Please set your exam date
Medication Administration and Intravenous Therapies
Study Questions
Practice Exercise 1
The following medications are listed on a client’s medication administration record (MAR). Which medication order should the nurse question?
Explanation
A valid order must include the drug name, dose, route, timing/frequency, and (for PRN meds) a clear indication (and often parameters). Ambiguous or incomplete orders must be clarified before administration.
Rationale for correct answer:
4. Codeine q4–6h, po, prn for pain: This PRN order omits the dose (and lacks PRN parameters like pain scale/maximum daily dose). You cannot safely administer a medication without a specified dose.
Rationale for incorrect answers:
1. Lasix 40 mg, po, STAT: Complete- drug, dose, route, and urgent timing (“STAT”). As always, assess BP, electrolytes, and need for rapid diuresis, but the order itself is clear.
2. Ampicillin 500 mg, q6h, IVPB: Complete: drug, dose, frequency, and route (IV piggyback). The nurse should still verify allergies and compatibility/infusion time per policy.
3. Humulin L (Lente) insulin 36 units, subcutaneously, every morning before breakfast: Complete- drug, dose, route, timing. If not on formulary, pharmacy may substitute an equivalent per protocol; that’s not a reason to reject the order outright. Monitor glucose and hypoglycemia risk.
Take home points
- Never give a medication from an incomplete order (missing dose, route, frequency, or PRN parameters). Clarify first.
- PRN orders require a dose and indication (often with pain scale parameters and max dose); otherwise, they are not safe to act on.
Which drug name is the name selected by the pharmaceutical company selling the drug and protected by trademark?
Explanation
Drug names come in several forms (chemical, generic/nonproprietary, official, and trade/brand). Knowing the difference matters for prescribing, dispensing, and patient education - especially because the trade/brand name is chosen for marketing and may differ between manufacturers.
Rationale for correct answer:
4. Trade name: Also called the brand name, this is selected by the pharmaceutical company, marketed under trademark (e.g., Tylenol), and protected legally.
Rationale for incorrect answers:
1. Chemical name: This is the precise chemical/IUPAC description of the molecule (long, technical), not a marketed brand name.
2. Generic name: The generic (nonproprietary) name is the official, non-brand name (e.g., acetaminophen) assigned by authoritative naming bodies; it is not trademarked.
3. Official name: Often refers to the name used in pharmacopeias (typically the generic name), not the proprietary name chosen by a company.
Take home points:
- The trade/brand name is proprietary and can vary between manufacturers; the generic name is universal and safer to use in clinical documentation.
- Always check both trade and generic names to avoid confusion and medication errors (many drugs have multiple brand names).
A medication order reads: “K-Dur, 20 mEq PO b.i.d.” When does the nurse correctly give this drug?
Explanation
Correct reading of route, frequency and medication name prevents administration errors.
Rationale for correct answer:
3. Twice a day by the oral route: PO = by mouth; b.i.d. (bis in die) = twice daily. So administer 20 mEq orally, two times per day.
Rationale for incorrect answers:
1. Daily before bedtime: “Before bedtime” = qhs; b.i.d. does not mean nightly.
2. By mouth every other day: “Every other day” = qod; b.i.d. means twice daily, not every other day.
4. Once a week after recording an apical rate: This is unrelated: once a week and apical rate monitoring are not indicated by “K‑Dur 20 mEq PO b.i.d.”
Take home points
- Read orders carefully: PO = by mouth, b.i.d. = twice daily. Confirm any unclear abbreviations.
- For potassium (K‑Dur), always check renal function and current serum potassium before administration and follow facility policy on monitoring and timing.
A patient refuses to take her noon medication, saying that she does not need it. Which of the following would be the best response?
Explanation
Patients have the legal right to refuse treatment, and the nurse’s role is to explore the reasons, provide education, and document the refusal - not to coerce or belittle. Using open-ended, nonjudgmental communication fosters trust and allows for problem-solving.
Rationale for correct answer:
4. Tell her that you will return the medications and discuss her reasons: This respects her right to refuse while opening dialogue to address concerns. It allows for education and clarification without pressure.
Rationale for incorrect answers:
1. Tell her that she must take the medication because the doctor ordered it: This is authoritarian and disregards patient autonomy. Orders must be explained and consented to; forcing medication is unethical unless legally justified (e.g., mental health commitment with court order).
2. Tell her that you went through a lot of preparation: This makes the conversation about the nurse’s effort, not the patient’s health needs. It is unprofessional and ineffective.
3. Tell her that you don’t care whether she takes the medications or not: This is dismissive, non-therapeutic, and damages rapport.
Take home points
- Patients have the right to refuse medications; the nurse must assess and document the reason.
- Therapeutic communication should be respectful, patient-centered, and focused on understanding concerns.
You are to administer a medication to Mr. Brown. In addition to checking his identification bracelet, you can correctly verify his identity by doing which of the following?
Explanation
Patient identification is a critical safety step before any medication, procedure, or blood draw. Best practice is to use two reliable patient identifiers (for example, name and date of birth) and to confirm them directly with the patient when possible.
Rationale for correct answer:
1. Asking the patient his name (and ideally date of birth) is an active, direct verification that should be matched to the ID bracelet and the MAR. It uses the patient as a safety checkpoint and provides two identifiers when you include DOB.
Rationale for incorrect answers:
2. Reading the patient’s name on the sign over the bed: Signs over the bed are not considered a reliable identifier (they may be outdated or incorrect) and should not replace checking the ID bracelet and asking the patient.
3. Asking the patient’s roommate to verify his name: Roommates may be mistaken, and using others to identify a patient breaches privacy and is unreliable.
4. Asking, “Are you Mr. Brown?” Yes/no questions are leading and less reliable. The patient may say “yes” to please the nurse or be confused; asking the patient to state name (and DOB) is preferred.
Take home points
- Always use two identifiers (e.g., patient states full name and DOB) and match them to the ID bracelet and the MAR before giving meds.
- If a patient cannot answer, use alternative approved identifiers (wristband with barcode, photo in chart, or two staff verification) per facility policy.
Practice Exercise 2
The primary care provider prescribed 5 mL of a medication to be given deep intramuscular for a 40-year-old female who is 5′7″ tall and weighs 135 pounds. Which is the most appropriate equipment for the nurse to use? Select all that apply
Explanation
Safe intramuscular (IM) administration depends on three things: how much you inject at one site (site capacity), how deep you reach (needle length vs body habitus/site), and how thick the needle is (gauge vs medication viscosity).
Rationale for correct answer:
1. Two 3-mL syringes: A total of 5 mL should be split (e.g., 2.5 mL + 2.5 mL) because most adult IM sites safely hold ≤3 mL. Splitting improves absorption and comfort and reduces tissue trauma.
3. A #20–#23-gauge needle: IM injections usually use 22–25 gauge for aqueous solutions; 22–23 gauge is ideal here. (A 20-gauge is larger and more painful-reserve for very viscous meds only.)
5. A 1½-inch needle: For an average-build adult female (5′7″, 135 lb), a 1½" needle reliably reaches the muscle in the ventrogluteal site for deep IM delivery.
Rationale for incorrect answers:
2. One 5-mL syringe: Injecting the entire 5 mL into one site exceeds typical site capacity, increasing pain, reflux/leakage, and risk of muscle damage or poor absorption.
4. A 1-inch needle: A 1" needle may suffice for deltoid in a slender adult, but for deep IM-especially in the ventrogluteal site and with this volume-it risks depositing medication subcutaneously.
Take home points:
- Don’t exceed ~3 mL per IM site. Split larger doses into two syringes/sites
- Use Z-track and pick a large muscle (ventrogluteal) for volumes >2 mL.
- Match the needle to the task: 1½" (deep IM gluteal) and 22–23 gauge for most aqueous meds; reserve larger gauges for viscous solutions.
The nurse is to administer 0.75 mL of medication subcutaneously in the upper arm to a 300-pound adult client. The nurse can grasp approximately 2 inches of the client’s tissue at the upper arm. Which is the most appropriate for the nurse to use?
Explanation
Needle gauge for SQ injections is usually finer (higher number) than IM needles; needle length depends on the pinch-up thickness and injection angle.
Rationale for correct answer:
3. 2-mL syringe, #25 gauge, 5/8-inch needle: A 2-mL syringe easily measures 0.75 mL. A 25-gauge needle is an appropriate fine gauge for subcutaneous injections. A 5/8-inch needle is a standard SQ length and, when the nurse can grasp ~2 inches of tissue, insertion at a 90° angle will reliably deposit medication into the subcutaneous tissue.
Rationale for incorrect answers:
1. Tuberculin syringe, #25–#27-gauge, 1/4- to 5/8-inch needle: Tuberculin syringes are primarily used for intradermal/TB testing and small-volume measurements; the variable length range (includes very short 1/4") makes this option less explicit.
2. Two 3-mL syringes, #20–#23-gauge, 1 1/2-inch needle: Two syringes are unnecessary for a single 0.75-mL dose. A 1½-inch needle and 20–23 gauge are appropriate for intramuscular injections (thicker and longer).
4. 2-mL syringe, #20–#23 gauge, 1-inch needle: The 1-inch length and lower-gauge needle (20–23) are more characteristic of IM injections; using these for an SQ injection increases the risk of injecting into muscle (and causes more pain).
Take home points
- Match needle length to the pinch-up thickness and angle.
- Use an appropriate gauge and syringe size: SQ injections commonly use 25–27 gauge needles.
- Choose a syringe that comfortably holds the ordered volume (a 2-mL syringe is ideal for 0.75 mL).
The nurse is to administer a tuberculin test to a client who is 6 feet tall and weighs 180 pounds. Which is the most appropriate for the nurse to use?
Explanation
The tuberculin (Mantoux) test is given intradermally, usually on the inner forearm. Intradermal injections require a small-volume syringe with a very fine, short needle so the solution is deposited just under the skin to form a visible wheal.
Rationale for correct answer:
1. Tuberculin syringe, #25–#27 gauge, 1/4–5/8-inch: Tuberculin (1 mL) syringes allow accurate measurement of the small volume used for skin testing. Fine gauges (25–27) and very short needles (commonly 1/4–1/2 inch) are standard for intradermal placement to produce a proper wheal.
Rationale for incorrect answers:
2. Two 3-mL syringes, #20–#23 gauge, 1½-inch needle: These are IM-type syringes/needles (too long and too large) and unnecessary for the tiny intradermal volume; using them risks injecting too deep.
3. 2-mL syringe, #25 gauge, 5/8-inch needle: While the gauge is acceptable, a 2-mL syringe is not the typical tuberculin syringe and a 5/8" needle is borderline long for intradermal use (risk of subcutaneous placement).
4. 2-mL syringe, #20–#23 gauge, 1-inch needle: Needle is far too long and gauge too large for intradermal testing; this would likely deposit medication too deep (subcutaneous or intramuscular).
Take home points:
- Use a tuberculin (1 mL) syringe with a fine (25–27 ga), very short needle for intradermal injections to ensure a proper wheal.
