Please set your exam date
Drugs Used for Pain Management
Study Questions
Practice Exercise 1
The nurse teaches the client relaxation techniques and guided imagery as an adjunct to medication for treatment of pain. What is the main rationale for the use of these techniques as an adjunct to analgesic medication?
Explanation
Nonpharmacological interventions such as relaxation techniques and guided imagery are valuable adjuncts to medication in pain management. These methods work by reducing anxiety, improving coping, and altering the perception of pain, which can enhance the effectiveness of analgesics. The key benefit is that if non-drug strategies successfully reduce pain intensity, lower doses of analgesics may be required, thereby decreasing the risk of adverse effects such as respiratory depression, constipation, or sedation.
Rationale for correct answer:
B. They may allow lower doses of drugs with fewer adverse effects: Combining pharmacological and nonpharmacological interventions can provide synergistic pain relief. By lowering reliance on higher analgesic doses, patients experience adequate pain control with reduced risk of complications such as opioid-induced constipation, dependence, or toxicity. This integrative approach is especially important in long-term pain management.
Rationale for incorrect answers:
A. They are less costly techniques: While relaxation and imagery are indeed inexpensive, cost reduction is not the main rationale for their use in clinical pain management. The focus is on enhancing patient safety and reducing drug-related risks.
C. They can be used at home: Although true, the ability to use these techniques at home is a secondary advantage. The primary rationale remains the potential to reduce drug dosage and adverse effects.
D. They do not require self-injection: This point is irrelevant, as not all analgesics are given by injection. Pain medications may be oral, transdermal, or intravenous, so avoiding injections is not the key rationale here.
Take-home points:
• Adjunctive techniques enhance analgesic effectiveness, reducing the need for higher drug doses.
• Fewer adverse effects are the main benefit of combining non-drug and drug therapies.
• Guided imagery and relaxation also empower patients with active coping strategies for pain management.
For best results when treating severe pain associated with pathologic spinal fractures related to metastatic bone cancer, the nurse should remember that the best type of dosage schedule is to administer the pain medication in which of these?
Explanation
Severe pain associated with metastatic bone cancer requires aggressive and consistent management. The goal is to maintain steady plasma levels of analgesics, prevent pain from escalating, and provide relief for sudden pain flares. The most effective approach combines scheduled baseline analgesia with additional doses for breakthrough pain.
Rationale for correct answer:
D. Around the clock, with additional doses as needed for breakthrough pain:
This strategy ensures continuous pain control by maintaining therapeutic drug levels while also addressing unexpected pain spikes. It improves quality of life, reduces suffering, and prevents the “roller-coaster” effect of pain cycling between unbearable and tolerable.
Rationale for incorrect answers:
A. As needed:
This leaves the patient waiting until pain becomes severe before taking medication, leading to unnecessary suffering and poor pain control.
B. Around the clock:
While helpful for steady control, it does not address breakthrough pain, which is common in cancer-related pain.
C. On schedule during waking hours only:
Cancer pain persists throughout the night. Restricting dosing to waking hours risks nighttime suffering and disturbed sleep.
Take-home points:
- Scheduled dosing with breakthrough coverage is the gold standard for severe cancer pain.
- “As needed” dosing alone is inadequate for managing chronic severe pain.
- Nurses should monitor effectiveness, side effects, and patient comfort when adjusting regimens.
The nurse administers morphine sulfate 4 mg IV to a client for treatment of severe pain. Which of the following assessments require immediate nursing interventions? Select all that apply
Explanation
Morphine sulfate is a potent opioid analgesic commonly used for severe pain. While effective, it can cause serious adverse effects such as respiratory depression, sedation, and decreased level of consciousness. After administration, the nurse must carefully monitor vital signs, level of consciousness, and pain relief. Certain findings require immediate intervention to prevent life-threatening complications.
Rationale for correct answers:
C. The client’s pain is unrelieved in 15 minutes: This indicates the medication may not be effective. Since morphine was given IV, pain relief should occur within minutes. Lack of relief requires reassessment and possibly contacting the provider for alternative orders.
D. The client’s respiratory rate is 10 breaths per minute: Opioids depress the respiratory center. A rate below 12 breaths/min signals respiratory depression, which is dangerous and requires immediate intervention (stimulate the patient, stop opioids, consider naloxone).
E. The client becomes unresponsive: This is a critical finding showing severe opioid-induced CNS depression. It requires emergency intervention to maintain airway, breathing, and circulation.
Rationale for incorrect answers:
A. Blood pressure 110/70 mmHg: This is a normal reading and does not require intervention.
B. The client is drowsy: Mild drowsiness is an expected effect of morphine. It only becomes concerning if the client progresses to unresponsiveness.
Take-home points:
- Respiratory depression and unresponsiveness are the most dangerous adverse effects of opioids and demand immediate nursing action.
- Unrelieved pain after IV opioid administration suggests inadequate analgesia and requires reassessment.
- Always distinguish between expected effects (drowsiness, normal BP changes) and life-threatening effects (respiratory depression, unresponsiveness).
Planning teaching needs for a client who is to be discharged postoperatively with a prescription for oxycodone with acetaminophen (Percocet) should include which of the following?
Explanation
Oxycodone with acetaminophen (Percocet) is a combination opioid analgesic frequently prescribed for postoperative pain management. While effective, it carries potential side effects such as constipation, sedation, and hepatotoxicity. Teaching must focus on the most common and preventable complications, helping the client manage their pain safely at home.
Rationale for correct answer:
B. Encourage increased fluids and fiber in the diet: Opioids like oxycodone slow gastrointestinal motility, leading to constipation. Preventive teaching about increasing fluids, fiber, and physical activity is essential to avoid discomfort and potential complications such as fecal impaction.
Rationale for incorrect answers:
A. Refer the client to a drug treatment center if addiction occurs: This is not an appropriate discharge teaching plan. The nurse’s role is prevention and education about safe use, not assuming addiction will develop.
C. Monitor for GI bleeding: GI bleeding is associated with NSAIDs, not opioids or acetaminophen. Acetaminophen toxicity primarily affects the liver, not the GI lining.
D. Teach the client to self-assess blood pressure: Opioids do not usually cause hypertension requiring home BP monitoring. While hypotension can occur, it is not the main concern for teaching.
Take-home points:
- Constipation is the most common adverse effect of opioids, so prevention with fluids, fiber, and mobility should be emphasized.
- GI bleeding is linked to NSAIDs, while acetaminophen toxicity mainly threatens the liver.
- Client teaching should always target the most likely and preventable complications of prescribed medications.
What is the most appropriate method to ensure adequate pain relief in the immediate postoperative period from an opioid drug?
Explanation
Oxycodone with acetaminophen (Percocet) is an opioid combination commonly used for postoperative pain. Important teaching focuses on the most likely adverse effects and how to prevent them—especially opioid-related constipation—while also noting acetaminophen’s hepatic risks.
Rationale for correct answer:
B. Encourage increased fluids and fiber in the diet: Opioids slow gastrointestinal motility and commonly cause constipation. Teaching the client to increase fluids, dietary fiber, and activity (and to use stool softeners or mild laxatives as ordered) helps prevent constipation and related complications.
Rationale for incorrect answers:
A. Refer the client to a drug treatment center if addiction occurs: This is not appropriate as routine discharge teaching. The nurse should focus on safe use, storage, and short-term use guidelines, plus signs of misuse and when to contact the provider—not assume addiction will occur.
C. Monitor for GI bleeding: GI bleeding is associated with NSAIDs and anticoagulants—not with oxycodone or acetaminophen. Acetaminophen’s major concern is hepatotoxicity, not GI bleeding.
D. Teach the client to self-assess blood pressure: Routine blood-pressure self-monitoring is not required for outpatient teaching about Percocet. While opioids can cause hypotension in some cases, the primary teachable risks are constipation, sedation, respiratory depression (especially with higher doses or other CNS depressants), and hepatotoxicity from excess acetaminophen.
Take-home points:
- Prevent constipation with increased fluids, fiber, activity, and stool softeners as appropriate.
- Warn about sedation and respiratory depression—avoid alcohol and other CNS depressants and follow dosing instructions.
- Limit acetaminophen intake (watch for other acetaminophen-containing products) to prevent liver injury.
For the patient receiving periodic morphine IV push, which is the most critical finding for the nurse to discover?
Explanation
Morphine is a strong opioid analgesic frequently administered intravenously for acute and severe pain management. While it provides effective relief, opioids act on the central nervous system and can suppress vital functions. Among their adverse effects, respiratory depression is the most critical and life-threatening, making careful assessment by the nurse essential after each dose.
