Please set your exam date
The child who is hospitalized
Study Questions
Practice Exercise 1
A nurse is caring for a 4-year-old child who is admitted to the hospital. The child states, "I am sick because I was bad." The nurse knows this statement is a characteristic of which developmental stage's coping mechanism?
Explanation
Children’s understanding of illness and their coping mechanisms are strongly influenced by their developmental stage. Nurses must interpret statements through a developmental lens to provide age-appropriate support and explanations.
Rationale for correct answer:
B. Magical thinking is characteristic of the preschool stage, where children may link unrelated events to their own actions or behavior. This belief can lead to feelings of guilt or fear about being “bad” and causing illness. Nurses should provide reassurance and simple explanations to correct misconceptions and reduce anxiety.
Rationale for incorrect answers:
A. Toddlers (1–3 years) have limited understanding of illness and are more focused on immediate needs and sensory experiences, rather than linking behavior to illness.
C. School-age children (6–12 years) think more logically and concretely; they understand cause and effect more realistically and are less likely to believe illness is punishment for behavior.
D. Adolescents are capable of abstract thinking and understand health and illness in logical, scientific terms; magical thinking is uncommon.
Take home points
- Preschoolers often demonstrate magical thinking and may feel responsible for illness.
- Nurses should reassure the child and provide clear, age-appropriate explanations about the cause of illness.
- Understanding developmental cognition helps anticipate fears, guide education, and support coping.
- This approach reduces guilt, anxiety, and stress during hospitalization.
Separation anxiety is something that affects children when they are hospitalized. Each developmental stage has a somewhat different reaction as they deal with this difficulty. Which stage corresponds to the adolescent stage?
Explanation
Separation anxiety in hospitalization varies with developmental stage. Adolescents (12–18 years) are in Erikson’s stage of identity vs. role confusion, where peers are central to emotional and social development. Hospitalization disrupts peer connections and threatens identity formation.
Rationale for correct answer:
C. Loss of peer group contact best reflects the adolescent stage. Hospitalization interrupts school, friendships, and social roles, causing anxiety, withdrawal, or rebellion. Peer acceptance is critical for adolescents’ self-concept and coping.
Rationale for incorrect answers:
A. Refusing to eat, crying quietly, continually asking for parents is more typical of preschool children, who express separation anxiety with clinginess, sadness, and visible distress.
B. Protest, despair, and detachment stages describe the toddler stage response to separation, where children first cry loudly (protest), then become withdrawn (despair), and finally show detachment if prolonged.
D. May need/desire parental guidance but unwilling to ask aligns more with school-age children, who seek security in adults but may avoid openly asking for support due to growing independence.
Take-Home Points
- Toddlers: separation anxiety shows in protest–despair–detachment stages.
- Preschoolers: cry, cling, ask for parents, show sleep/eating changes.
- School-age: may quietly need parental/adult support but hesitate to ask.
- Adolescents: peer separation is the greatest stressor, threatening identity and social belonging.
- Nursing care should provide age-appropriate support: facilitate visits, peer contact (calls, video chats), and involvement in care decisions.
The parents of a hospitalized 2½-year-old child tell the nurse and the child that they must leave the hospital to care for their children who are at home. Which of the following responses would the nurse expect the child to exhibit?
Explanation
In hospitalized toddlers, separation anxiety is common. At 2½ years old, children are in the protest stage of separation anxiety, which is often expressed through behaviors such as crying, screaming, kicking, and clinging to parents.
Rationale for correct answer:
A. Kicking and crying reflects the protest stage of separation anxiety, which is typical for toddlers when separated from parents. The child may be angry, loud, and inconsolable, showing distress over the parents’ departure.
Rationale for incorrect answers:
B. Waving goodbye is more characteristic of an older preschooler who has developed better coping mechanisms. A 2½-year-old is unlikely to calmly wave goodbye when faced with parental separation.
C. Sucking a thumb is a self-comforting behavior but is more commonly seen in the despair stage, when the child becomes quieter after prolonged separation, not immediately when parents leave.
D. Hugging a doll indicates detachment or self-comfort, seen in later stages of separation anxiety (despair or detachment), not in the immediate protest stage.
Take home points
- The protest stage involves crying, kicking, clinging, and resisting comfort from others.
- The despair stage involves withdrawal, sadness, and self-comforting behaviors (e.g., thumb-sucking, hugging a toy).
- The detachment stage may occur with prolonged separation; children seem to adjust but may show long-term attachment issues.
A 10-year-old child on a regular diet refuses to eat the food on her meal tray. She requests chicken nuggets, French fries, and ice cream. What is the best nursing action?
Explanation
School-age children (around 10 years old) are in Erikson’s stage of industry vs. inferiority. They seek independence and like to make choices but still need structure. Refusal to eat in the hospital often reflects a desire for control. Nurses should promote cooperation through negotiation and compromise rather than by giving in to demands or using punishment.
Rationale for correct answer:
B. Negotiating with the child to eat at least part of the food on the tray is the best approach because it balances the child’s need for autonomy with the nurse’s responsibility to maintain nutritional intake. Negotiation encourages cooperation, allows the child to feel some control, and ensures they still receive adequate nutrition from the hospital-approved meal.
Rationale for incorrect answers:
A. Asking that the child’s desired foods be sent up from the kitchen reinforces picky eating and gives in to demands, which undermines nutritional goals and sets an unhelpful precedent.
C. Using punishment is not therapeutic and may increase resistance, making mealtimes more stressful.
D. Offering the child cereal and milk from stock on the nursing unit bypasses negotiation and encourages food refusal by offering an easy alternative rather than teaching cooperation.
Take-Home Points
- School-age children value independence and choice, so negotiation is a useful strategy.
- Nurses should use therapeutic communication rather than punishment or indulgence.
- Nutrition in hospitalized children requires balancing medical needs with developmental understanding.
- Encouraging cooperation helps build trust and supports adherence to hospital routines.
Practice Exercise 2
A nurse is preparing a child for a blood draw in the outpatient clinic. What is the most appropriate action?
Explanation
Preparing children for procedures such as blood draws is an important nursing responsibility. Proper preparation reduces fear and anxiety, promotes cooperation, and supports a positive experience, which can influence the child’s response to future medical procedures.
Rationale for correct answer:
C. Using a treatment room ensures privacy, reduces distractions, and allows the nurse to focus on the procedure. Offering a choice of a sticker or toy afterward serves as positive reinforcement, encouraging cooperation and helping the child associate the procedure with a small reward. This method is aligned with best practices in pediatric procedural preparation and coping strategies.
Rationale for Incorrect Answers:
A. Telling the child it won’t hurt is misleading and may damage trust if the child experiences pain. Children should be given honest, age-appropriate explanations.
B. Immediately restraining the child should only be used as a last resort if other measures fail, and proper preparation is essential first.
D. While familiar surroundings may be comforting, treatment rooms are designed for safety, sterility, and privacy, making them more appropriate for procedures like blood draws.
Take home points:
- Always prepare the child honestly and use developmentally appropriate language.
- Use a designated treatment area for safety, privacy, and focus.
- Distraction and positive reinforcement (stickers, toys) reduce anxiety and improve cooperation.
- Restraints should be avoided unless absolutely necessary and always according to protocol.
The nurse providing home care to a 2-year-old listens to the child’s parents talk about how the child and family are adjusting to the child’s current illness. Which of the following roles is the nurse participating in?
Explanation
Advocacy in pediatric nursing involves listening to the concerns of children and families, supporting their needs, and ensuring their voices are heard in healthcare decisions. For a 2-year-old (toddler stage: autonomy vs. shame and doubt), family-centered care is crucial because parents are the primary decision-makers and caregivers.
Rationale for correct answer:
B. Listening to the parents’ concerns and experiences reflects advocacy, as the nurse ensures the family’s needs and perspectives are recognized in care planning. Advocacy empowers families and promotes holistic, family-centered care.
Rationale for incorrect answers:
A. Case management involves coordinating services, resources, and referrals. While important, this is not what’s happening here since the nurse is primarily listening and supporting.
C. Direct nursing care refers to hands-on clinical tasks such as administering medications, wound care, or performing assessments. Listening and discussing adjustment does not fall under direct care.
D. Child and family education involves teaching about illness, treatments, or home care. Education may occur later, but here the nurse is primarily listening and advocating, not teaching.
Take-Home Points
- Advocacy is a core nursing role, ensuring children and families have their voices included in care.
- Family-centered care emphasizes listening as much as teaching or providing direct care.
- In pediatrics, nurses support both the child’s health and the family’s coping and adjustment.
- Effective advocacy strengthens trust and improves long-term health outcomes.
Play is children’s work, even in the hospital. Which of the following are functions of play? Select all that apply
Explanation
Play is an essential part of pediatric care and is often called “the work of children.” In the hospital, play is not just recreational, it supports physical, emotional, cognitive, and social development. Therapeutic play helps children cope with illness, separation, and hospitalization while maintaining normal growth and development.
Rationale for correct answers:
A. Provides diversion and brings about relaxation: Play distracts from pain, anxiety, and medical procedures, promoting calmness.
B. Keeps the child occupied and directs concerns away from himself or herself: Play shifts focus from illness or treatments, decreasing stress.
C. Helps the child feel more secure in a strange environment: Familiar play and toys create a sense of normalcy and safety in the hospital.
D. Lessens the stress of separation and the feeling of homesickness: Play helps bridge the gap between home and hospital, reducing emotional distress.
E. Provides a means for release of tension and expression of feelings: Play is a natural outlet for emotions, especially for children who may not verbalize fears or frustrations.
Rationale for incorrect answer:
F. Allows the parents to have a break from the unit for a respite period: While this may happen as a side benefit, it is not the primary function of play for the child. The main purpose is developmental and therapeutic for the child, not parental relief.
Take-Home Points
- Play is a therapeutic tool that helps children cope with hospitalization.
- Functions of play: distraction, emotional expression, stress reduction, security, and adaptation.
- Play can be adapted by age and situation (e.g., medical play, expressive play, group play).
- Nurses should actively encourage and facilitate play as part of holistic pediatric care.
When discharging the pediatric patient from the outpatient setting, the nurse knows that which of the following responses indicate a need for more teaching? Select all that apply
Explanation
Safe pediatric discharge teaching ensures parents understand diet, medications, transportation, pain management, and follow-up. Misunderstanding instructions places the child at risk for complications at home. Nurses must confirm correct comprehension using teach-back and correct misconceptions before discharge.
