Please set your exam date
Somatic Symptom and Related Disorders
Study Questions
Practice Exercise 1
A 45-year-old female has constant complaints of dizziness and weakness. The client has been referred to specialists for medical evaluation. All tests have been negative. The physician has concluded that the client has a somatic disorder. How should the nurse deal with this client?
Explanation
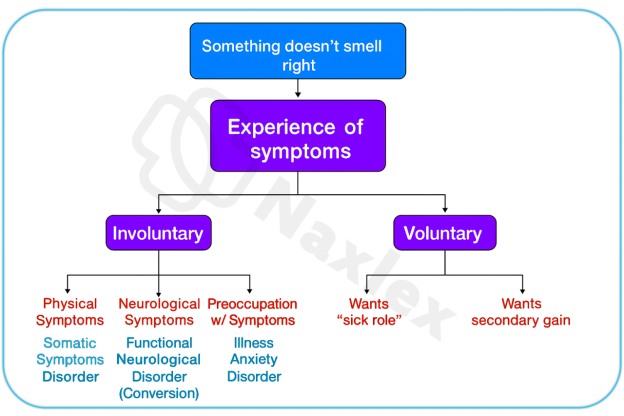
Somatic symptom disorderis a psychiatric condition characterized by persistent physical symptoms that cause significant distress or impairment, despite no identifiable medical cause. The symptoms are not intentionally produced or feigned, and the individual genuinely experiences them. The disorder involves excessive thoughts, feelings, or behaviorsrelated to the symptoms, often leading to frequent healthcare visits and functional impairment. It is crucial to validate the patient’s experience while avoiding unnecessary medical interventions.
Rationale for correct answers
3.The nurse must acknowledge that the client’s symptoms are realto her, even if no organic cause is found. This approach builds trustand supports therapeutic communication, which is essential in managing somatic symptom disorder.
Rationale for incorrect answers
1.Focusing on test results may invalidatethe client’s experience and reinforce the belief that the nurse does not understand her suffering, worsening distress.
2.Suggesting outside interests implies the symptoms are due to boredom, which trivializes the client’s condition and may be perceived as dismissive or judgmental.
4.Ignoring the complaints violates the principle of empathyand therapeutic presence, potentially increasing the client’s anxiety and feelings of isolation.
Take Home Points
- Somatic symptom disorder involves genuine physical symptoms without identifiable medical cause, requiring empathetic and supportive care.
- Validation of the patient’s experience is essential to build trust and reduce psychological distress.
- Avoid reinforcing symptom preoccupation by excessive medical testing or dismissive communication.
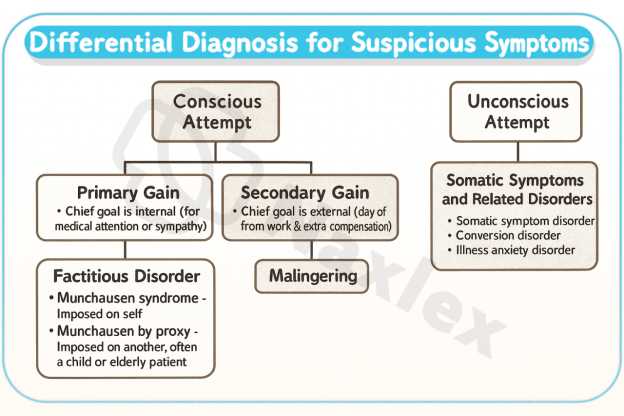
- Differentiate from factitious disorder and malingering, which involve intentional symptom production.
A nurse is caring for a client diagnosed with conversion disorder who has developed paralysis of her legs. Diagnostic tests fail to uncover a physiologic cause. During the working phase of the nurse-client relationship, the client says to her nurse, “You think I could walk if I wanted to, don’t you?” Which response by the nurse would be best?
Explanation
Conversion disorderis a subtype of functional neurological symptom disorder characterized by neurological symptoms—such as paralysis, blindness, or seizures—that are inconsistent with known medical conditions. These symptoms are not intentionally produced and often follow psychological stress. The disorder reflects a disruption in voluntary motoror sensory function, and the symptoms are real to the patient. Management requires a nonjudgmentaland validating approach that avoids reinforcing symptom preoccupation while maintaining therapeutic rapport.
Rationale for correct answers
4.This response affirms the client’s experiencewithout challenging the authenticity of the symptoms. It maintains neutralityand supports the therapeutic alliance during the working phase of care.
Rationale for incorrect answers
1.Suggesting volitional control implies the symptoms are intentional, which invalidates the client’s experience and may provoke defensiveness or shame.
2.Redirecting the conversation to the nurse’s opinion shifts focus away from the client’s concerns, missing an opportunity for therapeutic engagement.
3.Asking the client to self-assess volitional control may reinforce guilt, as it implies the client is responsible for the symptoms, which is clinically inappropriate.
Take Home Points
- Conversion disorder presents with neurological symptoms that lack a medical explanation but are not consciously produced.
- Therapeutic communication must validate the client’s experience without reinforcing symptom preoccupation or implying intentionality.
- Avoid statements that suggest the client has control over the symptoms; this can damage trust and worsen psychological distress.
- Differentiate conversion disorder from malingering and factitious disorder, which involve conscious symptom fabrication.
A nurse is caring for a client who displays gait disturbances, paralysis, pseudoseizures, and tremors. These symptoms may be manifestations of what psychiatric disorder?
Explanation
Conversion disorderis a psychiatric condition characterized by sudden onset of motor deficits, pseudo seizures, or sensory lossthat cannot be explained by medical findings. These symptoms often follow psychological stress and are not consciously produced. The disorder reflects a disruption in voluntary neurological function and is part of the somatic symptom and related disorders category. Symptoms are real to the patient and may include tremors, paralysis, or abnormal gait.
Rationale for correct answers
4.The presence of motor symptoms like tremors and gait disturbance without a medical cause is consistent with conversion disorder, which involves neurological symptomstriggered by psychological stress.
Rationale for incorrect answers
1.Pain disorder centers on painas the primary symptom, not motor or neurological deficits like paralysis or pseudo seizures.
2.Adjustment disorder involves emotional or behavioral symptoms in response to a stressor, not neurological manifestations.
3.Delirium presents with cognitiveimpairment and fluctuating consciousness, not isolated motor symptoms or pseudo seizures.
Take Home Points
- Conversion disorder presents with motor or sensory symptoms that lack a neurological basis and follow psychological stress.
- Symptoms are involuntary and real to the patient, requiring empathetic and nonjudgmental care.
- Differentiate from malingering and factitious disorder, which involve conscious symptom fabrication.
- Avoid reinforcing symptom preoccupation; focus on functional recovery and psychological support.
Lorraine has been diagnosed with somatic symptom disorder. Which of the following symptom profiles would you expect when assessing Lorraine?
Explanation
Somatic symptom disorderinvolves persistent and distressing physical symptomsthat affect multiple body systems and are accompanied by excessive thoughts, feelings, or behaviorsrelated to those symptoms. These symptoms are authentic and may coexist with medical conditions, but the patient’s response is disproportionate. The disorder is marked by high healthcare utilization and functional impairment, and the symptoms are not intentionally fabricated.
Rationale for correct answers
1.Multiple somatic complaints across systems reflect the broad symptomprofile typical of somatic symptom disorder, often accompanied by emotional distressand healthcare-seeking behavior.
Rationale for incorrect answers
2.Fear of disease is characteristic of illnessanxiety disorder, where the concern is about having a serious illness despite minimal symptoms.
3.Sensorimotor loss is seen in conversiondisorder, not somatic symptom disorder, which involves widespread physical complaints.
4.Belief in body deformity is typical of bodydysmorphic disorder, which involves preoccupation with perceived flaws, not multisystem symptoms.
Take Home Points
- Somatic symptom disorder involves multiple physical complaints with excessive emotional and behavioral responses.
- Symptoms are real and may coexist with medical conditions, but the distress is disproportionate.
- Illness anxiety disorder focuses on fear of disease without significant somatic symptoms.
- Body dysmorphic disorder involves distorted body image, not widespread somatic complaints.
Which of the following ego defense mechanisms describes the underlying psychodynamics of somatic symptom disorder?
Explanation
Somatic symptom disorderis a psychiatric condition where individuals experience multiple physicalsymptoms that are distressing and medically unexplained. These symptoms are not intentionally produced and often reflect underlying emotional conflict. Psychodynamically, the disorder is linked to unconscious defense mechanisms, particularly repression, where psychological distress is converted into physical symptoms to avoid conscious awareness of internal conflict.