Rationale for correct answer:
C. Decreased respirations: Morphine depresses the respiratory center in the brainstem. A slowing respiratory rate is the most critical finding because it can quickly progress to hypoxia, respiratory arrest, and death if not addressed. Continuous monitoring of rate and depth of respirations is essential when giving IV morphine.
Rationale for incorrect answers:
A. Increased temperature: Not directly related to morphine administration. Fever is more likely due to infection, not opioid use.
B. Decreased bowel sounds: Morphine does slow GI motility, but this leads to constipation and ileus, which are significant but not immediately life-threatening compared with respiratory depression.
D. Increased red blood cell count: Morphine has no effect on red blood cell production. This finding would be unrelated to opioid therapy.
Take-home points:
- The most critical risk of opioids is respiratory depression; always monitor breathing.
- Constipation and GI slowing are common but less urgent adverse effects.
- Nurses must prioritize airway and breathing when assessing opioid side effects.
Practice Exercise 2
A nurse is caring for a client who is diagnosed with salicylism. Which of the following findings should the nurse expect to assess in this client? Select all that apply
Explanation
Salicylism is the toxic effect that can occur with high levels of salicylates (such as aspirin). It most commonly presents with neurological and auditory symptoms, because salicylates directly affect the central nervous system and the inner ear. Recognizing the hallmark signs is essential for early intervention and preventing progression to severe toxicity.
Rationale for correct answers:
A. Dizziness: Salicylism often impairs the central nervous system, leading to vertigo and dizziness. This occurs because of alterations in the inner ear and brain function due to high salicylate levels.
D. Tinnitus: Ringing in the ears (tinnitus) is the classic early symptom of salicylism and is often the first clinical clue of toxicity. It reflects direct cochlear toxicity from salicylates and usually resolves once the drug is discontinued or the dose is reduced.
E. Headache: Headaches are common in salicylism because of cerebral effects caused by salicylates, which can alter blood flow and acid–base balance, leading to neurological manifestations.
Rationale for incorrect answers:
B. Diarrhea: While aspirin can irritate the gastrointestinal tract, diarrhea is not a typical finding in salicylism. More common GI effects would be nausea, vomiting, or gastric discomfort.
C. Jaundice: Jaundice is not a sign of salicylism. Although high doses of salicylates can cause liver stress in rare cases, jaundice is not expected and should prompt evaluation for another underlying condition.
Take-home points:
• Tinnitus, dizziness, and headache are hallmark findings of salicylism.
• Salicylism primarily affects the CNS and auditory system rather than the GI tract or liver.
• Early recognition of tinnitus is critical since it often appears before more severe toxicity develops.
A nurse in an emergency department is performing an admission assessment for a client who has severe aspirin toxicity. Which of the following findings should the nurse expect to find?
Explanation
Severe aspirin (salicylate) toxicity is a life-threatening condition that affects both the respiratory and metabolic systems. Initially, aspirin stimulates the respiratory center in the brain, causing hyperventilation and respiratory alkalosis. As toxicity worsens, however, the central nervous system becomes depressed, leading to respiratory depression—a late and dangerous sign that signals impending respiratory failure. This is the most critical complication to monitor for in advanced toxicity.
Rationale for correct answer:
D. Respiratory depression: In severe aspirin overdose, after prolonged stimulation of the respiratory center, the body’s ability to maintain hyperventilation is lost. The result is respiratory depression, which contributes to mixed respiratory and metabolic acidosis. This is a hallmark of severe toxicity and requires immediate intervention, often with ventilatory support.
Rationale for incorrect answers:
A. Body temperature 35° C (95° F): Hypothermia is not expected. Instead, aspirin toxicity more often causes hyperthermia due to increased metabolic activity and heat production.
B. Lung crackles: Crackles are not a typical finding of aspirin poisoning. While pulmonary edema may occur in very severe toxicity, the more direct and classic presentation is related to acid-base imbalance and respiratory drive changes.
C. Cool, dry skin: Clients with salicylate toxicity are more likely to present with sweating, dehydration, and flushed skin rather than cool, dry skin.
Take-home points:
• Respiratory depression is a late and critical sign of severe aspirin toxicity.
• Early signs include tachypnea, hyperthermia, tinnitus, and metabolic acidosis.
• Prompt recognition and treatment (activated charcoal, IV fluids, bicarbonate, dialysis if severe) are essential to prevent death.
A nurse is taking a history for a client who reports that he is taking aspirin about four times daily for a sprained wrist. Which of the prescribed medications taken by the client is contraindicated with aspirin?
Explanation
Aspirin is an antiplatelet drug that irreversibly inhibits platelet aggregation, thereby increasing the risk of bleeding. When combined with warfarin, an anticoagulant that inhibits clotting factor synthesis, the effects are synergistic, dramatically raising the risk of serious bleeding events such as gastrointestinal bleeding or intracranial hemorrhage. This combination is generally contraindicated unless specifically prescribed under very close monitoring by a healthcare provider.
Rationale for correct answer:
C. Warfarin (Coumadin): Both aspirin and warfarin impair hemostasis but through different mechanisms—aspirin inhibits platelet function while warfarin reduces clotting factor activity. When used together, they significantly increase the likelihood of severe bleeding complications. This makes the combination contraindicated unless the benefit clearly outweighs the risk and the patient is closely monitored.
Rationale for incorrect answers:
A. Digoxin (Lanoxin): Digoxin is a cardiac glycoside used for heart failure and atrial fibrillation. It does not directly interact with aspirin in a way that increases toxicity or bleeding risk.
B. Metformin (Glucophage): Metformin is an oral hypoglycemic agent. While aspirin at very high doses can potentially alter glucose metabolism, there is no significant contraindication for concurrent use at normal therapeutic levels.
D. Nitroglycerin (Nitro-Dur): Nitroglycerin is a vasodilator used in angina. It does not interact significantly with aspirin in a way that would contraindicate their use together. In fact, aspirin is often prescribed alongside nitrates in patients with coronary artery disease.
Take-home points:
• Aspirin plus warfarin = very high bleeding risk and is generally contraindicated.
• Other listed drugs (digoxin, metformin, nitroglycerin) do not pose the same bleeding danger with aspirin.
• Always review for drug–drug interactions when a patient is using aspirin frequently or chronically.
A patient is taking ibuprofen. The nurse understands that COX-1 and COX-2 inhibitors are different in that ibuprofen is more likely than celecoxib to cause which adverse effect?
Explanation
NSAIDs like ibuprofen inhibit both COX-1 and COX-2 enzymes. While this dual inhibition provides effective pain and inflammation relief, blocking COX-1 also reduces gastric mucosal protection, predisposing the client to gastrointestinal irritation, ulceration, and bleeding. In contrast, celecoxib, a selective COX-2 inhibitor, spares COX-1 and therefore has a lower risk of GI complications.
Rationale for correct answer:
C. Peptic ulcer disease: Because ibuprofen inhibits COX-1, it decreases protective gastric prostaglandins, increasing the risk of peptic ulcers, GI bleeding, and gastric discomfort. This is a hallmark difference compared with celecoxib, which is COX-2 selective and less likely to damage the GI tract.
Rationale for incorrect answers:
A. Fever: Both ibuprofen and celecoxib reduce fever due to COX-2 inhibition. This is not unique to ibuprofen.
B. Constipation: Constipation is not a common NSAID side effect; it is more commonly associated with opioids.
D. Metallic taste when eating: This is not a typical adverse effect of either ibuprofen or celecoxib.
Take-home points:
- Ibuprofen (COX-1 & COX-2 inhibitor) increases the risk of GI irritation and ulcers.
- Celecoxib (COX-2 selective) is gentler on the stomach but may have cardiovascular risks.
- Always assess for GI history (ulcers, bleeding) when prescribing or administering non-selective NSAIDs.
A nurse is admitting a toddler to the hospital after an acetaminophen overdose. Which of the following medications should the nurse anticipate administering to this client?
Explanation
Acetaminophen overdose is one of the most common causes of acute liver failure in children. Toxic levels overwhelm the liver’s ability to metabolize the drug safely, leading to the accumulation of a hepatotoxic metabolite (NAPQI). Acetylcysteine (Mucomyst) is the antidote because it replenishes glutathione, the substance needed to detoxify NAPQI, thereby protecting the liver from further damage.
Rationale for correct answer:
A. Acetylcysteine (Mucomyst): This is the specific antidote for acetaminophen toxicity. It works by restoring glutathione stores, allowing the body to neutralize toxic metabolites and prevent hepatocellular necrosis. It can be given orally or intravenously and is lifesaving when administered promptly.
