Please set your exam date
Postpartum Hemorrhage
Study Questions
More Questions on this Topic
A nurse is caring for a client who experienced a postpartum hemorrhage after delivering a large baby following oxytocin induction of labor.
Which of the following factors put this client at risk for developing postpartum hemorrhage? (Select all that apply)
Explanation
A. Grand multiparity is a known risk factor for postpartum hemorrhage, but it is not indicated for this client.
B. Uterine overdistention from delivering a large baby increases the risk for uterine atony, which can lead to postpartum hemorrhage.
C. Precipitous labor is not described in this scenario, so it does not apply to this client.
D. Oxytocin induction can desensitize uterine receptors, causing ineffective contractions and increasing the risk of hemorrhage.
E. Chorioamnionitis is not mentioned for this client, so it is not a contributing factor in this case.
A nurse is assisting with an emergency cesarean delivery for a client who has placenta previa and is experiencing profuse bleeding.
Which of the following medications should the nurse anticipate administering to this client after delivery?
Explanation
The correct answer is choice C. Misoprostol (Cytotec).This medication is used to prevent postpartum hemorrhage (excessive bleeding after delivery) in women with placenta previa.Placenta previa is a condition where the placenta covers the opening of the cervix and can cause severe bleeding during pregnancy.
Choice A is wrong because Methylergonovine (Methergine) is a medication that stimulates uterine contractions and can increase bleeding in women with placenta previa.
Choice B is wrong because Carboprost tromethamine (Hemabate) is also a medication that causes uterine contractions and can worsen bleeding in women with placenta previa.
Choice D is wrong because Terbutaline (Brethine) is a medication that relaxes uterine muscles and can delay labor, but it does not prevent postpartum hemorrhage in women with placenta previa.
Normal ranges for blood loss after delivery are less than 500 mL for vaginal delivery and less than 1000 mL for cesarean delivery.
A nurse is performing fundal massage for a client who has uterine atony and postpartum hemorrhage.
Which of the following actions should the nurse take when performing this procedure?
Explanation
Use one hand to stabilize the lower uterine segment while massaging the fundus with the other hand.
This action prevents the uterus from inverting and reduces the risk of trauma to the cervix and vagina.
The nurse should also monitor the amount and consistency of lochia.
Choice B is wrong because applying firm pressure on the fundus with both hands can cause uterine inversion, which is a life-threatening complication of postpartum hemorrhage.
The nurse should use gentle pressure and avoid overstimulation of the uterus.
Choice C is wrong because massaging the fundus in a circular motion with one hand while supporting the back with the other hand can cause displacement of the uterus and increase bleeding.
The nurse should massage the fundus in a downward motion from the top of the uterus to the umbilicus.
Choice D is wrong because rubbing the fundus vigorously with one hand until it becomes hard and expels clots can cause uterine rupture, which is another serious complication of postpartum hemorrhage.
The nurse should avoid excessive manipulation of the uterus and allow clots to pass naturally.
A nurse is caring for a client who has just delivered a baby and is experiencing postpartum hemorrhage due to uterine atony.
Which of the following medications should the nurse anticipate administering? Select all that apply:
Explanation
The correct answer is choice A, C, D and E. These medications are all uterotonic agents that can stimulate uterine contractions and reduce bleeding.
They act on different receptors in the uterus and have different side effects and contraindications.
Choice B is wrong because magnesium sulfate is a tocolytic agent that can relax uterine muscles and prevent preterm labor.
It is not indicated for postpartum hemorrhage and can worsen uterine atony.
Normal ranges for postpartum blood loss are less than 500 mL for vaginal delivery and less than 1000 mL for cesarean delivery.
Uterine atony is the most common cause of postpartum hemorrhage and occurs when the uterus fails to contract adequately after delivery.
Risk factors include prolonged or rapid labor, overdistension of the uterus, multiparity, retained placenta, infection and anesthesia.
A nurse is caring for a client who has just delivered a baby and is experiencing postpartum hemorrhage due to retained placental fragments.
Which of the following interventions should the nurse anticipate? Select all that apply:
Explanation
The correct answer is choices A, B, C, and E.These are all medications that can help contract the uterus and stop the bleeding caused by retained placental fragments.Oxytocin (Pitocin) is the most effective and commonly used uterotonic agent.Methylergonovine maleate (Methergine) and carboprost tromethamine (Hemabate) are alternative drugs that can be used if oxytocin is ineffective or unavailable.Misoprostol (Cytotec) is a prostaglandin analogue that can also help reduce blood loss.
Choice D is wrong because manual removal of placenta fragments is not an intervention that the nurse should anticipate.Manual removal of placenta fragments is a last resort option that can cause more bleeding and infection, and should only be performed by a skilled provider.
A nurse is caring for a client who has just delivered a baby and is experiencing postpartum hemorrhage due to lacerations on her cervix and vagina caused by rapid birth(Precipitous birth).
Which of the following interventions should be included in her plan of care? Select all that apply:
Explanation
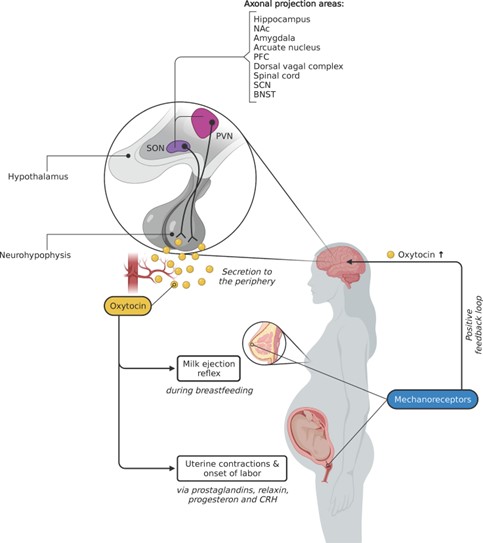
• Choice A: Administering oxytocin.Oxytocin is a uterotonic agent that stimulates uterine contractions and reduces bleeding from the placental site.It is the most effective intervention for preventing and treating postpartum hemorrhage.
• Choice B: Administering methylergonovine maleate.Methylergonovine maleate is another uterotonic agent that causes sustained uterine contraction and vasoconstriction.It can be used as an alternative or adjunct to oxytocin for postpartum hemorrhage.
• Choice C: Administering carboprost tromethamine.Carboprost tromethamine is a prostaglandin analog that induces strong and prolonged uterine contractions and decreases blood loss.
It can be used as a second-line treatment
Which of the following is the most common cause of postpartum hemorrhage?
Explanation
Uterine atony is the most common cause of postpartum hemorrhage, accounting for up to 80% of cases.It occurs when the uterus does not contract enough to stop the bleeding from the placental site.Uterine atony can be caused by factors such as prolonged labor, multiple pregnancy, large baby, infection or use of certain medications.
The other statements are wrong because:
• B.Retained placenta is the second most common cause of postpartum hemorrhage, but it only accounts for about 10% of cases.It occurs when part or all of the placenta remains attached to the uterine wall and prevents the uterus from contracting properly.
• C.Lacerations are tears or cuts in the cervix, vagina or perineum that can cause bleeding after delivery.They are usually minor and can be repaired with stitches, but they can also be severe and require surgery.Lacerations are not very common causes of postpartum hemorrhage, and they usually occur along with other factors such as uterine atony or retained placenta.
• D.Hematomas are collections of blood under the skin or in the tissues that can result from trauma during delivery.They can cause pain, swelling and pressure in the affected area, but they are usually small and resolve on their own.Hematomas are rare causes of postpartum hemorrhage, and they usually occur along with other factors such as lacerations or coagulation disorders.
Normal ranges for blood loss after delivery are less than 500 mL for vaginal birth and less than 1000 mL for cesarean birth.Blood loss greater than these amounts can indicate postpartum hemorrhage and require immediate medical attention.
Which of the following is a risk factor for postpartum hemorrhage?
Explanation
All of these conditions are risk factors for postpartum hemorrhage (PPH), which is severe bleeding after childbirth.
Choice A) Prolonged labor is a risk factor for PPH because it can cause uterine fatigue and atony, which is the inability of the uterus to contract and compress the blood vessels.
Choice B) Oligohydramnios is a risk factor for PPH because it can cause placental abruption, which is the premature separation of the
Which of the following is a nursing intervention for postpartum hemorrhage?
Explanation
Oxytocin is a uterotonic medication that stimulates uterine contractions and reduces bleeding.It is the most effective intervention for preventing and treating postpartum hemorrhage caused by uterine atony.
Uterine massage can also help to improve uterine tone and expel clots.
Choice B) Administering magnesium sulfate is wrong because magnesium sulfate is used to prevent seizures in patients with preeclampsia or eclampsia, not to control bleeding.
Choice C) Administering heparin is wrong because heparin is an anticoagulant that prevents blood clotting.
It is used to treat or prevent thromboembolic disorders, not to stop bleeding.
Choice D) Administering insulin is wrong because insulin is used to lower blood glucose levels in patients with diabetes mellitus, not to manage hemorrhage.
Normal blood loss after vaginal delivery is less than 500 mL and after cesarean delivery is less than 1000 mL.
Postpartum hemorrhage is defined as blood loss of at least 100
Which of the following laboratory tests should the nurse report to the obstetrician when monitoring a client who is one day postpartum and has experienced significant postpartum hemorrhage?
Explanation
Hemoglobin, which is an indicator of the number of RBCs and decreases during hypovolemia and hemorrhage.
Hemoglobin is a protein that carries oxygen in the blood and is measured in grams per deciliter (g/dL).
A normal range for hemoglobin is 12 to 16 g/dL for women.
A low hemoglobin level indicates anemia, which can be caused by blood loss or other factors.
A postpartum hemorrhage is a loss of more than 500 mL of blood after delivery, which can lead to hypovolemia (low blood volume) and shock.
Choice A is wrong because urine output 200 mL for the past 8 hours is within the normal range for a postpartum woman.
The kidneys may retain fluid during pregnancy and release it after delivery, resulting in increased urine output.
A normal urine output is 30 to 50 mL per hour.
Choice B is wrong because weight decrease of 2 pounds since delivery is expected for a postpartum woman.
The weight loss reflects the loss of fluid, blood, and placental tissue during delivery.
A normal weight loss after delivery is 10 to 12 pounds.
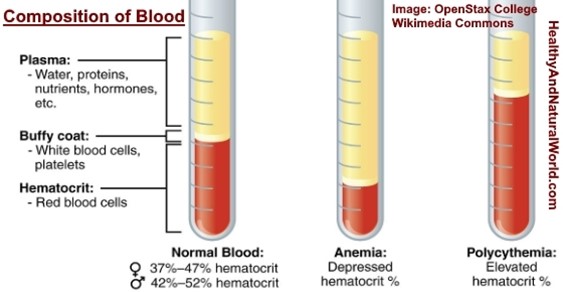
Choice D is wrong because hematocrit, which is the percent of RBCs in the total blood volume, and decreases during hypovolemia, may not reflect the true extent of blood loss in a postpartum hemorrhage.
Hematocrit is measured as a percentage and a normal range for hematocrit is 37 to 47% for women.
