. It doesn’t define the group being studied or the clinical issue in question.
C.Probability is a statistical concept, not part of the PICO structure. It may be relevant in data analysis, but it doesn't help define the clinical population or frame the research question.
D. Purpose: Although a research question has a purpose, the PICO acronym is not meant to outline the study's objective, but to provide a structure for breaking down the key components of a clinical question.
Take home points:
- “P” in the PICO format stands for Population (or Patient/Problem).
- Using the PICO format strengthens evidence-based practice by helping healthcare professionals develop focused questions.
Nurses in a community clinic are conducting an evidenced based practice (EBP) project focused on improving the outcomes of children with asthma. The PICO question asked by the nurses is “In school-age children, does the use of an electronic gaming education module versus educational books affect the usage of inhalers?” In the question, what is the “O”?
Explanation
The PICO format is a widely used tool in evidence-based practice (EBP) to develop focused clinical questions that guide the search for relevant evidence. PICO stands for: P = Population or Problem, I = Intervention, C = Comparison, O = Outcome.
Rationale for correct answer:
C. Use of inhalers: This is the “O” (Outcome). The goal of the project is to determine whether the use of inhalers is affected by the type of education provided. It is the measurable result that reflects the effectiveness of the interventions.
Rationale for incorrect answer:
A. Electronic gaming education: This is the “I” (Intervention). It is the new or experimental strategy being evaluated to see if it improves inhaler use compared to the standard approach.
B. Educational book: This is the “C” (Comparison). The educational book is the alternative to the main intervention and is used as a point of comparison to the electronic gaming module.
D. Electronic gaming education: This is the “I” (Intervention). It is the new or experimental strategy being evaluated to see if it improves inhaler use compared to the standard approach.
Take home points:
- The "Outcome" in a PICO question refers to the measurable result or effect the researchers hope to evaluate.
- Understanding how to break down a clinical question using the PICO framework strengthens evidence-based practice
A nurse research investigator is explaining a research study to a client. The client is interested in participating in the research study. The nurse investigator reviews the informed consent with the client. The client asks the nurse why he must sign the consent to participate in the study. What is the nurse’s best response(s) to the client’s question? Select all that apply
Explanation
Informed consent (IC) is a critical ethical and legal requirement that ensures respect for a person’s autonomy. It ensures that participants are fully informed about the purpose, procedures, risks, benefits, confidentiality, and voluntary nature of the study.
Rationale for correct answer:
A. “The informed consent (IC) provides you with complete information on the research study.” Informed consent includes comprehensive details about the study's purpose, procedures, risks, benefits, alternatives, and duration. Providing complete information helps the client make an informed decision.
B.“By reviewing the consent with you, I can make sure that you understand the study and what it means for you to participate.” One of the ethical principles of informed consent is ensuring comprehension. The nurse's role is not just to obtain a signature, but to ensure that the client fully understands what participation involves.
D. “The informed consent provides your voluntary agreement to participate in the research study.” This is the essence of informed consent. Signing the form demonstrates that the client has freely and voluntarily agreed to participate without coercion.
E.“The informed consent explains how the data collected from you will be kept confidential during and after the study.” Confidentiality is a key element of informed consent. The document explains how personal data will be protected, who will have access, and how it will be stored and used.
Rationale for incorrect answer:
C. “The informed consent provides details on the limitations of the study.” While a study’s limitations may be addressed in broader scientific discussions or the research publication, they are not typically a core part of informed consent.
Take home points:
- Informed consent is more than just a signature-it is a process of providing clear, complete, and understandable information.
- The nurse investigator plays a vital role in ensuring ethical research participation.
When a nurse asks a student nurse why it is necessary to change the client’s bed every day, he says, “I guess we have always done it that way.” This answer is an example of which of the following?
Explanation
In clinical nursing practice, the source of knowledge influences how and why care is delivered. Nurses are expected to base their actions on evidence-based practice rather than habit or hearsay. Understanding the types of knowledge in nursing-such as scientific, authoritative, traditional, and unsubstantiated-helps nurses critically evaluate practices and make informed, effective decisions.
Rationale for correct answer:
D. Traditional knowledge refers to customs, habits, or practices passed down from generation to generation without questioning or validating their rationale.
Rationale for incorrect answers:
A. Unsubstantiated knowledge: This refers to information or beliefs that lack evidence or support-often rooted in myths, personal opinions, or cultural misconceptions.
B. Scientific knowledge is evidence-based and derived from research and systematic investigation. If the student had cited research or a rationale based on infection control studies or hospital policy backed by evidence, it would reflect scientific knowledge.
C. Authoritative knowledge: This type of knowledge comes from an expert or trusted source, such as a nursing textbook, policy manual, or a senior clinician giving a directive.
Take home points:
- Relying solely on traditional knowledge without questioning its relevance or evidence can lead to outdated or ineffective practices.
- Professional nursing practice demands the integration of scientific and authoritative knowledge.
A nurse researcher is studying the effects of exercise and sleep on blood pressure. The researcher identifies blood pressure as which type of variable?
Explanation
In research studies, correctly identifying the type of variable is crucial to ensure that the design, data collection, and analysis are appropriately structured to answer the research question. Therefore, it is essential to determine which variable is being manipulated or measured in response to the others. This helps in distinguishing independent from dependent variables and understanding the nature of the research.