Rationale for correct answers:
A. “The physician said my son can have clear liquids when we return home, which would include Jell-O, pudding, and apple juice.” Clear liquids include apple juice, broth, popsicles, and clear gelatin, but pudding is not a clear liquid because it is opaque and requires digestion. This statement shows a need for more teaching.
C. “I can get my child’s prescription tomorrow, so I can go to my regular pharmacy where they can explain the medication to me.” Prescriptions should be filled immediately after discharge so pain or infection is managed promptly. Waiting until the next day places the child at risk for uncontrolled symptoms.
Rationale for incorrect answers:
B. “I can use other things to help with the pain, such as distraction (reading a book, music, or a movie), after the pain medication is given.” Nonpharmacologic interventions like distraction, relaxation, and play are encouraged alongside pain medication.
D. “I am waiting for my husband to come so he can drive us, and I can watch my son in the car on the way home.” A post-op child should not be driven home by the caregiver alone if they need to monitor the child; having another adult to drive is appropriate.
E. “I understand that I will be contacted tomorrow for follow-up on my child but that I should not hesitate to call if I have any concerns before then.” This demonstrates proper follow-up expectations and awareness of when to seek help.
Take-Home Points
- Clear liquids = transparent fluids only (apple juice, broth, gelatin, popsicles); not pudding or milk-based items.
- Prescriptions must be filled immediately to prevent complications.
- Discharge teaching should always use clear language and teach-back to check understanding.
- Safe transport and proper follow-up are key aspects of pediatric discharge planning.
You tell the parent of a 4-year-old patient being admitted that you need to ask some questions. She asks, “Why do you have to ask so many questions?” Which explanations should you offer? Select all that apply
Explanation
When admitting a pediatric patient, nurses ask parents detailed questions to gather information about the child’s health history, routines, medications, and psychosocial background. This helps create a safe and supportive care plan, reduces stress from hospitalization, and fosters family-centered care.
Rationale for correct answers:
A. “It is something we are required to do for every child who is hospitalized.” Admission assessments are standard for all pediatric patients to ensure safety and quality care.
B. “By learning about your child’s routines, we can try to minimize some of the changes he will be going through.” Maintaining familiar routines reduces stress, anxiety, and separation distress during hospitalization.
D. “Gaining more information about your child, such as current medications she is taking, will help us provide the best care.” Accurate information prevents medication errors and ensures safe, individualized care.
E. “This will give you an opportunity to ask questions as well.” Admission interviews are two-way; they provide time for parents to clarify concerns and improve communication with staff.
Rationale for incorrect answer:
C. “Knowing more about your child can help predict how the hospital stay will go and will also help us choose a good roommate for him when more children arrive at the hospital.” While knowing the child better improves care, roommate selection is not the main purpose of the admission questions, and this response could appear unprofessional or irrelevant.
Take-Home Points
- Pediatric admission interviews are essential for safety, continuity of care, and emotional support.
- Information gathered includes health history, medications, routines, coping strategies, and family needs.
- Nurses should explain the purpose clearly to build trust and collaboration with parents.
- The process also opens space for parents to ask questions and share concerns.
Practice Exercise 3
A nurse is preparing to administer an oral medication to a 2-year-old child. What is the most appropriate nursing action?
Explanation
Safe and accurate medication administration is a critical nursing responsibility in pediatrics. Children, especially toddlers, have smaller body size and immature organ systems, making precise dosing essential. Proper technique and developmentally appropriate strategies help ensure effectiveness and safety.
Rationale for correct answer:
C. Using a calibrated oral syringe is the most accurate and safe method for delivering liquid medications to young children. Administering into the side of the mouth reduces the risk of choking and ensures the full dose is received.
Rationale for incorrect answers:
A. The child may not finish the bottle of milk, leading to underdosing, and the medication may alter the taste, causing refusal. Always use a small amount of food or liquid if necessary.
B. Bribery can create negative associations with medications and is not a reliable long-term strategy. Positive reinforcement should be developmentally appropriate (e.g., stickers).
D. Holding the child's nose is incorrect and unsafe. Forcing medication in this way can cause trauma, increase anxiety, and risk aspiration.
Take home points
- Use a calibrated oral syringe for accurate dosing of liquid medications in children.
- Administer into the side of the mouth slowly to prevent choking.
- Avoid mixing medication in large amounts of food or drink.
- Never force or restrain a child unnecessarily to give oral medications.
A 6-month-old infant requires restraint to prevent removal of his nasogastric tube. What is the priority nursing intervention?
Explanation
Infants requiring nasogastric (NG) tubes are at risk of accidental removal if left unrestrained, but restraints also carry risks such as impaired circulation, skin breakdown, and delayed development. The nurse’s priority is safety with the least restrictive intervention.
Rationale for correct answer:
B. Leaving the baby unrestrained when directly observed is the safest and most appropriate nursing action. Continuous direct observation allows the infant freedom of movement while ensuring the NG tube remains secure. Restraints should only be used when absolutely necessary and discontinued as soon as possible.
Rationale for incorrect answers:
A. A loosely tied restraint is unsafe because the infant could remove it, slip out, or accidentally wrap it around themselves. Proper restraint application is important, but priority is to avoid restraint if supervision is available.
C. The prone position increases the risk of suffocation and aspiration, especially in infants. Supine or side-lying positions are safer.
D. Placing the infant in a room near the nurses’ station improves monitoring but is not equivalent to direct observation. The infant could still remove the NG tube if left unattended.
Take-Home Points
- Use least restrictive interventions first; restraints are a last resort.
- Direct supervision is preferred over restraints for infants.
- If restraints are necessary, monitor circulation, skin integrity, and comfort frequently.
- Safe positioning (supine or side-lying) is essential to reduce aspiration and suffocation risk.
When administering a medication to a child, the nurse knows that:
Explanation
Safe medication administration in children requires precise measurement because even small errors can lead to underdosing or toxicity due to their smaller body size and immature organ systems. Household measures like teaspoons are unreliable, and the nurse should use standardized, calibrated devices for accuracy.
Rationale for correct answer:
A. Plastic disposable calibrated oral syringe is the most accurate method for measuring small doses of liquid medications for infants and children. It allows for precise dosing, especially in milliliters (mL), and avoids the inconsistencies of household spoons.
Rationale for incorrect answers:
B. Household teaspoons vary widely in volume (from 3–7 mL), making them unsafe for medication dosing. Parents should always be instructed to use calibrated syringes or dosing cups.
C. Droppers are less accurate than oral syringes, especially for viscous medications or doses larger than 1 mL.
D. Medicine cups are not reliable for very small doses, as accuracy decreases when measuring less than 5 mL.
Take-Home Points
- Always use oral syringes for pediatric liquid medications, especially for doses <5 mL.
- Household spoons should never be used for dosing.
- Medication safety in pediatrics relies on accuracy, clear labeling, and parent teaching.
- Nurses should teach families proper use of oral syringes to prevent dosing errors at home.
During hospitalization, there may be a reason to use restraints. Protocol for using restraints may include which of the following? Select all that apply
Explanation
Restraints in children are methods used to limit movement temporarily to ensure safety during medical care. They are only used when absolutely necessary and must follow strict ethical and clinical guidelines.
Rationale for correct answers:
A. One finger breadth and quick-release knots prevents impaired circulation and allows for rapid removal in emergencies. Essential for safety and skin integrity.
B. Elbow restraints are common after cleft lip/palate surgery to prevent the child from touching or traumatizing the surgical site. Effective and safe when monitored.
C. Papoose board/mummy wrap are useful for short procedures, especially head/neck exams, to ensure safety and prevent accidental injury. Should be limited to short durations.
D. Assessment before behavioral restraints is a critical step to determine whether behavior is due to unmet needs (pain, fear, environment) before applying restraints. Ensures restraints are the last resort.
Rationale for incorrect answers:
E. Unless state laws is more restrictive, behavioral restraints for children must be reordered every 15 minutes for a personal restraint, every 1 hour for children under 9 years of age, and every 2 hours for children 9 to 17 years old; orders for adults 18 and older are required every 4 hours.
Take home points
- Restraints in children should only be used as a last resort after other measures fail.
- Always leave one finger breadth between skin and restraint; use quick-release knots for safety.
- Follow age-specific time limits and legal requirements for restraint reorders.
- Continuous monitoring of skin integrity, circulation, respiratory status, and emotional well-being is mandatory.
A. The nurse is preparing a 5-year-old boy for surgery on his lower leg. His mother is helping him into the hospital gown and the boy fights removal of his underwear. What is the most appropriate nursing action?
Explanation
Children, especially around age 5, often have modesty concerns and a strong desire for autonomy. Preparing a child for surgery should minimize stress and anxiety while maintaining safety. Unless contraindicated for the procedure, allowing the child to keep underwear on provides comfort and supports emotional well-being.
Rationale for correct answer:
D. Allowing the boy to keep his underwear on is the most appropriate action. It respects the child’s need for modesty, reduces preoperative anxiety, and still allows for safe surgical preparation since the underwear can typically remain until the time of surgery. Nursing care should support both emotional and physical needs.
Rationale for incorrect answers:
A. Allowing the mother to remove the underwear may escalate the child’s distress and increase resistance, worsening anxiety rather than providing comfort.
B. Telling the boy he is acting childishly is dismissive, non-therapeutic communication that invalidates the child’s feelings and could damage trust.
C. Notifying the OR that the underwear is on is unnecessary at this stage and does not address the child’s immediate emotional needs. The OR staff will ensure proper removal when required.
Take home points
- Respecting a child’s modesty helps reduce anxiety before surgery.
- Therapeutic communication and comfort measures are crucial in pediatric nursing care.
- Preoperative preparation should balance emotional reassurance with procedural safety.
- Children should be given as much control as possible within safe limits to promote cooperation.
Comprehensive Questions
You are working with a new nurse to give an intramuscular injection. Which principles do you want to include when doing this teaching? Select all that apply
Explanation
Intramuscular (IM) injections are a method of delivering medication directly into a muscle, where it’s absorbed quickly into the bloodstream due to the muscle’s rich vascular supply.
Rationale for correct answers:
B. Studies show that vaccines given at the ventrogluteal site have fewer local reactions such as redness and swelling, and systemic side effects such as fever, making it a safe and effective site.
