Please set your exam date
Hygiene
Study Questions
Practice Exercise 1
When planning for completion of a patient’s personal hygiene, it is most important to consider which of the following?
Explanation
Centering care on the patient’s preferences preserves dignity and autonomy, improves cooperation and comfort, and helps prevent complications such as skin breakdown or infection.
Rationale for correct answer:
2. The patient’s usual hygiene practices and preferences: This is primary because safe, effective hygiene care should be individualized: respect cultural practices, daily routines, independence level, and comfort.
Rationale for incorrect answers:
1. When the patient had his or her most recent bath: Knowing when the last bath occurred is useful - it helps assess current hygiene needs, skin condition, odor, and infection risk. It informs what to do, not how or when to plan care in a person-centered way.
3. Where the bathing fits in the nurse’s schedule: Nurse workflow considerations matter for practicality and staffing, but they are nurse-centered. Scheduling should be flexible to meet the patient’s needs.
4. The time that is convenient for the patient care assistant: Coordinating with assistants is necessary for safe delivery, but the assistant’s convenience should not drive the plan. The goal is to balance staff availability with the patient’s preferences and clinical needs.
Take home points
- Prioritize the patient’s usual hygiene habits and preferences - it promotes dignity, trust, and better clinical and psychosocial outcomes.
- Logistics (nurse/assistant schedules, last bath) inform safe, timely care but should be adjusted to fit the patient-centered plan, not replace it.
A client can bathe most of her body except for the back, hands, and feet. She also can walk to and from the bathroom and dress herself when given clothing. Which functional level describes this client?
Explanation
The semi dependent level indicates partial independence -the client performs most tasks but needs assistance with specific portions. Correctly identifying the level guides the amount of assistance, care planning, and how much to encourage independence.
Rationale for correct answer:
3. Semi dependent (+2): Semi dependent fits a client who can perform many ADLs independently (ambulates, dresses when given clothing) but needs help with parts of bathing (areas she cannot reach).
Rationale for incorrect answers:
1. Totally dependent (+4): Totally dependent means the client needs complete assistance with bathing, ambulation, and dressing; this client can walk and dress (with clothing provided), so not totally dependent.
2. Moderately dependent (+3): Moderately dependent implies more extensive help with most ADLs; here the client only needs help with specific areas (back, hands, feet).
4. Independent (0): The client is not fully independent because she requires help for some body areas.
Take home points
- Match the dependence level to what the client can actually do, not assumptions.
- Promote independence by assisting only where needed (help with back/hands/feet, encourage remaining self-care).
The nurse will delegate hygiene care for two patients of different cultures to the assistive personnel (AP). What cultural information does the nurse need to provide to the AP? Select all that apply
Explanation
When delegating hygiene tasks, the nurse must communicate culturally relevant information (preferred products, timing, gender preferences, religious practices) so APs can provide respectful, acceptable care that maintains dignity and promotes cooperation.
Rationale for correct answer:
1. Specific hygiene products: Important to communicate (e.g., preference for particular soap, culturally specific products) so AP can deliver culturally sensitive care.
2. Timing of hygiene care: Many cultures have preferred times for bathing or prayer-related washing -timing matters for respect and cooperation.
4. The need for gender congruent caregiver: Critical for many cultures/religions -patients may refuse care from opposite sex providers; AP must be informed to honor this.
5. Religious practices: Religious rules (e.g., modesty, ritual washing, fasting) can affect hygiene routines and must be communicated to ensure respectful care.
Rationale for incorrect answer:
3. Socioeconomic status: Not necessary for the AP to know when performing hygiene care; irrelevant to the immediate cultural care plan and risks stereotyping.
Take home points
- Share specific cultural/hygiene preferences (products, timing, gender preference, religious needs) when delegating to ensure respectful care.
- Avoid irrelevant personal data (like socioeconomic status) unless it directly affects care; focus on actionable cultural information.
Practice Exercise 2
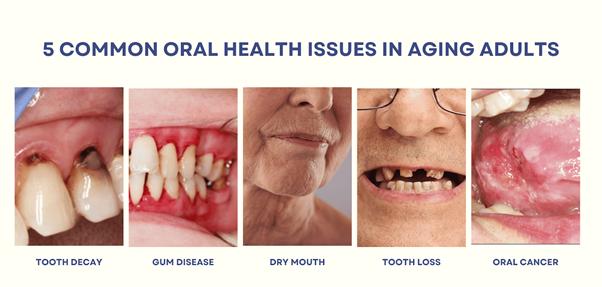
The nurse observes a marked inflammation of the gums, and recession and bleeding of the gums and documents this observation using which term?
Explanation
Accurate documentation is essential for communication and treatment planning. Differentiating between common oral conditions ensures proper referrals and interventions to prevent progression and complications.
Rationale for correct answer:
4. Periodontitis is a serious gum infection causing inflammation, bleeding, and gum recession, which can lead to tooth loss if untreated.
Rationale for incorrect answers:
1. Glossitis refers to inflammation of the tongue, often appearing red, swollen, and painful. It does not describe gum changes.
2. Caries are cavities caused by tooth enamel breakdown from bacterial action. Caries do not involve gum inflammation or bleeding.
3. Cheilosis is cracking or inflammation at the corners of the mouth, often linked to riboflavin deficiency. This is unrelated to gum recession or bleeding.
Take home points:
- Use correct terminology (e.g., periodontitis for gum inflammation and recession) when documenting oral findings.
- Oral health assessment is a key part of nursing care and can reveal both local and systemic health problems.
A nurse is caring for an 80-year-old patient who has become weak and fatigues easily. He is unable to wash his body and always asks the nurse to brush his teeth. Based on this information, which of the following is an appropriate nursing diagnosis for this patient?
Explanation
Accurate diagnosis requires linking observed data (weakness, inability to wash, need for help) to an appropriate label. Using NANDA-I terminology, “Self-Care Deficit” captures the patient’s limitation, guiding nursing interventions like assistance, energy conservation, and independence support.
Rationale for correct answer: 2
2. Bathing/Hygiene Self-Care Deficit related to decreased strength and endurance: This diagnosis directly matches the observed problem: inability to bathe and perform oral hygiene due to fatigue and weakness.
Rationale for incorrect answers:
1. Risk for Impaired Skin Integrity related to immobility: While immobility can cause skin issues, the scenario highlights difficulty performing hygiene tasks, not skin breakdown.
3. Social Isolation related to lack of visitors: There’s no evidence of social isolation; the patient’s problem is physical limitation, not social withdrawal.
4. Impaired Oral Mucous Membrane related to inability to brush his teeth: Oral mucosa impairment is not documented. The issue is inability to perform self-care, not tissue damage.
Take home points:
- Nursing diagnoses must match observed patient problems, not just possible risks.
- “Self-Care Deficit” diagnoses are key for older or weak patients needing help with ADLs.
Which of the following factors directly impairs salivary gland secretion? Select all that apply
Explanation
Major direct causes include gland damage from radiation and reduced fluid volume from dehydration. Xerostomia increases risk of dental decay, difficulty swallowing, and oral discomfort, so identifying and managing etiologies is important.
Rationale for correct answer:
3. Radiation therapy: Head-and-neck radiation commonly damages salivary glands, causing marked reduction in saliva (xerostomia).
4. Dehydration: Low body fluid volume reduces salivary production and causes dry mouth.
Rationale for incorrect answers:
1. Use of cough drops: Cough drops may stimulate saliva in some people; they do not directly impair gland secretion.
2. Immunosuppression: Immunosuppression per se doesn’t directly reduce salivary gland secretion (though some underlying causes/meds might).
5. Presence of oral airway: An oral airway may interfere with comfort or cause local trauma, but it does not directly reduce salivary gland secretion.
Take home points
- Radiation to the head/neck and dehydration are common direct causes of reduced saliva.
- Address xerostomia by treating underlying causes, encouraging hydration, and using saliva substitutes or frequent oral lubrication as needed.
A nurse is assigned to care for the following patients. Which patient is most at risk for developing skin problems that will require thorough bathing and skin care?
Explanation
Continuous exposure to urine/feces plus diabetes (impaired healing) and dementia (reduced ability to report discomfort or participate in care) places a patient at very high risk for incontinence-associated dermatitis, fungal infection, and pressure injuries; these patients require frequent cleansing, moisture management, and protective skin barriers.
Rationale for correct answer:
4. 70-year-old with diabetes, dementia, and urinary/fecal incontinence: Incontinence plus diabetes and cognitive impairment creates the highest immediate risk of moisture-associated skin damage, infection, and delayed healing-so intensive perineal care and frequent skin assessment are needed.
Rationale for incorrect answers:
1.44-year-old post breast lesion, in pain and unwilling to ambulate: While immobility raises risk, this patient is less likely to have ongoing skin contamination or the chronic risks linked to incontinence and cognitive impairment.
2. 56-year-old homeless with malnutrition and dehydration: High risk for skin problems overall (poor nutrition, hygiene), but the scenario does not describe active incontinence that mechanically increases local skin breakdown risk.
3. 60-year-old stroke patient with right-sided paralysis and an orthopedic brace: This patient is at risk for pressure areas under the brace and from immobility, but the question asks which patient is most at risk for skin problems requiring thorough bathing/skin care.
