Please set your exam date
Abruptio Placentae
Study Questions
Practice Exercise 1
A nurse is assessing a client with suspected abruptio placentae. Which of the following findings requires immediate intervention?
Explanation
Abruptio placentae involves the premature separation of a normally implanted placenta from the uterine wall before delivery. This detachment disrupts the maternal-fetal interface, leading to hemorrhage and impaired gas exchange. Significant placental abruption triggers maternal hypovolemic shock and fetal hypoxia, often manifesting as board-like abdominal rigidity and severe uterine tenderness.
Rationale for correct answer
The presence of maternal hypotension and tachycardia indicates compensated shock or impending circulatory collapse due to concealed or overt hemorrhage. These vital sign changes signal a critical loss of intravascular volume, necessitating rapid fluid resuscitation and potential emergency delivery.
Rationale for incorrect answers
Mild vaginal spotting is frequently associated with early placental separation or other cervical changes. While it requires monitoring, it does not always indicate life-threatening hemorrhage or immediate hemodynamic instability. This finding is less urgent than signs of active shock in the mother.
A fetal heart rate of 140 beats/min with moderate variability is a reassuring finding indicating adequate fetal oxygenation. Moderate variability reflects a healthy fetal nervous system responding to the environment. This does not require immediate intervention as it represents a Category 1 fetal heart rate tracing.
Intermittent uterine contractions are often observed in various stages of pregnancy and can occur with minor placental irritation. In abruptio placentae, the classic finding is uterine hypertonicity or high-frequency, low-amplitude contractions. Intermittent contractions alone do not signal acute distress requiring emergency surgical or medical intervention.
Test-taking strategy
- Identify the clinical urgency: The question asks for an immediate intervention, which directs the nurse to prioritize life-threatening complications.
- Apply ABC principles: Analyze the options for threats to Airway, Breathing, or Circulation.
- Evaluate maternal stability: Choice 3 (Hypotension and tachycardia) directly impacts maternal hemodynamics and indicates a circulatory crisis.
- Rule out stable findings:
- Choice 1 is a common symptom but not an acute emergency compared to shock.
- Choice 2 is a normal physiological response for a fetus.
- Choice 4 describes non-pathological contraction patterns.
- Select the option that indicates physiological instability and requires rapid resuscitation to prevent maternal or fetal mortality.
Take home points
- Abruptio placentae is characterized by painful vaginal bleeding and uterine tenderness.
- Maternal shock can occur even with minimal visible bleeding if the hemorrhage is concealed behind the placenta.
- Immediate intervention is required when vital signs indicate maternal hemodynamic compromise or fetal distress.
- Disseminated intravascular coagulation is a severe potential complication of placental abruption due to the release of thromboplastin.
A nurse assesses a client at 36 weeks gestation with sudden onset of severe abdominal pain and a rigid uterus. Which of the following conditions does the nurse suspect?
Explanation
Abruptio placentae involves the premature separation of a normally implanted placenta from the uterine wall before delivery. This detachment disrupts the maternal-fetal interface, leading to hemorrhage and impaired gas exchange. Significant placental abruption triggers maternal hypovolemic shock and fetal hypoxia, often manifesting as board-like abdominal rigidity and severe uterine tenderness.
Rationale for correct answer
2. The sudden onset of severe abdominal pain accompanied by a rigid uterus is the classic clinical presentation of placental abruption. The rigidity occurs due to extravasation of blood into the myometrium, causing significant uterine irritability and hypertonicity. These findings distinguish this obstetric emergency from other causes of late-pregnancy bleeding.
Rationale for incorrect answers
1. Placenta previa typically presents as painless bleeding in the third trimester of pregnancy. The placenta is implanted over or near the internal os, and it does not typically cause uterine rigidity or severe pain. Physical examination would reveal a soft, non-tender uterus rather than the firm, board-like abdomen seen here.
3. Preterm labor involves regular uterine contractions that result in cervical change before 37 weeks gestation. While contractions can be painful, they are usually intermittent rather than constant and severe. The uterus relaxes between contractions in preterm labor, unlike the sustained hypertonicity observed in a significant abruption.
4. Uterine atony is the failure of the uterus to contract effectively after delivery, leading to postpartum hemorrhage. It is characterized by a soft, boggy uterus upon palpation rather than a rigid one. Because the client in the scenario is still at 36 weeks gestation, atony is not a relevant diagnostic consideration.
Test-taking strategy
- Identify the cardinal signs: The question provides "sudden onset," "severe pain," and "rigid uterus" as the primary data points.
- Contrast painful vs. painless: In obstetric nursing, a major differentiator for third-trimester bleeding is the presence of pain. Abruptio is painful; Previa is painless.
