Please set your exam date
Bleeding
Study Questions
Practice Exercise 1
A nurse is educating a patient about implantation bleeding. Which statement is accurate?
Explanation
Implantation bleeding occurs when the fertilized blastocyst embeds into the endometrial lining, typically 6–12 days post-ovulation. This process involves vascular disruption, endometrial invasion, hormonal shifts, and trophoblast activity. It is usually light, painless, and self-limiting. Estrogen and progesterone levels rise rapidly, supporting decidualization. No intervention is needed unless bleeding is heavy or persistent.
Rationale for correct answer
3. Implantation bleeding is typically light and brief, often described as spotting that lasts 1–2 days. The question stem asks for an accurate statement, and this matches the expected clinical presentation. It occurs due to minor endometrial capillary disruption during blastocyst embedding.
Rationale for incorrect answers
1. Implantation bleeding does not occur 6–10 weeks after conception. By this time, the placenta is forming and hCG levels are rising. Bleeding at this stage may indicate other causes such as threatened miscarriage or ectopic pregnancy. Implantation occurs around day 6–12 post-ovulation, not weeks later.
2. Heavy bleeding with severe cramping is not characteristic of implantation. This presentation suggests pathologic processes like miscarriage or ectopic pregnancy. Implantation bleeding is painless or mildly uncomfortable, never associated with significant uterine contractions or blood loss.
4. Implantation bleeding does not require surgical intervention. It is a physiologic event, not a surgical emergency. Surgical management is reserved for complications such as ruptured ectopic pregnancy or retained products of conception, which present differently.
Take home points
- Implantation bleeding occurs 6–12 days post-ovulation, not weeks after conception.
- It is light, brief, and self-limiting, typically lasting 1–2 days.
- Heavy bleeding or cramping suggests other causes like miscarriage or ectopic pregnancy.
- Implantation bleeding does not require any medical or surgical intervention.
Which clinical feature best differentiates implantation bleeding from a threatened miscarriage?
Explanation
Implantation bleeding vs threatened miscarriage involves distinguishing between a benign post-conception event and a potentially pathologic early pregnancy complication. Timing, duration, bleeding pattern, and cervical status are critical. Implantation bleeding occurs 6–12 days post-ovulation due to endometrial capillary disruption. Threatened miscarriage presents with persistent bleeding, cramping, and a closed cervix, but may progress. Serum hCG levels and transvaginal ultrasound help differentiate.
Rationale for correct answer
1. Implantation bleeding presents as light spotting that resolves within 48 hours. It is due to minor vascular disruption during blastocyst embedding into the endometrium. The absence of pain, tissue passage, or cervical changes supports a benign process. This feature best differentiates it from a threatened miscarriage, which involves prolonged bleeding and uterine activity.
Rationale for incorrect answers
2. Passage of clots with severe cramping is not consistent with implantation bleeding. These findings suggest uterine contractions and decidual shedding, which are hallmark features of an evolving miscarriage. Implantation bleeding does not involve clot formation or significant pain.
3. Cervical dilation is not seen in implantation bleeding. Dilation indicates mechanical opening of the cervix, often due to expulsion forces from the uterus. This is diagnostic of inevitable or incomplete miscarriage, not a benign implantation event.
4. Persistent bleeding with open os is a clinical sign of miscarriage progression. The open os allows passage of products of conception, and ongoing bleeding reflects active tissue disruption. Implantation bleeding is transient and does not alter cervical integrity.
Take home points
- Implantation bleeding is light, brief, and self-limiting, typically resolving within 48 hours.
- Threatened miscarriage involves persistent bleeding, cramping, and a closed cervix.
- Cervical dilation or open os indicates miscarriage progression, not implantation.
- Clots and pain are not features of implantation bleeding.
Which diagnostic test is most reliable for confirming an intrauterine pregnancy in a patient with early bleeding?
Explanation
Confirmation of intrauterine pregnancy requires direct visualization of the gestational sac within the endometrial cavity. Transvaginal ultrasound, performed between 4–6 weeks gestation, provides high-resolution imaging capable of detecting a yolk sac, fetal pole, and cardiac activity. It distinguishes intrauterine from ectopic pregnancy. Beta-hCG correlation, endometrial location, and embryonic structures are critical for confirmation. A gestational sac is typically visible when serum beta-hCG exceeds 1,500 mIU/mL.
Rationale for correct answer
2. Transvaginal ultrasound is the most reliable method for confirming intrauterine pregnancy. It allows direct visualization of the gestational sac within the uterus, ruling out ectopic implantation. In early bleeding, this modality confirms location, viability, and presence of embryonic structures, making it diagnostic.
Rationale for incorrect answers
1. Complete blood count does not confirm pregnancy. It evaluates hemoglobin and white cell count, useful for assessing anemia or infection. It provides no information on gestational location or viability and is not diagnostic for pregnancy status.
3. Serum progesterone level reflects corpus luteum function and pregnancy support but does not confirm intrauterine location. Low levels may suggest nonviable pregnancy, but normal levels can occur in ectopic gestation. It lacks specificity for intrauterine confirmation.
4. Urine pregnancy test detects hCG presence but cannot determine implantation site. It confirms pregnancy status, not location. False negatives may occur in early gestation, and positive results do not exclude ectopic pregnancy.
Take home points
- Transvaginal ultrasound confirms intrauterine pregnancy by visualizing gestational structures.
- Serum progesterone and urine hCG indicate pregnancy but not location.
- CBC is not diagnostic for pregnancy; it assesses systemic parameters.
- Ectopic pregnancy must be excluded in early bleeding using ultrasound.
Which findings are consistent with implantation bleeding? Select all that apply.
Explanation
Implantation bleeding occurs during early embryonic development when the blastocyst embeds into the endometrial lining, typically 6–12 days post-ovulation. It results from endometrial capillary disruption, triggered by trophoblast invasion, progesterone surge, and decidual reaction. Bleeding is light, painless, and self-limiting. No systemic symptoms or tissue passage occur. Serum beta-hCG may begin rising but remains <50 mIU/mL initially.
Rationale for correct answers
1. Brown or pink spotting reflects minimal bleeding from superficial capillary disruption. The color indicates oxidized blood, typical of implantation. It is not fresh red bleeding and lacks volume or clot formation.
2. Duration less than 2 days is consistent with implantation bleeding. The brief timeframe corresponds to the limited extent of vascular injury during blastocyst embedding. Bleeding typically resolves spontaneously without intervention.
5. No passage of tissue or clots confirms benign nature. Implantation bleeding involves capillary oozing, not decidual shedding. Absence of clots or tissue rules out miscarriage or molar pregnancy.
Rationale for incorrect answers
3. Severe pelvic pain and hypotension are not features of implantation bleeding. These signs suggest hemodynamic instability and visceral irritation, commonly seen in ruptured ectopic pregnancy or ovarian torsion. Implantation bleeding is painless or mildly uncomfortable.
4. Passage of grape-like vesicles indicates molar pregnancy. These vesicles represent hydropic villi due to abnormal trophoblastic proliferation. Implantation bleeding never involves vesicular tissue or excessive hCG levels (>100,000 mIU/mL).
Take home points
- Implantation bleeding is light, brief, and painless, typically resolving within 48 hours.
- No clots, tissue, or systemic symptoms are present in implantation bleeding.
- Severe pain or hypotension suggests ectopic pregnancy or other pathology.
- Grape-like vesicles indicate molar pregnancy, not implantation.
Practice Exercise 2
A 28-year-old G1P0 woman at 8 weeks gestation presents to the emergency department with light vaginal spotting and mild abdominal cramping. On examination, the cervix is closed, and the fetal heart rate is detectable by ultrasound. What type of spontaneous abortion is the patient most likely experiencing?
Explanation
Threatened abortion refers to early pregnancy bleeding with a closed cervix and a viable intrauterine pregnancy. It results from decidual disruption, subchorionic hemorrhage, or hormonal insufficiency. The cervix remains closed, fetal cardiac activity is present, and bleeding is usually light. Symptoms include mild cramping and spotting. Beta-hCG levels typically rise appropriately, and ultrasound confirms viability.
Rationale for correct answer
3. Threatened abortion is defined by vaginal bleeding before 20 weeks gestation with a closed cervix and detectable fetal heart rate. The patient presents with mild cramping and light spotting, and ultrasound confirms viability. These findings match the clinical criteria for threatened abortion.
Rationale for incorrect answers
1. Inevitable abortion involves vaginal bleeding with an open cervix and often visible products of conception. The cervix in this case is closed, and fetal heart rate is present, ruling out inevitable abortion. Uterine contractions may also be present in inevitable cases.
2. Incomplete abortion presents with passage of tissue, persistent bleeding, and an open cervix. Ultrasound typically shows retained products. The presence of fetal cardiac activity and absence of tissue passage exclude incomplete abortion.
4. Missed abortion is characterized by absence of fetal cardiac activity despite retained products and a closed cervix. The patient in this case has a detectable fetal heart rate, excluding missed abortion. Bleeding may be minimal or absent in missed abortion.
Take home points
- Threatened abortion presents with bleeding, closed cervix, and viable fetus.
- Inevitable abortion involves open cervix and active expulsion of products.
- Incomplete abortion includes tissue passage and retained products.
- Missed abortion shows no fetal cardiac activity with retained products.
Which of the following is the leading cause of spontaneous abortion, particularly in the first trimester?
Explanation
Spontaneous abortion is the loss of a pregnancy before 20 weeks gestation, most commonly occurring in the first trimester. The most frequent cause is chromosomal abnormalities, which account for over 50% of cases. These errors arise during gametogenesis, fertilization, or early embryonic development. Common types include trisomy, monosomy, and polyploidy. Clinically, patients present with vaginal bleeding, cramping, and passage of tissue. Risk increases with advanced maternal age, especially over 35 years. Other relevant causes include uterine anomalies, infections, and endocrine dysfunction, but these are less common in early losses.
Rationale for correct answer
3. Chromosomal abnormalities are the most frequent cause of first trimester spontaneous abortion, responsible for approximately 50% to 70% of cases. These include autosomal trisomies (especially trisomy 16), monosomy X (Turner syndrome), and triploidy. The question specifies “leading cause,” making this the scientifically accurate choice. Trisomy and monosomy are the most implicated.
Rationale for incorrect answers
1. Maternal infections such as toxoplasmosis, rubella, cytomegalovirus, and herpes simplex virus can cause miscarriage, but they are more commonly associated with second trimester losses or fetal anomalies. In the first trimester, their contribution is significantly lower. TORCH pathogens and vertical transmission are relevant but not predominant.
2. Uterine abnormalities like septate uterus, fibroids, or adhesions (Asherman syndrome) can impair implantation or placental development, leading to miscarriage. However, these structural issues typically cause recurrent pregnancy loss or second trimester abortions. Anatomic defects and implantation failure are less common in early loss.
4. Endocrine disorders such as uncontrolled diabetes mellitus, luteal phase defects, or thyroid dysfunction can contribute to miscarriage, but they are not the leading cause. Their impact is more pronounced in recurrent losses or later gestational failures. Hormonal imbalance and thyroid dysfunction are contributory but not primary.
Take home points
- Chromosomal abnormalities are the most common cause of first trimester spontaneous abortion.
- Trisomy 16, monosomy X, and triploidy are the most frequent genetic errors.
- Uterine anomalies and infections are more associated with second trimester losses.
- Endocrine disorders contribute to miscarriage but are not the leading cause.
A patient presents with a missed abortion at 10 weeks gestation. The nurse understands that this condition carries a risk of which potential complication if the products of conception are retained for a prolonged period?
Explanation
Missed abortion involves retention of nonviable products of conception beyond 4 weeks, increasing risk of coagulopathy, particularly disseminated intravascular coagulation (DIC). The retained fetal tissue releases thromboplastin, triggering systemic coagulation cascade activation. This leads to widespread microthrombi, consumption of clotting factors, and secondary bleeding. Platelets drop below 100,000/mm³, fibrinogen falls under 150 mg/dL, and D-dimer levels rise. DIC may present with petechiae, bleeding gums, hematuria, and hypotension. It is a life-threatening emergency requiring rapid correction of underlying cause and replacement of clotting factors.
Rationale for correct answer
3. Retained products of conception beyond 4 weeks release thromboplastin, activating the extrinsic coagulation pathway. This leads to systemic fibrin deposition and consumption of platelets and clotting factors, resulting in DIC. The question stem specifies prolonged retention after missed abortion, which directly correlates with this pathophysiology.
Rationale for incorrect answers
1. Placenta previa involves abnormal placental implantation over the cervical os, typically diagnosed via ultrasound in the second or third trimester. It is unrelated to retained products in early pregnancy and does not result from missed abortion. No pathophysiologic link exists between retained fetal tissue and placental migration.
2. Ectopic pregnancy occurs when implantation happens outside the uterine cavity, most commonly in the fallopian tube. It presents with abdominal pain and vaginal bleeding, often before 8 weeks gestation. Missed abortion implies intrauterine pregnancy loss, not ectopic implantation, making this option pathologically incompatible.
4. Preterm labor refers to uterine contractions leading to cervical changes before 37 weeks gestation. It is associated with infections, uterine overdistension, or cervical insufficiency. In missed abortion, fetal demise has already occurred, and uterine activity is typically absent unless induced. Retained tissue does not trigger preterm labor mechanisms.
Take home points
- Missed abortion with retained products beyond 4 weeks increases risk of DIC due to thromboplastin release.
- DIC presents with bleeding, low platelets, elevated D-dimer, and low fibrinogen.
- Placenta previa and ectopic pregnancy are anatomically distinct and unrelated to retained intrauterine tissue.
- Preterm labor requires viable pregnancy and uterine contractions, absent in missed abortion.
Which of the following are common clinical manifestations of a spontaneous abortion? Select all that apply.
Explanation
Spontaneous abortion refers to the natural loss of a pregnancy before 20 weeks gestation. It results from chromosomal abnormalities, maternal infections, uterine anomalies, or hormonal insufficiency. Clinical signs include vaginal bleeding, cramping, and passage of tissue. Ultrasound may show absence of fetal cardiac activity. Serum hCG levels decline, and cervical dilation may be present. Types include threatened, inevitable, incomplete, complete, and missed abortion. Infection may occur if retained products persist, but fever is not a primary feature unless sepsis develops.
Rationale for correct answers
1. Vaginal bleeding is the most common initial symptom of spontaneous abortion. It results from decidual separation and endometrial disruption. Bleeding may range from spotting to heavy flow with clots, depending on the stage and type of abortion.
3. Passage of tissue occurs in incomplete or complete abortion. Expulsion of products of conception confirms uterine evacuation. Tissue may include fetal parts or placental fragments, often accompanied by cramping and cervical dilation.
5. Absence of fetal heart tones on ultrasound indicates embryonic or fetal demise. In viable pregnancies, cardiac activity is detectable by 6 to 7 weeks. Lack of cardiac motion and embryonic growth confirms nonviability.
Rationale for incorrect answers
2. Absence of abdominal pain is not typical. Most spontaneous abortions involve uterine cramping due to myometrial contractions expelling tissue. Pain may be mild to severe and often correlates with cervical dilation and tissue passage.
4. Fever without other symptoms is not a common manifestation of spontaneous abortion. Fever suggests infection, such as septic abortion, which presents with uterine tenderness, foul-smelling discharge, and systemic signs. In uncomplicated abortion, fever is absent unless retained tissue becomes infected.
Take home points
- Vaginal bleeding and cramping are hallmark signs of spontaneous abortion.
- Absence of fetal heart tones confirms nonviability in early pregnancy.
- Passage of tissue indicates incomplete or complete abortion.
Which factors are considered environmental or lifestyle contributors to an increased risk of spontaneous abortion? Select all that apply.
Explanation
Spontaneous abortion is the natural termination of pregnancy before 20 weeks gestation due to genetic abnormalities, maternal health factors, environmental exposures, or lifestyle risks. Risk increases with toxins, substance use, obesity, and maternal infections. Chromosomal anomalies account for over 50% of first-trimester losses. Elevated BMI >30, teratogenic exposures (e.g. lead, mercury), and drugs like cocaine or methamphetamine disrupt placental perfusion and fetal development. Smoking increases miscarriage risk by 1.2 to 1.8 times. Alcohol impairs trophoblast function and implantation.
Rationale for correct answers
2. Exposure to environmental toxins such as lead and mercury interferes with embryogenesis and placental development. These agents induce oxidative stress and DNA damage, increasing miscarriage risk. Industrial solvents and pesticides also impair fetal viability through endocrine disruption.
4. Illicit drug use, especially cocaine and methamphetamine, causes vasoconstriction and placental insufficiency. These substances reduce uteroplacental blood flow, leading to fetal hypoxia and spontaneous abortion. Cannabis and opioids also impair implantation and trophoblast invasion.
5. Obesity (BMI >30) alters hormonal regulation and increases inflammatory cytokines, disrupting endometrial receptivity. Hyperinsulinemia and leptin resistance impair implantation and early placental development. Obese women have up to 2-fold increased risk of miscarriage.
Rationale for incorrect answers
1. Advanced paternal age (>40 years) is associated with increased risk of genetic mutations and autism spectrum disorders, but its link to spontaneous abortion is weak. Sperm DNA fragmentation may contribute, but maternal factors dominate miscarriage risk. No strong epidemiologic evidence supports paternal age as a primary cause.
3. Regular moderate exercise improves placental perfusion and reduces inflammatory markers. It enhances insulin sensitivity and cardiovascular health, lowering miscarriage risk. Only excessive or high-impact activity in high-risk pregnancies may pose concern. Moderate aerobic activity is protective, not harmful.
Take home points
- Environmental toxins like lead and mercury increase miscarriage risk via oxidative damage.
- Illicit drugs impair placental perfusion and fetal oxygenation.
- Obesity disrupts hormonal balance and endometrial receptivity.
- Moderate exercise is protective, not a risk factor for spontaneous abortion.
Practice Exercise 3
What is the primary mechanism of action of mifepristone when used for medical abortion?
Explanation
Mifepristone is a synthetic steroid used for medical abortion. It works by antagonizing progesterone receptors, leading to decidual breakdown, cervical softening, and increased uterine sensitivity to prostaglandins. Progesterone is essential for maintaining pregnancy by stabilizing the endometrium and suppressing uterine contractions. Mifepristone is typically followed by misoprostol to induce uterine expulsion. Side effects include bleeding, cramping, nausea, and diarrhea. Contraindications include ectopic pregnancy, chronic adrenal failure, and long-term corticosteroid use.
Rationale for correct answer
3. Mifepristone blocks progesterone receptors, disrupting the hormonal support required to maintain the endometrial lining. This leads to decidual necrosis and detachment of the trophoblast. The question asks for the primary mechanism, which is receptor blockade, not downstream effects. This action initiates the abortion process before prostaglandins are administered.
Rationale for incorrect answers
1. Mifepristone does not directly induce uterine contractions. That role is fulfilled by misoprostol, a prostaglandin E1 analog given after mifepristone. While mifepristone increases uterine sensitivity to prostaglandins, its primary action is hormonal antagonism, not myometrial stimulation.
2. Mifepristone is not a prostaglandin analog. It is a steroidal compound that acts on hormone receptors, not prostaglandin pathways. Misoprostol, given after mifepristone, is the prostaglandin analog responsible for uterine contractions and cervical dilation.
4. Mifepristone does not inhibit folic acid synthesis. That mechanism is associated with drugs like methotrexate, which is used in ectopic pregnancy management. Mifepristone acts on progesterone, not folate metabolism, and has no antifolate properties.
Take home points
- Mifepristone blocks progesterone receptors to initiate medical abortion.
- Misoprostol is used after mifepristone to induce uterine contractions.
- Methotrexate inhibits folic acid synthesis and is used in ectopic pregnancy.
- Progesterone maintains pregnancy by stabilizing the endometrium and suppressing contractions.
Dilation and Evacuation (D&E) is typically the surgical method of choice for which gestational age range of pregnancy termination?
Explanation
Dilation and Evacuation (D&E) is a surgical technique used for second-trimester pregnancy termination. It involves cervical dilation, evacuation of uterine contents, and use of suction and forceps. It is preferred between 14 to 24 weeks due to fetal size and ossification. Risks include hemorrhage, uterine perforation, and infection. Cervical preparation with osmotic dilators or misoprostol is essential to reduce trauma. D&E is contraindicated in viable pregnancies and requires ultrasound guidance for safety.
Rationale for correct answer
3. D&E is the standard method for termination between 14 to 24 weeks gestation due to increased fetal size and calcification. At this stage, suction curettage alone is insufficient, and forceps are needed for complete evacuation. The question asks for the gestational age range where D&E is typically used, which aligns precisely with this window.
Rationale for incorrect answers
1. D&E is not used for pregnancies less than 6 weeks. At this early stage, the gestational sac is small and easily removed by manual vacuum aspiration or medical abortion using mifepristone and misoprostol. Surgical instrumentation is unnecessary and increases risk without benefit.
2. Between 6 to 10 weeks, suction curettage or medical abortion is preferred. The uterine contents are soft and easily evacuated without the need for forceps. D&E is excessive and not standard practice in this gestational range.
4. Beyond 28 weeks, termination is legally and ethically complex and typically involves induction abortion or cesarean delivery. D&E is contraindicated due to fetal viability and increased risk of uterine rupture and maternal morbidity. Surgical evacuation at this stage is rarely performed and not considered standard.
Take home points
- D&E is preferred for pregnancy termination between 14 to 24 weeks.
- Earlier gestations use suction curettage or medical abortion.
- Beyond 28 weeks, induction or cesarean is used due to fetal viability.
- Cervical preparation is essential before D&E to prevent trauma.
When is vacuum aspiration most commonly used as a method for induced abortion?
Explanation
Vacuum aspiration is a surgical method used for early pregnancy termination. It involves suction evacuation of uterine contents using a manual or electric vacuum source. It is most effective between 5 to 12 weeks gestation. The procedure requires cervical dilation, carries low risk of infection, and has a complication rate below 1%. It is contraindicated in ectopic pregnancy, coagulopathy, and severe pelvic infection. Compared to medical abortion, vacuum aspiration offers immediate completion and tissue confirmation.
Rationale for correct answer
1. Vacuum aspiration is most commonly used in the first trimester, specifically between 5 to 12 weeks gestation. At this stage, the uterine contents are soft and easily evacuated by suction. The question asks for the most common use, which aligns with early gestational termination where vacuum aspiration is standard.
Rationale for incorrect answers
2. In the second trimester, fetal size and ossification increase, making vacuum aspiration less effective. Dilation and evacuation (D&E) becomes the preferred method due to the need for forceps and ultrasound guidance. Vacuum aspiration is not routinely used beyond 12 weeks due to incomplete evacuation risks.
3. During the third trimester, termination is rare and legally restricted. Methods include induction abortion or cesarean delivery, not vacuum aspiration. The fetal size and viability make suction techniques inappropriate and unsafe. Vacuum aspiration is contraindicated due to high risk of uterine rupture and maternal morbidity.
4. Post-term pregnancy refers to gestation beyond 42 weeks, where termination is managed by labor induction or cesarean section. Vacuum aspiration has no role in post-term management. The uterus is large, the fetus is viable, and suction evacuation is neither effective nor safe.
Take home points
- Vacuum aspiration is preferred for abortion between 5 to 12 weeks gestation.
- D&E is used for second trimester termination due to fetal size.
- Third trimester termination requires induction or cesarean delivery.
- Post-term pregnancy is not managed with vacuum aspiration.
A nurse is preparing a patient for a medical abortion. What information should the nurse include in the education regarding what to expect? Select all that apply.
Explanation
Medical abortion involves pharmacologic termination of pregnancy using agents that induce uterine contractions and cervical dilation. The standard regimen includes mifepristone, a progesterone antagonist, followed by misoprostol, a prostaglandin E1 analog. Misoprostol causes uterine cramping, bleeding, and gastrointestinal effects. Expulsion typically occurs within 24 to 48 hours. Follow-up is essential to confirm complete evacuation and rule out retained products. Pain intensity varies, and analgesics are often required. Hemoglobin should be monitored if bleeding exceeds 500 mL.
Rationale for correct answers
1. Severe cramping and heavy bleeding are expected due to uterine contractions induced by misoprostol and decidual shedding. These mimic labor-like symptoms and are necessary for complete expulsion of the gestational sac. The question stem asks what to expect, and this is a physiologic response to the medication.
3. Follow-up is essential to confirm complete abortion and exclude retained products of conception, which can lead to infection or hemorrhage. Ultrasound or serial β-hCG levels are used. The question tests knowledge of post-abortion care, and this is a standard protocol.
4. Misoprostol commonly causes nausea and diarrhea due to its prostaglandin activity on smooth muscle. These side effects are dose-dependent and transient. The question asks about expected effects, and these are well-documented.
Rationale for incorrect answers
2. Expulsion is rarely immediate and never painless. Misoprostol induces strong uterine contractions and cervical dilation, which cause significant discomfort. Expulsion typically occurs within 24 to 48 hours, not instantly. The claim of painless and immediate expulsion contradicts the pharmacologic mechanism.
5. Pain medication is often required due to cramping and uterine contractions. NSAIDs like ibuprofen are commonly prescribed. The statement that no pain medication is needed is inaccurate and disregards patient comfort and standard practice.
Take home points
- Misoprostol causes cramping, bleeding, and gastrointestinal side effects during medical abortion.
- Follow-up is mandatory to confirm complete uterine evacuation.
- Pain management is essential; NSAIDs are commonly used.
- Medical abortion differs from surgical abortion in timing, symptoms, and monitoring.
Which of the following are methods used for induced abortion? Select all that apply.
Explanation
Induced abortion involves the deliberate termination of a pregnancy using medical or surgical techniques. The uterine contents are evacuated through either pharmacologic agents or mechanical procedures. Common methods include vacuum aspiration, medical induction, and dilation and curettage, depending on gestational age. Prostaglandins like misoprostol stimulate uterine contractions, while surgical methods physically remove products of conception. Indications include maternal health risks, fetal anomalies, or personal choice. Gestational age determines method: medical induction is preferred before 12 weeks, while D&C and vacuum aspiration are used up to 14 weeks. Complications include hemorrhage, infection, and uterine perforation.
Rationale for correct answers
1. Vacuum aspiration is a standard surgical method for induced abortion, especially effective between 6 and 14 weeks gestation. It uses suction to evacuate the uterine contents. It is associated with low complication rates and is widely used due to its efficacy and safety.
3. Medical induction with prostaglandins, such as misoprostol or mifepristone, is a recognized method for early abortion. These agents cause cervical softening and uterine contractions, leading to expulsion of the embryo or fetus. It is preferred in pregnancies under 12 weeks and is non-invasive.
4. Dilation and curettage (D&C) is a surgical abortion technique involving cervical dilation followed by scraping of the uterine lining. It is used for first-trimester abortions and post-abortion retained products. It provides direct visual control and is effective in complete evacuation.
Rationale for incorrect answers
2. Expectant management is not a method of induced abortion. It refers to watchful waiting in cases of spontaneous abortion or miscarriage, allowing the body to expel the products of conception naturally. It lacks active intervention and is inappropriate for elective termination.
5. Cerclage placement is a procedure used to prevent miscarriage or preterm birth in cases of cervical insufficiency. It involves placing a suture around the cervix to keep it closed. It is a pregnancy-preserving intervention, not a termination method, and contraindicated in abortion.
Take home points
- Induced abortion methods include medical and surgical approaches based on gestational age.
- Vacuum aspiration and D&C are surgical techniques used in early pregnancy termination.
- Prostaglandins like misoprostol are used for medical induction of abortion.
Practice Exercise 4
A nurse is caring for a patient with a suspected ectopic pregnancy. Which symptom requires immediate escalation of care?
Explanation
Ectopic pregnancy is a life-threatening condition where a fertilized ovum implants outside the uterine cavity, most commonly in the fallopian tube. Tubal rupture, hemorrhage, hypovolemia, and shock are critical complications. Symptoms include unilateral pelvic pain, vaginal bleeding, and signs of hemodynamic instability. Serum β-hCG levels may be lower than expected for gestational age. Transvaginal ultrasound confirms diagnosis. Rupture risk increases with gestational age and tubal distension.
