Please set your exam date
Digestive System Disorders
Study Questions
Peptic Ulcer Disease
Explanation
Choice A reason:
A diet high in fiber and low in fat is generally considered healthy, but it is not specifically associated with an increased or decreased risk of peptic ulcer disease.
Choice B reason:
Smoking and alcohol consumption are indeed risk factors for peptic ulcer disease. They can contribute to the development and exacerbation of ulcers.
Choice C reason:
This statement is correct. The use of NSAIDs, such as aspirin and ibuprofen, and Helicobacter pylori infection are well-established risk factors for peptic ulcer disease.
Choice D reason:
While stress and emotional factors may exacerbate peptic ulcer symptoms, they are not the primary cause of the condition. The primary causes are H. pylori infection and the use of NSAIDs.
Explanation
Choice A reason:
This question is relevant to assess for gastrointestinal symptoms, as changes in bowel movements may indicate issues with digestion or absorption.
Choice B reason:
Family history of heart disease is not directly related to peptic ulcer disease. However, it is essential for overall health assessment and risk factor identification.
Choice C reason:
Swelling or edema in the legs may be indicative of cardiovascular or circulatory issues, but it is not directly related to peptic ulcer disease.
Choice D reason:
The frequency of consuming high-fiber foods is not specifically related to peptic ulcer disease. However, diet history is essential for overall health assessment.
Explanation
Choice A reason:
Taking the PPI with meals is not the most effective timing for acid suppression. PPIs work best when taken on an empty stomach.
Choice B reason:
This statement is correct. PPIs are most effective when taken on an empty stomach, about 30 minutes before a meal. This allows the medication to be absorbed and inhibit acid secretion in the stomach before food intake.
Choice C reason:
While consistency in medication timing is important, taking the PPI at any time of the day may not optimize its effectiveness.
Choice D reason:
Taking the PPI before bedtime may not provide the best acid suppression throughout the day. Taking it on an empty stomach before a meal is a more appropriate approach.
Explanation
Choice A reason:
This statement describes an esophagoscopy, not an endoscopy. An endoscopy examines the upper gastrointestinal tract, including the stomach and duodenum.
Choice B reason:
This statement describes a colonoscopy, not an endoscopy. An endoscopy does not involve the lower gastrointestinal tract.
Choice C reason:
This statement describes an ultrasound, not an endoscopy. An endoscopy is a direct visualization procedure.
Choice D reason:
This statement is correct. An endoscopy involves inserting a flexible tube (endoscope) with a camera on the end through the mouth to examine the stomach and duodenum. It is a commonly used procedure to assess and diagnose peptic ulcer disease.
Explanation
Choice A reason:
Increasing the intake of spicy foods can exacerbate symptoms in a client with peptic ulcer disease, as they can irritate the stomach lining and increase acid production.
Choice B reason:
This statement is correct. Consuming small, frequent meals throughout the day can help reduce stomach distention and pressure, minimizing the symptoms of peptic ulcer disease.
Choice C reason:
Avoiding fluids with meals is not a standard recommendation for peptic ulcer disease. Adequate hydration is important, and drinking fluids with meals should not significantly affect stomach distention.
Choice D reason:
Citrus fruits and juices are acidic and can aggravate the stomach lining in a client with peptic ulcer disease. It is best to avoid or limit their consumption.
QUESTIONS
Explanation
Choice A reason:
This statement is correct. Family history and genetic factors are considered significant risk factors for peptic ulcer disease. A positive family history increases the likelihood of developing the condition.
Choice B reason:
Excessive consumption of fresh fruits and vegetables is not a risk factor for peptic ulcer disease. In fact, a diet rich in fruits and vegetables is generally associated with a lower risk of developing peptic ulcers.
Choice C reason:
Regular exercise and maintaining a healthy weight are not considered risk factors for peptic ulcer disease. These factors are essential for overall health but are not directly related to ulcer development.
Choice D reason:
While stress and emotional factors may exacerbate peptic ulcer symptoms, they are not the primary cause of the condition. The primary causes are Helicobacter pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Explanation
Choice A reason:
Consumption of spicy foods and carbonated beverages may exacerbate symptoms in individuals with peptic ulcer disease, but they are not direct risk factors for developing the condition.
Choice B reason:
Regular consumption of yogurt and probiotics may promote gastrointestinal health, but they are not specifically risk factors for peptic ulcer disease.
Choice C reason:
Frequent use of antacids for heartburn relief may indicate underlying acid-related issues, but it is not a risk factor for peptic ulcer disease.
Choice D reason:
This statement is correct. Long-term use of NSAIDs is a well-established risk factor for peptic ulcer disease. NSAIDs can irritate the stomach lining and increase the risk of ulcer formation.
Explanation
Choice A reason:
While Helicobacter pylori is a type of bacteria, it is not typically transmitted through food and does not directly cause peptic ulcer disease.
Choice B reason:
This statement is incorrect. Helicobacter pylori infection is indeed associated with an increased risk of peptic ulcer disease.
Choice C reason:
This statement is correct. Helicobacter pylori infection can weaken the stomach lining by producing substances that can damage the mucous layer, leading to increased vulnerability to acid and contributing to ulcer formation.
Choice D reason:
Helicobacter pylori infection is not caused by excessive consumption of spicy foods. The infection is typically acquired through person-to-person transmission, such as through contaminated water or food, and is unrelated to diet choices.
Explanation
Choice A reason:
Taking NSAIDs with alcohol can increase the risk of gastrointestinal irritation and ulcer development. Alcohol should be avoided while taking NSAIDs.
Choice B reason:
Taking NSAIDs on an empty stomach can increase the risk of irritation and ulcer formation. To minimize this risk, NSAIDs should be taken with food or milk.
Choice C reason:
This statement is correct. Using NSAID patches or creams can provide pain relief without affecting the gastrointestinal tract, reducing the risk of peptic ulcer development.
Choice D reason:
While a high-fiber diet is generally beneficial for digestive health, it does not specifically counteract the effects of NSAIDs on the stomach lining.
Explanation
Choice A reason:
Frequent consumption of spicy foods or citrus fruits can irritate the stomach lining and increase the risk of peptic ulcer development.
Choice B reason:
Family history of lung diseases is not directly related to the risk of peptic ulcer disease. However, family history of peptic ulcers or gastrointestinal conditions is relevant for risk assessment.
Choice C reason:
Experiencing frequent headaches is not a direct risk factor for peptic ulcer disease. However, the nurse should assess for other risk factors and medical history during the health screening.
Choice D reason:
Regular physical exercise is important for overall health, but it is not a direct risk factor for peptic ulcer disease. The nurse should focus on risk factors related to diet, medication use, and other medical conditions.
QUESTIONS
Explanation
Choice A reason:
This statement is correct. Right upper quadrant abdominal pain that radiates to the right shoulder is a hallmark symptom of cholecystitis. The pain is typically sudden, severe, and constant, and it is often triggered by a fatty meal.
Choice B reason:
Left lower quadrant abdominal pain with rebound tenderness is not characteristic of cholecystitis. It may indicate other conditions, such as diverticulitis or appendicitis.
Choice C reason:
Midline epigastric pain aggravated by lying down is more indicative of gastroesophageal reflux disease (GERD) rather than cholecystitis.
Choice D reason:
Diffuse abdominal pain with a low-grade fever may be seen in various conditions, but it does not specifically point to cholecystitis.
Explanation
Choice A reason:
Elevated white blood cell count may indicate inflammation or infection, but it is not directly related to jaundice and dark-colored urine, which are characteristic of increased bilirubin levels.
Choice B reason:
Impaired blood clotting is not directly related to jaundice and dark-colored urine. It may be a concern in liver disease but does not explain the specific manifestations mentioned in the question.
Choice C reason:
This statement is correct. Jaundice and dark-colored urine are indicative of increased bilirubin levels in the blood, which can occur in cholecystitis due to obstruction of the bile ducts.
Choice D reason:
Elevated serum amylase is more associated with pancreatitis rather than cholecystitis. It is not directly related to the clinical manifestations described.
Explanation
Choice A reason:
Nausea and vomiting after meals are common symptoms in acute cholecystitis, but they do not indicate a severe complication. They are typical manifestations of gallbladder inflammation.
Choice B reason:
Mild right upper quadrant pain may be present in acute cholecystitis, but it does not suggest a severe complication.
Choice C reason:
Referred pain to the left shoulder (Kehr's sign) is a classic symptom of splenic rupture or other conditions involving the spleen, not directly related to cholecystitis.
Choice D reason:
This statement is correct. High fever and chills may indicate the presence of infection and sepsis, which can be severe complications of acute cholecystitis.
Explanation
Choice A reason:
This statement is correct. Chronic cholecystitis can lead to impaired gallbladder emptying, resulting in difficulties in digesting fats. Indigestion and bloating after meals are common manifestations of this problem.
Choice B reason:
Excessive stomach acid production is more associated with conditions like GERD or peptic ulcer disease, and it is not directly related to chronic cholecystitis.
Choice C reason:
Inflammation of the small intestine may cause abdominal pain, diarrhea, or malabsorption issues, but it is not specifically related to the symptoms described in the question.
Choice D reason:
Decreased production of pancreatic enzymes may lead to malabsorption issues and cause symptoms like diarrhea and steatorrhea. However, it is not the primary cause of indigestion and bloating after meals in chronic cholecystitis.
Explanation
Choice A reason:
Percussion of the left lower quadrant is not relevant to assess for Boas' sign, which involves the right upper quadrant.
Choice B reason:
Deep palpation of the epigastric region is not associated with Boas' sign. Boas' sign involves palpation of the right subscapular area.
Choice C reason:
This statement is correct. Boas' sign is elicited by palpating the right upper quadrant during inspiration. The client may experience referred pain to the right subscapular area, indicating irritation of the phrenic nerve by the inflamed gallbladder.
Choice D reason:
Auscultation of the left upper quadrant is not relevant to assessing for Boas' sign, which involves the right upper quadrant.
Explanation
Choice A reason:
Abdominal CT scan can provide detailed images, but it is not typically the first-line imaging study for diagnosing cholecystitis. It may be used if complications are suspected.
Choice B reason:
MRI of the gallbladder can provide high-resolution images, but it is not the first-line imaging study for diagnosing cholecystitis.
Choice C reason:
This statement is correct. Abdominal ultrasound is the first-line imaging study for diagnosing cholecystitis. It can visualize the gallbladder, detect gallstones, and assess for signs of inflammation, such as gallbladder wall thickening and pericholecystic fluid.
Choice D reason:
ERCP is an invasive procedure used to visualize the biliary and pancreatic ducts, but it is not typically used as a first-line diagnostic test for cholecystitis.
Explanation
Choice A reason:
Fasting for 12 hours before an abdominal ultrasound is not necessary. Abdominal ultrasound does not require an empty stomach.
Choice B reason:
Drinking water is not typically restricted before an abdominal ultrasound. In fact, drinking water can improve image quality in some cases.
Choice C reason:
This statement is correct. There are no special preparations required for an abdominal ultrasound. The procedure is non-invasive and does not involve any special preparation or fasting.
Choice D reason:
Avoiding pain medications is not necessary before an abdominal ultrasound. The client can continue taking prescribed medications as usual.
Explanation
Choice A reason:
Elevated serum amylase levels are more indicative of pancreatitis, not cholecystitis.
Choice B reason:
Increased serum creatinine levels are suggestive of kidney dysfunction and are not directly related to cholecystitis.
Choice C reason:
This statement is correct. Cholecystitis is associated with inflammation and infection, which can lead to an elevated white blood cell count (leukocytosis).
Choice D reason:
Low serum bilirubin levels are not consistent with cholecystitis, which can cause obstructive jaundice and elevated bilirubin levels due to bile duct obstruction.
Explanation
Choice A reason:
Visualizing blood flow in the liver is not the purpose of a HIDA scan. This type of scan is primarily used to assess the biliary system.
Choice B reason:
This statement is correct. A HIDA scan is used to assess the function and patency of the bile ducts. It involves injecting a radioactive tracer that is taken up by the liver and excreted into the bile. The scan can visualize the flow of bile and detect any obstruction or abnormality in the biliary system.
Choice C reason:
Evaluating the motility of the small intestine is not the purpose of a HIDA scan. It is used specifically for assessing the biliary system.
Choice D reason:
Providing detailed images of the pancreas is not the primary purpose of a HIDA scan, although it can sometimes provide some information about the pancreas if the tracer reaches the duodenum and enters the common bile duct.
Explanation
Choice A reason:
CT scans use X-rays, not magnetic fields, to create detailed cross-sectional images of the body. They involve radiation exposure.
Choice B reason:
This statement is correct. While CT scans use X-rays, the amount of radiation used in modern CT machines is relatively low and considered safe. The benefits of the diagnostic information obtained from the scan usually outweigh the risks associated with the small amount of radiation exposure.
Choice C reason:
The speed of the scan does not impact the radiation exposure. The amount of radiation used in a CT scan remains the same regardless of the scan duration.
Choice D reason:
CT scans use X-rays, not sound waves. Sound waves are used in ultrasound imaging, not in CT scans.
Explanation
Choice A reason:
Avoiding NSAIDs is essential for clients with peptic ulcer disease as they can worsen the condition and increase the risk of bleeding.
Choice B reason:
Following a low-fat diet does not directly impact stomach acid production, but it can help prevent irritation to the stomach lining by reducing the intake of potentially irritating foods.
Choice C reason:
This statement is correct. Proton pump inhibitors (PPIs) are commonly prescribed to reduce stomach acid production and promote ulcer healing. It is crucial for the client to continue taking PPIs as directed by their healthcare provider.
Choice D reason:
This statement is incorrect and indicates a need for further teaching. Alcohol can irritate the stomach lining and exacerbate peptic ulcer disease. Clients with peptic ulcers should avoid or minimize alcohol consumption.
Explanation
Choice A reason:
Administering antacids one hour before meals would be less effective in providing pain relief during mealtime when stomach acid production is increased.
Choice B reason:
This statement is correct. Administering antacids with meals helps neutralize stomach acid during the digestion process and provides pain relief for clients with peptic ulcer disease.
Choice C reason:
Administering antacids two hours after meals may not effectively reduce pain during the mealtime when stomach acid production is at its peak.
Choice D reason:
Administering antacids at bedtime may help with overnight acid reduction, but it may not adequately address pain during meals when acid production is higher.
Explanation
Choice A reason:
Antibiotics do not directly heal the ulcer or reduce stomach acid production. They are prescribed specifically to treat Helicobacter pylori (H. pylori) infection, a common cause of peptic ulcers.
Choice B reason:
This statement is correct. Antibiotics are prescribed to treat H. pylori infection, which is a major cause of peptic ulcers. By eliminating the bacterial infection, the ulcer has a better chance of healing and preventing recurrence.
Choice C reason:
Antibiotics do not promote blood clotting or reduce the risk of bleeding from the ulcer. Other medications may be prescribed to manage bleeding if it occurs.
Choice D reason:
Antibiotics do not relax stomach muscles or alleviate abdominal pain. Pain relief is typically achieved through acid-reducing medications and other pain management strategies.
Explanation
Choice A reason:
Recovering fully within 1-2 weeks after surgery for a peptic ulcer perforation may be overly optimistic. The recovery time is typically longer and depends on the individual's health status and the extent of the surgery.
Choice B reason:
This statement is correct. The recovery time after surgery for a peptic ulcer perforation varies depending on factors such as the type of surgery performed, the extent of the perforation, and the client's overall health. It may take several weeks to months for the client to fully recover.
Choice C reason:
Resuming normal activities immediately after surgery for a peptic ulcer perforation is not advisable. Clients usually require a period of rest and limited activity to allow proper healing.
Choice D reason:
Recovering fully in 6 months may be an extended recovery period. While some clients may experience a longer recovery, it is not a standard time frame for everyone.
Explanation
Choice A reason:
Increasing intake of spicy foods is not recommended for clients with peptic ulcer disease, as they can irritate the stomach lining and exacerbate symptoms.
Choice B reason:
This statement is correct. Consuming frequent, small meals throughout the day helps prevent prolonged periods of fasting, which can reduce stomach acid production and irritation to the stomach lining. It also aids in maintaining steady blood sugar levels.
Choice C reason:
Drinking caffeinated beverages can increase stomach acid production and may worsen symptoms in clients with peptic ulcer disease. It is best to avoid or limit caffeinated drinks.
Choice D reason:
High-fiber foods can be beneficial for overall digestive health, but they are not specifically recommended for promoting ulcer healing. In some cases, high-fiber foods may need to be avoided if they cause discomfort.
Explanation
Choice A reason:
Mild bloating and gas after meals may be common gastrointestinal symptoms but are not specific warning signs of complications related to peptic ulcer disease.
Choice B reason:
This statement is correct. Black, tarry stools (melena) or vomiting blood (hematemesis) are potential signs of gastrointestinal bleeding, a serious complication of peptic ulcer disease. Clients should seek immediate medical attention if they experience these symptoms.
Choice C reason:
Occasional heartburn may occur during the course of ulcer healing but is not considered a warning sign of complications.
Choice D reason:
Feeling fatigued and sleepy after meals is not typically associated with peptic ulcer disease or its complications.
Explanation
Choice A reason:
A perforated peptic ulcer can lead to localized peritonitis, which may cause abdominal rigidity and guarding, rather than hypoactive bowel sounds.
Choice B reason:
Reduced abdominal tenderness is not expected in a client with a perforated peptic ulcer. Abdominal tenderness is likely to be present due to inflammation and irritation of the peritoneal lining.
Choice C reason:
Elevated blood pressure is not a typical finding in a client with a perforated peptic ulcer. The client may experience hypotension due to fluid loss and hemorrhage.
Choice D reason:
This statement is correct. A perforated peptic ulcer can cause increased abdominal rigidity due to the inflammation and irritation of the peritoneal lining. The abdomen may feel tense and rigid upon palpation.
Explanation
Choice A reason:
Taking NSAIDs with food can help reduce stomach irritation and the risk of developing peptic ulcers.
Choice B reason:
This statement is correct. Dark, tarry stools may indicate gastrointestinal bleeding, a potential complication of peptic ulcer disease. The client should promptly notify their healthcare provider if they experience this symptom.
Choice C reason:
This statement is incorrect and indicates a need for further education. While antacids can provide temporary relief from heartburn, they do not address the underlying issue of stomach irritation caused by NSAIDs. The client should avoid NSAIDs or discuss alternative pain management strategies with their healthcare provider.
Choice D reason:
Avoiding alcohol is advisable while on NSAIDs as alcohol can increase the risk of gastrointestinal bleeding and worsen peptic ulcer disease.
Explanation
Choice A reason:
Assessing for signs of fluid overload is a priority when administering PPIs intravenously, as these medications can increase the risk of fluid retention in some clients.
Choice B reason:
Monitoring liver function test results is important for clients taking certain medications, but it is not the priority when administering PPIs to this client.
Choice C reason:
Elevating the head of the client's bed is a standard measure to prevent aspiration and improve digestion, but it is not the priority in this scenario.
Choice D reason:
Checking for drug interactions with other medications is essential for safe medication administration, but it is not the priority when administering PPIs intravenously to this client.
Explanation
Choice A reason:
This statement is correct. An upper gastrointestinal endoscopy is a diagnostic procedure that uses a flexible tube with a camera (endoscope) to visualize the esophagus, stomach, and duodenum. It helps identify abnormalities, such as peptic ulcers, inflammation, or tumors.
Choice B reason:
Assessing blood flow to the intestines and colon is not the purpose of an upper gastrointestinal endoscopy. This procedure focuses on the upper digestive tract.
Choice C reason:
Evaluating kidney function and the urinary system is unrelated to an upper gastrointestinal endoscopy, which focuses on the upper digestive tract.
Choice D reason:
Diagnosing conditions in the lower digestive tract is not the purpose of an upper gastrointestinal endoscopy. Lower digestive tract evaluations are typically done using colonoscopy or sigmoidoscopy.
Explanation
Choice A reason:
This statement is correct. Sucralfate is best taken on an empty stomach at least 1 hour before meals to allow it to form a protective barrier over the ulcer and provide optimal therapeutic effects.
Choice B reason:
Crushing sucralfate tablets is not recommended, as it may interfere with the medication's ability to adhere to the ulcer site and provide protection.
Choice C reason:
Taking sucralfate with antacids may reduce its effectiveness, as antacids can interfere with its therapeutic actions. It is best to take sucralfate separately from antacids.
Choice D reason:
It is essential to avoid taking sucralfate with other medications, especially those that require an acidic environment for absorption. This is because sucralfate can decrease the absorption of certain drugs.
Explanation
Choice A reason:
Eating a large, well-balanced meal during mealtimes may exacerbate abdominal pain for the client with peptic ulcer disease. Instead, the client should be encouraged to eat smaller, more frequent meals to reduce stomach acid production.
Choice B reason:
This statement is correct. Administering prescribed antacids 30 minutes before meals can help reduce stomach acid levels during digestion and alleviate the client's pain.
Choice C reason:
Instructing the client to lie flat immediately after eating is not recommended, as it may increase the risk of reflux and worsen the client's symptoms.
Choice D reason:
Providing the client with spicy foods is not advisable, as they can irritate the stomach lining and worsen symptoms for the client with peptic ulcer disease.
Explanation
Choice A reason:
This statement is correct. H2 receptor blockers can sometimes cause an increase in serum potassium levels. The nurse should monitor the client's potassium levels closely to detect any abnormalities.
Choice B reason:
H2 receptor blockers do not typically affect blood glucose levels, so monitoring blood glucose is not the priority in this scenario.
Choice C reason:
H2 receptor blockers are not known to have a significant impact on serum creatinine levels, so monitoring creatinine is not the priority in this case.
Choice D reason:
H2 receptor blockers are not known to affect the CBC, so monitoring the complete blood count is not the priority for this client.
Explanation
Choice A reason:
Hypertension and increased heart rate are not early signs of gastrointestinal bleeding. In fact, hypotension and tachycardia are more common signs of significant blood loss.
Choice B reason:
Abdominal distention and bloating are not typical early signs of gastrointestinal bleeding. These symptoms may occur due to other gastrointestinal issues but are not specific to bleeding.
Choice C reason:
This statement is correct. Melena, or black, tarry stools, is a classic sign of upper gastrointestinal bleeding and indicates the presence of partially digested blood in the stool.
Choice D reason:
Hyperactive bowel sounds are not early signs of gastrointestinal bleeding. Bowel sounds may be hyperactive or hypoactive depending on the severity of the bleeding and associated factors.
Explanation
Choice A reason:
Misoprostol is not an antibiotic. It is a synthetic prostaglandin used to protect the stomach lining and prevent peptic ulcers, particularly in clients taking nonsteroidal anti-inflammatory drugs (NSAIDs).
Choice B reason:
Misoprostol should be taken with meals to minimize gastrointestinal side effects. Taking it on an empty stomach may increase the risk of adverse effects.
Choice C reason:
This statement is correct. Misoprostol is contraindicated during pregnancy and can cause uterine contractions and birth defects. Clients taking misoprostol should use effective contraception to prevent pregnancy.
Choice D reason:
Misoprostol is not used to reduce stomach acid production. Instead, it helps protect the stomach lining by increasing mucus production and promoting bicarbonate secretion.
Explanation
Choice A reason:
This statement is correct. Smoking and excessive alcohol intake can irritate the stomach lining and increase the risk of peptic ulcer recurrence. Avoiding these substances is important for promoting healing and preventing further damage.
Choice B reason:
Consuming a high-fat diet is not recommended for peptic ulcer prevention. High-fat foods can stimulate acid production and worsen symptoms for clients with peptic ulcers.
Choice C reason:
Engaging in strenuous exercise immediately after meals is not advisable, as it can increase the risk of acid reflux and worsen symptoms for clients with peptic ulcers.
Choice D reason:
Regular use of NSAIDs can increase the risk of developing peptic ulcers and is not a preventive strategy for clients with a history of peptic ulcer disease.
Explanation
Choice A reason:
This statement is incorrect and indicates a need for further education. PPIs should be taken on an empty stomach, at least 30 minutes before meals, to allow for optimal absorption and effectiveness.
Choice B reason:
This statement is correct. Clients should continue taking the PPI for the full duration as prescribed, even if they start to feel better, to prevent ulcer recurrence.
Choice C reason:
This statement is correct. PPIs can decrease calcium absorption and increase the risk of osteoporosis in some clients. Increasing calcium intake or taking calcium supplements may be necessary for clients on long-term PPI therapy.
Choice D reason:
This statement is correct. Antacids can interfere with the action of PPIs, and clients should avoid taking them together. If needed, antacids should be taken at least 1 hour before or after the PPI.
Explanation
Choice A reason:
Limiting fiber-rich foods is not a recommended preventive strategy for peptic ulcer disease. In fact, fiber can aid digestion and promote bowel regularity, which may be beneficial for some clients with peptic ulcers.
Choice B reason:
This statement is correct. Spicy and acidic foods can irritate the stomach lining and increase stomach acid production, potentially worsening symptoms for clients with peptic ulcers.
Choice C reason:
Increasing consumption of carbonated beverages is not advised, as they can cause bloating and increased gas production, which may exacerbate symptoms for clients with peptic ulcers.
Choice D reason:
Caffeine-containing beverages should be limited or avoided, as caffeine can stimulate gastric acid secretion and may worsen symptoms for clients with peptic ulcers.
Explanation
Choice A reason:
Avoiding all dairy products is not a preventive measure for H. pylori reinfection. Dairy consumption does not play a significant role in H. pylori colonization or infection.
Choice B reason:
This statement is correct. H. pylori is primarily transmitted through the oral-oral or fecal-oral route. Practicing strict hand hygiene, especially after using the restroom and before eating, can help reduce the risk of transmission and reinfection.
Choice C reason:
Including raw vegetables in the diet is not a specific preventive measure for H. pylori reinfection. A balanced diet that promotes overall gut health may be beneficial, but raw vegetables alone do not prevent H. pylori reinfection.
Choice D reason:
Taking over-the-counter antacids regularly is not a preventive strategy for H. pylori reinfection. Antacids do not target the bacterium and are not effective in eradicating H. pylori.
Explanation
Choice A reason:
Taking sucralfate with meals is not recommended, as it can reduce its effectiveness. Sucralfate should be taken on an empty stomach, at least 1 hour before meals, to allow it to form a protective barrier over the ulcerated areas.
Choice B reason:
Crushing sucralfate tablets is not advised, as it can interfere with the medication's ability to adhere to the ulcer site and provide protection.
Choice C reason:
This statement is correct. Taking antacids with sucralfate can reduce its effectiveness, as antacids can interfere with its therapeutic actions. Clients should avoid taking antacids together with sucralfate.
Choice D reason:
Sucralfate does not typically cause drowsiness, so taking it before bedtime is not necessary for this medication. It should be taken at regular intervals during the day as prescribed.
Cholecystitis
Explanation
Choice A reason:
This statement is correct and does not indicate a need for further teaching. Avoiding fatty foods is essential in managing cholecystitis as it reduces the stimulation of the gallbladder and may prevent symptom exacerbation.
Choice B reason:
This statement is correct and does not indicate a need for further teaching. Taking prescribed antibiotics is important if the cholecystitis is caused by an infection, as it helps in treating the underlying cause.
Choice C reason:
This statement is incorrect and indicates a need for further teaching. Increasing alcohol intake can worsen inflammation and exacerbate cholecystitis symptoms. Clients with cholecystitis should avoid alcohol to support their recovery.
Choice D reason:
This statement is correct and does not indicate a need for further teaching. Applying a warm compress to the abdomen can help relieve pain associated with cholecystitis and promote comfort.
Explanation
Choice A reason:
This statement is correct and is an appropriate preoperative intervention. Encouraging deep breathing and coughing exercises helps prevent postoperative respiratory complications such as atelectasis and pneumonia.
Choice B reason:
This statement is incorrect and is not an appropriate preoperative intervention. Placing the client in a supine position with legs elevated can increase intraabdominal pressure and worsen cholecystitis symptoms.
Choice C reason:
This statement is incorrect and is not an appropriate preoperative intervention. The client should be on a restricted diet, avoiding fatty and heavy foods, to prevent exacerbation of cholecystitis symptoms and reduce the risk of complications during surgery.
Choice D reason:
This statement is incorrect and is not an appropriate preoperative intervention. Anticoagulants are not typically administered preoperatively for cholecystectomy. Their use may increase bleeding risk during surgery and is generally avoided unless medically indicated.
Explanation
Choice A reason:
This statement is incorrect. Hyperactive bowel sounds are not typically associated with cholecystitis and may be seen in conditions such as gastroenteritis or irritable bowel syndrome.
Choice B reason:
This statement is incorrect. Severe left upper quadrant pain is not characteristic of cholecystitis. Cholecystitis typically presents with right upper quadrant pain.
Choice C reason:
This statement is correct. Right upper quadrant tenderness is a hallmark symptom of cholecystitis. The inflamed gallbladder causes pain and tenderness in this area.
Choice D reason:
This statement is incorrect. Pain radiating to the left shoulder is more indicative of conditions such as splenic disorders, not cholecystitis.
Explanation
Choice A reason:
This statement is correct and does not indicate a need for further teaching. Eating a low-fat diet after cholecystectomy is recommended to prevent symptoms and complications related to the digestion of fatty foods.
Choice B reason:
This statement is correct and does not indicate a need for further teaching. Avoiding heavy lifting for at least four weeks after cholecystectomy is important to allow the surgical site to heal properly and prevent strain on the incision site.
Choice C reason:
This statement is correct and does not indicate a need for further teaching. It is essential to continue taking prescribed antibiotics until they are finished to prevent infection and promote proper healing after surgery.
Choice D reason:
This statement is incorrect and indicates a need for further teaching. The client should not resume their regular exercise routine immediately after the surgery. After cholecystectomy, clients should avoid strenuous physical activities for a period specified by the healthcare provider to promote proper healing and prevent complications. The nurse should educate the client on gradually increasing their activity level and resuming exercise after receiving clearance from their healthcare provider.
Explanation
Choice A reason:
Severe lower back pain is not a classic manifestation of cholecystitis. Cholecystitis typically presents with pain in the right upper quadrant of the abdomen that may radiate to the right shoulder.
Choice B reason:
Epigastric pain radiating to the left shoulder is not a classic manifestation of cholecystitis. Cholecystitis typically presents with pain in the right upper quadrant of the abdomen that may radiate to the right shoulder.
Choice C reason:
This statement is correct. Right upper quadrant abdominal pain that radiates to the right shoulder is a classic manifestation of cholecystitis. The pain is often described as sharp or colicky and may worsen after eating fatty or greasy foods.
Choice D reason:
Left lower quadrant abdominal pain with rebound tenderness is not a classic manifestation of cholecystitis. Cholecystitis typically presents with pain in the right upper quadrant of the abdomen.
Explanation
Choice A reason:
This statement is correct and explains the difference between acute and chronic cholecystitis. Acute cholecystitis is characterized by a sudden onset of inflammation, often caused by gallstones blocking the cystic duct. On the other hand, chronic cholecystitis is a long-standing inflammation resulting from repeated episodes of acute cholecystitis or chronic irritation from gallstones.
Choice B reason:
This statement is incorrect. While gallstones can be a cause of both acute and chronic cholecystitis, gallbladder cancer is not a typical cause of either condition.
Choice C reason:
This statement is incorrect. Acute cholecystitis can affect individuals of all age groups, and age is not a differentiating factor between acute and chronic cholecystitis.
Choice D reason:
This statement is incorrect. Both acute and chronic cholecystitis may require surgical intervention, depending on the severity and complications of the condition. Lifestyle modifications are often recommended to prevent gallstone formation and manage symptoms, but they are not the sole treatment for acute cholecystitis.
A nurse is caring for a client with acute cholecystitis. Which of the following clinical manifestations is most commonly associated with this condition?
Explanation
A. Mild, intermittent right upper quadrant (RUQ) pain is more characteristic of chronic cholecystitis rather than acute cholecystitis, which typically presents with severe pain.
B. Left lower quadrant (LLQ) pain with rebound tenderness is more indicative of conditions like diverticulitis, not acute cholecystitis.
C. Severe, colicky abdominal pain radiating to the right shoulder is the most common presentation of acute cholecystitis, often caused by gallbladder inflammation and obstruction of the cystic duct. The pain is due to irritation of the phrenic nerve, which supplies both the gallbladder and right shoulder.
D. Epigastric pain worsened by fatty meals is often seen in gallbladder disease but is more characteristic of biliary colic rather than acute cholecystitis.
Explanation
Choice A reason:
While chronic cholecystitis can lead to complications, such as gallbladder inflammation and gallstones, it is not a typical cause of gallbladder cancer.
Choice B reason:
This statement is correct. Complications of chronic cholecystitis may include pancreatitis, which is inflammation of the pancreas, and cholangitis, which is inflammation of the bile ducts. These complications can occur if gallstones migrate from the gallbladder and obstruct the pancreatic or bile ducts.
Choice C reason:
This statement is incorrect. Chronic cholecystitis is inflammation of the gallbladder, not the pancreas. However, complications of chronic cholecystitis, such as gallstone migration, can cause acute inflammation of the pancreas (pancreatitis).
Choice D reason:
Complications of chronic cholecystitis do not typically include lung infections. The primary complications are related to the gallbladder, pancreas, and bile ducts.
Explanation
Choice A reason:
Avoiding foods high in fiber is not recommended to reduce gallstone formation. In fact, a diet high in fiber can promote regular bowel movements and may be beneficial in preventing gallstone formation.
Choice B reason:
Limiting fluid intake is not recommended to manage chronic cholecystitis. Staying adequately hydrated is essential for overall health and can help prevent gallstone formation.
Choice C reason:
This statement is correct. Avoiding fatty and greasy foods is recommended to manage chronic cholecystitis. These foods can trigger gallbladder contractions and exacerbate symptoms in individuals with gallstones or chronic inflammation.
Choice D reason:
Increasing the intake of carbonated beverages is not recommended to improve digestion or manage chronic cholecystitis. Carbonated beverages can potentially worsen symptoms in some individuals with gallbladder conditions.
Explanation
Choice A reason:
Encouraging the client to eat a high-fat meal the night before the surgery is not recommended. Instead, clients scheduled for surgery, especially abdominal surgery, are typically instructed to have a clear liquid diet or nothing by mouth (NPO) after midnight to prevent aspiration during anesthesia.
Choice B reason:
Administering antibiotics prophylactically before surgery is often done to prevent infection during the procedure. However, it is at the discretion of the healthcare provider based on the client's specific condition and surgical plan.
Choice C reason:
Avoiding deep breathing exercises is not recommended preoperatively. Deep breathing exercises help prevent respiratory complications after surgery and promote lung function.
Choice D reason:
This statement is correct. Instructing the client to remain NPO after midnight before the surgery is essential to prevent aspiration during anesthesia. Clients should not eat or drink anything after the specified time to ensure their stomach is empty during the surgery.
Explanation
Choice A reason:
Age below 30 years is not a risk factor for developing cholecystitis. Cholecystitis is more commonly seen in individuals over the age of 40, especially in those with additional risk factors such as obesity or a high-fat diet.
Choice B reason:
Regular physical exercise is not considered a risk factor for cholecystitis. In fact, staying physically active is generally beneficial for overall health and may help reduce the risk of gallstone formation.
Choice C reason:
This statement is correct. Family history of gallstones is a significant risk factor for developing cholecystitis. Genetics can play a role in the composition of bile and the propensity to form gallstones.
Choice D reason:
Consuming a low-fat diet is not a risk factor for cholecystitis. On the contrary, a high-fat diet is associated with an increased risk of gallstone formation and subsequent cholecystitis.
Explanation
Choice A reason:
Chronic alcohol consumption is not a common cause of gallbladder inflammation or cholecystitis. However, excessive alcohol consumption can contribute to liver disease, which may increase the risk of gallstone formation.
Choice B reason:
Excessive consumption of dairy products is not a common cause of gallbladder inflammation. The primary factors leading to cholecystitis are gallstones, inflammation of the gallbladder wall, or infection.
Choice C reason:
This statement is correct. Blockage of the cystic duct by a gallstone is a common cause of gallbladder inflammation. When a gallstone obstructs the cystic duct, bile cannot flow freely, leading to increased pressure and inflammation of the gallbladder wall, resulting in cholecystitis.
Choice D reason:
Allergic reactions to certain foods are not a common cause of gallbladder inflammation or cholecystitis. Cholecystitis is primarily related to gallstones, bile flow abnormalities, or infections.
Explanation
Choice A reason:
Obesity does not increase the production of bile. However, it can lead to changes in bile composition, increasing the risk of gallstone formation.
Choice B reason:
This statement is incorrect. Obesity is associated with an increased concentration of cholesterol in the bile, which can contribute to gallstone formation.
Choice C reason:
This statement is correct. Obesity increases the concentration of cholesterol in the bile, which promotes gallstone formation. When there is an excess of cholesterol in the bile, it can crystallize and form gallstones.
Choice D reason:
Obesity does not slow down the emptying of the gallbladder. On the contrary, obesity may lead to reduced gallbladder motility, which can contribute to gallstone formation due to stasis of bile.
Explanation
Choice A reason:
Diabetes does not increase bile production. However, it can lead to changes in bile composition, increasing the risk of gallstone formation.
Choice B reason:
This statement is incorrect. Diabetes is associated with increased cholesterol levels in the bile, which can contribute to gallstone formation.
Choice C reason:
This statement is correct. Diabetes can impair the function of the sphincter of Oddi, a muscular valve that controls the flow of bile into the duodenum. Dysfunction of the sphincter can lead to bile stasis and increase the risk of gallstone formation.
Choice D reason:
Diabetes does not increase the motility of the gallbladder. Instead, it may lead to reduced gallbladder motility, which can contribute to gallstone formation due to stasis of bile.
Explanation
Choice A reason:
This statement is incorrect. Genetic factors can influence bile composition and the risk of gallstone formation.
Choice B reason:
This statement is incorrect. Family history of gallstones can significantly increase the risk of developing gallstones, more than 10%.
Choice C reason:
This statement is correct. Genetic factors play a significant role in determining bile composition and gallstone formation. Certain genetic variations can increase cholesterol levels or affect the balance of bile components, predisposing individuals to gallstone formation.
Choice D reason:
Family history of gallstones can affect the risk of gallstones in both men and women. It is not limited to a specific gender.
Explanation
Choice A reason:
Appendicitis typically presents with pain in the lower right abdomen and may be associated with fever and rebound tenderness.
Choice B reason:
Gastroenteritis can cause abdominal pain and vomiting, but it does not usually cause pain radiating to the right shoulder.
Choice C reason:
This statement is correct. Cholecystitis is characterized by severe right upper quadrant abdominal pain that may radiate to the right shoulder, along with nausea and vomiting.
Choice D reason:
Pancreatitis may cause upper abdominal pain, but it typically radiates to the back rather than the right shoulder.
Explanation
Choice A reason:
Rebound tenderness in the right upper quadrant is not a hallmark sign of acute cholecystitis. It may be present in conditions such as appendicitis or peritonitis.
Choice B reason:
This statement is correct. Murphy's sign is a hallmark sign of acute cholecystitis. It is elicited by asking the client to take a deep breath while the nurse palpates the right upper quadrant. If the client abruptly stops breathing due to pain upon palpation, it indicates inflammation of the gallbladder (positive Murphy's sign).
Choice C reason:
Hypoactive bowel sounds may be present in some gastrointestinal conditions but are not specific to acute cholecystitis.
Choice D reason:
Left lower quadrant abdominal pain is not associated with acute cholecystitis. This type of pain is more commonly seen in conditions such as diverticulitis or colitis.
Explanation
Choice A reason:
Itching is not typically associated with an allergic reaction and is more likely related to cholecystitis itself or complications such as cholangitis or bile duct obstruction.
Choice B reason:
This statement is correct. Cholecystitis can cause bile salts to accumulate in the skin, leading to pruritus (itching). When the bile flow is obstructed or altered, bile salts may not be properly eliminated from the body, leading to their accumulation in the skin and causing itching.
Choice C reason:
Dehydration may occur in some cases of cholecystitis due to nausea, vomiting, or reduced fluid intake, but it is not the primary cause of pruritus.
Choice D reason:
Cholecystitis does not typically cause elevated blood sugar levels. However, certain conditions like diabetes mellitus may increase the risk of cholecystitis.
Explanation
Choice A reason:
Dark urine and pale-colored stools are not typically associated with a gastrointestinal infection. These symptoms are more indicative of changes in bile flow or bilirubin excretion.
Choice B reason:
While cholecystitis can lead to malabsorption of nutrients, it is not the primary cause of changes in stool color to pale.
Choice C reason:
This statement is correct. Cholecystitis can obstruct the bile duct, leading to a decrease in bilirubin excretion. Bilirubin gives urine its characteristic color, and when excretion is reduced, the urine becomes darker (brownish). Likewise, the absence of bilirubin in the stool leads to pale-colored or clay-colored stools.
Choice D reason:
Dehydration may occur in some cases of cholecystitis, but it is not the primary cause of changes in urine and stool color.
Explanation
Choice A reason:
Gastroenteritis typically presents with symptoms such as diarrhea, vomiting, and abdominal cramps. It does not cause jaundice or severe right upper quadrant pain.
Choice B reason:
This statement is correct. Cholecystitis with cholangitis is characterized by severe right upper quadrant abdominal pain, fever, and jaundice. Cholangitis is an inflammation of the bile ducts, often caused by gallstone migration and obstruction.
Choice C reason:
A urinary tract infection may cause symptoms such as burning urination and frequent urination but does not present with right upper quadrant abdominal pain or jaundice.
Choice D reason:
GERD is a condition characterized by acid reflux and heartburn. It does not cause severe right upper quadrant abdominal pain or jaundice.
Explanation
Choice A reason:
Fasting for 12 hours is not required before an abdominal ultrasound. However, the client may be asked to avoid eating fatty or heavy meals before the procedure.
Choice B reason:
Filling the bladder with a gallon of water is unnecessary and not related to an abdominal ultrasound. A full bladder is required for pelvic ultrasounds, not abdominal ultrasounds.
Choice C reason:
Avoiding drinking liquids for 2 hours before the ultrasound is not necessary. In fact, a full bladder is preferred for better visualization during an abdominal ultrasound.
Choice D reason:
This statement is correct. To have a full bladder for the ultrasound, the client should drink 16 ounces of water about one hour before the procedure. A full bladder helps lift the intestines and improves the visualization of the gallbladder and surrounding structures.
Explanation
Choice A reason:
This statement is incorrect. The HIDA scan does not use magnetic resonance imaging (MRI) to visualize the gallbladder. It is a nuclear medicine test that uses a radioactive tracer.
Choice B reason:
This statement is incorrect. While the HIDA scan involves the use of a radioactive tracer, its purpose is not to evaluate liver function. Instead, it assesses the biliary system and gallbladder.
Choice C reason:
This statement is correct. The HIDA scan is a nuclear medicine test used to assess the patency of the biliary system and the emptying of the gallbladder. A radioactive tracer is injected into the client's bloodstream, and its uptake and excretion into the biliary system are monitored.
Choice D reason:
This statement is incorrect. The HIDA scan does not involve the use of an endoscope. It is a non-invasive imaging test that is performed externally, not internally.
Explanation
Choice A reason:
Serum amylase is typically elevated in pancreatitis, not cholecystitis.
Choice B reason:
Blood urea nitrogen (BUN) is a kidney function marker and is not directly related to cholecystitis.
Choice C reason:
This statement is correct. Serum bilirubin is commonly elevated in cholecystitis due to bile duct obstruction or impaired bile flow. Elevated bilirubin levels can cause jaundice (yellowing of the skin and eyes) in some cases.
Choice D reason:
C-reactive protein (CRP) is a marker of inflammation and can be elevated in various conditions, including cholecystitis. However, it is not specific to cholecystitis and may also be elevated in other inflammatory processes.
Explanation
Choice A reason:
This statement is incorrect. ERCP does not involve the use of magnetic resonance imaging (MRI). It is an endoscopic procedure that combines endoscopy with fluoroscopy to visualize the biliary system.
Choice B reason:
This statement is incorrect. ERCP uses a contrast dye, not a radioactive tracer, to visualize the biliary system and identify abnormalities or obstructions.
Choice C reason:
This statement is correct. ERCP is an invasive procedure that involves the use of an endoscope. The endoscope is inserted through the mouth and guided through the digestive tract to the duodenum, where contrast dye is injected into the biliary and pancreatic ducts to visualize their structures and identify any abnormalities.
Choice D reason:
This statement is incorrect. ERCP is not a non-invasive test that uses sound waves. It is an invasive procedure that requires the insertion of an endoscope into the body to view the biliary system.
Explanation
Choice A reason:
This statement is correct. Laparoscopic cholecystectomy involves making several small incisions, resulting in less postoperative pain, reduced scarring, and a shorter hospital stay compared to open surgery.
Choice B reason:
Open surgery may have advantages in certain situations, but for uncomplicated cases of acute cholecystitis, laparoscopic surgery is generally preferred due to its minimally invasive nature.
Choice C reason:
Laparoscopic surgery is associated with a shorter recovery time and faster return to normal activities compared to open surgery.
Choice D reason:
Laparoscopic surgery is not associated with a higher risk of postoperative infection. In fact, it is known for having lower rates of surgical site infections compared to open surgery.
Explanation
Choice A reason:
This statement is correct. Administering an antiemetic medication can help alleviate nausea and vomiting, which are common side effects of opioid analgesics used for postoperative pain management.
Choice B reason:
Eating a high-fat diet is not recommended after cholecystectomy, as the gallbladder has been removed. Consuming high-fat foods may exacerbate symptoms and lead to digestive discomfort.
Choice C reason:
While nausea and vomiting can be common after surgery, it is important to address these symptoms to ensure the client's comfort and prevent dehydration or other complications.
Choice D reason:
Requesting additional opioids to manage pain may worsen the nausea and vomiting. It is essential to balance pain management with measures to minimize side effects like nausea.
Explanation
Choice A reason:
Engaging in strenuous physical activities may exacerbate the pain and discomfort in a client with chronic cholecystitis. Moderate physical activity is encouraged, but strenuous activities should be avoided.
Choice B reason:
This statement is correct. Applying a heating pad on the abdomen can help alleviate pain and discomfort associated with chronic cholecystitis. Heat therapy helps relax muscles and may ease the tension in the affected area.
Choice C reason:
Consuming a high-fat diet is not recommended for a client with chronic cholecystitis. A low-fat diet is recommended to reduce gallbladder stimulation and prevent symptoms.
Choice D reason:
While over-the-counter NSAIDs can be effective for mild pain relief, they should be used with caution in clients with cholecystitis, especially if there is any concern about gallstone-related inflammation. It is best to consult with a healthcare provider before using NSAIDs in this case.
Explanation
Choice A reason:
While pain relief is important, it is essential to address the redness and swelling first, as they may indicate an infection or other complication related to the cholecystostomy.
Choice B reason:
This statement is correct. The nurse should notify the healthcare provider immediately about the client's symptoms and findings to ensure prompt evaluation and appropriate interventions.
Choice C reason:
Applying an ice pack may provide some relief for pain and inflammation, but it does not address the potential underlying cause of redness and swelling.
Choice D reason:
Changing the dressing and cleaning the insertion site is important for maintaining cleanliness, but the nurse should first notify the healthcare provider about the client's symptoms for further evaluation.
Explanation
Choice A reason:
Resuming physical activities immediately after surgery may put the client at risk of complications and delayed healing. It is essential to allow sufficient time for recovery before engaging in physical activities.
Choice B reason:
Waiting only 24 hours may not provide enough time for the client to recover from the surgery and avoid potential complications.
Choice C reason:
This statement is correct. The client can start light physical activities within a few days after the surgery, as long as they are tolerated well. Gradually increasing physical activities over time is important to prevent strain and ensure a safe recovery.
Choice D reason:
Avoiding physical activities for four weeks is unnecessary and may lead to physical deconditioning. Gradual reengagement in physical activities is encouraged to support the healing process.
Explanation
Choice A reason:
Resuming a regular diet immediately after a cholecystectomy may be too heavy for the digestive system, which is still recovering from the surgery.
Choice B reason:
This statement is correct. Following a low-fat diet for several weeks after a cholecystectomy can reduce the strain on the digestive system and allow the body to adjust to the absence of the gallbladder.
Choice C reason:
While protein is essential for wound healing, a high-protein diet is not specifically recommended for a client recovering from a cholecystectomy.
Choice D reason:
Avoiding all solid foods for 24 hours after the surgery is unnecessary and may lead to nutritional deficits. The client can gradually resume a low-fat, solid diet after the surgery.
Explanation
Choice A reason:
Administering pain medication is important, but assessing the client's vital signs and pain level takes priority to determine the severity of the pain and the appropriate intervention.
Choice B reason:
This statement is correct. Assessing the client's vital signs and pain level is the first action the nurse should take to evaluate the client's condition and determine the appropriate intervention.
Choice C reason:
Placing the client in a semi-Fowler's position may provide some comfort, but it does not address the underlying pain or assist in determining the severity of the situation.
Choice D reason:
Offering herbal tea for relaxation is a non-pharmacological intervention that can be helpful, but it is not the first action the nurse should take when the client is experiencing severe abdominal pain.
Explanation
Choice A reason:
While cholecystectomy is a common procedure, minimizing the client's fear and anxiety by downplaying the risks is not appropriate. It is essential to acknowledge the client's concerns and address them appropriately.
Choice B reason:
Avoiding thinking about the surgery may not be helpful for the client. It is essential to encourage open communication and support the client in expressing their fears and concerns.
Choice C reason:
This statement is correct. Encouraging the client to express their fears and concerns allows the nurse to address them appropriately and provide the necessary support and information to reduce anxiety.
Choice D reason:
While sharing personal experiences can sometimes be helpful, it is essential to focus on the client's feelings and needs rather than diverting attention to the nurse's experience.
Explanation
Choice A reason:
Deep breathing exercises do not directly prevent postoperative infection. However, they can help with postoperative lung expansion and prevent respiratory complications, indirectly reducing the risk of infection.
Choice B reason:
While deep breathing exercises can help improve respiratory function, they are not specifically targeted at strengthening abdominal muscles.
Choice C reason:
This statement is correct. Deep breathing exercises promote lung expansion and prevent atelectasis (partial lung collapse) after surgery. They help maintain adequate oxygenation and prevent respiratory complications.
Choice D reason:
Deep breathing exercises are not directly related to reducing the risk of gallstone formation. Gallstone formation is primarily influenced by factors such as diet, bile composition, and gallbladder function.
Explanation
Choice A reason:
Avoiding heavy lifting is important after a cholecystectomy to prevent strain on the surgical site and reduce the risk of complications.
Choice B reason:
Reporting signs of infection or wound complications is essential for early detection and appropriate management.
Choice C reason:
This statement indicates a need for further teaching. After a cholecystectomy, the client should follow a low-fat diet for several weeks before gradually reintroducing regular foods.
Choice D reason:
Taking prescribed pain medication as needed is essential for managing postoperative discomfort and promoting recovery.
Liver Cirrhosis
A client with liver cirrhosis is prescribed spironolactone to manage fluid retention. Which laboratory test should the nurse monitor closely while the client is on this medication?
Explanation
A) Spironolactone is a potassium-sparing diuretic commonly used to manage fluid retention in liver cirrhosis. The nurse should monitor the client's serum potassium levels regularly as this medication can cause hyperkalemia (elevated potassium levels). It is important to assess potassium levels to avoid complications associated with imbalances in potassium levels.
B) Monitoring blood glucose levels is not specifically related to the use of spironolactone in liver cirrhosis. Spironolactone does not have a significant effect on blood glucose levels.
C) Monitoring the white blood cell count is not directly related to the use of spironolactone. White blood cell count is typically monitored to assess for signs of infection or immune system response.
D) Monitoring serum calcium levels is not directly related to the use of spironolactone in liver cirrhosis. Spironolactone does not significantly impact calcium levels in the blood.
A nurse is providing discharge instructions to a client with liver cirrhosis. Which statement by the nurse is appropriate regarding alcohol consumption?
Explanation
A) This statement is incorrect. Even moderate alcohol intake can be harmful to a client with liver cirrhosis. Alcohol should be completely avoided to prevent exacerbation of liver damage.
B) This statement is incorrect. The client should not resume their previous alcohol consumption habits. Continued alcohol consumption can lead to further liver damage and complications.
C) For a client with liver cirrhosis, alcohol consumption should be completely avoided. Alcohol is a significant contributor to liver damage and can worsen the condition, leading to further complications. Abstinence from alcohol is crucial to prevent further liver injury and improve the client's overall prognosis.
D) This statement is incorrect. The client should not consume any type of alcoholic beverage. All forms of alcohol can be harmful to the liver, and complete abstinence is necessary for individuals with liver cirrhosis.
A client with liver cirrhosis has developed ascites. Which nursing intervention is a priority for managing this complication?
Explanation
A) While adequate protein intake is important for overall health, encouraging the client to increase protein intake is not a priority in managing ascites. The priority is to address fluid retention through diuretic therapy.
B) While ambulation can be beneficial for clients with liver cirrhosis, it is not the priority for managing ascites. Diuretic therapy is more directly targeted at reducing fluid accumulation.
C) The priority nursing intervention for managing ascites in a client with liver cirrhosis is administering diuretics as prescribed by the healthcare provider. Diuretics help reduce fluid retention and alleviate the pressure caused by the accumulation of fluid in the abdomen. This intervention aims to improve the client's comfort and prevent the development of further complications associated with ascites.
D) Deep breathing exercises can be helpful for clients with liver cirrhosis, but they are not the priority for managing ascites. The focus should be on diuretic therapy and addressing the fluid retention in the abdomen.
Explanation
A) This statement is incorrect. Chronic hepatitis C infection is a significant risk factor for liver cirrhosis, and individuals with this infection require regular monitoring and appropriate medical management to prevent or delay the progression of cirrhosis.
B) While hepatitis D co-infection can worsen the course of chronic hepatitis B or C infection, it does not diminish the significance of hepatitis C infection as a risk factor for liver cirrhosis.
C) While chronic hepatitis B infection is also a known risk factor for liver cirrhosis, the client's history of hepatitis C infection is more relevant to the risk of developing cirrhosis in this case.
D) Chronic hepatitis C infection is a well-established risk factor for liver cirrhosis. The hepatitis C virus causes persistent inflammation in the liver, leading to liver cell damage and scarring (fibrosis). Over time, this fibrosis can progress to cirrhosis, which is the advanced stage of liver damage.
Explanation
A) Hemochromatosis is a genetic disorder characterized by excessive iron absorption from the diet, leading to the accumulation of iron in various organs, including the liver. In individuals with hemochromatosis, the excess iron can cause liver cell injury and lead to cirrhosis over time.
B) Wilson's disease is a genetic disorder that causes impaired copper metabolism, leading to copper accumulation in the liver and other organs. While it can lead to liver damage, it is not associated with elevated iron levels.
C) Alpha-1 antitrypsin deficiency is a genetic disorder that affects the lungs and liver. It can lead to liver disease, but it does not cause elevated iron levels.
D) Primary biliary cholangitis is an autoimmune liver disease that primarily affects the small bile ducts within the liver. While it can lead to liver damage and cirrhosis, it is not associated with elevated iron levels.
Explanation
A) Jaundice (yellowing of the skin and eyes) typically appears later in the course of liver cirrhosis and is usually associated with more advanced liver damage.
B) Ascites, the accumulation of fluid in the abdominal cavity, is a later manifestation of liver cirrhosis and usually occurs after significant liver damage has occurred.
C) Spider angiomas, also known as spider nevi or spider telangiectasias, are dilated blood vessels that appear as small red spots with tiny radiating legs. They are a common early sign of liver cirrhosis and result from increased pressure in the superficial blood vessels due to impaired liver function. Spider angiomas are often found on the face, neck, upper trunk, and arms.
D) Hepatic encephalopathy, a neuropsychiatric complication of advanced liver disease, is also a later manifestation of liver cirrhosis and is not an early sign of the condition.
Explanation
A) Hepatocellular carcinoma is a type of liver cancer and can be a complication of liver cirrhosis. However, it is not typically associated with difficulty sleeping or shortness of breath.
B) Portal hypertension, a common complication of liver cirrhosis, can lead to the development of ascites and esophageal varices, among other manifestations. It is not the likely cause of the client's difficulty sleeping and shortness of breath.
C) Hepatic encephalopathy is a neuropsychiatric complication of advanced liver disease and is not associated with difficulty sleeping or shortness of breath.
D) Hepatopulmonary syndrome is a complication of liver cirrhosis characterized by the development of pulmonary vascular dilation and arteriovenous shunting. This results in impaired oxygenation of blood, leading to difficulty breathing (dyspnea), especially while lying down (orthopnea). Clients with hepatopulmonary syndrome often experience frequent awakenings due to shortness of breath during sleep.
Explanation
A) Hematemesis refers to vomiting of blood and is a symptom that can occur as a result of bleeding from esophageal varices or other gastrointestinal sources.
B) Ascites is the accumulation of fluid in the abdominal cavity, leading to abdominal distension. It is not related to the presence of visible distended veins on the abdomen and chest.
C) Splenomegaly is the enlargement of the spleen and is not related to the finding of visible distended veins.
D) Varices are dilated and tortuous veins that can develop in various locations, including the esophagus (esophageal varices) and the abdomen and chest wall (caput medusae). In liver cirrhosis, portal hypertension causes increased pressure in the portal vein, leading to the development of these enlarged veins. Esophageal varices can be life-threatening if they rupture and cause severe bleeding.
Explanation
Jaundice refers to the yellowing of the skin and eyes and is caused by the accumulation of bilirubin in the blood. While jaundice can be associated with liver cirrhosis, it does not describe the symptom of severe itching.
Pruritus refers to severe itching of the skin, which can occur in clients with liver cirrhosis due to the buildup of bile acids in the blood and skin. Elevated levels of bile acids can irritate the skin, leading to itching.
Hematemesis refers to vomiting of blood and is not related to the symptom of severe itching.
Ascites is the accumulation of fluid in the abdominal cavity and is not related to the symptom of severe itching.
Explanation
A) Pain medication is not appropriate for managing altered mental status and confusion. The priority is to identify and address the underlying cause of the client's symptoms.
B) While documentation and ongoing monitoring are important, the priority is to take immediate action when the client is exhibiting signs of altered mental status. The nurse should promptly notify the healthcare provider for further evaluation and intervention.
C) A liver biopsy is a diagnostic procedure that provides information about the degree of liver damage and fibrosis. However, it is not the first action to take when the client is experiencing altered mental status and confusion. Immediate notification of the healthcare provider is the priority in this situation.
D) Altered mental status and confusion in a client with liver cirrhosis can indicate hepatic encephalopathy, a serious complication of advanced liver disease. Hepatic encephalopathy results from the accumulation of toxic substances in the blood due to impaired liver function. The nurse should prioritize notifying the healthcare provider immediately to initiate appropriate interventions and prevent further deterioration of the client's condition.
Explanation
A) Serum albumin is a protein synthesized by the liver, and its levels are often decreased in advanced liver cirrhosis due to impaired liver function. However, the question asks for an elevated finding, not a decreased one.
B) Prothrombin time (PT) measures the time it takes for blood to clot. In liver cirrhosis, PT is often prolonged due to impaired liver function and reduced production of clotting factors. However, the question asks for an elevated finding, not a prolonged one.
C) Aspartate aminotransferase (AST) is an enzyme found in the liver and other organs. While AST levels may be elevated in liver cirrhosis, it is not a specific marker for liver cirrhosis, and its elevation can occur in various liver diseases and conditions.
D) In liver cirrhosis, impaired liver function leads to reduced clearance of bilirubin, resulting in elevated total bilirubin levels in the blood. Elevated bilirubin is a common finding in liver cirrhosis and can contribute to jaundice.
Explanation
A) While MRI is also used to assess the liver, it may not be the first-line imaging modality for assessing the size and structure of the liver in clients with cirrhosis.
B) PET scans are mainly used to evaluate cellular metabolism and tissue function, including cancerous cells. While it can be helpful in detecting liver tumors, it may not be the primary choice for assessing liver size and structure in cirrhosis.
C) Computed tomography (CT) scan is commonly used to assess the liver's size, shape, and structure in clients with liver cirrhosis. CT provides detailed cross-sectional images of the liver, helping to identify any abnormalities, including liver nodules, fibrosis, and signs of portal hypertension.
D) An electroencephalogram (EEG) is a test used to record electrical activity in the brain. It is not used to assess the liver's size, shape, or structure in clients with liver cirrhosis.
Explanation
A) In liver cirrhosis, portal hypertension occurs due to increased pressure in the portal vein, which carries blood from the intestines to the liver. The increased pressure leads to the development of portosystemic collaterals (collateral circulation) to divert blood flow. This can cause hypersplenism, a condition where the spleen becomes enlarged and traps platelets, leading to a decreased platelet count (thrombocytopenia).
B) Ascites is the accumulation of fluid in the abdominal cavity and is not directly related to a decreased platelet count.
C) Hepatocellular carcinoma is a type of liver cancer and can be a complication of liver cirrhosis. However, it is not the likely cause of the client's decreased platelet count.
D) Splenomegaly (enlargement of the spleen) can occur in liver cirrhosis due to portal hypertension. However, splenomegaly itself is not the cause of the decreased platelet count; it is the hypersplenism resulting from the splenomegaly that causes thrombocytopenia.
A client with suspected liver cirrhosis undergoes a liver biopsy. Which nursing action is essential following the procedure?
Explanation
A. Encouraging the client to lie on the right side after a liver biopsy is essential because this position helps to apply pressure to the biopsy site, reducing the risk of bleeding.
B. While administering pain medication may be necessary, it is not the primary nursing action following a liver biopsy compared to ensuring hemostasis and preventing complications.
C. Monitoring vital signs is important, but in this case, vital signs should be checked more frequently than every 4 hours to assess for complications like bleeding. Initial monitoring is typically every 15 minutes for the first hour and then every 30 minutes to hourly based on facility protocols.
D. Although maintaining a supine position is typically advised, the focus should be on the right side position to ensure proper hemostasis following the biopsy procedure.
Explanation
A) Transient elastography is not used to assess esophageal varices. Endoscopy is the primary method for diagnosing and grading the severity of esophageal varices in clients with liver cirrhosis.
B) Transient elastography is primarily used to assess the degree of liver fibrosis, not to evaluate liver function or enzyme levels. Liver function and enzyme levels are typically evaluated through blood tests, such as liver function tests (LFTs), which measure liver enzymes, bilirubin, albumin, and other markers of liver health and function.
C) Transient elastography is a non-invasive imaging technique used to assess liver stiffness, which correlates with the degree of fibrosis in the liver. It provides information about the presence and severity of liver fibrosis, aiding in the diagnosis and staging of liver cirrhosis.
D) Transient elastography is not used to identify hepatic encephalopathy. Hepatic encephalopathy is a neuropsychiatric complication of advanced liver disease, and its diagnosis is based on clinical assessment, mental status evaluation, and laboratory tests. Transient elastography is not involved in identifying or diagnosing hepatic encephalopathy.
Explanation
A) While adequate protein intake is necessary for overall health, excessive protein intake may worsen hepatic encephalopathy in some clients with liver cirrhosis. The priority for this client is to avoid alcohol consumption, not necessarily to increase protein intake.
B) Clients with liver cirrhosis and associated ascites should be on a low-sodium diet to reduce fluid retention and prevent complications related to ascites.
C) Limiting fluid intake is not a standard recommendation for clients with liver cirrhosis. Instead, clients with ascites may be advised to follow a low-sodium diet and, if necessary, restrict fluid intake under the guidance of their healthcare provider.
D) For a client with liver cirrhosis, the most crucial dietary modification is to restrict alcohol consumption completely. Alcohol is a major contributing factor to liver damage and can exacerbate cirrhosis. Abstinence from alcohol is essential to prevent further liver injury and improve the client's overall prognosis.
Explanation
B) Furosemide is a diuretic used to treat fluid retention in clients with cirrhosis but is not effective in reducing ammonia levels or managing hepatic encephalopathy.
C) Propranolol is a beta-blocker often prescribed to reduce portal hypertension and prevent variceal bleeding in clients with liver cirrhosis. It is not used to treat hepatic encephalopathy.
D) Spironolactone is a diuretic used to manage fluid retention and ascites in clients with liver cirrhosis. Like furosemide, it is not effective in reducing ammonia levels or treating hepatic encephalopathy.
Explanation
A)Paracentesis is a procedure in which a needle or catheter is inserted into the peritoneal cavity to drain the accumulated fluid in clients with ascites. This procedure is performed to relieve abdominal pressure and discomfort, as well as to facilitate diagnostic testing on the ascitic fluid.
B) Thoracentesis is a procedure to drain fluid from the pleural cavity, which is the space surrounding the lungs. It is not used to treat ascites.
C) Pleurodesis is a procedure performed to create adhesions between the two layers of the pleura to prevent recurrent pleural effusions (fluid accumulation in the pleural cavity). It is not used to treat ascites.
D) Pericardiocentesis is a procedure to drain fluid from the pericardial sac surrounding the heart. It is not used to treat ascites.
Explanation
A) Lactulose is used to treat hepatic encephalopathy and is not prescribed to reduce the risk of bleeding from esophageal varices.
B) Omeprazole is a proton pump inhibitor used to reduce stomach acid production and treat conditions such as peptic ulcers and gastroesophageal reflux disease (GERD). While it may be prescribed to manage gastritis or peptic ulcers, it is not primarily used to reduce the risk of bleeding from esophageal varices.
C) Furosemide is a diuretic used to manage fluid retention and ascites in clients with liver cirrhosis. It is not prescribed to reduce the risk of bleeding from esophageal varices.
D) Propranolol is a beta-blocker commonly used to reduce the risk of bleeding from esophageal varices in clients with liver cirrhosis. Propranolol helps decrease portal hypertension by reducing the pressure in the portal vein, thereby reducing the likelihood of variceal rupture and bleeding.
Explanation
A) Iron supplements are not a priority intervention for a client with hepatic encephalopathy. In fact, administering iron supplements without proper indication can be harmful, as excessive iron can worsen liver damage in cirrhosis.
B) While monitoring fluid intake and output is important in managing various aspects of liver cirrhosis, it is not the essential intervention for hepatic encephalopathy. The priority in hepatic encephalopathy is to ensure seizure precautions and address the client's altered mental status.
C) Hepatic encephalopathy is a neuropsychiatric complication of liver cirrhosis that can lead to altered mental status, confusion, and potential seizures. Implementing seizure precautions is essential in the care of this client to ensure their safety and prevent injury during any potential seizure activity. Seizure precautions may include padding the side rails of the bed, ensuring a clear and clutter-free environment, and providing close supervision to the client. In severe cases, the healthcare provider may prescribe antiepileptic medications to manage and prevent seizures.
D) Encouraging a high-protein diet is not appropriate for a client with hepatic encephalopathy. High-protein diets can exacerbate hepatic encephalopathy by increasing ammonia production in the intestines. Instead, the client should be prescribed a controlled-protein diet and, in some cases, given lactulose to help reduce ammonia levels.
Explanation
A) Iron supplements are not indicated in the care of a client with liver cirrhosis and esophageal varices. The client's condition is related to portal hypertension and the risk of variceal bleeding, not blood clotting.
B) Monitoring fluid balance and daily weights is important in managing clients with liver cirrhosis, especially those with ascites. However, it is not the essential intervention specific to clients at risk of developing esophageal varices.
C) Elevating the head of the bed is a standard intervention to prevent aspiration in clients with various medical conditions. However, it is not the essential intervention specific to clients at risk of esophageal varices.
D) Encouraging the client to avoid straining during bowel movements is essential in the care of a client at risk of developing esophageal varices. Straining during bowel movements can increase intra-abdominal pressure, which may lead to increased pressure in the portal vein, potentially exacerbating portal hypertension and increasing the risk of variceal bleeding.
Explanation
A) Restricting fluid intake is not appropriate for managing ascites in clients with liver cirrhosis. Ascites occurs due to fluid accumulation in the peritoneal cavity and is not primarily influenced by oral fluid intake.
B) Encouraging a high-sodium diet is contraindicated in clients with ascites. High sodium intake can exacerbate fluid retention and worsen ascites. Instead, clients with ascites should be on a low-sodium diet to reduce fluid accumulation.
C) In a client with liver cirrhosis experiencing fluid retention and abdominal distension due to ascites, paracentesis is an essential intervention to drain the accumulated ascitic fluid from the abdominal cavity. Paracentesis helps to relieve discomfort, improve respiratory function, and reduce intra-abdominal pressure.
D) Diuretics are used in the management of ascites to promote urine output and reduce fluid retention. However, paracentesis is a more immediate intervention for relieving discomfort and removing a large volume of ascitic fluid.
Explanation
A) While lactulose can be taken with meals to minimize gastrointestinal discomfort, its effectiveness is not necessarily enhanced by taking it with meals. The timing and dosage of lactulose should be based on the healthcare provider's instructions.
B) Lactulose is a medication commonly used to manage hepatic encephalopathy in clients with liver cirrhosis. It works by reducing ammonia levels in the blood by promoting the excretion of ammonia through the stool. The nurse should instruct the client to expect one to two soft bowel movements per day while on lactulose, as this indicates the medication's effectiveness in removing ammonia from the body.
C) Lactulose is not associated with fluid overload, and there is no need to limit fluid intake while taking the medication. In fact, adequate hydration is important in clients with liver cirrhosis.
D) Lactulose is not known to significantly affect blood glucose levels, and there is no specific need for the client to monitor blood glucose levels while taking this medication.
A client with liver cirrhosis is at risk of bleeding due to decreased synthesis of clotting factors. Which nursing intervention is essential in preventing bleeding episodes?
Explanation
A) While ambulation and leg exercises are essential for maintaining overall health, they are not directly related to preventing bleeding episodes in clients with liver cirrhosis. The risk of bleeding in these clients is primarily related to clotting factor synthesis impairment.
B) Applying cold packs can help reduce swelling and inflammation but may not be the most appropriate intervention for preventing bleeding episodes in clients with liver cirrhosis. Cold packs may have limited effectiveness in addressing the underlying clotting factor deficiency.
C) Clients with liver cirrhosis may experience impaired clotting due to decreased synthesis of clotting factors by the liver. To prevent bleeding episodes, using a soft-bristle toothbrush for oral care is essential. A soft-bristle toothbrush is gentler on the gums and oral tissues, reducing the risk of causing trauma or bleeding during oral hygiene practices.
D) While it is important to administer intramuscular injections cautiously in clients with clotting disorders, this intervention is not the most essential for preventing bleeding episodes. Clients with liver cirrhosis are at risk of bleeding primarily due to the liver's decreased synthesis of clotting factors, not necessarily due to intramuscular injections.
A nurse is providing community education on the risk factors for liver cirrhosis. Which risk factor should the nurse emphasize as the leading cause of liver cirrhosis?
Explanation
A) Chronic viral hepatitis is a significant risk factor for liver cirrhosis, especially in regions where these viruses are prevalent. However, alcohol abuse is considered the leading cause of liver cirrhosis.
B) Among the listed risk factors, alcohol abuse is the leading cause of liver cirrhosis in many parts of the world. Prolonged and excessive alcohol consumption can directly damage liver cells, leading to inflammation and subsequent scarring. The risk of developing cirrhosis is closely related to the amount and duration of alcohol consumption.
C) NAFLD is a growing concern and a leading cause of liver disease globally. It is strongly associated with obesity, insulin resistance, type 2 diabetes, and metabolic syndrome. While NAFLD is a significant risk factor for liver cirrhosis, alcohol abuse holds the highest association with cirrhosis.
D) Autoimmune hepatitis is an immune-mediated liver disease that can lead to chronic inflammation and cirrhosis if not properly managed. While it is a risk factor for cirrhosis, alcohol abuse remains the leading cause of the condition.
Hernias
Explanation
Choice A reason:
This statement is correct. Hernias occur when an organ, such as the intestine or abdominal tissue, protrudes through a weakened area in the muscle or connective tissue.
Choice B reason:
This statement is correct. Heavy lifting, straining during bowel movements, or activities that increase intra-abdominal pressure can contribute to the development of hernias.
Choice C reason:
This statement is incorrect and indicates a need for further teaching. Not all hernias are visible as bulging lumps under the skin. Some hernias may not be externally noticeable and are diagnosed through imaging studies.
Choice D reason:
This statement is correct. Surgery is often the primary treatment for most types of hernias to repair the weakened area and prevent complications.
Explanation
Choice A reason:
This statement is incorrect. Being physically active and engaging in regular exercise can actually reduce the risk of hernias by strengthening the abdominal muscles and connective tissue.
Choice B reason:
This statement is incorrect. Having a high BMI is a risk factor for developing hernias. Excess weight can increase intra-abdominal pressure and weaken the abdominal muscles, making hernia development more likely.
Choice C reason:
This statement is correct. Smoking and chronic coughing can contribute to the development of hernias by putting increased pressure on the abdominal muscles and weakening the tissue.
Choice D reason:
This statement is incorrect. Family history can play a role in hernia development, as genetics can influence the strength of the abdominal muscles and connective tissue.
Explanation
Choice A reason:
A hiatal hernia occurs when a portion of the stomach protrudes into the chest through the diaphragm. It is not related to the groin area or influenced by coughing or heavy lifting.
Choice B reason:
An umbilical hernia occurs when a portion of the intestine or abdominal tissue pushes through the abdominal wall near the belly button. It is not related to the groin area or influenced by coughing or heavy lifting.
Choice C reason:
An incisional hernia occurs at the site of a previous surgical incision where the abdominal muscles have weakened. It is not related to the groin area or influenced by coughing or heavy lifting.
Choice D reason:
This statement is correct. An inguinal hernia is a type of hernia that occurs in the groin area and is characterized by a painful bulge that becomes more prominent during activities such as coughing or lifting heavy objects.
Explanation
Choice A reason:
A small, reducible lump that is painless to the touch is consistent with some types of hernias and may not be a cause for immediate concern. However, the healthcare provider should still be notified for further evaluation.
Choice B reason:
This statement is correct. Severe abdominal pain and distention with vomiting may indicate a complication of a hernia, such as bowel obstruction or strangulation, which requires immediate medical attention.
Choice C reason:
Mild discomfort that improves with rest and analgesics may be typical for some individuals with hernias. However, it is still essential to report any changes in symptoms to the healthcare provider.
Choice D reason:
Occasional burning sensation and acid reflux after meals are not directly related to hernias. These symptoms may indicate gastroesophageal reflux disease (GERD) or other gastrointestinal issues, which should be assessed by the healthcare provider.
Explanation
Choice A reason:
Lying down flat after meals can worsen heartburn and acid reflux, especially in clients with hiatal hernias. The client should remain in an upright position after meals to minimize symptoms.
Choice B reason:
Consuming large meals can increase stomach pressure and worsen symptoms for clients with hiatal hernias. Eating smaller, more frequent meals is recommended.
Choice C reason:
This statement is correct. Spicy and acidic foods can trigger heartburn and acid reflux in clients with hiatal hernias. Avoiding these foods can help alleviate symptoms.
Choice D reason:
Over-the-counter antacids may provide temporary relief for heartburn, but they are not a substitute for prescription medications. The client should follow the healthcare provider's prescribed treatment plan for managing the hiatal hernia and associated symptoms.
Explanation
Choice A reason:
This statement is correct. Umbilical hernias occur when a portion of the intestine or abdominal tissue pushes through the abdominal wall near the belly button (umbilicus).
Choice B reason:
This statement is correct. Umbilical hernias are more common in infants, as their abdominal muscles are still developing, and in pregnant women due to increased intra-abdominal pressure.
Choice C reason:
This statement is correct. Surgery is typically required to repair an umbilical hernia in adults, especially if the hernia is large, painful, or at risk of complications.
Choice D reason:
This statement is incorrect and indicates a need for further clarification. Umbilical hernias in adults can develop due to factors such as obesity, pregnancy, or chronic coughing. While avoiding heavy lifting may help prevent hernias in general, it is not the primary preventive measure for umbilical hernias.
Explanation
Choice A reason:
This statement describes the cause of an inguinal hernia, not an incisional hernia. An inguinal hernia occurs in the groin area and is often associated with heavy lifting or straining.
Choice B reason:
This statement is correct. An incisional hernia develops at the site of a previous surgical incision where the abdominal muscles have weakened. The weakness allows abdominal contents to protrude through the scar tissue.
Choice C reason:
This statement describes the cause of a hiatal hernia, not an incisional hernia. A hiatal hernia occurs when a portion of the stomach protrudes into the chest through the diaphragm.
Choice D reason:
This statement describes the cause of an umbilical hernia, not an incisional hernia. An umbilical hernia occurs near the belly button and is more common in infants.
Explanation
Choice A reason:
Mild discomfort and a reducible bulge in the hernia site may be present in some clients with hernias. While it is important to assess the hernia, these symptoms are not indicative of an incarcerated hernia.
Choice B reason:
This statement is correct. An incarcerated hernia occurs when the herniated tissue becomes trapped and cannot be reduced back into the abdominal cavity. It can lead to severe pain, nausea, and vomiting and requires immediate medical attention.
Choice C reason:
An occasional burning sensation after meals is not directly related to an incarcerated hernia. This symptom may indicate gastroesophageal reflux disease (GERD) or other gastrointestinal issues, which should be assessed by the healthcare provider.
Choice D reason:
A palpable lump that disappears when lying down is characteristic of a reducible hernia, not an incarcerated hernia. An incarcerated hernia cannot be manually reduced and may be associated with severe pain and other symptoms.
Explanation
Choice A reason:
This statement is incorrect. Femoral hernias are more common in women, not men. The anatomy of the female pelvis makes them more susceptible to femoral hernias.
Choice B reason:
This statement is correct. Chronic coughing and obesity can increase intra-abdominal pressure and contribute to the development of femoral hernias.
Choice C reason:
This statement describes the cause of an umbilical hernia in infants, not a femoral hernia. Femoral hernias are more common in adult women.
Choice D reason:
Wearing tight clothing can actually increase the risk of femoral hernias by putting additional pressure on the abdominal area. Loose, comfortable clothing is recommended to reduce the risk of hernia development.
Explanation
Choice A reason:
Having the client lift their legs while lying on their back is not a maneuver used to assess for a hiatal hernia. This position is more commonly used to assess for inguinal or femoral hernias in the groin area.
Choice B reason:
Palpating the abdomen for tender areas or masses is a general abdominal assessment and may not specifically assess for a hiatal hernia.
Choice C reason:
Auscultating for bowel sounds in all quadrants of the abdomen is also part of a general abdominal assessment and does not specifically target a hiatal hernia.
Choice D reason:
This statement is correct. Asking the client to take a deep breath and palpating the upper abdomen can help the nurse assess for a hiatal hernia. The nurse may feel for a soft bulge or protrusion in the upper abdominal area, which may indicate a hiatal hernia.
Explanation
Choice A reason:
This statement is incorrect. Engaging in regular physical activity and exercise can actually reduce the risk of hernias by promoting stronger abdominal muscles and overall health.
Choice B reason:
This statement is incorrect. Being underweight and having a low BMI may increase the risk of hernias as there may be reduced muscle mass and weaker tissues.
Choice C reason:
This statement is correct. Having a family history of hernias and weak connective tissues are significant risk factors for developing hernias.
Choice D reason:
This statement is incorrect. Wearing tight clothing and heavy lifting can increase intra-abdominal pressure and contribute to the development of hernias.
Explanation
Choice A reason:
Having a sedentary lifestyle and avoiding physical activity can increase the risk of hernias by promoting weaker abdominal muscles, but it is not specific to inguinal hernias.
Choice B reason:
This statement is correct. Chronic constipation and straining during bowel movements can increase intra-abdominal pressure and contribute to the development of inguinal hernias.
Choice C reason:
Being pregnant or using hormonal contraceptives may increase the risk of other types of hernias, such as umbilical hernias, but they are not significant risk factors for inguinal hernias.
Choice D reason:
Being of Asian descent and having a family history of hernias may be risk factors for hernias in general, but they are not specific to inguinal hernias.
Explanation
Choice A reason:
Being male and having a history of chronic constipation may increase the risk of other types of hernias, but they are not significant risk factors for femoral hernias.
Choice B reason:
Having a sedentary lifestyle and avoiding physical activity can increase the risk of hernias in general, but they are not specific to femoral hernias.
Choice C reason:
This statement is correct. Being pregnant or obese are significant risk factors for developing femoral hernias due to increased intra-abdominal pressure and weakened tissues.
Choice D reason:
Having a family history of hernias and weak abdominal muscles may be risk factors for hernias in general, but they are not specific to femoral hernias.
Explanation
Choice A reason:
The client's history of chronic coughing and straining during bowel movements may increase the risk of other types of hernias, but they are not significant risk factors for incisional hernias.
Choice B reason:
The client's recent history of heavy lifting and physical exertion can increase the risk of hernias in general, but they are not specific to incisional hernias.
Choice C reason:
The client's family history of hernias and weak connective tissues may be risk factors for hernias in general, but they are not specific to incisional hernias.
Choice D reason:
This statement is correct. Incisional hernias occur at the site of a previous surgical incision where the abdominal muscles and tissues may be weakened, leading to the protrusion of abdominal contents.
Explanation
Choice A reason:
While hernias can occur in infants and young children, they are not more common in this age group due to weak abdominal muscles. Inguinal hernias are more common in infants, but other types of hernias may have different age distributions.
Choice B reason:
This statement is correct. Hernias are primarily seen in older adults and the elderly due to age-related changes in connective tissues, such as a decrease in collagen and elastin fibers.
Choice C reason:
This statement is incorrect. Age is a significant risk factor for hernias, and they are more common in older adults.
Choice D reason:
Hernias are more common in older adults than in adolescents and young adults. Rapid growth during adolescence may increase the risk of certain types of hernias, but it is not the primary age group affected by hernias.
Explanation
Choice A reason:
This statement is correct. Inguinal hernias typically present with pain and swelling in the lower abdomen and groin area.
Choice B reason:
Severe back pain radiating to the legs is not a typical symptom of inguinal hernia. This symptom may indicate other conditions such as lumbar disc herniation.
Choice C reason:
Nausea and vomiting are not common symptoms of inguinal hernia. These symptoms may be present in other gastrointestinal conditions.
Choice D reason:
Pain and tenderness in the upper abdomen are not specific to inguinal hernia. These symptoms may indicate other conditions such as gallbladder problems.
Explanation
Choice A reason:
Incisional hernias occur at the site of a previous surgical incision and may not change with positional changes.
Choice B reason:
This statement is correct. Umbilical hernias are characterized by a bulge or lump in the abdominal area that is more noticeable when standing or exerting pressure and may disappear when lying down.
Choice C reason:
Femoral hernias are typically located in the upper thigh and may not be affected by positional changes.
Choice D reason:
Indirect inguinal hernias may present with a bulge or lump in the inguinal area, but the lump typically does not change with positional changes.
Explanation
Choice A reason:
Pain and swelling in the lower abdomen are not typical symptoms of hiatal hernia. These symptoms are more characteristic of inguinal or umbilical hernias.
Choice B reason:
This statement is correct. Heartburn and regurgitation of stomach acid are common symptoms of hiatal hernia. The herniated portion of the stomach can allow stomach acid to flow back into the esophagus, leading to heartburn and regurgitation.
Choice C reason:
Dyspnea and difficulty breathing are not typical symptoms of hiatal hernia. These symptoms may be present in other respiratory or cardiovascular conditions.
Choice D reason:
Pain and tenderness around the umbilicus are not specific to hiatal hernia. These symptoms may indicate other conditions such as umbilical hernia or appendicitis.
Explanation
Choice A reason:
This statement is correct. Assessing the client's blood pressure and heart rate is a priority in a client with an incarcerated hernia as it can indicate signs of compromised blood flow to the herniated tissue and potential strangulation.
Choice B reason:
