Please set your exam date
Health Supervision In Children
Study Questions
Practice Exercise 1
A child who was recently adopted internationally presents for their first health supervision visit. The nurse should be most concerned with:
Explanation
Correct answer: 3
In the United States, internationally adopted children are those who have been adopted by U.S. citizens from countries outside the U.S. This process is known as intercountry adoption, and it involves both adoption and immigration procedures.
Rationale for correct answer:
C. Incomplete immunization records and potential infectious diseases is the most urgent concern because it poses immediate public health and personal health risks. The nurse should initiate serologic testing for vaccine-preventable diseases, perform screenings for tuberculosis, hepatitis, HIV, and parasites, and plan catch-up immunizations according to CDC guidelines. Early detection prevents complications and protects others.
Rationale for incorrect answers:
A. Social and behavioral problems may occur, especially with attachment and adjustment, but they are not immediately life-threatening and can be addressed after urgent infectious disease concerns are managed.
B. While language barriers may impact communication and school readiness, they do not pose an urgent health risk; interpreters and language support can be arranged as part of long-term care.
D. Nutritional deficiencies such as iron and vitamin D are common in international adoptions and should be addressed, but they are typically less urgent than communicable disease control.
Take home points
- Newly adopted international children require comprehensive medical screening, including infectious disease testing and immunization verification.
- Catch-up vaccination should be started promptly if records are missing or unreliable.
- Nutritional, developmental, and behavioral assessments are important but follow after urgent public health safety measures.
- Early coordination with specialists such as infectious disease and developmental pediatrics can improve outcomes for internationally adopted children.
Which facility fulfills the characteristics of a medical home?
Explanation
A medical home is not a physical building but a model of care in which a primary care provider offers accessible, continuous, comprehensive, family-centered, coordinated, compassionate, and culturally effective care. It is the central place where all of a child’s healthcare needs are managed, including preventive care, acute care, chronic illness management, and coordination with specialists.
Rationale for correct answer:
B. A primary care pediatric practice provides continuity of care, maintains complete health records, and coordinates referrals to specialists. It fosters an ongoing relationship between the family and healthcare providers, which is central to the medical home concept.
Rationale for incorrect answers:
A. An urgent care center provides episodic, short-term treatment for acute illnesses or injuries, not ongoing comprehensive care.
C. A mobile outreach immunization program delivers a specific preventive service but does not coordinate or manage overall healthcare needs.
D. A dermatology practice focuses on a single specialty; does not provide comprehensive primary care or coordinate all aspects of a patient’s health.
Take home points
- A medical home is characterized by continuous, coordinated, and comprehensive care, not just a location.
- Primary care providers, especially in pediatrics, serve as the central point for managing a child’s preventive, acute, and chronic care needs.
- Specialty or urgent services can support the medical home but cannot replace it.
Practice Exercise 2
A nurse is conducting a 9-month well-child visit. Which of the following screening tests is most likely to be recommended at this age?
Explanation
Screening tests in children are essential components of preventive health care, designed to detect potential health issues before symptoms arise. These tests help identify children at risk for certain conditions so that early interventions can be made.
Rationale for correct answer:
C. Iron deficiency anemia screening based on risk factors: At 9 months, this is the most relevant screening. Infants in high-risk groups should have hemoglobin or hematocrit checked earlier than the universal 12-month screening. Early detection ensures timely dietary counseling and supplementation if needed.
Rationale for incorrect answers:
A. Blood pressure screening: Routine BP measurement typically starts at age 3 years unless there are risk factors such as congenital heart disease or kidney problems.
B. Lead screening for all children: Universal screening is not done at 9 months for all children; instead, lead testing is typically recommended at 12 and 24 months or earlier if specific risk factors are present.
D. Hyperlipidemia screening: Routine lipid screening is generally recommended between ages 9–11 years and again at 17–21 years, unless there is a strong family history of early cardiovascular disease.
Take home points
- At 9 months, iron deficiency anemia screening is risk-based, with universal testing at 12 months.
- Blood pressure, lead, and lipid screenings have different recommended ages and are not routine at this visit for healthy infants.
- Early detection of anemia supports optimal cognitive and motor development.