Take home points
- Incontinence, diabetes and cognitive impairment lead to a very high risk for skin breakdown.
- Provide frequent cleansing, moisture control, and barrier creams.
When the nurse is assigned to a patient who has a reduced level of consciousness and requires mouth care, which physical assessment techniques should the nurse perform before the procedure? Select all that apply
Explanation
Before providing mouth care to a patient who cannot protect their airway, the nurse should evaluate oxygenation (SpO₂), respiratory effort, and airway protective reflexes (gag/cough). These findings guide whether to proceed, take extra precautions (positioning, suction at bedside), or defer and request additional support.
Rationale for correct answer:
1. Oxygen saturation: Low SpO₂ suggests compromised respiratory function; you should assess oxygenation before mouth care because hypoxia and poor airway protection increase risk if aspiration occurs.
3. Respirations: Assessing respiratory rate and quality helps determine breathing adequacy and aspiration risk during mouth care.
4. Gag reflex: Presence or absence of gag/cough reflex indicates whether the patient can protect their airway; an absent gag reflex significantly increases aspiration risk during oral interventions.
Rationale for incorrect answers:
2. Heart rate: Heart rate is important for overall status but does not directly determine safety of oral care in a reduced-LOC patient.
5. Response to painful stimulus: This is a general neurologic assessment of responsiveness but not as directly relevant to airway protection prior to mouth care as gag reflex and respiratory/oxygen assessments.
Take home points
- Check gag reflex and respirations (and SpO₂) before oral care in patients with decreased consciousness
- These are direct indicators of airway protection and aspiration risk.
- If airway protection is compromised, position for drainage and have suction ready; modify or delay care and get help if needed.
During morning care, the patient asks the nurse to shave him with a disposable razor. Before shaving him, what should the nurse do?
Explanation
Before shaving, the nurse must assess bleeding risk (medications like warfarin, heparin, antiplatelet agents, or coagulopathies) because shaving with a blade can cause bleeding. If the patient is anticoagulated or at high bleeding risk, use an electric razor or consult policy/MD. Routine hygiene tasks require assessment and adaptation to the patient’s safety needs.
Rationale for correct answer:
2. Check to see if the patient is taking anticoagulants: Anticoagulants (and bleeding disorders) increase the risk of significant bleeding from nicks - so you must assess medications/bleeding risk and choose an electric razor or other safe method if indicated.
Rationale for incorrect answers:
1. Have him sign a permission form: Routine shaving is part of basic hygiene and does not require formal written consent.
3. Tell him that only a family member may shave a patient: Nurses routinely perform shaving; family is not required.
4. Position him flat in bed: Lying flat increases aspiration risk and may be uncomfortable; a seated or semi-upright position is preferred for shaving.
Take home points
- Always assess for anticoagulants or bleeding disorders before shaving with a blade.
- Choose safer alternatives (electric razor) when bleeding risk is present.
Practice Exercise 3
Why is adequate oral hygiene an essential part of nursing care? Select all that apply
Explanation
Oral care is not only about comfort; it plays a vital role in infection prevention, oral tissue health, and reducing systemic complications such as aspiration pneumonia. Nurses must prioritize oral hygiene, especially in dependent or critically ill patients, as neglect can lead to preventable, serious outcomes.
Rationale for correct answer:
1. It promotes the patient’s sense of well-being: Oral hygiene enhances comfort, self-image, and confidence. Patients often feel refreshed and more willing to interact socially after oral care, supporting psychological and emotional well-being.
2. It prevents deterioration of the oral cavity: Regular oral care reduces plaque buildup, tooth decay, gingivitis, halitosis, and ulcer formation. This preserves oral integrity, reduces pain, and prevents long-term complications.
3. It contributes to decreased incidence of aspiration pneumonia: In debilitated or ventilated patients, poor oral hygiene increases bacterial colonization, which can be aspirated into the lungs, causing pneumonia. Oral care reduces microbial load, lowering infection risk.
Rationale for incorrect answers:
4. It eliminates the need for flossing: Oral hygiene does not eliminate the need for flossing. Flossing helps remove debris and plaque between teeth, which brushing or swabbing may not reach. Nurses may adapt methods, but flossing is not made unnecessary.
5. It decreases oropharyngeal secretions: Oral hygiene improves comfort and reduces bacterial growth but does not physiologically decrease secretions. Instead, it helps manage them more effectively.
Take home points:
- Oral hygiene improves both comfort and clinical outcomes, particularly in preventing aspiration pneumonia.
- Nurses should integrate oral care as an essential intervention, not just as a comfort measure.
During a bath, the nurse observes that a patient has dry skin. Which action would be best?
Explanation
Skin is the body’s first defense against infection, and maintaining its health is vital. Observing changes during hygiene care allows nurses to intervene promptly with evidence-based strategies, such as using emollients, while avoiding harmful practices like excessive bathing or alcohol use.
Rationale for correct answer:
2. Use an emollient on the dry skin: Emollients restore moisture, improve skin barrier function, and prevent cracking and infection. This is the best intervention to address dryness directly.
Rationale for incorrect answers:
1. Bathe the patient more frequently: More frequent bathing actually worsens dryness by stripping natural oils, further irritating the skin. This is counterproductive in managing dry skin.
2. Massage the skin with alcohol: Alcohol is drying and irritating, removing essential oils and worsening the condition. It should never be used for dry skin care.
3. Discourage fluid intake: Hydration is essential for healthy skin. Discouraging fluids could worsen dehydration and dryness, increasing the risk of skin breakdown.
Take home points:
- Dry skin should be treated with moisturizing interventions, not drying agents.
- Nursing care should focus on preserving skin integrity as part of overall patient safety and comfort.
Which action would be the priority when administering oral care to a dependent patient?
Explanation
Dependent patients often have higher risks for infection and aspiration, so the nurse must first prioritize self-protection and patient safety. Using gloves is a fundamental standard of practice and should always precede the technical steps of oral care.
Rationale for correct answer:
2. Wearing disposable gloves: Gloves protect both the nurse and the patient from cross-infection. This is the priority because it ensures safe practice before any oral care is performed.
Rationale for incorrect answers:
1. Assisting the patient to the dorsal recumbent position: This position places the patient flat on the back, increasing aspiration risk. A side-lying or semi-Fowler’s position is safer.
3. Using a firm toothbrush to cleanse teeth and gums: Firm brushes may cause gum trauma. A soft-bristled toothbrush is safer and equally effective.
4. Irrigating forcefully with hydrogen peroxide: Forceful irrigation risks aspiration and mucosal irritation. Gentle rinsing with approved solutions is safer.
Take home points:
- Gloves are priority to protect against infection during oral care.
- Positioning and technique matter, but safety always starts with standard precautions.
Mr. James has an eye infection with a moderate amount of discharge. Which action would be most appropriate for the nurse to use when cleaning his eyes?
Explanation
The eyes are vulnerable to cross-contamination and irritation, so meticulous cleaning with separate materials for each eye and using correct wiping direction are critical for safe and effective care.
Rationale for correct answer:
4. Using only one cotton ball per eye: This prevents cross-contamination between the eyes and is essential in infection control.
Rationale for incorrect answers:
1.Using hydrogen peroxide: Hydrogen peroxide is too harsh for the delicate eye structures and can cause chemical irritation.
2. Wiping from the outer canthus to the inner canthus: Correct technique is inner canthus to outer canthus to avoid dragging debris into the nasolacrimal duct.
3. Positioning him on the same side as the eye to be cleansed: Proper technique is to position the patient on the opposite side so discharge drains away from the unaffected eye.
Take home points:
- Always use separate cleaning materials for each eye to prevent cross-infection.
- Clean the eye from inner to outer canthus, never the reverse.
Providing perineal care to a patient requires which of the following?
Explanation
Correct technique during perineal care emphasizes using clean strokes, moving from cleaner to dirtier areas, and ensuring all areas are thoroughly cleansed. Proper hygiene in this sensitive area prevents urinary tract infections, skin irritation, and discomfort.
Rationale for correct answer:
1. Using a clean portion of the washcloth for each stroke: This prevents reintroducing microorganisms and helps maintain infection control by keeping each stroke clean.
Rationale for incorrect answers:
2. Moving from most contaminated to least contaminated area: Correct technique is least to most contaminated (e.g., front to back in females) to prevent carrying bacteria from contaminated areas to cleaner ones.
3. Using sterile gloves: Sterile gloves are not required. Clean gloves are adequate for perineal care unless a sterile procedure (e.g., catheter insertion) is being performed.
4. Leaving the foreskin undisturbed in an uncircumcised adult male: The foreskin should be gently retracted for cleaning and then returned to its normal position to prevent infection and paraphimosis.
Take home points:
- Always use a clean washcloth section for each stroke during perineal care.
- Clean from least to most contaminated areas to reduce infection risk.
The student nurse is teaching a family member the importance of foot care for their mother, who has diabetes mellitus. Which safety precautions are important for the family member to know to prevent infection? Select all that apply
Explanation
Diabetes increases risk of neuropathy, poor circulation, and impaired healing-so prevention focuses on daily inspection, careful moisturizing (not between toes), gentle cleansing and drying, and avoiding activities that increase infection risk (like soaking or aggressive nail cutting).
