Please set your exam date
Depressive Disorders
Study Questions
Practice Exercise 1
A nurse is assessing a client with suspected major depression. Which findings would support a diagnosis of major depression? Select all that apply.
Explanation
Major depressive disorder is a psychiatric condition characterized by persistent low mood and loss of interest, accompanied by cognitive and somatic symptoms. It must last at least two weeks and cause functional impairment.
Rationale for correct answers
1. Loss of interest or pleasure is one of the two cardinal symptoms required for diagnosis. This reflects anhedonia, a core feature of depression, and must occur nearly daily for at least two weeks.
2. Psychomotor agitation is a recognized symptom when observable by others. It reflects neurovegetative changes and is part of the DSM-5 criteria when present nearly daily for two weeks.
3. Feelings of worthlessness are common in major depression and contribute to cognitive distortion. These must be persistent and not limited to transient guilt or self-reproach.
4. Depressed mood nearly every day is the other cardinal symptom required for diagnosis. It may be reported subjectively or observed by others and reflects affective disturbance.
6. Impaired concentration is a cognitive symptom of depression. It affects decision-making and attention, and when persistent, it supports the diagnosis due to executive dysfunction.
Rationale for incorrect answer
5. Pressured speech is typically associated with mania, not depression. It reflects increased psychomotor activity and flight of ideas, which are inconsistent with the slowed cognition seen in major depression.
Take Home Points
- Major depressive disorder requires five or more symptoms, including either depressed mood or anhedonia, lasting at least two weeks.
- Cognitive symptoms like impaired concentration and worthlessness are diagnostic when persistent and functionally impairing.
- Psychomotor agitation must be observable and not merely subjective restlessness.
- Pressured speech is a hallmark of manic episodes and should prompt evaluation for bipolar disorder.
A client is hospitalized because of severe depression. The client refuses to eat, stays in bed most of the time, does not talk with family members, and will not leave the room. The nurse attempts to initiate a conversation by asking questions but receives no answers. Finally, the nurse tells the client that if there is no response, the nurse will leave and the client will remain alone. How should the nurse’s behavior be interpreted?
Explanation
Severe depression is a debilitating mood disorder marked by pervasive sadness, psychomotor retardation, and impaired social and functional engagement. Clients often exhibit withdrawal, poor appetite, and anhedonia, with minimal verbal interaction. They may resist care, remain passive, and require structured behavioral interventions. Therapeutic strategies often include behavioral activation, reinforcement, and empathetic persistence. In acute phases, patients may not respond to verbal prompts, necessitating non-threatening, consistent approaches that preserve dignity while encouraging engagement.
Rationale for correct answer
1. The nurse’s statement reflects a behavioral strategy using consequences to shape engagement. Withholding interaction unless the client responds introduces a mild negative reinforcement to motivate participation. This aligns with operant conditioning principles often used in psychiatric care to encourage adaptive behaviors.
Rationale for incorrect answers
2. The nurse’s action is not about self-reflection but a deliberate attempt to elicit a response. The timing and context suggest a behavioral intervention rather than a pause for strategy development.
3. The client’s refusal to engage is not a request for solitude but a symptom of psychomotor retardation and social withdrawal. Respecting this behavior without intervention may reinforce isolation and worsen depressive symptoms.
4. The nurse’s statement lacks intentional harm or physical threat, which are required elements of assault. It is a therapeutic prompt, not a coercive or violent act.
Take Home Points
- Severe depression often presents with psychomotor retardation, withdrawal, and refusal to engage.
- Behavioral strategies like reinforcement can be effective in motivating depressed clients.
- Therapeutic communication must balance empathy with structured prompts to encourage interaction.
- Depression-related withdrawal should not be mistaken for voluntary solitude or autonomy.
Which symptom is an example of physiological alterations exhibited by clients diagnosed with moderate depression?
Explanation
Moderate depression is a clinical condition characterized by persistent low mood, anhedonia, and functional impairment across cognitive, emotional, and physiological domains. It involves neurovegetative symptoms, altered neurotransmitter activity, and dysregulation of the hypothalamic-pituitary-adrenal axis. These changes affect sleep, appetite, sexual function, and energy levels. Physiological symptoms are often underrecognized but are critical for diagnosis and treatment planning.
Moderate depression involves changes in serotonin and norepinephrine that impair autonomic regulation, leading to reduced libido, appetite changes, and sleep disturbances. These symptoms reflect dysfunction in basic physiological needs and are distinct from cognitive or affective features. The presence of such symptoms indicates deeper neurobiological involvement and often correlates with poorer treatment response if not addressed.
Rationale for correct answer
1. Decreased libido reflects a direct physiological alteration due to reduced hypothalamic stimulation and impaired serotonergic and dopaminergic signaling. It is a classic neurovegetative symptom seen in moderate depression and aligns with Maslow’s physiological domain.
Rationale for incorrect answers
2. Concentrating difficulty is a cognitive symptom, not physiological. It results from impaired prefrontal cortex function and reduced executive processing, typical in depression but not classified under physiological changes.
3. Posture changes like slumping are behavioral and psychomotor manifestations. They reflect affective withdrawal and low energy but are not physiological in nature. They do not involve autonomic or endocrine systems.
4. Helplessness is an emotional and cognitive distortion rooted in negative self-appraisal and learned hopelessness. It is a psychological symptom, not a physiological one, and does not involve bodily system dysfunction.
Take Home Points
- Physiological symptoms in depression include libido changes, appetite disturbances, and sleep dysregulation.
- Cognitive and emotional symptoms, while prominent, are distinct from physiological alterations.
- Neurovegetative signs indicate deeper biological involvement and may require targeted pharmacologic intervention.
- Differentiating physiological from cognitive and affective symptoms is essential for accurate diagnosis and treatment planning.
A nurse is teaching a class to assistive personnel on depression. Which statement(s) by the nurse provide accurate information about depression? Select all that apply.
Explanation
Depression is a mood disorder characterized by persistent sadness, loss of interest, and cognitive, emotional, and behavioral changes. It affects individuals across all age groups and varies by gender and developmental stage.
Depression can occur in children, adolescents, and adults, with increasing prevalence during adolescence. Females are at higher risk than males, especially after puberty. Symptoms may include sadness, withdrawal, sleep changes, and impaired concentration. Early detection is crucial for effective intervention.
Rationale for correct answers
2. Women are nearly twice as likely to develop depression due to hormonal fluctuations, psychosocial stressors, and gender-based vulnerabilities. This disparity emerges strongly during adolescence and persists across the lifespan.
3. Depression rates increase with age during adolescence due to neurodevelopmental changes, identity formation stress, and social pressures. Older teens show higher prevalence than younger children.
4. Children of all ages can experience depression, though symptoms may differ from adults. Developmental factors influence presentation, such as irritability in younger children and withdrawal in older ones.
Rationale for incorrect answers
1. Fluctuation between low mood and euphoria suggests bipolar disorder, not depression. Depression is marked by persistent low mood without manic or euphoric episodes.
5. Perfectionism and rigid thinking are more indicative of obsessive-compulsive traits or anxiety disorders. While they may co-occur, they are not diagnostic criteria for depression.
Take Home Points
- Depression affects individuals across the lifespan, including children and adolescents.
- Females have higher prevalence rates, especially after puberty.
- Bipolar disorder includes mood fluctuations, unlike unipolar depression.
- Rigid thinking and perfectionism are more aligned with anxiety or obsessive-compulsive patterns.
Practice Exercise 2
A nurse is assessing a client with dysthymia who reports symptoms of depressed mood. Which assessment finding supports the essential feature of dysthymia?
Explanation
Dysthymia, also known as persistent depressive disorder, is a chronic mood disturbance characterized by low-grade depression lasting for extended periods. The essential diagnostic feature is a depressed mood present most of the day, more days than not, for at least 2 years in adults. Symptoms may include fatigue, low self-esteem, poor concentration, and changes in appetite or sleep, but they are typically less severe than those seen in major depressive disorder. Despite its milder intensity, dysthymia significantly impairs functioning and quality of life due to its prolonged duration.
Rationale for correct answer
2. Chronically depressed mood for at least 2 years is the defining criterion for dysthymia. This persistent emotional state distinguishes it from episodic depressive disorders and is required for diagnosis in adults.
Rationale for incorrect answers
1. Recurrent thoughts of death are more indicative of major depression or suicidal ideation. While dysthymia may involve hopelessness, active death thoughts are not essential features.
3. Significant weight loss reflects somatic symptoms more common in major depressive episodes. Dysthymia may involve appetite changes, but dramatic weight shifts are not core diagnostic elements.
4. Diminished ability to think or concentrate can occur in dysthymia but is not unique to it. This symptom overlaps with other mood and anxiety disorders and lacks diagnostic specificity.
Take Home Points
- Dysthymia is defined by a chronically depressed mood lasting at least 2 years in adults.
- Symptoms are milder than major depression but persistent and functionally impairing.
- Suicidal ideation and significant weight loss are more typical of major depressive disorder.
- Accurate diagnosis depends on duration and consistency of mood symptoms, not severity alone.
As part of discharge education for a postpartum client, a nurse suggests prevention strategies for postpartum depression. Which prevention strategies should the nurse include when educating the client on postpartum depression? Select all that apply.
Explanation
Postpartum depression is a mood disorder that can emerge within weeks after childbirth, marked by persistent sadness, fatigue, and impaired bonding. Prevention focuses on emotional awareness, structured routine, and social support. Early recognition and proactive coping strategies reduce severity and improve maternal-infant outcomes.
Rationale for correct answers
1. Support groups provide peer connection and emotional validation, reducing isolation and normalizing postpartum experiences. This enhances coping and reduces depressive symptoms through shared understanding and social reinforcement.
3. Journaling promotes emotional processing, helping clients identify patterns in mood and triggers. It encourages self-reflection and can aid in recognizing when professional help is needed, improving mental clarity.
4. Promptly notifying a provider when overwhelmed ensures early intervention, preventing escalation of symptoms. Timely support can include therapy, medication, or community resources, improving clinical outcomes.
5. A daily schedule fosters predictability and control, reducing anxiety and enhancing time management. Structured routines help balance infant care with self-care, supporting psychological stability.
Rationale for incorrect answers
2. Prioritizing chores over rest during nap time can lead to exhaustion, increasing vulnerability to depression. Rest and recovery are essential for physical and emotional resilience postpartum.
6. Major life changes (e.g., moving, job shifts) during the first year add stress, disrupting emotional adjustment. Stability is crucial during the postpartum period to support recovery and bonding.
Take Home Points
- Postpartum depression prevention includes emotional awareness, structured routines, and strong social support.
- Early intervention is critical when feelings of overwhelm persist beyond normal adjustment.
- Rest and recovery should be prioritized over productivity during the postpartum period.
- Avoiding major life changes in the first year postpartum supports emotional stability and maternal-infant bonding.
The husband of a postpartum client, who has been diagnosed with postpartum depression (PPD), is concerned and asks a nurse what kind of treatment his wife will require. The nurse’s response should be based on the knowledge that the collaborative plan of care for PPD includes which of the following?
Explanation
Postpartum depression is a serious mood disorder that affects maternal functioning and infant bonding. Treatment requires a collaborative approach involving both pharmacologic and psychotherapeutic interventions. The goal is to stabilize mood, restore functioning, and ensure safety for both mother and infant. Evidence-based care includes antidepressants, especially SSRIs, and structured therapy such as CBT or IPT.
Rationale for correct answer
1. The combination of antidepressants and psychotherapy is the gold standard for moderate to severe postpartum depression. SSRIs are commonly used due to their safety profile in breastfeeding, while therapy addresses cognitive distortions and emotional regulation.
Rationale for incorrect answers
2. Psychotherapy alone may be insufficient for moderate to severe cases. Without pharmacologic support, symptom relief may be delayed, increasing risk for maternal and infant complications.
3. Removing the infant is not a therapeutic intervention for PPD unless there is imminent risk of harm. This approach can worsen bonding and maternal distress, and is not part of standard care.
4. Hypnotic agents are not first-line treatments for depression. They may be used short-term for insomnia, but do not address core mood symptoms and carry risks of dependency and sedation.
Take Home Points
- Postpartum depression requires a dual approach: antidepressants and psychotherapy for optimal recovery.
- SSRIs are preferred due to safety in lactation and efficacy in mood stabilization.
- Psychotherapy alone may suffice in mild cases but is inadequate for moderate to severe depression.
- Removal of the infant is not a treatment strategy and may exacerbate maternal distress.
A nurse is conducting a home visit with a client who had surgery 3 months ago that involved the creation of a colostomy. When the nurse arrives at the home, the client’s wife reports that her husband has lost interest in golf, which used to be his passion. She also says he cries often for no reason, is only able to sleep for a few hours each night, and reports fatigue daily. The wife asks the nurse for advice. A nurse’s response should be based on the knowledge that:
Explanation
Depression after ostomy surgery is a common psychological response to altered body image, lifestyle disruption, and loss of control. The emotional impact includes grief, impaired self-concept, and social withdrawal, often manifesting as anhedonia, sleep disturbance, and fatigue. Adjustment varies widely, and clinical depression may persist months after surgery, requiring timely recognition and intervention.
Rationale for correct answer
1. Studies show that approximately 25–43% of individuals develop clinically significant depression following ostomy surgery due to changes in body image, lifestyle limitations, and emotional distress. The client’s symptoms—loss of interest, crying, fatigue, and insomnia—are consistent with major depressive disorder.
Rationale for incorrect answers
2. Physical activities like golf are not contraindicated post-ostomy. With proper stoma care, many individuals resume sports and hobbies. Limiting activity may worsen emotional health and is not medically justified.
3. Psychological adjustment to body image after ostomy varies. Three months is not a universal benchmark for acceptance. Emotional recovery depends on support systems, coping mechanisms, and pre-existing mental health.
4. Sleep disruption is not inherently caused by an ostomy. While initial adjustment may affect sleep, persistent insomnia is more likely linked to underlying depression or anxiety, not the ostomy itself.
Take Home Points
- Depression is common after ostomy surgery and may persist beyond the initial recovery period.
- Resuming physical activities like golf is encouraged and feasible with proper stoma management.
- Body image acceptance varies; emotional support and counseling may be needed for adjustment.
- Sleep disturbances in ostomy patients often reflect underlying mood disorders rather than the ostomy itself.
A client with a diagnosis of end-stage renal disease states to a nurse, “I don’t think I want to be on dialysis anymore; it’s just too painful for me.” What is the most appropriate response by the nurse?
Explanation
End-stage renal disease (ESRD) is a progressive condition requiring renal replacement therapy, typically dialysis, to sustain life. The treatment is physically demanding and emotionally taxing, often leading to treatment fatigue, psychological distress, and existential questioning. Therapeutic communication is essential to explore the patient's experience, validate emotions, and support shared decision-making.
Rationale for correct answer
2. This response uses reflective listening, a therapeutic communication technique, acknowledging the client’s emotional experience and inviting further dialogue. It fosters trust and opens space for the client to express concerns, which is essential in evaluating readiness, coping, and potential alternatives.
Rationale for incorrect answers
1. Asking “why” may sound confrontational, triggering defensiveness. It lacks empathy and does not validate the client’s emotional pain, which is central to effective communication in ESRD care.
3. Minimizing the client’s experience by suggesting dialysis “isn’t hard” invalidates their distress. It dismisses the physical and emotional burden, potentially eroding rapport and trust.
4. While factually accurate, this response is fear-inducing and lacks compassion. It prioritizes clinical outcomes over emotional support, which may alienate the client and hinder open discussion.
Take Home Points
- Reflective listening is essential in supporting ESRD clients facing treatment fatigue or emotional distress.
- Therapeutic communication validates patient experience and promotes shared decision-making.
- Avoid minimizing or confronting patient concerns; empathy fosters trust and engagement.
- ESRD care must balance clinical needs with emotional and psychological support.
Practice Exercise 3
A nurse in a clinic is caring for a 16-year-old mother and her baby. The mother seems anxious about her new role as a mother. She looks at the nurse and says, “I don’t think I can do this.” What are some conclusions that the nurse might make about this situation? Select all that apply.
Explanation
Postpartum depression is a mood disorder that can affect mothers after childbirth, especially adolescents. It involves persistent sadness, anxiety, and feelings of inadequacy. Adolescent mothers are at higher risk due to limited coping skills, lack of support, and hormonal fluctuations. Early recognition is critical to prevent escalation into neglect or harm. Symptoms may include withdrawal, irritability, and verbal expressions of hopelessness. Screening tools and clinical interviews are essential for diagnosis and intervention.
Rationale for correct answers
1. The mother’s verbal expression of doubt and visible anxiety are consistent with emotional distress and possible postpartum depression. Adolescents are particularly vulnerable due to immature coping mechanisms and lack of support systems.
2. Feelings of inadequacy and hopelessness may escalate into neglectful behavior or abandonment, especially in young mothers lacking emotional or social resources. Early identification of risk factors is essential for safety planning.
Rationale for incorrect answers
3. Providing safe house information prematurely assumes intent, which is not clinically justified. The mother has expressed doubt, not intent to abandon, and such action may stigmatize or escalate her distress.
4. Blaming the mother for not learning coping strategies in prenatal classes reflects judgment, not therapeutic care. Many adolescent mothers lack access to comprehensive prenatal education, and this approach lacks empathy and clinical relevance.
5. Encouraging adoption without assessing the mother’s capacity and willingness undermines autonomy and therapeutic rapport. Adoption is a complex decision requiring multidisciplinary evaluation, not a reflexive response to distress.
Take Home Points
- Postpartum depression in adolescents requires early recognition and supportive intervention to prevent escalation.
- Expressions of doubt or anxiety may signal emotional distress, not intent to harm or abandon.
- Therapeutic responses should prioritize empathy, assessment, and safety—not judgment or premature referrals.
- Differentiating postpartum depression from normal adjustment reactions is essential for appropriate care planning.
An experienced nurse is teaching a new nurse about establishing therapeutic relationships with clients on a mental health unit. Which intervention should the nurse suggest when attempting to establish a therapeutic relationship with a client diagnosed with major depressive disorder?
Explanation
Major depressive disorder is a psychiatric condition characterized by persistent low mood, anhedonia, and cognitive disturbances. Clients often experience psychomotor retardation, impaired concentration, and social withdrawal. Establishing therapeutic rapport requires sensitivity to the client’s emotional state and energy level. Early interactions should prioritize presence, nonverbal support, and emotional safety over verbal engagement or activity-based interventions. Silence, when intentional and attuned, can convey empathy and respect for the client’s internal process.
Rationale for correct answer
1. Sitting in silence demonstrates empathic presence and respects the client’s limited energy and emotional capacity. It allows space for trust to develop without pressure, which is essential in early rapport-building with depressive clients.
Rationale for incorrect answers
2. A 2-hour movie may overwhelm the client’s cognition, given impaired concentration and low motivation typical in major depressive disorder. Long activities may increase withdrawal rather than foster engagement.
3. Exercise is beneficial in later stages of recovery, but early in treatment, clients may lack initiative and physical energy. Pushing activity prematurely may be perceived as invalidating or intrusive.
4. Asking the client to schedule their day assumes executive functioning that is often impaired in depression. This may increase anxiety or reinforce feelings of inadequacy rather than promote autonomy.
Take Home Points
- Therapeutic relationships in depression begin with empathic presence, not verbal or behavioral demands.
- Silence can be a powerful tool in psychiatric nursing when used intentionally and respectfully.
- Activities and decision-making should be introduced gradually, based on the client’s readiness and energy level.
- Depression impairs motivation, cognition, and social engagement—interventions must align with these limitations.
A nurse is educating a client diagnosed with depression who is experiencing insomnia. Which intervention should the nurse recommend to reduce episodes of insomnia?
Explanation
Insomnia in depression is a common comorbidity marked by difficulty initiating or maintaining sleep, often due to hyperarousal, disrupted circadian rhythms, and cognitive rumination. Sleep hygiene is foundational in managing insomnia, especially when linked to mood disorders. Regular sleep-wake cycles help stabilize melatonin secretion and reinforce the body’s natural circadian rhythm. Behavioral interventions are preferred over pharmacologic ones in mild to moderate cases, with emphasis on consistency, environmental cues, and minimizing stimulation before bedtime.
Rationale for correct answer
1. Maintaining regular bedtime hours reinforces circadian regulation and improves sleep efficiency. Consistency in sleep-wake timing helps synchronize melatonin release and reduces sleep latency, especially in depressive insomnia.
Rationale for incorrect answers
2. Sleeping late on weekends disrupts homeostasis and weakens circadian entrainment. Irregular sleep patterns worsen insomnia and may exacerbate depressive symptoms due to inconsistent melatonin and cortisol rhythms.
3. Fighting insomnia increases arousal, counteracting the relaxation needed for sleep onset. Cognitive struggle activates sympathetic pathways, worsening sleep latency and reinforcing maladaptive sleep behaviors.
4. Exercising close to bedtime elevates core temperature, delaying melatonin onset and sleep readiness. While exercise is beneficial, it should be scheduled earlier in the day to avoid stimulating effects.
Take Home Points
- Depression-related insomnia responds well to behavioral sleep hygiene strategies like consistent bedtime routines.
- Irregular sleep schedules and compensatory sleeping worsen circadian misalignment and mood instability.
- Cognitive arousal and physical stimulation before sleep delay onset and reduce sleep quality.
- Exercise improves sleep but should be timed to avoid interference with melatonin release and sleep initiation.
A nurse is assessing a client while attempting to differentiate the client’s symptoms between delirium and depression. Which symptoms of the client are unique to depression? Select all that apply.
Explanation
Depression is a mood disorder characterized by persistent emotional distress, cognitive slowing, and psychomotor changes. Unlike delirium, which presents with acute onset and fluctuating consciousness, depression develops gradually and maintains clear alertness. Clients often exhibit anhedonia, hopelessness, and impaired motivation. Sleep disturbances are common, including early morning awakening and hypersomnia. While hallucinations may occur in severe cases, they are not exclusive to depression and must be differentiated from delirium-related perceptual disturbances.
Rationale for correct answers
1. Sadness is a core affective symptom of depression, often persistent and unprovoked. It reflects internal emotional dysregulation and is not typical in delirium, which is more cognitive and perceptual.
2. Sleep disturbances such as early awakening, hypersomnia, or insomnia are hallmark features of depression. These are linked to dysregulated circadian rhythms and altered REM latency, not seen in delirium.
5. Lack of motivation stems from psychomotor retardation and diminished interest, central to depressive pathology. In delirium, activity may be agitated or withdrawn but not due to motivational deficits.
