Please set your exam date
Non-infectious Respiratory Disorders
Study Questions
Practice Exercise 1
When communicating with the grieving family after a death from sudden infant death syndrome (SIDS), the nurse should:
Explanation
Sudden infant death syndrome (SIDS) is the sudden and unexplained death of an apparently healthy infant, usually during sleep, and most often occurring between 2 and 4 months of age. The exact cause is unknown, and it can leave parents feeling shocked, guilty, and overwhelmed. The nurse’s primary role is to provide emotional support, compassion, and reassurance while helping the family begin to process their grief.
Rationale for correct answer:
2. Parents of infants who die suddenly often experience intense guilt and self-blame. The nurse’s immediate priority is to offer emotional support and reassurance that SIDS is unpredictable and not caused by anything the parents did or failed to do. This empathetic approach helps the family begin the grieving process and prevents further emotional trauma.
Rationale for incorrect answers:
1. While instructing the parents to place other infants on their backs to sleep is accurate health teaching to prevent SIDS, it is not appropriate immediately after a child’s sudden death. In the acute grieving phase, the parents need emotional support rather than educational advice.
3. Although an autopsy may be required for confirmation, emphasizing it during the parents’ initial shock may seem insensitive and is not the nurse’s role to stress. The healthcare provider or coroner usually discusses autopsy procedures.
4. Stressing that the parents are still young and can have more children is dismissive and minimizes the parents’ current loss and grief. Such statements can cause further emotional pain and should be avoided.
Take home points
- The nurse’s primary role is to provide compassionate emotional support to grieving parents.
- Avoid giving advice or future-oriented statements immediately after a death. Focus on presence and empathy.
- Reassure without blaming, acknowledge the parents’ loss and affirm that SIDS is unpredictable.
- Use active listening, touch (if appropriate), and therapeutic silence to convey support during grief.
What's the peak age for sudden infant death syndrome?
Explanation
Sudden infant death syndrome (SIDS) refers to the sudden, unexplained death of an infant under 1 year of age, typically during sleep. It is often related to a combination of developmental vulnerability, environmental stressors, and critical developmental periods in cardiorespiratory control.
Rationale for correct answer:
2. The peak age for SIDS is between 2 and 4 months of age, with the highest incidence around 3 months. This age coincides with a period of rapid development of the autonomic nervous system, making infants more vulnerable to sleep-related breathing irregularities. After 6 months, the risk of SIDS decreases significantly as the infant’s neurologic and respiratory control systems mature.
Rationale for incorrect answers:
1. SIDS is rare in the first month of life. Most deaths that occur during this period are related to perinatal or congenital conditions, not SIDS.
3. The risk of SIDS decreases significantly after 6 months and is uncommon beyond 12 months.
4. At 18 months, SIDS is extremely rare. Deaths in this age group are more likely caused by accidents, infections, or metabolic disorders, not SIDS.
Take home points
- Peak age of SIDS is 2–4 months.
- Risk declines sharply after 6 months and is rare after 1 year.
- Prevention strategies include placing the infant supine to sleep, avoiding soft bedding and overheating, and discouraging exposure to tobacco smoke.
- Breastfeeding and pacifier use during sleep are associated with a lower risk of SIDS.
Which factors are considered protective factors for sudden infant death syndrome (SIDS)?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an infant under 1 year of age, most often occurring during sleep. The exact cause is unknown, but it is believed to involve an interaction of vulnerable infants, critical developmental periods, and environmental stressors affecting breathing and arousal. Preventive education for parents and caregivers is essential to reduce modifiable risks.
Rationale for correct answer:
4. Supine sleeping position is the safest and most recommended sleeping position for infants. The “Back to Sleep” campaign significantly reduced SIDS incidence. Sleeping on the back keeps the airway open and prevents suffocation or rebreathing of exhaled carbon dioxide. Breastfeeding provides immunologic protection and enhances cardiorespiratory stability during sleep, reducing SIDS risk. Vaccinated infants have a lower incidence of SIDS, possibly due to better immune function and overall health.
Rationale for incorrect answers:
1. Side sleeping position, breastfeeding, updated childhood immunization status: Side-lying is not recommended because infants can easily roll into the prone position, increasing SIDS risk.
2. Supine sleeping position, breastfeeding, soft bedding: While the supine position and breastfeeding are protective, soft bedding increases SIDS risk due to potential suffocation and rebreathing hazards.
3. Prone sleeping position, exposure to maternal tobacco use, updated childhood immunization status: Prone sleeping and tobacco exposure are major risk factors for SIDS, not protective.
Take home points
- Protective factors: Supine sleeping, breastfeeding, up-to-date immunizations, firm mattress, room-sharing but not bed-sharing.
- Avoid risk factors: Prone or side sleeping, soft bedding, overheating, and exposure to smoke.
- Nurses should consistently reinforce safe sleep practices and the importance of breastfeeding and vaccination in reducing SIDS risk.
A community health nurse is planning a follow-up visit to a family after their firstborn child died from sudden infant death syndrome (SIDS). Which action is most important for the nurse to include in the initial visit?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an infant under 1 year of age, typically occurring during sleep and remaining unexplained after a thorough investigation. Supportive nursing care focuses on helping the family begin the grieving process and providing compassionate, nonjudgmental support.
Rationale for correct answer:
2. Allowing time for the parents to express their anger and grief is the priority during a follow-up visit is to provide emotional support and a safe environment for parents to express their feelings openly. Allowing the family to verbalize emotions facilitates the grieving process and helps the nurse assess their coping mechanisms and need for further support. The nurse should use active listening, empathy, and presence, rather than trying to give explanations or solutions during the first visit.
Rationale for incorrect answers:
1. Helping the family in making a plan for future children is premature and insensitive during the early grieving period. The family must first process their loss.
3. SIDS is not a hereditary or genetic condition. A genetic counseling referral is unnecessary unless there is suspicion of another underlying cause.
4. SIDS has no definitive cause, and providing education at this stage may lead to feelings of guilt or blame. Emotional support should take priority before any educational discussions.
Take home points
- Primary nursing goal is to provide emotional support and active listening to families after a SIDS loss.
- Avoid offering explanations or solutions too soon. Focus on presence and empathy.
- Encourage expression of emotions to help facilitate healthy grieving.
- Follow-up care should later include information on grief counseling and community support groups when the family is ready.
Which position is recommended for placing an infant to sleep?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an apparently healthy infant, typically during sleep and most often between 2 and 4 months of age. Research has shown that sleep position is one of the most significant modifiable risk factors associated with SIDS.
Rationale for correct answer:
2. The supine position is the safest and most recommended sleeping position for infants. Placing infants on their backs keeps the airway open, reduces the risk of rebreathing carbon dioxide, and lowers the likelihood of SIDS. Since the introduction of the “Back to Sleep” campaign, SIDS rates have dropped significantly worldwide.
Rationale for incorrect answers:
1. The prone position increases the risk of airway obstruction and suffocation. Infants may rebreathe exhaled carbon dioxide or become trapped in soft bedding, raising the risk of SIDS.
3. The side-lying position is not stable, and infants can easily roll onto their stomachs, which increases SIDS risk. The American Academy of Pediatrics (AAP) advises against side sleeping.
4. Elevating the head of the bed is not recommended and can cause the infant to slide into a dangerous position that may obstruct the airway. It also offers no proven benefit in preventing reflux or SIDS.
Take home points
- Always place infants on their backs to sleep for naps and nighttime.
- Use a firm sleep surface with a fitted sheet. Avoid soft bedding, pillows, or toys.
- Keep the infant’s sleep area smoke-free and cool, avoiding overheating.
- Encourage room-sharing without bed-sharing for the first 6–12 months.
Practice Exercise 2
Which of the following measures should be implemented for a child with von Willebrand disease who has a nosebleed?
Explanation
Von Willebrand disease (vWD) is a genetic bleeding disorder caused by a deficiency or dysfunction of von Willebrand factor (vWF), a protein essential for platelet adhesion and stabilization of factor VIII.
Children with vWD have an increased tendency to bleed from mucous membranes, particularly the nose (epistaxis), gums, and after injuries or surgeries.
Rationale for correct answer:
1. The first-line intervention for epistaxis in vWD is to apply firm, continuous pressure to the soft part of the nose just below the nasal bone for 10 minutes. The child should be instructed to lean forward slightly to prevent blood from flowing into the throat. This measure helps promote clot formation by allowing platelets and clotting factors to act locally.
Rationale for incorrect answers:
2. Lying supine increases the risk of swallowing blood, which may cause nausea, vomiting, or aspiration. The child should instead sit upright and lean forward.
3. Nasal packing is sometimes necessary if bleeding persists despite direct pressure, but it should be done gently and by a healthcare provider to avoid trauma and further bleeding.
4. Swallowing blood should be discouraged, as it can irritate the stomach and lead to vomiting, which can worsen bleeding.
Take home points
- For a child with von Willebrand disease and a nosebleed:
- Sit the child upright and leaning forward.
- Apply firm pressure to the soft part of the nose for at least 10 minutes.
- Avoid nasal trauma and instruct caregivers on gentle nose care.
- Seek medical attention if bleeding persists, as desmopressin (DDAVP) or factor replacement may be required.
A school-age pediatric client is brought to the emergency room experiencing significant blood loss following an episode of epistaxis. The nurse should assess the results of which priority laboratory tests? Select all that apply
Explanation
A school-age child with significant blood loss from epistaxis is at risk for hypovolemia and anemia due to acute hemorrhage. The priority for the nurse is to assess the extent of blood loss and the impact on oxygen-carrying capacity.
Rationale for correct answers:
2. Hemoglobin measures the amount of oxygen-carrying protein in red blood cells. In cases of acute or chronic bleeding, hemoglobin levels fall, reflecting the severity of blood loss. Monitoring Hgb helps guide interventions such as blood transfusion or fluid replacement.
3. Hematocrit (Hct) reflects the percentage of red blood cells in total blood volume. Decreased Hct indicates hemodilution or blood loss and helps assess the degree of anemia. It is commonly monitored alongside hemoglobin in any client with significant bleeding.
Rationale for incorrect answers:
1. Sodium is not a priority in acute blood loss. Sodium levels may change slightly due to fluid shifts but do not directly indicate the severity of hemorrhage.
4. Blood urea nitrogen (BUN) may rise if blood is swallowed and digested or if dehydration occurs, but it is not an immediate priority compared to Hgb/Hct.
5. Creatinine reflects renal function, not blood loss. It is not an urgent indicator in the initial evaluation of acute hemorrhage.
Take home points
- In acute blood loss, the priority laboratory tests are hemoglobin and hematocrit to evaluate oxygen-carrying capacity and the need for transfusion.
- Vital signs (heart rate, blood pressure, capillary refill) should also be closely monitored to assess for hypovolemic shock.
- Other labs such as electrolytes, BUN, and creatinine may be obtained later for overall assessment, but Hgb and Hct come first in determining the impact of bleeding.
