Please set your exam date
Individual & Family Health And Community Based Practice
Study Questions
Practice Exercise 1
A nurse is providing care based on Maslow’s hierarchy of basic human needs. For which of the following nursing activities is this approach useful?
Explanation
Nurses use Maslow’s Hierarchy of Needs to determine which client needs immediate attention to ensure survival and promote well-being. It guides decision-making, prioritization, and holistic care delivery.
Rationale for correct answer:
B. Establishing priorities of care: Maslow’s hierarchy helps nurses decide what to address first (e.g., oxygenation before emotional support).
Rationale for incorrect answers:
A. Making accurate nursing diagnoses: While understanding needs can inform diagnoses, Maslow's model is not primarily a diagnostic tool; it is more useful for setting priorities.
C. Communicating concerns more concisely: Maslow’s theory isn't a communication framework; it doesn’t directly aid in conciseness or clarity.
D. Integrating science into nursing care: Maslow’s theory is psychological, not scientific; it’s not a method for incorporating scientific data into care.
Take-home points:
- Maslow’s hierarchy is essential for nursing prioritization.
- Always address life-sustaining needs (e.g., airway, breathing) before psychological or social needs.
Which of the following levels of basic human needs is most basic?
Explanation
Maslow’s Hierarchy of Needs is a foundational theory in psychology and nursing that helps prioritize patient care based on five levels of human needs: physiological, safety, love/belonging, esteem, and self-actualization.
Rationale for correct answer:
A. Physiologic: These are the most basic survival needs (oxygen, food, water, rest). Without them, no other needs can be pursued.
Rationale for incorrect answers:
B. Safety and security: These needs are important but come after physiological ones are met.
C. Love and belonging: These are third-level needs related to relationships and emotional connection.
D. Self-actualization: This is the highest level, involving personal growth and reaching one’s full potential.
Take-home points:
- Physiological needs form the foundation of all nursing care-unless these are met, higher-level needs (like safety, love, or self-esteem) cannot be achieved.
Of all the physiologic needs, which one is the most essential?
Explanation
Maslow’s hierarchy of needs emphasizes that basic physiological requirements must be met before individuals can focus on safety, social, or higher-level psychological needs.
Rationale for correct answer:
D. Oxygen: Oxygen is the most essential physiologic need. Without oxygen, brain cells begin to die within 3–5 minutes, making it the top priority in any emergency or clinical scenario.
Rationale for incorrect answers:
A. Food: While essential for long-term survival and health, the body can survive for several days to weeks without food. It is not the most urgent need.
B. Water: Water is more critical than food and is necessary to maintain blood pressure, kidney function, and temperature regulation. However, humans can survive a few days without it.
C. Elimination: While elimination is necessary for removing waste and maintaining electrolyte balance, it is not as immediately life-threatening as the absence of oxygen.
Take-home points:
- Oxygen is the highest priority physiologic need.
- Maslow’s model guides life-saving decisions.
Practicing careful hand hygiene and using sterile techniques are ways in which nurses meet which basic human need?
Explanation
Nurses regularly perform interventions that protect clients from harm and promote healing. Infection control practices like hand hygiene and sterile techniques are not just tasks-they are essential strategies that fulfill a client’s foundational need for safety and well-being.
Rationale for correct answer:
B. Safety and security: Hand hygiene and sterile techniques are preventive actions that protect clients from infections, falls, or complications. These align with Maslow’s second level, which focuses on physical safety, health, and protection from harm.
Rationale for incorrect answers:
A. Physiologic: While infection control supports physiological function by preventing illness, the primary purpose of hygiene and sterile technique is to reduce risk-which aligns more directly with safety.
C. Self-esteem: Self-esteem needs involve confidence, respect, and self-worth. While cleanliness may influence a person’s dignity, sterile technique itself is not directly related to this level.
D. Love and belonging: This level relates to emotional support and interpersonal relationships, such as family, friendships, and social inclusion-not clinical infection control measures.
Take-home points:
- Hand hygiene and sterile technique directly support a patient’s safety and security by reducing the risk of healthcare-associated infections.
- Understanding how nursing actions map to Maslow’s hierarchy helps nurses prioritize care and meet patients’ holistic needs in the right order.
Of the following statements, which one is true of self-actualization?
Explanation
Self-actualization refers to the ongoing process of fulfilling one’s potential and becoming the most that one can be. It is not a one-time achievement but a lifelong journey influenced by life experiences, personal growth, and introspection.
Rationale for correct answer:
C. The self-actualization process continues throughout life: This statement reflects Maslow’s belief that self-actualization is an ongoing, evolving process. Individuals can reach higher levels of development throughout their lives.
Rationale for incorrect answers:
A.Humans are born with fully developed self-actualization: Self-actualization is not innate or fully developed at birth. It is a lifelong pursuit achieved through growth, challenges, and learning, after lower-level needs are met.
B. Self-actualization needs are met by having confidence and independence: Confidence and independence are part of self-esteem needs, not self-actualization. Self-actualization involves creativity, fulfillment, morality, and personal growth beyond just self-confidence.
D. Loneliness and isolation occur when self-actualization needs are unmet: Loneliness and isolation are linked to unmet love and belonging needs, which are lower than self-actualization on Maslow’s hierarchy.
Take-home points:
- Self-actualization is a lifelong journey, not a fixed state.
- It represents the continuous growth toward one’s highest potential.
- Maslow’s hierarchy helps nurses understand holistic care & guiding support.
Practice Exercise 2
A school nurse is teaching a class on domestic violence to high school students. Which of the following student statements indicates a need for further teaching?
Explanation
Domestic violence is a pervasive issue that can affect individuals across all ages, education levels, and socioeconomic backgrounds. Nurses and school health professionals play a key role in educating adolescents on healthy relationships and identifying early signs of abuse.
Rationale for correct answers:
B. “If you are educated and have money, abuse does not happen.” Domestic violence can happen to anyone regardless of education, income, or social status. Believing it only happens in disadvantaged communities prevents people from recognizing abuse in more affluent populations.
Rationale for incorrect answers:
A. “Abusers are often excessively jealous and possessive.” Jealousy and possessiveness are red flags in abusive relationships. Abusers may attempt to isolate victims from friends or family and control their actions.
C.“The abuser will often apologize and promise to stop.” Abusers frequently use apologies and promises during the honeymoon phase of the abuse cycle. These promises often manipulate the victim into staying, which is a classic part of the cycle of violence.
D. “Violence often begins in a dating relationship.” Teen dating violence is common, and early warning signs can be seen during adolescence. Education about healthy vs. unhealthy relationship behaviors is essential during this period.
Take-home points:
- Domestic violence can affect anyone, regardless of socioeconomic or educational background. It is not confined to poverty or lack of education.
- Education of adolescents about red flags in relationships-such as jealousy, control, and emotional manipulation-is critical for early identification and prevention of abuse.