- Avoid IM/SQ equipment (longer needles, larger gauges) for skin tests - they deposit the solution too deep and invalidate the result.
The nurse is to administer 0.5 mL of a medication by intramuscular injection to an older emaciated client. Which is the most appropriate for the nurse to use?
Explanation
Selecting IM equipment requires matching syringe size, needle gauge, and needle length to the patient’s body habitus and the medication volume. In an older, emaciated client muscle mass is reduced.
Rationale for correct answer:
3. 2-mL syringe, #25 gauge, 5/8-inch needle: A 2-mL syringe is appropriate for a 0.5-mL dose. A 25-gauge is a fine needle that reduces pain, and a 5/8-inch length is often appropriate for very thin or emaciated older adults to deliver into the muscle without risking deep tissue or bone injury.
Rationale for incorrect answers:
1. Tuberculin syringe, #25–#27 gauge, 1/4–5/8-inch needle: Tuberculin syringes are primarily for intradermal/intradermal or very small SQ injections. Although the 5/8" length is sometimes used SQ, a tuberculin syringe is not the preferred choice for IM administration.
2. Two 3-mL syringes, #20–#23-gauge, 1½-inch needle: This setup is for larger-volume IM injections and uses a long needle and larger bore-unnecessary and potentially harmful for a 0.5-mL dose in a frail, emaciated client (risk of overpenetration, more pain).
4. 2-mL syringe, #20–#23 gauge, 1-inch needle: Although 1-inch is commonly used for IM in average adults, for an emaciated older adult this length may be too long and risks hitting bone or causing excess trauma. The larger bore (20–23) causes more pain than a finer 25 ga.
Take home points:
- For older, thin clients choose a shorter needle (e.g., 5/8") and finer gauge (e.g., 25 ga) to reach the muscle safely while minimizing trauma.
- Always assess the injection site’s tissue depth and choose needle length accordingly; when in doubt, a shorter needle (with correct angle/technique) is safer than one that’s too long.
A nursing student is preparing to administer insulin to a client with diabetes. Indicate the correct order for the administration of this medication:
Explanation
Safe insulin administration requires assessment, correct preparation (including mixing when necessary), aseptic technique, proper injection technique (pinch, angle), and allowing the medication to be absorbed (counting in place) before removing the needle.
Rationale for correct answer:
4. Assess the skin for the injection: Verify the site is intact (no infection, edema, bruising, scars) and appropriate for injection. Assessment precedes any procedure.
3. Mix the insulins: If the order is for mixed insulin (e.g., NPH + regular), prepare and mix the insulin vials first (roll NPH gently). When drawing up into the syringe, follow “clear before cloudy” (draw regular first, then NPH) to avoid contaminating the short-acting insulin.
1. Cleanse the site with alcohol: Clean the skin (if policy requires/if site is dirty) and allow to air dry to reduce infection risk. Do this after preparation so the site remains clean until injection.
5. Pinch the skin lightly: Creates a fold of subcutaneous tissue to ensure the injection goes into SQ tissue (especially important in lean persons). Pinch position depends on the site and patient habitus.
2. Insert the needle quickly into the subcutaneous tissue: A quick, decisive insertion minimizes pain and places the needle at the correct depth (45° or 90° depending on needle length and amount of subcutaneous tissue).
6. Inject the medication: Depress the plunger steadily to administer the insulin.
7. Count to five: Hold the needle in place for about 5 seconds (some guidelines say 5–10 sec) to ensure full dose delivery and prevent medication tracking back up the tract.
8. Remove the syringe: Withdraw the needle smoothly and safely; dispose immediately in sharps container. Do not massage the site (unless specifically instructed).
Take home points
- Assess first, prepare (mix) then inject.
- Use proper SQ technique (pinch when indicated, insert at correct angle, hold for several seconds, DO NOT massage).
Practice Exercise 3
A client tells the nurse, “This pill is a different color than the one that I usually take at home.” Which is the best response by the nurse?
Explanation
When a patient raises a concern, the nurse must pause, verify the medication against the order/MAR, and resolve discrepancies before giving it. Patients are valuable safety checkpoints; acknowledging concerns and rechecking prevents errors.
Rationale for correct answer:
2. “I will recheck your medication orders.” Stops administration, validates the patient’s concern, and triggers verification (MAR, pharmacy label, bar code, possible generic substitution) before proceeding.
Rationale for incorrect answers:
1. “Go ahead and take your medicine.” Dismisses the patient’s concern and risks a medication error. The nurse must verify before administering.
3. “Maybe the doctor ordered a different medication.” Speculative and still unsafe-do not guess; verify.
4. “I’ll leave the pill here while I check with the doctor.” Never leave medications unattended at the bedside; the patient might take it before verification, defeating the safety check.
Take-home points
- If anything seems off (appearance, dose, timing)-stop and verify the order/MAR and the drug itself (including possible generic substitutions) before giving.
- Never leave meds at the bedside and never dismiss patient concerns; patients are key partners in preventing med errors.
Proper administration of an otic medication to a 2-year-old client includes which of the following?
Explanation
When instilling ear drops, the goal is to straighten the external auditory canal so the medication reaches the tympanic membrane area. Pinna manipulation differs by age because the ear canal angle changes as the child grows.
Rationale for correct answer:
2. Pull the ear down and back: For children younger than 3 years, the external auditory canal is more horizontal; pulling the pinna down and back straightens the canal so drops flow in and coat the tympanic membrane.
Rationale for incorrect answers:
1. Pull the ear straight back: Pulling straight back does not optimally straighten the canal in a toddler and may not provide the best route for drops to the tympanic membrane.
3. Pull the ear up and back: Up and back is the correct maneuver for older children and adults (generally >3 years), because their canal angle is different. Using up-and-back on a toddler may be uncomfortable and less effective.
4. Pull the ear straight upward: This does not adequately open the canal for optimal instillation in any age group and may be awkward or harmful.
Take home points:
- For children <3 years, pull the pinna down and back to straighten the canal before instilling otic drops.
- For older children/adults, pull up and back.
Ms. Hall has an order for hydromorphone, 2 mg, intravenously, q 4 hours p.r.n. pain. The nurse notes that according to Ms. Hall’s chart, she is allergic to Dilaudid. The order for medication was signed by Dr. Long. Which of the following would be the correct procedure in this situation?
Explanation
Hydromorphone is marketed under the brand name Dilaudid — meaning if a client is allergic to Dilaudid, they are allergic to hydromorphone. Giving a drug the patient is allergic to can cause anaphylaxis.
Rationale for correct answer:
2. Call Dr. Long and ask that she change the medication: The nurse must clarify with the prescribing provider when there is a potential allergy conflict. The safest course is to confirm and request an alternative analgesic.
Rationale for incorrect answers:
1. Administer the medication; the doctor knows best: Nurses are legally and ethically obligated to withhold medications that may harm the patient, even if prescribed by a physician. “The doctor knows best” is not an acceptable rationale when patient safety is at risk.
3. Ask the supervisor to administer the medication: This shifts responsibility but does not resolve the safety issue; if the patient reacts, liability still exists.
4. Ask the pharmacist to provide a medication to take the place of Dilaudid: Pharmacists cannot unilaterally change a prescribed medication; changes require a new or revised provider order.
Take home points
- Always verify allergies before giving any medication; brand and generic names must be recognized.
- Nurses have the duty to clarify or refuse unsafe orders - patient safety overrides blind compliance.
The nurse manager on your unit prepared medications for Mr. Giles. She is called to the phone and asks you to give the patient his medications. Which is the best response to this request?
Explanation
The “five rights” of medication administration require the nurse to verify the correct patient, drug, dose, route, and time. A nurse who did not prepare the medication cannot verify these rights with full certainty, increasing the risk of medication errors.
Rationale for correct answer:
3. Tell the nurse manager that because you did not pour the medication, you cannot administer it: The safest practice is that the nurse who prepares the medication should be the one to administer it. This ensures full accountability and safety verification.
Rationale for incorrect answers:
1. Give Mr. Giles the medication and record it in his chart: This violates safe practice because you did not prepare the medication, so you cannot be sure it is correct.
2. Tell the nurse manager that you do not have time and ask her to get someone else: This is avoiding responsibility without citing the correct safety rationale; time constraints are not the core issue.
4. Give the medication to Mr. Giles but have the nurse manager chart it: This is unsafe and dishonest; you are still the one administering, so you assume responsibility, even if another charts it.
Take home points
- The nurse who prepares the medication must be the one to administer it - this is a core safety standard.
- Accountability in medication administration cannot be delegated; charting must reflect the actual provider of care.
A nurse discovers that she has made a medication error. Which of the following should be her first response?
Explanation
The first priority in any medical error is patient safety - assess the client for any adverse effects, then take steps to correct and report the error. Documentation and reporting are essential but come after immediate patient assessment.
Rationale for correct answer:
3. Check the patient’s condition to note any possible effect of the error: This is the immediate priority - assessing the patient ensures that any necessary interventions can be started quickly.
Rationale for incorrect answers:
1. Record the error on the medication sheet: This is documentation, which is important but not the first step. The patient’s condition must be assessed first.
2. Notify the physician regarding course of action: The provider should be informed promptly, but only after checking the patient’s condition to provide accurate information about possible harm.
4. Complete an incident report, explaining how the mistake was made: The report is important for quality improvement but should be done after ensuring patient safety and notifying the provider.
Take home points
- When a medication error occurs, assess the patient first, then notify the provider, and finally complete documentation.
- Incident reports are for internal safety monitoring, not for the medical record, and should be factual without blame.
Comprehensive Questions
An older client with renal insufficiency is to receive a cardiac medication. Which is the nurse most likely to administer?
Explanation
Renal insufficiency decreases the kidneys’ ability to excrete drugs and their metabolites. For medications that are renally eliminated, this can cause accumulation and toxicity unless the dose or dosing interval is adjusted.
Rationale for correct answer:
1. A decreased dosage: Renal insufficiency often reduces drug clearance. Decreasing the dose (or alternatively increasing the dosing interval) helps prevent drug accumulation and toxicity for renally excreted cardiac drugs.
Rationale for incorrect answers:
2. The standard dosage: Giving a standard dose without adjustment risks accumulation and adverse effects when renal clearance is reduced.
3. An increased dosage: Increasing the dose would further increase the risk of toxicity in renal insufficiency and is inappropriate unless there is a compelling pharmacologic reason.
4. Divided dosages: Dividing a total daily dose into smaller more frequent doses does not necessarily prevent accumulation and may actually increase risk.
Take home points:
- For patients with renal impairment, adjust dose or dosing interval for renally eliminated drugs- check creatinine clearance and drug-specific dosing guidelines.
- Always monitor therapeutic levels and renal function and consult pharmacy when uncertain.
A primary care provider writes a prescription for 0.15 milligram of digoxin intravenously every day. The medication is available in a concentration of 400 micrograms per mL. How many mL will the nurse administer? Round off to one decimal point.
Explanation
Medication calculations require careful unit conversion and an exact volume calculation so the correct dose is given. Convert all quantities to the same units, then divide the desired dose by the concentration to get the volume to administer.