Obtaining a detailed history of the client's diet and eating habits may be important for certain conditions, but it is not a priority assessment in a client with a suspected incarcerated hernia.
Choice C reason:
Evaluating the client's range of motion and joint flexibility may be relevant for musculoskeletal assessments, but it is not a priority in a client with a suspected incarcerated hernia.
Choice D reason:
Monitoring the client's oxygen saturation and respiratory rate may be important in various conditions, but it is not a priority assessment in a client with a suspected incarcerated hernia.
Explanation
Choice A reason:
This statement is correct. Strangulation of the herniated tissue is a potential complication of ventral hernia, leading to compromised blood flow to the hernia and possible tissue necrosis.
Choice B reason:
Developing gallstones is not a complication of ventral hernia. Gallstones are unrelated to this type of hernia.
Choice C reason:
Experiencing urinary retention and difficulty passing stool are not typical complications of ventral hernia. These symptoms may indicate other conditions affecting the urinary or gastrointestinal system.
Choice D reason:
Experiencing severe back pain and leg numbness are not specific to ventral hernia. These symptoms may indicate other musculoskeletal or neurological issues.
Explanation
Choice A reason:
While a physical examination and medical history can provide valuable information, imaging studies are often needed to visualize and confirm the presence of a hernia accurately.
Choice B reason:
Blood tests and urinalysis are not typically used to diagnose hernias. They may be ordered to assess for other conditions or rule out other possible causes of symptoms.
Choice C reason:
This statement is correct. Imaging studies such as ultrasound, CT scan, or MRI are commonly used to visualize and confirm the presence of a hernia, assess its size, location, and determine the most appropriate treatment.
Choice D reason:
A biopsy is not necessary to diagnose a hernia. A biopsy involves the removal of tissue for examination and is usually performed to assess for cancer or other abnormal growths.
Explanation
Choice A reason:
An abdominal X-ray is not routinely used to diagnose inguinal hernias. It is more commonly used to assess for other conditions involving the abdominal organs.
Choice B reason:
A barium swallow test is not used to diagnose inguinal hernias. It is typically used to evaluate the upper gastrointestinal tract.
Choice C reason:
This statement is correct. A diagnostic laparoscopy is a minimally invasive procedure in which a small camera is inserted into the abdominal cavity to visualize the hernia more clearly and may be ordered for certain cases of inguinal hernia.
Choice D reason:
An ECG is not necessary to diagnose or rule out inguinal hernias. It is used to assess heart function and rhythm.
Explanation
Choice A reason:
This statement is correct. Palpation of the abdominal area is specifically used to assess for umbilical hernias. The nurse will feel for a bulge or protrusion around the umbilical region when the client coughs or strains.
Choice B reason:
Auscultation of bowel sounds is a general assessment technique used to listen to the bowel sounds in the abdomen and is not specific to umbilical hernias.
Choice C reason:
Inspection of the oral cavity is not relevant to assessing for umbilical hernias. It is used for oral and dental examinations.
Choice D reason:
Percussion of the lung fields is not relevant to assessing for umbilical hernias. It is used to assess the lungs for abnormalities.
Explanation
Choice A reason:
Ultrasound may be used to assess some types of hernias, but it is not the most commonly used imaging study for assessing incisional hernias.
Choice B reason:
MRI (Magnetic Resonance Imaging) provides detailed images and may be used for assessing hernias, but it is not the most commonly used imaging study for incisional hernias.
Choice C reason:
This statement is correct. A CT (Computed Tomography) scan is most commonly used to assess incisional hernias as it provides detailed cross-sectional images of the abdominal wall and herniated tissues.
Choice D reason:
X-rays are not typically used to assess incisional hernias. X-rays provide limited information on soft tissues and are more commonly used for bone-related assessments.
Explanation
Choice A reason:
An ultrasound is not used to determine bacterial infections. It is primarily used for imaging soft tissues and organs.
Choice B reason:
This statement is correct. An ultrasound provides detailed images and is commonly used to confirm the presence and location of hernias.
Choice C reason:
An ultrasound is not typically used to assess blood flow to hernias. This type of assessment may be done using Doppler ultrasound or other imaging studies.
Choice D reason:
An ultrasound is not used to measure lung capacity or assess breathing difficulties related to hernias. It is used to visualize soft tissues and organs.
Explanation
Choice A reason:
Surgery is not the only option for managing a small reducible hernia. Some clients may choose conservative management or the use of a hernia belt if surgery is not immediately necessary or feasible.
Choice B reason:
This statement is correct. Clients with small reducible hernias may choose between surgical repair or using a hernia belt to provide support and reduce symptoms. The choice depends on the client's preference, overall health, and the severity of the hernia.
Choice C reason:
Conservative management with lifestyle modifications alone is not typically sufficient for managing a hernia. Surgical intervention or the use of a hernia belt may be necessary for symptom relief and to prevent complications.
Choice D reason:
Applying a warm compress is not a standard treatment for managing hernias. It may provide temporary relief for discomfort but does not address the underlying issue.
Explanation
Choice A reason:
This statement may be accurate, but the specific weight restriction and duration of restriction will depend on the individual client's surgical procedure and the surgeon's post-operative instructions.
Choice B reason:
Resuming regular activities immediately with no restrictions is not typical after hernia surgery. Clients usually have post-operative limitations and activity restrictions to promote healing and prevent complications.
Choice C reason:
This statement is correct. After the surgery, clients with incarcerated hernias may need to stay in the hospital for a few days for observation and recovery. The healthcare team will monitor for any potential complications and ensure the client's safety during the initial recovery period.
Choice D reason:
Performing vigorous abdominal exercises immediately after hernia surgery is not recommended. Clients need to allow the surgical site to heal before starting any strenuous activities, including exercise.
Explanation
Choice A reason:
Increased risk of developing gallstones is not a complication related to femoral hernia repair. Gallstones are unrelated to hernia surgery.
Choice B reason:
This statement is correct. The potential for recurrent hernia formation after the surgical repair is a complication that the nurse should discuss with the client. Recurrence can happen in some cases, and the client needs to be aware of this possibility.
Choice C reason:
Changes in vocal cord function are not related to femoral hernia repair. This complication is not relevant to hernia surgery.
Choice D reason:
Development of skin rashes and allergic reactions postoperatively are not typical complications of femoral hernia repair. These complications may occur in response to medications or dressings, but they are not directly related to the hernia surgery.
Explanation
Choice A reason:
This statement is not accurate. While anesthesia is administered during surgery to prevent pain, clients typically experience postoperative pain as the anesthesia wears off.
Choice B reason:
This statement is correct. The nurse should inform the client that pain medications will be provided as needed to manage postoperative pain effectively.
Choice C reason:
Providing a prescription for over-the-counter pain relievers is not typical for postoperative pain management. Clients usually receive prescription pain medications after hernia surgery.
Choice D reason:
Requiring the client to tolerate the pain without any pain medication is not appropriate. Adequate pain management is essential for client comfort and recovery after surgery.
Explanation
Choice A reason:
This statement is not accurate. Small incisions from laparoscopic hernia repair will heal, but they may leave small scars at the incision sites.
Choice B reason:
This statement is correct. Clients who undergo laparoscopic hernia repair may notice small scars at the incision sites, but these scars tend to fade over time.
Choice C reason:
While surgeons use special techniques to close laparoscopic incisions, it is unlikely that there will be no scars at all. Small scars are a normal outcome of this type of surgery.
Choice D reason:
Applying vitamin E oil to the incision sites may be helpful for some individuals, but it is not a guaranteed method to prevent scarring. Scarring is a natural part of the healing process after surgery.
Explanation
Choice A reason:
This statement is correct. While some redness and swelling are normal after surgery, a fever or drainage from the wound may indicate an infection and require medical attention.
Choice B reason:
Wound infection is not common after hernia surgery. It is essential to provide accurate information to the client to avoid unnecessary concerns.
Choice C reason:
While some drainage is normal after surgery, foul-smelling drainage may indicate an infection and require medical attention.
Choice D reason:
Bruising or discoloration around the incision site may be expected after surgery and does not necessarily indicate an infection.
Explanation
Choice A reason:
Taking a laxative daily may not be necessary and should only be done under the guidance of a healthcare provider. Overusing laxatives can lead to dependency and other gastrointestinal issues.
Choice B reason:
Resting in bed for an extended period can worsen constipation. Physical activity helps promote bowel movement and should be encouraged.
Choice C reason:
Reducing fluid intake is not recommended for managing constipation. Staying hydrated is essential to prevent further complications and maintain overall health.
Choice D reason:
This statement is correct. Engaging in light physical activity, such as walking, helps stimulate bowel movement and may relieve constipation caused by pain medications.
Explanation
Choice A reason:
This statement is not accurate. While anesthesia is administered during surgery to prevent pain, clients typically experience postoperative pain as the anesthesia wears off.
Choice B reason:
Pain after hernia surgery can vary from person to person, and some clients may require pain medications to manage postoperative discomfort effectively.
Choice C reason:
This statement is correct. Clients undergoing hernia repair surgery will typically be prescribed pain medications to manage postoperative discomfort.
Choice D reason:
Pain after hernia surgery is normal but usually improves over time. The duration of postoperative pain varies, and the client should follow the healthcare provider's guidance on pain management.
Explanation
Choice A reason:
The size and location of the hernia can affect the risk of recurrence. Larger hernias or those in certain locations may have a higher risk of recurrence.
Choice B reason:
Age and overall health can influence the risk of hernia recurrence. Certain health conditions and age-related factors may affect the body's ability to heal and recover after surgery.
Choice C reason:
This statement is correct. Smoking and obesity are risk factors that can increase the likelihood of hernia recurrence after surgical repair. These factors can impair wound healing and weaken the abdominal wall, making recurrence more likely.
Choice D reason:
The type of surgical repair can affect the risk of hernia recurrence. Different surgical techniques may have varying rates of success and recurrence, and the choice of repair should be discussed with the healthcare provider.
Explanation
Choice A reason:
Hernia repair surgery, like any surgical procedure, carries potential risks and complications, and it is not entirely risk-free.
Choice B reason:
While complications during hernia repair surgery are relatively infrequent, they are not extremely rare and can occur in certain cases.
Choice C reason:
This statement is correct. While hernia repair surgery is generally safe, there are potential risks and complications, such as infection, bleeding, or recurrence of the hernia. It is essential for the client to be aware of the potential risks and discuss any concerns with the healthcare provider.
Choice D reason:
Complications during hernia repair surgery are not common, and they should not be expected as a routine outcome. While some minor complications may occur, the overall goal is to minimize the risk of complications and provide safe and effective surgical care.
Ascites
Explanation
Choice A reason:
Ascites is not caused by an infection in the abdominal cavity. It is the result of fluid accumulation.
Choice B reason:
This statement is correct. Ascites is caused by the accumulation of excess fluid in the abdominal cavity, usually due to liver disease or other conditions that affect fluid balance in the body.
Choice C reason:
Blockage in the bile ducts may cause jaundice or other symptoms but is not the primary cause of ascites.
Choice D reason:
Ascites is not a genetic disorder and is not inherited from one's parents. It is a condition that develops due to various underlying medical conditions.
Explanation
Choice A reason:
Avoiding all physical activities is not recommended. Moderate physical activity can actually help improve circulation and fluid balance in the body.
Choice B reason:
This statement is correct. Limiting salt intake in the diet can help reduce fluid retention in clients with ascites, as excess sodium can contribute to fluid accumulation.
Choice C reason:
Increasing fluid intake may worsen fluid retention in clients with ascites. Clients with this condition should follow their healthcare provider's recommendations for fluid restriction.
Choice D reason:
A high-protein diet is not specifically indicated to promote reabsorption of fluid in the abdomen. It is essential for clients with cirrhosis and ascites to follow a balanced diet that meets their individual nutritional needs.
Explanation
Choice A reason:
Administering prescribed diuretics is essential in managing ascites, but it may not immediately address the client's respiratory distress.
Choice B reason:
This statement is correct. Elevating the head of the bed can improve respiratory mechanics and ease breathing for a client experiencing respiratory distress due to ascites.
Choice C reason:
Providing oxygen therapy is important for clients with respiratory distress, but it may not directly address the underlying cause of the distress in this situation.
Choice D reason:
Deep breathing exercises are beneficial for promoting lung expansion, but they may not be the priority in a client experiencing severe respiratory distress.
Explanation
Choice A reason:
Increased urine output and dehydration are not early signs of ascites progression. Ascites involves fluid accumulation in the abdominal cavity, not fluid loss through the urinary system.
Choice B reason:
Weight loss and decreased abdominal girth are not early signs of ascites progression. Ascites typically leads to increased abdominal girth and swelling.
Choice C reason:
This statement is correct. Visible abdominal swelling and distention are early signs of ascites progression. As fluid accumulates in the abdominal cavity, the abdomen may become visibly swollen and distended.
Choice D reason:
Reduced ankle edema and lower extremity swelling are not early signs of ascites progression. Ascites primarily affects the abdominal cavity, not the extremities.
Explanation
Choice A reason:
This statement is correct. Avoiding alcoholic beverages is essential for clients with cirrhosis to prevent further liver damage and fluid accumulation leading to ascites.
Choice B reason:
Increasing sodium intake is not recommended for clients with ascites, as excess sodium can contribute to fluid retention.
Choice C reason:
Engaging in strenuous physical activities may not be appropriate for clients with cirrhosis and ascites, as excessive exertion can worsen fluid retention and increase the risk of complications.
Choice D reason:
A high-fat diet is not recommended for clients with cirrhosis and ascites. A balanced diet with appropriate protein and carbohydrate intake is more appropriate for managing this condition.
Explanation
Choice A reason:
Heart failure can lead to fluid retention in the body, but it is not the most common cause of ascites. Liver disease, such as cirrhosis, is the leading cause of ascites.
Choice B reason:
Kidney disease can result in fluid retention, but it is not the primary cause of ascites.
Choice C reason:
Lung cancer is not a common cause of ascites. Liver disease, particularly cirrhosis, is the most prevalent reason for this condition.
Choice D reason:
This statement is correct. Liver disease, particularly cirrhosis, is the leading cause of ascites due to its impact on fluid balance in the body.
Explanation
Choice A reason:
Excessive alcohol consumption can contribute to kidney damage, but it is not the primary cause of ascites in individuals with chronic alcohol abuse.
Choice B reason:
Increased bile production and obstruction are not directly related to the development of ascites in clients with alcohol abuse.
Choice C reason:
This statement is correct. Chronic alcohol abuse can lead to liver damage, particularly cirrhosis, which impairs the liver's ability to regulate fluid balance, leading to ascites.
Choice D reason:
Heart failure can result in fluid overload, but it is not directly related to the development of ascites in individuals with alcohol abuse.
Explanation
Choice A reason:
Elevated blood glucose levels and insulin resistance are not directly related to the development of ascites in clients with hepatitis C.
Choice B reason:
Impaired blood clotting and increased bleeding tendencies are not directly associated with the development of ascites in clients with hepatitis C.
Choice C reason:
Altered immune response and increased infection risk are not the primary factors contributing to ascites in clients with hepatitis C.
Choice D reason:
This statement is correct. Chronic hepatitis C infection can lead to liver inflammation and fibrosis, which, in turn, can progress to cirrhosis, increasing the risk of developing ascites.
Explanation
Choice A reason:
Coughing and wheezing during physical activity are typical symptoms of congestive heart failure (CHF), but they do not directly indicate the presence of ascites.
Choice B reason:
Rapid and irregular heart rate at rest is a common manifestation of congestive heart failure (CHF) but does not directly indicate the presence of ascites.
Choice C reason:
This statement is correct. Ascites is characterized by the accumulation of fluid in the abdominal cavity, leading to swelling and distention in the lower abdomen.
Choice D reason:
Cold and clammy extremities are not typical manifestations of ascites and are not directly related to fluid overload in congestive heart failure (CHF).
Explanation
Choice A reason:
Regulation of blood glucose levels is not a primary function of the kidneys in fluid balance. It is primarily related to the endocrine system and insulin regulation.
Choice B reason:
Maintenance of acid-base balance is a critical function of the kidneys but is not directly related to fluid balance leading to ascites.
Choice C reason:
Production of red blood cells occurs in the bone marrow, not the kidneys. While the kidneys produce erythropoietin, a hormone that stimulates red blood cell production, this is not the primary function related to fluid balance.
Choice D reason:
This statement is correct. The kidneys' primary function related to fluid balance is filtration and excretion of waste products and excess fluid, which helps maintain proper fluid balance in the body. In chronic kidney disease (CKD), impaired kidney function can lead to fluid retention and contribute to the development of ascites.
Explanation
Choice A reason:
Increased urine output and dehydration are not typical findings in clients with ascites. Ascites involves fluid accumulation in the abdominal cavity, not fluid loss through the urinary system.
Choice B reason:
This statement is correct. Visible abdominal swelling and distention are characteristic signs of ascites, indicating the accumulation of fluid in the abdominal cavity.
Choice C reason:
Dry, cracked skin and itching are not specific to ascites and may be related to other conditions such as skin disorders or dehydration.
Choice D reason:
Rapid and irregular heart rate is not directly related to ascites. It may be associated with other conditions such as heart disease or infection.
Explanation
Choice A reason:
Pleural effusion is fluid accumulation in the pleural cavity (around the lungs), and it can be associated with ascites, but it is not the specific complication described in the scenario.
Choice B reason:
Pneumonia is a lung infection and is not directly related to the difficulty breathing and increased respiratory rate described in the client with ascites.
Choice C reason:
This statement is correct. Pulmonary edema is a potential complication of ascites in which excess fluid accumulates in the lungs, leading to difficulty breathing and an increased respiratory rate.
Choice D reason:
Atelectasis is the collapse of part or all of a lung, and while it can be associated with difficulty breathing, it is not directly related to ascites.
Explanation
Choice A reason:
Increased liver enzyme levels are not directly related to the abdominal pain and discomfort experienced by the client with ascites. Elevated liver enzymes indicate liver damage, but they do not cause abdominal pain.
Choice B reason:
Gallstone formation in the gallbladder is not directly related to the abdominal pain and discomfort experienced by the client with ascites.
Choice C reason:
This statement is correct. The abdominal pain and discomfort experienced by the client with ascites are primarily due to the stretching of the abdominal wall from the accumulation of fluid in the abdominal cavity.
Choice D reason:
Inflammation of the pancreas (pancreatitis) is not directly related to the abdominal pain and discomfort experienced by the client with ascites.
Explanation
Choice A reason:
Mild ankle edema is not uncommon in clients with fluid retention, such as ascites. While it requires monitoring, it does not indicate an immediate need for intervention.
Choice B reason:
Moderate abdominal distention is a common finding in clients with ascites and should be monitored, but it does not require immediate intervention.
Choice C reason:
Complaints of thirst and dry mouth may indicate dehydration, which should be addressed, but it does not require immediate intervention as other options.
Choice D reason:
This statement is correct. Respiratory distress and cyanosis are concerning findings in a client with ascites, as they may indicate severe pulmonary edema or other respiratory complications that require immediate intervention and medical attention.
Explanation
Choice A reason:
Electrolyte imbalances can occur in clients with ascites, but they are not directly related to the symptoms of fatigue and weakness described by the client.
Choice B reason:
Iron deficiency anemia may be present in clients with chronic liver disease, but it is not the primary cause of the client's fatigue and weakness in this scenario.
Choice C reason:
Hepatic encephalopathy is a complication of liver disease, but it typically presents with neurological symptoms such as confusion, altered mental status, and behavior changes, not fatigue and weakness.
Choice D reason:
This statement is correct. Fatigue and weakness are common symptoms in clients with chronic liver disease and ascites, and they can be related to malnutrition, which is often seen in these clients due to poor appetite, nutrient malabsorption, and other factors related to liver dysfunction.
Explanation
Choice A reason:
An electrocardiogram (ECG) is used to assess heart rhythm and electrical activity, not to visualize ascites.
Choice B reason:
A chest X-ray is not specific to visualizing abdominal fluid accumulation and is not commonly used for diagnosing ascites.
Choice C reason:
This statement is correct. Abdominal ultrasound is commonly used to visualize and assess the presence of ascites by providing real-time images of the abdominal cavity, allowing healthcare providers to identify fluid accumulation.
Choice D reason:
A complete blood count (CBC) is a blood test that evaluates the number and types of blood cells. While it may be useful for other diagnostic purposes, it is not used to visualize ascites.
Explanation
Choice A reason:
Inserting a tube into the bladder to drain urine is not related to paracentesis, which involves withdrawing fluid from the abdominal cavity.
Choice B reason:
This statement is correct. Paracentesis is a procedure that involves inserting a needle into the abdomen to withdraw fluid from the abdominal cavity, typically to diagnose or relieve ascites.
Choice C reason:
Administering a contrast dye and performing an X-ray is not part of paracentesis and is not used to diagnose ascites.
Choice D reason:
Injecting medication into a joint for pain relief is not related to paracentesis or the management of ascites.
Explanation
Choice A reason:
Elevated blood glucose levels are not typically associated with ascites. Ascites is primarily related to fluid accumulation in the abdominal cavity, not glucose levels.
Choice B reason:
Increased white blood cell count may indicate infection or inflammation but is not directly related to the presence of ascites.
Choice C reason:
This statement is correct. Low albumin levels are commonly associated with ascites. Albumin is a protein produced by the liver that helps maintain fluid balance in the body. In liver disease, albumin levels may decrease, leading to fluid retention and the development of ascites.
Choice D reason:
Elevated thyroid-stimulating hormone (TSH) is not directly related to the presence of ascites.
Explanation
Choice A reason:
This statement is correct. Magnetic Resonance Imaging (MRI) is commonly used to evaluate the liver and abdominal organs, providing detailed images that can help assess the severity and extent of ascites in clients with cirrhosis.
Choice B reason:
An electroencephalogram (EEG) is used to assess brain activity and is not directly related to the evaluation of ascites in clients with cirrhosis.
Choice C reason:
Positron Emission Tomography (PET) scan is used to visualize metabolic activity in body tissues and is not commonly used for evaluating ascites.
Choice D reason:
Bone Density Scan (DEXA scan) is used to assess bone health and is not directly related to the evaluation of ascites in clients with cirrhosis.
Explanation
Choice A reason:
This statement is correct. Endoscopy can be used to visualize the upper gastrointestinal tract and assess for potential sources of bleeding or varices in the esophagus, which can be related to ascites in clients with liver disease.
Choice B reason:
Cardiac catheterization is used to assess the heart and blood vessels and is not directly related to determining the underlying cause of ascites.
Choice C reason:
Lumbar puncture is performed to obtain cerebrospinal fluid for diagnostic purposes and is not typically used to evaluate ascites.
Choice D reason:
Pulmonary function tests are used to assess lung function and are not directly related to determining the underlying cause of ascites.
Explanation
Choice A reason:
Administering diuretics may be part of the management plan, but it may not provide immediate relief to the client experiencing discomfort and difficulty breathing.
Choice B reason:
Elevating the head of the bed can help improve respiratory function, but placing the client in a side-lying position is more effective for facilitating fluid drainage from the abdomen and providing immediate relief to the client with ascites.
Choice C reason:
Deep breathing exercises are beneficial for improving lung capacity, but they may not provide immediate relief to the client experiencing discomfort and difficulty breathing due to ascites.
Choice D reason:
This statement is correct. Placing the client in a side-lying position helps to facilitate fluid drainage from the abdomen and can provide immediate relief to the client with ascites who is experiencing discomfort and difficulty breathing.
Explanation
Choice A reason:
Limiting protein intake is not typically recommended for clients with ascites, as protein is essential for maintaining muscle mass and overall health.
Choice B reason:
Avoiding foods high in potassium is important for clients with kidney problems, but it is not directly related to reducing fluid accumulation in the abdominal cavity for clients with ascites.
Choice C reason:
This statement is correct. Reducing sodium intake is essential to minimize fluid retention and help manage ascites. High sodium levels in the diet can lead to increased fluid retention in the body, exacerbating the accumulation of fluid in the abdominal cavity.
Choice D reason:
Increasing carbohydrate consumption for sustained energy is not directly related to reducing fluid accumulation in the abdominal cavity for clients with ascites.
Explanation
Choice A reason:
Withholding all oral medications on the day of the procedure may not be necessary and should be determined by the healthcare provider's instructions based on the specific medications the client is taking.
Choice B reason:
Administering an analgesic to the client before the procedure may be appropriate to relieve pain, but it should be prescribed and administered by the healthcare provider.
Choice C reason:
This statement is correct. Ensuring that the client has emptied the bladder before the paracentesis procedure is important to prevent any potential complications during the procedure.
Choice D reason:
Fasting for at least 12 hours before the procedure may not be necessary for a paracentesis, as it is typically a minor procedure and does not require prolonged fasting.
Explanation
Choice A reason:
Muscle weakness and fatigue are not commonly associated with spironolactone use.
Choice B reason:
Increased urine output and dehydration may occur with diuretics, but spironolactone is a potassium-sparing diuretic, so excessive urine output and dehydration are less likely to occur with this medication.
Choice C reason:
Hypotension and dizziness are potential side effects of some diuretics, but they are not specific to spironolactone use.
Choice D reason:
This statement is correct. Spironolactone is a potassium-sparing diuretic, which means it can lead to hyperkalemia (elevated potassium levels) if not monitored carefully. Hyperkalemia can cause irregular heart rhythms and other serious complications.
Explanation
Choice A reason:
Hypoglycemia and confusion are not commonly associated with therapeutic paracentesis. They may be related to other factors or underlying conditions in the client.
Choice B reason:
This statement is correct. After therapeutic paracentesis, the client may experience hypovolemia (decreased blood volume) due to the removal of a large amount of fluid. This can lead to decreased urine output and other signs of fluid depletion.
Choice C reason:
Hyperglycemia and increased thirst are not directly related to therapeutic paracentesis and are not commonly associated with this procedure.
Choice D reason:
Hypothermia and shivering are not typical complications of therapeutic paracentesis. The procedure is performed under controlled conditions to minimize the risk of temperature-related complications.
Explanation
Choice A reason:
Encouraging the client to lie flat in bed may worsen abdominal distention and discomfort. It is better to promote positions that facilitate fluid drainage, such as elevating the head of the bed or placing the client in a side-lying position.
Choice B reason:
Administering laxatives may not be appropriate for ascites management and could lead to electrolyte imbalances. It is essential to manage bowel movements cautiously, considering the client's fluid and electrolyte status.
Choice C reason:
This statement is correct. Assisting the client with regular and gentle ambulation can help facilitate fluid movement and reduce abdominal distention. Movement helps stimulate peristalsis and may improve drainage of fluid from the abdominal cavity.
Choice D reason:
Applying cold packs to the abdomen may provide temporary relief for localized pain but will not directly address the underlying issue of ascites or reduce abdominal distention.
Explanation
Choice A reason:
Hypoglycemia and confusion are not commonly associated with spironolactone use. They are unrelated to this medication.
Choice B reason:
This statement is correct. Spironolactone is a potassium-sparing diuretic, and one of its potential complications is hyperkalemia (elevated potassium levels). Hyperkalemia can lead to irregular heart rhythms and other serious cardiac problems.
Choice C reason:
Hypotension and dizziness may be potential side effects of certain diuretics but are not specific to spironolactone use.
Choice D reason:
Hypernatremia (elevated sodium levels) and increased thirst are not typically associated with spironolactone use.
Explanation
Choice A reason:
This statement is correct. Measuring abdominal girth and documenting findings are essential to monitor changes in fluid accumulation and assess the effectiveness of interventions.
Choice B reason:
Elevating the client's legs may help with edema in the lower extremities but will not directly address the fluid accumulation in the abdominal cavity.
Choice C reason:
Administering diuretics may be part of the management plan for ascites, but it may not be the initial intervention to address the client's current condition.
Choice D reason:
Applying an abdominal binder may be beneficial in certain cases, but it will not directly address the underlying cause of ascites or reduce fluid accumulation in the abdomen.
Explanation
Choice A reason:
This statement is correct. Weighing the client daily and recording the weight in the chart is an essential intervention to monitor fluid balance and detect any changes in body weight, which can indicate fluid retention or loss.
Choice B reason:
Measuring vital signs every four hours is important for assessing the client's overall condition, but it does not directly monitor fluid balance or hydration status.
Choice C reason:
Assessing urine output hourly is important, especially for clients with ascites who may have altered kidney function. However, it may not provide a comprehensive assessment of the client's overall fluid balance.
Choice D reason:
Restricting fluid intake may not be appropriate for all clients with ascites, as fluid restriction could lead to dehydration and further imbalances in fluid and electrolyte levels.
Explanation
Choice A reason:
Monitoring the client's blood pressure during the procedure is essential, but the nurse should prioritize administering an analgesic before the paracentesis to reduce pain and ensure the client's comfort during the procedure.
Choice B reason:
This statement is correct. Administering an analgesic before the procedure can help reduce pain and discomfort associated with paracentesis.
Choice C reason:
Restricting the client's fluid intake before the procedure is not necessary, as paracentesis is typically performed to remove fluid from the abdominal cavity and provide relief for the client.
Choice D reason:
Maintaining a supine position during the procedure is not required. The nurse should position the client comfortably, which may include elevating the head of the bed or placing the client in a side-lying position to facilitate fluid drainage.
QUESTION
Cholelithiasis
Explanation
Choice A reason:
Offering antacid medication may provide relief for indigestion, but it will not address the severe pain and other symptoms associated with cholelithiasis.
Choice B reason:
Placing the client in a supine position may not be the most comfortable position for someone experiencing severe pain from cholelithiasis. The client may prefer to find a position that eases the pain.
Choice C reason:
This statement is correct. Administering prescribed pain medication should be the first action to address the client's severe pain and discomfort related to cholelithiasis.
Choice D reason:
Encouraging the client to rest is important, but it is not the priority action in managing the client's severe pain and other symptoms.
Explanation
Choice A reason:
Instructing the client to eat a high-fat diet before surgery is not appropriate and may exacerbate the symptoms of cholelithiasis. The client should follow a low-fat diet instead.
Choice B reason:
This statement is correct. Demonstrating deep-breathing exercises helps promote lung expansion postoperatively and prevents respiratory complications after anesthesia and surgery.
Choice C reason:
While ambulating is essential after surgery, it may not be the primary focus of preoperative education for a client undergoing cholecystectomy for cholelithiasis.
Choice D reason:
Discussing the possibility of experiencing diarrhea after the surgery is not a priority in preoperative education for a client with cholelithiasis undergoing cholecystectomy.
Explanation
Choice A reason:
Administering an antipyretic medication may help reduce the fever, but it does not address the underlying issue of the suspected infection. Notifying the healthcare provider about the client's symptoms is the priority action.
Choice B reason:
This statement is correct. The nurse should notify the healthcare provider immediately about the client's severe pain, fever, and chills to initiate appropriate assessment and treatment for a possible infection.
Choice C reason:
Encouraging the client to increase oral fluid intake is important for overall hydration, but it may not be the priority action when an infection is suspected.
Choice D reason:
Placing a heating pad on the client's abdomen may provide temporary relief for discomfort but is not appropriate when the client has a fever and suspected infection.
Explanation
Choice A reason:
This statement is correct. UDCA is a medication used to dissolve gallstones, and one of its potential adverse effects is diarrhea and abdominal cramping.
Choice B reason:
Dizziness and lightheadedness are not common adverse effects of UDCA.
Choice C reason:
Dry mouth and blurred vision are not typical adverse effects of UDCA.
Choice D reason:
Muscle weakness and fatigue are not common adverse effects of UDCA.
Explanation
Choice A reason:
This statement is correct. Engaging in regular physical activity to promote weight loss and maintain a healthy weight can help prevent the formation of gallstones, as obesity is a significant risk factor for cholelithiasis.
Choice B reason:
Consuming a high-fat diet is not recommended for preventing gallstones. A high-fat diet is associated with an increased risk of gallstone formation.
Choice C reason:
Avoiding fruits and vegetables to reduce fiber intake is not a healthy approach to preventing gallstones. Adequate fiber intake is beneficial for overall health and may help prevent gallstone formation.
Choice D reason:
Drinking sugary beverages is not recommended for preventing gallstones. It is essential to maintain hydration, but sugary beverages can contribute to obesity and other health problems, increasing the risk of cholelithiasis.
Explanation
Choice A reason:
This statement is correct. A family history of gallbladder disease is a significant risk factor for cholelithiasis, and the 25-year-old male is at the highest risk among the options provided.
Choice B reason:
A low-fat diet and regular exercise may help reduce the risk of developing cholelithiasis, so the 40-year-old female is at a lower risk compared to the other options.
Choice C reason:
A history of diabetes and hypertension may increase the risk of certain health problems, but they are not the primary risk factors for cholelithiasis in this context.
Choice D reason:
Undergoing bariatric surgery for weight loss may affect the risk of developing gallstones, but it is not the highest risk factor among the options provided.
Explanation
Choice A reason:
While hormones can influence gallbladder function, they do not directly cause gallbladder inflammation leading to gallstone formation.
Choice B reason:
Hormones may affect bile production, but it is not the primary mechanism leading to gallstone formation.
Choice C reason:
This statement is correct. Hormones, especially estrogen, can influence cholesterol metabolism in the gallbladder, leading to an increased risk of cholesterol gallstone formation.
Choice D reason:
Hormones do not weaken the gallbladder wall, and this is not a direct mechanism for gallstone accumulation.
Explanation
Choice A reason:
Frequent consumption of whole grains and vegetables is generally beneficial for health and may not significantly impact the risk of gallstone formation.
Choice B reason:
Engaging in regular physical activity and exercise is important for overall health, but it is not the primary risk factor for cholelithiasis among the options provided.
Choice C reason:
This statement is correct. A sedentary lifestyle and prolonged sitting are significant risk factors for gallstone formation. Physical inactivity can contribute to gallbladder stasis and increase the risk of gallstone development.
Choice D reason:
High consumption of lean protein and low-fat dairy products may be part of a healthy diet, but they are not the primary risk factor for cholelithiasis.
Explanation
Choice A reason:
This statement is correct. Rapid weight loss, especially when accompanied by a high-fat diet, can increase the risk of gallstone formation. Rapid weight loss can lead to an imbalance in bile composition, increasing the likelihood of gallstone development.
Choice B reason:
This statement is incorrect. Rapid weight loss can impact gallstone formation, and it is essential for the client to be aware of this potential risk.
Choice C reason:
Rapid weight loss does not reduce the risk of gallstone formation. In fact, it may increase the risk due to changes in bile composition and gallbladder motility.
Choice D reason:
This statement is incorrect. Rapid weight loss, especially with a low-fat diet, can contribute to gallstone formation due to changes in bile composition and gallbladder function.
Explanation
Choice A reason:
Antacids are not typically associated with an increased risk of gallstone formation.
Choice B reason:
Statins are used for cholesterol management and are not directly associated with gallstone formation.
Choice C reason:
Antibiotics are used to treat infections and do not significantly impact the risk of gallstone formation.
Choice D reason:
This statement is correct. Hormonal contraceptives, especially those containing estrogen, are associated with an increased risk of gallstone formation due to their impact on cholesterol metabolism in the gallbladder.
Explanation
Choice A reason:
This statement is correct. The pain in the right upper abdomen that radiates to the right shoulder is characteristic of referred pain, which occurs when pain is perceived in an area away from the actual source of the pain.
Choice B reason:
Colicky pain is intermittent, severe pain that comes and goes and is not specific to the description given by the client.
Choice C reason:
Sharp pain may be used to describe certain types of pain, but it does not capture the radiation to the right shoulder as seen in referred pain.
Choice D reason:
Steady pain may not adequately describe the intermittent nature of the pain experienced by the client.
Explanation
Choice A reason:
Anorexia refers to a loss of appetite and is not specific to the client's complaint.
Choice B reason:
Dysphagia refers to difficulty swallowing and is not related to the client's symptoms.
Choice C reason:
This statement is correct. Dyspepsia is the medical term for indigestion or discomfort in the upper abdomen, often associated with nausea and vomiting after eating fatty or heavy meals, which is consistent with the client's complaint.
Choice D reason:
Steatorrhea refers to the presence of excess fat in the feces and is not related to the client's symptoms.
Explanation
Choice A reason:
Eructation refers to belching or burping and is not related to excessive gas after meals.
Choice B reason:
Borborygmi refers to stomach growling or rumbling and is not related to the client's symptom.
Choice C reason:
This statement is correct. Flatulence refers to the passing of excessive gas from the digestive system, which can cause feelings of bloating and discomfort after meals, as reported by the client.
Choice D reason:
Ascites refers to the accumulation of fluid in the abdominal cavity and is not related to the client's symptom.
Explanation
Choice A reason:
Referred pain is when pain is perceived in an area away from the actual source of the pain and does not specifically describe pain after eating a large meal.
Choice B reason:
Colicky pain is characterized by intermittent, severe pain that comes and goes and is not specific to the client's complaint.
Choice C reason:
This statement is correct. Biliary colic refers to the severe, cramping pain that occurs when the gallbladder contracts against a gallstone lodged in the cystic duct or common bile duct, and it is often triggered or worsened by eating a large or fatty meal.
Choice D reason:
Hyperalgesia refers to an increased sensitivity to pain and is not related to the client's symptom.
Explanation
Choice A reason:
This statement is correct. Jaundice refers to the yellowish discoloration of the skin and eyes caused by an accumulation of bilirubin, which can occur in cholelithiasis due to obstruction of the bile ducts by gallstones.
Choice B reason:
Erythema refers to redness of the skin and is not related to the client's complaint.
Choice C reason:
Pallor refers to paleness of the skin and is not related to the client's symptom.
Choice D reason:
Petechiae refers to small, pinpoint-sized red or purple spots on the skin caused by bleeding and is not related to the client's symptom.
Explanation
Choice A reason:
Assessing blood flow to the liver is not the primary purpose of an abdominal ultrasound in a client with suspected cholelithiasis.
Choice B reason:
This statement is correct. An abdominal ultrasound is a non-invasive imaging test that provides detailed images of the gallbladder and surrounding structures, helping to visualize the presence of gallstones and assess the gallbladder's condition.
Choice C reason:
Measuring acidity levels in the stomach is not related to the diagnostic evaluation of cholelithiasis.
Choice D reason:
Evaluating kidney function is not the primary purpose of an abdominal ultrasound for a client with suspected cholelithiasis.
Explanation
Choice A reason:
Fasting for 24 hours is not necessary for an abdominal ultrasound for cholelithiasis evaluation.
Choice B reason:
Avoiding drinking water for 6 hours before the test is not required for an abdominal ultrasound.
Choice C reason:
This statement is correct. Clients undergoing an abdominal ultrasound for suspected cholelithiasis may be asked to eat a low-fat meal before the test to stimulate gallbladder contraction and enhance visualization of the gallbladder and bile ducts.
Choice D reason:
While there may be no specific dietary restrictions, eating a low-fat meal is often recommended to facilitate the evaluation of cholelithiasis during the ultrasound.
Explanation
Choice A reason:
While elevated serum bilirubin levels can be associated with cholelithiasis, they are more indicative of obstruction of the bile ducts, which can occur in cholecystitis, a complication of cholelithiasis.
Choice B reason:
Increased blood glucose levels are not directly related to cholelithiasis or its complications.
Choice C reason:
This statement is correct. An elevated white blood cell count is often seen in cholecystitis, which is inflammation of the gallbladder that can occur as a complication of cholelithiasis.
Choice D reason:
Low serum amylase levels are not specific to cholelithiasis or its complications.
Explanation
Choice A reason:
Describing an endoscopy procedure, which is not involved in an oral cholecystogram, is not accurate.
Choice B reason:
This statement is correct. An oral cholecystogram (OCG) is a radiologic imaging test that involves swallowing a contrast dye, which outlines the gallbladder and bile ducts, allowing X-rays to visualize the presence of gallstones.
Choice C reason:
Removing a sample of the gallbladder tissue for examination would be a biopsy, not an oral cholecystogram.
Choice D reason:
A radioactive tracer injection is used in hepatobiliary iminodiacetic acid (HIDA) scan, not an oral cholecystogram.
Explanation
Choice A reason:
PTC is not used to remove gallstones from the common bile duct. It is primarily a diagnostic procedure.
Choice B reason:
Gallbladder function and contraction are not the primary focus of a percutaneous transhepatic cholangiography (PTC).
Choice C reason:
Obtaining a biopsy of the gallbladder is not the primary purpose of a PTC. It is mainly used for imaging and diagnostic purposes.
Choice D reason:
This statement is correct. PTC is a diagnostic imaging procedure that involves injecting contrast dye into the biliary tree to visualize the bile ducts and identify any obstructions, such as gallstones, which could be causing cholelithiasis.
A nurse is providing discharge instructions to a client who underwent cholecystectomy for cholelithiasis. Which statement by the client indicates a need for further teaching?
Explanation
Choice A reason:
This statement is correct. Avoiding fatty foods in the diet can help prevent the formation of future gallstones, as it reduces the likelihood of bile becoming too concentrated and forming stones.
Choice B reason:
This statement is correct. Taking prescribed antibiotics until they are finished is essential to prevent infection and complications after surgery.
Choice C reason:
This statement indicates a need for further teaching. Clients who have undergone cholecystectomy should avoid strenuous physical activities, including regular exercise, for several weeks after the surgery to promote proper healing and prevent complications.
Choice D reason:
This statement is correct. Reporting any signs of infection or bleeding at the incision site is crucial for the early detection and management of potential complications after surgery.
A nurse is caring for a client with cholelithiasis experiencing biliary colic. Which medication should the nurse anticipate administering to provide pain relief?
Explanation
Choice A reason:
Acetaminophen is an analgesic but may not provide sufficient pain relief for biliary colic.
Choice B reason:
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) but may not be the most effective option for pain relief in cases of biliary colic.
Choice C reason:
This statement is correct. Morphine sulfate is an opioid analgesic often used to provide pain relief for biliary colic, as it can effectively alleviate severe, cramping pain associated with gallstone obstruction.
Choice D reason:
Diphenhydramine is an antihistamine and is not used for pain relief in cases of biliary colic.
Explanation
Choice A reason:
This statement is correct. Clients undergoing ERCP should maintain NPO status for at least 8 hours before the procedure to ensure an empty stomach and reduce the risk of aspiration during sedation.
Choice B reason:
Administering a cleansing enema is not necessary for ERCP and is not a standard pre-procedure care intervention.
Choice C reason:
Withholding all medications for 24 hours before the procedure is not appropriate, as certain medications may be essential and should be discussed with the healthcare provider.
Choice D reason:
Providing a high-fat meal before the procedure is not recommended, as clients should maintain NPO status before ERCP.
Explanation
Choice A reason:
Resuming a normal diet immediately after surgery, especially if it is high in fat, can stress the digestive system and is not recommended after cholecystectomy.
Choice B reason:
Avoiding fatty foods for the first week after surgery is a general guideline, but clients should not limit their diet to this extent for an extended period.
Choice C reason:
This statement is correct. After cholecystectomy, clients can slowly reintroduce regular foods into their diet as tolerated. Gradually adding in more complex foods can help the body adjust to digestion without the gallbladder.
Choice D reason:
Continuing on a clear liquid diet for a few more days is not appropriate for a client who has already undergone cholecystectomy and has advanced past the initial post-operative phase.
Explanation
Choice A reason:
This statement is correct. Ursodeoxycholic acid is a medication used to dissolve cholesterol gallstones over time by reducing the cholesterol content of bile and promoting the solubility of cholesterol in bile.
Choice B reason:
While ursodeoxycholic acid can help prevent gallstone formation in some cases, its primary use is for dissolving existing cholesterol gallstones.
Choice C reason:
Ursodeoxycholic acid may have some anti-inflammatory properties, but its primary purpose is to dissolve gallstones.
Choice D reason:
Ursodeoxycholic acid is not typically used for pain relief during gallstone attacks. It is used for long-term management to dissolve gallstones and reduce the need for surgical intervention.
Explanation
Choice A reason:
Over-the-counter pain medications may not be sufficient to alleviate severe pain associated with gallstone obstruction.
Choice B reason:
This statement is correct. Severe pain caused by gallstone obstruction requires stronger pain management, and opioids may be prescribed to manage the pain effectively.
Choice C reason:
Applying a heating pad may not provide adequate pain relief for gallstone obstruction and could worsen the condition.
Choice D reason:
Position changes and deep breathing exercises may be helpful in some situations, but they are unlikely to provide sufficient relief for severe pain due to gallstone obstruction.
Explanation
Choice A reason:
While cholecystectomy is a common procedure, dismissing the client's concerns by downplaying the risk may not alleviate anxiety.
Choice B reason:
While expressing empathy is important, it does not address the client's concerns directly or provide detailed information about the procedure.
Choice C reason:
Involving family for support is beneficial, but it does not address the client's need for information and understanding about the surgery.
Choice D reason:
This statement is correct. The nurse should provide the client with detailed information about the cholecystectomy procedure, its benefits, potential risks, and complications. This information can help the client make informed decisions and alleviate anxiety.
Explanation
Choice A reason:
This statement is correct. The nurse's priority is to manage the client's pain effectively by administering prescribed pain medication.
Choice B reason:
Notifying the surgeon may be necessary if there are signs of complications, but managing the client's pain is the immediate priority.
Choice C reason:
Applying a cold pack may help with pain and swelling in some cases, but the nurse's priority is to administer pain medication first.
Choice D reason:
Instructing the client to perform deep breathing exercises is important for postoperative recovery, but it does not address the immediate need for pain management.
Explanation
Choice A reason:
Resuming normal activities immediately after surgery is not recommended, as the client needs time to recover and heal.
Choice B reason:
Avoiding physical activity for a whole week is not necessary in most cases, as clients are usually encouraged to ambulate and engage in light activity to prevent complications.
Choice C reason:
This statement is correct. After an open cholecystectomy, clients are generally encouraged to gradually increase their activity level as tolerated. However, they should avoid heavy lifting and strenuous activity for a few weeks to allow the surgical incision to heal.
Choice D reason:
Avoiding physical activity for six weeks is not typically required after a cholecystectomy. Gradual activity resumption is recommended earlier than that.
Explanation
Choice A reason:
Indigestion and discomfort are potential issues, but the primary reason for a low-fat diet after cholecystectomy is related to gallstone prevention and liver function.
Choice B reason:
There is no direct link between fatty foods and medication absorption in the context of post-cholecystectomy care.
Choice C reason:
This statement is correct. Following a low-fat diet after cholecystectomy helps prevent the formation of new gallstones and reduces stress on the liver, as the gallbladder's role in storing and releasing bile for
fat digestion is compromised.
Choice D reason:
While fatty foods can lead to digestive problems for some individuals, the primary concern in a client post-cholecystectomy is gallstone prevention and liver support.
Explanation
Choice A reason:
Avoiding foods high in fiber is not a recommended preventive strategy for gallstone formation.
Choice B reason:
This statement is correct. Staying well-hydrated and maintaining a healthy weight are important preventive measures for reducing the risk of gallstones.
Choice C reason:
Consuming a diet high in saturated fats can increase the risk of gallstone formation, not reduce it.
Choice D reason:
Limiting physical activity is not a preventive strategy for gallstone formation. Regular physical activity is beneficial for overall health, including gallbladder function.
Explanation
Choice A reason:
Avoiding all dairy products is not necessary for gallstone prevention, and it may lead to nutritional deficiencies.
Choice B reason:
This statement is correct. Including a variety of fruits and vegetables in the diet can promote gallbladder health and reduce the risk of gallstone formation.
Choice C reason:
Consuming large quantities of red meat is not a recommended preventive measure for gallstones. High red meat intake may actually increase the risk of gallstone formation.
Choice D reason:
Limiting fluid intake can lead to dehydration and increase the risk of gallstone formation. Adequate hydration is essential for gallbladder health.
Explanation
Choice A reason:
Continuing to eat a high-fat diet is not a preventive measure for gallstones. A low-fat diet is recommended after cholecystectomy.
Choice B reason:
Consuming small, frequent meals can help prevent gallbladder distension, but it is not the primary preventive measure for gallstones.
Choice C reason:
Avoiding physical activity is not a recommended preventive measure for gallstone formation. Regular exercise supports overall gallbladder function.
Choice D reason:
This statement is correct. Engaging in regular exercise is an important preventive measure for gallstone formation and overall gallbladder health.
Explanation
Choice A reason:
Avoiding all fruits and vegetables is not a recommended preventive strategy for gallstones. Fruits and vegetables are generally beneficial for overall health.
Choice B reason:
This statement is correct. Limiting the intake of fatty and fried foods is an important preventive measure to reduce the risk of gallstone formation.
Choice C reason:
Consuming large quantities of processed foods is not recommended for gallstone prevention. Processed foods are often high in unhealthy fats and additives.
Choice D reason:
Increasing alcohol intake is not a preventive measure for gallstones and may actually contribute to gallstone formation.
Explanation
Choice A reason:
Increasing the intake of fatty foods is not a recommended preventive measure for gallstones, especially in an overweight client.
Choice B reason:
Avoiding all carbohydrates is not necessary for gallstone prevention and may not be a healthy approach to weight management.
Choice C reason:
This statement is correct. Focusing on consuming a low-fat diet is an essential preventive measure for reducing the risk of gallstone formation, especially in overweight individuals.
Choice D reason:
Consuming large portions of dairy products is not a specific preventive measure for gallstones. A balanced diet with limited fat intake is recommended.
Explanation
Choice A reason:
Turmeric has anti-inflammatory properties and may be beneficial for gallbladder health.
Choice B reason:
Milk Thistle is commonly used to support liver function and can potentially be beneficial for gallstone prevention.
Choice C reason:
Ginger has anti-inflammatory properties and may help prevent gallstone formation.
Choice D reason:
Valerian Root is not typically used for gallstone prevention. It is primarily known for its sedative properties and may not have any direct impact on gallbladder health.
Explanation
Choice A reason:
Lithotripsy is not a surgical procedure to remove the gallbladder. It is a non-invasive method to break up gallstones.
Choice B reason:
This statement is correct. Lithotripsy involves using sound waves to break up gallstones into smaller fragments that can pass through the bile ducts.
Choice C reason:
Lithotripsy is not a medication. It is a procedure used to treat gallstones.
Choice D reason:
Lithotripsy is not a diagnostic test. It is a therapeutic procedure to treat gallstones.
Explanation
Choice A reason:
Gallstone formation is not a concern after cholecystectomy since the gallbladder has been removed.
Choice B reason:
This statement is correct. Proper incision care is essential to prevent infection and complications at the surgical site after laparoscopic cholecystectomy.
Choice C reason:
Dietary recommendations for constipation are not directly related to laparoscopic cholecystectomy and may not address the client's concerns about complications.
Choice D reason:
While discussing potential complications of general anesthesia is essential for preoperative education, it may not be the primary concern for a client recovering from cholecystectomy.
Peritonitis
Explanation
Choice A reason:
Cholecystitis is inflammation of the gallbladder, which is not related to a ruptured appendix.
Choice B reason:
Gastritis is inflammation of the stomach lining, which may cause abdominal pain but is not related to a ruptured appendix.
Choice C reason:
Peritonitis is inflammation of the peritoneum, the membrane lining the abdominal cavity. It can occur as a complication of a ruptured appendix and presents with severe abdominal pain, tenderness, and fever.
Choice D reason:
Diverticulitis is inflammation of the diverticula (small pouches) in the colon and is not related to a ruptured appendix.
Explanation
Choice A reason:
Fever and diarrhea are not specific early signs of peritonitis.
Choice B reason:
Abdominal distension and flatulence may occur for various reasons after abdominal surgery, but they are not specific to peritonitis.
Choice C reason:
Nausea and vomiting can be caused by various post-operative factors and are not specific to peritonitis.
Choice D reason:
Sudden-onset severe abdominal pain and tenderness are classic early signs of peritonitis and indicate the need for immediate medical attention.
Explanation
Choice A reason:
A chest X-ray is not the primary diagnostic test for peritonitis.
Choice B reason:
An ECG is used to assess cardiac function and is not specific to peritonitis.
Choice C reason:
An abdominal ultrasound is commonly used to diagnose peritonitis and can help visualize inflammation or fluid in the peritoneal cavity.
Choice D reason:
A CBC may show elevated white blood cell count, which is an indication of infection, but it is not a confirmatory test for peritonitis.
Explanation
Choice A reason:
Hypertension is not a common side effect of IV antibiotic therapy.
Choice B reason:
Hypoglycemia is not a common side effect of IV antibiotic therapy.
Choice C reason:
An allergic reaction is a potential side effect of antibiotic therapy and can range from mild skin rash to life-threatening anaphylaxis.
Choice D reason:
Bradycardia is not a common side effect of IV antibiotic therapy.
Explanation
Choice A reason:
Paracentesis is not used to remove excess air from the peritoneal cavity.
Choice B reason:
Paracentesis is a procedure used to drain infected fluid or pus from the peritoneal cavity in cases of peritonitis.
Choice C reason:
Visualizing the abdominal organs using a scope is not the purpose of a paracentesis.
Choice D reason:
Monitoring intra-abdominal pressure is not the purpose of a paracentesis.
Explanation
Choice A reason:
Intravenous antibiotics are the standard treatment for spontaneous bacterial peritonitis (SBP) to treat the bacterial infection.
Choice B reason:
A high-protein diet is not the primary intervention for SBP.
Choice C reason:
Oral rehydration solutions are used for rehydration in cases of dehydration but are not the primary treatment for SBP.
Choice D reason:
Bowel rest may be indicated for other conditions but is not the primary intervention for SBP.
Explanation
Choice A reason:
Abdominal distension and decreased bowel sounds are classic signs of paralytic ileus, a common complication of peritonitis.
Choice B reason:
Gastroenteritis is inflammation of the gastrointestinal tract and may cause diarrhea and abdominal pain but is not related to the specific symptoms described.
Choice C reason:
Appendicitis is inflammation of the appendix and is not related to abdominal distension and decreased bowel sounds.
Choice D reason:
Constipation may cause abdominal distension, but decreased bowel sounds are not characteristic of constipation.
Explanation
Choice A reason:
Increased blood pressure is not characteristic of septic shock. Septic shock is associated with low blood pressure.
Choice B reason:
Bradycardia is not a typical sign of septic shock. Tachycardia is more common in septic shock.
Choice C reason:
Warm, flushed skin is not typical in septic shock. Septic shock is associated with cold, clammy skin.
Choice D reason:
Rapid, shallow breathing is a common early sign of septic shock and indicates the body's attempt to compensate for the decreased cardiac output.
Explanation
Choice A reason:
Recent travel to a tropical region is not a risk factor for peritonitis.
Choice B reason:
A history of asthma is not a risk factor for peritonitis.
Choice C reason:
Prior abdominal surgery is a significant risk factor for peritonitis because it can lead to perforation of the gastrointestinal tract and the spread of bacteria into the peritoneal cavity.
Choice D reason:
A vegetarian diet is not a risk factor for peritonitis.
Explanation
Choice A reason:
Having a history of allergies is not a risk factor for peritonitis.
Choice B reason:
Having a history of diabetes is not a risk factor for peritonitis.
Choice C reason:
Having a history of hypertension is not a risk factor for peritonitis.
Choice D reason:
A history of inflammatory bowel disease is a significant risk factor for peritonitis, especially if there are complications such as bowel perforation.
Explanation
Choice A reason:
Hypothyroidism is not a risk factor for peritonitis.
Choice B reason:
Chronic kidney disease can weaken the immune system and make the client more susceptible to infections such as peritonitis.
Choice C reason:
Migraine headaches are not a risk factor for peritonitis.
Choice D reason:
GERD is not a risk factor for peritonitis.
Explanation
Choice A reason:
Increased production of stomach acid is not directly related to peritonitis.
Choice B reason:
Cirrhosis is a condition where the liver is scarred and impaired in function. The liver plays a crucial role in immune function, and impaired liver function can lead to increased susceptibility to infections like peritonitis.
Choice C reason:
Gallbladder dysfunction is not directly related to peritonitis.
Choice D reason:
Chronic lung disease is not directly related to peritonitis.
Explanation
Choice A reason:
Antibiotics are used to treat infections, including peritonitis, and do not increase the risk of developing peritonitis.
Choice B reason:
Antacids are used to neutralize stomach acid and do not increase the risk of peritonitis.
Choice C reason:
NSAIDs can cause gastrointestinal irritation and increase the risk of ulcers and perforation, which can lead to peritonitis.
Choice D reason:
Oral contraceptives do not increase the risk of developing peritonitis.
Explanation
Choice A reason:
Peritoneal dialysis involves inserting a catheter into the peritoneal cavity, which can increase the risk of infection at the insertion site and lead to peritonitis.
Choice B reason:
High blood pressure is not directly related to an increased risk of peritonitis in clients undergoing peritoneal dialysis.
Choice C reason:
Elevated cholesterol levels are not directly related to an increased risk of peritonitis in clients undergoing peritoneal dialysis.
Choice D reason:
An allergic reaction to the dialysis solution is a possibility but is not the primary reason for an increased risk of peritonitis in clients undergoing peritoneal dialysis.
Explanation
Choice A reason:
Excessive alcohol consumption can contribute to the development of gastric ulcers but is not directly related to an increased risk of peritonitis in clients with perforated gastric ulcers.
Choice B reason:
A sedentary lifestyle is not directly related to an increased risk of peritonitis in clients with perforated gastric ulcers.
Choice C reason:
Gastric acid hypersecretion can contribute to the formation of gastric ulcers and increase the risk of perforation, which can lead to peritonitis.
Choice D reason:
Frequent use of antacids may alleviate symptoms of gastric ulcers but is not directly related to an increased risk of peritonitis in clients with perforated gastric ulcers.
Explanation
Choice A reason:
Slower metabolism is a normal age-related change but is not directly related to an increased susceptibility to peritonitis in older adults.
Choice B reason:
Older adults may have decreased immune function, which can increase their susceptibility to infections, including peritonitis.
Choice C reason:
Increased bone density is not directly related to an increased susceptibility to peritonitis in older adults.
Choice D reason:
Reduced gastrointestinal motility is a normal age-related change but is not directly related to an increased susceptibility to peritonitis in older adults.
Explanation
Choice A reason:
Chest pain is not a typical symptom of peritonitis, as the condition primarily affects the abdomen.
Choice B reason:
A severe headache is not a characteristic symptom of peritonitis.
Choice C reason:
Abdominal pain and tenderness are hallmark symptoms of peritonitis, resulting from inflammation of the peritoneum lining the abdominal cavity.
Choice D reason:
Shortness of breath is not a common symptom of peritonitis unless there is an associated respiratory complication.
Explanation
Choice A reason:
Hypothermia refers to abnormally low body temperature and is not associated with the clinical presentation of peritonitis.
Choice B reason:
Hypertension refers to high blood pressure and is not directly associated with the signs of peritonitis.
Choice C reason:
Hyperventilation involves rapid breathing but may not always be present in peritonitis.
Choice D reason:
The client's elevated temperature, rapid heart rate, and shallow breathing are indicative of a systemic inflammatory response, which is a characteristic feature of peritonitis.
Explanation
Choice A reason:
Rebound tenderness refers to increased pain upon release of pressure during palpation and is not related to the finding of a rigid, board-like abdomen.
Choice B reason:
Paralytic ileus refers to a condition in which the intestines stop functioning, causing a lack of bowel sounds and distension, but it is not directly related to the rigid abdomen finding.
Choice C reason:
Abdominal compartment syndrome may cause abdominal distension and increased intra-abdominal pressure, but it does not necessarily result in a rigid, board-like abdomen.
Choice D reason:
The finding of a rigid, board-like abdomen upon palpation is known as guarding, which is a protective response of the abdominal muscles in peritonitis to minimize movement and protect the inflamed peritoneum.
Explanation
Choice A reason:
Referred pain is pain that is felt in a different location from its source, and it is not directly associated with the sharp, sudden-onset pain described by the client.
Choice B reason:
Visceral pain arises from the internal organs and is often described as sharp and colicky. It worsens with movement and is a characteristic feature of peritonitis.
Choice C reason:
Neuropathic pain is caused by nerve damage and is not typically associated with peritonitis.
Choice D reason:
Radiating pain is pain that extends from its source to other areas, and it is not specifically described in the scenario.
Explanation
Choice A reason:
Hypovolemic shock involves severe blood loss or fluid depletion and may present with signs of hypotension and tachycardia but is not directly related to the findings described.
Choice B reason:
Paralytic ileus is a lack of bowel motility that causes abdominal distension and decreased bowel sounds, and it is a common complication of peritonitis.
Choice C reason:
Intestinal obstruction involves a blockage of the intestines and may present with abdominal distension and altered bowel sounds, but it is not directly related to peritonitis in this context.
Choice D reason:
Urinary retention involves the inability to empty the bladder fully and is not related to the findings described in the scenario.
Explanation
Choice A reason:
Anemia refers to a low red blood cell count or hemoglobin level and is not directly related to an elevated white blood cell count.
Choice B reason:
An elevated white blood cell count is a common indicator of infection, such as in peritonitis, as the body's immune response is heightened to combat the inflammation and infection.
Choice C reason:
Hypoalbuminemia refers to low albumin levels in the blood and is not directly related to an elevated white blood cell count.
Choice D reason:
Dehydration may result in elevated blood cell counts due to hemoconcentration, but it is not the primary cause of an elevated white blood cell count in peritonitis.
Explanation
Choice A reason:
Anxiety may lead to restlessness, but the assumption of a fetal position suggests a pain response, which is a common finding in peritonitis.
Choice B reason:
Fatigue may lead to restlessness, but it does not explain the assumption of a fetal position, which is a pain-coping mechanism.
Choice C reason:
The client assuming a fetal position and exhibiting restlessness are indicative of pain, which is a common symptom in peritonitis.
Choice D reason:
Respiratory distress is not directly related to the findings described in the scenario.
Explanation
Choice A reason:
Hypoglycemia refers to low blood sugar levels and is not directly related to the signs described in the scenario.
Choice B reason:
Hyperthyroidism involves an overactive thyroid gland and may cause symptoms such as weight loss and heat intolerance but is not associated with the signs described.
Choice C reason:
The client's high fever, chills, and profuse sweating are suggestive of sepsis, a severe systemic infection often resulting from peritonitis.
Choice D reason:
Renal failure involves impaired kidney function and may present with specific signs, but it is not directly related to the signs described in the scenario.
Explanation
Choice A reason:
An electrocardiogram (ECG) is used to assess the electrical activity of the heart and is not specific to diagnosing peritonitis.
Choice B reason:
A complete blood count (CBC) may reveal elevated white blood cell count and inflammatory markers, but it alone cannot confirm the diagnosis of peritonitis.
Choice C reason:
A chest X-ray may be performed to rule out other conditions, but it is not the primary diagnostic test for peritonitis.
Choice D reason:
An abdominal computed tomography (CT) scan is a valuable diagnostic tool for identifying signs of inflammation and infection in the peritoneal cavity, aiding in the confirmation of peritonitis.
Explanation
Choice A reason:
Inserting a catheter into the bladder to collect urine is not related to diagnostic paracentesis for peritonitis.
Choice B reason:
Diagnostic paracentesis involves removing fluid from the peritoneal cavity for analysis, helping to identify the presence of infection or inflammation in the peritoneum.
Choice C reason:
Injecting contrast dye into the bloodstream for imaging is not a part of the diagnostic paracentesis procedure.
Choice D reason:
Taking a tissue sample from the peritoneal lining is not the purpose of diagnostic paracentesis.
Explanation
Choice A reason:
An electrocardiogram (ECG) is used to assess the electrical activity of the heart, not the abdomen.
Choice B reason:
An abdominal X-ray provides a basic overview of the abdomen but may not offer detailed images of the peritoneal organs and structures.
Choice C reason:
Magnetic resonance imaging (MRI) can provide high-resolution images of the abdominal organs and structures, including the peritoneum, making it a valuable diagnostic tool for suspected peritonitis.
Choice D reason:
Ultrasonography can provide images of the abdominal organs, but it may not offer the level of detail provided by MRI in assessing peritonitis.
Explanation
Choice A reason:
Elevated serum creatinine levels are associated with kidney function and are not specific to peritonitis.
Choice B reason:
Elevated amylase and lipase levels are indicative of pancreatitis and are not directly related to peritonitis.
Choice C reason:
Elevated blood glucose levels may be indicative of diabetes or stress-related hyperglycemia but are not specific to peritonitis.
Choice D reason:
An elevated white blood cell count (WBC) is a common finding in peritonitis, indicating an inflammatory response and possible infection in the peritoneal cavity.
Explanation
Choice A reason:
Severe headache and neck stiffness are signs of meningitis and are not directly related to peritonitis.
Choice B reason:
Rapid and shallow breathing may occur with other respiratory conditions but is not a hallmark sign of peritonitis.
Choice C reason:
Abdominal rigidity and tenderness are hallmark signs of peritonitis and are caused by the inflammation of the peritoneum.
Choice D reason:
Hyperactive bowel sounds may occur with gastrointestinal disorders but are not specific to peritonitis.
Explanation
Choice A reason:
Ascites refers to the accumulation of fluid in the peritoneal cavity and does not necessarily cause bloating and distension of the abdomen in the context of peritonitis.
Choice B reason:
Intestinal obstruction can occur in peritonitis when inflammation or infection causes the intestines to become blocked, leading to bloating and distension of the abdomen.
Choice C reason:
Appendicitis is inflammation of the appendix and may cause pain, but it is not associated with generalized bloating and distension of the abdomen.
Choice D reason:
Pancreatitis is inflammation of the pancreas and may cause abdominal pain, but it is not associated with generalized bloating and distension of the abdomen.
Explanation
Choice A reason:
Assessing heart function requires specific cardiac imaging, not the imaging indicated for peritonitis.
Choice B reason:
Identifying bone fractures would require imaging specific to the bones, not the peritoneum.
Choice C reason:
Diagnostic imaging in peritonitis aims to detect inflammation and infection in the peritoneum, helping to confirm the diagnosis and guide treatment.
Choice D reason:
Evaluating lung health would involve pulmonary imaging, not the imaging indicated for peritonitis.
Explanation
Choice A reason:
Removal of fluid from the pleural cavity would be a thoracentesis, not a paracentesis.
Choice B reason:
Removal of fluid from the pericardial sac would be a pericardiocentesis, not a paracentesis.
Choice C reason:
A diagnostic paracentesis involves removing fluid from the peritoneal cavity to analyze for signs of infection and inflammation, which is important in diagnosing peritonitis.
Choice D reason:
Removal of fluid from the spinal canal would be a lumbar puncture, not a paracentesis.
Explanation
Choice A reason:
Administering pain medication is important for the client's comfort, but it is not the highest priority in the management of peritonitis. Addressing the underlying infection with antibiotics takes precedence.
Choice B reason:
Monitoring vital signs is essential for assessing the client's condition, but initiating antibiotic therapy is more critical to address the underlying infection.
Choice C reason:
Initiating intravenous (IV) antibiotic therapy is the highest priority in the management of peritonitis. Prompt administration of antibiotics is essential to treat the bacterial infection and prevent its spread.
Choice D reason:
Encouraging deep breathing and coughing exercises is beneficial for preventing respiratory complications, but it is not the highest priority compared to addressing the infection with antibiotics.
Explanation
Choice A reason:
Assessing for peripheral edema is important for clients with various conditions, but it is not directly related to the potential complications of peritonitis.
Choice B reason:
Monitoring blood glucose levels regularly is essential in clients with peritonitis, as hyperglycemia can be a complication of the inflammatory response and stress associated with the condition.
Choice C reason:
Encouraging fluid intake is essential for clients with peritonitis, but the specific recommendation of 3 liters per day is not universally applicable and may vary based on individual client needs and medical status.
Choice D reason:
Implementing fall precautions is important for clients at risk of falls, but it is not directly related to potential complications of peritonitis.
Explanation
Choice A reason:
Lying flat in bed may provide some comfort for the client and is not likely to exacerbate the abdominal pain associated with peritonitis.
Choice B reason:
Using a heating pad on the abdomen may provide some relief for the client and is not likely to exacerbate the abdominal pain associated with peritonitis.
Choice C reason:
Deep breathing and coughing exercises may worsen the client's abdominal pain due to the stretching and movement of the peritoneum during these activities.
Choice D reason:
Administering prescribed analgesics is essential for managing the client's pain and providing comfort during the treatment of peritonitis.
Explanation
Choice A reason:
Changing the IV site every 24 hours is not necessary for IV antibiotic administration unless there is an indication of infiltration or infection at the site.
Choice B reason:
Administering the antibiotics using an infusion pump is essential to ensure accurate and controlled delivery of the medication, particularly when the client's condition requires a precise dosing schedule.
Choice C reason:
Discontinuing the antibiotics after 48 hours of improvement may lead to a recurrence of the infection. Clients with peritonitis often require a full course of antibiotic therapy to ensure complete eradication of the infection.
Choice D reason:
Administering the antibiotics through a peripheral IV catheter may not be suitable for the client's condition, as peritonitis may necessitate the use of a central line for administration of IV medications.
Explanation
Choice A reason:
Continuous gastric suction is not primarily intended to prevent aspiration pneumonia, although it may indirectly help reduce the risk of aspiration in some cases.
Choice B reason:
Reducing intra-abdominal pressure is not the primary purpose of continuous gastric suction, although it may have some effect on the overall abdominal pressure.
Choice C reason:
Continuous gastric suction is not primarily intended to manage pain and discomfort in the client with peritonitis, although it may help alleviate some symptoms.
Choice D reason:
Promoting bowel rest is the main purpose of continuous gastric suction in the management of peritonitis. By reducing the workload of the gastrointestinal tract, the inflamed peritoneum can heal and recover more effectively.
Explanation
Choice A reason:
Correcting electrolyte imbalances is important in fluid resuscitation, but the primary goal is to prevent circulatory collapse and restore hemodynamic stability.
Choice B reason:
The primary goal of fluid resuscitation in peritonitis is to prevent circulatory collapse and maintain adequate blood pressure and perfusion to vital organs.
Choice C reason:
Maintaining adequate urine output is one of the indicators of effective fluid resuscitation, but it is not the primary goal in this context.
Choice D reason:
Restoring fluid balance is a goal of fluid resuscitation, but the primary focus is on preventing circulatory collapse and ensuring adequate tissue perfusion.
Explanation
Choice A reason:
Bradycardia is not a common side effect of opioid use in clients with peritonitis.
Choice B reason:
Hypertension is not a common side effect of opioid use in clients with peritonitis.
Choice C reason:
Respiratory depression is a potential side effect of opioid use and is a significant concern in clients with peritonitis, as they may already have compromised respiratory function.
Choice D reason:
Diarrhea is not
a common side effect of opioid use in clients with peritonitis.
Explanation
Choice A reason:
Maintaining a low-fiber diet is not a standard recommendation for clients recovering from peritonitis.
Choice B reason:
Avoiding physical activity for two weeks is not necessary for all clients recovering from peritonitis, and individualized recommendations should be provided based on the client's condition and physician's instructions.
Choice C reason:
Taking prescribed antibiotics as directed is essential for clients recovering from peritonitis to complete the course of treatment and ensure the infection is fully eradicated.
Choice D reason:
Using a heating pad for abdominal pain relief may not be recommended for all clients recovering from peritonitis, as it may exacerbate inflammation or lead to complications. Individualized pain management strategies should be discussed with the healthcare provider.
Explanation
Choice A reason:
Administering pain medication is important for the client's comfort, but it is not the highest priority in managing sepsis, a life-threatening complication of peritonitis. Addressing the underlying infection with antibiotics takes precedence.
Choice B reason:
Monitoring vital signs is essential for assessing the client's condition, but initiating broad-spectrum antibiotic therapy is more critical in managing sepsis.
Choice C reason:
Initiating broad-spectrum antibiotic therapy is the highest priority in managing sepsis. Prompt administration of antibiotics is crucial to treat the bacterial infection and prevent its spread.
Choice D reason:
Providing deep breathing exercises is important for preventing respiratory complications, but it is not the highest priority compared to addressing sepsis with antibiotics.
Explanation
Choice A reason:
Increased urine output is not a concerning finding in this context and may indicate adequate fluid resuscitation.
Choice B reason:
Abdominal distension and firmness are concerning findings and may indicate the development of abdominal compartment syndrome, a serious complication of peritonitis.
Choice C reason:
Normal respiratory rate is a positive finding, but it does not directly relate to the development of abdominal compartment syndrome.
Choice D reason:
Mild incisional pain is expected after surgery, but it does not indicate the development of abdominal compartment syndrome.
Explanation
Choice A reason:
Monitoring blood glucose levels is important for clients with various conditions, but it is not directly related to the management of acute kidney injury (AKI) in peritonitis.
Choice B reason:
Administering pain medication is essential for managing the client's pain and providing comfort during treatment, but it is not directly related to the management of acute kidney injury.
Choice C reason:
Encouraging fluid intake is important for clients with peritonitis, but the specific recommendation of 3 liters per day is not universally applicable and may vary based on individual client needs and medical status.
Choice D reason:
Maintaining fluid and electrolyte balance is crucial in managing acute kidney injury in peritonitis. The nurse should closely monitor the client's fluid intake, output, and electrolyte levels and collaborate with the healthcare team to adjust the fluid therapy as needed.
Explanation
Choice A reason:
Abdominal compartment syndrome may present with abdominal distension and firmness but is not directly associated with hypotension and tachycardia.
Choice B reason:
Respiratory distress syndrome may manifest with respiratory symptoms such as dyspnea and decreased oxygen saturation but is not directly associated with hypotension and tachycardia.
Choice C reason:
Sepsis is a systemic inflammatory response to infection and can cause hypotension and tachycardia as part of its clinical presentation.
Choice D reason:
Gastrointestinal bleeding may present with symptoms such as melena or hematemesis but is not directly associated with hypotension and tachycardia.
Explanation
Choice A reason:
Preventing aspiration pneumonia is one of the benefits of an NG tube, but the primary purpose in peritonitis is to relieve abdominal distension caused by fluid and gas accumulation.
Choice B reason:
Relieving abdominal distension is the primary purpose of an NG tube in clients with peritonitis, as it helps remove fluid and gas from the stomach and intestines, reducing pressure on the peritoneum.
Choice C reason:
Monitoring gastric pH levels may be done with an NG tube in certain situations, but it is not the primary purpose in the context of peritonitis.
Choice D reason:
Administering enteral nutrition may be a secondary purpose of an NG tube in some cases, but it is not the primary goal in clients with peritonitis.
Explanation
Choice A reason:
Administering oxygen as prescribed is the priority intervention in managing acute respiratory distress to improve oxygenation and support respiratory function.
Choice B reason:
Elevating the head of the bed is helpful for promoting lung expansion, but it is not the priority intervention in managing acute respiratory distress.
Choice C reason:
Monitoring blood pressure regularly is essential in assessing the client's overall condition, but it does not directly address the respiratory distress.
Choice D reason:
Administering bronchodilator medication is not the priority intervention in managing acute respiratory distress unless there is a specific indication for its use.
A client with peritonitis is at risk of developing hypovolemic shock. Which assessment finding should the nurse be most concerned about?
Explanation
Choice A reason:
Bradycardia is not a concerning finding in this context and may indicate a vagal response or be a side effect of certain medications.
Choice B reason:
Hypotension is a concerning finding and may indicate hypovolemic shock, a potentially life-threatening complication of peritonitis.
Choice C reason:
Hyperactive bowel sounds are not a concerning finding in this context and may be a sign of gastrointestinal motility.
Choice D reason:
Increased urine output may be a positive finding but does not directly relate to the development of hypovolemic shock.
A client with peritonitis develops a wound infection at the surgical site. Which nursing intervention is essential in preventing the spread of infection?
Explanation
Choice A reason:
Administering oral antibiotics may be necessary for treating the wound infection, but it does not directly prevent the spread of infection.
Choice B reason:
Performing sterile dressing changes is essential in preventing the spread of infection and promoting wound healing.
Choice C reason:
Limiting visitors to the client's room may help reduce the risk of introducing new pathogens, but it is not the primary intervention for preventing wound infection.
Choice D reason:
Providing pain medication as needed is important for the client's comfort but does not directly prevent the spread of infection.
Exams on Digestive System Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Introduction To Digestive System Disorders
- The digestive system plays a crucial role in breaking down and absorbing nutrients from the food we consume, ensuring proper nourishment and overall health.
- Digestive system disorders encompass a range of conditions that affect the normal functioning of various organs within the gastrointestinal tract.
- Nurses play a vital role in identifying, managing, and providing education about digestive system disorders to promote optimal patient outcomes.
- Understanding the anatomy and physiology of the digestive system is essential for nurses to assess and address potential disorders effectively.
- This overview will explore common digestive system disorders encountered in nursing practice and highlight key assessment, intervention, and patient education considerations.
Peptic Ulcer Disease
Introduction to Peptic Ulcer Disease
- Peptic ulcer disease (PUD) is a condition that involves the formation of open sores or ulcers in the lining of the stomach or the duodenum, which is the first part of the small intestine.
- PUD can cause abdominal pain, bleeding, and other complications.
- The most common causes of PUD are infection with Helicobacter pylori (H. pylori) bacteria and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
- Peptic ulcers can affect the stomach (gastric ulcers) or the duodenum (duodenal ulcers). Less commonly, they can also occur in the lower esophagus or beyond the duodenum.
- Peptic ulcers are common, affecting about 10% of people in their lifetime.
- Peptic ulcers can cause symptoms such as burning stomach pain, nausea, vomiting, weight loss, and anemia.
- Some people may have no symptoms or only mild discomfort.
- Peptic ulcers can lead to serious complications such as bleeding, perforation, infection, and obstruction. These complications may require emergency treatment or surgery.
- Peptic ulcers can be diagnosed by tests such as blood tests, breath tests, stool tests, endoscopy, upper gastrointestinal series, and biopsy.
- Peptic ulcers can be treated by medications such as antibiotics, proton pump inhibitors, H2 blockers, and antacids. These medications aim to eradicate H. pylori infection, reduce acid production, and promote healing of ulcers.
Etiology and Risk Factors
- The main causes of peptic ulcers are infection with H. pylori bacteria and long-term use of NSAIDs.
i.H. pylori is a spiral-shaped bacterium that colonizes the stomach and duodenum. It can damage the mucosa by producing enzymes, toxins, and inflammatory substances. It can also interfere with the production of protective mucus and bicarbonate in the stomach. H. pylori infection is very common, affecting about half of the world's population. It is more prevalent in developing countries, where it is usually acquired in childhood. It can be transmitted from person to person through oral-oral or fecal-oral routes, or through contaminated food or water.
ii.NSAIDs are a group of drugs that are used to relieve pain, inflammation, and fever. They include aspirin, ibuprofen, naproxen, celecoxib, and others. NSAIDs can cause peptic ulcers by inhibiting an enzyme called cyclooxygenase (COX), which is involved in the synthesis of prostaglandins. Prostaglandins are substances that protect the mucosa from acid and injury. NSAIDs are widely used for various conditions such as arthritis, headache, menstrual cramps, and sports injuries. They can increase the risk of peptic ulcers by 2 to 4 times, especially if taken at high doses, for long periods, or in combination with other drugs such as steroids or anticoagulants.
- Other risk factors for peptic ulcers include:
- Smoking: Smoking can increase acid secretion, reduce blood flow to the mucosa, impair healing of ulcers, and reduce the effectiveness of medications.
- Alcohol: Alcohol can irritate the mucosa, increase acid production, and interfere with the action of prostaglandins.
- Stress: Stress can stimulate acid secretion and impair mucosal defense mechanisms. However, stress alone does not cause peptic ulcers unless there is also H. pylori infection or NSAID use.
- Spicy foods: Spicy foods do not cause peptic ulcers, but they may worsen symptoms in some people who have existing ulcers.
- Genetic factors: Some people may have a genetic predisposition to peptic ulcers due to variations in genes that affect acid secretion, mucosal protection, or immune response to H. pylori.
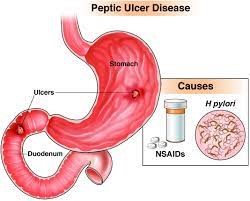
Clinical Manifestation and Symptoms
- The most common symptom of peptic ulcer disease is burning stomach pain that occurs between meals or at night. The pain may last from minutes to hours and may be relieved by eating food or taking antacids. The pain may vary in intensity, frequency, and location depending on the type and location of the ulcer.
- Gastric ulcers tend to cause pain shortly after eating, while duodenal ulcers tend to cause pain 2 to 5 hours after eating.
- Gastric ulcers may also cause loss of appetite, weight loss, and vomiting, while duodenal ulcers may cause increased appetite, weight gain, and bloating.
- Some people with peptic ulcers may have no symptoms or only mild discomfort. This is more common in older adults, who may have fewer pain receptors or more tolerance to pain. However, asymptomatic ulcers can still lead to complications such as bleeding or perforation.
- Other symptoms of peptic ulcer disease may include:
- Nausea and vomiting: Nausea and vomiting may occur due to irritation of the stomach or duodenum by acid or ulcer. Vomiting may also indicate a complication such as bleeding or obstruction. Vomiting blood or material that looks like coffee grounds may indicate a bleeding ulcer, while vomiting undigested food hours after eating may indicate an obstructed ulcer.
- Bleeding: Bleeding is the most common complication of peptic ulcer disease, occurring in about 15% of cases. Bleeding can be mild or severe, acute or chronic. Bleeding can cause hematemesis (vomiting blood), melena (black, tarry stools), or hematochezia (bright red blood in stools). Bleeding can also cause anemia, which can manifest as weakness, fatigue, dizziness, shortness of breath, and pale skin.
- Perforation: Perforation is a life-threatening complication of peptic ulcer disease, occurring in about 5% of cases. Perforation occurs when the ulcer erodes through the entire wall of the stomach or duodenum, creating a hole that allows the contents of the digestive tract to spill into the abdominal cavity. Perforation can cause sudden and severe abdominal pain that radiates to the back or shoulder, fever, nausea, vomiting, shock, and peritonitis (inflammation of the lining of the abdominal cavity).
- Obstruction: Obstruction is a rare complication of peptic ulcer disease, occurring in less than 1% of cases. Obstruction occurs when the ulcer narrows or blocks the passage of food through the stomach or duodenum. Obstruction can cause persistent vomiting, abdominal distension, dehydration, weight loss, and malnutrition.
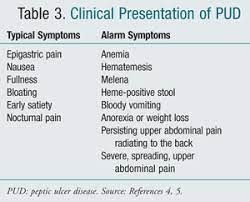
Diagnostic Evaluation
- The diagnosis of peptic ulcer disease is based on the history, physical examination, and diagnostic tests.
- The history should include information about the onset, duration, frequency, location, and characteristics of the pain; any factors that worsen or relieve the pain; any associated symptoms such as nausea, vomiting, bleeding, and weight loss; any history of H. pylori infection or NSAID use; any family history of peptic ulcers; and any previous treatments or medications for peptic ulcers.
- The physical examination should include inspection and palpation of the abdomen for signs of tenderness, distension, masses, or organomegaly; auscultation for bowel sounds; percussion for signs of fluid or air; and rectal examination for signs of bleeding or anemia.
- The diagnostic tests for peptic ulcer disease include:
- Blood tests: Blood tests can check for anemia due to bleeding; infection by H. pylori using serology (antibody test), antigen test (stool test), or urea breath test; inflammation using erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP); and liver and kidney function using liver enzymes and creatinine.
- Breath test: To check for H. pylori infection by measuring the amount of carbon dioxide in the breath after swallowing a urea solution.
- Stool test: To check for H. pylori infection by detecting antigens or DNA in the stool sample.
- Endoscopy: Endoscopy is the most accurate test for peptic ulcer disease. It involves inserting a thin flexible tube with a camera and a light source through the mouth into the stomach and duodenum. Endoscopy can visualize the ulcers and their size, location, shape and take biopsies for histological examination and culture.
- Upper gastrointestinal series: To take X-rays of the upper digestive tract after drinking a contrast agent that coats the lining.