Rationale for correct answer:
C. A dependent variable is the outcome or response that is measured in a study. In this case, blood pressure is what the researcher is observing or measuring to determine the effect of the independent variables (exercise and sleep).
Rationale for incorrect answers:
A. Exploratory: This refers to a type of research design. Exploratory research is conducted when the problem is not clearly defined, and the goal is to gather preliminary data or insights.
B. Correlational: This is also a type of study design. A correlational study assesses the strength and direction of the relationship between variables, but it does not involve manipulation of variables like in an experimental or quasi-experimental study.
D. An independent variable is the one that is manipulated or categorized to determine its effect on the dependent variable. In this case, exercise and sleep are the independent variables.
Take home points:
- The dependent variable is the outcome that is being measured or observed to determine the impact of changes in the independent variable.
- Understanding the distinction between types of variables and study designs is essential for designing valid studies and interpreting results accurately.
A research critique can best be defined as a/an
Explanation
A research critique is a systematic evaluation of a study’s design, methods, results, and conclusions. Its purpose is to identify strengths and weaknesses so clinicians can judge the credibility of the findings and their usefulness in practice.
Rationale for correct answer:
A. Appraisal of a study’s strengths and weaknesses: A critique examines methodological quality (sampling, bias control, measurements, analysis), interprets findings, and identifies limitations and strengths.
Rationale for incorrect answers:
B. Conclusion about the utilization potential of a study’s findings: Deciding on utilization may follow a critique, but a critique itself is the appraisal process; recommending implementation is a separate step informed by the critique.
C. Criticism of a study’s flaws: This is too narrow and negatively framed. A critique includes identification of both strengths and weaknesses, not just fault-finding.
D. Summary of a study’s key points: A summary (abstract) describes content; a critique goes deeper to evaluate how well the study was done and how trustworthy the results are.
Take home points
- A research critique is a balanced appraisal of strengths and weaknesses that informs evidence-based decisions.
- Use the critique to determine trustworthiness and clinical applicability, not just to summarize the article.
One method of developing a theory is by first examining a general idea and then considering specific actions or ideas. What is this method called?
Explanation
In nursing research and theory development, reasoning methods help bridge the gap between abstract concepts and practical application. Deductive and inductive reasoning are two complementary approaches used to explore, develop, and test theories.
Rationale for correct answer:
B. Deductive reasoning: Deductive reasoning starts with a general principle or theory and then derives specific predictions or actions to test or apply.
Rationale for incorrect answers:
A. Inductive reasoning: Inductive reasoning begins with specific observations and builds toward generalizations or theory, not the other way around.
C. Conceptual modeling: Conceptual modeling organizes concepts into a framework, but it is not specifically a method of reasoning from general to specific.
D. Concept development: Concept development focuses on refining and clarifying a concept for research or practice, not necessarily reasoning from general to specific.
Take home points
- Deductive reasoning applies broad theories to predict or explain specific instances; inductive reasoning works in the opposite direction.
- Understanding reasoning methods is essential in nursing research for both generating and testing new theories effectively.
When describing the term concept to a group of students, which word would the instructor most likely use?
Explanation
In nursing theory, a concept is a mental image or abstract idea that helps explain a phenomenon or guide clinical thinking. Concepts are the building blocks of theories-they allow nurses to organize observations, label phenomena, and create a shared language for practice.
Rationale for correct answer:
C. Idea: A concept is essentially an abstract idea or mental representation that defines or describes a phenomenon.
Rationale for incorrect answers:
A. Fact: A fact is something objectively verifiable and proven true through evidence; while a concept can be based on facts, it is broader, more abstract, and not always universally proven.
B. Science: Science is a systematic process of gaining knowledge; concepts are components of science but not synonymous with it.
D. Truth: Truth is a judgment or belief that is considered universally valid; concepts can be subjective and may vary depending on context or discipline.
Take home points
- In nursing theory, a concept is best described as an abstract idea used to explain phenomena.
- Concepts form the foundation for developing models and theories that guide nursing practice.
Which type of theory focuses on clinical nursing practice?
Explanation
Nursing theories vary in scope and purpose. Some describe phenomena (descriptive), some explain growth and changes (developmental), others explore complex interactions (systems), and some directly guide clinical decision-making (prescriptive).
Rationale for correct answer:
A. Prescriptive theories guide nursing interventions, predict outcomes, and provide direct instructions for clinical practice.
Rationale for incorrect answers:
B. Descriptive theory: Descriptive theories explain or describe a phenomenon without directing specific nursing actions.
C. Developmental theory: Focuses on the process of growth and development across the lifespan, not on nursing interventions.
D. Systems theory: Examines how components of a system interact, useful for understanding healthcare environments but not specifically for guiding direct care actions.
Take home points
- Prescriptive theories are designed to guide nursing interventions and predict patient outcomes.
- Different theory types serve different purposes-choosing the right one depends on whether you’re describing, explaining, or applying nursing knowledge.
When conducting research, information is collected. This would be identified as which of the following?
Explanation
When conducting research, investigators gather information systematically to answer specific questions or test hypotheses. This collected information is the foundation for analysis and interpretation, ultimately guiding decision-making in clinical and academic settings.
