Please set your exam date
Placenta Previa
Study Questions
Practice Exercise 1
A nurse is caring for a 32-year-old client at 34 weeks gestation presenting with painless, bright red vaginal bleeding. Which of the following is the most likely diagnosis?
Explanation
Placenta previa involves the abnormal implantation of the placenta in the lower uterine segment, partially or completely covering the internal cervical os. This condition manifests as sudden, painless vaginal bleeding during the third trimester as the cervix begins to efface and dilate. The lack of abdominal tenderness and the bright red nature of the blood are pathognomonic clinical features distinguishing it from other obstetric hemorrhages. Diagnosis is primarily confirmed via transvaginal ultrasonography, and digital vaginal examinations are strictly contraindicated to prevent catastrophic exsanguination.
Rationale for correct answers
The client's presentation of painless, bright red bleeding at 34 weeks gestation is the hallmark of placenta previa. As the lower uterine segment thins, placental attachment is disrupted, leading to maternal vascular bleeding. Because the blood escapes directly through the cervix, it remains bright red and does not cause uterine irritability or pain. This diagnosis is consistent with the absence of abdominal rigidity or maternal distress in early stages.
Rationale for incorrect answers
Abruptio placentae is the premature separation of a normally implanted placenta from the uterine wall. It typically presents with painful bleeding, uterine tenderness, and increased uterine resting tone. The blood is often dark red or concealed behind the placenta, causing a board-like abdomen. Unlike the painless nature of this client's bleeding, abruption is characterized by significant abdominal or back pain.
Uterine rupture is a catastrophic event involving a full-thickness tear of the uterine wall, most common in clients with previous scarring. Clinical signs include sudden, sharp abdominal pain, cessation of uterine contractions, and recession of the presenting part. While bleeding occurs, it is accompanied by profound maternal shock and fetal distress. The client's painless bleeding without a history of trauma or sudden abdominal pain makes this unlikely.
Vasa previa occurs when fetal vessels cross the internal os unprotected by the placenta or umbilical cord. While it presents with painless vaginal bleeding, it typically occurs immediately following the rupture of membranes. The bleeding is fetal in origin, leading to rapid fetal bradycardia and death even with minimal blood loss. Since this client is presenting with bleeding but no mention of membrane rupture or fetal distress, previa is more likely.
Test-taking strategy
- Analyze the Clinical Markers: Identify the two most critical descriptors in the stem, which are painless and bright red bleeding. These specific adjectives are used to differentiate between the various causes of third-trimester hemorrhage.
- Differentiate Pathophysiology: Compare the choices based on the presence of pain. Eliminate 1 and 3 because abruption and rupture are characterized by intense abdominal pain and uterine tenderness.
- Evaluate Timing and Context: Distinguish between 2 and 4 by looking for triggers. Eliminate 4 because vasa previa is typically associated with the sudden onset of bleeding at the time of amniotomy or spontaneous rupture of membranes, whereas placenta previa occurs spontaneously.
- Confirm the Diagnosis: Select the option that perfectly matches the classic triad of late-pregnancy bleeding: third trimester, painless, and bright red. This leads directly to the selection of placenta previa.
Take home points
- Placenta previa is characterized by painless, bright red vaginal bleeding in the third trimester due to placental location over the cervical os.
- Abruptio placentae must be differentiated by the presence of dark red blood, uterine hypertonicity, and significant abdominal pain.
- Digital vaginal examinations are strictly prohibited in any client presenting with third-trimester bleeding until placenta previa is ruled out by ultrasound.
- The primary maternal risk is hemorrhage, while the fetal risk is related to prematurity and potential hypoxia from maternal hypotension.
A nurse is assessing a client with suspected placenta previa. Which of the following assessment actions is contraindicated?
Explanation
Placenta previa occurs when the placenta implants over the internal cervical os, creating a high risk for maternal hemorrhage. During the third trimester, the lower uterine segment undergoes physiologic thinning and stretching, which can disrupt the placental attachment and shear the delicate vessels. This results in the classic presentation of painless vaginal bleeding, which can quickly escalate into life-threatening maternal exsanguination and fetal hypoxia. Because the placental tissue is positioned directly over the birth canal, any mechanical trauma to the cervix must be strictly avoided to prevent catastrophic bleeding.
Rationale for correct answers
A digital vaginal examination is strictly contraindicated because inserting fingers into the cervix can puncture the placenta previa or cause immediate, massive detachment. This mechanical disruption of the vascular bed can lead to rapid maternal shock and fetal death within minutes. Diagnosis must always be confirmed by transvaginal ultrasound before any pelvic manipulation is considered. Any manipulation of the cervical canal is avoided until the placental location is verified as being safe.
Rationale for incorrect answers
Monitoring the fetal heart rate is a mandatory assessment to evaluate fetal well-being and the impact of maternal blood loss on placental perfusion. Placenta previa increases the risk of fetal hypoxia if maternal hypotension occurs due to hemorrhage. Continuous or frequent intermittent monitoring provides essential data regarding the oxygenation status of the fetus. This action is non-invasive and does not pose a risk of mechanical trauma to the placental site.
Assessing maternal vital signs every 15 minutes is a critical component of hemodynamic monitoring in a client with active or suspected obstetric hemorrhage. Tachycardia and hypotension are late signs of hypovolemic shock in pregnant women due to their increased blood volume. Frequent assessment allows the nursing team to intervene early with fluid resuscitation or blood products. This is a standard safety protocol for any client presenting with third-trimester vaginal bleeding.
Quantifying vaginal bleeding by weighing peripads is the most accurate method for determining the volume of blood loss in an obstetric setting. One gram of pad weight is roughly equivalent to one milliliter of blood, providing an objective measurement of the severity of the hemorrhage. This assessment is essential for calculating the cumulative blood loss and guiding the intensity of the medical intervention. It is a non-invasive procedure that provides vital clinical information without disturbing the placenta.
Test-taking strategy
- Identify the Contraindication: The question asks for an action that is contraindicated, meaning it is harmful or dangerous given the suspected diagnosis of placenta previa.
- Prioritize Safety and Risk Reduction: Evaluate each choice based on its potential to cause physical harm to the client. Monitoring (1), vital signs (3), and weighing pads (4) are all observational and non-invasive.
- Apply Pathophysiology Knowledge: Recall that in placenta previa, the placenta is located over the cervical opening. Any action that involves entering the cervix (2) will directly contact the placental tissue.
- Rule out Non-Invasive Actions: Choices 1, 3, and 4 are standard nursing interventions for obstetric stabilization. Only Choice 2 involves a procedure that can physically disrupt the placental attachment, making it the clear nursing priority to avoid.
Take home points
- Digital vaginal examinations are strictly prohibited in the presence of third-trimester bleeding until placenta previa is ruled out by ultrasound.
- The primary goal of management is maintaining maternal hemodynamic stability and ensuring adequate fetal oxygenation.
- Placenta previa is characterized by painless, bright red bleeding, whereas abruptio placentae involves painful, dark red bleeding.
- Inaccurate estimation of blood loss can lead to delayed treatment of hypovolemic shock; weighing pads is the gold standard for quantification.
A client diagnosed with placenta previa is experiencing mild vaginal bleeding at 32 weeks gestation. What is the most appropriate initial nursing intervention?
Explanation
Placenta previa management prioritizes hemodynamic stability and fetal maturation when the bleeding is not life-threatening. During the third trimester, the primary goal for a preterm fetus is expectant management to prolong the pregnancy until 36 to 37 weeks gestation. This approach involves strict bed rest, continuous monitoring for increased hemorrhage, and the potential administration of antenatal corticosteroids to accelerate fetal lung development. By maintaining a quiet environment and ensuring venous access, the medical team prepares for sudden maternal status changes while avoiding the complications of iatrogenic prematurity.
Rationale for correct answers
The initial nursing action for mild bleeding is to establish intravenous access and initiate expectant management. Maintaining a patent 18-gauge catheter ensures the nurse can rapidly administer fluids or blood if hemorrhage suddenly escalates. Expectant management is appropriate at 32 weeks gestation to allow for further fetal development, provided both the mother and fetus remain stable. This conservative approach balances the risk of prematurity against the risk of maternal blood loss.
Rationale for incorrect answers
Immediate cesarean section is indicated only if there is active hemorrhage, maternal instability, or signs of non-reassuring fetal status. At 32 weeks, an immediate delivery increases the risk of neonatal respiratory distress and other complications of prematurity. Since the bleeding is described as mild and no maternal or fetal distress is noted, conservative management is preferred over surgical intervention.
Encouraging ambulation is contraindicated in a client with active or suspected placenta previa. Physical activity can increase the risk of further placental separation and exacerbate vaginal bleeding due to gravity and cervical pressure. Clients are traditionally placed on modified bed rest to minimize uterine activity and prevent mechanical disruption of the low-lying placental site.
While tocolytics are sometimes used to stop preterm labor, they are not the initial intervention for placenta previa bleeding. The primary concern is potential hypovolemic shock from blood loss, which requires immediate venous access for fluid resuscitation. Tocolytics may mask signs of abruptio placentae or cause maternal tachycardia, which complicates the assessment of the client's hemodynamic status.
Test-taking strategy
- Identify the Urgency: The stem describes the bleeding as mild and the gestation as 32 weeks, which is significantly preterm. This indicates that the situation is currently stable, favoring a conservative rather than an emergent approach.
- Prioritize the Nursing Process: Use the "Assess and Prepare" principle. Establishing IV access (3) is a foundational safety step for any client with potential for hemorrhage. It provides the means for intervention without committing to an immediate, risky delivery.
- Eliminate Unsafe Options: Rule out ambulation (2) because it increases the risk of bleeding. Eliminate immediate surgery (1) because it is too aggressive for mild bleeding in a preterm fetus.
- Evaluate Choice 4: While managing contractions is part of care, it is secondary to establishing a lifeline for fluids and monitoring the primary problem, which is the placental bleeding.
Take home points
- Expectant management is the standard of care for stable placenta previa when the fetus is less than 36 weeks gestation.
- Large-bore IV access is a critical safety intervention for any client at risk for sudden obstetric hemorrhage.
- Bed rest and avoidance of vaginal exams are mandatory to prevent the exacerbation of placental bleeding.
- Delivery is indicated regardless of gestational age if maternal hemorrhage is uncontrollable or fetal distress is present.
A nurse is educating a client with placenta previa. Which of the following instructions should the nurse include? Select all that apply
Explanation
Placenta previa occurs when the placenta covers the internal cervical os, creating a significant risk for maternal hemorrhage as the lower uterine segment prepares for labor. Management of this condition focuses on preventing mechanical trauma and minimizing activities that could induce uterine contractions or cervical changes. Because the placenta is positioned directly over the birth canal, even minor cervical irritation can lead to life-threatening exsanguination, necessitating a high level of vigilance and strict adherence to a modified lifestyle. The primary goal is to maintain the pregnancy until fetal lung maturity is achieved, typically aiming for a scheduled cesarean delivery.
Rationale for correct answers
Any manual or instrumental entry into the vagina is contraindicated because it can cause placental abruption or direct trauma to the placental vessels. Digital examinations can trigger massive hemorrhage, placing both the mother and the fetus in immediate danger of death. Clients must be taught to refuse pelvic exams in any healthcare setting unless the placental location has been confirmed to be safe by recent ultrasound.
Bright red bleeding indicates active maternal hemorrhage from the placental site and requires immediate clinical evaluation to ensure hemodynamic stability. Early detection of bleeding allows for the timely administration of intravenous fluids or blood products to prevent hypovolemic shock. Clients must understand that even small amounts of blood can precede a catastrophic bleeding event, making rapid reporting a life-saving priority.
Pelvic rest, which includes the avoidance of sexual intercourse and douching, prevents cervical stimulation and mechanical trauma to the low-lying placenta. Avoiding heavy lifting reduces intra-abdominal pressure, which could otherwise stress the lower uterine segment and provoke bleeding or preterm labor. These restrictions are essential for maintaining the integrity of the placental attachment throughout the remainder of the third trimester.
Rationale for incorrect answers
Strenuous exercise is strictly prohibited because it increases uterine blood flow and can stimulate uterine contractions, leading to placental separation. High-impact activities or heavy physical exertion can cause mechanical shearing at the site of the placenta previa, triggering a major bleeding episode. Clients are instead encouraged to maintain modified bed rest or limited non-strenuous activity to reduce the risk of maternal and fetal complications.
Iron supplements are actually encouraged for clients with placenta previa to optimize hemoglobin levels in preparation for potential blood loss during delivery. Maintaining a high iron intake helps build a hematologic reserve, reducing the severity of anemia if a hemorrhage occurs. While all medications should be discussed with a provider, iron is a standard prophylactic intervention rather than something to be avoided or limited under restrictive guidance.
Test-taking strategy
- Identify the Goal: The question asks for appropriate instructions for a client with placenta previa, focusing on safety and the prevention of maternal hemorrhage.
- Apply the Safety First Principle: Evaluate each choice based on whether it protects the cervical area from trauma. Choices 1 and 3 directly prevent physical contact or stress on the placenta.
- Prioritize Early Detection: Recognize that bright red bleeding (2) is a hallmark sign of emergency in this diagnosis, making immediate reporting a critical educational point.
- Use the Process of Elimination: Rule out Choice 4, as strenuous exercise is dangerous in high-risk pregnancies. Rule out Choice 5 because iron is generally beneficial and expected for clients at risk for blood loss.
- Select Multiple Options: In a "Select all that apply" format, ensure each chosen answer (1, 2, 3) independently supports the goal of pregnancy maintenance and risk reduction.
Take home points
- Pelvic rest is mandatory for placenta previa to avoid mechanical disruption of the placenta by intercourse or vaginal exams.
- Any new onset of vaginal bleeding must be treated as a potential emergency due to the risk of rapid maternal exsanguination.
- Strenuous physical activity is contraindicated as it can trigger uterine irritability and placental shearing at the cervical os.
- Education must emphasize that a cesarean section is the required mode of delivery for complete or partial placenta previa.
A nurse reviews an ultrasound report stating “placenta fully covering the internal cervical os.” This finding is consistent with which type of placenta previa?
Explanation
Complete placenta previa represents the most severe anatomical classification of this condition, where the placental tissue totally occludes the internal cervical os. This configuration prevents a vaginal delivery because the fetus cannot exit the uterus without causing massive placental detachment and life-threatening maternal hemorrhage. The diagnosis is typically established via transvaginal ultrasonography, which provides the necessary resolution to measure the exact distance between the placental edge and the cervical opening. In a complete previa, the central portion of the placenta is often positioned directly over the os, making exsanguination a critical risk during even minor cervical effacement.
Rationale for correct answers
The description of the placenta "completely covering" the internal os is the definitive diagnostic criterion for complete previa. This means there is no portion of the cervical opening that remains unobstructed by placental tissue. Because the os is entirely blocked, any amount of cervical dilation will result in the shearing of placental vessels, leading to the classic symptom of painless, bright red bleeding. This finding necessitates a scheduled cesarean delivery to ensure the safety of both the mother and the neonate.
Rationale for incorrect answers
Marginal previa occurs when the edge of the placenta is located at the margin of the os, but does not actually cover it. The placental edge is typically within 2 cm of the internal cervical os but does not cross the cervical threshold. While it still carries a risk of bleeding during labor, it is not characterized by "completely covering" the opening. In some cases, a vaginal delivery may be attempted with marginal previa if the bleeding remains minimal.
Partial previa involves the placenta partially covering the internal cervical os, rather than a total occlusion. This means that a portion of the cervical opening is still free of placental tissue at the time of the ultrasound. While clinically similar to complete previa in terms of risk, it does not match the specific "completely covering" language used in the ultrasound report. The management remains high-risk, usually requiring a cesarean section as the cervix dilates.
A low-lying placenta is defined as a placenta implanted in the lower uterine segment but whose edge is more than 2 cm away from the internal os. This is the least severe form of abnormal placental positioning and often migrates upward as the uterus grows throughout the second and third trimesters. It does not cover the os at all, and therefore, it does not fit the description provided in the client's diagnostic report.
Test-taking strategy
- Identify the Key Phrase: Focus on the specific wording of the report: "completely covering." This phrase is a technical descriptor that links directly to the medical classification of the condition.
- Use Medical Terminology: Match the word "completely" in the stem with the choice "Complete Previa" (3). In medical coding and diagnostic reporting, the terminology is literal regarding the degree of occlusion.
- Differentiate by Degree: Rank the options from least to most obstructive: Low-lying (4) is > 2 cm away, Marginal (1) is at the edge, Partial (2) covers some, and Complete (3) covers all.
- Eliminate Based on Definition: Rule out 1 and 4 immediately as they do not involve covering the os. Rule out 2 because "partial" implies a remaining gap, which contradicts the "complete" finding in the ultrasound report.
Take home points
- Complete placenta previa is a total obstruction of the internal cervical os by placental tissue, necessitating surgical delivery.
- Ultrasound findings of placental location are the primary factor in determining the safety of a vaginal delivery trial.
- Placental migration may occur in low-lying or marginal cases, but complete previa in the third trimester rarely resolves.
- The degree of cervical coverage by the placenta is directly proportional to the risk of significant antepartum hemorrhage.
Practice Exercise 2
A nurse is caring for a client at 34 weeks gestation presenting with painless, bright red vaginal bleeding. Which of the following is the most likely pathophysiological cause?
Explanation
Placenta previa involves blastocyst implantation within the lower uterine segment, leading to placental development over the internal cervical os. This malpositioning subjects the low-lying, fragile vascular network to mechanical shearing forces during cervical effacement or lower segment thinning, resulting in characteristic painless hemorrhage. Unlike other obstetric hemorrhages, this bleeding is primarily maternal in origin and occurs without the stimulus of uterine contractions or trauma, often requiring careful hemodynamic monitoring.
Rationale for correct answer
2. The most likely pathophysiological cause for painless, bright red bleeding in the third trimester is the disruption of placental vessels at the internal os. As the lower uterine segment thins near 34 weeks, the vascular implantation is stretched, causing small tears in the maternal sinuses. This allows for the escape of oxygenated blood, which appears bright red and remains painless. This mechanism is specific to placenta previa where the placenta occupies the distensible lower segment.
Rationale for incorrect answers
1. Separation of the placenta from the uterine wall describes abruptio placentae, which is characterized by painful, often dark red vaginal bleeding and uterine tenderness. This pathophysiology involves the rupture of maternal spiral arteries in the decidua basalis, leading to hematoma formation and compression of the placenta. Because this process causes significant uterine irritability and myometrial hypoxia, the patient experiences intense pain, which is absent in this clinical scenario.
3. Uterine fibroid degeneration, particularly carneous degeneration, occurs when a leiomyoma outgrows its blood supply, typically causing localized abdominal pain and low-grade fever. While fibroids can complicate pregnancy and increase the risk of malpresentation, they do not typically present with sudden, profuse bright red vaginal bleeding. The pain associated with degeneration is usually sharp and constant, contrasting with the painless nature of the bleeding described in the question stem.
4. Cervical insufficiency involves the premature, painless dilation of the cervix, usually occurring in the second trimester rather than at 34 weeks gestation. While it can cause light spotting or mucoid discharge, it is primarily associated with fetal membrane prolapse and subsequent preterm birth rather than significant bright red hemorrhage. The pathophysiology involves structural weakness of the cervical stroma, which is a distinct mechanism from the vascular bleeding observed in placenta previa.
Test-taking strategy
- Identify the Landmark Findings: Focus on the classic triad of 34 weeks gestation, painless bleeding, and bright red color. These descriptors are the gold standard for identifying placenta previa in nursing exams.
- Differentiate by Pain: Use the presence or absence of pain as the primary branching point in your logic. Eliminate 1 (Abruptio) and 3 (Fibroids) because they are typically painful conditions.
- Analyze Vascularity versus Structure: Compare 2 and 4. Choice 2 addresses the vascular nature of the bleeding, which matches the description of "bright red" blood. Choice 4 is a structural failure of the cervix that rarely causes frank hemorrhage.
- Match Pathophysiology to Anatomy: Recognize that lower uterine segment changes are the specific trigger for bleeding in placenta previa. This makes Choice 2 the most scientifically accurate explanation for the stem.
Take home points
- Placenta previa is characterized by painless, bright red vaginal bleeding caused by the stretching of the lower uterine segment.
- Abruptio placentae must be differentiated by its hallmark of painful, dark red bleeding and uterine rigidity.
- The presence of bright red blood indicates that the bleeding is fresh and has not been trapped behind the placenta.
- Medical management focuses on maintaining hemodynamic stability and avoiding any manual cervical stimulation.
A client with placenta previa experiences acute vaginal bleeding. Which maternal hemodynamic change should the nurse monitor most closely?
Explanation
Placenta previa results in maternal hemorrhage when the lower uterine segment thins, disrupting the placental-decidual interface. This blood loss triggers a compensatory sympathetic response designed to maintain perfusion to vital organs despite a decreasing intravascular volume. In the early stages of hypovolemic shock, the body increases heart rate to maintain cardiac output, while blood pressure may remain stable due to peripheral vasoconstriction. However, as blood loss exceeds 30% of total volume, these compensatory mechanisms fail, leading to significant hemodynamic instability and potential multi-organ failure if not rapidly corrected.
Rationale for correct answer
2. The nurse must monitor for tachycardia and hypotension as these are the hallmark signs of hypovolemic shock resulting from acute hemorrhage. Tachycardia occurs as a sympathetic reflex to maintain cardiac output in the face of reduced stroke volume. Hypotension is a later sign indicating that the compensatory mechanisms can no longer maintain mean arterial pressure. In a pregnant client, these signs are critical because the diverted blood flow away from the uterus causes immediate fetal hypoxia.
Rationale for incorrect answers
1. Bradycardia and hypertension are components of Cushing's triad, which is associated with increased intracranial pressure rather than acute obstetric hemorrhage. In the context of maternal bleeding, the heart rate increases rather than decreases to compensate for volume loss. Hypertension is inconsistent with blood loss, as intravascular depletion leads to a drop in systemic vascular resistance and pressure. These findings would suggest a neurological emergency rather than the circulatory collapse expected in placenta previa.