Management and Treatment of Peptic Ulcer Disease
- The main goals of treatment are to heal the ulcers, prevent complications, and eradicate H. pylori infection if present.
- The treatment options include:
- Medication: The most commonly used drugs are:
- proton pump inhibitors (PPIs) such as omeprazole, lansoprazole, rabeprazole, esomeprazole, and pantoprazole. These drugs reduce the production of stomach acid and promote ulcer healing.
- In addition, antibiotics such as amoxicillin, clarithromycin, metronidazole, tinidazole, tetracycline, and levofloxacin are given to eradicate H. pylori infection.
- Other drugs that may be used are antacids, histamine receptor blockers, sucralfate, and misoprostol.
- Surgery: Surgery is reserved for cases with severe complications such as bleeding, perforation, obstruction, or cancer.
- The surgical procedures may involve removing part of the stomach (gastrectomy), cutting the nerve that stimulates acid secretion (vagotomy), or creating a new connection between the stomach and the intestine (gastrojejunostomy).
- Lifestyle changes: Patients are advised to avoid smoking, alcohol, spicy foods, and NSAIDs that can worsen PUD.
- They are also encouraged to eat small and frequent meals, reduce stress, and seek psychological support if needed.

Complications of Peptic Ulcer Disease
- PUD can lead to serious complications if left untreated or poorly managed.
- These include:
- Bleeding: Ulcers can erode blood vessels and cause hemorrhage that can manifest as vomiting blood (hematemesis), passing black or tarry stools (melena), or having low blood pressure (hypotension) and shock.
- Perforation: Ulcers can penetrate through the wall of the stomach or duodenum and create a hole that allows stomach contents to leak into the abdominal cavity. This can cause severe pain, fever, abdominal rigidity, and peritonitis (inflammation of the lining of the abdomen).
- Obstruction: Ulcers can cause swelling, scarring, or spasm that narrows the opening of the stomach or duodenum and prevents food from passing through. This can result in nausea, vomiting, bloating, weight loss, and malnutrition.
- Cancer: Chronic inflammation and damage to the lining of the stomach or duodenum can increase the risk of developing gastric or duodenal cancer.
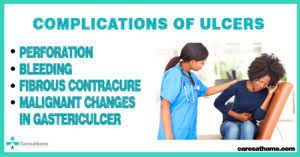
Nursing Consideration and Intervention
- Nurses play a vital role in caring for patients with PUD by providing education, monitoring, and support. Some of the nursing interventions are:
- Assessing the patient's pain level, location, frequency, duration, and aggravating or relieving factors.
- Administering prescribed medications as ordered and observing for their effectiveness and side effects.
- Checking the patient's vital signs, hemoglobin level, stool color and consistency, and signs of bleeding or perforation.
- Encouraging the patient to adhere to the treatment regimen and follow up with regular endoscopy.
- Teaching the patient about PUD causes, symptoms, complications, prevention strategies, and lifestyle modifications.
- Providing emotional support and coping strategies to help the patient deal with stress and anxiety.
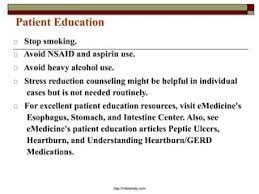
Preventive Strategies
- PUD can be prevented by avoiding or minimizing the risk factors that contribute to its development. Some of the preventive measures are:
- Testing and treating H. pylori infection if present.
- Limiting or avoiding the use of NSAIDs and taking them with food or antacids if necessary.
- Quitting smoking and reducing alcohol consumption.
- Eating a balanced diet that is rich in vitamin C and low in spicy foods.
- Practicing good hygiene and washing hands frequently.
- Managing stress and seeking professional help if needed.
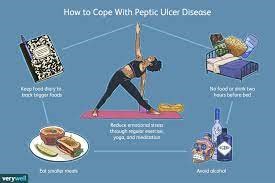
Summary
- PUD is a common digestive disorder that affects millions of people worldwide.
- It is characterized by ulcers in the stomach or duodenum that can cause pain, bleeding, infection, and obstruction.
- PUD is mainly caused by H. pylori infection and NSAID use.
- The diagnosis is made by history, physical examination, and laboratory tests.
- The treatment involves medication, surgery, and lifestyle changes.
- The complications of PUD include bleeding, perforation, obstruction, and cancer.
- The nursing care of PUD patients focuses on education, monitoring, and support.
- PUD can be prevented by avoiding or minimizing the risk factors and following preventive strategies.
Conclusion
- In conclusion, peptic ulcer disease (PUD) is a common and potentially serious gastrointestinal condition characterized by the formation of ulcers in the lining of the stomach, duodenum, or esophagus.
- This condition can cause various symptoms, ranging from mild discomfort to severe complications, including bleeding and perforation.
- Throughout this study, we have explored the etiology, risk factors, clinical manifestations, diagnosis, and management of peptic ulcer disease.
- One of the primary causes of PUD is the infection with Helicobacter pylori bacteria, which leads to chronic inflammation and ulcer formation.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) and lifestyle factors like smoking and excessive alcohol consumption also contribute significantly to the development of peptic ulcers.
- The clinical presentation of PUD can vary, with common symptoms including burning or gnawing abdominal pain, bloating, nausea, and vomiting.
- In some cases, patients may experience bleeding, leading to dark, tarry stools (melena) or vomiting of blood (hematemesis).
- Recognizing these symptoms early and seeking medical attention promptly is crucial to prevent complications and initiate appropriate treatment.
- Diagnosing peptic ulcer disease involves a combination of patient history, physical examination, and diagnostic tests.
- Endoscopy is a key procedure that allows direct visualization of ulcers and the collection of tissue samples for H. pylori testing. Other tests, such as stool tests, blood tests, and breath tests, can also help identify H. pylori infection.
- The management of peptic ulcer disease aims to alleviate symptoms, promote ulcer healing, eradicate H. pylori infection if present, and prevent complications.
- Treatment may involve a combination of medications, including proton pump inhibitors (PPIs), H2 receptor antagonists, and antibiotics for H. pylori eradication. In cases where NSAID use is necessary, gastroprotective agents may be prescribed to reduce the risk of ulcers.
- Additionally, patient education and lifestyle modifications, such as avoiding smoking, alcohol, and NSAID overuse, can play a vital role in preventing ulcer recurrence and promoting overall gastrointestinal health.
- Preventing complications of PUD, such as bleeding or perforation, requires vigilance in monitoring patients' symptoms and response to treatment.
- In severe cases of bleeding ulcers, endoscopic interventions or surgery may be necessary to stop the bleeding and repair the ulcer.
- In conclusion, peptic ulcer disease remains a prevalent gastrointestinal disorder with significant implications for patient health and quality of life.
- Early diagnosis, appropriate treatment, and lifestyle modifications are crucial in managing the condition effectively.
- Through ongoing research and continued efforts to raise awareness about risk factors and preventive measures, we can strive to reduce the incidence and impact of peptic ulcer disease in the population.
- Timely intervention and comprehensive patient care are essential in achieving successful outcomes and improving the overall well-being of individuals affected by PUD.
Cholecystitis
Introduction to Cholecystitis
- Cholecystitis is the inflammation of the gallbladder, a small pear-shaped organ that stores and secretes bile into the duodenum to aid in the digestion of fats.
- Bile is a fluid produced by the liver that contains bile salts, acids, cholesterol, phospholipids, proteins, bilirubin, and other compounds.
- Cholecystitis can be acute or chronic, depending on the duration and severity of the inflammation.
- It is usually caused by biliary stasis, either due to gallstones obstructing the cystic duct (calculous cholecystitis) or impaired gallbladder emptying in the absence of gallstones (acalculous cholecystitis).
- The clinical manifestations of cholecystitis primarily involve abdominal pain in the right upper quadrant, often accompanied by nausea, vomiting, fever, and other related symptoms.
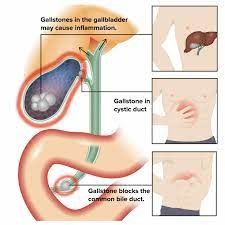
Acute vs Chronic Cholecystitis
A. Acute cholecystitis is a sudden onset of gallbladder inflammation, usually caused by a gallstone blocking the cystic duct, which is the tube that connects the gallbladder to the common bile duct.
- This leads to bile accumulation and increased pressure in the gallbladder, resulting in ischemia, edema and infection of the gallbladder wall.
- Acute cholecystitis can also occur without gallstones, in a condition called acalculous cholecystitis, which is more common in critically ill patients who have impaired gallbladder emptying due to factors such as dehydration, fasting, trauma, surgery or sepsis.
- Acute cholecystitis is a medical emergency that requires prompt diagnosis and treatment to prevent complications such as gangrene, perforation, abscess or peritonitis.
B. Chronic cholecystitis is a long-standing inflammation of the gallbladder, usually due to repeated episodes of acute cholecystitis or chronic irritation from gallstones.
- Chronic cholecystitis causes thickening and fibrosis of the gallbladder wall, reducing its function and increasing the risk of complications such as cholangitis (inflammation of the bile ducts), pancreatitis (inflammation of the pancreas) or gallbladder cancer.
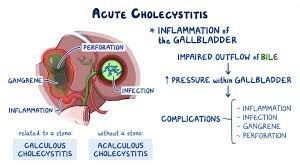
Etiology and Risk Factors
- The most common cause of cholecystitis is cholelithiasis, or gallstones, which are solid deposits of cholesterol, bilirubin or calcium salts that form in the gallbladder or bile ducts.
- Gallstones can vary in size, shape and number, and can be asymptomatic or symptomatic depending on their location and movement.
- Gallstones are more likely to form when there is an imbalance between the components of bile, such as excess cholesterol, decreased bile salts or stasis of bile flow.
- Risk factors for gallstone formation include:
- Female gender - women are more prone to develop gallstones than men due to hormonal factors such as estrogen and progesterone
- Age over 40 - older age increases the risk of gallstone formation due to decreased bile production and secretion
- Obesity - excess body weight increases the cholesterol content of bile and reduces the gallbladder motility
- Rapid weight loss - losing weight quickly can cause increased cholesterol secretion and decreased bile salt concentration in bile
- High-fat diet - consuming foods high in fat can stimulate excessive bile secretion and reduce its solubility
- Diabetes mellitus - diabetes can impair the function of the sphincter of Oddi and cause increased triglyceride levels in bile
- Pregnancy - pregnancy can increase the estrogen levels and decrease the gallbladder contractility
- Oral contraceptive use - oral contraceptives can increase the estrogen levels and decrease the bile salt levels in bile
- Family history - having a family member with gallstones can increase the genetic predisposition to develop gallstones
- Ethnicity (Native American, Hispanic) - some ethnic groups have higher rates of gallstone formation due to genetic factors that affect bile composition or metabolism
Other causes of cholecystitis include:
- Bacterial infection (e.g., E. coli, Klebsiella, Enterococcus) - bacteria can enter the biliary system through the bloodstream or through ascending infection from the duodenum; bacteria can cause inflammation and infection of the gallbladder wall or form biofilms on gallstones
- Parasitic infection (e.g., Ascaris lumbricoides) - parasites can migrate from the intestine to the biliary system and cause obstruction or inflammation of the bile ducts or gallbladder
- Trauma or surgery - injury or manipulation of the biliary system can cause damage or inflammation of the gallbladder or bile ducts
- Tumors - benign or malignant tumors can arise from or compress the biliary system and cause obstruction or inflammation of the bile flow
- Congenital anomalies - structural defects or malformations of the biliary system can impair the normal function or development of the gallbladder or bile ducts
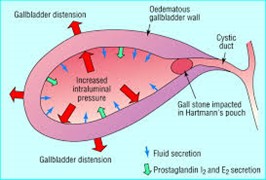
Clinical Manifestations and Symptoms
- The main symptom of cholecystitis is right upper quadrant (RUQ) abdominal pain that radiates to the right shoulder or scapula.
- The pain is typically sudden, severe and constant, and may be triggered by a fatty meal. The pain may last for several hours or days, and may be accompanied by nausea, vomiting, anorexia or fever.
- The pain may also be referred to the epigastric region or the right lower chest.
- Other signs and symptoms of cholecystitis include:
- Jaundice (yellowing of the skin and eyes) due to obstruction of bile flow
- Dark urine and pale stools due to reduced bilirubin excretion
- Pruritus (itching) due to the accumulation of bile salts in the skin
- Murphy's sign (pain on inspiration when palpating the RUQ) due to irritation of the diaphragm by the inflamed gallbladder
- Boas' sign (pain in the right subscapular area) due to irritation of the phrenic nerve by the inflamed gallbladder
- Courvoisier's sign (palpable non-tender gallbladder) due to distension of the gallbladder by a tumor in the head of the pancreas
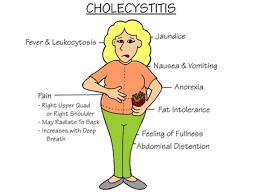
Diagnostic Evaluation
- The diagnosis of cholecystitis is based on clinical history, physical examination and laboratory and imaging tests.
i. Laboratory tests include:
- Complete blood count (CBC) - may show leukocytosis (increased white blood cells) due to infection or inflammation
- Liver function tests (LFTs) - may show elevated serum bilirubin, alkaline phosphatase, aspartate aminotransferase (AST) and alanine aminotransferase (ALT) due to impaired bile flow or liver damage
- Serum amylase and lipase - may show elevated levels due to pancreatitis
- Blood cultures - may show bacterial growth in cases of sepsis
- Urinalysis - may show bilirubinuria (bilirubin in urine) due to increased serum bilirubin
ii. Imaging tests include:
- Abdominal ultrasound - the first-line imaging test that can show gallstones, gallbladder wall thickening, pericholecystic fluid, gallbladder distension or sludge
- Abdominal computed tomography (CT) scan - can provide more detailed images of the gallbladder and surrounding structures, and can detect complications such as abscess, perforation or fistula
- Hepatobiliary iminodiacetic acid (HIDA) scan - a nuclear medicine test that can assess the function and patency of the biliary system by injecting a radioactive tracer that is taken up by the liver and excreted into the bile; a positive HIDA scan shows non-visualization of the gallbladder within 4 hours, indicating obstruction of the cystic duct
- Magnetic resonance cholangiopancreatography (MRCP) - a non-invasive test that can provide high-resolution images of the biliary and pancreatic ducts using magnetic resonance imaging (MRI)
- Endoscopic retrograde cholangiopancreatography (ERCP) - an invasive test that can visualize and treat the biliary and pancreatic ducts by inserting an endoscope through the mouth, esophagus, stomach and duodenum, and injecting contrast dye into the ampulla of Vater; ERCP can also be used
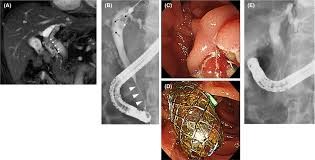
Management and Treatment
- The management and treatment of cholecystitis depend on the type, severity and complications of the condition.
- Medical management includes:
- Pain relief - using analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids
- Antibiotics - to treat or prevent infection, especially in cases of acute cholecystitis or sepsis
- Fluid and electrolyte replacement - to correct dehydration, acid-base imbalance or electrolyte abnormalities
- Nutritional support - using a low-fat diet or parenteral nutrition to reduce gallbladder stimulation and bile secretion
- Surgical management includes:
- Cholecystectomy - the surgical removal of the gallbladder, which is the definitive treatment for cholecystitis; it can be performed as an open surgery or a laparoscopic surgery, depending on the patient's condition and preference
- Cholecystostomy - the surgical drainage of the gallbladder through a tube inserted into the abdominal wall; it can be performed as a temporary measure to decompress the gallbladder and relieve symptoms until definitive surgery can be done
- Choledocholithotomy - the surgical removal of stones from the common bile duct; it can be performed as an open surgery or a laparoscopic surgery, depending on the location and size of the stones