Which actions should a school nurse include in the emergency treatment of a child diagnosed with von Willebrand’s disease who is experiencing epistaxis? Select all that apply
Explanation
Von Willebrand’s disease (vWD) is a genetic bleeding disorder caused by a deficiency or dysfunction of von Willebrand factor, a protein essential for platelet adhesion. Clients with vWD are prone to prolonged bleeding, including recurrent epistaxis. Emergency management focuses on stopping bleeding promptly, minimizing trauma, and administering specific treatment if available.
Rationale for correct answers:
3. Applying pressure to the child’s nose with the thumb and forefinger compresses blood vessels and helps stop bleeding. The child should sit up and lean forward slightly to prevent swallowing blood, which may cause nausea or vomiting.
4. Keeping pressure applied for at least 10 minutes provides continuous pressure is essential for clot formation. Releasing pressure too soon can disrupt clot stability and restart bleeding.
5. Applying ice or a cold cloth to the bridge of the child’s nose induces vasoconstriction, reducing blood flow and promoting hemostasis. It’s a simple, noninvasive measure that supports mechanical pressure.
6. Asking the child if he or she is carrying medication to treat the nosebleed is essential since some children with vWD carry desmopressin (DDAVP) nasal spray or clotting factor concentrate for emergency use. Prompt administration can enhance von Willebrand factor release and help control bleeding.
Rationale for incorrect answers:
1. Lying down increases the risk of swallowing blood, which can lead to nausea or vomiting. The preferred position is sitting up, leaning slightly forward.
2. Elevating the child’s feet is not appropriate. This measure is for shock management, not for controlling localized bleeding.
Take home points
- For a child with von Willebrand disease and a nosebleed:
- Sit the child upright and leaning forward.
- Apply firm pressure to the soft part of the nose for at least 10 minutes.
- Use ice or cold compresses to constrict vessels.
- Avoid nasal trauma and instruct caregivers on gentle nose care.
- If prescribed, administer desmopressin (DDAVP) as directed.
A nurse is working in a clinic and answers a telephone call from a parent who states that a 6-year-old child has a nose bleed that is not stopping. Which direction should the nurse provide to the parent?
Explanation
Epistaxis is a common condition in children, often caused by dry mucous membranes, digital trauma (nose picking), or local irritation. Most cases are anterior nosebleeds and can be controlled with simple first-aid measures at home. Proper technique is critical to stop bleeding and prevent aspiration or recurrence.
Rationale for correct answer:
2. The correct site for applying pressure is the soft part of the nose, just below the nasal bone. The child should sit upright and lean slightly forward to avoid swallowing blood. Continuous pressure for 10–15 minutes allows clot formation and effective hemostasis. This is the first-line management for most cases of anterior epistaxis.
Rationale for incorrect answers:
1. Tilting the child’s head back causes blood to flow into the throat, increasing the risk of swallowing blood, nausea, vomiting, and aspiration.
3. Taking the child to urgent care as soon as possible is not immediately necessary unless bleeding persists beyond 20 minutes, or the child has recurrent or heavy bleeding or an underlying bleeding disorder. Home management is appropriate as the first response.
4. Immediately insert a cotton ball or swab in each nare is contraindicated. Inserting objects can dislodge clots, irritate mucosa, and worsen bleeding.
Take home points
- For a child with epistaxis:
- Sit the child upright and leaning forward.
- Apply firm pressure to the soft part of the nose for at least 10 minutes without interruption.
- Use ice or cold compresses to constrict vessels.
- Avoid nasal trauma and instruct caregivers on gentle nose care.
- Seek medical care if bleeding continues >20 minutes, recurs frequently, or if the child has a bleeding disorder.
Practice Exercise 3
Children younger than age 3 are prone to aspirating foreign bodies. Which action is recommended to prevent aspiration?
Explanation
Children under 3 years old are at high risk for foreign body aspiration because their airways are small, chewing ability is immature, and they often explore objects with their mouths. Foods that are round, hard, or sticky can easily obstruct the airway.
Rationale for correct answer:
3. Whole grapes are one of the most common causes of choking and airway obstruction in toddlers. Cutting grapes into quarters (lengthwise) reduces the risk of aspiration by changing their round shape and making them easier to chew and swallow safely.
Rationale for incorrect answers:
1. Cutting hot dogs in half lengthwise still leaves pieces that can obstruct a child’s airway if round edges remain. The correct method is to cut hot dogs lengthwise and then into small pieces (quarter them), not just in half.
2. Limit popcorn and peanuts is insufficient since these foods should be completely avoided in children under 3 years old due to their high choking risk. The recommendation is avoidance, not limitation.
4. Hard candies pose a severe choking hazard and should be completely avoided, not just limited.
Take home points
- The airway diameter of a toddler is approximately the size of a small drinking straw, so even small round foods can fully block it.
- Avoid or modify high-risk foods:
- Avoid: nuts, popcorn, hard candy, whole grapes, hot dogs, raw carrots.
- Modify: cut grapes and hot dogs lengthwise and into small pieces.
- Supervise children during eating and encourage sitting upright during meals.
Which activity is recommended to prevent foreign body aspiration during meals?
Explanation
Foreign body aspiration is a leading cause of accidental injury and death in children under 3 years of age. It often occurs during eating, playing, or laughing while food or small objects are in the mouth.
Prevention centers on safe feeding practices and close supervision during meals to reduce choking risk.
Rationale for correct answer:
1.The most effective preventive measure during meals is ensuring that children sit upright while eating. Sitting reduces the likelihood of aspiration because it allows for better swallowing coordination and prevents sudden inhalation of food caused by movement, running, or playing. Children should also be taught to eat slowly, chew thoroughly, and avoid talking or laughing with food in their mouths.
Rationale for incorrect answers:
2. Allowing toys at mealtime is unsafe because they distract the child and increase the risk of placing small objects in the mouth, leading to aspiration.
3. Watching TV while eating diverts attention from proper chewing and swallowing, increasing choking risk.
4. Children should always be supervised while eating. Eating in a separate room increases the risk of delayed response if choking occurs.
Take home points
- Always supervise young children during meals.
- Ensure children sit upright and remain calm while eating.
- Avoid distractions such as toys, television, or playing.
- Educate caregivers to recognize signs of choking and provide infant/child CPR training for emergency preparedness.
The nurse is preparing a child for testing for a foreign body aspiration. The nurse explains to the child’s parents that the best diagnostic tool for diagnosis of foreign body aspiration is:
Explanation
Foreign body aspiration occurs when a solid object is inhaled into the respiratory tract, potentially causing partial or complete airway obstruction. It most commonly affects children aged 6 months to 3 years.
Diagnosis involves a combination of clinical assessment and imaging, but definitive confirmation and removal often require direct visualization of the airway.
Rationale for correct answer:
1. Bronchoscopy is the gold standard diagnostic and therapeutic tool for foreign body aspiration. It allows direct visualization of the airway to locate and remove the foreign body. Rigid bronchoscopy is typically used in children because it provides better airway control and facilitates removal under general anesthesia. It confirms diagnosis when imaging studies are inconclusive and also allows immediate intervention.
Rationale for Incorrect Answers:
2. A chest X-ray may show indirect signs such as air trapping, atelectasis, or localized hyperinflation, but many foreign bodies, especially organic materials, are radiolucent and not visible. Thus, it is helpful but not definitive.
3. Fluoroscopy may reveal dynamic airway obstruction or unilateral air trapping, but it is less specific and not routinely used due to radiation exposure and limited diagnostic yield.
4. Lateral neck X-ray may identify a radiopaque object in the upper airway or pharynx, but it cannot detect tracheal or bronchial foreign bodies effectively.
Take home points
- Bronchoscopy is the definitive diagnostic and therapeutic procedure for foreign body aspiration.
- Prompt diagnosis and removal are essential to prevent complications such as airway obstruction, pneumonia, or lung collapse.
- Nurses should prepare the child and parents for the bronchoscopy procedure, explaining that it is performed under anesthesia and is usually curative.
A toddler is being discharged after bronchoscopy for removal of a coin from his esophagus. Which statement is the most important topic of discharge teaching?
Explanation
Foreign body ingestion and aspiration are common in toddlers due to their natural curiosity and oral exploration of objects. Coins, small toys, beads, and buttons are frequent culprits. After successful removal through bronchoscopy or endoscopy, prevention of recurrence becomes the most important focus of discharge teaching.
Rationale for correct answer:
3. Toddlers are at high risk for repeat foreign body ingestion or aspiration if environmental risks are not addressed. Parents must be taught to childproof the home, ensuring small objects, coins, beads, buttons, and toy parts are kept out of reach. Prevention is critical because recurrence can lead to life-threatening airway obstruction or esophageal injury. This teaching emphasizes primary prevention, which is the nurse’s top priority at discharge.
Rationale for incorrect answers:
1. Emotional reassurance is important but not the priority discharge teaching point. The focus should be on preventing future incidents.
2. Soft foods may be recommended if the throat is sore, but this is temporary and not the most crucial teaching for long-term safety.
4. Mild throat discomfort is expected after bronchoscopy and can be managed with acetaminophen, but this is a comfort measure, not the most essential safety instruction.
Take home points
- Prevention is the priority after removal of an aspirated or ingested object.
- Educate caregivers to keep small items, coins, and toy parts out of reach of young children.
- Encourage supervision during meals and playtime to minimize choking risks.
- Teach parents to recognize signs of aspiration or airway obstruction and seek immediate care if they occur.
Practice Exercise 4
A 3-year-old child is brought to an emergency department with acute pulmonary edema. The child was seen in an emergency department 48 hours earlier for a near-drowning incident. Treatment was provided at that time, and the child was monitored and discharged home. Current chest radiography indicates diffuse bilateral infiltrates. There is no history of cardiopulmonary disease. Which pulmonary dysfunctions should a nurse think about when assessing the child?
Explanation
Acute respiratory distress syndrome (ARDS) is a life-threatening form of respiratory failure that can develop hours to days after a triggering event such as near-drowning, sepsis, aspiration, or trauma.
It results from increased permeability of the alveolar-capillary membrane, leading to non-cardiogenic pulmonary edema, hypoxemia, and diffuse bilateral infiltrates visible on chest X-ray.
Rationale for correct answer:
4. Acute respiratory distress syndrome: The child presents with bilateral infiltrates on chest X-ray and a history of near-drowning, consistent with non-cardiogenic pulmonary edema due to ARDS. ARDS typically develops 24–72 hours after the initial insult, matching this child’s presentation (symptoms appearing 48 hours later). Classic findings include severe hypoxemia, tachypnea, and respiratory distress unresponsive to oxygen therapy.
Rationale for incorrect answers:
1. Foreign body aspiration is unlikely because symptoms of airway obstruction such as sudden coughing, localized wheezing, or stridor occur immediately after aspiration. The delayed onset (48 hours later) and diffuse bilateral infiltrates do not support this diagnosis.