Rationale for correct answers
2.Repression involves the unconscious blocking of anxiety-provokingthoughts, which then manifest as physical symptoms. This mechanism underlies the conversionof emotional distress into somatic complaints.
Rationale for incorrect answers
1.Denial is a conscious or unconscious refusal to accept reality, but it does not explain the transformation of emotional conflict into physical symptoms.
3.Suppression is a consciousdecision to postpone dealing with distressing emotions, unlike repression which is unconscious and central to somatic symptom disorder.
4.Displacement involves redirecting emotionsto a safer target, not converting them into physical symptoms as seen in somatic presentations.
Take Home Points
- Somatic symptom disorder is linked to unconscious emotional conflict manifesting as physical symptoms.
- Repression is the primary defense mechanism, converting psychological distress into somatic complaints.
- Differentiation from suppression and displacement is essential due to their conscious nature.
- Management requires understanding the psychodynamic roots and avoiding reinforcement of symptom preoccupation.
Nursing care for a client with somatic symptom disorder would focus on helping her to:
Explanation
Somatic symptom disorderinvolves persistent physical symptoms that cause significant distress and functional impairment. These symptoms are not intentionally produced and often reflect maladaptive copingwith psychological stress. Nursing care emphasizes promoting adaptive strategies, improving emotional regulation, and reducing healthcare-seeking behaviors. The goal is to enhance functionalityand reduce symptom preoccupation through therapeutic engagement and behavioral interventions.
Rationale for correct answers
4.Teaching adaptive coping strategies helps the client manage stressmore effectively, reducing reliance on physical symptoms as a form of emotional expression and improving function.
Rationale for incorrect answers
1.Eliminating stress is unrealistic and may reinforce avoidancerather than teaching the client how to cope with stressors constructively.
2.Focusing on discontinuing complaints invalidates the client’s experience, potentially damaging the therapeutic relationship and increasing distress.
3.Medication adherence is important but does not address the corepsychological mechanisms driving the disorder, making it insufficient as a primary nursing goal.
Take Home Points
- Nursing care for somatic symptom disorder centers on promoting adaptive coping and emotional regulation.
- Reassurance and validation must be balanced with behavioral strategies to reduce symptom focus.
- Medication adherence alone is not sufficient to address underlying psychological distress.
- Avoid invalidating the client’s experience; instead, guide toward functional improvement and emotional insight.
Practice Exercise 2
Lorraine, a client diagnosed with somatic symptom disorder, states, “My doctor thinks I should see a psychiatrist. I can’t imagine why he would make such a suggestion.” What is the basis for Lorraine’s statement?
Explanation
Somatic symptom disorderinvolves persistent physical symptoms that cause significant distress and functional impairment, often without a clear medical cause. The symptoms are not intentionally produced and reflect maladaptive coping, emotional dysregulation, and heightened sensitivityto bodily sensations. Patients frequently lack insight into the psychological origins of their symptoms and may misinterpret psychiatric referrals as dismissive or irrelevant to their physical complaints.
Rationale for correct answers
2.Lorraine’s confusion reflects a lack of understanding of the linkbetween psychological stress and physical symptoms. This is common in somatic symptom disorder, where emotional distress is somatized.
Rationale for incorrect answers
1.The belief that the doctor wants to abandon her implies rejection, but this is not the core issue; Lorraine’s concern is rooted in misunderstanding.
3.Associating psychiatry with “crazy” implies stigma, but the stem does not suggest Lorraine holds this belief specifically.
4.Thinking the diagnosis is wrong reflects denial, but Lorraine’s statement centers more on confusion than disbelief in the diagnosis.
Take Home Points
- Patients with somatic symptom disorder often lack insight into the psychological basis of their symptoms.
- Psychiatric referrals may be misinterpreted as dismissive or irrelevant due to poor understanding of mind-body connections.
- Education on the role of stress and emotional factors in physical symptoms is essential.
- Empathetic communication helps reduce resistance and stigma around psychiatric care.
Lorraine, a client diagnosed with somatic symptom disorder, tells the nurse about a pain in her side. She says she has not experienced it before. Which is the most appropriate response by the nurse?
Explanation
Somatic symptom disorderpresents with recurrent physical complaints that are distressing and often medically unexplained. These symptoms are real, persistent, and emotionally charged. Nursing care must balance validationwith structured boundaries to avoid reinforcing symptom preoccupation. Therapeutic communication should acknowledge the symptom while maintaining routine and promoting functional engagement.
Rationale for correct answers
3.This response acknowledges the symptom and ensures continuityof care by reporting it, while maintaining structureby encouraging group therapy attendance.
Rationale for incorrect answers
1.Dismissing the complaint as “in your head” reflects invalidatinglanguage and undermines therapeutic rapport, increasing emotional distress.
2.Skipping group therapy reinforces avoidance, which may worsen functional impairment and reduce engagement in therapeutic activities.
4.Offering new medication without assessment promotes reinforcementof somatic focus and may lead to unnecessary pharmacologic interventions.
Take Home Points
- Nursing responses should validate symptoms while maintaining therapeutic boundaries and routine.
- Avoid reinforcing symptom preoccupation through excessive attention or unnecessary interventions.
- Encourage participation in structured activities to promote functional improvement.
- Balance empathy with clinical judgment to support emotional and physical well-being.
Lucille has a diagnosis of somatic symptom disorder, predominantly pain. Which of the following medications would the psychiatric nurse practitioner most likely prescribe for Lucille?
Explanation
Duloxetineis a serotonin-norepinephrine reuptake inhibitor (SNRI) used for chronic pain, major depression, and generalized anxiety disorder. It modulates descending inhibitory pain pathways by increasing serotonin and norepinephrine levels in the central nervous system. It is FDA-approved for fibromyalgia, diabetic neuropathy, and musculoskeletal pain, making it suitable for patients with somatic symptom disorder where pain is the predominant feature. It is contraindicated in uncontrolled narrow-angle glaucoma and should be used cautiously in hepatic impairment.
Rationale for correct answers
4.Duloxetine targets both painand mood symptoms by enhancing serotonergic and noradrenergic transmission, making it effective for somatic symptom disorder with pain predominance.
Rationale for incorrect answers
1.Chlorpromazine is an antipsychotic used for psychosis, not indicated for somatic symptom disorder or pain management.
2.Diazepam is a benzodiazepine used for anxietyand muscle spasms, but it carries dependency risks and lacks efficacy for chronic pain.
3.Carbamazepine is an anticonvulsant used for seizuresand trigeminal neuralgia, not appropriate for generalized somatic pain.
Take Home Points
- Duloxetine is effective for somatic symptom disorder with predominant pain due to its dual action on serotonin and norepinephrine.
- Benzodiazepines are not first-line for chronic somatic pain due to tolerance and dependency risks.
- Antipsychotics and anticonvulsants are reserved for specific psychiatric or neurological conditions, not somatic pain syndromes.
- Always assess comorbidities and contraindications before initiating pharmacologic treatment for somatic symptom presentations.
The nurse is caring for a client with a conversion disorder. Which of the following assessments will the nurse expect to see?
Explanation
Conversion disorderpresents with neurological symptoms such as paralysis, blindness, or seizuresthat are inconsistent with medical findings. A classic feature is la belle indifférence, an apparent lack of concern about the symptoms. This paradoxical indifference, despite potentially disabling symptoms, reflects the unconscious nature of the disorder and helps differentiate it from malingering or factitious disorder. The symptoms are real to the patient and not intentionally produced.
Rationale for correct answers
2.Indifference to symptoms, known as la belle indifférence, is a hallmark of conversion disorder and reflects unconscious defensemechanisms.
Rationale for incorrect answers
1.Extreme distress is more typical of somatic symptom disorder, where patients are highly preoccupied with their symptoms.
3.Labile mood is associated with affective disorders, not a defining feature of conversion disorder.
4.Multiple complaints suggest somatic symptom disorder, not conversion disorder which typically presents with one dramatic neurological symptom.
Take Home Points
- Conversion disorder features neurological symptoms without medical explanation and often includes la belle indifférence.
- Indifference to symptoms helps differentiate conversion disorder from other somatic-related disorders.
- Somatic symptom disorder involves multiple complaints and high emotional distress about symptoms.
- Accurate assessment of symptom presentation and emotional response is key to differential diagnosis.
Paroxetine (Paxil) has been prescribed for a client with a somatic symptom illness. The nurse instructs the client to watch out for which of the following side effects?