- Assess uterine tone: A "rigid" or "board-like" uterus is a specific indicator of concealed or overt hemorrhage within the uterine wall, ruling out atony or normal labor.
- Apply gestational timing: The client is at 36 weeks, focusing the assessment on antepartum complications rather than postpartum issues like atony.
- Use a rule-out method:
- Rule out 1 because previa lacks severe pain and rigidity.
- Rule out 3 because labor contractions are intermittent and the uterus relaxes.
- Rule out 4 because atony occurs after birth and presents as "boggy," not rigid.
Take home points
- Abruptio placentae is a leading cause of maternal and fetal morbidity characterized by painful bleeding and uterine hypertonicity.
- A rigid, board-like abdomen is a hallmark sign indicating that blood has infiltrated the uterine muscle fibers.
- Management requires immediate assessment of maternal hemodynamic stability and fetal heart rate patterns.
- Distinguishing between placenta previa and abruption is critical, as vaginal exams are contraindicated in suspected previa but not necessarily in abruption.
A nurse is caring for a client with abruptio placentae. Which of the following are clinical manifestations associated with this condition? Select all that apply
Explanation
Abruptio placentae involves the premature separation of a normally implanted placenta from the uterine wall, leading to decidual hemorrhage and compromised fetal oxygenation. The accumulation of blood between the placenta and myometrium causes uterine hypertonicity and severe localized pain. This condition often results in consumptive coagulopathy, specifically disseminated intravascular coagulation, if thromboplastin is released into the maternal circulation from the damaged placental site.
Rationale for correct answers
1. The presence of painful uterine tenderness occurs as blood infiltrates the myometrium, causing significant tissue irritation and nerve stimulation. In abruptio placentae, the pain is often sudden, constant, and severe, distinguishing it from labor. This clinical hallmark results from the physical detachment and subsequent hematoma formation behind the placental plate.
2. A board-like uterine rigidity is a classic sign of a concealed hemorrhage where blood remains trapped within the uterine cavity. This internal pressure causes the uterus to become perpetually firm and unable to relax between contractions. This finding is a critical indicator of maternal hemodynamic risk and potential uterine rupture or ischemia.
4. Fetal heart rate abnormalities occur due to the direct disruption of the placental perfusion and gas exchange interface. As the surface area for nutrient transfer decreases, the fetus may exhibit late decelerations or sustained bradycardia. These abnormal tracings signal acute fetal hypoxia and necessitate immediate medical evaluation for emergency delivery.
Rationale for incorrect answers
3. Painless bright red vaginal bleeding is the defining characteristic of placenta previa, not abruptio placentae. In previa, the placenta is located over the cervical os, and bleeding occurs without the significant muscular irritation or hypertonicity seen in abruption. Identifying the absence of pain is a primary diagnostic step in differentiating between these two major causes of third-trimester bleeding.
5. A soft, non-tender uterus is the expected physical finding in a normal pregnancy or in a client with placenta previa. In contrast, abruptio placentae causes the uterus to become extremely irritable and firm to the touch. Finding a soft uterus effectively rules out the diagnosis of a significant placental separation where blood has accumulated within the myometrium.
Test-taking strategy
- Identify the Main Idea: The question focuses on the clinical manifestations of abruptio placentae, which is a "painful" obstetric emergency.
- Differentiate Pathophysiology: Contrast Abruption (premature separation, painful, rigid) with Previa (abnormal implantation, painless, soft).
- Categorize Symptoms:
- Uterine Tone: Look for terms like rigid, firm, or hypertonic (Choices 1 and 2).
- Pain Status: Select painful clinical findings over painless ones (Rule out Choice 3).
- Fetal Impact: Recognize that any placental separation compromises fetal oxygenation (Choice 4).
- Rule out the "Normals": A soft, non-tender uterus (Choice 5) is inconsistent with the internal bleeding and pressure associated with abruption.
- Selection: Choose all options that align with the inflammatory and hemorrhagic nature of placental detachment.
Take home points
- Abruptio placentae presents with the triad of abdominal pain, uterine rigidity, and vaginal bleeding.
- Uterine rigidity, often described as board-like, indicates a concealed hemorrhage with high internal pressure.
- Fetal distress is a common and early complication due to reduced uteroplacental blood flow.
Maternal vital signs must be monitored closely for signs of shock, even if external bleeding appears minimal.
A nurse explains abruptio placentae to a client. Which of the following best describes the primary cause of bleeding in this condition?
Explanation
Abruptio placentae involves the premature separation of a normally implanted placenta from the uterine wall before delivery. This detachment disrupts the maternal-fetal interface, leading to hemorrhage and impaired gas exchange. Significant placental abruption triggers maternal hypovolemic shock and fetal hypoxia, often manifesting as board-like abdominal rigidity and severe uterine tenderness.