2. Aspiration pneumonia typically shows localized infiltrates, often in the dependent lobes of the lung, not diffuse bilateral involvement. Fever and localized crackles are usually present, which are not mentioned here.
3. Bronchopneumonia usually caused by bacterial infection, presenting with fever, cough, purulent sputum, and patchy infiltrates, not diffuse ones. The temporal relationship to the near-drowning event and lack of infection history make this less likely.
Take home points
- ARDS is a delayed complication of near-drowning due to inflammatory damage to the alveolar-capillary membrane.
- Nursing actions include:
- Support oxygenation (often requires mechanical ventilation).
- Monitor for hypoxemia, respiratory effort, and vital signs.
- Prevent complications such as infection or fluid overload.
A nurse is caring for a preterm infant with respiratory distress syndrome (RDS). To maximize the infant’s respiratory status, the nurse should intervene by:
Explanation
Respiratory distress syndrome (RDS) is a common condition in preterm infants, caused by surfactant deficiency leading to alveolar collapse, decreased lung compliance, and impaired gas exchange.
Supportive care focuses on maintaining adequate oxygenation, minimizing oxygen toxicity, and reducing respiratory effort.
Rationale for correct answer:
4. Positioning the infant in a prone position can improve oxygenation and ventilation by enhancing lung expansion, reducing chest wall pressure, and improving ventilation-perfusion matching. It helps reduce the work of breathing and may improve overall oxygen saturation in infants with RDS. This position must be used with continuous monitoring in a controlled hospital setting due to the risk of sudden infant death syndrome (SIDS) if used unsupervised.
Rationale for incorrect answers:
1. Although hypoglycemia can occur in preterm infants, monitoring blood glucose every 4 hours does not directly improve respiratory status. It’s part of general care, not a specific intervention to enhance oxygenation.
2. Inspired gases should be warmed and humidified to prevent cold stress, which increases oxygen consumption and worsens respiratory distress. Cooling gases would be harmful.
3. Daily or alternate-day weight checks help assess fluid balance but do not directly affect respiratory status. It’s a routine monitoring measure, not an intervention for respiratory improvement.
Take home points
- Prone positioning may enhance oxygenation in infants with RDS in a monitored hospital environment.
- Warmed, humidified oxygen should always be used to prevent cold stress and mucus thickening.
- Surfactant replacement therapy, positive pressure ventilation, and careful fluid management are key components of RDS management.
- Avoid prone positioning at home due to SIDS risk. It is appropriate only under intensive care supervision.
Following an unrestrained motor vehicle crash, a client presents to an emergency department with multiple injuries, including chest trauma. A physician notifies the care team that the client has progressed to acute respiratory distress syndrome (ARDS) and requests that the family be updated on the client’s condition. The nurse should plan to discuss with the family that:
Explanation
Acute respiratory distress syndrome (ARDS) is a severe, life-threatening form of respiratory failure that can develop after major trauma, sepsis, aspiration, or shock. It is characterized by widespread inflammation, increased alveolar-capillary permeability, and non-cardiogenic pulmonary edema, leading to severe hypoxemia refractory to oxygen therapy.
Rationale for correct answer:
4. The condition is highly life-threatening and that end-of-life concerns should be addressed: ARDS carries a high mortality rate (30–50%), especially when associated with trauma or sepsis. The condition often requires mechanical ventilation, intensive monitoring, and critical care support. The nurse must provide honest, compassionate communication with the family, explaining the serious, unpredictable nature of the condition. Families should be supported to understand prognosis, prepare for potential outcomes, and discuss end-of-life wishes early in the course of care if deterioration continues.
Rationale for incorrect answers:
1. The condition generally stabilizes with positive prognosis: Although some patients recover, ARDS is unpredictable and often fatal. Suggesting stabilization or a positive prognosis gives false reassurance.
2. The client can be discharged with home oxygen: ARDS is a critical illness requiring ICU management. Recovery, if achieved, is gradual and may include long-term pulmonary rehabilitation, but discharge with home oxygen is not part of the initial plan.
3. The condition is always fatal: ARDS is not always fatal, and many patients recover with aggressive treatment and ventilatory support. However, it remains life-threatening with a guarded prognosis.
Take home points
- ARDS is a critical emergency requiring intensive respiratory and hemodynamic support.
- The nurse’s role includes honest, empathetic communication with families about the serious and unpredictable prognosis.
- End-of-life discussions should be initiated early if the client’s condition worsens despite maximal therapy.
- Multidisciplinary support, including spiritual care and counseling, can help families cope during this crisis.
A nurse observes for early manifestations of acute respiratory distress syndrome (ARDS) in a client being treated for smoke inhalation. Which signs indicates the possible onset of ARDS in this client?
Explanation
Acute respiratory distress syndrome (ARDS) is a rapid-onset, life-threatening respiratory failure that develops after a direct or indirect lung injury, in this case, smoke inhalation. The injury causes increased alveolar-capillary membrane permeability, leading to non-cardiogenic pulmonary edema, alveolar collapse, and severe hypoxemia.
Rationale for correct answer:
3. Diaphoresis and low SaO₂ unresponsive to increased oxygen administration: In the early phase of ARDS, the hallmark finding is refractory hypoxemia, a low oxygen saturation (SaO₂) that does not improve even with increased oxygen therapy. Clients may exhibit dyspnea, tachypnea, diaphoresis, and restlessness due to hypoxemia. Despite supplemental oxygen, PaO₂ remains low, reflecting impaired gas exchange from alveolar damage. These signs often appear within 24–48 hours after the precipitating event (e.g., smoke inhalation, trauma, sepsis).
Rationale for incorrect answers:
1. Cough with blood-tinged sputum and respiratory alkalosis: Hemoptysis is not a typical early sign of ARDS. It suggests airway injury or infection. Early ARDS presents with tachypnea and respiratory alkalosis, but this alone is not diagnostic without refractory hypoxemia.
2. Decrease in both white and red blood cell counts: These changes are not related to ARDS. They may occur in bone marrow suppression or sepsis, but they do not indicate the onset of respiratory distress.
4. Hypertension and elevated PaO₂: These are opposite of ARDS findings. Clients typically show hypotension due to hypoxia and decreased cardiac output and decreased PaO₂, not elevated values.
Take home points
- Earliest sign of ARDS includes refractory hypoxemia, tachypnea, dyspnea, restlessness, and diaphoresis.
- Later findings include decreased lung compliance, diffuse crackles, and respiratory acidosis.
- Common triggers include smoke inhalation, sepsis, trauma, aspiration, near-drowning, and shock.
Comprehensive Questions
Following the death of an infant from sudden infant death syndrome (SIDS), which response by a nurse to the grieving parents is most appropriate?
Explanation
Sudden infant death syndrome (SIDS) is the unexplained death of an infant, typically occurring during sleep, and most often between 2 and 4 months of age. It is a devastating and unexpected loss that leaves parents with feelings of guilt, shock, and profound grief. The nurse’s role is to provide emotional support through compassionate communication, helping the parents begin to cope while avoiding statements that may sound dismissive or educational at this sensitive time.
Rationale for correct answer:
1. “You didn’t cause your infant’s death.” This statement offers reassurance and emotional support to parents who may be experiencing guilt or self-blame. It acknowledges their feelings while emphasizing that SIDS is not their fault. Such a response is therapeutic and focuses on providing comfort, which is the nurse’s priority in the immediate aftermath of a sudden loss.
Rationale for incorrect answers:
2. “An autopsy will confirm the cause of your infant’s death.” While factually correct, this statement is clinical and lacks emotional sensitivity. The grieving parents need compassion and reassurance, not procedural information, at this moment.
3. “Don’t worry, you'll have more children.” This response is dismissive of the parents’ current grief. It minimizes their loss and can be perceived as insensitive. Grieving parents need acknowledgment of their pain, not future-focused reassurance.
4. “Be sure to place your next infant on his back to sleep.” Although this is valid preventive advice, it is not appropriate immediately after the death. The family is not emotionally ready to receive educational information during acute grief.
Take home points
- In cases of sudden infant loss, the nurse’s primary focus is emotional support, not education or procedural discussion.
- Reassurance and empathy help parents begin to process their grief and reduce guilt.
- Avoid giving premature advice or future-oriented statements that can invalidate the family’s feelings.
- Therapeutic communication after a loss should center on acknowledging the parents’ emotions, providing a safe space for expression, and reassuring them that SIDS is not their fault.
Which child has an increased risk of sudden infant death syndrome (SIDS)?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an apparently healthy infant, usually occurring during sleep and most often between 2 and 4 months of age. The exact cause remains unknown, but several risk factors have been identified, including prematurity, low birth weight, prone sleeping position, maternal smoking, and overheating during sleep.
Rationale for correct answer:
1. A neonate born at 32 weeks’ gestation weighing 4 lb (1.8 kg): Premature and low–birth-weight infants are at the highest risk for SIDS due to immature respiratory and autonomic nervous system development, which can impair the infant’s ability to regulate breathing and arousal during sleep. This makes them more vulnerable to sudden, unexplained death during sleep.
Rationale for incorrect answers:
2. A 2-year-old with a broken arm: SIDS typically occurs in infants under 12 months of age. A 2-year-old child is not at risk.
3. An infant hospitalized with a temperature of 103.4° F (39.7° C): While fever indicates infection, it is not a direct risk factor for SIDS. SIDS is not caused by infections or fever but by unexplained respiratory or cardiac events during sleep.
4. A first-born child: Birth order is not associated with an increased risk of SIDS. Risk is more closely linked to factors such as prematurity, low birth weight, exposure to tobacco smoke, and unsafe sleep environments.
Take home points
- High-risk groups: Premature, low–birth-weight infants, and those exposed to cigarette smoke or unsafe sleep practices.
- Prevention strategies: Place infants on their backs to sleep, use a firm sleep surface, avoid soft bedding or overheating, and eliminate exposure to tobacco smoke.
- Nurses’ role: Provide parent education on safe sleep practices and early identification of high-risk infants.
- Age range: SIDS risk peaks between 2–4 months and declines after 12 months of age.
A 6-week-old infant is brought to the emergency department not breathing; a preliminary finding of sudden infant death syndrome (SIDS) is made to the parents. Which intervention should the nurse take initially?
Explanation
Sudden infant death syndrome (SIDS) is the unexpected and unexplained death of an apparently healthy infant, usually occurring during sleep, most often between 2 and 4 months of age. The suddenness of the loss often leaves parents in shock, disbelief, and deep grief. During this highly emotional time, the nurse’s role is to provide compassionate, supportive care that allows the family to begin to process the reality of the loss.
Rationale for correct answer:
3. The initial and most therapeutic intervention is to give the parents the opportunity to see, hold, and say goodbye to their infant in a quiet, private environment. This helps them begin the grieving process, acknowledge the reality of the loss, and can provide emotional closure. The nurse should remain present, supportive, and sensitive during this time.
Rationale for incorrect answers:
1. While spiritual support is important, it is not the first step. This should be offered after the parents have been given time to be with their infant and begin processing their grief.