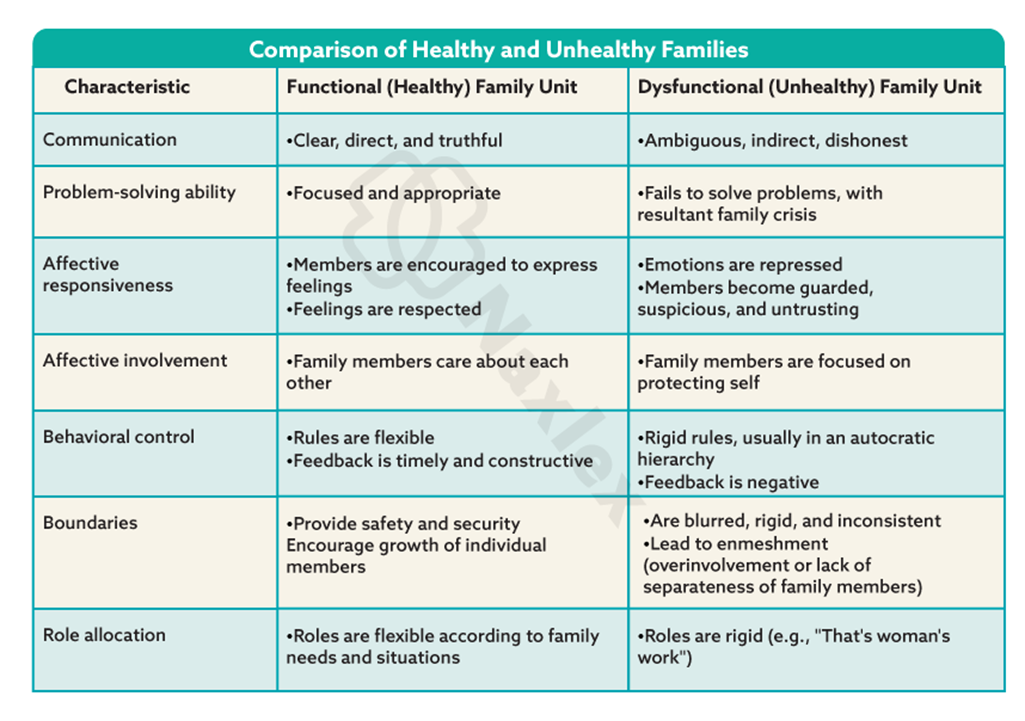
Which of the following is a trait of a functional (healthy) family?
Explanation
Functional families provide support, structure, and nurturing to all members, promoting emotional well-being and effective coping strategies during stress or conflict.
Rationale for correct answer:
D. Timely feedback is a hallmark of a healthy family. It reflects open, honest, and effective communication where family members respond to each other's emotional and practical needs appropriately and without delay.
Rationale for incorrect answers:
A. Ambiguous communication involves unclear, contradictory, or indirect messages. It can lead to confusion, mistrust, and emotional distress among family members. Healthy families practice clear, direct communication.
B. Enmeshment refers to blurred boundaries between family members, often resulting in overinvolvement in each other’s lives. In functional families, members maintain individual identity and independence while still being emotionally connected.
C. Hierarchy of rules: While structure is important, rigid hierarchies and strict, inflexible rules are more characteristic of dysfunctional family systems. Healthy families often use flexible roles and collaborative decision-making, promoting mutual respect and adaptability.
Take-home points:
- Healthy families demonstrate open, clear, and timely communication, which fosters emotional safety and mutual understanding.
- Dysfunctional traits like enmeshment, ambiguous communication, and rigid hierarchies can hinder healthy development and coping.
Where do individuals learn their health beliefs and values?
Explanation
Health beliefs and values significantly influence how individuals perceive illness, adhere to treatments, and engage in health-promoting behaviors.
Rationale for correct answer:
A. In the family: The family is the primary socializing agent where individuals first learn health-related beliefs, values, behaviors, and practices. Children observe and imitate how family members handle illness, nutrition, hygiene, and health-seeking behaviors.
Rationale for incorrect answers:
B. In school: Schools provide structured health education, but they generally reinforce, rather than originate, an individual's health beliefs. While important, schools are typically secondary sources after the family.
C. From school nurses: School nurses play an important supportive and educational role, particularly in addressing acute issues and promoting health in school settings. However, they are not the primary source of health belief development.
D. From peers: Peers may influence health behaviors, especially in adolescence (e.g., substance use, diet trends), but they usually affect short-term behaviors more than deeply rooted values and beliefs, which are primarily learned from the family.
Take-home points:
- Family is the foundational source for the development of health beliefs, attitudes, and behaviors, influencing individuals long before exposure to formal health education.
- Understanding family influence helps nurses tailor education and interventions to align with or gently challenge existing beliefs for better health outcomes.
Two priority actions of the community nurse that address family violence are:
Explanation
Family violence is a serious public health issue that affects individuals physically, emotionally, and socially. Community health nurses play a critical role in identifying and intervening in cases of abuse through prevention, detection, and coordination of care.
Rationale for correct answer:
A. Assessment: Community nurses must first assess for signs of abuse-physical, emotional, or behavioral indicators-through screening and observation.
D. Interdisciplinary communication: Addressing family violence requires collaboration with social workers, law enforcement, mental health professionals, and legal systems. Effective communication ensures a coordinated response for protection and support of the victim.
Rationale for incorrect answers:
B. Diagnosing: While diagnosing (nursing diagnosis) is part of the nursing process, it is not a priority action specific to addressing family violence. The immediate concern is recognizing the abuse and ensuring safety through proper assessment and referral.
C. Education: Education is important in the long-term prevention of family violence but is not the top priority when responding to suspected or active abuse. Safety and coordination of care come first.
E. Planning: Planning is part of the overall nursing process, but in the context of immediate family violence response, it comes after assessment and initial collaboration. It is not a priority action on its own.
F. Political advocacy: Advocacy for policy change is vital to broader systems change, but not a priority during the actual response to an individual or family experiencing violence. It is a secondary or long-term public health strategy.
Take-home points:
- Assessment and interdisciplinary communication are the two most critical actions for a community nurse addressing family violence.
- While education and advocacy play important roles in prevention and systems change, initial safety, recognition, and referral are the highest priorities when family violence is suspected.
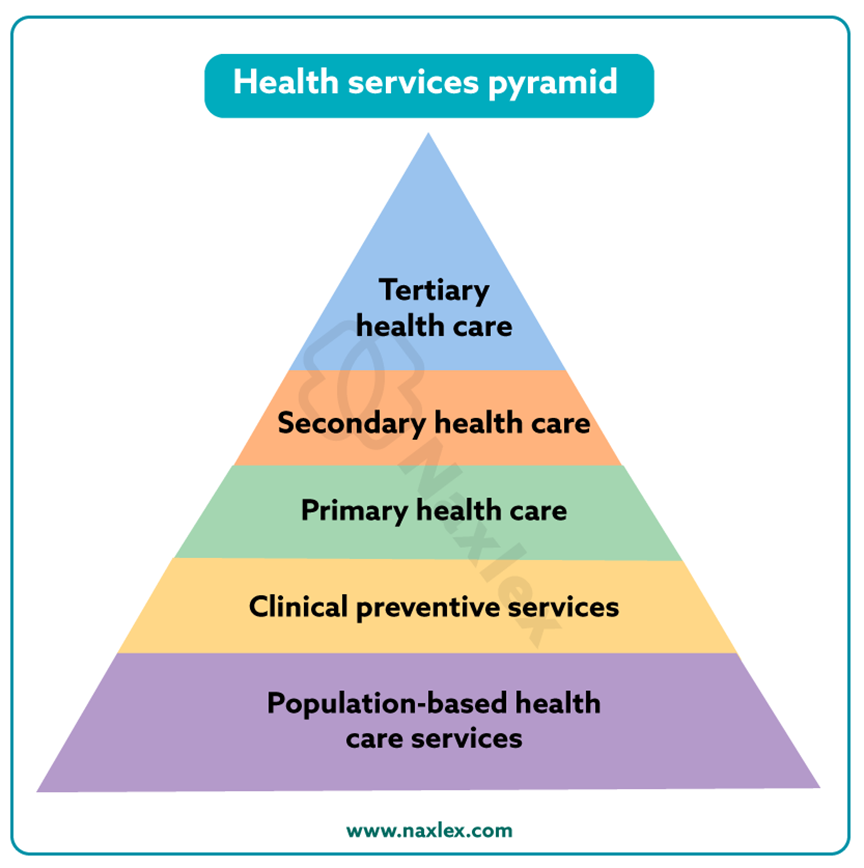
Which of the following is an example of tertiary prevention activities for the nurse to perform with abused children?