Rationale for correct answer:
2. Assess skin for redness, abrasions, and open areas daily: Daily inspection detects early problems (breaks in skin, infection) so treatment can begin promptly.
4. Apply lotion to feet daily: But avoid applying lotion between toes (to prevent fungal growth). Moisturizing prevents cracking and preserves skin integrity.
5. Clean between toes after bathing: Cleaning and then thoroughly drying between toes reduces fungal and bacterial growth.
Rationale for incorrect answers:
1. Cut nails frequently: Frequent cutting can cause trauma; nails should be trimmed carefully and not overly short, and diabetic patients often need podiatry referral for nail care.
3. Soak feet in water at least 10 minutes before nail care: Prolonged soaking can macerate skin and increase infection risk; caution is advised.
Take home points
- Inspect feet daily and report any redness, blisters, or breaks immediately.
- Moisturize daily (but not between toes) and avoid risky practices-refer nail problems to a podiatrist.
Comprehensive Questions
Which recommendation by the nurse to an adolescent patient with acne would be most appropriate?
Explanation
Acne management requires teaching safe and effective hygiene and discouraging harmful practices. Nurses should emphasize consistent cleansing, avoidance of pore-clogging products, and not manipulating lesions. Proper guidance empowers adolescents to manage their condition while reducing risk of infection and scarring.
Rationale for correct answer:
1. Wash the skin twice a day: Gentle cleansing twice daily removes excess oil and bacteria without over-drying or irritating the skin. This is the best evidence-based recommendation for acne care.
Rationale for incorrect answer:
2. Use cosmetics liberally to cover blackheads: Heavy cosmetic use clogs pores and worsens acne. Non-comedogenic products may be used sparingly, but liberal cosmetic use is not advisable.
3. Use emollients on the area: Emollients are meant to hydrate dry skin, but in acne-prone skin, they can worsen oiliness and clog pores, aggravating lesions.
4. Squeeze blackheads as they appear: Squeezing introduces bacteria, increases inflammation, and can lead to scarring. Patients should be advised against this practice.
Take home points:
- Encourage gentle cleansing twice daily for acne management.
- Discourage harmful practices like squeezing lesions or overusing cosmetics.
Which of the following interventions would the nurse include in the plan of care when providing foot care to an older patient?
Explanation
Older adults are at high risk for foot complications due to poor circulation, diabetes, or fragile skin. Nurses must emphasize gentle cleansing, moisturizing, and safe nail care while avoiding practices that increase risk of infection or injury.
Rationale for correct answer:
4. Bathing the feet at least daily: Daily washing removes bacteria, reduces odor, and promotes comfort. Proper drying (especially between toes) helps prevent fungal infections.
Rationale for incorrect answers:
1. Using scissors to correct an ingrown toenail: Nurses should not attempt to cut or correct ingrown toenails; this is a podiatrist’s responsibility due to the risk of infection and poor healing in older adults.
2. Trimming toenails as short as possible: Nails should be trimmed straight across, not too short, to prevent ingrown nails and injury.
3. Using an alcohol rub if the feet are dry: Alcohol dries the skin further, increasing the risk of cracks and infection. Emollients or mild moisturizers are preferred.
Take home points:
- Daily cleansing and moisturizing are safe, essential practices in foot care for older adults.
- Nail trimming and ingrown nail correction should be referred to qualified professionals to prevent complications.
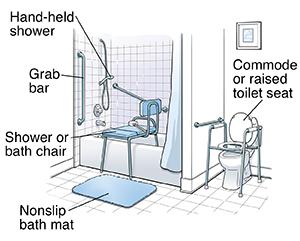
An older patient with an unsteady gait requests a tub bath. Which of the following actions would be most appropriate?
Explanation
Falls are a leading cause of injury in the elderly, especially in slippery environments like bathrooms. Nurses must prioritize fall prevention strategies, while also supporting comfort and dignity in bathing.
Rationale for correct answer:
3. Assist the patient in and out of the tub to prevent falling: This addresses the main risk- falls- while still respecting the patient’s wish for a tub bath. It balances safety with patient preference.
Rationale for incorrect answers:
1. Add Alpha-Keri oil to the water to prevent dry skin: Oils make the tub slippery, increasing fall risk. Safer skin-hydrating methods (like moisturizers after bathing) should be used.
2. Allow the patient to lock the door to guarantee privacy: Safety outweighs privacy in this case. The door should not be locked so staff can respond quickly if the patient falls.
4. Keep the water temperature very warm because the patient chills easily: Very warm water can cause burns, dizziness, or hypotension in older adults. Lukewarm water is safer.
Take home points:
- Safety comes first when providing hygiene care to older adults with mobility issues.
- Assistive care (help in/out of tub, no locking door) prevents falls while maintaining dignity.
An unresponsive patient is wearing gas-permeable contact lenses. How would the nurse remove these lenses?
Explanation
Gas-permeable (rigid) lenses are removed differently from soft lenses -often by a gentle pinching or using a small suction device. The nurse should use clean gloves, moisten the eye if needed with saline, stabilize the lids, and remove the lens gently to avoid corneal abrasion. If removal is difficult or ocular damage is suspected, stop and get specialized help.
Rationale for correct answer:
4. Ensure that the lens is centered on the cornea before gently manipulating the lids to release it: The lens must be situated on the cornea, not the sclera, before removal. To remove hard contact lenses, the upper and lower eyelids are gently maneuvered to help loosen the lens and slide it out of the eye.
Rationale for incorrect answers:
1. Gently irrigate the eye with an irrigating solution from the inner canthus outward: Irrigation can help remove debris but typically will not remove a rigid gas-permeable lens; also direction of irrigation should avoid pushing material toward nasolacrimal duct.
2. Grasp the lens with a gentle pinching motion: An attempt to grasp a hard lens might result in a scratch on the cornea.
3. Don sterile gloves before attempting the removal procedure: Sterile gloves are not required; clean gloves are appropriate. Sterile technique is reserved for invasive procedures.
Take home points
- For rigid lenses, a gentle pinch technique (with clean gloves and lubrication if needed) is commonly used- be very gentle to avoid corneal injury.
- Use clean technique (not sterile) and consult eye care specialists if removal is difficult or if there is redness, pain, or corneal abrasion.
The nurse is about to bathe a female patient who has an intravenous access in place in her forearm. The patient’s gown, which does not have snaps on the sleeves, needs to be removed prior to bathing. What should the nurse do?
Explanation
Maintaining a closed IV system when changing clothing or gowns minimizes the risk of contamination, interruption of therapy, and air embolism. The nurse should plan the gown change so the tubing/infusion bag remains intact and secure, and never disconnect tubing unnecessarily.
Rationale for correct answer:
3. Thread the bag and tubing through the gown sleeve, keeping the line intact: Keep the IV system closed and intact; carefully thread the tubing/bag through the sleeve so the gown can be removed without disconnecting or contaminating the line.
Rationale for incorrect answers:
1. Temporarily disconnect the IV tubing at a point close to the patient and thread it through the gown sleeve. Unnecessary disconnection increases infection risk and interrupts infusion.
2. Cut the gown with scissors to allow arm movement. Cutting the gown damages clothing and is unsafe/inappropriate around an IV site.
4. Temporarily disconnect the tubing from the IV container, threading it through the gown. Avoid disconnecting the system unless absolutely necessary and under appropriate aseptic conditions.
Take home points
- Never disconnect IV tubing unnecessarily- keep the infusion system intact to prevent infection and infusion interruption.
- When removing clothing, thread the tubing/bag through the sleeve or remove the gown from the uninvolved side first to protect the IV site.
When making an occupied bed, which of the following is most important for the nurse to do?
Explanation
When making an occupied bed, the nurse must prioritize actions that minimize risk to the patient. Other considerations like privacy, warmth, and proper technique are important but secondary to safety.
Rationale for correct answer:
1. Keep the bed in the low position: The priority while making an occupied bed is patient safety- a low bed reduces fall risk if the patient moves or tries to get up.
Rationale for incorrect answers:
2. Use a bath blanket or top sheet for warmth and privacy: Important for comfort and privacy, but not the single most important safety action.
3. Constantly keep the side rails raised on both sides: Side rails are not a substitute for assessment and may be considered a restraint if used improperly; they should be used judiciously per policy.
4. Move back and forth from one side to the other when adjusting the linens: Frequent, unnecessary movement around the bed can confuse or stress the patient; use safe, coordinated turns and good body mechanics but prioritize patient safety (bed height, call light within reach).
Take home points
- Safety first: keep the bed low to reduce fall risk when a patient is in bed.
- Maintain privacy and comfort (use bath blanket/sheet), but don’t let comfort measures override safety precautions
What is the proper position to use for an unresponsive patient during oral care to prevent aspiration? Select all that apply
Explanation
Positioning to prevent aspiration during oral care for patients with reduced consciousness. Proper positioning (side-lying or semi-Fowler’s with the head turned) allows saliva and oral secretions to drain away from the airway so they can be suctioned or cleared, decreasing the chance of aspiration pneumonia.