Rationale for incorrect answers
3. Fluctuating levels of consciousness are indicative of delirium, not depression. Delirium involves waxing and waning alertness, often with disorientation and impaired attention.
4. Labile affect is more characteristic of delirium, especially in hyperactive forms. Emotional instability in delirium may be abrupt and inconsistent, unlike the sustained low mood in depression.
6. Presence of hallucinations occurs in both conditions but is more transient and visual in delirium. In depression, hallucinations are typically mood-congruent and auditory, seen in psychotic depression.
Take Home Points
- Depression presents with persistent sadness, sleep disruption, and motivational decline, while delirium involves acute cognitive and consciousness changes.
- Fluctuating alertness and labile affect are more consistent with delirium than depression.
- Hallucinations may occur in both but differ in type, duration, and context.
- Differentiating these conditions is critical for appropriate treatment and safety planning.
A client notifies a staff member of current suicidal ideations. Which intervention by the nurse would take priority?
Explanation
Suicidal ideation is a psychiatric emergency requiring immediate action to prevent self-harm. The highest priority is safety, especially when ideation is current. Clients may present with varying degrees of intent, but any disclosure of suicidal thoughts demands direct supervision. One-to-one observation ensures continuous monitoring, reduces risk of impulsive behavior, and allows for rapid intervention. This level of care is critical during the initial phase of ideation disclosure, before further assessment or planning.
Rationale for correct answer
1. Continuous supervision is the most urgent intervention. One-to-one observation ensures the client is never left alone, preventing any opportunity for self-harm.
Rationale for incorrect answers
2. Plan assessment is essential but secondary. It informs risk level but does not prevent immediate harm if the client is left unsupervised.
3. History of attempts contributes to risk stratification but does not address the current threat. Past behavior is predictive, not protective.
4. Precautions are necessary but not sufficient. Notifying staff and initiating protocols must follow immediate physical safety measures like one-to-one observation.
Take Home Points
- One-to-one observation is the highest priority when suicidal ideation is disclosed to prevent immediate harm.
- Risk assessment tools are important but secondary to direct supervision in acute phases.
- Suicide precautions include environmental safety, staff awareness, and monitoring, but must be paired with direct observation.
- Past suicide attempts increase risk but do not replace the need for immediate protective interventions.
A nurse is assessing a client’s alcohol intake as part of a routine screening examination. The client reports drinking 3 to 4 beers, five times per week. The client is being treated for depression with sertraline (Zoloft®) 100 mg daily. Which statement by the nurse about the client’s alcohol consumption is accurate?
Explanation
Alcohol and depression interact negatively, especially when combined with sertraline, a selective serotonin reuptake inhibitor (SSRI). Alcohol is a central nervous system depressant that can counteract the therapeutic effects of antidepressants, worsen mood symptoms, and increase the risk of sedation, impaired judgment, and suicidal ideation. Chronic alcohol use disrupts serotonin regulation, undermines medication efficacy, and may trigger relapse or treatment resistance. Even moderate intake can interfere with neurochemical balance and emotional stability in clients with depression.
Rationale for correct answer
3. Alcohol worsens depression by interfering with serotonin modulation, reducing the effectiveness of SSRIs like sertraline. It also increases sedation and impairs cognitive function, complicating recovery and increasing relapse risk.
Rationale for incorrect answers
1. Alcohol may temporarily numb emotional pain but ultimately exacerbates neurochemical imbalance. It impairs serotonin transmission and deepens depressive symptoms, especially in clients on SSRIs.
2. Defining intake as “normal” based on quantity ignores clinical context. For clients with depression and SSRI use, even moderate alcohol can disrupt treatment and increase adverse effects.
4. Alcohol is a depressant, not a stimulant. While it may reduce inhibition briefly, it impairs mood regulation and social functioning over time, especially in individuals with underlying depression.
Take Home Points
- Alcohol is a depressant that worsens mood symptoms and interferes with antidepressant efficacy.
- Sertraline and alcohol together increase sedation, cognitive impairment, and emotional instability.
- Even moderate alcohol intake can undermine depression treatment and increase relapse risk.
- Nurses should educate clients on the risks of alcohol use during SSRI therapy and promote abstinence or reduction.
A client diagnosed with major depressive disorder expresses to a nurse that death would be better than living with depression. The nurse determines that the client is suffering from suicidal ideation and is at risk for committing suicide. Which nursing intervention is priority for the client experiencing suicidal ideation?
Explanation
Suicidal ideation in major depressive disorder represents a psychiatric emergency requiring immediate safety measures. Clients may experience hopelessness, impaired judgment, and impulsivity, increasing the risk of self-harm. The priority is to ensure physical safety through direct observation, environmental control, and activation of emergency protocols. Therapeutic interventions and education follow only after stabilization. Suicide risk assessment includes evaluating intent, plan, means, and protective factors. Nurses must act decisively to prevent harm while maintaining therapeutic rapport.
Rationale for correct answer
3. Alerting authorities and initiating frequent monitoring ensures immediate safety, which is the highest priority in suicidal ideation. This action activates crisis protocols and allows for continuous observation, reducing the risk of impulsive self-harm.
Rationale for incorrect answers
1. Discussing reasons to live may be helpful later, but in acute ideation, it delays intervention. Clients in crisis may not be receptive to affirmations and require immediate safety measures before cognitive reframing.
2. Education on treatment is not appropriate during active suicidal ideation. It assumes stability, which is not present. Safety must precede psychoeducation to ensure the client is emotionally and cognitively ready.
4. Environmental assessment is important but secondary to activating external support. Without monitoring and authority involvement, the client remains at risk even if means are removed temporarily.
Take Home Points
- Suicidal ideation in depression requires immediate safety interventions, including monitoring and emergency activation.
- Therapeutic communication and education are secondary to physical protection in acute crisis.
- Environmental control is supportive but insufficient without external supervision and crisis response.
- Nurses must prioritize safety before initiating therapeutic or educational strategies in suicidal clients.
Which nursing diagnosis should a nurse give highest priority when caring for a client with major depressive disorder?
Explanation
Major depressive disorder is a psychiatric condition marked by persistent low mood, hopelessness, and impaired functioning. Clients may experience suicidal ideation, psychomotor retardation, and cognitive impairment, increasing the risk for self-harm. The highest priority in nursing care is safety, especially when symptoms suggest potential for injury. While emotional and spiritual needs are important, they are secondary to preserving life. Risk assessments must be ongoing, and interventions should focus on environmental control, observation, and crisis management.
Rationale for correct answer
3. Potential for injury is the highest priority due to the risk of suicidal behavior or self-harm. Depression can impair judgment and increase impulsivity, making safety interventions critical to prevent irreversible outcomes.
Rationale for incorrect answers
1. Powerlessness reflects emotional distress and lack of control but does not pose an immediate physical threat. It can be addressed after ensuring the client’s safety and stabilization.
2. Potential for spiritual distress may affect coping, but it is not life-threatening. Addressing existential concerns is important but follows after physical safety is secured.
4. Disturbed sleep patterns are common in depression but are not urgent. While they affect quality of life and recovery, they do not carry the same immediate risk as injury or suicide.
Take Home Points
- Safety is the top priority in clients with major depressive disorder, especially when suicidal ideation is present.
- Emotional and spiritual concerns are important but secondary to physical protection.
- Sleep disturbances and feelings of powerlessness require attention after stabilization.
- Nursing diagnoses must be prioritized based on risk to life and immediate clinical needs.
The physician diagnoses Stanley with major depression. A suicide assessment is conducted. Why is Stanley at high risk for suicide?
Explanation
Suicide risk in major depression is heightened by access to lethal means, demographic factors, and psychosocial stressors. The most immediate predictor of suicide completion is means availability, particularly firearms, which drastically increase lethality. While demographic and psychosocial factors contribute to risk, access to a gun represents a direct and actionable threat.
Rationale for correct answer
4. The presence of a firearm in the home is the most critical risk factor in this scenario. Firearms are associated with high lethality and impulsivity in suicide attempts, especially in individuals with major depression.
Rationale for incorrect answers
1. Not all individuals with depression are at equal risk. Suicide risk varies based on severity, comorbid conditions, and access to means. This statement is overly general and lacks clinical precision.
2. While older adults have elevated suicide rates, the highest completion rates are in elderly white males. Age alone is not the most predictive factor in this case.
3. Although being a white male, bereaved, and living alone increases risk, these are indirect contributors. They do not pose the same immediate danger as firearm access.
Take Home Points
- Firearm access is the most immediate and lethal risk factor for suicide in depressed individuals.
- Depression alone does not uniformly predict suicide; context and access to means are critical.
- Demographic factors like age, race, and isolation elevate risk but are less actionable than means.
- Suicide assessments must prioritize identifying access to lethal methods, especially firearms.
A nurse is caring for a client who complains of chronic pain. Given this complaint, why would the nurse simultaneously evaluate both general physical and psychosocial problems?
Explanation
Chronic pain and depression frequently co-occur, forming a complex clinical picture that involves both somatic symptoms and emotional distress. Pain perception is modulated by neurochemical pathways involving serotonin, norepinephrine, and the limbic system—areas also implicated in mood regulation. Depression can amplify pain sensitivity, reduce coping capacity, and impair treatment response. Conversely, chronic pain may trigger or worsen depressive symptoms due to functional limitations, social isolation, and hopelessness. Integrated assessment is essential to identify overlapping symptoms and guide comprehensive care.
Rationale for correct answer
1. Depression is commonly associated with pain disorders due to shared neurochemical mechanisms and overlapping symptomatology. Evaluating both domains allows for accurate diagnosis and treatment planning, improving outcomes and reducing relapse risk.
Rationale for incorrect answers
2. While time efficiency is desirable, prioritizing speed over clinical accuracy may lead to missed diagnoses. Comprehensive evaluation is necessary to address the multifactorial nature of chronic pain and its psychological impact.
3. Insurance coverage varies and should not dictate clinical judgment. The need for dual assessment is based on patient presentation and evidence-based practice, not administrative constraints.
4. Physicians are trained to assess psychosocial factors, especially in integrated care models. Nurses collaborate with physicians and mental health professionals to ensure holistic evaluation, not assume lack of expertise.
Take Home Points
- Chronic pain and depression share neurobiological pathways and often present together.
- Integrated assessment improves diagnostic accuracy and treatment effectiveness.
- Clinical decisions should be based on patient needs, not time or insurance constraints.
- Nurses play a key role in identifying psychosocial factors and coordinating interdisciplinary care.
Practice Exercise 4
Which statement made by a client, who is being treated for severe depression and receiving information regarding self-help groups, best reflects understanding of the priority goal for crisis intervention?
Explanation
Crisis intervention is a short-term, focused approach aimed at restoring psychological equilibrium and preventing long-term dysfunction. It prioritizes stabilization, empowerment, and hope. The goal is not deep insight or long-term therapy, but immediate relief and mobilization of internal and external resources. In the context of severe depression, the priority is to reestablish a sense of control and future orientation, often through therapeutic engagement and support systems. The client must demonstrate readiness to engage in recovery and express belief in the possibility of improvement.
Rationale for correct answer
4. The client’s statement reflects hope and goal orientation, which are central to crisis resolution. Expressing a desire to regain their previous life shows psychological mobilization and readiness to engage in recovery. This aligns with the therapeutic goal of restoring baseline functioning and fostering adaptive coping.
Rationale for incorrect answers
1. The focus on learning to cope with stress is educational, not crisis-focused. While stress management is important, it does not reflect the immediate goal of emotional stabilization or psychological recovery.
2. This statement is cognitive, identifying a cause-effect relationship. However, it lacks emotional engagement or forward movement. Insight alone does not meet the criteria for crisis resolution, which requires active coping and hope.
3. Medication adherence is behavioral, but it reflects compliance rather than emotional recovery. While important for long-term management, it does not address the immediate psychological needs during crisis intervention.
Take Home Points
- Crisis intervention prioritizes emotional stabilization, hope, and mobilization of coping resources.
- Statements reflecting goal-directed behavior and belief in recovery indicate effective crisis resolution.
- Insight and education are secondary to emotional engagement during acute intervention.
- Depression management includes both pharmacologic and psychosocial strategies, but crisis care emphasizes immediate psychological restoration.
Which intervention should be implemented initially when providing crisis intervention for a client being treated for exacerbation of depression who states, “Caring for all my children is just too hard!”?
Explanation
Crisis intervention in the context of depression aims to stabilize the client emotionally and prevent further deterioration. The initial goal is to establish trust, reduce isolation, and ensure safety. When a client expresses being overwhelmed by parenting responsibilities, the priority is not problem-solving or long-term planning, but immediate emotional containment and therapeutic presence. Depression often impairs executive functioning and decision-making, so interventions must first restore psychological safety before addressing external stressors.
Rationale for correct answer
2. One-on-one nurse-client time provides emotional containment and therapeutic presence, which are essential in early crisis intervention. This approach reinforces the nurse’s commitment, builds trust, and helps the client feel less alone. It also allows for real-time assessment of risk factors such as suicidal ideation or hopelessness, which are common in depressive exacerbations.
Rationale for incorrect answers
1. Delegating childcare to grandparents is a logistical solution, not an emotional intervention. While it may reduce external stress, it bypasses the immediate need for psychological stabilization and therapeutic engagement.
3. Self-help groups are supportive, but not appropriate as an initial step in crisis. The client may lack the emotional readiness to engage with others, and group settings may increase anxiety or feelings of inadequacy during acute distress.
4. Identifying stressors is a cognitive task that requires introspection and emotional regulation. In the early phase of crisis, the client may be too overwhelmed to process or articulate these factors, making this intervention premature.
Take Home Points
- Initial crisis intervention for depression prioritizes emotional containment and therapeutic presence.
- Practical solutions and cognitive tasks should follow after psychological stabilization is achieved.
- One-on-one engagement allows for real-time assessment of risk and builds trust.
- Group interventions and stressor identification are more appropriate in post-crisis recovery phases.
The spouse of a client who has been on hemodialysis for the past 5 years calls a clinic because the client has stopped eating, is taking long naps, and refuses to talk with the spouse. A nurse interprets that the client is most likely experiencing:
Explanation
Depression is a common comorbidity in individuals with chronic illnesses such as end-stage renal disease. It is characterized by anhedonia, withdrawal, and fatigue, often mistaken for disease-related symptoms. In patients undergoing long-term hemodialysis, psychological burden accumulates due to lifestyle restrictions, physical discomfort, and perceived loss of autonomy. Depression in this population is underdiagnosed and often presents with somatic complaints, reduced appetite, and social disengagement rather than overt sadness.
Rationale for correct answer
1. The client’s refusal to eat, excessive sleeping, and social withdrawal are hallmark signs of anhedonia and psychomotor retardation, both core features of depression. These symptoms are not explained by dialysis alone and suggest a mood disorder requiring clinical attention. The chronicity of dialysis increases vulnerability to depressive episodes due to cumulative psychosocial stressors.
Rationale for incorrect answers
2. Displacement involves emotional redirection, typically seen in interpersonal conflict or projection. The client’s behavior reflects internal withdrawal, not outward redirection of feelings, making this an inaccurate interpretation.
3. Noncompliance refers to intentional refusal or neglect of medical advice or treatment. The scenario lacks evidence of defiance or disregard for dialysis protocols, and the symptoms described are more consistent with mood disturbance than behavioral opposition.
4. Activity intolerance is a physiologic limitation in performing tasks due to fatigue or dyspnea. While fatigue is present, the broader behavioral symptoms—social withdrawal and anorexia—are not explained by physical deconditioning alone, ruling out this option.
Take Home Points
- Depression in dialysis patients often presents with somatic symptoms and social withdrawal rather than sadness.
- Differentiating mood disorders from physiologic fatigue is essential in chronic illness management.
- Displacement and noncompliance are behavioral constructs that require specific contextual cues.
- Activity intolerance must be distinguished from psychomotor slowing seen in depressive states.
A nurse is developing a care plan for an older adult female client diagnosed with depression. The inclusion of the nursing diagnosis Risk for injury due to osteopenia demonstrates that the nurse understands which evidence-based concept related to the client’s medical diagnosis?
Explanation
Depression and osteopenia are interlinked conditions in older adult females, particularly postmenopausal women. Evidence shows that low bone mineral density is associated with increased risk of depression due to hormonal changes, reduced physical activity, and inflammatory pathways. Conversely, depression may exacerbate bone loss through behavioral factors like poor nutrition, inactivity, and medication effects such as SSRIs. This bidirectional relationship highlights the need for integrated care planning that addresses both psychological and skeletal health.
Rationale for correct answer
3. The link between hip bone loss and depression is supported by research showing that postmenopausal women with reduced bone mineral density have a higher prevalence of depressive symptoms. The physiological stress of bone fragility, combined with reduced mobility and fear of falling, contributes to mood disturbances. Including “Risk for injury due to osteopenia” in the care plan reflects understanding of this dual vulnerability.
Rationale for incorrect answers
1. While older females are generally more prone to injury, this statement lacks specificity. It does not connect the injury risk to depression or osteopenia, making it a generic observation rather than an evidence-based concept.
2. Self-destructive behavior is more typical in severe psychiatric disorders or acute depressive episodes with suicidal ideation. The scenario describes a chronic condition, and osteopenia-related injury risk is not primarily due to intentional harm.
4. Confusion is more commonly associated with delirium, dementia, or medication effects. Depression may cause cognitive slowing, but not confusion in the clinical sense. This choice misrepresents the cognitive profile of geriatric depression.
Take Home Points
- Depression and osteopenia share a bidirectional relationship in older adult females.
- Bone loss increases risk of depression through physical limitations and hormonal changes.
- Depression may worsen osteopenia via inactivity and poor self-care.
- Care plans should integrate physical and psychological risk factors to prevent injury and improve outcomes.
A home-care nurse is visiting the home of a client diagnosed with Alzheimer’s disease. Which question by the nurse is most appropriate when attempting to assess the level of depression that the client’s husband is experiencing as the primary caregiver?
Explanation
Caregiver depression is a prevalent and often underrecognized condition among individuals providing long-term care for loved ones with Alzheimer’s disease. It is driven by emotional exhaustion, social isolation, and chronic stress. Symptoms may include irritability, sleep disturbances, loss of interest in previously enjoyed activities, and feelings of hopelessness. Effective assessment requires emotionally attuned, open-ended questions that invite reflection and reveal the caregiver’s internal experience rather than surface-level logistics.
Rationale for correct answer
4. This question reflects empathy and emotional insight, prompting the caregiver to explore how their role has impacted personal fulfillment. It indirectly assesses loss of pleasure and social withdrawal—core features of depression—without being confrontational. The phrasing encourages disclosure and opens space for deeper conversation about emotional burden.
Rationale for incorrect answers
1. This question is task-oriented, focusing on logistics rather than emotional state. While helpful in care planning, it does not assess psychological well-being or depressive symptoms.
2. Asking about spare time is neutral and may not elicit meaningful responses. It assumes the caregiver has leisure time and does not directly probe emotional impact or mood changes.
3. This question is leading and may provoke defensiveness. It frames caregiving as inherently stressful, which may not align with the caregiver’s self-perception, limiting honest emotional disclosure.
Take Home Points
- Depression in caregivers often presents as loss of interest, emotional fatigue, and social withdrawal.
- Open-ended, empathetic questions are more effective in assessing caregiver emotional health.
- Task-based inquiries may miss underlying psychological distress.
- Caregiver well-being directly influences the quality of care provided to Alzheimer’s patients.
A client diagnosed with major depressive disorder has the nursing diagnosis of Disturbed sleep pattern. When developing a plan of care for this client, which nursing actions are most appropriate? Select all that apply.
Explanation
Disturbed sleep pattern in clients with major depressive disorder is often characterized by insomnia, early morning awakening, or hypersomnia. Sleep architecture is disrupted, with reduced REM latency and fragmented sleep cycles. Depression alters circadian rhythms and melatonin secretion, contributing to poor sleep quality. Effective nursing care targets behavioral, environmental, and physiological contributors to sleep disruption, aiming to restore restorative sleep and improve daytime functioning.
Rationale for correct answers
1. Determining baseline sleep patterns prior to hospitalization helps identify changes and tailor interventions. It provides insight into pre-existing habits, environmental triggers, and the severity of sleep disruption.
2. Discouraging daytime sleep promotes sleep hygiene and helps reestablish a consistent circadian rhythm. Excessive napping can reduce sleep drive at night and worsen insomnia symptoms.
3. Recording and limiting caffeine intake addresses a modifiable stimulant that interferes with sleep onset and depth. Caffeine affects adenosine receptors and delays melatonin release, worsening sleep fragmentation.
5. Encouraging relaxation techniques such as guided imagery, progressive muscle relaxation, or breathing exercises reduces sympathetic arousal and facilitates sleep initiation. These methods are non-pharmacologic and enhance parasympathetic tone.
Rationale for incorrect answer
4. Reinforcing reality is a cognitive intervention more relevant to psychotic features or disorientation. It does not directly address sleep disturbances and is not a primary strategy for managing insomnia in depression.
Take Home Points
- Sleep disturbances in depression stem from altered circadian rhythms and neurochemical imbalances.
- Behavioral strategies like limiting caffeine and discouraging daytime naps improve sleep hygiene.
- Relaxation techniques enhance parasympathetic activation and support sleep onset.
- Cognitive interventions like reality orientation are not first-line for sleep pattern disturbances.
A nurse is caring for a client who reveals symptoms of a sleep disorder during the admission assessment. The client also admits that he has “broken down and cried for no apparent reason.” Which criterion is most important for the nurse to initially consider to gain insight into the client’s patterns of sleep and feelings of depression?
Explanation
Depression-related sleep disorders often manifest as insomnia, hypersomnia, or fragmented sleep, and are tightly linked to psychosocial stressors, emotional dysregulation, and neurochemical imbalances. The presence of unexplained crying suggests underlying affective disturbance, possibly triggered or exacerbated by life events. Sleep disturbances in depression are rarely isolated; they reflect broader disruptions in mood, cognition, and coping mechanisms. Understanding the client’s stress context is essential for accurate diagnosis and targeted intervention.
Rationale for correct answer
1. Exploring life stressors provides insight into emotional triggers that may underlie both sleep disturbance and depressive symptoms. Stress activates the hypothalamic-pituitary-adrenal axis, disrupting sleep architecture and serotonin regulation. Identifying psychosocial burdens allows the nurse to assess coping capacity, emotional resilience, and the potential need for therapeutic support.