Rationale for correct answer
3. Hypotension and tachycardia indicate hypovolemic shock due to intra-abdominal bleeding from a ruptured ectopic pregnancy. These are signs of circulatory compromise and require immediate surgical intervention. The presence of both vital sign abnormalities confirms systemic decompensation and mandates urgent escalation.
Rationale for incorrect answers
1. Light vaginal spotting is a common symptom in early pregnancy and may occur in ectopic pregnancy but does not indicate rupture or hemodynamic compromise. It reflects localized bleeding and lacks systemic signs. Without accompanying pain or instability, it does not warrant immediate escalation.
2. Mild cramping is nonspecific and may be seen in normal early pregnancy, implantation, or ectopic pregnancy. It lacks severity and does not suggest tubal rupture or internal bleeding. Absence of vital sign changes makes it a low-priority symptom.
4. Nausea and vomiting are common in early pregnancy due to rising hCG levels. They are not specific to ectopic pregnancy and do not indicate acute deterioration. Without abdominal pain or hemodynamic signs, they are not alarming in isolation.
Take home points
- Ectopic pregnancy can cause rapid hemodynamic collapse due to tubal rupture.
- Hypotension and tachycardia signal internal bleeding and require immediate intervention.
- Mild symptoms like spotting or cramping are not reliable indicators of rupture.
- Always prioritize signs of shock over localized symptoms in early pregnancy.
What is the primary medical treatment for an unruptured ectopic pregnancy in a hemodynamically stable patient?
Explanation
Medical management of unruptured ectopic pregnancy involves pharmacologic intervention to halt trophoblastic growth and preserve tubal integrity. Methotrexate, a folate antagonist, inhibits DNA synthesis, cell replication, and trophoblastic proliferation. It is used in hemodynamically stable patients with no signs of rupture, β-hCG < 5,000 IU/L, and no fetal cardiac activity. Tubal preservation, non-surgical approach, and monitoring of β-hCG levels are essential components. Contraindications include hepatic dysfunction, renal impairment, and breastfeeding.
Rationale for correct answer
2. Methotrexate is the first-line medical therapy for unruptured ectopic pregnancy in stable patients. It targets rapidly dividing trophoblastic cells, halting pregnancy progression. The patient must be hemodynamically stable, with no evidence of rupture, and meet strict criteria including β-hCG < 5,000 IU/L and absence of fetal cardiac activity.
Rationale for incorrect answers
1. Misoprostol is a prostaglandin E1 analog used for cervical ripening and uterine evacuation in intrauterine pregnancy loss. It does not target trophoblastic tissue and is ineffective in ectopic pregnancy. It cannot reach extrauterine implantation sites and does not prevent tubal rupture.
3. Oxytocin stimulates uterine contractions and is used in labor induction or postpartum hemorrhage. It has no role in ectopic pregnancy management because the uterus is not the implantation site. It does not affect tubal gestation or trophoblastic growth and may worsen pain without therapeutic benefit.
4. RhoGAM is an immunoglobulin used to prevent Rh sensitization in Rh-negative mothers after exposure to fetal Rh-positive blood. It does not treat ectopic pregnancy and has no effect on trophoblastic tissue. It is adjunctive only if the mother is Rh-negative, not a primary treatment.
Take home points
- Methotrexate is the drug of choice for stable, unruptured ectopic pregnancy.
- Misoprostol and oxytocin are ineffective in extrauterine gestation.
- RhoGAM prevents Rh sensitization but does not treat ectopic pregnancy.
- Always confirm eligibility criteria before administering methotrexate.
Which factor increases the risk of ectopic pregnancy?
Explanation
Risk factors for ectopic pregnancy include structural damage or functional impairment of the fallopian tubes, which disrupts normal embryo transport. Pelvic inflammatory disease, especially due to Chlamydia trachomatis or Neisseria gonorrhoeae, causes tubal scarring, adhesions, and ciliary dysfunction. Other contributors include prior tubal surgery, assisted reproductive techniques, and smoking. Tubal obstruction, delayed ovum transport, and abnormal implantation are central mechanisms. β-hCG levels may rise abnormally slow, and transvaginal ultrasound may show no intrauterine gestation despite positive pregnancy test.
Rationale for correct answer
1. History of pelvic inflammatory disease increases ectopic pregnancy risk due to tubal damage and scarring. Inflammation from pathogens like Chlamydia leads to fibrosis and impaired ciliary motion, preventing normal ovum migration. This predisposes to implantation outside the uterus, most commonly in the ampullary portion of the fallopian tube.
Rationale for incorrect answers
2. Regular prenatal care does not increase ectopic pregnancy risk. It is associated with early detection and preventive screening, improving maternal outcomes. It does not alter tubal anatomy or ovum transport and is protective rather than causative.
3. Maternal age <20 years is not a recognized independent risk factor for ectopic pregnancy. Younger age may correlate with higher STI exposure, but without documented PID, the risk remains low. Age alone does not impair tubal function or increase implantation outside the uterus.
4. Normal uterine anatomy supports proper implantation and does not contribute to ectopic pregnancy. Intact tubal patency and unobstructed endometrial cavity facilitate intrauterine gestation. Structural anomalies like septate uterus or tubal stenosis—not normal anatomy—are associated with abnormal implantation.
Take home points
- Pelvic inflammatory disease causes tubal scarring and increases ectopic pregnancy risk.
- Normal uterine anatomy does not predispose to ectopic implantation.
- Maternal age <20 years is not an independent risk factor without PID history.
- Regular prenatal care improves outcomes and does not increase ectopic risk.
A patient with early pregnancy bleeding reports shoulder pain. What does this suggest?
Explanation
Ectopic pregnancy is a potentially life-threatening condition where a fertilized ovum implants outside the uterine cavity, most commonly in the fallopian tube. Hemoperitoneum, referred pain, rupture, and shock are critical features. Tubal rupture leads to intraperitoneal bleeding, which irritates the diaphragm and causes shoulder pain. β-hCG levels may be lower than expected for gestational age. Transvaginal ultrasound may show an empty uterus with adnexal mass. Risk factors include prior ectopic pregnancy, pelvic inflammatory disease, and tubal surgery.
Rationale for correct answer
2. Shoulder pain in the context of early pregnancy bleeding strongly suggests diaphragmatic irritation from hemoperitoneum, a hallmark of ruptured ectopic pregnancy. The presence of referred pain indicates blood in the peritoneal cavity, which stimulates the phrenic nerve. This is a surgical emergency requiring immediate intervention.
Rationale for incorrect answers
1. Cervical friability refers to increased vascularity and fragility of the cervix, often seen in infections or hormonal changes. It may cause contact bleeding but does not lead to referred pain or hemoperitoneum. It is not associated with shoulder pain and does not present as an acute emergency.
3. Threatened miscarriage presents with vaginal bleeding and a closed cervical os. There is no intraperitoneal bleeding or diaphragmatic irritation, so shoulder pain is not expected. The uterus may still contain a viable pregnancy, and management is usually expectant unless bleeding worsens.
4. Molar pregnancy involves abnormal trophoblastic proliferation and elevated β-hCG levels. It presents with painless vaginal bleeding, uterine enlargement, and sometimes hyperemesis or preeclampsia. It does not cause hemoperitoneum or shoulder pain, as there is no rupture or blood in the peritoneal cavity.
Take home points
- Shoulder pain in early pregnancy bleeding suggests hemoperitoneum from ruptured ectopic pregnancy.
- Ectopic pregnancy must be differentiated from miscarriage and molar pregnancy.
- Transvaginal ultrasound and β-hCG levels are essential for diagnosis.
- Referred pain from diaphragmatic irritation is a red flag for internal bleeding.
Which symptoms are associated with an ectopic pregnancy? Select all that apply.
Explanation
Ectopic pregnancy occurs when a fertilized ovum implants outside the uterine cavity, most commonly in the ampullary portion of the fallopian tube. Tubal distension, rupture, hemoperitoneum, and referred pain are hallmark features. β-hCG levels typically rise slower than expected, and transvaginal ultrasound shows no intrauterine gestation. Hemodynamic instability, peritoneal irritation, and loss of gestational symptoms are critical indicators. Risk factors include prior pelvic inflammatory disease, tubal surgery, and assisted reproductive techniques.
Rationale for correct answers
1. Unilateral pelvic pain results from tubal distension or irritation due to the ectopic implantation. The pain is typically sharp and localized to one side, correlating with the site of implantation. It may worsen with movement or rupture.
2. Shoulder pain is a sign of referred diaphragmatic irritation from intra-abdominal bleeding. Blood in the peritoneal cavity irritates the phrenic nerve, causing pain perceived in the shoulder. This is a classic sign of ruptured ectopic pregnancy.
4. Loss of pregnancy symptoms occurs when trophoblastic activity declines, often due to nonviable implantation. Decreased β-hCG leads to resolution of nausea, breast tenderness, and fatigue. This suggests failed gestation and may precede rupture.
Rationale for incorrect answers
3. Heavy vaginal bleeding is not typical of ectopic pregnancy. Most patients experience light spotting due to hormonal withdrawal. Heavy bleeding suggests intrauterine miscarriage or cervical pathology, not tubal implantation. Ectopic rupture causes internal bleeding, not external hemorrhage.
5. Passage of grape-like vesicles is characteristic of hydatidiform mole, a form of gestational trophoblastic disease. It involves abnormal proliferation of chorionic villi, not ectopic implantation. β-hCG levels are markedly elevated, and ultrasound shows a snowstorm pattern, not an empty uterus.
Take home points
- Unilateral pelvic pain and shoulder pain are hallmark signs of ectopic pregnancy.
- Loss of pregnancy symptoms may indicate nonviable ectopic gestation.
- Heavy vaginal bleeding is more typical of intrauterine miscarriage.
- Grape-like vesicles suggest molar pregnancy, not ectopic implantation.
Practice Exercise 5
Which condition is characterized by abnormal placental growth and the passage of grape-like vesicles?
Explanation
Molar pregnancy is a gestational trophoblastic disease caused by abnormal fertilization resulting in a nonviable pregnancy. It involves trophoblastic proliferation, hydropic villi, absence of fetal tissue, and excessive hCG. Complete moles arise from fertilization of an empty ovum by one sperm that duplicates (46XX) or two sperms (46XY), while partial moles result from fertilization of a normal ovum by two sperms (69XXY or 69XXX). Symptoms include vaginal bleeding, uterine enlargement greater than gestational age, and passage of grape-like vesicles. Serum hCG is markedly elevated, often >100,000 mIU/mL. Complications include theca lutein cysts, hyperemesis gravidarum, and progression to choriocarcinoma.
Rationale for correct answer
2. Molar pregnancy presents with abnormal placental growth and the passage of grape-like vesicles, which are swollen chorionic villi. The question stem directly describes this hallmark feature. The markedly elevated hCG and absence of fetal parts further support the diagnosis. These vesicles are expelled vaginally and resemble clusters of grapes due to hydropic degeneration.
Rationale for incorrect answers
1. Ectopic pregnancy involves implantation of the embryo outside the uterine cavity, most commonly in the fallopian tube. It presents with abdominal pain and vaginal bleeding, but does not produce grape-like vesicles. Ultrasound typically shows an empty uterus with adnexal mass. hCG levels rise abnormally slowly. There is no trophoblastic overgrowth or vesicular tissue passage.
3. Threatened miscarriage refers to vaginal bleeding in early pregnancy with a closed cervical os and viable intrauterine pregnancy. It does not involve abnormal placental growth or vesicle passage. The uterus is appropriate for gestational age, and hCG levels are consistent with normal pregnancy. No hydropic villi or trophoblastic proliferation is present.
4. Cervical friability is a physical finding where the cervix bleeds easily on contact, often due to infection, inflammation, or hormonal changes. It is unrelated to pregnancy loss or placental pathology. It does not involve trophoblastic tissue or vesicle formation. No abnormal hCG levels or uterine enlargement are seen.
Take home points
- Molar pregnancy involves hydropic degeneration of chorionic villi and excessive trophoblastic proliferation.
- Grape-like vesicle passage is pathognomonic for molar pregnancy.
- hCG levels are markedly elevated, often >100,000 mIU/mL.
- Must differentiate from ectopic pregnancy and miscarriage based on ultrasound and clinical features.
A nurse is assessing a patient with suspected molar pregnancy. Which finding is most characteristic?
Explanation
Molar pregnancy is a gestational trophoblastic disorder caused by abnormal fertilization leading to proliferation of trophoblastic tissue, formation of hydropic villi, and absence or malformation of fetal structures. Complete moles are typically 46XX and lack fetal parts, while partial moles are 69XXY or 69XXX and may contain fetal tissue. Excessive hCG, uterine enlargement, and vaginal bleeding are common. The uterus may be larger than expected for gestational age, and hCG levels often exceed 100,000 mIU/mL. Complications include theca lutein cysts, hyperemesis gravidarum, and progression to choriocarcinoma.
Rationale for correct answer
2. The passage of grape-like vesicles is the most characteristic finding in molar pregnancy. These vesicles represent swollen, edematous chorionic villi expelled through the vagina. This finding is pathognomonic and results from hydropic degeneration of trophoblastic tissue. The question stem directly refers to this hallmark feature, confirming the diagnosis.
Rationale for incorrect answers
1. Light spotting with mild cramping is more consistent with early pregnancy changes or a threatened miscarriage. Molar pregnancy typically presents with heavy bleeding and uterine enlargement, not mild symptoms. The spotting lacks the diagnostic specificity of vesicle passage and does not reflect trophoblastic overgrowth.
3. Unilateral pelvic pain is a hallmark of ectopic pregnancy, especially when associated with tubal rupture. Molar pregnancy does not cause localized pain but rather diffuse uterine symptoms. There is no implantation outside the uterus, and no adnexal tenderness or mass is expected.
4. Loss of pregnancy symptoms may occur in missed miscarriage but is not characteristic of molar pregnancy. In fact, molar pregnancy often exaggerates symptoms due to excess hCG, leading to severe nausea, breast tenderness, and early-onset preeclampsia. Symptom loss contradicts the hyperactive hormonal profile of molar gestation.
Take home points
- Grape-like vesicle passage is pathognomonic for molar pregnancy.
- Molar pregnancy presents with elevated hCG and uterine enlargement.
- Must differentiate from ectopic pregnancy and miscarriage based on ultrasound and symptoms.
- Risk of choriocarcinoma requires post-evacuation hCG monitoring.
What is the primary surgical intervention for a molar pregnancy?
Explanation
Molar pregnancy is a form of gestational trophoblastic disease characterized by abnormal trophoblastic proliferation, hydropic degeneration of chorionic villi, and absence of viable fetal tissue. It results from aberrant fertilization, leading to either a complete mole (46XX or 46XY) or partial mole (69XXY or 69XXX). Patients present with vaginal bleeding, uterine enlargement, and markedly elevated hCG levels, often >100,000 mIU/mL. Diagnosis is confirmed via ultrasound showing a “snowstorm” pattern. The primary goal of treatment is complete evacuation of molar tissue to prevent persistent disease or choriocarcinoma.
Rationale for correct answer
2. Dilation and curettage (D&C) is the primary surgical intervention for molar pregnancy. It allows for complete evacuation of molar tissue from the uterus, minimizing the risk of retained trophoblastic cells and progression to malignancy. Suction curettage is preferred over sharp curettage due to lower risk of uterine perforation and more effective removal of hydropic villi.
Rationale for incorrect answers
1. Laparoscopy is not indicated for molar pregnancy. It is used for ectopic pregnancy, pelvic masses, or diagnostic exploration. Molar pregnancy is intrauterine and best managed by uterine evacuation. Laparoscopy does not provide adequate access to the uterine cavity for removing trophoblastic tissue.
3. Hysterectomy is reserved for select cases such as women who have completed childbearing and have invasive mole or uncontrolled bleeding. It is not the first-line treatment. D&C remains the standard unless there are complications or recurrence. Hysterectomy also precludes future fertility, making it inappropriate for most patients.
4. Myomectomy is a procedure for removing uterine fibroids, not molar tissue. It targets smooth muscle tumors and has no role in managing gestational trophoblastic disease. Molar pregnancy involves placental tissue, not myometrial pathology, and requires complete evacuation of chorionic villi.
Take home points
- D&C is the first-line surgical treatment for molar pregnancy.
- Laparoscopy is used for ectopic pregnancy, not intrauterine molar disease.
- Hysterectomy is reserved for invasive mole or non-fertility-preserving cases.
- Myomectomy treats fibroids, not trophoblastic disease.
Which findings are characteristic of a molar pregnancy? Select all that apply.
Explanation
Molar pregnancy is a gestational trophoblastic disorder caused by abnormal fertilization resulting in trophoblastic hyperplasia, hydropic degeneration, and absence of fetal tissue in complete moles. It presents with vaginal bleeding, uterine enlargement, and markedly elevated hCG levels, often >100,000 mIU/mL. Ultrasound shows a “snowstorm” pattern due to swollen chorionic villi. The most characteristic clinical sign is the passage of grape-like vesicles, which are clusters of edematous villi expelled vaginally. Complications include theca lutein cysts, hyperemesis gravidarum, and progression to choriocarcinoma.
Rationale for correct answers
1. The passage of grape-like vesicles is pathognomonic for molar pregnancy. These vesicles are swollen chorionic villi expelled through the vagina due to hydropic degeneration. Their appearance resembles translucent grapes and confirms the diagnosis clinically.
2. Elevated hCG levels are a hallmark of molar pregnancy due to excessive trophoblastic proliferation. Levels often exceed 100,000 mIU/mL and correlate with symptoms like hyperemesis and early-onset preeclampsia. The hCG elevation is disproportionate to gestational age and supports the diagnosis.
Rationale for incorrect answers
3. Light spotting with mild cramping is nonspecific and more typical of a threatened miscarriage. Molar pregnancy presents with heavy bleeding and uterine enlargement, not mild symptoms. The spotting lacks diagnostic specificity and does not reflect trophoblastic overgrowth.
4. Empty uterus on ultrasound is characteristic of ectopic pregnancy, not molar pregnancy. In molar pregnancy, ultrasound shows a snowstorm pattern or diffuse echogenic material due to hydropic villi. The uterus is enlarged and filled with abnormal tissue, not empty.
5. Unilateral pelvic pain is typical of ectopic pregnancy, especially with tubal rupture. Molar pregnancy causes diffuse uterine symptoms, not localized pain. There is no implantation outside the uterus, and no adnexal tenderness or mass is expected.
Take home points
- Grape-like vesicle passage is pathognomonic for molar pregnancy.
- hCG levels are markedly elevated, often >100,000 mIU/mL.
- Ultrasound shows a snowstorm pattern, not an empty uterus.
- Must differentiate from ectopic pregnancy and miscarriage based on clinical and imaging features.
Practice Exercise 6
A nurse is assessing a patient with vaginal bleeding at 7 weeks gestation. Which finding warrants immediate escalation to the obstetric team?
Explanation
Early pregnancy bleeding requires careful evaluation to distinguish benign causes from life-threatening emergencies. At 7 weeks gestation, bleeding may result from implantation, threatened miscarriage, ectopic pregnancy, or gestational trophoblastic disease. The most critical concern is hemodynamic instability, which signals active hemorrhage or rupture. Hypotension, tachycardia, abdominal pain, and syncope suggest significant blood loss. In ectopic pregnancy, rupture can occur between 6–10 weeks, leading to intraperitoneal bleeding. A pulse >120 bpm and systolic BP <90 mmHg indicate shock and require urgent obstetric and surgical intervention.
Rationale for correct answer
2. Hypotension and pulse 130 bpm indicate hemodynamic instability, which is a medical emergency. These findings suggest significant blood loss, possibly from ruptured ectopic pregnancy or hemorrhagic miscarriage. Immediate escalation is required to prevent cardiovascular collapse and initiate resuscitation, imaging, and surgical management.
Rationale for incorrect answers
1. Light spotting with no pain is common in early pregnancy and often benign, related to implantation or cervical irritation. It does not indicate active bleeding or instability. Without pain or systemic signs, observation and routine follow-up are appropriate.
3. Mild cramping relieved by rest is nonspecific and may reflect uterine stretching or early pregnancy changes. It lacks signs of tissue passage, hemodynamic compromise, or acute pathology. No escalation is needed unless symptoms worsen or bleeding increases.
4. Passage of small clots can occur in threatened miscarriage, but without pain or instability, it does not warrant immediate escalation. Monitoring and ultrasound evaluation are appropriate. Clots alone do not confirm complete miscarriage or rupture.
Take home points
- Hypotension and tachycardia in early pregnancy bleeding signal possible rupture or hemorrhage.
- Ectopic pregnancy rupture typically occurs between 6–10 weeks gestation.
- Benign spotting and mild cramping do not require urgent escalation.
- Clot passage without instability may reflect threatened miscarriage, not emergency.
What is the primary purpose of administering crystalloid fluids in a patient with pregnancy-related bleeding?
Explanation
Pregnancy-related hemorrhage requires rapid stabilization to prevent maternal morbidity and mortality. The primary concern is hypovolemia, which leads to decreased tissue perfusion, organ dysfunction, and hemodynamic instability. Crystalloid fluids such as normal saline or lactated Ringer’s are used to expand intravascular volume, restore circulatory pressure, and maintain perfusion. Blood loss exceeding 500 mL in vaginal delivery or 1000 mL in cesarean section is considered postpartum hemorrhage. Early fluid resuscitation prevents progression to shock, acidosis, and coagulopathy. Monitoring includes blood pressure, urine output, and lactate levels.
Rationale for correct answer
2. Crystalloid fluids restore intravascular volume by expanding plasma compartment and improving circulatory stability. In pregnancy-related bleeding, rapid volume replacement is essential to maintain perfusion and prevent hypovolemic shock. Crystalloids are first-line due to availability, low cost, and compatibility with blood products.
Rationale for incorrect answers
1. Inducing uterine contractions is achieved pharmacologically using oxytocin, misoprostol, or ergometrine, not crystalloid fluids. Fluids do not stimulate myometrial activity. Their role is volume expansion, not uterine tone modulation.
3. Preventing infection requires antibiotics, sterile technique, and wound care. Crystalloid fluids do not possess antimicrobial properties. They do not alter immune response or reduce microbial load.
4. Reducing pain involves analgesics such as acetaminophen, NSAIDs, or opioids. Crystalloids do not affect nociceptive pathways or pain perception. Their use is hemodynamic, not analgesic.
Take home points
- Crystalloids are used to restore intravascular volume in hemorrhagic states.
- They do not induce uterine contractions or reduce pain.
- Infection prevention requires antibiotics, not fluids.
- Hemodynamic monitoring guides fluid resuscitation effectiveness.
A nurse is preparing to administer RhoGAM to a patient with a miscarriage. Within what timeframe must this medication be given to prevent Rh isoimmunization?
Explanation
Rh isoimmunization occurs when an Rh-negative mother is exposed to Rh-positive fetal erythrocytes, leading to maternal production of anti-D antibodies. These antibodies cross the placenta in subsequent pregnancies, causing hemolysis, fetal anemia, and hydrops fetalis. Rho(D) immune globulin (RhoGAM) prevents sensitization by binding fetal Rh-positive cells before the maternal immune system reacts. It must be administered within a strict time-sensitive window to ensure efficacy. The standard dose is 300 µg IM, which protects against up to 30 mL of fetal whole blood or 15 mL of packed red cells.
Rationale for correct answer
2. RhoGAM must be administered within 72 hours of a miscarriage, delivery, or any event involving fetomaternal hemorrhage. This timeframe ensures neutralization of fetal Rh-positive cells before maternal sensitization occurs. Beyond 72 hours, the risk of antibody formation increases, compromising future pregnancies.
Rationale for incorrect answers
1. Within 24 hours is unnecessarily restrictive. While earlier administration is ideal, the immune response takes time to develop. The validated window for effective prophylaxis is up to 72 hours. Limiting to 24 hours may delay appropriate care if logistics prevent immediate administration.
3. Within 7 days exceeds the recommended prophylactic window. After 72 hours, maternal B-cell activation and IgG production may begin, rendering RhoGAM ineffective. Delayed administration increases the risk of alloimmunization and fetal complications in future Rh-positive pregnancies.
4. Within 14 days is clinically unsafe. By this time, sensitization is likely complete, and RhoGAM cannot reverse the immune response. Administering beyond 72 hours offers no protective benefit and falsely reassures providers and patients.
Take home points
- RhoGAM must be given within 72 hours of Rh exposure to prevent isoimmunization.
- Delayed administration beyond 72 hours risks antibody formation and fetal hemolysis.
- Rh-negative mothers with miscarriage, trauma, or delivery require prophylaxis.
- RhoGAM dose protects against 30 mL fetal whole blood or 15 mL packed cells.
Which interventions are appropriate for a patient with hemodynamic instability due to pregnancy bleeding? Select all that apply.
Explanation
Hemodynamic instability due to pregnancy bleeding involves acute circulatory compromise secondary to blood loss. The pathophysiology centers on reduced blood volume, impaired oxygen delivery, and compensatory tachycardia. Causes include placental abruption, uterine rupture, or previa. Signs include systolic BP <90 mmHg, HR >100 bpm, pallor, and altered LOC. Management prioritizes oxygenation, volume resuscitation, and frequent monitoring. Hemoglobin <11 g/dL and hematocrit <33% in pregnancy signal anemia. Rapid intervention prevents hypovolemic shock, fetal compromise, and maternal death.
Rationale for correct answers
1. High-flow oxygen improves tissue perfusion and compensates for reduced oxygen-carrying capacity due to hemorrhage. It supports maternal and fetal oxygenation during circulatory compromise. The stem indicates hemodynamic instability, which requires immediate oxygen supplementation.
3. Large-bore IV access enables rapid fluid resuscitation and blood product administration. In hemorrhagic shock, restoring intravascular volume is critical. Peripheral 16G or 18G cannulas are preferred for high-flow infusion.
4. Monitoring vital signs every 15 minutes detects deterioration and guides intervention timing. Frequent checks allow early recognition of worsening hypotension or tachycardia, which are markers of ongoing bleeding or inadequate resuscitation.
Rationale for incorrect answers
2. Oral fluid intake is contraindicated in hemodynamic instability due to risk of aspiration and delayed absorption. In acute bleeding, IV fluids are required for rapid volume expansion. Oral intake is insufficient and unsafe in compromised patients.
5. Oral analgesics are inappropriate in unstable patients due to delayed onset and potential hypotension. Parenteral analgesia is preferred if pain control is needed, but only after stabilization. Oral route is contraindicated in shock states.
Take home points
- Hemodynamic instability in pregnancy requires rapid oxygenation, IV access, and close monitoring.
- Oral interventions are contraindicated in acute bleeding due to delayed absorption and aspiration risk.
- Vital signs guide resuscitation and detect deterioration early.
Large-bore IV access is essential for fluid and blood product delivery
Which components should be included in discharge teaching for a patient post-miscarriage? Select all that apply.
Explanation
Post-miscarriage recovery involves physical and emotional healing following spontaneous pregnancy loss. The uterine involution, hormonal regulation, and infection risk are central to management. Bleeding typically lasts 1 to 2 weeks, and hCG levels decline gradually. Heavy bleeding, fever, or foul discharge may indicate retained products or infection. Emotional support and contraception counseling are essential. Sexual activity should be delayed until bleeding stops and cervix closes. Follow-up includes hCG monitoring to confirm complete resolution and rule out ectopic or molar pregnancy.
Rationale for correct answers
1. Fever and heavy bleeding are signs of infection or retained products. Immediate reporting allows prompt evaluation and intervention. Post-miscarriage patients are at risk for endometritis and hemorrhage.
3. Avoiding heavy lifting reduces abdominal strain and supports uterine healing. Physical exertion may increase bleeding or delay recovery. One week of rest is standard unless complications arise.
5. hCG monitoring confirms complete resolution and excludes gestational trophoblastic disease. Serial measurements should show a consistent decline to <5 mIU/mL. Persistent elevation may indicate retained tissue or molar pregnancy.
Rationale for incorrect answers
2. Intercourse within 24 hours is contraindicated due to infection risk and cervical vulnerability. The cervix remains open post-miscarriage, increasing susceptibility to ascending pathogens. Sexual activity should resume only after bleeding stops and cervix closes.