Rationale for correct answer:
- Prescribed dose = 0.15 mg.
- Convert to micrograms (since available strength is in µg/mL):
0.15 mg × 1000 = 150 micrograms (µg). - Concentration available = 400 µg/mL.
- Volume = dose ÷ concentration = 150 µg ÷ 400 µg/mL = 0.375 mL.
Correct answer: 0.4 ml
Take home points
- Always convert units to match (mg → µg) before calculating volume.
- Draw the exact calculated volume when possible; if rounding is required, follow facility policy and document/verify.
The process by which a drug is transferred from its site of entry into the body to the bloodstream is known as which of the following?
Explanation
Pharmacokinetics describes how a drug moves through the body: absorption, distribution, metabolism (biotransformation), and excretion. Identifying each step helps predict onset, intensity, and duration of drug action.
Rationale for correct answer:
1. Absorption: Absorption is the process by which a drug moves from its site of administration (oral mucosa, GI tract, intramuscular site, skin, etc.) into the systemic circulation.
Rationale for incorrect answers:
2. Distribution: Distribution describes movement of the drug from the bloodstream into tissues and organs.
3. Metabolism: Metabolism (biotransformation) is the chemical alteration of the drug (mostly in the liver) to metabolites.
4. Excretion: Excretion is elimination of the drug and its metabolites from the body (kidneys, bile, lungs, sweat).
Take home points:
- Absorption determines how quickly and how much of a drug reaches the circulation - route (IV vs PO), formulation, and blood flow all matter.
- IV administration bypasses absorption, producing immediate bioavailability; oral drugs undergo variable absorption and often first-pass metabolism.
A patient has an abnormal, unexpected response to a drug. This is defined as which of the following?
Explanation
Knowing the difference between tolerance, cumulative effect, idiosyncratic reaction, and anaphylaxis helps nurses recognize, document, and respond appropriately to adverse or unusual patient reactions.
Rationale for correct answer:
3. An idiosyncratic effect: An idiosyncratic effect is an unusual or unexpected reaction to a drug that is not related to its known pharmacologic action, often unpredictable and sometimes genetically mediated (e.g., paradoxical excitation from a sedative).
Rationale for incorrect answers:
1. Drug tolerance means a reduced response to a drug after repeated use, so higher doses are needed to achieve the same effect. It is expected with some drugs (e.g., opioids).
2. A cumulative effect occurs when repeated dosing leads to drug accumulation (often because elimination is slower than dosing), producing progressively greater effect or toxicity. It’s a predictable pharmacokinetic issue.
4. An anaphylactic reaction is a severe, immediate hypersensitivity (allergic) reaction with bronchospasm, hypotension, urticaria - it’s not the general term for any unexpected drug response.
Take home points
- Idiosyncratic reactions are unpredictable and not dose-dependent; treat promptly and document thoroughly.
- Differentiate idiosyncrasy from predictable problems (tolerance, accumulation) and immune-mediated reactions (anaphylaxis) because management and prevention differ.
You are to administer a medication using a nasogastric tube. Before giving the medication, what should you do?
Explanation
Administering meds via an NG tube requires first confirming the tube is in the stomach (not the lungs or a misplaced position). Giving medications into a malpositioned NG tube can cause aspiration, respiratory injury, or fatal outcomes.
Rationale for correct answer:
3. Check for proper placement of the nasogastric tube: Confirm placement before administering meds. Methods include initial radiographic confirmation (gold standard), and routine bedside checks per facility (aspirate gastric contents and check pH, or other approved methods).
Rationale for incorrect answers:
1. Crush the enteric-coated pill for mixing in a liquid: Do not crush enteric-coated or sustained-release formulations; crushing destroys their release properties and can cause irritation or toxicity.
2. Flush open the tube with 60 mL of very warm water: “Very warm” water is unnecessary and could scald; also you must confirm placement before irrigating or instilling anything. Typical flush volumes vary (e.g., 15–30 mL) and depend on tube size and policy.
4. Take the patient’s vital signs: VS may be clinically relevant but are not the immediate priority for safe NG medication administration; placement verification is essential first.
Take home points
- Always confirm NG-tube placement before giving medications or feeds.
- Do not crush enteric-coated or extended-release tablets for NG administration; obtain an appropriate formulation.
The medication order reads: “Hydromorphone, 2 mg IV every 3 to 4 hours p.r.n. pain.” The prefilled cartridge is available with a label reading “Hydromorphone 2 mg/ 1 mL.” The cartridge contains 1.2 mL of hydromorphone. Which of the following actions is correct?
Explanation
Nurses must verify the prescribed dose, compare it with the supplied medication, and administer only the ordered amount-discarding any excess according to facility policy.
Rationale for correct answer:
4. Dispose of 0.2 mL correctly before administering the drug: The order is for 2 mg (1 mL), but the cartridge has 1.2 mL. The extra 0.2 mL (0.4 mg) must be discarded following facility waste procedures (often with a witness for controlled substances) before giving the dose.
Rationale for incorrect answers:
1. Give all the medication in the cartridge because it expanded when it was mixed: Liquid volume in prefilled cartridges may slightly exceed the labeled amount to allow for dead space in syringes, not because of expansion. The nurse must still give only the ordered dose and discard the extra.
2. Call the pharmacy and request the proper dose: The cartridge contains the proper concentration (2 mg/1 mL) for the order. There is no need to request another dose; the nurse can simply measure and administer the correct amount.
3. Refuse to give the medication: There is no valid reason to refuse administration since the medication is correct and available; the nurse simply needs to measure and give the ordered amount.
Take home points
- Always administer exactly the prescribed dose, discarding any extra per policy to avoid overdosing.
- Prefilled syringes may contain slightly more than the labeled dose; never assume it’s “all to be given.”
A patient requires 40 units of NPH insulin and 10 units of regular insulin daily subcutaneously. Which of the following gives the correct sequence when mixing insulins?
Explanation
When mixing NPH (intermediate-acting) and regular (short-acting) insulin in one syringe, the correct method prevents contamination of the short-acting insulin with NPH, ensuring proper onset and action. The golden rule: clear before cloudy- draw up regular insulin (clear) before NPH (cloudy).
Rationale for correct answer:
2. The correct sequence is: Inject air into the NPH vial (do not touch the solution). Inject air into the regular insulin vial. Withdraw regular insulin (clear) first. Withdraw NPH insulin (cloudy) last. This prevents contaminating the regular insulin vial with NPH.
Rationale for incorrect answers:
1. Air should be injected into both vials before withdrawing insulin to avoid creating a vacuum, but you do not draw up regular insulin before injecting air into the NPH vial-this sequence can cause cross-contamination.
3. This results in withdrawing NPH before regular insulin, violating the “clear before cloudy” rule, increasing risk of contaminating the short-acting insulin.
4. This would result in injecting a needle containing NPH into the regular vial, contaminating it and altering its pharmacologic profile.
Take home points:
- Follow the clear before cloudy rule: draw up regular insulin before NPH to avoid contamination.
- Always inject air into both vials before withdrawing any insulin to prevent pressure issues.
Why is the intravenous method of medication administration called the “most dangerous route of administration”?
Explanation
The intravenous (IV) route bypasses absorption barriers, delivering drugs directly into the bloodstream. This provides rapid onset but also eliminates the chance to reverse or slow absorption if an adverse reaction occurs, making safety precautions critical.
Rationale for correct answer:
4. The drug is placed directly into the bloodstream, and its action is immediate: IV administration results in immediate systemic effects; any error in dose, drug choice, or rate of administration can cause rapid, potentially life-threatening consequences.
Rationale for incorrect answers:
1. The vein can take only a small amount of fluid at a time: While very rapid administration of large volumes can cause complications, veins can generally tolerate prescribed infusion volumes if properly administered.
2. The vein may harden and become nonfunctional: This refers to phlebitis or sclerosis, which can occur with repeated IV use, but this is not the main reason the route is considered most dangerous.
3. Blood clots may become a serious problem: IV therapy can cause thrombophlebitis, but this is a potential complication, not the defining reason for the route’s danger.
Take home points
- IV administration delivers drugs directly to systemic circulation, giving no margin for error.
- Always double-check drug, dose, route, and patient before IV administration, especially for high-alert medications.
Mr. King is receiving heparin subcutaneously. Which of the following demonstrates correct technique for this procedure?
Explanation
Heparin is given subcutaneously to prevent clot formation. To minimize tissue damage and bruising, certain practices (no aspiration, no massage) are recommended because the drug’s action and site characteristics make these steps risky.
Rationale for correct answer:
3. Do not aspirate before or massage after the injection: This is the safe and recommended technique for subcutaneous heparin: no aspiration and no massage.
Rationale for incorrect answers:
1. Aspirate before giving and gently massage after the injection: Aspiration is avoided with heparin because it increases bleeding risk, and massaging can cause bruising and hematoma formation.
2. Do not aspirate; massage the site for 1 minute: Massaging is still contraindicated, even without aspiration, because it can increase local bleeding and bruising.
4. Massage the site of the injection; aspiration is not necessary but will do no harm: Even without aspiration, massaging after heparin injection is harmful due to increased risk of bleeding.
Take home points
- For subcutaneous heparin: inject without aspiration, and do not massage afterward.
- Avoiding tissue trauma is key in anticoagulant administration to reduce risk of hematomas and bleeding.
The nurse takes an 8 a.m. medication to the patient and properly identifies her. The patient asks the nurse to leave the medication on the bedside table and states that she will take it with breakfast when it comes. What is the best response to this request?
Explanation
Nurses must ensure the “five rights” (right patient, drug, dose, route, time) at the time of administration and cannot leave medications unattended where they might be misplaced, taken by the wrong person, or incorrectly stored.
Rationale for correct answer:
3. Tell her that you cannot leave the medication but will return with it when breakfast arrives: This respects patient autonomy (she intends to take it with breakfast), maintains safety (meds are not left unattended), and provides a plan of care. Best practice: document the discussion and the plan/time.
Rationale for incorrect answers:
1. Leave the medication and return later to make sure that it was taken: Leaving meds unattended risks loss, wrong ingestion by someone else, accidental double dosing, or improper storage. Returning later still fails the responsibility to ensure safe administration at the bedside.
2. Tell her that it is against the rules, and take the medication with you: While telling the patient you cannot leave meds is correct, simply taking it away without arranging a plan (e.g., returning with it at breakfast) is not patient-centered. Also sounds punitive rather than collaborative.
4. Take the drug from the room and record it as refused: The patient did not refuse - she asked to take it later. Recording a refusal would be inaccurate and could cause inappropriate follow-up actions.
Take home points
- Never leave medications unattended at the bedside; arrange a safe plan.
- Document what the patient said and your agreed plan.
An older adult states that she cannot see her medication bottles clearly to determine when to take her prescription. What actions should the nurse take to help the older adult patient? Select all that apply
Explanation
Promoting medication safety and adherence in older adults with visual impairment or literacy issues involves practical solutions include making labels and packaging accessible, using adherence aids, and confirming understanding with teach-back.