Rationale for correct answer:
C. Data refers to the raw information collected during research, which is later analyzed to draw conclusions.
Rationale for incorrect answers:
A. A subject is the person or entity from whom data is collected, not the information itself.
B. Analysis refers to the process of examining data, not the data itself.
D. An abstract is a summary of a research study, usually found at the beginning of a report or article.
Take home points
- In research, the term data refers to the actual pieces of information collected for analysis.
- Distinguishing between data, subjects, and analysis prevents confusion in interpreting research methodology.
Which type of quantitative research is conducted to directly influence or improve clinical practice?
Explanation
Quantitative research can be broadly categorized based on its purpose-whether to generate theoretical knowledge or to address immediate, practical problems.
Rationale for correct answer:
B. Applied research aims to solve real-world problems and directly improve practice, making it highly relevant to clinical nursing.
Rationale for incorrect answers:
A. Basic research seeks to expand theoretical knowledge without immediate application to practice.
C. Experimental research involves manipulating variables to establish cause-effect relationships but is not always focused on direct clinical improvement.
D. Descriptive research provides detailed observations of phenomena but does not necessarily aim to change practice directly.
Take home points
- Applied research is designed to directly address practical issues and improve clinical care.
- Choosing the correct research type is essential for aligning study goals with desired patient care outcomes.
Exams on Research And Evidence Based Practice In Nursing
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Explain the relationship between research and evidence-based nursing practice.
- Apply the steps of change used in implementing evidence-based practice.
- Develop a PICOT question.
- Summarize the levels of evidence available in the literature.
- Describe limitations in relying on research as the primary source of evidence for practice.
- Differentiate the quantitative approach from the qualitative approach in nursing research.
- Outline the steps of the research process.
- Describe research-related roles and responsibilities for nurses.
- Describe the nurse’s role in protecting the rights of human participants in research.
- Discuss how performance improvement (PI) affects health care.
Introduction
Current standards of professional performance for nurses include using evidence and research findings in practice.
All nurses are expected to use evidence and research to determine proper nursing actions, to engage in research activities as appropriate to their abilities, and to share knowledge with other nurses.
Nursing research is a ‘‘scientific process that validates and refines existing knowledge and generates new knowledge that directly and indirectly influences nursing practice’’.
Evidence-based practice (EBP) is using the best evidence available to guide clinical decision making.
Nursing has historically acquired knowledge through:
- Traditions: basing practice on customs and past trends
- Authority: crediting another person as the source of information
- Borrowing: using knowledge from other disciplines to guide nursing practice
- Trial and error: using unknown outcomes in a situation of uncertainty
- Personal experience: gaining knowledge by being personally involved in an event, situation, or circumstance
- Role modeling and mentorship: imitating the behaviors of an exemplar
Evidence Based Practice
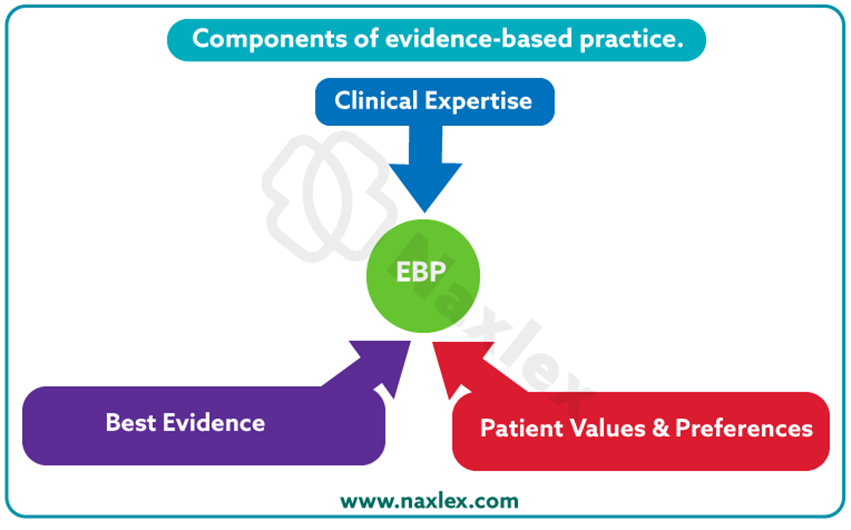
Evidence-based practice (EBP), or evidence-based nursing, occurs when the nurse can “integrate best current evidence with clinical expertise and client/family preferences and values for delivery of optimal health care”.
Model for changing practice as a result of evidence:
- Cultivate a spirit of inquiry.
- Ask clinical questions in standard format eg. PICOT
- Search for the best evidence.
- Critically appraise the evidence.
- Integrate the evidence with clinical expertise and client/family preferences and values.
- Implement and evaluate the outcomes of the intervention.
While evidence includes theories, opinions of recognized experts, clinical expertise, clinical experiences, and findings from client assessments, findings from research studies are often given the most weight in the decision-making process.
This emphasis is because research entails using formal and systematic processes to address problems and answer questions.
The disciplined thinking and the careful planning and execution that characterize research means that the resulting findings should be accurate, dependable, and free from bias.
Concerns about reliance solely on research for EBP:
- Research evidence suggests that there is one best solution to a problem for all clients and this limited perspective stifles creativity.