The nurse is providing anticipatory guidance to the mother of a 6-month-old infant. What is the best instruction by the nurse in relation to the infant’s oral health?
Explanation
Oral health is tightly connected to nutrition. Poor oral hygiene can lead to early childhood caries, which may affect an infant’s ability to eat comfortably and get adequate nutrients. Starting oral hygiene early promotes healthy feeding and supports lifelong dental habits.
Rationale for correct answer:
C. The best practice is to begin oral hygiene before teeth erupt by cleaning the gums with a soft, damp washcloth. Once teeth emerge (typically around 6 months), continue cleaning with a washcloth or soft infant toothbrush without toothpaste. This practice reduces bacterial growth and helps the infant get used to oral care routines.
Rationale for incorrect answers:
A. Oral care should begin before tooth eruption, not after full dentition. Delaying increases risk of early childhood caries.
B. Infants should not use toothpaste until at least age 12–18 months, and even then, only a rice-grain amount of fluoride toothpaste under supervision. Toothpaste is not needed for early oral cleaning.
D. Rinsing is not necessary and may pose a choking hazard in young infants. Instead, cleaning with a washcloth is safer and more effective for removing milk residue and bacteria.
Take home points
- Begin oral care before teeth erupt using a damp washcloth to clean gums.
- Continue daily cleaning as new teeth come in to promote healthy oral development.
- Avoid toothpaste in infants under 12 months unless directed by a dentist.
- Early oral hygiene helps prevent nutritional disruptions due to dental discomfort or caries and builds lifelong habits.
A nurse is educating a parent regarding the immunizations that a child is to receive during the
Explanation
- Polio vaccine is part of the first-year immunization schedule, typically at 2, 4, and 6 months.
- MMR (measles, mumps, rubella) is not given until after the first year (12–15 months).
- Nurses should use calm, supportive language to explain vaccine timing and importance.
- Accurate vaccine education helps reduce hesitancy and strengthens caregiver confidence in health decisions.
A mother of an 8-month-old boy states that the family is vacationing in a beach house for the next 2
weeks. Which of the following information should the nurse educate the mother about in relation to sun exposure? Select all that apply
Explanation
Sun exposure refers to the amount of time a child’s skin is exposed to ultraviolet (UV) rays from the sun. While some sunlight is beneficial by helping the body produce vitamin D, it also carries risks, especially for children, whose skin is more delicate and sensitive than adults.
Rationale for correct answers:
B. Broad-spectrum sunscreen offers protection from both types of harmful ultraviolet radiation. UVA contributes to skin aging, while UVB causes sunburn. For infants over 6 months, using a broad-spectrum, SPF 30 or higher sunscreen on exposed skin is recommended.
C. UV rays can damage the eyes. Sunglasses that block 100% of UVA and UVB rays help protect the infant’s developing eyes from long-term harm like cataracts or retinal damage.
E. Lightweight, long-sleeved shirts and pants offer effective physical protection from the sun. A wide-brimmed hat also helps shield the face and neck.
Rationale for incorrect answers:
A. Sunscreen should be reapplied every 2 hours or more frequently if the child is sweating or in water, even if the sunscreen is labeled as “water-resistant.” Waiting 4–6 hours between applications is insufficient.
D. The most intense sun exposure occurs between 10 a.m. and 4 p.m., not just 12–2 p.m. During these hours, children should be kept in the shade, wear protective clothing, and have sunscreen applied to exposed areas.
Take home points
- Infants over 6 months should use broad-spectrum sunscreen and wear protective clothing and sunglasses.
- Reapply sunscreen every 2 hours or after swimming/sweating.
- Avoid sun exposure between 10 a.m. and 4 p.m., not just midday.
- Therapeutic teaching should empower caregivers to enjoy outdoor activities safely, using clear, supportive communication.
A nurse advises the parent of a 2-year-old that the child will have blood drawn during that day’s
well-child checkup. The nurse should advise the parents that the child’s blood levels are being checked for which of the following substances?
Explanation
At 2 years of age, children are especially vulnerable to environmental toxins due to increased hand-to-mouth activity, crawling, and developing neurological systems. During well-child visits, nurses and providers screen for exposures that can impact long-term growth and development.