Explanation
Paroxetineis a selective serotonin reuptake inhibitor (SSRI) commonly prescribed for depression, anxiety, and somatic symptom disorders. It works by increasing serotonin levels in the central nervous system, which helps regulate mood and perception of pain. Among its most frequent side effects are nausea, sexual dysfunction, insomnia, and dry mouth. It may also cause withdrawal symptoms if discontinued abruptly and should be used cautiously in patients with hepatic impairment or those taking other serotonergic agents.
Rationale for correct answers
4.Nausea is a well-documented and commonside effect of SSRIs like paroxetine due to increased serotoninactivity in the gastrointestinal tract.
Rationale for incorrect answers
1.Constipation is a less frequentside effect and not among the most commonly reported with paroxetine use.
2.Increased appetite may occur but is not a primaryconcern with paroxetine; weight gain is more variable and dose-dependent.
3.Flatulence is not a notableside effect of paroxetine and is rarely reported in clinical practice or literature.
Take Home Points
- Paroxetine is an SSRI used for mood and somatic symptom disorders, with nausea as a common side effect.
- Gastrointestinal symptoms are frequent due to serotonin’s role in gut motility and sensitivity.
- Always monitor for withdrawal symptoms and serotonin syndrome when adjusting or combining serotonergic medications.
- Educate patients on gradual dose changes and the importance of adherence to minimize adverse effects.
Practice Exercise 3
Which of the following is true about clients with illness anxiety disorder?
Explanation
Illness anxiety disorderis a psychiatric condition marked by excessive preoccupation, fear, and hypervigilanceabout having or acquiring a serious illness. Individuals often misinterpret normal bodily sensations—such as belching, sweating, or mild discomfort—as signs of severe disease. Despite minimal or absent somatic symptoms, their anxiety persists for at least six months and leads to significant distress or impairment. The disorder may present as care-seeking or care-avoidant behavior, and reassurance rarely alleviates their concern.
Rationale for correct answers
1.Clients with illness anxiety disorder often misinterpret normal sensationsas pathological, driven by persistent health-related anxietyand catastrophic thinking.
Rationale for incorrect answers
2.Fabrication of symptoms is typical of factitiousdisorder or malingering, not illness anxiety disorder, which involves genuine fear without intentional deception.
3.Clients with illness anxiety disorder show distress, not indifference; their anxiety is centered on the possibility of serious illness.
4.Not all listed statements are true; only the misinterpretation of normal sensations aligns with the diagnostic criteria for illness anxiety disorder.
Take Home Points
- Illness anxiety disorder involves misinterpretation of normal bodily sensations as signs of serious illness.
- It differs from factitious disorder and malingering, which involve intentional symptom fabrication.
- Clients often experience significant distress and impairment despite minimal physical symptoms.
- Reassurance is typically ineffective; cognitive behavioral strategies are preferred for management.
Which of the following statements would indicate that teaching about somatic symptom disorder has been effective?
Explanation
Somatic symptom disorderinvolves persistent physical symptoms that are distressing and often medically unexplained. These symptoms are accompanied by excessive thoughts, emotional distress, and behavioral responses. The disorder reflects maladaptive coping with psychological stress, and education focuses on helping clients understand the mind-body connection and develop healthier coping strategies. Effective teaching should lead to insight into how stress influences physical symptoms and promote functional improvement.
Rationale for correct answers
3.This statement reflects understanding that stress managementcan reduce symptom intensity, indicating insight into the psychological componentof the disorder.
Rationale for incorrect answers
1.Believing the doctor thinks symptoms are fake reflects misunderstandingand perpetuates stigma, not therapeutic insight.
2.Trying harder to control symptoms implies volitional control, which is inaccurate and reinforces guilt and frustration.
4.Hopelessness about improvement reflects cognitive distortion, not effective learning or engagement with treatment strategies.
Take Home Points
- Effective teaching about somatic symptom disorder emphasizes the role of stress and emotional regulation in symptom management.
- Insight into the psychological basis of symptoms supports therapeutic progress.
- Misbeliefs about faking or control hinder recovery and must be addressed.
- Education should promote adaptive coping and reduce symptom preoccupation.
The client’s family asks the nurse, “What is illness anxiety disorder?” The best response by the nurse is, “Illness anxiety disorder is:
Explanation
Illness anxiety disorderis defined by persistent preoccupation, fear, and misinterpretationof bodily sensations as signs of serious illness. The condition persists for at least six months and causes significant distress or impairment. Unlike somatic symptom disorder, physical symptoms are minimal or absent. Clients may frequently seek medical reassurance or avoid care altogether due to fear of diagnosis. The disorder is rooted in cognitive distortions and anxiety sensitivity, and management includes psychoeducation and behavioral therapy.
Rationale for correct answers
1.This definition accurately captures the persistent preoccupationand fear of illness central to the disorder, aligning with DSM-5 criteria and clinical presentation.
Rationale for incorrect answers
2.Illness anxiety disorder is not defined by unexplained illness, but by fear of illness despite minimal symptoms.
3.Chronicity and variety of symptoms describe somatic symptom disorder, not illness anxiety disorder.
4.Excessive worry does not causeillness anxiety disorder; it is a symptom, not the outcome.
Take Home Points
- Illness anxiety disorder involves persistent fear of serious illness despite minimal or no physical symptoms.
- It differs from somatic symptom disorder, which includes multiple distressing physical complaints.
- Accurate education helps families understand the psychological nature of the disorder.
- Management includes cognitive behavioral therapy and supportive clinician relationships.
A client with somatic symptom disorder has been attending group therapy. Which of the following statements indicates that therapy is having a positive outcome for this client?
Explanation
Somatic symptom disorderinvolves persistent physical symptoms that are distressing and often medically unexplained. These symptoms are accompanied by emotional distress, maladaptive coping, and preoccupationwith bodily concerns. Group therapy aims to reduce symptom focus, improve emotional insight, and foster interpersonal support. A positive therapeutic outcome is reflected when clients begin to associate emotional expression and interpersonal connection with physical relief, indicating progress in emotional processing.
Rationale for correct answers
1.Feeling physically better after talking reflects emotional releaseand growing awareness of the mind-bodyconnection, a key therapeutic goal in somatic symptom disorder.
Rationale for incorrect answers
2.Passive listening may offer some benefit, but lack of engagementlimits emotional processing and therapeutic growth.
3.Minimizing one’s own symptoms reflects suppression, not insight; it may hinder emotional validation and self-awareness.
4.Labeling others as having emotional problems shows externalization, which deflects personal insight and perpetuates denial.
Take Home Points
- Positive outcomes in group therapy include emotional insight and reduced symptom preoccupation.
- Verbal expression of feelings can alleviate physical distress in somatic symptom disorder.
- Passive participation limits therapeutic benefit; active engagement is encouraged.
- Externalizing or minimizing symptoms reflects poor insight and impedes progress.
When planning care for a client with somatic symptom disorder, the nurse would include the following interventions: Select all that apply.
Explanation
Somatic symptom disorderis characterized by excessive focus on physical symptoms and associated emotional distress. Effective nursing care involves promoting functionality, emotional insight, and validationwithout reinforcing symptom preoccupation. Interventions should encourage routine, help clients connect symptoms to stressors, and validate their experience to build trust and therapeutic alliance.
Rationale for correct answers
2.Encouraging daily activities promotes function, reduces symptom focus, and supports behavioral activation, which improves mood and coping.
3.Helping the client link symptoms to stress fosters insightand supports cognitive restructuring, a core component of therapeutic progress.
6.Validation of distress builds rapportand therapeutic trust, essential for engagement and emotional regulation.
Rationale for incorrect answers
1.Confronting test results may provoke defensivenessand worsen anxiety, undermining therapeutic goals.
4.Providing extra attention during symptom discussion reinforces somatic focus, which perpetuates maladaptive coping.
5.Refusing to listen invalidates the client’s experience, damages rapport, and increases emotional distress.
Take Home Points
- Nursing care for somatic symptom disorder should promote function, insight, and emotional validation.
- Avoid reinforcing symptom preoccupation through excessive attention or confrontation.
- Encourage routine and structured activities to reduce distress and improve coping.
- Therapeutic communication must balance empathy with boundaries to support recovery.
Comprehensive Questions
The nurse understands that secondary gain for the client with a somatic symptom illness can include: Select all that apply.
Explanation
Secondary gainrefers to the indirect benefits a person receives from being ill, which may unconsciously reinforce the persistence of symptoms. In somatic symptom disorder, these gains can include attention, avoidance, and relieffrom responsibilities or emotional distress. While the symptoms are not intentionally produced, the reinforcement from these gains can perpetuate the illness behavior and complicate recovery.