Nursing Interventions and Patient Education
- Nursing interventions for cholecystitis include:
- Monitoring vital signs, pain level, fluid intake, and output, laboratory results, and signs of complications
- Administering medications as prescribed, such as analgesics, antibiotics, antiemetics, or antipruritics
- Providing comfort measures, such as positioning, heat application, relaxation techniques, or distraction
- Maintaining intravenous access and administering fluids and electrolytes as ordered
- Providing nutritional support, such as encouraging oral intake of clear liquids or low-fat foods, or administering parenteral nutrition as ordered
- Preparing the patient for surgery if indicated, such as obtaining informed consent, performing preoperative assessment, providing preoperative teaching and administering preoperative medications
- Providing postoperative care if surgery is done, such as monitoring vital signs, pain level, wound healing, drainage output, bowel sounds, and signs of complications
- Educating the patient about cholecystitis and its management, such as:
- explaining the causes, symptoms, diagnosis, treatment, and possible complications of cholecystitis
- teaching the patient how to prevent recurrence or complications by following a low-fat diet, avoiding alcohol and smoking, maintaining a healthy weight, and adhering to a medication regimen
- instructing the patient how to care for themselves at home after surgery by following wound care instructions, reporting signs of infection or bleeding, resuming activity gradually, and attending follow-up appointments