2. Explaining the etiology of SIDS at this point is not appropriate because the parents are in shock and not emotionally ready to absorb details. Emotional support should take priority.
4. Collecting the infant’s belongings and giving them to the parents should occur after the parents have seen their infant. Giving belongings immediately may feel abrupt or insensitive and does not support their initial emotional needs.
Take home points
- The first nursing action after a child’s sudden death is to support the parents emotionally, not to provide explanations or logistical information.
- Allowing the parents to see and hold their infant facilitates acceptance and healing.
- Therapeutic presence through listening, silence, and empathy, is more helpful than explanations during acute grief.
- After initial emotional support, the nurse can help arrange spiritual care, answer questions, and return belongings in a sensitive, timely manner.
The family of an infant that died from sudden infant death syndrome (SIDS) asks the nurse what risk factors could have predisposed their child to SIDS. Which response would be the most accurate?
Explanation
Sudden infant death syndrome (SIDS) refers to the sudden, unexplained death of an apparently healthy infant, typically during sleep, and most commonly between 2 and 4 months of age. Although the exact cause remains unknown, several risk factors have been identified that increase the likelihood of SIDS.
Rationale for correct answer:
4. Infants with low birth weight are at greater risk for SIDS because they often have immature respiratory and autonomic control systems. This immaturity makes it harder for them to regulate breathing and respond appropriately to hypoxia or hypercapnia during sleep. Additionally, low-birth-weight infants may have weaker muscle tone, which can affect airway patency.
Rationale for incorrect answers:
1. Breastfeeding the infant reduces the risk of SIDS. It strengthens the infant’s immune system and promotes better sleep patterns. The American Academy of Pediatrics (AAP) recommends breastfeeding as a preventive measure against SIDS.
2. Post-term infants, born after 42 weeks, are not at increased risk of SIDS. The risk is higher in preterm or low-birth-weight infants.
3. Immunizations do not increase SIDS risk but instead, they have been shown to lower the risk. Vaccinated infants are generally healthier and less prone to infections that can compromise breathing during sleep.
Take home points
- Major risk factors for SIDS include, low birth weight, prematurity, prone or side sleeping, overheating, exposure to cigarette smoke, and unsafe sleep environments.
- Protective factors include, breastfeeding, up-to-date immunizations, using a firm mattress, and placing infants on their backs to sleep.
- Nurse’s role is to provide parents with accurate, evidence-based education on safe sleep practices and risk reduction while offering empathetic emotional support after a loss.
An infant is brought to the emergency department (ED) and pronounced dead with the preliminary finding of sudden infant death syndrome (SIDS). Which question to the parents is appropriate?
Explanation
Sudden infant death syndrome (SIDS) is the unexpected, unexplained death of an apparently healthy infant, typically during sleep and most often between 2 and 4 months of age. Because the cause is unknown, a careful history of events surrounding the death is essential for documentation and investigation. However, during this time, parents are in deep shock and grief, and questions must be asked with sensitivity, empathy, and compassion.
Rationale for correct answer:
4. “How did the infant look when you found him?” This is an appropriate and sensitive question that helps the nurse obtain factual, objective information about the circumstances without implying blame. It allows the parents to describe the situation in their own words, which is important for both emotional expression and accurate medical documentation. The nurse’s tone should remain gentle and nonjudgmental, focusing on supporting the parents while gathering necessary information for the medical team.
Rationale for incorrect answers:
1. “Did you hear the infant cry out?” This question may sound accusatory or imply that the parents could have prevented the death by responding sooner. It can increase feelings of guilt.
2. “Was the infant’s head buried in a blanket?” Although this might seem relevant to identifying a cause, it is inappropriately phrased and can make parents feel blamed or responsible for the death.
3. “Were any of the siblings jealous of the new baby?” This is irrelevant and inappropriate. SIDS is not related to sibling interactions, and such a question may seem insensitive and distressing during the grieving process.
Take home points
- When communicating with grieving parents, compassion, empathy, and sensitivity are essential.
- Nurses should ask open-ended, factual questions in a gentle manner to support both documentation and emotional expression.
- Avoid questions that imply blame or responsibility since SIDS is unpredictable and not caused by parental actions.
- Therapeutic presence including listening, validating feelings, and offering comfort, is often more meaningful than detailed questioning during early grief.
Which diagnostic test should be included in the care plan for children with an increased risk of sudden infant death syndrome (SIDS)?
Explanation
Sudden infant death syndrome (SIDS) is the sudden and unexplained death of an apparently healthy infant, most often occurring during sleep. Although the exact cause remains unknown, certain infants are at increased risk, including those who are premature, have low birth weight, experienced previous episodes of apnea or bradycardia, or have siblings who died of SIDS.
Rationale for correct answer:
2. Infants at high risk for SIDS may be prescribed a home apnea monitor to detect apneic or bradycardic episodes. This device sounds an alarm if the infant stops breathing for a set period or if the heart rate drops below a preset level, allowing caregivers to intervene quickly. While this does not prevent SIDS, it can help detect potentially life-threatening events in vulnerable infants and provide reassurance to families.
Rationale for incorrect answers:
1. Pulmonary function tests at regular intervals are not appropriate or feasible for infants. Pulmonary function testing requires voluntary effort and is used for older children or adults with chronic respiratory conditions.
3. Continuous pulse oximetry is not routinely used at home for SIDS risk reduction. It can lead to false alarms and unnecessary anxiety. It is typically used in clinical or hospital settings, not as a preventive measure for SIDS.
4. Chest X-ray at age 1 month provides no information related to SIDS risk and would expose the infant to unnecessary radiation. There are no imaging studies that can predict or prevent SIDS.
Take home points
- Home apnea monitoring may be used for infants at high risk for SIDS or those with documented apnea or bradycardia.
- The monitor helps detect, not prevent, apnea or bradycardia.
- Preventive strategies for all infants include, placing the infant on the back to sleep, using a firm mattress, avoiding soft bedding, keeping the sleep area smoke-free, and avoiding overheating.
- The nurse’s role includes educating parents on both safe sleep practices and appropriate use and maintenance of home monitoring equipment.
Which reaction is usually exhibited by the family of an infant who has died from sudden infant death syndrome (SIDS)?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an apparently healthy infant, usually occurring during sleep and most commonly between 2 and 4 months of age. Because the death is unexpected and unexplained, it leaves parents and families in shock, disbelief, and deep grief.
Rationale for correct answer:
1. Parents commonly experience intense guilt and self-blame following a SIDS death. They may feel they could have done something to prevent the death or believe their actions somehow caused it. These feelings are part of the normal grief response, and the nurse’s role is to provide empathetic, nonjudgmental support, helping the parents understand that SIDS is unpredictable and not their fault.
Rationale for incorrect answers:
2. Acceptance of the diagnosis does not occur immediately after such a sudden and devastating loss. Families often go through stages of shock, denial, anger, and guilt before acceptance can occur.
3. Parents are usually in acute shock immediately after the death. While they may later request the infant’s belongings for closure, this is not the typical initial reaction.
4. Although questions regarding the etiology of the diagnosis may arise later, during the initial stage of grief, families are usually too overwhelmed with shock and disbelief to seek detailed explanations. Emotional support takes precedence over education at this time.
Take home points
- Initial reactions to SIDS often include shock, denial, guilt, anger, and profound sadness.
- The nurse’s priority is to listen, comfort, and reassure the family that SIDS is not their fault.
- Avoid explanations or education until the family is emotionally ready to process information.
- Therapeutic communication, such as empathy, silence, and presence, is the most effective approach in the immediate period following loss.
The parents of an infant who just died from sudden infant death syndrome (SIDS) are angry at God and refuse to see any member of the clergy. Which nursing diagnosis is most appropriate?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an apparently healthy infant, typically occurring during sleep and most often between 2 and 4 months of age. The unexpected nature of SIDS often leads to intense emotional turmoil, including shock, denial, guilt, anger, and confusion.
Rationale for correct answer:
2. Spiritual distress occurs when an individual’s belief system, values, or relationship with a higher power is disrupted, often in response to suffering or loss. In this case, the parents’ anger toward God and refusal to engage with clergy demonstrate a crisis of faith directly linked to their grief. This diagnosis reflects a disruption in spiritual well-being, not a lack of coping skills or prolonged grief.
Rationale for incorrect answers:
1. Although grief and anger can affect coping, the key issue here is anger directed toward God, which is spiritual in nature, not primarily behavioral or emotional.
3. Complicated grieving refers to prolonged or unresolved grief that interferes with functioning over time. At this stage, the parents are experiencing acute grief, not chronic dysfunction.
4. Chronic sorrow is a long-term recurring sadness often seen in parents of children with chronic illnesses or disabilities. It does not apply to this sudden, traumatic loss.
Take home points
- Spiritual distress can manifest as anger, guilt, withdrawal, or questioning one’s faith following a profound loss.
- The nurse should respect the parents’ beliefs and coping pace, avoiding pressure to engage with clergy or religious rituals.
- Therapeutic communication, listening, presence, and empathy, is essential for supporting spiritual healing.
- Later, when the parents are ready, offering referrals to spiritual care or counseling may help them reconcile their beliefs and begin to heal emotionally and spiritually.
Which plan is most appropriate for a nurse scheduling a home visit to parents who lost an infant to sudden infant death syndrome (SIDS)?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an apparently healthy infant, most often occurring during sleep. The event is profoundly traumatic for families, often leading to shock, denial, guilt, anger, and deep grief.
Rationale for correct answer:
3. As soon after death as possible: A prompt home visit following the infant’s death allows the nurse to provide timely emotional support, assess the family’s grief reactions and coping mechanisms, and identify needs for ongoing counseling or community support. Early contact demonstrates caring, helps prevent feelings of abandonment, and allows the nurse to offer resources such as grief support groups or referrals for professional counseling.
Rationale for incorrect answers:
1. One visit in 2 weeks: Waiting this long delays emotional support during a time when the parents are most vulnerable. Immediate intervention helps stabilize emotional well-being and builds trust.
2. No visit is necessary: This response is inappropriate and neglectful. Families who lose a child to SIDS often need ongoing emotional and psychological support. Avoiding contact can worsen feelings of guilt and isolation.
4. One visit with parents only, no siblings: Siblings should be included, as they also grieve and may have misconceptions or guilt about the death. Excluding them can lead to unresolved emotional issues.
Take home points
- A home visit should occur as soon as possible after the loss to provide emotional support and assess family needs.
- Include all family members in follow-up care. Siblings often require reassurance and help expressing grief.
- The nurse’s role is to listen empathetically, acknowledge the family’s loss, and reaffirm that SIDS is not their fault.
- Early, compassionate follow-up fosters healing, reduces guilt, and connects families with long-term grief and community support resources.
A child is admitted with a possible tracheal foreign body. Which findings would most likely indicate a foreign body in the trachea?