Rationale for correct answer
2. The primary cause of bleeding is the mechanical detachment of the placenta from the decidua basalis. This separation causes rupture of the maternal spiral arteries, leading to hemorrhage into the retroplacental space. This specific disruption of the vascular attachment directly results in the clinical manifestations of abruption.
Rationale for incorrect answers
1. Placental implantation over the cervical os describes placenta previa, which is a distinct clinical entity from abruptio placentae. While both cause third-trimester bleeding, previa is characterized by painless hemorrhage due to the placenta's low-lying position. This anatomical malposition does not involve the premature detachment of a normally situated placenta.
3. Rupture of fetal blood vessels is the pathophysiology of vasa previa, where unprotected fetal vessels cross the internal os. In abruptio placentae, the bleeding is primarily maternal in origin from the decidua basalis vessels. Fetal vessel rupture causes rapid fetal exsanguination, which is a different mechanism than placental separation.
4. Degeneration of uterine fibroids, or leiomyomas, can cause localized pain and discomfort during pregnancy but is not a cause of placental hemorrhage. Fibroids are benign tumors of the myometrium that do not typically interfere with the structural integrity of the placental-uterine attachment. This condition does not result in the board-like rigidity seen in abruption.
Test-taking strategy
- Define the core pathology: The term "abruption" literally means to break off or tear away, which identifies separation as the key mechanism.
- Differentiate between placental emergencies: Distinguish between implantation errors (previa) and detachment errors (abruption) to eliminate Choice 1.
- Identify vascular source: Recognize that the hemorrhage in abruption stems from the maternal side (maternal spiral arteries) of the placenta-uterine interface rather than fetal vessels.
- Eliminate unrelated gynecological issues: Rule out Choice 4 as it describes a myometrial growth rather than a primary placental-vascular event.
- Focus on the anatomical disruption: Select the option that correctly describes the physical tearing of the placenta from its site of attachment.
Take home points
- Abruptio placentae is the premature separation of the placenta from the uterine wall after 20 weeks gestation.
- The primary pathology is the rupture of maternal spiral arteries in the decidua basalis.
- Clinical indicators include painful vaginal bleeding, uterine tenderness, and abdominal rigidity.
- Risk factors include maternal hypertension, abdominal trauma, cocaine use, and cigarette smoking.
A nurse is differentiating concealed from revealed abruptio placentae. Which findings are most consistent with concealed hemorrhage? Select all that apply
Explanation
Placental abruption with concealed hemorrhage involves blood trapped behind the placenta without egress through the cervix. This internal sequestration triggers retroplacental hematoma formation, leading to severe myometrial irritation and intravascular depletion despite absent external flow. Consumers of this condition often develop disseminated intravascular coagulation due to the massive release of tissue thromboplastin into the maternal venous circulation.
Rationale for correct answers
1. In a concealed abruption, the blood is trapped between the detached placenta and the uterine wall. Consequently, the nurse will observe minimal bleeding or even a total absence of vaginal discharge despite significant internal blood loss. This discrepancy often delays the diagnosis of life-threatening maternal hypovolemia.
2. Rapid maternal hypotension occurs because significant blood volume is lost into the retroplacental space rather than exiting the body. This occult blood loss leads to decreased cardiac output and systemic circulatory collapse. The nurse must monitor for tachycardia and narrow pulse pressures even when external bleeding is not visible.
4. Increasing fundal height is a definitive sign that the uterus is expanding to accommodate an accumulating internal hematoma. As blood fills the uterine cavity, the uterine fundus rises higher than expected for the current gestational age. This measurement provides an indirect quantification of the volume of concealed blood trapped within.