3. Hyperthermia and tachypnea are more indicative of an infectious process like chorioamnionitis or a pulmonary embolism rather than simple hypovolemia. While tachypnea (rapid breathing) can occur during shock to compensate for metabolic acidosis, hyperthermia is not a standard response to acute blood loss. In fact, severe hemorrhage often leads to hypothermia as the body loses the ability to thermoregulate. Therefore, these combined signs do not represent the primary hemodynamic profile of a bleeding placenta previa.
4. Hypoglycemia and bradycardia are not typical physiological responses to acute maternal hemorrhage in the third trimester. While a stressed body may eventually exhaust glucose stores, hypoglycemia is not a primary monitoring parameter for acute bleeding. Bradycardia in the mother during a hemorrhage is a terminal sign of impending cardiac arrest, not an early hemodynamic change. The body's natural response to reduced preload is to increase the heart rate via the baroreceptor reflex.
Test-taking strategy
- Identify the Core Problem: The question asks about acute vaginal bleeding, which is a form of hemorrhage leading to hypovolemia.
- Apply ABCs (Circulation): Focus on the circulatory system. Hemorrhage causes a decrease in blood volume, which directly impacts heart rate and blood pressure.
- Recognize Compensation: Recall that the body's first response to low volume is to speed up (tachycardia) and then eventually fall down (hypotension). This makes Choice 2 the only logical physiological progression.
- Eliminate Outliers: Rule out Choice 1 because hypertension contradicts blood loss. Rule out Choice 3 because fever is not a sign of bleeding. Rule out Choice 4 because bradycardia is the opposite of the expected compensatory response.
Take home points
- Tachycardia is often the earliest sign of maternal hypovolemia because pregnancy-related blood volume expansion masks early blood loss.
- Hypotension in a pregnant client is a late and ominous sign, indicating a loss of at least 1500 mL of blood.
- Maternal vital signs should be assessed every 5 to 15 minutes during an active bleeding episode to guide fluid resuscitation.
- Fetal tachycardia or late decelerations often precede maternal blood pressure drops, as blood is shunted away from the placenta.
A nurse is providing care for a client with placenta previa. Which of the following are appropriate nursing interventions? Select all that apply
Explanation
Placenta previa occurs when the placenta attaches to the lower uterine segment, necessitating a management plan focused on preventing mechanical trauma and maintaining hemodynamic stability. The vascular integrity of the placental site is highly compromised as the cervix begins to efface, making the client susceptible to sudden, massive hemorrhage. Nursing care centers on fetal surveillance, monitoring for maternal blood loss, and maintaining readiness for emergency surgical intervention. Strict adherence to safety protocols is mandatory to prevent iatrogenic complications such as accidental placental perforation or delayed response to hypovolemic shock.
Rationale for correct answers
1. Performing a digital vaginal examination is strictly contraindicated as it can cause placental perforation or trigger immediate, life-threatening hemorrhage. Mechanical disruption of the vascular bed located over the cervical os can lead to rapid maternal exsanguination and fetal death. The nurse must ensure that no pelvic exams are performed until ultrasound confirms the placental position is safe. This intervention protects the anatomical integrity of the placenta.
2. Continuous fetal heart rate monitoring is essential to assess fetal oxygenation and detect early signs of placental insufficiency. Maternal blood loss can lead to decreased intervillous perfusion, manifesting as fetal tachycardia or late decelerations. Monitoring allows the nurse to identify fetal distress immediately, which is a primary indication for shifting from expectant management to emergency delivery. This provides a continuous data stream regarding the status of the fetus.
4. Maintaining large-bore IV access (18-gauge or larger) is critical for the rapid administration of intravenous fluids or blood products. In the event of an acute bleed, the client can lose a significant volume of blood in minutes, requiring volume resuscitation to prevent shock. Having a patent, large-diameter line ensures that hemodynamic stability can be supported without delay during a crisis. This is a foundational safety measure for all high-risk obstetric clients.
5. Preparing for a possible cesarean delivery is a standard part of the nursing plan because vaginal delivery is physically obstructed and dangerous in placenta previa. The nurse must ensure that the client is NPO, surgical consents are discussed, and laboratory work like type and cross-match is updated. Readiness for surgery reduces the decision-to-incision time, which is vital if maternal hemorrhage or fetal compromise occurs. This anticipates the most likely mode of delivery.
Rationale for incorrect answers
3. Encouraging ambulation is incorrect because physical activity and gravity can increase the pressure on the cervical os, potentially triggering or worsening vaginal bleeding. Clients with placenta previa are typically placed on modified bed rest to minimize uterine activity and reduce the risk of placental shearing. Movement can exacerbate vascular disruption at the low-lying placental site, whereas rest helps maintain the stability of the attachment. Ambulation is avoided until the client has been bleed-free for a significant period.
Test-taking strategy
- Identify the Diagnosis: The core condition is placenta previa, which means the placenta is over the birth canal.
- Prioritize Safety: Evaluate each choice for its impact on bleeding risk. Choice 1 and 3 are about physical safety. Avoiding exams (1) is safe; ambulation (3) is dangerous.
- Apply Emergency Preparedness: In a condition with high hemorrhage risk, the nurse must be ready to resuscitate and deliver. This confirms the need for IV access (4) and surgical prep (5).
- Monitor the Most Vulnerable: The fetus depends entirely on maternal blood flow. Continuous fetal monitoring (2) is the only way to track fetal response to maternal bleeding.
- Select All That Apply: Check each remaining option against the standard of care. Options 1, 2, 4, and 5 all align with the goal of maternal-fetal safety and emergency readiness.
Take home points
- Digital vaginal examinations are the most dangerous intervention to perform on a client with placenta previa.
- Maternal hemodynamic stability must be supported by maintaining large-bore intravenous access for rapid fluid replacement.
- Continuous electronic fetal monitoring is the gold standard for assessing fetal tolerance of maternal hemorrhagic episodes.
- Cesarean section is the mandatory route of delivery for complete placenta previa to avoid catastrophic placental detachment.
A nurse is explaining to a client why placenta previa can cause fetal hypoxia. Which of the following statements is correct?
Explanation
Placenta previa induces fetal hypoxia through the mechanism of placental hypoperfusion secondary to maternal volume depletion. During a hemorrhagic event, the maternal body initiates a compensatory shunting response, diverting blood flow away from the uteroplacental unit to preserve perfusion to the maternal brain and heart. This reduction in the intervillous space blood flow directly limits the amount of oxygen available for diffusion across the placental membrane to the fetal circulation. Because the fetus has limited oxygen reserves, prolonged or severe maternal hemorrhage can lead to progressive metabolic acidosis and potential intrauterine fetal demise if the circulatory volume is not rapidly restored.
Rationale for correct answer
1. Maternal blood loss is the primary driver of fetal hypoxia in placenta previa because it reduces the effective circulating volume required to perfuse the placenta. When maternal blood pressure drops, the pressure gradient necessary for oxygen diffusion across the chorionic villi is compromised. This results in a direct decrease in fetal oxygen saturation, often manifested as late decelerations on the electronic fetal monitor. Ensuring maternal hemodynamic stability is therefore the most critical factor in maintaining fetal oxygenation.
Rationale for incorrect answers
2. While a fetal heart rate increase (tachycardia) is a compensatory response to hypoxia, it does not increase oxygen extraction from the maternal blood. Instead, fetal tachycardia represents an attempt to increase cardiac output to circulate the limited oxygen already present in the fetal system more rapidly. Eventually, if the hypoxia is not relieved, the fetal heart will exhaust its glycogen stores, leading to bradycardia and circulatory collapse. This is a symptom of the problem rather than a corrective mechanism for oxygen delivery.
3. Placental implantation in the fundus is actually the normal anatomical location for a placenta and does not restrict blood flow. In placenta previa, the problem is specifically that the placenta is implanted in the lower uterine segment, not the fundus. Implantation in the fundus provides the most stable and vascular environment for fetal growth and is the ideal position to avoid the shearing forces that cause bleeding. Therefore, this statement is anatomically incorrect regarding the pathophysiology of placenta previa.
4. Uterine contractions do not improve placental perfusion; they actually temporarily decrease it by compressing the intramyometrial vessels. During a contraction, the flow of oxygenated maternal blood into the intervillous space is restricted or completely halted until the uterus relaxes. In a client with placenta previa, contractions are particularly dangerous because they cause cervical effacement, which leads to further placental separation and increased bleeding. Effective placental perfusion occurs only during the periods of uterine relaxation between contractions.
Test-taking strategy
- Focus on Cause and Effect: The question asks why the condition causes fetal hypoxia. Look for the answer that links maternal status to fetal oxygen supply.
- Apply Pathophysiology: Recognize that the fetus is entirely dependent on the maternal cardiovascular system. If the mother loses blood (1), the "supply chain" to the fetus is broken.
- Eliminate Anatomical Errors: Rule out Choice 3 immediately because it describes a normal placenta, not a previa.
- Understand Uterine Dynamics: Use the knowledge that contractions (4) are generally stressors to fetal oxygenation, not improvers, especially in the context of a bleeding placenta.
- Evaluate Fetal Response: Identify that Choice 2 describes a reaction to hypoxia, not the "how" or "why" the hypoxia started in the first place.
Take home points
- Fetal hypoxia in placenta previa is a direct result of reduced maternal blood volume and subsequent placental hypoperfusion.
- The maternal body prioritizes its own vital organs over the uterus during a hemorrhage, leading to rapid fetal distress.
- A soft, non-tender uterus is expected in previa; the presence of contractions increases the risk of further hemorrhage.
- Maintaining a maternal Mean Arterial Pressure (MAP) > 65 mmHg is essential for ensuring adequate oxygen delivery to the fetus.
A nurse is assessing a client with placenta previa. Which of the following maternal and fetal complications should the nurse anticipate? Select all that apply
Explanation
Placenta previa places the maternal-fetal unit at high risk for significant morbidity due to the vascular vulnerability of the lower uterine segment. When the placenta is implanted over the cervix, the structural changes of the third trimester induce shearing forces that disrupt maternal-fetal gas exchange and maternal circulatory integrity. These disruptions often necessitate iatrogenic preterm delivery to prevent fetal demise or maternal exsanguination. Furthermore, massive hemorrhage can trigger a systemic inflammatory response and the exhaustion of clotting factors, leading to secondary hemostatic failure and multi-organ dysfunction.
Rationale for correct answers
1. Hypovolemic shock is a primary maternal complication resulting from the profuse hemorrhage that can occur when placental vessels are torn. As the mother loses blood volume, the compensatory tachycardia eventually fails to maintain cardiac output, leading to hypotension and decreased tissue perfusion. This is a life-threatening emergency that requires immediate volume resuscitation with crystalloids and blood products to prevent maternal death. The nurse must monitor for signs of end-organ hypoperfusion such as oliguria or altered mental status.
2. Preterm birth is a frequent complication of placenta previa because emergency delivery is often required to save the mother or fetus during a major bleeding episode. Even if the bleeding is controlled, many providers opt for a scheduled cesarean at 36 or 37 weeks to avoid the risks of spontaneous labor. This increases the neonate's risk for respiratory distress syndrome and other complications associated with prematurity. The timing of delivery is a delicate balance between fetal maturity and maternal safety.
3. Disseminated intravascular coagulation (DIC) is a serious secondary complication triggered by abrupt blood loss and the release of thromboplastin from the injured placental site. The widespread activation of the clotting cascade depletes fibrinogen, platelets, and other coagulation factors, leading to paradoxical systemic bleeding. In the context of placenta previa, DIC typically follows a massive hemorrhagic event, resulting in oozing from IV sites, gums, and the surgical incision. The nurse must monitor the fibrinogen levels and prothrombin time closely.
Rationale for incorrect answers
4. Fetal macrosomia, defined as a birth weight > 4000 grams, is not a complication associated with placenta previa. In fact, placenta previa is more likely to be associated with intrauterine growth restriction (IUGR) due to the suboptimal blood supply available in the lower uterine segment compared to the fundus. Macrosomia is typically linked to gestational diabetes or maternal obesity rather than abnormal placental implantation. The focus in previa is on fetal size related to prematurity and potential hypoxia rather than excessive growth.
5. Uterine rupture is a catastrophic tearing of the uterine wall, most commonly occurring at the site of a previous scar from a cesarean or myomectomy. While placenta previa is a risk factor for placenta accreta, which can complicate surgery, the implantation itself does not typically cause the uterus to rupture spontaneously. Uterine rupture is characterized by sudden, tearing pain and the recession of the fetal presenting part, whereas placenta previa presents with painless bleeding. The pathophysiology of these two emergencies is distinct and requires different clinical management.
Test-taking strategy
- Identify the Core Risks: Analyze the diagnosis of placenta previa and identify its two main threats: hemorrhage and obstruction of the birth canal.
- Connect Hemorrhage to Systemic Effects: Ask what happens to the mother after a massive bleed. This leads directly to hypovolemic shock (1) and DIC (3) due to clotting factor depletion.
- Evaluate Fetal Outcome: Consider the management of a bleeding placenta at 34 weeks. The most likely outcome is an early delivery, leading to preterm birth (2).
- Rule out Irrelevant Conditions: Eliminate 4 and 5 because macrosomia is a metabolic/growth issue and rupture is a structural failure usually associated with labor or scars, not the location of the placenta.
- Select All That Apply: Confirm that 1, 2, and 3 are all logical extensions of the vascular disruption inherent in this condition.
Take home points
- Maternal hypovolemic shock is the most immediate life-threatening complication of placenta previa.
- DIC can occur following massive hemorrhage and is marked by the depletion of systemic clotting factors.
- Preterm delivery is often necessary to manage recurrent or heavy bleeding, leading to neonatal risks.
- Placenta previa is associated with an increased risk of placenta accreta spectrum, where the placenta grows into the myometrium.
Practice Exercise 3
A nurse is assessing a client at 34 weeks gestation with painless, bright red vaginal bleeding. Which of the following diagnostic evaluations should the nurse anticipate first?
Explanation
Placenta previa is a condition where the placenta implants in the lower uterine segment, partially or completely covering the cervical os. It presents with painless bright red bleeding in the third trimester. Risk factors include multiparity, advanced maternal age, and prior cesarean section. Diagnosis is confirmed by ultrasound, and management involves maternal stabilization, avoidance of digital cervical examination, and fetal surveillance. Severe bleeding can cause maternal hypovolemia and fetal compromise, necessitating prompt evaluation and delivery if unstable.
Rationale for correct answer/s
3. Biophysical profile is indicated to assess fetal well-being when maternal bleeding occurs. It evaluates fetal movement, tone, breathing, and amniotic fluid volume. In placenta previa, maternal stability must be ensured, but fetal compromise requires immediate assessment. The fetus and oxygenation are prioritized, making this the correct initial evaluation.
Rationale for incorrect answers
1. Transvaginal ultrasound is the gold standard for diagnosing placenta previa, but it is not the first step when acute bleeding occurs. Immediate fetal assessment is prioritized. Although placental location is important, maternal-fetal stabilization precedes definitive imaging.
2. Immediate digital cervical examination is contraindicated in suspected placenta previa because it can provoke catastrophic hemorrhage. The cervix should not be manipulated until placental location is confirmed. This makes it unsafe and inappropriate as an initial evaluation.
4. MRI is useful for diagnosing placenta accreta spectrum disorders, especially in surgical planning. However, it is not appropriate in acute bleeding scenarios. The imaging modality is too advanced for initial stabilization and does not address immediate fetal compromise.
Test-taking strategy
- Identify the hallmark presentation: painless, bright red bleeding in late pregnancy strongly suggests placenta previa.
- Apply safety principles: avoid interventions that increase risk of hemorrhage, such as digital cervical examination.
- Use prioritization frameworks: maternal stabilization and fetal well-being are immediate priorities.
- ABCs: airway, breathing, circulation must be stabilized in the mother.
- Fetal assessment: biophysical profile provides rapid information about fetal oxygenation and movement.
- Rule out distractors:
- Ultrasound is diagnostic but not the first step in acute bleeding.
- MRI is advanced imaging, not urgent stabilization.
- Cervical examination is unsafe in placenta previa.
- Select the option that addresses fetal compromise while maintaining maternal safety.
Take home points
- Placenta previa presents with painless, bright red bleeding in the third trimester.
- Digital cervical examination is contraindicated due to risk of hemorrhage.
- Biophysical profile is essential for immediate fetal assessment in maternal bleeding.
- Ultrasound confirms diagnosis, but stabilization and fetal evaluation come first.
A nurse is collecting the medical history of a client suspected of having placenta previa. Which of the following is a primary risk factor?
Explanation
Placenta previa is an obstetric complication characterized by the abnormal implantation of the placenta in the lower uterine segment. The pathophysiology of this condition is closely linked to endometrial scarring, which alters the uterine environment and influences where the blastocyst attaches. When the upper uterine segment is compromised by previous surgical procedures, the placenta is more likely to implant in the lower, less vascularized regions. This malimplantation can lead to significant maternal morbidity, including catastrophic hemorrhage during the third trimester as the cervix undergoes effacement and dilation.
Rationale for correct answer
2. A previous cesarean delivery is a primary risk factor because the surgical procedure leaves a permanent myometrial scar on the uterine wall. The placenta is naturally attracted to areas of high vascularity, but if previous scarring or decidual damage is present in the fundus, the blastocyst may implant lower in the uterus. Research indicates that the risk of placenta previa increases linearly with the number of prior cesarean sections. This structural alteration of the uterine lining significantly predisposes the client to future abnormal placental attachments.
Rationale for incorrect answers
1. History of chronic hypertension is a major risk factor for abruptio placentae, not placenta previa. Hypertension causes degenerative changes in the spiral arteries, leading to placental ischemia and premature separation of a normally implanted placenta. While hypertension complicates the vascular health of the pregnancy, it does not influence the initial site of blastocyst implantation in the lower uterine segment. Therefore, it is a vascular complication rather than an anatomical risk factor for previa.
3. Gestational diabetes mellitus is associated with complications such as fetal macrosomia, polyhydramnios, and neonatal hypoglycemia, but it is not a recognized cause of placenta previa. The metabolic environment of diabetes affects fetal growth and maternal glucose regulation rather than the physical location of placental attachment. While a diabetic client may require a cesarean delivery, the diabetes itself does not cause the placental malpositioning observed in previa.
4. Maternal hypothyroidism is a common endocrine disorder in pregnancy that requires careful management with levothyroxine to prevent neurodevelopmental delays in the fetus. However, there is no established pathophysiological link between low thyroid hormone levels and the implantation site of the placenta. Hypothyroidism is associated with an increased risk of miscarriage or preeclampsia, but it does not contribute to the formation of a placenta previa in the lower uterine segment.
Test-taking strategy
- Identify the Core Mechanism: Placenta previa is an anatomical issue regarding where the placenta grows. Look for risk factors that physically change the uterus.
- Link Scarring to Implantation: Recognize that the uterus is "damaged" or altered by surgery. Previous cesarean delivery (2) is the most common cause of uterine scarring in the obstetric population.
- Differentiate the "Big Two": Remember that Hypertension (1) is the classic risk factor for Abruption (painful bleeding), whereas Scarring/Surgery (2) is the classic risk factor for Previa (painless bleeding).
- Eliminate Metabolic Factors: Choices 3 and 4 are metabolic/endocrine issues. These affect the quality of the pregnancy or fetal growth, but they do not typically change the location of the placenta.
Take home points
- Previous uterine surgery, especially cesarean sections and suction curettage, is the leading risk factor for placenta previa.
- Advanced maternal age (typically > 35 years) and multiparity also increase the statistical likelihood of abnormal placental implantation.
- Cigarette smoking and cocaine use are environmental risk factors that may cause placental hypertrophy, increasing the surface area covered.
- Placenta previa in a client with a previous cesarean section significantly increases the risk for the placenta accreta spectrum.
A nurse is planning care for a client with placenta previa. Which of the following laboratory and diagnostic measures should be included? Select all that apply
Explanation
Placenta previa involves the implantation of the placenta in the lower uterine segment, which creates a high risk for significant third-trimester hemorrhage. Management of this condition requires a multidisciplinary approach focused on hemodynamic surveillance and emergency preparedness. Because the bleeding is often sudden and can be voluminous, laboratory monitoring must prioritize the detection of acute anemia and the early onset of coagulopathy. Diagnostic imaging is utilized to assess the placental relationship to the cervix and to ensure that the uteroplacental circulation remains sufficient to support fetal life during expectant management.
Rationale for correct answers
1. A complete blood count is essential to monitor the client's hemoglobin and hematocrit levels during active or intermittent bleeding. Serial assessments allow the nurse to quantify the impact of blood loss and identify the need for iron supplementation or transfusion. A significant drop in these values can indicate occult bleeding or a loss of hemodynamic compensation. This laboratory measure provides a baseline for maternal oxygen-carrying capacity.
2. Prothrombin time and activated partial thromboplastin time are critical for monitoring the client's coagulation status, especially if a large hemorrhage occurs. Massive blood loss can trigger consumptive coagulopathy, leading to disseminated intravascular coagulation where clotting factors are exhausted. Monitoring these parameters ensures that the medical team can provide fresh frozen plasma or cryoprecipitate if the coagulation cascade fails. This is a vital safety measure for preventing uncontrolled systemic bleeding.
4. Type and crossmatch are mandatory for any client with placenta previa to ensure that compatible blood products are immediately available. In the event of a catastrophic bleed, there is no time for the traditional crossmatching process, which can take 45 to 60 minutes. Having units of packed red blood cells ready reduces the risk of prolonged maternal hypotension and shock. This preparation is a cornerstone of emergency obstetric care.
5. Doppler ultrasound is used to assess the umbilical artery flow and ensure that the fetus is receiving adequate perfusion despite placental malposition. This diagnostic tool can detect placental insufficiency before it manifests as non-reassuring heart rate patterns on a monitor. It is particularly useful in clients with suspected placenta accreta, where the blood flow patterns may be abnormally high or turbulent. This provides a non-invasive assessment of fetal-placental well-being.