Rationale for correct answer:
1. Provide a dispensing system for each day of the week: A pill organizer or single-week dispenser reduces errors (pre-sorted doses), helps adherence, and compensates for poor label visibility.
2. Provide larger, easier-to-read labels: Enlarged print or high-contrast labels directly address the visual problem and help independence. Many pharmacies can print large-font labels.
5. Use teach-back to ensure that the patient knows what medication to take and when: Teach-back verifies understanding and helps identify gaps; it’s a best practice for safe medication management.
Rationale for incorrect answers:
3. Tell the patient what is in each container: While verbally telling the patient helps short-term, it relies on memory and is not a durable fix. It’s appropriate as an immediate, supportive measure but should be paired with lasting aids (labels, dispensers).
4. Have a family caregiver administer the medication: This may be appropriate if the patient consents and a competent caregiver is available and willing. However, it isn’t the nurse’s first default action.
Take home points
- Prioritize tools that promote independence and reduce error risk (large labels, dispensers) before relying solely on others to administer meds.
- Always confirm understanding with teach-back - don’t assume the patient understands instructions just because they nod.
Which of the following guidelines must a nurse use for taking verbal or telephone orders? Select all that apply
Explanation
To ensure safe communication and documentation when a provider gives orders by phone or in person (verbally). Because these orders bypass the usual written route, strict procedures exist to prevent errors: only authorized staff may accept them, orders must be identified, clarified, read back, and documented precisely.
Rationale for correct answers:
1. Follow the health care agency guidelines regarding authorized staff who may receive and record verbal or telephone orders: Facilities define who is permitted to accept VO/TOs to ensure qualified personnel record and implement them correctly.
2. Clearly identify patient’s name, room number, and diagnosis: Using two or more patient identifiers (name, DOB, room, etc.) prevents giving an order for the wrong patient and clarifies context for the order. Including diagnosis helps the receiver recognize potential discrepancies.
3. Read back all orders to health care provider: “Read-back” or “repeat-back” reduces misheard words/numbers and is a required safety step in most agencies.
4. Use clarification questions to avoid misunderstandings: Asking for clarification (spell drug names, confirm dose/route/frequency) prevents errors from assumptions or poor audio quality.
5. Write “VO” (verbal order) or “TO” (telephone order), including date and time, name of patient, and complete order; sign the name of the health care provider and nurse. Documentation must clearly identify the order as VO/TO, show who gave it and when, include the full order, and show who transcribed it - the nurse signs it and usually the provider must countersign within the agency’s timeframe.
Take home points
- Always follow agency policy: accept VO/TO only if you are authorized, use read-back, and document it as VO/TO with date/time and signatures.
- Clarify any unclear element (drug name, dose, route, frequency) before acting - never assume.
Which aspects of the patient’s care related to the administration of heparin can the nurse delegate to the nursing AP? Select all that apply
Explanation
Heparin is a high-risk anticoagulant, so the RN retains assessment, clinical judgment, and medication administration responsibilities. APs may perform routine observations and report abnormal findings, but they must not perform assessments or interventions that require nursing judgment.
Rationale for correct answers:
1. Notify the nurse if there are any signs of bleeding: Observing and reporting is within AP scope; they should promptly notify the nurse if they see signs (bruising, bleeding, blood in stool/urine).
4. Notify the nurse if there is blood noted in the patient’s urine: Noticing and reporting visible blood is an observational task appropriate for APs.
5. Notify the nurse if there is oozing from any puncture sites: Observing oozing and reporting it is within AP scope; the RN determines further actions (e.g., hold heparin, apply pressure, lab tests).
Rationale for incorrect answers:
2. Assess the vital signs for possible symptoms of bleeding: Because heparin is high-risk, never delegate clinical assessment, or independent evaluation of bleeding to an AP.
3.Assess bleeding sites and apply appropriate pressure to the sites: Detailed assessment of bleeding and deciding/applying clinical interventions (beyond basic first-aid) require nursing judgment.
Take-home points
- Use the Five Rights of Delegation (right task, right person, right circumstance, right direction/communication, right supervision/evaluation).
- APs can observe and report; RNs must assess, interpret, and intervene for heparin therapy.
A patient is to receive medications through a small-bore nasogastric feeding. Which nursing actions are appropriate? Select all that apply
Explanation
Administering medications through a small-bore nasogastric feeding tube requires following safety protocols to ensure correct tube placement, prevent clogging, avoid drug–formula interactions, and reduce aspiration risk. Each step must be performed in sequence to maintain patient safety and medication efficacy.
Rationale for correct answers:
3. Using an enteral tube syringe to administer medications: Large-bore (≥ 30 mL) enteral syringes reduce pressure and prevent tube rupture, and are designed for safe delivery through feeding tubes.
4. Flushing tube with 30 to 60 mL of water after the last dose of medication: This clears the tube, prevents clogging, and ensures all medication is delivered into the stomach/intestine.
5. Checking for gastric residual before giving the medications: Residual checks help ensure that the stomach is emptying properly and reduce aspiration risk; large residual volumes may require holding meds/feeds and notifying the provider.
6. Keeping the head of the bed elevated for 30 to 60 minutes after the medications are given: Elevation decreases aspiration risk and aids in gastric emptying.
Rationale for incorrect answers:
1. Verifying tube placement after medications are given: Placement should be verified before administering medications, not after, to ensure the tube is in the stomach/intestine and not misplaced in the lungs.
2. Mixing all medications together to give all at once: This increases the risk of drug interactions, clogging, and altered absorption. Each medication should be given separately, flushing with water between
Take home points:
- Always verify tube placement before giving meds and flush before and after each medication.
- Give medications separately, flush between, and keep HOB elevated post-administration to prevent aspiration.
After receiving an IM injection in the deltoid, a patient states, “My arm really hurts. It’s burning and tingling where I got my injection.” What should the nurse do next? Select all that apply
Explanation
Burning or tingling after an intramuscular injection may indicate nerve involvement, injection site injury, or inflammatory reaction. Prompt assessment and appropriate interventions prevent worsening injury and guide reporting/documentation.
Rationale for correct answers:
1. Assess the injection site: Immediate inspection and palpation help determine swelling, redness, hematoma, or nerve injury signs.
3. Notify the patient’s health care provider of assessment findings: Persistent burning/tingling could indicate nerve injury or reaction, and the provider needs to be informed for further evaluation.
4. Document assessment findings and related interventions in the patient’s medical record: Documentation is essential for continuity of care, legal record, and quality improvement.
6. Apply ice to the site for relief of burning pain: Ice can reduce inflammation and provide comfort if no contraindications exist and after assessment; however, priority is assessment and provider notification.
Rationale for incorrect answers:
2. Administer an oral medication for pain: Pain medication should not be given before assessing the site and determining the cause; masking symptoms can delay recognition of a complication.
5. This is a normal finding, so nothing needs to be done: While mild soreness is normal, burning/tingling is not routine and may signal a complication.
Take-home points:
- New burning or tingling after an IM injection is not a normal finding - assess first, then notify the provider.
- Always document findings and interventions, and apply comfort measures only after ruling out serious complications.
Exams on Medication Administration and Intravenous Therapies
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Legal Aspects Of Drug Administration
- Medication Orders
- Practice Exercise 1
- Routes Of Administration
- Oral Medications
- Sublingual And Buccal Medications
- Parenteral Medications
- Practice Exercise 2
- Topical Medications
- Administering Medications By Inhalation
- Preventing And Responding To Medication Errors
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define selected terms related to the administration of medications.
- Describe legal aspects of administering medications.
- Describe various routes of medication administration.
- Identify essential parts of a medication order.
- List examples of various types of medication orders
Introduction
Pharmacology is the study of the effect of drugs on living organisms.
Pharmacy is the art of preparing, compounding, and dispensing drugs.
A medication is a substance administered for the diagnosis, cure, treatment, or relief of a symptom or for prevention of disease.
In the health care context, the words medication and drug are generally used interchangeably.
The term drug also has the connotation of an illicitly obtained substance such as heroin, cocaine, or amphetamines.
The written direction for the preparation and administration of a drug is called a prescription.
One drug can have as many as four kinds of names: its generic name, trade name (or brand name), official name, and chemical name.
- The generic name is assigned by the United States Adopted Names (USAN) Council and is used throughout the drug’s lifetime.
- A drug’s trade name (sometimes called the brand name) is the name given by the drug manufacturer and identifies it as property of that company.
- The official name is the name under which a drug is listed in one of the official publications (e.g., the United States Pharmacopeia).
- The chemical name is the name by which a chemist knows it; this name describes the constituents of the drug precisely.
Legal Aspects Of Drug Administration
Within the United States, laws have been enacted to control the development and administration of drugs.
To function beyond the limits of nursing practice acts or one’s ability is to endanger clients’ lives and leave oneself open to professional negligence lawsuits.
Under the law, nurses are responsible for their own actions regardless of whether there is a written order. Therefore, nurses should question any order that appears unreasonable and refuse to give the medication until the order is clarified.
Another aspect of nursing practice governed by law is the use of controlled substances. Most health care agencies maintain a list of high-alert medications, including controlled substances, which require the verification of two registered nurses.
When a portion or all of a controlled substance dose is discarded, the nurse must ask a second nurse to witness the discarding. Both nurses must sign the control inventory form.
In most agencies, counts of controlled substances are taken at the end of each shift. The count total should tally with the total at the end of the last shift minus the number used. If the totals do not tally and the discrepancy cannot be resolved, it must be reported immediately to the nurse manager, nursing supervisor, and pharmacy according to agency policy.
Medication Orders
A physician usually determines the client’s medication needs and orders medications, although in some settings nurse practitioners and physician assistants now order some drugs.
4.1 Types of Medication Orders
Four types of medication orders are commonly used:
1. A stat order indicates that the medication is to be given immediately and only once (e.g., morphine sulfate 10 milligrams IV stat).
2. The single order or one-time order is for medication to be given once at a specified time (e.g., Seconal 100 milligrams at bedtime before surgery).
3. The standing order may or may not have a termination date. A standing order may be carried out indefinitely.
4. A prn order, or as-needed order, permits the nurse to give a medication when, in the nurse’s judgment, the client requires it.
4.2 Essential Parts of a Medication Order
-
Full name of the client
- Date and time the order is written
- Name of the drug to be administered
- Dosage of the drug
- Frequency of administration
- Route of administration
- Signature of the person writing the order
Parts of a Prescription
- Descriptive information about the client: name, address, and sometimes age
- Date on which the prescription was written
- The Rx symbol, meaning “take thou”
- Medication name, dosage, and strength
- Route of administration
- Dispensing instructions for the pharmacist, for example, “Dispense 30 capsules”
- Directions for administration to be given to the client, for example, “take on an empty stomach”
- Refill and/or special labeling, for example, “Refill × 1”
- Prescriber’s signature
4.3 Calculation of the correct dosage
-
When calculating dosages of oral medications, check the calculation and question the prescription if the calculation calls for more than 3 tablets.
- When calculating dosages of parenteral medications, check the calculation and question the prescription if the amount to be given is too large a dose.