Explanation
In the context of child abuse, tertiary prevention focuses on minimizing long-term consequences and preventing recurrence. This includes interventions directed at rehabilitation, healing, and behavior change among those already affected.
Rationale for correct answer:
C. Performing family therapy for abusive parents: This is a tertiary prevention activity. It addresses rehabilitation and behavioral change in already affected families to prevent recurrence and support recovery.
Rationale for incorrect answers:
A. Assessing for signs of child abuse: This is a secondary prevention activity. It involves early detection to prevent escalation or further harm.
B. Identifying at-risk households: This is an example of primary prevention, where the nurse aims to prevent abuse before it occurs by targeting risk factors (e.g., poverty, substance use, family stress).
D. Teaching parenting classes on developmental milestones: This falls under primary prevention, aiming to prevent abuse through education and support before abuse happens.
Take-home points:
- Tertiary prevention in child abuse focuses on recovery and preventing re-abuse through interventions like counseling and therapy.
- Knowing the level of prevention helps the nurse select appropriate interventions depending on whether the goal is to prevent, detect, or treat abuse.
Practice Exercise 3
The Pew Commission competencies for future practitioners included the need for providers to become skilled in which of the following?
Explanation
The Pew Health Professions Commission was established to guide reforms in healthcare education and workforce preparation in response to a rapidly evolving healthcare environment. The Commission emphasized competency-based education, interdisciplinary collaboration, and adaptability in the use of modern tools like technology and evidence-based practice.
Rationale for correct answer:
A. Use of technology: The Pew Commission highlighted the importance of providers being proficient in information and communication technology to support clinical decision-making, care coordination, and evidence-based practice.
Rationale for incorrect answers:
B. Emphasizing practice in tertiary settings: The Commission advocated for expanded care in primary and community-based settings, rather than focusing only on tertiary (specialized hospital-based) care.
C. Traditional clinical approaches: While clinical skills remain important, the Commission emphasized innovation and adaptability over strict reliance on traditional models.
D. Making decisions for incompetent clients: Although healthcare providers must be knowledgeable about ethical and legal aspects of decision-making, the focus of the Pew competencies was not on providers unilaterally making decisions for incompetent clients.
Take-home points:
- Technological competence is a key expectation for future healthcare providers, enabling safer, more efficient, and evidence-based care.
- The Pew Commission encouraged a shift from hospital-centric care toward community-focused, preventive, and collaborative models of practice.
Which of the following is characteristic of nursing care provided in community-based health?
Explanation
Community-based nursing is a practice that emphasizes health promotion, illness prevention, and chronic condition management outside of traditional hospital settings.
Rationale for correct answer:
B. Clients are individuals in groups according to their geographic commonalities: Community-based care often organizes services based on geographic areas (e.g., neighborhoods, rural areas), addressing the unique health needs of people living in the same community or region.
Rationale for incorrect answers:
A. Clients are primarily those with identified illnesses: Community-based nursing includes clients across the health-illness spectrum, not just those who are ill. It involves preventive, promotive, and curative services and targets healthy individuals, at-risk populations, and the chronically ill.
C. Care is paid for by the community as a whole rather than by individuals: While some public health services may be funded through taxes or grants, most community-based services are paid for by individuals, insurance, or mixed sources-not collectively by the community.
D. All clients are case managed: Although case management is an important strategy, especially for clients with chronic or complex conditions, it is not applied universally to all clients in community-based settings.
Take-home points:
- Community-based nursing serves populations grouped by geographic and social contexts, not just by diagnosis or illness.
- It promotes a holistic and preventive approach, emphasizing accessibility and relevance to the community’s specific needs.
What factor results in vulnerable populations being more likely to develop health problems?
Explanation
Vulnerable populations-such as individuals with low income, the homeless, refugees, the elderly, and those with chronic illnesses-face greater health challenges due to a range of social determinants of health.
Rationale for correct answer:
D. Limited access to health care services: When individuals cannot access primary, preventive, or specialty care, they are more likely to develop untreated or worsened health conditions, contributing to poorer overall health.
Rationale for incorrect answers:
A. The ability to use available resources to find housing: This reflects a strength, not a vulnerability. The ability to find housing is a protective factor and supports improved health outcomes, rather than contributing to increased health problems.
B. Adequate transportation to the grocery store and community clinics: Adequate transportation reduces health risks by increasing access to nutritious food and medical care. This is a facilitator of health, not a contributor to vulnerability.
C. Availability of others to help provide care: Having social support and caregivers contributes to better health outcomes. Social networks can help individuals manage chronic illnesses, adhere to treatment plans, and attend appointments.
Take-home points:
- Access to health care is a critical determinant of health.
- Nurses must assess and address barriers such as transportation, insurance coverage, and availability of clinics to improve health equity and outcomes for at-risk populations.
Many older homes in a neighborhood are undergoing a lot of restoration. Lead paint was used to paint the homes when they were built. The community clinic in the neighborhood is initiating a lead screening program. This activity is based on which social determinant of health?
Explanation
Social determinants of health are the non-medical factors that influence health outcomes. Nurses and public health professionals must understand how environments-physical, social, economic, and educational-affect community health.
Rationale for correct answer:
A. The physical environment includes the built environment and exposures. Lead exposure from deteriorating paint in old homes is a direct threat to health, especially in children, and justifies environmental health interventions like screening.
Rationale for incorrect answers:
B. Economic environment: Although economic status may affect the ability to renovate safely or relocate, this specific scenario is centered on environmental exposure due to the physical conditions of the homes.
C. Educational environment: While education impacts awareness about risks such as lead exposure, the driver of the clinic’s action here is the hazard in the built environment, not a gap in education or school systems.
D. Health care environment: The screening program may be part of the health care response, but the underlying determinant prompting the action is the unsafe physical housing.
Take-home points:
- The physical environment is a major determinant of community health.
- Hazards like lead in old paint can cause significant health issues, particularly in children, requiring proactive community-level screening and prevention programs.
- Public health interventions are often shaped by environmental risks.
- Nurses and health workers must assess community settings to identify and address threats rooted in housing, pollution, and infrastructure.
A community health nurse conducts a community assessment focused on adolescent health behaviors. The nurse determines that a large number of adolescents smoke. Designing a smoking-cessation program at the youth community center is an example of which nursing role?
Explanation
Community health nurses play diverse roles aimed at promoting wellness and preventing illness in populations. Their responsibilities extend beyond bedside care to include assessing population needs, developing interventions, and coordinating services.
Rationale for correct answer:
B. Counselor: By designing a smoking-cessation program, the nurse is providing guidance and support aimed at behavioral change-central to the counseling role.
Rationale for incorrect answers:
A. An epidemiologist focuses on collecting and analyzing data about the distribution and determinants of health issues in a population.
C. Collaboration involves working with other professionals, agencies, or community members to plan and implement programs.
D. Case managers coordinate services and resources for individual clients to ensure their health needs are met efficiently. This role is more client-specific, whereas the question describes a population-level educational intervention.
Take-home points:
- The counselor role in community health nursing emphasizes behavior change.
- Nurses in this role educate, support, and empower individuals and groups to make healthier decisions, such as quitting smoking.
Comprehensive Questions
The ANA’s Health System Reform Agenda (2008) included which of the following?
Explanation
The American Nurses Association (ANA) plays a vital role in shaping health policy that promotes accessible, high-quality, and cost-effective care for all individuals. In its 2008 Health System Reform Agenda, the ANA emphasized a framework for improving the U.S. healthcare system by addressing coverage, access, quality, and the role of nurses in care coordination.
Rationale for correct answer:
C. Case management should be focused on clients with enduring health care needs: The reform agenda specifically supported nurse-led case management for individuals with chronic and complex conditions to ensure coordination and continuity of care.
Rationale for incorrect answers:
A. Primary health care should be based in acute care hospitals: The ANA agenda proposed that primary health care should be community-based, not based in acute care settings. Hospitals are meant for acute episodes, not routine or preventive care.