C. Having the child supine on a parent’s lap provides comfort, distraction, and physical control, reducing the risk of sudden movements that could cause injury.
D. In older children, the deltoid muscle may be associated with less pain and fewer side effects compared with vastus lateralis, though it is not typically used in infants due to limited muscle mass.
Rationale for incorrect answers:
A. For small infants, volumes should actually be lower such as 0.5–1 mL. Thus, this option is less universally correct in pediatrics compared to the chosen answers.
E. Aspiration is not recommended during vaccine administration. It causes unnecessary pain and is not needed since recommended injection sites for children do not have large blood vessels at risk.
Take home Points
- Ventrogluteal site is increasingly supported for vaccines due to fewer reactions and good muscle depth.
- Parent lap positioning is both comforting and a safety measure to prevent movement.
- Deltoid site is appropriate for older children/adolescents and may cause less discomfort than vastus lateralis in some cases.
- Injection volumes must always be adjusted to the child’s age and muscle size (infants ≤1 mL, older children up to 2 mL per site).
The nurse is assessing whether or not an 8-year-old child has given assent for a scheduled painful procedure. Which of the following statements by the child would reflect that the child has given assent?
Explanation
Assent is the child’s affirmative agreement to the procedure. It means the child understands, in their developmental capacity, what will happen and why, and expresses willingness to proceed.
Rationale for correct answer:
B. “The procedure is going to be done at 10 a.m. this morning.” This statement shows the child understands what is happening and when it will occur. It reflects awareness and agreement, which is age-appropriate for an 8-year-old.
Rationale for incorrect answers:
A. “I know that the procedure is supposed to make me better.” While this reflects some understanding of why the procedure is being done, it does not confirm the child’s willingness or agreement to undergo it.
C. “Dr. Jones wants to perform the procedure on me.” This reflects awareness of who is performing the procedure, but it does not demonstrate the child’s assent.
D. “My mother signed the form that the doctor brought in.” This reflects parental consent, not the child’s assent. The parent has the legal authority to consent, but assent still requires the child’s understanding and willingness.
Take home points
- Consent is the legal, by parent/guardian.
- Assent involves:
- Basic understanding of the procedure.
- Awareness of its purpose/benefit.
- Voluntary agreement (without coercion).
- Nurses play a key role in ensuring that assent is sought when appropriate, even if legal consent is already given by parents.
Children and adolescents should be prepared for procedures according to their level of development and understanding. Which interventions by the nurse would be helpful? Select all that apply
Explanation
Preparing children and adolescents for medical procedures is an essential part of pediatric nursing care. Since each developmental stage brings different levels of understanding, fears, and coping abilities, nurses must tailor their approach accordingly.
Rationale for correct answers:
A. Children understand best when information is concrete. Describing what they will see, hear, taste, smell, and feel reduces fear and prepares them realistically.
D. As children grow older, modesty becomes very important, especially for school-age children and adolescents. Explaining how their body will be covered shows respect, maintains dignity, and reduces anxiety.
Rationale for Incorrect Answers:
B. While infants may not consciously remember painful experiences, they do experience stress responses and can develop negative associations. Thus, this is not a recommended teaching point.
C. While school-aged children need clear explanations, too much advance time can increase anxiety and rumination. Preparation is most effective closer to the procedure.
E. Peer support often reduces anxiety by normalizing experiences and providing reassurance.
Take home points
- Use sensory-based explanations to help children anticipate and cope with procedures.
- Respect privacy and modesty, especially in older children/adolescents.
- Adolescents often benefit from peer support and opportunities to ask questions.
- Preparation should always be honest, developmentally appropriate, and supportive to minimize fear.
The nurse is developing a plan of care to prevent separation behaviors in children who are hospitalized for long periods of time. Which of the following items should the nurse include in the plan of care? Select all that apply
Explanation
Separation behaviors in children hospitalized for extended periods often reflect their emotional response to being away from familiar caregivers, routines, and environments. These behaviors vary by developmental stage but they all result in distress from disrupted attachment and loss of control.
Rationale for correct answers:
A. Provide the child with the child’s favorite transitional object: Transitional objects (blankets, stuffed animals, dolls) provide comfort, familiarity, and security in the hospital environment, helping reduce anxiety related to separation.
B. When possible, assign the same nurse to care for the child each day: Consistency of caregivers fosters trust and security, reducing feelings of abandonment and fear of strangers.
D. Tape pictures of the child’s friends and family members to the walls of the child’s hospital room: Familiar images help the child feel connected to loved ones, reducing separation distress and promoting a sense of security.
Rationale for incorrect answers:
C. Admit the child to the patient room that is closest to the nurse’s station: While this increases staff observation, it does not reduce separation behaviors. Proximity to nurses does not replace parental presence or emotional comfort.
E. Inform the parents that at least one person must stay with the child at all times during the hospitalization: While encouraging parental presence is beneficial, making it a requirement is unrealistic and may place undue stress on families who have other obligations (work, siblings, etc.). Instead, flexible visitation policies and supportive measures should be encouraged.
Take home points
- Key strategies to prevent separation distress in hospitalized children include transitional objects, consistent caregivers, and family photos.
- Parental presence is valuable, but nursing care plans should support families without imposing unrealistic expectations.
- Nurses play a central role in promoting continuity, familiarity, and emotional security to minimize long-term effects of separation anxiety.
The nurse is caring for a 14-year-old adolescent after a serious injury. A twice-daily dressing change has been ordered by the child’s primary health-care provider. When planning care with the patient, which of the following statements would be best for the nurse to make?
Explanation
Adolescents are in Erikson’s stage of identity vs. role confusion and have a strong need for independence, autonomy, and control over their environment.
Rationale for correct answer:
B. “When do you think will be the best times for me to change your dressing?” Allowing the adolescent to help determine the schedule supports their developmental need for control, fosters cooperation, and builds trust in the nurse–patient relationship.
Rationale for incorrect answers:
A. “I’ll be in to change your dressing twice today.” This is authoritative and gives the adolescent no control or input, which may increase resistance and frustration.
C. “I’m going to have you help me when I change your dressing.” While involving the adolescent is good, this statement does not address their need to have a say in planning their care. It is directive, not collaborative.
D. “Can you help me to figure out how best to change your dressing?” This may be overwhelming and unrealistic. The adolescent is not expected to know how best to perform the procedure; that’s the nurse’s responsibility.
Take home points
- Adolescents value independence and participation in their care.
- Nurses should encourage shared decision-making (e.g., timing, comfort measures) while maintaining professional responsibility for safe care.
- Involving adolescents in planning care improves compliance, trust, and self-esteem.
- Effective communication balances nurse expertise with adolescent autonomy.
An 8-year-old child, who is post-op appendectomy, is playing with a set of building blocks. The child’s pulse and blood pressure are slightly elevated above their presurgery levels. When asked what level the child would rate the postoperative pain on a numeric pain scale, the child states that the pain is “8 on a scale of 1 to 10.” The child’s primary health-care provider has ordered Tylenol (acetaminophen) and morphine sulfate for pain. Which of the following actions should the nurse perform at this time?
Explanation
Pain control post-surgery refers to the strategies and treatments used to manage discomfort and promote healing after a surgical procedure. It’s a critical part of recovery that affects mobility, emotional well-being, and risk of complications.
Rationale for correct answer:
C. Administering morphine to the child based on the child’s rating of the pain is correct. The gold standard for pain assessment is the child’s self-report, as long as the child is developmentally capable of using a numeric pain scale (which an 8-year-old is). Even though the child appears to be playing, this does not negate the reported pain score. Children can sometimes distract themselves with play but still experience significant pain.
Rationale for incorrect answers:
A. Reporting the child’s pain level to the child’s primary health-care provider is not necessary at this point. The provider has already prescribed pain medications, and the nurse has the autonomy to administer them according to the child’s needs.
B. Administering acetaminophen to the child based on the child’s behavior undermines the child’s self-report. Behavior (playing) is not always a reliable indicator of pain severity. Acetaminophen alone would likely be insufficient for reported severe pain.
D. Querying the child about how the child is able to play with such severe pain could make the child feel disbelieved or dismissed. Nurses should validate, not question, the child’s reported pain level.
Take home points
- Self-report is the most reliable indicator of pain in children who can use numeric or other validated pain scales.
- Children may still engage in play despite experiencing significant pain.
- Nurses should trust the child’s pain rating and treat accordingly.
- Opioids like morphine are indicated for severe postoperative pain, while acetaminophen may be used for mild pain or as part of multimodal therapy.
An 8-year-old child, who is post-op appendectomy, is playing with a set of building blocks. The child’s pulse and blood pressure are slightly elevated above their presurgery levels. When asked what level the child would rate the postoperative pain on a numeric pain scale, the child states that the pain is “8 on a scale of 1 to 10.” The child’s primary health-care provider has ordered Tylenol (acetaminophen) and morphine sulfate for pain. Which of the following actions should the nurse perform at this time?
Explanation
Pain control post-surgery refers to the strategies and treatments used to manage discomfort and promote healing after a surgical procedure. It’s a critical part of recovery that affects mobility, emotional well-being, and risk of complications.
Rationale for correct answer:
C. Administering morphine to the child based on the child’s rating of the pain is correct. The gold standard for pain assessment is the child’s self-report, as long as the child is developmentally capable of using a numeric pain scale (which an 8-year-old is). Even though the child appears to be playing, this does not negate the reported pain score. Children can sometimes distract themselves with play but still experience significant pain.
Rationale for incorrect answers:
A. Reporting the child’s pain level to the child’s primary health-care provider is not necessary at this point. The provider has already prescribed pain medications, and the nurse has the autonomy to administer them according to the child’s needs.
B. Administering acetaminophen to the child based on the child’s behavior undermines the child’s self-report. Behavior (playing) is not always a reliable indicator of pain severity. Acetaminophen alone would likely be insufficient for reported severe pain.
D. Querying the child about how the child is able to play with such severe pain could make the child feel disbelieved or dismissed. Nurses should validate, not question, the child’s reported pain level.
Take home points
- Self-report is the most reliable indicator of pain in children who can use numeric or other validated pain scales.
- Children may still engage in play despite experiencing significant pain.
- Nurses should trust the child’s pain rating and treat accordingly.
- Opioids like morphine are indicated for severe postoperative pain, while acetaminophen may be used for mild pain or as part of multimodal therapy.