- Be sure that all measures are in the same system and that all units are in the same size, converting when necessary; carefully consider what the reasonable amount of the medication that would be administered is.
- Round standard injection doses to tenths and measure in a 3-mL syringe (follow agency policy).
- Per agency policy, it may be acceptable to round down (avoid rounding up) small, critical amounts or children’s doses to hundredths and measure in a 1-mL tuberculin syringe (example: 1.752 mL can be rounded to 1.75 mL).
Nursing insights
Standard formula: DA ×Q=X
D (desired) is the dosage that the primary health care provider prescribed.
A (available) is the dosage strength as stated on the medication label.
Q (quantity) is the volume or form in which the dosage strength is available, such as tablets, capsules, or milliliters.
Intravenous flow rates:
- Monitor IV flow rate frequently even if the IV solution is being administered through an electronic infusion device.
- Whenever a prescribed IV rate is increased, the nurse needs to assess the client for increased respirations and increased lung congestion, which could indicate fluid overload.
- Intravenously administered fluids are prescribed most frequently based on milliliters per hour.
- The volume per hour prescribed is administered by setting the flow rate, which is counted in drops per minute.
Reconstitution of medications:
- In reconstituting a medication, locate the instructions on the label or in the vial package insert, and read and follow the directions carefully.
- Instructions will state the volume of diluent to be used and the resulting volume of the reconstituted medication.
- Often, the powdered medication adds volume to the solution in addition to the amount of diluent added.
- The total volume of the prepared solution will exceed the volume of the diluent added.
- When reconstituting a multiple-dose vial, label the medication vial with the date and time of preparation, your initials, and the date of expiration.
- Indicating the strength per volume on the medication label also is important.
Routes Of Administration
Pharmaceutical preparations are generally designed for one or two specific routes of administration.
Include:
- Oral
- Sublingual
- Buccal
- Parenteral:
- Subcutaneous (hypodermic)—into the subcutaneous tissue, just below the skin
- Intramuscular (IM)—into a muscle
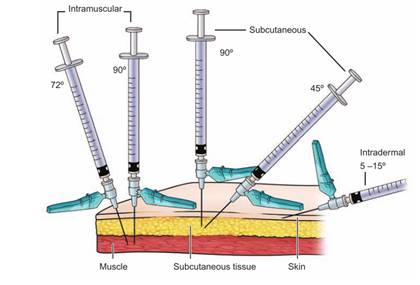
- Intradermal (ID)—under the epidermis (into the dermis)
- Intravenous (IV)—into a vein.
- Topical
Oral Medications
The oral route is the most common route by which medications are given. As long as a client can swallow and retain the drug in the stomach, this is the route of choice.
Oral medications are contraindicated when a client is vomiting, has gastric or intestinal suction, or is unconscious and unable to swallow.
SKILL: Administering oral medications
- Complete necessary assessments before administering medications. Check the patient’s allergy bracelet or ask the patient about allergies. Explain the purpose and action of each medication to the patient.
- Assist the patient to an upright or lateral position.
- Administer medications:
- Offer water or other permitted fluids with pills, capsules, tablets, and some liquid medications.
- Ask whether the patient prefers to take the medications by hand or in a cup.
- Remain with the patient until each medication is swallowed. Never leave medication at the patient’s bedside.
- Assist the patient to a comfortable position. Remove PPE, if used. Perform hand hygiene.
- Document the administration of the medication immediately after administration.
- Evaluate patient’s response to medication within appropriate time frame
SKILL: Administering Medications by Nasogastric or Gastrostomy Tube
Always check with the pharmacist to see if the client’s medications come in a liquid form because these are less likely to cause tube obstruction.
If medications do not come in liquid form, check to see if they may be crushed.
Sterile water is recommended for use in adult and neonatal/pediatric clients before and after medication administration.
Assess tube placement prior to administration of medications.
Before giving the medication, aspirate all the stomach contents and measure the residual volume. Check agency policy if residual volume is greater than 100 mL.
When administering the medication(s):
- Remove the plunger from the syringe and connect the syringe to a pinched or kinked tube. Pinching or kinking the tube prevents excess air from entering the stomach and causing distention.
- Put 15 to 30 mL (5 to 10 mL for children) of sterile water into the syringe barrel to flush the tube before administering the first medication.
- Raise or lower the barrel of the syringe to adjust the flow as needed.
- Pinch or clamp the tubing before all the water is instilled to avoid excess air entering the stomach.
- Pour liquid or dissolved medication into the syringe barrel and allow to flow by gravity into the enteral tube.
- If you are giving several medications, administer each one separately and flush with at least 15 to 30 mL (5 mL for children) of tap water between each medication.
- When you have finished administering all medications, flush with another 15 to 30 mL (5 to 10 mL for children) of warm water to clear the tube.
Sublingual And Buccal Medications
Certain drugs, such as nitroglycerin, are administered sublingually; that is, a tablet is placed under the patient’s tongue.
Another method is to administer the medication between the cheek and gum, known as buccal administration.
These areas are rich in superficial blood vessels, which allow the drug to be absorbed relatively rapidly into the bloodstream for quick systemic effects.
Sublingual and buccal medications should not be swallowed, but rather held in place so that complete absorption can occur.
Before administering a sublingual or buccal drug, offer the patient a drink of water (if the patient is permitted to have fluids) or oral care (if the patient is NPO). This ensures that the tablet will dissolve appropriately.
Parenteral Medications
Nurses give parenteral medications intradermally (ID), subcutaneously, intramuscularly (IM), or intravenously (IV).
Because these medications are absorbed more quickly than oral medications and are irretrievable once injected, the nurse must prepare and administer them carefully and accurately.
EQUIPMENT
Syringes:
Syringes have three parts:
- the tip, which connects with the needle
- the barrel, or outside part, on which the scales are printed
- plunger, which fits inside the barrel
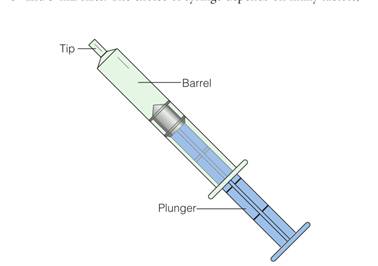
The choice of syringe depends on many factors, such as medication, location of injection, and type of tissue.
Syringes range in sizes from 1 to 60 mL.
Syringes ranging from 1 to 3 mL may have two scales marked on them: the minim and the milliliter. The milliliter scale is the one normally used; the minim scale is used for very small dosages.
The larger sized syringes (e.g., 10, 20, and 50 mL) are not used to administer drugs directly but can be useful for adding medications to IV solutions or for irrigating wounds.
- A hypodermic syringe comes in 3- and 5-mL sizes.
- An insulin syringe is similar to a hypodermic syringe, but the scale is specially designed for insulin: a 100-unit calibrated scale intended for use with U-100 insulin
- The tuberculin syringe was originally designed to administer tuberculin solution. It is a narrow syringe, calibrated in tenths and hundredths of a milliliter (up to 1 mL) on one scale and in sixteenths of a minim (up to 1 minim) on the other scale.
The tip of a syringe varies and is classified as either a LuerLok or non–Luer-Lok.
- A Luer-Lok syringe has a tip that requires the needle to be twisted onto it to avoid accidental removal of the needle
- The non–Luer-Lok syringe has a smooth graduated tip, and needles are slipped onto it.
Needles:
Needles are made of stainless steel, and most are disposable.
Reusable needles (e.g., for special procedures) need to be sharpened periodically before resterilization because the points become dull with use and are occasionally damaged or acquire burrs on the tips.
A needle has three discernible parts: the hub, which fits onto the syringe; the cannula, or shaft, which is attached to the hub; and the bevel, which is the slanted part at the tip of the needle.
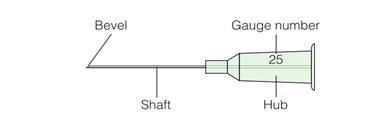
Needles used for injections have three variable characteristics:
- Slant/ length of the bevel:
- Longer bevels provide the sharpest needles and cause less discomfort. They are commonly used for subcutaneous and intramuscular injections.
- Short bevels are used for intradermal and IV injections because a long bevel can become occluded if it rests against the side of a blood vessel.
- Length of the shaft: The shaft length of commonly used needles varies from 1/2 to 2 inches.
- Gauge/ diameter of the shaft: The gauge varies from #18 to #30. The larger the gauge number, the smaller the diameter.
PREVENTING NEEDLESTICK INJURIES
Needlestick injuries present a major risk for infection with hepatitis B virus, human immunodeficiency virus (HIV), and many other pathogens.
Use appropriate puncture-proof disposal containers to dispose of uncapped needles and sharps.
Never bend or break needles before disposal.
Never recap used needles.
When recapping a needle (i.e., drawing up a medication into a syringe prior to administration):
- Use a safety mechanical device that firmly grips the needle cap and holds it in place until it is ready to recap
- Use a one-handed “scoop” method. This is performed by (a) placing the needle cap and syringe with needle horizontally on a flat surface, (b) inserting the needle into the cap, using one hand and then (c) using your other hand to pick up the cap and tighten it to the needle hub.

6.3.1 INTRADERMAL INJECTION
SKILL: Administering an Intradermal Injection
Equipment: Sterile syringe, usually a tuberculin syringe calibrated in tenths and hundredths, and needle, 1⁄4” to 1⁄2”, 26 or 27-gauge, antimicrobial swab, disposable gloves, small gauze square
- Select an appropriate administration site. Assist the patient to the appropriate position for the site chosen. Drape as needed to expose only area of site to be used.
- Cleanse the site with an antimicrobial swab while wiping with a firm, circular motion and moving outward from the injection site. Allow the skin to dry.
- Remove the needle cap with the nondominant hand by pulling it straight off.
- Use the nondominant hand to spread the skin taut over the injection site.
- Hold the syringe in the dominant hand, between the thumb and forefinger with the bevel of the needle up.
- Using the dominant hand allows for easy, appropriate handling of syringe. Having the bevel up allows for smooth piercing of the skin and introduction of medication into the dermis.
- Hold the syringe at a 5- to 15- degree angle from the site. Place the needle almost flat against the patient’s skin, bevel side up, and insert the needle into the skin. Insert the needle only about 1/8” under the skin,
- Once the needle is in place, steady the lower end of the syringe. Slide your dominant hand to the end of the plunger.
- Slowly inject the agent while watching for a small wheal or blister to appear.
- Withdraw the needle quickly at the same angle that it was inserted. Do not recap the used needle. Engage the safety shield or needle guard.
- Do not massage the area after removing needle. Tell patient not to rub or scratch the site. If necessary, gently blot the site with a dry gauze square. Do not apply pressure or rub the site.
6.3.2 SUBCUTANEOUS INJECTION
Subcutaneous injections are administered into the adipose tissue layer just below the epidermis and dermis.
This tissue has few blood vessels, so drugs administered here have a slow, sustained rate of absorption into the capillaries. This route is used to administer drugs such as insulin and heparin.