However, hematocrit may be falsely elevated due to hemoconcentration (increased concentration of blood cells) caused by fluid loss.
Hematocrit may take several days to reflect the actual blood loss.
Postpartum hemorrhage is classified into two groups: early postpartum hemorrhage and late postpartum hemorrhage.
What is the most common cause of early postpartum hemorrhage?
Explanation
Uterine atony is the most common cause of early postpartum hemorrhage, accounting for up to 80% of cases.Uterine atony is when the uterus fails to contract after delivery of the placenta, leading to excessive bleeding from the blood vessels where the placenta was attached.
Choice B is wrong because trauma is not the most common cause of early postpartum hemorrhage.Trauma accounts for about 20% of cases and includes uterine rupture, cervical and vaginal lacerations, and uterine inversion.
Choice C is wrong because lacerations are not the most common cause of early postpartum hemorrhage.Lacerations are a type of trauma that can cause bleeding from the cervix, vagina, or perineum.
Choice D is wrong because hematomas are not the most common cause of early postpartum hemorrhage.Hematomas are a type of trauma that can cause bleeding into the tissues of the vulva, vagina, or perineum.
Normal ranges for blood loss after delivery are less than 500 ml for vaginal delivery and less than 1000 ml for cesarean delivery.Postpartum hemorrhage is defined as blood loss greater than these amounts or when bleeding causes symptoms of hypovolemia (low blood volume) or hemodynamic instability (low blood pressure or high heart rate).
What is the most common cause of late postpartum hemorrhage?
Explanation
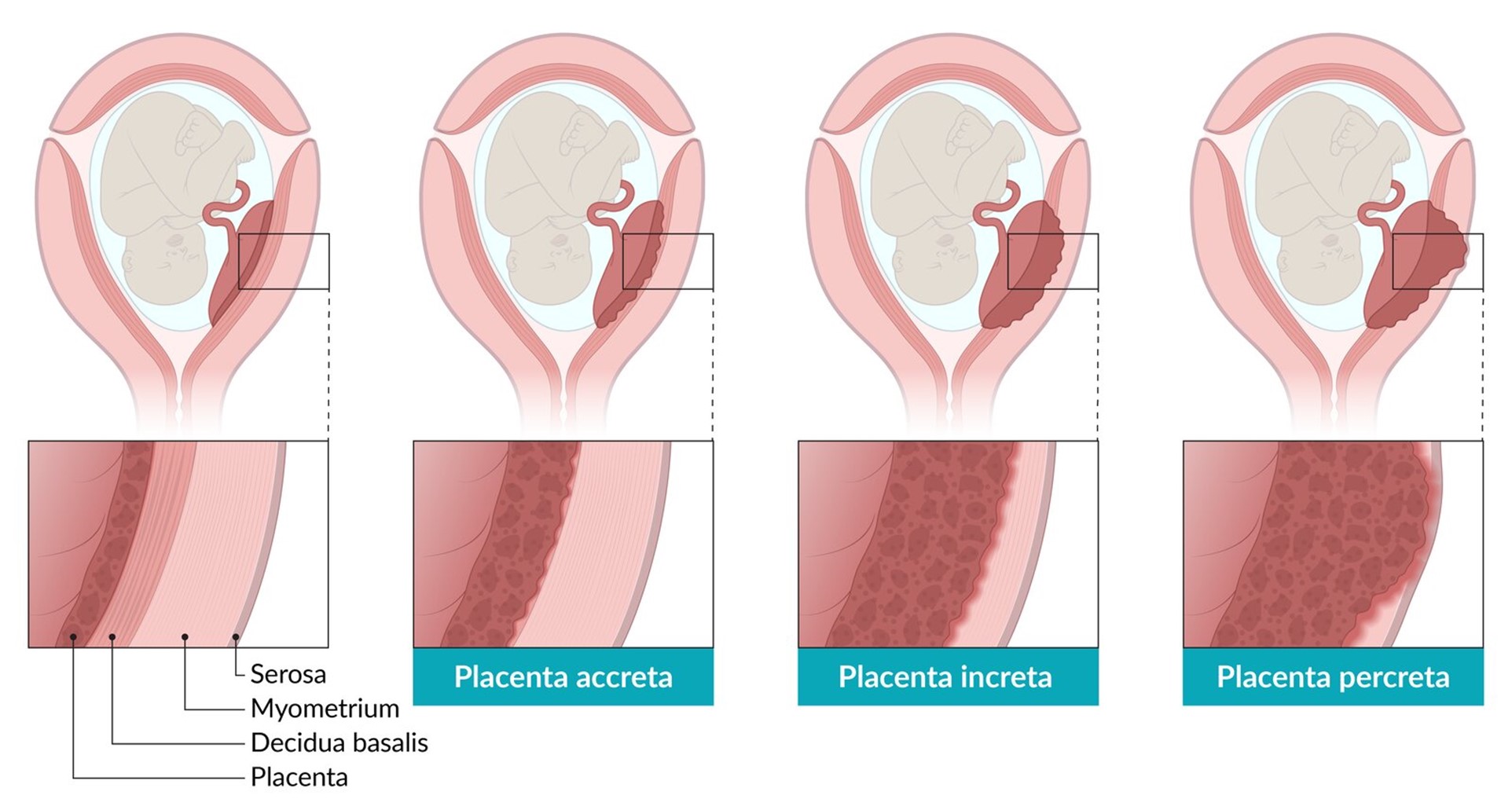
Retained placental fragments are the most common cause of late postpartum hemorrhage.Retained placental fragments can lead to infection and subinvolution of the placental site, which prevents the uterus from contracting and stopping the bleeding.
Choice B is wrong because uterine atony is the most common cause of early postpartum hemorrhage, not late postpartum hemorrhage.Uterine atony occurs when the uterus fails to contract after delivery.
Choice C is wrong because trauma is a rare cause of late postpartum hemorrhage.Trauma can occur during delivery and cause lacerations or hematomas that can bleed later, but this is uncommon.
Choice D is wrong because lacerations are also a rare cause of late postpartum hemorrhage.Lacerations can occur in the cervix, vagina or perineum during delivery and cause bleeding, but this usually happens immediately or within 24 hours after delivery.
A nurse is caring for a client who has just delivered her baby and is at risk for postpartum hemorrhage (PPH).
Which intervention should be included in this client’s plan of care?
Explanation
Oxytocin is a medication that helps the uterus contract and prevent excessive bleeding after birth.It is the most effective treatment for postpartum hemorrhage, even if already used for labor induction or augmentation or as part of active management of the third stage of labor.
Choice B) Encouraging frequent voiding is wrong because it does not directly affect the risk of postpartum hemorrhage.However, a full bladder can interfere with uterine contraction and cause bleeding, so voiding should be encouraged as part of routine care.
Choice C) Assessing vital signs every 4 hours is wrong because it is not enough to detect and treat postpartum hemorrhage early.Vital signs should be monitored more frequently in the first hour after delivery, when most cases of postpartum hemorrhage occur.
Choice D) Encouraging ambulation as soon as possible is wrong because it does not prevent postpartum hemorrhage.
Ambulation can help prevent thromboembolic complications and promote recovery, but it has no effect on uterine contraction
A nurse is caring for a client who has just delivered her baby and is at risk for PPH due to uterine atony.Which interventions should be included in this client’s plan of care? (Select all that apply)
Explanation
The correct answer is choice A and B. Administering oxytocin after delivery and encouraging frequent voiding are interventions that can help prevent or treat PPH due to uterine atony.Uterine atony is the most common cause of PPH and it occurs when the uterus fails to contract after birth, leading to excessive bleeding.Oxytocin is a medication that stimulates uterine contractions and reduces blood loss.Frequent voiding can help empty the bladder and allow the uterus to contract more effectively.
Choice C is wrong because assessing vital signs every 4 hours is not frequent enough for a client who is at risk for PPH.Vital signs should be monitored more closely to detect signs of hypovolemia and shock.
Choice D is wrong because encouraging ambulation as soon as possible can increase the risk of bleeding in a client who has uterine atony.Ambulation should be delayed until the uterus is firm and the bleeding is controlled.
Choice E is wrong because massaging the fundus is not an intervention for PPH due to uterine atony, but rather for PPH due to retained placental fragments.Massaging the fundus can help expel any remaining tissue from the uterus and prevent infection.
A nurse is caring for a client who has just delivered her baby and is at risk for PPH due to retained placental fragments.
Which interventions should be included in this client’s plan of care? (Select all that apply.)
Explanation
The correct answer is choice A and B.Administering oxytocin after delivery is an effective way to prevent and treat uterine atony, which is the most common cause of PPH.Encouraging frequent voiding can help reduce bladder distension, which can interfere with uterine contraction and increase bleeding.
Choice C is wrong because assessing vital signs every 4 hours is not frequent enough for a client who is at risk for PPH.Vital signs should be monitored every 15 minutes for the first hour, then every hour for the next 4 hours, and then every 4 hours thereafter.
Choice D is wrong because encouraging ambulation as soon as possible can increase the risk of bleeding and shock in a client who has retained placental fragments.Ambulation should be delayed until the fragments are removed and the bleeding is controlled.
A nurse is caring for a client who has postpartum hemorrhage and is receiving IV fluids and blood products.
Which of the following interventions should the nurse include in the plan of care? (Select all that apply.)