To enhance the effectiveness of the pharmacological pain intervention administered to a 4-year-old child with an injured knee, the nurse plans to add a nonpharmacological pain intervention. Which of the following actions would be appropriate for the nurse to perform? Select all that apply
Explanation
Nonpharmacological pain interventions in children are non-drug strategies used to reduce pain, anxiety, and distress, especially during medical procedures or recovery. These approaches are developmentally tailored, often family-centered, and can be just as powerful as medications when used appropriately.
Rationale for correct answers:
A. Distraction through storytelling and reading a book to the child engages the child’s attention and helps divert focus away from pain.
B. Comforting touch and physical closeness such as cuddling provide security and reduce anxiety, which enhances pain relief.
C. Cold therapy reduces inflammation, numbs pain, and is an appropriate adjunct for musculoskeletal injuries in children.
D. Distraction via television provides sensory engagement, diverting attention from pain and supporting the pharmacological intervention.
Rationale for incorrect answer:
E. Performing passive range of motion exercises on the injured knee is inappropriate during acute injury and pain because it can worsen pain, aggravate tissue damage, and delay healing. Movement should only be initiated when prescribed during rehabilitation, not as an immediate comfort measure.
Take home points
- Nonpharmacological pain interventions for children include distraction (books, TV, play), comfort (cuddling, holding), and physical measures (ice/heat as appropriate).
- These interventions are adjuncts to medication and can reduce the required analgesic dose.
- Avoid interventions that exacerbate pain or cause harm, such as unnecessary movement of the injured area.
- Combining pharmacological and nonpharmacological approaches is best practice in pediatric pain management.
An 8-year-old child is in the playroom drawing a picture. The child’s painful dressing change is due to be performed. Which of the following actions by the nurse is appropriate?
Explanation
Pain is a complex sensory and emotional experience that signals actual or potential harm to the body. Pain can exist without visible injury. It’s influenced by past experiences, emotions, and environment. It is subjective hence only the person experiencing it can truly describe its intensity and impact.
Rationale for correct answer:
C. Painful or stressful procedures should not be performed in the child’s playroom or hospital bed. The playroom should remain a safe, positive environment for coping and distraction. Performing the procedure in a designated treatment room preserves the child’s sense of security and allows the playroom to remain associated with fun and comfort. Escorting the child back afterward helps re-establish normalcy and security.
Rationale for incorrect answers:
A. Delaying procedures unnecessarily can interfere with treatment schedules and may prolong anxiety.
B. Performing the dressing change in the playroom while the child finishes drawing the picture is inappropriate. The playroom must remain a safe space for positive experiences; painful procedures should never be done there.
D. Offering choices is good in pediatric care, but in this case the timing of the dressing change is a medical necessity. Giving the child this option may create false expectations or resistance.
Take home points
- Never perform painful procedures in a child’s playroom or hospital bed, these spaces should be safe, comforting zones.
- Use a treatment room for procedures to help children cope better with hospitalization.
- Escorting the child back to play afterward helps restore a sense of normalcy and reduces trauma.
- Offer choices only when appropriate (e.g., which arm for a blood pressure cuff), but not when the procedure’s timing is medically necessary.
A nurse has been assigned to care for a 12-year-old child who will likely die from his illness. The child asks the nurse, “Do you think I am going to die?” Which of the following responses would be appropriate for the nurse to make?
Explanation
When caring for children with life-threatening or terminal illnesses, nurses often face difficult questions about death. School-age children, around 12 years old, understand that death is final and irreversible, and they seek honest, empathetic answers.
Rationale for correct answer:
C. “Some children who have been diagnosed with your illness do die.” This response is honest, developmentally appropriate, and empathetic. At age 12, children in the concrete–formal operational stage (Piaget) understand that death is permanent and universal. They deserve truthful answers. The nurse’s role is to provide open, supportive communication, allowing the child to express fears, feelings, and questions while fostering trust.
Rationale for incorrect answers:
A. “Don’t talk like that. You are going to get better very soon.” This is false reassurance and invalidates the child’s feelings and undermines trust.
B. “It would be best if you were to ask your doctor about that.” This avoids the child’s question, shuts down communication, and conveys that the nurse is uncomfortable discussing important concerns.
D. “It’s hard for me to talk about death. It would be best if you were to ask your parents.” This focuses on the nurse’s feelings instead of the child’s. This avoidance leaves the child unsupported and isolated with their fears.
Take home points
- Children around 10–12 years old understand the permanence of death and may ask direct questions.
- The nurse should respond with honesty, empathy, and openness, validating the child’s feelings while providing comfort.
- Avoid false reassurance or deflection, these erode trust and increase anxiety.
- Facilitating discussions with parents, providers, and chaplains may also help, but the nurse should not avoid the child’s direct questions.
A 7-year-old child, who must have a lumbar puncture, begins to cry and squirm when the nurse advises him that he must lie curled on his side with his back facing the primary health-care provider. Which of the following actions should the nurse perform at this time?
Explanation
When preparing children for invasive procedures such as a lumbar puncture, it is essential for the nurse to use developmentally appropriate communication and strategies. The nurse’s priority is to ensure safety, cooperation, and emotional support while avoiding threats, shaming, or placing the burden solely on parents.
Rationale for correct answer:
C. A lumbar puncture requires absolute immobility to avoid injury and obtain an accurate sample. A 7-year-old may understand instructions but can still become fearful and unable to stay still on their own. The safest approach is for the nurse to request help so the child can be gently but firmly held in the correct position, ensuring safety and comfort.
Rationale for incorrect answers:
A. While immobility is critical, threatening the child with possible injury increases fear and does not provide supportive guidance.
B. Parents can offer comfort, but the nurse cannot rely solely on them to manage positioning during such a critical and invasive procedure.
D. Telling the child that children who are in elementary school are big enough to be still during procedures dismisses the child’s fear and is developmentally inappropriate. Guilt or shame is not an effective strategy for cooperation.
Take home points
- During invasive procedures like a lumbar puncture, safety and immobility are top priorities.
- The nurse should provide age-appropriate explanations, use comforting techniques, and ensure adequate assistance for positioning.
- Avoid threatening, shaming, or relying only on parents to maintain control — professional staff support is essential.
- A calm, supportive approach helps reduce fear while keeping the procedure safe.
An 18-month-old child has just returned from the operating room with intravenous solution running into a vein in the right hand, a nasogastric tube in place, and a dressing covering the abdomen. Which of the following actions by the nurse would be appropriate? Select all that apply
Explanation
Postoperative care for toddlers requires close monitoring of safety, fluid balance, pain control, and equipment management. Since 18-month-old children are active and curious, they may try to pull at tubes or IV lines, so nurses must anticipate needs and prevent complications.
Rationale for correct answers:
B. Accurate I&O monitoring is essential for a post-op child with IV fluids and an NG tube to assess hydration, kidney function, and fluid balance.
C. An elbow restraint prevents the child from pulling out the NG tube or IV line or interfering with the abdominal dressing. Always requires a provider’s order. A nurse cannot apply it independently.
D. At 18 months, the child cannot use a numeric scale. The nurse should use a validated tool such as the FLACC (Face, Legs, Activity, Cry, Consolability) scale to assess pain.
E. Safe practice requires verification of IV solution and rate against the provider’s orders before continuing infusion. This prevents medication or fluid errors.
Rationale for incorrect answers:
A. NSAIDs are not typically first-line in immediate post-op care for an 18-month-old with abdominal surgery due to risk of bleeding and gastric irritation. Stronger analgesics (opioids, acetaminophen IV/PO) are often ordered instead.
Take home points
- Post-op care for toddlers focuses on safety (verify orders), comfort (age-appropriate pain assessment), and monitoring (I&O, vital signs, wound care).
- Pain assessment tools must be developmentally appropriate (e.g., FLACC scale for infants and toddlers).
- NSAIDs are not routine post-op measures and require careful consideration of risks and alternatives.
- Nurses should always double-check IV solutions against provider orders to prevent errors.
A 5-month-old girl’s arms are encased in elbow restraints following facial surgery. Which of the following situations would warrant removal of the restraints?
Explanation
Elbow restraints are commonly used in infants after facial or cleft palate surgery to prevent them from touching or disrupting the operative site. However, restraints should never be used continuously; they must be removed periodically to allow for skin checks, circulation assessment, range of motion, and bonding with caregivers.
Rationale for correct answer:
D. The purpose of elbow restraints after facial surgery (e.g., cleft lip/palate repair) is to prevent the infant from touching or disrupting the operative site. Restraints should only be used when necessary, and they should be removed when a responsible adult can directly supervise and protect the child. This reduces risk of complications while allowing the infant comfort, mobility, and bonding time.
Rationale for incorrect answers:
A. Pain relief does not eliminate the risk of the infant reaching for or rubbing the operative site. Restraints are still necessary unless directly supervised.
B. Even while asleep, infants may reflexively move their hands to their mouth or face, risking injury to the surgical site. Restraints must remain in place if the infant is unsupervised.
C. The infant’s hands being pink with spontaneous movement and capillary refill of two seconds indicates good circulation and neurovascular status, which is important to monitor while restraints are on, but it is not a reason for removal.
Take home points
- Elbow restraints are used post-facial surgery to protect the operative site.
- They should be removed only when a responsible adult is directly supervising the infant and preventing self-injury.
- Nurses must perform regular neurovascular checks (color, warmth, movement, sensation, cap refill) to ensure restraint safety.
- Restraints should be used as minimally as possible and alternated with supervised periods of freedom to promote comfort and bonding.
A 13-year-old adolescent is in hospital for reconstructive surgery after a severe automobile accident. During rounds, the nurse notes that the teen is watching television and playing a video game. Which of the following should the nurse assess regarding the patient’s well-being? Select all that apply
Explanation
Adolescents recovering from surgery face not only physical healing but also psychological and social challenges. The nurse must focus on clinical and developmental priorities such as pain management, wound healing, and psychosocial support, such as peer connections.
Rationale for correct answers:
A. Teen’s pain level is always a priority in postoperative care. Even if the adolescent appears engaged in TV or games, pain may still be present. Self-report remains the gold standard for pain assessment.
B. Socialization is very important for adolescents. According to Erikson’s psychosocial stage (identity vs. role confusion), peer support directly affects self-esteem and coping during hospitalization.
C. Level of healing of the teen’s surgical site is essential to evaluate wound healing, risk of infection, and overall recovery progress after reconstructive surgery.