Rationale for incorrect answers
3. A digital vaginal examination is strictly contraindicated in clients with placenta previa as it can cause mechanical disruption of the placenta. Inserting a finger into the cervical os can tear the placental sinuses, resulting in immediate and massive maternal hemorrhage. Diagnosis of cervical status must be limited to visual inspection via a speculum (only after ultrasound confirms the placenta is not over the os) or via ultrasound imaging. This action is a major safety violation in obstetric nursing.
Test-taking strategy
- Identify the Diagnosis: The question centers on placenta previa, which is synonymous with high-risk bleeding.
- Prioritize "Circulation" (ABCs): Laboratory tests that support the circulatory system are the priority. Choices 1, 2, and 4 all relate to blood volume and clotting ability.
- Apply the "No Vaginal Exam" Rule: Automatically eliminate Choice 3. This is a standard safety contraindication for any bleeding in the second or third trimester.
- Assess Fetal Safety: Choice 5 is a valid diagnostic tool for evaluating the placenta's functional ability to support the fetus, making it an appropriate inclusion in the plan of care.
- Select All That Apply: Ensure that your final list includes all interventions that prepare for hemorrhage and monitor for fetal compromise.
Take home points
- Maintaining updated type and crossmatch is the most critical preparation for placenta previa emergencies.
- Coagulation studies are necessary to detect the early development of disseminated intravascular coagulation following hemorrhage.
- Serial CBCs help track the severity of chronic or acute blood loss and the need for transfusion.
- Digital vaginal exams must be avoided at all costs to prevent triggering a life-threatening bleed.
A client with suspected placenta previa asks why vaginal examination is avoided. Which of the following is the most appropriate explanation?
Explanation
Placenta previa occurs when the placenta develops in the lower uterine segment, directly over or near the internal cervical os. This anatomical positioning places the fragile vascular network of the placenta in the direct path of any instrument or finger entering the cervical canal. Unlike a normally implanted placenta in the fundus, a previa is highly susceptible to mechanical trauma, where even minor contact can shear the maternal-fetal interface. Because the lower segment is thin and lacks the robust contractile power of the upper myometrium, the resulting decidual bleeding cannot be easily tamponaded, leading to rapid exsanguination.
Rationale for correct answer
3. The most appropriate explanation is that a vaginal examination may precipitate life-threatening hemorrhage by causing direct mechanical trauma to the placenta. Because the placenta is located over the cervix, digital manipulation can tear the placental sinuses, leading to an immediate and profuse flow of maternal blood. This hemorrhage can result in hypovolemic shock for the mother and catastrophic hypoxia for the fetus within minutes. Avoiding vaginal entry is the most critical safety precaution in the management of suspected or confirmed placenta previa.
Rationale for incorrect answers
1. While cervical stimulation can sometimes release prostaglandins that might theoretically irritate the uterus, inducing preterm labor is not the primary reason for avoiding the exam. The immediate and far more dangerous risk is vascular disruption and hemorrhage. In the context of placenta previa, the focus shifts from the timing of labor to the circulatory integrity of the mother. Contractions would actually be secondary to the massive bleeding that an exam would likely trigger.
2. Maternal hypotension is a symptom of hypovolemic shock, which is the result of the hemorrhage, not the direct effect of the examination itself. A vaginal exam does not have a vasovagal effect that primarily causes hypotension in these clients. The drop in blood pressure would be a secondary consequence of the massive blood loss initiated by the trauma to the placenta. Therefore, while hypotension is a major concern, the explanation provided to the client must focus on the cause (hemorrhage) rather than the symptom.
4. Altered fetal heart rate patterns, such as bradycardia or late decelerations, are signs of fetal distress that occur after placental perfusion is compromised. A vaginal exam does not directly change the fetal heart rhythm through nerve stimulation; rather, it causes bleeding that reduces the oxygen supply to the fetus. The pathophysiological sequence begins with hemorrhage, leading to placental insufficiency, which then manifests on the monitor. Explaining the risk of bleeding is more direct and accurate for the client's understanding.
Test-taking strategy
- Identify the Diagnosis: The client has suspected placenta previa, which is a high-alert condition for bleeding.
- Assess the Risk: Evaluate each option for its level of urgency and severity. While labor (1) and heart rate changes (4) are important, "life-threatening hemorrhage" (3) represents the highest priority and greatest risk to life.
- Apply the "Nothing per Vagina" Rule: In nursing education, the absolute contraindication for third-trimester bleeding is a vaginal exam. The reason is always the risk of puncturing or detaching the placenta.
- Differentiate Cause vs. Effect: Recognize that hypotension (2) and heart rate changes (4) are outcomes of bleeding. Choice 3 identifies the primary event that the nurse is trying to prevent.
Take home points
- Digital vaginal examinations are strictly contraindicated in clients with placenta previa due to the risk of placental tearing.
- The primary clinical goal in placenta previa is to prevent any trauma that could lead to maternal exsanguination.
- Ultrasound is the only safe diagnostic method used to determine the exact location of the placenta.
- Any client with third-trimester bleeding must be treated as having placenta previa until imaging proves otherwise.
A nurse is reviewing the results of a transabdominal and transvaginal ultrasound for a client with placenta previa. Which findings should the nurse anticipate? Select all that apply
Explanation
Placenta previa is characterized by the implantation of the placenta in the lower uterine segment, which is definitively diagnosed through sonographic visualization. Transvaginal ultrasound is the gold standard for diagnosis, as it allows for precise measurement of the distance between the placental edge and the internal cervical os. During the assessment, the sonographer also evaluates the retroplacental interface and the uterine wall to rule out morbidly adherent placenta, while clinical assessment confirms the absence of myometrial irritability. Successful management depends on identifying the exact degree of coverage to determine the safety of expectant management versus the necessity of a surgical delivery.
Rationale for correct answers
1. The primary diagnostic finding in placenta previa is the visualization of the placenta covering or near the internal cervical os. Transvaginal ultrasound provides high-resolution images that allow the clinician to classify the previa as complete, partial, or marginal based on the percentage of coverage. If the placental edge is within 2 cm of the os, it is clinically managed as a previa due to the high risk of hemorrhage. This finding confirms the anatomical malposition that defines the condition.
2. A soft, non-tender uterine wall is a hallmark clinical finding that distinguishes placenta previa from abruptio placentae. In previa, the bleeding originates from the placental site without significant myometrial irritation or intrauterine pressure elevation. On ultrasound, the uterine wall appears thin and relaxed, consistent with the clinical lack of abdominal rigidity. This finding is crucial for differential diagnosis, as it indicates that the bleeding is not caused by a premature separation of a normally implanted placenta.
4. Visualizing an intact umbilical cord insertion is a standard part of the ultrasound evaluation to rule out vasa previa or velamentous insertion. In placenta previa, the cord typically inserts into the placental mass normally, although the mass itself is malpositioned. Ensuring that the vessels are not crossing the os unprotected (vasa previa) is vital because fetal exsanguination occurs much more rapidly if the vessels themselves are ruptured. This assessment confirms the stability of the fetal circulatory attachment.
5. Ultrasound may reveal possible signs of placenta accreta spectrum, which is a frequent and dangerous co-morbidity of placenta previa. Sonographic markers include the loss of the retroplacental clear zone, abnormal placental lacunae, and hypervascularity at the bladder-uterine interface. This is especially relevant if the client has a history of previous cesarean sections, as the placenta can grow into the old surgical scar. Early identification of invasion allows for complex surgical planning and prevents catastrophic postpartum hemorrhage.
Rationale for incorrect answers
3. Clear evidence of uterine rupture is a catastrophic finding that is not a characteristic feature of placenta previa. Uterine rupture involves a full-thickness tear of the myometrium, usually manifesting on ultrasound as fetal parts outside the uterus, a retracted uterus, or massive hemoperitoneum. This condition presents with sudden, sharp pain and maternal shock, contrasting with the painless bleeding seen in previa. While both are emergencies, their pathophysiological mechanisms and sonographic appearances are entirely different.
Test-taking strategy
- Identify Diagnostic Findings: The question asks what the nurse should see on an ultrasound report for a client with known or suspected placenta previa.
- Focus on Anatomy: Select Choice 1 because it defines the location of the problem. Select Choice 4 and 5 because they represent the standard anatomical survey performed during a placental ultrasound.
- Use Differential Diagnosis: Recall that previa is painless (2) while abruption is painful. A soft uterus on assessment correlates with a normal-looking myometrium on ultrasound, making Choice 2 correct.
- Rule out Catastrophes: Eliminate Choice 3 because uterine rupture is a separate, distinct obstetric emergency that is not a standard finding or a common result of placenta previa itself.
- Select All That Apply: Ensure that the selected options (1, 2, 4, 5) provide a comprehensive picture of the diagnostic and safety assessments required for this condition.
Take home points
- Transvaginal ultrasound is the most accurate method for determining the distance between the placenta and the cervical os.
- A soft, non-tender uterus helps differentiate placenta previa from the board-like rigidity of abruptio placentae.
- Placenta previa in a client with prior uterine surgery necessitates a high suspicion for placenta accreta spectrum.
- Sonographic evaluation must also confirm normal umbilical cord insertion to exclude vasa previa.
Practice Exercise 4
A nurse is caring for a client with complete placenta previa at 36 weeks gestation. Which of the following is the most appropriate delivery plan?
Explanation
Complete placenta previa represents total placental occlusion of the internal cervical os, necessitating surgical intervention. This malimplantation prevents safe fetal descent and carries a high risk of maternal exsanguination if labor commences. Management requires a multidisciplinary approach focusing on hemodynamic stability and controlled delivery.
Rationale for correct answer
2. A scheduled cesarean delivery at 36–37 weeks is the standard of care for stable complete previa. This timing minimizes the risk of spontaneous labor and catastrophic antepartum hemorrhage while ensuring fetal maturity. Surgical delivery is mandatory because the placenta physically obstructs the birth canal, making a safe vaginal exit impossible. Controlled surgical intervention significantly reduces maternal and neonatal morbidity.
Rationale for incorrect answers
1. Expectant management at home is inappropriate at 36 weeks because the risk of sudden, profuse vaginal bleeding increases as the lower uterine segment thins. At this advanced gestational age, the benefits of continued fetal development are outweighed by the danger of maternal hemorrhage. Clients with complete previa often require hospitalization to ensure immediate access to surgical services and blood products if bleeding occurs.
3. Induction of labor with oxytocin is absolutely contraindicated in complete placenta previa because uterine contractions would cause the cervical os to dilate against the placenta. This would lead to immediate, massive placental detachment and maternal-fetal death. Oxytocin increases the frequency and intensity of myometrial activity, which would accelerate vascular shearing at the placental site. A vaginal birth cannot occur when the placenta blocks the passage.
4. Vaginal delivery with forceps is impossible and life-threatening in the presence of a complete previa. Forceps are used to assist a vaginal birth, which is physically blocked by the placental tissue covering the cervix. Any attempt to deliver the fetus through the vagina would require the fetus to pass through the placental mass, resulting in fetal exsanguination and maternal shock. Cesarean section remains the only viable delivery route.
Test-taking strategy
- Analyze the Anatomy: Recognize that "complete" placenta previa means the door (cervix) is totally blocked by a highly vascular organ.
- Safety and Contraindications: Identify that any form of vaginal delivery (3 and 4) is physically impossible and would cause fatal bleeding. These must be eliminated immediately.
- Evaluate Gestational Age: Note the client is at 36 weeks. This is near term. Choice 1 (expectant management) is used earlier in pregnancy (e.g., 28–32 weeks) but is less appropriate as the client reaches term.
- Select the Standard of Care: Choose the option that provides a controlled environment. A scheduled cesarean (2) is the most scientific and safe way to manage a total obstruction of the birth canal.
Take home points
- Complete placenta previa is a total contraindication for vaginal delivery and labor induction.
- Scheduled cesarean delivery is typically performed between 36 0/7 and 37 6/7 weeks to prevent emergency hemorrhage.
- The primary maternal risk in late-term previa is catastrophic hemorrhage during cervical effacement.
- Hospitalization is often required for clients with recurrent bleeding or limited access to emergency surgical care.
A nurse is monitoring a hospitalized client with placenta previa. Which sign indicates a need for immediate intervention?
Explanation
Placenta previa occurs when the placenta implements in the lower uterine segment, necessitating strict monitoring for vascular compromise. Acute hemorrhage results from the mechanical disruption of the placental-decidual interface as the cervix thins. This can lead to a rapid depletion of the maternal intravascular volume, compromising both maternal organ perfusion and fetal gas exchange. Immediate intervention is required to prevent hypovolemic shock and fetal demise.
Rationale for correct answer
2. A sudden increase in bright red vaginal bleeding indicates active maternal hemorrhage and requires immediate nursing and medical intervention. Bright red blood signifies fresh arterial bleeding from the placental site, which can rapidly lead to maternal hemodynamic collapse. The nurse must immediately initiate volume resuscitation and notify the surgical team for a potential emergency delivery. This sign represents a transition from stable expectant management to a life-threatening crisis.
Rationale for incorrect answers
1. Minimal vaginal spotting is a common finding in hospitalized clients with placenta previa and, while requiring documentation and assessment, does not typically necessitate immediate emergency intervention. Spotting often occurs as the lower segment undergoes minor physiologic changes without a full-scale vascular rupture. The nurse should continue to monitor the pad count and maternal vitals. However, it does not carry the same urgency as a profuse, sudden hemorrhage.
3. A fetal heart rate of 140 bpm with moderate variability is a reassuring finding indicating adequate fetal oxygenation and an intact autonomic nervous system. Moderate variability is the most important indicator of fetal well-being and the absence of metabolic acidosis. Since the fetus is currently stable, this finding does not trigger an emergency protocol. The nurse would continue routine electronic fetal monitoring as part of the standard plan of care.
4. Mild intermittent uterine contractions are common in the third trimester and, while they can lead to cervical changes, do not always require immediate intervention unless they become regular or increase in intensity. The nurse should assess for cervical effacement via ultrasound rather than a digital exam. While contractions are a risk factor for bleeding, they are managed with bed rest or tocolytics. They are a warning sign rather than an indicator of an active, catastrophic event.
Test-taking strategy
- Prioritize the ABCs: In any clinical scenario, Circulation (bleeding) is a top priority. Choice 2 represents a major circulatory threat.
- Identify the Most Unstable Sign: Compare a stable fetal heart rate (3), minor spotting (1), and mild contractions (4) against a sudden increase in hemorrhage (2).
- Focus on the Diagnosis: Placenta previa's most dangerous complication is exsanguination. Any shift toward heavy bleeding is the primary trigger for emergency action.
- Eliminate Normal/Reassuring Data: Choice 3 is a normal finding and can be ruled out immediately as it indicates fetal stability.
Take home points
- Sudden, profuse bright red bleeding is the most critical indicator of maternal and fetal jeopardy in placenta previa.
- Maternal tachycardia and hypotension are late signs of shock; bleeding volume must be assessed first.
- A soft, non-tender uterus is typical even during an active bleed in placenta previa.
- Any escalation in bleeding requires the nurse to notify the provider and prepare for a potential STAT cesarean section.
A nurse is planning care for a client with placenta previa who is receiving betamethasone for fetal lung maturity and is on bed rest. Which of the following interventions are appropriate? Select all that apply
Explanation
Placenta previa involves the implantation of the placenta in the lower uterine segment, requiring a management strategy that balances fetal maturation with maternal safety. When a client is at risk for preterm delivery due to hemorrhage, antenatal corticosteroids like betamethasone are administered to induce surfactant production in the fetal lungs. This pharmacological intervention reduces the incidence of neonatal respiratory distress syndrome. Concurrently, nursing care focuses on the prevention of mechanical placental disruption and the early detection of hemodynamic instability through frequent assessment and activity restriction.
Rationale for correct answers
1. The nurse must monitor maternal blood glucose levels because betamethasone is a corticosteroid that can induce maternal hyperglycemia. Steroids stimulate gluconeogenesis and decrease peripheral glucose uptake, which is particularly significant in pregnant clients who may have underlying gestational diabetes. Maintaining glycemic control is essential to prevent maternal metabolic derangements and subsequent neonatal hypoglycemia after birth. This is a critical pharmacological monitoring requirement.
3. Assessing vaginal bleeding every 15 minutes is a standard nursing protocol for clients with active or high-risk obstetric hemorrhage. Frequent assessment allows for the early quantification of blood loss and the detection of a shift from stable spotting to profuse bleeding. Early detection of increased volume is vital for initiating timely fluid resuscitation and surgical intervention. This intervention ensures maternal-fetal safety through vigilant surveillance of the placental site.
4. Educating the client on the signs of labor and hemorrhage empowers the patient to report sentinel events immediately. Since the client is on bed rest, they are the first to notice changes such as sudden bright red discharge, pelvic pressure, or regular uterine activity. Clear communication regarding the "painless" nature of previa bleeding helps the client differentiate it from other sensations. This education is a cornerstone of collaborative management in high-risk pregnancy.
Rationale for incorrect answers
2. Encouraging ambulation is contraindicated because physical activity and the force of gravity increase the risk of cervical irritation and placental shearing. Clients with placenta previa are traditionally managed with modified bed rest to reduce the pressure on the lower uterine segment. Ambulation could provoke a major hemorrhagic episode or stimulate preterm labor. Instead, the nurse should implement venous thromboembolism (VTE) prophylaxis through passive range-of-motion exercises and sequential compression devices.
5. Administering magnesium sulfate is not a routine intervention for placenta previa unless there is a specific indication for neuroprotection (before 32 weeks) or if the client has concurrent preeclampsia. While magnesium has tocolytic properties, it is not the primary drug used to "suppress contractions" in a stable previa client. Using it without a clear diagnosis of preterm labor or a need for neuroprotection exposes the client to unnecessary risks of magnesium toxicity, such as respiratory depression.
Test-taking strategy
- Identify the Drug Effects: Recognize that betamethasone is a steroid. Steroids always raise blood glucose (1).
- Apply Safety Precautions: Recall that placenta previa requires bed rest to prevent bleeding. Therefore, "encourage ambulation" (2) must be incorrect.
- Prioritize Assessment: In any condition involving hemorrhage, frequent bleeding assessments (3) are a priority for patient safety.
- Determine Clinical Relevancy: Education (4) is almost always a correct nursing intervention in a stable client.
- Analyze the Choice of Tocolytic: Magnesium sulfate (5) is a high-alert medication with specific indications. It is not the "go-to" for simple contraction suppression in a previa patient unless delivery is imminent and preterm.
Take home points
- Betamethasone is administered to promote fetal lung maturity but requires monitoring of maternal glucose levels.
- Strict bed rest is maintained to prevent mechanical stress on the low-lying placental site.
- Frequent bleeding assessments are necessary to detect the transition to an emergency hemorrhagic state.
- Client education must focus on the immediate reporting of painless, bright red vaginal bleeding.
A nurse is caring for a client admitted with marginal placenta previa and intermittent bleeding. Which nursing actions are appropriate? Select all that apply
Explanation
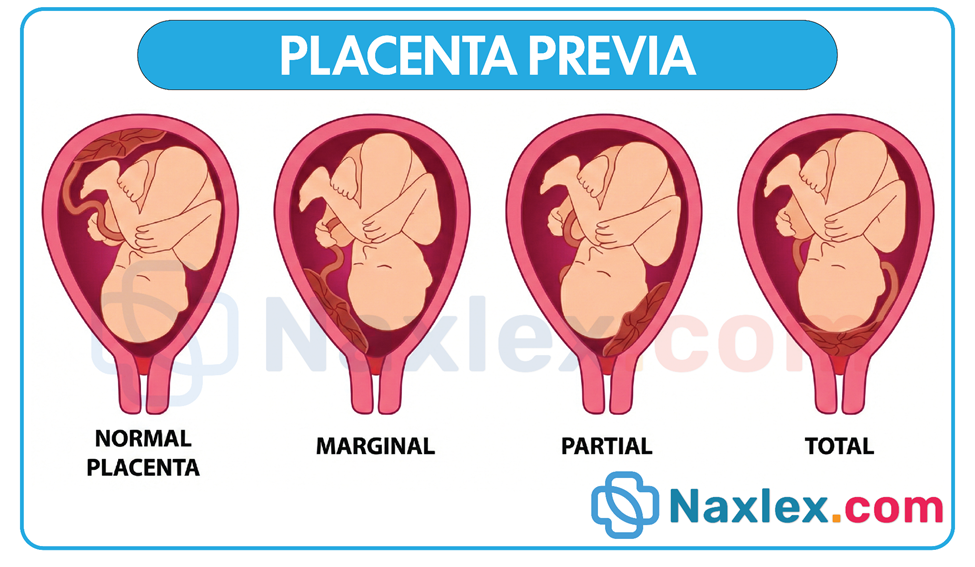
Marginal placenta previa occurs when the placental edge is located within 2 cm of the internal cervical os but does not cover it. This anatomical position creates a risk for decidual hemorrhage as the lower uterine segment undergoes physiologic changes or contractions. Nursing management focuses on expectant management, which aims to prolong the pregnancy toward 37 weeks while maintaining a high state of readiness for acute hemorrhage. Because the placental attachment is precarious, all interventions must prioritize mechanical stability of the uterus and continuous surveillance of fetal oxygenation to detect early signs of placental insufficiency.
Rationale for correct answers
1. Maintaining strict bed rest with bathroom privileges is a standard intervention to reduce gravitational pressure and mechanical stress on the lower uterine segment. Limiting physical activity helps prevent the shearing forces that lead to placental separation and subsequent bleeding. By reducing maternal exertion, the nurse helps maintain the stability of the placental-decidua interface. This conservative activity level is essential for clients experiencing intermittent bleeding to prevent an escalation to major hemorrhage.
2. Initiating continuous external fetal monitoring is necessary to evaluate fetal heart rate patterns and uterine activity. Because the placenta is near the cervix, any uterine contractions could lead to bleeding that compromises intervillous gas exchange. Monitoring allows for the immediate detection of late decelerations or tachycardia, which are indicators of fetal distress. This non-invasive assessment provides a continuous safety net for the fetus during episodes of maternal bleeding.
4. Preparing type and cross-matched blood products is a critical safety protocol because marginal previa can transition into a life-threatening hemorrhage without warning. Having 2 to 4 units of packed red blood cells available in the blood bank ensures that volume resuscitation can begin immediately if the client becomes hemodynamically unstable. This minimizes the risk of hypovolemic shock and ensures that maternal oxygen-carrying capacity is maintained. It is a cornerstone of emergency obstetric preparedness.