Rationale for correct answers
1.Acceptable absence from work provides avoidanceof stressors and responsibilities, reinforcing the sick role and reducing external pressure.
2.Freedom from chores offers relieffrom daily demands, which may unconsciously reinforce symptom persistence.
3.Increased attention from family satisfies emotional needs, reinforcing the behavior through interpersonal validation.
4.Provision of care by others enhances dependency, which may be comforting and reduce anxiety, reinforcing illness behavior.
6.Temporary relief of anxiety occurs when physical symptoms distract from emotional conflict, serving as an unconscious coping mechanism.
Rationale for incorrect answers
5.Resolution of family conflict is not a typical secondary gain; it implies problem-solving, not reinforcement of illness behavior.
Take Home Points
- Secondary gain in somatic symptom disorder includes avoidance of stressors and increased interpersonal attention.
- These gains are unconscious and can perpetuate symptom expression.
- Nurses must recognize secondary gain to guide therapeutic interventions.
- Addressing emotional needs and promoting adaptive coping reduces reliance on illness behavior.
The information that is least relevant when assessing a patient with a suspected somatization disorder is:
Explanation
Somatization disorderinvolves multiple physical complaints that lack a clear medical cause and are linked to psychological distress, coping deficits, and functional impairment. Assessment focuses on understanding the patient’s emotional state, coping mechanisms, and impact on daily life. While safety is always a priority, violence riskis not typically associated with somatization unless comorbid conditions exist.
Rationale for correct answers
4.Potential for violence is not a core concern in somatization disorder unless there are comorbid psychiatricconditions; it is least relevantin standard assessment.
Rationale for incorrect answers
1.Understanding coping mechanisms is essential to identify maladaptive strategiesand guide therapeutic interventions.
2.Diagnostic workups help rule out organic causes, supporting accurate diagnosis and avoiding unnecessary medical procedures.
3.Limitations in daily living reflect the functional impactof symptoms and guide care planning and outcome evaluation.
Take Home Points
- Violence risk is not a primary concern in somatization disorder unless other psychiatric risks are present.
- Assessment should focus on coping, functional limitations, and diagnostic clarity.
- Understanding the psychological basis of symptoms is essential for effective care.
- Functional impairment guides nursing interventions and outcome planning.
A suitable outcome criterion for the nursing diagnosis Ineffective coping related to dependence on pain relievers to treat chronic pain of psychological origin is:
Explanation
Ineffective copingrelated to psychological pain and medication dependence reflects poor emotional regulation and reliance on external reliefrather than internal strategies. Nursing goals should focus on developing adaptive coping, reducing reliance on pharmacologic interventions, and improving emotional resilience. Behavioral and cognitive strategies are central to long-term improvement.
Rationale for correct answers
2.Learning and practicing coping skills directly addresses the core issueof ineffective coping and supports functional recoverywithout medication dependence.
Rationale for incorrect answers
1.Participation in self-care is important but does not specifically target copingor medication reliance.
3.Improved self-esteem is beneficial but does not directly address coping mechanismsor pain management.
4.Replacing manipulative behaviors may reflect progress but lacks specificity in addressing copingand psychological pain.
Take Home Points
- Effective coping skills are the cornerstone of managing psychological pain without medication dependence.
- Outcome criteria must directly address the nursing diagnosis to guide measurable progress.
- Self-esteem and behavior change are secondary outcomes, not primary goals in this context.
- Nursing care should promote emotional regulation and reduce reliance on pharmacologic relief.
You are caring for Aaron, a 38-year-old patient diagnosed with somatic symptom disorder. When interacting with you, Aaron continues to focus on his severe headaches. In planning care for Aaron, which of the following interventions would be appropriate?
Explanation
Somatic symptom disorderinvolves persistent physical complaints that are distressing and often medically unexplained. These symptoms are accompanied by emotional dysregulation, maladaptive coping, and preoccupationwith bodily sensations. Nursing care should redirect focus from symptoms to emotional processing and coping strategies. Therapeutic communication must validate the experience while guiding the patient toward insight and behavioral change.
Rationale for correct answers
4.Shifting focus to feelings and coping promotes emotional insightand reduces symptom fixation, supporting therapeutic goals and functional recovery.
Rationale for incorrect answers
1.Confrontation in a family meeting may provoke defensiveness, damage trust, and worsen emotional distress.
2.Educating on alternative therapies is helpful but does not address emotional processing, which is central to care planning.
3.Denying the reality of symptoms undermines validation, increasing resistance and emotional withdrawal.
Take Home Points
- Redirecting focus from symptoms to emotional coping is essential in somatic symptom disorder.
- Confrontation and invalidation hinder therapeutic rapport and worsen distress.
- Education alone is insufficient without emotional engagement and behavioral strategies.
- Nursing care must balance empathy with structured redirection to promote recovery.
Which statement describes the etiology of somatization disorder from a learning theory perspective?
Explanation
Learning theoryexplains somatization disorder as a behavior shaped by reinforcement, conditioning, and modeling. When physical symptoms receive attention, care, or relief from responsibilities, they are unintentionally reinforced. This positive reinforcementincreases the likelihood of symptom persistence. The behavior is not consciously produced but maintained through environmental responses that reward illness behavior.
Rationale for correct answers
2.Reinforcement of symptoms through attention or relief from duties supports the learning theoryview that behavior is shaped by external rewards.
Rationale for incorrect answers
1.Genetic predisposition reflects a biologicalmodel, not learning theory.
3.Viewing oneself as “bad” aligns with psychodynamictheory, involving unconscious guilt and atonement.
4.Repression of anxiety is a psychodynamicexplanation, not based on behavioral reinforcement.
Take Home Points
- Learning theory attributes somatization to reinforcement of illness behaviors.
- Attention and relief from responsibilities can unintentionally perpetuate symptoms.
- Differentiating behavioral from psychodynamic and biological models is essential for targeted intervention.
- Nursing care must reduce reinforcement and promote adaptive coping strategies.
A client diagnosed with somatization disorder visits multiple physicians because of various, vague symptoms involving many body systems. Which nursing diagnosis takes priority?
Explanation
Somatization disorderinvolves chronic, medically unexplained symptoms across multiple body systems. These symptoms are accompanied by health-seeking behavior, emotional distress, and frequent visits to multiple providers. The risk of harm increases when patients undergo unnecessary procedures, duplicate treatments, or conflicting medical advice. The priority is to prevent injuryfrom excessive or inappropriate interventions while addressing psychological needs.
Rationale for correct answers
1.Multiple consultations and treatments increase the risk of iatrogenic harm, making injury prevention the primary concernin care planning.
Rationale for incorrect answers
2.Anxiety is present but secondary to the physical risksposed by fragmented care and excessive medical interventions.
3.Ineffective coping is relevant but does not pose an immediate safetythreat, making it a lower priority.
4.Fear is part of the emotional profile but does not carry the same clinical urgencyas injury risk.
Take Home Points
- Risk for injury is the top priority in somatization disorder when multiple providers are involved.
- Fragmented care increases the likelihood of unnecessary or harmful interventions.
- Psychological diagnoses must be balanced with physical safety concerns.
- Coordinated care and provider communication are essential to reduce harm.
The nurse is teaching a client diagnosed with somatization disorder ways to assist in recognizing links between anxiety and somatic symptoms. Which client statement would indicate that the intervention was effective?
Explanation
Somatization disorderreflects the conversion of emotional distress into physical symptoms, often without conscious awareness. Therapeutic interventions aim to build insight, emotional awareness, and self-monitoring. Journaling is a cognitive-behavioral tool that helps clients identify patterns between stress and physical complaints, promoting emotional regulation and reducing symptom intensity.
Rationale for correct answers
4.Journaling supports self-awarenessand helps the client recognize the connectionbetween anxiety and physical symptoms, indicating therapeutic progress.
Rationale for incorrect answers
1.Rating anxiety is useful but does not reflect insightinto how it affects physical symptoms.
2.Requesting family involvement may reflect externalization, not internal understanding of symptom triggers.
3.Interest in assertiveness training is positive but does not directly demonstrate link recognitionbetween anxiety and somatic symptoms.
Take Home Points
- Journaling fosters insight into emotional triggers and physical symptom patterns.
- Recognition of mind-body connections is a key therapeutic goal in somatization disorder.
- Self-monitoring tools enhance emotional regulation and reduce symptom preoccupation.