B. A minimum standard of health care for all persons should be paid for completely with public funds: While the ANA supports a minimum standard of care for all, it did not propose exclusive public funding. Instead, it emphasized a hybrid system of public and private sources to ensure broad access and sustainability.
D. Essential services should be initiated simultaneously to avoid gaps: The ANA recommended a phased implementation of essential services-not all at once-to ensure the system can adapt effectively and sustainably.
Take home points:
- The ANA supports community-based primary care and emphasizes the role of nurses in case management.
- The reform agenda proposed blended funding (public and private) and a gradual rollout of services.
When performing collaborative health care, the nurse must implement which of the following?
Explanation
Collaborative health care is a key principle in modern nursing practice and emphasizes interdisciplinary teamwork to achieve optimal patient outcomes. This model fosters shared decision-making, respect for roles, and improved continuity of care.
Rationale for correct answer:
B.Rely on the expertise of other health care team members: Effective collaboration requires the nurse to recognize and utilize the specific expertise of other professionals (e.g., physical therapists, dietitians, physicians) to ensure comprehensive and holistic care.
Rationale for incorrect answers:
A. Assume a leadership role in directing the health care team: Collaborative care is not about directing others, but about working as equal team members who contribute their own expertise while valuing the input of others.
C. Be physically present for the implementation of all aspects of the care plan: Collaboration involves delegation and trust in other professionals to fulfill their responsibilities appropriately within their scopes of practice.
D. Delegate decision-making authority to each health care provider: Decision-making in collaborative care is shared, not delegated. Each provider independently exercises professional judgment within their scope; the nurse does not "delegate" authority to others.
Take-home points:
- Collaborative care involves mutual respect and reliance on each team member's specialized knowledge to provide effective, patient-centered care.
- Nurses contribute as equal partners-not as directors or sole decision-makers-in a team that works collectively toward common health goals.
The nurse concludes that effective discharge planning (hospital to home) has been conducted when the client states which of the following?
Explanation
Discharge planning is a critical part of the nursing process, especially as clients transition from hospital care to home or other settings. Effective discharge planning ensures that the client is informed, prepared, and supported to continue recovery safely.
Rationale for correct answer:
D. “I have the phone numbers of the home care nurse and the therapist who will visit me at home tomorrow.” This statement shows that home services are already arranged, the client has contact information, and care continuity is in place, reflecting thorough and effective discharge planning.
Rationale for incorrect answers:
A. “As soon as I get home, the nurse will come out, look at where I live, and see what kind of care I will need.” This indicates that planning has not yet occurred. Assessment and coordination of home care needs should happen before discharge, not after the client is already home.
B. “All I need are my medications and a ride home. Then I’m all ready for discharge.” While important, this response reflects a narrow view of discharge readiness. Effective discharge involves more than transport and medications-it includes follow-up care, services, and education.
C. “When I visit my doctor in 10 days, they will show me how to change my bandages.” Waiting 10 days to learn wound care implies lack of preparation for self-care, which is unsafe and does not meet discharge criteria. Education should be provided before discharge.
Take-home points:
- Effective discharge planning includes clear arrangements for home care services.
- Nurses must verify client understanding and readiness before discharge to ensure safety, adherence, and successful recovery at home.
A large disaster in a community resulted in the destruction of many family homes and many individuals were injured. The assistance of community health nurses and home health nurses is needed. The home health nurse is most likely to perform which of the following?
Explanation
During a large-scale community disaster, a coordinated response from various healthcare professionals is crucial. Both community health nurses and home health nurses play essential but distinct roles. While public health nurses often focus on population-level needs like surveillance, sanitation, and coordination, home health nurses primarily deliver direct, individualized care to clients in their homes or temporary shelters.
Rationale for correct answer:
D. Assess and treat individual clients: After a disaster, their role includes assessing wounds, monitoring vital signs, administering medications, and ensuring continuity of care for displaced or injured individuals.
Rationale for incorrect answers:
A. Provide for a safe water supply: Ensuring safe water access is typically the role of public health officials and environmental health specialists. This is a population-level intervention.
B. Monitor for communicable diseases: While home health nurses may observe signs of infection, surveillance and outbreak monitoring fall under the community health nurse's responsibilities during disasters.
C. Establish communication and support systems: This task is better suited for community leaders, social workers, and disaster coordinators, who focus on rebuilding infrastructure and ensuring systems are in place for broad community functioning.
Take-home points:
- Home health nurses focus on direct care for individual clients, especially after a disaster when access to hospitals or clinics may be limited.
- Public and community health nurses handle population-level needs, such as sanitation, disease surveillance, and system coordination in emergency settings.
The public health nurse is working with the local city/county health department during a pandemic that has created a crisis within the community. What are the responsibilities of the public health nurse during the pandemic? Select all that apply
Explanation
Public health nurses play a crucial frontline role during public health emergencies such as pandemics. Their work shifts from routine community outreach to urgent responsibilities involving disease surveillance, case investigation, health education, and population-level interventions.
Rationale for correct answers:
A. Educate the public on disease prevention: Education is a core function of public health nursing. During a pandemic, nurses provide evidence-based education on prevention measures such as hand hygiene, mask use, quarantine, and vaccination.
B. Serve as liaison between patients and health care services and providers: Public health nurses help connect individuals to testing centers, clinics, and other services. They facilitate access to care, especially for vulnerable or underserved populations.
C. Investigate cases as they arise: Case investigation is a key public health function. Nurses work to identify index cases, trace contacts, and ensure isolation/quarantine to contain disease spread.
D. Monitor trends of the disease outbreak: Public health nurses track infection rates, identify patterns, and contribute to surveillance efforts to inform public health decisions and response planning.
E. Assist with testing for identification of the disease: Depending on training and local needs, public health nurses may help coordinate or conduct testing efforts, especially during mass testing drives or in underserved areas.
Take-home points:
- Public health nurses are multi-skilled professionals who play a central role in disease prevention, surveillance, case investigation, and public education during pandemics.
- Their ability to bridge clinical services and community needs makes them critical to any public health emergency response.
A community health nurse is working in a clinic with a focus on asthma and allergies. What is the primary focus of the community health nurse in this clinic setting? Select all that apply
Explanation
Community health nurses serve a vital role in the prevention and management of chronic diseases. In community settings, the focus shifts from treating acute episodes to promoting long-term health through education, outreach, prevention, and empowerment of individuals and populations.
Rationale for correct answers:
A. Decrease the incidence of asthma attacks in the community: Community health nurses focus on prevention by helping clients reduce exposure to triggers, follow medication regimens, and understand early warning signs to reduce asthma attacks.
B. Increase patients’ ability to self-manage their asthma: Teaching self-management skills such as inhaler technique, trigger avoidance, and peak flow monitoring is a key goal. Empowered clients are more likely to stay out of the hospital.
D. Provide asthma education programs for the teachers in the local schools: This reflects the community nurse’s role in health promotion and outreach. Educating school personnel helps ensure prompt recognition and response to asthma symptoms in children.
Rationale for incorrect answers:
C. Treat acute asthma in the hospital: Hospital-based treatment of acute asthma falls under acute care or emergency nursing, not community health nursing. Community nurses focus on outpatient and preventive care.
E. Provide scheduled immunizations to people who come to the clinic: While not asthma-specific, this is part of the preventive care role of a community health nurse.
Take-home points:
- Community health nurses emphasize prevention, education, and chronic disease management to reduce complications and hospitalizations.
- Their role includes outreach beyond the clinic, such as partnering with schools and promoting public health measures.
The nurse caring for a refugee community identifies that the children are under vaccinated and the community is unaware of resources. The nurse assesses the community and determines that there is a health clinic within a 5-mile radius. The nurse meets with the community leaders and explains the need for immunizations, the location of the clinic, and the process of accessing health care resources. Which of the following practices is the nurse providing? Select all that apply
Explanation
Nurses serve as advocates, educators, and coordinators, bridging the gap between health services and the community. Community health nursing plays a crucial role in addressing the needs of vulnerable populations such as refugee communities. These populations often experience disparities in access to healthcare services.