5. Educating the client to report increased bleeding immediately is vital for early intervention and maternal safety. The client is often the first to feel a "gush" of fluid or notice bright red blood on their peripads. Rapid reporting allows the nursing team to assess cumulative blood loss and adjust the plan of care, such as moving from expectant management to an emergency delivery. Empowering the client with specific discharge-style instructions while inpatient enhances the surveillance of the condition.
Rationale for incorrect answers
3. Performing a vaginal examination to assess cervical dilation is strictly contraindicated in all forms of placenta previa. Digital manipulation can puncture the placental edge or cause a massive detachment from the lower uterine segment. This iatrogenic trauma can lead to uncontrolled exsanguination and fetal demise within minutes. If cervical assessment is required, it must be performed using transvaginal ultrasound by a qualified provider to avoid direct contact with the placenta.
Test-taking strategy
- Identify the Diagnosis: The client has marginal placenta previa. Any placenta previa (marginal, partial, or complete) carries the same risk for hemorrhage during vaginal entry.
- Apply Safety Constraints: Rule out Choice 3 immediately. A vaginal exam is the number one "Never Event" for a nurse caring for a patient with third-trimester bleeding until previa is ruled out.
- Prioritize Preparation: Since the client has intermittent bleeding, the risk of a "big bleed" is high. Choice 4 is a proactive safety step that follows the principle of risk reduction.
- Monitor the Vitals: Choice 2 (fetal monitoring) follows the Assessment step of the nursing process, ensuring the nurse has data on fetal tolerance of the bleeding.
- Manage Activity: Choice 1 (bed rest) and Choice 5 (education) are standard conservative interventions for a stable but high-risk obstetric patient.
Take home points
- Marginal placenta previa requires a "nothing per vagina" policy to prevent catastrophic mechanical hemorrhage.
- Expectant management includes bed rest and continuous fetal monitoring to maximize the chances of reaching fetal maturity.
- Blood bank readiness (Type and Crossmatch) is the most important preparatory action for potential obstetric shock.
- Any increase in bright red vaginal bleeding is a clinical emergency that necessitates immediate provider notification.
A nurse is reviewing orders for a client with placenta previa. Which pharmacologic order should be questioned?
Explanation
Placenta previa is an obstetric condition where the placenta implants in the lower uterine segment, creating a physical barrier over the birth canal. This malpositioning makes vaginal delivery impossible and dangerous because the mechanical pressure of the fetal presenting part during labor would cause catastrophic placental detachment. Pathophysiologically, the lower uterine segment lacks the myometrial thickness to provide effective hemostasis after placental separation, leading to rapid maternal exsanguination. Any pharmacologic intervention that promotes cervical changes or uterine activity must be avoided to prevent the onset of life-threatening hemorrhage.
Rationale for correct answer
3. An oxytocin infusion to stimulate labor must be questioned because it is strictly contraindicated in the presence of placenta previa. Oxytocin increases the frequency and intensity of uterine contractions, which would force the placental tissue to separate from the thinning lower uterine segment. This would lead to immediate, massive maternal hemorrhage and fetal hypoxia as the oxygen supply is severed. Because the placenta obstructs the cervix, labor cannot result in a vaginal birth and instead results in maternal-fetal death.
Rationale for incorrect answers
1. Betamethasone 12 mg IM is an appropriate order for a client at 34 weeks gestation to promote fetal lung maturity. Corticosteroids stimulate the production of pulmonary surfactant in the fetal alveoli, which reduces the risk of respiratory distress syndrome (RDS) if the client requires a preterm delivery. This is a standard prophylactic intervention for any high-risk pregnancy where delivery is anticipated before 37 weeks. It does not negatively impact the placental site or maternal hemodynamics.
2. Magnesium sulfate IV is an appropriate order if the goal is to provide neuroprotection for the fetus or to manage preterm contractions (tocolysis) to allow for the completion of steroid therapy. In placenta previa, stopping contractions is vital to prevent cervical effacement and subsequent bleeding. While magnesium is a high-alert medication, its use to stabilize the uterus and protect the fetal brain from intraventricular hemorrhage is clinically indicated in preterm scenarios.
4. Iron supplementation for anemia is a standard and necessary order for clients with placenta previa, especially those experiencing intermittent bleeding. Chronic or acute blood loss depletes maternal iron stores, leading to a reduction in hemoglobin and maternal oxygen-carrying capacity. Optimizing the client’s hematologic status helps build a vascular reserve in case a major hemorrhagic event occurs during delivery. This is a supportive treatment that poses no risk to the placental attachment.
Test-taking strategy
- Identify the Core Constraint: In placenta previa, the "exit" is blocked. Any action that tries to force the fetus through that exit (labor) is a safety violation.
- Evaluate Pharmacologic Goals: Determine the purpose of each drug. Betamethasone (1) helps the baby's lungs; Magnesium (2) keeps the uterus quiet; Iron (4) fixes the mother's blood. These all support the pregnancy.
- Identify the Conflict: Oxytocin (3) is a labor-inducing agent. This directly conflicts with the anatomical reality of a blocked cervix.
- Prioritize Risk Reduction: Choose the intervention that would cause the most immediate harm. Inducing labor in a patient with a total placenta previa is a catastrophic error, making Choice 3 the most critical order to question.
Take home points
- Labor induction with oxytocin is an absolute contraindication for any client with placenta previa.
- Antenatal corticosteroids are used to reduce neonatal morbidity associated with preterm birth in previa cases.
- Maintaining uterine quiescence (no contractions) is a primary goal of expectant management.
- The only safe method of delivery for a complete or partial placenta previa is a scheduled or emergency cesarean section.
Practice Exercise 5
A nurse is caring for a client with placenta previa in active labor. Which maternal assessment finding requires immediate intervention?
Explanation
Placenta previa involves abnormal blastocyst implantation within the lower uterine segment, potentially obstructing the internal cervical os. This malpositioning subjects the low-lying, fragile vascular network to mechanical shearing forces during cervical effacement or lower segment thinning, resulting in characteristic painless hemorrhage. Unlike other obstetric hemorrhages, this bleeding is primarily maternal in origin and occurs without the stimulus of uterine contractions or trauma, often requiring careful hemodynamic monitoring.
Rationale for correct answer
2. Bright red vaginal bleeding soaking one peripad per hour indicates a significant hemorrhagic event that requires immediate medical intervention. In placenta previa, active labor accelerates placental detachment, leading to rapid maternal blood loss and potential hypovolemic shock. This volume of bleeding suggests the compensatory mechanisms may soon fail, jeopardizing maternal and fetal stability. The nurse must immediately notify the surgical team for an emergency cesarean section to prevent exsanguination.
Rationale for incorrect answers
1. A soft, non-tender uterus is a classic clinical finding in placenta previa that indicates the absence of abruptio placentae. While it is a defining characteristic of the condition, it is a reassuring finding rather than a trigger for emergency intervention. It confirms that the bleeding is not caused by high-pressure intrauterine hematomas or myometrial rigidity. The nurse should continue to document this finding as part of the routine assessment of uterine tone.
3. Mild lower abdominal cramping is an expected finding during active labor and does not necessarily signify an immediate life-threatening complication in placenta previa. While contractions are dangerous because they cause cervical dilation, the presence of mild cramping is less urgent than active, profuse hemorrhage. The nurse must monitor the frequency and intensity of these cramps to prevent precipitous labor. However, in the hierarchy of clinical urgency, this finding is secondary to maternal blood loss.
4. A maternal blood pressure of 120/78 mmHg is within the normotensive range and indicates that the client is currently hemodynamically stable. Although pregnancy induces a higher blood volume that can mask early signs of shock, this specific reading does not indicate circulatory collapse. The nurse should continue to monitor for trends such as narrowing pulse pressure or orthostatic changes. Currently, this stable vital sign does not require the immediate emergency intervention associated with acute maternal-fetal jeopardy.
Test-taking strategy
- Identify the Priority Concern: The question asks for the finding requiring immediate intervention in a patient with placenta previa. In any obstetric hemorrhage scenario, the amount of visible blood loss is the primary indicator of instability.
- Quantify the Blood Loss: Choice 2 provides a specific rate of bleeding (one peripad per hour). In maternal-newborn nursing, saturating a pad in less than 2 hours is a critical threshold for hemorrhage.
- Differentiate Normal vs. Abnormal: Choice 1 (soft uterus) and Choice 4 (normal BP) are expected or stable findings. They do not trigger an "immediate" emergency response.
- Evaluate Clinical Urgency: Compare Choice 3 (cramping) with Choice 2 (bleeding). While labor is risky for previa, the actual hemorrhage is always more life-threatening than the uterine activity itself.
- Apply the ABCs: Focus on Circulation. Active bleeding directly impacts the circulating volume, making Choice 2 the priority assessment finding to address first.
Take home points
- Saturating a peripad in one hour or less is a definitive sign of obstetric hemorrhage requiring immediate intervention.
- Placenta previa typically presents with a soft, non-tender uterus, which helps distinguish it from the rigidity of placental abruption.
- Active labor is a contraindication for expectant management in placenta previa due to the high risk of placental shearing.
- Maternal blood pressure may remain normal even after significant blood loss due to the expanded blood volume of pregnancy.
A nurse is monitoring a neonate born at 34 weeks due to maternal placenta previa. Which complication is most likely?
Explanation
Neonates born prematurely following placenta previa complications frequently encounter issues related to hepatic and hematologic immaturity. While maternal hemorrhage triggers delivery, the resulting preterm birth at 34 weeks subjects the neonate to an underdeveloped physiological system. The liver’s inability to efficiently conjugate bilirubin, combined with a higher rate of red blood cell turnover, leads to a significant risk of unconjugated hyperbilirubinemia. Management requires monitoring serum levels to prevent bilirubin encephalopathy, as the blood-brain barrier is more permeable in late-preterm infants.
Rationale for correct answer
2. Hyperbilirubinemia is the most likely complication for a neonate born at 34 weeks because of hepatic immaturity. At this gestational age, the enzyme glucuronyl transferase is produced in lower quantities, limiting the liver's ability to convert fat-soluble bilirubin into a water-soluble form for excretion. Furthermore, late-preterm infants often have shorter erythrocyte lifespans, leading to an increased bilirubin load. This creates a physiological imbalance where bilirubin production exceeds the infant's ability to clear it from the circulation.
Rationale for incorrect answers
1. While hypoglycemia can occur in preterm infants due to low glycogen stores, it is not the most "likely" or specific complication tied to 34-week delivery in placenta previa cases unless there is concurrent maternal diabetes. Most 34-week infants can maintain glucose levels if early feeding is established. Hyperbilirubinemia affects a higher percentage of this specific gestational cohort compared to symptomatic hypoglycemia. Therefore, while relevant, it is not the primary expected hematologic/metabolic complication for a late-preterm neonate.
3. A congenital anomaly is not a direct result of placenta previa or preterm birth itself. Congenital malformations typically occur during the first trimester during organogenesis, whereas placenta previa is a complication of placental implantation and third-trimester growth. There is no evidence-based link suggesting that abnormal placental location increases the incidence of genetic or structural birth defects. The complications seen in these neonates are typically functional and related to prematurity rather than structural anomalies.
4. Polycythemia is an excess of red blood cells, which is more commonly seen in post-term infants or those with intrauterine growth restriction (IUGR) due to chronic hypoxia. In the context of placenta previa with maternal bleeding, the neonate is actually at a higher risk for anemia if fetal-maternal hemorrhage occurred during the placental separation. Preterm infants generally have lower hematocrit levels and are less likely to present with the hyperviscosity associated with polycythemia.
Test-taking strategy
- Identify the Gestational Age: Focus on "34 weeks." This is the definition of a late-preterm infant.
- Recall Prematurity Risks: Common issues for late-preterm babies (34-36 weeks) include respiratory distress, feeding difficulties, and jaundice.
- Prioritize Statistics: Hyperbilirubinemia (2) occurs in nearly 80% of preterm infants, making it the "most likely" choice.
- Match Pathology to Timing: Eliminate Choice 3 as anomalies happen early in pregnancy. Eliminate Choice 4 as it is usually a post-mature or chronic stress finding.
- Evaluate the Previa Link: Understand that the main "complication" for the baby in previa is the preterm delivery itself, and jaundice is the hallmark of the 34-week neonate.
Take home points
- Late-preterm neonates (34–36 weeks) are at high risk for hyperbilirubinemia due to immature hepatic conjugation.
- Monitoring of transcutaneous or serum bilirubin levels is essential within the first 24 to 48 hours of life.
- Phototherapy is the primary treatment used to prevent kernicterus in infants with rising bilirubin levels.
- Preterm infants born via emergency cesarean for previa must also be assessed for neonatal anemia and respiratory distress.
A nurse is planning care for a client in labor with placenta previa. Which interventions are appropriate? Select all that apply
Explanation
Placenta previa involves abnormal blastocyst implantation within the lower uterine segment, potentially obstructing the internal cervical os. This malpositioning subjects the low-lying, fragile vascular network to mechanical shearing forces during cervical effacement or lower segment thinning, resulting in characteristic painless hemorrhage. Unlike other obstetric hemorrhages, this bleeding is primarily maternal in origin and occurs without the stimulus of uterine contractions or trauma, often requiring careful hemodynamic monitoring.
Rationale for correct answers
1. Avoiding digital vaginal examinations is the most critical intervention to prevent iatrogenic hemorrhage in a client with placenta previa. Inserting fingers into the cervix can cause mechanical disruption of the placental-decidual interface, leading to immediate and massive maternal blood loss. Any assessment of cervical status must be performed via transvaginal ultrasound by a qualified provider. This precaution maintains the anatomical integrity of the placental attachment.
2. Continuous external fetal heart rate monitoring is essential to assess fetal tolerance of uterine activity and potential occult bleeding. Placenta previa increases the risk of placental insufficiency and fetal hypoxia if the placental surface area begins to detach. Continuous data allow for the immediate detection of late decelerations or fetal tachycardia, which are early indicators of fetal jeopardy. This ensures a rapid response to any decline in fetal oxygenation.
4. Maintaining IV access with a large-bore catheter (18 gauge or larger) is a vital safety measure for rapid volume resuscitation. Placenta previa can cause sudden, profuse bleeding that leads to hypovolemic shock within minutes. A patent, large-diameter intravenous line allows for the high-volume administration of isotonic crystalloids or blood products. This intervention is foundational for maintaining maternal hemodynamic stability during an acute hemorrhagic event.
5. Monitoring vaginal bleeding frequently allows the nurse to quantify maternal blood loss and assess the severity of the previa. The nurse should track the number of peripads used and the color of blood, as bright red indicates fresh arterial bleeding. Frequent assessment is necessary to identify the transition from stable spotting to active hemorrhage. This data is critical for determining the timing of emergency surgical intervention.
Rationale for incorrect answers
3. Encouraging ambulation to accelerate labor is strictly contraindicated because physical activity and gravity increase the pressure on the lower segment, potentially triggering massive bleeding. Furthermore, labor is not desired in a client with a confirmed previa because vaginal delivery is physically obstructed and dangerous. Management focuses on uterine quiescence and pelvic rest to prevent placental shearing. Accelerating labor in this context would lead to catastrophic placental detachment.
Test-taking strategy
- Identify the Diagnosis: The client has placenta previa, which is a high-alert condition for life-threatening hemorrhage.
- Prioritize Safety Constraints: Use the "Nothing per Vagina" rule. Choice 1 is a mandatory safety action.
- Assess for Hemorrhagic Risk: Any intervention that prepares for or monitors bleeding is a priority. This validates Choice 4 (IV access) and Choice 5 (bleeding assessment).
- Fetal Surveillance: In a placental disorder, the fetus is at risk for hypoxia. Continuous monitoring (Choice 2) is a standard of care.
- Eliminate Harmful Actions: Choice 3 (ambulation) encourages the very thing the nurse must prevent: labor and mechanical stress on the placenta. Eliminate this option immediately.
Take home points
- Digital vaginal examinations are strictly prohibited in the presence of placenta previa to avoid triggering massive hemorrhage.
- Large-bore IV access and blood type-and-crossmatch are the most important preparations for maternal resuscitation.
- Continuous electronic fetal monitoring is required to detect early signs of fetal hypoxia secondary to placental separation.
- Any intervention that stimulates or accelerates labor is contraindicated due to the risk of catastrophic placental detachment.
A nurse is providing postpartum care to a client who underwent cesarean section for placenta previa. Which interventions are appropriate? Select all that apply
Explanation
Placenta previa increases the risk for postpartum hemorrhage because the lower uterine segment, where the placenta was implanted, contains fewer muscle fibers than the fundus. This anatomical deficiency limits the uterus's ability to contract effectively and compress the torn venous sinuses after placental delivery. Postoperative care following a cesarean section for previa must focus on intensive hemodynamic monitoring and the prevention of secondary complications such as venous thromboembolism or surgical site infection.
Rationale for correct answers
1. Monitoring uterine tone and lochia every 15 min is a critical intervention to detect early postpartum hemorrhage. In a client with placenta previa, the lower uterine segment often experiences atony, leading to significant blood loss even if the fundus feels firm. Frequent assessment allows the nurse to quantify lochia flow and identify a transition from normal rubra to excessive bleeding. This vigilance is essential during the first hour following surgery when the risk of circulatory collapse is highest.
2. Encouraging early ambulation is an appropriate intervention to prevent deep vein thrombosis and pulmonary embolism. Pregnancy and major surgery both create a hypercoagulable state, and immobility further increases the risk of clot formation in the lower extremities. Once the effects of anesthesia have subsided and the client is hemodynamically stable, assisted movement promotes venous return and respiratory function. This is a standard postoperative recovery goal to reduce maternal morbidity.
3. Educating the client on warning signs of postpartum hemorrhage is vital for safety and self-care following discharge. The client must be able to recognize abnormal symptoms such as saturating a peripad in less than 1 hour, passing large clots, or experiencing lightheadedness. Because delayed hemorrhage can occur days after delivery, providing clear discharge instructions ensures the client seeks medical attention before hemodynamic compromise occurs. This empowers the client to participate in their clinical surveillance.
5. Maintaining IV fluids and preparing for blood transfusion is necessary because of the high hemorrhagic risk associated with the previous placental site. The nurse must ensure that large-bore IV access remains patent to allow for the rapid administration of isotonic crystalloids or blood products if hemoglobin levels drop. Pre-emptive preparation, including an active type and crossmatch, reduces the time required to respond to a late-onset bleed. This maintains the client's intravascular volume and oxygen-carrying capacity.
Rationale for incorrect answers
4. Allowing unrestricted visitors is inappropriate because it can lead to maternal exhaustion and interfere with essential nursing assessments and breastfeeding. Postoperative recovery requires a balance between psychosocial support and adequate rest and privacy. High-risk clients, particularly those who have experienced a stressful delivery like a cesarean for previa, need a controlled environment to recover and bond with the neonate. Restricting visitors ensures the nurse can perform frequent fundal and lochia checks without interruption.
Test-taking strategy
- Identify Post-Op Risks: The client just had surgery and previously had placenta previa. The two biggest risks are hemorrhage (due to the lower segment site) and clots (due to surgery).
- Prioritize "Circulation" (ABCs): Choices 1, 3, and 5 all address the risk of blood loss. These are high-priority nursing actions that ensure maternal safety.
- Address Surgical Recovery: Choice 2 (ambulation) is a standard of care for any post-cesarean patient to prevent emboli.
- Evaluate Support vs. Safety: While psychosocial support is important, "unrestricted" visitors (4) usually represents an incorrect nursing choice on exams because it violates the need for rest and clinical monitoring.
- Select All That Apply: Ensure your final selections (1, 2, 3, 5) cover both the specific risks of the previa diagnosis and general surgical recovery.
Take home points
- The lower uterine segment does not contract as efficiently as the fundus, making postpartum hemorrhage more likely after placenta previa.
- Frequent assessment of uterine tone and lochia is the primary nursing action to detect early hemorrhage.
- Post-cesarean clients require early ambulation and VTE prophylaxis to mitigate the risks of a hypercoagulable state.
- Preparation for blood transfusion should continue into the postpartum period for any client who experienced significant antepartum bleeding.
A nurse is assessing a client with severe placenta previa postpartum. Which maternal complication is most concerning?
Explanation
Placenta previa involves blastocyst implantation within the lower uterine segment, which lacks the robust, interlacing myometrial musculature of the uterine fundus. This anatomical deficiency prevents the "living ligatures" of the uterus from effectively constricting torn venous sinuses following placental expulsion. Consequently, the primary risk is immediate hypovolemic collapse due to ineffective hemostasis at the implantation site, often complicated by the presence of a previous surgical scar or placental invasion into the uterine wall.
Rationale for correct answer
2. Postpartum hemorrhage is the most concerning complication because the lower uterine segment does not contract with sufficient force to achieve spontaneous hemostasis. Unlike fundal implantation, where the thick myometrium compresses vessels, the thin lower segment remains atonic, leading to rapid, profuse blood loss. This can quickly escalate to hypovolemic shock, multi-organ failure, and disseminated intravascular coagulation if not managed with aggressive uterotonic therapy or surgical intervention. Vigilant monitoring of uterine tone and quantitative blood loss is the absolute nursing priority in the immediate puerperium.
Rationale for incorrect answers
1. A urinary tract infection is a potential postpartum risk, especially if indwelling catheterization was required during a cesarean delivery. While significant, it is an infectious complication that typically manifests days after delivery with symptoms like dysuria or low-grade fever. It does not pose an immediate life threat to maternal stability in the same manner as an acute hemorrhagic event. The nurse manages this through sterile technique and early catheter removal rather than emergency resuscitation protocols.
3. Constipation is a common but minor postpartum issue resulting from progesterone-induced decreased gastrointestinal motility and the effects of opioid analgesics used during surgery. While uncomfortable and requiring management with stool softeners or increased fiber intake, it is a physiological nuisance rather than a concerning clinical emergency. It has no direct impact on hemodynamic stability or the surgical integrity of the uterine segment. Nursing care focuses on patient comfort and the resumption of normal bowel function over several days.