Rationale for correct answer:
2. Modified left lateral recumbent position: Side-lying (modified lateral) helps secretions drain out of the mouth instead of being aspirated into the airway; it is commonly used for unresponsive patients during mouth care.
3. Semi-Fowler’s position with head to side: Semi-Fowler’s (head elevated) with the head turned to the side permits gravity-assisted drainage and reduces aspiration risk while allowing access to the mouth.
Rationale for incorrect answers:
1. Prone position: Prone makes access to the mouth difficult and may allow secretions to pool in ways that are hard to suction; it’s not recommended for oral care in an unresponsive patient.
4. Trendelenburg position: Head-down increases risk of aspiration and is inappropriate for oral care.
5. Supine position: Lying flat on the back allows secretions to pool and raises aspiration risk.
Take home points
- Position unresponsive patients so secretions can drain (side-lying or semi-Fowler’s with head to side) before oral care.
- Always have suction available and monitor the patient’s respiratory status during mouth care.
The American Dental Association suggests that patients who are at risk for poor hygiene use the following interventions for oral care: Select all that apply
Explanation
Evidence-based oral care interventions for patients at increased risk of oral disease or systemic infection- Preventive measures (fluoride toothpaste, soft toothbrush) preserve dental health, while antiseptic rinses like CHG are added tools for high-risk patients to reduce pathogenic oral flora. Oral mucosa, gums, and tongue should be included in care.
Rationale for correct answer:
1. Use fluoride toothpaste: Fluoride helps prevent dental caries and strengthens enamel -a standard preventive measure for patients at risk of poor oral health.
3. Use 0.12% chlorhexidine gluconate (CHG) oral rinses for high-risk patients: CHG is often recommended for high-risk or critically ill patients to reduce oral microbial load and decrease risk of nosocomial infections (used per policy).
4. Use a soft toothbrush for oral care: Soft bristles clean effectively while minimizing gum trauma -important in fragile or inflamed oral tissues.
Rationale for incorrect answers:
2. Brush teeth 4 times a day: Excessively frequent vigorous brushing isn’t generally recommended; routine care is usually twice daily with additional cleaning after certain events (e.g., after vomiting). Overbrushing can injure gums.
5. Avoid cleaning the gums and tongue: Cleaning gums and tongue is important to reduce bacterial colonization, maintain comfort, and prevent halitosis and infection.
Take home points
- Use gentle, effective daily oral care (soft brush and fluoride) as the foundation.
- For high-risk patients, add antiseptic measures (e.g., CHG) per facility policy- never omit cleaning gums/tongue.
While planning morning care, which of the following patients would have the highest priority to receive a bath first?
Explanation
When scheduling limited resources (morning care), prioritize patients whose hygiene needs directly affect safety and tissue integrity -e.g., those with incontinence, draining wounds, or heavy soiling. Prompt perineal/skin care prevents moisture-associated skin damage and infection.
Rationale for correct answer:
3. Patient with frequent incontinent diarrheal stools and urine: Ongoing fecal and urinary contamination rapidly damages skin, promotes infection, and requires prompt cleansing and skin protection.
Rationale for incorrect answers:
1. Patient just returned from a diagnostic test: May need assessment or rest after the test; not the highest hygiene priority unless contaminated.
2. Patient with a fever who just finished IV antibiotics: Fever may require comfort measures, but immediate skin/mucosal contamination from incontinence presents greater risk of skin breakdown and infection.
4. Patient who has been awake all night with pain 8/10: Pain management and rest are priorities, but active contamination leading to skin breakdown takes precedence for immediate bathing/cleansing.
Take home points
- Give highest priority to patients with active contamination (incontinence, diarrhea) to prevent skin breakdown and infection.
- Other needs (pain, post-procedure rest) are important but can often be deferred until immediate infection/skin-risk issues are addressed.
A patient with a malignant brain tumor requires oral care. The patient’s level of consciousness has declined, with the patient only being able to respond to voice commands. Place the following steps in the correct order for administration of oral care.
Explanation
Correct order emphasizes safe positioning first, removal of prostheses, airway management if needed, and systematic cleaning (teeth then tongue), using appropriate devices (brush vs. toothette) and antiseptic agents (chlorhexidine) to lower infection risk while avoiding gag stimulation or aspiration.
Rationale for correct answers:
2. Begin by raising the bed, lowering the side rail, and positioning the patient close to the side of the bed with the head of the bed elevated to about 30 degrees: This positioning is essential for safety and accessibility. Elevating the head helps prevent aspiration and allows gravity to assist in draining fluids away from the airway.
5. Next, remove any partial plates or dentures if the patient has them: Dentures can obstruct access to the oral cavity and may pose a choking hazard if left in during care. Removing them ensures a thorough and safe cleaning process.
1. If the patient is uncooperative or has difficulty keeping their mouth open, insert an oral airway: This device helps maintain mouth opening without requiring active cooperation from the patient, which is especially important when consciousness is impaired.
3. Using a toothbrush moistened with chlorhexidine paste, clean the chewing surfaces and the inner surfaces of the teeth first: Chlorhexidine is an effective antimicrobial agent that reduces oral bacteria. Starting with the teeth targets the areas most prone to plaque and debris buildup.
6. Gently brush the tongue, being careful not to stimulate the gag reflex: Cleaning the tongue helps reduce bacterial load and improve oral hygiene, but care must be taken to avoid triggering vomiting or choking, especially in neurologically compromised patients.
4. If the patient does not have teeth, use a toothette moistened with chlorhexidine rinse to clean the oral cavity: Toothettes are soft and gentle, making them ideal for cleaning gums and other soft tissues in edentulous patients. The chlorhexidine rinse helps disinfect and maintain oral health.
Take home points
- Positioning and removing dentures come before mechanical cleaning; airway protection (oral airway, suction) is essential if needed.
- Use the appropriate cleaning tool (toothbrush vs. toothette) and be cautious with tongue manipulation to avoid triggering gag/aspiration.
The client is unresponsive and requires total care by nursing staff. Which assessment does the nurse check first before providing special oral care to the client?
Explanation
The nurse must evaluate airway-protective functions (gag/cough reflex) before performing oral interventions. If protective reflexes are absent or impaired, position the patient for drainage, have suction available, or delay/modify care.
Rationale for correct answer:
3. Gag reflex: Checking gag reflex tells you whether the patient can protect the airway; absence increases aspiration risk during mouth care.
Rationale for incorrect answers:
1. Presence of pain: Important for comfort, but an unresponsive client’s gag reflex is more immediately relevant to airway protection before oral care.
2. Condition of the skin: Important for overall care, but not the first check before oral care.
4. Range of motion: Not relevant to performing oral care for an unresponsive client.
Take home points
- Always assess gag reflex (and breathing) before oral care in unresponsive or low-LOC patients.
- If airway protection is questionable, position for drainage and have suction ready -patient safety first.
A client with diabetes has very dry skin on her feet and lower extremities. The nurse plans to inform the client to do which of the following to maintain intact skin?
Explanation
Diabetes predisposes to dry, cracked skin that can become a portal for infection. Safe care emphasizes gentle cleansing, daily inspection, moisturizing with an appropriate lotion (not between toes), and avoiding practices that increase maceration or trauma.
Rationale for correct answer:
2. Use a nonperfumed lotion: Moisturizing with a nonperfumed lotion helps prevent cracking while avoiding irritants; avoid putting lotion between the toes.
Rationale for incorrect answers:
1. Soak her feet frequently: Frequent soaking can macerate skin and increase infection risk in diabetic patients.
3. Apply foot powder: Powders may dry but can also irritate or mask skin breakdown; not first-line for very dry diabetic skin.
4. Avoid knee-high elastic stockings: Not the best direct intervention for dry skin; stockings relate more to circulation/pressure, not moisturizing.
Take home points
- Use nonperfumed lotion to hydrate dry diabetic skin-but do not apply between toes.
- Avoid soaking and risky self-care (aggressive nail cutting); inspect feet daily and refer to podiatry as needed.
The client wears an in-the-ear (ITE) hearing aid and because of arthritis needs someone to insert the hearing aid. Which action does the nurse teach the unlicensed assistive personnel (UAP) to do before inserting the client’s hearing aid?
Explanation
Safe handling and basic pre-insertion checks for in-the-ear (ITE) hearing aids- For clients who need assistance with insertion (e.g., due to arthritis), caregivers/UAP should turn the device off and ensure it’s clean/dry and the correct orientation before placing it in the ear.
Rationale for correct answer:
1. Turn the hearing aid off: Turning the device off before insertion prevents sudden loud feedback, reduces noise that may frighten the patient, and conserves battery life while handling.
Rationale for incorrect answers:
2. Soak the hearing aid in soapy solution to clean it: Electronic hearing aids should not be soaked; they should be cleaned per manufacturer instructions (dry methods, wipes) and batteries removed if immersion is needed.
3. Turn the volume all the way up: That can produce painful feedback and should never be done before insertion.
4. Remove the batteries: Removing batteries makes the device nonfunctional. Batteries are removed for certain cleaning procedures, but not as a routine pre-insert step.
Take home points
- Turn the hearing aid off before inserting to avoid feedback and ensure comfort.