- External solutions are helpful but must be paired with internal awareness for lasting change.
Which intervention is a nurse’s priority when working with a client suspected of having a conversion disorder?
Explanation
Conversion disorderpresents with neurological symptoms such as paralysis, seizures, or sensory lossthat lack a medical basis. Before confirming the diagnosis, it is essential to rule out organic pathologyto avoid misdiagnosis and ensure appropriate care. This step protects patient safety and guides further psychiatric evaluation and treatment.
Rationale for correct answers
4.Ruling out organic causes ensures diagnostic accuracyand prevents mismanagement, making it the first priority in suspected conversion disorder.
Rationale for incorrect answers
1.Avoiding secondary gain is important but not the initial clinical priorityduring assessment.
2.Confrontation may provoke defensivenessand worsen symptoms; it is not therapeutic or diagnostic.
3.Teaching coping skills is valuable but follows confirmationof diagnosis and safety clearance.
Take Home Points
- Ruling out organic pathology is the first step in managing suspected conversion disorder.
- Accurate diagnosis prevents inappropriate treatment and supports safe psychiatric care.
- Confrontation is contraindicated; supportive and nonjudgmental approaches are preferred.
- Coping strategies are introduced after diagnostic clarity and patient engagement.
A client is suspected to be experiencing a conversion disorder. Which of the following would the nurse expect to assess? Select all that apply.
Explanation
Conversion disorderis a psychiatric condition where psychological stress manifests as neurological symptoms without an organic cause. It often presents with motor deficits, sensory changes, or seizure-like activity, and symptoms are not intentionally produced. Clients may show indifference to symptoms and lack insight into their psychological origin.
Rationale for correct answers
1.Deep tendon reflexes remain intactbecause conversion disorder does not involve actual damage to the neuromuscular system. Reflex arcs are preserved despite motor symptoms.
3.Clients are typically unawareof the psychological origin of their symptoms. The dissociation between emotional conflict and physical manifestation is unconscious.
5.A lack of concern, termed la belle indifférence, is common. Clients may appear oddly calm or indifferent about significant functional impairments.
Rationale for incorrect answers
2.Wasting does not occur because the paralysis is psychogenic, not due to disuse or neuromuscular pathology. Muscle bulk remains preserved.
4.Physiological causes are ruled out in conversion disorder. Symptoms are not explained by any identifiable medical or neurological condition.
Take Home Points
- Conversion disorder presents with neurological symptoms that lack a medical explanation and are linked to psychological stress.
- Clients often lack insight and may show indifference to their symptoms.
- Neurological examination typically reveals intact reflexes and preserved muscle tone.
- It must be differentiated from malingering, factitious disorder, and true neurological conditions.
A client fearful of an upcoming deployment to Iraq develops a paralytic conversion disorder. Which nursing diagnosis takes priority?
Explanation
Conversion disordercan be triggered by acute psychological stress, such as fear of combat. The priority nursing diagnosis addresses the underlying anxiety, which precipitates the physical symptoms. Addressing emotional distress is essential for symptom resolution.
Rationale for correct answer
3.The client’s anxietyabout deployment is the psychological stressor that led to the conversion symptoms. Addressing this root cause is essential for recovery.
Rationale for incorrect answers
1.Integrity is not compromised in conversion disorder. Paralysis is functional, not due to tissue breakdown or immobility-related damage.
2.Image disturbance may occur, but it is not the priority. Emotional distress precedes and drives the physical symptoms.
4.Intolerance is a physical limitation, but it stems from psychological origin. Addressing anxiety takes precedence over managing mobility.
Take Home Points
- Psychological stressors are the primary cause of conversion disorder symptoms.
- Anxiety-related diagnoses take priority over physical manifestations.
- Functional paralysis does not result in tissue damage or muscle wasting.
- Emotional support and stress management are central to nursing care.
A client diagnosed with a conversion disorder has a nursing diagnosis of disturbed sensory perception related to anxiety as evidenced by paralysis. Which short-term outcome would be appropriate for this client?
Explanation
Conversion disorderinvolves unconscious expression of psychological conflict through physical symptoms. Acknowledging anxietyis a critical therapeutic milestone, indicating insight and readiness for recovery. Short-term goals should focus on emotional awareness and coping.
Rationale for correct answer
4.Recognition of underlyinganxiety by day 4 reflects progress in insight and emotional processing, which is essential for symptom resolution.
Rationale for incorrect answers
1.Recovery of function may occur, but it is not a short-term goal. Emotional insight precedes physical improvement.
2.Coping mechanisms are important, but using one by day 3 is premature without acknowledging the psychological origin.
3.Fear expression is valid, but it does not address the core issue of unconscious anxiety driving the symptoms.
Take Home Points
- Emotional insight is key to managing conversion disorder.
- Short-term goals should focus on psychological awareness, not physical recovery.
- Functional symptoms resolve as emotional conflicts are addressed.
- Therapy should prioritize helping clients connect emotions to physical symptoms.
An anxious client reports experiencing pain in the abdomen and feeling empty and hollow. A diagnostic workup reveals no physical causes of these clinical findings. What term best reflects what the client is experiencing?
Explanation
Somatizationrefers to the unconscious expression of psychological distress through physical symptoms that lack a medical explanation. It involves pain, gastrointestinal symptoms, and neurological complaintsthat are not intentionally produced. These symptoms are real and often cause significant impairment, but they arise from emotional conflict rather than organic pathology.
Rationale for correct answers
2.The client’s abdominal pain and hollow sensation without physical findings reflect somatization, where emotional distress manifests as physical symptoms. This is a subconscious process.
Rationale for incorrect answers
1.Dissociationinvolves a disruption in consciousness, memory, or identity, not physical pain or somatic complaints.
3.Response to stressmay include physiological changes, but it does not typically present as persistent unexplained pain.
4.Reaction to anxietymay cause transient symptoms like palpitations or sweating, but not chronic somatic pain without cause.
Take Home Points
- Somatization involves physical symptoms without medical cause, driven by psychological distress.
- It must be differentiated from malingering and factitious disorder, which involve conscious symptom production.
- Clients are not faking symptoms; they experience real distress and impairment.
- Treatment focuses on emotional insight and coping strategies, not symptom suppression.
A nurse considers that in a conversion disorder pseudoneurologic symptoms such as paralysis or blindness:
Explanation
Conversion disorderpresents with pseudoneurologic symptoms such as paralysis or blindness that are not explained by medical conditions. These symptoms are unconscious, functional, and often emerge inresponse to psychological stress. They serve as a coping mechanism for internal conflict and are not under voluntary control.
Rationale for correct answers
3.Symptoms are necessaryfor psychological adaptation. They allow the client to unconsciously avoid confronting distressing emotions or situations.
Rationale for incorrect answers
1.Attention seeking implies conscious symptom production, which is not the case in conversion disorder.
2.Healthy focus may aid recovery, but symptoms do not resolve solely through behavioral redirection.
4.Conflicts may contribute, but resolution of family issues alone does not guarantee symptom disappearance.
Take Home Points
- Conversion symptoms are unconscious and serve a psychological function.
- They are not intentionally produced and differ from malingering or factitious disorder.
- Emotional stressors often precede symptom onset.
- Treatment involves psychotherapy and stress management, not confrontation.
A client newly diagnosed with a conversion disorder is manifesting paralysis of a leg. The nurse can expect this client to:
Explanation
Conversion disordersymptoms such as paralysis often resolve spontaneously but may recur under stress. The disorder is episodic, stress-sensitive, and typically involves motor or sensory deficits. Clients may regain function but are vulnerable to relapse during emotional distress.
Rationale for correct answers
3.Symptom recurrenceunder stress is characteristic. The brain converts emotional conflict into physical symptoms, which may reappear with future stressors.
Rationale for incorrect answers
1.Spread of paralysis is not typical. Symptoms usually remain localized and consistent with the initial presentation.
2.Continuous psychiatric care is not always required. Many clients recover with short-term therapy and support.
4.Emotional course may vary, but symptom recurrence is more predictable than general emotional instability.
Take Home Points
- Conversion disorder symptoms may resolve but recur with stress.
- Motor and sensory deficits are functional, not due to organic pathology.
- Long-term psychiatric care is not always necessary.
- Relapse prevention focuses on stress management and emotional insight.
A nurse is caring for a client who has a diagnosis of conversion disorder with paralysis of the lower extremities. Which is the most therapeutic nursing intervention?