Rationale for correct answers:
A. Raising awareness about community resources for the children: The nurse informs the community about a nearby clinic and how to access services, directly increasing awareness of local healthcare resources.
B. Teaching the community about health promotion and illness prevention: By educating the community leaders on the importance of immunizations, the nurse is promoting disease prevention and health promotion.
D. Improving the health care of the community’s children: Facilitating access to immunizations contributes to better preventive care and reduces the risk of vaccine-preventable illnesses.
Rationale for incorrect answers:
C. Promoting autonomy in decision making about health practices: There’s no mention of helping the community weigh pros and cons or engaging them in dialogue about personal or cultural preferences.
E. Participating in professional development activities to maintain nursing competency: While important in general, this activity is not reflected in the scenario. The nurse is not depicted as engaging in personal professional development.
Take-home points:
- Community health nurses serve as crucial links between underserved populations and healthcare services, helping overcome barriers to care.
- Health education, advocacy, and culturally appropriate communication empower communities to make informed decisions and improve public health outcomes.
A nurse in a community health clinic reviews screening results from students in a local high school during the most recent academic year. The nurse discovers a 10% increase in the number of positive tuberculosis (TB) skin tests when comparing these numbers to the previous year. The nurse contacts the school nurse and the director of the health department. Together they begin to expand their assessment to all students and employees of the school district. The community nurse is acting in which nursing role(s)? Select all that apply
Explanation
Community health nurses take on various professional roles, including surveillance, counseling, collaboration, care coordination, and direct care, depending on the needs of the population.
Rationale for correct answers:
A. Epidemiologist: The nurse recognized an increase in TB cases and began surveillance and data collection, which are key tasks of an epidemiologist. This role involves identifying patterns of disease occurrence and collaborating to manage public health threats.
C. Collaborator: The nurse reached out to the school nurse and health department director to address the rising TB cases. This reflects interprofessional collaboration to coordinate a community-wide response and ensure comprehensive assessment and care.
Rationale for incorrect answers:
B. Counselor: There is no indication in the scenario that the nurse provided emotional support or behavioral guidance, which defines the counselor role.
D. Case manager: The nurse is involved in coordinating a system-wide approach to assessing and potentially managing TB cases among students and employees.
E. Caregiver: The caregiver role involves delivering direct clinical care to individuals. In this scenario, the nurse is acting in a public health capacity rather than providing hands-on treatment.
Take-home points:
- Community health nurses often function in multiple roles simultaneously-such as epidemiologist, collaborator-especially in the face of emerging public health issues like TB.
- Recognizing a rise in disease incidence and initiating a coordinated response reflects advanced nursing practice in public health surveillance and population-focused care.
A nursing student is giving a presentation to a group of other nursing students about the needs of patients with mental illnesses in the community. Which statement by the student indicates that the nursing professor needs to provide further teaching?
Explanation
Nurses must understand social determinants such as housing instability, unemployment, risk of violence, and where care is actually provided. Misconceptions about the mental health care system can lead to poor advocacy, ineffective planning, and missed opportunities to support clients in the community.
Rationale for correct answers:
C. “The majority of patients with mental illnesses live in long-term care settings.” Most individuals with mental illnesses live independently or with family in the community, not in long-term institutional settings.
Rationale for incorrect answers:
A. “Many patients with mental illness do not have a permanent home.” Homelessness is a well-documented issue among individuals with mental illness due to factors like poverty, stigma, lack of support, and fragmented care.
B. “Unemployment is a common problem experienced by people with a mental illness.” Individuals with mental illness often face challenges in maintaining employment due to symptom burden, discrimination, and lack of workplace accommodations.
D. “Patients with mental illnesses are often at a higher risk for abuse and assault.” Studies show that individuals with mental illness are more likely to be victims, rather than perpetrators, of violence.
Take-home points:
- Most individuals with mental illness live in community settings, not long-term institutions, due to a shift in treatment models and the emphasis on deinstitutionalization.
- Effective mental health nursing requires understanding the social challenges that influence health outcomes and care planning.
The nurse in a new community-based clinic is requested to complete a community assessment. Order the steps for completing this assessment.
Explanation
A community assessment helps nurses gather data to identify health needs, plan interventions, and allocate resources effectively. The assessment typically follows a structured approach
Rationale for correct answers:
Step 1: Structure or locale
The assessment begins by evaluating the physical environment and setting of the community. Understanding the geographic and environmental context lays the foundation for identifying how the community is organized and what resources are available.
Step 2: Population
After understanding the locale, the nurse assesses the people who live in the community. This helps identify who the community members are and what their specific health needs may be.
Step 3: Social systems
Finally, the nurse evaluates how the population interacts within their environment by assessing the community's social systems. These systems affect access to care, health behaviors, and the overall well-being of the population.
Take-home points:
- A thorough community assessment starts with understanding the environment (structure), then the people (population), and finally their interactions and support networks (social systems).
- Community health nurses use these steps to identify needs, plan care, and implement effective health interventions within the context of the local environment.
The public health nurse is working with the county health department on a task force to fully integrate the goals of Healthy People 2030. Most of the immigrant population do not have a primary care provider, nor do they participate in health promotion activities; the unemployment rate in the community is 25%. How does the nurse determine which goals need to be included or updated? Select all that apply
Explanation
Healthy People 2030 outlines national objectives aimed at improving health and well-being by addressing social determinants of health, improving access to care, and reducing health disparities.
Rationale for correct answers:
A. Assess the health care resources within the community: This is an essential first step to understanding what services are already available and where the gaps lie.
B. Assess the existing health care programs offered by the county health department: Evaluating current programs ensures that the nurse does not duplicate services and identifies what programs can be strengthened or expanded.
C. Compare existing resources and programs with Healthy People 2030 goals: This step ensures alignment with national priorities. By comparing local services to national health goals, the nurse can identify areas that require improvement or new initiatives.
Rationale for incorrect answers:
D. Initiate new programs to meet Healthy People 2030 goals: Before launching new initiatives, a full assessment and comparison with Healthy People 2030 must be completed to ensure efforts are evidence-based and appropriately targeted.
E. Implement educational sessions in the schools to focus on nutritional needs of the children: The nurse must first assess and align goals before selecting specific interventions like school-based education.
Take-home points:
- Effective community planning starts with a comprehensive assessment of current resources and programs before implementing new interventions.
- Healthy People 2030 serves as a national guide to help public health professionals set measurable, evidence-based goals that reflect community-specific needs.
The community health nurse is teaching a parenting skills class to new parents. Which of the following parent statements indicates that the teaching has been effective? Select all that apply
Explanation
Community health nurses play a vital role in educating new parents on the concept of family and how family dynamics can influence child development and overall health. The definition of "family" has evolved over time and now includes diverse structures beyond the traditional nuclear family.
Rationale for correct answers:
C. “My husband has a child by another marriage, so when our child is born we will be a blended family.” This is an accurate recognition of a blended family, which consists of two parents and their children from current or previous relationships. It reflects a good understanding of evolving family dynamics.
D. “Our family’s beliefs may affect the health of our children.” Family values, traditions, and cultural beliefs can significantly influence health behaviors, such as diet, preventive care, and attitudes toward illness or healthcare providers.
E. “There are many different types of families.” This demonstrates inclusive and accurate understanding of modern family structures. Recognizing diversity in family types helps promote acceptance and adaptability in parenting and caregiving.
Rationale for incorrect answers:
A.“In order to be considered a family, those living together must be related by blood.” This statement reflects a narrow and outdated view of family. Families can be formed through adoption, marriage, cohabitation, or mutual commitment, regardless of blood relation.