Summary
- Cholecystitis is the inflammation of the gallbladder, which can be acute or chronic.
- It is usually caused by biliary stasis, either due to gallstones obstructing the cystic duct (calculous cholecystitis) or impaired gallbladder emptying in the absence of gallstones (acalculous cholecystitis).
- Cholecystitis can lead to complications such as empyema, gangrene, perforation, and sepsis if left untreated.
- The main clinical manifestations are right upper quadrant pain, fever, leukocytosis, and palpable gallbladder. The diagnosis is based on clinical findings, laboratory tests, and imaging studies such as ultrasound or cholescintigraphy.
- The treatment options include pharmacologic therapy with antibiotics and analgesics and surgical management with cholecystectomy or cholecystostomy.
Conclusion
- In conclusion, cholecystitis is a condition that involves inflammation of the gallbladder, which can be acute or chronic.
- The most common cause of cholecystitis is the presence of gallstones, although other factors such as infections, trauma, and tumors can also contribute to its development.
- It is crucial to differentiate between acute and chronic cholecystitis as their treatment and management may vary significantly.
- The clinical manifestations of cholecystitis primarily involve abdominal pain in the right upper quadrant, often accompanied by nausea, vomiting, fever, and other related symptoms.
- Proper diagnostic evaluation, including laboratory tests and imaging studies, plays a crucial role in confirming the diagnosis and determining the appropriate course of action.
- The management of cholecystitis can be medical or surgical, depending on the severity and complications of the condition.
- Medical management involves pain relief, antibiotics, and supportive measures such as fluid and electrolyte replacement.
- However, the definitive treatment for cholecystitis is usually surgical removal of the gallbladder through cholecystectomy.
- Nursing interventions are essential in providing comprehensive care to patients with cholecystitis. Monitoring vital signs, administering medications, and offering comfort measures are vital aspects of nursing care.
- Additionally, patient education is crucial in helping patients understand the condition, its management, and the importance of lifestyle modifications to prevent recurrence.
- Early diagnosis and appropriate management of cholecystitis are critical to preventing complications and improving patient outcomes.
- With prompt medical attention, surgical intervention if required, and proper postoperative care, patients can recover and resume a healthy lifestyle.
- Furthermore, raising awareness about risk factors and preventive measures can contribute to a reduction in the incidence of cholecystitis and its associated complications.
- By collaborating with healthcare providers, patients can play an active role in managing their condition and maintaining their overall well-being.
Liver Cirrhosis
Introduction
- Liver cirrhosis is a chronic condition that results from the scarring and damage of the liver tissue. It can be caused by various factors, such as:
- viral infections
- alcohol abuse
- autoimmune diseases
- genetic disorders
- toxins.
- Liver cirrhosis affects the normal functioning of the liver, which is responsible for many vital processes in the body, such as:
- Metabolism
- Detoxification
- blood clotting
- immunity.
- If left untreated, liver cirrhosis can lead to serious complications, such as:
- portal hypertension
- bleeding varices
- ascites
- hepatic encephalopathy
- liver cancer.
- Therefore, it is important for nurses to understand the pathophysiology, diagnosis, management, and prevention of liver cirrhosis and its complications.
- This study guide will provide an overview of these topics and help nurses prepare for caring for patients with liver cirrhosis.
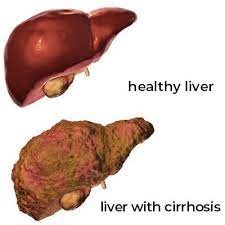
Etiology and Risk Factors
The most common causes of liver cirrhosis are:
- Chronic Viral Hepatitis (B, C, or D):
Chronic viral hepatitis is a long-term infection caused by hepatitis B virus (HBV), hepatitis C virus (HCV), or hepatitis D virus (HDV). These viruses can lead to persistent inflammation in the liver, which, over time, can result in the development of cirrhosis. The inflammation triggers the body's immune response, causing damage to liver cells and leading to fibrosis (scar tissue formation). In some cases, this fibrosis progresses to cirrhosis, which is the advanced stage of liver damage.
- Alcohol Abuse:
Alcohol abuse is one of the leading causes of liver cirrhosis in many parts of the world. Prolonged and excessive alcohol consumption can directly damage liver cells, leading to inflammation and subsequent scarring. The risk of developing cirrhosis is closely related to the amount and duration of alcohol consumption. Individuals who regularly consume large amounts of alcohol over a prolonged period are at a higher risk of developing cirrhosis.
- Nonalcoholic Fatty Liver Disease (NAFLD):
NAFLD is a condition characterized by the accumulation of fat in the liver in individuals who consume little or no alcohol. The exact cause of NAFLD is not fully understood, but it is strongly associated with obesity, insulin resistance, type 2 diabetes, and metabolic syndrome. Over time, NAFLD can progress to nonalcoholic steatohepatitis (NASH), which is a more severe form of the disease. NASH can lead to liver inflammation and fibrosis, eventually resulting in cirrhosis in some cases.
- Autoimmune Hepatitis:
Autoimmune hepatitis is a condition where the body's immune system mistakenly attacks the liver cells, leading to chronic inflammation. The exact cause of autoimmune hepatitis is not well understood, but genetic and environmental factors likely play a role. If left untreated, chronic inflammation can lead to fibrosis and cirrhosis.
- Biliary Disorders:
Biliary disorders, such as primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC), can cause damage and inflammation to the bile ducts in the liver. In PBC, the immune system attacks the small bile ducts, leading to inflammation and scarring. PSC is characterized by inflammation and scarring of the larger bile ducts inside and outside the liver. Over time, the damage to the bile ducts can progress to cirrhosis.
- Genetic Disorders:
Certain genetic disorders can lead to the accumulation of substances in the liver, causing damage and eventual cirrhosis. Three common genetic disorders associated with cirrhosis include:
- Hemochromatosis: This disorder causes the body to absorb too much iron from the diet, leading to the deposition of iron in the liver and other organs. The excess iron can cause liver cell damage and cirrhosis.
- Wilson's Disease: Wilson's disease results in the accumulation of copper in the liver and other organs due to the body's inability to properly metabolize copper. The excess copper buildup can cause liver inflammation and cirrhosis.
- Alpha-1 Antitrypsin Deficiency: This genetic disorder can lead to the abnormal accumulation of a protein called alpha-1 antitrypsin in liver cells. The buildup of this protein can cause liver cell injury and cirrhosis.
- Drugs or Toxins:
Certain medications, chemicals, and toxins, when taken in excessive amounts or over a prolonged period, can cause liver damage and cirrhosis. Some examples of drugs and toxins known to be associated with cirrhosis include:
- Acetaminophen: Overdosing on acetaminophen (paracetamol) can cause severe liver injury and potentially lead to cirrhosis.
- Methotrexate: This medication, used for various medical conditions such as autoimmune diseases and cancer, can be toxic to the liver and contribute to cirrhosis in some cases.
- Amiodarone: This antiarrhythmic medication can cause liver damage, and in rare cases, cirrhosis.
- It's essential to note that some individuals may have multiple risk factors, and the presence of more than one cause can increase the likelihood of developing liver cirrhosis. Early detection and appropriate management of the underlying causes are crucial in preventing the progression of cirrhosis and its complications.