Rationale for incorrect answers
2. Weight may influence sleep apnea risk but does not directly explain emotional breakdowns or depressive symptoms. It is a secondary consideration unless physical comorbidities are suspected.
3. Apnea involves respiratory disruption, typically presenting with snoring, gasping, or daytime fatigue. It does not account for emotional symptoms like crying and is not the most immediate criterion for assessing mood-related sleep issues.
4. Sexual activity may reflect libido changes in depression but is not a primary lens for evaluating sleep patterns or emotional distress. It is more relevant in comprehensive psychosocial assessments than initial screening.
Take Home Points
- Psychosocial stressors are central to understanding sleep and mood disturbances.
- Depression-related sleep disorders often reflect broader emotional dysregulation.
- Physical factors like weight and apnea are important but secondary in mood-focused assessments.
- Initial nursing evaluations should prioritize emotional context over behavioral or physiological details.
A client who abuses cocaine tells the nurse that he’s seeking treatment because he’s struggling with withdrawal symptoms. Which assessment question should help the nurse to understand the withdrawal symptoms the client is experiencing?
Explanation
Cocaine withdrawal is primarily characterized by psychological symptoms rather than physical ones. Unlike opioids, which produce prominent somatic signs during withdrawal, cocaine’s effects stem from its action on dopamine and norepinephrine pathways. When use is discontinued, individuals often experience a crash marked by dysphoria, fatigue, and intense cravings. The absence of euphoria leads to a rebound of negative affect, and depression is one of the most consistent and clinically significant features of withdrawal.
Rationale for correct answer
4. Asking about depression and hopelessness directly targets the emotional core of cocaine withdrawal. These symptoms reflect the neurochemical depletion following stimulant cessation and are critical for assessing suicide risk and treatment needs. This question helps the nurse evaluate the severity of withdrawal and the need for psychiatric support.
Rationale for incorrect answers
1. Yawning is a classic sign of opioid withdrawal, not stimulant-related syndromes. Cocaine does not affect the mu-opioid receptors responsible for autonomic symptoms like yawning.
2. Nasal discharge may result from chronic intranasal use, but it is not a withdrawal symptom. It reflects local irritation or damage rather than systemic withdrawal effects.
3. Goose bumps and chills are associated with autonomic instability seen in opioid withdrawal. Cocaine withdrawal lacks these physical manifestations and instead presents with emotional and cognitive symptoms.
Take Home Points
- Cocaine withdrawal is dominated by psychological symptoms such as depression, fatigue, and cravings.
- Physical signs like yawning, chills, and nasal discharge are not typical of stimulant withdrawal.
- Depression during withdrawal may be severe and requires careful assessment for suicidality.
- Differentiating stimulant withdrawal from opioid withdrawal is essential for accurate diagnosis and management.
Practice Exercise 5
Electroconvulsive therapy is most commonly prescribed for:
Explanation
Electroconvulsive therapy (ECT) is a neurostimulation treatment primarily used for severe psychiatric conditions. It induces a controlled seizure under anesthesia, leading to rapid symptom relief in cases resistant to pharmacologic therapy. ECT is especially effective in treatment-resistant depression, catatonia, and severe mood disorders with suicidal ideation. It is considered when rapid response is needed or when medications are contraindicated. Memory impairment is a common side effect, typically transient, and bilateral electrode placement increases efficacy but also cognitive risks.
Rationale for correct answer
3. ECT is most commonly used for major depression, particularly when it is severe, refractory to medications, or accompanied by suicidal ideation or psychotic features. The rapid onset of action and high efficacy make it the preferred intervention in such cases. Suicidality and poor oral intake often necessitate urgent intervention, and ECT provides a safe and effective option when pharmacologic agents are too slow or contraindicated.
Rationale for incorrect answers
1. While ECT can be used in mania, especially when severe or refractory, it is not the most common indication. Pharmacologic stabilization with mood stabilizers and antipsychotics is typically first-line, and ECT is reserved for cases with poor response or life-threatening symptoms.
2. ECT is not routinely used for schizophrenia, particularly paranoid subtype. Antipsychotic medications are the mainstay of treatment. ECT may be considered in catatonic schizophrenia or when there is comorbid affective symptoms, but it is not the primary modality.
4. ECT is rarely indicated for OCD. First-line treatments include SSRIs and cognitive behavioral therapy. ECT may be considered only in extreme, treatment-resistant cases, and even then, its efficacy is limited compared to other conditions.
Take Home Points
- ECT is most effective for severe, treatment-resistant major depressive disorder, especially with psychotic features or suicidality.
- It is considered when rapid symptom relief is needed or when medications are contraindicated.
- ECT is not first-line for schizophrenia, mania, or OCD, though it may be used in select refractory cases.
- Differentiating ECT indications requires understanding of symptom severity, treatment history, and urgency of intervention.
Which of the following best describes the average number of ECT treatments given and the timing of administration?
Explanation
Electroconvulsive therapy (ECT) is administered in a structured series to induce therapeutic seizures under anesthesia. The treatment course typically spans several weeks, with frequency and duration tailored to clinical response. ECT is most effective when delivered consistently, allowing for cumulative neurochemical changes. Seizure threshold, electrode placement, and patient-specific factors influence the regimen. Maintenance ECT may follow acute treatment in chronic or relapsing cases. Cognitive effects are monitored closely, especially with bilateral stimulation.
Rationale for correct answer
2. The standard ECT protocol involves three treatments per week, typically on alternate days, totaling 6 to 12 sessions in the acute phase. This schedule balances efficacy and safety, allowing time for seizure recovery while maintaining therapeutic momentum. Symptom remission often begins after the third or fourth session, with full response by the twelfth. This regimen is supported by clinical guidelines and minimizes cognitive side effects compared to daily administration.
Rationale for incorrect answers
1. Monthly ECT is used in maintenance therapy, not during the acute phase. This schedule is insufficient for initial symptom resolution, as therapeutic effects require repeated stimulation over a short period.
3. Administering ECT three times weekly is correct, but a total of 20 to 30 sessions exceeds the typical acute course. This number may apply in chronic or refractory cases, but not as the average.
4. Daily ECT increases risk of cognitive impairment and is rarely used. It may be considered in life-threatening situations like catatonia or suicidality, but not as a standard regimen.
Take Home Points
- Acute ECT is typically administered every other day, totaling 6 to 12 sessions.
- Maintenance ECT may follow with less frequent treatments to prevent relapse.
- Excessive frequency or duration increases cognitive risks without added benefit.
- ECT protocols vary based on diagnosis, severity, and individual response.
Electroconvulsive therapy is thought to effect a therapeutic response by:
Explanation
Electroconvulsive therapy (ECT) exerts its antidepressant effects through complex neurobiological mechanisms. It induces generalized seizures that trigger neurotransmitter modulation, neuroplasticity, and neuroendocrine changes. ECT enhances monoaminergic transmission, particularly serotonin, norepinephrine, and dopamine, which are implicated in mood regulation. It also promotes hippocampal neurogenesis, increases brain-derived neurotrophic factor (BDNF), and modulates the hypothalamic-pituitary-adrenal axis. These changes contribute to symptom relief in severe depression and other psychiatric disorders.
Rationale for correct answer
3. ECT increases levels of serotonin, norepinephrine, and dopamine, which are critical in mood regulation. This monoamine enhancement is central to its therapeutic efficacy in depression. The induced seizure activity stimulates neurochemical release and receptor sensitivity, leading to improved affective symptoms. These neurotransmitters are deficient in major depressive disorder, and their restoration correlates with clinical improvement.
Rationale for incorrect answers
1. While ECT does activate the central nervous system via seizure induction, this is not the primary mechanism of its therapeutic effect. The benefit arises from downstream neurochemical and neuroplastic changes, not mere stimulation.
2. ECT does not decrease acetylcholine or monoamine oxidase. In fact, monoamine oxidase activity may remain unchanged or decrease slightly, but the therapeutic effect is due to increased monoamine levels, not reduction.
4. Altering sodium metabolism is not a recognized mechanism of ECT. While ionic shifts occur during seizures, they are transient and not linked to the antidepressant response. This choice confuses seizure physiology with therapeutic action.
Take Home Points
- ECT enhances serotonin, norepinephrine, and dopamine levels, improving mood and affective symptoms.
- Its mechanism involves neuroplasticity, neurotrophic factors, and hypothalamic-pituitary-adrenal modulation.
- Seizure induction is a trigger, but therapeutic effects stem from biochemical and structural brain changes.
- ECT is not associated with changes in sodium metabolism or reductions in acetylcholine or monoamine oxidase.
The most common side effects of ECT are:
Explanation
Electroconvulsive therapy (ECT) is a controlled medical procedure that induces a brief seizure under anesthesia to treat severe psychiatric conditions. It is considered safe and effective when administered properly. The most frequent adverse effects are transient cognitive changes, particularly short-term memory loss and confusion. These effects typically resolve within hours to days post-treatment. Modern ECT uses muscle relaxants and anesthesia to prevent physical injury, and cardiac monitoring minimizes cardiovascular risks. Bilateral electrode placement may increase cognitive side effects but also enhances efficacy.
Rationale for correct answer
4. The most common side effects of ECT are temporary memory loss and confusion, especially immediately after treatment. These cognitive effects are usually short-lived and resolve within hours to days. They result from seizure-induced changes in hippocampal and cortical activity. Confusion is more pronounced in older adults and with bilateral electrode placement.
Rationale for incorrect answers
1. Permanent brain damage and irreversible memory loss are rare and not typical. While retrograde amnesia may occur, especially with bilateral ECT, it is usually limited and improves over time. Modern techniques have significantly reduced these risks.
2. Fractures and dislocations were risks in early ECT before muscle relaxants were used. Today, succinylcholine prevents violent motor activity during seizures, making such injuries extremely rare.
3. Cardiac complications like myocardial infarction or arrest are uncommon. ECT is contraindicated in unstable cardiac conditions, and patients are pre-screened and monitored. When used appropriately, ECT poses minimal cardiovascular risk.
Take Home Points
- Temporary memory loss and confusion are the most common side effects of ECT.
- Modern ECT uses anesthesia and muscle relaxants to prevent physical injury.
- Serious complications like brain damage or cardiac arrest are rare with proper screening.
- Cognitive effects are transient and typically resolve within days post-treatment.
Sam has just been admitted to the inpatient psychiatric unit with a diagnosis of major depression. Sam has been treated with antidepressant medication for 6 months without improvement. His psychiatrist has suggested a series of ECT treatments. Sam says to the nurse on admission, “I don’t want to end up like McMurphy on One Flew Over the Cuckoo’s Nest! I’m scared!” The following questions pertain to Sam.
Sam’s priority nursing diagnosis at this time would be:
Explanation
Major depressive disorder is a chronic psychiatric condition marked by persistent low mood, anhedonia, and cognitive changes. When pharmacologic treatment fails, electroconvulsive therapy (ECT) may be considered. ECT is a safe and effective intervention for treatment-resistant depression, especially when rapid symptom relief is needed. Despite its efficacy, misconceptions and stigma often lead to fear and refusal. Education and therapeutic communication are essential to reduce anxiety and promote informed consent.
Rationale for correct answer
1. Sam’s verbalized fear and reference to a negative media portrayal indicate emotional distress stemming from misinformation. His anxiety is directly linked to a lack of accurate understanding about ECT, making this the most appropriate and immediate nursing diagnosis. Addressing this anxiety through education and reassurance is essential before initiating treatment.
Rationale for incorrect answers
2. The risk for injury during ECT is minimal due to pre-procedure muscle relaxants and anesthesia. Sam is not currently undergoing ECT, and there is no evidence of physical instability or seizure-related complications at this time. The priority is psychological, not physical.
3. While Sam’s fear is influenced by media, the diagnosis of deficient knowledge alone does not capture the emotional component of his distress. Anxiety is the dominant issue, and focusing solely on knowledge deficit misses the urgency of his fear response.
4. There is no indication that Sam is experiencing cognitive disturbances or altered thought processes. He is expressing coherent concerns and referencing specific cultural imagery, which suggests intact cognition. This diagnosis would be premature and inaccurate.
Take Home Points
- Anxiety related to ECT is common and often stems from misinformation and stigma.
- Priority nursing diagnoses must address the most immediate and distressing patient need.
- ECT is a safe and effective treatment for refractory depression when properly explained and consented.
- Differentiating between emotional, cognitive, and physical risks is essential in psychiatric nursing assessment.
Which of the following statements would be most appropriate by the nurse in response to Sam’s expression of concern?
Explanation
Therapeutic communication is a foundational nursing skill used to build trust, validate emotions, and promote understanding. In psychiatric care, especially when addressing fear or stigma around treatments like ECT, nurses must respond with empathy, clarity, and reassurance. The goal is to reduce anxiety and foster informed consent through education and emotional support.
Rationale for correct answer
3. This response acknowledges Sam’s fear, validates his emotional state, and introduces a plan for education and discussion. It reflects therapeutic communication principles by combining empathy with a commitment to provide accurate information, which is essential when confronting stigma and misinformation about ECT.
Rationale for incorrect answers
1. Making guarantees is inappropriate and undermines the complexity of medical procedures. It dismisses Sam’s concerns and may create false expectations, which can erode trust if complications arise.
2. This statement is dismissive and paternalistic. It fails to validate Sam’s emotions and implies blind trust in authority rather than encouraging informed understanding and shared decision-making.
4. While emotionally supportive, this response lacks direction and does not address the underlying fear or knowledge deficit. It may comfort temporarily but does not empower Sam with the information he needs to make an informed choice.
Take Home Points
- Therapeutic communication combines empathy with education to reduce fear and promote informed decisions.
- Avoid dismissive or overly reassuring statements that lack factual support or emotional validation.
- ECT-related anxiety often stems from misinformation; nurses must address both emotional and cognitive needs.
- Effective psychiatric nursing requires balancing emotional support with clear, accurate information about treatment options.
The priority nursing intervention before starting Sam’s therapy is to:
Explanation
Electroconvulsive therapy (ECT) is a medical procedure used to treat severe psychiatric conditions such as treatment-resistant depression. It involves inducing a controlled seizure under general anesthesia and muscle relaxation. Before initiating ECT, it is essential to ensure informed consent, as the procedure carries risks including transient memory loss, confusion, and anesthesia-related complications. Consent must be obtained voluntarily after thorough education about benefits, risks, and alternatives.
Rationale for correct answer
4. The most critical nursing intervention before ECT is verifying that the informed consent form has been signed. This ensures legal and ethical compliance and confirms that the patient understands the procedure, its risks, and benefits. Without consent, the procedure cannot proceed, regardless of clinical urgency.
Rationale for incorrect answers
1. While recording vital signs is important for baseline assessment, it is not the priority intervention. Vital signs are routinely taken before many procedures but do not address the legal and ethical prerequisites of ECT.
2. Having the patient void is a standard pre-procedure step to prevent incontinence during anesthesia, but it is secondary to confirming informed consent. It supports comfort and safety but does not impact the decision to proceed.
3. Succinylcholine is a muscle relaxant administered immediately before ECT to prevent injury during the induced seizure. However, it is given only after consent is confirmed and anesthesia is initiated. Administering it without consent would be a serious violation.
Take Home Points
- Informed consent is the legal and ethical cornerstone of initiating ECT.
- Pre-procedure nursing care includes education, emotional support, and procedural preparation.
- Succinylcholine is used to prevent musculoskeletal injury during ECT-induced seizures.
- Consent must be obtained before any pharmacologic or procedural steps are taken.
Atropine sulfate is administered to Sam for what purpose?
Explanation
Atropine sulfate is an anticholinergic agent used in various clinical settings, including preoperative preparation for procedures like electroconvulsive therapy (ECT). Its primary role is to inhibit parasympathetic activity, thereby reducing salivary and bronchial secretions. This minimizes the risk of aspiration and enhances airway safety during anesthesia. It also helps prevent bradycardia by blocking vagal stimulation, which can occur during ECT.
Rationale for correct answer
2. Atropine is administered before ECT to reduce secretions, particularly salivary and respiratory tract fluids. This is crucial for preventing aspiration and maintaining a clear airway during anesthesia and seizure induction. Its anticholinergic properties inhibit muscarinic receptors, decreasing glandular output.
Rationale for incorrect answers
1. Atropine does not have anxiolytic properties. It does not act on GABAergic or serotonergic pathways involved in anxiety modulation. Benzodiazepines or other sedatives are used for anxiety, not anticholinergics.
3. Muscle relaxation during ECT is achieved using agents like succinylcholine, not atropine. Atropine does not affect nicotinic receptors at the neuromuscular junction and thus has no role in skeletal muscle relaxation.
4. Atropine is not an anesthetic. It does not induce unconsciousness or analgesia. Short-acting anesthetics like methohexital or thiopental are used in ECT to induce sedation before seizure induction.
Take Home Points
- Atropine sulfate reduces secretions and prevents vagal-induced bradycardia during ECT.
- It is not used for anxiety relief, muscle relaxation, or anesthesia induction.
- Succinylcholine is the muscle relaxant of choice in ECT procedures.
- Anxiolytics and anesthetics are separate pharmacologic classes from anticholinergics like atropine.
Succinylcholine is administered to Sam for what purpose?
Explanation
Succinylcholine is a depolarizing neuromuscular blocker used during procedures like electroconvulsive therapy (ECT) to induce rapid and short-term muscle relaxation. It mimics acetylcholine at the neuromuscular junction, causing sustained depolarization and temporary paralysis. This prevents physical injury during seizure induction while preserving the therapeutic effect. Its onset is within 30–60 seconds and duration is typically under 5 minutes, making it ideal for brief procedures like ECT.
Rationale for correct answer
3. Succinylcholine is administered to produce muscle relaxation during ECT. It binds to nicotinic receptors at the neuromuscular junction, causing depolarization followed by paralysis. This prevents violent motor convulsions while allowing the seizure to occur in the brain, minimizing risk of musculoskeletal injury.
Rationale for incorrect answers
1. Succinylcholine does not alleviate anxiety. It has no central nervous system activity and does not affect emotional or psychological states. Anxiolytics like benzodiazepines are used for anxiety management.
2. It does not reduce secretions. Anticholinergic agents like atropine are used to decrease salivary and respiratory secretions prior to ECT. Succinylcholine has no effect on glandular output.
4. Succinylcholine is not an anesthetic. It does not induce unconsciousness or analgesia. Anesthesia must be administered separately before succinylcholine to prevent awareness during paralysis.
Take Home Points
- Succinylcholine is used in ECT to induce rapid, short-term muscle paralysis and prevent injury.
- It acts at the neuromuscular junction by mimicking acetylcholine and causing sustained depolarization.
- It does not affect consciousness, anxiety, or secretions—other drugs are needed for those roles.
- Always administer anesthesia before succinylcholine to avoid awake paralysis and psychological distress.
Comprehensive Questions
A client whose husband died 6 months ago is diagnosed with major depressive disorder. She says to the nurse, “I start feeling angry that Harold died and left me all alone; he should have stopped smoking years ago! But then I start feeling guilty for feeling that way.” What is an appropriate response by the nurse?
Explanation
Grief response is a multifaceted emotional and psychological process that follows significant loss. It includes stages such as denial, anger, bargaining, depression, and acceptance. In individuals with major depressive disorder, grief may be complicated by persistent sadness, guilt, and hopelessness. Recognizing that anger and guilt are normal reactions within the grieving process helps validate the client’s experience and supports emotional healing.
Rationale for correct answer
3. This response normalizes the client’s emotional experience and provides validation without judgment. It reflects an understanding of the grief process and helps the client feel supported in expressing complex emotions like anger and guilt, which are common in bereavement and do not indicate pathology.
Rationale for incorrect answers
1. This statement reinforces blame, which can intensify guilt and hinder emotional processing. It lacks therapeutic value and may escalate the client’s distress by focusing on preventability rather than acceptance.
2. While empathetic, this response is vague and does not provide the client with insight or reassurance about the normalcy of her feelings. It misses the opportunity to educate and support emotional integration.
4. This response encourages avoidance of current emotions by redirecting focus to positive memories. It may invalidate the client’s present feelings and discourage open expression of grief-related anger and guilt.
Take Home Points
- Grief involves a range of emotions including anger, guilt, and sadness, which are normal and should be validated.
- Therapeutic communication in grief care must normalize emotional responses and support expression.
- Avoid statements that reinforce blame or redirect away from the client’s current emotional state.
- Major depressive disorder can complicate grief, requiring sensitive and structured emotional support.
A newly admitted depressed client isolates herself in her room and just sits and stares into space. How best might the nurse begin an initial therapeutic relationship with this client?
Explanation
Depression with psychomotor retardation often presents as withdrawal, slowed movements, and diminished verbal engagement. Clients may appear disengaged or nonresponsive, but this reflects internal suffering rather than defiance. Establishing a therapeutic alliance requires consistent presence, emotional attunement, and non-demanding interaction. Early interventions should prioritize trust-building over verbal or social engagement, especially when the client is isolating.
Rationale for correct answer
2. Making short, frequent visits and sitting quietly communicates presence without pressure. This approach respects the client’s current emotional state and initiates connection through nonverbal support. It lays the foundation for trust and future engagement by showing reliability and empathy without demanding interaction.
Rationale for incorrect answers
1. Inviting the client to group therapy prematurely may feel overwhelming and intrusive. It assumes readiness for social interaction, which contradicts her current withdrawn behavior and may increase anxiety or resistance.
3. Introducing her to other clients is premature and socially demanding. It bypasses the essential first step of building a one-on-one therapeutic relationship and may reinforce feelings of isolation if she declines.
4. Exploring stressors requires verbal engagement and insight, which the client is not currently demonstrating. This intervention is more appropriate once rapport is established and the client is emotionally ready to reflect.
Take Home Points
- Psychomotor retardation in depression requires gentle, nonverbal therapeutic engagement.
- Trust-building precedes verbal or social interventions in severely withdrawn clients.
- Avoid overwhelming clients with premature group or social activities.
- Consistent, quiet presence is a powerful tool in initiating therapeutic relationships.
A client has just been admitted to the psychiatric unit with a diagnosis of major depressive disorder. Which of the following behavioral manifestations might the nurse expect to assess? Select all that apply.
Explanation
Major depressive disorder is a mood disorder characterized by persistent sadness, loss of interest, and neurovegetative changes. It affects emotional, cognitive, and physical functioning. Common behavioral signs include psychomotor retardation, poor posture, social withdrawal, and appetite disturbances. Clients often experience despair, hopelessness, and slowed movements. Somatic symptoms such as anorexia and fatigue are frequent, while psychotic features like delusions are less common unless the depression is severe.