Explanation
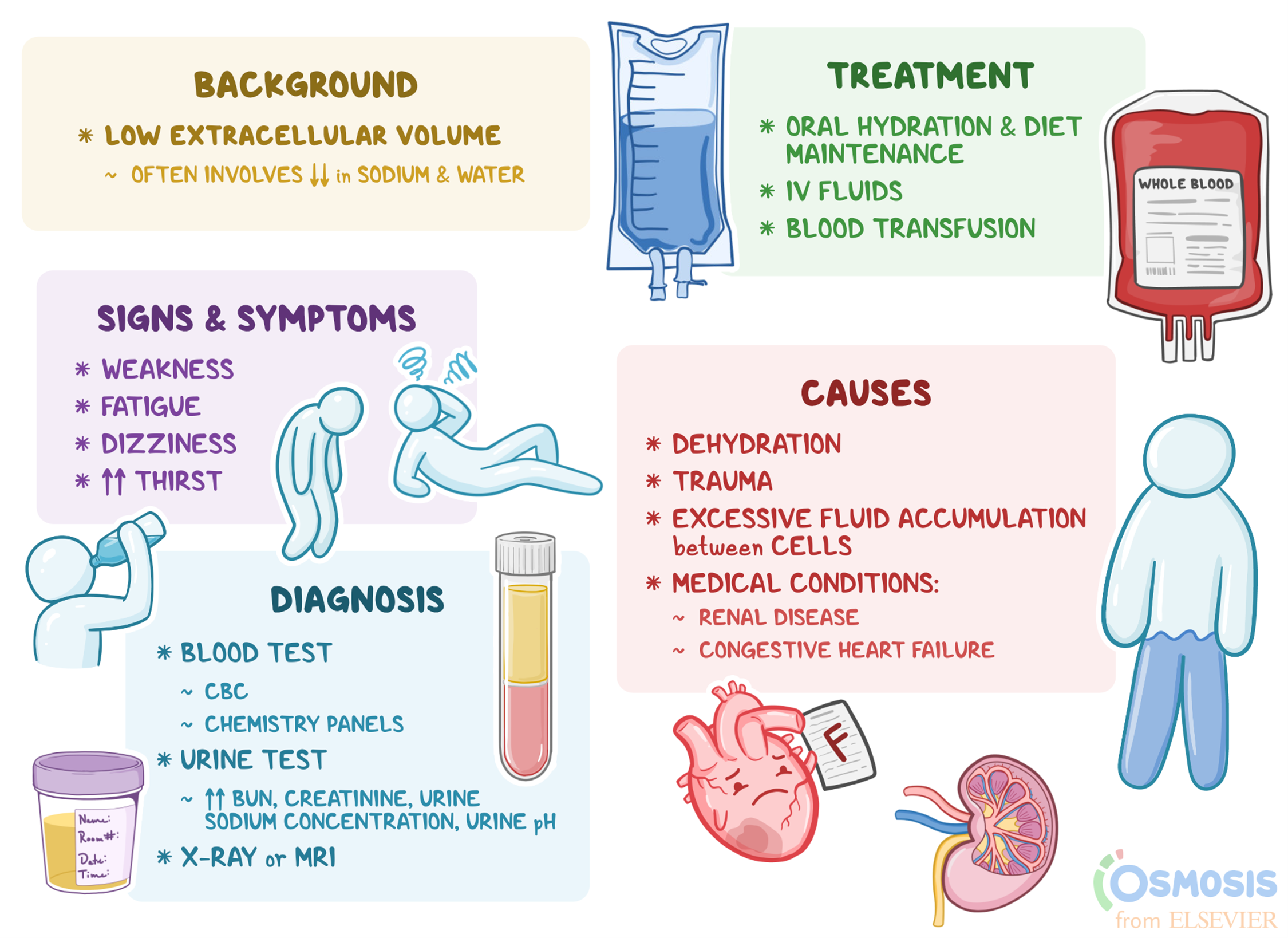
The correct answer is choice A, B and C. The nurse should monitor intake and output to assess the client’s fluid status and blood loss.
The nurse should elevate the head of the bed to reduce the risk of hypovolemic shock and improve tissue perfusion.
The nurse should apply oxygen via nasal cannula to increase oxygen delivery to the vital organs and prevent hypoxia.
Choice D is wrong because inserting a nasogastric tube is not indicated for a client who has postpartum hemorrhage.
A nasogastric tube is used to decompress the stomach or administer medications or feedings in some conditions.
Choice E is wrong because administering pain medication as needed is not a priority intervention for a client who has postpartum hemorrhage.
Pain medication can mask the signs of shock and lower the blood pressure further.
The nurse should focus on restoring the blood volume and preventing complications.
A nurse is evaluating the effectiveness of interventions for a client who has postpartum hemorrhage due to retained placental fragments.
Which of the following outcomes indicates that the interventions are successful?
Explanation
The client has a firm and midline uterus at the umbilicus.This indicates that the interventions for postpartum hemorrhage due to retained placental fragments are successful because the uterus has contracted and expelled the fragments, and there is no excessive bleeding.
Choice A is wrong because minimal cramping and discomfort are not specific signs of successful interventions for postpartum hemorrhage.
They may also occur in normal postpartum recovery.
Choice C is wrong because passing small clots with moderate lochia rubra may indicate that there are still some retained placental fragments or that the uterus is not contracting adequately.
Choice D is wrong because a pulse rate of 100 beats/min and a blood pressure of 110/70 mm Hg are not normal ranges for an adult.A pulse rate of 60 to 100 beats/min and a blood pressure of less than 120/80 mm Hg are considered normal.A high pulse rate and a low blood pressure may indicate hypovolemia or shock due to blood loss.
A nurse is providing discharge instructions to a client who had postpartum hemorrhage and received blood transfusions during her hospital stay.
Which of the following information should the nurse include in the teaching? (Select all that apply)
Explanation
The correct answer is choice B, D and E. The nurse should include the following information in the teaching:
• Increase iron-rich foods in the diet.This can help replenish the blood loss and prevent anemia.
• Report any signs of infection, such as fever or foul-smelling lochia.These can indicate a serious complication that needs immediate medical attention.
• Resume sexual intercourse as soon as desired.There is no evidence that sexual activity increases the risk of bleeding or infection after postpartum hemorrhage.
Choice A is wrong because increasing fluid intake to at least 3 L per day is not necessary for postpartum hemorrhage recovery.Fluid intake should be based on thirst and urine output.
Choice C is wrong because avoiding strenuous activities for 6 weeks is not a specific recommendation for postpartum hemorrhage.The nurse should advise the client to gradually resume normal activities as tolerated and to rest when needed.
A nurse is caring for a client who delivered vaginally 4 hours ago and has a boggy uterus that is displaced to the right of midline.
Which of the following actions should the nurse take first?
Explanation
This is because a boggy uterus that is displaced to the right of midline indicates that the bladder is full and pushing the uterus out of place.A full bladder can prevent the uterus from contracting effectively after delivery, leading to excessive bleeding and postpartum hemorrhage (PPH).
Emptying the bladder can help the uterus return to its normal position and tone.
Choice A is wrong because applying ice packs to the perineum may help reduce swelling and pain, but it will not address the underlying cause of the boggy uterus.
Choice C is wrong because increasing the rate of IV fluids may worsen the bleeding by diluting the blood and reducing its clotting ability.
Choice D is wrong because administering carboprost, a medication that stimulates uterine contractions, may be indicated if other measures fail to restore uterine tone, but it is not the first action to take.Carboprost also has side effects such as fever, nausea, vomiting, and diarrhea.
Normal ranges for uterine size and position after delivery are:
• Immediately after delivery: at or slightly below the level of the umbilicus (navel)
• 6 hours after delivery: 1 fingerbreadth above the umbilicus
• 12 hours
A nurse is assessing a client who had a cesarean birth and is experiencing postpartum hemorrhage due to uterine dehiscence.
Which of the following manifestations should alert the nurse to this complication?
Explanation
Heavy vaginal bleeding and clots are symptoms of postpartum hemorrhage due to uterine dehiscence.Uterine dehiscence is the opening of the incision line after cesarean section and it is a rare complication.It can be caused by infection, hematoma, suture technique or trauma.
Choice A is wrong because abdominal pain and tenderness are more likely to be caused by other postpartum complications such as endometritis, wound infection, hematoma or uterine rupture.
Choice B is wrong because foul-smelling lochia and fever are signs of postpartum infection such as endometritis or wound abscess.
Choice C is wrong because absent or decreased bowel sounds and distension are not specific to postpartum hemorrhage.They can be caused by ileus, bowel obstruction, peritonitis or other abdominal disorders.
Normal ranges for blood loss after delivery are less than 500 mL for vaginal delivery and less than 1000 mL for cesarean delivery.Normal ranges for vital signs after delivery are pulse 50 to 90 beats/minute, blood pressure 85/60 to 140/90 mm Hg, respiratory rate 12 to 20 breaths/minute and temperature 36.2 to 37.6 °C.
A nurse is providing discharge instructions to a client who had postpartum hemorrhage due to placenta accreta and underwent hysterectomy.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
“I will seek counseling if I have feelings of grief or loss.” This statement indicates that the client understands the potential psychological impact of having a hysterectomy due to postpartum hemorrhage and placenta accreta, which is a condition where the placenta invades the uterine wall and causes severe bleeding.The client may experience emotional distress, such as sadness, anger, guilt, or anxiety, due to the loss of fertility and the traumatic event.
Seeking counseling can help the client cope with these feelings and adjust to the changes in her life.
Choice A is wrong because iron supplements are not necessary for at least 6 months after a hysterectomy.Iron supplements are usually prescribed for anemia caused by blood loss, but the duration of treatment depends on the severity of the anemia and the client’s response to therapy.
The client should have regular blood tests to monitor her hemoglobin and iron levels and follow the advice of her health care provider regarding iron supplementation.
Choice B is wrong because avoiding lifting anything heavier than the baby for 2 weeks is not enough to prevent complications after a hysterectomy.
A hyster ...
A nurse is caring for a client who delivered vaginally 4 hours ago and has saturated two perineal pads in 15 minutes.
The nurse identifies this as which of the following types of postpartum hemorrhage?
Explanation
Early postpartum hemorrhage occurs within the first 24 hours after delivery.The client has saturated two perineal pads in 15 minutes, which indicates severe bleeding and a possible complication of the third stage of labor.
Choice B is wrong because late postpartum hemorrhage occurs 24 hours to 12 weeks postpartum.This type of hemorrhage is usually caused by retained placental fragments or infection.
Choice C is wrong because chronic postpartum hemorrhage is not a recognized term.
Postpartum hemorrhage is an acute condition that requires immediate attention.
Choice D is wrong because acute postpartum hemorrhage is not a specific type of hemorrhage, but a general term for any excessive bleeding after childbirth.Postpartum hemorrhage can be classified into mild, moderate, or severe based on the amount of blood loss.
A nurse is preparing to administer methylergonovine to a client who has a postpartum hemorrhage due to uterine atony.
Which of the following assessments should the nurse perform prior to administration?
Explanation
The nurse should assess the client’s blood pressure before administering methylergonovine because this medication can cause hypertension and vasoconstriction.The nurse should also monitor the client’s blood pressure after administration for any signs of hypertensive crisis.
Choice B.Temperature is wrong because methylergonovine does not affect the body temperature significantly.
However, the nurse should monitor the client’s temperature for any signs of infection or fever.
Choice C.Respiratory rate is wrong because methylergonovine does not affect the respiratory system significantly.
However, the nurse should monitor the client’s respiratory rate for any signs of distress or hypoxia.
Choice D.Oxygen saturation is wrong because methylergonovine does not affect the oxygen saturation significantly.
However, the nurse should monitor the client’s oxygen saturation for any signs of hypoxemia or cyanosis.
Methylergonovine is a uterine stimulant that helps prevent postpartum hemorrh
A nurse is evaluating a client who had a postpartum hemorrhage and received fluid resuscitation and blood transfusion therapy.
Which of the following findings indicates an improvement in the client’s condition?
Explanation
Urine output of 40 mL/hr indicates an improvement in the client’s condition.According to the MSF Medical Guidelines, the objective of resuscitation in postpartum hemorrhage is to maintain a urine output of at least 30 mL/hour.
A urine output of 40 mL/hr suggests that the client has adequate fluid replacement and blood transfusion therapy.
Choice B is wrong because a pulse rate of 110 beats/min is still high and indicates tachycardia.
Tachycardia is a sign of hypovolemia and shock due to blood loss.The normal pulse rate for an adult is 60 to 100 beats/min.
Choice C is wrong because a hematocrit level of 32% is low and indicates anemia.
Anemia is a complication of postpartum hemorrhage due to reduced red blood cell count.The normal hematocrit level for women is 36% to 48%.
Choice D is wrong because a blood pressure of 90/60 mm Hg is low and indicates hypotension.