4. Persistent pregnancy symptoms are not expected post-miscarriage. Continued symptoms may suggest incomplete miscarriage or ectopic pregnancy. hCG levels should fall, resolving nausea, breast tenderness, and fatigue. Ongoing symptoms warrant evaluation.
Take home points
- Fever or heavy bleeding post-miscarriage may signal retained products or infection.
- hCG monitoring ensures complete resolution and rules out molar pregnancy.
- Physical rest supports uterine recovery and reduces bleeding risk.
Comprehensive Questions
Which of the following is the leading cause of spontaneous abortion, particularly in the first trimester?
Explanation
Spontaneous abortion is the loss of a pregnancy before 20 weeks gestation, most commonly occurring in the first trimester. The most frequent cause is chromosomal abnormalities, which disrupt normal embryonic development. These errors include trisomies, monosomies, and polyploidy, often incompatible with life. Other causes include maternal infections, uterine anomalies, and endocrine dysfunctions, but these are less prevalent. Clinically, spontaneous abortion presents with vaginal bleeding, cramping, and passage of tissue. Ultrasound may show absent fetal cardiac activity or empty gestational sac. Serum β-hCG levels typically fail to rise appropriately. Risk increases with maternal age over 35 years and prior miscarriages.
Rationale for correct answer
3. Chromosomal abnormalities account for approximately 50% to 70% of first trimester spontaneous abortions. These include autosomal trisomies (especially trisomy 16), monosomy X (Turner syndrome), and triploidy. These genetic errors result in nonviable embryos due to disrupted cell division and organogenesis. The question stem emphasizes “leading cause,” making this the most scientifically supported answer.
Rationale for incorrect answers
1. Maternal infections such as toxoplasmosis, rubella, cytomegalovirus, herpes simplex virus, and syphilis can cause fetal demise, but they are far less common than chromosomal errors. Their impact is more pronounced in later trimesters or when congenital anomalies develop. Infections may also cause intrauterine growth restriction or preterm labor rather than early spontaneous abortion.
2. Uterine abnormalities like septate uterus, fibroids, or adhesions can impair implantation or placental development, increasing miscarriage risk. However, these structural issues are more associated with second trimester losses or recurrent pregnancy loss rather than isolated first trimester events. They are not the leading cause statistically.
4. Endocrine disorders such as uncontrolled diabetes mellitus, thyroid dysfunction, and luteal phase defects can contribute to miscarriage. Progesterone deficiency may impair endometrial support. However, these are modifiable risk factors and less frequent than chromosomal anomalies. Their role is more significant in recurrent pregnancy loss than in sporadic first trimester abortions.
Take home points
- Chromosomal abnormalities are the most common cause of first trimester spontaneous abortion.
- Trisomy 16, monosomy X, and triploidy are frequent lethal genetic errors.
- Uterine anomalies and endocrine disorders are less common and often linked to recurrent losses.
- Maternal infections are important but not the leading cause of early pregnancy loss.
Which type of uterine anomaly is most commonly associated with recurrent pregnancy loss due to its impact on implantation and blood supply?
Explanation
Uterine anomalies are congenital malformations resulting from incomplete fusion or resorption of the Müllerian ducts. The most clinically significant is the septate uterus, which has a fibrous or muscular septum dividing the endometrial cavity. This anomaly impairs implantation, disrupts vascular supply, and increases risk of recurrent pregnancy loss. The septum is poorly vascularized, leading to inadequate support for the developing embryo. Diagnosis is confirmed via MRI, 3D ultrasound, or hysteroscopy, and surgical correction with hysteroscopic metroplasty significantly improves outcomes.
Rationale for correct answer
3. Septate uterus is the most common Müllerian anomaly and the one most strongly associated with first trimester recurrent pregnancy loss. The fibrous septum lacks adequate vascularization, leading to poor implantation and early miscarriage. The question emphasizes impact on implantation and blood supply, which directly implicates the septate anomaly.
Rationale for incorrect answers
1. Bicornuate uterus results from incomplete fusion of the Müllerian ducts, creating two endometrial cavities. While it may cause second trimester losses or malpresentation, it does not significantly impair early implantation or vascular supply. Its association with recurrent first trimester loss is weaker than that of septate uterus.
2. Unicornuate uterus arises from complete agenesis or hypoplasia of one Müllerian duct, resulting in a single horn. It can lead to poor pregnancy outcomes due to reduced uterine volume and abnormal placentation, but it is less common and less directly linked to implantation failure compared to septate uterus.
4. Didelphys uterus involves complete failure of fusion of the Müllerian ducts, resulting in two separate uteri and cervices. While it may cause obstetric complications like breech presentation or preterm labor, it is not the leading anomaly for recurrent pregnancy loss due to implantation or vascular issues.
Take home points
- Septate uterus is the most common uterine anomaly linked to recurrent first trimester pregnancy loss.
- Poor vascularization of the septum impairs implantation and embryonic development.
- Bicornuate and didelphys uteri are more associated with second trimester complications.
- Surgical correction of septate uterus improves pregnancy outcomes significantly.
Which acquired uterine abnormality is characterized by scar tissue formation within the uterine cavity, potentially leading to recurrent pregnancy loss or infertility?
Explanation
Asherman’s Syndrome is an acquired intrauterine condition marked by fibrous adhesions, scar tissue, and endometrial damage. It typically follows dilation and curettage, postpartum hemorrhage, or pelvic surgery, especially when infection is present. The resulting intrauterine synechiae disrupt normal endometrial regeneration, impairing implantation and leading to infertility or recurrent pregnancy loss. Patients may present with hypomenorrhea, amenorrhea, or cyclic pain without bleeding. Diagnosis is confirmed via hysteroscopy, which allows direct visualization and lysis of adhesions. Sonohysterography and hysterosalpingography may also show filling defects.
Rationale for correct answer
3. Asherman’s Syndrome is the only acquired uterine abnormality in the list characterized by intrauterine scar tissue formation. The adhesions interfere with endometrial receptivity and vascularization, leading to infertility and recurrent miscarriage. The question highlights “scar tissue” and “acquired,” which directly point to this diagnosis.
Rationale for incorrect answers
1. Uterine fibroids are benign smooth muscle tumors that may distort the uterine cavity or impair implantation depending on their location. However, they are not characterized by scar tissue formation. Submucosal fibroids may cause miscarriage, but they are not acquired through trauma or surgery and do not involve adhesions.
2. Cervical insufficiency involves painless cervical dilation in the second trimester, leading to pregnancy loss. It is a structural weakness of the cervix, not an intrauterine condition. It does not involve scar tissue or adhesions and is unrelated to endometrial integrity or implantation failure.
4. Bicornuate uterus is a congenital Müllerian anomaly resulting from incomplete fusion of the paramesonephric ducts. It presents with two endometrial cavities and is not acquired. It does not involve scar tissue and is not caused by surgical trauma or infection.
Take home points
- Asherman’s Syndrome is caused by intrauterine adhesions following trauma or infection.
- It leads to infertility, hypomenorrhea, and recurrent pregnancy loss.
- Diagnosis is best confirmed by hysteroscopy.
- It must be differentiated from congenital anomalies and cervical insufficiency.
What is the primary reason for administering misoprostol after mifepristone in a medical abortion?
Explanation
Medical abortion involves pharmacologic termination of early pregnancy using a combination of agents that disrupt progesterone support, induce decidual breakdown, and trigger uterine contractions. Mifepristone is a progesterone receptor antagonist that destabilizes the endometrial lining, while misoprostol is a prostaglandin E1 analog that stimulates myometrial contractility. The regimen is most effective when misoprostol is administered 24 to 48 hours after mifepristone. Common side effects include cramping, bleeding, nausea, and diarrhea. Contraindications include ectopic pregnancy, coagulopathy, and chronic adrenal failure. Complete abortion typically occurs within 7 days.
Rationale for correct answer
3. Misoprostol induces strong uterine contractions by binding to prostaglandin receptors in the myometrium, facilitating expulsion of the products of conception. Its role is mechanical, not hormonal. The question asks for the “primary reason,” which is the contractile action necessary to complete the abortion process initiated by mifepristone.
Rationale for incorrect answers
1. Blocking progesterone receptors is the mechanism of mifepristone, not misoprostol. Mifepristone antagonizes progesterone, leading to decidual necrosis and detachment of the gestational sac. Misoprostol does not interact with progesterone receptors and has no hormonal antagonism.
2. Misoprostol does not reduce nausea and vomiting; it may actually cause these symptoms due to its gastrointestinal effects. It stimulates smooth muscle contraction in the GI tract, often leading to cramping, diarrhea, and emesis. Its use is not for symptom control but for uterine evacuation.
4. Misoprostol does not prevent infection. Infection risk is managed through aseptic technique and, if needed, prophylactic antibiotics. Misoprostol’s role is mechanical, not antimicrobial. Incomplete abortion may increase infection risk, but misoprostol itself does not have direct anti-infective properties.
Take home points
- Misoprostol’s primary role in medical abortion is to induce uterine contractions.
- Mifepristone blocks progesterone receptors, initiating endometrial breakdown.
- Misoprostol does not prevent infection or reduce nausea.
Cervical insufficiency is a significant cause of spontaneous abortion, typically occurring in which trimester?
Explanation
Cervical insufficiency is a structural weakness of the cervix that leads to painless dilation, premature effacement, and expulsion of the fetus without contractions. It typically manifests in the second trimester, between 14 and 24 weeks, when fetal weight increases and intrauterine pressure rises. The cervix fails to maintain closure due to congenital defects, trauma from prior procedures, or collagen disorders. Clinical presentation includes sudden painless cervical dilation, membrane prolapse, and rapid pregnancy loss. Diagnosis is confirmed via transvaginal ultrasound showing cervical length <25 mm or funneling. Management includes cerclage placement, progesterone therapy, and close surveillance.
Rationale for correct answer
2. Cervical insufficiency typically causes spontaneous abortion in the second trimester due to the increasing uterine pressure and fetal weight. The cervix dilates painlessly, often without contractions, leading to premature loss. The question specifies “significant cause,” and second trimester losses are the hallmark of this condition.
Rationale for incorrect answers
1. First trimester losses are usually due to chromosomal abnormalities, not cervical insufficiency. The fetus is too small to exert enough pressure to cause cervical dilation. Cervical insufficiency rarely presents this early unless accompanied by other uterine anomalies.
3. Third trimester losses are more commonly associated with placental abruption, preterm labor, or intrauterine fetal demise. Cervical insufficiency typically leads to loss before viability, not in the third trimester. If undiagnosed, it may cause preterm birth, but not spontaneous abortion at this stage.
4. Cervical insufficiency does not occur in any trimester equally. It is specifically associated with second trimester losses due to mechanical failure of the cervix under increasing fetal weight. The term “any trimester” is scientifically inaccurate for this condition.
Take home points
- Cervical insufficiency causes painless second trimester pregnancy loss.
- Cervical length <25 mm and funneling on ultrasound support diagnosis.
- First trimester losses are usually genetic, not structural.
- Cerclage and progesterone are key preventive strategies.
Which of the following lifestyle factors is known to increase the risk of spontaneous abortion?
Explanation
Spontaneous abortion is the loss of a pregnancy before 20 weeks gestation due to natural causes. It is associated with chromosomal abnormalities, maternal infections, uterine anomalies, and toxic exposures. Risk factors include maternal age over 35 years, poorly controlled diabetes, and substance use. Clinical signs include vaginal bleeding, cramping, and cervical dilation. Serum β-hCG levels typically decline, and ultrasound may show absent fetal cardiac activity. Environmental exposures like alcohol, tobacco, and radiation increase risk. Fetal loss is confirmed by transvaginal ultrasound showing no growth or heartbeat.
Rationale for correct answer
3. Heavy alcohol consumption is a teratogen that disrupts fetal development and increases miscarriage risk. Ethanol crosses the placenta and impairs cellular differentiation and placental function, leading to fetal hypoxia and death. Studies show that consuming more than 5 drinks per week increases risk of spontaneous abortion by up to 2-fold. The stem asks for a lifestyle factor known to increase risk, and alcohol is the only one with direct embryotoxic effects.
Rationale for incorrect answers
1. Moderate caffeine intake, defined as less than 200 mg per day (about 2 cups of coffee), is not associated with increased miscarriage risk. High doses above 300 mg may pose risk, but moderate levels are considered safe. Caffeine is a mild stimulant and vasoconstrictor, but does not directly impair fetal viability at low doses.
2. Regular, moderate exercise improves maternal cardiovascular health and reduces gestational complications. It does not increase miscarriage risk unless associated with trauma or overheating. Exercise enhances placental perfusion and glucose regulation, supporting fetal development. The stem specifies regular moderate activity, which is protective.
4. Balanced nutritional diet supports fetal growth and reduces risk of miscarriage. Adequate intake of folate, iron, and protein is essential for placental development and embryogenesis. Malnutrition or deficiencies increase risk, but a balanced diet is beneficial. The stem refers to a healthy intake, which is protective.
Take home points
- Heavy alcohol use increases risk of spontaneous abortion due to direct embryotoxic effects.
- Moderate caffeine intake under 200 mg/day is not linked to miscarriage.
- Regular, moderate exercise supports pregnancy and reduces complications.
- Balanced nutrition is protective; deficiencies increase risk of fetal loss.
A patient is diagnosed with recurrent pregnancy loss. What type of specialist referral would be most appropriate for this patient?
Explanation
Recurrent pregnancy loss is defined as two or more consecutive pregnancy losses before 20 weeks gestation. It is associated with genetic abnormalities, anatomical defects, hormonal imbalances, and autoimmune disorders. Common causes include antiphospholipid syndrome, uterine septum, and luteal phase defects. Evaluation includes karyotyping, hysterosalpingography, and hormonal assays. Progesterone levels below 10 ng/mL in luteal phase suggest insufficiency. Management requires a multidisciplinary approach, often involving advanced reproductive techniques and immunologic testing.
Rationale for correct answer
2. Reproductive endocrinologist specializes in evaluating and treating infertility and recurrent pregnancy loss. They assess hormonal dysfunction and implantation failure, and manage conditions like polycystic ovarian syndrome, luteal phase defect, and uterine anomalies. The stem indicates recurrent losses, which require targeted hormonal and structural evaluation beyond general obstetrics.
Rationale for incorrect answers
1. Pediatrician focuses on child health post-delivery, not maternal reproductive issues. They manage neonatal care and developmental disorders, not pregnancy loss. Referral to a pediatrician does not address the maternal pathophysiology causing recurrent miscarriage.
3. Ophthalmologist treats eye diseases such as glaucoma and retinal disorders, unrelated to reproductive health. They do not evaluate hormonal or uterine factors contributing to miscarriage. No ocular pathology is relevant in recurrent pregnancy loss.
4. Dermatologist manages skin conditions like psoriasis and acne, not reproductive or endocrine disorders. Skin findings may be present in autoimmune disease, but they do not manage pregnancy loss directly. Their scope excludes uterine or hormonal evaluation.
Take home points
- Reproductive endocrinologists are key in evaluating recurrent pregnancy loss.
- Pediatricians manage child health, not maternal reproductive issues.
- Ophthalmologists and dermatologists are unrelated to miscarriage evaluation.
- Hormonal, genetic, and anatomical factors must be assessed in recurrent loss.
What is the general definition of recurrent pregnancy loss?
Explanation
Recurrent pregnancy loss is a clinical diagnosis referring to repeated spontaneous abortions before fetal viability. It is defined by three or more consecutive losses before 20 weeks gestation. Causes include genetic abnormalities, uterine anomalies, hormonal imbalances, and autoimmune disorders. Evaluation includes parental karyotyping, antiphospholipid antibody testing, and uterine imaging. Serum progesterone levels below 10 ng/mL in luteal phase suggest insufficiency. Thrombophilias, luteal phase defects, and uterine septum are common contributors. Management depends on etiology and may involve anticoagulation, hormonal support, or surgical correction.
Rationale for correct answer
3. Three or more consecutive spontaneous abortions before 20 weeks gestation is the standard clinical definition of recurrent pregnancy loss. This threshold reflects a pattern of reproductive failure and prompts investigation into underlying pathology. The stem asks for general definition, and this choice aligns with established criteria used in reproductive medicine.
Rationale for incorrect answers
1. Two or more non-consecutive spontaneous abortions do not meet the strict definition of recurrent pregnancy loss. While concerning, non-consecutive losses may be sporadic and not indicative of a persistent underlying issue. Recurrent loss requires consecutive events to suggest a pattern.
2. One spontaneous abortion after 20 weeks gestation is classified as stillbirth, not miscarriage. Loss after 20 weeks involves different etiologies such as placental abruption or fetal anomalies. It does not meet the criteria for recurrent pregnancy loss, which is limited to early gestation.
4. Induced abortion due to medical reasons is a therapeutic termination, not spontaneous loss. These are elective procedures based on maternal or fetal indications and are not included in the definition of recurrent pregnancy loss. The condition requires natural, unintentional fetal demise.
Take home points
- Recurrent pregnancy loss is defined as three or more consecutive spontaneous abortions before 20 weeks.
- Loss after 20 weeks is classified as stillbirth, not miscarriage.
- Induced abortions are not included in the definition of recurrent loss.
- Evaluation includes genetic, anatomical, hormonal, and immunologic testing.
Which of the following complications is more likely to occur with a second-trimester Dilation and Evacuation (D&E) compared to a first-trimester vacuum aspiration?
Explanation
Second-trimester Dilation and Evacuation (D&E) is a surgical abortion procedure typically performed between 13 and 24 weeks gestation. It involves cervical dilation, mechanical evacuation, and often ultrasound guidance. Compared to first-trimester vacuum aspiration, D&E carries increased risk due to larger fetal size, thinner uterine wall, and greater cervical manipulation. Common complications include uterine perforation, cervical laceration, and retained products. The procedure requires skilled technique and may involve osmotic dilators or pharmacologic agents like misoprostol for cervical preparation.
Rationale for correct answer
2. Uterine perforation is more likely with second-trimester D&E due to increased uterine distension and thinning of the myometrium. The use of rigid instruments and forceful evacuation increases risk of penetrating the uterine wall. The stem compares complication rates between procedures, and perforation is significantly more common in later gestational interventions.
Rationale for incorrect answers
1. Nausea is a nonspecific symptom and not a procedural complication. It may occur due to anesthesia or prostaglandin use, but it is not more common in second-trimester D&E compared to first-trimester aspiration. It reflects systemic response, not mechanical injury.
3. Mild cramping is expected after both procedures due to uterine contraction. It is not a complication and does not differ significantly between first and second trimester. Cramping is a normal post-procedural effect, not a risk factor.
4. Light spotting is a common post-abortion symptom due to endometrial shedding. It is not a complication and occurs with both procedures. It reflects normal healing and does not indicate increased risk in second-trimester D&E.
Take home points
- Uterine perforation risk increases with second-trimester D&E due to uterine thinning and instrument use.
- Nausea and cramping are common but not complications specific to gestational age.
- Light spotting is expected post-procedure and not indicative of complication.
- D&E requires careful cervical preparation and skilled technique to minimize risks.
What is the primary role of laminaria, or other osmotic dilators, in the context of abortion procedures?
Explanation
Cervical preparation is a critical step in second-trimester abortion procedures to reduce trauma and complications. Laminaria and other osmotic dilators work by absorbing moisture, expanding gradually, and mechanically dilating the cervix. This process reduces the risk of cervical laceration, uterine perforation, and incomplete evacuation. Laminaria are derived from seaweed and expand over 4 to 6 hours. Synthetic alternatives like Dilapan-S offer more predictable expansion. Cervical ripening is essential before Dilation and Evacuation (D&E), especially after 14 weeks gestation, when the cervix is less compliant.
Rationale for correct answer
2. Laminaria and osmotic dilators ripen and gradually dilate the cervix by absorbing cervical moisture and expanding. This mechanical dilation facilitates safer instrument passage during D&E. The stem asks for primary role, and cervical dilation is the main function, reducing risk of trauma and perforation.
Rationale for incorrect answers
1. Inducing uterine contractions is the role of pharmacologic agents like misoprostol or oxytocin, not laminaria. Osmotic dilators act locally on the cervix, not the myometrium. They do not stimulate uterine contractility.
3. Preventing infection requires aseptic technique and prophylactic antibiotics, not laminaria. While retained dilators may increase infection risk, their role is mechanical, not antimicrobial. They do not contain bactericidal properties.
4. Pain relief is managed with NSAIDs, local anesthesia, or sedation, not laminaria. Dilators may cause discomfort, but they do not alleviate pain. Their function is structural, not analgesic.
Take home points
- Laminaria dilate the cervix by absorbing moisture and expanding gradually.
- They reduce risk of cervical trauma during second-trimester D&E.
- They do not induce contractions or prevent infection.
- Pain relief requires pharmacologic agents, not mechanical dilators.
Which of the following are risk factors for miscarriage? Select all that apply.
Explanation
Miscarriage is the spontaneous loss of pregnancy before 20 weeks gestation. It results from chromosomal abnormalities, maternal comorbidities, and environmental exposures. Risk increases with advanced maternal age due to higher rates of aneuploidy. Smoking, alcohol, and drugs impair placental perfusion and fetal development. Conditions such as chronic hypertension compromise uteroplacental circulation. Normal BMI and regular exercise are not risk factors.
Rationale for correct answers
1. Maternal age >35 years is a significant risk factor. Oocyte quality declines with age, increasing the risk of chromosomal abnormalities such as trisomies. Miscarriage rates increase sharply after age 35, reaching >50% by age 45 due to genetic errors in meiosis.
2. Smoking or illicit drug use increases miscarriage risk by impairing uteroplacental perfusion. Nicotine and carbon monoxide reduce oxygen delivery, while substances like cocaine cause vasospasm and placental abruption. These exposures directly compromise embryonic and fetal development.
4. Chronic hypertension contributes to miscarriage by damaging vascular integrity and reducing uteroplacental blood flow. Poorly controlled hypertension can cause placental ischemia, intrauterine growth restriction, and early pregnancy loss. The chronic vascular disease impairs implantation and increases miscarriage risk.
Rationale for incorrect answers
3. Regular exercise is not a risk factor for miscarriage. Moderate physical activity is safe in pregnancy and is associated with improved cardiovascular function, reduced gestational diabetes risk, and healthy weight gain. Only extreme trauma or excessive exertion could pose concern, not routine exercise.
5. Normal BMI does not increase miscarriage risk. In fact, it lowers risk compared to obesity or underweight status. Abnormal BMI values are linked to miscarriage due to hormonal imbalance, anovulation, or poor endometrial receptivity, but a normal BMI is protective.
Take home points
- Advanced maternal age strongly increases risk due to chromosomal abnormalities.
- Smoking and illicit drug use impair uteroplacental oxygenation and increase miscarriage risk.
- Chronic hypertension damages placental blood flow and predisposes to pregnancy loss.
- Normal BMI and moderate exercise are protective, not risk factors.
What are common causes of recurrent pregnancy loss? Select all that apply.
Explanation
Recurrent pregnancy loss (RPL) refers to ≥3 consecutive spontaneous abortions before 20 weeks gestation. Major causes include chromosomal abnormalities, uterine structural defects, and immunologic disorders. Parental balanced translocations increase risk of embryo aneuploidy. Cervical insufficiency causes painless dilation and second-trimester losses. Antiphospholipid Syndrome induces placental thrombosis and fetal demise. Uncontrolled gestational diabetes and young maternal age are not established causes of RPL.
Rationale for correct answers
1. Parental chromosomal abnormalities, such as balanced translocations or inversions, predispose embryos to unbalanced karyotypes. These genetic errors often result in early miscarriage due to severe developmental arrest. Cytogenetic testing identifies these abnormalities in 2–5% of couples with RPL.
2. Cervical insufficiency causes recurrent second-trimester pregnancy losses. It involves structural weakness of the cervix, leading to painless dilation and expulsion of pregnancy. Causes include prior cervical trauma, surgery, or congenital weakness. Management involves cerclage placement to maintain cervical competence.
3. Antiphospholipid Syndrome is a major immunologic cause of RPL. Autoantibodies promote placental thrombosis, impair implantation, and restrict fetal growth. It is diagnosed by presence of lupus anticoagulant, anticardiolipin antibodies, or anti-β2 glycoprotein I antibodies. Treatment includes low-dose aspirin and heparin to improve outcomes.
Rationale for incorrect answers
4. Uncontrolled gestational diabetes does not typically cause recurrent pregnancy loss. While it increases risks of macrosomia, congenital anomalies, and stillbirth, miscarriage is not a consistent feature. Pre-gestational poorly controlled diabetes can contribute to early loss, but gestational diabetes develops later and does not explain RPL.
5. Maternal age less than 20 years is not a cause of recurrent pregnancy loss. Younger women have lower rates of chromosomal abnormalities and better oocyte quality. The major age-related risk factor for RPL is advanced maternal age, particularly over 35 years, due to increased aneuploidy.
Take home points
- Recurrent pregnancy loss is most often due to chromosomal, anatomic, or immunologic factors.
- Parental balanced translocations are responsible for early genetic miscarriages.
- Cervical insufficiency causes painless second-trimester pregnancy loss.
- Antiphospholipid Syndrome is a key autoimmune cause requiring anticoagulation therapy.
Which of the following are potential complications of an incomplete abortion? Select all that apply.
Explanation
Incomplete abortion occurs when pregnancy tissue is partially retained in the uterus after pregnancy loss. It is associated with heavy bleeding, pelvic pain, and risk of intrauterine infection. Retained tissue stimulates uterine contractions but prevents complete expulsion, predisposing to complications such as septic abortion, hemorrhagic shock, and uterine perforation during evacuation.
Rationale for correct answers
1. Hemorrhage occurs because retained products prevent effective uterine contraction, resulting in continuous endometrial bleeding. Excessive blood loss may lead to hypovolemic shock. Persistent heavy bleeding after miscarriage strongly indicates incomplete abortion.
2. Infection develops due to retained tissue serving as a nidus for bacterial colonization. Organisms such as Escherichia coli and anaerobes ascend from the vagina, producing fever, foul vaginal discharge, and uterine tenderness. Sepsis risk is high without prompt uterine evacuation.
3. Uterine perforation may occur as a complication of surgical evacuation in incomplete abortion. During dilation and curettage, the uterine wall can be penetrated, causing bleeding, peritonitis, or injury to surrounding organs such as bowel or bladder.
4. Retained products of conception define incomplete abortion itself. They manifest as tissue fragments in the uterus seen on ultrasound and cause ongoing bleeding and cramping. Definitive treatment requires surgical evacuation or pharmacological induction for complete removal.
Rationale for incorrect answers
5. Complete spontaneous expulsion is not a complication but the desired outcome. It indicates that all pregnancy tissue has been expelled from the uterus. The uterus contracts effectively, bleeding subsides, and the risk of infection decreases. Unlike incomplete abortion, no further intervention is typically required.
Take home points
- Incomplete abortion results from partial retention of products of conception.
- Major complications include hemorrhage, infection, and iatrogenic uterine perforation.
- Diagnosis relies on ultrasound findings and clinical features like persistent bleeding.
- Complete expulsion contrasts with incomplete abortion and usually needs no intervention.
When counseling a patient about the emotional impact of pregnancy loss, which points should the nurse emphasize? Select all that apply.
Explanation
Pregnancy loss is a deeply distressing reproductive event with major psychological consequences. The grief response involves complex emotions such as sadness, guilt, and anger, which differ across individuals. Risk of depression and anxiety increases, particularly if coping mechanisms are limited. Supportive counseling and structured communication strategies help reduce long-term psychological morbidity.
Rationale for correct answers
1. Grief is highly individual because cultural, psychological, and relational factors influence how loss is processed. No two patients grieve identically, and recognizing this variation allows for patient-centered care. Nurses must validate unique emotional expressions and avoid imposing generalized timelines.
2. Experiencing a range of emotions such as sadness, anger, or guilt is normal after pregnancy loss. These responses are part of the physiological and psychological processing of trauma. Acknowledging them prevents pathologizing normal grieving and helps patients feel understood.
3. Support groups and counseling are critical resources for patients coping with pregnancy loss. Group therapy provides shared experiences, while professional counseling reduces the risk of complicated grief. Offering these resources empowers patients with options for support beyond the clinical setting.