Explanation
Foreign body aspiration in children occurs when an object is accidentally inhaled into the airway or lungs, leading to partial or complete obstruction of the respiratory tract. This is a potentially life-threatening emergency, especially common in children under age four due to their tendency to explore the world by putting objects in their mouths.
Rationale for correct answer:
3. Expiratory wheeze and inspiratory stridor: These findings indicate airflow limitation both above and below the obstruction, characteristic of a tracheal foreign body. Inspiratory stridor results from turbulent airflow through a narrowed upper airway. Expiratory wheeze occurs as air is forced past the obstruction during expiration.
Rationale for incorrect answers:
1. Cough, dyspnea, and drooling: These are more typical of oropharyngeal or esophageal obstruction, not tracheal. Drooling occurs when swallowing is impaired, suggesting the object is not in the airway.
2. Cough, stridor, and changes in phonation: These findings are more consistent with laryngeal obstruction, where the vocal cords or glottis are affected. Changes in voice or hoarseness occur when the larynx is involved, not the trachea.
4. Cough, asymmetrical breath sounds, and wheeze: This pattern suggests a bronchial foreign body, where one lung receives less airflow, causing unequal breath sounds and localized wheezing.
Take home points
- Tracheal foreign body results in inspiratory stridor and expiratory wheeze (biphasic sounds).
- Laryngeal foreign body results in stridor, hoarseness, voice changes.
- Bronchial foreign body causes unilateral wheezing, decreased breath sounds on affected side.
- Always assess for sudden onset of respiratory distress with a history of choking.
Which activity should be recommended for long-term support of parents with an infant who has died of sudden infant death syndrome (SIDS)?
Explanation
Sudden infant death syndrome (SIDS) is the sudden and unexplained death of an infant younger than one year, typically occurring during sleep. The loss is devastating and often leaves parents experiencing intense grief, guilt, and feelings of isolation because the death is unexpected and without a clear cause. Long-term emotional recovery requires structured and continuous support.
Rationale for correct answer:
1. Support groups specifically for parents who have lost infants to SIDS provide a safe, understanding environment where individuals can share their experiences, express emotions freely, and connect with others who have endured similar losses. These groups help normalize the grieving process, reduce isolation, and promote healthy coping mechanisms.
Rationale for incorrect answers:
2. While faith and spirituality may comfort some parents, not all grieving parents find solace through religious practices, especially if they are experiencing anger toward God or loss of faith following the death. It should not be the only recommended long-term strategy.
3. Counseling is beneficial in the short-term for grief and trauma, but ongoing peer support groups often provide longer-term emotional reinforcement. Counseling may complement, but not replace, group support.
4. Family and friends can offer love and comfort, but they may struggle to understand the unique pain associated with SIDS loss. Parents may feel misunderstood or judged, making professional or peer-based support groups more effective for sustained healing.
Take home points
- SIDS is a sudden, traumatic event that requires sensitive, continuous emotional support for the family.
- Nurses should encourage participation in SIDS-specific support groups for both parents and siblings.
- Grief from SIDS often resurfaces during anniversaries and developmental milestones; long-term support is crucial.
- Collaboration with community resources and SIDS foundations can help families feel less isolated and more empowered to cope.
The parent of a 9-month-old calls the ED because his child is choking on a marble. The parent asks how to help his child while awaiting Emergency Medical Services. Which is the nurse’s best response?
Explanation
Airway obstruction in infants commonly occurs due to foreign body aspiration, such as small toys, food pieces, or marbles. Because infants have small, narrow airways, even minor obstructions can rapidly become life-threatening. Immediate first aid by caregivers can save the child’s life while awaiting emergency medical help.
Rationale for correct answer:
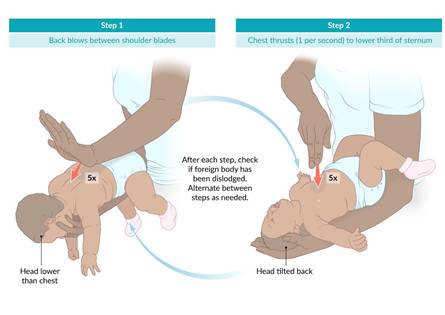
4. “You should administer five back blows followed by five chest thrusts.” For infants under 1 year, the recommended choking management sequence is five firm back blows between the shoulder blades with the heel of the hand then five chest thrusts using two fingers on the lower half of the sternum. Alternate back blows and chest thrusts until the object is expelled or the infant becomes unresponsive. This method generates enough pressure to dislodge the object without causing internal injury, unlike abdominal thrusts, which are unsafe for infants.
Rationale for incorrect answers:
1. “You should administer five abdominal thrusts followed by five back blows.” Abdominal thrusts (Heimlich maneuver) are contraindicated in infants under 1 year because they can injure the liver and other abdominal organs.
2. “You should try to retrieve the object by inserting your finger in your child’s mouth.” Blind finger sweeps should never be performed, since they can push the object deeper, worsening obstruction or causing airway trauma.
3. “You should perform the Heimlich maneuver.” The Heimlich maneuver is appropriate only for children older than 1 year and adults, not infants.
Take home points
- For infants under 1 year: alternate five back blows and five chest thrusts for choking.
- For children over 1 year and adults: use abdominal thrusts (Heimlich maneuver).
- Never perform blind finger sweeps. Only remove the object if it is visible and easy to grasp.
- Immediate intervention and calling emergency services are critical to prevent hypoxia and cardiac arrest.
Which information will be most helpful in teaching parents about the primary prevention of foreign body aspiration?
Explanation
Foreign body aspiration is a leading cause of preventable injury and death in children under 3 years of age. It occurs when solid or semi-solid objects are inhaled into the respiratory tract, causing partial or complete airway obstruction.
Rationale for correct answer:
3. Teaching parents about the specific objects most commonly aspirated helps them prevent exposure and reduce the risk of choking incidents. Examples include foods such as nuts, popcorn, grapes, raw carrots, hot dogs, hard candy and non-food items such as coins, beads, buttons, small toy parts, marbles, pen caps. Understanding these common items empowers caregivers to childproof the environment and supervise toddlers closely during meals and playtime which are the foundation of primary prevention.
Rationale for incorrect answers:
1. Recognizing symptoms such as coughing, choking, wheezing, or stridor is secondary prevention, aimed at early detection, not preventing the event itself.
2. Therapeutic management of foreign body aspiration refers to intervention after aspiration has occurred such as bronchoscopy, which is tertiary prevention, not primary.
4. While risks associated with foreign body aspiration are important for awareness, simply discussing risks such as airway obstruction, hypoxia does not provide actionable strategies to prevent aspiration events.
Take home points
- Primary prevention focuses on removing hazards before an event occurs.
- Common aspirated items are small, round, hard, or smooth objects.
- Caregiver education should include:
- Avoiding high-risk foods and toys.
- Supervising toddlers during eating and play.
- Keeping small objects out of reach.
Which is the most appropriate treatment for epistaxis?
Explanation
Epistaxis is a frequent occurrence in children, usually due to trauma, dry air, allergies, or upper respiratory infections. Most cases are anterior bleeds from Kiesselbach’s plexus and can be effectively managed with simple pressure techniques. The goal is to control bleeding, prevent aspiration, and avoid recurrence.
Rationale for correct answer:
4. With the child sitting up and leaning forward, pinch the lower third of the nose closed: The correct position for controlling epistaxis is sitting upright and leaning slightly forward, which helps reduce venous pressure in the nasal vessels and prevents swallowing blood. Pinching the lower third of the nose (the soft part below the nasal bone) applies direct pressure to the bleeding site, helping promote clot formation. This position ensures effective bleeding control and reduces the risk of aspiration or vomiting.
Rationale for incorrect answers:
1. With the child lying down and breathing through the mouth, apply pressure to the bridge of the nose: Lying down increases blood flow to the nasal vessels and may cause blood to pool in the throat, leading to nausea or aspiration. Pressure to the bridge does not effectively compress the bleeding vessels in the anterior septum.
2. With the child lying down and breathing through the mouth, pinch the lower third of the nose closed: Although pressure is applied correctly, lying down is contraindicated because it increases the risk of aspiration and difficulty managing secretions.
3. With the child sitting up and leaning forward, apply pressure to the bridge of the nose: Sitting up and leaning forward is correct, but pressure must be applied to the soft part of the nose, not the bony bridge, which does not stop anterior bleeding.
Take home points
- For a child with epistaxis:
- Sit the child upright and leaning forward.
- Apply firm pressure to the soft part of the nose for at least 10 minutes without interruption.
- Use ice or cold compresses to constrict vessels.
- Avoid nasal trauma and instruct caregivers on gentle nose care.
- Seek medical care if bleeding continues >20 minutes, recurs frequently, or if the child has a bleeding disorder.
A child is presenting with burn injuries. What should be the nurse’s priority during the initial assessment?
Explanation
In pediatric clients with burn injuries, airway compromise is the greatest immediate threat to life, especially if the burns involve the face, neck, or chest. Thermal injury or inhalation of smoke and toxic gases can lead to airway edema, obstruction, and respiratory failure, often progressing rapidly.
Therefore, the initial assessment priority follows the ABCs (Airway, Breathing, Circulation) principle of emergency care.
Rationale for correct answer:
3. Burns to the face, mouth, or neck may indicate inhalation injury, leading to upper airway edema and potential airway obstruction. Early signs include singed nasal hairs or eyebrows, soot in the mouth or nostrils, hoarseness or stridor, coughing up carbonaceous sputum, and difficulty breathing. Airway compromise can occur suddenly, even when the client initially appears stable. Immediate airway assessment and possible intubation are critical.
Rationale for incorrect answers:
1. Inspecting location, extent, and shape of burn injuries using tools like the Lund-Browder chart) is important but not the first priority. It is performed after airway and breathing are stabilized.
2. Assessing the child’s and family’s concerns regarding the child’s appearance is appropriate after life-threatening issues have been managed. Psychosocial support comes later in the care process.
4. Assessing for signs and symptoms of infection is not an immediate priority during initial assessment since infection is a later complication. Airway and circulation must be secured before evaluating for infection risk.
Take home points
- Always apply the ABCs of emergency care for burn victims:
- A – Airway: Assess for smoke inhalation or obstruction.
- B – Breathing: Evaluate for adequate ventilation.
- C – Circulation: Assess for shock and fluid loss.
- Facial burns or singed nasal hairs are red flags for airway injury.
- Immediate airway management (intubation if needed) takes precedence over burn extent or infection risk.
Exams on Non-infectious Respiratory Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Sudden Infant Death Syndrome
- Practice Exercise 1
- Epistaxis
- Practice Exercise 2
- Foreign Body Aspiration
- Practice Exercise 3
- Pulmonary Edema
- Acute Respiratory Distress Syndrome
- Smoke Inhalation Injury
- Environmental Tobacco Exposure
- Practice Exercise 4
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the incidence, pathophysiology, etiology, risk factors, protective factors, diagnostic evaluation, and prevention of sudden infant death syndrome (SIDS).