Rationale for incorrect answers:
B. Pegfilgrastim (Neulasta): This drug stimulates white blood cell production and is used to prevent infection in clients receiving chemotherapy. It has no role in the treatment of acetaminophen overdose.
C. Misoprostol (Cytotec): Misoprostol is used to prevent gastric ulcers from NSAID therapy or to induce labor. It does not protect the liver or reverse acetaminophen toxicity.
D. Naltrexone (ReVia): Naltrexone is an opioid antagonist used for opioid or alcohol dependence. It is not effective against acetaminophen overdose because it does not interact with hepatic metabolism.
Take-home points:
• Acetylcysteine is the antidote for acetaminophen overdose—it prevents liver failure by neutralizing toxic metabolites.
• Early treatment (within 8–10 hours) gives the best chance of full recovery.
• Always differentiate antidotes: acetylcysteine for acetaminophen, naloxone for opioids, flumazenil for benzodiazepines.
A nurse is preparing to administer 10 mg/kg acetaminophen (Tylenol) PO to a toddler who weighs 9 kg (19.8 lb). Available is acetaminophen liquid 160 mg/5 mL. How many mL should the nurse plan to administer? (Round the answer to the nearest tenth.)
Explanation
Pediatric medication administration requires careful weight-based calculations to ensure both safety and effectiveness. For drugs like acetaminophen, accurate conversion from milligrams to milliliters is crucial to avoid underdosing or overdosing in children.
Rationale for correct answer:
Step 1: Calculate the Total Dose
First, determine the total dose of acetaminophen the toddler should receive based on their weight.
- Formula: Total Dose = Weight (kg) × Dose per kg
- Calculation: 9kg×10mg/kg=90mg
Step 2: Calculate the Volume to Administer
Next, use the total dose and the concentration of the available medication to find the volume to be administered. The concentration is 160 mg in 5 mL.
- Formula: Volume = Total Dose ÷ Concentration
- Calculation:
- Find the concentration: 160mg÷5mL=32mg/mL
- Find the volume: 90mg÷32mg/mL=2.8125mL
Step 3: Round to the Nearest Tenth
Round the final answer to the nearest tenth as requested.
- Correct answer: 2.8125mL≈2.8mL
Take-home points:
- Always calculate pediatric doses using the child’s weight in kilograms and the prescribed mg/kg dosage.
- Convert the supplied concentration into mg/mL before calculating the required volume.
- For a 9 kg toddler receiving 10 mg/kg acetaminophen, the correct dose is 2.8 mL of a 160 mg/5 mL solution.
A client admitted with hepatitis B is prescribed hydrocodone with acetaminophen (Vicodin) 2 tablets for pain. What is the most appropriate action for the nurse to take?
Explanation
Clients with hepatitis B have impaired liver function, which increases their risk for drug-induced hepatotoxicity. Since acetaminophen is metabolized by the liver and can cause severe hepatotoxicity in excessive or even normal doses when the liver is compromised, caution is essential. Any acetaminophen-containing medication prescribed to a client with hepatitis should be carefully verified before administration.
Rationale for correct answer:
C. Recheck the order with the health care provider: The nurse’s priority is patient safety. Because acetaminophen poses a significant risk of worsening liver injury in a client with hepatitis B, the nurse should clarify the prescription before giving the drug. This ensures the provider considers an alternative analgesic or adjusts the dose to protect the client’s liver.
Rationale for incorrect answers:
A. Administer the drug as ordered: Unsafe, because giving acetaminophen without verifying may exacerbate hepatotoxicity in a client already at risk from hepatitis.
B. Administer 1 tablet only: Reducing the dose without provider input is outside the nurse’s scope. The underlying concern isn’t just the dose but the appropriateness of acetaminophen at all in this client.
D. Hold the drug until the health care provider arrives: Holding the drug without communicating directly may delay pain management unnecessarily. The best step is to clarify the order promptly.
Take-home points:
- Acetaminophen is hepatotoxic and must be used cautiously—or avoided—in clients with liver disease such as hepatitis B.
- Nurses should not independently alter prescribed medication doses; clarification with the prescriber is the safe approach.
- Always prioritize patient safety by questioning orders that could potentially harm clients with underlying conditions.
Tension Headaches And Migraines
The emergency department nurse is caring for a client with a migraine headache. Which drug would the nurse anticipate administering to abort the client’s migraine attack?
Explanation
Migraines are severe, recurrent headaches often accompanied by nausea, photophobia, and phonophobia. The goal of treatment during an acute migraine attack is to abort the headache quickly and effectively by targeting the underlying mechanisms, such as cranial vasodilation and neurogenic inflammation. Triptans, such as sumatriptan, are considered the first-line agents for acute migraine relief.
Rationale for correct answer:
D. Sumatriptan (Imitrex) is a serotonin (5-HT1B/1D) receptor agonist that works by producing cranial vasoconstriction and inhibiting neuropeptide release, both of which are central to stopping migraine pathophysiology. This makes it the most effective drug among the options for aborting an acute migraine attack. Patients typically experience rapid relief of headache pain and associated symptoms, which confirms its role as the treatment of choice.
Rationale for incorrect answers:
A. Morphine: While it may relieve pain, opioids are not recommended for migraines due to risk of dependency, rebound headaches, and lack of effect on the underlying cause. They are only considered when other therapies fail.
B. Propranolol (Inderal): This beta-blocker is effective for migraine prophylaxis but not for aborting an acute attack. It reduces the frequency and severity of future migraines rather than treating current symptoms.
C. Ibuprofen (Motrin): NSAIDs like ibuprofen may help with mild to moderate migraines, but they are not as effective as triptans for severe attacks. They may be used in combination therapy but are not the first-line choice for acute management in this scenario.
Take-home points:
- Sumatriptan is the first-line drug to abort acute migraine attacks because it directly addresses the underlying pathophysiology.
- Opioids are avoided in migraines due to risk of dependence and rebound headaches.
- NSAIDs may help mild migraines, but triptans are superior for moderate to severe attacks.
A patient is having a migraine attack. The nurse should know that which drugs are used to treat migraine attacks?
Explanation
Migraines are treated with two main strategies: preventive therapy to reduce frequency and abortive therapy to stop acute attacks. During a migraine episode, the priority is fast symptom relief. Triptans are the drug class most commonly prescribed for acute migraine treatment because they directly target serotonin receptors to reverse the vascular and neurochemical changes involved.
Rationale for correct answer:
A. Triptans:
These drugs (e.g., sumatriptan, rizatriptan) are first-line therapy for acute migraine attacks. They act as serotonin (5-HT1B/1D) receptor agonists, producing cranial vasoconstriction and reducing neuropeptide release, which alleviates pain and associated symptoms like nausea and photophobia.
Rationale for incorrect answers:
B. Anticonvulsants:
Agents like valproate and topiramate are used for migraine prevention, not for aborting acute attacks.
C. Tricyclic antidepressants:
Drugs such as amitriptyline are prescribed for prophylaxis of chronic migraines but are ineffective during an active attack.
D. Beta-adrenergic blockers:
Propranolol and similar drugs are also preventive agents for frequent migraines, not abortive therapy.
Take-home points:
- Triptans are the drugs of choice for treating acute migraine attacks.
- Preventive therapies (anticonvulsants, tricyclics, beta-blockers) do not stop active migraines.
- Patient teaching should include limiting triptan overuse to avoid rebound headaches.
Comprehensive Questions
A patient is taking aspirin for arthritis. Which adverse reaction should the nurse teach the patient to report to the health care provider?
Explanation
Aspirin is a salicylate commonly prescribed for its analgesic, antipyretic, and anti-inflammatory effects in conditions like arthritis. However, it carries a risk of toxicity (salicylism), especially with long-term or high-dose use. One of the earliest warning signs of toxicity is tinnitus, which must be promptly reported to prevent progression to severe complications.
Rationale for correct answer:
A. Tinnitus: Persistent ringing in the ears is a hallmark early symptom of salicylism. Reporting it immediately allows the provider to adjust the dose or discontinue therapy before more serious effects (vertigo, metabolic acidosis, respiratory depression) develop.
Rationale for incorrect answers:
B. Seizures: While seizures may occur in severe salicylate poisoning, they are a late and rare manifestation. The nurse should emphasize earlier warning signs like tinnitus rather than seizures.
C. Sinusitis: This is unrelated to aspirin use and not an expected adverse effect.
D. Palpitations: Aspirin does not typically cause palpitations. Cardiac symptoms are not primary concerns with salicylates.
Take-home points:
- Tinnitus is an early indicator of aspirin toxicity and must be reported promptly.