4. Mild edema of the lower extremities is a frequent finding in the early postpartum period due to the physiologic shift of extracellular fluid back into the intravascular space. While the nurse must monitor for signs of deep vein thrombosis, bilateral mild edema is generally a benign transition following the administration of intravenous fluids during delivery. It does not indicate the vascular crisis associated with the primary diagnosis of placenta previa. This finding is addressed through elevation and early ambulation rather than emergency medical intervention.
Test-taking strategy
- Identify the Diagnosis: The question specifies severe placenta previa, which is a high-risk vascular condition.
- Prioritize the ABCs: Use the Circulation priority. Only one choice (2) represents a life-threatening circulatory failure.
- Apply Anatomical Knowledge: Recall that the lower uterine segment is thin and weak. This leads directly to a higher risk of atony and bleeding compared to a normal pregnancy.
- Evaluate Severity: Compare "mild edema" (4) and "constipation" (3) against "hemorrhage" (2). In any NCLEX-style question, the answer that leads to maternal death is the one that is "most concerning."
- Rule out Timing: Infections (1) usually take 24 to 72 hours to develop, whereas hemorrhage (2) is an immediate threat in the "postpartum" period mentioned in the stem.
Take home points
- Postpartum hemorrhage is the leading cause of maternal morbidity in clients with placenta previa due to lower segment atony.
- The absence of fundal contraction does not always accurately reflect the amount of bleeding occurring at a low-lying placental site.
- Hemodynamic stability must be confirmed through frequent vital sign assessment and measurement of quantitative blood loss.
- Placenta previa is a significant risk factor for placenta accreta, which further increases the risk of catastrophic postpartum hemorrhage.
Comprehensive Questions
A nurse is caring for a client at 36 weeks gestation with a history of placenta previa. Which assessment finding requires immediate intervention?
Explanation
Placenta previa involves the blastocyst implantation within the lower uterine segment, potentially obstructing the internal os. This maladaptation causes vascular shearing during cervical effacement, leading to profuse maternal hemorrhage. Blood loss often exceeds the maternal circulatory reserve, necessitating aggressive volume replacement.
Rationale for correct answer
3. A maternal blood pressure of 85/55 mmHg and heart rate of 125 bpm indicates hypovolemic shock. In obstetric hemorrhage, these vital signs suggest a critical loss of intravascular volume exceeding 1500 mL. The nurse must prioritize immediate fluid resuscitation and surgical intervention to prevent maternal collapse. This hemodynamic instability represents an end-stage compensatory failure requiring emergency resuscitation.
Rationale for incorrect answers
1. Bright red, painless vaginal bleeding is the hallmark diagnostic sign of placenta previa. While this requires careful monitoring and quantification of blood loss, it is an expected finding for the condition. In the absence of hemodynamic instability or fetal distress, it does not supersede the urgency of active shock. The nurse continues to assess the volume and color of the discharge.
2. A soft, non-tender uterus is an expected assessment finding that helps differentiate previa from abruptio placentae. This finding indicates a lack of myometrial irritability or intrauterine pressure elevation. Because it is a normal characteristic of the disease process, it does not require emergency intervention. It serves as a baseline for ongoing maternal assessment.
4. A fetal heart rate of 140 bpm with moderate variability indicates a reassuring fetus with adequate oxygenation. This finding suggests the fetoplacental unit is currently tolerating the maternal condition. Since the fetus is stable, this does not represent an immediate crisis. The nurse continues routine electronic fetal monitoring to detect future decelerations.
Test-taking strategy
- Prioritize the ABCs: Focus on Circulation. Choice 3 shows clear evidence of cardiovascular instability and decompensated shock.
- Identify the Most Unstable: Compare the symptoms. While bleeding (1) is the cause, the low blood pressure and high heart rate (3) describe the physiological effect that is life-threatening.
- Exclude Reassuring Data: Choice 4 (normal FHR) and Choice 2 (soft uterus) are stable findings and should be eliminated first.
- Distinguish Expected vs. Emergency: Choice 1 is expected for the diagnosis, but Choice 3 is a critical complication requiring immediate resuscitation.
Take home points
- Hypotension and tachycardia in a pregnant client signify late-stage hypovolemic shock due to significant blood loss.
- Placenta previa presents with painless, bright red bleeding and a non-tender, soft uterine wall.
- Normal fetal heart rate variability is the best indicator of fetal well-being during maternal hemorrhagic episodes.
- Maternal hemodynamic stability must be the priority to ensure adequate end-organ perfusion and fetal oxygenation.
A client diagnosed with complete placenta previa is admitted with minor bleeding. Which nursing action is most appropriate?
Explanation
Placenta previa is an obstetric complication resulting from the implantation of the placenta in the lower uterine segment, potentially obstructing the internal cervical os. This malpositioning makes the placental-decidual interface highly vulnerable to shearing forces as the lower segment thins during late pregnancy. Complete previa indicates total coverage of the os, necessitating a focus on uterine quiescence to prevent the transition from minor spotting to catastrophic, life-threatening maternal-fetal hemorrhage. Management is primarily conservative until fetal maturity is reached or maternal hemodynamic stability is compromised.
Rationale for correct answer
3. Maintaining bed rest and continuous fetal monitoring is the most appropriate action to promote mechanical stability of the placenta and ensure fetal well-being. Physical activity can increase the pressure on the cervix and trigger decidual bleeding, so restricting movement helps minimize the risk of placental shearing. Continuous fetal monitoring allows the nurse to detect occult hemorrhage through changes in fetal heart rate patterns, such as late decelerations or tachycardia. This expectant management strategy aims to prolong the pregnancy safely while maintaining a state of high vigilance.
Rationale for incorrect answers
1. Encouraging ambulation is contraindicated because the force of gravity and the mechanical movement of the pelvis increase the risk of placental detachment. In complete placenta previa, any pressure on the lower uterine segment can initiate profuse bleeding. Nursing care focuses on reducing uterine irritability and preventing cervical changes, making activity restriction a cornerstone of the care plan. Ambulation would only be considered once the diagnosis of previa is ruled out by ultrasound.
2. Performing a digital cervical examination is an absolute contraindication in the presence of suspected or confirmed placenta previa. Inserting fingers into the cervix can cause direct trauma to the placental tissue, leading to immediate, massive maternal hemorrhage and hypovolemic shock. Any assessment of the cervix in a bleeding third-trimester client must be performed via transvaginal ultrasound only. This procedure represents one of the most dangerous iatrogenic risks in obstetric nursing.
4. Administering oxytocin to stimulate contractions is dangerous and strictly prohibited in clients with placenta previa. Uterine contractions cause the cervical os to dilate and the lower segment to efface, which would tear the placenta away from its attachment site. This results in maternal exsanguination and severing of the fetal oxygen supply. Furthermore, because the placenta blocks the birth canal, a vaginal delivery is physically impossible and should never be attempted.
Test-taking strategy
- Identify the Core Contraindication: In placenta previa, the "Nothing per Vagina" rule is absolute. This immediately eliminates Choice 2.
- Assess Delivery Feasibility: Because the placenta is "complete" (covering the os), a vaginal birth is impossible. Therefore, any action to promote labor (Choice 4) is incorrect and life-threatening.
- Prioritize Stability: For a client with "minor bleeding," the goal is expectant management. This involves keeping the patient still (bed rest) and watching the baby (monitoring). Choice 3 is the only option that addresses both safety and surveillance.
- Rule out Activity: Ambulation (Choice 1) is generally encouraged in healthy pregnancies but is a major risk factor for bleeding in placental disorders.
Take home points
- Digital vaginal examinations are strictly prohibited in placenta previa to prevent catastrophic hemorrhage.
- Expectant management for stable placenta previa includes bed rest and continuous fetal monitoring.
- Oxytocin and other labor-inducing agents are contraindicated due to the risk of placental shearing and the physical obstruction of the birth canal.
- The primary clinical goal is to maintain hemodynamic stability while awaiting fetal lung maturity.
A nurse is teaching a client with placenta previa about activity restrictions. Which instruction is most accurate?
Explanation
Placenta previa occurs when the placenta develops in the lower uterine segment, necessitating strict adherence to pelvic rest protocols. This anatomical malpositioning places the highly vascular placental tissue directly over the cervical os, where mechanical friction or cervical manipulation can trigger profuse, life-threatening hemorrhage. Because the lower segment is thin and poorly contractile, any disruption to the placental-decidual interface results in bleeding that is difficult to control. Management focuses on preventing any activity that induces uterine irritability or direct cervical trauma.
Rationale for correct answer
1. The nurse must instruct the client to limit sexual activity and avoid heavy lifting to prevent mechanical stress on the cervix and lower uterine segment. Sexual intercourse is strictly prohibited because penile-cervical contact or female orgasm can stimulate uterine contractions and cause direct trauma to the low-lying placenta. Heavy lifting increases intra-abdominal pressure, which can lead to placental shearing and sudden hemorrhage. These restrictions are the cornerstone of home management for stable clients with this diagnosis.
Rationale for incorrect answers
2. Engaging in light jogging is contraindicated because the high-impact motion and repetitive jarring of the pelvic area can cause placental displacement and bleeding. While circulation is important, aerobic exercise in the context of placenta previa carries a high risk of triggering vascular shearing at the implantation site. The nurse should instead recommend non-stressful movements or gentle range-of-motion exercises that do not increase the risk of placental detachment. Jogging is never appropriate for a client requiring activity restriction.
3. Performing daily pelvic examinations at home is an extremely dangerous and incorrect instruction. Digital vaginal entry, whether performed by a clinician or the client, can puncture the placental mass and cause catastrophic, fatal hemorrhage. Clients are educated to avoid any insertion into the vagina, including tampons or fingers, to maintain the circulatory integrity of the placenta. The nurse must emphasize that any cervical assessment must only be performed by a physician using ultrasound in a hospital setting.
4. Increasing physical activity to reduce blood clots is inappropriate because the risk of hemorrhagic shock from placenta previa far outweighs the general risk of thromboembolism in a mobile client. While pregnancy is a hypercoagulable state, activity for a previa patient is strictly limited to prevent placental separation. To reduce the risk of clots without endangering the pregnancy, the nurse should suggest frequent position changes in bed and the use of anti-embolism stockings rather than increased physical exertion.
Test-taking strategy
- Identify the Condition: The diagnosis is placenta previa, which is a "bleeding risk" condition.
- Apply the "Pelvic Rest" Rule: In obstetric nursing, any condition involving placental malposition or bleeding requires the total avoidance of vaginal penetration and heavy strain. This confirms Choice 1.
- Eliminate High-Risk Activities: Choices 2 and 4 involve increased movement or impact. These are always incorrect for a client whose placental attachment is precarious and prone to shearing.
- Identify Safety Violations: Choice 3 is a major safety violation. A nurse would never instruct a patient to perform a pelvic exam on themselves, especially with a placenta previa diagnosis.
- Focus on Prevention: Choose the instruction that best prevents hemorrhage. Limiting sexual activity and lifting (1) is the standard evidence-based approach to home care.
Take home points
- Pelvic rest, including the avoidance of sexual intercourse and vaginal insertion, is mandatory for placenta previa.
- Heavy lifting and high-impact exercises are prohibited to prevent increased intra-abdominal pressure and placental shearing.
- Any occurrence of bright red vaginal bleeding at home requires immediate transport to the hospital via ambulance.
- Bed rest or modified activity is maintained to minimize the risk of preterm labor and emergency delivery.
A client with placenta previa at 32 weeks gestation is stable but experiencing intermittent bleeding. Which pharmacologic intervention should the nurse anticipate?
Explanation
Placenta previa involves the blastocyst implantation within the lower uterine segment, potentially obstructing the internal os. This maladaptation causes vascular shearing during cervical effacement, leading to profuse maternal hemorrhage. When bleeding occurs before 34 to 37 weeks, management focuses on prolonging the pregnancy to achieve fetal maturity while maintaining a high state of hemodynamic readiness. Pharmacologic strategies are directed toward enhancing the neonatal transition in anticipation of a high-probability preterm delivery.
Rationale for correct answer
2. Betamethasone is a corticosteroid administered to accelerate fetal lung maturity in cases of threatened preterm birth. For a client at 32 weeks, the nurse anticipates this intervention to stimulate the production of pulmonary surfactant by type 2 pneumocytes. This significantly reduces the risk of respiratory distress syndrome, intraventricular hemorrhage, and necrotizing enterocolitis in the neonate. The standard protocol involves 2 doses of 12 mg administered intramuscularly 24 hours apart.
Rationale for incorrect answers
1. Magnesium sulfate is not used for labor induction; rather, it is used for tocolysis (suppressing labor) or fetal neuroprotection before 32 weeks. Inducing labor in a client with placenta previa is strictly contraindicated because the placenta obstructs the birth canal, making vaginal delivery impossible and life-threatening. Using magnesium to induce contractions would be a pharmacological error that contradicts the goal of maintaining uterine quiescence.
3. Oxytocin is used to stimulate uterine contractions, which is an absolute contraindication for placenta previa. Stimulating the uterus would cause the cervix to dilate and the lower segment to efface, leading to catastrophic placental detachment and maternal-fetal exsanguination. Any medication that promotes labor must be avoided to prevent the onset of a hemorrhagic crisis. Cesarean section is the only safe delivery route for this condition.
4. Methylergonovine is an oxytocic ergot alkaloid used to treat postpartum hemorrhage, but it is not administered before delivery. Giving this medication to a pregnant client could cause tetanic uterine contractions, leading to immediate placental separation and fetal hypoxia. While it helps "prevent bleeding" in the postpartum period by constricting uterine vessels, its antenatal use would precipitate the exact emergency the medical team is trying to avoid.
Test-taking strategy
- Analyze the Gestational Age: The client is at 32 weeks, which is preterm. In high-risk obstetric scenarios, the priority for the baby is almost always lung maturity.
- Identify the Diagnosis: Placenta previa means the exit is blocked. Eliminate any drug that induces labor or contractions (1 and 3).
- Assess Drug Timing: Recognize that methylergonovine (4) is a postpartum drug. It is never used while the fetus is still in the uterus.
- Select the Standard Protocol: Choice 2 (betamethasone) is the gold-standard treatment for any risk of preterm delivery before 34–37 weeks.
Take home points
- Antenatal corticosteroids (Betamethasone) are the priority for fetal lung maturity in preterm placenta previa.
- Labor-inducing agents like oxytocin are strictly contraindicated due to the risk of catastrophic hemorrhage.
- Expectant management aims to stabilize the mother and prolong the pregnancy until at least 36 weeks.
- Maternal blood glucose monitoring is required when administering steroids, as they can cause transient hyperglycemia.
A nurse is reviewing the ultrasound of a client with placenta previa. The placenta partially covers the cervical os. Which type of placenta previa is this?
Explanation
Placenta previa is defined by the abnormal implantation of the placenta in the lower uterine segment, resulting in a physical relationship with the internal cervical os. This malpositioning is classified based on the degree of cervical occlusion identified during a transvaginal ultrasound. Pathophysiologically, as the lower uterine segment thins and the cervix undergoes effacement in the third trimester, the placental-decidual interface is disrupted, leading to the characteristic painless, bright red bleeding. Accurate classification is essential for determining the safety of expectant management versus the necessity of a scheduled cesarean delivery.
Rationale for correct answer
2. Partial previa occurs when the placenta partially covers the internal cervical os. This classification is identified via sonography when the leading edge of the placenta extends over a portion of the cervical opening but does not completely occlude it. Even a partial covering represents a significant mechanical obstruction that renders vaginal delivery unsafe. The partial coverage carries a high risk of maternal hemorrhage as the cervix begins to dilate during the onset of preterm labor.
Rationale for incorrect answers
1. Complete previa is characterized by the placental mass entirely covering the internal cervical os. In this scenario, the center or a large portion of the placenta lies directly over the opening, creating a total obstruction of the birth canal. This is the most severe form and carries the highest risk for catastrophic hemorrhage and placenta accreta. Because the os is fully occluded, there is no possibility of the fetus passing through the cervix without causing total placental detachment.
3. Marginal previa occurs when the edge of the placenta is located at the margin of the internal os but does not cover it. In this classification, the placental edge touches the border of the opening without extending across the space. While it still poses a risk for bleeding during the effacement process, it is anatomically distinct from a partial previa where the tissue actually crosses over the os. Current clinical guidelines often group marginal and low-lying placentas together for management purposes.
4. A low-lying placenta is identified when the placental edge is implanted in the lower uterine segment but is not touching the internal os. Specifically, the edge is typically located between 1 mm and 20 mm from the cervical margin. Unlike partial or complete previa, a low-lying placenta may allow for a trial of labor if the distance is ≥ 20 mm. This condition is often monitored for "placental migration" as the uterus expands upward during the third trimester.
Test-taking strategy
- Define the Terms: Use the literal definitions of the words. "Complete" means 100%, "Partial" means some but not all, and "Marginal" means just the edge.
- Match the Stem: The question states the placenta partially covers the os. This directly matches the definition of Choice 2.
- Use Process of Elimination: Rule out Choice 1 because the placenta does not fully cover the os. Rule out Choice 3 and 4 because they describe the placenta being near or at the edge, not actually covering any part of the opening.
- Focus on Anatomy: Visualize the internal os. If any part of the placental tissue is "on top" of the hole but the hole is still visible, it is partial.
Take home points
- Partial placenta previa involves the placental edge extending over a portion of the internal cervical os.
- Transvaginal ultrasound is the gold standard for classifying the degree of placental coverage.
- Any degree of placental coverage (partial or complete) necessitates delivery via cesarean section.
- Placental location can change as the lower uterine segment develops, a phenomenon known as placental migration.
A nurse is monitoring a client with placenta previa postpartum. Which finding requires urgent intervention?
Explanation
Placenta previa involves abnormal blastocyst implantation within the lower uterine segment, which lacks the robust, interlacing myometrial musculature found in the fundus. This anatomical deficiency prevents the "living ligatures" of the uterus from effectively constricting torn venous sinuses following placental expulsion. Consequently, the primary risk is immediate hypovolemic collapse due to ineffective hemostasis at the implantation site.
Rationale for correct answer
3. Saturation of perineal pads in 15 minutes with hypotension indicates decompensated shock secondary to catastrophic postpartum hemorrhage. In placenta previa, the lower segment often fails to contract (atony), leading to rapid exsanguination even if the fundus feels firm. Hypotension is a late sign of circulatory failure, suggesting a loss of ≥ 30% of total blood volume. The nurse must immediately initiate massive transfusion protocols and notify the surgical team for possible emergency hysterectomy or tamponade.
Rationale for incorrect answers
1. Lochia progressing from bright red to brown is an expected, normal finding during the puerperium. This transition from lochia rubra to lochia serosa typically occurs around the third or fourth day postpartum as the volume of blood decreases and the concentration of serous exudate and leukocytes increases. It indicates that the placental site is healing normally and that uterine involution is proceeding without complication. This finding does not require any clinical intervention.
2. A soft, contracted uterus is a contradictory description; however, a contracted uterus is the desired outcome after delivery. Effective myometrial contraction compresses the intrauterine vessels, which is the primary mechanism for preventing excessive blood loss. While a "soft" uterus (atony) is concerning, the term "contracted" implies hemostatic stability. If the fundus is firm and the patient is stable, this represents a reassuring assessment of the involution process.
4. A maternal temperature of 37°C (98.6°F) is a normal finding and indicates the absence of a febrile response or systemic infection. While the nurse monitors for postpartum endometritis, especially after a cesarean section for previa, a temperature within this range is not a cause for concern. It confirms that the patient's thermoregulation is intact and there is no immediate inflammatory crisis. No nursing intervention is required for this stable vital sign.
Test-taking strategy
- Prioritize the ABCs: Focus on Circulation. Choice 3 is the only option that describes an active failure of the circulatory system.
- Identify Quantitative Extremes: In maternity nursing, saturating a pad in 15 minutes is the universal "red flag" for hemorrhage.
- Recognize Late Signs: Hypotension is a late and ominous sign of shock in a young, pregnant patient who has a higher blood volume.
- Rule Out Normals: Choice 1 (lochia transition), Choice 2 (contracted uterus), and Choice 4 (normal temp) are all physiological goals and do not require intervention.
- Connect Pathology to Outcome: Link the diagnosis of previa directly to the risk of hemorrhage to confirm Choice 3.
Take home points
- Saturating a perineal pad in 15 minutes or less is a clinical emergency indicating primary postpartum hemorrhage.
- Hypotension and tachycardia are late indicators of hypovolemic shock due to the physiological expansion of blood volume in pregnancy.
- The lower uterine segment is less contractile than the fundus, increasing the risk of atony in clients with placenta previa.
- Immediate nursing actions for hemorrhage include fundal massage, administration of uterotonics, and rapid fluid resuscitation.
A nurse is educating a client with placenta previa on postpartum care. Which instruction is most appropriate?
Explanation
Placenta previa is an obstetric condition characterized by blastocyst implantation within the lower uterine segment, resulting in a proximity to or total coverage of the internal cervical os. This malpositioning subjects the thin, less contractile lower uterine segment to significant vascular stress during delivery. Unlike the uterine fundus, the lower segment lacks the dense, interlacing myometrial musculature required to effectively constrict blood vessels after placental detachment. This anatomical deficiency places the postpartum client at a sustained risk for delayed hemorrhage and necessitates meticulous monitoring of the placental site's involution and hemostatic integrity.
Rationale for correct answer
1. Reporting heavy or bright red vaginal bleeding immediately is the most appropriate instruction because of the high risk of secondary hemorrhage. In placenta previa, the lower uterine segment may not achieve sufficient vessel occlusion, leading to profuse bleeding even after the initial recovery period. Bright red blood signifies active arterial bleeding, which can rapidly progress to hypovolemic shock. Educating the client to recognize and report these symptoms ensures early clinical intervention and prevents life-threatening complications following discharge.
Rationale for incorrect answers
2. Resuming sexual activity as tolerated is an incorrect and dangerous instruction because clients with placenta previa or recent uterine surgery require a period of pelvic rest. Any vaginal penetration or orgasm can stimulate uterine contractions or cause mechanical trauma to the healing placental site in the lower uterine segment. Most providers recommend a minimum of 6 weeks of pelvic rest to ensure complete endometrial healing and closure of the cervix. Resuming activity too early increases the risk of both infection and hemorrhage.