Hypotension is a sign of hypovolemia and shock due to blood loss.The normal blood pressure for an adult is 120/80 mm Hg.
Introduction
A nurse is caring for a client who had a vaginal delivery 4 hours ago.
The nurse notes that the client’s fundus is boggy, deviated to the right, and above the umbilicus.
The client’s perineal pad is saturated with blood.
What is the most likely cause of this client’s postpartum hemorrhage?
Explanation
This is when the uterus does not contract enough to stop the bleeding from the placental site after delivery.It is the most common cause of postpartum hemorrhage.A boggy, deviated and above the umbilicus fundus indicates uterine atony.
Choice B. Retained placenta is wrong because it occurs when some or all of the placenta remains in the uterus after delivery.It can also cause postpartum hemorrhage, but it usually presents with a firm fundus and a continuous trickle of blood.
Choice C. Uterine inversion is wrong because it is a rare condition where the uterus turns inside out after delivery.It can also cause postpartum hemorrhage, but it usually presents with severe pain, shock and a palpable mass at the introitus.
Choice D. Cervical laceration is wrong because it is a tear in the cervix that can occur during delivery.It can also cause postpartum hemorrhage, but it usually presents with a firm fundus and bright red bleeding that does not respond to uterine massage.
A nurse is administering oxytocin to a client who had a cesarean delivery and has uterine atony.
What is the primary purpose of this medication in this situation?
Explanation
Oxytocin is a hormone that causes the uterine muscles to contract and compress the blood vessels that connect the uterus to the placenta.This helps prevent excessive bleeding after delivery, especially in cases of uterine atony, which is the failure of the uterus to contract sufficiently.
Choice B is wrong because oxytocin does not have any direct effect on infection or wound healing.
Choice C is wrong because oxytocin does not enhance milk production, although it does facilitate milk ejection during breastfeeding.Choice D is wrong because oxytocin does not relieve pain or discomfort from uterine cramping, but rather causes it by stimulating contractions.
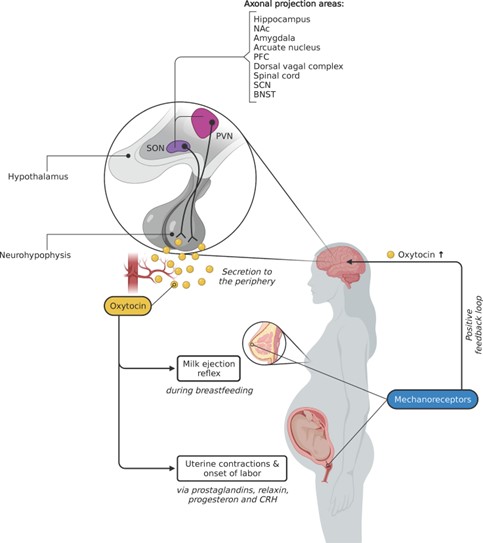
A nurse is assessing a client who had a prolonged labor and vacuum-assisted birth.
The nurse observes a large, tense, bluish bulge on the client’s perineum.
The client reports severe pain in the area.
What is the most likely diagnosis for this client?
Explanation
Perineal hematoma.A perineal hematoma is a collection of blood in the soft tissues of the perineum that can result from trauma during delivery, such as vacuum-assisted birth.The client may present with a large, tense, bluish bulge on the perineum and severe pain in the area.
Choice B. Vulvar varicosity is wrong because it is a condition where the veins in the vulva become enlarged and swollen due to increased blood flow and pressure during pregnancy.It usually appears as bluish or purple veins on the vulva and may cause discomfort, itching, or heaviness in the area.
It is not related to vacuum-assisted birth or prolonged labor.
Choice C. Rectocele is wrong because it is a condition where the rectum bulges into the vagina due to weakening of the pelvic floor muscles and connective tissue.
It may cause symptoms such as difficulty with bowel movements, a feeling of pressure or fullness in the vagina, or sexual dysfunction.
It is not related to vacuum-assisted birth or prolonged labor.
Choice D. Episiotomy is wrong because it is a surgical incision made in the perineum to enlarge the vaginal opening during delivery.
It may be done to facilitate delivery, prevent severe tearing, or protect the baby’s head from trauma.
It is not a diagnosis but a procedure that may be performed during vacuum-assisted birth or normal vaginal delivery.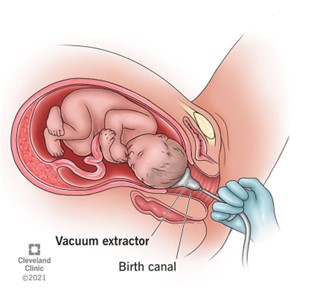
A nurse is reviewing the laboratory results of a client who had a postpartum hemorrhage due to placenta accreta.
The nurse notes that the client’s platelet count is 80,000/mm3, fibrinogen level is 150 mg/dL, and prothrombin time is 18 seconds.
What is the most appropriate interpretation of these findings?
Explanation
The client has severe coagulation impairment.
This is because the client’s platelet count, fibrinogen level, and prothrombin time are all significantly abnormal compared to the normal ranges.
• The normal platelet count is 150,000 to 450,000/mm3.
A platelet count of 80,000/mm3 indicates thrombocytopenia, which is a low number of platelets that can impair clotting and cause bleeding.
• The normal fibrinogen level is 200 to 400 mg/dL.
A fibrinogen level of 150 mg/dL indicates hypofibrinogenemia, which is a low level of fibrinogen that can impair clotting and cause bleeding.
• The normal prothrombin time is 11 to 13.5 seconds.
A prothrombin time of 18 seconds indicates a prolonged clotting time that can impair clotting and cause bleeding.
Choice A is wrong because the client does not have normal coagulation parameters.
All three tests are abnormal and indicate a severe coagulation impairment.
Choice B is wrong because the client does not have mild coagulation impairment.
The degree of abnormality in the test results is too high to be considered mild.
Choice C is wrong because the client does not have moderate coagulation impairment.
The degree of abnormality in the test results is too high to be considered moderate.
A nurse is preparing to discharge a client who had a postpartum hemorrhage due to uterine atony.
Which of the following instructions should the nurse include in the teaching? (Select all that apply)
Explanation
These are the instructions that the nurse should include in the teaching for a client who had a postpartum hemorrhage due to uterine atony.
• Choice A is correct because foul-smelling lochia or fever can indicate an infection of the uterus or other reproductive organs, which can worsen bleeding and cause complications.
• Choice B is correct because iron intake and supplements can help replenish the blood loss and prevent anemia.
• Choice C is correct because sexual intercourse can cause trauma to the healing tissues and increase the risk of infection and bleeding.The lochia usually stops within four to six weeks after delivery.
• Choice D is wrong because limiting fluid intake can cause dehydration and impair blood circulation and clotting.The client should drink plenty of fluids to stay hydrated and promote healing.
• Choice E is correct because pelvic floor exercises can help strengthen the muscles that support the uterus and bladder, and prevent prolapse and urinary incontinence.
Uterine atony is a condition where the uterus does not contract enough after delivery, which can lead to excessive bleeding or postpartum hemorrhage.It is the most common cause of postpartum hemorrhage, accounting for up to 80% of cases.It can be caused by several factors, such as multiple pregnancy, large baby, prolonged or rapid labor, obesity, uterine fibroids, or medications that affect uterine contractions.It requires immediate medical treatment to stop the bleeding and prevent shock and organ failure.
A nurse is caring for a client who has experienced postpartum hemorrhage due to uterine atony.
Which of the following medications should the nurse anticipate administering?
Explanation
Oxytocin is the most effective medication for preventing and treating postpartum hemorrhage caused by uterine atony, which is the failure of the uterus to contract after delivery.Oxytocin stimulates uterine contractions and reduces bleeding.
Choice A is wrong because methylergonovine maleate (Methergine) is a second-line uterotonic drug that can cause hypertension and should not be used in women with high blood pressure.
Choice B is wrong because magnesium sulfate (MgSO4) is used to prevent seizures in women with preeclampsia or eclampsia, not to treat postpartum hemorrhage.
Choice D is wrong because carboprost tromethamine (Hemabate) is another second-line uterotonic drug that can cause severe diarrhea and bronchospasm and should not be used in women with asthma.
Risk factors
A nurse is caring for a client who is 1 day postpartum (PP) and is being monitored carefully after a significant postpartum hemorrhage.
Which of the following should the nurse report to the obstetrician?
Explanation
This is because a normal urine output in the postpartum period ranges from1.03 to 1.40 cc/kg/hror500 to 1000 mLper void.A urine output of 200 mL for the past 8 hours is much lower than the normal range and indicatesoliguria, which can be a sign ofhypovolemia,renal failure, orurinary retentiondue to postpartum hemorrhage.
Choice B is wrong because a weight decrease of 2 pounds since delivery is normal and expected due to the loss of blood, amniotic fluid, and placenta.
Choice C is wrong because a blood pressure of 110/70 mm Hg is within the normal range and does not indicate hypotension or hypertension.
Choice D is wrong because a hemoglobin level of 12 g/dL is also within the normal range and does not indicate anemia or polycythemia.
A nurse is caring for a client who has just delivered a baby and is at risk for postpartum hemorrhage.
Which of the following interventions should the nurse include in the plan of care?
Explanation
Administering oxytocin (Pitocin) after delivery is the most effective intervention to prevent postpartum hemorrhage caused by uterine atony.Oxytocin is a uterotonic agent that stimulates uterine contractions and reduces bleeding.
Choice B is wrong because encouraging the client to ambulate as soon as possible may increase the risk of bleeding and shock if the client has uterine atony or lacerations.
Choice C is wrong because encouraging the client to drink fluids only when thirsty may lead to dehydration and hypovolemia, which can worsen the effects of hemorrhage.
Choice D is wrong because administering magnesium sulfate (MgSO4) during labor is used to prevent seizures in clients with preeclampsia or eclampsia, not to prevent postpartum hemorrhage.Magnesium sulfate may also cause uterine relaxation and increase bleeding.
A client who has just delivered a baby is at risk for postpartum hemorrhage due to uterine atony.
Which of the following interventions should the nurse include in the plan of care?
Explanation
Oxytocin is a hormone that stimulates uterine contractions and helps prevent postpartum hemorrhage due to uterine atony.Uterine atony is the most common cause of postpartum hemorrhage, and it occurs when the uterus does not contract enough to stop the bleeding from the placental site.
Choice A is wrong because encouraging frequent voiding does not directly affect uterine contractions.However, it can help reduce bladder distension, which can interfere with uterine contraction and cause bleeding.
Choice B is wrong because magnesium sulfate (MgSO4) is used to prevent seizures in preeclampsia and eclampsia, not to prevent postpartum hemorrhage.In fact, magnesium sulfate can cause uterine relaxation and increase the risk of bleeding.
Choice C is wrong because encouraging early ambulation does not prevent postpartum hemorrhage due to uterine atony.Early ambulation can help prevent thromboembolic complications, such as deep vein thrombosis and pulmonary embolism, but it does not affect uterine contractions.
A nurse is caring for a client who has just delivered a baby and is at risk for postpartum hemorrhage.
Which of the following findings should alert the nurse to the possibility of hemorrhage?