- Salicylism may progress to more severe CNS and metabolic effects if unrecognized.
- Patient teaching for long-term aspirin use should focus on GI safety (ulcer risk) and early signs of toxicity.
The nurse is teaching a patient about taking aspirin. Which are important points for the nurse to include? Select all that apply
Explanation
Aspirin is a widely used NSAID and antiplatelet agent with important implications for bleeding risk, GI irritation, and safety in children. Patient teaching is essential to prevent complications, especially when aspirin is used long term or in higher doses.
Rationale for correct answers:
A. Advise the patient to avoid alcohol while taking aspirin: Both aspirin and alcohol irritate the gastric mucosa, greatly increasing the risk of GI bleeding and ulcers.
C. Instruct the patient to inform the dentist of the aspirin dosage before having dental work: Since aspirin inhibits platelet aggregation, it increases the risk of bleeding during dental procedures. The dentist must be aware to take necessary precautions.
D. Instruct the patient to inform the surgeon of the aspirin dosage before having surgery: Aspirin’s antiplatelet effect lasts the life of a platelet (7–10 days). Surgeons often recommend discontinuing aspirin before surgery to reduce the risk of excessive bleeding.
Rationale for incorrect answers:
B. Instruct the patient to take aspirin before meals on an empty stomach: This is incorrect. Aspirin should be taken with food, milk, or water to reduce gastric irritation.
E. Suggest that aspirin may be given to children for flu symptoms: Aspirin should not be given to children with viral illnesses (such as influenza or chickenpox) because it increases the risk of Reye’s syndrome, a rare but potentially fatal condition.
Take-home points:
- Aspirin increases bleeding risk—patients must inform dentists and surgeons before procedures.
- Avoid alcohol while taking aspirin to reduce GI bleeding risk.
- Never give aspirin to children with viral illnesses due to the risk of Reye’s syndrome.
A patient requires a nonopioid medication. The nurse knows that which medication will cause the least gastrointestinal distress?
Explanation
Celecoxib is a COX-2 selective inhibitor that provides anti-inflammatory and analgesic effects while sparing COX-1 activity, which helps protect the gastric mucosa. Because of this selectivity, it causes less gastrointestinal irritation and ulceration than nonselective NSAIDs.
Rationale for correct answer:
C. Celecoxib: Unlike traditional NSAIDs, celecoxib selectively inhibits COX-2, reducing pain and inflammation while minimizing gastric irritation, ulcer risk, and GI bleeding associated with COX-1 inhibition.
Rationale for incorrect answers:
A. Aspirin: Strongly inhibits COX-1, making it highly irritating to the gastric mucosa and increasing the risk of ulcers and GI bleeding.
B. Ketorolac: A potent nonselective NSAID with a high risk of GI ulceration and bleeding, especially with prolonged use.
D. Ibuprofen: Less irritating than aspirin or ketorolac but still a nonselective COX inhibitor, so it carries moderate risk for GI upset and ulceration.
Take-home points:
- Celecoxib (COX-2 inhibitor) causes the least GI distress compared with other NSAIDs.
- Aspirin, ketorolac, and ibuprofen all inhibit COX-1, which increases the risk of gastric irritation and ulcers.
- Patients on any NSAID should be advised to take with food and report GI symptoms promptly.
A patient states during a medical history that he takes several acetaminophen tablets throughout the day. The nurse teaches the patient that the dosage should not exceed which amount?
Explanation
Acetaminophen is widely used for pain and fever, but overdose can cause severe hepatotoxicity. Safe dosing limits are critical to prevent liver damage, especially in patients taking multiple acetaminophen-containing products.
Rationale for correct answer:
C. 4 g/day:
The maximum recommended adult dose of acetaminophen is 4 grams per day when taken in divided doses. Exceeding this amount increases the risk of liver injury or acute liver failure, particularly in patients who consume alcohol or have preexisting liver disease.
Rationale for incorrect answers:
A. 1 g/day:
This is well below the therapeutic maximum. While safe, it may not provide adequate analgesia or antipyresis for adults.
B. 2 g/day:
This is below the recommended upper limit for healthy adults and may be unnecessarily restrictive for short-term use.
D. 6 g/day:
This exceeds the safe limit and significantly increases the risk of hepatotoxicity, even with short-term use.
Take-home points:
- Do not exceed 4 g/day of acetaminophen for adults.
- Assess all sources of acetaminophen, including combination OTC and prescription products.
- Monitor for signs of liver injury such as jaundice, dark urine, or abdominal pain in patients using high or chronic doses.
A patient is admitted to the emergency department in respiratory depression following self-injection with hydromorphone. The admitting nurse knows that which drug will reverse respiratory depression caused by opioid overdose?
Explanation
Hydromorphone is a potent opioid analgesic that, in overdose, can cause profound central nervous system and respiratory depression. In emergency situations, the priority is to restore adequate ventilation and prevent death. The specific antidote for opioid overdose is naloxone, an opioid receptor antagonist.
Rationale for correct answer:
B. Naloxone: Naloxone rapidly displaces opioids from the mu-opioid receptors in the CNS, reversing respiratory depression, sedation, and hypotension. It works within minutes when given IV, making it the drug of choice for opioid overdose emergencies.
Rationale for incorrect answers:
A. Fentanyl: Another opioid analgesic, fentanyl would worsen respiratory depression, not reverse it.
C. Butorphanol: This is a mixed agonist–antagonist opioid that can provide pain relief but will not reliably reverse life-threatening respiratory depression.
D. Sufentanil: An even stronger opioid analgesic than fentanyl, it would intensify opioid toxicity instead of reversing it.
Take-home points:
- Naloxone is the antidote for all opioid overdoses, including hydromorphone.
- It acts by blocking opioid receptors and rapidly restoring respiration.
- Other opioids (fentanyl, sufentanil, butorphanol) do not reverse overdose and may worsen the condition.
Assessing a patient following IV morphine administration, the nurse notes cold, clammy skin; a pulse of 40 beats/min; respirations of 10 breaths/min; and constricted pupils. Which medication will the patient likely need next?
Explanation
Morphine and other opioids can cause serious adverse effects when overdosed, including respiratory depression, bradycardia, hypotension, and pinpoint pupils. These are classic signs of opioid toxicity, and prompt reversal is critical to prevent respiratory and cardiac arrest. The antidote is naloxone (Narcan), an opioid receptor antagonist.
Rationale for correct answer:
A. Naloxone (Narcan): Naloxone binds to opioid receptors and displaces morphine, reversing respiratory depression, bradycardia, and CNS depression within minutes. It is the life-saving antidote in cases of opioid overdose.
Rationale for incorrect answers:
B. Meloxicam (Mobic): This is a nonsteroidal anti-inflammatory drug (NSAID) used for arthritis pain. It does not reverse opioid toxicity.
C. Pentazocine (Talwin): A mixed agonist–antagonist opioid. While it has some antagonistic activity, it is not appropriate for treating life-threatening respiratory depression.
D. Propoxyphene (Darvon): A weak opioid analgesic (now largely discontinued due to toxicity). It would worsen opioid overdose rather than treat it.
Take-home points:
- Naloxone is the emergency antidote for opioid overdose.
- Classic signs of opioid toxicity: respiratory depression, bradycardia, pinpoint pupils, cold/clammy skin.
- Prompt reversal prevents respiratory and cardiac arrest in opioid emergencies.
For the patient who is taking acetaminophen (Tylenol), what should the nurse do? Select all that apply
Explanation
Acetaminophen (Tylenol) is one of the most widely used analgesics and antipyretics. While generally safe at therapeutic doses, overdose or long-term use can cause hepatotoxicity. Nurses play a key role in teaching patients how to safely use acetaminophen, especially because it is present in many combination OTC medications. Patients with comorbid conditions, such as diabetes, also require specific teaching.
Rationale for correct answers:
A. Monitor routine liver enzyme tests:
Acetaminophen is metabolized by the liver, and excessive use can cause severe liver damage. Routine monitoring of liver enzymes (AST, ALT) is important, especially for patients on long-term therapy or with existing liver disease.
B. Encourage the patient to check package labels of OTC drugs to avoid overdosing:
Many cold, flu, and pain relief medications contain acetaminophen. Without careful attention, patients may unknowingly exceed the maximum daily dose (usually 4 g for adults), increasing the risk of hepatotoxicity.
C. Teach the diabetic patient taking acetaminophen to check blood glucose more frequently:
Acetaminophen may cause false readings with certain blood glucose monitors, particularly those using the glucose oxidase-peroxidase method. This makes frequent monitoring important for diabetic patients.