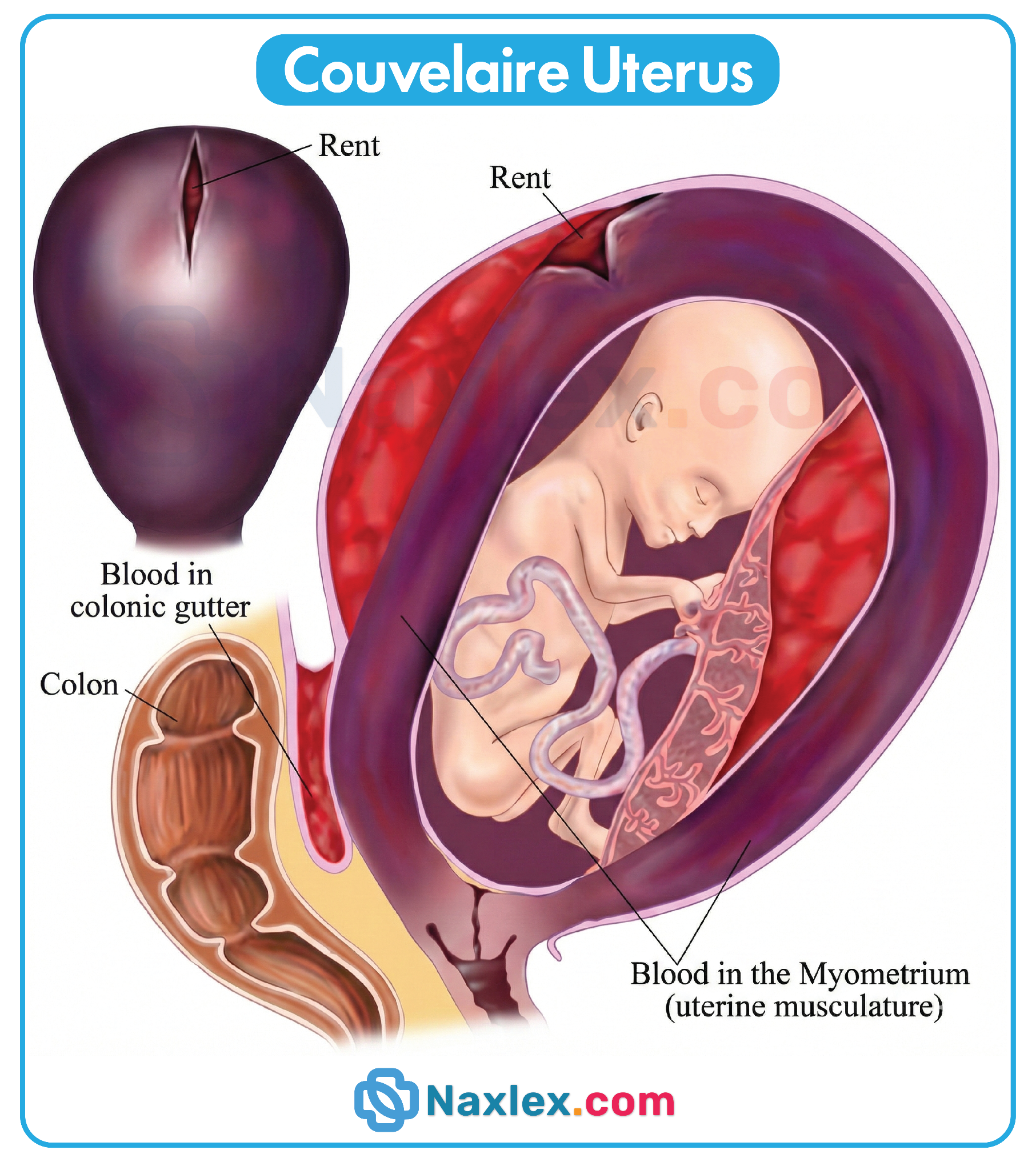
5. Board-like uterine rigidity results from blood infiltrating the uterine muscle fibers, a phenomenon known as Couvelaire uterus. The trapped blood causes intense muscular irritability and sustained hypertonicity. The uterus feels wood-like or exceptionally firm upon palpation and fails to relax, reflecting severe internal pressure.
Rationale for incorrect answers
3. A soft uterine tone is characteristic of a normal pregnancy or placenta previa, not abruptio placentae. In any significant abruption, the uterus becomes highly irritable and hypertonic due to the presence of retroplacental blood. Finding a soft uterus would effectively rule out the diagnosis of a concealed hemorrhage where internal pressure is high.
Test-taking strategy
- Analyze the Subtype: The question specifically asks for "concealed" abruption findings, which requires focusing on "hidden" blood loss versus "revealed" (visible) bleeding.
- Identify Internal Expansion Signs: Look for clinical indicators that the uterus is filling with fluid, such as increasing fundal height (Choice 4).
- Evaluate Uterine Response: Trapped blood acts as a severe irritant to the myometrium; therefore, the uterus must be rigid or board-like (Choice 5) rather than soft (Rule out Choice 3).
- Prioritize Systemic Stability: Recognize that the body reacts to intravascular volume loss regardless of whether the blood is visible. This justifies selecting hypotension (Choice 2) as a sign of hidden shock.
- Recognize the Paradox: Understand that in concealed cases, the severity of shock is often disproportionate to the amount of visible vaginal bleeding (Choice 1).
Take home points
- Concealed abruptio placentae is characterized by hidden retroplacental hemorrhage that does not escape through the vagina.
- The clinical triad for concealed abruption includes increasing fundal height, board-like uterine rigidity, and signs of shock.