B.“My family is typical because we have a husband, wife, and soon-to-be two children.” While this describes a nuclear family, it's important to recognize that no single family structure is more “typical” or valid than others.
Take-home points:
- Family is defined by relationships, support, and shared commitment, not just by blood or legal ties.
- Effective parenting education includes recognizing and respecting all family structures.
- Family beliefs and structure significantly influence children’s health and development.
According to the American Nurses Association, which of the following standards of care must be implemented during response to a disaster? Select all that apply
Explanation
During disaster response, nurses must adhere to established standards of care even in chaotic environments. According to the American Nurses Association (ANA), disaster nursing involves prioritizing life-saving interventions.
Rationale for correct answer:
A. Airway, breathing, and circulation maintenance: This is the highest priority in disaster triage-based on the ABCs of life support. It reflects the ANA standard to preserve life and stabilize critical conditions.
B. Confidentiality: Despite the urgency, HIPAA and ANA ethics still require nurses to maintain client confidentiality unless legal or safety exceptions apply.
C. Documentation of care: Even in disasters, accurate documentation is essential for continuity of care, legal protection, and resource tracking.
E. Infection control practices: Infections can spread rapidly in crowded or compromised settings. Hand hygiene, PPE, and isolation protocols must be upheld to protect both clients and responders.
F. Safety for both nurse and client(s): The ANA emphasizes the dual duty to protect both care providers and recipients. Nurses should not enter unsafe environments and should advocate for safe operations.
Rationale for incorrect answer:
D. Elective procedures are not a priority during a disaster response. Resources must be allocated to emergency, life-saving interventions.
Take-home points:
- Disaster response requires nurses to maintain core ethical and clinical standards, such as ABCs, safety, and infection control.
- While emergencies may alter prioritization, elective or non-essential care is postponed in favor of life-preserving actions.
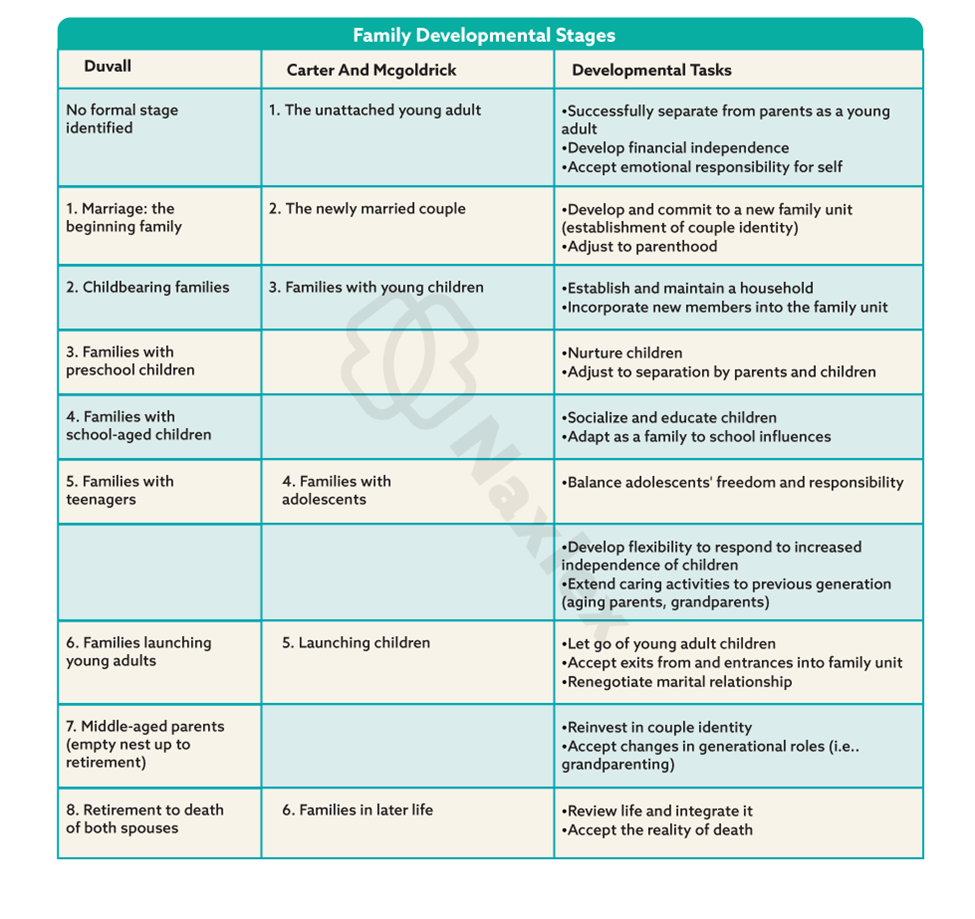
Which of the following is one of the developmental tasks of the older adult family?
Explanation
As individuals age, both personal and family roles evolve. Understanding the common challenges and adjustments that older adult families face helps nurses provide age-appropriate emotional, psychological, and social support to enhance the well-being of aging clients and their families.
Rationale for correct answer:
D.Adjust to loss of spouse: A significant task of older adulthood is coping with bereavement, especially the loss of a life partner. This stage involves emotional adjustment, restructuring daily life, and often increased dependence on extended family or community resources.
Rationale for incorrect answers:
A.Maintain a supportive home base: While maintaining a home environment is important, this is more relevant to middle adulthood when parents are actively supporting children or young adults.
B. Prepare for retirement: Preparing for retirement is a developmental task of late middle age, not of the older adult stage. By older adulthood, most individuals have already retired and are adjusting to its realities.
C. Cope with loss of energy and privacy: This is more associated with the childbearing or child-rearing stage, where new parents experience fatigue and reduced personal space due to parenting demands.
Take-home points:
- Adjusting to the loss of a spouse is a critical developmental challenge in older adulthood that impacts emotional well-being and daily functioning.
- Developmental tasks vary by life stage and help guide nurses in tailoring care and support to meet age-specific psychosocial needs.
Which of the following is one element of a healthy community?
Explanation
A healthy community supports the well-being of its residents by promoting safety, access to services, environmental health, and social support.
Rationale for correct answer:
B. Offers access to healthcare services: A key component of a healthy community is equitable access to healthcare services. This ensures residents can receive preventive care, treatment, and health education, improving overall health outcomes.
Rationale for incorrect answers:
A.Meets all the needs of its inhabitants: No community can meet all the needs of every resident. This choice is overly idealistic and unrealistic, making it inaccurate as a defining element.
C. Has mixed residential and industrial areas: Mixing industrial and residential zones can lead to environmental hazards (e.g., noise, pollution) and may compromise public safety, which is not ideal for community health.
D. Is little concerned with air and water quality: Clean air and water are critical to community health. Lack of concern for environmental quality leads to increased disease burden (e.g., respiratory illness, waterborne infections).
Take-home points:
- Access to healthcare is essential in a healthy community-it supports disease prevention, timely treatment, and health promotion.
- Environmental safety and thoughtful urban planning (e.g., separating industrial zones from homes) are vital to protect and maintain public health.
Exams on Individual & Family Health And Community Based Practice
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe each level of Maslow’s hierarchy of basic human needs.
- Explain nursing care necessary to meet needs for each level of Maslow’s hierarchy.
- Discuss family concepts, including family roles, structures, functions, developmental stages, tasks, and health risk factors.
- Identify aspects of the community that affect individual and family health.
- Discuss the role of the community health nurse.
- Discuss the role of the nurse in community-based practice
- Explain the relationship between public health and community health nursing
Introduction
Community-based health care is a collaborative, patient-centered approach to provide culturally appropriate health care within a community.
Community-based care focuses on health promotion, disease prevention, and restorative care.
A healthy community includes elements that maintain a high quality of life and productivity, such as access to health services, preventive care, nutrition, safety, physical activity, oral health, and environmental quality.