Rationale for incorrect answers:
D. Teach the female patient that oral contraceptives can increase the effect of acetaminophen:
Oral contraceptives actually increase the metabolism of acetaminophen, potentially decreasing its effectiveness, not increasing it.
E. Teach the patient that caffeine decreases the effects of acetaminophen:
Caffeine actually enhances the analgesic effect of acetaminophen and is sometimes included in combination medications (e.g., Excedrin).
Take-home points:
- Monitor liver function closely during acetaminophen therapy.
- Diabetic patients should check blood glucose more often while taking acetaminophen.
- Caffeine enhances, not decreases, acetaminophen’s pain-relieving action.
For the patient who is taking nalbuphine (Nubain), what should the nurse do? Select all that apply
Explanation
Nalbuphine (Nubain) is an opioid agonist-antagonist used for moderate to severe pain. While effective, it carries opioid-related risks such as respiratory depression and CNS effects, requiring close nursing monitoring and thorough patient teaching.
Rationale for correct answers:
A. Monitor any changes in respirations:
As with other opioids, nalbuphine can depress the respiratory center. Monitoring rate, depth, and pattern is critical, especially after IV administration.
B. Instruct the patient to report bradycardia:
Nalbuphine can slow heart rate. Patients must promptly report dizziness, faintness, or slow pulse to prevent complications.
C. Administer IV nalbuphine undiluted:
This drug may be given undiluted IV, usually slowly over 2 minutes, to reduce adverse effects like hypotension or respiratory depression.
E. Instruct the patient to avoid alcohol when taking nalbuphine to avoid respiratory depression:
Alcohol potentiates CNS and respiratory depression from opioids, so complete avoidance is essential.
Rationale for incorrect answer:
D. Explain to the patient to expect an excessive amount of urine output:
This is false. Nalbuphine does not increase urine output; instead, opioids may cause urinary retention.
Take-home points:
- Always monitor respiratory status and heart rate with nalbuphine.
- Give IV doses undiluted, administered slowly.
- Warn patients about alcohol and CNS depressant interactions.
A patient is receiving an opioid via a PCA pump as part of his postoperative pain management program. During rounds, the nurse finds him unresponsive, with respirations of 8 breaths/min and blood pressure of 102/58 mm Hg. After stopping the opioid infusion, what should the nurse do next?
Explanation
Opioid therapy via PCA (patient-controlled analgesia) is effective for postoperative pain, but overdose or accumulation can cause life-threatening respiratory depression. When a patient is found unresponsive with shallow respirations, the immediate priority is to reverse the opioid’s effects with an antagonist such as naloxone. Rapid intervention can prevent respiratory arrest and stabilize the patient before additional assessments or notifications are made.
Rationale for correct answer:
C. Administer an opiate antagonist per standing orders:
Naloxone is the antidote for opioid-induced respiratory depression. Given this patient’s unresponsiveness and low respiratory rate, reversal must occur immediately to restore adequate ventilation and prevent further complications.
Rationale for incorrect answers:
A. Notify the charge nurse:
While communication is important, notifying others delays lifesaving intervention. The nurse must act first to stabilize the patient.
B. Draw arterial blood gases:
ABG testing can help determine the extent of respiratory compromise, but it is a diagnostic step, not a priority in an emergency. Immediate reversal with naloxone takes precedence.
D. Perform a thorough assessment, including mental status examination:
A full assessment is important, but not before addressing the acute emergency of respiratory depression. Stabilization comes first, then further assessment.
Take-home points:
- Naloxone is the antidote for opioid-induced respiratory depression and must be administered immediately when a patient is unresponsive and hypoventilating.
- In emergencies, airway and breathing stabilization come before notification and diagnostics.
- Nurses must recognize signs of opioid toxicity early and act rapidly to prevent respiratory arrest.
A patient with bone pain caused by metastatic cancer will be receiving transdermal fentanyl patches. The patient asks the nurse what benefits these patches have. The nurse's best response includes which of these features?
Explanation
Transdermal fentanyl patches are a common choice for patients with chronic cancer-related pain because they provide continuous systemic absorption of the drug. This allows for stable plasma concentrations and sustained pain relief, reducing the peaks and troughs that occur with oral or injectable opioids. The patches are not free of adverse effects, but their main advantage is consistent analgesia.
Rationale for correct answer:
A. More constant drug levels for analgesia:
The patch delivers fentanyl steadily over 72 hours, ensuring stable pain control without the fluctuations seen with short-acting opioids. This makes it particularly useful for persistent cancer pain.
Rationale for incorrect answers:
B. Less constipation and minimal dry mouth:
Constipation and dry mouth are common opioid side effects regardless of the route. Fentanyl patches do not eliminate these adverse effects, so laxatives and oral care are still necessary.
C. Less drowsiness than with oral opioids:
Fentanyl can still cause CNS depression and drowsiness. The patch does not prevent this effect—it mainly changes how the drug is delivered.
D. Lower dependency potential and no major adverse effects:
Fentanyl is a potent opioid with the same risks of tolerance, dependence, and adverse effects as other opioids. It must be carefully monitored.
Take-home points:
- Transdermal fentanyl provides stable and continuous analgesia, which is ideal for chronic cancer pain.
- Side effects such as constipation, sedation, and dependency risks remain and require monitoring.
- The main advantage is avoiding peaks and troughs in pain relief, improving patient comfort and quality of life.
Intravenous morphine is prescribed for a patient who has had surgery. The nurse informs the patient that which common adverse effects can occur with this medication? Select all that apply
Explanation
Morphine is a potent opioid analgesic commonly used for postoperative pain. While effective for pain relief, it has several predictable adverse effects due to its action on the central nervous system and gastrointestinal tract. Nurses must educate patients about these effects and implement strategies to manage or prevent them.
Rationale for correct answers:
B. Constipation:
Opioids decrease gastrointestinal motility, leading to constipation. Patients should be encouraged to increase fluid intake, dietary fiber, and activity, and stool softeners or mild laxatives may be prescribed prophylactically.
C. Pruritus:
Morphine can cause itching due to histamine release. This is usually mild but may require antihistamines if bothersome.
E. Nausea:
Opioids often stimulate the chemoreceptor trigger zone, leading to nausea and sometimes vomiting. Anti-emetic medications may be needed.
Rationale for incorrect answers:
A. Diarrhea:
Morphine decreases gut motility rather than increases it, making diarrhea uncommon unless the patient has other contributing factors.
D. Urinary frequency:
Opioids may cause urinary retention rather than increased frequency, due to relaxation of bladder detrusor muscles and increased sphincter tone.
Take-home points:
- Constipation, pruritus, and nausea are common opioid adverse effects.
- Preventive measures, such as stool softeners and antiemetics, should be part of patient teaching.
- Monitor for these effects to ensure patient comfort and adherence to pain management therapy.
Several patients have standard orders for acetaminophen as needed for pain. While reviewing their histories and assessments, the nurse discovers that one of the patients has a contraindication to acetaminophen therapy. Which patient should receive an alternate medication?
Explanation
Acetaminophen is a widely used analgesic and antipyretic. While generally safe, it is primarily metabolized by the liver, and excessive or prolonged use can cause hepatotoxicity. Nurses must assess liver function and consider alternative pain management for patients with significant hepatic impairment.
Rationale for correct answer:
C. A patient admitted with severe hepatitis:
Acetaminophen is contraindicated in patients with active liver disease because it can exacerbate liver injury. Even standard doses may pose a risk in severe hepatic impairment, so an alternate analgesic should be chosen.
Rationale for incorrect answers:
A. A patient with a fever of 103.4°F (39.7°C):
Fever is a standard indication for acetaminophen. It is safe and effective for reducing elevated body temperature.
B. A patient admitted with deep vein thrombosis:
Acetaminophen does not affect coagulation or increase thrombotic risk, making it safe in this context.
D. A patient who had abdominal surgery 1 week earlier:
Postoperative pain is a common indication for acetaminophen. It can be safely used unless there is concurrent liver disease.
Take-home points:
- Acetaminophen is hepatotoxic at high doses or in patients with liver disease.
- Always review patient history for liver impairment before administration.
- Consider alternative analgesics in patients with active hepatitis or severe liver dysfunction.
The nurse is administering an intravenous dose of morphine sulfate to a 48-year-old postoperative patient. The dose ordered is 3 mg every 3 hours as needed for pain. The medication is supplied in vials of 4 mg/mL. How much will be drawn into the syringe for this dose?
Explanation
Accurate dosage calculation is essential in nursing practice to ensure patient safety and effective pain management. When administering intravenous medications like morphine sulfate, the nurse must carefully convert the ordered dose into the correct volume based on the supplied concentration.