D. Academic progress should be included in a holistic nursing assessment of adolescents. School work provides normalcy, supports developmental tasks, and helps maintain a sense of routine and achievement. It is part of psychosocial well-being, not just physical health.
Rationale for incorrect answer:
E. How well the teen is performing on the video games is not a relevant measure of health or recovery. Games are simply a distraction tool and a coping mechanism.
Take home points
- Nursing care for adolescents must be holistic:
- Physical including pain and wound healing
- Emotional/Social including peer and family support
- Developmental/Academic including school progress, independence
- Maintaining normal routines such as schoolwork helps adolescents cope with hospitalization and prepares them for reintegration post-discharge.
- Distractions like games are useful coping tools but are not indicators of well-being.
A child is to undergo a tympanostomy tube placement in a freestanding outpatient surgery center. What is the major disadvantage associated with this location?
Explanation
A tympanostomy tube placement is a minor outpatient procedure typically done in children with recurrent otitis media. Freestanding outpatient surgery centers, also known as ambulatory surgical centers (ASCs), are independent medical facilities designed specifically for same-day surgical procedures that don’t require an overnight hospital stay.
Rationale for correct answer:
C. Freestanding centers do not have the capacity for inpatient admissions. This is the major disadvantage compared to hospital-based surgery centers, as unplanned transfers delay continuity of care and increase risks in case of complications.
Rationale for incorrect answers:
A. Outpatient centers actually have lower infection risks compared to hospitals due to shorter stays and reduced exposure to hospital-acquired infections.
B. Care at outpatient centers is usually less expensive, making this an advantage rather than a disadvantage.
D. Outpatient centers allow same-day discharge, which reduces family disruption, making this incorrect.
Take-Home Points
- Main disadvantage of freestanding surgery centers: inability to provide overnight care, requiring transfer if complications arise.
- Outpatient centers are generally safe, cost-effective, and less disruptive for families.
- Nurses should educate parents about possible transfer needs and what to expect in the rare event of complications.
- Preoperative and postoperative planning should always consider the setting’s limitations.
While orienting a new nurse to the ICU, she asks, “How do these children sleep and not become frightened with all the lights and noises?” How should you respond? Select all that apply
Explanation
Children in the ICU are exposed to continuous stimuli from lights, alarms, and procedures, which can disrupt sleep and increase fear or anxiety. Promoting rest, comfort, and family presence helps protect sleep cycles, reduces stress, and supports healing. Nurses play a key role by clustering care, minimizing disturbances, and encouraging parental involvement.
Rationale for correct answers:
B. “We try to organize care into clusters so that infants and children can sleep and we can turn down lights.” Clustering care minimizes interruptions, and dimming lights helps mimic normal circadian rhythms.
D. “When possible, we allow for uninterrupted sleep cycles—for infants 90 minutes and for older children 60 minutes.” Preserving natural sleep cycles supports growth, healing, and emotional regulation.
E. “We encourage parents to sit with and touch their child as often as possible.” Parental presence provides comfort, reduces fear, and helps normalize the ICU environment for children.
Rationale for incorrect answers:
A. “These children are sicker than those on the pediatric unit, so the noises and lights are necessary.” While monitoring is necessary, this response is dismissive and does not explain strategies used to reduce stress and promote sleep.
C. “We silence alarms to allow for periods of sleep, especially at night.” Alarms are safety-critical and must never be silenced; instead, noise reduction strategies such as closing doors and reducing unnecessary sounds are used.
Take-Home Points
- Promote sleep in pediatric ICUs by clustering care, dimming lights, and respecting natural sleep cycles.
- Parental presence is therapeutic and reduces children’s fear in stressful environments.
- Never silence safety alarms—instead, minimize noise through environmental control.
- Protecting rest is essential for healing, immune function, and emotional stability in critically ill children.
Exams on The child who is hospitalized
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Stressors of Hospitalization and Children’s Reactions
- Stressors and Reactions of the Family of the Child Who Is Hospitalized
- Practice Exercise 1
- Nursing Care of the Child Who Is Hospitalized
- Nursing Care of the Family
- Care of the Child and Family in Special Hospital Situations
- Practice Exercise 2
- Practice Exercise 3
- Pediatric nursing Interventiona and skills
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Analyze the primary stressors of hospitalization for children, specifically separation anxiety, loss of control, and fear of bodily injury.
- Evaluate the three stages of separation anxiety (protest, despair, and detachment) across different developmental levels.
- Identify the psychosocial impact of hospitalization on family dynamics, including parental guilt and sibling jealousy or resentment.
- Formulate nursing interventions to minimize the "loss of control" by promoting autonomy and maintaining home-like routines.
- Develop age-appropriate preparation strategies for children undergoing procedures in ambulatory, emergency, and intensive care settings.
- Apply the principles of family-centered care by encouraging parent participation and providing clear, consistent information.
- Calculate and safely administer pediatric medications via various routes, ensuring the "six rights" are adapted for childhood physiology.
- Prioritize safety and skin integrity through the use of developmentally appropriate restraints, hygiene practices, and procedural positions.
Introduction
- Caring for children in diverse clinical settings requires the nurse to move beyond technical proficiency and into the realm of psychological advocacy.
- Whether in an outpatient clinic, an emergency department, or an intensive care unit, the environment is inherently stressful for a child. This stress is primarily driven by three factors such as separation anxiety, loss of control, and fear of bodily injury.
- Separation anxiety is most acute in toddlers, manifesting in predictable stages that the nurse must recognize to provide comfort.
- Loss of control occurs when the child’s familiar routines are replaced by the rigid protocols of a hospital, leading to feelings of powerlessness.
- Fear of bodily injury is often exacerbated by the child’s cognitive developmental stage, such as the preschooler's "magical thinking" where a small bandage is seen as holding their insides together.
- The nurse’s role begins with an admission assessment that treats the child and family as a single unit.
- Preparation for hospitalization should be a proactive process, utilizing therapeutic play and developmentally appropriate language to demystify the experience.
- In special situations, such as isolation or the high-stimulus environment of the ICU, the nurse must work double-duty to maintain the child’s sense of security while managing complex medical interventions.
- By providing opportunities for play and expressive activities, the nurse helps the child process the trauma of illness, turning a potentially negative event into an opportunity for mastery and growth.
- The nurse must navigate the legal and clinical complexities of pediatric procedures and medication administration. From determining precise dosages based on weight to selecting the correct needle gauge for intramuscular injections, the margin for error is slim.
- Safety is paramount, involving not just the physical prevention of falls, but the emotional safety of the child during painful procedures.
- By integrating family-centered principles with advanced clinical skills, the nurse ensures that the child’s physical recovery is matched by their emotional resilience.
Stressors of Hospitalization and Children’s Reactions
- Hospitalization disrupts a child's familiar routine, environment, and social connections, leading to significant stress. The three major stressors are separation anxiety, loss of control, and fear of bodily injury and pain.
3.1 Separation Anxiety
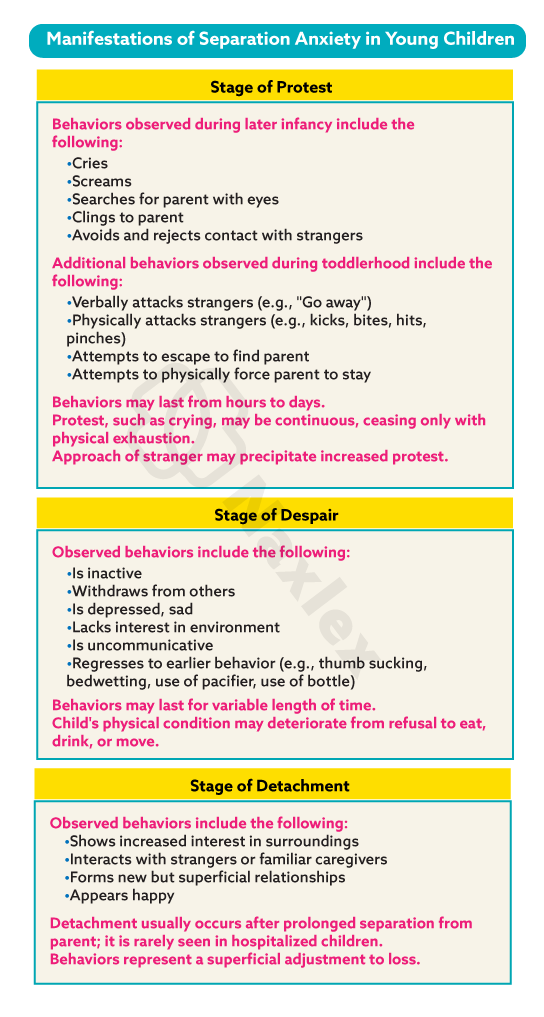
Separation anxiety is a major stressor for young children (6 months to 30 months) and is the most significant. It occurs when a child is separated from their primary caregiver and home environment. It is a predictable response and can be seen in three distinct phases:
- Protest Phase: This is the most obvious phase. The child reacts aggressively and actively to the separation. They may cry, scream, cling to parents, and reject contact with strangers. They may also physically fight or attempt to escape. The duration of this phase can vary, and it is a healthy sign that the child has a strong attachment to their caregiver.
- Despair Phase: As the protest phase subsides, the child enters a state of hopelessness and sadness. They may be withdrawn, quiet, inactive, and may refuse to eat or play. They seem to mourn the loss of their parent, often crying intermittently or appearing depressed. The child may regress to earlier behaviors, such as thumb-sucking or bed-wetting.
- Detachment Phase (Denial): This phase is rare in short-term hospitalizations. The child becomes more interested in their surroundings, interacts with strangers, and appears to have adjusted to the separation. However, this is a sign of detachment and resignation, not contentment. The child has given up on their parents returning and is protecting themselves from further emotional pain. The child may ignore their parents when they return, which can be heartbreaking for the parents.
Manifestations of Separation Anxiety in Young Children
3.2 Loss of Control
- Hospitalization takes away a child's sense of control over their life. They are subjected to new routines, strict schedules, unfamiliar people, and invasive procedures without a full understanding of why.
- This lack of control can lead to feelings of helplessness, fear, and frustration. Children may express this through regressive behaviors (e.g., bed-wetting, thumb-sucking), aggression (e.g., temper tantrums, hitting), or resistance to care. Their routine, which provides a sense of predictability, is completely disrupted.