Rationale for correct answers
1. A slumped posture reflects psychomotor retardation, a hallmark of major depression. It indicates diminished energy, slowed movement, and emotional withdrawal, often seen in severely depressed clients.
3. Feelings of despair are central to the emotional experience of depression. They manifest as hopelessness, helplessness, and a sense of futility, contributing to suicidal ideation and impaired functioning.
5. Anorexia is a common neurovegetative symptom in depression. It results from reduced appetite and interest in food, often leading to weight loss and nutritional deficiencies.
Rationale for incorrect answers
2. Delusional thinking is associated with psychosis, not typical major depressive disorder. It may occur in severe cases with psychotic features, but is not a standard behavioral manifestation.
4. Clients with depression often feel worse in the morning due to diurnal variation. Improvement later in the day is more typical, making this statement inconsistent with common depressive patterns.
Take Home Points
- Major depressive disorder commonly presents with psychomotor retardation, hopelessness, and appetite changes.
- Delusions are not typical unless depression is severe with psychotic features.
- Diurnal variation in depression often causes worse symptoms in the morning.
- Behavioral assessment should focus on posture, affect, and neurovegetative signs.
A client recently diagnosed with depression tells a nurse that she is 2 months pregnant and is reluctant to take an antidepressant medication. The client asks what other treatment options are available. Which type of therapy should a nurse recommend as an alternate treatment for depression?
Explanation
Cognitive behavioral therapy (CBT) is a structured, evidence-based psychotherapeutic approach that targets maladaptive thoughts, emotional distress, and behavioral patterns. It is especially effective in treating depression, including during pregnancy, where pharmacologic options may be limited due to fetal safety concerns. CBT helps clients identify and reframe negative thought processes, develop coping strategies, and improve mood through behavioral activation and cognitive restructuring.
Rationale for correct answer
4. CBT is the most widely recommended nonpharmacologic treatment for depression in pregnancy. It is safe, effective, and adaptable to individual needs. CBT addresses distorted thinking and promotes behavioral engagement, making it ideal for clients who are reluctant to use medications during gestation.
Rationale for incorrect answers
1. Client-centered therapy emphasizes unconditional positive regard and empathy but lacks the structured cognitive and behavioral techniques necessary for targeted depression treatment. It may support emotional expression but is less effective in modifying depressive thought patterns.
2. Gestalt therapy focuses on awareness and present-moment experience, often using experiential techniques. It is not first-line for depression and lacks the empirical support and structured framework that CBT provides, especially in perinatal populations.
3. Therapeutic touch therapy is based on energy field manipulation and lacks robust scientific validation. It is not considered an evidence-based intervention for depression and should not be recommended as a primary treatment modality.
Take Home Points
- CBT is the most effective and evidence-based nonpharmacologic therapy for depression during pregnancy.
- It targets cognitive distortions and promotes behavioral activation, improving mood and functioning.
- Other therapies may offer emotional support but lack the structured approach and empirical backing of CBT.
- Safety and efficacy are critical when selecting treatments for pregnant clients with mood disorders.
Which client statement is evidence of the etiology of major depressive disorder from a genetic perspective?
Explanation
Major depressive disorder (MDD) has a multifactorial etiology involving genetic, neurobiological, and environmental components. Family and twin studies show that individuals with a first-degree relative diagnosed with a mood disorder have a significantly increased risk of developing MDD. Genetic predisposition is linked to variations in genes regulating serotonin transport, neuroplasticity, and stress response. Heritability estimates range from 30–50%, with higher risks observed in families with recurrent or early-onset mood disorders.
Rationale for correct answer
1. A family history of bipolar affective disorder reflects a genetic vulnerability to mood disorders, including MDD. Bipolar disorder and MDD share overlapping genetic markers, and having a first-degree relative with either condition increases the likelihood of developing depressive symptoms due to inherited neurobiological traits.
Rationale for incorrect answers
2. This statement reflects current mood status and safety assessment, not etiology. It provides clinical information about emotional state and risk but does not indicate any underlying genetic or familial predisposition.
3. This reflects a psychosocial factor—childhood trauma—which is an environmental contributor to depression. While significant, it does not represent genetic etiology and instead points to experiential influences on emotional development.
4. Feelings of worthlessness are a symptom of depression, not a cause. This statement illustrates cognitive distortions typical in MDD but does not provide insight into the origin or contributing factors of the disorder.
Take Home Points
- Genetic predisposition plays a significant role in the development of major depressive disorder.
- Family history of mood disorders increases risk due to shared neurobiological traits.
- Environmental factors like trauma also contribute but are distinct from genetic etiology.
- Symptoms of depression reflect the disorder’s manifestation, not its underlying cause.
A depressed client states that her daughter uses amphetamines, then asks the nurse, “What will happen when my daughter can’t get them and goes into withdrawal from them?” Which response by the nurse would be helpful information for the client?
Explanation
Amphetamine withdrawal occurs when chronic use of stimulant drugs like amphetamine or methamphetamine is abruptly discontinued. The body, having adapted to elevated dopamine and norepinephrine levels, experiences a neurochemical crash. This leads to symptoms such as fatigue, hypersomnia, depression, and anhedonia. The withdrawal process is largely psychological, with physical symptoms being mild. While cravings and mood instability are common, seizures and severe neurological complications are rare unless there is co-occurring substance use or underlying pathology.
Rationale for correct answer
1. Fatigue and depression are hallmark symptoms of amphetamine withdrawal. The sudden drop in stimulant-induced neurotransmitter activity leads to lethargy, hypersomnia, and low mood. These symptoms reflect the body’s attempt to recalibrate after prolonged stimulation and are expected in most cases of withdrawal.
Rationale for incorrect answers
2. Mild nausea is not a defining feature of amphetamine withdrawal. This response minimizes the psychological impact and may mislead the client into underestimating the seriousness of mood-related symptoms like depression and anhedonia.
3. While agitation can occur, it is not the most common or defining symptom. Aggression is more typical during intoxication or in cases of polysubstance withdrawal. This response may unnecessarily alarm the client and misrepresent the usual withdrawal profile.
4. Seizures are not a high-risk feature of amphetamine withdrawal. Unlike alcohol or benzodiazepines, stimulants do not typically cause withdrawal seizures unless there is concurrent use of other substances or predisposing neurological conditions.
Take Home Points
- Amphetamine withdrawal commonly causes fatigue, hypersomnia, and depressed mood due to neurotransmitter depletion.
- Severe neurological symptoms like seizures are rare unless other substances are involved.
- Agitation may occur but is less common than emotional and energy-related symptoms.
- Accurate education helps families anticipate and support withdrawal safely and effectively.
Which nursing diagnosis would be most appropriate for the client who has undergone the full course of electroconvulsive therapy (ECT)?
Explanation
Electroconvulsive therapy (ECT) is a highly effective treatment for severe major depressive disorder, especially when pharmacologic options fail. While ECT can rapidly alleviate symptoms, it is associated with transient memory loss, particularly around the time of treatment. Post-ECT care focuses on educating clients about expected cognitive changes, monitoring recovery, and reinforcing understanding of the procedure’s effects. Most memory deficits resolve over time, but confusion or concern may persist without proper education.
Rationale for correct answer
1. After completing ECT, clients often experience memory loss, especially short-term or retrograde amnesia. If the client lacks understanding of this expected side effect, the most appropriate nursing diagnosis is deficient knowledge. Education helps reduce anxiety and promotes realistic expectations about recovery and cognitive function.
Rationale for incorrect answers
2. Noncompliance implies refusal or failure to follow treatment, which is not applicable post-ECT if the client has completed the full course. The issue is not adherence but understanding of residual effects.
3. Disturbed thought processes suggest cognitive disorganization, hallucinations, or delusions, which are not typical post-ECT. Mild confusion may occur transiently, but it does not meet the criteria for this diagnosis unless severe or persistent.
4. Fear related to the unknown is relevant before ECT, when clients may be anxious about the procedure. After completion, the focus shifts to recovery and education, not anticipatory fear.
Take Home Points
- Memory loss is a common and expected side effect of ECT, requiring post-treatment education.
- Noncompliance is not applicable once the treatment course is completed.
- Thought disturbances are not typical post-ECT unless other psychiatric symptoms persist.
- Pre-treatment fear transitions to post-treatment knowledge needs in nursing care planning.
Which nursing diagnosis supports the psychoanalytic theory of development of major depressive disorder?
Explanation
Psychoanalytic theory posits that unresolved unconscious conflicts, often rooted in early childhood experiences, contribute to the development of major depressive disorder. According to this model, depression may result from internalized anger turned inward, typically stemming from loss, abandonment, or unmet emotional needs. The theory emphasizes the role of self-directed aggression, guilt, and repressed emotions in shaping depressive symptoms.
Rationale for correct answer
1. This diagnosis reflects the psychoanalytic concept of self-directed anger, where the client isolates due to unconscious hostility turned inward. Freud’s model suggests that unresolved grief or loss leads to internalized rage, manifesting as withdrawal and depressive symptoms. This aligns directly with psychoanalytic etiology.
Rationale for incorrect answers
2. Learned helplessness is a cognitive-behavioral construct, not psychoanalytic. It describes a belief system formed through repeated failures, leading to passivity and low self-worth, but does not involve unconscious conflict or repressed anger.
3. Neurochemical imbalances are central to the biological model of depression, focusing on serotonin, norepinephrine, and dopamine dysregulation. This explanation is physiological, not psychodynamic, and does not involve unconscious processes.
4. Nutritional deficits relate to somatic symptoms of depression and are addressed in physical care planning. They do not reflect the psychological or unconscious mechanisms emphasized in psychoanalytic theory.
Take Home Points
- Psychoanalytic theory attributes depression to unconscious conflicts and internalized anger.
- Self-directed aggression and isolation are key manifestations of psychodynamic depression.
- Learned helplessness and neurochemical imbalance reflect cognitive and biological models, respectively.
- Somatic symptoms like poor nutrition are consequences, not etiologic indicators, of depression.
Which of the following conditions is considered to be the only absolute contraindication for ECT?
Explanation
Electroconvulsive therapy (ECT) induces a controlled seizure to treat severe psychiatric conditions such as major depression, catatonia, and psychosis. The procedure causes transient increases in cerebral blood flow and metabolic demand, which can elevate intracranial pressure. While many medical conditions are considered relative contraindications, increased intracranial pressure (ICP) remains the only absolute contraindication due to the risk of cerebral herniation and irreversible brain damage.
Rationale for correct answer
1. Elevated intracranial pressure is the only absolute contraindication for ECT. The seizure-induced surge in cerebral perfusion and oxygen demand can dangerously exacerbate ICP, risking brainstem compression and herniation. This makes ECT unsafe until ICP is stabilized or resolved.
Rationale for incorrect answers
2. A recent myocardial infarction is a relative contraindication. ECT causes transient sympathetic stimulation, which may strain cardiac function, but with proper monitoring and stabilization, it can be safely administered in select cases.
3. Severe hypertension increases cardiovascular risk during ECT but is not absolute. Pre-treatment antihypertensive management and intra-procedural monitoring allow safe administration in many hypertensive clients.
4. Congestive heart failure poses hemodynamic concerns due to fluid overload and reduced cardiac output. However, it is a relative contraindication, and ECT may still be used with cardiac clearance and close monitoring.
Take Home Points
- Increased intracranial pressure is the only absolute contraindication for ECT due to risk of herniation.
- Cardiac conditions like MI and CHF are relative contraindications requiring individualized risk assessment.
- ECT elevates cerebral blood flow and metabolic demand, making ICP management critical.
- Most medical conditions can be managed to allow safe ECT with proper precautions.
The nurse is interviewing a client admitted to an in-patient psychiatric unit with major depressive disorder. Which is the primary goal in the assessment phase of the nursing process for this client?
Explanation
Nursing assessment is the foundational phase of the nursing process, focused on gathering comprehensive data about the client’s physical, emotional, cognitive, and behavioral status. In clients with major depressive disorder, this includes evaluating mood, affect, sleep patterns, appetite, energy levels, and suicidal ideation. The goal is to collect and organize subjective and objective information to guide accurate nursing diagnoses and individualized care planning.
Rationale for correct answer
3. The primary goal during assessment is to collect and organize relevant data. This includes health history, current symptoms, psychosocial context, and risk factors. Accurate data collection enables the nurse to formulate appropriate nursing diagnoses and interventions tailored to the client’s depressive presentation.
Rationale for incorrect answers
1. Building rapport is essential but not the primary goal of the assessment phase. It supports data collection and therapeutic engagement, but the phase itself is defined by systematic information gathering.
2. Identifying goals and outcomes occurs in the planning phase, after assessment and diagnosis. It involves setting measurable objectives based on the client’s needs and expected responses to interventions.
4. Validating the medical diagnosis is the role of the physician or psychiatrist. Nurses focus on nursing diagnoses, which are based on client responses to health conditions, not the confirmation of medical pathology.
Take Home Points
- The assessment phase centers on collecting and organizing data to guide nursing care.
- Building rapport supports assessment but is not its primary objective.
- Goal setting and outcome identification occur in the planning phase.
- Nurses do not validate medical diagnoses; they identify nursing responses to health conditions.
Which statement describes a major difference between a client diagnosed with major depressive disorder and a client diagnosed with dysthymic disorder?
Explanation
Persistent depressive disorder (formerly dysthymia) is a chronic mood disturbance characterized by a depressed mood lasting at least two years in adults. Symptoms are less severe than major depressive disorder but more enduring. Individuals often experience low energy, poor concentration, and feelings of hopelessness. The condition may coexist with major depressive episodes, known as double depression. Diagnosis requires a depressed mood most of the day, more days than not, for at least two years, along with two or more additional symptoms such as appetite changes, sleep disturbances, or low self-esteem. Duration, severity, and functional impact distinguish it from major depressive disorder.
Rationale for correct answer
4. The defining criterion for persistent depressive disorder is a depressed mood lasting at least two years in adults. This chronicity differentiates it from major depressive disorder, which requires a minimum of two weeks of symptoms. The two-year duration is essential for diagnosis and reflects the enduring nature of the disorder.
Rationale for incorrect answers
1. The risk of suicide is generally higher in major depressive disorder due to the severity of symptoms, including suicidal ideation and psychomotor retardation. Dysthymia carries a risk, but it is typically lower unless compounded by a major depressive episode.
2. Psychotic features such as delusions or hallucinations are associated with severe major depressive episodes, not dysthymia. Persistent depressive disorder does not include psychotic symptoms in its diagnostic criteria.
3. While guilt may be present in both disorders, excessive guilt is more characteristic of major depressive disorder. In dysthymia, symptoms are milder and chronic, and guilt is not a defining feature.
Take Home Points
- Persistent depressive disorder requires a minimum of two years of depressed mood and associated symptoms.
- Major depressive disorder is more severe and episodic, often with psychotic features and higher suicide risk.
- Dysthymia may coexist with major depressive episodes, forming a condition known as double depression.
- Differentiating based on duration and symptom severity is critical for accurate diagnosis and treatment planning.
Which client is at highest risk for the diagnosis of major depressive disorder?
Explanation
Major depressive disorder risk is influenced by age, gender, and marital status. Older adults, especially women, face increased vulnerability due to biological changes, social isolation, and cumulative stressors.
Major depressive disorder is more prevalent in older women, particularly those who are single, widowed, or divorced. Risk increases with age due to declining physical health, reduced social support, and hormonal changes. Women have higher lifetime prevalence and report more severe symptoms.
Rationale for correct answer
2. Older single women are at elevated risk due to age-related vulnerability, lack of spousal support, and higher prevalence of chronic illness. Social isolation and hormonal factors compound the risk for depression.
Rationale for incorrect answers
1. Younger married women have protective factors including spousal support and lower age-related risk. While women are generally at higher risk, marriage and youth reduce susceptibility.
3. Single men have lower prevalence compared to women. Though being single increases risk, men report fewer depressive symptoms and are less likely to seek help, affecting diagnosis rates.
4. Older married men have the lowest risk among the options. Marriage offers emotional support, and men generally have lower depression rates than women, especially in older age groups.
Take Home Points
- Older age and single marital status increase risk for major depressive disorder, especially in women.
- Women have higher lifetime prevalence and more severe symptom profiles than men.
- Social isolation and chronic illness contribute significantly to depression in older adults.
- Marital status is a protective factor, particularly in elderly populations.
Which symptom is an example of an affective alteration exhibited by clients diagnosed with severe depression?
Explanation
Severe depression is a mood disorder characterized by persistent sadness, loss of interest, and impaired functioning. It affects emotional expression, cognition, and physical behavior. Affective symptoms reflect changes in mood and emotional tone. These include anhedonia, apathy, hopelessness, and feelings of worthlessness. Neurobiologically, dysregulation of serotonin, norepinephrine, and dopamine pathways contributes to affective flattening and emotional blunting. These symptoms are central to diagnosis and often precede cognitive or somatic manifestations.
Rationale for correct answer
1. Apathy reflects a diminished emotional responsiveness and lack of motivation, which are hallmark affective symptoms in major depressive disorder. It indicates a blunting of emotional tone and loss of interest in previously valued activities, consistent with affective flattening.
Rationale for incorrect answers
2. Delusion is a psychotic symptom, not affective. Somatic delusions involve false beliefs about bodily functions or health and are categorized under thought content disturbances, not mood alterations.
3. Insomnia is a physiological symptom. Difficulty falling asleep is a vegetative sign of depression, linked to circadian rhythm disruption and hyperarousal, but it does not reflect affective tone.
4. Isolation is behavioral. Social withdrawal results from decreased energy and motivation but is considered a behavioral response to affective and cognitive symptoms, not an affective symptom itself.
Take Home Points
- Affective symptoms in depression include apathy, anhedonia, and hopelessness, reflecting emotional blunting.
- Somatic delusions are psychotic features and not part of affective symptomatology.
- Sleep disturbances are vegetative signs and reflect physiological dysregulation in depression.
- Social isolation is a behavioral consequence, not a direct affective alteration.
Which is the key to understanding if a child or adolescent is experiencing an underlying depressive disorder?
Explanation
Depressive disorder in youth presents differently than in adults, often with behavioral and somatic complaints rather than verbalized sadness. Diagnostic criteria emphasize a persistent change in functioning. Irritability, withdrawal, and academic decline may be present, but diagnosis hinges on sustained shifts in mood or behavior. The DSM-5 outlines that symptoms must last at least two weeks and cause significant impairment. Early recognition is critical, as untreated depression in youth increases risk for substance use, academic failure, and suicide.
Rationale for correct answer
3. A sustained behavioral change over a 2-week period meets the DSM-5 threshold for diagnosing depressive disorders in children and adolescents. This duration reflects a persistent alteration in mood, energy, or functioning, distinguishing clinical depression from transient emotional states.
Rationale for incorrect answers
1. Irritability alone is nonspecific and may reflect normal developmental defiance, oppositional behavior, or situational stress. Without duration or associated symptoms, it cannot confirm depression.
2. Uninterest in school may stem from academic challenges, peer conflict, or boredom. While it can be a symptom of depression, it lacks diagnostic specificity without broader behavioral context.
4. Insecurity in social settings is common in adolescence due to developmental changes in self-concept and peer dynamics. It may reflect social anxiety or shyness, not necessarily depression.
Take Home Points
- Depression in youth requires a persistent change in mood or behavior lasting at least two weeks.
- Irritability is common but not diagnostic without other sustained symptoms.
- School disengagement may signal depression but must be evaluated in context.
- Social discomfort alone does not indicate depressive disorder; broader patterns must be assessed.
A client admitted with major depressive disorder has a nursing diagnosis of ineffective sleep pattern related to aches and pains. Which is an appropriate short-term outcome for this client?
Explanation
Sleep disturbance in depression is a core symptom, often presenting as insomnia or hypersomnia. In clients with major depressive disorder, sleep disruption is frequently exacerbated by somatic pain, which interferes with sleep initiation and maintenance. The goal of nursing care is to restore restorative sleep patterns through behavioral, pharmacologic, and environmental interventions. Sleep quality directly influences mood regulation, cognitive function, and pain perception. Short-term goals must be measurable, time-bound, and focused on functional improvement.
Rationale for correct answer
3. A goal of sleeping 6 to 8 hours by day 5 is measurable and time-specific, aligning with short-term outcome criteria. It reflects a realistic target for sleep restoration in clients with depression and pain, allowing evaluation of nursing interventions and adjustment of care plans.
Rationale for incorrect answers
1. Rested is a subjective term and lacks measurable criteria. While feeling rested is desirable, it cannot be objectively evaluated or tracked over time, making it unsuitable for short-term outcome documentation.
2. Pain rating addresses the physical symptom but not the sleep pattern directly. Although pain management is essential, this outcome does not reflect improvement in sleep behavior, which is the focus of the nursing diagnosis.
4. Steady sleep pattern is vague and lacks a defined timeframe or quantifiable metric. Without specifying duration or quality, it cannot be reliably assessed or used to guide care.
Take Home Points
- Sleep goals in depression should be specific, measurable, and time-bound to evaluate progress.
- Pain management supports sleep but must be linked to sleep outcomes for relevance.
- Subjective feelings like “rested” are not reliable indicators for nursing outcomes.
- Vague terms like “steady” lack the precision needed for short-term goal setting.
A newly admitted client diagnosed with major depressive disorder isolates self in room and stares out the window. Which nursing intervention would be the most appropriate to implement initially, when establishing a nurse-client relationship?
Explanation
Major depressive disorder is a mood disorder marked by persistent sadness, anhedonia, and impaired functioning. Clients often exhibit psychomotor retardation, social withdrawal, and diminished verbal engagement, making initial therapeutic connection difficult. Early nursing goals prioritize presence, safety, and nonverbal rapport over verbal processing or group participation.
Rationale for correct answer
1. Establishing a therapeutic relationship with a client in acute depression requires nonverbal presence and emotional availability. Sitting quietly and offering self respects the client's limited energy and avoids pressure to engage. This intervention aligns with early-stage depression care, where trust-building precedes verbal interaction. It also addresses physiological needs by reducing isolation and promoting safety.
Rationale for incorrect answers
2. Group therapy requires motivation and cognitive engagement, which are often impaired in early stages of major depression. Introducing structured activities prematurely may overwhelm the client and hinder rapport.
3. Social introductions demand interpersonal energy and initiative, which are typically absent in clients with severe depression. Forcing socialization may increase anxiety and reinforce withdrawal.
4. Identifying stressors involves introspection, which is not feasible when the client is disengaged and nonverbal. This step is more appropriate after trust and communication have been established.