Rationale for correct answers:
Step-by-Step Calculation
To determine the volume of medication to administer, you can use the following formula:
Volume(mL)=ConcentrationSupplied(mg/mL)DoseOrdered(mg)
- Identify the ordered dose: The order is for 3 mg of morphine sulfate.
- Identify the concentration supplied: The vial is supplied as 4 mg/mL.
- Calculate the volume: Volume(mL)=4mg/mL3mg=0.75mL
Therefore, the nurse will draw 0.75 mL into the syringe for this dose.
Take-home points:
- Always use the formula: Volume (mL) = (Dose Ordered ÷ Dose on Hand) × Volume on Hand.
- Double-check the medication concentration on the vial before calculating to avoid errors.
- Correctly calculated, a 3 mg dose from a 4 mg/mL supply equals 0.75 mL to be drawn.
An opioid analgesic is prescribed for a patient. The nurse checks the patient's medical history knowing this medication is contraindicated in which disorder? Select all that apply
Explanation
Opioid analgesics are effective for moderate to severe pain but have significant central nervous system and respiratory depressant effects. Nurses must assess for conditions that increase the risk of respiratory compromise or intracranial pressure before administration.
Rationale for correct answers:
B. Severe asthma:
Opioids can depress respiratory drive and reduce the body’s response to hypoxia and hypercapnia. In patients with severe asthma, this can precipitate life-threatening respiratory compromise.
C. Sleep apnea:
Patients with sleep apnea already have intermittent airway obstruction during sleep. Opioids can worsen hypoventilation and apnea episodes, increasing the risk of severe hypoxia.
D. Severe head injury:
Opioids can increase intracranial pressure and mask changes in neurological status, making monitoring of head injury patients more difficult and potentially dangerous.
Rationale for incorrect answers:
A. Renal insufficiency:
Opioids can be used with caution in renal impairment, adjusting doses if necessary. They are not strictly contraindicated.
E. Liver disease:
Most opioids are metabolized by the liver, so caution and dose adjustment may be needed, but they are not absolute contraindications unless there is severe hepatic failure.
Take-home points:
- Opioids can depress respiration, so avoid in severe asthma, sleep apnea, and head injury.
- Dose adjustments may be necessary for renal or hepatic impairment, but these conditions are not absolute contraindications.
- Always monitor for signs of respiratory depression and CNS changes in high-risk patients.
While preparing aspirin for a patient, the nurse reviewed which of the pharmacologic effects of salicylates? Select all that apply
Explanation
Aspirin is a salicylate with multiple pharmacologic actions, but its main therapeutic effects are pain relief, reduction of inflammation, and fever reduction. Understanding these effects helps guide its appropriate clinical use and patient education.
Rationale for correct answers:
A. Analgesic:
Aspirin inhibits prostaglandin synthesis, which reduces pain, making it effective for mild to moderate pain such as headaches, musculoskeletal pain, or postoperative discomfort.
D. Anti-inflammatory:
By inhibiting cyclooxygenase (COX) enzymes, aspirin reduces the production of prostaglandins involved in inflammation, making it useful in conditions like arthritis.
F. Antipyretic:
Aspirin acts on the hypothalamic heat-regulating center to lower fever, helping manage febrile conditions.
Rationale for incorrect answers:
B. Anesthetic:
Aspirin does not produce loss of sensation. Local or general anesthetics are required for that effect.
C. Antidote:
Aspirin cannot reverse toxic effects of other drugs; it has no antidotal properties.
E. Antiemetic:
Aspirin does not prevent nausea or vomiting. Other medications like ondansetron are used for that purpose.
G. Antiepileptic:
Aspirin does not prevent seizures; antiepileptic drugs are required for seizure control.
Take-home points:
- Aspirin’s primary actions are analgesic, anti-inflammatory, and antipyretic.
- It does not act as an anesthetic, antidote, antiemetic, or antiepileptic.
- Understanding these effects ensures safe and effective use while minimizing unnecessary or ineffective administration.
Exams on Drugs Used for Pain Management
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define pain and differentiate acute versus chronic pain, and explain how classification guides treatment strategies.
- List and describe nonpharmacologic pain management techniques and explain their role in reducing medication use and side effects.
- Identify opioid receptor types (mu, kappa, delta, nociceptin) and summarize the mechanism, indications, and adverse effects of opioid agonists.
- Explain the use of opioid antagonists and mixed agonist–antagonist opioids in reversing overdose, managing dependence, and providing analgesia.
- Describe NSAIDs and acetaminophen in terms of mechanism, therapeutic use, contraindications, adverse effects, and nursing considerations.
- Compare centrally acting analgesics (tramadol, ziconotide) regarding mechanism, indications, and safety considerations.
- Identify tension and migraine headaches, including triggers, symptoms, and appropriate pharmacologic and nonpharmacologic management.
- Explain the use of antimigraine medications (triptans, ergot alkaloids, prophylactic drugs, Botox) in aborting and preventing migraines, including precautions and nursing responsibilities.
Introduction
- Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, often described in terms of severity, quality, and location.
- Defense mechanism: Pain alerts the body to injury, promoting avoidance of harmful situations and encouraging patients to seek timely medical evaluation.
- Psychological and emotional influences: Anxiety, fatigue, depression, and stress can heighten pain perception, whereas positive mental attitude, patient education, and caregiver support can help reduce the intensity of pain experienced.

- Clinical relevance: Effective pain management requires comprehensive understanding of the source, type, intensity, and duration of pain, as well as consideration of patient-specific factors including age, comorbidities, and prior pain experiences.
- Universal experience: All humans encounter pain in some form, making standardized assessment essential for both acute and chronic pain management.
Assessment and Classification of Pain
-
Subjective experience: Pain is inherently subjective; two patients with identical injuries may report vastly different pain levels.
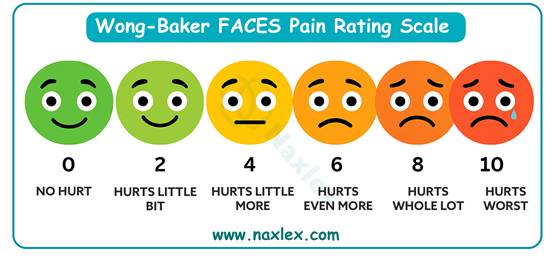
- Assessment tools:
- Numeric Rating Scales (0–10)
- Visual Analog Scales (VAS)
- Wong-Baker Faces Pain Rating Scale (especially for children)
- McGill Pain Questionnaire
- NIH Pain Consortium provides standardized scales for clinical use: http://painconsortium.nih.gov/pain_scales/index.html
- Classification by duration:
- Acute pain: Short-term, sudden onset, typically linked to injury, surgery, or illness; serves as a warning sign.
- Chronic pain: Lasts >6 months, persists beyond normal healing time, interferes with ADLs, and may cause depression, sleep disturbances, and social withdrawal.
- Classification by source:
- Nociceptive pain: Pain resulting from tissue damage.
- Somatic: Localized, sharp, aching, throbbing (e.g., cuts, fractures, arthritis).
- Visceral: Diffuse, dull, poorly localized, often associated with internal organs (e.g., pancreatitis, myocardial ischemia).
- Neuropathic pain: Caused by nerve injury or dysfunction. Described as burning, shooting, tingling, or numbness (e.g., diabetic neuropathy, postherpetic neuralgia).
- Nociceptive pain: Pain resulting from tissue damage.
- Importance in clinical care: Correct classification guides pharmacologic selection, nonpharmacologic interventions, and patient education.
Nonpharmacologic Techniques for Pain Management
-
Purpose: Reduce pain perception, enhance comfort, and potentially lower the dose of medications, minimizing adverse effects.
- Examples:
- Acupuncture: Stimulates specific points to modulate pain pathways.

-
- Biofeedback therapy: Teaches patients to control physiological responses, reducing pain perception.
- Massage therapy: Promotes circulation, reduces muscle tension.
- Heat or cold therapy: Heat relaxes muscles; cold decreases inflammation and nerve conduction.
- Meditation, relaxation, and prayer: Reduces anxiety and stress that exacerbate pain.
- Art or music therapy: Distracts and soothes the mind, reducing pain awareness.
- Imagery and hypnosis: Cognitive methods to alter pain perception.
- Chiropractic manipulation and physical therapy: Corrects musculoskeletal alignment and strengthens supportive structures.

-
- Therapeutic touch and TENS (Transcutaneous Electrical Nerve Stimulation): Provides sensory distraction to block pain signals.