3.3 Effects of Hospitalization on the Child
The effects of hospitalization vary widely depending on the child's age, developmental stage, temperament, prior experiences, and the length and nature of the hospitalization.
- Infants: They are primarily affected by separation from their primary caregiver and the disruption of their feeding and sleep schedules. They may experience a lack of trust due to inconsistent care.
- Toddlers: They have a limited ability to understand illness and procedures. Their major stressors are separation anxiety and the fear of procedures. They may regress to earlier behaviors and exhibit temper tantrums and resistance to care.
- Preschoolers: They have a very active imagination and may believe their illness is a punishment for a misdeed (magical thinking). They have a strong fear of mutilation and bodily injury. They also experience separation anxiety.
- School-age children: They are concerned about missing school and friends, which affects their sense of normalcy and social development. Their major fears are of loss of control, bodily injury, and death. They may appear brave on the outside but are still afraid.
- Adolescents: They are most concerned about the loss of independence, privacy, and identity. They worry about body image, peer relationships, and missing out on social activities. They may withdraw from their family and become non-compliant with care.
Nursing Insight: It is crucial for the nurse to tailor care to the child's developmental level. For infants, consistent care from a limited number of nurses helps establish trust. For a toddler, using play and simple language is vital. A preschooler's fears of mutilation can be addressed by explaining that the body will be "fixed" and bandaged. With school-age children, providing honest information and a sense of control is essential. Adolescents need privacy, respect, and involvement in their care decisions to maintain their sense of autonomy.
- STRESSORS AND REACTIONS OF THE FAMILY OF THE CHILD WHO IS HOSPITALIZED
Stressors and Reactions of the Family of the Child Who Is Hospitalized
- The family is the central support system for the child. The child's hospitalization is a family crisis that affects everyone.
4.1 Parental Reactions
Parents often experience a wide range of emotions, including shock, denial, anxiety, fear, helplessness, and guilt. They may feel overwhelmed by the medical information and the demands of their child's care. Parents may feel like they are losing their parental role and feel powerless.
- Guilt: Parents often blame themselves, thinking they could have prevented the illness. They may feel they didn't act quickly enough or that their child's illness is a result of their poor parenting.
- Fear and Anxiety: They fear for their child's well-being, the pain of procedures, and the possibility of a poor outcome. They may also worry about the financial burden of the hospitalization.
- Lack of Control: Parents feel helpless as their child's care is taken over by professionals. They may feel that their role has been reduced to a passive bystander.
4.2 Sibling Reactions
Siblings are often the "forgotten mourners." They may experience a variety of emotions and reactions to their sibling's hospitalization, including:
- Loneliness and Fear: They miss their sibling and are afraid they won't get better. They may also fear that their parents will not return or that they will also get sick.
- Jealousy and Resentment: They may resent the attention the sick child is receiving and feel that their own needs are being ignored.
- Guilt: Younger siblings may engage in magical thinking and believe they caused the illness through a negative thought or action.
- Anxiety: They may have a heightened sense of anxiety about their own health and the family's stability. They may also regress to earlier behaviors to get attention.
Nursing Insight: Nurses must act as a compassionate liaison between the medical team and the parents. Providing clear, consistent, and honest information is vital. Encouraging parents to be present and to participate in their child's care empowers them and reinforces their parental role. For siblings, it's crucial to acknowledge their feelings, provide age-appropriate information, and encourage parents to maintain open communication. A child life specialist can be a valuable resource in helping both the child and siblings cope.
STRESSORS AND REACTIONS OF THE FAMILY OF THE CHILD WHO IS HOSPITALIZED
- The family is the central support system for the child. The child's hospitalization is a family crisis that affects everyone.
Nursing Insight: Nurses must act as a compassionate liaison between the medical team and the parents. Providing clear, consistent, and honest information is vital. Encouraging parents to be present and to participate in their child's care empowers them and reinforces their parental role. For siblings, it's crucial to acknowledge their feelings, provide age-appropriate information, and encourage parents to maintain open communication. A child life specialist can be a valuable resource in helping both the child and siblings cope.
Sibling Reactions
Siblings are often the "forgotten mourners." They may experience a variety of emotions and reactions to their sibling's hospitalization, including:
Loneliness and Fear: They miss their sibling and are afraid they won't get better. They may also fear that their parents will not return or that they will also get sick. Jealousy and Resentment: They may resent the attention the sick child is receiving and feel that their own needs are being ignored. Guilt: Younger siblings may engage in magical thinking and believe they caused the illness through a negative thought or action. Anxiety: They may have a heightened sense of anxiety about their own health and the family's stability. They may also regress to earlier behaviors to get attention.
Parental Reactions
Parents often experience a wide range of emotions, including shock, denial, anxiety, fear, helplessness, and guilt. They may feel overwhelmed by the medical information and the demands of their child's care. Parents may feel like they are losing their parental role and feel powerless.
Guilt: Parents often blame themselves, thinking they could have prevented the illness. They may feel they didn't act quickly enough or that their child's illness is a result of their poor parenting. Fear and Anxiety: They fear for their child's well-being, the pain of procedures, and the possibility of a poor outcome. They may also worry about the financial burden of the hospitalization. Lack of Control: Parents feel helpless as their child's care is taken over by professionals. They may feel that their role has been reduced to a passive bystander.
Nursing Care of the Child Who Is Hospitalized
- The goal of pediatric nursing care is to minimize the stress of hospitalization and promote the child's normal growth and development. This is achieved through preparation, providing comfort, and creating a therapeutic environment.
6.1 Preparation for Hospitalization
- Preparation is the single most effective way to reduce a child's anxiety and fear. It is a proactive nursing intervention that provides a child with a sense of predictability and control. The nurse acts as an educator and a guide, helping the child and family navigate the unknown.
6.1.1 Admission assessment
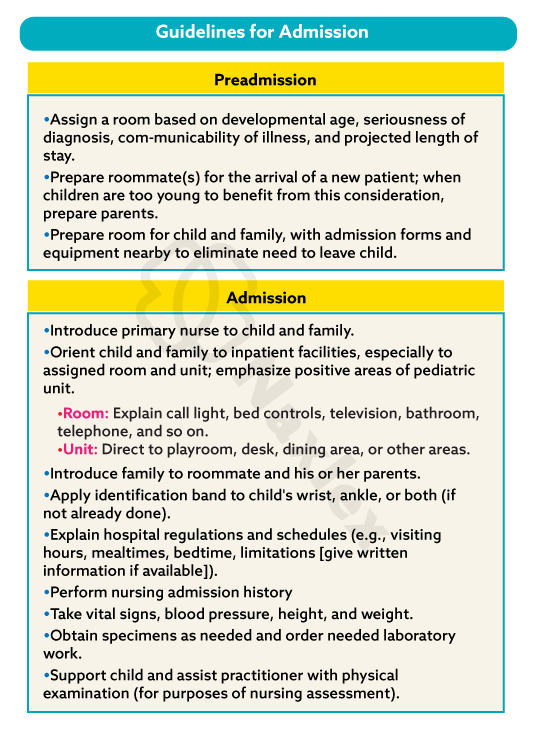
The nursing admission assessment is the foundation of the child's care plan. It is a comprehensive process that includes:
- Physical assessment: Vital signs, weight, height, and a head-to-toe assessment to establish a baseline.
- Psychosocial assessment: The child's developmental level, typical behaviors, fears, coping mechanisms, and temperament.
- Family assessment: Family structure, support systems, cultural beliefs, and the parents' understanding of the illness.
- History: Past medical history, allergies, immunizations, and a detailed review of the current illness.
Preparing the child for admission
Preparation should be honest, simple, and tailored to the child's developmental age.
- Infants: No specific cognitive preparation is needed; focus on parental presence and comfort.
- Toddlers and Preschoolers: Explain a few hours before the event, using simple, concrete terms. Use a doll or a toy to demonstrate procedures.
- School-age children: Explain in simple, factual terms a day or two before. They are capable of understanding cause and effect.
- Adolescents: Provide detailed information and allow them to ask questions. Involve them in decision-making as much as possible, as this promotes a sense of autonomy.
Parental absence during infant hospitalization
When parents cannot be present, the nurse must act as a surrogate parent to meet the infant's needs for consistent care and comfort.
- Maintain the infant's routine as closely as possible.
- Provide consistent care from a limited number of nurses to promote trust.
- Use a blanket or an item with the parent's scent to provide a sense of security.
- Hold and comfort the infant frequently.
Minimizing loss of control
- Maintaining the child's routine: Adhere to the child's typical sleep, feeding, and play schedules as much as possible. This provides a sense of predictability.
- Promoting freedom of movement: Avoid unnecessary restraints. When restraints are needed, explain their purpose, ensure they are not too tight, and check circulation frequently.
- Encouraging independence: Let the child participate in their care by holding the syringe to their mouth or choosing their pajamas.
- Promoting understanding: Use simple, honest language to explain procedures. Use diagrams or pictures.
Preventing or minimizing fear of bodily injury
- Explain procedures simply: Use a "show and tell" approach. Let the child touch safe equipment, like an IV tubing or a stethoscope.
- Use therapeutic play: Allow the child to act out their fears with dolls or puppets.
- Provide comfort: Use pain management techniques, distraction (e.g., bubbles, stories), and comfort items (e.g., blanket, stuffed animal).
- Be honest: Never tell the child something won't hurt if it will. Instead, say, "It will feel like a quick pinch, but it will be over soon."
Providing developmentally appropriate activities
- Infants: Provide mobiles, soft toys, and music.
- Toddlers: Offer push-pull toys, stacking blocks, and simple puzzles.
- Preschoolers: Give them crayons, paper, puppets, and books.
- School-age children: Provide board games, video games, books, and art supplies.
- Adolescents: Offer music, movies, and opportunities for social interaction with other teens.
Providing opportunities for play and expressive activities
Play is the "work" of the child and is essential for their development.
- Diversional activities: These are activities that provide entertainment and a break from the routine, like watching a movie or playing a game.
- Toys: Toys should be safe, age-appropriate, and easily cleaned. They should also be non-toxic and durable.
- Expressive activities: This includes drawing, painting, or writing, which allows a child to express their emotions non-verbally.
- Creative expression: Music, storytelling, and imaginative play allow the child to process their experiences and fears in a safe way.
- Dramatic play: Using medical equipment (e.g., stethoscope, syringe without a needle) to play "hospital" or "doctor" helps the child master their fears and gain a sense of control over their situation.