Rationale for correct answer:
C. Lead screening is routinely recommended for children at 12 and 24 months, particularly for those at increased risk such as living in older homes, exposed to peeling paint, or residing in areas with known environmental risks. Lead is a neurotoxin that can cause cognitive delays, attention problems, and behavioral issues, even at low blood levels.
Rationale for incorrect answers:
A. Routine calcium level screening is not indicated during a standard well-child visit unless there is a specific medical concern, such as rickets or a metabolic disorder.
B. Mercury testing is only done if there is known exposure, such as from contaminated fish or environmental sources. It is not part of routine screening in toddlers.
D. Fluoride is important for dental health, but its levels are not typically measured in blood. Instead, fluoride exposure is assessed through water source and dental hygiene practices.
Take home points
- Lead screening is standard at the 1- and 2-year well-child visits, especially for children in high-risk environments.
- Lead exposure can be asymptomatic but harmful, making early detection critical.
- Nurses should educate parents on lead prevention, such as avoiding peeling paint, using cold tap water for cooking, and maintaining good hygiene practices.
- Routine testing for mercury, calcium, or fluoride is not part of standard 2-year-old care unless clinically indicated.
A nurse is providing health promotion education to a 10-year-old child during a well-child clinic visit.
Which of the following is an appropriate patientcare goal for the teaching session? The child will:
Explanation
Health promotion for school-age children includes education on nutrition, physical activity, dental hygiene, injury prevention, and immunizations. At this stage, children begin to take more personal responsibility for their health behaviors, and nurses play a crucial role in reinforcing developmentally appropriate preventive practices during routine visits.
Rationale for correct answer:
A. Dental hygiene is a key area of health promotion for 10-year-olds. Brushing twice daily with fluoride toothpaste helps prevent cavities and gum disease, which are common issues in this age group. This goal is age-appropriate, promotes daily self-care, and aligns with recommended guidelines from dental associations.
Rationale for incorrect answers:
B. The first dose of meningococcal conjugate vaccine (MenACWY) is recommended at age 11–12, not at age 10. Therefore, this is premature for a 10-year-old child during a routine visit.
C. While swimming lessons are encouraged earlier in childhood, this statement is not a measurable or time-specific goal for a 10-year-old. It’s too vague and lacks the clarity needed for an actionable teaching objective during a clinic visit.
D. Bicyclists should ride on the right-hand side of the road, going with the flow of traffic, not against it. Teaching otherwise increases the risk of injury.
Take home points
- Daily dental hygiene using fluoride toothpaste is essential and age-appropriate for school-age children.
- Meningococcal vaccination begins at age 11–12, not 10.
- Safety education should include correct bicycle riding practices, including riding with traffic.
- Health goals for children should be specific, measurable, realistic, and developmentally appropriate.
Comprehensive Questions
During the health interview, the mother of a 4-month-old says, “I’m not sure my baby is doing what he should be.” What is the nurse’s best response?
Explanation
When a parent expresses worry about their child’s development, the nurse’s role is to use therapeutic communication to explore the concern. This approach builds trust, encourages information sharing, and provides a clearer understanding of the child’s developmental progress.
Rationale for correct answer:
C. “Tell me more about your concerns.” This is an open-ended, supportive, and nonjudgmental response that invites the mother to elaborate on her observations. It validates her feelings and gives the nurse important context to guide further assessment and screening.
Rationale for incorrect answers:
A. “I’ll be able to tell you more after I do his physical.” This delays addressing her concern and shuts down immediate dialogue. It also misses the opportunity to gather parental insight.
B. “Fill out this developmental screening questionnaire and then I can let you know.” While screening tools are important, jumping to paperwork before discussion can feel impersonal and may overlook key details.
D. “All mothers worry about their babies. I’m sure he’s doing well.” This dismisses the mother’s concern, risks invalidating her feelings, and could prevent disclosure of important developmental issues.
Take home points
- Use open-ended questions to explore caregiver concerns in detail.
- Parents are often the first to notice subtle developmental delays.