Individual Health
Basic Human Needs
Something is a basic need if it has the following characteristics:
- Its absence results in illness.
- Its presence helps prevent illness or signals health.
- Meeting it restores health.
- It is preferred over other satisfactions when unmet.
- One feels something is missing when the need is unmet.
- One feels satisfaction when the need is met.
Abraham Maslow (1968) developed a hierarchy of basic human needs that can be used to consider which needs of a person are the most important at any given time.
Maslow’s hierarchy is useful for understanding the relationships of basic human needs and for establishing priorities of care. The 5 levels of needs:
Level 1: Physiologic needs
Level 2: Safety and security needs
Level 3: Love and belonging needs
Level 4: Self-esteem needs
Level 5: Self-actualization needs

Physiologic needs
Physiologic needs-oxygen, water, food, temperature, elimination, sexuality, physical activity, and rest-must be met at least minimally to maintain life.
Safety and security needs
Physical safety and security means being protected from potential or actual harm.
Nurses carry out a wide variety of activities to meet patients’ physical safety needs, such as the following:
- Using proper hand hygiene and sterile techniques to prevent infection
- Using electrical equipment properly
- Administering medications knowledgeably
- Using skill when moving and ambulating patients
- Teaching parents about household chemicals that are dangerous to children
Love and belonging needs
Include the understanding and acceptance of others in both giving and receiving love, and the feeling of belonging to families, peers, friends, a neighborhood, and a community.
Some nursing interventions to help meet this need are as follows:
- Including family and friends in the care of the patient
- Establishing a nurse–patient relationship based on mutual understanding and trust (by demonstrating caring, encouraging communication, and respecting privacy)
- Referring patients to specific support groups (such as a cancer support group or Alcoholics Anonymous)
Self-esteem needs
Include the need for a person to feel good about himself or herself, to feel pride and a sense of accomplishment, and to believe that others also respect and appreciate those accomplishments.
Nurses can help meet patients’ self-esteem needs by respecting their values and beliefs, encouraging patients to set attainable goals, and facilitating support from family or significant others.
Self-actualization needs
Include the need for individuals to reach their full potential through development of their unique capabilities. In general, each lower level of need must be met to some degree before this need can be satisfied.
Maslow lists the following qualities that indicate achievement of one’s potential:
- Acceptance of self and others as they are
- Focus of interest on problems outside oneself
- Ability to be objective
- Feelings of happiness and affection for others
- Respect for all people
- Ability to discriminate between good and evil
- Creativity as a guideline for solving problems and pursuing interests
Applying Maslow’s Theory
Nurses can apply Maslow’s hierarchy of basic needs in the assessment, planning, implementation, and evaluation of patient care.
As the nurse identifies and carries out interventions to help meet patients’ needs, it is important to remember that this is only a framework or guideline and that, in actuality, each individual sets priorities for meeting needs on levels most important to that person.
Nursing Insights:
- Nursing care is often directed toward meeting unmet or threatened needs.
- Maslow’s hierarchy provides a framework for nursing assessment and for understanding the needs of patients at all levels, so that interventions to meet priority needs become a part of the plan of care.
Family Health
A family is a dynamic system of people living together who are united by significant emotional bonds.
Family structure is the form that a family takes in order to maintain function.
Types of families include, but are not limited to, the following:
- Nuclear family-composed of husband, wife, and children (naturally conceived, adopted, or both)
- Blended family-combination of two divorced families through remarriage; may include stepchildren, halfsiblings, or combinations
- Extended family-usually members of a nuclear family and other blood-related people (such as grandparents, aunts, uncles, and cousins)
Family roles are the behaviors expected of family members. These roles are learned and transmitted within the family unit and help the family to fulfill its functions.
Family roles include, but are not limited to, the following:
- Nurturance and support
- Allocation of resources
- Development of life skills
- Division of labor
- Socialization of members
Family functions are the roles that allow family members to adapt in order to develop as individuals and as members of the family unit.
Family development theories:
The family unit has a developmental process with expected tasks that are to be achieved at each developmental stage.
The family that achieves specific developmental tasks is considered to be a healthy family.
The way in which a family achieves the tasks of one developmental stage greatly influences the family’s ability to handle subsequent developmental issues.
- Duvall’s model: Based on classic work of Duvall and Miller. Duvall’s theory is somewhat limited in that it assumes that the family unit consists of a married couple that becomes involved in child-rearing activities.
- Carter and McGoldrick’s (2004) model: Describes six stages of the family life cycle that are more reflective of adult needs in current society.
Threats to Family Integrity:
Domestic violence:
Occurs in all socioeconomic groups, is an ever-increasing social problem. Several studies document the harmful effects of family violence that may include acute trauma, death, unwanted pregnancy, depression, suicide, posttraumatic stress disorder, and substance abuse.
Child abuse:
Many factors are related to child abuse and neglect. These factors include stress, financial problems, inadequate parenting skills, parental substance abuse, parental impulsivity, social isolation, and parents themselves being abused as children.
Older adult abuse:
Maltreatment of older adults takes many forms, including physical, sexual, and psychological abuse and financial exploitation
Spouse and partner abuse:
The vast majority of assaults by partners are directed at women. Women are also at greater risk than men for being killed during intimate partner violence.
Poverty:
Food insecurity occurs when a member of a household has an altered eating pattern as a result of lack of money for food. There are higher rates of health problems in families affected by food insecurity.
Nursing response to family violence
Detecting Abuse
Home health and public health nurses have a unique opportunity to detect indicators of abuse (in children, elders, and intimate partners). Assessing the home and community environment can provide cues to abuse and, thus, trigger early intervention.
Levels of Prevention of Child Abuse:
- Primary:
- Parenting classes that provide information about childhood growth and development
- Identification of at-risk households
- Telephone ‘‘hot lines’’ for parents who are feeling out of control
- Secondary:
- Behavior management programs for at-risk families, such as those referred to child protective services
- Assessment of signs of abuse
- Tertiary:
- Removal of children from homes with abusive parents
- Family therapy for abusive parents
Nursing insights:
-Family structure is the form that a family takes in order to maintain function. Family structures vary depending on cultural context.
-Family functions are the roles that allow family members to adapt in order to develop as individuals and as members of the family unit.
-A healthy family is characterized by these traits:
- communicates and listens
- supports its members
- teaches respect for others
- develops trust
- plays and shares a sense of humor
- has a strong sense of family (as evidenced by rituals and traditions)
- seeks help with problems as necessary
Community Health
A community is a collection of people who share some attributes of their lives and interact with each other in some way.
A population is composed of people who share some common characteristics but who do not necessarily interact with each other.
Community health nursing focuses on promoting and preserving the health of population groups.
5 main functions of a community:
- Production, distribution, and consumption of goods and services: These are the means by which the community provides for the economic needs of its members
- Socialization: Socialization refers to the process of transmitting values, knowledge, culture, and skills to others.
- Social control: Social control refers to the way in which order is maintained in a community.
- Social interparticipation: Social interparticipation refers to community activities that are designed to meet people’s needs for companionship.
- Mutual support: Mutual support refers to the community’s ability to provide resources at a time of illness or disaster
Ten Characteristics of a healthy community
- Is one in which members have a high degree of awareness of being a community.
- Uses its natural resources while taking steps to conserve them for future generations.
- Openly recognizes the existence of subgroups and welcomes their participation in community affairs.
- Is prepared to meet crises.
- Is a problem-solving community; it identifies, analyzes, and organizes to meet its own needs.
- Possesses open channels of communication that allow information to flow among all subgroups of citizens in all directions.
- Seeks to make each of its systems’ resources available to all members.
- Has legitimate and effective ways to settle disputes that arise within the community.
- Encourages maximum citizen participation in decision making.
- Promotes a high level of wellness among all its members.