3. Avoiding monitoring lochia unless instructed is inappropriate because lochia assessment is the primary method for the client to monitor their own recovery at home. The client should be taught to observe the color, amount, and odor of the discharge to detect signs of postpartum atony or endometritis. Failure to monitor lochia could lead to a delay in identifying a pathologic bleed. Standard nursing practice involves empowering the client to track their lochia progression from rubra to serosa as a marker of normal involution.
4. Engaging in strenuous exercise to prevent blood clots is contraindicated in the early postpartum period, especially after a high-risk delivery. While early ambulation (walking) is encouraged to prevent deep vein thrombosis, strenuous activity increases intra-abdominal pressure and can trigger primary or secondary uterine bleeding. Heavy exertion can disrupt the healing of the uterine vessels and the surgical incision if a cesarean was performed. The client should be advised to gradually increase activity based on their physical tolerance and provider guidance.
Test-taking strategy
- Identify the Primary Risk: Placenta previa's biggest threat is always hemorrhage, both antepartum and postpartum.
- Prioritize Safety: Choice 1 directly addresses the Circulation aspect of the ABCs and provides a clear safety boundary for the patient.
- Apply the 6-Week Rule: In postpartum care, "resuming activity" (2) and "strenuous exercise" (4) are almost always incorrect in the early weeks following a high-risk complication.
- Focus on Patient Empowerment: Any instruction that tells a patient to "avoid monitoring" (3) a vital sign or discharge is typically a distractor and should be eliminated.
- Analyze Medical Jargon: Use the term lochia rubra to identify that bright red bleeding (1) is what the patient must watch for.
Take home points
- The lower uterine segment is prone to atony after placenta previa delivery due to fewer muscle fibers.
- Bright red vaginal bleeding postpartum is a sentinel sign of hemorrhage and requires immediate evaluation.
- Pelvic rest is mandatory for 6 weeks postpartum to prevent trauma to the healing lower uterine segment.
- Lochia should naturally transition from red (rubra) to pink/brown (serosa) over the first week; any reversal requires medical attention.
A client with placenta previa is admitted in labor. Which maternal position promotes optimal uteroplacental perfusion?
Explanation
Placenta previa involves the blastocyst implantation within the lower uterine segment, potentially obstructing the internal os. This maladaptation causes vascular shearing during cervical effacement, leading to profuse maternal hemorrhage. When bleeding occurs, the physiological priority is maintaining the oxygen-carrying capacity of the mother to ensure fetal survival. In a gravid uterus, the physical mass of the fetus and placenta can compress the maternal inferior vena cava, leading to a reduction in cardiac output and placental blood flow.
Left lateral tilt is the most appropriate position because it achieves aortocaval decompression by shifting the heavy uterus away from the inferior vena cava and descending aorta. This optimization of maternal venous return enhances stroke volume and cardiac output, which directly increases the volume of oxygenated blood reaching the intervillous spaces of the placenta. Maintaining this position is a critical nursing intervention for any client with a placental disorder to prevent maternal hypotension and subsequent fetal hypoxia.
Rationale for incorrect answers
1. The supine position is contraindicated because it causes supine hypotensive syndrome due to the weight of the pregnant uterus compressing the great vessels against the vertebral column. This compression reduces venous return to the heart, leading to a drop in maternal blood pressure and a secondary decrease in uterine artery perfusion. In a client already compromised by the bleeding of a placenta previa, this position can rapidly lead to fetal bradycardia.
3. The Trendelenburg position, where the head is lower than the feet, is not typically used for uteroplacental perfusion and can actually impair maternal respiratory effort by pushing abdominal contents against the diaphragm. While it was historically used for cord prolapse, it does not specifically address the hemodynamic needs of a client with placenta previa. Furthermore, it can increase intracranial pressure and is uncomfortable for the laboring client.
4. High Fowler's position involves sitting the client upright at a 60–90 degree angle, which increases gravitational pressure on the lower uterine segment and cervix. In placenta previa, this increased pressure can exacerbate placental shearing and increase the volume of vaginal bleeding. While this position may assist with maternal breathing, it is not the optimal choice for maximizing blood flow to the placenta compared to a lateral tilt.
Test-taking strategy
- Identify the Physiological Goal: The question asks for "optimal uteroplacental perfusion." This is a keyword for circulation and blood flow.
- Recall Pregnancy Anatomy: Remember that the heavy uterus compresses the vena cava when the mother is flat. The solution is always to tilt or turn the patient.
- Select the Standard of Care: Left lateral (2) is the "gold standard" position for improving blood flow to the baby in almost all obstetric emergencies.
- Eliminate Risks: Supine (1) is always a risk for hypotension. High Fowler's (4) increases pressure on the cervix, which is dangerous in previa.
Take home points
- Left lateral tilt prevents aortocaval compression, maximizing maternal cardiac output and placental perfusion.
- The supine position must be avoided to prevent supine hypotensive syndrome and fetal distress.
- Maintaining optimal maternal position is a non-invasive way to improve fetal oxygenation during hemorrhagic episodes.
- In placenta previa, avoiding upright positions reduces gravitational stress on the fragile lower uterine segment.
A nurse is planning care for a client with placenta previa. Which interventions are appropriate? Select all that apply
Explanation
Placenta previa involves abnormal blastocyst implantation within the lower uterine segment, potentially obstructing the internal cervical os. This malpositioning subjects the low-lying, fragile vascular network to mechanical shearing forces during cervical effacement or lower segment thinning, resulting in characteristic painless hemorrhage. Unlike other obstetric hemorrhages, this bleeding is primarily maternal in origin and occurs without the stimulus of uterine contractions or trauma, often requiring careful hemodynamic monitoring.
Rationale for correct answers
1. Avoiding all vaginal examinations is the most critical intervention to prevent iatrogenic hemorrhage in a client with placenta previa. Inserting fingers into the cervix can cause mechanical disruption of the placental-decidual interface, leading to immediate and massive maternal blood loss. Any assessment of cervical status must be performed via transvaginal ultrasound by a qualified provider. This precaution maintains the anatomical integrity of the placental attachment.
2. Continuous external fetal heart rate monitoring is essential to assess fetal tolerance of uterine activity and potential occult bleeding. Placenta previa increases the risk of placental insufficiency and fetal hypoxia if the placental surface area begins to detach. Continuous data allow for the immediate detection of late decelerations or fetal tachycardia, which are early indicators of fetal jeopardy. This ensures a rapid response to any decline in fetal oxygenation.
4. Maintaining IV access with a large-bore catheter (18 gauge or larger) is a vital safety measure for rapid volume resuscitation. Placenta previa can cause sudden, profuse bleeding that leads to hypovolemic shock within minutes. A patent, large-diameter intravenous line allows for the high-volume administration of isotonic crystalloids or blood products. This intervention is foundational for maintaining maternal hemodynamic stability during an acute hemorrhagic event.
5. Monitoring vaginal bleeding frequently allows the nurse to quantify maternal blood loss and assess the severity of the previa. The nurse should track the number of peripads used and the color of blood, as bright red indicates fresh arterial bleeding. Frequent assessment is necessary to identify the transition from stable spotting to active hemorrhage. This data is critical for determining the timing of emergency surgical intervention.
Rationale for incorrect answers
3. Encouraging ambulation to speed labor is strictly contraindicated because physical activity and gravity increase the pressure on the lower segment, potentially triggering massive bleeding. Furthermore, labor is not desired in a client with a confirmed previa because vaginal delivery is physically obstructed and dangerous. Management focuses on uterine quiescence and pelvic rest to prevent placental shearing. Accelerating labor in this context would lead to catastrophic placental detachment.
Test-taking strategy
- Identify the Diagnosis: The client has placenta previa, which is a high-alert condition for life-threatening hemorrhage.
- Prioritize Safety Constraints: Use the "Nothing per Vagina" rule. Choice 1 is a mandatory safety action.
- Assess for Hemorrhagic Risk: Any intervention that prepares for or monitors bleeding is a priority. This validates Choice 4 (IV access) and Choice 5 (bleeding assessment).
- Fetal Surveillance: In a placental disorder, the fetus is at risk for hypoxia. Continuous monitoring (Choice 2) is a standard of care.
- Eliminate Harmful Actions: Choice 3 (ambulation) encourages the very thing the nurse must prevent: labor and mechanical stress on the placenta. Eliminate this option immediately.
Take home points
- Digital vaginal examinations are strictly prohibited in the presence of placenta previa to avoid triggering massive hemorrhage.
- Large-bore IV access and blood type-and-crossmatch are the most important preparations for maternal resuscitation.
- Continuous electronic fetal monitoring is required to detect early signs of fetal hypoxia secondary to placental separation.
- Any intervention that stimulates or accelerates labor is contraindicated due to the risk of catastrophic placental detachment.
A nurse is providing discharge teaching for a client with placenta previa. Which instructions should be included? Select all that apply
Explanation
Placenta previa involves abnormal blastocyst implantation within the lower uterine segment, potentially obstructing the internal cervical os. This malpositioning subjects the low-lying, fragile vascular network to mechanical shearing forces during cervical effacement or lower segment thinning, resulting in characteristic painless hemorrhage. Unlike other obstetric hemorrhages, this bleeding is primarily maternal in origin and occurs without the stimulus of uterine contractions or trauma, often requiring careful hemodynamic monitoring and strict activity restrictions.
Rationale for correct answers
1. Reporting any bright red vaginal bleeding immediately is a vital instruction because it is the primary indicator of placental separation. In placenta previa, bleeding can escalate from a minor "warning leak" to a catastrophic hemorrhage within minutes. Early notification allows for immediate hospital admission and potentially life-saving surgical intervention. The nurse must emphasize that even painless bleeding is a medical emergency in this context.
2. Avoiding sexual intercourse until cleared by the primary health care provider is essential to maintain pelvic rest. Penile-cervical contact or the uterine contractions associated with orgasm can cause mechanical disruption of the placental-decidual interface. This trauma triggers immediate maternal bleeding and compromises the integrity of the placental attachment. Pelvic rest is a non-negotiable component of home management for stable previa.
4. Maintaining scheduled prenatal follow-up visits is necessary for the ongoing sonographic monitoring of placental location. As the lower uterine segment grows, a phenomenon known as "placental migration" may occur, where the placenta appears to move upward and away from the os. Regular visits ensure that the delivery plan is updated based on the most current anatomical relationship between the placenta and the cervix. These visits also allow for the assessment of fetal growth and maternal hematologic status.
Rationale for incorrect answers
3. Engaging in heavy lifting to prevent placental displacement is a dangerous and incorrect instruction. Heavy lifting increases intra-abdominal pressure, which can exert downward force on the uterus and trigger placental shearing. There is no physiological mechanism by which lifting "prevents" displacement; rather, it is a known trigger for acute hemorrhagic episodes. Clients with previa are typically restricted from lifting anything heavier than 10 pounds.
5. Resuming normal physical activity immediately is contraindicated because high-impact or strenuous movement increases the risk of uterine irritability. Clients with placenta previa are usually placed on modified bed rest or restricted activity to minimize mechanical stress on the lower uterine segment. Resuming normal activities, such as jogging or vigorous exercise, could lead to a sudden detachment of the placenta. Activity levels must be increased only under the strict guidance of a healthcare provider.
Test-taking strategy
- Identify the Priority Concern: For placenta previa, the primary goal is preventing hemorrhage.
- Apply the "Pelvic Rest" Principle: This rule prohibits anything in the vagina and any heavy strain. Choices 1 and 2 directly support this principle.
- Evaluate Safety Boundaries: Choice 3 (heavy lifting) and Choice 5 (normal activity) increase mechanical risk. These should be eliminated as they could cause harm.
- Determine Clinical Necessity: Choice 4 (follow-up) is a standard safety measure for high-risk pregnancies to monitor for changes in condition.
- Select All That Apply: Ensure your final selections (1, 2, 4) focus on risk reduction and clinical surveillance.
Take home points
- Bright red vaginal bleeding must be reported immediately as it signifies active placental detachment.
- Pelvic rest, including the total avoidance of sexual intercourse, is mandatory to prevent mechanical trauma to the placenta.
- Heavy lifting is strictly prohibited as it increases intra-abdominal pressure and the risk of hemorrhage.
- Serial ultrasounds are required during follow-up to track placental location and plan the mode of delivery.
A nurse is caring for a client with placenta previa experiencing mild bleeding. Which interventions are appropriate? Select all that apply
Explanation
Placenta previa involves the abnormal implantation of the placenta in the lower uterine segment, potentially obstructing the internal cervical os. This malpositioning places the highly vascular placental tissue in a zone prone to mechanical shearing during cervical changes, resulting in characteristic painless, bright red hemorrhage. Because the lower segment lacks the robust myometrial thickness of the fundus, it cannot effectively compress vessels once they begin to bleed, making hemodynamic stability a primary clinical concern. Management focuses on minimizing uterine irritability and maintaining optimal placental perfusion.
Rationale for correct answers
1. Placing the client in a left lateral tilt is appropriate to optimize aortocaval decompression. In late pregnancy, the gravid uterus can compress the inferior vena cava and aorta when the client is supine, reducing cardiac output and placental blood flow. Shifting the uterine mass to the left enhances venous return to the heart, thereby maximizing the delivery of oxygenated blood to the fetus. This positioning is a fundamental nursing intervention to prevent maternal hypotension and secondary fetal hypoxia during bleeding episodes.
2. Monitoring vital signs and fetal heart rate is essential for the early detection of hemodynamic compromise. Tachycardia is often the first maternal sign of circulatory depletion, occurring before a significant drop in blood pressure. Continuous fetal heart rate monitoring allows the nurse to identify late decelerations or a loss of variability, which are indicators of placental insufficiency. These assessments provide the clinical data necessary to determine if expectant management remains safe or if immediate delivery is required.
4. Encouraging bed rest and pelvic rest is a mandatory intervention to reduce mechanical stress on the lower uterine segment. Physical activity and gravity can increase the pressure on the cervix, potentially triggering further placental detachment and bleeding. Pelvic rest, which includes the absolute avoidance of vaginal penetration, protects the fragile placental-decidual interface from iatrogenic trauma. This strategy aims to maintain uterine quiescence and prolong the pregnancy until fetal lung maturity is achieved.
Rationale for incorrect answers
3. Preparing for emergency cesarean delivery immediately is inappropriate for a client experiencing only mild bleeding and who is otherwise stable. Current obstetric guidelines favor expectant management for stable previa to allow for maximum fetal development and the administration of antenatal corticosteroids. Immediate surgical intervention is reserved for cases of profuse hemorrhage, maternal shock, or non-reassuring fetal status. Jumping to an emergency delivery without clinical necessity increases the risks associated with prematurity and unnecessary surgical complications.
5. Performing a digital vaginal examination to assess cervical dilation is an absolute contraindication and a major safety violation in placenta previa. Inserting fingers into the cervix can cause direct trauma to the placenta, leading to sudden, catastrophic maternal hemorrhage and fetal death. Any assessment of the cervix must be performed strictly via transvaginal ultrasound by a qualified provider. The "nothing per vagina" rule is the most critical safety boundary for a nurse managing this condition.
Test-taking strategy
- Identify Clinical Status: The stem specifies mild bleeding, which suggests the client is currently stable and appropriate for expectant management.
- Prioritize Perfusion: Choice 1 (tilt) is a standard intervention to maximize blood flow to the placenta, supporting the ABCs (Circulation).
- Assess Monitoring Needs: Choice 2 is a universal priority for any high-risk obstetric patient to detect early signs of decline.
- Apply Safety Constraints: Identify Choice 5 (vaginal exam) as an absolute "Never Event" in placenta previa and eliminate it immediately.
- Differentiate Urgency: Choice 3 (emergency C-section) is too aggressive for "mild" bleeding. The nurse should be prepared, but it is not an immediate action unless stability is lost.
- Promote Stability: Choice 4 (rest) is the hallmark of conservative treatment for placental disorders.
Take home points
- Left lateral positioning maximizes maternal cardiac output and fetal oxygenation by relieving pressure on the great vessels.
- Digital vaginal examinations are strictly prohibited in placenta previa to prevent life-threatening iatrogenic hemorrhage.
- Expectant management involves bed rest and intensive monitoring to prolong the pregnancy for fetal benefit.
- Maternal tachycardia and fetal heart rate changes are earlier indicators of blood loss than a drop in maternal blood pressure.
A nurse is caring for a neonate born at 33 weeks due to maternal placenta previa. Which interventions are appropriate? Select all that apply
Explanation
Placenta previa often necessitates iatrogenic preterm delivery if maternal hemorrhage or fetal distress occurs. Neonates born at 33 weeks are classified as moderate-to-late preterm and lack the physiological maturity of term infants. These infants have significant deficits in pulmonary surfactant production, brown fat stores for non-shivering thermogenesis, and hepatic glycogen reserves. Consequently, the neonate is susceptible to a cascade of metabolic and respiratory failures. Nursing interventions must focus on extrauterine stabilization and close surveillance of the respiratory and metabolic systems to prevent long-term morbidity.
Rationale for correct answers
1. Monitoring blood glucose for hypoglycemia is appropriate because 33-week neonates have limited glycogen stores and a higher metabolic rate. These infants are often unable to maintain stable glucose levels (typically ≥ 40 to 45 mg/dL) due to their immature liver function and the stress of preterm birth. Undetected hypoglycemia can lead to neurological injury or seizures. The nurse must perform serial heel stick measurements to ensure metabolic stability during the transition period.
2. Assessing for respiratory distress syndrome is a priority because surfactant production is typically insufficient before 34 to 35 weeks. The nurse must monitor for clinical signs such as nasal flaring, grunting, intercostal retractions, and cyanosis. These symptoms indicate that the alveoli are collapsing at the end of expiration, leading to impaired gas exchange. Early identification allows for interventions such as Continuous Positive Airway Pressure (CPAP) or exogenous surfactant administration.
4. Maintaining thermoregulation in an incubator is essential because preterm neonates have a high surface-area-to-mass ratio and minimal subcutaneous fat. At 33 weeks, the infant cannot effectively regulate body temperature and is prone to cold stress, which increases oxygen consumption and glucose utilization. A neutral thermal environment provided by an isolette or radiant warmer prevents the infant from diverting energy away from growth and healing to maintain heat. This is a foundational component of preterm neonatal care.
5. Notifying the NICU team for high-risk preterm care is necessary to ensure the presence of specialized personnel at the time of delivery. A 34-week or younger neonate is at high risk for neonatal depression and requires advanced resuscitation skills. The NICU team provides the expertise needed for endotracheal intubation, umbilical line placement, and intensive monitoring that exceeds the capabilities of a standard newborn nursery. Coordination of care between the obstetric and neonatal teams is vital for optimizing outcomes.
Rationale for incorrect answers
3. Encouraging immediate breastfeeding without monitoring is inappropriate for a 33-week neonate. Infants born before 34 weeks often lack the coordinated suck-swallow-breathe reflex required for safe oral feeding. Attempting to breastfeed without assessment increases the risk of aspiration pneumonia and significant energy expenditure that the infant cannot afford. Initial feedings are usually provided via an orogastric or nasogastric tube until the infant demonstrates the developmental readiness for nipple feedings.
Test-taking strategy
- Identify the Gestational Age: The key detail is 33 weeks. This indicates a preterm infant with specific physiological needs.
- Prioritize the ABCs: Choice 2 (Respiratory) and Choice 4 (Thermoregulation/Circulation) address the immediate survival needs of a preterm neonate.
- Assess Metabolic Risk: Preterm babies are "small and cold," which leads to low sugar. This makes Choice 1 a standard priority.
- Consider Resource Management: Choice 5 is a proactive safety step to ensure the correct level of care is available for a high-risk birth.
- Eliminate Unsafe Practices: Choice 3 is unsafe because it ignores the neurological immaturity of a 33-week infant's feeding reflex.
Take home points
- Respiratory distress syndrome is a primary risk for 33-week neonates due to insufficient pulmonary surfactant.
- Preterm infants require intensive thermoregulation to prevent cold stress and metabolic exhaustion.
- Blood glucose must be monitored closely in preterm neonates to prevent hypoglycemia-related neurological damage.
- Coordination with the NICU team is mandatory for all deliveries occurring before 34 to 35 weeks gestation.
Exams on Placenta Previa
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Definition And Classification
- Epidemiology And Risk Factors
- Practice Exercise 1
- Pathophysiology
- Clinical Manifestations
- Practice Exercise 2
- Diagnostic Evaluation
- Practice Exercise 3
- Management And Interventions
- Practice Exercise 4
- Intrapartum Care
- Postpartum Care
- Complications
- Practice Exercise 5
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define placenta previa as a placental implantation anomaly in which the placenta is positioned partially or completely over the internal cervical os, and differentiate between complete, partial, marginal, and low-lying types.
- Describe maternal risk factors including advanced maternal age, multiparity, previous cesarean delivery, and smoking.
- Explain the abnormal implantation of the placenta in the lower uterine segment and the physiological mechanisms leading to maternal hemorrhage.
- Identify hallmark clinical signs of placenta previa, including painless bright red vaginal bleeding, uterine tone characteristics, and vital sign changes.
- Explain the role of maternal history and physical assessment in identifying placenta previa.
- Describe expectant management strategies including activity restrictions, monitoring of maternal-fetal status, and hospitalization criteria.
- Implement maternal monitoring techniques including vital signs, uterine activity assessment, and signs of hemorrhage.
- Monitor maternal status for postpartum hemorrhage, hemodynamic instability, and signs of infection.
- Implement interventions to manage postpartum hemorrhage, including pharmacologic and mechanical measures.
- Recognize neonatal considerations, including risk for preterm birth complications and respiratory distress syndrome.
- Identify maternal complications associated with placenta previa, including hemorrhagic shock, anemia, and need for blood transfusions.
- Apply knowledge of placenta previa pathophysiology, clinical presentation, diagnostics, and management to answer NCLEX-style questions that integrate critical thinking, clinical judgment, and prioritization of care.