- Follow manufacturer cleaning instructions (no soaking) and handle batteries per policy; teach helpers safe, gentle technique.
The client is in surgery and will be returning to his bed via a stretcher. Which bed option reflects that the nurse appropriately planned ahead for this client?
Explanation
Preparing a surgical bed in a high position makes transferring a patient from a stretcher safer and quicker, reduces staff strain, and helps preserve patient dignity and comfort during transfer.
Rationale for correct answer:
4. Surgical bed in high position: A surgical bed (fan-folded linens to the foot in a high bed position) facilitates a safe, efficient transfer from stretcher to bed and protects linens and patient during the move.
Rationale for incorrect answers:
1. Open bed in low position: An open bed (top linens folded) is for daytime rest; low position is safe for occupied patients but not ideal for receiving a stretcher transfer.
2. Occupied bed in low position: The patient is not in the bed yet; an occupied bed is for a patient already in it.
3. Closed bed in high position: A closed bed indicates no immediate return; a high position alone is not the specific preparation for stretcher transfer.
Take home points
- Plan the bed type and height ahead of the patient’s return.
- A little prep improves safety, decreases transfer time, and reduces fall/injury risk.
Exams on Hygiene
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe hygienic care that nurses provide to clients.
- Identify factors influencing personal hygiene.
- Identify normal and abnormal assessment findings while providing hygiene care.
- Apply the nursing process to common problems related to hygienic care.
- Demonstrate techniques for assisting patients with hygiene measures, including those used when administering various types of baths and those used in cleaning each part of the body.
- Describe agents commonly used on the skin and scalp, including any precautions necessary for their use.
- Plan, implement, and evaluate nursing care for common problems of the skin and mucous membranes.
Introduction
Personal hygiene is the self-care by which people attend to such functions as bathing, toileting, general body hygiene, and grooming.
Illness, hospitalization, and institutionalization generally require modifications in hygiene practices.
Nurses assisting patients with basic hygiene must respect individual patient preferences, providing only the care that patients cannot, or should not, provide for themselves.
Hygiene Practices
Hygienic practices include caring for the skin, hair, nails, mouth, teeth, and perineal area.
- Early morning care is provided to clients as they awaken in the morning. This care consists of providing a urinal or bedpan to the client confined to bed, washing the face and hands, and giving oral care.
- Morning care is often provided after clients have breakfast, although it may be provided before breakfast. It usually includes providing for elimination needs, a bath or shower, perineal care, back massages, and oral, nail, and hair care. Making the client’s bed is part of morning care.
- Hour of sleep or PM care is provided to clients before they retire for the night. It usually involves providing for elimination needs, washing face and hands, giving oral care, and giving a back.
- As-needed (prn) care is provided as required by the client
Functions of skin:
- Protects underlying tissues from injury
- Regulates the body temperature
- It secretes sebum- softens and lubricates the hair and skin, prevents the hair from becoming brittle, and decreases water loss. Bactericidal.
- Transmits sensations through nerve receptors.
- Produces and absorbs vitamin d
FACTORS AFFECTING PERSONAL HYGIENE
1. Culture
People from some cultures place a high value on personal cleanliness and feel unclean unless they shower or bathe at least once daily.
Culture may also influence whether bathing is a private or communal activity.
2. Socioeconomic class:
A person’s socioeconomic class and financial resources often define the hygiene options available to him or her eg. homeless people.
3. Spiritual practices
Spiritual practices, including religious beliefs, may dictate ceremonial washings and purifications, sometimes as a prelude to prayer or eating.
4. Developmental level
Family practices often dictate hygiene habits, such as morning or evening baths; the frequency of shampooing, tooth brushing, and clothing changes; feelings about nudity; and so on.
As adolescents become more concerned about their personal appearance, they may adopt new hygiene measures, such as taking showers more frequently and wearing deodorant.
5. Health state
Disease, surgery, or injury may reduce a person’s ability to perform hygiene measures or motivation to follow usual hygiene habits.
Weakness, dizziness, and fear of falling may prevent an individual from entering a tub or shower or from bending to wash the lower extremities.
6. Personal preferences:
People have different preferences with regard to hygiene practices such as taking a shower versus a tub bath, using bar soap versus liquid soap, and washing to wake oneself or to relax before sleep.
The Nursing Process For Skin Care And Personal Hygiene
5.1 ASSESSING
The comprehensive nursing assessment uses interview and physical assessment skills to elicit data about the patient’s hygiene status.
NURSING HISTORY
|
HYGIENE PRACTICES ASSESSMENTS |
|
|
Factors to assess |
Questions & approaches |
|
Daily and weekly bathing habits |
Tell me about your daily and weekly bathing habits. Are there special bathing or hygiene products you routinely use or can’t use? How can nurses best help you to meet your hygiene needs? |
|
Factors interfering with hygiene practices |
What recently or in the past has interfered with your hygiene practices? Does anything interfere with your ability to be as clean as you would like? |
|
Pain |
Do you have pain? Describe characteristics, onset, location, duration, associated symptoms, and intensity. Does the pain interfere with your ability to perform personal hygiene tasks? Does caring for yourself cause pain or discomfort? |
|
Exposure history |
Do you sunbathe? How much sun or tanning-booth exposure do you get? Do you use sunscreen? Does your job or daily activities/hobbies expose you to chemicals, such as bleach, petroleum, paint, insecticides, or cleaning products? |
|
History of skin or mucous membrane problems (nature, onset of problem and frequency, causes, severity, symptoms, interventions attempted, results) |
Describe any skin problems with rashes, lumps, itching, dryness, lesions, ecchymosis, or masses. What have you used to relieve these symptoms? |
|
Special hygiene practices • Mouth |
How do you clean your teeth and gums? How often do you have a dental examination? Do you have any dental appliances? Are there any tender areas or lesions in your mouth? |
|
• Eyes, ears, and nose |
Do you wear glasses or contact lenses to improve your vision? Do you wear a hearing aid? Have you experienced any discharge or bleeding from or swelling of your eyes, ears, or nose? |
|
• Hair |
Have you noticed any unusual dryness of the scalp or changes in hair texture and amount? |
|
• Feet and nails |
Is the appearance of the nails normal? How do you normally care for and clean your nails? Is the skin intact on the feet? Have you noticed any swelling of one or both feet? Do you wear any special shoes? |
|
• Perineum |
Have you noticed any unusual discharge, swelling, itching, or inflammation? Are you able to complete your own perineal care? Do you follow any special hygiene practices during menstruation? What type of feminine hygiene products (e.g., pads, tampons, douches) do you use? |
|
• Piercings |
Do you have any body piercings on your face, neck, arms, legs, torso, navel, or genitals? Have you experienced any problems related to the procedure? How do you care for your piercing(s)? |
Hygiene practices include bathing and care of the skin and specific body areas, including the oral cavity, eyes, ears, nose, hair, nails, feet, and perineal and vaginal areas.
1. Skin:
Any past or current problems:
- How long have you had this problem?
- Does it bother you?
- How does it bother you? Does it itch?
- Have you found anything that helps relieve these symptoms?
2. Oral cavity:
Obtain a nursing history related to the oral cavity, including structures such as the teeth, tongue, and salivary glands.
Identify any variables known to cause oral problems, such as:
- deficient self-care abilities
- poor nutrition
- excessive intake of refined sugars
- family history of periodontal disease
- ingestion of chemotherapeutic agents that produce oral lesions
Patients at increased risk for oral problems include:
- Those who are seriously ill, comatose, dehydrated, confused, depressed, or paralyzed
- Patients who are mouth breathers
- Those who can have no oral intake of nutrition or fluids
- Those with nasogastric tubes or oral airways in place
- Those who have had oral surgery are also at increased risk.
3. Eyes, ears and nose:
- Ask the patient to identify any special eye, ear, or nose care that he or she performs.
- Also, address any specific care measures related to the use and care of visual aids or prosthetics (glasses, contact lenses, artificial eye) and hearing aids.
- Inquire about any history of eye, ear, and nose problems, and related treatments.
4. Hair:
Identify the patient’s usual hair and scalp care practices, including styling preferences. Note any history of hair or scalp problems; possible causes of changes in the distribution, texture, or amount of hair; and related treatments.
Be alert for any factors that are known to cause hair or scalp problems or that require special care such as deficient self-care abilities, immobility, malnutrition, and treatments known to result in hair loss (e.g., certain chemotherapeutic agents).
5. Nails and feet:
- Gather information about the patient’s normal nail and foot care practices.
- Include the type of footwear worn and any history of nail or foot problems and their treatments.
- Foot problems, particularly common in people with diabetes mellitus and peripheral vascular disease, often require hospitalization.
- Identify any variables known to cause nail and foot problems, such as deficient self-care abilities, vascular disease, arthritis, diabetes mellitus, history of biting nails or trimming them improperly, frequent or prolonged exposure to chemicals or water, trauma, ill-fitting shoes, or obesity.
6. Perineal and vaginal areas:
Note any history of perineal or vaginal problems and related treatments.