- Describe the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluation, therapeutic management, and complications of epistaxis.
- Outline the incidence, pathophysiology, commonly ingested/aspirated items, clinical manifestations, diagnostic evaluation, complications, therapeutic management, and prevention of foreign Body Aspiration (FBA).
- Describe the pathophysiology, etiology, clinical manifestations, diagnostic evaluation, and therapeutic management of pulmonary Edema.
- Define and describe the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluation, therapeutic management, and complications of acute Respiratory Distress Syndrome (ARDS).
- Describe the incidence, pathophysiology, clinical manifestations, diagnostic evaluation, therapeutic management of smoke Inhalation Injury.
- Define and describe the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluation, therapeutic management, and complications of Environmental Tobacco Exposure (ETE).
Introduction
- The respiratory system in children presents unique anatomical and physiological differences compared to adults, making them particularly vulnerable to respiratory compromise.
- Pediatric airways are smaller and narrower, increasing the risk of obstruction from edema, mucus, or foreign objects. Infants are obligate nose breathers for the first few months, and their small nasal passages easily become occluded.
- Furthermore, children have a more compliant chest wall (cartilaginous ribs), which offers less support and leads to significant retractions during respiratory distress.
- They also have fewer and less functional alveoli at birth, and the diaphragm, their primary respiratory muscle, fatigues more easily.
- Non-infectious respiratory disorders are conditions not directly caused by a viral, bacterial, or fungal pathogen, but rather by internal factors (e.g., developmental/neurological issues, trauma, underlying chronic disease) or external environmental exposures.
- A foundational understanding of these pediatric differences and the specific non-infectious pathologies is crucial for the student nurse to provide safe, effective, and evidence-based care.
Sudden Infant Death Syndrome
- SIDS is defined as the sudden, unexplained death of an infant younger than 1 year of age, which remains unexplained after a thorough case investigation, including a complete autopsy, examination of the death scene, and review of the clinical history. It is often referred to as "crib death."
Incidence
SIDS is the leading cause of death in infants between 1 month and 1 year of age, with the highest incidence occurring between 2 and 4 months of age. Incidence has significantly declined since the launch of the "Back to Sleep" (now "Safe to Sleep") campaign.
Pathophysiology
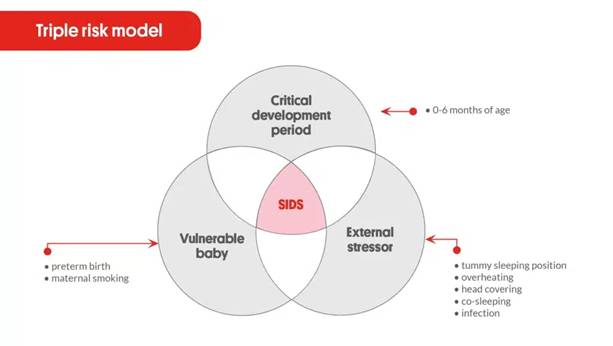
The widely accepted theory is the Triple-Risk Model. SIDS occurs when three overlapping factors coincide:
- Vulnerable Infant: An intrinsic vulnerability, often an underlying brainstem abnormality in areas that control breathing, heart rate, and arousal (e.g., defects in serotonergic signaling in the arcuate nucleus). This impairs the infant's ability to arouse or respond to challenges like rebreathing carbon dioxide during sleep.
- Critical Developmental Period: The infant is in a specific period of rapid physiological change, typically between 2 and 4 months of age.
- Exogenous Stressor (Trigger): An external factor such as a prone (stomach) or side sleeping position, co-sleeping, or soft bedding that causes mild asphyxia or thermal stress.
Etiology
The exact cause is unknown. It is believed to be multifactorial, involving a combination of genetic, environmental, and developmental factors.
Risk Factors
|
Category |
Risk Factors |
|
Sleep Environment |
Prone or side sleeping position (greatest risk factor)
Soft bedding (pillows, quilts, sheepskins), Overheating (excessive clothes, blankets), Bed sharing (Co-sleeping), Pacifier not used during sleep. |
|
Infant Characteristics |
Age 2–4 months, Prematurity/Low birth weight, Males, Race (Higher in African American and Native American infants). |
|
Maternal/Pregnancy |
Maternal smoking (prenatal and postnatal), Maternal substance abuse (alcohol, drugs), Inadequate prenatal care, Young maternal age. |
Protective Factors
- Supine sleeping position (Back to Sleep).
- Firm sleep surface (crib mattress covered with a fitted sheet).
- Room-sharing without bed-sharing (infant sleeps in a crib or bassinet in the parents’ room).
- Breastfeeding.
- Offer a pacifier at nap and bedtime (do not reinsert if it falls out).
- Complete routine immunizations.
- Avoid overheating.
Diagnostic Evaluation
SIDS is a diagnosis of exclusion:
- Complete Autopsy: Essential to rule out infectious, metabolic, or congenital causes of death.
- Death Scene Investigation (DSI): Detailed review of the sleep environment, position, and circumstances.
- Review of Clinical History: Comprehensive history of the infant's health and family background.
Management
There is no treatment for SIDS. Management focuses entirely on prevention through risk reduction and providing support to the family after the event.
Nursing Diagnosis
- Readiness for Enhanced Knowledge regarding SIDS prevention.
- Dysfunctional Grieving related to sudden, unexpected loss of an infant.
- Interrupted Family Processes related to a sudden death crisis.
Nursing Education (SIDS Prevention)
- Educate all caregivers on the "Safe to Sleep" recommendations:
- "Back is Best": Always place the infant on their back for every sleep, nap, or night.
- Use a firm, flat sleep surface.
- Keep the crib bare: no blankets, pillows, bumper pads, or stuffed toys.
- Room-share, but do not bed-share.
- Avoid overheating (dress the infant in no more than one layer more than an adult would wear).
- Avoid exposure to smoke (prenatal and postnatal).
Nursing Insight: Home Apnea Monitor- The American Academy of Pediatrics does not recommend the use of home cardiorespiratory monitors, commercial devices, or positioning wedges as a SIDS prevention strategy. They are only recommended for infants with extreme prematurity, symptomatic apnea, or other specific diagnoses, not for preventing SIDS in healthy infants. Educate parents that these monitors have not been shown to decrease the incidence of SIDS.
Therapeutic Communication to Parents and Caring for the Family After SIDS
- Acknowledge the Loss: Use the infant's name and acknowledge the depth of their tragedy ("I am so sorry for the loss of your baby").
- Avoid Judgment: Maintain a non-judgmental and compassionate demeanor. SIDS is a sudden, unexplained death; parents often struggle with overwhelming guilt.
- Address Guilt: Gently assure the parents that SIDS is a medical phenomenon and is not their fault, despite the safe sleep education.
- Support the Investigation: Explain the need for the autopsy and death scene investigation as a standard, mandatory procedure to rule out other causes, which can alleviate their fear of being accused.
- Grief Support:
- Provide information on local and national SIDS support groups (e.g., SUDC Foundation, First Candle).
- Ensure both parents and siblings receive counseling. Anticipatory guidance about the grief process is essential.
- Offer the option to spend time with the infant to say goodbye, if culturally and personally appropriate.
Epistaxis
- Epistaxis is a hemorrhage from the nose, usually self-limiting. The majority of pediatric nosebleeds are anterior, originating from Kiesselbach's plexus (Little's area) on the anterior nasal septum, a highly vascular area.
Incidence
Extremely common in childhood, with peak incidence between 3 to 8 years of age.
Pathophysiology
The mucous membranes of the nasal septum are rich in superficial, delicate blood vessels. Trauma, drying, or irritation to this area causes the vessels to rupture.
Etiology
- Nose Picking is the most common cause in children.
- Dry mucous membranes due to low humidity, especially in winter.
- Allergic rhinitis/URI which causes congestion and rubbing/blowing the nose.
- Foreign bodies in the nose.
- Trauma from falls or sports injuries.
- Underlying conditions though rare, such as vascular abnormalities, coagulopathies (e.g., hemophilia, von willebrand), or medications (e.g., NSAIDs).
Clinical Manifestations
- Bleeding from one or both nostrils.
- Anxiety and fear in the child and parent.
- Posterior bleeds (rare) may present with bleeding in the back of the throat/swallowing of blood, which can cause vomiting.
Diagnostic Evaluation
Diagnosis is typically based on the history and physical exam.
- History: Determine the frequency, duration, amount of blood loss, unilateral/bilateral nature, and any predisposing factors (picking, trauma, medications).
- Visual Inspection: Anterior rhinoscopy to identify the source of bleeding (usually a small vessel in Kiesselbach's plexus).
- Labs (if recurrent/severe): Complete Blood Count (CBC) and Coagulation studies (PT/PTT) to rule out underlying bleeding disorders.
Therapeutic Management
Emergency Treatment
- Proper Positioning: Have the child sit up and lean slightly forward. This prevents blood from running down the throat and being swallowed, which can cause nausea and vomiting.
- Direct Pressure: Pinch the soft part of the nose (nostrils/alae) together against the septum using the thumb and forefinger for a full 10 to 15 minutes without stopping to check for bleeding.
- Adjunctive Measures:
- Apply a cool cloth or ice pack to the bridge of the nose or the back of the neck to promote vasoconstriction (vasoconstriction is what stops the bleeding).
- Maintain a calm, reassuring manner to reduce the child’s anxiety.
DO'S and DON'TS
|
DO'S |
DON'TS |
|
Do remain calm and reassure the child. |
Don’t have the child lie down or tilt their head back (increases swallowing/vomiting risk). |
|
Do apply firm pressure for a full 10–15 minutes. |
Don’t plug the nose with tissue or cotton. |
|
Don’t have the child breathe through their mouth. |
Don’t let the child vigorously blow or pick their nose for several hours after bleeding stops. |
|
Don’t seek medical attention if bleeding persists beyond 20 minutes. |
Don’t use excessive force when applying pressure. |
Medical Interventions (if bleeding persists)
- Chemical Cautery: Using a silver nitrate stick to chemically coagulate the bleeding site.
- Nasal Packing: Insertion of an absorbable product, gauze, or a nasal balloon into the anterior nasal cavity.
- Topical Vasoconstrictors: Application of gauze soaked in a vasoconstrictive agent (e.g., epinephrine).
Epistaxis Management
Complications
- Aspiration or vomiting from swallowing large amounts of blood.
- Anemia is rare, usually only with severe, recurrent posterior bleeds.
- Septal perforation is rare, from aggressive or repeated cautery.
- Airway compromise is extremely rare, usually only with massive posterior hemorrhage.
Foreign Body Aspiration
- Foreign Body Aspiration (FBA) is the inhalation of an object (food or non-food) into the respiratory tract, leading to partial or complete airway obstruction.
Incidence
Most common in children under 3 years of age, with a peak incidence between 1 and 2 years. Infants and toddlers are at high risk because they use their mouths to explore, have immature swallowing and chewing coordination, and are easily distracted while eating.