- Therapeutic communication strengthens the nurse–family relationship and guides appropriate screening or referral.
- Avoid responses that dismiss or minimize parental concerns.
An infant boy is at your facility for his initial health supervision visit. He is 2 weeks old and responds to a bell during his examination. You review all his birth records and find no documentation that a newborn hearing screening was performed. What is the best action by the nurse?
Explanation
Universal newborn hearing screening is recommended for all infants before 1 month of age to detect congenital hearing loss early. Even if an infant appears to respond to sound, this does not rule out mild, unilateral, or frequency-specific hearing loss that could affect speech and language development.
Rationale for Correct Answer:
B. Schedule the infant immediately for newborn hearing screening: The absence of documented screening means the infant’s hearing status is unknown. Formal screening (e.g., otoacoustic emissions [OAE] or auditory brainstem response [ABR]) is necessary, as informal bedside tests with bells or voices are not accurate diagnostic tools.
Rationale for incorrect answers:
A. Do nothing; responding to the bell proves the infant does not have a hearing deficit: This is incorrect because informal sound-response checks can miss partial or frequency-specific hearing loss.
C. Ask the mother to observe for signs that the infant is not hearing well: Observation alone is unreliable for early detection; delays in diagnosis can harm speech and language development.
D. Screen again with the bell at the infant’s 2-month visit: Waiting risks missing the early intervention window and using an inaccurate method.
Take home points
- All infants should have a documented newborn hearing screening before 1 month of age.
- Informal sound checks are not a substitute for standardized screening methods like OAE or ABR.
- Early identification and intervention for hearing loss significantly improve language and developmental outcomes.
- If screening was missed, it should be scheduled immediately, even if the infant appears to respond to sound.
A 15-month-old girl is having her first health supervision visit at your facility. Her mother has not brought a copy of the child’s immunization record but believes she is fully immunized: “She had immunizations 3 months ago at the local health department.” Which would be the best action by the nurse?
Explanation
Accurate immunization documentation is essential to ensure children are up to date and to avoid unnecessary repeat vaccinations. Verbal reports from caregivers are not reliable evidence of vaccination status.
Rationale for correct answer:
D. Calling the local health department and verifying the child’s immunization status allows the nurse to confirm exactly which vaccines were given and when, ensuring the child’s immunization schedule remains accurate and avoiding unnecessary repeats or missed doses. This is the safest and most efficient action.
Rationale for incorrect answers:
A. Asking the mother to bring the records to the 18-month health supervision visit delays verification and could result in a missed opportunity to update needed immunizations promptly.
B. Starting the “catch-up” schedule because there are no immunization records could lead to unnecessary repeat vaccinations, discomfort, and expense if the child is actually up to date.
C. Keeping the child at the facility while the mother returns home for the records is inconvenient for the family and unnecessary when verification can be done quickly through a phone call to the local health department.
Take home points
- Always verify immunization status using written, official records or direct confirmation from the provider who administered the vaccines.
- Verbal caregiver reports are not sufficient for documentation.
- Prompt verification prevents unnecessary repeat doses and ensures the child is adequately protected.
- Health departments and immunization registries are valuable resources for confirming vaccination history.
A 4-year-old child is having a vision screening performed. Which screening chart would be best for determining the child’s visual acuity?
Explanation
Vision screening in preschool-aged children requires tools that match their developmental level. Many 4-year-olds cannot consistently recognize letters, so charts that use symbols or simple pictures are preferred.
Rationale for correct answer:
D. The Cardiff Visual Acuity Test for Matching or Estimation (CVTME) is specifically designed for young children, this chart uses simple, recognizable images arranged to measure acuity reliably in preschoolers. It’s ideal for children around 3–5 years old who may not know their letters but can identify or match pictures.
Rationale for incorrect answers:
A. Snellen uses letters and requires literacy or letter recognition; generally more suitable for children ≥6 years old.
B. Ishihara is used to assess color vision, not visual acuity; inappropriate for standard acuity screening.
C. Allen figures uses familiar pictures (e.g., animals, objects) and is also suitable for young children, but CVTME is considered more accurate and developmentally appropriate for a 4-year-old’s formal acuity testing.