Identify any variables known to cause perineal or vaginal problems or to create a need for special care, such as urinary or fecal incontinence, an indwelling Foley catheter, childbirth, douching, rectal or genital surgery, and diseases such as urinary tract infection, diabetes mellitus, and certain sexually transmitted infections (STIs) (e.g., herpes).
PHYSICAL ASSESSMENT
Assessment of body systems provides data about hygiene status and ability to maintain personal hygiene. Nurses can detect problems early and initiate appropriate interventions.
1. Musculoskeletal System
- Purpose: Determines ability to perform hygiene tasks independently.
- Common issues: Muscle weakness, decreased range of motion, impaired balance, fatigue, lack of coordination.
- Impact: May limit bathing, grooming, or oral care.
2. Skin Assessment
- Method: Inspect and palpate systematically (head-to-toe, good lighting, compare bilaterally).
- Assess: Cleanliness, color, texture, temperature, turgor, moisture, sensation, vascularity, lesions.
- Risk factors for skin problems: Immobility, poor self-care, malnutrition, dehydration, decreased sensation, sun exposure, vascular disorders, irritants (secretions, devices).
- Documentation: Use precise terms-location, size, distribution, appearance, consistency.
Common Skin Problems
- Dry Skin
- Symptoms: Scaling, flaking, itching, cracks.
- Care: Short lukewarm baths, mild soap, gentle drying, daily moisturizers, hydration, humidifier.
- Acne
- Symptoms: Plugged pores, pustules.
- Care: Gentle cleansing, oil-free products, avoid squeezing, keep hair clean/off face, sunscreen (avoid sun sensitivity).
- Skin Rashes
- Causes: Allergens, sun, systemic meds.
- Care: Mild cleansing, moisturizing (dry rash), drying agent (wet rash), tepid baths, antiseptic sprays, avoid irritant, see MD if worsening.

3. Oral Cavity
- Assess:
- Lips: Color, moisture, ulcers, edema.
- Mucosa/Gums: Color, lesions, bleeding, edema, exudate.
- Teeth: Caries, dentures, devices.
- Tongue: Color, symmetry, texture, lesions.
- Palates/Oropharynx: Intactness, lesions, tonsils, uvula movement.
- Other: Odors, mastication, swallowing ability.
Common Oral Problems
- Dental Caries: From plaque buildup- cavities. Prevention: limit sweets, fluoride toothpaste, flossing, regular dental visits.
- Periodontal Disease: Gingivitis/periodontitis- bleeding gums, pockets, tooth loss, halitosis. Requires dental care.
- Stomatitis: Oral mucosa inflammation; causes: infection, trauma, deficiencies.
- Glossitis: Inflamed tongue; causes: Vit B12, folate, iron deficiency.
- Cheilosis: Lip fissures; cause: Vit B complex deficiency.
- Dry mucosa: From dehydration, mouth breathing, meds.
- Oral Malignancies: Persistent sores, patches, swelling-early detection critical.
4. Eyes, Ears, Nose
- Eyes: Position, alignment, appearance, lashes, conjunctivae, blink reflex, visual acuity.
- Ears: Position, wax buildup, discharge, hearing acuity. (Older adults-dry cerumen may impair hearing).
- Nose: Appearance, patency, tenderness, discharge, bleeding, edema.
5. Hair & Scalp
- Assess: Texture, cleanliness, oiliness, scaling, lesions, dandruff, infestations, hair loss.
- Common Problems:
- Dandruff: Flaking/itching - treat with medicated shampoo.
- Alopecia: Hair loss (localized/systemic causes). Can be due to infection, hormones, deficiencies, medications, aging. Treatments: Minoxidil, hairpieces, transplantation.
- Pediculosis (Lice): Head, body, pubic lice. Signs: Nits, itching, scratch marks. Treatment: Pediculicides, environmental cleaning, repeat treatment.
- Ticks: Disease carriers. Remove with tweezers (close to skin), cleanse area.
6. Nails & Feet
- Assess nails: Cleanliness, intactness, contour, cap refill, nail base (redness, swelling, discharge, tenderness).
- Skin of feet: Cleanliness, swelling, lesions, inflammation, orthopedic problems, condition between toes.
7. Perineal & Vaginal Areas
- Male: Lesions, swelling, tenderness, discharge.
- Female: Color, size, lesions, masses, discharge.
- Anal area: Cracks, nodules, veins, polyps.
- Note odors (may indicate infection/poor hygiene).
5.2 DIAGNOSING
A careful assessment of the adequacy of a patient’s hygiene practices and the assessment of the skin, mucous membranes, and other body areas may lead to the identification of numerous patient problems that can be classified as nursing diagnoses.
The etiology of the problem directs nursing interventions
Each nursing diagnosis statement identifies a patient problem and suggests expected patient outcomes.
The following are examples of appropriate nursing diagnoses:
- Bathing Self-Care Deficit related to postoperative weakness
- Pain related to alteration in skin integrity
- Ineffective Coping related to chronic skin disease
- Ineffective Health Maintenance: dental caries related to deficient oral hygiene practices
- Impaired Oral Mucous Membrane related to malnutrition and dehydration
- Impaired Social Interaction related to negative body image: acne
- Imbalanced Nutrition: Less Than Body Requirements related to stomatitis
Outcome Identification And Planning
The plan of nursing care identifies nursing measures to assist the patient to develop or maintain hygiene practices that contribute to a sense of well-being. Appropriate expected outcomes include the following: The patient will:
- Verbalize feeling comfortable and clean
- Participate fully in necessary hygiene measures according to cognitive, sensory, mobility, and endurance abilities
- Maintain intact skin and mucous membranes
- Demonstrate correct skin care measures (when indicated) such as oral care, care of eyes, ears, and nose, nail and foot care, and perineal and vaginal care
- Demonstrate signs of healing in existing lesions (oral, scalp, or perineal)
- Exhibit lips, oral mucosa, gums, and tongue that are intact, moist, and free of inflammation and lesions
- Verbalize importance of good teeth-brushing habits, fluoride use, and regular dental examinations
- Demonstrate healthy functioning of eyes, ears, and nose
- Exhibit eyes, ears, and nose that appear clean
- Demonstrate proper use and care of visual or auditory aids
- Exhibit clean hair
- Verbalize satisfaction with appearance
- Participate in hair and scalp care as able
- Exhibit intact, clean, and manicured nails
- Demonstrate intact, clean, and lesion-free foot skin
- Report reduced or absent nail and foot problems (specify: calluses, corns, plantar warts, ingrown nails, athlete’s foot)
Implementation
General Principles
- Respect patient preferences and cultural norms.
- Encourage self-care as much as possible to maintain independence.
- Maintain privacy and dignity.
- Promote physiologic and psychological wellness.
- Hygiene care is an opportunity for:
- Assessing skin and overall health
- Teaching self-care
- Strengthening nurse-patient rapport
Scheduled Hygiene Care
1. Early Morning Care
- Soon after waking.
- Focus: Toileting, face and hand washing, oral care, comfort measures.
- Prepares patient for breakfast or tests.
2. Morning Care (A.M.)
- After breakfast.
- Includes: Toileting, oral care, bathing, back massage, hair care (shaving if indicated), dressing, skin care (e.g., pressure ulcer prevention), cosmetics, positioning.
- Enhances morale and hygiene.
3. Afternoon Care (P.M.)
- After lunch, before visitors/rest.
- Focus: Comfort, handwashing, oral care, toileting, bed linen straightening, repositioning for mobility-impaired patients.
4. Hour of Sleep Care (H.S.)
- Before bedtime.
- Include: Toileting, face and hand washing, oral care, back massage, linen change, positioning, and accessibility of call light and personal items.
5. As-Needed Care (P.R.N.)
- Provided in addition to scheduled care.
- Examples: Oral care every 1-2 hours for high-risk patients, changing linens/clothing for diaphoretic patients.
- Sometimes care may be withheld for uninterrupted rest if clinically appropriate.
Bathing and Skin Care
Purposes of Bathing
- Cleansing and conditioning skin
- Relaxation and comfort
- Promoting circulation and joint mobility
- Stimulating respiration
- Improving self-image and sensory input
- Strengthening nurse-patient relationship
Types of Bathing
- Shower
- Preferred for ambulatory patients.
- Safety: Mats, non-slip strips, proper temperature (110-115°F / 43-46°C).
- Provide a chair or stool if needed.
- Assist with entering/exiting tub; maintain privacy.
- Reduce stimuli for confused patients.
- Tub Bath
- Used based on patient tolerance and facility policy.
- Assist with safe entry/exit and provide support.
- Bed Bath
- For patients confined to bed or with limited mobility.
- Provide basin of warm water, bath blanket, privacy, and accessible call light.
- Patients may assist with areas they can reach; nurse completes rest.
- Bag Bath / Disposable Bath
- Pre-moistened or reusable washcloths in a bag.
- No rinsing required; skin allowed to air-dry.
- Time-saving, effective for patients with mild to moderate skin impairments.
Promoting Skin Health
- Use soap substitutes or nonsoap emollient cleansers to prevent drying.
- Apply topical emollients (lotions, creams, gels, ointments) post-bath to hydrate and restore skin barrier.
- Use skin barrier products (creams, films, ointments) to protect vulnerable skin (e.g., around stomas, wounds, exposure to urine/feces).