Pathophysiology
The foreign body is inhaled and most commonly lodges in the bronchial system (more frequently the right main bronchus due to its wider, shorter, and more vertical angle). The obstruction can create different physiological effects:
- Bypass Valve: Air passes in both directions around the object (minimal symptoms).
- Check Valve: Air enters on inspiration but is trapped on expiration, leading to air-trapping and hyperinflation distal to the object.
- Stop Valve (Complete Obstruction): No air passes, leading to atelectasis (collapse) distal to the object.
Commonly Ingested/Aspirated Items
- Food: Nuts (especially peanuts), seeds, hot dogs, grapes, popcorn, raw carrots, hard candies.
- Non-Food: Small toys, toy parts, coins, buttons, batteries, pins, marbles, deflated balloons (most likely to cause death).

Clinical Manifestations Based on Location
|
Location |
Manifestation (Acute Phase) |
|
Larynx |
Acute, severe distress: Stridor, aphonia (inability to speak), severe respiratory distress, cyanosis, and rapid progression to airway complete obstruction/death. |
|
Trachea |
Coughing, choking, wheezing (often stridor/rales), dyspnea, "tracheal tug" (neck movement with breathing). Less common site than bronchi. |
|
Bronchi (Most Common) |
Initial choking/coughing episode (often unwitnessed or quickly forgotten), followed by a symptom-free period, then persistent cough, localized wheezing (not relieved by bronchodilators), decreased breath sounds on the affected side, and potentially recurrent pneumonia. |
Diagnostic Evaluation
- History and Physical Exam: A high index of suspicion is required, especially with a history of a sudden onset of coughing/choking in an otherwise well child, even if the parent didn't see an object. Auscultation may reveal a focal wheeze or decreased air entry.
- Radiography (X-ray):
- Inspiratory/Expiratory Chest X-ray: May show air-trapping (hyperinflation on the affected side in expiration) or mediastinal shift away from the affected side.
- A normal X-ray does not rule out FBA, as most foreign bodies (especially food) are radiolucent (not visible).
- Fluoroscopy: Live X-ray observation of diaphragm movement (affected side's diaphragm may move less).
- Bronchoscopy (Gold Standard): Both a diagnostic and therapeutic procedure. Rigid bronchoscopy is the definitive procedure for visualizing and removing the foreign body under general anesthesia.
Complications
- Pneumonia (Post-obstructive).
- Atelectasis.
- Bronchiectasis from chronic dilation of the airway.
- Pneumothorax.
- Airway injury or erosion.
- Death from acute airway obstruction.
Therapeutic Management (Emergency Management for Choking)
Management is guided by the child's age and whether they can cough effectively.
|
Age Group |
Conscious, Severe Obstruction/Ineffective Cough |
Unconscious or Cardiopulmonary Arrest |
|
Infant (under 1 year) |
5 Back Blows (supported in a prone position) followed by 5 Chest Thrusts (supported supine, thrusts over the sternum) until the object is expelled or the infant becomes unconscious.
|
Begin Cardiopulmonary Resuscitation (CPR). Look in the mouth and remove the foreign body only if visualized. |
|
Child (over 1 year) |
Abdominal Thrusts (Heimlich Maneuver) until the object is expelled or the child becomes unconscious.
|
Begin Cardiopulmonary Resuscitation (CPR). Look in the mouth and remove the foreign body only if visualized. |
Nursing Insight: Blind finger sweeps are contraindicated as they may push the object further down.
Nursing Care Management
- Monitor: Place the child in a position of comfort, maintain NPO status, provide humidified oxygen if needed, and monitor for signs of distress (stridor, wheezing, effort).
- Pre-Procedure Care: Prepare the child and family for a rigid bronchoscopy. Ensure informed consent is signed.
- Post-Procedure Care: Monitor for post-bronchoscopy complications (laryngospasm, stridor, hemorrhage, respiratory distress). Maintain airway patency, ensure humidified oxygen, and keep the child NPO until the gag reflex returns.
- Parent Education: Provide anticipatory guidance on age-appropriate safety.
Prevention Strategies
- Age-Appropriate Food: Teach parents to cut round foods (hot dogs, grapes) into small pieces. Avoid high-risk foods (nuts, popcorn) until age 5.
- Supervision: Closely supervise small children while eating and playing.
- Safety Standards: Adhere to age recommendations on toys (no small, detachable parts for children under 3 years).
- Eating Rules: Encourage children to sit still while eating (avoid running, jumping, or laughing with food in the mouth).
Pulmonary Edema
- Pulmonary edema is the accumulation of fluid in the air spaces (alveoli) and parenchyma of the lungs, leading to impaired gas exchange and respiratory failure.
Pathophysiology
Fluid leaks out of the pulmonary capillaries into the interstitial space and then the alveoli. It is typically categorized as:
- Cardiogenic (Hydrostatic) Pulmonary Edema: The most common form. Caused by an increase in pulmonary capillary hydrostatic pressure, for instance, from heart failure or fluid overload, which pushes fluid out of the vessels.
- Non-Cardiogenic (Permeability) Pulmonary Edema: Caused by a damage to the alveolar-capillary membrane, for instance, in ARDS or smoke inhalation, which increases the membrane's permeability and allows protein-rich fluid to leak out, regardless of pulmonary pressure.
Pathophysiology of Pulmonary Edema
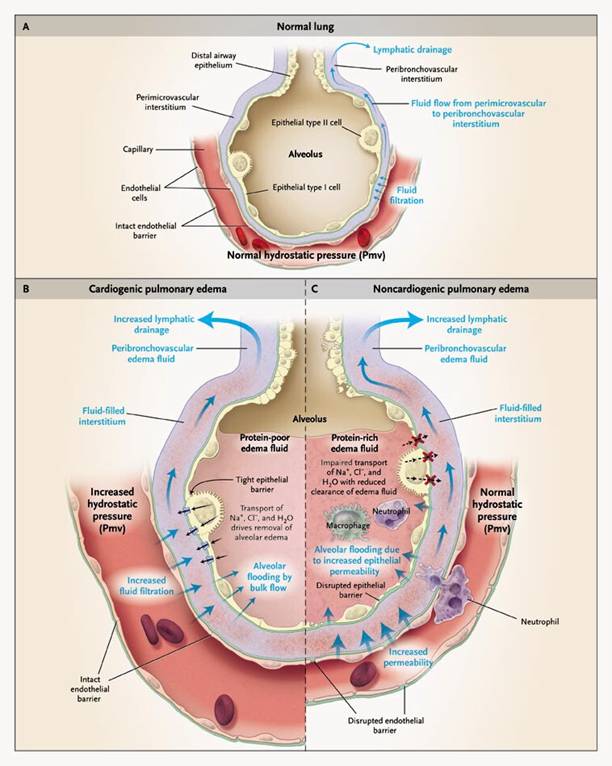
Etiology
- Cardiac: Left-sided heart failure (most common), Myocarditis, Valvular disease, Hypertension.
- Non-Cardiac: Near-drowning, acute respiratory distress syndrome (ARDS), Sepsis, Smoke Inhalation, Rapid infusion of IV fluids (Iatrogenic), High altitude pulmonary edema (HAPE), Neurogenic causes (e.g., head trauma).
Clinical Manifestations
- Severe Respiratory Distress: Dyspnea, tachypnea, orthopnea (difficulty breathing when lying flat).
- Auscultation: Crackles (rales), often described as coarse, wet, or "bubbly" sounds in the lung bases, which may progress throughout the lung fields.
- Cough: May be frothy, pink-tinged sputum (classic sign of severe edema).
- Cardiovascular: Tachycardia, pallor, hypotension (with severe failure/shock).
- Behavioral: Restlessness, anxiety, and altered mental status (due to hypoxemia).
Diagnostic Evaluation
- Chest X-ray (CXR): Classic findings are bilateral, diffuse infiltrates (white), often described as a "bat wing" or "butterfly" pattern, evidence of interstitial or alveolar fluid, and potentially cardiomegaly (in cardiogenic causes).
- Arterial Blood Gas (ABG): Shows initial respiratory alkalosis (due to hyperventilation) followed by respiratory acidosis and severe hypoxemia.
- Brain Natriuretic Peptide (BNP): Elevated in cardiogenic pulmonary edema.
- Echocardiogram: To assess left ventricular function and rule out cardiac causes.
Therapeutic Management
- Oxygenation and Ventilation: High-flow oxygen (non-rebreather mask), Positive-Pressure Ventilation (e.g., CPAP/BiPAP) to push fluid out of the alveoli, or Endotracheal intubation with Mechanical ventilation in severe cases.
- Positioning: Fowler's position or sitting upright to decrease venous return and lung congestion.
- Cardiogenic Edema Treatment
- The goal is to reduce preload and afterload:
- Diuretics: Furosemide (Lasix) to promote rapid fluid excretion.
- Vasodilators: Nitrates or other medications to reduce preload and afterload.
- Inotropes: If cardiac function is severely depressed (e.g., Dopamine, Dobutamine).
- The goal is to reduce preload and afterload:
- Non-Cardiogenic Edema Treatment: Focus on treating the underlying cause (e.g., ARDS management, removing the toxin) and providing aggressive respiratory support.
- Monitoring: Continuous cardiac and pulse oximetry monitoring, frequent vital signs, strict Intake and Output (I&O), and daily weights.
Acute Respiratory Distress Syndrome
- ARDS (sometimes called Acute lung injury (ALI) or Non-Cardiogenic pulmonary edema) is a sudden, life-threatening form of non-cardiogenic pulmonary edema and progressive hypoxemia that occurs due to a systemic or pulmonary insult, resulting in diffuse injury to the alveolar-capillary membrane.
Pathophysiology
ARDS is characterized by a systemic inflammatory response (SIRS) that damages the alveolar-capillary membrane, leading to a breakdown of the normal barrier.
- Injury: A direct (e.g., pneumonia, aspiration) or indirect (e.g., sepsis, trauma) injury initiates a massive inflammatory response.
- Increased Permeability: Inflammatory mediators damage the membrane, increasing its permeability. This allows protein-rich fluid to leak into the alveoli (non-cardiogenic pulmonary edema).
- Surfactant Dysfunction: The fluid and inflammation deactivate or destroy pulmonary surfactant.
- Alveolar Collapse/Atelectasis: Loss of surfactant increases surface tension, leading to widespread collapse of the alveoli, reducing the surface area for gas exchange.
- Refractory Hypoxemia: The resulting "shunting" of blood past non-ventilated alveoli causes severe hypoxemia that is often refractory (unresponsive) to high concentrations of oxygen.
Pathogenesis of Acute Respiratory Distress Syndrome
Etiology
- Sepsis (Most Common Cause).
- Severe Trauma.
- Aspiration.
- Near-Drowning.
- Smoke Inhalation/Toxic Inhalation.
- Pneumonia (rarely).
Clinical Manifestations
Initial symptoms occur 12–48 hours after the insult:
- Increasing Respiratory Distress: Tachypnea, dyspnea, increased work of breathing, use of accessory muscles.