Community-based healthcare:
Community-based health care (CBHC) is a PHC system that provides health-related services within the context of people’s daily lives-that is, in places where people spend their time, for example, in the home, in shelters, in long-term care residences, at work, in schools, in senior citizens’ centers, in ambulatory settings, and in hospitals.
In contrast to the traditional health care system that focuses primarily on those who are ill or injured, community-based care is holistic.
It involves a broad range of services designed not only to restore health but also to promote health, prevent illness, and protect the public.
To be truly effective, a CBHC system needs to:
- provide easy access to care
- be flexible in responding to the care needs that individuals and families identify
- promote care between and among health care agencies through improved communication mechanisms
- provide appropriate support for family caregivers
- be affordable.
Community-Based Settings
Traditionally, community nursing services have been provided in county and state health departments (public health nursing), in schools (school nursing), in workplaces (occupational nursing), and in homes (home health care and hospice nursing).
Over the years, numerous other settings have been established, including day care centers, senior centers, storefront clinics, homeless shelters, mental health centers, crisis centers, drug rehabilitation programs, and ambulatory care centers.
More recent settings for community nursing practice include nurse-managed community nursing centers, parish nursing, corrections nursing, and telehealth projects.
Community factors affecting health
- Number and availability of healthcare institutions and services
- Housing codes
- Police and fire departments
- Nutritional services for low-income infants, mothers, school-aged children (e.g., lunch programs), and older people
- Zoning regulations separating residential and industrial areas
- Waste disposal services and locations
- Air and water pollution
- Food sanitation
- Health education services and dissemination
- Recreational opportunities
- Violent crimes or drug use
Competencies Required for Community-Based Care
Nurses practicing in community-based integrated health care systems need to have specialized knowledge and skills.
In 1998, the Pew Health Professions Commission identified 21 competencies that future health professionals would require. Include:
-
- Embrace a personal ethic of social responsibility and service.
- Exhibit ethical behavior in all professional activities.
- Provide evidence-based, clinically competent care.
- Incorporate the multiple determinants of health in clinical care.
- Apply knowledge of the new sciences.
- Demonstrate critical thinking, reflection, and problem-solving skills.
- Understand the role of primary care.
- Rigorously practice preventive health care.
- Integrate population-based care and services into practice.
- Improve access to health care for those with unmet health needs.
- Practice relationship-centered care with individuals and families.
- Provide culturally sensitive care to a diverse society.
- Partner with communities in health care decisions.
- Use communication and information technology effectively and appropriately.
- Work in interdisciplinary teams.
- Ensure care that balances individual, professional, system, and societal needs.
- Practice leadership.
- Take responsibility for quality of care and health outcomes at all levels.
- Contribute to continuous improvement of the health care system.
- Advocate for public policy that promotes and protects the health of the public.
- Continue to learn and help others learn.
Community assessment
Community assessment is the systematic data collection on the population, monitoring the health status of the population, and making information available about the health of the community.
This is the environment in which patients live, work, play, and learn. Without an adequate understanding of that environment, any effort to promote a patient’s health and bring about necessary change is unlikely to be successful.
The community has three components: structure or locale, the people, and the social systems
Structure
• Name of community or neighborhood
• Geographical boundaries
• Emergency services
• Water and sanitation
• Housing
• Economic status (e.g., average household income, number of residents on public assistance)
• Transportation
• Safety
Population
• Age distribution
• Sex distribution Growth trends
• Density
• Education level
• Predominant ethnic groups
• Predominant religious groups
Social system
• Educational system
• Government
• Communication system
• Welfare system
• Volunteer programs
• Health system
Once you have a good understanding of the community, you can perform all individual patient assessments against that background.
Role of the nurse in community-based practice:
- Caregiver.
- Case managers establish an appropriate plan of care based on assessment of patients and families and coordinate needed resources and services for a patient’s wellbeing across a continuum of care.
- Change agent: This involves identifying and implementing new and more effective approaches to problems.
- Patient advocate: Ensure patients have the information necessary to make informed decisions in choosing and using services appropriately.
- Collaborator: Working in a combined effort with all those involved in care delivery, is necessary to develop a mutually acceptable plan that will achieve common goals.
- Counselor: Helps patients identify and clarify health problems as well as choose appropriate courses of action to solve those problems.
- Educator: Patients and families need to gain skills and knowledge to care for themselves.
- Epidemiologist: Apply principles of epidemiology, the science dealing with the incidence, distribution, and possible control of diseases and other health problems.
Public health nursing:
Public health nursing is a specialization within community-based nursing.
The public health perspective focuses on prevention as opposed to illness. In order to promote community health, public health nurses perform the following functions:
- Prevention of epidemics and spread of disease
- Protection against environmental hazards
- Prevention of injuries
- Promotion of health behaviors
- Response to disasters
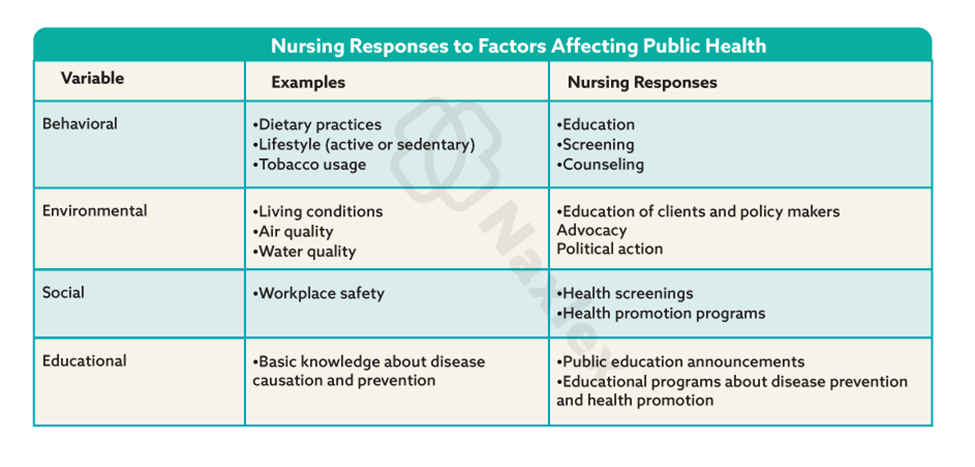
Social determinants of health
Social determinants of health are biological, socioeconomic, psychosocial, behavioral, or social factors that contribute to a person’s current state of health. Healthy People 2030 lists five determinants of health that are grouped into five domains:
- economic stability
- education access and quality
- health care access and quality
- neighborhood and built environment
- social and community context
Vulnerable populations
Vulnerable populations are groups of patients who are more likely to develop health problems because of excess health risks, who are limited in their access to health care services, or who depend on others for care.
Vulnerable populations include:
- those living in poverty
- older adults
- the disabled
- people who are homeless
- immigrants
- individuals in abusive relationships
- people living with substance abuse
- people with mental illnesses
These vulnerabilities are often associated with the individual’s/community’s social determinants of health or individual health disparities.
Public and community health nursing and primary care providers share health care responsibility for health promotion, screening, and early detection and disease prevention for vulnerable populations
Nursing insights:
-Community-based nursing focuses on individuals, families, and aggregates living and working within a community.
-The major goal of community health nursing is the preservation and improvement of the health of populations and communities worldwide.
-Public health nurses perform the following functions:
- prevention of epidemics and spread of disease
- protection against environmental hazards
- prevention of injuries
- promotion of health behaviors
- response to disasters.
Summary
- A family is a dynamic system of people living together who are united by significant emotional bonds.
- Healthy families are often described as functional, in that they are able to cope with stressors and deal with crises as they arise.
- Community health nurses practice in neighborhoods and homes in rural and urban areas. Settings in which community health nurses commonly practice include primary care offices, schools, workplaces, and public health units.
- The public health perspective focuses on prevention as opposed to illness.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Individual & Family Health And Community Based Practice
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