Explanation
Conversion disorderis a type of functional neurological symptom disorder characterized by motor or sensory deficits that are not explained by medical conditions. Symptoms arise unconsciously in response to psychological stress and often reflect symbolic resolution of internal conflict. Paralysis, blindness, or seizuresmay manifest without organic pathology. Management involves a multidisciplinary approach including psychotherapy and rehabilitation, with emphasis on restoring function while avoiding reinforcement of symptoms.
Rationale for correct answers
4.Physical therapyprovides a structured, goal-directed approach that supports functional recovery without reinforcing the sick role. It promotes independence and helps shift focus from symptoms to capability. Behavioral reinforcement of normal movement patterns is central to recovery.
Rationale for incorrect answers
1.Premature encouragementto walk may provoke anxiety or resistance, especially if the client is not yet psychologically ready. It risks invalidating the client’s experience and may worsen symptoms.
2.Invalidation of symptomsby stating “nothing is wrong” undermines therapeutic rapport. Conversion symptoms are real to the client, and dismissing them can increase distress and resistance to care.
3.Avoidance of symptomdiscussion may hinder therapeutic engagement. While excessive focus is discouraged, acknowledging symptoms within a supportive framework is essential for trust and progress.
Take Home Points
- Conversion disorder presents with neurological symptoms without organic cause, often linked to psychological stress.
- Physical therapy is a key intervention, using behavioral reinforcement to restore function.
- Therapeutic communication must validate the client’s experience while guiding toward recovery.
- Differentiation from malingering and factitious disorder is essential, as conversion symptoms are unconscious and not intentionally produced.
What characteristic of anxiety is associated with a diagnosis of conversion disorder?
Explanation
Conversion disorderis a subtype of somatic symptom and related disorders where psychological stress is unconsciously transformed into physical symptoms. These symptoms often reflect symbolic resolution of internal conflict and are not intentionally produced. The disorder is marked by motor, sensory, or seizure-likesymptoms that lack a medical explanation. Anxiety is often present but not consciously acknowledged, and the physical symptom serves to reduce psychological distress by shifting focus away from the emotional conflict.
Rationale for correct answers
2.Symptom relief occurs because the physical manifestation symbolically resolves the internal psychological conflict. The anxiety is unconsciously converted, and the symptom provides psychological escape from distress. This defense mechanism reduces conscious awareness of anxiety.
Rationale for incorrect answers
1.Free-floatinganxiety refers to generalized anxiety disorder, where anxiety is persistent and not linked to a specific trigger. In conversion disorder, anxiety is linked to unconscious conflict and not diffusely experienced.
3.Consciously felt anxietycontradicts the nature of conversion disorder, where the anxiety is repressed and not directly experienced. The client is unaware of the psychological origin of the symptom.
4.Projected anxietyinvolves attributing internal feelings to external sources, which is more characteristic of psychotic or personality disorders. Conversion disorder involves internalization and somatization, not projection.
Take Home Points
- Conversion disorder involves unconscious transformation of psychological stress into physical symptoms.
- Anxiety is present but not consciously acknowledged; symptoms serve to relieve internal conflict.
Differentiation from malingering and factitious disorder is essential, as symptoms are not intentionally produced.
Exams on Somatic Symptom and Related Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- By the end of these notes, learners will be able to:
- Define and classify somatic symptom and related disorders according to established psychiatric frameworks.
- Identify key epidemiological data, etiological factors, and pathophysiological mechanisms underlying these disorders.
- Describe the clinical features, diagnostic criteria, and differential diagnoses for each specific disorder.
- Apply nursing assessment techniques and develop evidence-based care plans for patients with these conditions.
- Discuss pharmacological, psychotherapeutic, and multidisciplinary interventions, including the nurse's role in patient education and ethical considerations.
- Evaluate potential complications, prognostic factors, and cultural influences to enhance holistic nursing practice.
Introduction
- Somatic symptom and related disorders represent a category of mental health conditions characterized by physical symptoms that cause significant distress and impairment, often without a clear medical explanation.
- These disorders highlight the intricate interplay between psychological factors and bodily experiences, as recognized in psychiatric classifications.
- In nursing practice, understanding these disorders is crucial because nurses frequently encounter patients who present with somatic complaints in various healthcare settings, such as primary care, emergency departments, and psychiatric units.
- The DSM-5 reorganizes these disorders from earlier editions to emphasize the psychological distress associated with somatic symptoms rather than the absence of medical findings, promoting a more patient-centered approach.
- This shift encourages nurses to validate patients' experiences while addressing both physical and emotional needs.
- Comprehensive nursing care in this area involves thorough assessment, empathetic communication, and collaborative interventions to improve patient outcomes and reduce healthcare utilization.
- These notes will delve into the scientific underpinnings, clinical management, and nursing-specific insights to equip students for effective practice.
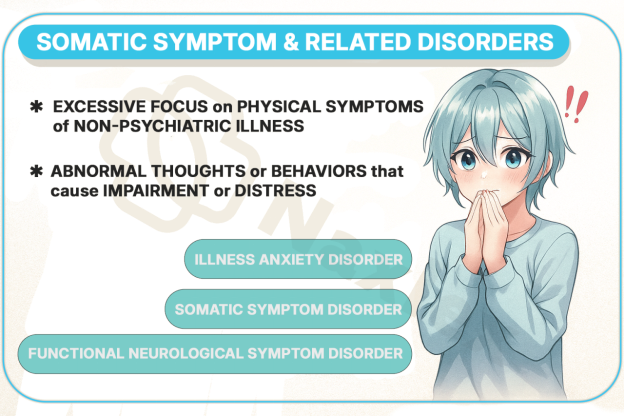
Overview Of Somatic Symptom And Related Disorders
- Somatic symptom and related disorders encompass a group of conditions where individuals experience physical symptoms that are distressing or disruptive to daily life, often accompanied by excessive thoughts, feelings, or behaviors related to these symptoms.
- These disorders are not better explained by another medical condition and persist despite medical reassurance.
- The scientific understanding of these disorders draws from biopsychosocial models, integrating biological vulnerabilities, psychological stressors, and social influences.
1.1 Definition and Classification
- The definition of somatic symptom and related disorders focuses on the presence of one or more somatic symptoms that cannot be fully explained by a general medical condition and are associated with psychosocial distress.
- Classification in the DSM-5 includes several distinct disorders based on the predominant features, such as the focus on symptoms versus fear of illness.
- This classification system aids in precise diagnosis and tailored treatment planning.
- Somatic symptoms are physical complaints like pain, fatigue, or gastrointestinal issues that lead to significant impairment in social, occupational, or other areas of functioning.
- Related disorders involve similar presentations but with specific emphases, such as imposed symptoms in factitious disorder.
- The DSM-5 criteria require that symptoms persist for at least six months for certain disorders, emphasizing chronicity.
1.2 Epidemiology
- Epidemiological studies indicate that somatic symptom and related disorders are prevalent across diverse populations, with higher rates in certain demographics.
- Prevalence estimates vary, but somatic symptom disorder affects approximately 5–7% of the general population, while illness anxiety disorder is seen in 1–5%.
- These disorders are more common in women than men, with a ratio of about 2:1, and onset often occurs in early adulthood.
- Cultural variations exist, with higher reporting in some ethnic groups due to differences in symptom expression and healthcare access.
- Lifetime prevalence for any somatic symptom-related disorder is around 10–15% in primary care settings.
- Risk factors include history of childhood adversity, chronic medical conditions, or psychiatric comorbidities like depression.
- Global data (WHO) suggest higher incidence in low- and middle-income countries, possibly due to limited mental health resources.
1.3 Etiology and Risk Factors
- The etiology of somatic symptom and related disorders is multifactorial, involving genetic, neurobiological, psychological, and environmental contributors.
- Genetic studies show heritability estimates of 30–50%, with polymorphisms in genes related to serotonin and pain perception pathways.
- Psychological factors include cognitive biases toward symptom amplification and learned behaviors from family models.
- Environmental risks encompass chronic stress, trauma, and socioeconomic disadvantages.
- Biological risk factors include dysregulation in the hypothalamic-pituitary-adrenal axis, leading to heightened stress responses and somatic manifestations.
- Psychological risks involve alexithymia, where individuals struggle to identify emotions, resulting in somatic expression of distress.
- Social factors such as stigma around mental health can perpetuate symptom-focused behaviors.
Nursing Insights
- Nurses must recognize that these disorders are not "imagined" but involve real physiological responses amplified by psychological factors; dismissing symptoms can erode trust and worsen outcomes.