Maximizing potential benefits of hospitalization
- Fostering parent-child relationships: The hospital can be an opportunity for a parent and child to spend quality, uninterrupted time together.
- Providing educational opportunities: The nurse can teach the child and family about the illness, a healthy lifestyle, and self-care.
- Promoting self-mastery: As the child successfully copes with procedures and the illness, they gain a sense of competence and confidence.
- Providing socialization: A child may have the opportunity to interact with other children with similar illnesses, which can reduce feelings of isolation.
Nursing Care of the Family
- Family-centered care is paramount in pediatric nursing. Supporting the family is a direct way to support the child.
Supporting Family Members
- Encourage parental presence: Provide a comfortable place for parents to stay overnight, such as a cot or a sleeper chair.
- Offer emotional support: Listen to their fears and concerns without judgment. Validate their feelings and let them know that their reactions are normal.
- Provide practical support: Offer to help with basic needs, like finding food, a place to rest, or connecting them with social services.
Providing Information
- Communicate honestly and clearly: Use simple language and avoid medical jargon. Use visual aids or diagrams to help explain complex concepts.
- Update them regularly: Give frequent updates on their child's condition, even if there are no major changes. This reduces anxiety.
- Involve them in rounds: Encourage them to be present when the medical team visits so they can hear the plan of care directly.
Encouraging Parent Participation
- Involve parents in care: Allow them to do things they are comfortable with, like feeding, bathing, or changing their child.
- Teach them skills: Show them how to do things like check a temperature or administer a medication so they feel empowered and confident in their ability to care for their child.
- Respect their knowledge: Acknowledge that they are the experts on their child and that their insights are invaluable to the care team.
Preparation for Discharge and Home Care
- Begin on admission: Discharge planning should begin the day the child is admitted to ensure a smooth transition.
- Teach home care: Educate parents on all aspects of care, including medication schedules, wound care, dietary needs, and when to call the doctor.
- Provide written instructions: A clear, written plan with emergency contact information is essential. This can be a checklist to help them remember all the instructions.
- Connect them to resources: Provide information on support groups, home health services, or financial assistance.
Nursing Insight: The nurse's role is to empower the family, not replace them. By providing information, encouraging participation, and offering emotional and practical support, the nurse helps the family maintain their role as the primary caregiver and ensures a smoother, more effective recovery for the child.
Care of the Child and Family in Special Hospital Situations
- Special circumstances require tailored nursing interventions to meet the unique needs of the child and family.
8.1 Ambulatory or Outpatient Setting
- Goal: Provide care in a non-threatening environment to minimize trauma.
- Interventions: Prepare the child and parent immediately before the procedure. Use a treatment room rather than a patient room to keep the room a "safe place." Provide quick, efficient care and comfort measures.
8.2 Isolation
- Goal: Provide necessary care while minimizing the negative effects of social isolation.
- Interventions: Explain the reason for isolation in simple terms. Ensure frequent visits from the nursing staff. Provide a variety of toys and activities. Encourage parents to visit and stay with their child.
8.3 Emergency Admission
- Goal: Provide urgent care while addressing the child's and family's high levels of fear and anxiety.
- Interventions: Rapidly assess the child's condition. Speak calmly and reassuringly. Provide brief, clear explanations. Allow a parent to be with the child during procedures whenever possible, as their presence is a source of comfort.
8.4 Intensive Care Unit
- Goal: Provide critical, specialized care while supporting the family through a traumatic experience.
- Interventions: Maintain a consistent care routine to provide a sense of stability. Explain all monitors and tubes to the family. Encourage family presence and participation in non-critical tasks like holding a hand or speaking to the child. Provide opportunities for the family to take a break.
Nursing Insight: Each special setting presents a unique challenge. In all of them, the principles of family-centered care, honest communication, and age-appropriate interventions are paramount. The nurse must be a source of calm, stability, and information during times of crisis.
Pediatric nursing Interventiona and skills
- Pediatric nursing requires specific skills and a keen understanding of child development to provide safe and effective care.
10.1 General Concepts Related to Pediatric Procedures
- Informed Consent: The legal guardian must provide informed consent for all major medical and surgical procedures. The nurse's role is to ensure the guardian understands the procedure and has had all their questions answered by the physician.
- Assent in pediatric care is the process of getting a child's affirmative agreement to participate in a medical procedure, treatment, or research study. It is not the same as legal consent, which can only be given by an adult who has reached the legal age of consent (typically 18) or a child's parent or legal guardian. Assent is a way to respect a child's developing autonomy and include them in their own healthcare decisions.
- Preparation for Diagnostic and Therapeutic Procedures: Explain procedures in age-appropriate terms, using a calm tone. Use distraction techniques like bubbles, music, or a video to minimize fear and pain.
10.2 Skin Care and General Hygiene
- Maintaining healthy skin: Regular bathing and moisturizing are crucial, especially for infants and children with sensitive skin. Inspect the skin for signs of breakdown or rash.
- Bathing: A warm, comfortable environment is essential. Use a mild soap.
- Oral Hygiene: Brushing teeth twice a day is a must. For infants, use a soft cloth to wipe the gums.
- Hair Care: Use a gentle shampoo and comb. Be mindful of culturally specific hair care practices.
- Feeding the sick child: Offer small, frequent meals of their favorite foods. Encourage fluids to prevent dehydration.
- Controlling elevated temperatures: Administer antipyretics like acetaminophen or ibuprofen as prescribed. Use non-pharmacological methods like tepid sponge baths with caution, as they can cause shivering and increase metabolic demand.
- Family teaching and home care: Educate parents on proper hygiene techniques, fever management, and signs of dehydration.
10.3 Safety
- Environmental factors: Ensure the bed rails are up and locked. Remove small, choking-hazard toys from the cribs of infants and toddlers.
- Infection control: Practice meticulous hand hygiene. Use personal protective equipment (PPE) as needed.
- Transporting infants and children: Infants should be transported in a crib. Toddlers and children can be transported in a wagon or wheelchair, with safety belts secured.
- Restraining methods: Restraints should only be used as a last resort and for the shortest time possible. An order with a rationale for the restraint and a time frame for restraint use is required.
- Mummy Restraint or Swaddle: Used for short-term procedures on infants and young children, like an IV start or a blood draw.

-
- Arm and Leg Restraints: Used to prevent a child from disrupting an IV site or other lines.
- Elbow Restraint: Used to prevent the child from bending their elbow to reach their face or head (e.g., after cleft lip repair).

-
- Jacket restraint: May be applied to a toddler who is in skeletal traction.
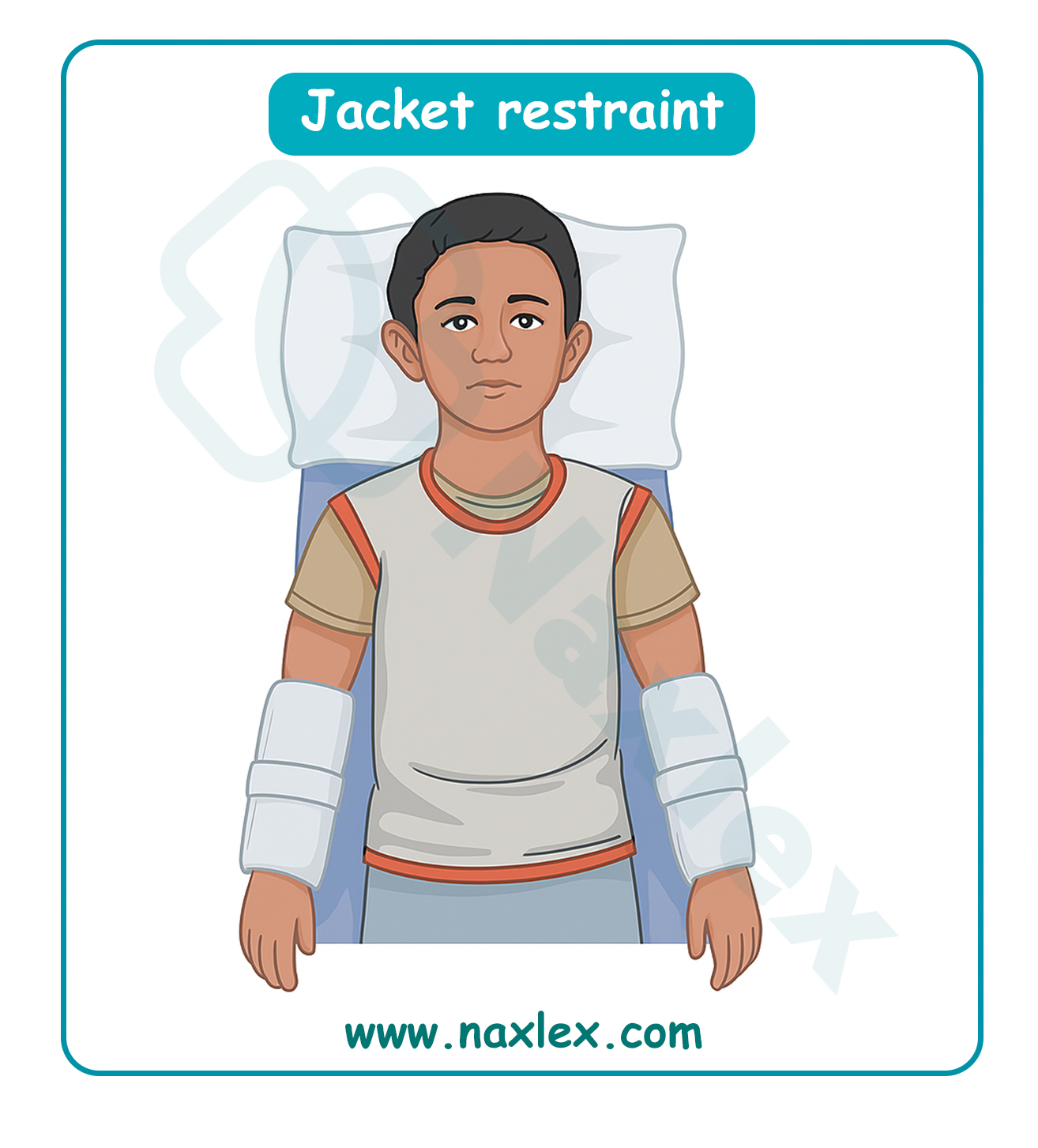
- Non-violent/non-self-destructive patients may also require restraints to support medical healing. Examples of situations where a nonbehavioral restraint may be necessary for the patient’s safety include removal of an artificial airway or airway adjunct for delivery of oxygen, indwelling catheters, tubes, drains, lines, pacemaker wires, or disruption of suture sites. The medical-surgical restraint is used to ensure that safe care is given to the patient. Patient confusion, agitation, unconsciousness, and developmental inability to understand direct requests or instructions may warrant the use of nonbehavioral restraints to maintain patient safety. The potential risks of the restraint are offset by the potential benefit of providing safer care.