Clinical Manifestations and Symptoms
- The signs and symptoms of liver cirrhosis depend on the severity and stage of the disease.
- In the early stages, patients may be asymptomatic or have nonspecific symptoms such as:
- fatigue
- Weakness
- Anorexia
- weight loss
- nausea
- abdominal pain
- pruritus.
- As the disease progresses, patients may develop more specific symptoms such as:
- spider angiomas
- palmar erythema
- jaundice
- gynecomastia
- ascites
- peripheral edema
- splenomegaly
- caput-medusae
- esophageal varices
- hematemesis
- melena
- hepatic encephalopathy
- asterixis
- coagulopathy
- hypoalbuminemia
- hypoglycemia.
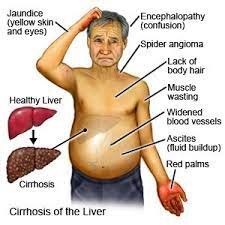
Diagnostic Evaluation
- The diagnosis of liver cirrhosis is based on a combination of history, physical examination, laboratory tests, imaging studies, and liver biopsy.
- Laboratory tests may show elevated liver enzymes (AST, ALT), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), bilirubin (total and direct), ammonia; decreased albumin, globulin, prothrombin time (PT), international normalized ratio (INR), platelets; and abnormal electrolytes (hyponatremia, hypokalemia).
- Imaging studies such as ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), or elastography may show changes in the liver size, shape, texture, echogenicity, or stiffness.
- Liver biopsy is the gold standard for confirming the diagnosis and grading the severity of liver cirrhosis.
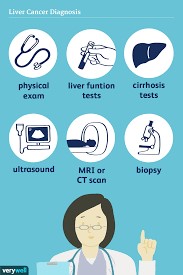
Management and Treatment
- The management and treatment of liver cirrhosis aim to:
- slow down the progression of the disease
- prevent or treat complications
- improve the quality of life of patients.
- The main strategies include:
- Treating the underlying cause of liver cirrhosis (e.g., antiviral therapy for hepatitis B or C; corticosteroids or immunosuppressants for autoimmune hepatitis; chelation therapy for hemochromatosis; penicillamine for Wilson's disease; abstaining from alcohol or drugs; weight loss and lifestyle modification for NAFLD).
- Managing portal hypertension and its complications (e.g., beta-blockers or nitrates for variceal prophylaxis; endoscopic band ligation or sclerotherapy for variceal bleeding; diuretics or paracentesis for ascites; lactulose or rifaximin for hepatic encephalopathy; trans-jugular intrahepatic portosystemic shunt [TIPS] or surgical shunt for refractory cases).
- Providing supportive care and symptom relief (e.g., anti-pruritics for pruritus; vitamin K or fresh frozen plasma for coagulopathy; albumin or glucose infusion for hypoalbuminemia or hypoglycemia; nutritional supplements for malnutrition).
- Considering liver transplantation for patients with end-stage liver disease who meet the criteria and have no contraindications.
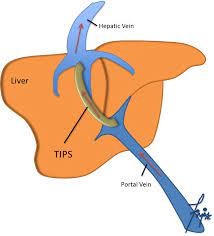
Nursing Interventions and Patient Education
- Nurses play a vital role in caring for patients with liver cirrhosis by providing holistic and individualized care that addresses their physical, psychological, social, and spiritual needs.
- Some of the nursing interventions and patient education topics include:
- Assessing the patient's vital signs, fluid status, neurological status, skin integrity, nutritional status, pain level, and risk for bleeding.
- Monitoring the patient's laboratory results and reporting any abnormal findings to the health care provider.
- Administering medications as prescribed and observing for any adverse effects or interactions.
- Assisting with procedures such as paracentesis or endoscopy and providing post-procedure care.
- Educating the patient about the disease process, complications, and treatment options.
- Teaching the patient about self-care measures such as avoiding alcohol, drugs, or hepatotoxic substances.
- Providing emotional support and counseling to the patient and family and referring them to appropriate resources such as social workers, psychologists, support groups, or palliative care teams.
Summary
- Liver cirrhosis is a chronic condition that results from the irreversible scarring and fibrosis of the liver tissue.
- It affects the normal structure and function of the liver, leading to impaired blood flow, bile production, detoxification, and metabolism.
- Liver cirrhosis can progress to liver failure, portal hypertension, variceal bleeding, ascites, hepatic encephalopathy, and hepatocellular carcinoma.
- The diagnosis of liver cirrhosis is based on a combination of history, physical examination, laboratory tests, imaging studies, and liver biopsy.
- The management and treatment of liver cirrhosis aim to slow down the progression of the disease, prevent or treat complications, and improve the quality of life of patients.
- Nurses play a vital role in caring for patients with liver cirrhosis by providing holistic and individualized care that addresses their physical, psychological, social, and spiritual needs.
Liver cirrhosis is a chronic condition that results from the irreversible scarring and fibrosis of the liver tissue.
- It affects the normal structure and function of the liver, leading to impaired blood flow, bile production, detoxification, and metabolism.
- Liver cirrhosis can progress to liver failure, portal hypertension, variceal bleeding, ascites, hepatic encephalopathy, and hepatocellular carcinoma.
- The diagnosis of liver cirrhosis is based on a combination of history, physical examination, laboratory tests, imaging studies, and liver biopsy.
- The management and treatment of liver cirrhosis aim to slow down the progression of the disease, prevent or treat complications, and improve the quality of life of patients.
- Nurses play a vital role in caring for patients with liver cirrhosis by providing holistic and individualized care that addresses their physical, psychological, social, and spiritual needs.
Conclusion
- In conclusion, liver cirrhosis is a complex and serious condition characterized by the progressive and irreversible scarring of the liver tissue.
- It is a result of various underlying causes, each impacting the liver in distinct ways.
- The most common etiological factors include:
- chronic viral hepatitis (B, C, or D)
- alcohol abuse
- nonalcoholic fatty liver disease (NAFLD)
- autoimmune hepatitis
- biliary disorders (primary biliary cholangitis or primary sclerosing cholangitis)
- genetic disorders (hemochromatosis, Wilson's disease, alpha-1 antitrypsin deficiency)
- Drugs or toxins (acetaminophen, methotrexate, amiodarone).
- The development of cirrhosis is a gradual process, often taking years to manifest clinically. During this time, the liver's normal functions are compromised, and the accumulated scar tissue disrupts its ability to detoxify the blood, produce proteins, and regulate various metabolic processes.
- As cirrhosis progresses, it can lead to severe complications, such as portal hypertension, ascites (fluid buildup in the abdomen), hepatic encephalopathy (brain dysfunction due to liver failure), and an increased risk of liver cancer.
- Early diagnosis and prompt management of the underlying causes are essential to prevent or delay the progression of cirrhosis. For instance, antiviral medications can effectively control chronic viral hepatitis, lifestyle changes (such as alcohol cessation and weight loss) can improve NAFLD, and immunosuppressive drugs can help manage autoimmune hepatitis. Additionally, genetic disorders require specialized treatment and close monitoring.
- However, in advanced cases of cirrhosis, where significant liver damage has occurred, the only definitive treatment option may be a liver transplant.
- Liver transplantation offers hope to eligible patients by replacing the damaged liver with a healthy donor organ, potentially restoring normal liver function and improving overall health.
- Preventive measures are crucial to reducing the incidence of liver cirrhosis. Public health campaigns, early screening, and education on the risks of excessive alcohol consumption and hepatitis infections can make a significant impact.
- Additionally, healthcare professionals play a vital role in identifying individuals at risk, providing appropriate counseling, and offering timely interventions to prevent the progression of liver disease.
- Liver cirrhosis is a grave health concern that demands attention from individuals, healthcare providers, and policymakers alike.
- By addressing the underlying causes, promoting healthy lifestyle choices, and improving access to healthcare services, we can strive to reduce the burden of liver cirrhosis and improve the quality of life for those affected by this condition.
Hernias
Introduction
- Hernias are a common medical condition that affects millions of people worldwide.
- They occur when an organ or tissue pushes through a weakened or torn area of the abdominal wall or surrounding connective tissues.
- This protrusion can cause discomfort, pain, and other symptoms, and in severe cases, it may lead to serious complications requiring urgent medical attention.
- Hernias can develop in various parts of the body, with the most common types including inguinal hernias, umbilical hernias, and incisional hernias.
- Each type of hernia has its own distinct characteristics and risk factors, but they all share the underlying mechanism of weakened abdominal walls allowing internal organs or tissues to push through.
- While some hernias may be asymptomatic or cause only mild discomfort, others can become incarcerated or strangulated, leading to severe pain, bowel obstruction, and potential impairment of blood flow to the herniated tissue.
- Recognizing the signs and symptoms of hernias is crucial for timely diagnosis and appropriate management.
- Understanding hernias and their management is vital for healthcare professionals, as well as individuals at risk of developing hernias.
- By raising awareness and providing accurate information, we can work towards better prevention, early diagnosis, and effective treatment, ultimately improving the overall well-being and quality of life for those affected by hernias.
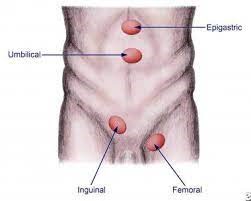
Types of hernias
- Hernias are classified into different types depending on their location and cause. The most common types of hernias are:
- Inguinal hernia: occurs when the intestine or the bladder bulges through the abdominal wall or into the inguinal canal in the groin. It is more common in men than women.
- Femoral hernia: occurs when fatty tissue or a segment of the intestine enters the groin, carrying the femoral artery, and goes to the lower abdomen, on top of the inner thigh. It is more common in women than men, especially older, pregnant, or obese women.
- Umbilical hernia: occurs when part of the small intestine or an adipose tissue pushes around the abdomen closer to the belly button (periumbilical) or at the navel area. It is common among newborns, obese women, and mothers who have many children.
- Incisional hernia: occurs when the intestines protrude to the abdominal wall at the site of a previous abdominal or pelvic surgical operation. It is more common in elderly or obese patients who have lesser physical activity after surgery.
- Hiatal hernia: occurs when a portion of the stomach pushes up to the chest cavity through an opening in the diaphragm. The diaphragm is a muscle used for respiration, located between the chest and abdomen.
- Hernias can be further classified into two types based on their reducibility:
- Reducible hernia: a hernia that can be pushed back into its original position manually or spontaneously. It does not cause any obstruction to the blood flow or bowel movement.
- Irreducible or incarcerated hernia: a hernia that cannot be pushed back into its original position and remains trapped outside the abdominal cavity. It can cause obstruction to the blood flow or bowel movement and lead to complications such as strangulation, ischemia, necrosis, or perforation.