Explanation
This is a sign of hypovolemia (low blood volume) due to excessive blood loss.A normal urine output is at least 60 mL/hour for an adult.
Choice A is wrong because a blood pressure of 130/80 mm Hg is within the normal range for an adult.
A low blood pressure would indicate postpartum hemorrhage.
Choice C is wrong because a fundus that is firm and midline indicates that the uterus is contracting well and preventing bleeding.A soft or boggy fundus would indicate uterine atony, the most common cause of postpartum hemorrhage.
Choice D is wrong because lochia rubra with small clots is normal for the first few days after delivery.
Large clots or excessive bleeding would indicate postpartum hemorrhage.
Signs and symptoms
What is the amount of heavy vaginal bleeding in normal delivery that may indicate postpartum hemorrhage?
Explanation
Heavy vaginal bleeding in normal delivery that may indicate postpartum hemorrhage is more than 500 mL.
Postpartum hemorrhage (PPH) is a serious condition that can lead to death if not treated promptly.It is caused by the uterus not contracting properly or by retained placenta fragments or damage to the reproductive organs.
Choice B is wrong because more than 1000 mL of blood loss is the definition of PPH after a cesarean delivery, not a vaginal delivery.
Choice C is wrong because less than 500 mL of blood loss is normal after a vaginal delivery and does not indicate PPH.
Choice D is wrong because less than 1000 mL of blood loss is normal after a cesarean delivery and does not indicate PPH.
What is the amount of heavy vaginal bleeding in cesarean delivery that may indicate postpartum hemorrhage?
Explanation
Heavy vaginal bleeding in cesarean delivery that may indicate postpartum hemorrhage is more than 500 mL.
Postpartum hemorrhage (PPH) is severe bleeding and loss of blood after childbirth.It’s a serious and dangerous condition that can lead to death.
Choice B is wrong because more than 1000 mL of blood loss is too high for the definition of PPH after cesarean delivery.
Choice C is wrong because less than 500 mL of blood loss is normal after cesarean delivery.
Choice D is wrong because less than 1000 mL of blood loss is not considered heavy bleeding after cesarean delivery.
What may indicate internal bleeding in postpartum hemorrhage?
Explanation
relaxed uterus may indicate internal bleeding in postpartum hemorrhage.This is because the uterus is not contracting properly to compress the blood vessels where the placenta was attached, leading to excessive blood loss.A relaxed uterus is also known as uterine atony, which is the most common cause of postpartum hemorrhage.
Choice A is wrong because a tense and rigid uterus may indicate retained placenta or uterine clot, which are other causes of postpartum hemorrhage.
These conditions prevent the uterus from contracting fully and expelling the placental fragments or clots.
Choice C is wrong because a soft uterus is similar to a relaxed uterus and may also indicate internal bleeding in postpartum hemorrhage.
Choice D is wrong because a normal uterus is not a sign of postpartum hemorrhage.A normal uterus should be firm and contracted after delivery to prevent excessive bleeding.
Normal ranges for blood loss after delivery are less than 500 mL for vaginal delivery and less than 1000 mL for cesarean delivery.Postpartum hemorrhage is defined as blood loss of more than these amounts or blood loss accompanied by signs of hypovolemia within 24 hours of delivery.
What is the specific gravity of concentrated urine in postpartum hemorrhage?
Explanation
The specific gravity of urine is a measure of the concentration of solutes in urine.
It reflects the ability of the kidneys to regulate water balance and excrete waste products.The normal range for urine specific gravity is1.005 to 1.030.
In postpartum hemorrhage, there is a loss of blood volume that leads to decreased blood pressure and reduced perfusion of the kidneys.The kidneys respond by conserving water and producing concentrated urine with a high specific gravity, usuallygreater than 1.030.
ChoiceBis wrong because a urine specific gravity lower than 1.030 indicates a dilute urine that is not consistent with postpartum hemorrhage.
ChoiceCis wrong because a urine specific gravity greater than 1.020 is still within the normal range and does not reflect the degree of water conservation that occurs in postpartum hemorrhage.
ChoiceDis wrong because a urine specific gravity lower than 1.020 indicates a very dilute urine that suggests excessive fluid intake, diabetes insipidus, or kidney failure.
These conditions are not associated with postpartum hemorrhage.
What is the decrease in red blood cell count that may indicate postpartum hemorrhage?
Explanation
Hematocrit is the percentage of red blood cells in the blood.
A decrease in hematocrit indicates blood loss or anemia.Postpartum hemorrhage (PPH) is defined as blood loss of ≥ 500–1000 ml within 24 hours after delivery.PPH can cause a significant drop in hematocrit and hemoglobin levels, which can lead to hypovolemia and shock.A normal hematocrit range for women is 36% to 48%.
Therefore, a hematocrit level below 30% may indicate PPH.
Choice B. Hematocrit > 30% is wrong because it does not indicate a decrease in red blood cell count or blood loss.A hematocrit level above 30% may be normal or indicate dehydration, polycythemia, or other conditions.
Choice C.Hematocrit < 40% is wrong because it is within the normal range for women and does not indicate a significant decrease in red blood cell count or blood loss.
Choice D. Hematocrit > 40% is wrong because it does not indicate a decrease in red blood cell count or blood loss.
A hematocrit level above 40% may be normal or indicate dehydration
Medical interventions
A nurse is caring for a client who is experiencing postpartum hemorrhage.
Which medication should the nurse anticipate administering to promote sustained uterine contractions?
Explanation
Carboprost tromethamine (Hemabate) is a medication that should be anticipated for a client who is experiencing postpartum hemorrhage.It is a synthetic prostaglandin that stimulates strong and sustained uterine contractions and reduces bleeding.
Choice A is wrong because Pitocin is a uterotonic medication that is used to prevent postpartum hemorrhage by inducing contractions between delivery of the baby and the placenta.
It is not as effective as carboprost for treating severe bleeding.
Choice C is wrong because Methylergonovine maleate (Methergine) is another uterotonic medication that causes sustained uterine contractions and vasoconstriction.
However, it is contraindicated in patients with hypertension, which is a common complication of pregnancy.
Choice D is wrong because Misoprostol (Cytotec) is a synthetic prostaglandin that can be used to prevent or treat postpartum hemorrhage by causing uterine contractions.However, it is less effective than carboprost and has more side effects such as fever, diarrhea and shivering.
A nurse is caring for a client who is experiencing postpartum hemorrhage.
Which medication should the nurse anticipate administering to enhance uterine tone?
Explanation
Carboprost tromethamine (Hemabate) is a prostaglandin that stimulates uterine contractions and reduces bleeding.It is used when other uterotonic medications such as oxytocin (Pitocin) or methylergonovine maleate (Methergine) are ineffective or contraindicated.
Choice A is wrong because oxytocin is the first-line drug for preventing and treating postpartum hemorrhage due to uterine atony, but it may not be enough to enhance uterine tone in some cases.
Choice C is wrong because methylergonovine maleate is an ergot alkaloid that causes sustained uterine contractions, but it has more side effects and contraindications than oxytocin, such as hypertension, nausea, vomiting and headache.
Choice D is wrong because misoprostol (Cytotec) is a synthetic prostaglandin E1 analogue that can be used orally, sublingually, rectally or vaginally to induce uterine contractions, but it is less effective and has more adverse effects than oxytocin or carboprost tromethamine.
A nurse is caring for a client who is experiencing postpartum hemorrhage.
Which medication should the nurse anticipate administering to inhibit fibrinolysis and reduce blood loss?
Explanation
Tranexamic acid (TXA) is a medication that inhibits fibrinolysis and reduces blood loss in postpartum hemorrhage.According to a practice guideline from the International Federation of Gynecology and Obstetrics (FIGO), tranexamic acid given within three hours of vaginal delivery after 500 mL of blood loss reduces mortality by up to 30%.
Choice A is wrong because pitocin (oxytocin) is a medication that stimulates uterine contractions and is used to prevent or treat uterine atony, which is the most common cause of postpartum hemorrhage.
However, it does not inhibit fibrinolysis.
Choice B is wrong because carboprost tromethamine (Hemabate) is a prostaglandin that also stimulates uterine contractions and is used to treat postpartum hemorrhage due to uterine atony.
However, it does not inhibit fibrinolysis.
Choice C is wrong because methylergonovine maleate (Methergine) is an ergot alkaloid that also stimulates uterine contractions and is used to treat postpartum hemorrhage due to uterine atony.
However, it does not inhibit fibrinolysis.
Choice D is wrong because misoprostol (Cytotec) is another prostaglandin that also stimulates uterine contractions and is used to prevent or treat postpartum hemorrhage due to uterine atony.
However, it does not inhibit fibrinolysis.
Normal ranges for blood loss after vaginal delivery are ...
A nurse is caring for a client who is experiencing postpartum hemorrhage.
Which medication should the nurse anticipate administering to induce uterine contractions?
Explanation
Carboprost tromethamine (Hemabate) is a prostaglandin that stimulates uterine contractions and reduces bleeding.It is used for postpartum hemorrhage when other medications such as oxytocin (Pitocin) are ineffective or contraindicated.
Choice A is wrong because oxytocin is the first-line medication for preventing and treating postpartum hemorrhage due to uterine atony, but it may not be effective in some cases.
Choice C is wrong because methylergonovine maleate (Methergine) is an ergot alkaloid that also induces uterine contractions, but it has more side effects and contraindications than prostaglandins.
Choice D is wrong because misoprostol (Cytotec) is another prostaglandin that can be used for postpartum hemorrhage, but it is less effective and has more adverse effects than carboprost tromethamine.
A nurse is caring for a client who is experiencing postpartum hemorrhage and has lost blood volume and clotting factors.
Which medication should the nurse anticipate administering to replace blood volume and clotting factors?
Explanation
Blood products (packed red blood cells, fresh frozen plasma, platelets).Blood products are used to replace blood volume and clotting factors in patients with postpartum hemorrhage who have lost a significant amount of blood and are at risk of hypovolemic shock and coagulopathy.
Choice A is wrong because Pitocin (oxytocin) is a uterotonic medication that stimulates uterine contractions and reduces bleeding from uterine atony, which is the most common cause of postpartum hemorrhage.
However, it does not directly replace blood volume or clotting factors.
Choice B is wrong because Hemabate (carboprost tromethamine) is another uterotonic medication that can be used to treat postpartum hemorrhage caused by uterine atony, especially if oxytocin is ineffective or contraindicated.
However, it also does not directly replace blood volume or clotting factors.
Choice C is wrong because Methergine (methylergonovine maleate) is a third uterotonic medication that can be used to treat postpartum hemorrhage caused by uterine atony, especially if oxytocin and carboprost are ineffective or contraindicated.
However, it also does not directly replace blood volume or clotting factors.
Choice ...
Surgical Management
A nurse is caring for a client who is experiencing postpartum hemorrhage.
Which of the following surgical management should the nurse expect to be performed on the client?
Explanation
Uterine artery embolization to block blood flow to the uterus.This is a minimally invasive procedure that involves injecting small particles into the uterine arteries to occlude them and stop the bleeding.It is an effective and fertility-preserving option for postpartum hemorrhage that does not respond to medical management.