5. Nurse availability to listen without judgment is essential in fostering trust. Active listening validates the patient’s grief and provides a therapeutic outlet. Non-judgmental presence helps reduce isolation and stigma associated with pregnancy loss.
Rationale for incorrect answers
4. Advising a patient to forget about the loss is scientifically unsound because suppressed grief increases risk for depression and post-traumatic stress. Attempting to prematurely silence emotional processing leads to unresolved trauma. Acknowledging the pregnancy and allowing space for healing is the appropriate approach.
Take home points
- Pregnancy loss has variable emotional impact that requires individualized support.
- Normal grief involves multiple emotions that must be validated.
- Suppressing grief worsens psychological outcomes.
- Nurses provide crucial support through empathy, listening, and referral to resources.
What are essential components of post-procedure care following a surgical abortion? Select all that apply.
Explanation
Surgical abortion requires structured post-procedure care to minimize complications and promote recovery. The uterus is at risk for hemorrhage, while the endometrium remains vulnerable to infection due to cervical dilation. Rh-negative patients need immune prophylaxis with Rho(D) immune globulin to prevent alloimmunization. Post-care must also include contraception counseling to reduce risk of unintended pregnancy.
Rationale for correct answers
1. Monitoring for excessive bleeding is critical because uterine atony or retained products may cause hemorrhage. Vital signs, pad counts, and hemodynamic monitoring ensure early recognition and intervention.
2. Providing discharge instructions regarding signs of infection is essential since cervical dilation increases ascending infection risk. Patients should be taught to watch for fever, foul discharge, or pelvic pain.
3. Administering Rh immune globulin is required for Rh-negative patients to prevent alloimmunization. Fetal red blood cells entering maternal circulation can trigger maternal antibody formation, risking hemolytic disease in future pregnancies.
5. Offering contraception counseling ensures patients understand fertility may return rapidly, often within 2 weeks. Providing options prevents unintended pregnancy and supports reproductive planning.
Rationale for incorrect answers
4. Immediate vigorous activity is inappropriate after surgical abortion because the body requires time for uterine involution and hemostasis. Strenuous exertion increases risk of bleeding and delays recovery. Patients are instead advised rest with gradual resumption of activity.
Take home points
- Post-surgical abortion care focuses on preventing hemorrhage and infection.
- Rh-negative patients require immune prophylaxis with Rho(D) immune globulin.
- Fertility returns quickly, requiring immediate contraceptive counseling.
- Patient education on warning signs ensures early recognition of complications.
Exams on Bleeding
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Implantation Bleeding
- Practice Exercise 1
- Spontaneous Abortion (Miscarriage)
- Practice Exercise 2
- Induced Abortion
- Practice Exercise 3
- Ectopic Pregnancy
- Practice Exercise 4
- Gestational Trophoblastic Disease (Hydatidiform Mole)
- Practice Exercise 5
- Nursing Management Of Pregnancy Bleeding
- Practice Exercise 6
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
After reviewing this study guide, the learner will be able to:
- Define implantation bleeding and differentiate it from abnormal pregnancy bleeding.
- Identify the types of abortion and their pathophysiological processes.
- Recognize clinical signs and symptoms associated with each type of abortion.
- Outline nursing assessment and interventions for pregnancy bleeding emergencies.
- Describe medical and surgical management options for induced and spontaneous abortion.
- Discuss ectopic pregnancy and gestational trophoblastic disease, including risks and complications.
- Provide patient education, psychosocial support, and counseling for women experiencing pregnancy loss.
- Apply critical thinking skills to practice and comprehensive questions related to pregnancy bleeding.
Introduction
Early pregnancy bleeding occurs particularly in the first trimester and represents a common clinical challenge in maternal-newborn nursing, necessitating a thorough understanding of its etiologies, assessment strategies, and management protocols. Vaginal bleeding occurs in approximately 15-25% of early pregnancies, with causes ranging from benign implantation bleeding to life-threatening conditions such as ectopic pregnancy or gestational trophoblastic disease. Implantation bleeding results from the embryo’s attachment to the uterine endometrium, typically presenting as light spotting. In contrast, spontaneous abortion—encompassing threatened, inevitable, incomplete, complete, missed, and recurrent types—accounts for a significant proportion of early pregnancy losses, often due to chromosomal abnormalities, maternal health conditions, or uterine anomalies. Other critical causes, including ectopic pregnancy and molar pregnancy, require urgent recognition due to their potential for severe maternal complications, such as hemorrhage or malignancy. Effective nursing care hinges on accurate assessment, including detailed history-taking, physical examination, and diagnostic testing, such as transvaginal ultrasound and quantitative human chorionic gonadotropin (hCG) levels. Interventions range from expectant management for threatened abortions to medical or surgical approaches for incomplete or ectopic pregnancies, alongside psychosocial support to address emotional distress. These comprehensive notes aim to equip nursing students with the scientific knowledge and practical skills necessary to manage pregnancy bleeding, emphasizing evidence-based practice and patient-centered care. The following sections will provide an in-depth exploration of implantation bleeding, abortion types, assessment techniques, interventions, and critical nursing insights to prepare students for clinical practice and academic success.
Implantation Bleeding
1.1 Definition and Pathophysiology
- Definition:
- Implantation bleeding refers to light vaginal spotting that occurs when a fertilized ovum (blastocyst) attaches to the endometrium of the uterine wall.
- Timing:
- Usually occurs 6–12 days after fertilization, often coinciding with the time a woman expects her menses.
- Pathophysiology:
- Following fertilization, the blastocyst travels through the fallopian tube to the uterus.
- Enzymatic activity from trophoblastic cells invades the endometrial lining to establish vascular connections for nutrient exchange.
- During this invasion, small endometrial capillaries rupture, producing minimal bleeding.
- Unlike menstrual bleeding, which results from progesterone withdrawal and endometrial shedding, implantation bleeding is a localized vascular disruption.

Nursing Insights:
- Implantation bleeding is scant, self-limiting, and painless, unlike abnormal pregnancy bleeding.
- Many patients confuse it with early miscarriage or light menses. Nurses must carefully differentiate implantation spotting from pathological bleeding.
- Misinterpretation may lead to unnecessary anxiety or delayed prenatal care.
1.2 Clinical Presentation and Differentiation from Pathological Bleeding
- Typical clinical features:
- Light spotting, usually pink or brown in color.
- Duration: 1–2 days, rarely longer.
- Not associated with tissue passage or clots.
- Not accompanied by significant pain; mild uterine cramping may occur.
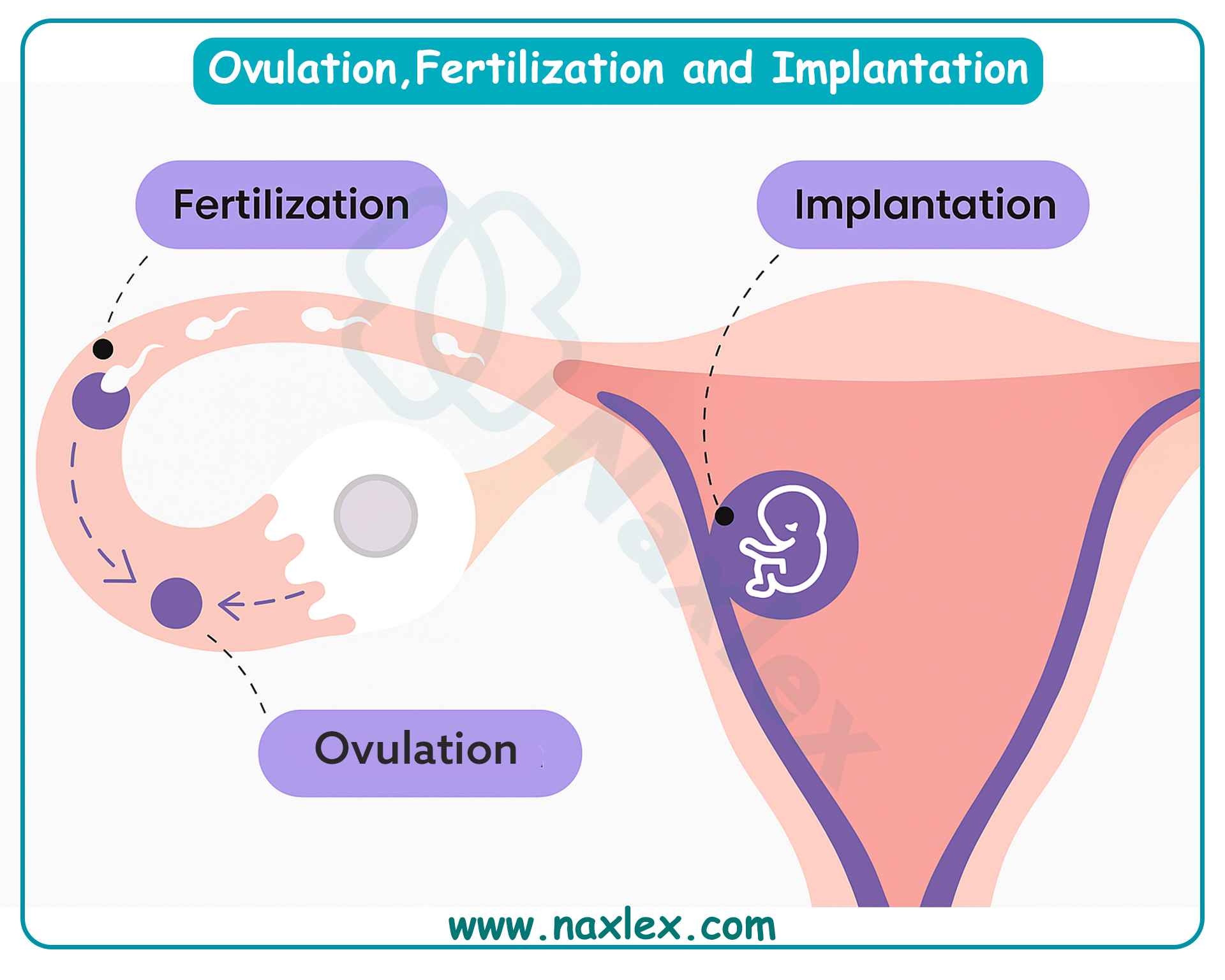
- Differentiation from pathological bleeding:
|
Feature |
Implantation Bleeding |
Threatened/Spontaneous Abortion |
Ectopic Pregnancy |
Molar Pregnancy |
|
Amount |
Light, scant |
Often heavier, may have clots/tissue |
Variable, often dark brown or bright red |
Can be profuse, abnormal |
|
Color |
Pink or brown |
Bright red |
Dark red/brown |
Grape-like vesicles possible |
|
Duration |
1–2 days |
Ongoing until resolved |
Persistent or sudden onset |
Prolonged |
|
Pain |
Minimal or none |
Moderate cramping |
Unilateral pelvic pain, shoulder pain if ruptured |
Uterine distension possible |
|
Cervical os |
Closed |
May be open |
May be closed or open |
Closed |
|
Associated findings |
No systemic signs |
Possible hypotension, tachycardia if severe |
Signs of shock if rupture |
High hCG, absence of fetus |
Nursing Insights:
- Always assess hemodynamic stability (BP, HR) when a pregnant patient presents with bleeding. Even if the patient suspects implantation spotting, the nurse should rule out life-threatening conditions like ectopic pregnancy.
- Nurses should instruct patients to report heavy bleeding, clots, severe pain, or dizziness immediately, as these are not features of implantation bleeding.
1.3 Diagnostic Considerations
- Implantation bleeding is a diagnosis of exclusion.
- Investigations may be minimal but are sometimes necessary to distinguish from pathological causes:
- Pregnancy test (urine or serum hCG): Confirms pregnancy. hCG levels will be rising but may still be low in very early implantation.
- Serial quantitative serum hCG:
- In viable pregnancy: doubles every 48–72 hours in early gestation.
- In abnormal pregnancy: plateauing or falling levels.
- Transvaginal ultrasound:
- May not yet show gestational sac if <5 weeks.
- Useful to exclude ectopic pregnancy or molar pregnancy in cases of abnormal presentation.
- Speculum exam:
- To rule out cervical pathology or trauma.
Nursing Insights:
- Nurses should avoid reassuring patients without evaluation. A small percentage of patients who believe they have implantation bleeding may actually be experiencing early pregnancy loss.
- Documentation of bleeding characteristics (onset, color, volume, associated symptoms) is essential for monitoring progression.
1.4 Nursing Interventions and Patient Education
- Assessment:
- Detailed history of bleeding (onset, duration, color, volume).
- Obstetric history (LMP, parity, prior miscarriages).
- Associated symptoms (pain, dizziness, passage of tissue).
- Vital signs for hemodynamic stability.
- Interventions:
- Reassure the patient if presentation is consistent with implantation bleeding.
- Provide anticipatory guidance: bleeding should not worsen, and systemic symptoms should not appear.
- Arrange follow-up for confirmation of viable pregnancy (serial hCG, ultrasound).
- Instruct on warning signs requiring urgent care:
- Heavy bleeding (soaking >1 pad/hour).
- Severe abdominal pain.
- Syncope or dizziness.
- Passage of tissue or clots.
- Patient Education:
- Explain that implantation bleeding is usually benign and self-limited.
- Emphasize that not all women experience implantation bleeding, and its absence does not indicate pregnancy failure.
- Encourage early initiation of prenatal care.
Nursing Insights:
- Nurses must always individualize care. While implantation bleeding is usually benign, nurses should never dismiss any first-trimester bleeding without evaluation.
- Emotional reassurance is critical. Patients may fear miscarriage, and clear, empathetic communication prevents unnecessary anxiety.
Spontaneous Abortion (Miscarriage)
Spontaneous abortion, commonly referred to as miscarriage, represents the unintended termination of a pregnancy before 20 weeks gestation or before the fetus reaches a weight of 500 grams, the threshold for viability. This clinical entity is a prevalent complication in early pregnancy, necessitating comprehensive nursing knowledge to assess, manage, and support affected patients. The following sections provide an in-depth exploration of the definition, epidemiology, etiology, pathophysiology, classification, assessment, interventions, complications, and psychosocial considerations of spontaneous abortion, equipping nursing students with the scientific foundation and practical skills required for effective maternal-newborn care.
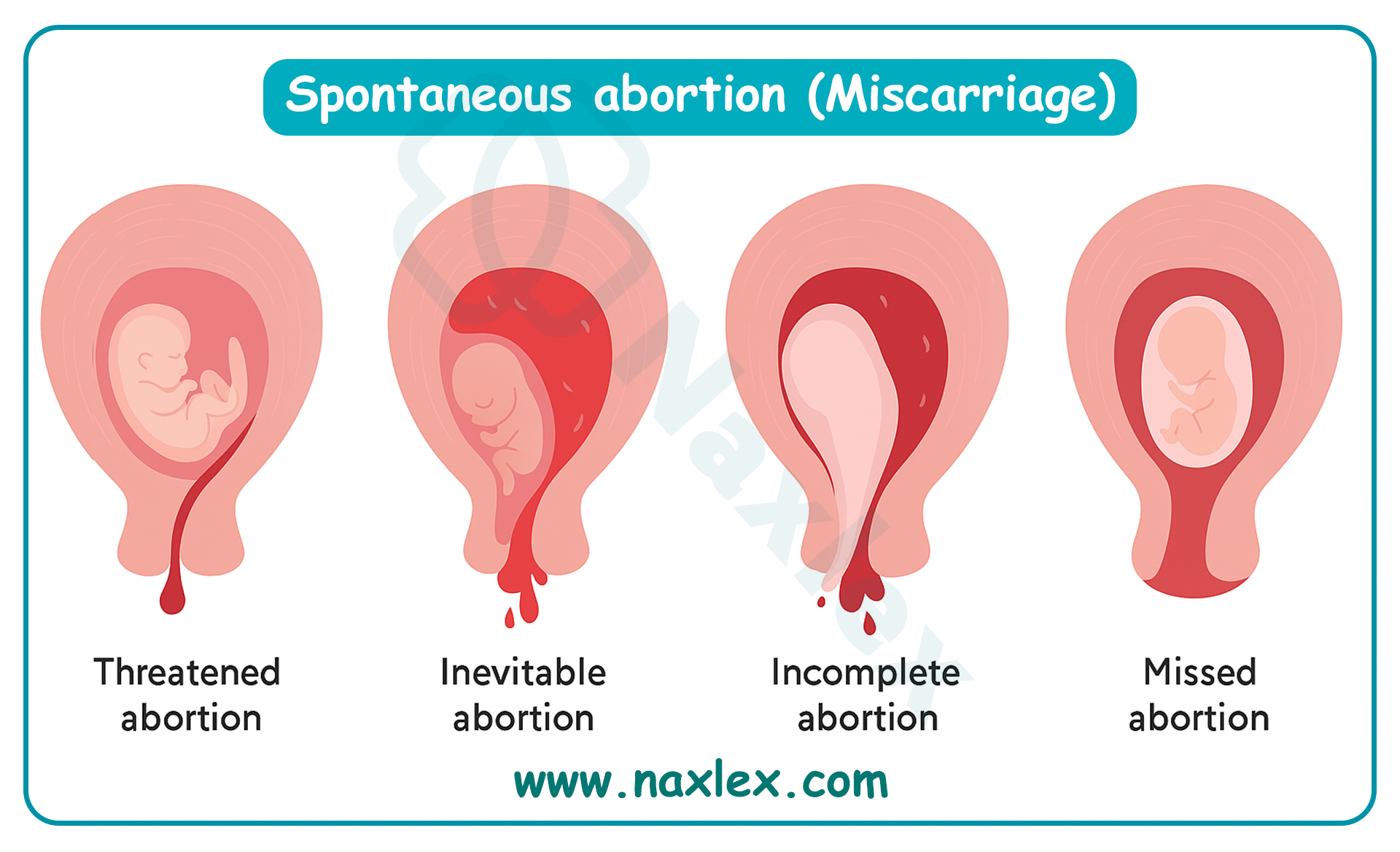
1.1 Definition and Epidemiology
Spontaneous abortion is defined as the spontaneous loss of a pregnancy before 20 weeks gestation or a fetal weight less than 500 grams, resulting from natural causes without external intervention. It is a common obstetric complication, occurring in approximately 10-20% of recognized pregnancies, with higher rates in clinically unrecognized pregnancies.
- Epidemiological data:
- Approximately 80% of spontaneous abortions occur in the first trimester, with the incidence decreasing significantly after 12 weeks gestation.
- The true prevalence is likely higher, as many early losses occur before pregnancy confirmation, often mistaken for delayed menstruation.
- Advanced maternal age (>35 years) increases the risk, with miscarriage rates rising to 20-35% in women aged 35-40 and over 50% in women over 40.
- Recurrent spontaneous abortion, defined as three or more consecutive losses, affects approximately 1-2% of reproductive-age women.
- Impact on maternal health:
- Spontaneous abortion can lead to significant emotional and physical consequences, including grief, anxiety, and potential complications like hemorrhage or infection.
- The condition is a leading cause of first-trimester hospitalization among pregnant women, necessitating prompt nursing assessment and intervention.
Nursing Insights
- Nurses must recognize that spontaneous abortion is a common occurrence, particularly in the first trimester, to provide accurate patient education and reduce unnecessary alarm.
- Understanding the higher incidence in older maternal age groups guides nurses in identifying at-risk patients during prenatal assessments.
- Accurate documentation of pregnancy history, including prior losses, is essential for identifying patients at risk for recurrent spontaneous abortion.
- Nurses should anticipate the emotional impact of miscarriage and prepare to offer empathetic support and resources during patient interactions.
1.2 Etiology and Risk Factors
Spontaneous abortion results from a complex interplay of genetic, maternal, environmental, and lifestyle factors. Identifying these etiologies and risk factors is critical for risk assessment and patient counseling.
- Genetic factors:
- Chromosomal abnormalities, primarily aneuploidy (e.g., trisomy 16, 21, or monosomy X), account for 50-60% of first-trimester spontaneous abortions.
- Parental balanced translocations or inversions increase the risk of embryonic chromosomal errors.
- Maternal medical conditions:
- Endocrine disorders, such as uncontrolled diabetes mellitus or hypothyroidism, impair embryonic development and implantation.
- Autoimmune conditions, like antiphospholipid syndrome (APS), cause recurrent thrombosis and placental insufficiency.
- Polycystic ovary syndrome (PCOS) is associated with hormonal imbalances that may disrupt early pregnancy maintenance.
- Uterine anomalies:
- Congenital anomalies, such as septate or bicornuate uterus, compromise endometrial blood supply and implantation.
- Acquired conditions, like Asherman syndrome (intrauterine adhesions), impair endometrial receptivity.
- Infections:
- Maternal infections, such as cytomegalovirus, toxoplasmosis, or bacterial vaginosis, may lead to embryonic demise or preterm labor.
- Lifestyle and environmental factors:
- Smoking, heavy alcohol consumption, and illicit drug use (e.g., cocaine) increase oxidative stress and impair fetal development.
- Exposure to environmental toxins, such as lead or radiation, is linked to higher miscarriage rates.
- Obesity (BMI >30) and extreme underweight (BMI <18.5) alter hormonal balance and increase risk.
- Other risk factors:
- Advanced paternal age (>40 years) may contribute to sperm DNA fragmentation, increasing miscarriage risk.
- Cervical insufficiency typically causes second-trimester losses due to premature cervical dilation.
- Trauma or severe stress may exacerbate underlying risk factors, though direct causation is less clear.
Nursing Insights
- Nurses must conduct a thorough history to identify risk factors, such as prior miscarriages, maternal age, or chronic conditions, to tailor patient education and referrals.
- Screening for lifestyle factors, including smoking or substance use, enables nurses to provide targeted counseling to mitigate modifiable risks.
- Recognizing the role of chromosomal abnormalities reassures patients that many miscarriages are not preventable, reducing feelings of guilt.
- Nurses should advocate for early screening for maternal infections or autoimmune disorders in patients with a history of pregnancy loss.
1.3 Pathophysiology of Pregnancy Loss
The pathophysiology of spontaneous abortion involves disruptions in the complex processes of embryonic development, implantation, and placental formation, leading to pregnancy failure.
- Embryonic factors:
- Chromosomal aneuploidy disrupts normal cell division and organogenesis, leading to nonviable embryos.
- Failure of trophoblast invasion impairs placental development, reducing nutrient and oxygen supply to the embryo.
- Maternal factors:
- Insufficient progesterone production by the corpus luteum or placenta fails to maintain endometrial integrity, triggering uterine contractions and expulsion.
- Thrombotic events in APS or other coagulopathies cause placental infarction and fetal demise.
- Endometrial and uterine factors:
- Inadequate decidualization due to hormonal imbalances or uterine anomalies compromises implantation stability.
- Intrauterine adhesions (Asherman syndrome) reduce endometrial surface area, hindering embryonic attachment.
- Immune and inflammatory responses:
- Dysregulated immune responses, such as excessive natural killer cell activity, may reject the embryo as foreign tissue.
- Systemic infections or localized endometritis trigger inflammatory cascades, leading to pregnancy loss.
- Vascular disruptions:
- Impaired spiral artery remodeling reduces uteroplacental blood flow, causing embryonic hypoxia and demise.
- Microhemorrhages or hematomas (e.g., subchorionic hematoma) may destabilize the implantation site.
Nursing Insights
- Understanding the role of progesterone in maintaining pregnancy guides nurses in monitoring for signs of hormonal insufficiency, such as early bleeding or cramping.
- Nurses must recognize that chromosomal abnormalities are the leading cause of first-trimester losses, informing empathetic patient education.
- Knowledge of uterine anomalies and their impact on implantation helps nurses advocate for imaging studies in patients with recurrent losses.
- Awareness of immune-mediated causes, such as APS, prompts nurses to assess for clotting disorders and coordinate multidisciplinary care.
1.4 Classification of Spontaneous Abortion
Spontaneous abortions are classified into distinct types based on clinical presentation, cervical status, and ultrasound findings. Each type has unique implications for management and nursing care.
1.4.1 Threatened Abortion
Threatened abortion is characterized by vaginal bleeding in the first 20 weeks of pregnancy with a closed cervical os and a viable intrauterine pregnancy confirmed by ultrasound.
- Clinical features:
- Light to moderate vaginal bleeding, typically bright red or brown, without passage of tissue.
- Mild cramping or pelvic discomfort may be present, but severe pain is absent.
- Fetal heart tones are detectable, and the cervix remains closed on examination.
- Prognosis:
- Approximately 50% of threatened abortions progress to normal pregnancies with appropriate management.
- Persistent bleeding or worsening symptoms may indicate progression to inevitable or incomplete abortion.
Nursing Insights
- Nurses must reassure patients that threatened abortion does not always lead to pregnancy loss, emphasizing the importance of pelvic rest and monitoring.
- Regular assessment of bleeding volume and vital signs is critical to detect progression to more severe types of abortion.
- Educating patients to avoid intercourse, tampons, and strenuous activity reduces the risk of exacerbating bleeding.
- Nurses should coordinate ultrasound follow-up to confirm fetal viability and monitor for complications like subchorionic hematoma.
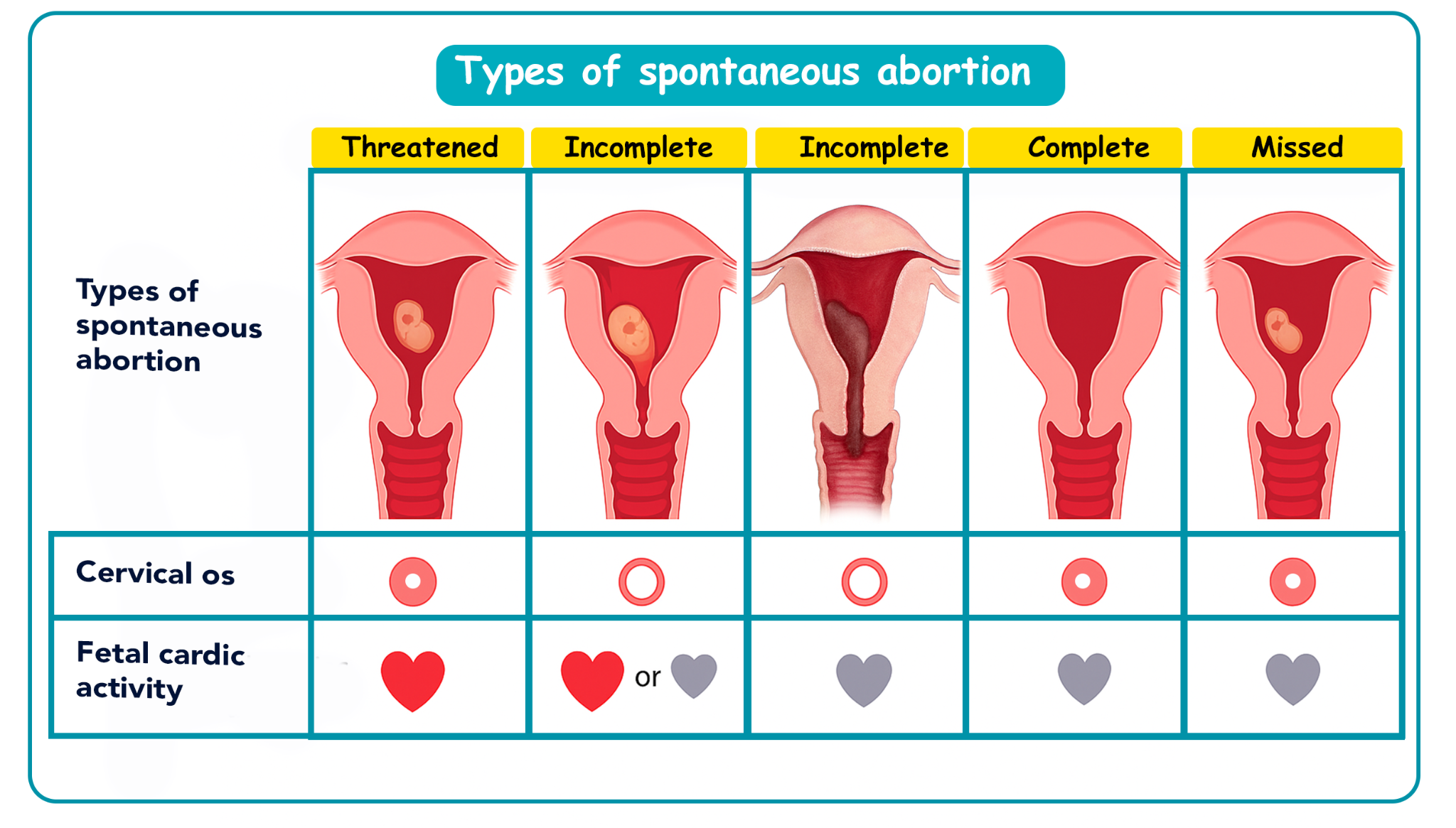
1.4.2 Inevitable Abortion
Inevitable abortion is diagnosed when vaginal bleeding and uterine contractions occur with cervical dilation, indicating that pregnancy loss is unavoidable.