- Research is often done under very controlled circumstances, which is very different from the real world of health care delivery.
- Not all published research is robust and flawless.
- EBP should promote cost-effective care, but cost is often not included in traditional research studies
- Research may ignore the significance of life events to the individual.
3.1 Developing a PICOT Question
P = Patient/ population of interest
Identify patients by age, gender, ethnicity, and disease or health problem.
I = Intervention or area of interest
Which intervention is worthwhile to use in practice (e.g., a treatment, diagnostic test, prognostic factor)?
What area of interest influences a desired outcome (e.g., complementary therapy, motivational interviewing)?
C = Comparison intervention or area of interest
What is the usual standard of care or current intervention used now in practice?
O = Outcome
What result do you wish to achieve or observe as a result of an intervention (e.g., change in patient behavior, physical finding, or patient perception)?
Make an outcome statement nondirectional. For example: “Does use of chlorhexidine affect incidence of CLABSI?” instead of “Does the use of chlorhexidine reduce incidence of CLABSI?”
A directional outcome may limit the articles in your search.
T = Time
What amount of time is needed for an intervention to achieve an outcome (e.g., the amount of time needed to change quality of life or patient
In some cases, additional components are added to make PICO into PICOD by adding study Design, PICOS by adding Setting or PICOC adding Context.
Nursing insights:
- Proper question formatting allows you to identify key words to use when conducting your literature search
- Note that a well-designed EBP question does not have to follow the sequence of P, I, C, O, and T.
- The aim is to ask a question that contains as many of the PICOT elements as possible to identify knowledge gaps within a clinical situation.
3.2 Levels of Evidence
Once you have a clear and concise PICOT question, you are ready to search for scientific evidence.
A variety of sources will provide the evidence needed to answer your question, such as agency policy and procedure manuals, quality improvement data, existing clinical practice guidelines, and journal articles.
A peer-reviewed article is reviewed for accuracy, validity, and rigor and approved for publication by experts before it is published.
Searchable Scientific Literature Databases and Sources include:
- AHRQ
- CINAHL
- MEDLINE
- EMBASE
- PsycINFO
- Cochrane Database of Systematic Reviews
- PubMed
- World Views on Evidence-Based Nursing
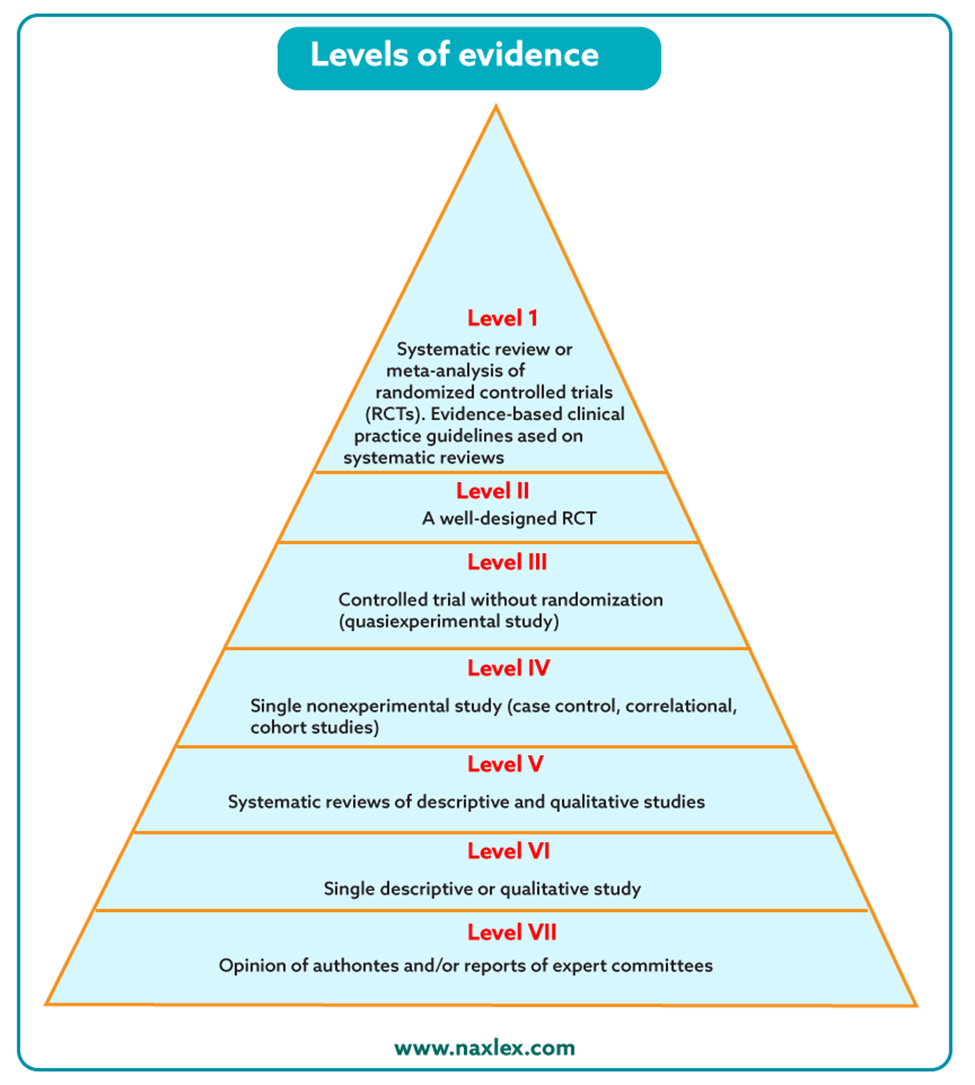
It is important to use the hierarchy of evidence available as depicted in the figure. The level of rigor or amount of confidence you can have in the evidence (e.g., findings from a study) decreases as you move down the pyramid.