Take home points
- Vision screening should be adapted to the child’s developmental and cognitive level.
- For preschoolers who cannot read letters, picture-based charts like CVTME or Allen figures are preferred.
- Snellen charts are for older children and adults, while Ishihara is for color vision testing only.
- Early detection of vision problems prevents long-term learning and developmental difficulties.
When should the child’s first examination by a dentist occur?
Explanation
The American Academy of Pediatrics (AAP) and the American Academy of Pediatric Dentistry (AAPD) recommend that a child’s first dental visit occur within 6 months of the first tooth eruption and no later than 12 months of age.
Rationale for correct answer:
A. By the first birthday: This allows early detection of oral health problems, parent education on brushing, fluoride use, and diet, and establishes a dental home for the child. Early visits also help the child become comfortable with dental care.
Rationale for incorrect answers:
B. By the second birthday: This delays preventive education and may allow dental decay to progress before intervention.
C. By entry into kindergarten: Far too late for prevention; caries and other oral health issues can already be advanced by this age.
D. By entry into first grade: This is well beyond the ideal window for establishing preventive oral health practices and may lead to missed opportunities for early intervention.
Take home points
- First dental visit: by 12 months or within 6 months of first tooth eruption.
- Early visits focus on prevention, education, and risk assessment.
- Establishing a dental home early supports lifelong oral health habits.
- Parents should be taught to clean the infant’s gums and teeth with a soft cloth or brush and avoid prolonged bottle use, especially at night.
An experienced nurse is orienting a new nurse to the care of children in a clinic. Which immunizations
should the experienced nurse inform the new nurse to plan to administer to normally healthy children between ages 1 and 5 years? Select all that apply
Explanation
Vaccinations in children are a cornerstone of preventive health care, protecting them from serious and potentially life-threatening diseases. They work by stimulating the immune system to recognize and fight specific pathogens before a child is exposed to them naturally. Between the ages of 1 and 5 years, children receive routine booster doses of key vaccines to maintain immunity against serious diseases.
Rationale for correct answers:
A. Inactivated poliovirus (IPV) booster doses are given between ages 4–6 years after the primary series in infancy.
B. The 5th dose of Diphtheria, tetanus, pertussis (DTaP) is given at 4–6 years to maintain protection.
C. The second dose of Measles, mumps, rubella (MMR) is given between 4–6 years for long-term immunity.
Rationale for incorrect answers:
D. The Hepatitis B (HepB) series is typically completed by 6–18 months of age, so it is not routinely given to healthy children aged 1–5 unless they are catching up.
E. The first routine dose of meningococcal vaccine is recommended at 11–12 years for healthy children, unless earlier vaccination is indicated for high-risk groups.
Take home points
- Ages 4–6 years are key for booster doses before school entry (DTaP, IPV, MMR, Varicella).
- HepB and meningococcal vaccines are not routine in healthy 1–5-year-olds unless catch-up or high-risk.
- Following the national immunization schedule ensures timely, lasting protection.
A school nurse is teaching adolescents about oral care. Which point should the nurse address with the
Explanation
Good oral hygiene during adolescence is critical for preventing cavities, gingivitis, periodontal disease, and bad breath. This age group often experiences increased sugar intake, orthodontic appliances, and sometimes lapses in hygiene habits. Professional dental visits twice a year allow for preventive care, early detection of issues, and reinforcement of healthy habits.
Rationale for correct answer:
A. Floss daily, brush teeth twice a day, and see the dentist two times per year: This follows the American Dental Association (ADA) recommendations for maintaining optimal oral health. Brushing removes plaque from tooth surfaces, flossing cleans between teeth where a brush can’t reach, and regular dental visits provide professional cleaning and monitoring.
Rationale for incorrect answers:
B. Brushing only once daily is insufficient to remove plaque and food debris effectively.
C. Annual dental visits may delay diagnosis and treatment of problems; twice-yearly visits are preferred.
D. Flossing and brushing habits are good here, but annual visits alone may not provide the best preventive care.
Take home points
- Adolescents should brush twice daily with fluoride toothpaste and floss once daily.