- In nursing school exams, remember that these disorders contribute to high healthcare costs, accounting for up to 20% of outpatient visits; nurses should screen for them to prevent unnecessary testing.
- Key for nurses: Early identification of risk factors like a family history of similar disorders can guide preventive education; always assess for comorbid anxiety or depression, as they coexist in 50–70% of cases.
1.4 Pathophysiology
- Pathophysiological mechanisms in somatic symptom and related disorders involve altered neural processing in brain regions like the amygdala and somatosensory cortex, leading to amplified perception of bodily signals.
- Neuroimaging studies reveal hyperactivity in pain-processing networks and reduced connectivity in emotion-regulation areas.
- Inflammatory markers, such as elevated cytokines, may contribute to fatigue and pain symptoms, suggesting an immune-mediated component.
- Central sensitization amplifies nociceptive signals, making normal sensations feel painful.
- Autonomic nervous system dysregulation can manifest as gastrointestinal or cardiovascular symptoms.
- Epigenetic changes from chronic stress may alter gene expression related to symptom persistence.
- Understanding pathophysiology helps nurses explain to patients that symptoms are "real" due to brain-body interactions; this validation is crucial for therapeutic alliance.
Specific Disorders
- This section provides a detailed examination of each disorder within the somatic symptom and related category, drawing on DSM-5 frameworks for diagnostic clarity.
Each disorder has unique features, but all involve disproportionate responses to somatic experiences.
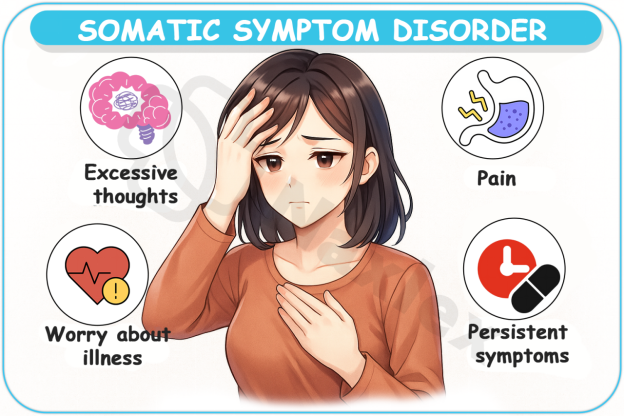
1.1 Somatic Symptom Disorder
- Characterized by one or more somatic symptoms that are distressing and result in significant disruption of daily life, accompanied by excessive thoughts, feelings, or behaviors related to the symptoms.
- Symptoms must persist for more than six months, with focus on the psychological impact rather than the absence of medical explanation.
- Common symptoms include pain in multiple sites, gastrointestinal complaints like nausea or bloating, neurological issues such as dizziness, and fatigue.
- Behavioral manifestations involve persistent health-related anxiety, excessive time spent on symptom management, and repeated medical consultations.
Frequently co-occurs with major depressive disorder or generalized anxiety disorder, complicating management.
Nursing Insights
- Patients may undergo numerous unnecessary procedures; prioritize holistic assessment to avoid iatrogenic harm.
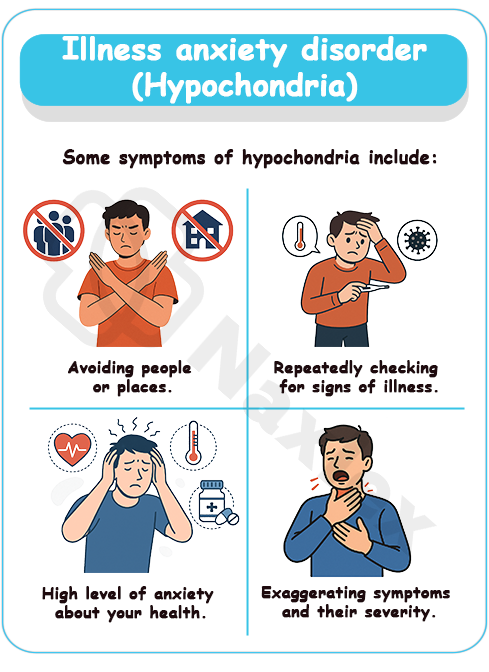
1.2 Illness Anxiety Disorder
- Involves preoccupation with having or acquiring a serious illness, despite minimal or no somatic symptoms.
- Individuals exhibit high health anxiety, leading to either excessive care-seeking or avoidance of medical care.
- Key features include misinterpretation of benign bodily sensations as signs of severe disease (e.g., interpreting a headache as a brain tumor).
- Duration is at least six months, with anxiety not better explained by another mental disorder.
- Variants include:
- Care-seeking type (frequent doctor visits).
- Care-avoidant type (fear prevents seeking help).
Nursing Insights
- For exams, recall that this disorder replaces hypochondriasis in DSM-5; nurses must use reassurance techniques without reinforcing anxiety.
1.3 Conversion Disorder (Functional Neurological Symptom Disorder)
- Presents with neurological symptoms (paralysis, blindness, seizures) that are incompatible with recognized neurological or medical conditions.
- Symptoms are involuntary and often precipitated by stress.
- Clinical signs include sudden onset, inconsistency with anatomical pathways (e.g., glove anesthesia), and resolution with suggestion or hypnosis.
- DSM-5 requires evidence of incompatibility between symptoms and known neurological disorders, without implying intentionality.
- More common in younger adults and in rural or low-socioeconomic populations.
- Nurses should conduct thorough neurological exams but avoid accusing patients of faking; focus on functional rehabilitation.
1.4 Psychological Factors Affecting Other Medical Conditions
- Psychological or behavioral factors adversely affect a verified medical condition (e.g., anxiety worsening asthma, nonadherence worsening diabetes).
- Factors include stress, denial, or poor coping, leading to increased symptom severity or delayed recovery.
- Diagnosis requires a temporal association between psychological factors and medical outcomes.
Differs from other disorders by the presence of a confirmed medical illness.
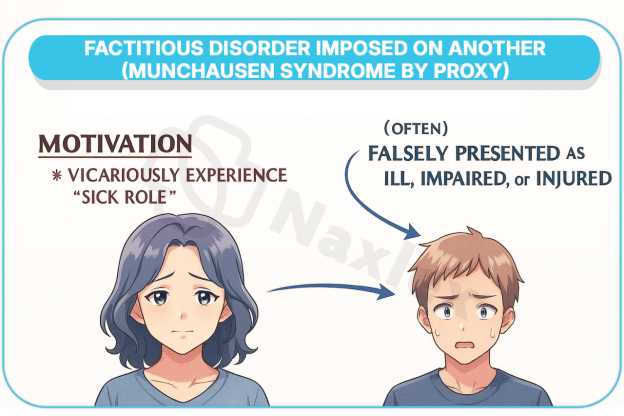
1.5 Factitious Disorder
- Factitious disorder entails falsification of physical or psychological signs/symptoms, or induction of injury/disease, in the absence of obvious external rewards.
- Can be imposed on self or another (formerly Munchausen syndrome by proxy).
- Motivations are often to assume the sick role, gaining attention or care.
- Behaviors include tampering with tests, self-harm, or exaggerating symptoms.
DSM-5 distinguishes between imposed on self vs. imposed on another, with the latter often involving child/elder abuse.
1.6 Other Specified Somatic Symptom and Related Disorder
- Applied when symptoms cause clinically significant distress but do not meet full criteria for other disorders.
- Examples: brief somatic symptom disorder (< 6 months), pseudocyesis (false pregnancy), illness anxiety < 6 months.
- Provides a diagnosis when full criteria are unmet but intervention is still needed.
1.7 Unspecified Somatic Symptom and Related Disorder
- Used when symptoms do not fit specified criteria and clinician chooses not to specify the reason.
- Often used in emergency settings where full evaluation is pending.
- Applicable in cases with insufficient information or mixed features.
Nursing Insights
- Vigilance is essential; nurses must document inconsistencies objectively and involve ethics teams for suspected cases.
- Nurses play a key role in identifying these factors through patient interviews; integrate behavioral interventions to improve medical compliance.
- Use this for atypical presentations; ensures patients receive care without rigid diagnostic barriers.
- In acute care, this label prevents premature closure; nurses should advocate for follow-up evaluations.
Assessment And Diagnosis
- Assessment and diagnosis of somatic symptom and related disorders require a systematic approach integrating history, physical examination, and psychological evaluation.
- Nurses contribute significantly by gathering detailed patient narratives and observing behaviors.
1.1 Clinical Presentation and Symptoms
- Patients typically present with persistent somatic complaints that dominate their lives, often leading to frequent healthcare encounters.