- Clinical features:
- Heavy vaginal bleeding, often with clots, accompanied by moderate to severe uterine cramping.
- Open cervical os on speculum examination, with or without passage of tissue.
- Fetal heart tones may be absent, though early in the process, viability may still be present.
- Progression:
- Inevitable abortion typically progresses to incomplete or complete abortion without intervention.
- Immediate management is required to prevent complications like hemorrhage.
Nursing Insights
- Nurses must prepare patients for the likelihood of pregnancy loss, providing emotional support while explaining the clinical findings.
- Monitoring for signs of hypovolemic shock (e.g., tachycardia, hypotension) is essential due to the risk of heavy bleeding.
- Nurses should ensure rapid access to medical or surgical interventions, such as misoprostol or dilation and curettage (D&C), to manage tissue expulsion.
- Accurate documentation of bleeding volume and cervical status guides the healthcare team in determining the urgency of intervention.
1.4.3 Incomplete Abortion
Incomplete abortion occurs when partial expulsion of the products of conception takes place, with retained tissue remaining in the uterus.
- Clinical features:
- Heavy vaginal bleeding with passage of clots or tissue fragments.
- Persistent uterine cramping due to incomplete expulsion.
- Open cervical os and ultrasound evidence of retained products of conception.
- Management considerations:
- Requires medical or surgical intervention to complete evacuation and prevent complications like infection or hemorrhage.
Nursing Insights
- Nurses must monitor for signs of infection, such as fever or foul-smelling discharge, in patients with incomplete abortion due to retained tissue.
- Assessing bleeding volume (e.g., soaking a pad in <1 hour) is critical to identify the need for urgent intervention.
- Nurses should prepare patients for potential procedures, such as D&C or misoprostol administration, explaining the process and expected outcomes.
- Providing pain management, such as ibuprofen or prescribed analgesics, improves patient comfort during the expulsion process.
1.4.4 Complete Abortion
Complete abortion is characterized by the full expulsion of all products of conception, with cessation of bleeding and a closed cervical os.
- Clinical features:
- Initial heavy bleeding and cramping, followed by cessation of symptoms.
- Ultrasound confirms an empty uterus with no retained tissue.
- Declining hCG levels post-expulsion, indicating complete resolution.
- Prognosis:
- Typically requires minimal intervention, with focus on monitoring for complications and providing emotional support.
Nursing Insights
- Nurses must confirm complete expulsion through ultrasound and declining hCG levels to ensure no retained tissue remains.
- Patient education on post-miscarriage care, including avoiding tampons and intercourse for 2-4 weeks, reduces infection risk.
- Monitoring for excessive bleeding or signs of infection post-expulsion is essential, even in complete abortion cases.
- Nurses should provide empathetic support, as patients may experience significant grief despite resolution of physical symptoms.
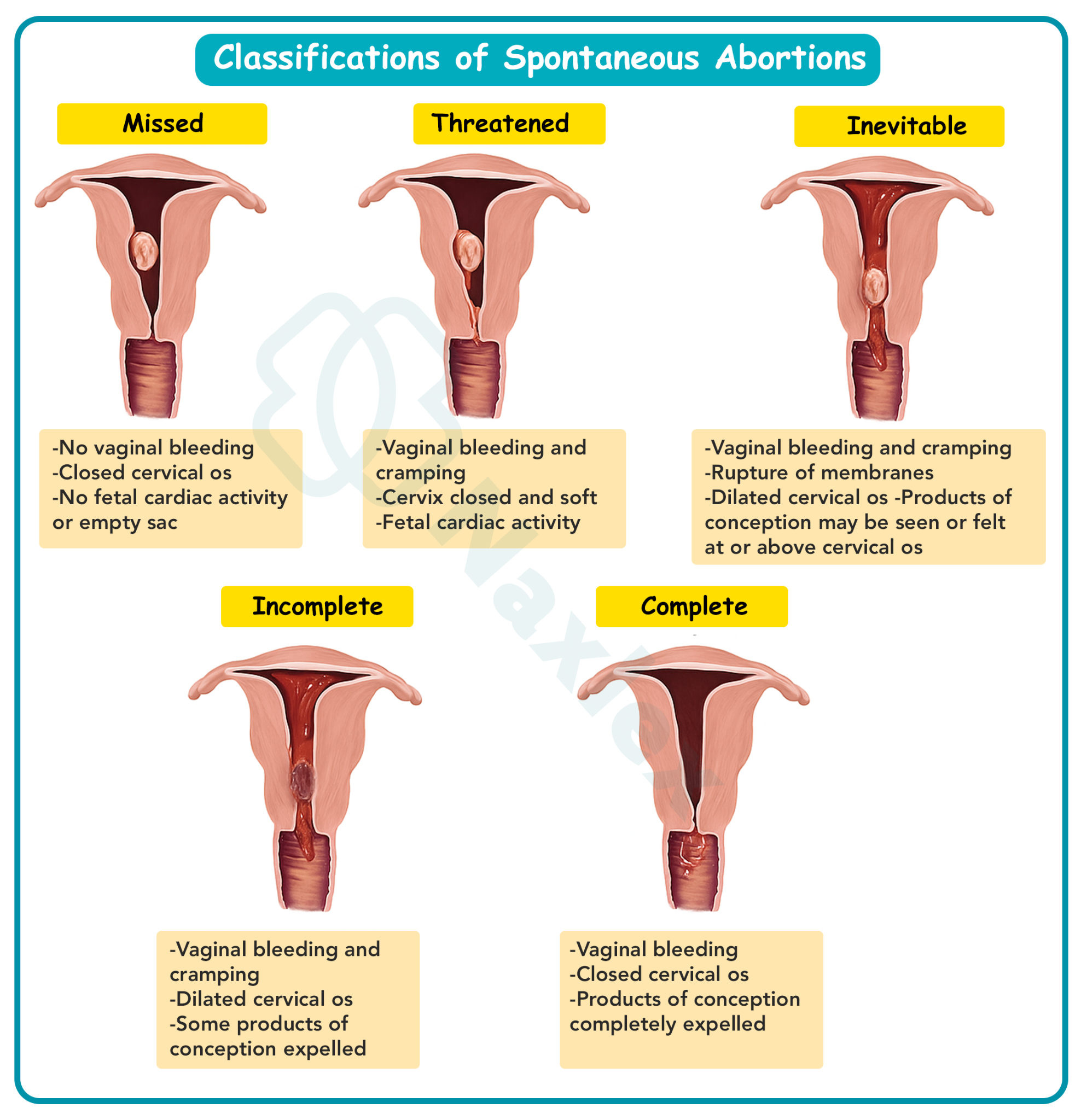
1.4.5 Missed Abortion
Missed abortion is defined as fetal demise without expulsion of the products of conception, often detected incidentally on ultrasound.
- Clinical features:
- Loss of pregnancy symptoms (e.g., nausea, breast tenderness) without vaginal bleeding.
- Ultrasound reveals an empty gestational sac or no fetal heartbeat.
- Closed cervical os, with no immediate signs of expulsion.
- Management considerations:
- May be managed expectantly, medically, or surgically, depending on patient preference and clinical stability.
Nursing Insights
- Nurses must recognize the absence of bleeding in missed abortion, prompting ultrasound evaluation in patients reporting loss of pregnancy symptoms.
- Providing emotional support is critical, as patients may be unaware of the loss until diagnostic confirmation, leading to sudden grief.
- Nurses should educate patients on management options (expectant, medical, or surgical), ensuring informed decision-making.
- Monitoring for complications, such as disseminated intravascular coagulation (DIC) with prolonged retention, is essential in missed abortion cases.
1.4.6 Recurrent (Habitual) Abortion
Recurrent abortion is defined as three or more consecutive spontaneous abortions before 20 weeks gestation, affecting 1-2% of women.
- Clinical features:
- Repeated pregnancy losses with similar clinical presentations (e.g., bleeding, cramping, or missed abortion).
- Often associated with underlying maternal or genetic factors requiring specialist evaluation.
- Etiology:
- Includes parental chromosomal abnormalities, uterine anomalies, APS, or endocrine disorders.
- Psychological stress and grief may compound physical risk factors.
Nursing Insights
- Nurses must advocate for referral to a reproductive endocrinologist for comprehensive evaluation in patients with recurrent abortion.
- Detailed history-taking to identify patterns of loss (e.g., timing, symptoms) guides diagnostic workup and management planning.
- Providing psychosocial support is critical, as recurrent losses lead to significant emotional distress and potential depression.
- Nurses should educate patients on modifiable risk factors, such as smoking cessation, to reduce the likelihood of future losses.
1.5 Assessment and Diagnostic Evaluation
Accurate assessment and diagnostic evaluation of spontaneous abortion are critical to determine the type, guide management, and identify complications.
- History taking:
- Document the onset, volume, and characteristics of vaginal bleeding (e.g., color, clots, tissue passage).
- Assess associated symptoms, such as cramping, loss of pregnancy symptoms, or systemic signs (e.g., fever, dizziness).
- Review obstetric history, including prior miscarriages, gestational age, and risk factors (e.g., smoking, chronic conditions).
- Physical examination:
- Speculum examination: Assess cervical os status (open vs. closed) and presence of tissue or clots at the os.
- Bimanual examination: Evaluate uterine size, consistency, and adnexal tenderness to rule out ectopic pregnancy or masses.
- Vital signs: Monitor for tachycardia, hypotension, or fever, indicating potential hemorrhage or infection.
- Diagnostic tests:
- Transvaginal ultrasound: Confirms intrauterine pregnancy, fetal viability, or retained products; key findings include empty gestational sac (missed abortion), open cervical os (inevitable/incomplete), or empty uterus (complete).
- Quantitative hCG levels: Doubling every 48-72 hours indicates viable pregnancy; plateauing or declining levels suggest nonviability.
- Serum progesterone: Levels <5 ng/mL indicate nonviable pregnancy; levels >25 ng/mL suggest viability.
- Complete blood count (CBC): Assesses hemoglobin/hematocrit for anemia due to blood loss.
- Blood type and Rh factor: Determines need for Rh immune globulin in Rh-negative patients.
- Coagulation studies: Rules out DIC in cases of prolonged retention (missed abortion).
- Differential diagnosis:
- Ectopic pregnancy: Adnexal mass or pain, abnormal hCG trends.
- Molar pregnancy: Grape-like vesicles, excessively elevated hCG, “snowstorm” ultrasound pattern.
- Cervical pathology: Friability or polyps causing bleeding without intrauterine pathology.
Nursing Insights
- Nurses must ensure accurate documentation of bleeding patterns and associated symptoms to guide diagnostic evaluation and management.
- Preparing patients for transvaginal ultrasound involves explaining the procedure and ensuring comfort to facilitate accurate imaging.
- Monitoring vital signs regularly detects early signs of hemodynamic instability, prompting timely intervention.
- Nurses should confirm Rh status and advocate for RhoGAM administration within 72 hours for Rh-negative patients to prevent isoimmunization.
1.6 Nursing and Medical Interventions for Each Type
Interventions for spontaneous abortion vary by type, ranging from expectant management to medical or surgical approaches, with nursing care focusing on monitoring, support, and complication prevention.
- Threatened abortion:
- Expectant management: Pelvic rest (avoiding intercourse, tampons, strenuous activity), serial hCG monitoring, and ultrasound follow-up to confirm viability.
- Nursing role: Educate on pelvic rest, monitor bleeding and vital signs, provide emotional support, and coordinate follow-up appointments.
- Inevitable abortion:
- Medical management: Misoprostol to facilitate uterine evacuation if incomplete expulsion occurs.
- Surgical management: Dilation and curettage (D&C) for excessive bleeding or patient preference.
- Nursing role: Administer pain relief, monitor for hemorrhage, prepare for surgical intervention, and provide empathetic communication.
- Incomplete abortion:
- Medical management: Misoprostol (800 mcg vaginally or orally) to promote expulsion of retained tissue.
- Surgical management: D&C to remove retained products and prevent complications.
- Nursing role: Monitor bleeding volume, administer medications as prescribed, assess for infection, and educate on post-procedure care.
- Complete abortion:
- Management: Confirm complete expulsion via ultrasound and declining hCG levels; no further intervention typically required.
- Nursing role: Monitor for complications (e.g., infection), provide discharge instructions, and offer grief counseling.
- Missed abortion:
- Expectant management: Await spontaneous expulsion if stable, with close monitoring.
- Medical management: Misoprostol or mifepristone to induce expulsion.
- Surgical management: D&C or vacuum aspiration for patient preference or prolonged retention.
- Nursing role: Educate on management options, monitor for DIC, provide emotional support, and coordinate follow-up.
- Recurrent abortion:
- Management: Referral to a reproductive endocrinologist for evaluation of underlying causes (e.g., APS, uterine anomalies).
- Nursing role: Coordinate specialist referrals, educate on modifiable risk factors, and provide ongoing psychosocial support.
Nursing Insights
- Nurses must educate patients on the rationale for pelvic rest in threatened abortion to enhance compliance and reduce bleeding risk.
- Administering misoprostol requires explaining side effects (e.g., cramping, diarrhea) and monitoring for excessive bleeding post-dose.
- Preparing patients for D&C involves preoperative education, ensuring informed consent, and monitoring for post-procedure complications.
- Nurses should advocate for RhoGAM administration in Rh-negative patients within 72 hours of miscarriage to prevent future complications.
1.7 Complications of Abortion
Spontaneous abortion may lead to several complications, necessitating vigilant nursing assessment and timely intervention.
- Hemorrhage:
- Excessive bleeding due to incomplete expulsion or uterine atony, leading to hypovolemic shock (tachycardia, hypotension, dizziness).
- Management includes fluid resuscitation, uterotonics (e.g., oxytocin), or surgical evacuation.
- Infection:
- Endometritis or sepsis from retained tissue or post-procedure contamination, presenting with fever, foul-smelling discharge, or pelvic pain.
- Treated with antibiotics and removal of retained products.
- Asherman syndrome:
- Intrauterine adhesions from repeated D&C procedures, leading to infertility or recurrent pregnancy loss.
- Diagnosed via hysteroscopy and managed with adhesiolysis.
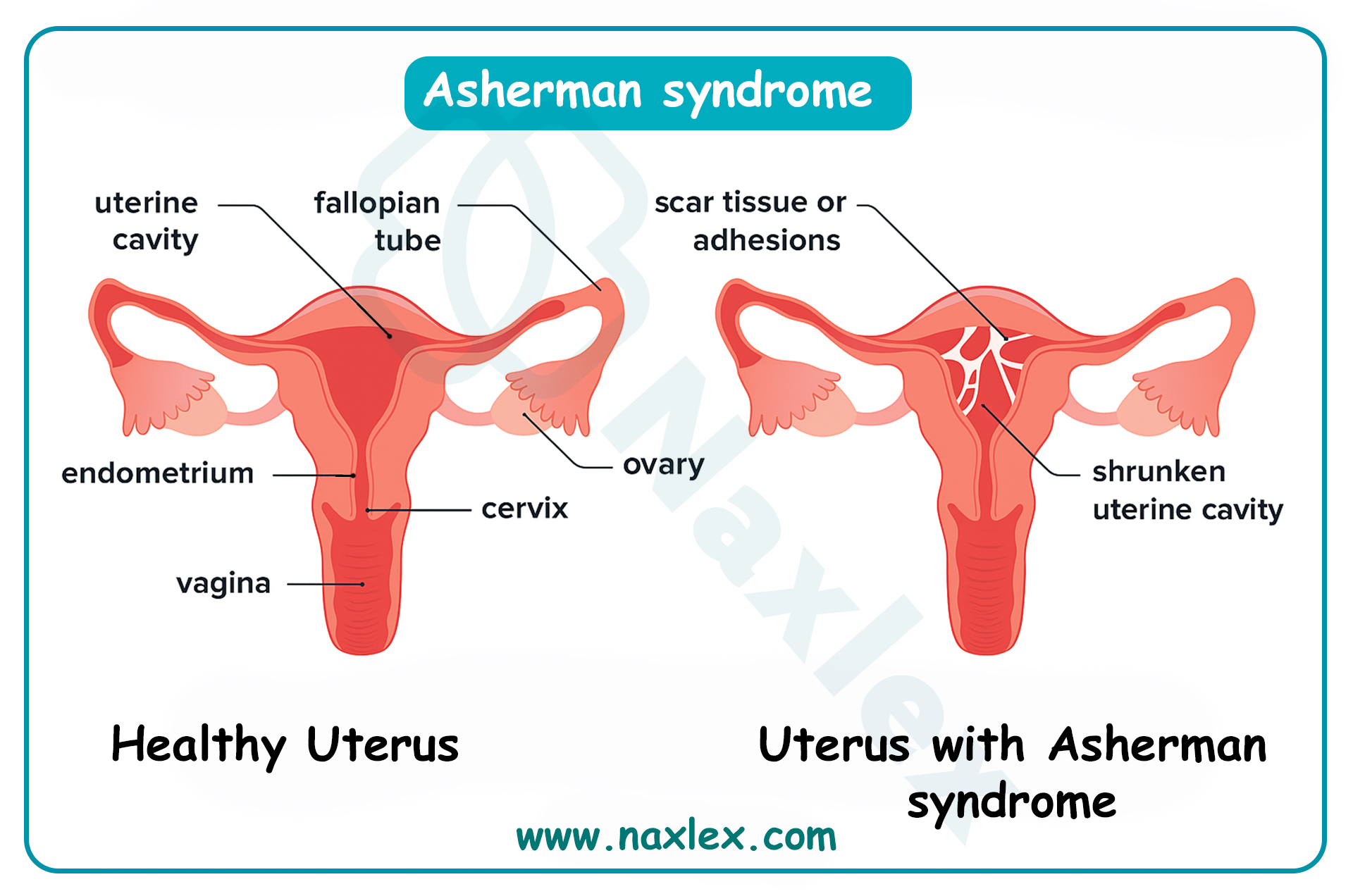
- Disseminated intravascular coagulation (DIC):
- Rare in missed abortion with prolonged retention of nonviable tissue, causing coagulopathy and bleeding tendencies.
- Requires urgent hematological management and tissue evacuation.
- Rh isoimmunization:
- Occurs in Rh-negative mothers exposed to Rh-positive fetal blood, risking alloimmunization in future pregnancies.
- Prevented with RhoGAM administration within 72 hours.
- Psychological impact:
- Grief, depression, or anxiety following pregnancy loss, potentially requiring counseling or support group referral.
Nursing Insights
- Nurses must monitor for signs of hemorrhage, such as soaking a pad in <1 hour, and initiate fluid resuscitation promptly if instability is detected.
- Assessing for fever or foul-smelling discharge post-miscarriage is critical to identify and treat infection early.
- Educating patients on the risks of repeated D&C procedures, such as Asherman syndrome, supports informed decision-making for management options.
- Nurses should ensure RhoGAM is administered to Rh-negative patients to prevent isoimmunization, documenting the dose and timing.
1.8 Psychosocial and Emotional Considerations in Pregnancy Loss
Spontaneous abortion often results in significant emotional distress, requiring nurses to provide empathetic, patient-centered support to address grief and promote coping.
- Emotional responses:
- Patients may experience a range of emotions, including sadness, guilt, anger, or denial, which vary in intensity and duration.
- Partners and family members may also require support, as pregnancy loss affects the entire support system.
- Nursing interventions:
- Use active listening to validate patient feelings, avoiding dismissive phrases like “you can try again.”
- Offer information on support groups, counseling services, or chaplaincy for spiritual support.
- Provide a nonjudgmental environment, acknowledging the individual nature of grief.
- Cultural considerations:
- Cultural or religious beliefs may influence grieving processes, requiring tailored support and sensitivity.
- Nurses should inquire about cultural practices to ensure respectful care delivery.
- Follow-up care:
- Schedule follow-up appointments to assess emotional well-being and provide ongoing support.
- Refer patients with prolonged grief or depression to mental health professionals.
Nursing Insights
- Nurses must use empathetic communication, such as acknowledging the loss with phrases like “I’m so sorry for your loss,” to build trust and support patients.
- Offering resources, such as grief counseling or support group contacts, empowers patients to seek help during the grieving process.
- Recognizing cultural differences in grief expression ensures culturally competent care and enhances patient comfort.
- Nurses should monitor for signs of prolonged grief or depression, advocating for mental health referrals as needed.
Induced Abortion
Induced abortion constitutes the deliberate termination of a pregnancy through medical or surgical means, performed under controlled clinical conditions to ensure patient safety and efficacy. This procedure, encompassing both therapeutic and elective indications, requires comprehensive nursing knowledge of legal frameworks, indications, methodologies, and supportive care to address the physical, emotional, and ethical dimensions of patient care. The following sections delineate the definition, legal considerations, indications, methods, nursing responsibilities, complications, and post-procedure counseling for induced abortion, providing nursing students with a scientifically rigorous foundation for evidence-based practice in maternal-newborn nursing.
1.1 Definition and Legal Considerations
Induced abortion is defined as the intentional interruption of pregnancy before fetal viability, utilizing pharmacological agents or mechanical procedures to expel the products of conception. It is distinguished from spontaneous abortion by its elective or therapeutic intent, with procedures typically performed before 20 weeks gestation to minimize maternal risks.
- Therapeutic versus elective abortion:
- Therapeutic abortion is performed to preserve maternal life or health, or due to fetal anomalies incompatible with life.
- Elective abortion occurs at the patient's request without medical necessity, often for socioeconomic, personal, or psychological reasons.
- Legal considerations:
- In the United States, following the 2022 Dobbs v. Jackson Women's Health Organization Supreme Court decision, abortion legality is regulated at the state level, with variations ranging from permissive access up to viability to near-total bans with exceptions for maternal life endangerment.
- Federal laws, such as the Partial-Birth Abortion Ban Act of 2003, prohibit certain late-term procedures, while the Hyde Amendment restricts federal funding for abortions except in cases of rape, incest, or life endangerment.
- Internationally, the World Health Organization advocates for safe abortion access as a reproductive right, with legal frameworks varying by country (e.g., liberal in Canada and Europe, restrictive in many Latin American and African nations).
- Informed consent is mandatory, requiring patients to receive comprehensive information on risks, benefits, alternatives, and gestational age limitations.
- Ethical implications for nursing:
- Nurses must adhere to institutional policies, personal ethics, and professional codes (e.g., American Nurses Association Code of Ethics), which support patient autonomy while allowing conscientious objection with appropriate referral.
- Documentation of consent, gestational age verification via ultrasound, and compliance with state-mandated waiting periods or counseling requirements are essential.
Nursing Insights
- Nurses must verify state-specific legal requirements, such as mandatory ultrasound or waiting periods, to ensure procedural compliance and protect patient rights.
- Obtaining comprehensive informed consent involves explaining procedure details, risks, and alternatives in a nonjudgmental manner to empower patient decision-making.
- In cases of conscientious objection, nurses should facilitate seamless referral to another provider without delaying care, maintaining professional integrity.
- Accurate documentation of gestational age and fetal viability assessment prevents legal challenges related to late-term procedures.
1.2 Indications for Induced Abortion
Indications for induced abortion encompass a broad spectrum of maternal, fetal, and psychosocial factors, guiding clinical decision-making to optimize patient outcomes.
- Maternal health indications:
- Life-threatening conditions, such as severe preeclampsia, eclampsia, or cardiac disease (e.g., Eisenmenger syndrome), where continuation poses imminent risk.
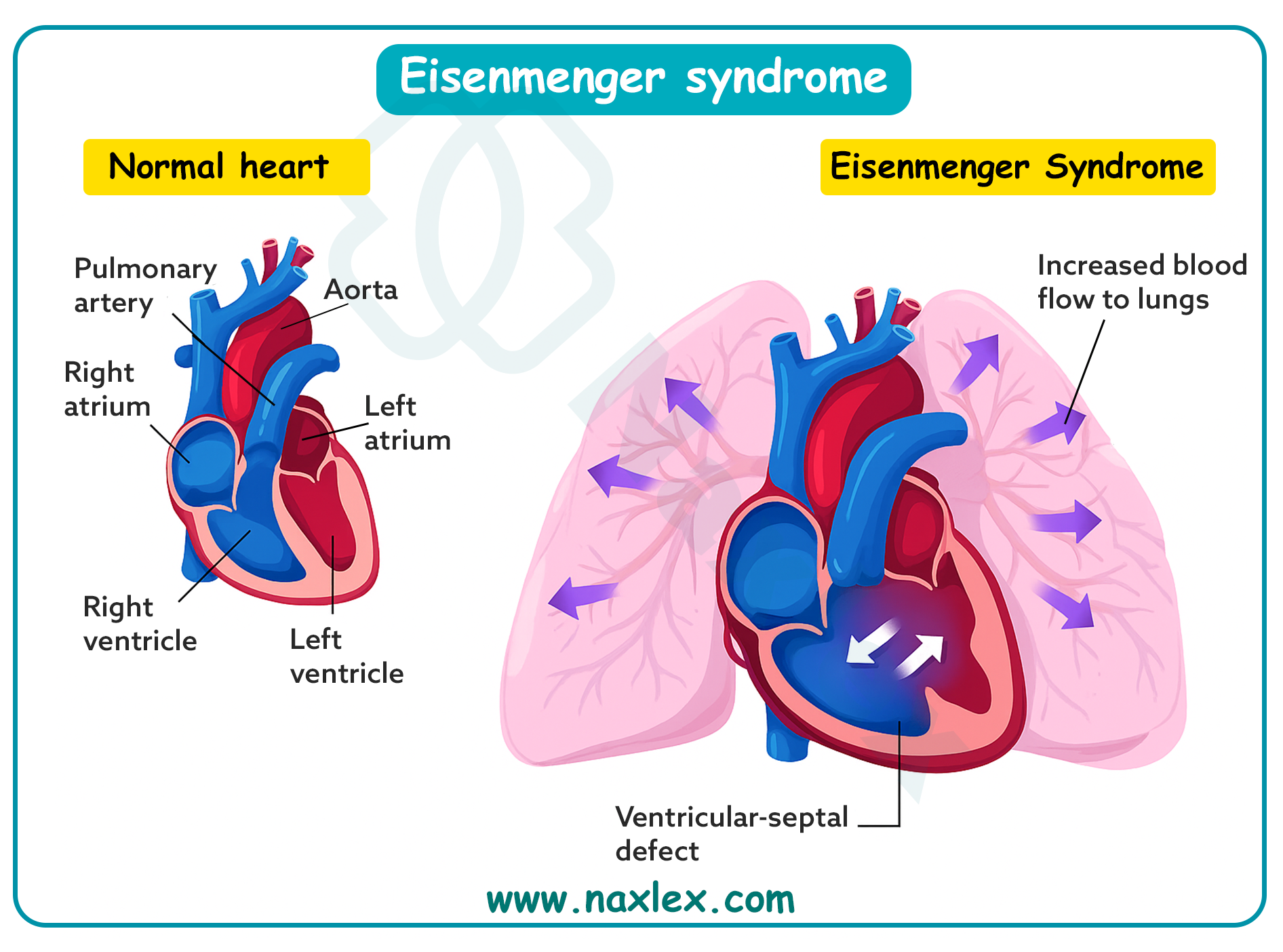
- Oncological diagnoses requiring immediate chemotherapy or radiation incompatible with pregnancy.