- Professional dental visits twice yearly help maintain oral health and prevent disease.
- Teaching should emphasize the link between oral health and overall health, including heart health, nutrition, and self-esteem.
Exams on Health Supervision In Children
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the objectives of health supervision for children.
- Discuss the principles guiding health supervision, including the concept of a medical home.
- Identify the components of a comprehensive health supervision visit.
- Explain the importance of developmental surveillance and screening.
- Summarize key injury and disease prevention strategies, including common screening tests and the immunization schedule.
- Recognize the role of anticipatory guidance and health promotion in pediatric care.
- Understand special issues in health supervision, such as cultural influences and caring for children with chronic illnesses or those adopted internationally.
Introduction
- Health supervision, also known as well-child care, is a proactive, preventative approach to healthcare that focuses on the ongoing needs of children from birth through adolescence.
- Unlike sick visits, which address acute illnesses, well-child visits are designed to promote optimal physical, cognitive, and psychosocial development.
- These regular visits are a cornerstone of modern pediatrics, aiming to keep children healthy rather than just treating them when they are sick.
- The primary objective of health supervision is to ensure a child's optimal physical, mental, and developmental well-being. The main goals include:
- Preventing Illness and Injury: This is the most crucial goal. Well-child visits provide an opportunity to administer necessary immunizations and offer guidance on injury prevention (e.g., car seat safety, poison control).
- Monitoring Growth and Development: The healthcare provider tracks a child's growth using charts for weight, height, and head circumference. They also assess developmental milestones, such as language skills, motor skills, and cognitive abilities.
- Early Detection and Screening: These visits are essential for identifying health problems early, before they become serious. Screenings may include tests for hearing, vision, anemia, lead poisoning, and developmental disorders.
- Health Promotion and Education: Healthcare providers provide anticipatory guidance to parents and caregivers. This includes advice on nutrition, sleep habits, behavior, and what to expect as the child grows.
- Building a Relationship: Regular visits help establish a trusting relationship between the child, the family, and the healthcare provider. This creates a safe space for parents to ask questions and discuss concerns.
Principles of Health Supervision
3.1. Wellness
- Health supervision is centered on the concept of wellness, which goes beyond the absence of disease. It emphasizes a holistic view of a child's health, encompassing physical, emotional, social, and mental well-being.
- This principle focuses on strengthening a child's health and protective factors, such as strong family bonds and positive peer relationships, rather than just treating problems after they arise.
3.2. Medical Home
A medical home is a model of care that is accessible, continuous, comprehensive, family-centered, coordinated, and compassionate. It's not a physical place but rather a partnership between a child's healthcare providers and their family.
Characteristics of a Medical Home:
- Accessible: Care is easy to reach geographically, financially, and culturally. Families can communicate with the care team by phone or email.
- Continuous: The same healthcare team cares for the child from infancy through adolescence, fostering a trusting relationship.
- Comprehensive: The team addresses all of a child’s health needs, including acute illness, preventative care, and chronic conditions.
- Family-Centered: The family is an equal partner in decision-making and care planning. The care team respects the family's cultural beliefs and values.
- Coordinated: The care team ensures seamless transitions between different specialists, schools, and community services.
- Compassionate: The team provides care with respect and empathy, recognizing the emotional and social impact of health issues.
Nursing Insight: As a nurse, you are often the central point of contact in the medical home. You can facilitate communication and coordinate care between specialists, schools, and other services to ensure a seamless experience for the family.
3.3. Partnerships
Effective health supervision is built on a strong partnership between the healthcare provider, the child, and the family. This relationship is collaborative, with the provider acting as a guide and educator, and the family as the primary advocate and decision-maker for the child. This partnership extends to other professionals, such as teachers, school nurses, and social workers, creating a network of support for the child.
3.4. Special Issues in Health Supervision
- Cultural Influences: A family’s cultural background significantly impacts their health beliefs, practices, and interactions with the healthcare system. Nurses must be culturally competent and respectful of diverse traditions, such as dietary habits, views on illness, and communication styles. For example, some cultures may rely more on traditional healers or herbal remedies, and it’s important to understand and integrate these beliefs into the care plan whenever possible and safe.