Etiology and risk factors
- The exact cause of hernias is not always clear, but some factors that can contribute to their development are:
- Increased intra-abdominal pressure: caused by chronic coughing, straining during bowel movement or urination, heavy lifting, pregnancy, obesity, or ascites.
- Weakness of the abdominal wall or surrounding tissue: caused by congenital defects, aging, previous surgery, injury, infection, or collagen disorders.
- Family history: having a close relative with a hernia increases the risk of developing one.
- Smoking: smoking can impair wound healing and increase coughing, which can increase intra-abdominal pressure and weaken the abdominal wall.
- Certain medications: some medications such as corticosteroids can affect collagen synthesis and weaken the abdominal wall.
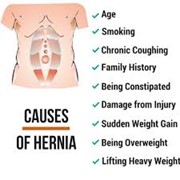
Clinical Presentation and Symptoms
- Some patients might not experience any signs and symptoms in the early stage of hernia.
- The signs and symptoms will depend on what kind of hernia the patient has.
- Some common signs and symptoms are:
- A visible bulge in the affected area: this is the most common sign of hernia and it may become more prominent when standing, coughing, or straining.
- Pain or discomfort in the affected area: this may vary from mild to severe depending on the size and type of hernia. The pain may worsen when standing, coughing, or straining.
- Heartburn, chest pain, dysphagia, or regurgitation: these may occur in patients with hiatal hernia due to reflux of gastric contents into the esophagus.
- Constipation, blood in stool, nausea, vomiting: these may occur in patients with incarcerated hernia due to bowel obstruction.
- In severe cases of hernia, the symptoms below indicating a medical emergency may be evident:
- Fever
- Tachycardia
- Hypotension
- Peritonitis
- Shock

Diagnostic Evaluation
- The diagnosis of hernia is mainly based on history taking and physical examination.
- The following tests may be done to confirm the diagnosis and rule out other conditions:
- Abdominal ultrasound: this can help visualize the size and location of the hernia and detect any complications such as strangulation or incarceration.
- Abdominal X-ray: this can help detect any signs of bowel obstruction such as air-fluid levels or dilated loops of the bowel.
- Barium swallow or upper gastrointestinal endoscopy: these can help diagnose hiatal hernia by showing the position of the stomach and esophagus.
- Blood tests: these can help detect any signs of infection or inflammation such as elevated white blood cell count or C-reactive protein.
Management and Treatment
- The treatment of hernia depends on the type, size, and symptoms of the hernia.
- The main options are:
- Watchful waiting: this is suitable for patients with small, asymptomatic, or reducible hernias. The patient is advised to avoid activities that increase intra-abdominal pressure and to monitor the hernia for any changes or complications.
- Surgery: this is the definitive treatment for hernias and it involves repairing the defect in the abdominal wall or surrounding tissue and restoring the normal anatomy.
- Surgery can be done by open or laparoscopic techniques.
- The type of surgery depends on the type, size, and location of the hernia, as well as the patient's preference and general health.
- Surgery can prevent complications such as strangulation, incarceration, or bowel obstruction.
- However, surgery also carries some risks such as infection, bleeding, recurrence, or nerve injury.

Nursing Considerations and Patient Education
- Nurses play an important role in the care of patients with hernias.
- Some of the nursing considerations and patient education are:
- Assess the patient's history, symptoms, vital signs, and abdominal examination.
- Monitor the patient for any signs of complications such as:
- Fever
- Tachycardia
- Hypotension
- Peritonitis
- Shock
- bowel obstruction
- Administer pain relief, antibiotics, fluids, or other medications as prescribed.
- Prepare the patient for surgery if indicated and provide preoperative and postoperative care.
- Educate the patient about the causes, types, symptoms, and complications of hernia.
- Teach the patient how to reduce intra-abdominal pressure by avoiding heavy lifting, straining, coughing, smoking, or obesity.
- Teach the patient how to perform self-care such as wound care, activity restriction, pain management, and signs of infection or recurrence.
- Encourage the patient to seek medical attention if they notice any changes or worsening of their hernia.

Summary
- Hernias are protrusions of internal organs or fatty tissues through a weakened abdominal wall or surrounding tissue.
- They can cause pain, discomfort, and complications if left untreated.
- Hernias are classified into different types depending on their location and cause.
- The diagnosis is mainly based on history taking and physical examination. The treatment options are watchful waiting or surgery depending on the type, size, and symptoms of the hernia.
- Nurses play an important role in the care of patients with hernias by providing assessment, monitoring, medication administration, surgery preparation and care, patient education, and self-care teaching.
Conclusion
- In conclusion, hernias are a common medical condition characterized by the protrusion of an organ or tissue through a weakened area of the abdominal wall or surrounding connective tissues.
- They can occur in various regions of the body, with inguinal, umbilical, and incisional hernias being the most prevalent types.
- Throughout this study, we have explored the different types of hernias, their causes, risk factors, symptoms, and treatment options.
- Hernias often develop due to a combination of factors, including increased intra-abdominal pressure, weakened muscles or connective tissues, and genetic predisposition.
- Certain lifestyle choices, such as heavy lifting, obesity, and chronic coughing, can also contribute to the development of hernias.
- The clinical presentation of hernias can vary depending on the type and severity.
- Common symptoms include a visible bulge or swelling at the hernia site, discomfort or pain, especially during physical activities or when lifting objects, and a feeling of heaviness or pressure in the affected area. In some cases, hernias may become incarcerated or strangulated, leading to severe pain, nausea, vomiting, and potential obstruction of blood flow to the herniated organ or tissue.
- Prompt medical attention is crucial in such instances to avoid serious complications.
- Diagnosing hernias typically involves a physical examination by a healthcare professional, where the protrusion is often evident.
- In some cases, imaging tests such as ultrasound or CT scan may be required to confirm the diagnosis or assess the severity of the hernia.
- The treatment of hernias typically involves surgical repair, especially if the hernia is symptomatic or has the potential for complications.
- Hernia surgery aims to reinforce the weakened abdominal wall and return the protruding organ or tissue to its proper position.
- Minimally invasive techniques, such as laparoscopic or robotic-assisted hernia repair, have become increasingly common, offering shorter recovery times and reduced postoperative pain compared to traditional open surgery.
- Preventive measures for hernias include maintaining a healthy weight, avoiding heavy lifting and straining during bowel movements, and treating chronic cough or constipation promptly. Additionally, individuals with a family history of hernias or other risk factors should be vigilant in monitoring for potential signs and seek medical advice if they suspect a hernia.
- Public awareness and education about hernias and their management are crucial to encourage timely medical attention and reduce the burden of hernias in the population.
Ascites
Introduction
- Ascites is the abnormal accumulation of fluid in the peritoneal cavity, which can cause abdominal distension, discomfort, and complications such as infection, bleeding, and respiratory compromise.
- The development of ascites is primarily attributed to an imbalance between the formation and drainage of fluid within the peritoneal cavity. In liver cirrhosis, for example, the scarring of liver tissue impairs its ability to produce albumin, which plays a vital role in maintaining proper fluid balance. As a result, fluid accumulates in the peritoneal cavity, leading to ascites.
- Other mechanisms, such as increased pressure within the portal vein system or decreased oncotic pressure, can also contribute to fluid retention.
- Ascites is most commonly caused by portal hypertension due to liver cirrhosis, but other conditions such as:
- Malignancy
- heart failure
- nephrotic syndrome
- tuberculosis
- The diagnosis of ascites is based on clinical examination, imaging studies, and paracentesis with ascitic fluid analysis.
- The management of ascites depends on the underlying cause, the severity of symptoms, and the presence of complications.
- The main goals of treatment are to reduce fluid retention, prevent complications, and improve quality of life.