ChoiceA.
Manual removal of placenta or retained fragments under anesthesiais wrong because it is not a surgical management, but a manual one.It is usually done before resorting to surgery, and it may not be sufficient to control the bleeding if there is uterine atony or lacerations.
ChoiceB.
Repair of lacerations or hematomas under anesthesiais wrong because it is not a surgical management for postpartum hemorrhage, but a surgical repair of the injuries that may have caused the bleeding.
It may be necessary to perform this repair, but it does not address the underlying cause of hemorrhage, such as uterine atony or placental abnormalities
A nurse is caring for a client who is experiencing postpartum hemorrhage.
Which of the following surgical management should the nurse expect to be performed on the client as a last resort?
Explanation
Hysterectomy to remove the uterus.This is because hysterectomy is the last resort for surgical management of postpartum hemorrhage when all other methods have failed or are contraindicated.Hysterectomy is the definitive treatment for uncontrollable bleeding from the uterus.
Choice A. Manual removal of placenta or retained fragments under anesthesia is wrong because this is not a surgical procedure but a manual one.It is done to remove any retained products of conception that may cause bleeding or infection.
Choice B. Repair of lacerations or hematomas under anesthesia is wrong because this is not a surgical procedure but a repair one.It is done to stop bleeding from any tears or bruises in the genital tract that may occur during delivery.
Choice C. Uterine tamponade with balloon catheter or gauze packing to compress bleeding vessels is wrong because this is not a surgical procedure but a minimally invasive one.It is done to apply pressure inside the uterine cavity to stop bleeding from the placental site or uterine atony.
Choice D. B-Lynch suture to compress the uterus with stitches is wrong because this is not a last resort but a conservative surgical procedure.
A nurse is caring for a client who is experiencing postpartum hemorrhage.
Which of the following surgical management should the nurse expect to be performed on the client if she has uterine atony?
Explanation
Uterine tamponade with balloon catheter or gauze packing to compress bleeding vessels is a surgical management that can be used for postpartum hemorrhage due to uterine atony.
Uterine atony is the failure of the uterus to contract and retract after delivery, which can lead to excessive bleeding from the placental site.
Choice A is wrong because manual removal of placenta or retained fragments under anesthesia is not a surgical management for uterine atony, but for retained placenta, which is a different cause of postpartum hemorrhage.
Choice B is wrong because repair of lacerations or hematomas under anesthesia is not a surgical management for uterine atony, but for genital tract trauma, which is another cause of postpartum hemorrhage.
Choice D is wrong because uterine artery embolization to block blood flow to the uterus is not a surgical management for uterine atony, but for refractory cases of postpartum hemorrhage that do not respond to other interventions.It is also a minimally invasive procedure that does not require laparotomy.
Normal ranges for blood loss after vaginal delivery are less than 500 mL and after cesarean delivery are less than 1000 mL.Postpartum hemorrhage is defined as blood loss greater than these amounts within 24 hours of delivery.
A nurse is caring for a client who is experiencing postpartum hemorrhage due to bleeding vessels in her uterus that are not responding to other treatments.
Which of the following surgical management should the nurse expect to be performed on the client?
Explanation
Uterine artery embolization to block blood flow to the uterus.This is a surgical procedure that can be used to control postpartum hemorrhage when medical management and other conservative surgical techniques have failed.Uterine artery embolization involves injecting small particles into the uterine arteries to occlude the bleeding vessels and reduce blood loss.
Choice A is wrong because manual removal of placenta or retained fragments under anesthesia is not a surgical procedure, but a manual technique that can be used to treat postpartum hemorrhage caused by retained placental tissue.
Choice B is wrong because repair of lacerations or hematomas under anesthesia is a surgical procedure that can be used to treat postpartum hemorrhage caused by genital tract trauma, not by bleeding vessels in the uterus.
Choice C is wrong because uterine tamponade with balloon catheter or gauze packing to compress bleeding vessels is not a surgical procedure, but a minimally invasive technique that can be used to treat postpartum hemorrhage caused by uterine atony or placenta accreta.
A nurse is caring for a client who is experiencing postpartum hemorrhage due to bleeding vessels in her uterus that are not responding to other treatments and has already undergone uterine artery embolization but still has excessive bleeding.
Which of the following surgical management should the nurse expect to be performed on the client?
Explanation
B-Lynch suture to compress the uterus with stitches.This is a surgical technique that may be used to arrest postpartum hemorrhage resulting from uterine atony.
It involves placing sutures around the uterus in a compression pattern to reduce the blood flow and contract the uterus.
Choice A is wrong because manual removal of placenta or retained fragments under anesthesia is not a surgical management but a medical one.
It is used to remove any retained products of conception that may prevent the uterus from contracting and cause bleeding.
Choice B is wrong because repair of lacerations or hematomas under anesthesia is not a surgical management for bleeding vessels in the uterus, but for trauma to the genital tract or vulva.
Lacerations or hematomas may occur due to delivery or instrumentation and can cause significant blood loss.
Choice C is wrong because uterine tamponade with balloon catheter or gauze packing to compress bleeding vessels is not a surgical management but a minimally invasive one.
It is used to apply pressure inside the uterine cavity and stop the bleeding from the placental site or other sources.
Nursing Assessment
A nurse is assessing a newborn’s color and oxygenation.
What is the term for the bluish discoloration of the hands and feet that is normal in newborns?
Explanation
Acrocyanosis is the term for the bluish discoloration of the hands and feet that is normal in newborns.It is caused by poor peripheral circulation and ineffective temperature regulation.It usually disappears within 24 to 48 hours after birth.
Choice B is wrong because cyanosis is the bluish discoloration of the skin and mucous membranes that indicates inadequate oxygenation.
It is not normal in newborns and requires immediate intervention.
Choice C is wrong because pallor is the paleness of the skin that indicates poor perfusion or anemia.
It is not normal in newborns and requires further evaluation.
Choice D is wrong because jaundice is the yellowish discoloration of the skin and sclera that indicates elevated bilirubin levels.
It is not normal in newborns within the first 24 hours of life and may indicate hemolytic disease or liver dysfunction.
A nurse is caring for a client who has postpartum hemorrhage due to uterine atony.
Which of the following actions should the nurse take first?
Explanation
Massaging the fundus stimulates uterine contractions and helps to stop the bleeding.
This is the first action the nurse should take to manage uterine atony.
Choice B is wrong because administering oxytocin is a pharmacological intervention that can be used after massaging the fundus if bleeding persists.
Oxytocin is a hormone that also stimulates uterine contractions and reduces blood loss.
Choice C is wrong because inserting an indwelling urinary catheter is not a priority action for postpartum hemorrhage.
A full bladder can interfere with uterine contractions and cause displacement of the uterus, but it is not the main cause of uterine atony.
Choice D is wrong because starting an IV infusion of lactated Ringer’s solution is a supportive measure that can be used to replace fluid loss and maintain blood pressure in postpartum hemorrhage.
However, it does not address the underlying cause of bleeding and should not be done before massaging the fundus.
A nurse is assessing a client who has postpartum hemorrhage.
Which of the following findings is an early sign of hypovolemic shock?
Explanation
Tachycardia is an early sign of hypovolemic shock, which is a life-threatening condition caused by excessive blood loss.Tachycardia is the body’s attempt to compensate for the reduced blood volume and maintain adequate blood pressure and perfusion to vital organs.
Choice B.Hypotension is wrong because it is a late sign of hypovolemic shock, indicating severe blood loss and decompensation.
Hypotension can lead to organ failure and death if not corrected promptly.
Choice C.Oliguria is wrong because it is not a specific sign of hypovolemic shock, but rather a consequence of reduced renal perfusion due to low blood pressure and volume.
Oliguria can also be caused by other factors such as dehydration, urinary tract obstruction, or renal disease.
Choice D.Pallor is wrong because it is not a reliable sign of hypovolemic shock, as it can be influenced by skin color, temperature, and lighting conditions.
Pallor can also occur in other conditions such as anemia, hypoxia, or vasovagal syncope.
Normal ranges for vital signs in postpartum women are:
• Heart rate: 60-100 beats per minute
• Blood pressure
A nurse is teaching a client who has postpartum hemorrhage about the risk factors for this condition.
Which of the following statements by the client indicates a need for further teaching?
Explanation
Having a history of fibroids can increase the risk of bleeding, but not postpartum hemorrhage.Fibroids are benign tumors that grow in the uterus and can cause heavy menstrual bleeding, but they do not affect the placenta or the uterus after delivery.
Choice A is wrong because having a large baby can increase the risk of postpartum hemorrhage.
A large baby can overstretch the uterine muscle and cause atony, which is the failure of the uterus to contract properly after delivery.Atony is the most common cause of postpartum hemorrhage.
Choice B is wrong because having a prolonged labor can increase the risk of postpartum hemorrhage.
A prolonged labor can exhaust the uterine muscle and impair its ability to contract after delivery.This can also lead to atony and excessive bleeding.
Choice D is wrong because having a low-lying placenta can increase the risk of postpartum hemorrhage.
A low-lying placenta, also called placenta previa, is when the placenta covers part of the cervix. This condition can increase the risk of postpartum hemorrhage, which is excessive bleeding after childbirth.
A nurse is preparing to administer methylergonovine to a client who has postpartum hemorrhage.
Which of the following assessments should the nurse perform before giving the medication?
Explanation
The nurse should perform a blood pressure assessment before giving methylergonovine to a client who has postpartum hemorrhage because methylergonovine can cause hypertension and cerebrovascular accidents.The nurse should administer methylergonovine over more than one minute and monitor blood pressure.
Choice B. Temperature is wrong because temperature is not affected by methylergonovine and is not a priority assessment for postpartum hemorrhage.
Choice C. Respiratory rate is wrong because respiratory rate is not affected by methylergonovine and is not a priority assessment for postpartum hemorrhage.
Choice D. Blood glucose is wrong because blood glucose is not affected by methylergonovine and is not a priority assessment for postpartum hemorrhage.
Postpartum hemorrhage is severe vaginal bleeding after childbirth that can lead to shock and death.
The major causes of postpartum hemorrhage are uterine atony, lacerations, retained placenta or clots, and clotting factor deficiency.
A nurse is reviewing the laboratory results of a client who has postpartum hemorrhage.
Which of the following findings should the nurse report to the provider?
Explanation
This is because a low platelet count (<150,000/mm3) indicates thrombocytopenia, which can increase the risk of bleeding and hemorrhage.
The nurse should report this finding to the provider as it may require treatment or transfusion.
Choice A is wrong because hemoglobin 10 g/dL is within the normal range for postpartum women (10-14 g/dL) and does not indicate hemorrhage.
Choice B is wrong because hematocrit 30% is also within the normal range for postpartum women (30-39%) and does not indicate hemorrhage.
Choice D is wrong because white blood cells 12,000/mm3 is slightly elevated but not abnormal for postpartum women, who may have a physiological leukocytosis due to stress, inflammation, or infection.
This finding does not indicate hemorrhage.
Nursing Diagnosis
A nurse is caring for a client who had a vaginal delivery and is experiencing postpartum hemorrhage due to uterine atony.