- Cancer pain considerations:
- Intractable pain may require nerve blocks, tumor debulking, radiation therapy, or surgical interventions.
- Topical agents like capsaicin create reversible pain blockade, providing local relief without systemic side effects.
Neural Mechanisms of Pain
-
Nociceptors: Free nerve endings sensitive to mechanical, thermal, or chemical stimuli.
- Sensory fibers:
- Aδ fibers: Myelinated → fast transmission → sharp, localized pain.
- C fibers: Unmyelinated → slow transmission → dull, aching pain.
- Neurotransmitters:
- Substance P: Facilitates transmission of pain signals to the spinal cord and brain.
- Endogenous opioids: Endorphins, dynorphins, enkephalins modulate pain perception by inhibiting neurotransmitter release.
- Pharmacologic intervention targets:
- CNS: Opioids reduce central perception of pain.
- Peripheral tissues: NSAIDs reduce inflammation and nociceptor activation.
- Pain modulation: Cognitive, emotional, and sensory inputs influence pain perception via descending inhibitory pathways.
Opioid Analgesics
Classification
- Natural Opiates: Derived from the opium poppy (Papaver somniferum).
- Morphine: Gold standard for severe pain; used for post-operative pain, cancer pain, and severe chronic pain. Rapidly absorbed orally; metabolized in liver to morphine-3-glucuronide and morphine-6-glucuronide (active).
- Codeine: Mild-to-moderate pain, often combined with acetaminophen. Also an effective antitussive. Metabolized in the liver by CYP2D6 to morphine, which contributes to its analgesic effect. Genetic polymorphisms may affect efficacy.
- Synthetic Opioids: Chemically synthesized; potent, with variable duration.
- Meperidine (Demerol): Short-acting, moderate pain relief. Risk of neurotoxicity (normeperidine) in renal impairment or elderly → tremors, seizures.
- Fentanyl: Extremely potent, rapid onset, short duration. Used for anesthesia, chronic pain (transdermal patches), and breakthrough cancer pain. Highly lipophilic → crosses blood-brain barrier quickly.
- Hydromorphone (Dilaudid): Potent opioid, shorter half-life than morphine; preferred in renal dysfunction as less accumulation occurs.
- Methadone: Long-acting opioid, NMDA receptor antagonist → useful in neuropathic pain and opioid dependence treatment. Risk of QT prolongation.
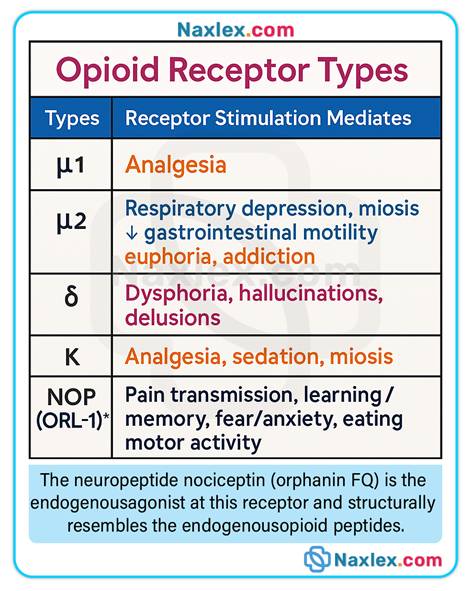
- Opioid Receptors & Mechanism of Action:
- Bind CNS and peripheral receptors:
- Mu (μ): Analgesia, euphoria, respiratory depression, sedation, constipation, miosis.
- Kappa (κ): Analgesia, sedation, dysphoria.
- Delta (δ): Modulate analgesia, may affect mood and emotional response.
- Nociceptin (NOP): Pain modulation, tolerance development.
- Bind CNS and peripheral receptors:
- Types of Opioids:
- Agonists: Full stimulation → potent analgesia; high dependence risk.
- Antagonists: Block receptors → reverse opioid toxicity.
- Mixed Agonist–Antagonists: Partial activity → moderate analgesia, lower respiratory depression; safe in some patients with risk of abuse.
- Clinical Relevance:
- Assess pain using standard scales before and after opioid administration.
- Monitor for respiratory depression, sedation, and hypotension.
- Educate patients about safe opioid use and not to combine with CNS depressants (alcohol, benzodiazepines).
Opioid Agonists
-
Prototype: Morphine – gold standard for severe pain; used in PCA pumps, oral extended-release formulations, IV bolus for acute pain.
-
Other Common Agents: Fentanyl, Hydromorphone, Methadone, Oxycodone, Oxymorphone, Hydrocodone.
- Indications:
- Severe acute or chronic pain (post-surgery, trauma, burns).
- Cancer-related pain and palliative care.
- Adjunct therapy for dyspnea in end-stage heart failure or pulmonary edema.
- Off-label uses: Sedation for mechanically ventilated patients, severe anxiety.
- Mechanism of Action:
- Bind primarily mu and kappa receptors → inhibit ascending nociceptive signals → alter pain perception and emotional response.
- Indirectly modulate neurotransmitters (dopamine, serotonin) → euphoria and sedation.
- Additional Therapeutic Effects:
- Antitussive: Codeine suppresses cough.
- Antidiarrheal: Slows GI motility; useful in severe diarrhea.
- CNS Depressant: Reduces anxiety, promotes rest in critically ill patients.
- Adverse Effects:
- Respiratory depression: Most serious; monitor RR <10/min, use naloxone if needed.
-
- Constipation: Often requires preventive stool softeners or laxatives.
- Nausea and vomiting: Common initially; may diminish with tolerance.
- Sedation/euphoria: Risk of abuse and dependence.
- Urinary retention: Monitor in older men with BPH or renal impairment.
- Pruritus: Often histamine-mediated.
- Dependence Potential: High; Schedule II drugs include fentanyl, morphine, oxycodone.
- Administration Routes: Oral (immediate or extended-release), IV, subcutaneous, PCA pumps, transdermal patches, buccal, sublingual, intranasal.
- Combination Therapy:
- Opioid + nonopioid (acetaminophen, NSAIDs) → opioid-sparing, reduces adverse effects.
- Examples: Vicodin (hydrocodone + acetaminophen), Percocet (oxycodone + acetaminophen), Tylenol with Codeine.
- Tip: Monitor total acetaminophen dose (≤4 g/day) to prevent hepatotoxicity.
- Nursing Insights:
- Assess pain scale before and after administration.
- Monitor vital signs and sedation levels.
- Educate patients and families about opioid safety, fall risk, and constipation prevention.
Opioid Antagonists
-
Examples: Naloxone (Narcan), Naltrexone.
- Uses:
- Reverse opioid overdose, respiratory depression, and sedation.
- Acute toxicity management.
- Diagnostic tool to distinguish opioid vs nonopioid overdose.
- Naltrexone: Maintenance therapy for opioid or alcohol dependence.
- Mechanism: Competitive inhibition at opioid receptors → displaces opioids, reversing effects.
- Administration:
- IV, IM, subcutaneous, intranasal.
- Rapid onset with IV naloxone; short half-life → repeated dosing may be needed.
- Nursing Insights:
- Titrate carefully in chronic opioid users → prevent acute withdrawal.
- Monitor for return of pain, vital signs, and signs of withdrawal.
- Educate patients/families on emergency use of naloxone.
Mixed Agonist–Antagonists
-
Examples: Buprenorphine, Pentazocine, Nalbuphine.
- Mechanism: Partial receptor activation → analgesia with lower respiratory depression and lower abuse potential.
- Clinical Uses:
- Moderate pain where full agonists are contraindicated.
- Opioid withdrawal therapy and addiction management.
- Postoperative analgesia in patients at risk for opioid misuse.
- Nursing Insights:
- Combining with full agonist opioids may precipitate withdrawal or reduce analgesia.
- Monitor for dizziness, sedation, nausea, mild respiratory depression.
- Educate patients on safe use and avoidance of other CNS depressants.
Treatment for Opioid Dependence

- Methadone:
- Long-acting oral opioid; reduces euphoria, stabilizes function, prevents withdrawal.
- Requires supervised programs; risk of QT prolongation.
- Buprenorphine (Buprenex, Butrans, Suboxone):
- Partial agonist → safer, prevents withdrawal.
- Can be used outpatient with monitoring.
- Suboxone:
- Buprenorphine + naloxone → reduces abuse potential.
- Used for long-term maintenance therapy.
- Nursing Insight:
- Monitor adherence, misuse, withdrawal symptoms.
- Assess cardiovascular status (QT interval with methadone).
- Educate patients on tapering and avoiding abrupt discontinuation.