- The absence of heavy vaginal bleeding does not exclude a diagnosis of severe placental abruption or maternal instability.
- Couvelaire uterus occurs when blood infiltrates the myometrium, leading to a purple discoloration and loss of contractile ability.
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Overview Of Abruptio Placentae
- Practice Exercise 1
- Etiology And Risk Factors
- Clinical Manifestations And Assessment Findings
- Practice Exercise 2
- Diagnostic Evaluation
- Practice Exercise 3
- Complications Of Abruptio Placentae
- Practice Exercise 4
- Medical And Obstetric Management
- Practice Exercise 5
- Nursing Management Of Abruptio Placentae
- Practice Exercise 6
- Patient Education And Prevention Strategies
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
Upon completion of this section, the nursing student will be able to:
- Define abruptio placentae using correct obstetric terminology and medical language.
- Distinguish abruptio placentae from other causes of antepartum hemorrhage.
- Describe the epidemiology and incidence of abruptio placentae across maternal populations.
- Identify population-level trends and high-risk groups.
- Explain the pathophysiology of placental separation at the maternal–fetal interface.
- Correlate placental separation with maternal hemorrhage and fetal hypoxia.
- Differentiate the types of abruptio placentae based on bleeding patterns and clinical presentation.
- Compare revealed, concealed, and mixed hemorrhage.
- Apply foundational knowledge of abruptio placentae to early clinical recognition and nursing assessment.
Introduction
Abruptio placentae is a serious obstetric complication characterized by premature separation of a normally implanted placenta from the uterine wall after 20 weeks of gestation and before delivery of the fetus.
- Abruptio placentae represents a true obstetric emergency due to the risk of:
- Severe maternal hemorrhage
- Fetal hypoxemia and acidosis
- Disseminated intravascular coagulation (DIC)
- Maternal and fetal mortality
- The condition disrupts uteroplacental perfusion, impairing oxygen and nutrient delivery to the fetus.
- Clinical severity varies widely, ranging from mild separation with minimal symptoms to catastrophic placental detachment.
Nursing Insights
- Vaginal bleeding may be absent or minimal despite massive internal blood loss.
- Pain is a key differentiating feature between abruptio placentae and placenta previa.
- A firm or board-like uterus is a red flag finding that requires immediate escalation of care.
Overview Of Abruptio Placentae
3.1 Definition and Terminology
Abruptio placentae is defined as the partial or complete premature separation of the placenta from the decidua basalis of the uterus prior to fetal delivery.
- Occurs after 20 weeks gestation
- Results in hemorrhage between the placenta and uterine wall
- Leads to compromised maternal–fetal exchange
Key Terminology
- Placental abruption: Synonymous with abruptio placentae
- Antepartum hemorrhage: Vaginal bleeding occurring after 20 weeks gestation
- Couvelaire uterus: Blood infiltration into the myometrium causing uterine atony
Nursing Insights
- The degree of placental separation does not always correlate with visible bleeding.
- Fetal compromise can occur rapidly even with small placental detachments.
3.2 Epidemiology and Incidence
- Incidence ranges from 0.5–1.5% of all pregnancies.
- Abruptio placentae accounts for a significant proportion of antepartum fetal deaths.
- Higher incidence is observed in:
- Clients with chronic hypertension
- Clients with a history of prior placental abruption
- Clients exposed to trauma or substance use
Nursing Insights
- A prior history of abruptio placentae increases recurrence risk by 10–15%.
- Disparities exist due to access to prenatal care and chronic disease burden.
3.3 Pathophysiology of Placental Separation
Abruptio placentae begins with rupture of maternal vessels in the decidua basalis.
- Blood accumulates between the placenta and uterine wall forming a retroplacental hematoma.
- Progressive separation reduces surface area available for gas exchange.
- Uterine irritability and hypertonicity develop due to blood infiltration.
Physiological Consequences
- Maternal hypovolemia due to acute blood loss
- Fetal hypoxemia and metabolic acidosis
- Activation of coagulation cascade leading to DIC
Nursing Insights
- Fetal distress reflects placental insufficiency, not primary fetal pathology.
- Continuous uterine rigidity suggests ongoing concealed hemorrhage.