Various sites may be used for subcutaneous injections, including the outer aspect of the upper arm, the abdomen (from below the costal margin to the iliac crests), the anterior aspects of the thigh, the upper back, and the upper ventral or dorsogluteal area.
Equipment: A 25- to 30-gauge, 3/8” to 1”needle can be used. The 3/8” and 5/8” needles are most commonly used. Usually, no more than 1 mL of solution is given subcutaneously.
SKILL: Administering a Subcutaneous Injection
Equipment: Sterile syringe and needle. Needle size depends on the medication administered and patient body type. Antimicrobial swab, Disposable gloves, Small gauze square
- Cleanse the area around the injection site with an antimicrobial swab. Use a firm, circular motion while moving outward from the injection site. Allow area to dry.
- Remove the needle cap with the nondominant hand, pulling it straight off.
- Grasp and bunch the area surrounding the injection site or spread the skin taut at the site.
- Hold the syringe in the dominant hand between the thumb and forefinger. Inject the needle quickly at a 45- to 90degree angle.
- After the needle is in place, release the tissue. If you have a large skin fold pinched up, ensure that the needle stays in place as the skin is released. Immediately move your nondominant hand to steady the lower end of the syringe. Slide your dominant hand to the end of the plunger. Avoid moving the syringe.
- Inject the medication slowly (at a rate of 10 seconds per milliliter).
- Withdraw the needle quickly at the same angle at which it was inserted, while supporting the surrounding tissue with your nondominant hand.
- Using a gauze square, apply gentle pressure to the site after the needle is withdrawn. Do not massage the site.
- Do not recap the used needle. Engage the safety shield or needle guard. Discard the needle and syringe in the appropriate receptacle.
- Document the administration of the medication immediately after administration.
- Evaluate the response of the patient to the medication within an appropriate time frame for the particular medication.

6.3.3 INTRAMUSCULAR INJECTION
Intramuscular injections deliver medication through the skin and subcutaneous tissues into certain muscles.
Muscles have larger and a greater number of blood vessels than does subcutaneous tissue, allowing faster onset of action than with subcutaneous injections.
Consider the age of the patient, medication type, and medication volume when selecting a site for intramuscular injection.
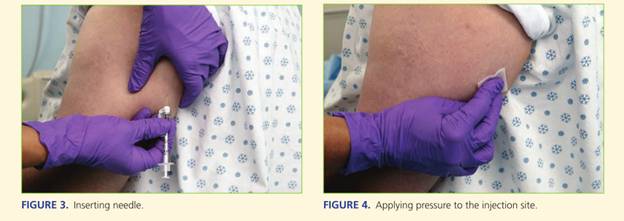
SKILL: Administering an Intramuscular Injection
- Identify the appropriate landmarks for the site chosen.
- Cleanse the area around the injection site with an antimicrobial swab. Use a firm, circular motion while moving outward from the injection site. Allow area to dry.
- Remove the needle cap by pulling it straight off. Hold the syringe in your dominant hand between the thumb and forefinger.
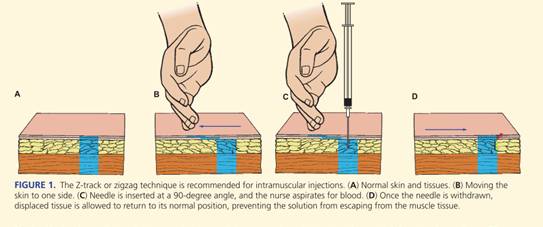
- Displace the skin in a Z-track manner by pulling the skin down or to one side about 1” (2.5 cm) with your nondominant hand and hold the skin and tissue in this position.
- Quickly dart the needle into the tissue so that the needle is perpendicular to the patient’s body. This should ensure that it is given using an angle of injection between 72 and 90 degrees.
- As soon as the needle is in place, use the thumb and forefinger of your nondominant hand to hold the lower end of the syringe. Slide your dominant hand to the end of the plunger. Inject the solution slowly (10 seconds per milliliter of medication).
- Once the medication has been instilled, wait 10 seconds before withdrawing the needle.
- Withdraw the needle smoothly and steadily at the same angle at which it was inserted, supporting tissue around the injection site with your nondominant hand.
- Apply gentle pressure at the site with a dry gauze. Do not massage the site.
6.3.4 INTRAVENOUS ADMINISTRATION
SKILL: Administering Medications by Intravenous Bolus or Push Through an Intravenous Infusion
- Complete necessary assessments before administering medications. Check the patient’s allergy bracelet or ask the patient about allergies. Explain the purpose and action of the medication to the patient.
- Scan the patient’s bar code on the identification band, if required.
- Assess IV site for presence of inflammation or infiltration.
- If IV infusion is being administered via an infusion pump, pause the pump.
- Put on clean gloves.
- Select injection port on tubing that is closest to venipuncture site. Clean port with antimicrobial swab.
- Uncap syringe. Steady port with your nondominant hand while inserting syringe into center of port.
- Move your nondominant hand to the section of IV tubing just above the injection port. Fold the tubing between your fingers.
- Pull back slightly on plunger just until blood appears in tubing.
- Inject the medication at the recommended rate
- Release the tubing. Remove the syringe. Do not recap the used needle, if used. Discard the needle and syringe in the appropriate receptacle.
- Check IV fluid infusion rate. Restart infusion pump, if appropriate.
- Evaluate patient’s response to medication within appropriate time frame.
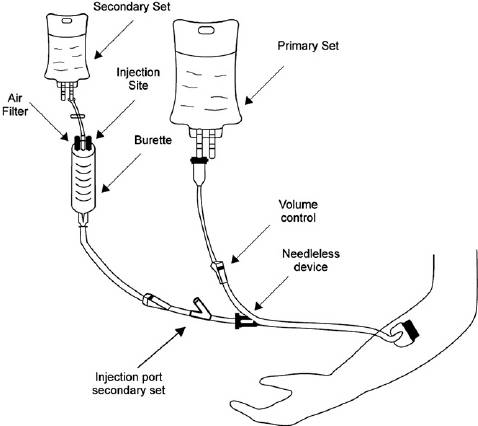
SKILL: Administering a Piggyback Intermittent Intravenous Infusion of Medication
- Complete necessary assessments before administering medications. Check the patient’s allergy bracelet or ask the patient about allergies. Explain the purpose and action of the medication to the patient.
- Scan the patient’s bar code on the identification band, if required.
- Assess the IV site for the presence of inflammation or infiltration.
- Close the clamp on the short secondary infusion tubing. Using aseptic technique, remove the cap on the tubing spike and the cap on the port of the medication container, taking care to avoid contaminating either end.
- Attach infusion tubing to the medication container by inserting the tubing spike into the port with a firm push and twisting motion, taking care to avoid contaminating either end.
- Hang piggyback container on IV pole, positioning it higher than primary IV according to manufacturer’s recommendations. Use metal or plastic hook to lower primary IV fluid container.
- Place label on tubing with appropriate date.
- Squeeze drip chamber on tubing and release. Fill to the line or about half full. Open clamp and prime tubing. Close clamp. Place needleless connector on the end of the tubing, using sterile technique, if required.
- Use an antimicrobial swab to clean the access port or stopcock above the roller clamp on the primary IV infusion tubing.
- Connect piggyback setup to the access port or stopcock. If using, turn the stopcock to the open position.
- Open clamp on the secondary tubing. Set rate for secondary infusion on infusion pump and begin infusion. If using gravity infusion, use the roller clamp on the primary infusion tubing to regulate flow at prescribed delivery rate. Monitor medication infusion at periodic intervals.
- Clamp tubing on piggyback set when solution is infused. Follow facility policy regarding disposal of equipment.
- Replace primary IV fluid container to original height. Check primary infusion rate on infusion pump. If using gravity infusion, readjust flow rate of primary IV.
- Remove PPE, if used. Perform hand hygiene.
- Document.
- Evaluate the patient’s response.
Topical Medications
Medications delivered via the topical route are applied to the skin or mucous membranes, including the eyes, ears, nose, rectum, vagina, and lungs.
Topical applications are usually intended for direct action at a particular site, although some can have systemic effects and are given for systemic effect.
6.5.1 SKIN APPLICATIONS
When a drug is incorporated in an agent such as an ointment and rubbed into the skin for absorption, the procedure is referred to as an inunction.
On normal skin, drugs are absorbed into the lining of the sebaceous glands.
The following are typical preparations applied to skin areas:
- Powders are used to promote drying of the skin and prevent friction on the skin.
- Ointments provide prolonged contact of a medication with the skin and soften the skin.
- Creams and oils lubricate and soften the skin and prevent drying of the skin.
- Lotions protect and soothe the skin
- Transdermal delivery systems utilize reservoirs, micro reservoirs, adhesives, or matrices. The drug layer of the system contains drug, with a rate-controlling layer to slow the release of the drug over time, ending with an adhesive layer to enhance the attachment of the system to the patient’s skin. Are commonly used to deliver hormones, narcotic analgesics, cardiac medications, and nicotine.
SKILL: APPLYING TRANSDERMAL PATCHES
- Perform hand hygiene.
- Identify the patient.
- Explain procedure to patient.
- Put on gloves.
- Assess patient’s skin where patch is to be placed, looking for any signs of irritation or breakdown. Site should be clean, dry, and free of hair. Rotate application sites.
- Remove the old patch before applying the new one. Fold patch in half with adhesive sides sticking together and discard according to facility policy.
- Gently wash the area where the old patch was with soap and water.
- Remove the patch from its protective covering. Write your initials and the date and time of administration on the label side of the patch.
- Remove the covering without touching the medication surface. Apply the patch to the patient’s skin. Use the palm of your hand to press firmly for about 10 seconds. Do not massage.
- Remove gloves and perform hand hygiene.
- Apply the patch at the same time of the day, according to the order and medication specifications.
- Document site of application on the MAR.
- Evaluate patient’s response to medication within appropriate time frame.
- Check for dislodgement of the patch if the patient is active. Read information about the patch or consult with the prescriber or pharmacist to determine reapplication schedule and procedure.
- Assess for any skin irritation at application site. If necessary, remove the patch, wash the area carefully with soap and water, and allow skin to air dry. Apply a new patch at a different site. Assess the potential for adverse reaction.
- Aluminum backing on a patch necessitates precautions if defibrillation is required. Burns and smoke may result.
6.5.2 EYE INSTILLATIONS AND IRRIGATIONS
Because direct application cannot be made onto the sensitive cornea, applications intended to act on the eye or the lids are placed onto, or instilled or irrigated into, the lower conjunctival sac.
- EYEDROPS
Eyedrops are instilled for their local effects, such as for pupil dilation or constriction when examining the eye, for treating an infection, or for controlling intraocular pressure in patients with glaucoma
SKILL: INSTILLING EYE DROPS
- Perform hand hygiene.
- Identify the patient.
- Explain procedure to patient.
- Put on gloves.
- Offer the patient paper tissues to remove solution and tears that may spill from the eye during the procedure.
- Clean the eyelids and eyelashes of any drainage with cotton balls or gauze squares moistened with normal saline solution. Debris can be carried into the eye when the conjunctival sac is exposed. Use each area of the cleaning surface once, moving from the inner toward the outer canthus to prevent carrying debris to the lacrimal ducts.