Etiology and risk factors
- The etiology of ascites can be classified into three categories:
- portal hypertension-related
- non-portal hypertension-related
- mixed.
- Portal hypertension-related ascites account for about 80% of cases and are mainly due to liver cirrhosis.
- Cirrhosis causes increased resistance to blood flow in the liver, leading to increased pressure in the portal vein and its branches.
- This results in splanchnic vasodilation, reduced effective arterial blood volume, activation of neurohormonal systems that promote sodium and water retention, and increased lymphatic drainage into the peritoneal cavity.
- The risk factors for cirrhosis include:
- viral hepatitis
- alcohol abuse
- non-alcoholic fatty liver disease
- autoimmune hepatitis
- biliary diseases
- metabolic disorders
- genetic diseases.
- Non-portal hypertension-related ascites account for about 10% of cases and are caused by conditions that increase capillary permeability or decrease oncotic pressure in the peritoneal vessels.
These include:
- malignancy (e.g., ovarian cancer, peritoneal carcinomatosis)
- infections (e.g., tuberculosis, peritonitis)
- pancreatitis
- nephrotic syndrome
- hypothyroidism
- malnutrition.
- Mixed ascites account for about 10% of cases and are caused by a combination of portal hypertension and other factors.
These include:
- heart failure
- constrictive pericarditis
- hepatic venous outflow obstruction (e.g., Budd-Chiari syndrome)
- portal vein thrombosis.
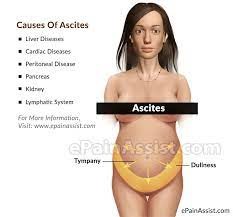
Clinical presentation and symptoms
- The clinical presentation of ascites varies depending on the volume of fluid accumulation, the rate of fluid accumulation, and the underlying cause.
- The most common symptom of ascites is abdominal distension, which can cause discomfort, early satiety, indigestion, nausea, vomiting, dyspnea, orthopnea, reduced mobility, and impaired quality of life.
- Other symptoms may include:
- abdominal pain (due to stretching of the capsule or peritoneum)
- fever (due to infection)
- jaundice (due to liver dysfunction)
- lower extremity edema (due to hypoalbuminemia or right-sided heart failure)
- weight gain (due to fluid retention)
- encephalopathy (due to hepatic failure)
- The physical examination of ascites may reveal:
- increased abdominal girth
- shifting dullness (change in percussion note with change in position)
- fluid wave (transmission of a wave across the abdomen when one flank is tapped)
- flank dullness (dull percussion note over the dependent flank)
- umbilical or inguinal hernia (due to increased intra-abdominal pressure)
- caput medusae (dilated veins around the umbilicus due to portal-systemic shunting) spider angiomas or palmar erythema (due to hyperestrogenism or vasodilation)
- asterixis (flapping tremor of the hands due to encephalopathy)
- signs of underlying causes (e.g., hepatomegaly or splenomegaly)

Diagnostic Evaluation
- Ascites is the accumulation of fluid in the abdominal cavity, often associated with liver disease.
- To diagnose ascites, the following steps are recommended:
- Perform a comprehensive history and physical exam to assess the presumptive cause and extent of the condition. Look for signs and symptoms such as increased abdominal girth, weight gain, shortness of breath, nausea, swelling of the lower extremities, indigestion, loss of appetite, abdominal pain, and fever.
- Perform a diagnostic paracentesis to obtain ascitic fluid for analysis. This is a procedure that involves inserting a needle into the abdomen and draining some fluid.
- The initial ascitic fluid analysis should include total protein concentration and calculation of the serum ascites albumin gradient (SAAG). The SAAG is the difference between the serum albumin and the ascitic fluid albumin levels. A high SAAG (>1.1 g/dL) indicates portal hypertension as the cause of ascites, while a low SAAG (<1.1 g/dL) indicates other causes such as infection, inflammation, or malignancy.
- Other tests that may be done on the ascitic fluid include cytology, amylase, brain natriuretic peptide (BNP), and adenosine deaminase, depending on the suspected cause of ascites.
- Perform imaging studies such as ultrasound or CT scan to identify the cause and complications of ascites, such as liver cirrhosis, portal vein thrombosis, hepatocellular carcinoma, splenomegaly, or spontaneous bacterial peritonitis.

Management and Treatment
- The management and treatment of ascites depend on the underlying cause and the severity of the condition.
- The general principles are:
- Treat the cause of ascites if possible. For example, if ascites is due to liver cirrhosis, antiviral therapy for hepatitis B or C infection, abstinence from alcohol, or liver transplantation may be indicated.
- Restrict sodium intake to less than 2 g/day to reduce fluid retention and edema. A low-sodium diet consists of avoiding processed foods, canned foods, salted snacks, cheese, cured meats, sauces, and adding salt to food.
- Use diuretics to increase urine output and decrease fluid accumulation. The most commonly used diuretics are spironolactone and furosemide. The dose and frequency of diuretics should be adjusted according to the patient's weight, urine output, serum electrolytes, and renal function. The goal is to achieve a weight loss of 0.5 kg/day for patients with peripheral edema and 0.25 kg/day for patients without peripheral edema.
- Perform therapeutic paracentesis to remove large volumes of fluid from the abdomen and relieve symptoms such as abdominal discomfort, dyspnea, or early satiety. This procedure should be done under sterile conditions and with local anesthesia. The amount of fluid removed depends on the patient's tolerance and hemodynamic status. Generally, no more than 5 L of fluid should be removed at one time. Albumin infusion may be given to prevent circulatory dysfunction after large-volume paracentesis.
- Consider transjugular intrahepatic portosystemic shunt (TIPS) for patients with refractory ascites that do not respond to diuretics or repeated paracentesis. TIPS is a procedure that creates a shunt between the portal vein and the hepatic vein using a stent, thereby reducing portal pressure and improving blood flow. TIPS can improve ascites control but may also increase the risk of hepatic encephalopathy, bleeding, infection, or shunt dysfunction.
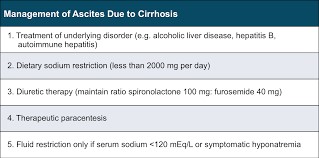
Nursing Interventions and Patient Support
- Nursing interventions and patient support for patients with ascites include:
- Monitor vital signs, weight, urine output, fluid intake and output, serum electrolytes, renal function, and signs of complications such as infection, bleeding, or encephalopathy.
- Educate the patient about the causes and consequences of ascites, the importance of sodium restriction and medication adherence, the signs and symptoms of worsening conditions or complications, and when to seek medical attention.
- Provide emotional support and counseling to the patient and family members. Ascites can affect the patient's quality of life, self-image, mobility, and social interactions. Address any concerns or fears that the patient may have regarding their condition or treatment options.
- Refer the patient to appropriate resources or services such as dietitian, social worker, psychologist, support group, or palliative care team.

Summary
- Ascites is a common complication of liver disease that requires prompt diagnosis and management.
- The evaluation of ascites involves:
- history taking,
- physical examination,
- paracentesis,
- ascitic fluid analysis,
- and imaging studies.
- The treatment of ascites aims to:
- treat the underlying cause,
- restrict sodium intake,
- use diuretics,
- perform therapeutic paracentesis,
- and consider TIPS for refractory cases.
- Nursing interventions and patient support focus on:
- monitoring the patient's condition and response to treatment,
- educating the patient and family members,
- providing emotional support and counseling,
- and referring the patient to appropriate resources or services.
Conclusion
- In conclusion, ascites is a significant medical condition characterized by the abnormal accumulation of fluid within the peritoneal cavity, leading to abdominal distension.
- It is often a manifestation of an underlying systemic disease, most commonly liver cirrhosis, but can also be caused by various other conditions, including heart failure, kidney disease, and malignancies.
- Understanding the underlying causes of ascites is crucial in tailoring appropriate treatment and managing the condition effectively.
- The development of ascites is primarily attributed to an imbalance between the formation and drainage of fluid within the peritoneal cavity. In liver cirrhosis, for example, the scarring of liver tissue impairs its ability to produce albumin, which plays a vital role in maintaining proper fluid balance. As a result, fluid accumulates in the peritoneal cavity, leading to ascites.
- Other mechanisms, such as increased pressure within the portal vein system or decreased oncotic pressure, can also contribute to fluid retention.
- Clinical manifestations of ascites can range from mild abdominal discomfort to severe distension, causing respiratory compromise and affecting the patient's quality of life.
- Alongside the physical symptoms, patients with ascites may also experience weight gain, difficulty breathing, and ankle swelling.
- Diagnosing ascites typically involves a combination of physical examination, imaging studies, and laboratory tests. Abdominal ultrasound and computed tomography (CT) scans are commonly used to visualize the presence and quantity of ascitic fluid. Paracentesis, the removal and analysis of ascitic fluid, aids in identifying the underlying cause of ascites and guiding further management.
- The management of ascites depends on addressing the underlying condition and alleviating fluid accumulation. For patients with liver cirrhosis, dietary sodium restriction, diuretic therapy, and sometimes large-volume paracentesis are used to manage ascites. In cases of refractory ascites or severe complications, transjugular intrahepatic portosystemic shunt (TIPS) procedures or liver transplantation may be considered.
- Preventive measures for ascites focus on managing the underlying conditions contributing to fluid retention. Timely diagnosis and treatment of liver disease, heart failure, or kidney disease can prevent or slow the development of ascites. Moreover, lifestyle modifications, such as reducing alcohol consumption and maintaining a healthy diet, play a vital role in mitigating the risk of liver cirrhosis and other related conditions.
- A multidisciplinary approach involving gastroenterologists, hepatologists, and other healthcare specialists is essential in managing ascites effectively.
- Emphasizing preventive measures and raising awareness about the underlying causes of ascites can contribute to early diagnosis and timely intervention, improving patient outcomes and overall quality of life.
Cholelithiasis
Introduction
- Cholelithiasis is the medical term for the presence of gallstones in the gallbladder.
- Gallstones are solid concretions that form from the hardening of bile, a digestive fluid that is stored and released by the gallbladder.
- Bile consists of water, cholesterol, bile salts, lecithin, bilirubin, and other substances.
- Gallstones can vary in size, shape, number, and composition.
- They can cause inflammation, infection, obstruction, or damage to the gallbladder and the bile ducts.
- Timely diagnosis, appropriate management, and preventive measures are crucial in mitigating the impact of gallstones on patients' health and well-being.
- By understanding the underlying causes and risk factors, healthcare professionals can work collaboratively with patients to implement effective strategies for prevention and optimize patient outcomes.
- Public awareness and education regarding cholelithiasis are essential in empowering individuals to take charge of their health and make informed decisions regarding their lifestyle choices.
- Through these efforts, we can strive to reduce the burden of cholelithiasis and improve the overall quality of life for affected individuals.
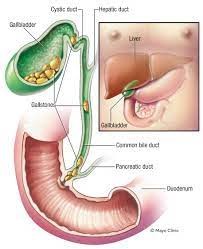
Etiology and risk factors
- The exact cause of cholelithiasis is not fully understood, but it is believed to result from an imbalance in the components of bile.
- Some factors that can contribute to this imbalance are:
- Excess cholesterol production by the liver or intake from the diet
- Reduced bile salt production or secretion by the liver
- Decreased gallbladder motility or emptying
- Increased bilirubin production or excretion due to hemolysis, liver disease, or infection
- Genetic factors that affect bile composition or metabolism
- Some risk factors that increase the likelihood of developing cholelithiasis are:
- Female gender
- Older age
- Obesity
- Rapid weight loss or fasting
- Pregnancy or use of oral contraceptives
- Diabetes mellitus
- Family history of gallstones
- Ethnicity (more common in Native Americans, Hispanics, and Scandinavians)
- Certain medications (such as ceftriaxone, octreotide, or thiazide diuretics)
- Certain diseases (such as Crohn's disease, cirrhosis, sickle cell anemia, or cystic fibrosis)

Clinical Manifestation and Symptoms
- Many people with cholelithiasis are asymptomatic and do not experience any signs or symptoms. However, when a gallstone blocks the flow of bile from the gallbladder or the bile ducts, it can cause acute or chronic inflammation and infection of the gallbladder (cholecystitis) or the bile ducts (cholangitis).
- This can lead to the following signs and symptoms:
- Biliary colic: a sudden and severe pain in the upper right abdomen or epigastrium that may radiate to the back, shoulder, or chest. The pain usually occurs after a fatty meal and lasts for 15 minutes to several hours. It may be associated with nausea, vomiting, sweating, or restlessness.
- Jaundice: a yellowing of the skin and eyes due to elevated levels of bilirubin in the blood. It may also cause dark urine, pale stools, itching, or malaise.
- Fever and chills: a sign of infection or inflammation of the gallbladder or the bile ducts. It may also be accompanied by leukocytosis, increased liver enzymes, or increased bilirubin levels.
- Murphy's sign: a positive physical examination finding in which there is pain or cessation of breathing when the examiner palpates the right upper quadrant of the abdomen during inspiration.
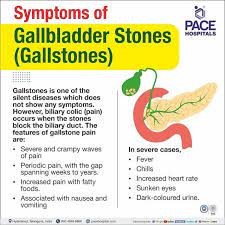
Diagnostic Evaluation
- The diagnosis of cholelithiasis is based on the history, physical examination, laboratory tests, and imaging studies.
- Some of the diagnostic tests that can be used are:
- Ultrasound: a non-invasive and accurate imaging technique that uses sound waves to visualize the gallbladder and the bile ducts. It can detect the presence, size, number, and location of gallstones as well as signs of inflammation or infection.
- Computed tomography (CT) scan: an imaging technique that uses X-rays to create cross-sectional images of the abdomen. It can provide more detailed information about the anatomy and pathology of the gallbladder and the bile ducts than ultrasound.
- Magnetic resonance cholangiopancreatography (MRCP): an imaging technique that uses magnetic fields to create images of the biliary tree and pancreas. It can detect gallstones as well as other causes of biliary obstruction such as tumors or strictures.
- Endoscopic retrograde cholangiopancreatography (ERCP): an invasive procedure that combines endoscopy and fluoroscopy to visualize and treat the biliary tree and pancreas. It involves inserting a flexible tube (endoscope) through the mouth into the duodenum and injecting contrast dye into the bile ducts. It can diagnose and remove gallstones as well as perform other interventions such as sphincterotomy, stent placement, or biopsy.
- Hepatobiliary iminodiacetic acid (HIDA) scan a nuclear medicine test that evaluates the function and patency of the biliary system. It involves injecting a radioactive tracer into the bloodstream and measuring its uptake and excretion by the liver, gallbladder, and bile ducts. It can detect acute or chronic cholecystitis as well as biliary obstruction or leakage.
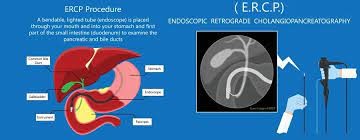
Management and Treatment
- The treatment of cholelithiasis depends on the severity of the symptoms, the presence of complications, and the patient's preference.
- Some of the treatment options are:
- Conservative management: this involves dietary modification, pain relief, and observation. It is suitable for asymptomatic or mild cases of cholelithiasis that do not require surgery.
- Dietary modification includes avoiding fatty, spicy, or fried foods and increasing fluid and fiber intake.
- Pain relief can be achieved with nonsteroidal anti-inflammatory drugs (NSAIDs), antispasmodics, or opioids.
- Observation involves regular follow-up and monitoring for signs of complications or worsening symptoms.
- Cholecystectomy: this is the surgical removal of the gallbladder. It is the definitive treatment for symptomatic or complicated cases of cholelithiasis that do not respond to conservative management. It can be performed either laparoscopically or open.
- Laparoscopic cholecystectomy involves making small incisions in the abdomen and inserting a camera and instruments to remove the gallbladder. It has advantages such as less pain, faster recovery, and fewer complications than open cholecystectomy.
- Open cholecystectomy involves making a large incision in the abdomen and removing the gallbladder through it. It may be necessary if laparoscopic cholecystectomy is not feasible or safe due to factors such as inflammation, infection, adhesions, or anatomy.
- Endoscopic management: this involves using ERCP to diagnose and treat biliary obstruction or infection caused by gallstones. It can be performed either before or after cholecystectomy depending on the clinical situation. It can remove gallstones from the bile ducts, relieve biliary pressure, drain pus or bile, place stents, or perform other interventions.
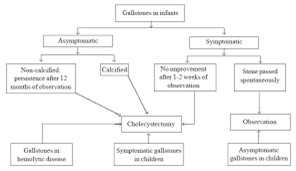
Prevention Strategies and Patient Education
- The prevention of cholelithiasis involves modifying the risk factors that contribute to gallstone formation.
- Some of the prevention strategies and patient education are:
- Maintain a healthy weight and avoid rapid weight loss or fasting
- Eat a balanced diet that is low in cholesterol and fat and high in fiber and antioxidants
- Drink plenty of water and avoid alcohol and caffeine
- Exercise regularly and avoid a sedentary lifestyle
- Control blood sugar levels and avoid diabetes mellitus
- Consult a doctor before taking any medications or supplements that may affect bile composition or metabolism
- Seek medical attention if experiencing any signs or symptoms of cholelithiasis or its complications

Summary
- Cholelithiasis is a common condition that affects the gallbladder and the bile ducts.
- It is caused by an imbalance in the components of bile that leads to gallstone formation. Gallstones can cause inflammation, infection, obstruction, or damage to the biliary system.
- The diagnosis of cholelithiasis is based on history, physical examination, laboratory tests, and imaging studies.
- The treatment of cholelithiasis depends on the severity of the symptoms, the presence of complications, and the patient's preference.
- It can range from conservative management to surgical removal of the gallbladder to endoscopic intervention.
- The prevention of cholelithiasis involves modifying the risk factors that contribute to gallstone formation.
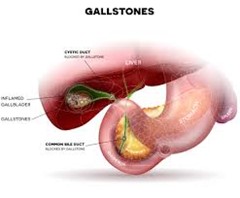
Conclusion
- In conclusion, cholelithiasis, commonly known as gallstones, is a prevalent and significant medical condition affecting the gallbladder.
- It is characterized by the formation of solid deposits within the gallbladder or bile ducts, primarily composed of cholesterol, bilirubin, or calcium salts.
- Cholelithiasis can cause various symptoms, ranging from mild discomfort to severe complications, such as acute cholecystitis, biliary colic, or pancreatitis.
- Throughout this study, we have explored the etiology, risk factors, clinical manifestations, diagnosis, and management of cholelithiasis.
- Understanding the factors contributing to gallstone formation is essential in developing preventive strategies and providing appropriate medical care to affected individuals.
- The development of gallstones is influenced by multiple factors, including genetic predisposition, hormonal imbalances, and lifestyle choices.
- High cholesterol levels, obesity, rapid weight loss, and a diet high in fats and low in fiber can increase the risk of gallstone formation.
- Furthermore, certain medical conditions, such as diabetes and liver diseases, may also contribute to gallstone development.
- The clinical presentation of cholelithiasis can vary, with many individuals remaining asymptomatic and unaware of the presence of gallstones.
- However, when symptoms do arise, they often include severe right upper quadrant abdominal pain, nausea, vomiting, and intolerance to fatty foods.
- Timely diagnosis and appropriate management are crucial in preventing complications and improving patient outcomes.
- Diagnosing cholelithiasis involves a combination of patient history, physical examination, and imaging studies. Ultrasonography is the most commonly used imaging modality to visualize gallstones and assess their size, number, and location. Other imaging techniques, such as computed tomography (CT) scans or magnetic resonance cholangiopancreatography (MRCP), may be utilized to provide more detailed information if needed.
- The management of cholelithiasis depends on the presence of symptoms and the risk of complications.
- Asymptomatic gallstones may not require immediate intervention, and lifestyle modifications, such as a healthy diet and exercise, may be recommended to prevent symptom development.
- For symptomatic gallstones or those causing complications, cholecystectomy, the surgical removal of the gallbladder, is the definitive treatment.
- Preventive measures for cholelithiasis involve maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding rapid weight loss.
- Educating individuals about the risk factors and lifestyle modifications can play a pivotal role in reducing the incidence of gallstone formation.
Peritonitis
Introduction
- The peritoneum is a thin layer of tissue that covers the inner surface of the abdominal wall and the organs within the abdomen.
- It has two layers:
- The parietal peritoneum, which lines the abdominal wall, and the visceral peritoneum, which covers the organs.
- The peritoneal cavity is the space between these two layers, which contains a small amount of fluid that lubricates and protects the organs from friction.
- The peritoneum is normally sterile, despite the presence of bacteria in the GI tract. However, when bacteria or other foreign substances enter the peritoneal cavity, either through a perforation or a rupture of an organ, or through the bloodstream or lymphatic system, they can cause inflammation and infection of the peritoneum. This condition is called peritonitis.
- Peritonitis can be classified as primary or secondary.
- Primary peritonitis occurs when bacteria enter the peritoneal cavity without an obvious source of infection, such as in patients with liver cirrhosis or ascites.
- Secondary peritonitis occurs when bacteria enter the peritoneal cavity from a source of infection within the abdomen, such as appendicitis, diverticulitis, peptic ulcer, ulcerative colitis, volvulus, abdominal neoplasms, or trauma.
- Peritonitis can also be classified as localized or generalized.
- Localized peritonitis affects only a limited area of the peritoneum and may form an abscess.
- Generalized peritonitis affects the entire peritoneum and may spread to other organs and systems.
- Peritonitis is a medical emergency that requires immediate diagnosis and treatment. If left untreated, it can cause septic shock, organ failure, intestinal obstruction, adhesions, fistulas, and death.

Etiology and risk factors
- The most common cause of peritonitis is a bacterial infection, which can result from diseases of the GI tract, such as appendicitis, diverticulitis, peptic ulcer, ulcerative colitis, or volvulus. Bacteria can also enter the peritoneal cavity through external sources, such as stab wounds, gunshot wounds, or peritoneal dialysis.
- The most common bacteria implicated are Escherichia coli, Klebsiella, Proteus, Pseudomonas, and Streptococcus.
- Other causes of peritonitis include inflammation that extends from an organ outside the peritoneal area, such as the kidneys, pancreas, or gallbladder; chemical irritation from substances such as bile, blood, or gastric juice; or foreign bodies such as parasites or tumors.
- The risk factors for developing peritonitis include:
- Abdominal surgery or trauma
- Peritoneal dialysis
- Immunocompromised status
- Malnutrition
- Advanced age
- Female gender
- Use of nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids
Clinical Manifestation and Symptoms
- The symptoms of peritonitis depend on the extent and location of the inflammation.
- The most common symptom is abdominal pain, which is usually diffuse at first and then becomes constant, localized, and more intense over the site of the infection.
- The pain is aggravated by movement, coughing, or breathing.
- The abdomen becomes tender, distended, and rigid due to muscle spasms and fluid accumulation.
- Other symptoms include:
- Fever and chills
- Nausea and vomiting
- Anorexia and weight loss
- Diarrhea or constipation
- Decreased urine output
- Tachycardia and hypotension
- Altered mental status
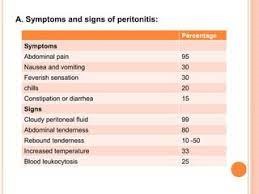
Diagnostic Evaluation
The diagnosis of peritonitis is based on the following:
- History and physical examination- The patient may present with signs and symptoms such as abdominal pain, tenderness, rigidity, distension, fever, tachycardia, nausea, vomiting, anorexia, and altered bowel sounds. The pain may be diffuse or localized depending on the extent and location of the inflammation. The patient may also have a history of GI disorders, abdominal surgery, trauma, or peritoneal dialysis.
- Laboratory tests- The white blood cell (WBC) count is usually elevated, indicating infection and inflammation. The serum electrolyte levels may be abnormal due to fluid and electrolyte imbalance. The blood urea nitrogen (BUN) and creatinine levels may be increased due to renal impairment. The blood culture may identify the causative organism of the infection.
- Imaging studies- The abdominal X-ray may show air-fluid levels, indicating intestinal obstruction or perforation. The abdominal ultrasound or computed tomography (CT) scan may reveal fluid accumulation, abscess formation, or organ involvement.
- Paracentesis: involves inserting a needle into the peritoneal cavity and withdrawing fluid for analysis. The fluid is examined for appearance, cell count, protein level, and glucose level.
Management and Treatment
- The management and treatment of peritonitis depend on the cause, severity, and complications of the condition.
- The main goals are to control the infection, correct the fluid and electrolyte imbalance, relieve the pain and discomfort, and prevent further complications.
- The following are some of the interventions that may be implemented:
- Antibiotics- Antibiotics are administered to treat the infection and prevent sepsis. The choice of antibiotics depends on the source and type of infection, as well as the susceptibility of the organism. Broad-spectrum antibiotics are usually started empirically until the culture results are available. The duration of antibiotic therapy may vary from 7 to 14 days or longer depending on the response and resolution of the infection.
- Fluid resuscitation- Fluid resuscitation is initiated to restore the fluid volume and correct the dehydration and hypovolemia caused by peritonitis. Intravenous (IV) fluids such as normal saline or lactated Ringer's solution are given to replace the fluid losses and maintain adequate urine output and blood pressure. The amount and type of fluids are adjusted based on the patient's condition and laboratory results.
- Analgesics- Analgesics are given to relieve the pain and discomfort associated with peritonitis. Opioids such as morphine or fentanyl are commonly used for moderate to severe pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or ketorolac may be used for mild to moderate pain. However, NSAIDs should be used with caution in patients with renal impairment or bleeding disorders.
- Surgical intervention- Surgical intervention may be required to remove the source of infection or perforation, drain the abscess or fluid collection, repair the damaged tissue or organ, or perform a bowel resection or ostomy if necessary. The type and extent of surgery depend on the cause and severity of peritonitis.
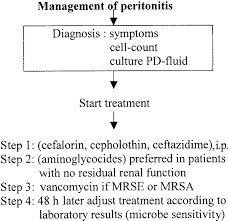
Complications and Nursing Considerations
- Peritonitis can cause various complications that require close monitoring and intervention by the nurse.
- Some of the common complications are:
- Sepsis: Sepsis is a life-threatening condition that occurs when the body's response to infection causes widespread inflammation and organ dysfunction.
- Sepsis can result from peritonitis due to bacterial translocation from the peritoneal cavity into the bloodstream.
- Sepsis can cause fever, tachycardia, hypotension, altered mental status, oliguria, and coagulopathy.
- The nurse should monitor the patient's vital signs, level of consciousness, urine output, and laboratory values such as white blood cell count, blood cultures, lactate, prothrombin time, and partial thromboplastin time.
- The nurse should also administer antibiotics, fluids, vasopressors, and other supportive therapies as prescribed.
- Shock: Shock is a state of inadequate tissue perfusion that leads to cellular hypoxia and organ failure.
- Shock can result from peritonitis due to hypovolemia (from fluid loss into the peritoneal cavity), sepsis (from systemic inflammation and vasodilation), or cardiogenic causes (from myocardial depression or arrhythmias).
- Shock can cause hypotension, tachycardia, tachypnea, cold and clammy skin, weak pulses, and decreased urine output.
- The nurse should monitor the patient's hemodynamic status, fluid balance, and tissue oxygenation.
- The nurse should also administer fluids, blood products, vasopressors, inotropes, and oxygen as prescribed.
- Intestinal obstruction: Intestinal obstruction is a partial or complete blockage of the GI tract that prevents the passage of food, fluids, and gas.
- Intestinal obstruction can result from peritonitis due to paralytic ileus (from decreased intestinal motility), adhesions (from scar tissue formation), or volvulus (from twisting of the bowel). Intestinal obstruction can cause abdominal pain, distension, nausea, vomiting, constipation, and bowel sound changes.
- The nurse should monitor the patient's abdominal assessment, bowel movements, and nasogastric tube drainage.
- The nurse should also maintain the patient's fluid and electrolyte balance, provide decompression with a nasogastric tube or rectal tube as prescribed, and prepare the patient for surgery if indicated.
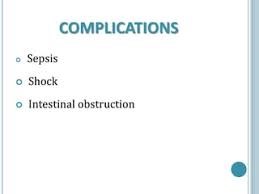
Summary
- Peritonitis is a serious condition that requires prompt diagnosis and treatment to prevent complications and death.
- The nurse plays a vital role in assessing, managing, and educating the patient with peritonitis.
- The nurse should be aware of the signs and symptoms of peritonitis, such as:
- abdominal pain
- tenderness
- rigidity
- fever
- leukocytosis,
- peritoneal fluid analysis.
- The nurse should also be familiar with the medical and surgical treatments for peritonitis,
such as:
- antibiotics
- fluid resuscitation
- analgesics
- antiemetics
- laparotomy or laparoscopy.
- The nurse should also monitor the patient for potential complications of peritonitis, such as sepsis, shock, and intestinal obstruction, and provide appropriate interventions to prevent or treat them.
Conclusion
- Peritonitis is a challenging condition that requires a comprehensive approach to care by the nurse and the multidisciplinary team.
- The nurse should be able to apply evidence-based knowledge and skills to assess, manage, and educate the patient with peritonitis.
- The nurse should also be able to collaborate with other healthcare professionals to provide optimal care for the patient with peritonitis.
- The nurse should also be able to evaluate the outcomes of care and identify areas for improvement.
- By doing so, the nurse can contribute to improving the quality of life and reducing mortality and morbidity of patients with peritonitis.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Digestive System Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