- Severe psychiatric disorders, including suicidal ideation, where pregnancy exacerbates mental health crises.
- Fetal indications:
- Congenital anomalies incompatible with extrauterine life, such as anencephaly or bilateral renal agenesis, confirmed via amniocentesis or chromosomal analysis.
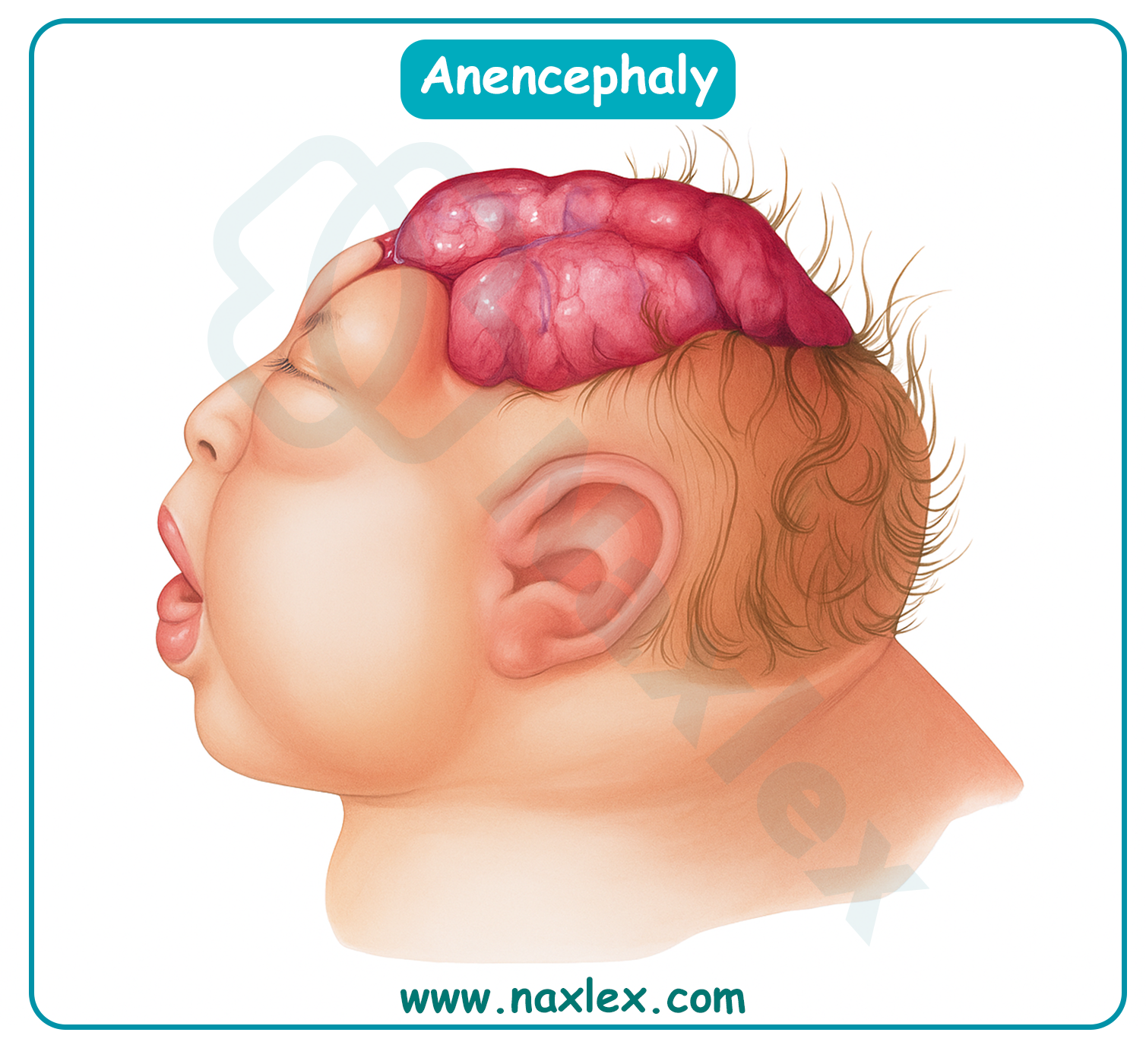
-
- Genetic disorders, including trisomy 13 or 18, detected through noninvasive prenatal testing (NIPT) or invasive diagnostics.
- Elective indications:
- Socioeconomic constraints, including financial instability, lack of support, or career considerations.
- Personal circumstances, such as relationship issues, age, or parity preferences.
- Contraceptive failure or unintended pregnancy, particularly in adolescents or women with multiple prior pregnancies.
- Combined indications:
- Rape, incest, or sexual assault, often compounded by psychological trauma.
- Substance use disorders, where fetal exposure risks developmental abnormalities.
Nursing Insights
- Nurses must conduct sensitive history-taking to identify indications, ensuring confidentiality and nonjudgmental support for patients disclosing sensitive information like assault.
- Verifying fetal anomalies through ultrasound or genetic testing requires empathetic communication of results to facilitate informed decision-making.
- Assessing psychosocial factors, such as support systems, guides referral to social services or counseling to address barriers to care.
- Nurses should advocate for timely access to abortion services in maternal health emergencies to prevent complications like maternal mortality.
1.3 Methods of Induced Abortion
Induced abortion methods are selected based on gestational age, patient preference, medical history, and facility resources, with efficacy rates exceeding 95% for most procedures.
1.3.1 Medical (Mifepristone, Misoprostol, Methotrexate)
Medical abortion involves pharmacological induction of pregnancy termination, suitable for gestations up to 10-11 weeks, offering a non-invasive alternative.
- Mifepristone and misoprostol regimen:
- Mifepristone (200 mg orally) antagonizes progesterone receptors, inhibiting uterine decidualization, reducing hCG production, and sensitizing the myometrium to prostaglandins.
- Misoprostol (800 mcg buccally, vaginally, or sublingually) 24-48 hours later induces cervical softening, uterine contractions, and expulsion of products, mimicking spontaneous abortion.
- Efficacy: 95-98% complete abortion rate; follow-up ultrasound or hCG assessment confirms success.
- Methotrexate:
- Administered intramuscularly (50 mg/m²) for early gestations (<7 weeks) or ectopic pregnancies, it inhibits dihydrofolate reductase, disrupting trophoblastic cell proliferation and DNA synthesis.
- Followed by misoprostol 3-7 days later to facilitate expulsion.
- Monitoring includes serial hCG levels (decline >15% by day 4 indicates success) and liver function tests due to hepatotoxicity risk.
- Pharmacokinetics and side effects:
- Common side effects include nausea, vomiting, diarrhea, and heavy bleeding/cramping; rare complications involve incomplete abortion (5%) or sepsis.
- Contraindications: Ectopic pregnancy, adrenal insufficiency, chronic corticosteroid use, or IUD in situ.
Nursing Insights
- Nurses must educate patients on the expected timeline of expulsion (4-6 hours post-misoprostol) and provide pain management strategies, such as ibuprofen, for cramping.
- Monitoring for excessive bleeding (soaking >2 pads/hour) post-medication requires telephone triage protocols to ensure timely intervention.
- Administering methotrexate involves assessing baseline liver and renal function, with follow-up labs to detect rare toxicities like leukopenia.
- Providing antiemetics prophylactically enhances patient comfort during the medical abortion process.
1.3.2 Surgical (Vacuum Aspiration, D&C, D&E)
Surgical methods provide definitive termination through mechanical evacuation, preferred for gestations beyond medical limits or patient preference for immediacy.
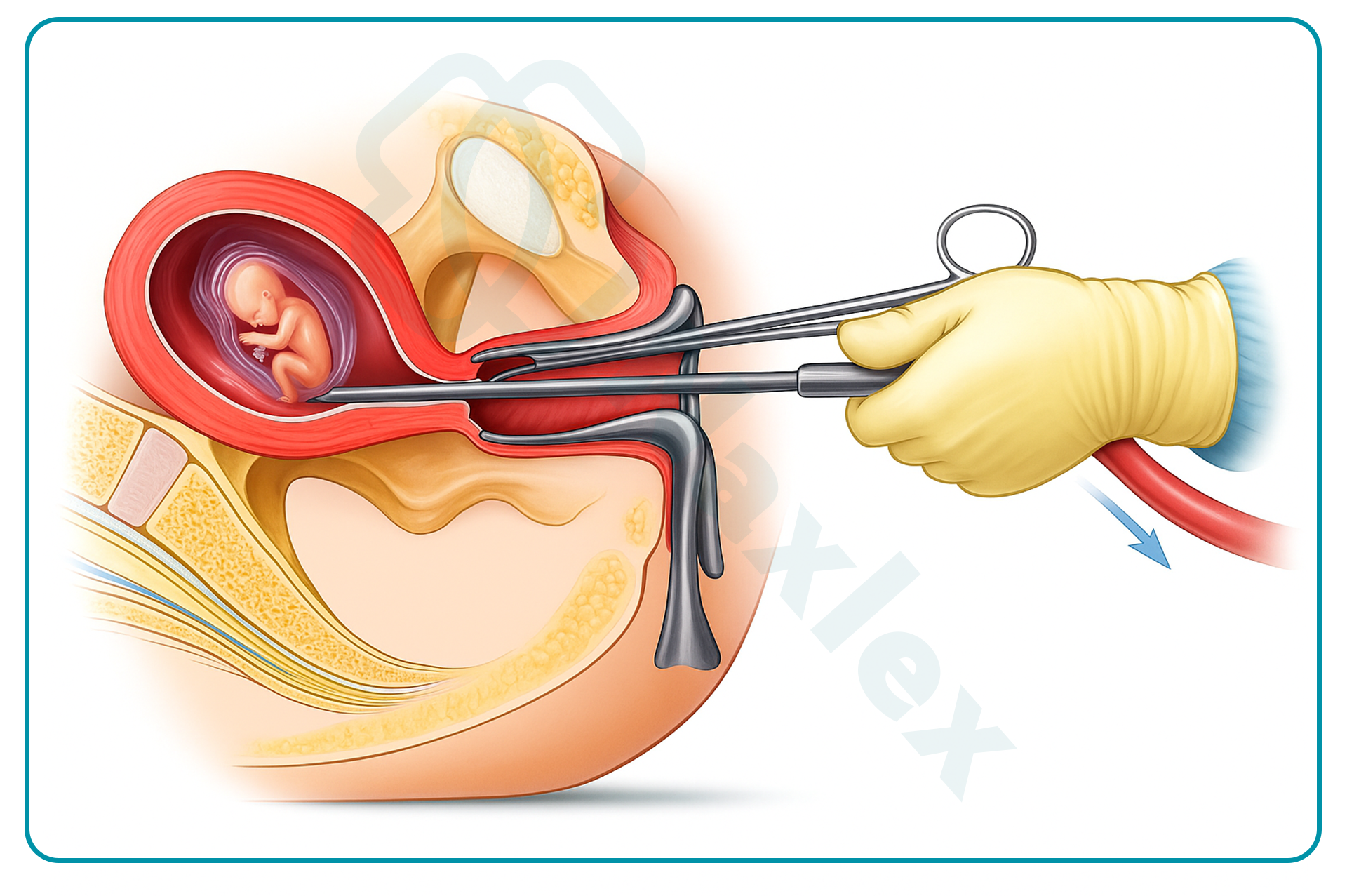
- Manual vacuum aspiration (MVA):
- Performed under local anesthesia up to 12 weeks, involving cervical dilation followed by aspiration using a 50-60 mL syringe to remove products.
- Efficacy: >99%; minimal blood loss (<50 mL) and rapid recovery.
- Electric vacuum aspiration (EVA):
- Utilizes suction cannula connected to electric pump for gestations 6-14 weeks, often with paracervical block or sedation.
- Sharp curettage may be combined for complete evacuation.
- Dilation and curettage (D&C):
- Involves mechanical dilation of cervix with laminaria or misoprostol, followed by sharp curette scraping of endometrium; used for incomplete spontaneous abortions or early induced terminations.
- Risks include uterine perforation (0.5%) or Asherman syndrome with repeated use.
- Dilation and evacuation (D&E):
- For second-trimester (13-24 weeks), combines vacuum aspiration with forceps extraction of fetal parts after osmotic dilators (laminaria) soften cervix over 24-48 hours.
- Requires general anesthesia; efficacy >99%, but higher risks of hemorrhage or infection.
- Procedural considerations:
- Preoperative ultrasound confirms gestational age and location; RhoGAM for Rh-negative patients.
- Postoperative verification via ultrasound or pathology ensures complete evacuation.
Nursing Insights
- Nurses must prepare patients for vacuum aspiration by explaining the procedure's brevity (5-10 minutes) and providing sedation options for anxiety reduction.
- Intra-procedure monitoring includes vital signs and pain assessment during D&E to detect complications like perforation.
- Post-D&C, nurses assess for retained products by monitoring bleeding and scheduling follow-up ultrasound if hCG persists.
- Using osmotic dilators requires patient education on expected cramping and discharge during overnight placement.
1.4 Nursing Responsibilities Pre, Intra, and Post Procedure
Nursing responsibilities in induced abortion span preoperative preparation, intraoperative support, and postoperative monitoring to ensure safety and holistic care.
- Pre-procedure responsibilities:
- Conduct comprehensive assessment, including vital signs, laboratory tests (CBC, Rh type, coagulation profile), and psychosocial evaluation.
- Verify informed consent, administer preoperative medications (e.g., misoprostol for cervical ripening, antibiotics prophylaxis).
- Provide education on procedure expectations, pain management, and recovery timeline; confirm gestational age via ultrasound.
- Intra-procedure responsibilities:
- Assist with positioning, monitor vital signs, and administer sedation or analgesia as ordered.
- Ensure sterile technique, prepare instruments, and provide emotional support during the procedure.
- Observe for immediate complications, such as vasovagal response or excessive bleeding.
- Post-procedure responsibilities:
- Monitor recovery in PACU for vital signs, bleeding, and pain; assess for perforation or infection signs.
- Provide discharge instructions on bleeding (expect light for 1-2 weeks), activity restrictions (no heavy lifting for 1 week), and warning signs (fever >100.4°F, foul discharge).
- Administer RhoGAM if indicated and schedule follow-up for hCG or ultrasound confirmation.
Nursing Insights
- Preoperative anxiety assessment allows nurses to offer calming techniques or referrals to counseling, enhancing patient cooperation.
- Intra-procedure, maintaining a supportive presence reduces patient distress during painful aspects like speculum insertion.
- Post-procedure vital sign monitoring every 15 minutes initially detects hypovolemia from undetected hemorrhage.
- Discharge teaching includes contraception options to prevent unintended pregnancies, tailored to patient preferences.
1.5 Complications and Risk Reduction
Complications of induced abortion are rare (<2%) but require vigilant monitoring and preventive strategies to mitigate risks.
- Immediate complications:
- Hemorrhage (0.4-1%), due to uterine atony or laceration, managed with uterotonics or re-aspiration.
- Infection (0.5%), endometritis or pelvic inflammatory disease, prevented with doxycycline prophylaxis.
- Uterine perforation (0.1-0.3%), detected intraoperatively via resistance or ultrasound, potentially requiring laparoscopy.
- Delayed complications:
- Retained products (1-2%), causing persistent bleeding; confirmed by ultrasound and treated with repeat evacuation.
- Asherman syndrome from aggressive curettage, leading to amenorrhea; risk reduced with ultrasound guidance.
- Cervical incompetence from trauma, increasing future preterm labor risk.
- Risk reduction strategies:
- Preoperative antibiotics (doxycycline 100 mg BID x 2 doses) reduce infection by 50%.
- Ultrasound guidance minimizes perforation and incomplete evacuation.
- Patient selection excludes contraindications like coagulopathy.
Nursing Insights
- Nurses monitor post-procedure bleeding pad counts hourly to quantify loss and intervene early for hemorrhage.
- Administering prophylactic antibiotics pre-procedure prevents ascending infections in high-risk patients.
- Educating on signs of perforation, such as severe pain or shoulder tip pain, prompts immediate return to care.
- Follow-up calls 24-48 hours post-discharge assess for delayed complications like retained tissue.
1.6 Post-Abortion Counseling and Contraception
Post-abortion counseling addresses emotional recovery and reproductive planning, integrating contraception to support future autonomy.
- Counseling components:
- Validate emotional responses, including relief, guilt, or grief; refer to counseling for complex reactions.
- Discuss physical recovery, resuming menses (2-4 weeks), and fertility return (immediately post-procedure).
- Address myths, such as infertility risk (no increased long-term risk with safe procedures).
- Contraception options:
- Immediate initiation: Progestin-only pills, patch, or ring effective from day 1; IUD insertion post-procedure.
- Long-acting reversible contraception (LARC): Intrauterine devices (copper or levonorgestrel) with >99% efficacy, inserted immediately to reduce repeat unintended pregnancies.
- Barrier methods: Condoms for STI prevention; combined hormonal methods after 1 week.
- Follow-up care:
- Clinic visit 1-2 weeks post-procedure for complication assessment and contraception initiation.
- hCG monitoring if medical abortion to confirm decline (>90% drop indicates success).
Nursing Insights
- Nurses facilitate open discussions on emotions, using active listening to identify needs for grief support or psychiatric referral.
- Offering immediate contraception, like etonogestrel implant, empowers patients and reduces unintended pregnancy rates by 80%.
- Tailoring contraception to patient lifestyle (e.g., depot medroxyprogesterone for irregular access) enhances adherence.
- Scheduling follow-up ensures resolution of complications and reinforces education on warning signs.
Ectopic Pregnancy
Ectopic pregnancy constitutes a critical obstetric emergency wherein the fertilized ovum implants outside the endometrial cavity, predominantly within the fallopian tube, posing substantial risks to maternal health and fertility. This pathological implantation disrupts normal embryonic development and may culminate in life-threatening complications, necessitating prompt recognition and intervention in maternal-newborn nursing practice. The ensuing sections expound upon the definition, pathophysiology, risk factors, clinical manifestations, diagnostic modalities, therapeutic interventions, and associated complications of ectopic pregnancy, furnishing nursing students with an exhaustive, scientifically grounded compendium to facilitate proficient clinical acumen and patient-centered care.
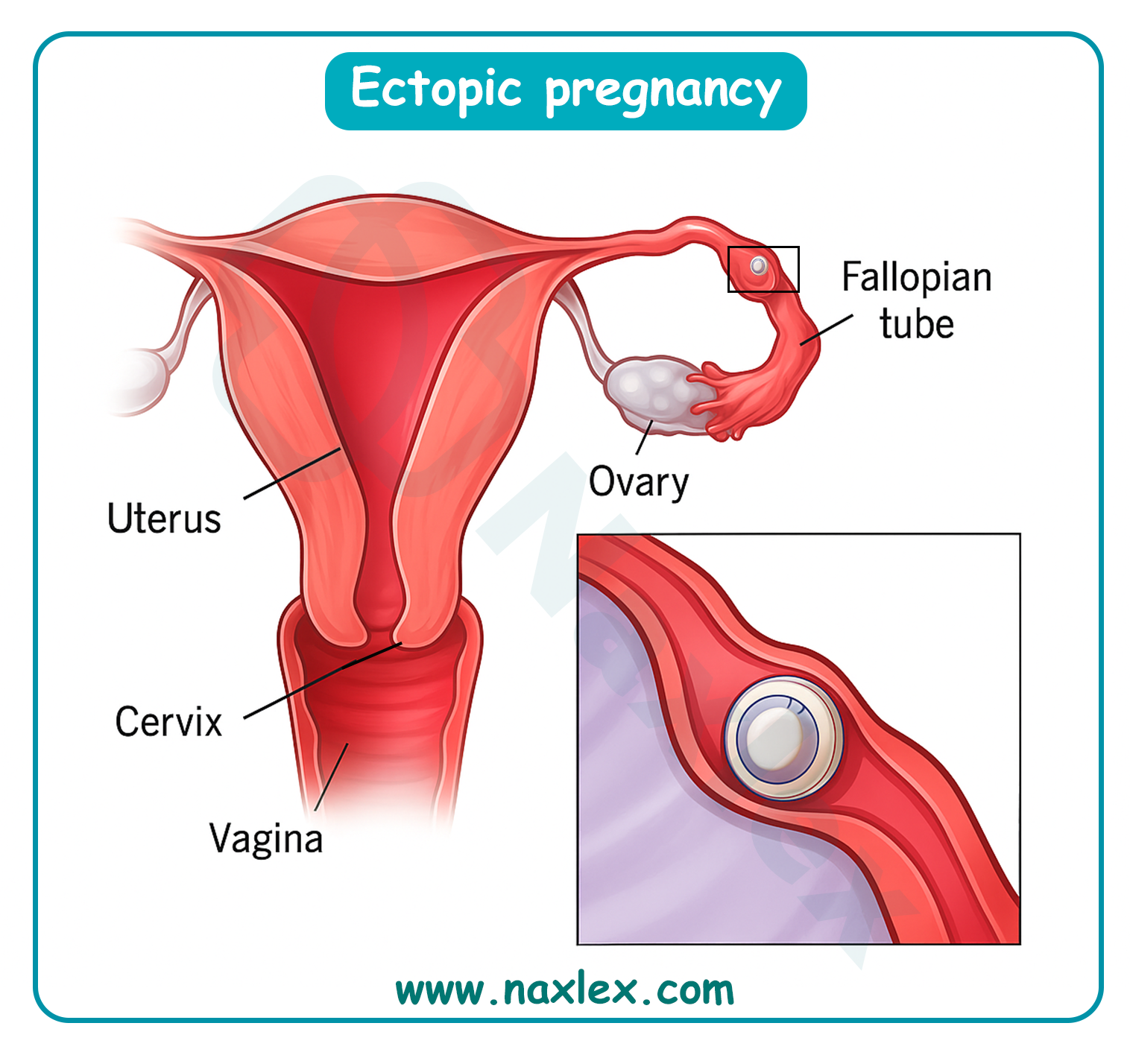
1.1 Definition and Pathophysiology
Ectopic pregnancy is delineated as the aberrant implantation of a fertilized ovum exterior to the uterine endometrial cavity, with approximately 97% of instances occurring within the fallopian tube, encompassing ampullary (70%), isthmic (12%), fimbrial (11%), and interstitial (2-3%) segments. Extratubal sites, comprising ovarian, abdominal, cervical, and cesarean scar implantations, account for the residual 3%, each engendering distinctive pathophysiological sequelae and management imperatives.
- Pathophysiological mechanisms:
- The primordial etiology resides in impeded zygotic transit through the fallopian tube, attributable to ciliary dysfunction, muscular dysmotility, or anatomical obstructions, precipitating premature trophoblastic invasion and implantation within the tubal mucosa.
- Inflammatory perturbations, such as those induced by Chlamydia trachomatis or Neisseria gonorrhoeae, engender salpingitis, culminating in ciliary epithelial damage, intraluminal adhesions, and hydrosalpinx formation, thereby retarding embryonic progression and fostering ectopic nidation.
- Hormonal disequilibria, including elevated progesterone levels from progestin-only contraceptives or luteal phase defects, attenuate tubal peristalsis and ciliary beat frequency, augmenting the propensity for tubal implantation.
- Trophoblastic proliferation within the confined tubal lumen elicits distension, vascular erosion, and potential rupture, instigating hemoperitoneum and hypovolemic shock.
- In extratubal ectopics, such as ovarian pregnancies, implantation ensues upon fertilization within the ovarian cortex or peritoneal surface, adhering to Spiegelberg's criteria: intact ipsilateral tube, fetal sac occupying ovarian position, tubo-ovarian ligament connection, and histologically confirmed ovarian tissue.
- Cesarean scar ectopics arise from implantation within myometrial dehiscence at prior hysterotomy sites, potentially evolving into placenta accreta spectrum disorders if undiagnosed.
Nursing Insights
- Nurses must apprehend that ectopic pregnancy predominantly manifests in the fallopian tube's ampullary segment, where the luminal diameter permits initial embryonic growth prior to symptomatic presentation.
- Recognition of inflammatory etiologies, such as pelvic inflammatory disease, mandates nurses to elicit comprehensive sexual histories to identify at-risk patients during initial assessments.
- Comprehension of hormonal influences on tubal motility equips nurses to counsel patients on the augmented ectopic risk associated with progestin-based contraceptives.
- Awareness of extratubal variants, like cesarean scar ectopics, prompts nurses to scrutinize obstetric histories for prior cesarean deliveries in symptomatic patients.
1.2 Risk Factors
Risk factors for ectopic pregnancy encompass a multifarious array of anatomical, infectious, hormonal, and iatrogenic elements that compromise fallopian tube integrity and functionality, escalating the incidence from the baseline 1-2% in the general populace to substantially higher strata in predisposed cohorts.
- Tubal pathology and surgical history:
- Prior pelvic inflammatory disease (PID), engendered by ascending chlamydial or gonococcal infections, inflicts irreversible tubal scarring, amplifying risk sixfold.
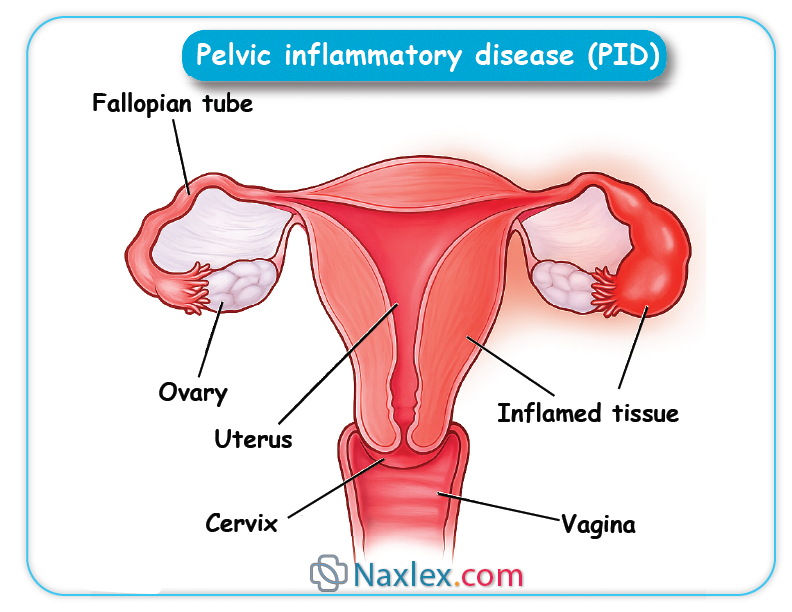
-
- Previous ectopic pregnancy confers a 10-15% recurrence risk, escalating to 25% following two incidents, attributable to persistent tubal aberrations.
- Tubal reconstructive surgery, including salpingostomy or salpingectomy, predisposes to ectopic implantation due to altered tubal architecture and ciliary impairment.
- Infectious and inflammatory contributors:
- Endometriosis induces peritubal adhesions and inflammatory milieux, hindering zygotic transit.
- History of sexually transmitted infections (STIs) correlates with tubal damage, necessitating serological screening in at-risk demographics.
- Hormonal and contraceptive influences:
- Progestin-only contraceptives, including intrauterine devices (IUDs), attenuate tubal motility, with 50% of IUD-associated pregnancies being ectopic.