3.4 Types of Abruptio Placentae
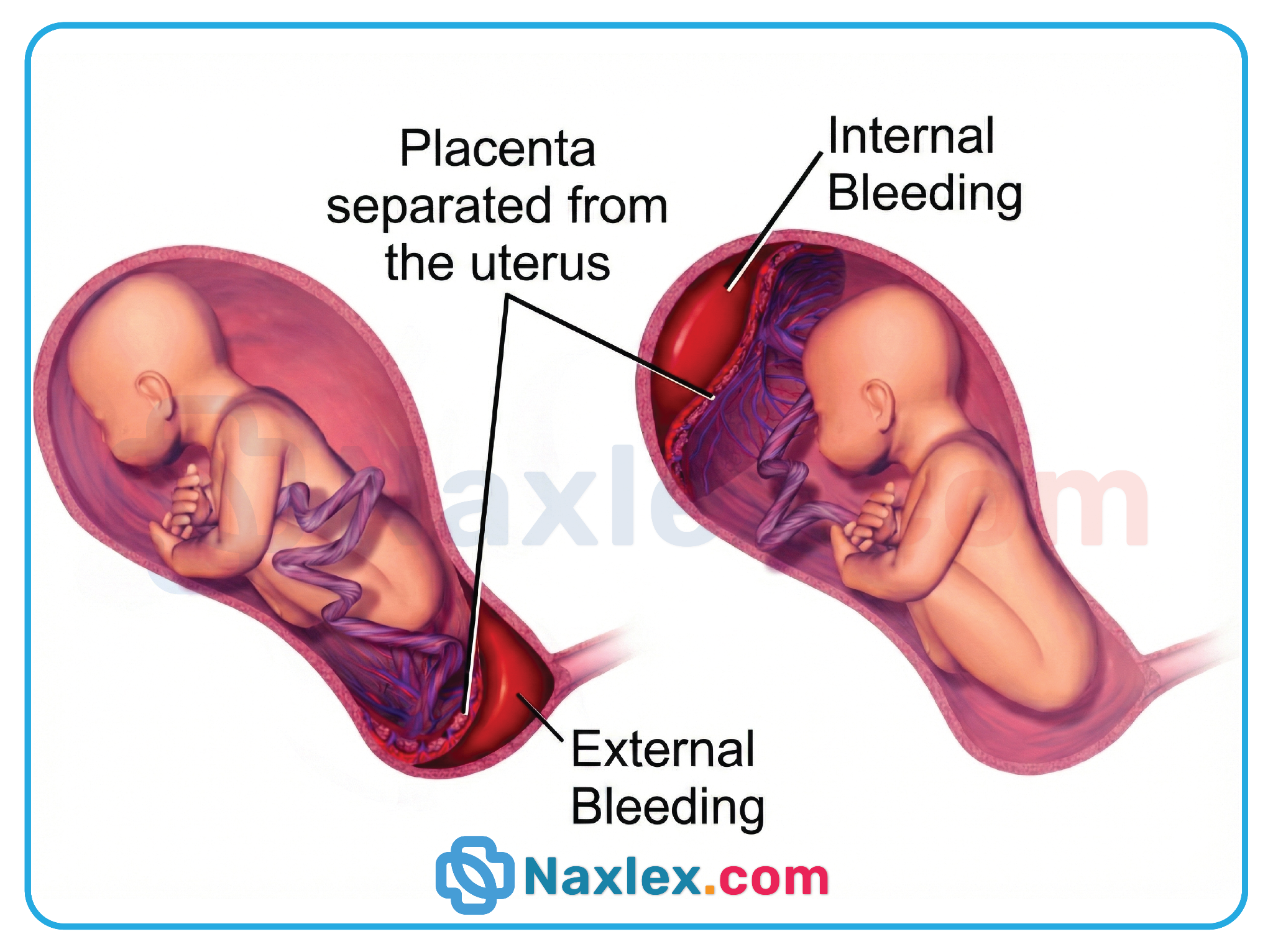
Revealed (External) Hemorrhage
- Blood escapes through the cervix resulting in visible vaginal bleeding.
- Uterus may be tender but less rigid.
- Bleeding severity is more accurately estimated.