- Community Influences: The child’s community environment—including access to healthy foods, safe playgrounds, and quality schools—profoundly affects their health. Nurses should be aware of community resources and challenges to provide relevant guidance. A child living in a food desert, for instance, requires different nutritional guidance than one with easy access to fresh produce.
- Health Supervision and the Child with Chronic Illness: For children with chronic conditions like asthma or diabetes, health supervision visits are crucial. These visits not only focus on typical well-child components but also on managing the specific chronic illness, coordinating with specialists, and providing emotional support to the child and family. The goal is to optimize the child's quality of life and minimize the impact of the illness.
- Health Supervision and the Child Adopted Internationally: Children adopted from other countries often have unique health needs. They may have incomplete immunization records, be at risk for infectious diseases (like tuberculosis or hepatitis), have nutritional deficiencies, or have developmental delays due to early life trauma or poor living conditions. The initial health supervision visits must include comprehensive screenings and a review of all available medical records.
Nursing Insight: A detailed health history is crucial for children with special issues. This includes gathering information about their community, cultural background, and prior medical care.
Components of Health Supervision
Developmental Surveillance and Screening
- Developmental surveillance is an ongoing, flexible process of monitoring a child's development over time. It involves a mix of formal and informal observations, listening to parental concerns, and using standardized screening tools.
- Developmental screening is a more formal, standardized process using validated tools (e.g., ASQ-3, M-CHAT) to identify children at risk for developmental delays. Early identification is critical for timely intervention, which can significantly improve a child's long-term outcomes.
5.2. Injury and Disease Prevention
Screening Tests: These are used to detect potential health problems in children who appear healthy.
- Metabolic Screening: The newborn screen (done in the first few days of life) tests for a range of genetic, metabolic, and endocrine disorders like Phenylketonuria (PKU) and congenital hypothyroidism. Early detection prevents severe intellectual disability.
- Hearing Screening: All newborns are screened for hearing loss before hospital discharge. Early detection is crucial for language and speech development.
- Vision Screening: Starts in infancy with observing red reflexes and eye alignment. The Cardiff Visual Acuity Test for Matching or Estimation (CVTME) is a specialized test used to measure visual acuity in young children, particularly those between the ages of 1 to 3 years old. It is designed for a developmental stage where a child may not be able to name or point to letters or pictures on a standard eye chart. Formal screening with a Snellen chart begins around age 3 or 4 to detect conditions like amblyopia (lazy eye).
- Iron Deficiency Anemia: Screening typically begins between 9 and 12 months of age, and again in toddlerhood, based on risk factors. Untreated anemia can affect cognitive development.
- Lead Screening: Recommended for children at high risk, particularly those living in older homes. Lead exposure can cause irreversible neurological damage. Based on guidelines from the Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP), all children should be screened for lead exposure at ages 1 and 2 years old. This recommendation is part of a universal screening strategy, as it's the age at which children are most likely to be exposed to lead, primarily through hand-to-mouth behaviors.
- Hypertension: Blood pressure screening begins at age 3.
- Hyperlipidemia: Universal screening for high cholesterol is recommended once between ages 9 and 11 and again between 17 and 21.
Immunizations: These are one of the most effective tools for disease prevention.
- ACIP Guidelines: The Advisory Committee on Immunization Practices (ACIP) provides evidence-based recommendations for the immunization schedule. Nurses must be familiar with the current schedule and proper administration techniques.
Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2025
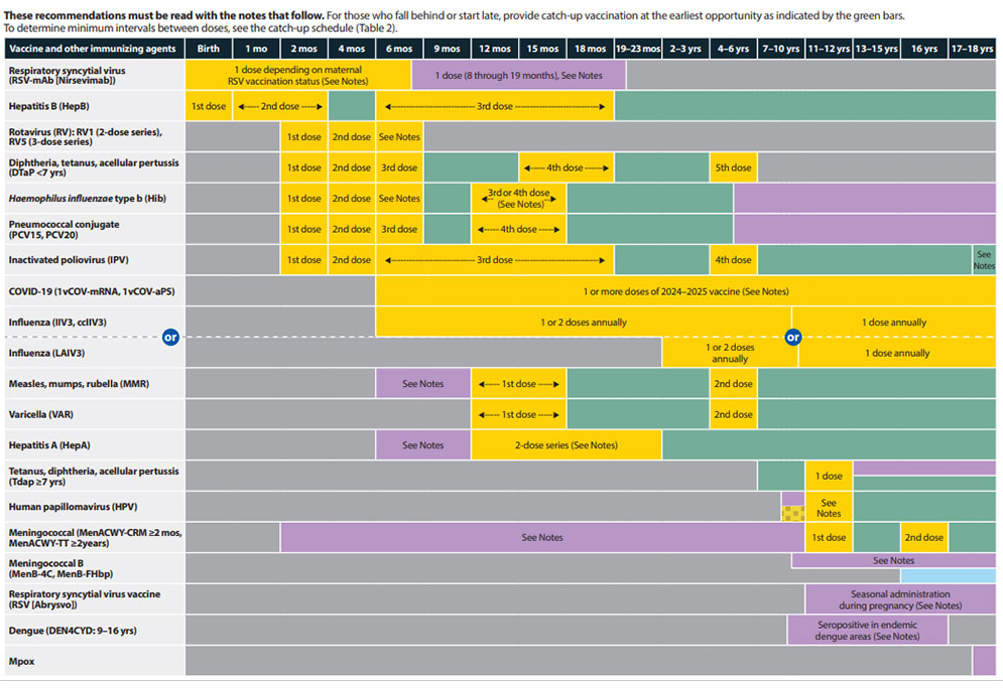
- Barriers to Immunization: Common barriers include parental misinformation, fear of side effects, religious beliefs, lack of access to healthcare, and complex schedules.
- Overcoming Barriers: Nurses play a vital role in educating parents about vaccine safety and efficacy, addressing their concerns respectfully, providing a supportive environment, and referring families to community resources or public health clinics.
- Nursing Insight: Catch-up Schedule: If a child falls behind on this schedule, a "catch-up" schedule is available to ensure they receive all necessary immunizations. The Influenza (Flu) vaccine is recommended for all children aged 6 months and older every year. Other vaccines, such as Meningococcal B (MenB) and the COVID-19 vaccine, may also be recommended based on individual risk factors, lifestyle, or as a healthcare provider advises.
5.3. Health Promotion
Anticipatory Guidance: This is the process of providing practical information and advice to parents about what to expect in their child's development over the next period (e.g., safety measures for a newly crawling infant, preparing for potty training).
- Promoting Oral Health Care: Begins with advice on wiping a newborn's gums and progresses to encouraging proper brushing habits and regular dental visits. It also includes discussing the importance of fluoride and the dangers of bottle caries.
- Promoting Healthy Weight: Involves educating families on balanced nutrition, portion control, and the risks of obesity. It's a key topic at every visit, with a focus on healthy eating habits rather than dieting.
- Promoting Healthy Activity: Encouraging age-appropriate physical activity, limiting screen time, and fostering a love for movement are essential for physical and mental health.
- Promoting Personal Hygiene: Teaching children about hand washing, bathing, and proper toileting habits is crucial for preventing the spread of illness.
- Promoting Safe Sun Exposure: Educating families on the use of sunscreen, protective clothing, and avoiding peak sun hours to prevent skin cancer later in life.
Nursing Insight: Tailor anticipatory guidance to the child's age and the family's specific needs. Use "teachable moments" during the visit to provide relevant, practical advice.
Summary
- Health supervision is a crucial component of pediatric care, focusing on a proactive, preventative approach to ensure optimal child health and development.
- The principles guiding this care, wellness, the medical home, and partnerships, create a foundation for a holistic, family-centered model.
- Well-child visits are not just about immunizations; they involve essential components like developmental surveillance and screening, a variety of injury and disease prevention strategies, and health promotion through anticipatory guidance.
- Addressing special issues, such as cultural differences and chronic illnesses, ensures care is tailored to the individual child's needs.
- By embracing these principles and components, nurses and other healthcare providers play a critical role in supporting children and their families on their journey to a healthy future.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Health Supervision In Children
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