Meta-analyses and systematic reviews are the perfect answers to PICOT questions because they rigorously summarize current evidence about a specific topic or intervention.
The use of clinical experts may be at the bottom of the evidence pyramid, but do not consider clinical experts to be poor sources of evidence.
Expert clinicians use evidence frequently as they build their own practices, and they are rich sources of information for clinical problems.
Nursing insights:
- Evidence-based practice, or evidence-based nursing, involves clinical decision making using a variety of sources of evidence modified for use in specific settings and for individual clients.
- Change in practice requires assessing the need for change; locating and analyzing the best evidence; designing, implementing, and evaluating the practice change; and integrating and maintaining the change.
Nursing Research
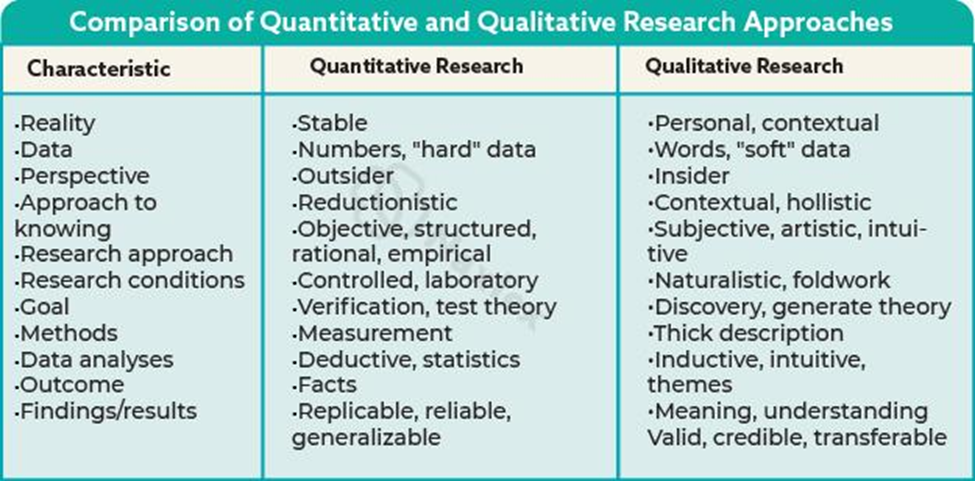
Nurse researchers use two major approaches to investigating clients’ responses to health alterations and nursing interventions.
Quantitative research:
Quantitative research entails the systematic collection, statistical analysis, and interpretation of numerical data.
The quantitative approach to research is linked to the philosophical perspective of logical positivism, which maintains that “truth” is absolute and can be discovered by careful measurement.
It focuses on the who, what, where, when, why, and how questions.
Qualitative research:
Qualitative research is the systematic collection and thematic analysis of narrative data.
The qualitative approach to research is rooted in the philosophical perspective of naturalism (sometimes referred to as constructivism), which maintains that reality is relative or contextual and constructed by individuals who are experiencing a phenomenon.
Nurse researchers tend to use one of three distinct qualitative traditions: phenomenology, ethnography, or grounded theory.
- Phenomenology focuses on lived experiences. Eg. What is the experience of receiving diagnosis X or undergoing treatment Y?
- Ethnography focuses on cultural patterns of thoughts and behaviors. Eg. What are typical behaviors of certain groups of clients?
- Grounded theory focuses on social processes. Additional qualitative types include historical and case study research. Eg. How do individuals cope with X?