Which of the following actions should the nurse take first?
Explanation
Massaging the uterine fundus gently is the first action that the nurse should take to stimulate uterine contractions and control bleeding due to uterine atony.Uterine atony is the most common cause of postpartum hemorrhage and occurs when the uterus fails to contract after delivery.
Choice A is wrong because administering oxytocin as prescribed is a secondary action that can be taken after massaging the uterine fundus if bleeding persists.Oxytocin is a medication that promotes uterine contraction and reduces blood loss.
Choice C is wrong because starting an intravenous line with a large bore catheter is a tertiary action that can be taken after massaging the uterine fundus and administering oxytocin if bleeding continues.An intravenous line can provide fluid replacement and blood transfusion if needed.
Choice D is wrong because placing the client in a side lying position is not a priority action for postpartum hemorrhage due to uterine atony.This position may help reduce pressure on the vena cava and improve blood flow, but it does not address the underlying cause of bleeding.
A nurse is reviewing the laboratory results of a client who had a significant postpartum hemorrhage.
Which of the following findings indicates a need for blood transfusion?
Explanation
This indicates a need for blood transfusion because it is below the normal range of 12 to 16 g/dL for women.
Hemoglobin is the protein in red blood cells that carries oxygen to the tissues.A low hemoglobin level can cause symptoms of anemia, such as fatigue, weakness, shortness of breath, and dizziness.
Choice B is wrong because hematocrit 30% is within the normal range of 37 to 47% for women.
Hematocrit is the percentage of red blood cells in the blood.A low hematocrit can indicate blood loss, but it is not a criterion for blood transfusion by itself.
Choice C is wrong because platelets 150,000/mm3 are within the normal range of 150,000 to 450,000/mm3 for both men and women.
Platelets are the cells that help with blood clotting.A low platelet count can increase the risk of bleeding, but it is not a criterion for blood transfusion by itself.
Choice D is wrong because potassium 4 mEq/L is within the normal range of 3.5 to 5 mEq/L for both men and women.
Potassium is an electrolyte that helps with nerve and muscle function.
A high or low potassium
A nurse is teaching a client who is at risk for postpartum hemorrhage about the signs and symptoms of hypovolemic shock.
Which of the following should the nurse include in the teaching? (Select all that apply)
Explanation
The correct answer is choice A, C, D and E.These are the signs and symptoms of hypovolemic shock, which is a life-threatening condition caused by severe blood loss.Hypovolemic shock can occur in postpartum women who have postpartum hemorrhage (PPH), which is excessive bleeding after childbirth.
Choice B is wrong because hypertension is not a sign of hypovolemic shock.In fact, hypotension (low blood pressure) is one of the signs of hypovolemic shock.
Normal ranges for vital signs in postpartum women are:
• Heart rate: 60 to 100 beats per minute
• Blood pressure: 110/70 to 140/90 mmHg
• Respiratory rate: 12 to 20 breaths per minute
• Urine output: at least 30 mL per hour
Question 34.
A nurse is preparing to administer methylergonovine to a client who has postpartum hemorrhage due to retained placental fragments.
Which of the following assessments should the nurse perform before giving the medication?
Explanation
Methylergonovine is a medication that stimulates uterine contractions and helps prevent or treat postpartum hemorrhage due to uterine atony or retained placental fragments.However, it can also cause an increase in blood pressure, so the nurse should monitor the client’s blood pressure before and after giving the medication.
Choice B. Temperature is wrong because methylergonovine does not affect the client’s temperature.
Choice C. Respiratory rate is wrong because methylergonovine does not affect the client’s respiratory rate.
Choice D. Oxygen saturation is wrong because methylergonovine does not affect the client’s oxygen saturation.
Normal ranges for blood pressure are 120/80 mmHg or lower for systolic and diastolic pressures respectively.
Normal ranges for temperature are 36.5°C to 37.5°C or 97.7°F to 99.5°F.
Normal ranges for respiratory rate are 12 to 20 breaths per minute.Normal ranges for oxygen saturation are 95% to 100%.
A nurse is evaluating the effectiveness of oxytocin infusion for a client who has postpartum hemorrhage.
Which of the following findings indicates that the medication is working?
Explanation
This indicates that the uterus has contracted well and the bleeding has stopped.Oxytocin is a drug that helps the uterus to contract and prevent postpartum hemorrhage (PPH), which is excessive bleeding after childbirth.
Choice B is wrong because the lochia flow should be moderate and dark red, not bright red.Bright red blood suggests active bleeding and possible PPH.
Choice C is wrong because the blood pressure is low and the pulse is high, which are signs of shock due to blood loss.PPH can cause a dangerous drop in blood pressure and lead to shock or death.
Choice D is wrong because the urine output is low and the specific gravity is high, which are signs of dehydration due to blood loss.PPH can cause fluid imbalance and kidney damage.
Evaluation
A nurse is caring for a client who had a postpartum hemorrhage due to uterine atony.
Which of the following interventions should the nurse perform first?
Explanation
This is the first intervention that the nurse should perform to stimulate uterine contractions and prevent excessive bleeding due to uterine atony.Uterine atony is a condition where the uterus does not contract enough after delivery and is the most common cause of postpartum hemorrhage.
The other statements are wrong because:
•
A. Administer oxytocin as prescribed.
This is a medication that can help with uterine contractions, but it is not the first intervention.The nurse should first try a nonpharmacologic method such as fundal massage before giving any drugs.
•
C. Assess vital signs and oxygen saturation.
This is an important assessment to monitor the patient’s condition, but it is not the first intervention.The nurse should first try to stop the bleeding by massaging the fundus.
•
D. Insert an indwelling urinary catheter.
This is a procedure that can help with emptying the bladder and reducing pressure on the uterus, but it is not the first intervention.The nurse should first try to stimulate uterine contractions by massaging the fundus.
Normal ranges for vital signs and oxygen saturation are:
• Blood pressure: 110/60 to 140/90 mm Hg
• Pulse: 60 to 100 beats per minute
• Respirations: 12 to 20 breaths per minute
• Temperature: 36.5 to 37.5°C (97.7 to 99.5°F)
• Oxygen saturation: 95% to 100%
A nurse is teaching a client who is at risk for postpartum hemorrhage about the signs and symptoms to report.
Which of the following should the nurse include in the teaching? (Select all that apply.)
Explanation
The correct answer is choices A, B and D. These are signs and symptoms of postpartum hemorrhage, which is excessive bleeding after childbirth.
The nurse should teach the client to report these signs and symptoms to the health care provider immediately.
Choice C is wrong because having a temperature above 38°C (100.4°F) is a sign of infection, not hemorrhage.
The client should also report this symptom, but it is not related to the risk of bleeding.
Choice E is wrong because having a firm uterus with fundus at or below umbilicus is a normal finding after childbirth.
This indicates that the uterus is contracting and preventing bleeding.
A soft or boggy uterus with fundus above umbilicus is a sign of uterine atony, which is a common cause of postpartum hemorrhage.
A nurse is reviewing the laboratory results of a client who had a postpartum hemorrhage.
The nurse notes that the client’s hematocrit level is 28%.
Which of the following actions should the nurse take?
Explanation
Encourage oral intake of iron-rich foods.A hematocrit level of 28% indicates mild anemia, which can be treated with dietary iron supplementation.The normal range of hematocrit for women is 36% to 48%.
Choice A is wrong because a blood transfusion is not indicated for mild anemia and may carry risks of infection or transfusion reaction.
Choice C is wrong because increasing the rate of intravenous fluids may dilute the blood and lower the hematocrit level further.
Choice D is wrong because notifying the provider of the finding is not a direct action that the nurse can take to treat the anemia.The provider may already be aware of the laboratory results and may not need to be notified unless there are signs of worsening anemia or bleeding.
A nurse is assessing a client who had a vacuum-assisted vaginal delivery and is experiencing a postpartum hemorrhage.
Which of the following findings should alert the nurse to a possible laceration of the birth canal?
Explanation
This indicates that the bleeding is from an arterial source, such as a laceration of the birth canal.
Fundal massage stimulates uterine contractions and may increase the blood flow from the laceration site.
Choice A is wrong because a boggy uterus with fundus above umbilicus suggests uterine atony, which is the most common cause of postpartum hemorrhage.
Uterine atony is the failure of the uterus to contract and retract after delivery, leading to bleeding from the placental site.
Choice C is wrong because a firm uterus with fundus at umbilicus indicates that the uterus is well contracted and not likely to be the source of bleeding.
A well-contracted uterus prevents excessive bleeding from the placental site.
Choice D is wrong because dark red bleeding that decreases with fundal massage suggests that the bleeding is from a venous source, such as a hematoma.
Fundal massage may help to compress the hematoma and reduce the bleeding.
Normal ranges for blood loss after vaginal delivery are up to 500 mL and after cesarean delivery are up to 1000 mL.Postpartum hemorrhage is defined as blood loss of more than 1000 mL or signs of hypovolemia within 24 hours of delivery.
A nurse is planning care for a client who has chorioamnionitis and is at risk for postpartum hemorrhage.
Which of the following interventions should the nurse include in the plan? (Select all that apply)
Explanation
The correct answer is choice A, C, D and E. Here is why:
• Choice A: Administer antibiotics as prescribed.
This is correct because chorioamnionitis is a bacterial infection of the membranes and amniotic fluid surrounding the fetus.Antibiotics can help treat the infection and prevent complications for the mother and the baby.
• Choice B: Monitor temperature every 4 hours.
This is wrong because temperature should be monitored more frequently (at least every 2 hours) for signs of infection.Fever is an important symptom of chorioamnionitis and occurs in 95 to 100% of cases.
• Choice C: Provide warm blankets and fluids.
This is correct because chorioamnionitis can cause dehydration and hypothermia due to fever and sweating.Warm blankets and fluids can help maintain fluid balance and body temperature.
• Choice D: Assess lochia for amount and color.
This is correct because chorioamnionitis can cause excessive bleeding and abnormal lochia (vaginal discharge) after delivery.Lochia should be assessed for amount, color, odor and consistency to detect signs of infection or hemorrhage.
Exams on Postpartum Hemorrhage
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define postpartum hemorrhage and its causes
- Identify the risk factors and signs and symptoms of postpartum hemorrhage
- Describe the medical and surgical interventions for postpartum hemorrhage
- Explain the nursing assessment and management of postpartum hemorrhage
- Evaluate the outcomes of nursing interventions for postpartum hemorrhage
Introduction
- Postpartum hemorrhage (PPH) is a life-threatening complication of childbirth that occurs when a woman loses more than 500 mL of blood in a normal delivery and more than 1000 mL of blood in a cesarean delivery within 24 hours.
- PPH is the fifth leading cause of maternal mortality in the United States and causes approximately 11-12% of maternal deaths. It is the leading cause of maternal morbidity and mortality globally.
- The four main causes of PPH are the four T’s: tone (uterine atony), trauma (lacerations, hematomas, uterine inversion or rupture), tissue (retained placental fragments), and thrombin (disseminated intravascular coagulation).