Introduction
- Placenta previa is a significant obstetric complication characterized by placental implantation in the lower uterine segment, partially or completely covering the internal cervical os.
- This condition is a major cause of painless third-trimester vaginal bleeding and can lead to maternal and fetal morbidity if not promptly identified and managed.
- Placenta previa interferes with normal fetal descent and delivery, often necessitating cesarean delivery depending on the type and severity.
- The condition is differentiated from abruptio placentae, in which the placenta prematurely separates from the uterine wall, often causing painful bleeding and uterine tenderness.
- Early detection through ultrasound imaging and risk assessment is critical to prevent complications such as maternal hemorrhage, preterm birth, and fetal hypoxia.
- Management focuses on maternal stabilization, fetal monitoring, and timing of delivery according to gestational age and maternal-fetal status.
Definition And Classification
1.1 Definition of Placenta Previa
- Placenta previa is defined as the implantation of the placenta in the lower uterine segment in a manner that partially or completely covers the internal cervical os.
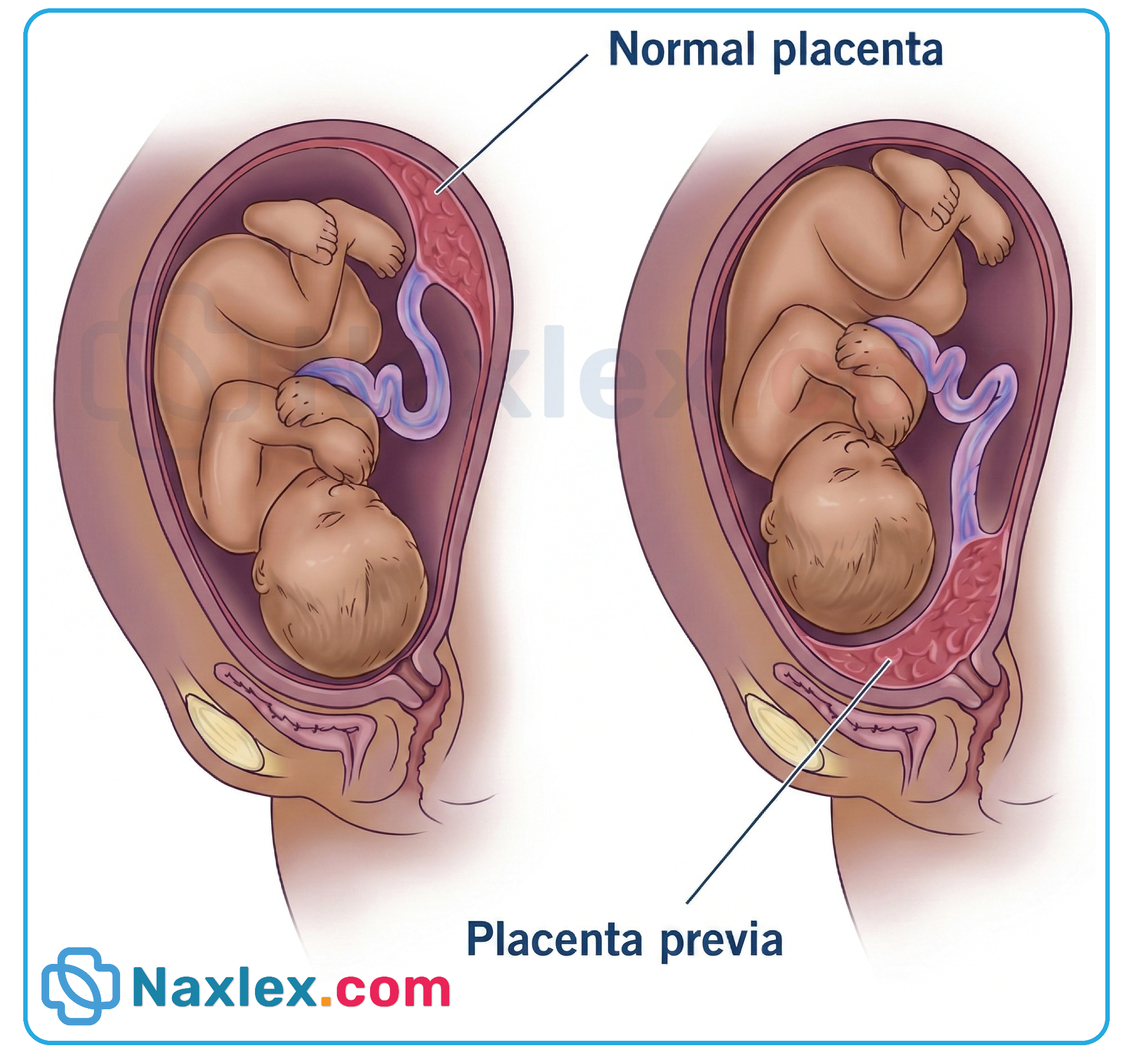
- It is considered a third-trimester obstetric complication and a leading cause of painless antepartum bleeding.
- Clinical significance: The proximity of the placenta to the cervical os increases the risk of maternal hemorrhage during the third trimester or labor.
- Pathophysiology:
- Abnormal placental implantation in the decidualized lower uterine segment disrupts normal vascularization.
- The lower segment is less muscular, predisposing to incomplete uterine contraction after bleeding episodes.
1.2 Types of Placenta Previa
|
Type |
Description |
Clinical Implication |
|
Complete Previa |
Placenta completely covers the cervical os |
High risk of severe antepartum bleeding; cesarean delivery required |
|
Partial Previa |
Placenta partially covers the cervical os |
May still obstruct vaginal delivery; cesarean often required |
|
Marginal Previa |
Placental edge reaches the margin of the cervical os |
Vaginal delivery sometimes possible; monitor closely |
|
Low-Lying Placenta |
Placental edge lies within 2 cm of cervical os but does not cover it |
May migrate upward as pregnancy progresses; usually resolves by third trimester |
1.3 Nursing Insights
- Nursing Assessment: Monitor for painless bright red vaginal bleeding, uterine tone, and maternal vital signs.
- Clinical Considerations: Avoid digital vaginal examinations unless cesarean delivery is imminent to prevent exacerbation of bleeding.
- Patient Education: Advise clients to report any vaginal bleeding immediately, maintain pelvic rest, and avoid heavy lifting or sexual intercourse.
- Fetal Monitoring: Continuous non-stress tests (NSTs) and ultrasound evaluations to assess growth and well-being are essential.
- Anticipatory Guidance: Prepare for possible preterm cesarean delivery depending on gestational age and severity of bleeding.
Epidemiology And Risk Factors
1.1 Incidence and Prevalence
- Occurs in ~0.5–1% of all pregnancies.
- Incidence has increased with rising cesarean section rates and advanced maternal age.
- More common in multiparous women and those with a history of placental complications.
1.2 Maternal Risk Factors
- Advanced maternal age (>35 years)
- Multiparity (more than 2 prior births)
- History of cesarean section or other uterine surgery
- Smoking or substance use
- Previous placenta previa or placental abruption
1.3 Obstetric Risk Factors
- Multiple gestations (twins, triplets)
- Abnormal uterine anatomy (fibroids, septate uterus)
- Previous uterine curettage or myomectomy
- Assisted reproductive technology pregnancies
1.4 Nursing Insights
- Risk Assessment: Identify clients with high-risk profiles early in pregnancy to schedule targeted ultrasound evaluations.
- Education and Counseling: Discuss modifiable risk factors, such as smoking cessation, and educate about warning signs of bleeding.
- Monitoring: Frequent monitoring for antepartum bleeding, fetal growth restriction, and maternal hemodynamic instability.
- Collaboration: Work closely with the primary health care provider to plan timing of delivery and ensure availability of blood products for potential hemorrhage.
Pathophysiology
1.1 Placental Implantation Abnormalities
- Definition: Placental implantation abnormalities occur when the placenta attaches improperly to the uterine wall. In placenta previa, the placenta implants in the lower uterine segment, which may partially or completely cover the internal cervical os.
- Normal Placental Implantation: Normally, the placenta implants in the upper uterine segment (fundus), where vascularity and muscularity support placental growth and uterine contractions at term.
- Abnormal Implantation in Placenta Previa:
- The lower uterine segment is less muscular and has poor contractility, predisposing to hemorrhage.
- Vascular connections in the lower segment are fragile and easily disrupted during uterine expansion or cervical dilation.
- Types of abnormal implantation:
- Complete Previa: Placenta entirely covers the cervical os.
- Partial Previa: Placenta partially covers the cervical os.
- Marginal Previa: Placenta touches the edge of the cervical os.
- Low-Lying Placenta: Placental edge is within 2 cm of the os but does not cover it.
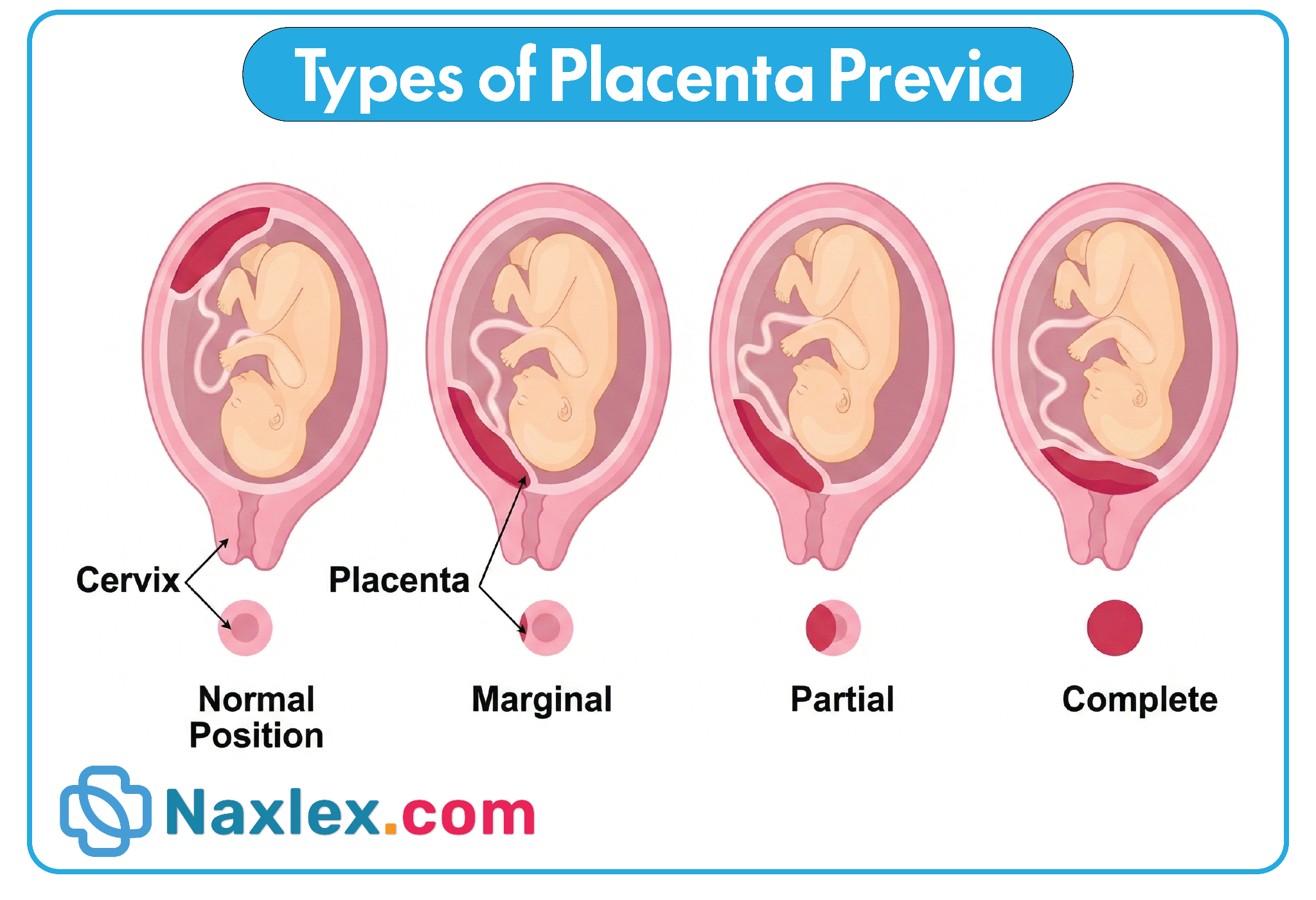
Nursing Insights – Placental Implantation Abnormalities
- Risk Assessment: Clients with a history of cesarean delivery, uterine surgery, or multiparity are at higher risk.
- Monitoring: Early ultrasound screening at 18–20 weeks can identify abnormal implantation and guide surveillance.
- Patient Education: Advise clients to report any vaginal bleeding and avoid digital cervical exams unless delivery is imminent.
- Practical Nursing Application: Prepare for possible cesarean delivery if placenta remains over the os near term.
1.2 Mechanisms Leading to Bleeding
- Primary Cause: Bleeding occurs due to disruption of fragile vessels in the lower uterine segment as the uterus stretches in the third trimester or cervix begins to efface and dilate.
- Characteristics of Bleeding:
- Painless, bright red vaginal bleeding (distinct from abruptio placentae, which is painful).
- Can be intermittent or sudden and vary from mild spotting to profuse hemorrhage.
- Pathophysiological Mechanism:
- Uterine growth stretches the lower segment, causing shearing of placental villi.
- Contractions may further disrupt vessels, increasing blood loss.
- Hemorrhage is usually external but can occasionally be concealed.
Nursing Insights – Mechanisms Leading to Bleeding
- Maternal Monitoring: Frequent vital signs checks, particularly blood pressure, heart rate, and oxygen saturation, to detect early signs of hypovolemia.
- Fetal Monitoring: Continuous non-stress tests (NSTs) or biophysical profiles to assess fetal oxygenation during bleeding episodes.
- Emergency Preparedness: Have IV access, blood products, and emergency cesarean kit ready.
1.3 Maternal and Fetal Hemodynamic Changes
- Maternal Hemodynamic Changes:
- Acute blood loss leads to hypovolemia, tachycardia, hypotension, and potential shock if not managed.
- Compensatory mechanisms include vasoconstriction, increased cardiac output, and tachypnea.
- Severe hemorrhage can result in disseminated intravascular coagulation (DIC).
- Fetal Hemodynamic Changes:
- Reduced uteroplacental perfusion leads to fetal hypoxemia and acidosis.
- Chronic or repeated bleeding episodes may cause intrauterine growth restriction (IUGR).
- Acute hemorrhage can lead to preterm delivery or fetal demise.
Nursing Insights – Maternal and Fetal Hemodynamic Changes
- Maternal Nursing Care:
- Maintain large-bore IV access for fluid resuscitation.
- Monitor urine output hourly as a marker of perfusion.
- Prepare for blood transfusion if hemorrhage is significant.
- Fetal Nursing Care:
- Continuous electronic fetal monitoring to detect late decelerations, decreased variability, or bradycardia.
- Prepare for emergency cesarean delivery if fetal compromise occurs.
- Patient Safety: Ensure the client remains on bed rest with pelvic rest to minimize risk of further bleeding.
Clinical Manifestations
1.1 Typical Symptoms
- Painless vaginal bleeding during the second or third trimester, often bright red and intermittent.
- No uterine tenderness or rigidity, differentiating it from abruptio placentae.
- May occur after sexual intercourse or uterine activity.
- Bleeding can resolve spontaneously or recur unpredictably.
Nursing Insights – Typical Symptoms
- Educate clients to report any vaginal bleeding immediately.
- Avoid digital or speculum exams unless delivery is indicated.
- Monitor hemodynamic stability, even if bleeding seems minor.
1.2 Maternal Complications
- Hemorrhagic shock due to rapid blood loss.
- Anemia from chronic or acute bleeding episodes.
- Disseminated intravascular coagulation (DIC) in severe cases.
- Need for blood transfusion or hysterectomy in cases of uncontrolled bleeding.
- Emotional stress and anxiety related to hospitalization and risk of preterm delivery.
1.3 Fetal Complications
- Preterm birth due to early cesarean delivery.
- Hypoxia and acidosis secondary to maternal blood loss and decreased placental perfusion.
- Intrauterine growth restriction (IUGR) with repeated bleeding episodes.
- Fetal demise in severe, uncontrolled hemorrhage.
1.4 Nursing Insights – Maternal and Fetal Complications
- Maternal Monitoring: Frequent vital signs, pulse oximetry, and lab work (hemoglobin, hematocrit, coagulation profile).
- Fetal Monitoring: Continuous NST or biophysical profile for fetal well-being.
- Psychosocial Support: Provide emotional support and patient education regarding bed rest, hospitalization, and potential preterm delivery.
- Emergency Preparedness: Ensure blood products, oxygen, and surgical team availability for acute hemorrhage.
Diagnostic Evaluation
1.1 Medical History and Risk Assessment
- Purpose: To identify risk factors and history that may predispose the client to placenta previa.
- Key Components of History:
- Obstetric history: Number of pregnancies, parity, history of placenta previa in previous pregnancies.
- Surgical history: Previous cesarean deliveries, uterine surgeries (myomectomy, curettage).
- Maternal factors: Advanced maternal age (>35 years), multiparity, smoking, cocaine or other drug use.
- Current pregnancy: Episodes of vaginal bleeding, gestational age at onset, associated symptoms (pain, cramping, contractions).
- Family history: Rarely relevant but may note placental anomalies.
Nursing Insights – Medical History and Risk Assessment
- Obtain precise details of bleeding onset, amount, and color; these can differentiate placenta previa from abruptio placentae.
- Ask about activity or trauma preceding bleeding, as minor trauma may precipitate bleeding in placenta previa.
- Assess medication use, including anticoagulants, which can exacerbate hemorrhage risk.
- Document frequency and severity of previous obstetric complications, including preterm labor or hemorrhage.
1.2 Physical Examination Considerations
- General Assessment:
- Vital signs: Monitor for hypotension, tachycardia, or signs of shock.
- Skin and mucous membranes: Look for pallor or signs of anemia.
- Abdominal Examination:
- Assess fundal height to determine gestational age correlation.
- Evaluate uterine tone; in placenta previa, uterus is usually soft and non-tender, unlike abruptio placentae which is firm and rigid.
- Palpate fetal presentation and position.
- Pelvic Examination:
- Contraindicated unless delivery is imminent, as digital vaginal examination may precipitate life-threatening hemorrhage.
- Fetal Assessment:
- Auscultate fetal heart tones; monitor for variability, decelerations, or bradycardia indicating fetal compromise.
Nursing Insights – Physical Examination
- Avoid digital cervical exams to prevent triggering massive hemorrhage.
- Use external fetal monitoring to track fetal heart rate and uterine activity.
- Maintain IV access prior to any potentially invasive assessment.
- Document bleeding episodes accurately with quantified peripads or collection devices.
1.3 Ultrasound Evaluation
- Transabdominal Ultrasound (TAS):
- First-line imaging modality for placental localization.
- Allows assessment of placental location, fetal growth, amniotic fluid volume, and umbilical cord insertion.
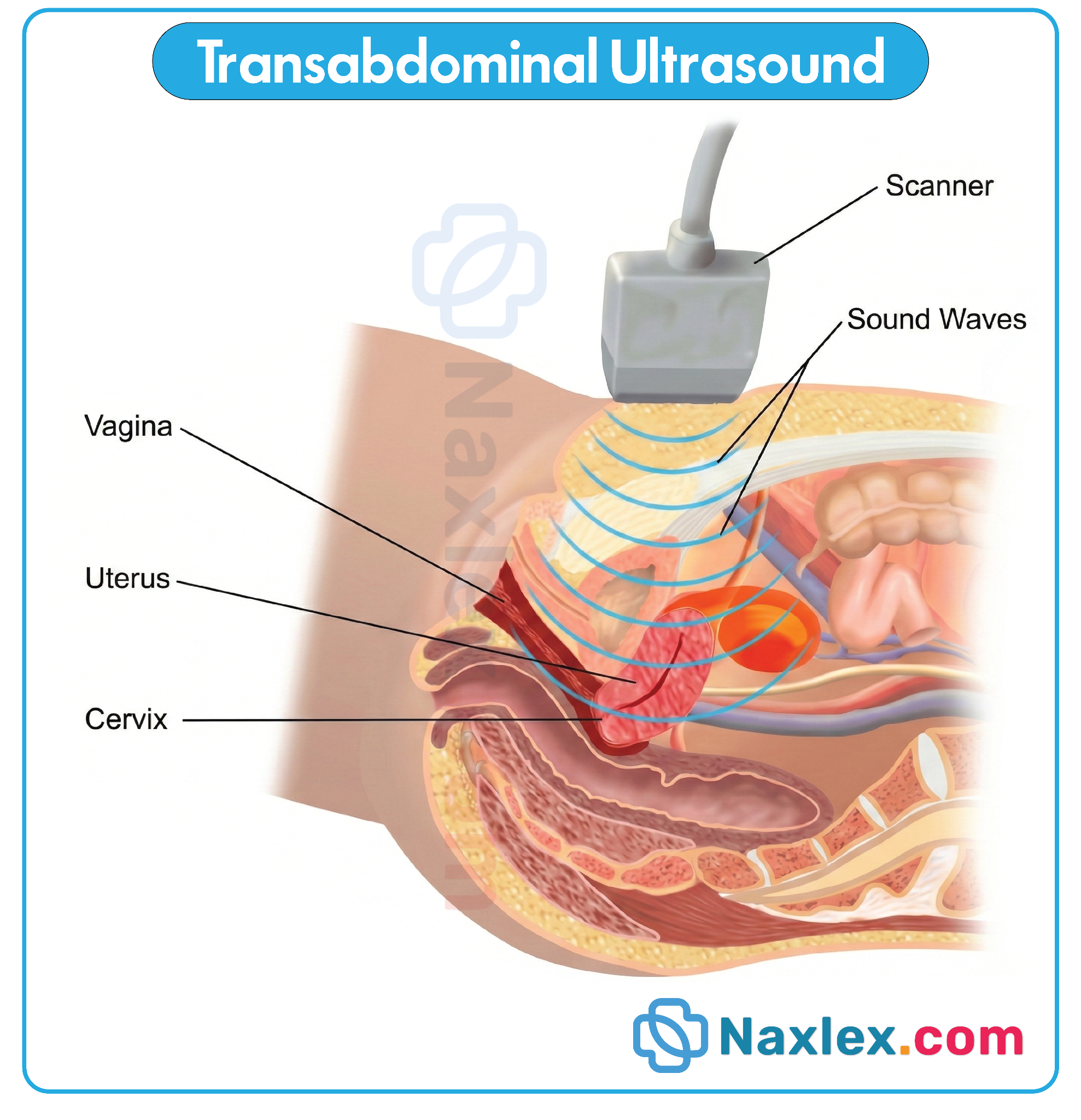
- Transvaginal Ultrasound (TVS):
- More sensitive and accurate for identifying low-lying or marginal placenta previa.