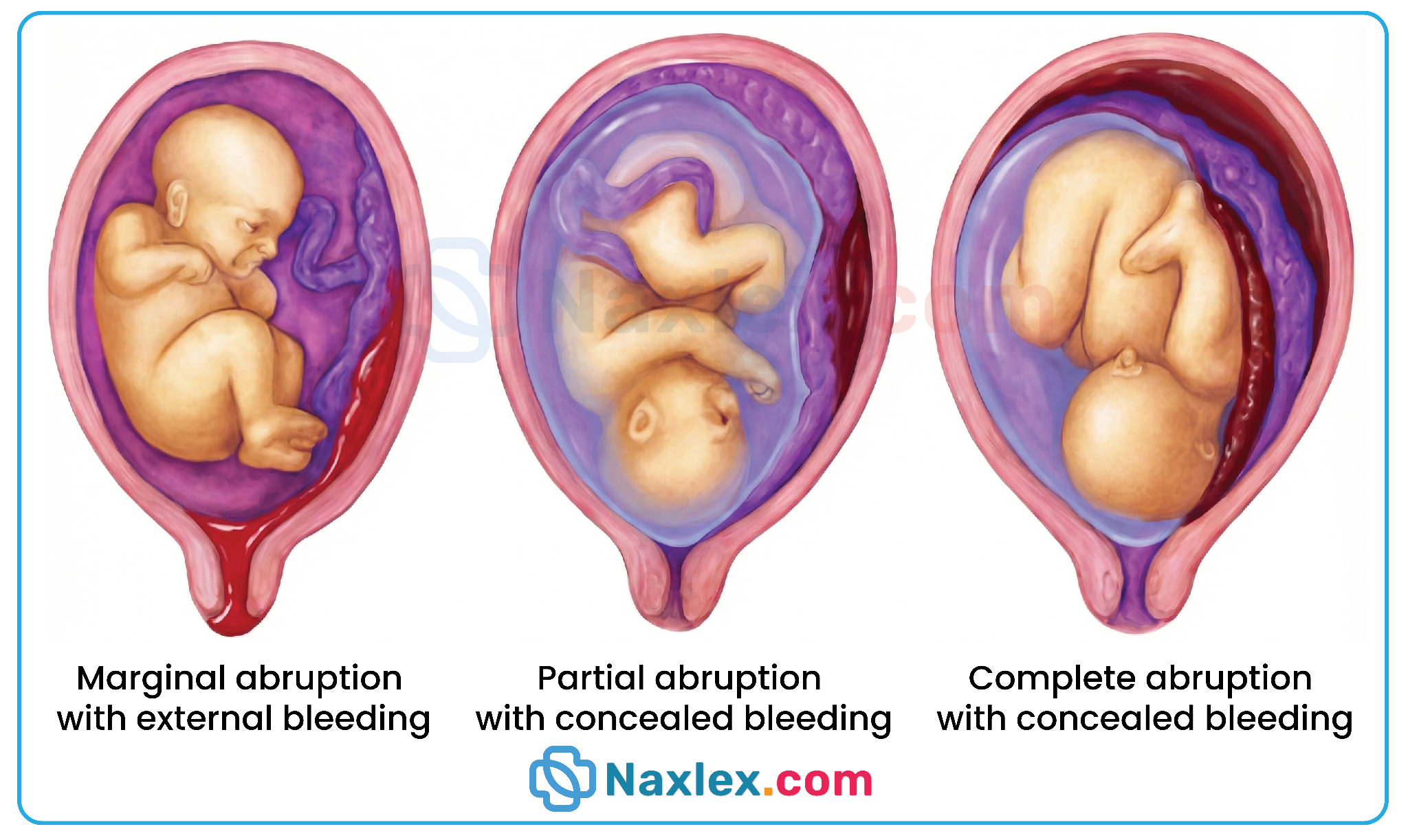
Concealed (Internal) Hemorrhage
- Blood remains trapped behind the placenta.
- Minimal or absent vaginal bleeding.
- Uterus becomes firm, tense, and board-like.
- High risk for maternal shock and DIC.
Mixed Hemorrhage
- Features of both concealed and revealed bleeding.
- Partial external bleeding with ongoing internal accumulation.
Nursing Insights
- Concealed hemorrhage is more dangerous due to delayed recognition.
- Maternal vital signs may deteriorate before bleeding is visually apparent.
Etiology And Risk Factors
The precise primary etiology of abruptio placentae is often multifactorial, involving a combination of chronic vascular degeneration and acute mechanical or chemical triggers.
- Vascular Pathologies and Hypertension
- Chronic Hypertension: This is the most consistent maternal predisposing factor, leading to degenerative changes in the spiral arterioles.
- Preeclampsia and Gestational Hypertension: Acute vasospasm and endothelial damage increase the friability of the placental-uterine interface.
- Lifestyle and Substance Use
- Cocaine Use: This is a high-yield risk factor due to the profound localized vasoconstriction and acute maternal hypertension it induces, which can cause immediate placental shearing.

-
- Tobacco Smoking: Nicotine and carbon monoxide cause placental hypoxemia and vasoconstriction, leading to vascular necrosis of the decidua.
- Mechanical and Physical Factors
- Abdominal Trauma: Blunt force trauma from motor vehicle accidents, falls, or domestic violence can cause a "shearing" effect where the inelastic placenta detaches from the elastic uterine wall.