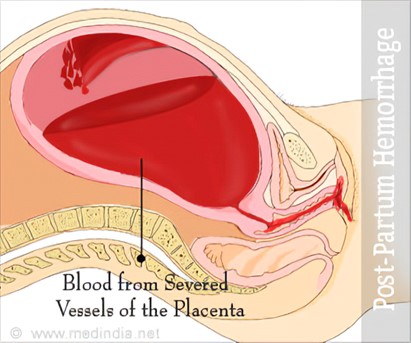
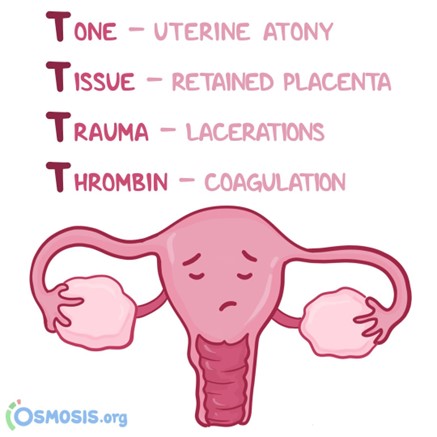
Risk factors
- Conditions that distend the uterus beyond average capacity, such as multiple gestations, hydramnios, a large baby, and uterine myomas.
- Conditions that could have caused cervical or uterine lacerations, such as operative birth or rapid birth.
- Conditions with varied placental site attachment, such as placenta previa and abruption placenta.
- Uterus that cannot contract readily, such as deep anesthesia during cesarean delivery, advanced maternal age, and high parity.
- Inadequate blood coagulation, such as disseminated intravascular coagulation.
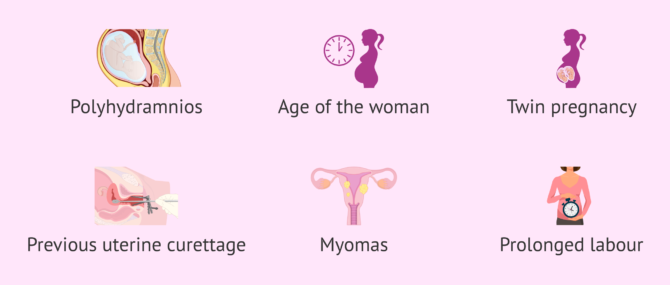
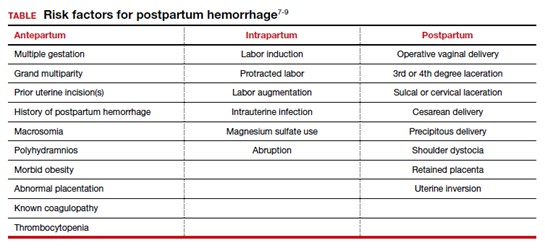
Signs and symptoms
- Heavy vaginal bleeding (> 500 mL in normal delivery or > 1000 mL in cesarean delivery)
- Tense and rigid uterus (may indicate internal bleeding)
- Changes in mental status (confusion, drowsiness)
- Concentrated urine (specific gravity > 1.030)
- Delayed capillary refill (> 3 seconds)
- Decrease in red blood cell count (hematocrit < 30%)
- Decrease in blood pressure (hypotension < 90/60 mm Hg)
- Dry skin/mucous membrane
- Increase in heart rate (tachycardia > 100 beats per minute)
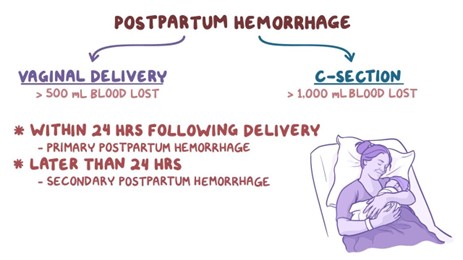
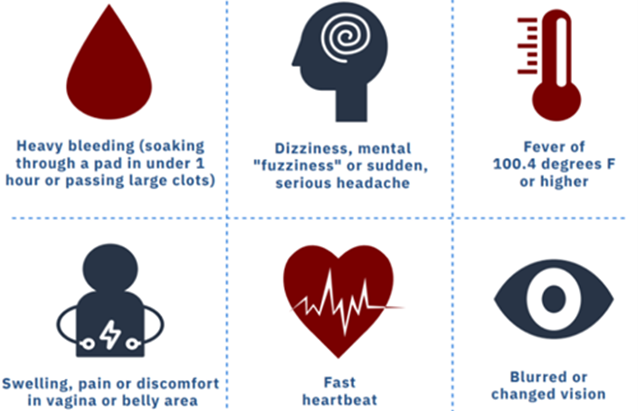
Medical interventions
Medical Interventions
- Administration of Pitocin (oxytocin) to stimulate uterine contractions
- Administration of Carboprost tromethamine (Hemabate) to promote sustained uterine contractions
- Administration of Methylergonovine maleate (Methergine) to enhance uterine tone
- Administration of Misoprostol (Cytotec) to induce uterine contractions
- Administration of Tranexamic acid (TXA) to inhibit fibrinolysis and reduce blood loss
- Administration of blood products (packed red blood cells, fresh frozen plasma, platelets) to replace blood volume and clotting factors

Surgical Management
- Manual removal of placenta or retained fragments under anesthesia
- Repair of lacerations or hematomas under anesthesia
- Uterine tamponade with balloon catheter or gauze packing to compress bleeding vessels
- Uterine artery embolization to block blood flow to the uterus
- B-Lynch suture to compress the uterus with stitches
- Hysterectomy to remove the uterus as a last resort
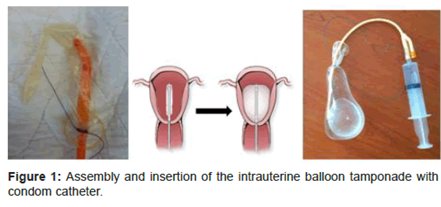
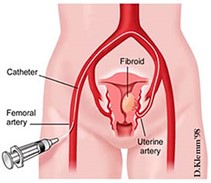
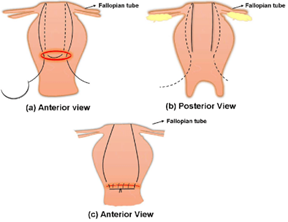
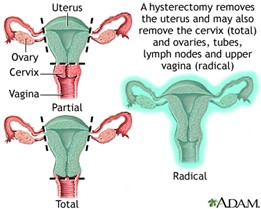
Nursing Assessment
- Assess the amount and characteristics of vaginal bleeding by weighing perineal pads and inspecting for clots
- Assess the condition and tone of the uterus by palpating its fundus and checking for displacement
- Assess the vital signs and oxygen saturation for signs of hypovolemia and shock
- Assess the urine output and specific gravity for signs of renal impairment and dehydration
- Assess the skin color, temperature, and moisture for signs of poor perfusion and fluid loss
- Assess the mental status and level of consciousness for signs of cerebral hypoxia and ischemia
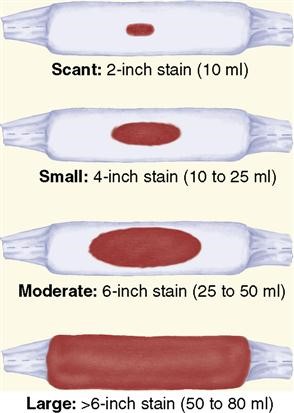
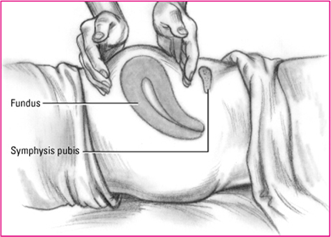
Nursing Diagnosis
Deficient fluid volume related to excessive bleeding after birth.
Nursing interventions
|
Nursing Interventions |
Rationale |
|
Save all perineal pads used during bleeding and weigh them to determine the amount of blood loss |
One gram of weight equals one milliliter of blood loss; this helps to estimate the severity of hemorrhage |
|
Place the woman in a side lying position to prevent blood pooling underneath her |
This allows for accurate assessment of blood loss and prevents hypotension |
|
Massage the uterine fundus gently until firm if atonic |
This stimulates uterine contractions and reduces bleeding from placental sites |
|
Express clots from the uterus if present |
This prevents uterine distension and promotes contraction |
|
Administer oxytocic drugs as ordered |
These drugs augment uterine contractions and tone |
|
Monitor vital signs and oxygen saturation frequently |
These parameters reflect the hemodynamic status and tissue perfusion of the woman |
|
Start an intravenous line with a large bore catheter and infuse isotonic fluids as ordered |
This provides access for fluid resuscitation and blood transfusion if needed |
|
Administer oxygen via face mask or nasal cannula as ordered |
This increases oxygen delivery to vital organs |
|
Monitor urine output and specific gravity hourly |
These indicators reflect renal function and fluid balance |
|
Monitor laboratory results such as hematocrit, hemoglobin, coagulation profile, electrolytes, etc. |
These values reflect the extent of blood loss, clotting ability, acid-base balance, etc. |
|
Prepare the woman for possible surgical intervention if medical therapy fails |
This may be necessary to control bleeding and save her life |
|
Provide emotional support and reassurance to the woman and her family |
This helps to reduce anxiety and fear |
Evaluation
The expected outcomes are:
- The client will maintain a blood pressure of at least 100/60 mm Hg.
- The client will have a pulse rate between 60 and 100 beats per minute.
- The client will have a respiratory rate between 12 and 20 breaths per minute.
- The client will have an oxygen saturation above 95%.
- The client will have a urine output of at least 30 mL per hour.
- The client will have a hematocrit level above 30%.
- The client will have a firm uterus with fundus at or below umbilicus.
- The client will have minimal vaginal bleeding (< 50 mL per hour).
- The client will report no pain or discomfort.
- The client will express understanding of the cause and treatment of postpartum hemorrhage.
Summary
- Postpartum hemorrhage is a serious complication that can cause maternal death if not treated promptly.
- The main causes are uterine atony, lacerations, retained placenta, and coagulation disorders.
- The risk factors include conditions that overstretch or injure the uterus or affect its contractility or clotting ability.
- The signs and symptoms include heavy vaginal bleeding, tense uterus, changes in vital signs, mental status, urine output, skin condition, etc.
- The medical interventions include oxytocic drugs, tranexamic acid, blood products, etc.
- The surgical management includes manual removal of placenta, repair of lacerations, uterine tamponade, uterine artery embolization, B-Lynch suture, hysterectomy, etc.
- The nursing assessment includes monitoring vaginal bleeding, uterine tone, vital signs, oxygen saturation, urine output, specific gravity, skin condition, mental status, etc.
- The nursing diagnosis is deficient fluid volume related to excessive bleeding after birth.
- The nursing interventions include weighing perineal pads, massaging uterine fundus, expressing clots, administering oxytocic drugs, starting intravenous line, administering oxygen, monitoring laboratory results, preparing for possible surgery, providing emotional support, etc.
- The evaluation includes maintaining adequate blood pressure, pulse rate, respiratory rate, oxygen saturation, urine output, hematocrit level, uterine firmness, minimal bleeding, no pain, understanding of condition.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Postpartum Hemorrhage
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