- Hypoxemia: Worsening hypoxemia despite increasing $O_2$ concentrations (refractory).
- Auscultation: Initial clear lungs, followed by the development of crackles/rales (due to fluid accumulation).
- Late Signs: Cyanosis, lethargy, confusion.
Diagnostic Evaluation
- Clinical Criteria (Pediatric-Specific Criteria apply): Acute onset, presence of a known risk factor, bilateral infiltrates on CXR consistent with pulmonary edema, and lack of evidence for left atrial hypertension (cardiogenic cause).
- CXR: Diffuse, bilateral, fluffy infiltrates (ground-glass appearance) that rapidly worsen.
- ABG: Severe hypoxemia.
- Pulse Oximetry: Persistent low saturation despite 100% O2.
Therapeutic Management
There is no specific cure, so treatment is supportive, focusing on oxygenation, ventilation, and managing the underlying cause.
- Mechanical Ventilation: Requires aggressive support, often with high levels of Positive End-Expiratory Pressure (PEEP) to keep the damaged alveoli open and improve oxygenation. Lung-Protective Strategies (low tidal volumes) are used to prevent further lung injury.
- Optimal Fluid Management: Conservative fluid management is preferred to avoid worsening pulmonary edema, while maintaining adequate perfusion and blood pressure.
- Treat Underlying Cause: Aggressive treatment of sepsis, trauma, or pneumonia.
- Prone Positioning: Turning the child onto their stomach to help with better ventilation/perfusion matching.
- Pharmacology:
- Inotropes/Vasopressors: To maintain adequate blood pressure.
- Neuromuscular Blockade/Sedation: To ensure the child is comfortable and synchronized with the ventilator.
Nursing Care Management
- Airway and Ventilation: Frequent respiratory assessment, meticulous care of the endotracheal tube and mechanical ventilation circuit. Monitor PEEP, peak inspiratory pressure, and O2 saturation continuously.
- Positioning: Frequent turning, including prone positioning (requires multiple staff and careful attention to lines/tubes).
- Hemodynamic Monitoring: Close monitoring of vital signs, blood pressure, and I&O.
- Comfort and Sedation: Pain assessment and adequate sedation/analgesia to reduce O2 consumption and anxiety.
- Infection Control: Strict asepsis for all invasive lines and procedures (e.g., suctioning) to prevent secondary infection.
- Nutrition: Initiate early enteral or parenteral nutrition to support healing.
Smoke Inhalation Injury
- Respiratory injury resulting from the inhalation of thermal irritants, smoke, or toxic fumes produced during a fire.
Pathophysiology
Injuries are categorized into three types:
- Heat Injury (Thermal): Usually confined to the upper airway (nasopharynx, oropharynx, larynx) because the heat is rapidly dissipated. Causes mucosal edema and potential upper airway obstruction.
- Local Chemical Injury (Aerosolized Toxins): Caused by irritating chemicals (e.g., aldehydes, sulfur dioxide) in the smoke that travel to the lower airways (trachea, bronchi, alveoli). Causes chemical pneumonitis, severe inflammation, bronchospasm, loss of ciliary action, and sloughing of the mucosa. This can lead to atelectasis, non-cardiogenic pulmonary edema, and ARDS.
- Systemic Injury (Toxic Gases): Caused by gases that are absorbed into the bloodstream. The most critical are:
- Carbon Monoxide (CO): A colorless, odorless gas that has a 200 times greater affinity for hemoglobin than oxygen, forming carboxyhemoglobin (COHb). This severely impairs the blood's oxygen-carrying capacity, leading to tissue hypoxia.
- Cyanide: Interferes with cellular oxygen use, leading to cellular asphyxia.
Clinical Manifestations
- Upper Airway: Facial/neck burns, singed nasal/facial hair, soot around the nose or mouth, hoarseness, stridor, drooling (ominous signs of impending obstruction).
- Lower Airway/Parenchymal: Cough, wheezing/bronchospasm, copious secretions, dyspnea, crackles, or signs of ARDS. Symptoms may be delayed 24–48 hours.
- Systemic:
- CO Poisoning: Headache, nausea, vomiting, dizziness, confusion, or a deceptive "cherry-red" skin/mucosa (due to COHb). Pulse oximetry is unreliable as it reads COHb as normal O2 saturation.
- Cyanide Poisoning: Altered mental status, hypotension, and cardiorespiratory arrest.
Diagnostic Evaluation
- Arterial Blood Gas (ABG): To assess oxygenation and ventilation.
- COHb Level: Direct measurement of carboxyhemoglobin (essential for CO poisoning diagnosis).
- CXR: May be initially clear, but develops infiltrates later as pulmonary edema/pneumonitis worsens.
- Bronchoscopy: Used to directly visualize the extent of mucosal damage (burns, edema, soot).
Nursing Insight: With carbon monoxide poisoning, the oxygen saturation (SaO2) obtained by pulse oximetry will be normal because the device measures only oxygenated and deoxygenated hemoglobin; it does not measure dysfunctional hemoglobin, such as COHb.
Therapeutic Management
- Secure Airway: Immediate concern is upper airway edema/obstruction. Early intubation is often done prophylactically if stridor, hoarseness, or significant facial/mouth burns are present, as swelling can rapidly make intubation impossible.
- Oxygenation: 100% High-Flow Oxygen for all suspected CO exposure, regardless of pulse oximetry reading, to rapidly displace CO from the hemoglobin. Continue until COHb level is near normal.
- Cyanide Treatment: Antidote Kit (e.g., Hydroxocobalamin) if cyanide poisoning is suspected.
- Lower Airway: Humidified O2, aerosolized bronchodilators (for bronchospasm), chest physiotherapy (CPT), and suctioning.
- Fluid Management: Careful administration of IV fluids to prevent hypovolemic shock (due to burns) without exacerbating pulmonary edema.
Nursing Care Management
- Continuous Respiratory Assessment: Monitor for signs of airway obstruction (stridor, hoarseness) and respiratory failure. Prepare for intubation.
- CO Monitoring: Ensure COHb levels are drawn and monitored frequently.
- Pain/Anxiety Management: Administer analgesics and sedatives, especially in the presence of burns.
- Pulmonary Hygiene: Aggressive chest physiotherapy and suctioning to remove sloughed mucosa and secretions.
- Burn Care: Manage associated thermal injuries.
Environmental Tobacco Exposure
- Environmental Tobacco Exposure (ETE), also known as Secondhand Smoke (SHS) or Passive Smoking, is the inhalation of smoke from burning tobacco products by non-smokers.
Pathophysiology
Tobacco smoke contains over 7,000 chemicals, including hundreds that are toxic or carcinogenic. When inhaled, these chemicals:
- Irritate Airways: Cause inflammation and swelling of the respiratory tract lining.
- Impair Cilia: Damage the ciliary function, reducing the ability to clear mucus and pathogens.
- Increase Mucus Production: Leading to chronic cough and increased susceptibility to infection.
- Systemic Absorption: Nicotine and carbon monoxide are absorbed, affecting respiratory control and oxygen-carrying capacity (similar to the effects on adult smokers).
Etiology
The primary etiology is living in a household with a smoker (parent, caregiver, or sibling) or frequent exposure in other environments (e.g., cars). Thirdhand Smoke (THS) is the residue from tobacco smoke that clings to surfaces and clothing and can also be a source of exposure.
Second-Hand Smoke Exposure Effects
- Lower Respiratory Tract Illnesses: Bronchitis, bronchiolitis, and pneumonia (especially in infants).
- Chronic Symptoms: Chronic cough, wheezing, and dyspnea.
- Asthma: Increased frequency and severity of asthma attacks.
- Middle Ear Infections (Otitis Media): Increased incidence and chronic effusions.
- SIDS: ETE is a significant, independent risk factor for SIDS.
- Decreased Lung Function: Long-term reduced lung growth and function.
Influences of Second-Hand Smoke Exposure
Diagnostic Evaluation
- History: The most important tool is a detailed history of the child's home environment, including who smokes, where, and how often.
- Cotinine Levels: A laboratory test (urine, serum, or saliva) that measures cotinine, a metabolite of nicotine, which confirms exposure to tobacco smoke.
- Pulmonary Function Tests (PFTs): May show decreased lung capacity and function in older children.
Therapeutic Management
- Elimination of Exposure (Primary Goal): The only effective treatment is the complete elimination of ETE.
- Symptomatic Treatment: Treatment of associated conditions (e.g., bronchodilators and corticosteroids for asthma exacerbations, antibiotics for recurrent infections).
Nursing Care Management
- Education: Provide compassionate but direct education to parents/caregivers on the causal link between ETE and pediatric morbidity (SIDS, ear infections, asthma).
- Focus on the child's health as the primary motivation for change.
- Emphasize that smoking outside the house does not eliminate the risk (smoke residue remains on clothes/hair).
- Advise parents to make their homes and cars 100% smoke-free.
- Referral: Offer referrals for adult smoking cessation programs (nicotine replacement therapy, counseling).
- Support: Avoid judgment; understand that nicotine addiction is a chronic disease requiring support.
- Anticipatory Guidance: Educate all families on ETE's link to SIDS as part of the "Safe to Sleep" education.
Summary
- Non-infectious pediatric respiratory disorders require the student nurse to integrate knowledge of anatomical vulnerabilities, physiological principles, and emergency interventions.
- SIDS is a medical tragedy managed solely by prevention through the strict adherence to "Safe to Sleep" guidelines, especially supine sleeping and avoiding soft bedding. The nursing role is paramount in non-judgmental education and providing intensive family support after a loss.
- Epistaxis is common and benign, typically managed by proper positioning (sitting up, leaning forward) and direct pressure on the soft part of the nose for 10–15 minutes.
- Foreign Body Aspiration (FBA) is a critical emergency, predominantly affecting toddlers, with the most severe complications occurring in the larynx. Immediate management for choking involves back blows/chest thrusts for infants and abdominal thrusts for older children, followed by definitive diagnosis and removal via rigid bronchoscopy. Prevention is key through age-appropriate food and toy safety.
- Pulmonary Edema and ARDS represent a spectrum of acute, life-threatening conditions involving fluid in the lungs. ARDS, specifically, involves damage to the alveolar membrane, resulting in severe refractory hypoxemia. Management is supportive, focusing on high-level mechanical ventilation (with PEEP and lung-protective strategies), fluid optimization, and treating the underlying cause.
- Smoke Inhalation Injury presents a multi-faceted challenge, requiring vigilance for impending airway obstruction (thermal injury) and recognition of systemic toxicity (CO poisoning), which demands immediate 100% O2 therapy.
- Environmental Tobacco Exposure (ETE) is a major preventable pediatric health risk, increasing the likelihood of SIDS, asthma, and recurrent infections. The primary nursing intervention is focused, non-judgmental patient/family education and referral for smoking cessation to ensure a smoke-free home environment.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Non-infectious Respiratory Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now