Take Home Points
- Initial nursing interventions for major depressive disorder should prioritize presence and nonverbal support over verbal engagement.
- Clients with psychomotor retardation and social withdrawal benefit from quiet companionship before structured therapy.
- Group therapy and stressor identification are secondary interventions once rapport and communication are established.
- Differentiating depression from conditions like schizophrenia or catatonia requires careful assessment of affect, engagement, and thought content.
Which of the following medications may be administered before electroconvulsive therapy? Select all that apply.
Explanation
Electroconvulsive therapy (ECT) is a procedure that induces a controlled seizure to treat severe psychiatric conditions. Prior to ECT, specific medications are administered to reduce cardiac complications, facilitate anesthesia, and prevent muscle injury. These agents are chosen to optimize safety and seizure quality without interfering with the therapeutic mechanism.
Rationale for correct answers
1. Glycopyrrolate is an anticholinergic used pre-ECT to reduce salivary secretions and prevent bradycardia during the procedure. Its peripheral action minimizes central side effects, making it ideal for ECT preparation.
2. Thiopental sodium is a barbiturate anesthetic that induces rapid unconsciousness before ECT. It has a short duration of action and minimal impact on seizure threshold, making it suitable for brief procedures.
3. Succinylcholine is a neuromuscular blocker administered to prevent musculoskeletal injury during the seizure. It produces short-term paralysis, reducing the risk of fractures or dislocations during convulsions.
Rationale for incorrect answers
4. Lorazepam is a benzodiazepine that raises the seizure threshold and may blunt the therapeutic seizure. Its sedative properties interfere with ECT efficacy, making it contraindicated before the procedure.
5. Divalproex sodium is an anticonvulsant that suppresses seizure activity. Administering it before ECT would counteract the intended seizure induction, reducing treatment effectiveness.
Take Home Points
- Pre-ECT medications include anticholinergics, anesthetics, and muscle relaxants to optimize safety and seizure quality.
- Benzodiazepines and anticonvulsants are avoided as they interfere with seizure induction.
- Glycopyrrolate prevents bradycardia and excessive secretions during ECT.
- Succinylcholine minimizes physical injury by inducing short-term paralysis during the seizure.
A client is admitted to an in-patient psychiatric unit with a diagnosis of major depressive disorder. Which of the following data would the nurse expect to assess? Select all that apply.
Explanation
Major depressive disorder is a psychiatric illness marked by persistent low mood or loss of interest, accompanied by somatic, cognitive, and behavioral symptoms that impair daily functioning and last at least two weeks.
Major depressive disorder presents with diminished interest in activities, significant weight changes, sleep disturbances, and psychomotor changes. Symptoms must be present nearly daily and cause functional impairment. Appetite and sleep may increase or decrease.
Rationale for correct answers
1. Loss of interest and anhedonia are core symptoms of depression. They reflect a diminished ability to experience pleasure and are required for diagnosis when present nearly daily for two weeks.
2. A weight change of more than 5% in one month indicates appetite dysregulation, a vegetative symptom of depression. It may manifest as weight loss or gain, independent of intentional dieting.
4. Psychomotor retardation or agitation is a behavioral marker of depression. These changes must be observable by others and reflect slowed movements or restlessness, not just subjective feelings.
5. Insomnia or hypersomnia are common neurovegetative symptoms. Sleep disturbances occur nearly daily and may alternate between difficulty sleeping and excessive sleep, contributing to fatigue and impaired functioning.
Rationale for incorrect answer
3. Fluctuating energy levels suggest bipolarity, not unipolar depression. Increased energy is more consistent with manic or hypomanic episodes, which are excluded in major depressive disorder diagnosis.
Take Home Points
- Major depressive disorder requires five or more symptoms, including either depressed mood or anhedonia, lasting at least two weeks.
- Psychomotor changes and sleep disturbances are observable and diagnostically significant.
- Appetite and weight changes must be unintentional and clinically relevant.
- Fluctuating energy levels may indicate bipolar spectrum disorders and should prompt differential evaluation.
A client diagnosed with major depressive disorder is being considered for electroconvulsive therapy (ECT). Which client teaching should the nurse prioritize?
Explanation
Electroconvulsive therapy (ECT) is a neuromodulation treatment used for severe, treatment-resistant major depressive disorder. It involves brief electrical stimulation of the brain under anesthesia to induce a controlled seizure. The most common adverse effect is short-term memory loss, which may persist for weeks. ECT is contraindicated in patients with recent myocardial infarction or unstable cardiac conditions due to transient increases in intracranial pressure and cardiovascular strain. Despite its risks, ECT remains one of the most effective interventions for severe depression, especially with psychotic features or suicidality.
Rationale for correct answer
3. Memory loss is the most frequent and expected side effect of ECT. Clients and families must be informed of transient anterograde and retrograde memory deficits.
Rationale for incorrect answers
1. Empathy is important but not a priority teaching point. Therapeutic communication supports trust but does not address physiological or procedural risks.
2. Cardiac monitoring is essential during ECT, especially for clients with known heart disease, but it is not the primary teaching focus unless cardiac risk is present.
4. Injury from induced seizure is rare due to muscle relaxants and anesthesia. Modern ECT protocols minimize physical harm, making this teaching point less relevant.
Take Home Points
- ECT is indicated for severe, treatment-resistant depression, especially with suicidality or psychotic features.
- Short-term memory loss is the most common adverse effect and must be discussed with clients and families.
- Cardiac risks exist but are rare in healthy individuals; pre-procedure screening mitigates complications.
- ECT is safe when administered under anesthesia with muscle relaxants, reducing seizure-related injury.
Which intervention takes priority when working with newly admitted clients experiencing suicidal ideations?
Explanation
Suicidal ideation involves thoughts of self-harm or death and may be passive or active. Active ideation includes a plan or intent and requires immediate intervention. The most critical priority is ensuring safety, preventing access to lethal means, and initiating continuous observation. Risk increases with prior attempts, psychiatric comorbidities, and recent losses. Monitoring must be direct and unpredictable to prevent manipulation or concealment of intent.
Rationale for correct answer
1. Close monitoring is essential to prevent self-harm during the acute phase. Irregular intervals reduce predictability, making it harder for the client to plan an attempt.
Rationale for incorrect answers
2. Group therapy is contraindicated in acute suicidal states due to risk of triggering, lack of insight, and inability to engage safely.
3. Discharge planning is secondary. Immediate safety during admission takes precedence before involving external support systems.
4. Antidepressant education is important but not urgent. Delayed onset of action does not address immediate risk of self-harm.
Take Home Points
- Active suicidal ideation requires immediate safety interventions including unpredictable monitoring.
- Group therapy is inappropriate during acute suicidal crises due to emotional instability and risk of contagion.
- Discharge planning is important but secondary to inpatient safety stabilization.
- Antidepressants take weeks to work; acute suicidal risk must be managed before pharmacologic effects are expected.
Which of the following medications may be administered before electroconvulsive therapy? Select all that apply.
Explanation
Electroconvulsive therapy (ECT) is a controlled procedure used to treat severe depression, catatonia, and treatment-resistant psychiatric conditions. It involves inducing a brief generalized seizure under anesthesia. Pre-ECT medications are administered to reduce secretions, induce anesthesia, and prevent musculoskeletal injury. The goal is to optimize safety and minimize complications such as aspiration, prolonged seizures, or cardiovascular instability. Agents used must not interfere with seizure threshold or therapeutic efficacy.
Rationale for correct answers
1. Anticholinergic agents like glycopyrrolate reduce salivary and bronchial secretions, lowering aspiration risk and preventing bradycardia during ECT.
2. Anesthetic induction is achieved with thiopental, a short-acting barbiturate that provides rapid unconsciousness without significantly altering seizure threshold.
3. Muscle relaxation is critical to prevent injury during seizure. Succinylcholine, a depolarizing neuromuscular blocker, minimizes convulsive movements while preserving seizure activity.
Rationale for incorrect answers
4. Benzodiazepines like lorazepam raise seizure threshold and may blunt ECT efficacy. They are avoided unless treating status epilepticus or severe agitation.
5. Anticonvulsants such as divalproex suppress seizure activity and counteract ECT’s therapeutic mechanism. They are contraindicated unless treating comorbid epilepsy.
Take Home Points
- Pre-ECT medications include anticholinergics, anesthetics, and muscle relaxants to ensure safety and efficacy.
- Benzodiazepines and anticonvulsants interfere with seizure induction and are avoided before ECT.
- Glycopyrrolate prevents bradycardia and aspiration by reducing secretions.
- Succinylcholine minimizes physical injury during seizure without suppressing therapeutic activity.
A nursing student is studying major depressive disorder. Which student statement indicates that learning has occurred?
Explanation
Major depressive disorder is a chronic psychiatric condition characterized by persistent low mood, anhedonia, and functional impairment. It affects neurotransmitter systems including serotonin, norepinephrine, and dopamine. Symptoms must persist for at least 2 weeks and include changes in sleep, appetite, energy, and cognition. It is highly comorbid with anxiety and substance use disorders and is a major contributor to global disease burden due to its impact on daily functioning and productivity.
Rationale for correct answer
4. Disability impact is profound in major depression. It interferes with occupational, social, and physical functioning, making it one of the top causes of disability globally and in the U.S.
Rationale for incorrect answers
1. Prevalence is underestimated. Annual prevalence of major depression is closer to 7% in the general population, not 1%.
2. Women experience higher lifetime prevalence, around 10–25%, not 2–5%. Hormonal and psychosocial factors contribute significantly.
3. Men have lower reported rates due to underdiagnosis, but actual lifetime prevalence is closer to 5–12%, not 1–3%.
Take Home Points
- Major depressive disorder is a leading cause of disability due to its chronicity and impact on functioning.
- Lifetime prevalence is significantly higher than 1–5%, especially among women.
- Men may underreport depressive symptoms, contributing to underestimated prevalence.
- Accurate epidemiological understanding is essential for early recognition and intervention.
A client diagnosed with major depressive disorder has an outcome that states, “The client will verbalize a measure of hope about the future by day 3.” Which client statement indicates this outcome was successful?
Explanation
Hopefulness in depression reflects a shift from passive despair to active engagement with future possibilities. Major depressive disorder impairs motivation, cognition, and affect, often leading to hopelessness and withdrawal. A sign of improvement is when the client begins to express future-oriented thinking, problem-solving, or plans that imply belief in change. Statements that show initiative, intention, or desire to resolve issues signal emerging hope and therapeutic progress.
Rationale for correct answer
3. Future planning is evident in the client’s intent to address workplace conflict. This shows restored motivation and belief in personal agency, aligning directly with the outcome of verbalizing hope.
Rationale for incorrect answers
1. Despair is still present. Avoiding suicide due to guilt or concern for others does not reflect internal hope or future engagement.
2. Activity participation is positive but nonspecific. It reflects behavioral activation, not necessarily hope about the future or resolution of internal distress.
4. Gratitude is interpersonal and reflective, not future-oriented. It does not indicate the client’s outlook or plans beyond the present moment.
Take Home Points
- Hope in depression is marked by future-oriented statements and problem-solving intentions.
- Behavioral activation alone does not confirm hope unless tied to future goals.
- Avoidance of suicide due to guilt or external pressure is not equivalent to internal hope.
- Therapeutic progress includes both emotional recovery and cognitive re-engagement with life plans.
Exams on Depressive Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Definition of Depressive Disorders
- Practice Exercise 1
- Types Of Depressive Disorders
- Practice Exercise 2
- Diagnostic Framework
- Practice Exercise 3
- Nursing Assessment
- Nursing Process In Depression Care
- Practice Exercise 4
- Interventions And Treatments
- Contributing Factors
- Practice Exercise 5
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
By the end of this topic, the student should be able to:
- Define and provide a comprehensive overview of Depressive Disorders as a major category of mental health conditions.
- Identify and differentiate the various types of Depressive Disorders according to the DSM-5-TR, including Major Depressive Disorder, Persistent Depressive Disorder, and others.
- Master the scientific diagnostic framework, including the core criteria, risk factors, and underlying theories of depression.
- Recognize the critical importance of suicide risk assessment in all individuals with depressive disorders.
- Perform a comprehensive nursing assessment of a client with a depressive disorder, identifying key assessment findings across multiple domains.
- Formulate appropriate nursing diagnoses and develop a thorough nursing care plan for clients with depression.
- Identify and implement a wide range of evidence-based nursing interventions and therapeutic treatments.
- Understand the principles, indications, and nursing care associated with key treatments such as pharmacotherapy, Electroconvulsive Therapy (ECT), and psychotherapy.
- Provide comprehensive patient and family education to promote self-care and coping skills.
Definition of Depressive Disorders
- Depressive disorders are a category of mood disorders characterized by persistent and significant changes in an individual's mood state, primarily marked by feelings of sadness, emptiness, or irritability.
- These mood disturbances are often accompanied by a loss of interest or pleasure in activities that were once enjoyable, a cardinal symptom known as anhedonia.
- The term “Depressive Disorders” in the DSM-5-TR encompasses a range of conditions that share core features of low mood but differ in their duration, timing, or presumed etiology.
- The symptoms are severe enough to cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- These disorders are not simply normal sadness or a temporary emotional response to a stressful life event; they represent a pathological state that requires professional intervention.
1.1 Epidemiology and Prevalence
- Depressive disorders are among the most common mental health conditions globally, affecting people of all ages, genders, and socioeconomic backgrounds.
- The lifetime prevalence of Major Depressive Disorder (MDD) in the United States is estimated to be approximately 20%, making it a highly prevalent and impactful disorder.
- Females are diagnosed with MDD at a rate of 1.5 to 3 times higher than males, particularly during their reproductive years, though this gender disparity becomes less pronounced after menopause.
- The onset of MDD can occur at any age, but the median age of onset is in the early 20s.
- The prevalence of depression in older adults is often under-diagnosed due to atypical presentations and the tendency to attribute symptoms to normal aging or co-occurring medical conditions.
1.2 Levels of Depression
- The severity of depressive symptoms is a crucial aspect of diagnosis and treatment planning. The DSM-5-TR provides severity specifiers for Major Depressive Disorder.
- Mild Depression:
- Characterized by the presence of the minimum number of symptoms required for a diagnosis.
- Symptoms cause only minor impairment in social or occupational functioning.
- The individual may still be able to function, but with increased effort and a sense of being "down" or "not themselves."
- Tends to respond well to psychotherapy and is sometimes managed without medication.
- Moderate Depression:
- The number of symptoms and the intensity of those symptoms are intermediate between mild and severe.
- Symptoms lead to noticeable impairment in social, occupational, and other areas of functioning.
- The individual may struggle significantly with work, school, or relationships.
- This level of severity often warrants a combination of psychotherapy and pharmacotherapy.
- Severe Depression:
- The presence of most or all of the diagnostic criteria for a major depressive episode.
- Symptoms are intensely distressing and almost unmanageable for the individual.
- Symptoms cause significant impairment in functioning, making it difficult or impossible to perform daily activities, such as self-care, work, or social interaction.
- This level of severity often requires hospitalization to ensure safety and intensive treatment, including pharmacotherapy and potentially Electroconvulsive Therapy (ECT).
- Severe depression can be further specified "with psychotic features," where the individual experiences hallucinations (auditory or visual) or delusions (e.g., of worthlessness, guilt, or nihilism).
1.3 Course and Prognosis
- The course of depressive disorders is highly variable among individuals.
- A single episode of Major Depressive Disorder can last for several months, with a median duration of about six months.
- The vast majority of individuals who experience a major depressive episode will experience a full or partial remission of symptoms.
- However, depression is a highly recurrent illness. Approximately 50% of individuals who have one episode will have a second, and the risk increases with each subsequent episode.
- The prognosis is generally good with appropriate and timely treatment, but recurrence and chronicity are significant concerns.
- Persistent Depressive Disorder (Dysthymia) is a chronic condition, lasting for at least two years. It has a high comorbidity with Major Depressive Disorder, a phenomenon referred to as "double depression."
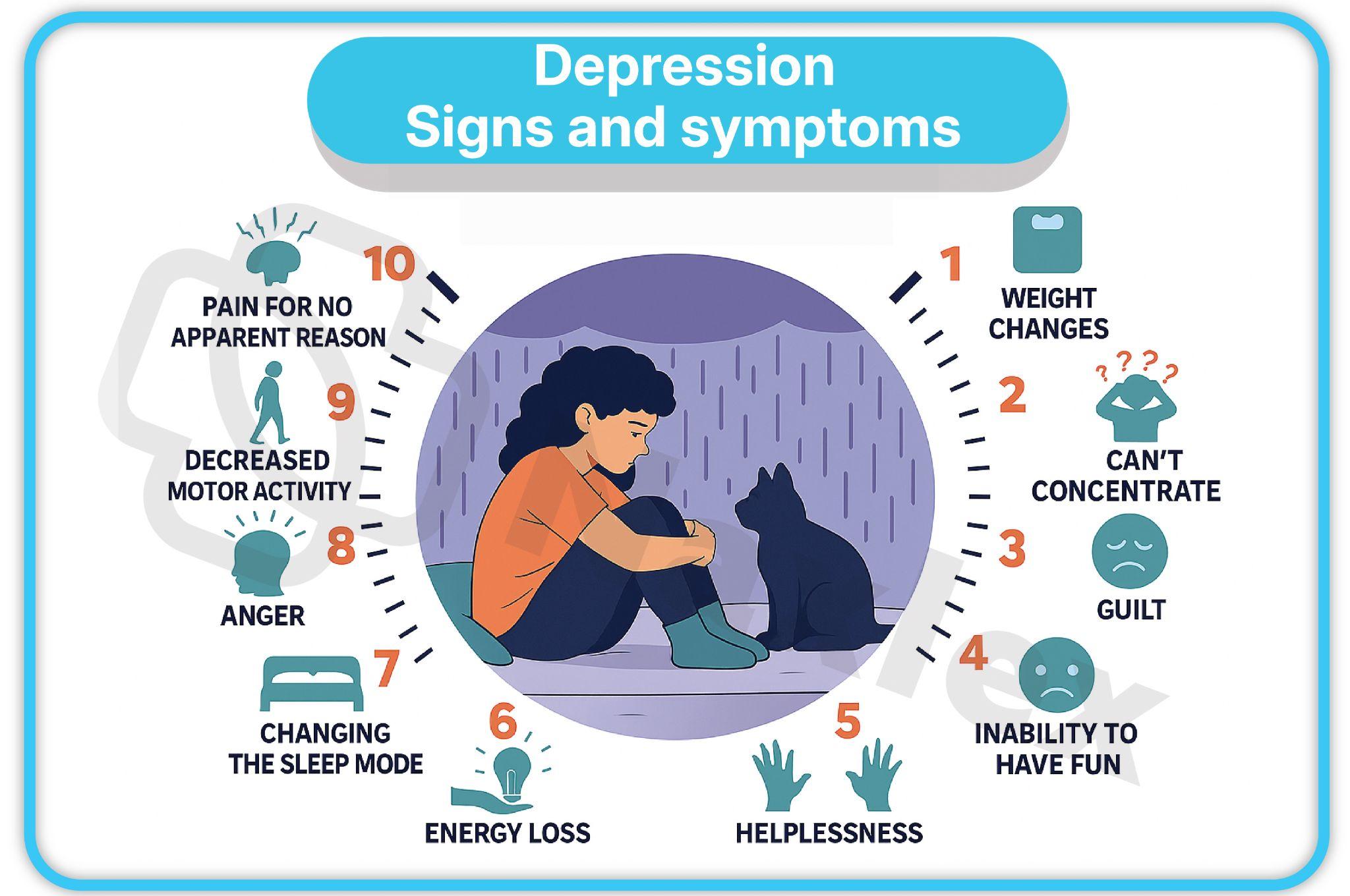
Types Of Depressive Disorders
1.1 Major Depressive Disorder (MDD)
- The quintessential depressive disorder. The diagnosis requires the presence of five or more of the defining symptoms during the same 2-week period, representing a change from previous functioning. At least one of the symptoms must be either depressed mood or loss of interest or pleasure (anhedonia).
- Symptoms include:
- Depressed mood most of the day, nearly every day (subjective report or observation by others).
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day.
- Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day.
- Insomnia or hypersomnia nearly every day.
- Psychomotor agitation or retardation nearly every day (observable by others).
- Fatigue or loss of energy nearly every day.
- Feelings of worthlessness or excessive or inappropriate guilt nearly every day.
- Diminished ability to think or concentrate, or indecisiveness, nearly every day.
- Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan.
- With Peripartum Onset Specifier:
- This specifier applies to a major depressive episode that occurs during pregnancy or in the first four weeks following delivery.
- It is often referred to as postpartum depression, although the DSM-5-TR uses the broader term "peripartum onset."
- The symptoms are identical to those of a major depressive episode but carry unique risk factors and implications.
- Risks include hormonal fluctuations, psychosocial stressors (e.g., sleep deprivation, new parental roles), and a history of previous depression.
- Untreated peripartum depression poses significant risks to both the mother and the infant, including impaired mother-infant bonding and developmental delays in the child.
- With Seasonal Pattern (SAD):
- This specifier applies to recurrent major depressive episodes that occur during a specific time of year, most commonly in the fall or winter, and remit in the spring.
- The temporal relationship is a key feature, with at least two episodes occurring in the past two years with a seasonal pattern and no non-seasonal episodes during that same period.
- Symptoms often include hypersomnia (excessive sleeping), increased appetite, weight gain, and a craving for carbohydrates.
- The pathophysiology is believed to involve a dysregulation of circadian rhythms and a decrease in serotonin and melatonin levels due to reduced exposure to sunlight.
NURSING INSIGHTS:
- When assessing a patient for Major Depressive Disorder, a critical nursing responsibility is to differentiate between normal sadness and a clinical depressive episode.
- A key distinguishing factor is the duration and pervasiveness of the symptoms, particularly the presence of anhedonia and functional impairment.
- The nurse must not dismiss a patient's symptoms as simply "feeling down" and should instead use a structured approach, like the DSM-5-TR criteria, to guide their assessment.
- The presence of at least one of the two cardinal symptoms—depressed mood or anhedonia—is a non-negotiable requirement for a diagnosis of MDD.