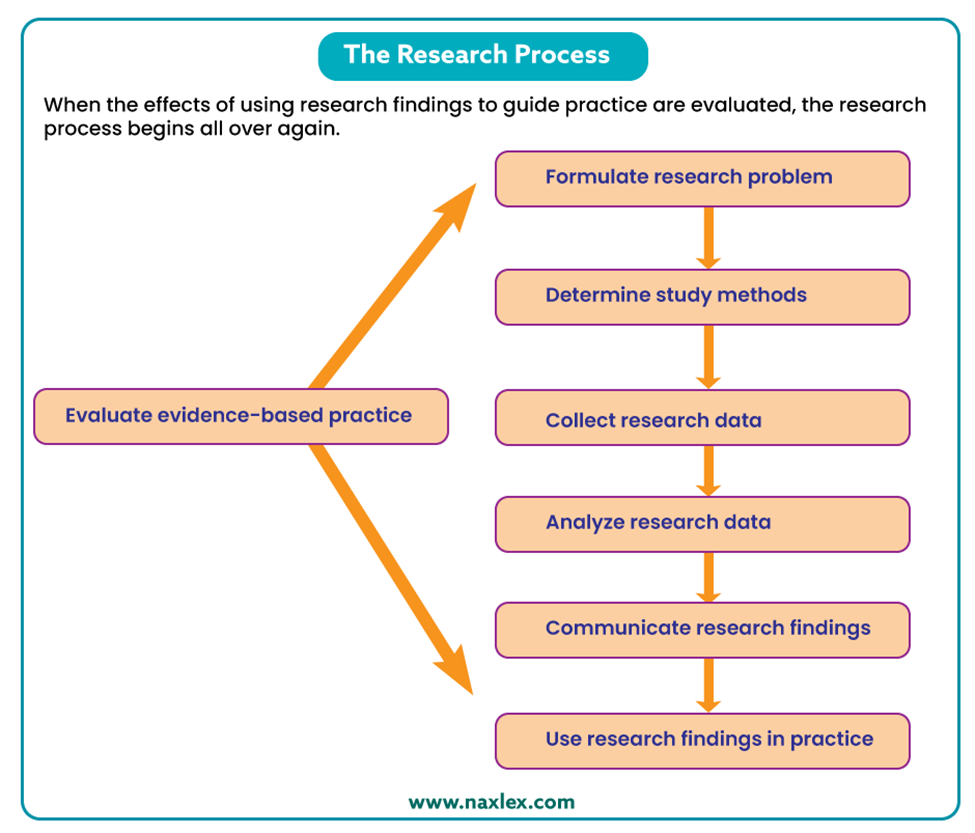
The Research Process:
The research process is a process in which decisions are made that result in a detailed plan or proposal for a study, as well as the actual implementation of the plan.
Although the research process unfolds somewhat differently for quantitative and qualitative studies, the same general steps are involved:
- formulating the research problem and purpose
- determining study methods
- collecting research data
- analyzing research data
- communicating research findings
- using research findings in practice
FORMULATING THE RESEARCH PROBLEM AND PURPOSE:
The researcher’s first task is to narrow a broad area of interest into a more specific problem that indicates the issue of concern behind the study.
Ideas for research problems may arise from recurrent problems encountered in practice, questions that are difficult to resolve because of contradictions in the literature, or areas in which minimal or no research has been done.
The problem must also be feasible to study in light of the resources (including time and skill) that are available to conduct the study.
One strategy for stating the problem you wish to explore is to use the PICOT format.
Reviewing the literature can also help the researcher identify strategies that have been used successfully (and unsuccessfully) in the past to investigate the problem and to measure the variables of interest
- A dependent variable is a behavior, characteristic, or outcome that the researcher wishes to explain or predict.
- An independent variable is the presumed cause of or influence on the dependent variable.
- In some studies, the researcher may develop a hypothesis or a predictive statement about the relationship between two or more variables.DETERMINING STUDY METHODS
The methodological elements of the research process deal with how the study is organized, who or what will be the sources of information for the study, and data collection details such as what data will be collected, how data will be collected, and the timing of data collection.
Research design refers to the overall structure or blueprint or general layout of a study.
There are two major types of research designs:
- Experimental design, the researcher controls the independent variable by administering an experimental treatment to some participants while withholding it from others. Used to determine cause-and-effect relationships.
- Nonexperimental design, there is no manipulation of the independent variable; in fact, there may be no identifiable independent and dependent variables in the study. Nonexperimental designs are used for descriptive research studies.
COLLECTING RESEARCH DATA
Researchers expend great effort to ensure that data collection occurs in a consistent manner throughout the course of the study.
Detailed data collection protocols or instructions and careful training of research assistants are strategies that can be used to ensure the consistency and integrity of data collection procedures.
- Reliability refers to the consistency of measures.
- Validity refers to the completeness and conceptual accuracy of measures
ANALYZING RESEARCH DATA
The collected data are organized and analyzed to answer the research question(s) or test the study’s hypothesis.
Quantitative approach:
Descriptive statistics are procedures that organize and summarize large volumes of data including measures of central tendency and measures of variability.
- Measures of central tendency provide a single numerical value that denotes the “average” value for a variable. Eg. mean, median, mode
- Measures of variability describe how values for a variable are dispersed or spread out. Eg. range, standard deviation
Inferential statistics allows researchers to test hypotheses about relationships between variables or differences between groups. Eg. Independent t-test, Paired t-test, ANOVA, Chi-square
After inferential statistics have been computed, the results are inspected for statistical significance.
Qualitative approach:
Data analysis involves searching for themes and patterns.
This procedure is sometimes referred to as content analysis because the content of narrative materials is being analyzed.
Qualitative researchers may synthesize their findings to develop a theory or conceptual framework of the phenomenon being studied.
COMMUNICATING RESEARCH FINDINGS:
Research findings can be communicated through publication in journals or at conferences.
Newsletter articles and research posters are ideally suited for small-scale research projects that are carried out in a clinical setting.
USING RESEARCH FINDINGS IN PRACTICE
Before a study’s findings are used to guide practice, they should undergo three types of evaluation:
- Scientific validation-thorough critique of a study for its conceptual and methodological integrity
- Comparative analysis-involves assessing study findings for their implementation potential. Involves:
- How the study’s findings compare to findings from other studies about the problem.
- How the study’s findings will transfer from the research conditions to the clinical practice conditions in which they will be used.
- Practical or feasibility considerations that need to be addressed when applying the findings in practice
- Cost–benefit appraisal-consideration of the potential risks and benefits of both implementing a change based on a study’s findings and not implementing a change.