- Nonbehavioral restraints can be initiated by an individual order or by protocol; the use of the protocol must be authorized by an individual order. The order for continued use of restraints must be renewed each day. Patients are monitored per facility policy, typically at least every 2 hours.
- Restraints with ties must be secured to the stationary bed or crib frame, not the side rails. Suggestions for increasing safety and comfort while the child is in a restraint include leaving one finger breadth between skin and the device and tying knots that allow for quick release.
- The nurse can also increase safety by ensuring the restraint does not tighten as the child moves and decreasing wrinkles or bulges in the restraint. Placing jacket restraints over an article of clothing; placing limb restraints below waist level, below knee level, or distal to the IV; and tucking in dangling straps also increase safety and comfort.
Nursing Insight: The nurse must assess the restraint site regularly. Check site distal to the restraint for circulatory compromise by assessing capillary refill, color, temperature, and movement. Assess under the restraint for signs of altered skin integrity (e.g., decubiti). Assess neurological status distal to the site by monitoring pain levels and movement.
10.4. Administration of Medication
- 10.4.1 Determination of drug dosage: Pediatric medication dosages are based on weight (mg/kg). Accurate weight is essential. Two nurses should double-check all high-alert medications.
- 10.4.2 Oral administration: Use an oral syringe or a medicine cup. Never refer to medication as candy. For infants, use a syringe and place the medication in the side of the mouth to prevent aspiration.
- 10.4.3 Intramuscular administration:
- Selecting the syringe and needle: Use a smaller gauge needle (22-25 gauge) and a shorter needle length (0.5 to 1 inch).
- Determining the site:
- Vastus Lateralis: Preferred site for infants and toddlers due to its large muscle mass and lack of major nerves or blood vessels.
- Deltoid: Used for older children.
- Ventrogluteal: A safe site for all ages but often not used in children under 7 months.
- Administration: Distract the child. Use a quick, smooth motion to insert the needle.
- Vastus lateralis. B. Ventrogluteal. C. Deltoid
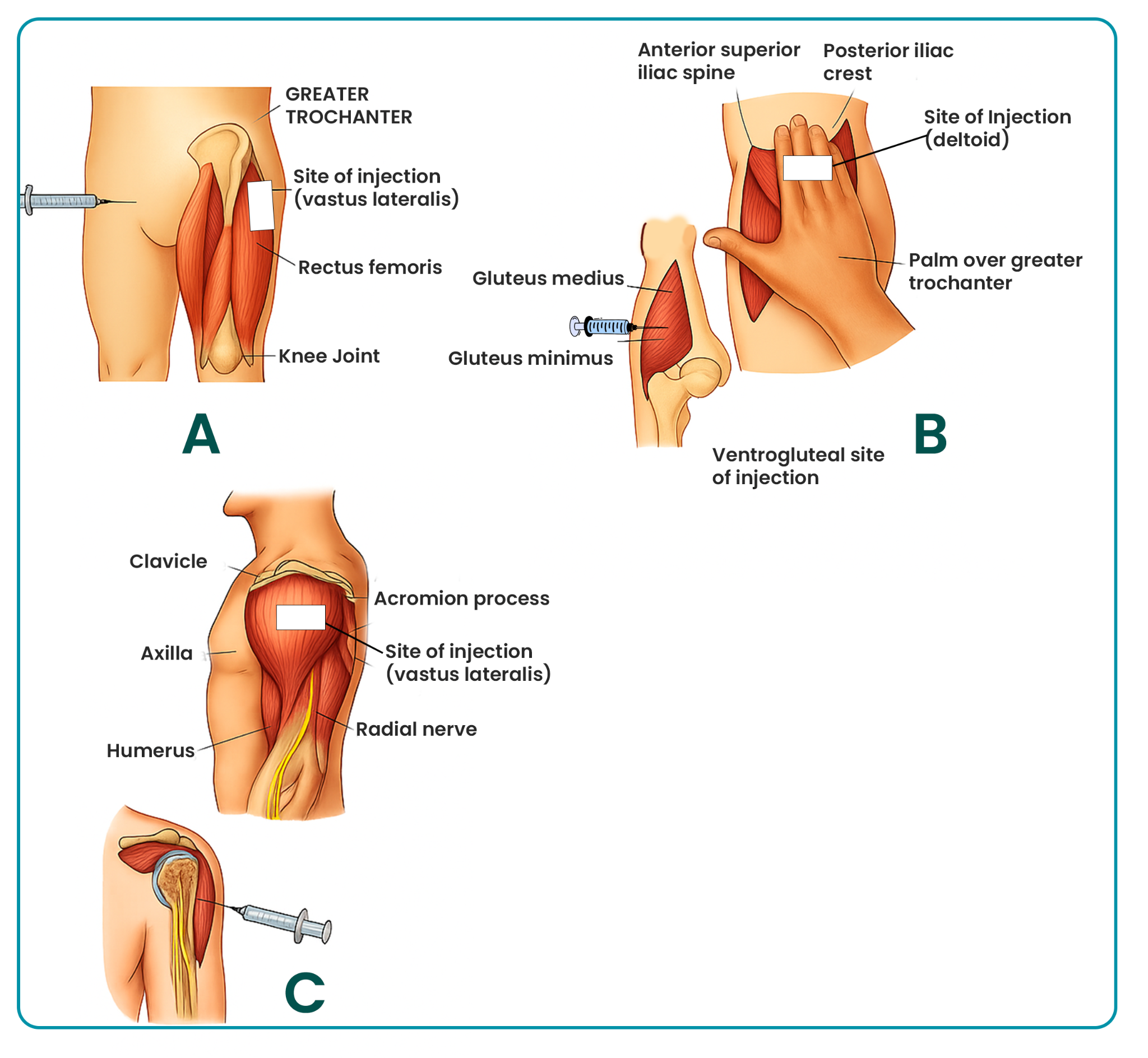
- 10.4.4 Subcutaneous and Intradermal Administration: Use a short, small-gauge needle. The abdomen and the outer aspect of the upper arm are common sites.
- 10.4.5 Intravenous Administration: Requires a meticulous technique to avoid infiltration and infection. Use a saline lock to maintain patency.
Preferred sites for venous access in infants
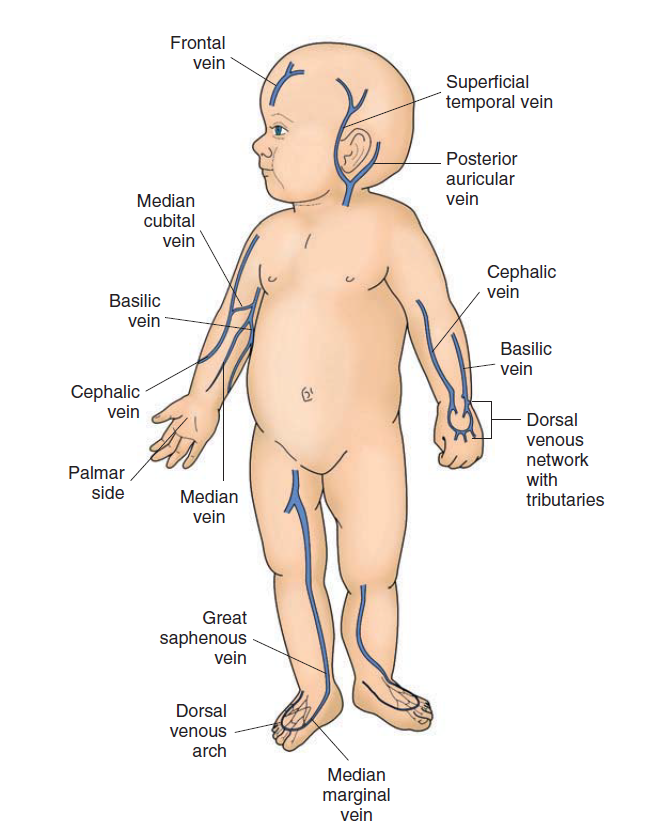
- 10.4.6 Rectal Administration: Used when the oral route is not possible. Place the child in a side-lying position. Hold the buttocks together for a few minutes.
- 10.4.7 Optic, Otic, and Nasal Administration:
- Optic: Pull the lower lid down and instill drops into the conjunctival sac.
- Otic: For children under 3, pull the pinna down and back. For children over 3, pull the pinna up and back.
- Nasal: Place the child in a head-hyperextended position.
- 10.4.8 Aerosol therapy: Use a mask or mouthpiece. Explain that it is "breathing medicine."
- 10.4.9 Nasogastric, Orogastric, and Gastrostomy Administration: Check placement before administering medication or feeding. Flush the tube with water before and after each medication.
Nursing Insight: The administration of medication in pediatrics requires an extremely high degree of accuracy and skill. The nurse must not only be precise with the dosage and route but also use a gentle, reassuring approach to minimize the child's fear and discomfort.
Summary
- Caring for children in diverse settings requires a holistic approach that centers on the unique needs of the child and their family.
- The nurse's role is to minimize the stressors of hospitalization, promote a sense of control and security, and provide skilled, developmentally appropriate, and family-centered care.
- By understanding the stressors, implementing therapeutic play, ensuring safety, and mastering essential pediatric skills, nurses can positively impact the health and well-being of their young patients.
- Unlike adults, children have limited coping mechanisms and a developing understanding of illness and procedures. Their reactions are largely influenced by their developmental stage, temperament, previous experiences with illness, and the support they receive from their family and healthcare providers.
- Pediatric nursing is centered on a family-centered care approach, which recognizes the family as the constant in the child's life and emphasizes collaboration between healthcare providers and the family to ensure the best outcomes.
- This approach promotes the child's well-being by reducing stress, supporting normal development, and empowering the family.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on The child who is hospitalized
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