- Application frequency: Ideally twice daily or as indicated by skin condition.
Massaging the Back
- Follow bath with backrub to:
- Relieve muscle tension, promote relaxation
- Improve circulation
- Reduce pain, anxiety, and distress
- Improve sleep quality
- Assess skin for breakdown
- Duration: 4-6 minutes; warm lotion recommended.
- Contraindications: Recent back surgery, fractures, or other specific medical conditions.
- Position: Prone or side-lying if prone not possible.
SKILL: Giving a Bed Bath
Purpose: To maintain patient hygiene, prevent infection, promote comfort, preserve skin integrity, and respect patient dignity and privacy.
Preparation
- Review Patient Chart: Assess limitations in mobility or activity to prevent discomfort or injury.
- Gather Supplies: Basin, warm water (110-115°F), soap/skin cleanser, towels, washcloths, bath blanket, clean gown, gloves, PPE if indicated. Bring all equipment to bedside to save time and avoid unnecessary strain.
- Hand Hygiene & PPE: Perform hand hygiene. Use gloves or other PPE based on transmission precautions.
- Patient Identification & Communication: Identify patient. Explain procedure. Assess ability to assist and personal hygiene preferences.
- Privacy & Environment: Close curtains and doors if possible. Adjust room temperature. Ensure comfort and prevent heat loss.
- Pre-Bath Preparations: Remove sequential compression devices and antiembolism stockings per protocol. Offer bedpan or urinal to reduce interruptions. Adjust bed to caregiver elbow height for proper ergonomics.
Positioning & Linen Management
- Position Patient: Assist patient to side of bed nearest to you. Patient lies on back.
- Linen Handling: Loosen top covers; place bath blanket over patient. Remove top sheet while maintaining privacy. Fold soiled linen carefully; place in laundry bag to prevent contamination.
- Gown Removal: Remove gown while keeping bath blanket in place. Handle IV lines carefully, maintaining flow rates.
- Safety Measures: Raise side rails for safety. Ensure gloves are worn if contact with body fluids is anticipated.
Bathing Procedure
Face, Neck, and Ears: Use a clean, damp washcloth; no soap unless indicated. Apply emollient for skin integrity.
Arms: Expose far arm first; place towel underneath. Wash hand, arm, axilla with firm strokes. Rinse and dry; apply emollient.
Chest and Abdomen: Cover chest with towel; lower bath blanket. Wash, rinse, dry chest and abdominal folds. Inspect umbilical area and skin creases.
Legs and Feet: Expose far leg; place towel underneath. Wash from ankle to groin, rinse, dry; apply emollient. Wash and dry feet thoroughly, including between toes. Repeat for near leg and foot.
Back and Buttocks: Assist patient to prone or side-lying position. Expose back/buttocks with bath blanket and towel for privacy. Wash, rinse, dry; focus on skin folds and bony prominences. Inspect for redness or skin breakdown.
Backrub: Optional, if not contraindicated. Improves circulation, relaxation, and tissue integrity. Apply emollient or skin barrier as needed.
Perineal Care: Refill basin with clean water; use fresh washcloth and towel. Assist patient or perform care if unable. Apply skin barrier if indicated to protect skin from moisture and irritants. Maintain privacy and warmth.


Finishing Up
- Gown & Grooming: Help patient into a clean gown. Assist with personal toiletries (deodorant, cosmetics). Protect pillow with towel and groom hair.
- Safety & Comfort: Ensure patient is comfortable. Raise side rails. Return bed to lowest position.
- Bed Linen: Change soiled linens per policy. Dispose of contaminated linens properly.
- Hand Hygiene & PPE: Remove gloves and PPE. Perform hand hygiene.
Key Principles of giving a bed bath:
|
Step |
Rationale |
|
Hand hygiene & PPE |
Prevents spread of microorganisms. |
|
Privacy & warmth |
Maintains dignity and prevents heat loss. |
|
Patient participation |
Encourages independence and individualized care. |
|
Proper bed height & positioning |
Prevents caregiver musculoskeletal strain. |
|
Emollients |
Maintain and restore skin integrity. |
|
Firm, long strokes |
Stimulate circulation, remove debris, relax patient. |
|
Skin fold inspection |
Prevent odor, skin breakdown, infections, and decubitus ulcers. |
|
Perineal care |
Reduces risk of infection and discomfort. |
|
Gloves change for perineal care |
Prevents contamination and transmission of pathogens. |
|
Backrub |
Enhances circulation, relaxation, and tissue health. |
Documentation
- Note patient’s tolerance, assistance needed, areas of skin breakdown, and any abnormal findings.
- Record skin care products applied, patient response, and completion of procedure.
Oral Hygiene
Importance
- Prevents deterioration of oral cavity.
- Reduces colonization of pathogens- lowers risk of aspiration pneumonia and systemic infection.
- Supports comfort and well-being.
Techniques
- Tooth Brushing
- Soft-bristled, small brush to reach all teeth; clean tongue.
- Brush after meals; clean brushes between uses.
- Electric/automatic brushes are effective.
- Flossing
- Removes debris and bacteria between teeth once daily.
- Mouthwash
- Reduces plaque, gingivitis, halitosis; fluoride rinses prevent cavities.
- Not effective for systemic halitosis (e.g., onion/garlic).
- Dentures
- Remove and clean daily; use cool/lukewarm water, soft brush.
- Store in cold water when not in use; avoid wrapping in tissue.
- Encourage patient to brush gums and tongue before reinsertion.
- Handle carefully to prevent damage.
Nursing insights: Special Considerations
- Patients with physical/cognitive limitations may require frequent assistance (every 1-2 hours).
- Moisturize lips and oral mucosa regularly if patient cannot drink.
- Older adults or patients with dexterity issues are at higher risk for inadequate oral hygiene.
SKILL: Assisting patient with oral care
Purpose: To maintain oral hygiene, prevent infection, promote comfort, and preserve healthy teeth and gums.
Preparation
- Hand Hygiene & PPE: Perform hand hygiene. Put on gloves if assisting; use additional PPE as indicated. Prevents spread of microorganisms.
- Patient Identification & Communication: Identify the patient. Explain the procedure to promote cooperation and reduce anxiety.
- Equipment & Environment
- Assemble equipment (toothbrush, toothpaste, dental floss, mouthwash, towel, emesis basin) on overbed table within reach.
- Close room door or curtains for privacy.
- Adjust bed to comfortable working height (elbow height of caregiver). Organization facilitates task performance; privacy maintains dignity; proper bed height reduces caregiver strain.
- Patient Positioning: Assist patient to sitting position if allowed, or side-lying if necessary- prevents aspiration of fluids. Place towel across patient’s chest; towel protects patient’s clothing.
Oral Care Procedure
Brushing Teeth
- Moisten toothbrush and apply toothpaste.
- Hold brush at 45-degree angle to gum line.
- Brush from gum line to crown:
- Outer and inner surfaces.
- Biting surfaces.
- Back-and-forth motion.
- Brush tongue gently.
- Have patient rinse vigorously with water; use suction if patient cannot expectorate.
Proper brushing removes plaque, tartar, and debris. Tongue brushing removes coating and bacteria. Suction prevents aspiration if patient cannot spit.
Flossing (if indicated)
- Remove ~6 inches of floss or use floss holder.
- Wrap floss around index fingers, keeping 1-1.5 inches taut.
- Insert gently between teeth, moving down to gums; then up and down along both sides of each tooth.
- Repeat between all teeth.
- Have patient rinse thoroughly.
Flossing removes plaque and promotes healthy gums. Taut floss ensures proper cleaning. Gentle technique prevents gum trauma.
Optional Care
- Offer mouthwash for freshening- Mouthwash improves oral freshness.
- Apply lip balm or petroleum jelly to prevent dryness.

Finishing Up
- Remove equipment; discard gloves.
- Raise side rail and lower bed.
- Assist patient to comfortable position.
- Remove any PPE used.
- Perform hand hygiene.
Note:
- Proper removal of gloves and PPE prevents infection transmission.
- Hand hygiene protects both patient and caregiver.
- Positioning ensures comfort and safety.
Key Principles of oral care
|
Step |
Key Point |
Rationale |
|
Hand hygiene & PPE |
Before procedure |
Prevents spread of microorganisms |
|
Patient ID & explanation |
Communication before care |
Promotes cooperation, reduces anxiety |
|
Proper positioning |
Sitting or side-lying |
Prevents aspiration; enhances comfort |
|
Brushing technique |
45° angle, thorough coverage |
Removes plaque, tartar, and debris; protects gums |
|
Tongue brushing |
Gentle |
Reduces coating, bacteria, and odor |
|
Flossing |
Taut floss, gentle |
Cleans interdental surfaces; prevents gum trauma |
|
Mouthwash/lip care |
Optional |
Promotes freshness and comfort |
|
Disposal & hygiene |
Remove gloves/PPE, hand hygiene |
Prevents infection transmission |
|
Comfort & safety |
Bed rails, patient positioning |
Ensures safety and dignity |
Eye Care
Normal Eye Care:
- Eyes are naturally cleaned by lacrimal secretions.
- During illness, eyes may produce excess secretions; appear glasslike.