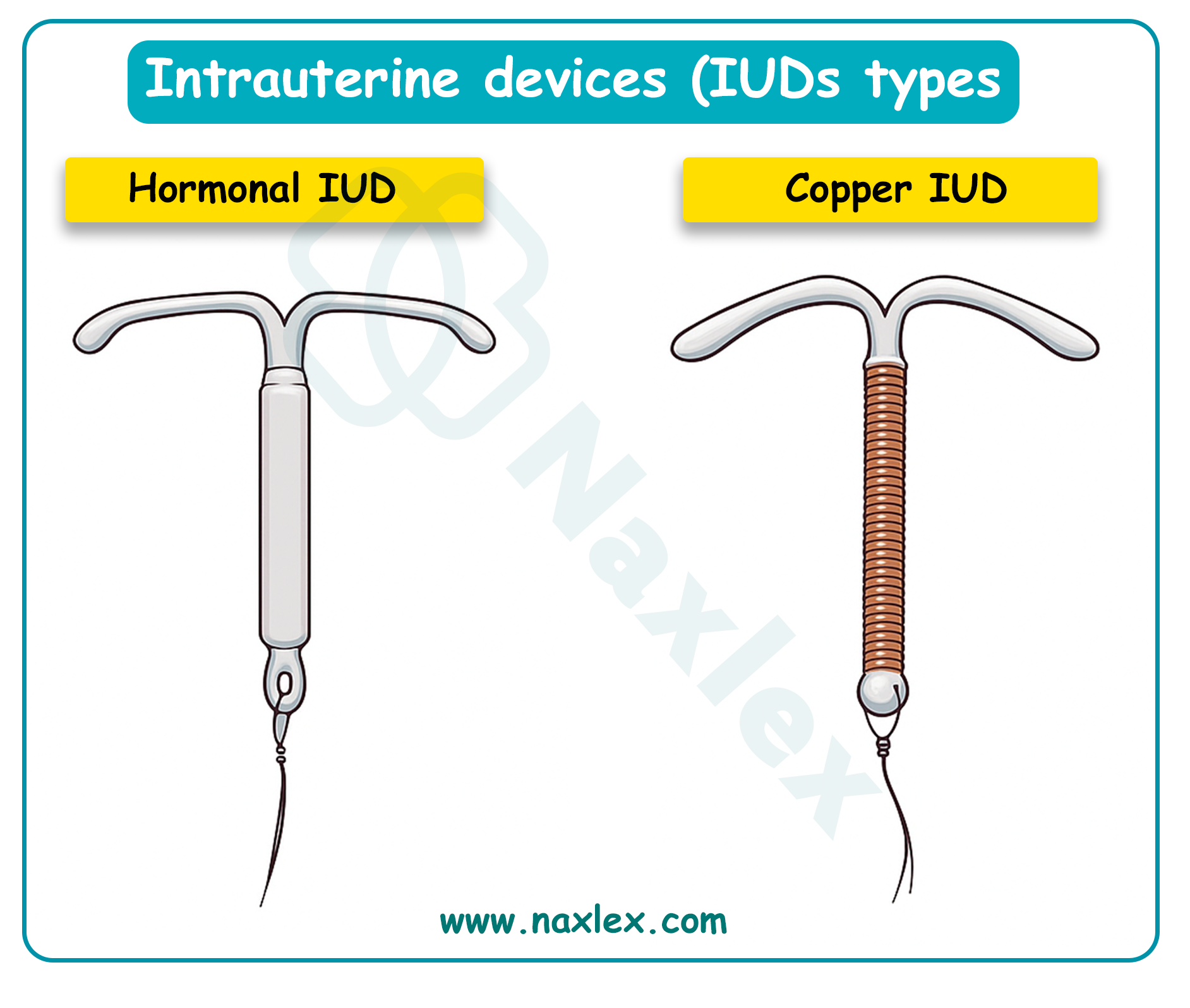
- Assisted reproductive technologies (ART), such as in vitro fertilization (IVF), heighten risk threefold owing to multiple embryo transfers and underlying infertility etiologies.
- Demographic and lifestyle factors:
- Advanced maternal age (>35 years) correlates with diminished tubal function and cumulative exposure to risk elements.
- Cigarette smoking impairs ciliary activity via nicotine-induced vasoconstriction and oxidative stress, conferring a twofold risk elevation.
- Prior abdominal surgeries, including appendectomy or cesarean sections, may engender adhesions impeding tubal patency.
- Genetic and anatomical predispositions:
- Congenital tubal anomalies, such as diverticula or elongated tubes, inherently obstruct zygotic passage.
- Diethylstilbestrol (DES) exposure in utero historically augmented tubal malformations, though contemporary incidence wanes.
Nursing Insights
- Nurses must prioritize elicitation of PID history during antepartal assessments, as it constitutes the paramount modifiable risk factor amenable to prophylactic antibiotic therapy.
- Counseling on smoking cessation is imperative, given its dose-dependent augmentation of ectopic risk, with nurses facilitating nicotine replacement referrals for gravid patients.
- In patients utilizing IUDs, nurses should advocate for prompt pregnancy testing upon missed menses to expedite ectopic detection.
- Recognition of ART-associated risks mandates nurses to coordinate multidisciplinary care with reproductive endocrinologists for high-risk surveillance.
1.3 Clinical Manifestations
Clinical manifestations of ectopic pregnancy are insidious and protean, often masquerading as normal early gestation or other gynecologic pathologies, necessitating astute nursing vigilance for timely intervention.
- Primary symptoms:
- Unilateral lower abdominal pain, emanating from tubal distension or rupture, frequently colicky or sharp, intensifying with movement or palpation.
- Vaginal bleeding or spotting, typically scant and dark, arising from endometrial decidual shedding secondary to suboptimal hCG support.
- Shoulder-tip pain (Kehr's sign), indicative of diaphragmatic irritation from hemoperitoneum, heralding tubal rupture.
- Associated systemic symptoms:
- Dizziness, syncope, or orthostatic hypotension, reflective of hypovolemic compromise from intra-abdominal hemorrhage.
- Gastrointestinal perturbations, including nausea, vomiting, or diarrhea, attributable to peritoneal irritation or hormonal fluxes.
- Urinary frequency or dysuria, ensuing from bladder compression by adnexal masses.
- Advanced presentations:
- Hemodynamic instability, encompassing tachycardia, hypotension, and pallor, signifying massive hemoperitoneum post-rupture.
- Abdominal rigidity, rebound tenderness, or guarding, denoting peritonitis from blood extravasation.
- Atypical manifestations:
- In cervical ectopics, profuse painless bleeding predominates due to vascular erosion.
- Abdominal ectopics may present with fetal movements or acute abdomen from organ compression.
Nursing Insights
- Nurses must discern unilateral abdominal pain as a cardinal ectopic harbinger, prompting immediate β-hCG quantification and ultrasonographic evaluation.
- Elicitation of shoulder-tip pain during physical assessments signifies hemoperitoneum, necessitating emergent surgical consultation.
- Monitoring for syncope in ambulatory patients underscores the need for orthostatic vital signs to unmask occult hypovolemia.
- Recognition of gastrointestinal symptoms mandates differential consideration of appendicitis or ovarian torsion in diagnostic algorithms.
1.4 Diagnostic Evaluation
Diagnostic evaluation of ectopic pregnancy integrates biochemical assays, imaging modalities, and clinical correlation to affirm extrauterine implantation and appraise stability, circumventing misdiagnosis that could precipitate morbidity.
- Biochemical markers:
- Quantitative serum β-hCG assay, wherein subnormal doubling (less than 53% increment over 48 hours) or plateauing levels intimate ectopic gestation.
- Discriminatory zone threshold (1500-2000 mIU/mL) whereby absence of intrauterine sac on transvaginal ultrasound strongly suggests ectopy.
- Serum progesterone levels below 5 ng/mL corroborate nonviability, albeit nonspecific for localization.
- Imaging techniques:
- Transvaginal ultrasonography (TVUS), the diagnostic cornerstone, visualizing adnexal masses, extrauterine gestational sacs, or yolk sacs with 84-97% sensitivity.
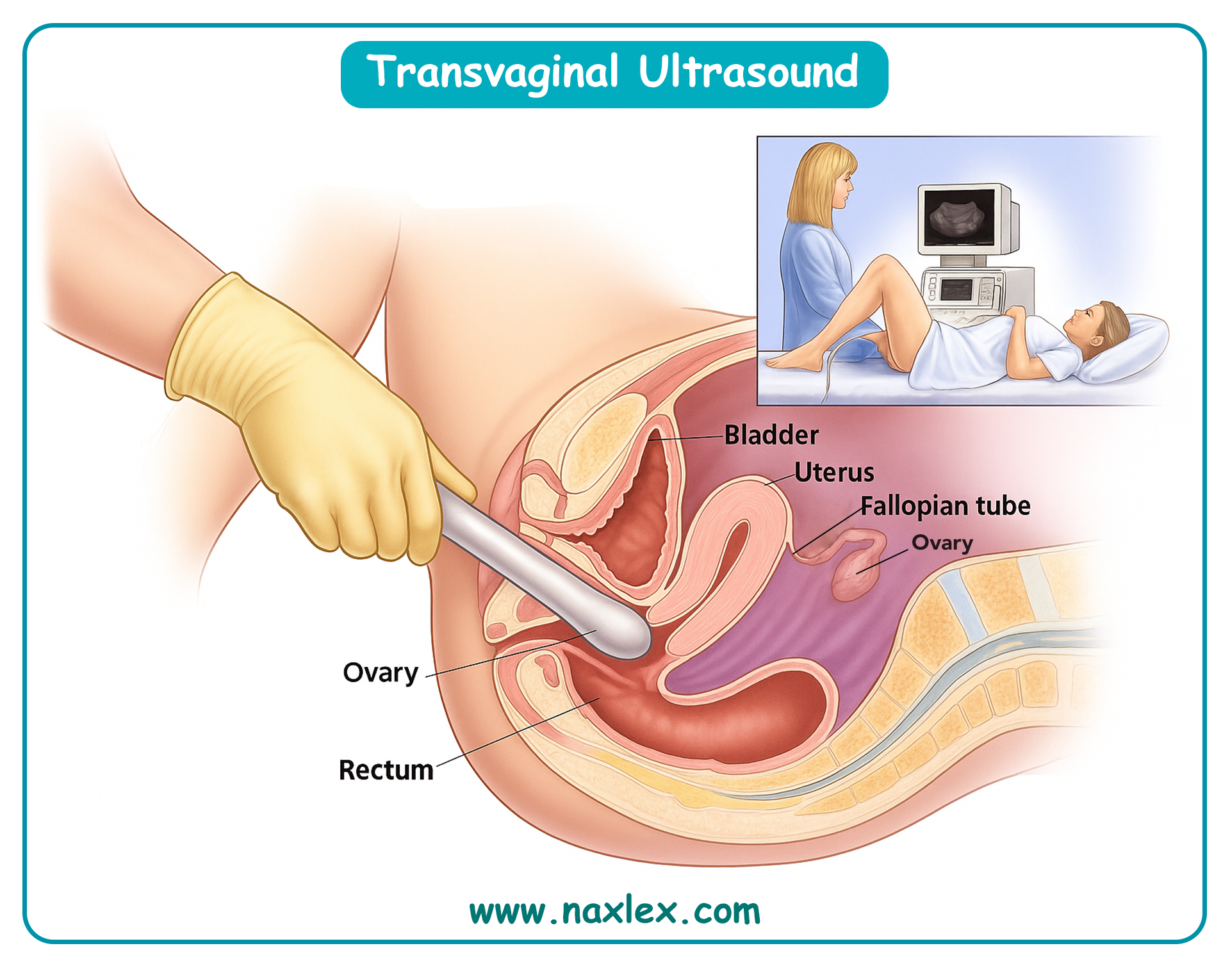
- Color Doppler enhancement delineates trophoblastic vascularity (ring-of-fire sign) in tubal ectopics.
- Transabdominal ultrasound supplements for advanced gestations or abdominal ectopics, though less resolute.
- Magnetic resonance imaging (MRI) elucidates atypical implantations, such as interstitial or cesarean scar ectopics, via T2-weighted sequences.
- Invasive diagnostics:
- Culdocentesis, aspirating nonclotting blood from the cul-de-sac, confirms hemoperitoneum in ruptured cases, albeit infrequently employed.
- Diagnostic laparoscopy affords definitive visualization and therapeutic potential in equivocal scenarios.
- Differential diagnostic considerations:
- Exclusion of intrauterine pregnancy via TVUS, with pregnancy of unknown location (PUL) warranting serial β-hCG surveillance.
Nursing Insights
- Nurses must ensure patient preparation for TVUS, including bladder emptying and consent procurement, to optimize imaging quality.
- Interpretation of β-hCG trends necessitates nurses to schedule serial draws precisely 48 hours apart for accurate viability assessment.
- Advocacy for MRI in complex cases equips nurses to coordinate with radiologists for expeditious atypical ectopic delineation.
- In PUL scenarios, nurses implement vigilant monitoring protocols, educating patients on rupture warning signs to avert delays.
1.5 Nursing and Medical Interventions
Nursing and medical interventions for ectopic pregnancy prioritize hemodynamic stabilization, pregnancy termination, and fertility preservation, tailored to patient stability and gestational locale.
- Medical management:
- Methotrexate administration (50 mg/m² intramuscularly) for unruptured ectopics with β-hCG <5000 mIU/mL, adnexal mass <3.5 cm, and absent fetal cardiac activity, inhibiting folate-dependent trophoblastic proliferation.
- Single-dose protocol entails β-hCG monitoring on days 4 and 7, with >15% decline signifying success; two-dose regimen augments efficacy for higher-risk cases.
- Contraindications encompass hemodynamic instability, renal impairment (creatinine >1.3 mg/dL), or hepatic dysfunction (AST/ALT >2x upper limit).
- Surgical interventions:
- Laparoscopic salpingostomy evacuates the ectopic while conserving the tube, ideal for fertility-desirous patients with contralateral tube compromise.
- Salpingectomy excises the affected tube, preferred in recurrent ectopics or rupture scenarios.
- Laparotomy reserved for massive hemorrhage or surgical instability.
- Nursing interventions:
- Preoperative preparation includes NPO status, intravenous access for fluid resuscitation, and RhoGAM administration (300 mcg) for Rh-negative patients within 72 hours.
- Intraoperative monitoring encompasses vital signs, blood loss quantification, and analgesia provision.
- Postoperative care involves pain management, bleeding surveillance, and infection prophylaxis with cefazolin.
- Expectant management:
- Reserved for asymptomatic patients with β-hCG <200 mIU/mL and declining trends, entailing weekly β-hCG assays until resolution.
Nursing Insights
- Nurses administer methotrexate post-counseling on side effects (stomatitis, gastrointestinal distress), ensuring follow-up β-hCG compliance to detect treatment failure.
- Preparation for salpingostomy involves educating patients on fertility implications, with nurses facilitating reproductive counseling referrals.
- Intravenous fluid bolus (crystalloids 20 mL/kg) in unstable patients stabilizes hemodynamics prior to surgical transfer.
- RhoGAM prophylaxis mandates nurses to confirm Rh status expeditiously to avert isoimmunization in subsequent pregnancies.
1.6 Complications (Rupture, Hemorrhagic Shock, Future Fertility)
Complications of ectopic pregnancy principally encompass tubal rupture, hemorrhagic shock, and impaired future fertility, mandating proactive nursing surveillance and mitigative strategies.
- Tubal rupture:
- Occurs in 15-20% of ectopics, precipitating hemoperitoneum from trophoblastic erosion of tubal vasculature, manifesting as acute abdominal agony and peritonitis.
- Risk escalates with β-hCG >5000 mIU/mL or adnexal mass >3 cm.
- Hemorrhagic shock:
- Ensues from voluminous intraperitoneal bleeding (up to 2 liters), evoking class III/IV shock with tachycardia (>120 bpm), hypotension (<90 mmHg systolic), oliguria, and altered mentation.
- Management entails massive transfusion protocol activation, with packed red blood cells, fresh frozen plasma, and platelets in 1:1:1 ratio.
- Impact on future fertility:
- Post-ectopic infertility afflicts 30-50% of patients, attributable to tubal scarring, adhesions, or contralateral tube involvement.
- Salpingectomy halves fertility rates compared to salpingostomy, though recurrence risk diminishes.
- Chronic pelvic pain or dyspareunia may ensue from pelvic adhesions.
- Other sequelae:
- Sepsis from infected hemoperitoneum or post-surgical infection, necessitating broad-spectrum antibiotics.
- Psychological ramifications, including anxiety or post-traumatic stress, warranting mental health referrals.
Nursing Insights
- Nurses monitor for rupture via serial abdominal exams, alerting for rebound tenderness indicative of peritonitis.
- In hemorrhagic shock, nurses initiate large-bore IV access and crystalloid infusion while preparing for blood product administration.
- Fertility counseling post-salpingectomy involves discussing IVF options, with nurses coordinating endocrinologist consultations.
- Surveillance for sepsis includes temperature monitoring and prompt antibiotic initiation for fever >38.3°C.
Gestational Trophoblastic Disease (Hydatidiform Mole)
Gestational trophoblastic disease (GTD) encompasses a spectrum of proliferative disorders originating from placental trophoblastic tissue, with hydatidiform mole representing the benign antecedent characterized by aberrant villous edema and trophoblastic hyperplasia. This pathological entity poses significant risks for malignant transformation and maternal complications, necessitating vigilant nursing surveillance and multidisciplinary management in maternal-newborn care. The subsequent sections delineate the definition, pathophysiology, clinical presentation, diagnostic workup, management strategies, long-term surveillance, and patient education facets of hydatidiform mole, equipping nursing students with a comprehensive, scientifically rigorous framework for clinical proficiency and patient advocacy.
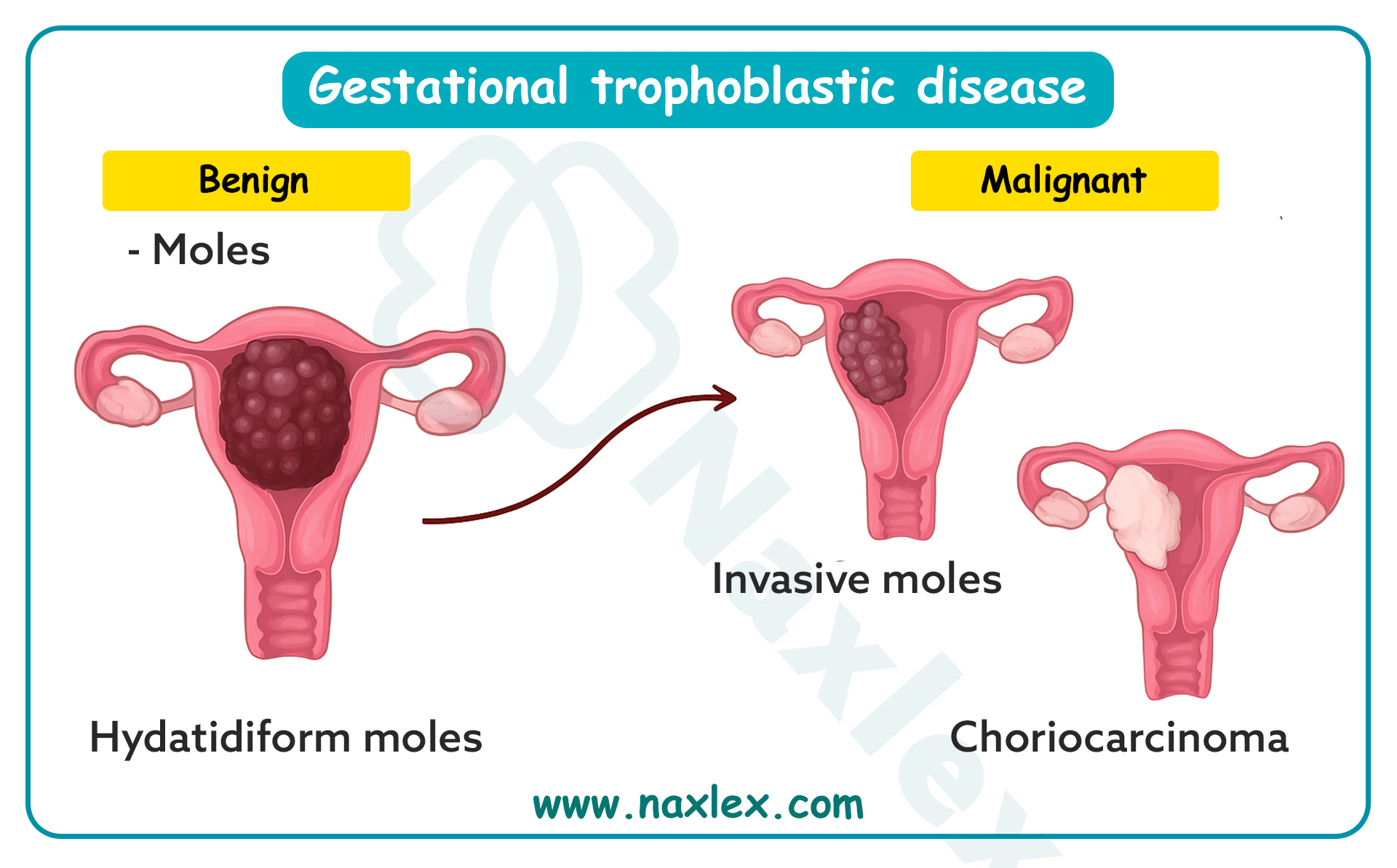
1.1 Definition and Pathophysiology
Gestational trophoblastic disease is defined as a heterogeneous group of neoplastic disorders arising from anomalous trophoblastic proliferation, with hydatidiform mole constituting a premalignant variant manifesting as cystic degeneration of chorionic villi and exuberant syncytiotrophoblastic and cytotrophoblastic hyperplasia. Complete moles exhibit diploid androgenetic karyotypes devoid of fetal tissue, whereas partial moles display triploid karyotypes with rudimentary fetal elements, both culminating in placental malformation and potential metastatic sequelae.
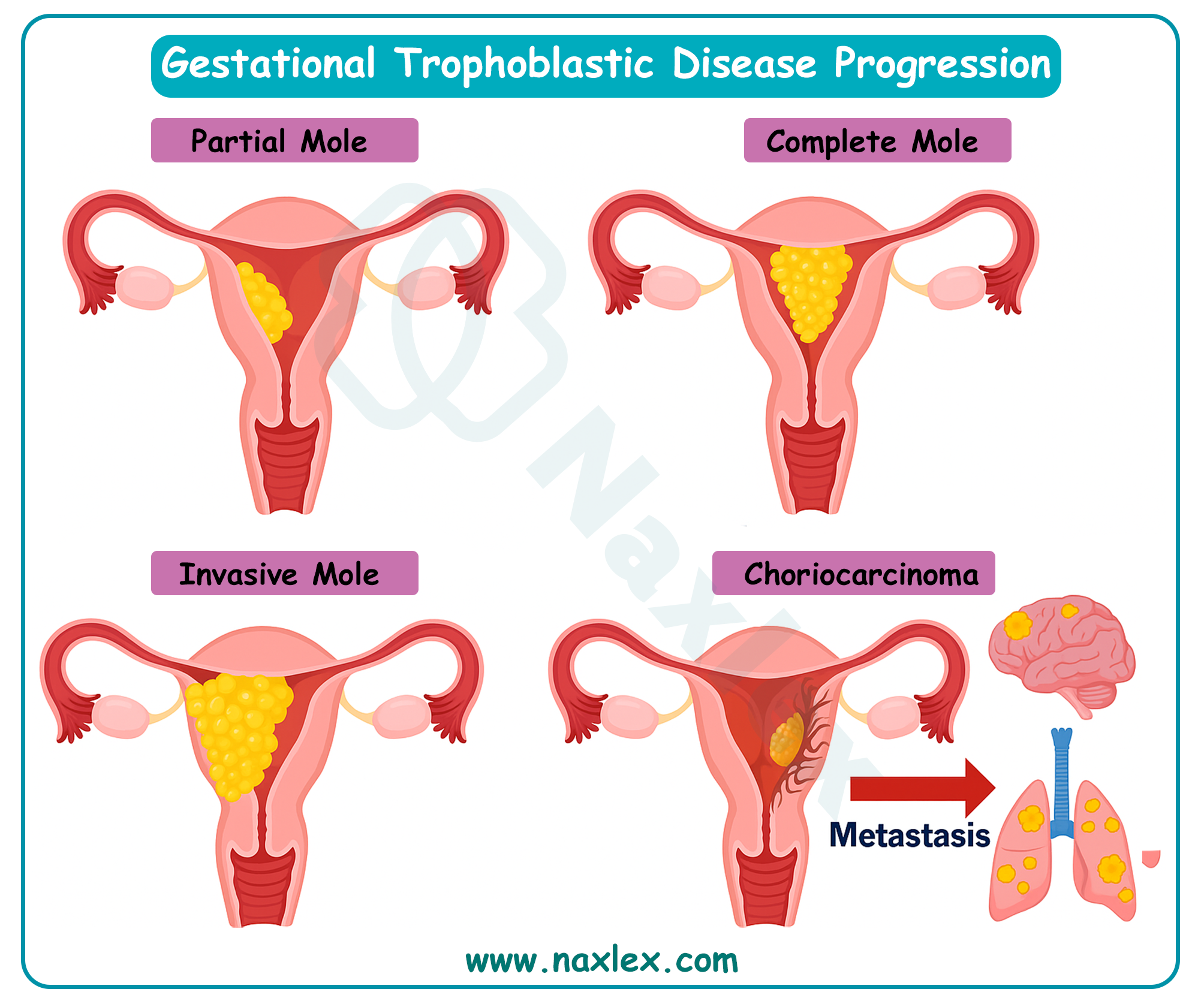
- Genetic underpinnings:
- Complete hydatidiform moles predominantly harbor a 46,XX karyotype derived from paternal duplication of a haploid sperm fertilizing an anucleate ovum, or rarely 46,XY from dispermic fertilization, resulting in absent maternal genomic contribution and universal trophoblastic hyperplasia.
- Partial hydatidiform moles arise from dispermic fertilization of a haploid ovum, yielding a 69,XXY or 69,XXX triploid karyotype, incorporating both maternal and paternal genomes, and manifesting focal villous edema with identifiable fetal structures.
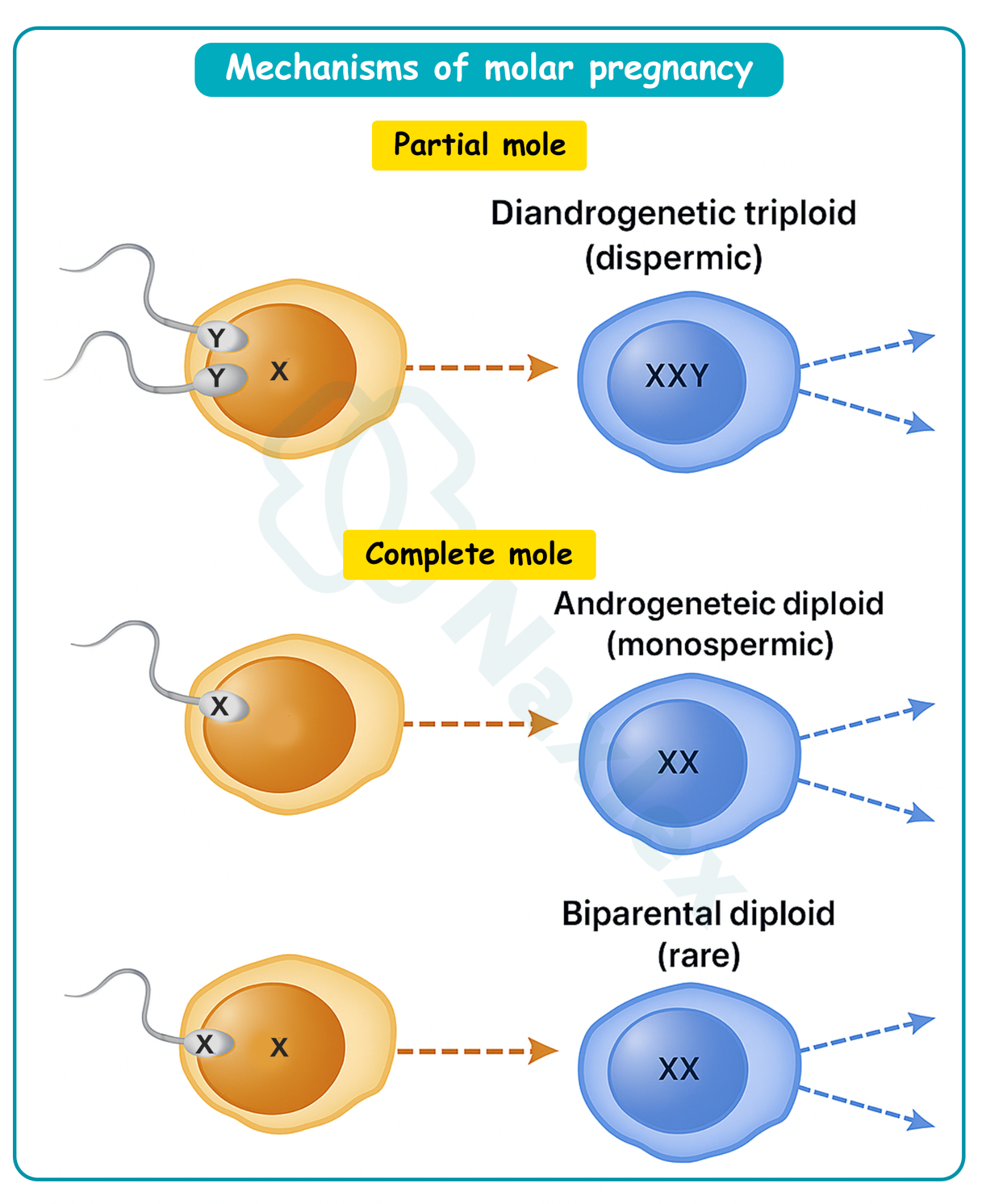
-
- Molecular aberrations, including paternal uniparental disomy or imprinting defects in genes like NLRP7 and KHDC3L, predispose to recurrent moles, particularly in familial biparental complete moles.