- Tilt the patient’s head back slightly if sitting, or place the patient’s head over a pillow if lying down. The head may be turned slightly to the affected side to prevent solution or tears from flowing toward the opposite eye.
- Remove the cap from the medication bottle, being careful not to touch the inner side of the cap.
- Invert the monodrip plastic container that is commonly used to instill eyedrops.
- Have the patient look up while focusing on something on the ceiling.
- Place the thumb or two fingers near the margin of the lower eyelid immediately below the eyelashes, and exert pressure downward over the bony prominence of the cheek. The lower conjunctival sac is exposed as the lower lid is pulled down.
- Hold the dropper close to the eye but avoid touching the eyelids or lashes. Touching the eye, eyelids, or lashes can contaminate the medication in the bottle; startle the patient, causing blinking; or injure the eye.
- Squeeze the container and allow the prescribed number of drops to fall in the lower conjunctival sac. Do not allow medication to fall onto cornea. This may injure the cornea or cause the patient to have an unpleasant sensation.
- Release the lower lid after the eyedrops are instilled. Ask the patient to close the eyes gently.
- Apply gentle pressure with your gloved finger over the inner canthus to prevent the eyedrops from flowing into the tear duct. This minimizes the risk of systemic effects from the medication.
- Instruct the patient not to rub the affected eye.
- Remove gloves and perform hand hygiene.
- Chart the administration of medication on the MAR after the drops have been administered.
- Evaluate the patient’s response to the medication within the appropriate time frame.
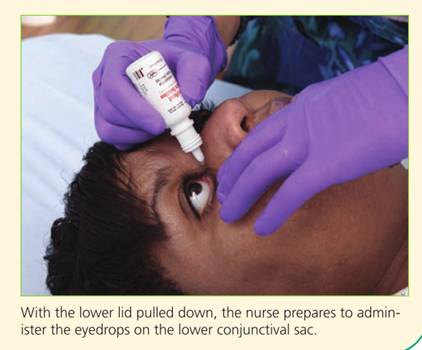
- EYE IRRIGATION
Eye irrigation is performed to remove secretions or foreign bodies or to cleanse and soothe the eye. In an emergency, eye irrigation can be used to remove chemicals that may burn the eye.
The irrigation should continue for at least 15 minutes, and then professional help should be sought.
SKILL: PERFORMING AN IRRIGATION OF THE EYE
- Warm the solution to be instilled to body temperature to minimize discomfort for the patient.
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Position the patient, sitting or lying, with head tilted toward side of affected eye. Protect patient and bed with a waterproof pad.
- Put on gloves.
- Clean the patient’s eye with a moistened washcloth, wiping from the inner canthus to outer canthus. Use a different part of the washcloth for each stroke.
- Place curved basin at cheek on side of affected eye to receive irrigating solution.
- Fill irrigation syringe with prescribed solution.
- Gently pull down on lower eyelid to expose conjunctival sac. Hold upper lid open.
- Hold syringe about 1 inch from eye. Direct flow of solution from inner to outer canthus along conjunctival sac. Avoid touching any part of the eye with the syringe.
- Pause irrigation periodically. Have patient close eye for a moment. Irrigate until solution is clear or all solution has been used.
- Dry periorbital area after irrigation.
- Remove gloves and perform hand hygiene.
- Evaluate the patient’s response to the procedure.
- Document the administration of irrigation on the MAR. Document the procedure, assessments, and patient response.
6.5.3 EAR INSTILLATIONS AND IRRIGATIONS
Drugs or irrigations are instilled into the auditory canal for their local effect.
They are used to soften wax, relieve pain, apply local anesthesia, destroy organisms, or destroy an insect lodged in the canal, which can cause almost intolerable discomfort.
- EAR DROPS
SKILL: INSTILLING EAR DROPS
- Warm the solution to be instilled to body temperature to minimize discomfort for the patient.
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Put on gloves.
- Offer a tissue to the patient.
- Clean the external ear of drainage with cotton balls moistened with normal saline solution, as necessary.
- Place the patient on the unaffected side in bed, or if ambulatory, have the patient sit with the head well tilted to the side so that the affected ear is uppermost. This positioning prevents the drops from escaping from the ear.
- Draw up the amount of solution needed in the dropper. Excess medication should not be returned to a stock bottle. A monodrip plastic container may also be used.
- Straighten the auditory canal by pulling the cartilaginous portion of the pinna up and back in an adult , straight back for a school-aged child, and down and back in an infant or a child under age 3 years. Pulling on the pinna as described helps to straighten the canal properly for ear instillation.
- Hold the dropper in the ear with its tip above the auditory canal. For an infant or an irrational or restless patient, protect the dropper with a piece of soft tubing to help prevent injury to the ear.
- Allow the drops to fall on the side of the canal. It is uncomfortable for the patient if drops fall directly onto the tympanic membrane.
- Release the pinna after instilling the drops, and have the patient maintain the position to prevent the medication from escaping.
- Gently press on the tragus a few times to help move the medication from the canal toward the tympanic membrane.
- If ordered, loosely insert a cotton ball to prevent medication from leaking out.
- Wait 5 minutes before instilling drops in the second ear, if ordered.
- Remove gloves and perform hand hygiene.
- Document the medication administration on the MAR. Document the procedure, assessments, and patient response.
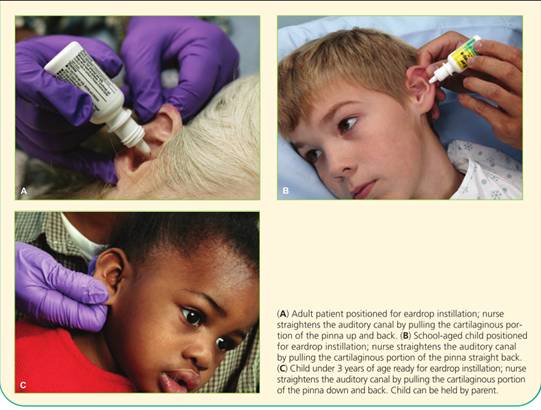
- IRRIGATION OF THE EAR
Irrigations of the external auditory canal are ordinarily done for cleaning purposes or for applying heat to the area.
To prevent pain, the irrigation solution should be at least at room temperature.
SKILL: IRRIGATING THE EAR
- Warm the solution to be instilled to body temperature to minimize discomfort for the patient.
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Put on gloves.
- Position patient, sitting or lying, with head tilted toward side of affected ear. Protect patient and bed with waterproof pad. Position basin under ear to receive irrigating solution.
- Clean pinna and meatus of auditory canal as necessary with cotton-tipped applicators moistened with tap water.
- Fill syringe with warm solution. If irrigating container is used, prime the tubing.
- Straighten auditory canal by pulling cartilaginous portion of pinna up and back for an adult.
- Direct a steady, slow stream of solution against the roof of the auditory canal, using only enough force to remove secretions. Do not occlude the auditory canal with the irrigating nozzle. Allow solution to flow out unimpeded.
- When irrigation is complete, place cotton ball loosely in auditory meatus. Position patient on the same side as the affected ear, with towel or absorbent pad under ear.
- Remove gloves and perform hand hygiene.
- Document the medication administration on the MAR. Document the procedure, assessments, and patient response.
- Evaluate the patient’s response. Remove cotton ball after 10 to 15 minutes, or per order. Assess drainage.
6.5.4 NASAL INSTILLATIONS
Nasal instillations are used to treat allergies, sinus infections, and nasal congestion. Medications with a systemic effect, such as vasopressin, may also be prepared as a nasal instillation.
SKILL: INSTILLING NOSE DROPS
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Put on gloves.
- Provide the patient with paper tissues and ask that the patient blow his or her nose before instilling the nose drops.
- Have the patient sit up with head tilted well back. If the patient is lying down, tilt the head back over a pillow. These positions allow the solution to flow well back into the naris.
- Draw sufficient solution into the dropper for both nares. Excess solution should not be returned to a stock bottle.
- Hold up the tip of the nose and place the dropper just inside the naris about one third of an inch without touching the nare. Instill the prescribed number of drops in one naris and then into the other. Protect the dropper with a piece of soft tubing if the patient is an infant or young child. Touching the nares with the dropper may cause the patient to sneeze and contaminate the dropper.
- Have the patient remain in position with the head tilted back for a few minutes to prevent the solution from escaping.
- Remove gloves and perform hand hygiene.
- Document the medication administration on the MAR. Document the procedure, assessments, and patient response.
6.5.5 VAGINAL APPLICATIONS
Creams, foams, and tablets can be applied intravaginally using a narrow, tubular applicator with an attached plunger. Suppositories that melt when exposed to body heat are also administered by vaginal insertion.
SKILL: INSERTING VAGINAL SUPPOSITORY OR CREAM
-
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Put on gloves.
- Fill a vaginal applicator with the prescribed amount of cream, or have a suppository ready.
- Introduce the applicator gently in a rolling manner while directing it downward and backward to follow the normal contour of the vagina for its full length. Push the plunger to its full length, and then gently remove the applicator with the plunger depressed. Insert a suppository with gloved fingers well into the vagina.
- Lubricate the applicator with water, as necessary. A suppository may be lubricated with a water-soluble gel.
- Ask patient to void before inserting medication.
- Use lithotomy position and provide draping.
- Spread the labia well with the fingers, and clean the area at the vaginal orifice with a washcloth and warm water to remove discharge. Use a different corner of the washcloth with each stroke, moving downward.
- Introduce the applicator gently in a rolling manner while directing it downward and backward to follow the normal contour of the vagina for its full length. Push the plunger to its full length, and then gently remove the applicator with the plunger depressed. Insert a suppository with gloved fingers well into the vagina.
- Ask the patient to remain in the supine position for 5 to 10 minutes after insertion.
- Offer the patient a perineal pad to collect excess drainage.
- Remove gloves and perform hand hygiene.
- Document the medication administration on the MAR. Document the procedure, assessments, and patient response.
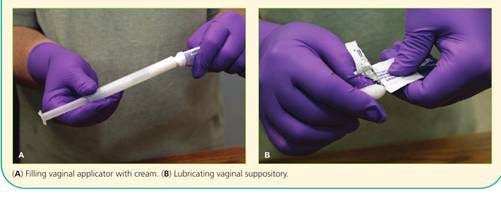
6.5.6 RECTAL INSTILLATIONS
Rectal suppositories are used primarily for their local action, such as laxatives and fecal softeners. Systemic effects are also achieved with rectal suppositories.
SKILL: INSERTING A RECTAL SUPPOSITORY
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Put on gloves.
- Assist the patient to his left side in a Sims position. Drape accordingly to expose only the buttocks.
- Remove the suppository from its wrapper. Apply lubricant to the rounded end. Lubricate the index finger of your dominant hand.
- Separate the buttocks with your nondominant hand and instruct the patient to breathe slowly and deeply through the mouth while the suppository is being inserted.
- Using your index finger, insert the suppository, round end first, along the rectal wall. Insert about 3 to 4 inches.