Research-Related Roles and Responsibilities for Nurses
RESEARCH CONSUMER
Means routinely searching and reading the current research literature in order to stay current with new insights in client experiences and nursing and medical interventions.
Two skills are fundamental to this role:
- locating relevant literature
- critiquing research reports- research critique enables the nurse, as a research consumer, to determine whether the findings of a study are of sufficient quality to be used to influence practice decisions.
Tips for Conducting a Literature Review:
- Be a detective.
- Be organized.
- Identify keywords you will use to guide your search. Some articles and online search engines identify keywords associated with particular articles. It may be useful to use these to guide your own search.
- If possible, start with a manual search by going to the library. If you prefer to begin with an online search, keep track of references you locate so you can find them again when you need them.
- Consult the reference lists in useful articles.
- Be flexible and creative.
- Consider conducting separate searches for key variables.
- Ask for help from a librarian.
RESEARCH TEAM MEMBER:
Nurses in hospitals with this designation are expected to be involved in research and EBP activities on an ongoing basis including:
- Identifying clinically relevant problems that need to be studied
- Reviewing the literature to provide background information for a study
- Recruiting study participants
- Securing clients’ consent to participate in a study
- Designing data collection instruments
- Pilot-testing data collection procedures
- Collecting research data
- Monitoring for adverse effects of study participation
- Implementing research interventions
- Assisting with interpretation of study findings.
Protecting the rights of study participants
Because nursing research usually involves humans, a major nursing responsibility is to be aware of and to advocate on behalf of clients’ rights.
Before any research on humans can be started, the researcher must obtain approval from the relevant committee designated to protect human subjects’ rights- the Institutional Review Board (IRB).
The IRB ensures that all clients are informed of and understand the consequences of consenting to serve as research participants.
Elements of Informed Consent:
- Subject status
- Study purpose Sponsorship (“This study is being paid for by [name of pharmaceutical company, research grant, hospital].”)
- Subject selection (“You are being asked to take part in this study because [identify relevant subject characteristics or eligibility requirements].”)
- Study procedures, type of data to be collected
- Nature of commitment (“Taking part in this study should take no longer than [period of time].”)
- Potential risks and costs associated with participation
- Potential benefits associated with participation
- Protection of privacy
- Voluntary consent (“By signing this form, you are indicating that you are freely agreeing to take part in this study and are indicating that no one is forcing you to take part.”)
- Alternatives (If the individual is being asked to take part in a study about an experimental treatment, information must be provided about other ways in which his or her condition could be treated.)
- Right to decline to participate or to withdraw from the study; nonprejudicial treatment
- Comprehension of information
- Contact information: whom to contact with questions about the study or complaints about treatment during the course of the study
All nurses who practice in settings where research is being conducted with human subjects or who participate in such research play an important role in safeguarding their rights.
Right not to be harmed:
The risk of harm to a research subject is exposure to the possibility of injury going beyond everyday situations. The risk can be immediate or delayed and can be physical, emotional, legal, financial, or social in nature.
Right to full disclosure:
This means that deception, by either withholding information about a client’s participation in a study or giving the client false or misleading information about what participating in the study will involve, must not occur.
Right to self-determination:
Participants should feel free from constraints, coercion, or any undue influence to participate in a study.
Right to privacy:
Confidentiality means that any information a participant relates will not be made public or available to others without the participant’s consent
Nursing insights:
- All nurses need to be well-informed consumers of research and able to serve as effective research team members.
- A key responsibility for nurses who are assisting on a research team is to protect the rights of clients who are participating in the study.
Barriers to utilizing nursing research:
- Research itself: inadequate scientific base
- Practicing nurses: educational preparation with limited exposure to research utilization and resistance to change
- Organizational settings: unfavorable organizational climates and resource constraints
- Nursing profession: limited communication and collaboration between practitioners and researchers
Performance Improvement
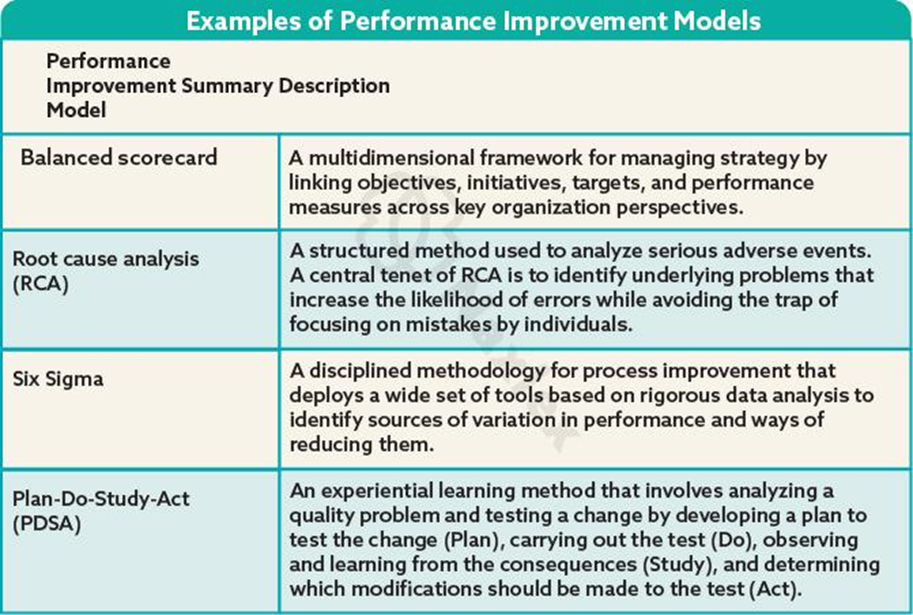
Performance improvement (PI) is a formal approach for the analysis of health care– related processes at a local level.