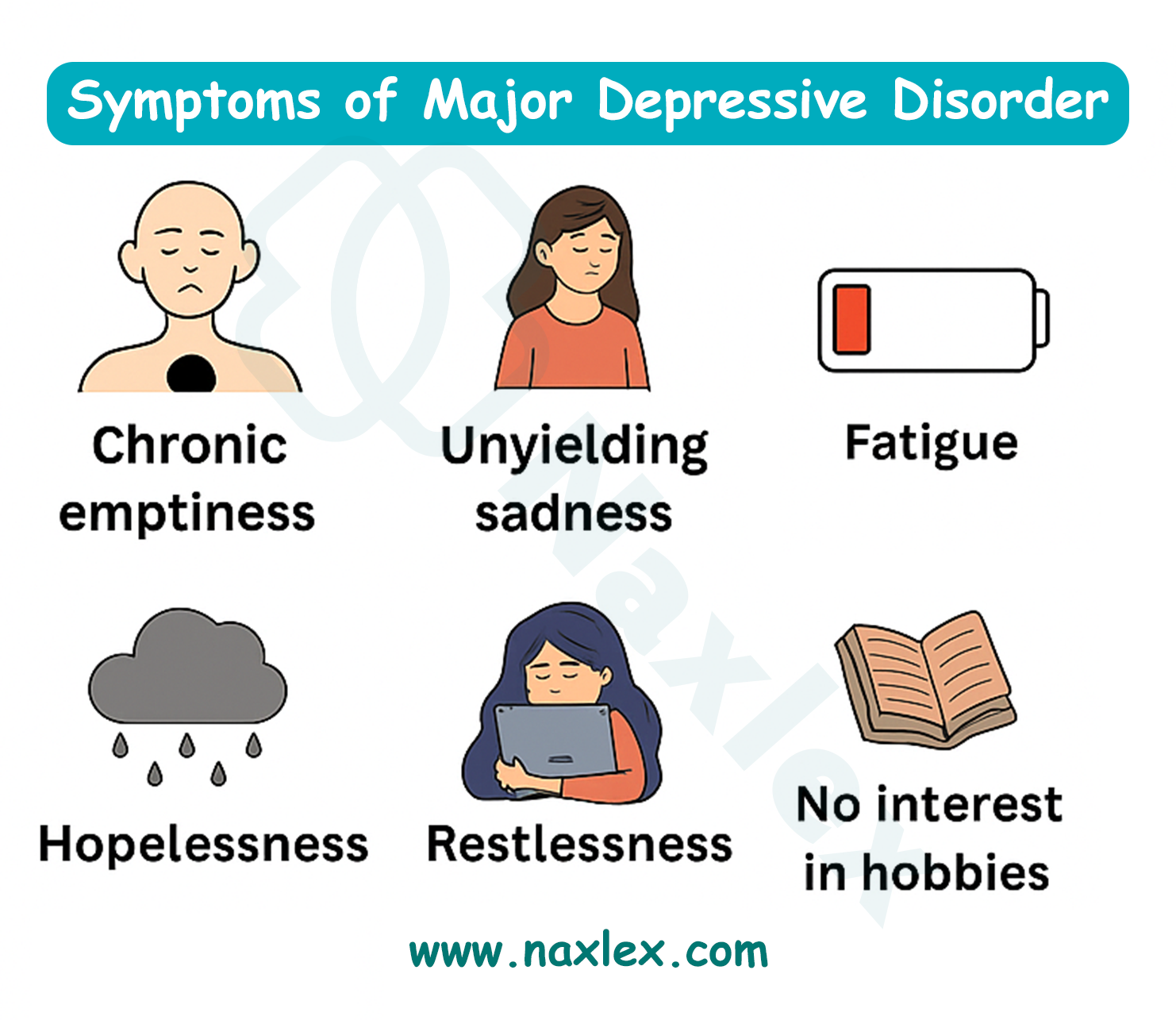
1.2 Persistent Depressive Disorder (Dysthymia)
- Characterized by a chronically depressed mood for most of the day, for more days than not, for at least two years (or one year for children and adolescents).
- The symptoms are generally less severe than those of MDD but are more persistent and chronic.
- During the two-year period, the individual has not been without the symptoms for more than two consecutive months.
- Symptoms must include at least two of the following:
- Poor appetite or overeating.
- Insomnia or hypersomnia.
- Low energy or fatigue.
- Low self-esteem.
- Poor concentration or difficulty making decisions.
- Feelings of hopelessness.
- The diagnosis is not made if the criteria for a major depressive episode have been met continuously for the two-year period, as this would be considered Major Depressive Disorder.
- However, individuals with persistent depressive disorder are at a high risk for developing a major depressive episode, leading to "double depression."
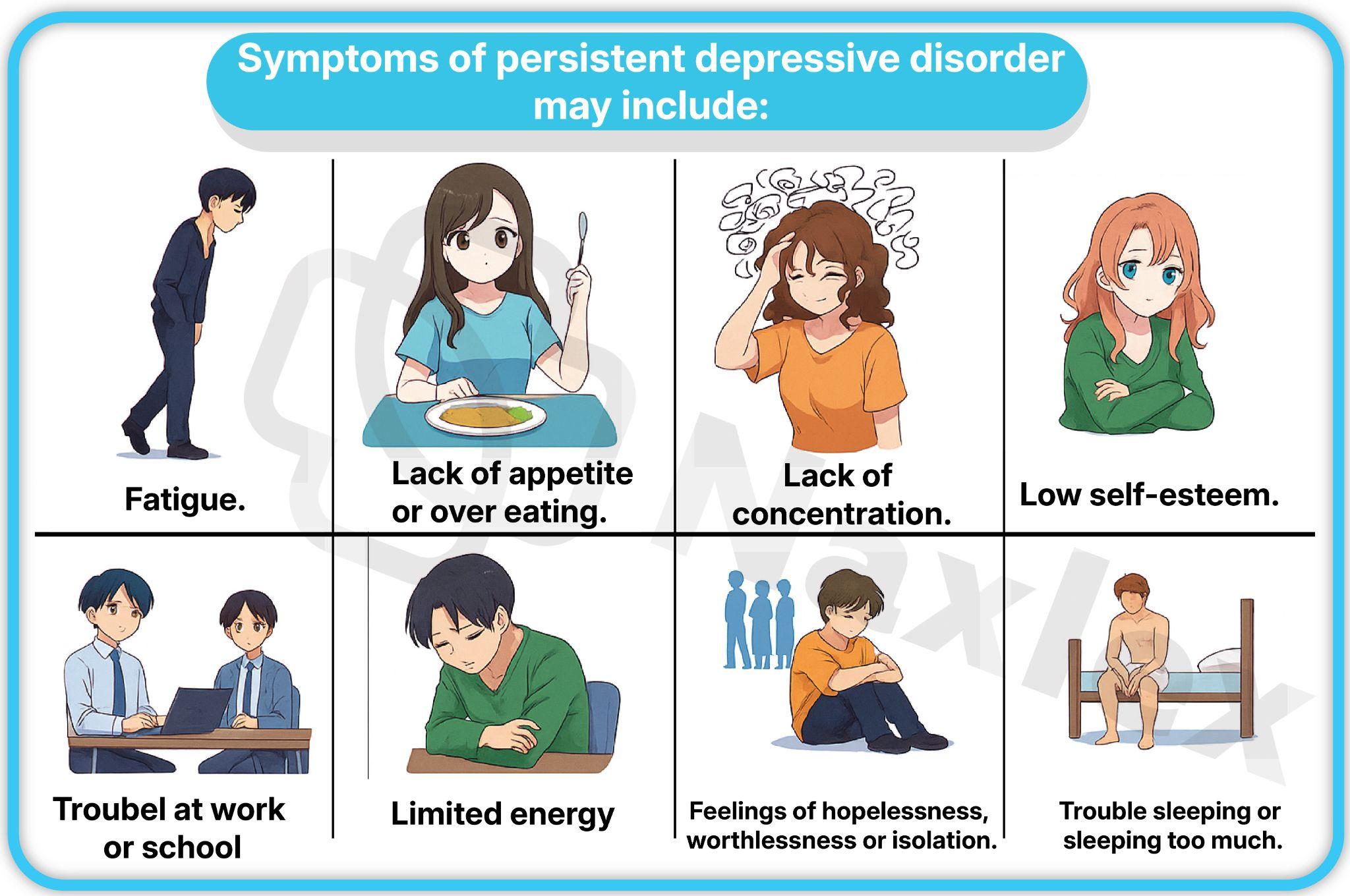
1.3 Disruptive Mood Dysregulation Disorder (DMDD)
- This diagnosis is specifically for children and adolescents up to age 18.
- It is characterized by chronic, severe irritability and frequent temper outbursts that are out of proportion to the situation.
- The temper outbursts occur at least three times a week for at least a year and are present in at least two different settings (e.g., home, school).
- In between the outbursts, the child's mood is persistently irritable or angry for most of the day, nearly every day.
- The onset of symptoms must be before age 10.
- The purpose of this diagnosis is to prevent the over-diagnosis of pediatric bipolar disorder, which has a different clinical course and treatment plan.
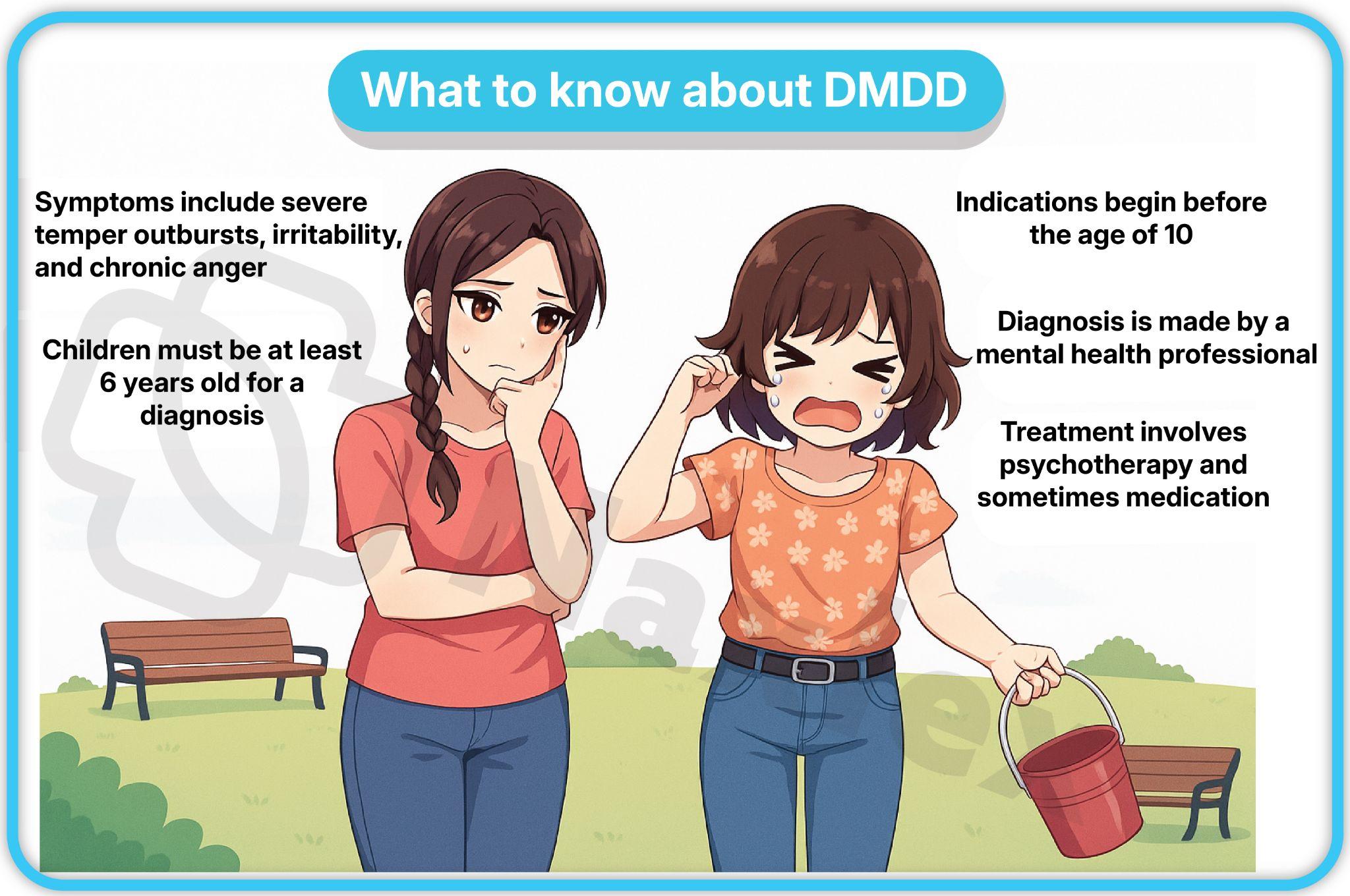
1.4 Premenstrual Dysphoric Disorder (PMDD)
- A severe and debilitating form of premenstrual syndrome (PMS).
- Symptoms occur in the week before the onset of menses, start to improve within a few days after menses begins, and become minimal or absent in the week post-menses.
- The diagnosis requires the presence of five or more symptoms, with at least one from each of the two core categories:
- Core Mood Symptoms: Marked affective lability (mood swings), marked irritability or anger, marked depressed mood or hopelessness, and marked anxiety.
- Other Symptoms: Decreased interest in activities, difficulty concentrating, lethargy or fatigue, change in appetite, hypersomnia or insomnia, a sense of being overwhelmed or out of control, and physical symptoms like breast tenderness or joint pain.
- PMDD causes significant distress or interference with work, school, or social activities.
- The condition is thought to be related to an abnormal response to the normal hormonal fluctuations of the menstrual cycle.
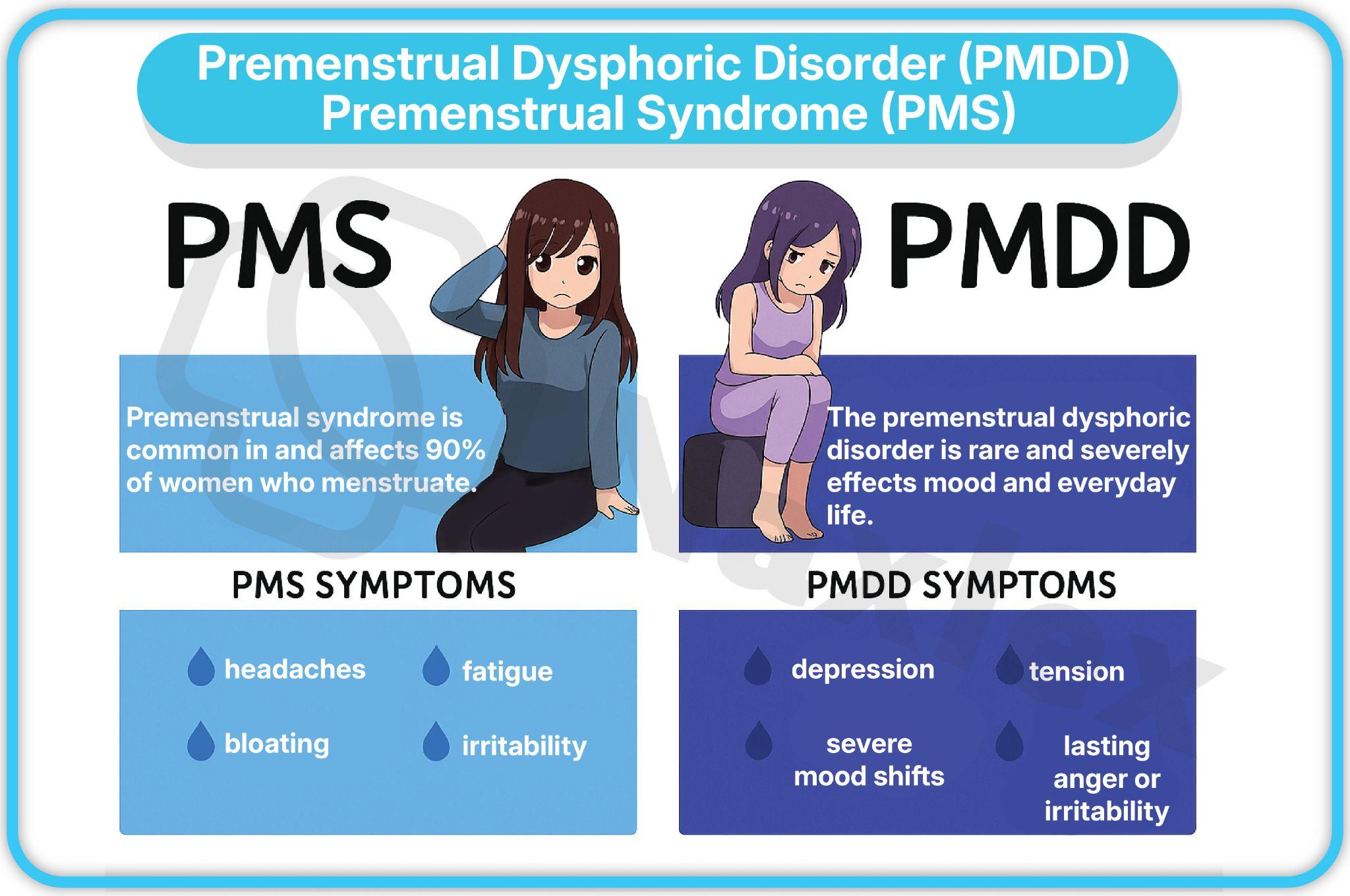
1.5 Substance/Medication-Induced Depressive Disorder
- This diagnosis is made when the symptoms of a major depressive episode develop during or soon after substance intoxication or withdrawal, or after exposure to a medication.
- The substance or medication is judged to be etiologically related to the mood disturbance.
- Examples of substances include alcohol, opioids, sedatives, hypnotics, and cannabis.
- Examples of medications that can induce depressive symptoms include corticosteroids, interferon-alpha, and some antihypertensives.
- The symptoms must be severe enough to cause clinically significant distress or impairment in functioning.
1.6 Depressive Disorder Due to Another Medical Condition
- This diagnosis is made when a prominent and persistent depressed mood or anhedonia is the direct physiological consequence of another medical condition.
- The evidence must suggest a direct pathophysiological link.
- Examples of medical conditions that can cause depressive symptoms include hypothyroidism, Cushing's disease, multiple sclerosis, stroke, and Parkinson's disease.
- The symptoms must not be better explained by another mental disorder.
1.7 Other Specified Depressive Disorder
- This is a category for depressive presentations that cause significant distress or impairment but do not meet the full criteria for any of the other depressive disorders.
- The clinician specifies the reason why the criteria were not met, such as:
- Recurrent brief depression (episodes lasting from 2 days to 2 weeks).
- Short-duration depressive episode (lasting 4-13 days).
- Depressive episode with insufficient symptoms.
1.8 Unspecified Depressive Disorder
- This is used when the clinician chooses not to specify the reason the criteria are not met for a specific depressive disorder.
- This category is often used in emergency department settings or other situations where there is insufficient time or information to make a more specific diagnosis.
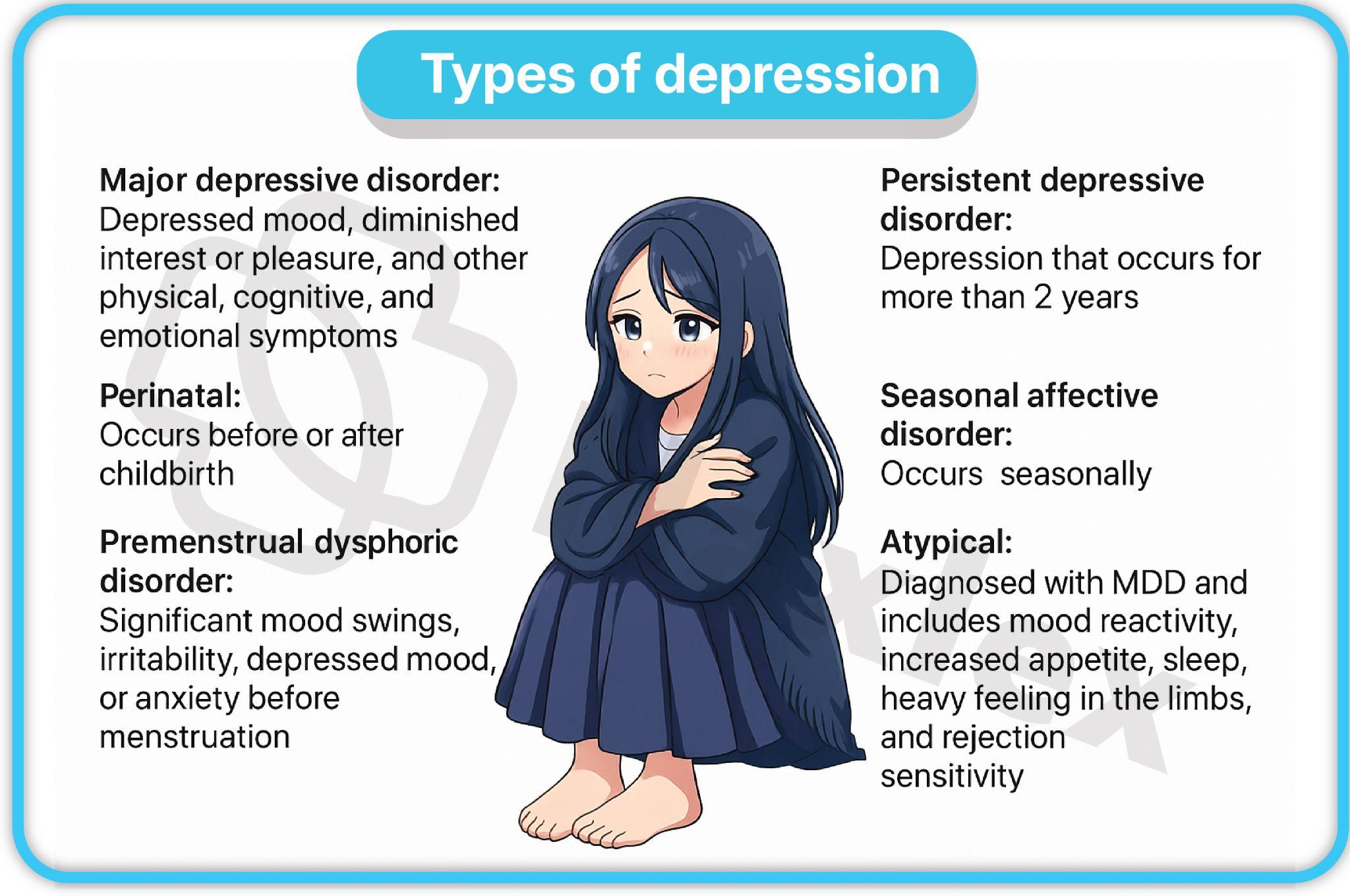
Diagnostic Framework
1.1 Diagnostic Criteria (per DSM-5-TR)
- As outlined in the MDD section, the diagnosis requires five or more specific symptoms present during a 2-week period, including either depressed mood or anhedonia.