- Use toilet tissue to clean any stool or lubricant from around the anus. Release the buttocks. Encourage the patient to remain on his side for at least 5 minutes and retain the suppository for the appropriate amount of time for the specific medication.
- Remove gloves and perform hand hygiene.
- Document the medication administration on the MAR. Document the procedure, assessments, and patient response.
Administering Medications By Inhalation
Drugs for inhalation are aerosolized, delivered in small particles, and breathed in by the patient.
The lungs are supplied richly with blood and have a large surface area. These characteristics allow drugs to be absorbed easily from the lower respiratory tract.
Drugs for inhalation may be administered by a hand atomizer or a nebulizer. These devices break up the medication into a mist for more efficient inhalation.
SKILL: USING THE SMALL-VOLUME NEBULIZER
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Remove the nebulizer cup from the device, open it, and place it on a flat working surface.
- Place premeasured unit dose medication in the bottom section of the cup or use a dropper to place concentrated dose of medication in cup and add prescribed fluid to dilute it.
- Screw the top portion of nebulizer cup back in place and attach the cup to the nebulizer.
- Attach one end of tubing to the stem on the bottom of the nebulizer cuff and the other end to the air compressor or oxygen source (if valve to control airflow is not available, a Y tube can be added to the tubing so that one branch of the Y tube connects to the nebulizer cup and the other branch is left open).
- Turn on the air compressor or oxygen.
- Check that a fine medication mist is produced by opening valve or placing thumb over open branch of Y tube.
- Place mouthpiece into mouth and grasp securely with teeth and lips.
- Inhale slowly through the mouth (a nose clip may be necessary if patient is also breathing through the nose).
- Hold each breath for 5 to 10 seconds or as long as possible before exhaling.
- Continue this inhalation technique until all medication in the nebulizer cup has been aerosolized (usually about 15 minutes).
- If desired, gargle with tap water after using nebulizer.
- Rinse the equipment in warm water and allow to air dry on a clean towel.
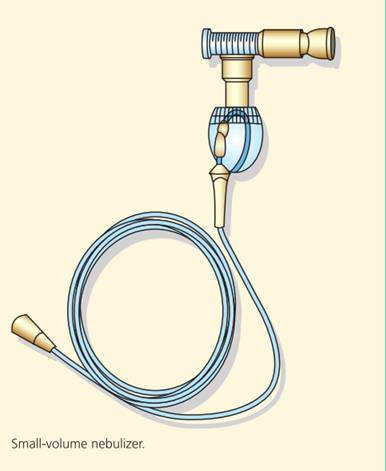
SKILL: USING THE METERED-DOSE INHALER
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Remove the mouthpiece cover and shake inhaler well.
- Follow caregiver’s or manufacturer’s recommendations for placement of the mouthpiece. Two methods are possible:
- Hold the inhaler 1 to 2 inches in front of open mouth; or
- Place mouthpiece into mouth grasping securely with teeth and lips (an MDI coupled with a spacer or extender is always placed in the mouth).
- Take a deep breath and exhale.
- Inhale slowly and deeply through the mouth. Press down on the medication canister while continuing to inhale a full breath (when using a spacer or extender, depress the canister about one fourth or one third through the inspiration).
- Hold your breath for 5 to 10 seconds or as long as possible.
- Exhale slowly through pursed lips.
- If another puff is prescribed, wait 1 to 5 minutes before the next inhalation.
- If desired, gargle with tap water and blow nose into a tissue to remove any remaining trace of medication. If MDI is a steroid, this must be done to prevent oral fungal infection.
- Use mild soap and water to clean the mouthpiece, rinse it, and let it dry before replacing it.
- Follow physician’s order regarding frequency of inhaler use.
SKILL: USING THE DRY POWDER INHALER (DPI)
- Understand the specific instructions for your DPI.
- Perform hand hygiene.
- Identify the patient.
- Explain the procedure to the patient.
- Remove the cap and load a dose if necessary.
- Seal your lips around the mouthpiece.
- Do not block the opening with your tongue or teeth.
- Breathe in quickly and deeply, over 2 to 3 seconds.
- Remove the DPI from your mouth.
- Hold your breath for 5 to 10 seconds, or as long as possible.
- If a second dose is necessary, wait 1 to 5 minutes.
- Rinse your mouth or brush your teeth after using.
- Never exhale into the mouthpiece.
- If mist can be seen from the mouth or nose, the DPI is being used incorrectly.
- Keep the cap in place to prevent dirt from entering the DPI.
- Follow the manufacturer’s directions to clean the DPI.
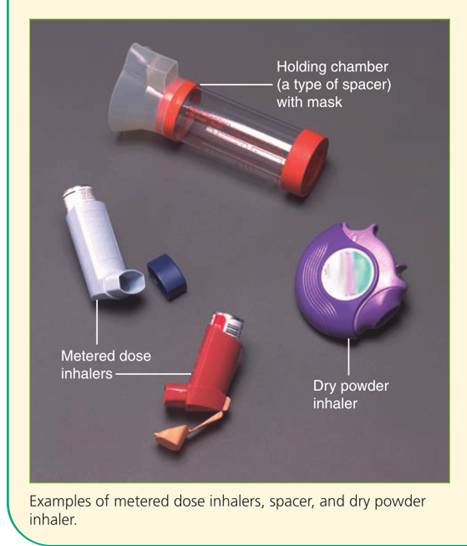
Preventing And Responding To Medication Errors
Nurses should take every precaution to avoid errors when administering therapeutic agents.
Common types of medication errors include the following:
-
- Inappropriate prescribing of the drug (e.g., incorrect dose, quantity, or route, or inadequate instruction)
- Extra, omitted, or wrong doses
- Administration of a medication to a patient that was not ordered for him or her.
- Administration of a drug by an incorrect route or at an incorrect rate
- Failure to give a medication within the prescribed time interval
- Incorrect preparation of a drug before administration
- Improper technique when administering a drug
- Giving a drug that has deteriorated
Nursing insights
Medication errors occur most often at points of transition in care: on admission to a hospital, at transfer from one department to another, and at discharge home or to another facility.
The principal cause of medication error at these times is the incorrect or incomplete transfer of medication information.
7.1 THE TEN RIGHTS OF MEDICATION ADMINISTRATION
RIGHT MEDICATION
The medication given was the medication ordered.
RIGHT DOSE
- The dose ordered is appropriate for the client.
- Give special attention if the calculation indicates multiple pills/ tablets or a large quantity of a liquid medication. This can be an indication that the math calculation may be incorrect.
- Double-check calculations that appear questionable.
- Know the usual dosage range of the medication.
- Question a dose outside of the usual dosage range.
RIGHT TIME
- Give the medication at the right frequency and at the time ordered according to agency policy.
- Medications should be given within the agency guidelines.
RIGHT ROUTE
- Give the medication by the ordered route.
- Make certain that the route is safe and appropriate for the client.
RIGHT CLIENT
- Medication is given to the intended client.
- Check the client’s identification band with each administration of a medication.
- Know the agency’s name alert procedure when clients with the same or similar last names are on the nursing unit.
RIGHT CLIENT EDUCATION
Explain information about the medication to the client (e.g., why receiving, what to expect, any precautions).
RIGHT DOCUMENTATION
- Document medication administration after giving it, not before.
- If time of administration differs from prescribed time, note the time on the MAR and explain the reason and follow-through activities (e.g., pharmacy states medication will be available in 2 hours) in nursing notes.
- If a medication is not given, follow the agency’s policy for documenting the r eason why.
RIGHT TO REFUSE
- Adult clients have the right to refuse any medication.
- The nurse’s role is to ensure that the client is fully informed of the potential consequences of refusal and to communicate the client’s refusal to the health care provider.
RIGHT ASSESSMENT
- Some medications require specific assessments prior to administration (e.g., apical pulse, blood pr essure, lab results).
- Medication orders may include specific parameters for administration (e.g., do not give if pulse less than 60 or systolic blood pressure less than 100).
RIGHT EVALUATION
Conduct appropriate follow-up (e.g., was the desired effect achieved or not? Did the client experience any side effects or adverse reactions?)

The following steps are recommended when a medication error occurs:
1. Check the patient’s condition immediately when the error is noted. Observe for the development of adverse effects related to the error.
2. Notify the nurse manager and the primary care provider to discuss possible courses of action, depending on the patient’s condition.
3. Write a description of the error on the patient’s medical record, including remedial steps that are taken.
4. Complete the form used for reporting errors, as dictated by facility policy. These forms, called special event, event, or unusual occurrence reports, require an objective, complete account of the medication error. Include the steps taken after the error was recognized. For legal reasons, describe the error fully and accurately. Medication errors are a common allegation in nursing liability cases. Do not document in the patient’s record the fact that an incident report was filed.
7.2 TEACHING ABOUT MEDICATIONS AND ABUSE
|
Health Topic |
Teaching Tip |
Why Is This Important? |
|
General information |
Medication name and dosage • Intended effects of medication • Expected adverse effects of medication |
Patients should know the names and reasons for medications in case of medical emergencies. Patients should also know expected adverse effects of the medication so they do not stop taking the medication. |
|
Taking the medication |
Medications should be taken at the same time every day. • Teach whether food, beverages, or other medications have any effect on the medication. • Teach what patient should do if a dose is missed. • Teach patient to take medications as prescribed for as long as prescribed. • Teach not to alter drug dosage without consulting healthcare provider. |
If patients make taking medications a part of their daily routine, they are less likely to miss a dose. Some medications require food to prevent stomach irritation; absorption of other medications is impeded by food in the stomach. Patients are likely to miss a dose of medication and need to know what to do if this happens. Some medications have severe consequences if stopped abruptly; others need to be taken for a set period of time and at a recommended dosage to be effective. |
|
Special instructions |
Teach what to do when adverse effects occur. • Keep medications with them when traveling. • Do not share medications with other people. • Proper storage • Keep a list of all medications, including OTC drugs, dietary supplements, herbs, and natural supplements. |
Patients need to know whom to contact if any adverse effects occur. Luggage can be lost or misplaced. Teach patients that just because someone else has similar symptoms, it does not mean that the same medication should be taken. Medication should be kept out of the reach of children and pets. For labeling purposes, medications should be kept in the container in which they were dispensed. Some medications are sensitive to humidity and light; keep medications in a cool, dry place. Keep your healthcare providers up to date about your list. |
Summary
- Medications have several names. Nurses need to know the generic and trade names of a medication and be aware of both its therapeutic and side effects.
- Federal drug legislation regulates the production, prescription, distribution, and administration of drugs.
- Nurse practice acts define limits on the nurse’s responsibilities regarding medications.
- Various routes are used to administer medications: oral, sublingual, buccal, parenteral, topical, or via a nasogastric or gastrostomy tube. When administering a medication, the nurse must ensure that it is appropriate for the route specified.
- Medication orders must include the client name; date and time the order is written; name of the medication; dosage, frequency, and route of administration; and signature of the ordering primary care provider or nurse. Nurses must question any unclear orders before implementing the order.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Medication Administration and Intravenous Therapies
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