PI is one approach that organizations use to learn how processes can be altered to yield higher-quality care, better patient experience, and lower costs.
In many cases the same trending from PI data reveals problems that lead to EBP projects. PI projects usually occur more quickly than an EBP or research project.
An organization analyzes and evaluates current performance data to solve system problems.
Performance improvement programs
A well-organized PI program focuses on processes or systems that significantly contribute to outcomes of a specific organization, and how to sustain measurable improvements over time.
A sentinel event- an unexpected occurrence involving death or serious physical or psychological injury of a patient. After a sentinel event, the unit conducts a root cause analysis (RCA).
The goal of the RCA is to review all information and identify how the event occurred through identification of:
- active errors (i.e., the acts that personnel perform)
- why it occurred through identification and analysis of latent errors (i.e., the organization or steps of the process).
Once a committee defines the problem, it applies a formal PI model for exploring and resolving quality concerns.
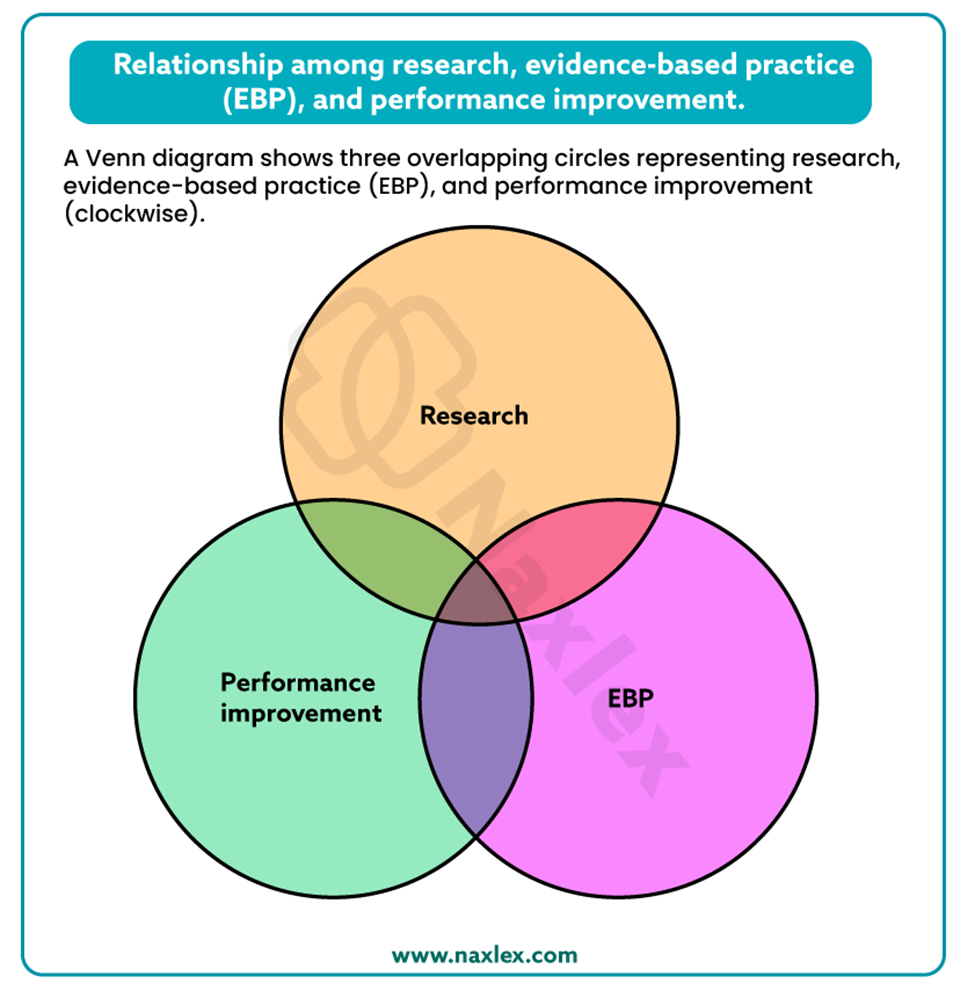
The relationship among evidence-based practice, research, and performance improvement
EBP, research, and PI are closely interrelated and exist along a continuum of clinical scholarship. All three processes require you to ultimately use the best evidence to provide the highest quality of patient care.
EBP and PI sometimes reveal problems that then create opportunities for research.
Summary
EBP promotes quality care that has been demonstrated to be effective.
The science of nursing is established by the same systematic, investigative process used by all science-based disciplines, the research process.
The five steps of the research process are:
- statement of the research problem
- delineation of a conceptual framework and review of the literature
- selection of a research design
- analysis and interpretation of the findings
- communication of the results of the research study.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Research And Evidence Based Practice In Nursing
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