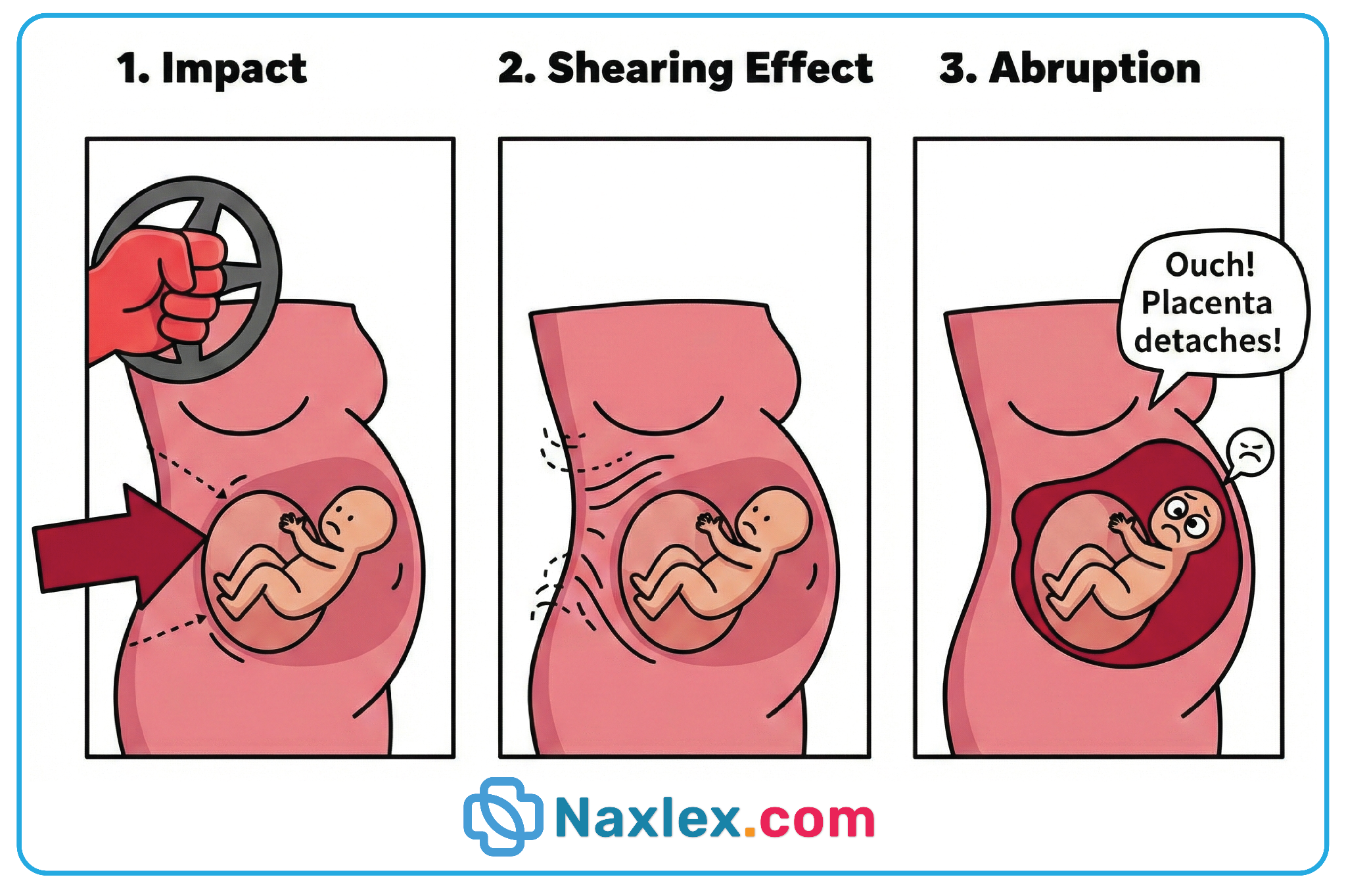
-
- Sudden Uterine Decompression: Rapid loss of amniotic fluid, such as during spontaneous rupture of membranes in polyhydramnios or the delivery of the first twin, can cause the uterus to shrink rapidly, pulling away from the placenta.
- Obstetric History and Demographics
- Prior Abruption: A client with one previous abruption has a 5% to 17% recurrence risk; after 2 previous abruptions, the risk exceeds 25%.
- Advanced Maternal Age: Increased risk in clients > 35 years of age due to associated vascular comorbidities.
- Multiparity: High parity is statistically correlated with a higher incidence of placental attachment anomalies.
Nursing Insights
A nurse must prioritize screening every pregnant client for domestic violence and substance use at every prenatal visit and upon admission to the labor unit. Because cocaine-induced abruption can occur with minimal external bleeding but extreme uterine tetany, a toxicology screen is a critical component of the assessment for any client presenting with sudden, unexplained abdominal pain.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Abruptio Placentae
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