Nonopioid Analgesics
NSAIDs
-
Mechanism: Inhibit COX-1 and COX-2 → reduce prostaglandins → decrease pain, inflammation, fever.
- Examples:
- First-generation: Aspirin, Ibuprofen (Motrin, Advil), Naproxen (Aleve), Indomethacin, Diclofenac (Voltaren), Ketorolac, Meloxicam.
- Second-generation (COX-2 selective): Celecoxib (Celebrex).
- Therapeutic Uses:
- Mild-to-moderate pain (musculoskeletal, post-operative, arthritis).
- Anti-inflammatory → RA, OA.
- Fever reduction.
- Dysmenorrhea.
- Aspirin → inhibits platelet aggregation → cardio-protection.
- Complications & Nursing Interventions:
- GI discomfort: Take with food or milk; monitor for ulcers/bleeding; use PPIs or H2 blockers if necessary.
- Renal dysfunction: Monitor I&O, BUN, creatinine; avoid in severe CKD.
- Cardiovascular risk: COX-2 inhibitors increase risk of MI/stroke; use lowest effective dose.
- Salicylism (aspirin): Tinnitus, headache, dizziness, sweating, respiratory alkalosis; stop drug if symptoms occur.
-
- Reye Syndrome: Avoid aspirin in children/adolescents with viral illness.
- Aspirin toxicity: Emergency management → cooling, IV fluids, bicarbonate, gastric lavage, activated charcoal, hemodialysis if severe.
- Contraindications/Precautions:
- Pregnancy (Category D), peptic ulcer disease, bleeding disorders, hypersensitivity, children/adolescents with viral infection.
- Use cautiously in older adults, smokers, H. pylori infection, asthma, alcoholism.
- Celecoxib contraindicated in sulfonamide allergy; ketorolac contraindicated in advanced renal dysfunction.
- Drug Interactions:
- Anticoagulants → increased bleeding risk. Monitor PT/INR, PTT.
- Glucocorticoids → increased GI bleeding risk.
- Alcohol → avoid; risk of GI bleeding.
- Ibuprofen may reduce cardioprotective effects of low-dose aspirin.
- Nursing Administration:
- Take NSAIDs with food, milk, or water.
- Stop aspirin 1 week before surgery.
- Ketorolac → short-term use (<5 days), often with opioids for opioid-sparing.
- IV ibuprofen → infuse over 30 minutes, ensure hydration.
- Evaluation of Effectiveness:
- Reduction in inflammation, pain, fever.
- Absence of injury or discomfort.
Acetaminophen
-
Mechanism: Inhibits prostaglandin synthesis centrally in CNS; antipyretic and analgesic.
- Advantages:
- No GI irritation, platelet inhibition, or cardiotoxicity.
- Safe for patients with PUD or anticoagulation.
- Limitations:
- No anti-inflammatory effect.
- Hepatotoxicity >4 g/day; caution in alcohol use.
- Nursing Insights:
- Monitor total acetaminophen from all sources.
- Educate patients to avoid exceeding 4 g/day.
-
- Administer antidote acetylcysteine for overdose.
- Interactions:
- Alcohol → increases risk of liver damage.
- Warfarin → may increase bleeding risk; monitor PT/INR.
- Evaluation of Effectiveness:
- Relief of mild-moderate pain.
- Reduction of fever.
Centrally Acting Drugs
-
Tramadol:
- Weak opioid; inhibits norepinephrine and serotonin reuptake → spinal analgesia.
-
- Adverse effects: Dizziness, vertigo, headache, nausea, vomiting, constipation, sedation.
- Less respiratory depression than full opioids; used for moderate pain.
- Ziconotide:
- Delivered intrathecally; blocks N-type calcium channels in CNS → potent analgesia.
- Reserved for severe, refractory chronic pain.
- Side effects: psychiatric (anxiety, hallucinations), neurological.
Tension Headaches And Migraines
Tension Headaches
- Muscle tightness in head/neck → stress, anxiety, fatigue, poor posture.
- Symptoms: Steady, dull, pressure-like, often bilateral, may last hours to days.
- Treatment:
- OTC: Aspirin, Ibuprofen, Acetaminophen.
- Prescription: Butalbital combinations (Fioricet), Phrenilin.
- Nonpharmacologic: Stress management, relaxation, yoga, posture correction, heat/cold therapy.
- Nursing Insights: Educate patients to identify triggers, avoid overuse to prevent rebound headaches.
Migraines
- Symptoms: Unilateral, pulsating/throbbing pain, aura, nausea, vomiting, photophobia, phonophobia.
- Triggers: Nitrates, MSG, red wine, caffeine, chocolate, aspartame, hormonal changes, stress, perfumes, sleep deprivation.
- Treatment Goals:
- Abort acute attacks promptly.
- Prevent future attacks with prophylactic therapy.
- Impact: Severe migraines interfere with ADLs, work, social life. Early intervention improves outcomes.
ANTIMIGRAINE DRUGS
Triptans
- Examples: Sumatriptan, Rizatriptan, Zolmitriptan.
- Mechanism: 5-HT1 receptor agonist → intracranial vasoconstriction, inhibits neurogenic inflammation → reduces pain signaling.
- Formulations: Oral, intranasal, subcutaneous, prefilled syringe.
- Adverse Effects: Chest tightness, dizziness; contraindicated in ischemic heart disease, uncontrolled hypertension.
Ergot Alkaloids
-
Examples: Ergotamine, Dihydroergotamine (DHE 45).
- Mechanism: Serotonergic agonist; also interacts with adrenergic and dopaminergic receptors → vasoconstriction.
- Precautions: Pregnancy Category X; risk of ergotism (ischemia, vasospasm).
- Nursing Insights: Monitor for chest pain, numbness, tingling, vascular compromise.
Prophylactic Therapy
-
Drug Classes:
- Beta-blockers (Propranolol, Timolol) → prevent vasodilation, reduce migraine frequency.
- Antidepressants (Amitriptyline, Venlafaxine) → modulate serotonin/norepinephrine; improve sleep.
- Antiseizure drugs (Topiramate, Valproate) → stabilize neuronal hyperexcitability.
- Calcium channel blockers (Verapamil) → reduce vascular spasm.
- Neuromuscular blockers → reduce head/neck muscular tension.
- Botox (OnabotulinumtoxinA): Blocks acetylcholine release → inhibits neuromuscular transmission → reduces chronic migraine frequency (3 months).
- Nursing Insights:
- Educate patients on trigger avoidance, medication adherence, and proper injection timing for Botox.
- Monitor for adverse effects: hypotension, fatigue, mood changes, GI upset depending on prophylactic therapy.
Summary
Pain is a complex, subjective experience that serves as a protective mechanism alerting the body to injury or potential harm.
Effective pain management requires accurate assessment using standardized scales, classification by duration (acute vs. chronic) and type (nociceptive vs. neuropathic), and consideration of patient-specific factors such as age, comorbidities, and psychological state.
Nonpharmacologic interventions—including heat/cold therapy, massage, acupuncture, biofeedback, relaxation, and TENS—play a key role in reducing pain perception, enhancing comfort, and minimizing medication doses and side effects.
Opioid analgesics act on mu, kappa, delta, and nociceptin receptors to modulate pain centrally and peripherally.
Full agonists like morphine, fentanyl, and hydromorphone provide potent analgesia but carry risks of respiratory depression, sedation, constipation, and dependence.
Antagonists (naloxone, naltrexone) reverse opioid toxicity, while mixed agonist–antagonists and partial agonists (buprenorphine) offer safer alternatives in select patients or for dependence treatment.
Nonopioid analgesics include NSAIDs and acetaminophen.
NSAIDs inhibit COX enzymes to reduce inflammation, pain, and fever but pose risks of GI bleeding, renal impairment, and cardiovascular events.
Acetaminophen provides analgesia and antipyresis with minimal GI or cardiovascular effects but carries a risk of hepatotoxicity with excessive dosing.
Centrally acting drugs like tramadol and ziconotide offer alternative mechanisms for moderate to severe pain, with unique safety profiles.
Headaches are classified mainly as tension or migraine. Tension headaches often result from muscle tension and stress, while migraines are triggered by vascular and neurologic factors.
Treatment strategies combine pharmacologic agents (OTC analgesics, triptans, ergot alkaloids, prophylactic medications, Botox) with nonpharmacologic interventions (stress management, relaxation, trigger avoidance) to abort acute attacks and prevent recurrence.
Overall, safe and effective pain management relies on individualized assessment, multimodal interventions, patient education, and ongoing evaluation of treatment efficacy and adverse effects.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Pain Management
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