- Symptoms are varied but cause marked distress.
- Physical symptoms may include chronic pain, shortness of breath, or palpitations, often migrating or changing over time.
- Emotional symptoms encompass anxiety about health, frustration with medical providers, or depressive features.
- Behavioral indicators involve doctor-shopping or excessive internet research on illnesses.
1.2 Diagnostic Criteria Based on DSM-5
- Diagnostic criteria emphasize the disruptive nature of symptoms and associated cognitions.
- For somatic symptom disorder, criteria include one or more symptoms, excessive health-related behaviors, and duration over six months.
- Criteria are symptom-focused, requiring evidence of disproportionate concern.
- Exclusion of other disorders ensures accuracy, such as ruling out delirium.
|
Disorder |
Key Criteria |
Duration Requirement |
|
Somatic Symptom Disorder |
One or more somatic symptoms with excessive thoughts/behaviors |
At least 6 months |
|
Illness Anxiety Disorder |
Preoccupation with serious illness; somatic symptoms absent or mild |
At least 6 months |
|
Conversion Disorder |
Neurological symptoms incompatible with medical conditions |
Variable, often acute onset |
|
Factitious Disorder |
Falsification of symptoms without external incentives |
Variable |
Nursing Insights
- Memorize that DSM-5 de-emphasizes “medically unexplained” to reduce stigma; nurses should use person-first language.
- High-yield: Always assess for suicide risk, as chronic distress can lead to hopelessness; use validated scales like the PHQ-15 for somatic symptom burden.
1.3 Differential Diagnosis
- Differential diagnosis involves distinguishing these disorders from medical conditions, other psychiatric disorders, or substance-related issues.
- For example, ruling out multiple sclerosis in conversion disorder requires neuroimaging.
- Common differentials include anxiety disorders, depressive disorders, or somatoform variants from prior classifications.
- Medical mimics like thyroid dysfunction or autoimmune diseases must be excluded through lab tests.
- Cultural syndromes, such as "ataque de nervios," may overlap and require culturally sensitive evaluation.
- Nursing Insights: Nurses should collaborate with physicians for comprehensive workups; avoid over-testing by focusing on history.
Table 1: Differential Diagnosis for Somatic and Related Disorders
|
Disorder |
Key Characteristic |
Presence of Somatic Symptoms |
Patient Intent |
Primary Motivation |
|
Somatic Symptom Disorder (SSD) |
Excessive thoughts, feelings, behaviors in response to symptoms |
Present; distressing |
Unintentional |
None (unconscious) |
|
Illness Anxiety Disorder (IAD) |
Preoccupation with fear of having a serious disease |
Absent or very mild |
Unintentional |
None (unconscious) |
|
Conversion Disorder |
Neurologic symptoms with no medical cause |
Present; distressing |
Unintentional |
None (unconscious) |
|
Factitious Disorder |
Intentional production of symptoms to assume sick role |
May be feigned or produced |
Intentional (conscious) |
Primary gain (sick role) |
|
Malingering |
Intentional production of symptoms for an external benefit |
May be feigned or exaggerated |
Intentional (conscious) |
Secondary gain (e.g., drugs, money, avoiding work) |
1.4 Nursing Assessment Tools and Techniques
- Nursing assessments utilize structured interviews, observation, and standardized tools to quantify symptom severity and functional impact.
- Tools include the Somatic Symptom Scale-8 (SSS-8) for quick screening and the Patient Health Questionnaire (PHQ) for comorbid depression.
- Techniques involve active listening, exploring symptom timelines, and assessing social support.
- Physical exams should be thorough but empathetic, noting any inconsistencies without confrontation.
Treatment And Management
- Management of somatic symptom and related disorders involves multimodal interventions integrating psychotherapy, pharmacotherapy, and nursing care.
- The focus is on improving function and quality of life rather than eliminating symptoms.
1.1 General Principles of Treatment
- Establish a therapeutic alliance with the patient through validation and consistent follow-up.
- Educate patients that symptoms are real but influenced by brain-body interactions.
- Limit unnecessary diagnostic testing and specialist referrals to prevent iatrogenic harm.
- Integrate care among primary providers, psychiatrists, and nursing staff.
- Emphasize functional improvement rather than complete symptom resolution.
- Nursing Insights: For exams, remember the phrase: "Structure, Support, Symptom Management" — the three pillars of effective treatment.
1.2 Psychotherapy
- Psychotherapy is the cornerstone of treatment, particularly cognitive-behavioral therapy (CBT).
- CBT targets maladaptive thought patterns, reduces health anxiety, and encourages adaptive coping strategies.
- Mindfulness-based therapies reduce symptom catastrophizing and improve pain tolerance.
- Psychodynamic therapy may help explore unconscious conflicts manifesting as somatic symptoms.
- Group therapy offers social support and normalizes experiences.
- Nursing Insights: High-yield: CBT is first-line therapy in most somatic disorders; nurses should reinforce therapy goals in everyday interactions.
1.3 Pharmacotherapy
- Pharmacological options address comorbid conditions like depression or anxiety rather than somatic symptoms directly.
- SSRIs (e.g., fluoxetine, sertraline) reduce somatic distress and improve mood.
- SNRIs (e.g., duloxetine) are useful for patients with significant pain.
- Tricyclic antidepressants (e.g., amitriptyline) may reduce pain but have more side effects.
- Benzodiazepines are discouraged due to dependency risks.
- Nurses should monitor for adherence and adverse effects; emphasize that medications manage emotional distress, not “cure” somatic symptoms.
1.4 Role of Nursing Interventions
- Nurses play a pivotal role by providing consistent, empathetic care and serving as patient advocates.
- Interventions include:
- Regular scheduled visits to reduce emergency care-seeking.
- Patient education about stress-symptom connections.
- Encouraging journaling to track symptom triggers.
- Facilitating referral to psychotherapy.
- Nurses also coordinate with families to reduce reinforcement of illness behaviors.
- Nursing Insights: Nursing exam tip: Always validate patient experiences before introducing psychosocial explanations; this prevents perceived dismissal.
1.5 Multidisciplinary Care Approaches
- Optimal outcomes are achieved through collaboration among primary care, psychiatry, nursing, and allied health.
- Physical therapy supports mobility in conversion disorder.
- Occupational therapy enhances functional independence.
- Social workers address psychosocial stressors and connect patients with community resources.
- Regular team meetings ensure consistent communication and prevent fragmented care.
- Nursing Insights: Key exam point: Multidisciplinary care prevents “doctor shopping” by providing coordinated treatment plans.
Complications And Prognosis
- Prognosis of somatic symptom and related disorders varies depending on disorder type, severity, and treatment adherence.
- Chronic forms often persist for years, while acute conversion disorder may resolve spontaneously.
- Early intervention with psychotherapy improves long-term outcomes.
- Comorbid psychiatric conditions (e.g., depression, anxiety) worsen prognosis.
- Social support and a strong therapeutic alliance are protective factors.
Nursing Insights
- Nurses should emphasize realistic recovery goals — improving daily functioning and coping rather than eliminating all symptoms.
1.1 Factors Influencing Prognosis
- Positive factors: early diagnosis, patient engagement in therapy, family support.
- Negative factors: chronicity, high healthcare utilization, comorbid psychiatric or personality disorders.
- Socioeconomic stressors can exacerbate illness perception and persistence.
1.2 Long-Term Outcomes
- Some patients achieve partial remission with reduced symptom severity.
- Others remain impaired with fluctuating symptoms over time.
- Suicide risk is elevated in severe, chronic cases.
- Functional disability, work absenteeism, and strained relationships are common.
Summary
- Somatic symptom and related disorders represent a group of conditions where psychological distress manifests as physical symptoms.
- They are prevalent, disabling, and often misunderstood.
- Diagnosis requires a biopsychosocial approach and exclusion of medical mimics.
- Treatment is multidisciplinary, emphasizing psychotherapy, symptom management, and coordinated care.
- Nurses have a central role in assessment, education, and therapeutic engagement.
- Prognosis depends on timely intervention, patient engagement, and social context.
- Key takeaway for exams: Focus on patient-centered care, validation, and integration of psychological and medical approaches.
- Nurses should routinely assess quality of life domains (work, family, daily activities) to evaluate true outcomes beyond symptom reports.
- In exams, link prognosis to “modifiable” vs. “non-modifiable” factors (e.g., family support = modifiable; chronicity = non-modifiable).
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Somatic Symptom and Related Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