- Can be performed safely in experienced hands if precautions taken and no active heavy bleeding.
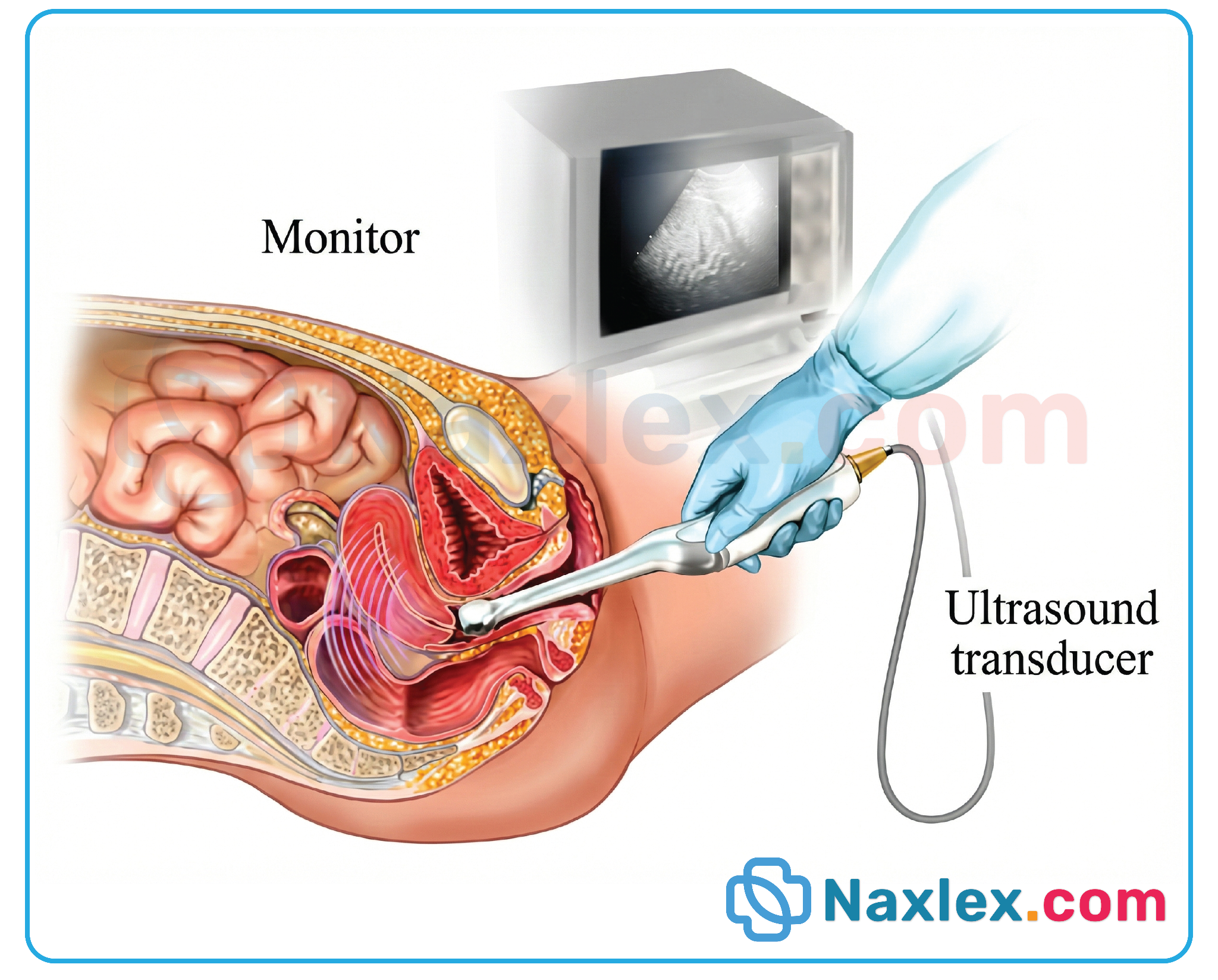
- Doppler Ultrasound:
- Used to assess umbilical artery flow and detect compromised placental perfusion.
- MRI:
- Considered when placenta accreta spectrum is suspected, especially for surgical planning.
Table: Comparison of Ultrasound Modalities in Placenta Previa
|
Modality |
Advantages |
Limitations |
Clinical Use |
|
Transabdominal (TAS) |
Non-invasive, widely available |
Less sensitive in late pregnancy or obese patients |
Initial screening |
|
Transvaginal (TVS) |
High accuracy for low-lying placenta |
Requires trained operator |
Confirmatory evaluation |
|
Doppler |
Evaluates fetal-placental blood flow |
Does not locate placenta precisely |
Assess fetal well-being |
|
MRI |
Detailed placental invasion visualization |
Expensive, less available |
Suspected accreta spectrum |
Nursing Insights – Ultrasound Evaluation
- Prepare the client with a full bladder for TAS if needed to improve visualization.
- Educate client regarding procedure safety and non-invasive nature.
- Reinforce importance of follow-up ultrasounds as placenta may migrate upward in the second trimester.
1.4 Laboratory Tests
- Complete Blood Count (CBC):
- Monitor hemoglobin and hematocrit for blood loss assessment.
- Coagulation Profile:
- Prothrombin time (PT), activated partial thromboplastin time (aPTT), fibrinogen to detect coagulopathy or disseminated intravascular coagulation (DIC).
- Blood Typing and Crossmatch:
- Prepare for emergency blood transfusion.
- Other Labs:
- Iron studies for chronic blood loss.
- Basic metabolic panel to monitor renal function if hypovolemia occurs.
Nursing Insights – Laboratory Tests
- Ensure timely collection of labs before bleeding worsens.
- Maintain accurate documentation of blood loss and laboratory trends.
- Communicate abnormal results immediately to the primary health care provider to prepare for interventions.
1.5 Nursing Insights – Diagnostic Evaluation Summary
- Assessment Integration: Correlate history, physical exam, and lab findings to detect placenta previa early.
- Patient Education: Explain the rationale for avoiding vaginal exams and the need for serial ultrasounds.
- Safety Measures: Ensure IV access, blood products, and emergency equipment are ready prior to any assessment.
- Documentation: Meticulously document bleeding episodes, fetal status, maternal vitals, and lab trends.
- Collaboration: Communicate findings to interdisciplinary team, including obstetrics, neonatology, and anesthesia.
Management And Interventions
1.1 Expectant Management
- Definition:
- Expectant management refers to careful monitoring and supportive care for a client with placenta previa who is stable, has minimal bleeding, and the fetus is preterm or not in distress. This approach aims to prolong pregnancy to optimize fetal maturity while minimizing maternal and fetal risk.
- Key Components:
- Activity Restrictions:
- Bed rest or limited physical activity to reduce uterine contractions and risk of hemorrhage.
- Avoidance of sexual intercourse, vaginal examinations, and heavy lifting.
- Maternal Monitoring:
- Frequent assessment of vital signs (BP, HR, RR, O2 saturation).
- Serial assessment of vaginal bleeding (color, amount, presence of clots).
- Monitoring for signs of hypovolemia (dizziness, pallor, tachycardia).
- Fetal Monitoring:
- Nonstress tests (NST) and biophysical profiles (BPP) to assess fetal well-being.
- Ultrasound evaluation for fetal growth and amniotic fluid volume.
- Laboratory Monitoring:
- Complete blood count (CBC) to detect anemia.
- Type and crossmatch in anticipation of possible transfusion.
- Coagulation studies (PT, aPTT, fibrinogen) if bleeding persists.
- Corticosteroids:
- Administer betamethasone or dexamethasone if gestational age <34 weeks to enhance fetal lung maturity.
- Activity Restrictions:
Nursing Insights – Expectant Management
- Prepare for rapid intervention if bleeding increases or maternal/fetal compromise occurs.
- Maintain continuous communication with primary health care provider regarding maternal-fetal status.
- Educate the client on signs of hemorrhage (e.g., sudden increase in vaginal bleeding, dizziness, shortness of breath).
- Ensure IV access, emergency medications, and blood products are readily available.
1.2 Hospitalization Criteria
- Indications for Hospital Admission:
- Persistent or recurrent vaginal bleeding.
- Maternal hemodynamic instability (BP <90/60 mmHg, HR >100 bpm).
- Signs of preterm labor or uterine contractions.
- Non-reassuring fetal status or abnormal fetal heart rate patterns.
- Inability to maintain bed rest or close monitoring at home.
Nursing Insights – Hospitalization
- Hospitalized clients require continuous maternal-fetal monitoring and rapid response to bleeding episodes.
- Educate family and client on bed rest protocols, fluid management, and activity limitations.
- Prepare for potential emergency cesarean delivery if bleeding worsens.
- Maintain psychological support for anxiety due to restricted activity and hospitalization.
1.3 Indications for Cesarean Delivery
- Absolute Indications:
- Complete placenta previa covering the cervical os.
- Significant maternal hemorrhage endangering maternal or fetal life.
- Fetal malpresentation preventing safe vaginal delivery.
- Relative Indications:
- Partial or marginal placenta previa with recurrent bleeding.
- Fetal compromise requiring immediate delivery.
Delivery Planning:
- Cesarean delivery is typically scheduled between 36–37 weeks in stable clients with placenta previa to reduce risk of labor onset and hemorrhage.
- Blood products should be available due to high risk of maternal hemorrhage.
- Multidisciplinary approach: obstetrics, anesthesia, neonatology, and nursing teams must coordinate care.
Nursing Insights – Cesarean Delivery
- Monitor for signs of hemorrhage, both intraoperatively and postoperatively.
- Prepare neonatal resuscitation equipment due to potential preterm birth.
- Educate client on surgical procedure, anesthesia, and postoperative expectations.
- Implement post-cesarean care, including infection prevention, pain management, and early ambulation when safe.
1.4 Pharmacologic Interventions
- Corticosteroids:
- Betamethasone 12 mg IM q24h × 2 doses or Dexamethasone 6 mg IM q12h × 4 doses to enhance fetal lung maturity.
- Tocolytics (if preterm contractions present):
- Magnesium sulfate or nifedipine to inhibit uterine contractions temporarily.
- Iron and Hematinics:
- Oral or IV iron supplementation to prevent or treat anemia due to chronic blood loss.
- Blood Products:
- Packed red blood cells for acute blood loss.
- Fresh frozen plasma or platelets if coagulopathy develops.
- Analgesics:
- Acetaminophen for mild pain; avoid NSAIDs due to risk of bleeding.
Nursing Insights – Pharmacologic Interventions
- Monitor for side effects of corticosteroids: hyperglycemia, fluid retention, mood changes.
- Assess for magnesium sulfate toxicity: respiratory depression, decreased deep tendon reflexes.
- Ensure blood products are cross-matched and administered safely, monitoring for transfusion reactions.
- Educate the client regarding purpose, timing, and side effects of all medications.
1.5 Nursing Insights – Management and Interventions Summary
- Continuous maternal and fetal assessment is critical for timely intervention.
- Avoid digital vaginal examinations to prevent triggering massive hemorrhage.
- Maintain IV access, emergency medications, and blood products ready for rapid transfusion.
- Implement bed rest, pelvic rest, and limited activity as appropriate.
- Educate client on bleeding recognition, warning signs, and need for immediate reporting.
- Coordinate multidisciplinary care including obstetrics, anesthesia, and neonatology.
Intrapartum Care
1.1 Maternal Monitoring
- Purpose:
- Ensure maternal hemodynamic stability and early detection of hemorrhage, shock, or labor complications in clients with placenta previa.
- Key Assessments:
- Vital Signs:
- BP, HR, RR, O₂ saturation, and temperature (°C & °F). Monitor for hypotension (<90/60 mmHg), tachycardia (>100 bpm), or hypoxemia (<95% O₂ saturation).
- Bleeding Assessment:
- Observe vaginal bleeding: color (bright red vs dark), quantity (weigh peripads), presence of clots.
- Document onset, duration, and triggers of bleeding episodes.
- Uterine Assessment:
- Palpate uterine tone: soft, non-tender, and relaxed indicates placenta previa; avoid vaginal examination.
- Monitor for contractions or preterm labor signs.
- Laboratory Monitoring:
- Serial CBC for hemoglobin/hematocrit trends.
- Coagulation profile (PT, aPTT, fibrinogen) if significant bleeding occurs.
- Type and crossmatch in preparation for potential transfusion.
- Vital Signs:
Nursing Insights – Maternal Monitoring
- Avoid digital vaginal exams unless ordered for cesarean preparation; may precipitate massive hemorrhage.
- Maintain IV access with large-bore catheter for rapid fluid and blood administration.
- Educate client to report sudden bleeding, dizziness, or shortness of breath immediately.
- Position client in left lateral tilt to optimize uteroplacental perfusion and reduce vena cava compression.
- Ensure continuous communication with primary health care provider for rapid intervention.
1.2 Fetal Monitoring
- Purpose:
- Assess fetal well-being and detect early signs of distress, hypoxia, or compromised oxygenation.
- Techniques:
- External Fetal Monitoring:
- Continuous electronic fetal heart rate (FHR) monitoring.
- Evaluate baseline FHR, variability, accelerations, and decelerations.
- Ultrasound Assessment:
- Confirm fetal presentation, growth, amniotic fluid index, and placental location.
- Biophysical Profile (BPP):
- Assess fetal breathing movements, body movements, muscle tone, and amniotic fluid volume.
- External Fetal Monitoring:
Nursing Insights – Fetal Monitoring
- Monitor for non-reassuring patterns: recurrent late decelerations, decreased variability, or bradycardia (<110 bpm).
- Notify primary health care provider immediately if fetal distress is detected.
- Ensure availability of emergency cesarean delivery if distress persists.
- Educate client that movement monitoring at home may be indicated if stable.
1.3 Emergency Interventions
- Indications:
- Sudden increase in vaginal bleeding.
- Maternal hypotension or tachycardia.
- Non-reassuring fetal heart rate patterns.
- Immediate Interventions:
- Stabilize maternal hemodynamics:
- Administer IV fluids (normal saline or lactated Ringer’s).
- Prepare for blood transfusion if indicated.
- Positioning:
- Left lateral tilt to optimize uteroplacental perfusion.
- Oxygen Therapy:
- Administer 8–10 L/min via face mask for maternal hypoxemia.
- Prepare for Cesarean Delivery:
- Ensure neonatal resuscitation team is present.
- Preoperative labs, type & crossmatch, and IV access confirmed.
- Avoid Vaginal Exams:
- May precipitate massive hemorrhage.
- Stabilize maternal hemodynamics:
Nursing Insights – Emergency Interventions
- Rapid assessment and multidisciplinary coordination are essential.
- Ensure emergency equipment, blood products, and medications are readily available.
- Provide psychological support to client and family during crisis.
- Document all assessments, interventions, and client responses meticulously.
1.4 Nursing Insights – Intrapartum Care Summary
- Continuous maternal and fetal assessment is critical for early detection of hemorrhage and fetal compromise.
- Avoid digital vaginal exams to prevent triggering severe bleeding.
- Maintain IV access, oxygen, and emergency medications at bedside.
- Educate client on bed rest, activity limitations, and early signs of complications.
- Ensure rapid communication with primary health care provider and neonatal team if cesarean delivery is required.
Postpartum Care
1.1 Maternal Assessment
- Vital Signs:
- Monitor BP, HR, RR, temperature (°C & °F). Watch for hypotension, tachycardia, or fever indicating infection.
- Bleeding Assessment:
- Evaluate lochia for amount, color, and odor.
- Watch for postpartum hemorrhage (PPH): saturation of perineal pads within 15 min or continuous bright red bleeding.
- Uterine Assessment:
- Palpate fundus for tone, height, and position.
- Massage fundus if soft to prevent uterine atony.
- Laboratory Assessment:
- Monitor CBC for hemoglobin/hematocrit.
- Coagulation studies if significant hemorrhage occurs.
Nursing Insights – Maternal Assessment
- Educate client to report heavy bleeding, dizziness, or feeling faint immediately.
- Assess for signs of shock: pallor, tachycardia, hypotension, altered mental status.
- Monitor IV sites and fluid status carefully.
1.2 Management of Postpartum Hemorrhage
- Causes in Placenta Previa:
- Uterine atony, retained placental tissue, trauma, coagulopathy.
- Interventions:
- Uterine Massage: Encourage firm contraction.
- Medications:
- Oxytocin IV infusion for uterine contraction.
- Methylergonovine IM (if not hypertensive).
- Misoprostol PR or sublingual if refractory.
- Blood Products: PRBCs, FFP, platelets as needed.
- Surgical Intervention:
- Dilation & curettage, uterine balloon tamponade, hysterectomy if conservative measures fail.
Nursing Insights – PPH Management
- Continuous monitoring of vital signs, uterine tone, and bleeding.
- Maintain two large-bore IV lines for rapid infusion.
- Prepare emergency equipment and collaborate with surgical and anesthesia teams.
- Educate client and family regarding postpartum bleeding expectations and warning signs.
1.3 Neonatal Considerations
- Preterm Risks:
- Respiratory distress syndrome (RDS), hypoglycemia, hypothermia.
- Fetal Assessment:
- Apgar scores at 1 and 5 minutes.
- Monitor for oxygenation, temperature, and signs of distress.
- NICU Referral:
- For neonates <34 weeks or with complications.
Nursing Insights – Neonatal Care
- Provide thermoregulation, glucose monitoring, and oxygen support.
- Educate parents about preterm care and signs of neonatal distress.
- Ensure safe transport to NICU if indicated.
1.4 Nursing Insights – Postpartum Care Summary
- Prioritize maternal hemodynamic stability and early detection of PPH.
- Educate on lochia monitoring and warning signs.
- Monitor neonates for respiratory and metabolic complications due to prematurity.
- Collaborate with multidisciplinary team for maternal and neonatal safety.
Complications
1.1 Maternal Complications
- Hemorrhagic shock.
- Anemia.
- Coagulopathy (disseminated intravascular coagulation).
- Infection (endometritis, wound infection post-cesarean).
- Need for hysterectomy if bleeding is uncontrollable.
1.2 Fetal Complications
- Preterm birth.
- Low birth weight.
- Hypoxia and acidosis.
- Intrauterine growth restriction (IUGR).
- Perinatal mortality.
1.3 Nursing Insights – Complications Summary
- Close monitoring of maternal vital signs, bleeding, and labs is essential.
- Prepare for rapid transfusion and surgical intervention if needed.
- Educate client and family about potential maternal and fetal risks.
- Document all interventions, responses, and education clearly.
Summary
- Placenta Previa is a condition characterized by abnormal implantation of the placenta in the lower uterine segment, partially or completely covering the internal cervical os.
- It is classified as:
- Complete Previa: Placenta entirely covers the cervical os.
- Partial Previa: Placenta partially covers the cervical os.
- Marginal Previa: Placenta reaches the margin of the cervical os.
- Low-Lying Placenta: Placenta is implanted in the lower uterine segment but does not reach the cervical os.
- Epidemiology and Risk Factors:
- Incidence: ~0.3–0.5% of pregnancies.
- Maternal risk factors: Advanced maternal age (>35 years), multiparity, previous cesarean sections, uterine scarring, smoking, multiple gestations.
- Obstetric risk factors: Prior placenta previa, prior abortion or curettage, history of assisted reproductive technologies.
- Pathophysiology:
- Abnormal implantation in the lower uterine segment prevents adequate decidualization, leading to fragile placental attachment.
- During the third trimester, cervical dilation or uterine contractions can disrupt placental vessels, causing painless bright red vaginal bleeding.
- Maternal complications: Hemorrhagic shock, anemia, disseminated intravascular coagulation, infection, need for hysterectomy.
- Fetal complications: Preterm birth, intrauterine growth restriction, hypoxia, perinatal mortality.
- Clinical Manifestations:
- Classic presentation: Painless, bright red vaginal bleeding, usually in the third trimester.
- Uterus is soft and non-tender, distinguishing it from abruptio placentae.
- Maternal vital signs may remain stable initially; hypovolemic signs appear with severe bleeding.
- Diagnostic Evaluation:
- Transvaginal ultrasound is the gold standard for identifying placental location.
- Laboratory tests: CBC, coagulation profile, type and crossmatch.
- Vaginal examinations are contraindicated until cesarean delivery is planned.
- Management and Interventions:
- Expectant management: Bed rest, pelvic rest, hospitalization if bleeding is significant.
- Cesarean delivery is indicated for complete or partial previa, active bleeding, or fetal/maternal compromise.
- Pharmacologic interventions: Corticosteroids for fetal lung maturity, tocolytics if preterm contractions, oxytocin post-delivery to prevent hemorrhage.
- Intrapartum Care:
- Continuous maternal vital signs and fetal monitoring.
- Avoid vaginal examinations to prevent hemorrhage.
- Emergency interventions: Rapid IV fluid replacement, blood transfusions, oxygen therapy, preparation for immediate cesarean delivery.
- Postpartum Care:
- Monitor for postpartum hemorrhage, uterine atony, and infection.
- Neonatal care: Assess for prematurity-related complications such as respiratory distress syndrome, hypoglycemia, and NICU admission if necessary.
- Nursing Insights:
- Nursing care focuses on preventing hemorrhage, maintaining maternal-fetal safety, and preparing for emergency interventions.
- Patient and family education is critical regarding activity restrictions, warning signs of bleeding, and preterm neonatal risks.
- Documentation of bleeding episodes, maternal and fetal status, interventions, and responses is essential for continuity of care.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Placenta Previa
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