- Pathophysiological progression:
- Trophoblastic hyperplasia engenders excessive human chorionic gonadotropin (hCG) secretion, precipitating theca lutein cysts, hyperthyroidism, and early-onset preeclampsia via angiogenic dysregulation.
- Villous stromal edema and cistern formation disrupt placental architecture, impeding embryonic development and fostering grape-like vesicular clusters.
- Invasive potential manifests as myometrial penetration in invasive moles, or distant metastases in choriocarcinoma, driven by unchecked cytotrophoblastic invasion and vascular remodeling.
- Epidemiological correlates:
- Incidence approximates 1 in 1000 pregnancies in Western nations, escalating to 1 in 400 in Asian populations, attributable to dietary folate deficiencies or genetic predispositions.
Nursing Insights
- Nurses must distinguish complete from partial moles genetically, as complete variants harbor higher malignant transformation risks, guiding intensified surveillance protocols.
- Recognition of hCG-driven hyperthyroidism mandates thyroid function assessment in symptomatic patients to avert thyrotoxicosis complications.
- Awareness of familial recurrent moles prompts genetic counseling referrals for affected patients, facilitating preconception risk mitigation.
- Comprehension of villous edema mechanisms equips nurses to anticipate vesicular passage, preparing patients for potential expulsion events.
1.2 Clinical Presentation
Clinical presentation of hydatidiform mole typically emerges in the first trimester, characterized by exaggerated gestational symptoms secondary to supraphysiologic hCG levels and uterine distension, often mimicking normal pregnancy or miscarriage but distinguished by hallmark vesicular expulsion and multisystemic manifestations.
- Primary obstetric symptoms:
- Vaginal bleeding, ranging from spotting to profuse hemorrhage, arises from trophoblastic erosion of endometrial vessels, often accompanied by passage of grape-like hydropic villi.
- Uterine size-date discrepancy, with fundal height exceeding gestational age by 4-6 cm, attributable to molar tissue proliferation and theca lutein cyst formation.
- Absence of fetal heart tones or movements, reflecting embryonic demise or absence in complete moles.
- Endocrine and systemic manifestations:
- Severe hyperemesis gravidarum, induced by elevated hCG stimulating chemoreceptor trigger zones and gastric dysmotility.
- Hyperthyroidism, presenting with tachycardia, tremors, and heat intolerance, secondary to hCG's thyrotropin-like activity on thyroid-stimulating hormone receptors.
- Early preeclampsia before 20 weeks, manifesting as hypertension (>140/90 mmHg), proteinuria, and edema, driven by angiogenic imbalance with elevated soluble fms-like tyrosine kinase-1 (sFlt-1).
- Rare presentations:
- Respiratory distress from trophoblastic embolization or hyperthyroidism-induced high-output cardiac failure.
- Ovarian torsion secondary to enlarged theca lutein cysts (>6 cm), eliciting acute abdominal pain.
- Asymptomatic detection:
- Incidental ultrasonographic identification during routine antenatal screening, revealing characteristic snowstorm patterns.
Nursing Insights
- Nurses must quantify vaginal bleeding via pad counts to gauge hemorrhagic risk, intervening promptly for hemodynamic instability.
- Palpation for uterine size discrepancies during examinations alerts nurses to molar suspicion, prompting expeditious ultrasonographic referral.
- Assessment for hyperemesis involves electrolyte monitoring to prevent dehydration and metabolic derangements in affected patients.
- Vigilance for preeclamptic signs pre-20 weeks distinguishes moles from normal gestations, facilitating antihypertensive initiation.
1.3 Diagnostic Workup
Diagnostic workup for hydatidiform mole integrates biochemical assays, imaging modalities, and histopathological confirmation to differentiate from viable pregnancies or other gestational pathologies, ensuring accurate classification and risk stratification.
- Biochemical evaluations:
- Quantitative serum hCG exceeding 100,000 mIU/mL, disproportionately elevated for gestational age, reflecting trophoblastic hyperactivity.
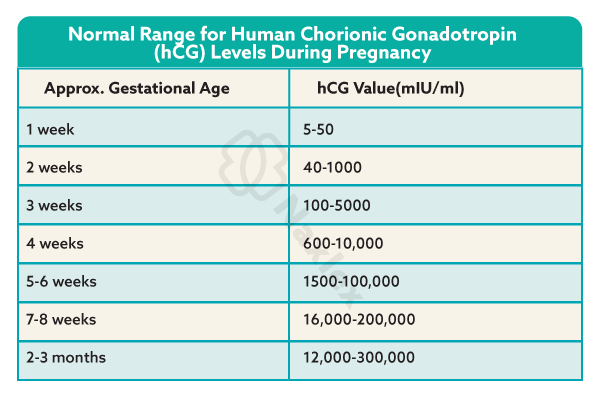
- Thyroid function tests revealing suppressed thyroid-stimulating hormone and elevated free thyroxine, corroborating hCG-induced thyrotoxicosis.
- Complete blood count and coagulation profile to assess anemia or disseminated intravascular coagulation from hemorrhagic complications.
- Imaging modalities:
- Transvaginal ultrasonography, the diagnostic mainstay, depicting a heterogeneous intrauterine mass with cystic spaces (snowstorm appearance) sans fetal structures in complete moles, or focal cystic changes with fetal remnants in partial moles.
- Doppler ultrasonography identifies absent fetal heartbeat and augmented vascularity surrounding the molar tissue.
- Chest radiography screens for pulmonary metastases in suspected invasive disease, manifesting as cannonball lesions.
- Histopathological confirmation:
- Post-evacuation tissue examination reveals edematous villi with central cisterns, trophoblastic proliferation, and karyotypic analysis (diploid vs. triploid).
- Immunohistochemical staining for p57 (absent in complete moles due to paternal imprinting) differentiates complete from partial variants.
- Differential diagnostics:
- Exclusion of multiple gestation or anembryonic pregnancy via ultrasound, with serial hCG trends distinguishing nonviable intrauterine pregnancies.
Nursing Insights
- Nurses facilitate hCG sampling, educating patients on the necessity of serial measurements to monitor disease regression post-evacuation.
- Preparation for ultrasonography involves bladder management and consent, optimizing visualization of molar characteristics.
- Coordination of histopathological submissions ensures timely karyotyping, informing malignancy risk assessments.
- Interpretation of chest radiographs in high-risk patients prompts nurses to advocate for oncologic consultations upon metastatic detection.
1.4 Management and Interventions
Management of hydatidiform mole prioritizes uterine evacuation, complication mitigation, and prevention of malignant progression, employing surgical, pharmacological, and supportive interventions tailored to molar subtype and patient stability.
- Surgical interventions:
- Suction dilation and curettage (D&C) under ultrasonographic guidance constitutes the primary evacuative modality, minimizing perforation risks and ensuring comprehensive molar tissue removal.
- Hysterectomy reserved for patients with completed childbearing or invasive disease, obviating surveillance needs but preserving ovaries.
- Pharmacological management:
- Prophylactic uterotonics (oxytocin or methylergonovine) post-evacuation to avert atony-induced hemorrhage.
- RhoGAM administration (300 mcg) for Rh-negative patients to preclude isoimmunization from fetal-maternal hemorrhage.
- Chemoprophylaxis with methotrexate in high-risk complete moles (e.g., hCG >100,000 mIU/mL) to mitigate persistent disease, though controversial due to toxicity.
- Supportive care:
- Fluid resuscitation and blood transfusion for hemorrhagic shock, guided by hemoglobin levels and vital signs.
- Antihypertensives (labetalol or hydralazine) for preeclamptic management, with magnesium sulfate for seizure prophylaxis.
- Risk-stratified approaches:
- Partial moles managed conservatively with D&C, given lower malignant potential (5%) versus complete moles (15-20%).
Nursing Insights
- Nurses administer uterotonics post-D&C, monitoring for contractile efficacy to prevent postpartum hemorrhage.
- RhoGAM dosing requires Rh status confirmation, with nurses documenting administration to safeguard future pregnancies.
- Fluid balance assessment in preeclamptic patients prevents pulmonary edema from overhydration.
- Advocacy for chemoprophylaxis in select cases involves toxicity education, ensuring informed consent.
1.5 Long-Term Follow-Up and Surveillance
Long-term follow-up and surveillance post-molar evacuation are imperative to detect persistent gestational trophoblastic neoplasia (GTN) or choriocarcinoma, employing serial hCG monitoring and contraceptive counseling to preclude confounding pregnancies.
- hCG surveillance protocols:
- Weekly quantitative hCG assays until three consecutive normal levels (<5 mIU/mL), followed by monthly assessments for 6-12 months, with plateauing or rising titers indicating GTN.
- Urinary hCG testing supplements serum assays for patient convenience in resource-limited settings.
- Imaging and laboratory follow-up:
- Baseline chest X-ray post-evacuation, with computed tomography or magnetic resonance imaging for suspected metastases (e.g., pulmonary, hepatic).
- Thyroid function normalization monitoring in hyperthyroid cases, with levothyroxine if persistent.
- Contraceptive mandates:
- Hormonal contraception (excluding IUDs initially) for 6-12 months to avert pregnancy interference with hCG surveillance.
- Malignancy risk stratification:
- High-risk features (age >40, hCG >100,000 mIU/mL, uterine size >20 weeks) warrant intensified monitoring and potential prophylactic chemotherapy.
Nursing Insights
- Nurses schedule hCG follow-ups, educating patients on compliance to detect GTN early, preventing metastatic dissemination.
- Contraceptive counseling emphasizes barrier methods initially, transitioning to hormonal agents post-normalization.
- Monitoring for metastatic symptoms (e.g., hemoptysis) prompts urgent imaging referrals.
- Documentation of surveillance adherence ensures continuity in multidisciplinary care.
1.6 Patient Education and Emotional Support
Patient education and emotional support in hydatidiform mole encompass malignancy risk elucidation, surveillance adherence, and psychosocial interventions to ameliorate grief and anxiety associated with pregnancy loss and oncologic potential.
- Educational components:
- Instruction on recognizing GTN signs (persistent bleeding, abdominal pain) and the imperative of contraceptive compliance to facilitate hCG monitoring.
- Counseling on future pregnancy deferral for 6-12 months post-normal hCG, with preconception folate supplementation to mitigate recurrence.
- Emotional support strategies:
- Validation of grief through active listening, acknowledging the dual loss of pregnancy and malignancy threat.
- Referral to support groups or psychologists for coping with anxiety, particularly in recurrent cases.
- Cultural and holistic considerations:
- Tailoring education to cultural beliefs, incorporating family involvement where appropriate.
- Provision of written resources and follow-up calls to reinforce teaching and assess emotional well-being.
Nursing Insights
- Nurses educate on GTN warning signs, empowering patients for self-monitoring and prompt reporting.
- Grief validation involves empathetic phrasing, such as "Your feelings are valid," fostering therapeutic alliances.
- Contraceptive education includes efficacy discussions, ensuring patient autonomy in method selection.
- Follow-up calls assess adherence and emotional status, facilitating timely interventions.
Nursing Management Of Pregnancy Bleeding
Nursing management of pregnancy bleeding encompasses a systematic approach to assessment, stabilization, pharmacological administration, fluid resuscitation, and psychosocial support to mitigate maternal morbidity and mortality associated with conditions such as spontaneous abortion, ectopic pregnancy, and gestational trophoblastic disease. Nurses play a pivotal role in orchestrating timely interventions, coordinating multidisciplinary care, and advocating for patient-centered outcomes in the context of early pregnancy complications. The following sections elucidate the comprehensive nursing strategies for initial assessment, emergency interventions, pharmacological management, fluid replacement, and patient education, providing a scientifically robust foundation for nursing students to excel in maternal-newborn care.
1.1 Initial Nursing Assessment of a Patient with Bleeding
Initial nursing assessment of a patient presenting with vaginal bleeding in early pregnancy is a critical step to determine the etiology, severity, and urgency of intervention, integrating subjective history, objective physical findings, and diagnostic adjuncts to formulate a differential diagnosis and guide care.
- Subjective assessment:
- Elicit a detailed obstetric history, including gestational age, last menstrual period, gravidity, parity, and prior pregnancy losses or ectopic pregnancies.
- Quantify bleeding characteristics, including onset, duration, volume (number of pads soaked per hour), color, and presence of clots or tissue passage.
- Ascertain associated symptoms, such as abdominal pain (location, quality, intensity), shoulder pain, syncope, nausea, or loss of pregnancy symptoms.
- Review risk factors, including smoking, pelvic inflammatory disease, assisted reproductive technology use, or history of uterine anomalies.
- Objective physical examination:
- Measure vital signs (pulse, blood pressure, respiratory rate, temperature) to detect tachycardia (>100 bpm), hypotension (<90/60 mmHg), or fever (>100.4°F).
- Perform abdominal palpation to assess for tenderness, guarding, rebound, or uterine size-date discrepancies suggestive of molar pregnancy.
- Conduct a speculum examination to evaluate cervical os status (open vs. closed), bleeding source (cervical vs. uterine), and presence of vesicular tissue.
- Execute a bimanual examination to assess uterine size, adnexal masses, or tenderness indicative of ectopic pregnancy.
- Diagnostic support:
- Order quantitative serum β-human chorionic gonadotropin (β-hCG) levels to evaluate pregnancy viability, with subnormal doubling (<53% over 48 hours) suggesting ectopic or nonviable gestation.
- Arrange transvaginal ultrasonography to confirm intrauterine pregnancy, identify ectopic masses, or visualize molar snowstorm patterns.
- Obtain complete blood count (CBC) to assess hemoglobin and hematocrit for anemia, and blood type with Rh factor for isoimmunization risk.
- Collect coagulation profiles (PT/INR, aPTT) to rule out disseminated intravascular coagulation in prolonged missed abortions or molar pregnancies.
Nursing Insights
- Quantification of bleeding via pad counts (e.g., soaking >2 pads/hour indicates heavy bleeding) guides urgency of escalation to obstetric providers.
- Assessment of shoulder pain during history-taking prompts immediate suspicion of hemoperitoneum from ectopic rupture, necessitating urgent ultrasound.
- Accurate documentation of cervical os status during speculum exam differentiates threatened from inevitable miscarriage, informing management.
- Obtaining obstetric history, including prior ectopic pregnancies, heightens vigilance for recurrence, prompting expedited β-hCG and imaging.
1.2 Emergency Nursing Interventions for Hemodynamic Instability
Emergency nursing interventions for hemodynamic instability in pregnancy bleeding focus on rapid stabilization, hemorrhage control, and preparation for definitive treatment to avert hypovolemic shock and maternal mortality, particularly in ectopic rupture or severe miscarriage-related hemorrhage.
- Immediate stabilization measures:
- Position the patient supine with legs elevated to enhance venous return, unless contraindicated by respiratory distress.
- Administer high-flow oxygen (10-15 L/min via non-rebreather mask) to optimize tissue perfusion in hypovolemic states.
- Establish large-bore intravenous access (16-18 gauge, two lines) for rapid fluid administration and potential blood transfusion.
- Hemorrhage control:
- Monitor bleeding via pad counts and visual estimation, reporting saturation of >2 pads/hour or passage of large clots (>5 cm).
- Administer uterotonics (e.g., oxytocin 20 units in 1 L normal saline at 125 mL/hour) as ordered to promote uterine contraction in miscarriage-related bleeding.
- Prepare for emergent surgical intervention (e.g., dilation and curettage, laparoscopy) in cases of persistent hemorrhage or ectopic rupture.
- Hemodynamic monitoring:
- Continuously monitor vital signs every 5-15 minutes, noting tachycardia (>120 bpm), hypotension (<90 mmHg systolic), or oliguria (<30 mL/hour).
- Assess for signs of shock, including pallor, cool clammy skin, altered mentation, or delayed capillary refill (>2 seconds).
- Initiate continuous pulse oximetry and electrocardiography to detect hypoxia or arrhythmias secondary to hypovolemia.
- Coordination of care:
- Alert obstetric and surgical teams for immediate consultation in cases of suspected rupture or massive hemorrhage.
- Prepare for transfer to operating room or intensive care unit if class III/IV shock (blood loss >1500 mL) is evident.
Nursing Insights
- Rapid establishment of IV access with two large-bore catheters ensures adequate fluid delivery, critical for stabilizing hypovolemic patients.
- Continuous vital sign monitoring every 5 minutes in unstable patients detects deteriorating trends, prompting immediate escalation.
- Administration of oxygen enhances oxygen delivery to tissues, mitigating hypoxic injury during hemorrhagic shock.
- Accurate communication of bleeding volume to surgical teams facilitates timely operative intervention, reducing maternal morbidity.
1.3 Pharmacological Management (e.g., Rh Immune Globulin, Misoprostol, Methotrexate)
Pharmacological management in pregnancy bleeding employs targeted medications to prevent isoimmunization, facilitate uterine evacuation, or treat ectopic pregnancies, with nursing responsibilities encompassing administration, monitoring, and patient education.
- Rh immune globulin (RhoGAM):
- Administered intramuscularly (300 mcg) within 72 hours to Rh-negative patients with bleeding to prevent alloimmunization from fetal-maternal hemorrhage.
-
- Indications include miscarriage, ectopic pregnancy, molar pregnancy, or invasive procedures (e.g., D&C).
- Dosage adjustments (e.g., microdose 50 mcg for <12 weeks gestation) depend on gestational age and bleeding volume.
- Misoprostol:
- Utilized (800 mcg vaginally, buccally, or sublingually) to induce uterine contractions in incomplete or inevitable miscarriages, promoting expulsion of retained products.
- Side effects include severe cramping, nausea, diarrhea, and fever, necessitating pre-administration antiemetics (e.g., ondansetron) and analgesics (e.g., ibuprofen 800 mg).
- Contraindications include pelvic infection or known hypersensitivity.
- Methotrexate:
- Administered intramuscularly (50 mg/m²) for unruptured ectopic pregnancies with β-hCG <5000 mIU/mL, adnexal mass <3.5 cm, and no fetal cardiac activity.
- Inhibits folate-dependent trophoblastic proliferation, requiring serial β-hCG monitoring (days 4 and 7) for >15% decline to confirm efficacy.
- Side effects include stomatitis, gastrointestinal distress, and rare hepatotoxicity, necessitating baseline liver function tests.
- Supportive medications:
- Antibiotics (e.g., doxycycline 100 mg BID for 7 days) for infection prophylaxis post-D&C or in septic abortions.
- Uterotonics (e.g., methylergonovine 0.2 mg IM every 2-4 hours) to control post-evacuation hemorrhage from uterine atony.
Nursing Insights
- Verification of Rh status prior to RhoGAM administration prevents unnecessary dosing and ensures timely prophylaxis for isoimmunization prevention.
- Patient education on misoprostol includes expected cramping and bleeding within 4-6 hours, with instructions to report excessive bleeding (>2 pads/hour).
- Monitoring methotrexate patients involves assessing for abdominal pain post-dose, indicating potential ectopic rupture, and ensuring follow-up β-hCG compliance.
- Administration of prophylactic antibiotics pre-D&C reduces endometritis risk, with nurses confirming patient allergies to avoid adverse reactions.
1.4 Fluid and Blood Replacement Therapy
Fluid and blood replacement therapy is a cornerstone of managing pregnancy bleeding with significant blood loss, aiming to restore intravascular volume, maintain tissue perfusion, and correct anemia or coagulopathy in conditions like ectopic rupture or molar hemorrhage.
- Fluid resuscitation:
- Initiate crystalloid infusion (normal saline or lactated Ringer’s) at 20 mL/kg bolus for hypotension or tachycardia, titrating to stabilize blood pressure (>90 mmHg systolic).
- Monitor fluid balance to prevent overload, assessing for pulmonary edema (crackles, dyspnea) or renal compromise (urine output <30 mL/hour).
- Use warmed fluids to prevent hypothermia in massive hemorrhage scenarios.
- Blood transfusion:
- Transfuse packed red blood cells (PRBCs) for hemoglobin <7 g/dL or symptomatic anemia (e.g., syncope, dyspnea), targeting hemoglobin >8 g/dL.
- Administer fresh frozen plasma (FFP) and platelets in a 1:1:1 ratio with PRBCs for massive transfusion protocols in class III/IV shock (>1500 mL loss).
- Crossmatch blood products, confirming compatibility and monitoring for transfusion reactions (fever, urticaria, hemolysis).
- Coagulopathy management:
- Assess for disseminated intravascular coagulation (DIC) in prolonged missed abortions or molar pregnancies, monitoring fibrinogen (<200 mg/dL), D-dimer, and platelet counts.
- Administer cryoprecipitate or fibrinogen concentrates for hypofibrinogenemia, guided by coagulation studies.
- Monitoring and evaluation:
- Perform serial CBCs to track hemoglobin trends post-transfusion, ensuring resolution of anemia.
- Evaluate hemodynamic response via vital signs and urine output, adjusting infusion rates accordingly.
Nursing Insights
- Nurses initiate crystalloid boluses promptly in hypotensive patients, monitoring urine output to confirm adequate renal perfusion.
- Crossmatching for blood products requires accurate patient identification to prevent transfusion errors, with nurses verifying labels at bedside.
- Assessment for transfusion reactions involves monitoring vital signs every 15 minutes during initial PRBC infusion, stopping transfusion for fever or chills.
- Documentation of fluid input/output and transfusion volumes ensures precise tracking, guiding multidisciplinary fluid management decisions.
1.5 Patient Education, Counseling, and Supportive Care
Patient education, counseling, and supportive care in pregnancy bleeding address physical recovery, emotional processing, and future reproductive planning, fostering informed decision-making and psychosocial resilience in patients experiencing miscarriage, ectopic pregnancy, or molar pregnancy.
- Physical recovery education:
- Instruct on expected bleeding patterns (light spotting for 1-2 weeks post-miscarriage or D&C) and warning signs (soaking >2 pads/hour, fever >100.4°F, foul discharge).
- Advise pelvic rest (no intercourse, tampons, or douching) for 2-4 weeks to prevent infection or cervical trauma.
- Recommend activity restrictions, avoiding heavy lifting (>10 lbs) for 1 week post-procedure to minimize bleeding risk.
- Emotional and psychosocial support:
- Employ active listening and validate emotions (e.g., grief, guilt, anger), acknowledging the individual nature of pregnancy loss experiences.
- Refer to grief counseling or support groups for patients exhibiting prolonged distress or signs of depression.
- Involve partners or family members, with patient consent, to enhance support networks and reduce isolation.
- Reproductive planning:
- Counsel on contraception options (e.g., hormonal pills, IUDs) to prevent unintended pregnancies, particularly in molar pregnancies requiring 6-12 months hCG surveillance.
- Discuss fertility prospects, reassuring patients that one miscarriage does not significantly increase future risk, but recurrent losses warrant specialist referral.
- Educate on preconception folate supplementation (400-800 mcg daily) to reduce recurrence in molar or spontaneous abortions.
- Follow-up care:
- Schedule follow-up visits 1-2 weeks post-event for hCG monitoring, ultrasound, or complication assessment.
- Provide written discharge instructions and 24/7 contact numbers for reporting complications like persistent bleeding or fever.
Nursing Insights
- Education on warning signs empowers patients to seek timely care for complications like infection or hemorrhage, reducing morbidity.
- Active listening during counseling builds trust, encouraging patients to express fears about future pregnancies or malignancy risks.
- Contraceptive counseling post-molar pregnancy emphasizes barrier methods initially to avoid confounding hCG results, transitioning to long-acting options.
- Scheduling follow-up hCG tests ensures compliance, with nurses reinforcing the importance of detecting persistent trophoblastic disease.
Summary
Pregnancy bleeding, encompassing implantation bleeding, spontaneous abortion, induced abortion, ectopic pregnancy, gestational trophoblastic disease (GTD), and comprehensive nursing management, represents a critical domain in maternal-newborn nursing, requiring precise assessment, timely interventions, and empathetic psychosocial support to mitigate maternal morbidity and emotional distress. Implantation bleeding, a benign process occurring 6-12 days post-conception due to blastocyst embedding, presents as light, self-limiting spotting, distinguished from pathological bleeding (e.g., miscarriage, ectopic) through clinical history, transvaginal ultrasound, and β-hCG monitoring; nurses reassure patients and educate on warning signs like heavy bleeding or pain.
Spontaneous abortion, affecting 10-20% of pregnancies before 20 weeks, arises from chromosomal abnormalities, maternal conditions (e.g., diabetes), or lifestyle factors (e.g., smoking), with classifications including threatened (light bleeding, closed cervix), inevitable (open cervix, nonviable), incomplete (partial tissue expulsion), complete (full expulsion, empty uterus), missed (fetal demise without expulsion), and recurrent (≥3 losses). Nurses assess bleeding volume, cervical status, and perform diagnostics (ultrasound, β-hCG, CBC), administering misoprostol or preparing for D&C while providing RhoGAM for Rh-negative patients and counseling for grief; complications include hemorrhage, infection, and Asherman syndrome. Induced abortion, either therapeutic (e.g., maternal health risks) or elective, employs medical methods (mifepristone/misoprostol, methotrexate) or surgical techniques (vacuum aspiration, D&C, D&E), with nurses ensuring informed consent, monitoring for complications (e.g., uterine perforation), and offering contraception counseling post-procedure.
Ectopic pregnancy, primarily tubal (97%), results from impaired zygotic transit due to pelvic inflammatory disease, prior ectopics, or smoking, manifesting as unilateral pain, scant bleeding, or shoulder pain (hemoperitoneum); diagnostics involve β-hCG (subnormal doubling), ultrasound, and laparoscopy, with methotrexate for unruptured cases and salpingostomy/salpingectomy for rupture, while nurses monitor for hemorrhagic shock and reduced fertility (30-50%). Gestational trophoblastic disease, specifically hydatidiform mole, features villous edema and trophoblastic hyperplasia (complete: diploid, no fetus; partial: triploid, fetal remnants), presenting with bleeding, vesicle passage, hyperemesis, and early preeclampsia; suction D&C is primary, with hCG surveillance for 6-12 months to detect persistent neoplasia, and nurses educate on contraception and GTN signs. Nursing management of pregnancy bleeding integrates initial assessment (history, vitals, speculum exam), emergency interventions (oxygen, IV access, uterotonics), pharmacological administration (RhoGAM within 72 hours, misoprostol, methotrexate), and fluid/blood replacement for hypovolemia, with crystalloids and transfusions guided by hemoglobin and vital signs.
Nurses educate on bleeding expectations, pelvic rest, and complication signs (fever, foul discharge), employing active listening to validate grief and referring for counseling, while ensuring follow-up for hCG monitoring and contraception planning. Practice questions across sections emphasize symptom recognition (e.g., shoulder pain for ectopic rupture), interventions (e.g., D&C for molar pregnancy), and risk factors (e.g., PID, smoking), reinforcing clinical acumen. Comprehensive questions cover miscarriage causes (chromosomal abnormalities), uterine anomalies (septate uterus, Asherman syndrome), and post-procedure care, ensuring no overlap with prior questions. This holistic framework equips nursing students to navigate the complexities of pregnancy bleeding, balancing scientific precision with compassionate care to optimize maternal outcomes and emotional resilience.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Bleeding
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