- The symptoms must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- The episode is not attributable to the physiological effects of a substance or another medical condition.
- The occurrence of the major depressive episode is not better explained by Schizoaffective Disorder, Schizophrenia, or other psychotic disorders.
- There has never been a manic or hypomanic episode, as this would suggest Bipolar Disorder.
1.2 Diagnostic Features
- The essential feature is a period of at least two weeks during which there is either depressed mood or a loss of interest or pleasure in nearly all activities.
- In children and adolescents, the mood can be irritable rather than sad.
- The individual may report feeling "sad," "empty," "hopeless," or "down."
- Anhedonia is a prominent feature and is considered a core symptom. Patients may describe feeling "flat" or "lacking emotion."
- Somatic symptoms are common, including fatigue, changes in appetite, and sleep disturbances (insomnia or hypersomnia).
- Cognitive symptoms include difficulty concentrating, indecisiveness, and recurrent thoughts of death or suicide.
1.3 Development and Course
- The mean age of onset for Major Depressive Disorder is in the mid-20s, but it can occur at any age.
- The onset is often insidious, with symptoms gradually worsening over days or weeks.
- A major depressive episode can last from a few weeks to several months, with a median duration of about six months if untreated.
- Approximately two-thirds of individuals with MDD will have a recurrent episode within a few years of the initial one.
- The risk of recurrence is higher for individuals with earlier onset, a history of multiple episodes, or persistent residual symptoms.
- Chronic or untreated depression can lead to significant long-term disability and impairment.
NURSING INSIGHTS:
- A major point for nurses to understand is the crucial difference between Major Depressive Disorder (MDD) and Persistent Depressive Disorder (Dysthymia). While both involve a low mood, MDD is defined by discrete episodes of at least two weeks with significant impairment, while Dysthymia is a chronic, lower-grade depression lasting for at least two years.
- Recognizing this distinction is vital for care planning.
- Dysthymia requires long-term management strategies, often a combination of pharmacotherapy and psychotherapy, to address chronic low mood and function, while MDD may require more intensive, episodic intervention.
1.4 Risk and Prognostic Factors
- Predisposing Factors:
- Genetics: A strong family history of depressive disorders is a significant risk factor. The heritability of MDD is estimated to be around 40%.
- Temperamental: Neuroticism (the tendency to experience negative emotions) is a well-established risk factor.
- Environmental: Adverse childhood experiences (e.g., abuse, neglect), chronic stress, lack of a social support network, and poverty increase the risk.
- Biological Theories:
- Neurotransmitter Dysregulation: The monoamine hypothesis of depression posits that a deficiency in monoamine neurotransmitters—specifically serotonin, norepinephrine, and dopamine—in the synaptic cleft is a primary cause.
-
- Serotonin (5-HT): Regulates mood, appetite, and sleep. Low levels are associated with feelings of sadness, anxiety, and a craving for carbohydrates. SSRIs (Selective Serotonin Reuptake Inhibitors) work by increasing serotonin availability.
- Norepinephrine (NE): Modulates attention, concentration, energy, and motivation. Low levels are linked to fatigue, psychomotor retardation, and anhedonia.
- Dopamine (DA): Involved in pleasure, reward, and motivation. Low levels are associated with anhedonia, fatigue, and lack of motivation.
-
- Neurobiological Changes: Depression is associated with structural and functional changes in key brain regions.
-
- Limbic System: The amygdala (involved in emotion) and the hippocampus (involved in memory and stress response) often show abnormalities. The hippocampus may shrink with chronic stress and depression.
- Prefrontal Cortex (PFC): The PFC, particularly the dorsolateral PFC, is involved in executive function and mood regulation. Decreased activity in this area is a common finding.
-
- Endocrine and Inflammatory Markers:
-
- HPA Axis Dysregulation: The Hypothalamic-Pituitary-Adrenal (HPA) axis, which controls the stress response, is often overactive in depression, leading to elevated cortisol levels.
- Cytokines: Research suggests a link between inflammation and depression. Increased levels of pro-inflammatory cytokines may contribute to depressive symptoms.
-
- Neurotransmitter Dysregulation: The monoamine hypothesis of depression posits that a deficiency in monoamine neurotransmitters—specifically serotonin, norepinephrine, and dopamine—in the synaptic cleft is a primary cause.
- Psychosocial Theories:
- Cognitive Theory (Aaron Beck): Proposes that depression results from a triad of negative and distorted cognitive beliefs about oneself, the world, and the future. These negative schemas lead to automatic negative thoughts that reinforce depressive feelings.
- Learned Helplessness (Martin Seligman): Suggests that depression arises when individuals learn that they have no control over negative life events, leading to a sense of powerlessness and an inability to take action to change their circumstances.
- Interpersonal Theory (Harry Stack Sullivan): Focuses on the role of interpersonal relationships and social support in depression. Depression is seen as a consequence of interpersonal difficulties, such as social isolation, unresolved grief, or role disputes.
1.5 Culture-Related Diagnostic Issues
- Cultural context significantly influences the expression and experience of depressive symptoms.
- In some cultures, particularly non-Western ones, psychological distress may be expressed through somatic symptoms (e.g., headache, fatigue, joint pain) rather than affective symptoms like sadness.
- Nurses must be culturally competent and avoid making assumptions based on Western symptom presentations. It is crucial to ask about "idioms of distress" and how the individual or their culture describes "feeling bad."
- Cultural stigma surrounding mental illness can prevent individuals from seeking help or openly discussing their symptoms.
1.6 Gender-Related Diagnostic Issues
- The higher prevalence of depression in females is a complex issue.
- Possible contributing factors include hormonal fluctuations (e.g., puberty, pregnancy, menopause), differences in coping styles (e.g., rumination is more common in women), and greater exposure to interpersonal violence and trauma.
- Men may be more likely to mask depressive symptoms with substance use, anger, irritability, or risk-taking behavior, leading to under-diagnosis.
- The nurse must be aware of these gender-specific presentations and tailor their assessment questions accordingly.
1.7 Specifiers for Depressive Disorders
- Specifiers provide more detailed information about the current or most recent depressive episode.
- Examples include:
- With Anxious Distress: The presence of at least two symptoms of anxiety.
- With Mixed Features: The presence of at least three symptoms of a manic or hypomanic episode.
- With Melancholic Features: Characterized by a near-complete loss of pleasure, lack of reactivity to pleasurable stimuli, and at least three other specific symptoms (e.g., profound despondency, psychomotor agitation/retardation).
- With Atypical Features: Characterized by mood reactivity (mood brightens in response to positive events), significant weight gain or increase in appetite, hypersomnia, and a feeling of being "leaden" or heavy in the limbs.
- With Psychotic Features: The presence of delusions or hallucinations.
- With Catatonia: A rare and severe psychomotor disturbance.
- With Peripartum Onset: A severe and debilitating form of premenstrual syndrome (PMS).
-
- With Seasonal Pattern: A recurrent major depressive episodes that occur during a specific time of year, most commonly in the fall or winter, and remit in the spring.
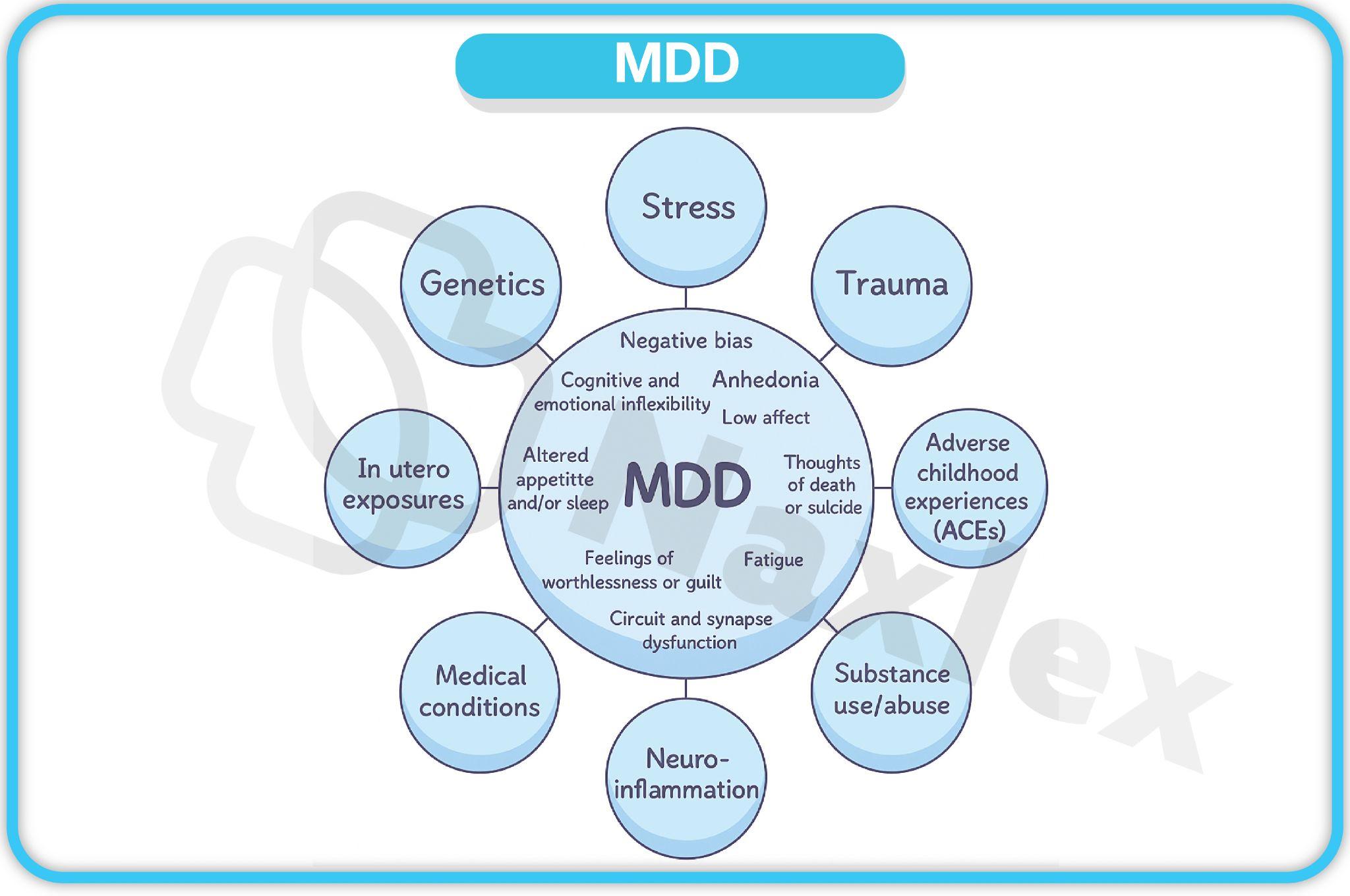
1.8 Differential Diagnosis
- It is critical to rule out other conditions that can mimic depression.
- Medical Conditions: A thorough medical workup is essential to rule out conditions like hypothyroidism, anemia, vitamin B12 deficiency, or neurological disorders.
- Bipolar Disorders: The presence of a history of a manic or hypomanic episode rules out a diagnosis of Major Depressive Disorder.
- Bereavement: Normal grief is a natural response to loss and typically does not meet the full criteria for a major depressive episode. However, prolonged or complicated grief may warrant a diagnosis.
- Substance/Medication-Induced Mood Disorder: A thorough history of substance and medication use is crucial.
- Other Psychiatric Disorders: Schizoaffective Disorder, Schizophrenia, and other psychotic disorders must be considered if there are psychotic features.
1.9 Comorbidity
- Depressive disorders frequently co-occur with other mental and physical health conditions.
- Anxiety Disorders: Approximately 60-70% of individuals with MDD also have a co-occurring anxiety disorder.
- Substance Use Disorders: Individuals with depression may use substances as a form of self-medication, leading to a co-occurring substance use disorder.
- Eating Disorders: There is a high comorbidity between depression and eating disorders like Anorexia Nervosa and Bulimia Nervosa.
- Medical Illnesses: Depression is highly prevalent in individuals with chronic medical conditions such as cardiovascular disease, diabetes, and cancer.
1.10 Suicide Risk
- A fundamental and non-negotiable component of any nursing assessment for a patient with a depressive disorder is a comprehensive suicide risk assessment.
- The risk of suicide is significantly elevated in individuals with depressive disorders, with a 20-fold increase in risk compared to the general population.
- The nurse must ask direct, non-judgmental questions about suicidal ideation, intent, plan, and means.
- Key risk factors for suicide include:
- A history of prior suicide attempts.
- Current suicidal ideation with a specific plan and intent.
- A family history of suicide.
- Social isolation or lack of social support.
- Co-occurring substance use disorder.
- Access to lethal means.
- Impulsivity or hopelessness.
- Recent stressful life events or losses.
- The nurse's role is not only to assess the risk but also to take immediate action, which may include implementing suicide precautions, notifying the healthcare team, and providing a safe environment.
|
Risk Factor |
Description |
Nursing Implication |
|
Hopelessness |
Perception of no future improvement |
Assess via Beck Hopelessness Scale; intervene with CBT elements |
|
Prior Attempts |
History increases 30-fold risk |
Document and escalate to psychiatry |
|
Comorbid Substance Use |
Impairs judgment |
Monitor detox and dual-diagnosis programs |
|
Male Gender |
Higher completion rates |
Screen routinely despite stoicism |
NURSING INSIGHTS:
- The presence of suicidal ideation is a major red flag in any patient with depression. A common misconception is that asking about suicide will plant the idea in the patient's mind; however, scientific evidence demonstrates the opposite.
- Directly and compassionately asking about suicide is the most effective way to determine a patient's risk and open the door for them to disclose their thoughts.
- The nurse must document the assessment thoroughly and implement immediate safety measures based on the level of risk identified.
- The nurse's ability to perform this assessment accurately and without hesitation can be life-saving.
Nursing Assessment
1.1 Assessment Findings
- A thorough nursing assessment goes beyond a simple diagnostic checklist and aims to understand the patient’s holistic experience of depression. It is organized into several domains:
- Affective Symptoms:
- The patient's subjective report of mood, which may include feelings of sadness, emptiness, hopelessness, or despair.
- Anhedonia, the loss of interest or pleasure in previously enjoyed activities.
- Irritability, anger, or frustration, which can be a predominant symptom, especially in men and adolescents.
- Feelings of guilt, worthlessness, or self-blame, which can be delusional in severe cases.
- Cognitive Symptoms:
- Impaired concentration and indecisiveness, leading to difficulty with tasks at work or school.
- Negative cognitive distortions, such as all-or-nothing thinking, catastrophizing, and personalization.
- Recurrent thoughts of death or suicide, which must be assessed for intent, plan, and means.
- Memory impairment, often presenting as "pseudo-dementia" in older adults.
- Behavioral Symptoms:
- Psychomotor retardation (slowed movements, speech, and thought processes) or psychomotor agitation (restlessness, pacing, hand-wringing).
- Social withdrawal and isolation, avoidance of social activities.
- Neglect of personal hygiene and self-care.
- Crying spells or emotional lability.
- Physiological Symptoms (Vegetative Symptoms):
- Sleep disturbances: Insomnia (difficulty falling asleep or staying asleep, early morning awakening) or hypersomnia (excessive sleeping).
- Appetite changes: Significant weight loss due to decreased appetite or weight gain due to overeating (especially for high-carbohydrate foods).
- Fatigue and loss of energy: Feeling tired or "drained" most of the time, regardless of activity level.
- Somatic complaints: Vague physical pains, headaches, or gastrointestinal issues that have no clear medical cause.
- Decreased libido: A significant decrease in sexual interest and function.
- Affective Symptoms:
1.2 Common Screening Tools for Depression
- Screening tools are essential for the systematic identification of depressive symptoms and monitoring treatment response.
- They should not be used as the sole basis for diagnosis but rather as an adjunct to a comprehensive clinical interview.
- PHQ-9 (Patient Health Questionnaire-9):
- A self-report questionnaire with 9 items that correspond to the DSM-5 criteria for a major depressive episode.
- The scoring is straightforward: 0-4 (minimal depression), 5-9 (mild), 10-14 (moderate), 15-19 (moderately severe), and 20-27 (severe).
- It also includes a question on suicidal ideation, which serves as an immediate trigger for further assessment.
- Beck Depression Inventory (BDI):
- A 21-item self-report scale that assesses the severity of depression.
- It covers a wide range of symptoms, including emotional, cognitive, and somatic.
- It is widely used in both clinical practice and research.
- Hamilton Depression Rating Scale (HAM-D):
- A clinician-administered scale with 17 to 21 items.
- The clinician rates the severity of the patient's symptoms based on a structured interview.
- It is considered a gold standard for measuring treatment response in clinical trials.
- Geriatric Depression Scale (GDS):
- A 30-item scale (or a shorter 15-item version) designed specifically for older adults.
- It focuses on non-somatic symptoms to avoid confusion with physical illnesses common in this population.
- It uses a simple yes/no response format.
- Edinburgh Postnatal Depression Scale (for peripartum cases):
- A 10-item self-report scale specifically designed to screen for depression in mothers during the peripartum period.
- It has been validated for use in various cultures and languages.
- It includes a question on suicidal thoughts, which should prompt immediate follow-up.
Table: Screening Tools Overview
|
Screening Tool |
Target Population |
Key Features |
Nursing Role |
|
PHQ-9 |
General adults |
9 items, self-report, quick |
Administer in primary care, monitor item 9 for suicide risk |
|
BDI |
Adults, outpatient |
21 items, detailed cognitive focus |
Interpret for psychiatric referrals, note cognitive distortions |
|
HAM-D |
Inpatient, research |
Clinician-rated, somatic emphasis |
Collaborate with providers, assess vegetative symptoms |
|
GDS |
Older adults |
Yes/no format, dementia-friendly |
Screen in nursing homes, differentiate from neurocognitive issues |
|
EPDS |
Peripartum women |
10 items, maternal focus |
Use in postpartum checks, flag bonding issues |
1.3 Measuring Depression (scoring interpretation)
- The scores from screening tools are used to guide the next steps of care.
- A score indicating moderate to severe depression (e.g., PHQ-9 score > 10) should prompt a referral for a comprehensive psychiatric evaluation and a more in-depth suicide risk assessment.
- A score indicating mild depression may be managed with psychoeducation and supportive care, with a plan for re-evaluation.
- Scores are also used to track the patient's progress over time and evaluate the effectiveness of interventions.
1.4 Risk Assessment (suicidal ideation, self-harm, harm to others)
- The nursing assessment must always include a detailed and non-judgmental risk assessment.
- Suicidal Ideation:
- Ask directly about thoughts of death or suicide, including passive ideation ("I wish I were dead") and active ideation ("I have thought about killing myself").
- Inquire about the frequency, duration, and intensity of these thoughts.
- Suicide Plan and Intent:
- If ideation is present, ask about the details of a plan:
- Plan: What is the method? When will it happen? Where will it happen?
- Means: Do they have access to the means they have identified? (e.g., firearms, medications, a high building)
- Intent: How likely are they to carry out the plan?
- Self-Harm:
- Assess for non-suicidal self-injury (NSSI), such as cutting, burning, or scratching. This behavior is often a maladaptive coping mechanism to deal with intense emotional pain.
- Harm to Others:
- In cases with psychotic features or severe paranoia, assess for thoughts or plans to harm others.
- This is particularly important if the patient has a history of violence or has expressed homicidal ideation.
Nursing Process In Depression Care
1.1 Nursing Diagnoses
- Based on the assessment, the nurse formulates individualized nursing diagnoses. Common diagnoses include:
- Risk for Suicide (Priority Diagnosis) related to feelings of hopelessness and suicidal ideation.
- Hopelessness related to long-term stress and failed coping mechanisms.
- Social Isolation related to social withdrawal and anhedonia.
- Self-Care Deficit related to low energy, lack of motivation, and fatigue.
- Ineffective Coping related to personal vulnerability and cognitive distortions.
- Imbalanced Nutrition: Less Than Body Requirements related to decreased appetite.
- Disturbed Sleep Pattern related to insomnia or hypersomnia.
1.2 Outcomes Identification
- The nurse collaborates with the patient to identify specific, measurable, achievable, relevant, and time-bound (SMART) outcomes.
- Examples:
- Patient will remain free from self-harm and suicide attempts throughout hospitalization.
- Patient will verbalize three positive statements about self by (date).
- Patient will engage in one social activity per day by (date).
- Patient will demonstrate proper hygiene and grooming daily.
- Patient will verbalize an increase in energy and a desire to participate in activities.
1.3 Planning Interventions
- Nursing care plans should be comprehensive and address the patient's physical, psychological, and social needs. The plan is a dynamic document that is revised as the patient's condition changes.
- Priorities in planning include:
- Safety: The absolute highest priority, especially in the presence of suicidal ideation.
- Physiological Needs: Addressing sleep, nutrition, and personal hygiene.
- Psychological Needs: Promoting a sense of self-worth and hope.
- Social Needs: Encouraging social engagement and rebuilding support systems.
- Education: Providing the patient and family with knowledge about depression, treatment, and coping strategies.
1.4 Implementation
- The nurse puts the care plan into action, utilizing a wide range of therapeutic interventions.
- This stage involves not only performing the planned actions but also continually assessing the patient's response and adapting the plan as needed.
- Therapeutic communication is a cornerstone of implementation.
1.5 Evaluation of Care
- The final step of the nursing process involves evaluating the effectiveness of the interventions and the achievement of outcomes.
- The nurse asks:
- Were the outcomes met?
- If not, why? What barriers were encountered?
- Is the patient's condition improving, declining, or stable?
- Based on the evaluation, the care plan is either continued, revised, or terminated.
Interventions And Treatments
1.1 Nursing Interventions
- Safety monitoring (suicide precautions, self-harm risk):
- For hospitalized patients, this may include one-on-one observation, frequent checks, removal of all sharp or potentially harmful objects from the room, and use of plastic utensils.
- For outpatients, it involves establishing a safety plan with the patient and family, including a list of warning signs, coping strategies, and crisis contacts.
- Promotion of self-care and coping skills:
- Encourage and assist with basic self-care activities, such as showering, dressing, and grooming.
- Use a matter-of-fact, gentle approach; avoid being overly cheerful or demanding.