Techniques for Cleaning Eyes:
- Wear gloves.
- Use water or normal saline; never use soap.
- Position patient on the same side as the eye being cleaned.
- Wipe from inner canthus to the outer canthus.
- Use a clean section of cloth or a new cotton ball for each wipe.
- For stubborn secretions: apply a warm, wet compress for 3-5 minutes.
- Always clean the other eye afterward.
Unconscious Patients:
- Blink reflex may be diminished/absent; eyelids may remain open.
- Provide eye care every 4 hours to prevent corneal ulceration.
- Use saline or artificial tears and a protective eye shield.
Eyeglass Care
- Place glasses lenses up when not in use.
- Clean over a terry towel with warm water and soap or special cleaner.
- Rinse thoroughly and dry with soft cotton cloth.
- Avoid hot water, paper tissues, or silicone tissues to prevent scratching.
Contact Lens Care
- Types: Hard (rigid gas-permeable) and soft (daily, extended, or disposable).
- Perform strict hand hygiene; wear gloves before handling.
- Avoid exposure to cosmetics, soaps, smoke, or noxious vapors.
- Hard lenses: wear 12-16 hours max; remove before sleeping.
- Extended-wear soft lenses: 1-30 days, cleaned at least weekly.
- Disposable lenses: vary from daily to 14 days depending on type.
- Remove immediately if excessive tearing, redness, or pain occurs.
- Nurses are responsible for removing lenses in unconscious patients.
- Use gentle pressure or suction device for hard lenses; do not remove if eye injury present.
Artificial Eye Care
- Encourage patient self-care if possible.
- Equipment: basin, soap, water, saline.
- Flush socket with saline before replacing the prosthesis.
- Keep patient lying down to prevent dropping the prosthesis.
Ear Care and Nose care
Ear care
- Clean outer ears only; dry carefully with a soft towel.
- Avoid cotton swabs, pins, paper clips, or fingernails.
- Hearing aid care:
- Check batteries regularly.
- Clean earpieces daily with mild soap and water.
- Whistling sound- battery functioning.
- For mild hearing loss without hearing aid:
- Avoid noisy areas, ensure good lighting, face speaker, ask for repetition, consider amplitude devices.
Nose Care
- Clean by gently blowing both nostrils open.
- Apply warm, moist compress to soften crusts.
- Use disposable tissues.
- Avoid irrigations and inserting cotton swabs deeply.
Hair Care
- Daily brushing: distributes oils, prevents matting, stimulates circulation.
- Long hair: consider braiding; avoid tight braids.
- Special considerations for curly or chemically straightened hair.
- Shampooing:
- Can be done in shower by patient or bedside if on bedrest.
- Bedside hair care: use warm water, shampoo, conditioner; protect with towel or hair tray.
- Rinseless shampoos or shampoo caps available.
- Cultural sensitivity: style hair according to patient preference.
Shaving
- Requires patient consent.
- Electric razors recommended for patients on anticoagulants or bleeding disorders.
- Shave after warm bath/shower to soften hair.
Procedure:
- Perform hand hygiene and put on disposable gloves (contact with blood is possible if any skin nicks occur).
- Cover patient’s chest with a towel or waterproof pad. Fill bath basin with warm (43° to 46°C [110° to 115 °F]) water. Press a warm washcloth on the patient’s facial skin to soften the hair.
- Dispense shaving cream into palm of hand. Rub hands together, then apply to area to be shaved in a layer approximately 0.5” thick.
- With one hand, pull the skin taut at the area to be shaved. Using a smooth stroke, begin shaving. If shaving the face, shave with the direction of hair growth in downward, short strokes. If shaving a leg, shave against the hair in upward, short strokes.
- Wash off residual shaving cream.
- If patient requests, apply aftershave or lotion to area shaved.
- Remove and discard gloves and perform hand hygiene.
Fingernail Care
- File nails in oval shape; avoid cutting too deep.
- Remove hangnails carefully.
- Push back cuticles gently after soaking.
- Apply emollient to prevent hangnails.
- Avoid contact with harsh soaps and acetone-based polish removers.
Foot Care
- Especially important for elderly, diabetics, or patients with circulatory problems.
- Techniques:
- Wash with mild soap and tepid water; clean interdigital spaces.
- Dry thoroughly; apply moisturizer to dry areas.
- Diabetics: sprinkle talcum/cornstarch between toes; file nails, avoid cutting.
- Avoid cutting corns/calluses; consult podiatrist if present.
- Wear appropriate footwear and socks; avoid going barefoot.
- Elevate feet if swollen; avoid heating pads.
- Report any foot problems promptly.
Perineal and Genital Care:
1. Perineal Care
- Perform in a matter-of-fact, dignified manner to reduce embarrassment.
- Supplies: mild unscented soap, water, washcloths, disposable gloves.
- Steps:
- Provide privacy, explain procedure, perform hand hygiene, wear gloves.
- Wash and rinse groin area:
- Female: spread labia, wash from pubic area to the anal area.
- Male: wash tip of penis first (circular motion), then shaft downward.
- Uncircumcised males: retract foreskin while washing, return it afterward.
- Wash and rinse scrotum gently.
- Dry thoroughly, apply emollient as indicated; avoid powder.
- Turn patient to side, cleanse anal area from least to the most contaminated.
- Remove gloves, perform hand hygiene.
Nursing insights: Special Considerations
-
- Patients with indwelling catheters: catheter care usually follows perineal care.
- Incontinent patients:
- Risk for skin damage due to moisture, pH changes, bacterial overgrowth, friction.
- Use perineal skin cleansers, moisturizers, barriers.
- Clean immediately after soiling; avoid harsh soap and forceful scrubbing.
2. Vaginal Care
- Vaginal secretions are normally odor-free; mild soap and water sufficient.
- Routine douching is unnecessary and discouraged (removes normal flora, may cause irritation or infection).
- Deodorants:
- Not necessary; no proven therapeutic benefit.
- External use only; avoid broken skin and sanitary products.
- Educate patients on safe use if insisted upon.
3. Care for Body Piercings
- Piercings may be present on face, ears, neck, torso, genitals.
- Care includes assessment and wound aftercare.
- Techniques aim to prevent infection and promote healing.
Environmental Care
- Clean, clutter-free, safe, and pleasant environment improves well-being.
- Essentials: bed, overbed table, bedside stand, chairs, call light, oxygen, suction, bath/emesis basins, linens.
- Always ask permission before handling patient’s personal items.
- Maintain ventilation and odor control (empty waste, use deodorizers as needed).
- Room temperature: 20-23°C (68-74°F); respect patient preference.
- Minimize noise and harsh lighting; protect patient privacy.
Bed Safety and Comfort
- Bed responsibilities: safe, comfortable, and functional.
- Motorized beds: adjust height, head, and foot positions; teach patient/family safe use.
- Side rails: use as indicated and per policy.
- Locks: wheels/casters locked when stationary.
- Before leaving bedside:
- Bed lowest position.
- Safe bed position.
- Functioning bed controls and call light.
- Side rails raised if indicated.
- Mattress firm, clean, water-repellent; therapeutic mattresses as needed.
- Bed linens: clean, free of crumbs/wrinkles, patient comfortably warm.
- Change after bath or when soiled; coordinate with assistive personnel.
Making a Bed
- Occupied bed: use appropriate technique to maintain comfort.
- Minor variations are acceptable depending on patient condition or equipment.
- Protect pressure areas from rough edges or wrinkles.
Skin Care and Hygiene Education
1. Soaps and Detergents
- Soaps: vegetable/animal fats; detergents: petroleum derivatives.
- Non-soap cleansers may benefit dry or sensitive skin.
- Expensive products are not more effective than standard options.
2. Deodorants and Antiperspirants
- Perspiration odor caused by bacterial action on sweat.
- Keep body and clothing clean.
- Use deodorants/antiperspirants after cleansing.
- Use with care to prevent irritation; contraindicated in some situations (e.g., pre-mammography, post-mastectomy).
3. Cosmetics
- Enhance appearance; may improve self-esteem.
- Cultural/religious considerations may limit use.
- Avoid contaminated cosmetics; do not share.
- Discard after 2-4 months, especially near eyes.
- Keep applicators clean.
Summary
- Various health beliefs, personal, sociocultural, economic, and developmental factors influence patients’ hygiene preferences and practices.
- Sound clinical judgment requires you to consider a patient’s condition, anticipate any risks or problems, gather thorough assessment data, and then analyze data to form nursing diagnoses.
- Hygiene needs, preferences, and the ability to participate in care change as people age.
- Assess a patient’s skin, feet and nails, oral mucosa, hair, and eyes and ears to obtain a complete assessment of the patient’s hygiene needs.
- Assess a patient’s physical and cognitive ability to perform basic hygiene measures.
- Vascular insufficiency and reduced mobility, cognition, and sensation increase a patient’s risk for impaired skin integrity.
- Diabetes mellitus and peripheral vascular diseases increase the patient’s risk for foot and nail problems.
- Clinical judgment and critical thinking about a patient’s hygiene preferences, needs, and ability to participate in care results in patient-centered hygiene care matching the patient’s needs and preferences.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Hygiene
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