- Promote a structured routine with a regular sleep-wake cycle and scheduled activities.
- Teach and reinforce adaptive coping skills, such as journaling, deep breathing exercises, or engaging in a simple hobby.
- Patient and family education:
- Educate the patient and family about the nature of depression, its biological basis, and the importance of treatment adherence.
- Explain the purpose, dose, and side effects of medications.
- Teach them to recognize early warning signs of a depressive episode or a relapse.
- Provide information on community resources, support groups, and crisis hotlines.
- Therapeutic communication & therapeutic milieu:
- Use a non-judgmental, empathetic, and accepting approach.
- Listen actively and validate the patient's feelings without being overly sympathetic.
- Use simple, direct, and concrete language. Avoid cheerleading or platitudes like "Cheer up!"
- The therapeutic milieu is a structured, supportive, and safe environment that promotes healing. This includes a consistent routine, group activities, and opportunities for social interaction.
- Referrals (support groups, crisis hotlines, psychotherapy):
- A key nursing role is to connect patients with appropriate resources to ensure continuity of care.
- Provide information on local support groups (e.g., Depression and Bipolar Support Alliance).
- Ensure the patient has access to crisis hotlines and emergency services.
- Facilitate referrals to a qualified psychotherapist for long-term treatment.
1.2 Key Treatments
- Pharmacological
- Antidepressants:
- SSRIs (Selective Serotonin Reuptake Inhibitors): The first-line treatment for depression due to their effectiveness and favorable side effect profile. They work by increasing the concentration of serotonin in the synaptic cleft. Examples: Fluoxetine (Prozac), Sertraline (Zoloft), Escitalopram (Lexapro).
- SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors): Increase both serotonin and norepinephrine levels. They may be more effective for patients with severe anhedonia or fatigue. Examples: Venlafaxine (Effexor), Duloxetine (Cymbalta).
- TCAs (Tricyclic Antidepressants): Older class of drugs that inhibit the reuptake of serotonin and norepinephrine. They have more significant side effects (anticholinergic, cardiac) and are generally reserved for patients who do not respond to newer agents. Examples: Amitriptyline, Nortriptyline.
- MAOIs (Monoamine Oxidase Inhibitors): Older but highly effective antidepressants that inhibit the enzyme monoamine oxidase, which metabolizes monoamines. They require a strict tyramine-free diet to prevent a hypertensive crisis. Examples: Phenelzine, Selegiline.
- Atypical Antidepressants: A heterogeneous group of drugs with different mechanisms of action. Examples: Bupropion (Wellbutrin) is a norepinephrine-dopamine reuptake inhibitor that is useful for depression with fatigue and is less likely to cause sexual dysfunction. Mirtazapine (Remeron) is an alpha-2 antagonist that can improve sleep and appetite.
- Mood stabilizers (for overlap with bipolar spectrum):
- If a patient with depression is suspected of having an underlying bipolar disorder, mood stabilizers like Lithium, Valproic Acid, or Lamotrigine may be used to prevent a manic or hypomanic episode.
- Augmentation strategies:
- For treatment-resistant depression, a second medication may be added to the antidepressant, such as a low-dose atypical antipsychotic (e.g., Aripiprazole, Quetiapine), or lithium.
- Considerations in older adults and pregnancy:
- Older Adults: Start low, go slow with medication doses due to decreased liver and kidney function and increased risk of side effects. Avoid TCAs due to cardiac and anticholinergic side effects.
- Pregnancy: The risks and benefits of medication must be carefully weighed. SSRIs are generally considered safer than other classes, but their use should be monitored by a perinatal psychiatrist.
- Antidepressants:
- Electroconvulsive Therapy (ECT)
- ECT is a psychiatric treatment where controlled electrical currents are passed through the brain to induce a brief seizure.
- It is primarily used for severe depression, treatment-resistant mood disorders, catatonia, and some forms of acute psychosis.
- The procedure is performed under general anesthesia with muscle relaxants to prevent injury.
- ECT has been shown to be highly effective, especially when rapid symptom relief is needed (e.g., suicidal ideation, refusal to eat).
- It is considered safe and well-tolerated, especially in older adults or those unable to take medications.
- ECT is typically administered 2–3 times per week.
- A full course usually consists of 6 to 12 sessions, depending on the client’s response and diagnosis.
- Maintenance ECT may be scheduled weekly or monthly to prevent relapse in chronic or recurrent cases.
- Timing is individualized based on clinical severity, response to treatment, and side effect profile (e.g., memory changes).
- Pre-treatment fasting is required (usually 6–8 hours) due to anesthesia.
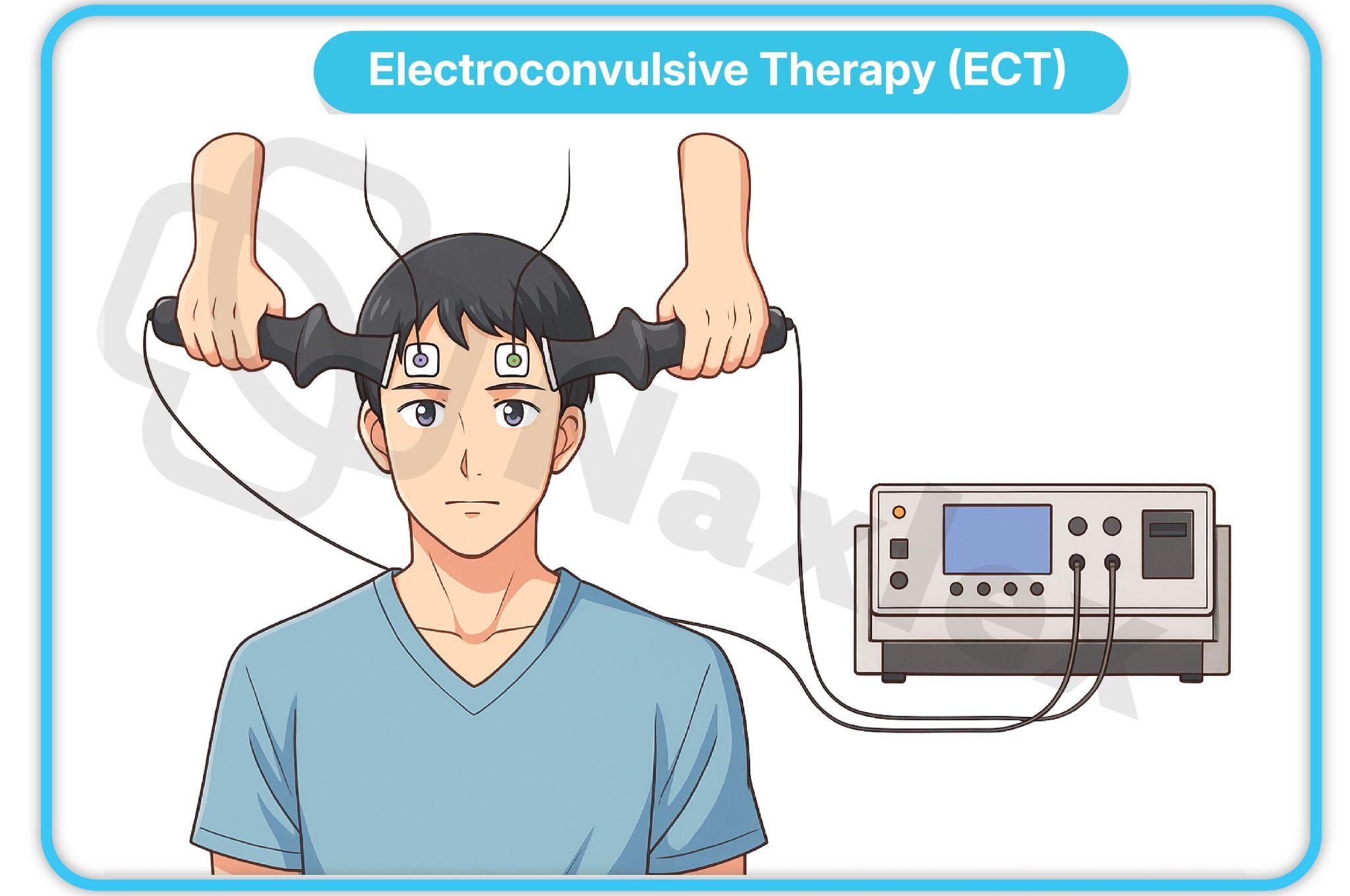
-
- Indications for ECT include:
- Severe, treatment-resistant depression.
- Depression with psychotic features.
- Severe psychomotor retardation or stupor.
- Situations where a rapid response is needed (e.g., for a patient with severe suicidal ideation or catatonia).
- Patients who cannot tolerate or do not respond to pharmacotherapy.
- Contraindications:
- Absolute contraindication: Increased intracranial pressure
- Relative contraindications: Recent MI, CVA, unstable cardiac conditions
- Pre-procedure:
- The nurse's role includes a comprehensive pre-procedure assessment, including a history of past ECT, allergies, and baseline vital signs.
- Pre-ECT evaluation includes cardiac clearance, neuro exam, and informed consent
- Medications administered: A short-acting anesthetic (e.g., Propofol) is given to induce unconsciousness, and a muscle relaxant (e.g., Succinylcholine) is given to prevent motor convulsions. Atropine may be given to decrease secretions.
- During the procedure:
- The nurse assists the anesthesiologist and psychiatrist, monitors vital signs, and ensures the patient's airway is protected.
- Electrodes are placed on the scalp to induce a generalized seizure.
- Post-procedure care:
- The patient is monitored in the recovery area until they are fully awake and stable.
- The nurse assesses for confusion, memory loss, headache, or muscle soreness.
- Reorientation and reassurance are crucial.
- Potential side effects:
- Memory Loss: Retrograde and anterograde amnesia is the most common side effect. It is usually temporary, but some memory gaps may be permanent.
- Headache, muscle soreness, and nausea.
- Indications for ECT include:
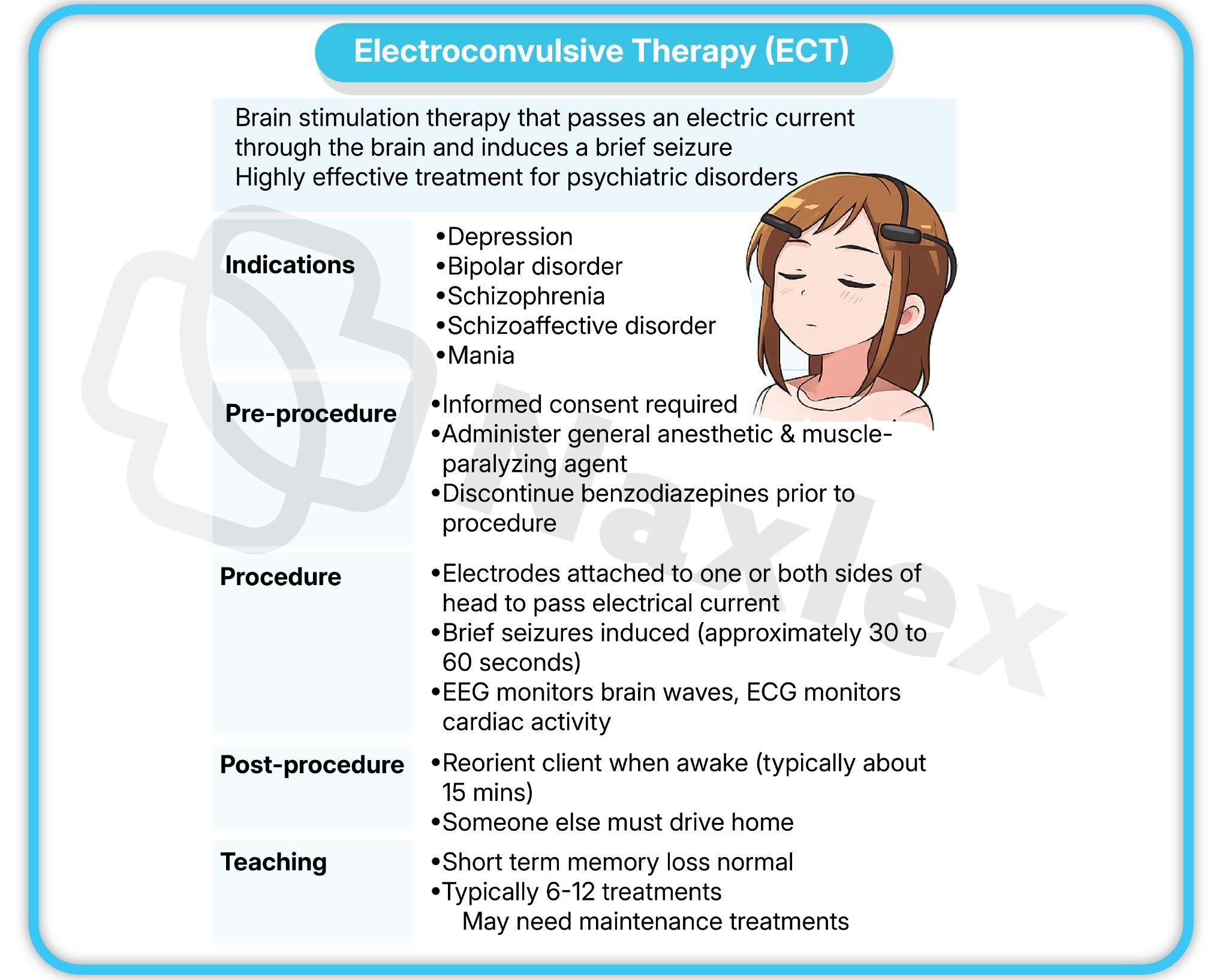
-
- Nursing Responsibilities
- Ensure NPO status 6–8 hours prior
- Administer prescribed pre-ECT medications (e.g., atropine to reduce secretions)
- Monitor vital signs, oxygenation, and mental status post-procedure
- Provide emotional support and education to client and family
- Document response to treatment and any adverse effects
- Nursing Responsibilities
- Transcranial Magnetic Stimulation (TMS)
- Mechanism: A non-invasive procedure that uses a magnetic field to generate an electric current in a specific area of the brain, usually the prefrontal cortex.
- Indications and uses: Approved for Major Depressive Disorder in adults who have not responded to at least one antidepressant medication.
- Side effects: Generally well-tolerated. The most common side effect is a mild to moderate headache at the site of stimulation. Seizures are a very rare but serious risk.
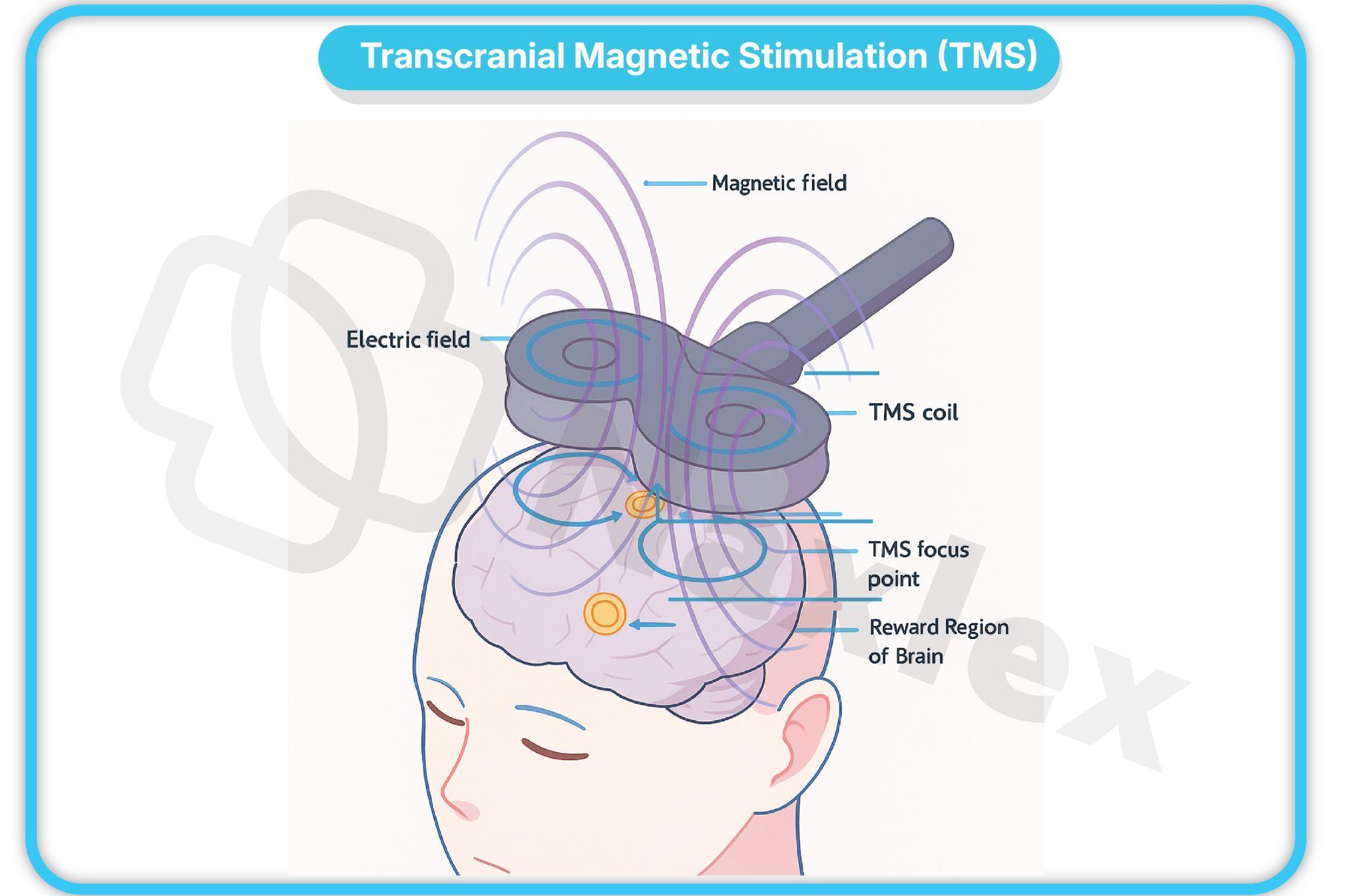
- Psychotherapy
- Psychotherapy is a cornerstone of depression treatment, often used in conjunction with medication.
- Cognitive Behavioral Therapy (CBT):
- A structured, goal-oriented therapy that focuses on identifying and changing negative thought patterns and behaviors.
- The therapist helps the patient challenge and reframe cognitive distortions.
- Interpersonal Therapy (IPT):
- A time-limited therapy that focuses on the patient's current interpersonal relationships and social roles.
- It addresses four key problem areas: grief, role disputes, role transitions, and interpersonal deficits.
- Psychodynamic approaches:
- Explores how past experiences and unconscious conflicts contribute to current depressive symptoms.
- Group therapy and family therapy:
- Group therapy: Provides a forum for patients to share experiences, receive support, and learn from others.
- Family therapy: Involves the family in the treatment process, addressing family dynamics that may contribute to or maintain the depression.
- Other Somatic Treatments
- Light therapy (for seasonal depression):
- Used to treat Seasonal Affective Disorder (SAD) by exposing the patient to a specific type of light.
- The light box simulates sunlight, helping to regulate the patient's circadian rhythm and increase serotonin levels.
- Vagus Nerve Stimulation (VNS):
- An implantable device that sends electrical signals to the brain via the vagus nerve.
- It is approved for chronic or recurrent treatment-resistant depression.
- Light therapy (for seasonal depression):
Contributing Factors
1.1 Biological:
- Genetics: As family history of depression significantly increases risk.
- Neurobiology: Dysregulation of neurotransmitters (serotonin, norepinephrine, dopamine) and structural/functional changes in brain regions like the hippocampus and prefrontal cortex.
- Endocrine: Hormonal changes, such as those associated with the peripartum period or thyroid dysfunction. Overactivity of the HPA axis and elevated cortisol levels are common in depression.
- Inflammatory Markers: The emerging field of psychoneuroimmunology suggests that chronic inflammation, measured by markers like C-reactive protein, may play a role in the pathophysiology of depression.
1.2 Psychological:
- Personality Traits: Neuroticism, low self-esteem, and a pessimistic outlook are all predisposing psychological factors.
- Maladaptive Coping: Using ineffective or unhealthy coping mechanisms, such as avoidance, rumination, or substance use.
- Cognitive Distortions: The negative thinking patterns described by Aaron Beck, including negative views of self, world, and future.
1.3 Social/Environmental:
- Trauma and Loss: Adverse childhood experiences (ACEs), major life stressors, and significant losses (e.g., loss of a loved one or a job).
- Poverty: Financial stress and lack of access to resources can be significant stressors that contribute to depression.
- Lack of Support: Social isolation
Summary
- Depressive disorders are a heterogeneous group of conditions characterized by a persistent low mood and a loss of interest or pleasure, causing significant functional impairment.
- The DSM-5-TR delineates several types, including Major Depressive Disorder (MDD), Persistent Depressive Disorder (Dysthymia), Disruptive Mood Dysregulation Disorder (DMDD), and Premenstrual Dysphoric Disorder (PMDD).
- Diagnosis is based on specific criteria, and severity is classified as mild, moderate, or severe.
- Underlying theories of depression involve a complex interplay of biological factors, such as neurotransmitter dysregulation and HPA axis abnormalities, and psychosocial factors, including negative cognitive schemas and interpersonal difficulties.
- The nursing process in depression care begins with a comprehensive assessment that includes an evaluation of affective, cognitive, behavioral, and physiological symptoms.
- This assessment must always prioritize suicide risk. Nurses use standardized screening tools like the PHQ-9 and BDI to inform their evaluation.
- Based on the assessment, the nurse formulates individualized nursing diagnoses, identifies SMART outcomes, and plans and implements a wide range of interventions.
- These interventions include providing a safe environment, promoting self-care, educating the patient and family, and using therapeutic communication.
- Treatment for depression is multifaceted and often involves a combination of pharmacotherapy and psychotherapy.
- Antidepressants, particularly SSRIs and SNRIs, are the first-line pharmacological treatment. For treatment-resistant cases, more intensive somatic therapies like Electroconvulsive Therapy (ECT) and Transcranial Magnetic Stimulation (TMS) may be used.
- Psychotherapies, such as Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT), are crucial for addressing underlying cognitive and interpersonal factors.
- The nurse plays a pivotal role in every stage of the care process, from initial assessment and risk management to patient education and the coordination of care, ultimately aiming to help the patient achieve remission and regain a sense of hope and well-being.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Depressive Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


