Please set your exam date
Schizophrenia
Study Questions
Practice Exercise 1
A nurse is assessing the mood and cognitive state of mind of a client diagnosed with schizophrenia. Which signs and symptoms is the nurse most likely to observe? Select all that apply.
Explanation
Schizophrenia is a chronic psychiatric disorder marked by psychosis, cognitive impairment, and negative symptoms. It disrupts perception, thought, and behavior. Cognitive deficits include poor attention and memory. Negative symptoms involve flat affect, anhedonia, and avolition. Sleep and appetite disturbances are common.
Rationale for correct answers
1. Poor appetite reflects negative symptoms due to reduced motivation and diminished interest in self-care, frequently seen in schizophrenia.
2. Disrupted sleep is a common disturbance in schizophrenia, often linked to disorganized thought and circadian rhythm dysregulation.
3. Poor concentration arises from cognitive deficits, especially in attention and working memory, which impair daily functioning.
4. Incongruous affect is a hallmark negative symptom, where emotional expression does not match internal mood or social context.
Rationale for incorrect answers
5. Compulsive behavior is more typical of obsessive-compulsive disorder, not schizophrenia, and lacks diagnostic relevance here.
6. Involuntary muscle movement suggests extrapyramidal side effects from antipsychotics, not intrinsic symptoms of schizophrenia.
Take Home Points
- Schizophrenia presents with psychotic, cognitive, and negative symptoms; mood and behavior are often blunted.
- Negative symptoms include flat affect, poor motivation, and reduced social engagement.
- Cognitive deficits impair attention, memory, and executive function, affecting daily life.
- Differentiate schizophrenia from medication side effects and other psychiatric disorders like OCD or depression.
A nurse is assessing a client in the mental health clinic 6 months after the client’s discharge from in-patient psychiatric treatment for schizophrenia. The client has no active symptoms, but has a flat affect and has recently been placed on disability. What should the nurse document?
Explanation
Residual phase of schizophrenia follows the acute psychotic episode and is marked by persistent negative symptoms such as flat affect, social withdrawal, and reduced motivation. Positive symptoms like hallucinations or delusions are absent or significantly diminished. Clients may show functional impairment, including inability to maintain employment or relationships. Residual symptoms often reflect chronicity and may persist for months or years despite treatment.
Rationale for correct answer
4. Negative symptoms such as flat affect and social withdrawal without active psychosis indicate the client is in the residual phase. The recent placement on disability reflects functional decline, a hallmark of this phase.
Rationale for incorrect answers
1. Personality disorders like schizoid are distinct from schizophrenia and do not follow its phases. Schizoid traits are lifelong and not episodic.
2. Prodromal phase precedes the first psychotic break and includes subtle changes in mood, cognition, and behavior—not post-treatment symptoms.
3. Schizophrenia diagnosis requires active symptoms like delusions or hallucinations. The absence of these excludes this phase.
Take Home Points
- Residual phase follows acute psychosis and includes persistent negative symptoms like flat affect and social withdrawal.
- Schizoid personality disorder is not a phase of schizophrenia and differs in onset and symptom profile.
- Prodromal phase precedes psychosis and includes subtle behavioral and cognitive changes.
- Functional decline post-treatment, such as disability placement, supports residual phase documentation.
A client diagnosed with schizophrenia is brought to the emergency department by a family member. The client is experiencing social withdrawal, flat affect, and impairment in role functioning. To distinguish whether this client is in the prodromal or residual phase of schizophrenia, what question would the nurse ask?
Explanation
Both distinguishing prodromal and residual phase involve negative symptoms, but the prodromal phase occurs before the first psychotic episode, while the residual phase follows it. The key differentiator is the history of prior psychosis. Residual phase includes lingering symptoms after treatment, whereas prodromal signs are early warnings. Asking about recent exacerbation helps determine if the client is recovering from a psychotic episode or approaching one.
Rationale for correct answer
1. Exacerbation history confirms whether the client had prior psychotic symptoms, distinguishing residual from prodromal. Residual phase follows an acute episode.
Rationale for incorrect answers
2. Duration of symptoms does not clarify phase; both prodromal and residual can persist for weeks to years.
3. Mood changes are nonspecific and may occur in various psychiatric conditions, not phase-specific for schizophrenia.
4. Developmental disorders are unrelated to schizophrenia phases and do not aid in phase differentiation.
Take Home Points
- Residual phase follows a psychotic episode; prodromal precedes it.
- Asking about recent exacerbation helps distinguish between the two phases.
- Negative symptoms like flat affect and withdrawal occur in both phases.
- Duration and mood changes are not reliable phase indicators.
A client diagnosed with schizophrenia is experiencing anhedonia. Which nursing diagnosis addresses concerns regarding this client’s problem?
Explanation
Anhedonia is the inability to experience pleasure from activities usually found enjoyable, such as social interaction, hobbies, or intimacy. It is a negative symptom of schizophrenia and reflects emotional blunting and motivational deficits. It is associated with increased risk for depression and suicidal ideation, especially when combined with hopelessness and social withdrawal. Anhedonia is not caused by medication alone and may persist even in remission.
Rationale for correct answer
3. Suicide risk increases with anhedonia due to emotional numbness and loss of interest in life. The client may feel hopeless, especially if other negative symptoms are present.
Rationale for incorrect answers
1. Thought disturbances relate to delusions or disorganized thinking, not emotional blunting or loss of pleasure.
2. Sensory perception issues involve hallucinations, not inability to enjoy activities or emotional flatness.
4. Communication impairment involves speech production or coherence, not emotional experience or pleasure capacity.
Take Home Points
- Anhedonia is a negative symptom of schizophrenia linked to emotional blunting and loss of pleasure.
- It increases suicide risk due to hopelessness and social withdrawal.
- It differs from thought or sensory disturbances which involve cognition and perception.
- Impaired verbal communication is unrelated to emotional experience or pleasure.
The nurse documents that a client diagnosed with schizophrenia is expressing a flat affect. What is an example of this symptom?
Explanation
Flat affect refers to a lack of emotional expression, including facial movement, voice tone, and gestures. It is a negative symptom and reflects diminished emotional responsiveness. Clients may appear indifferent, unreactive, or emotionally vacant even in emotionally charged situations. It differs from inappropriate affect, which involves mismatched emotional responses.
Rationale for correct answer
3. Expression is absent despite emotional context. The client shows no visible reaction, which defines flat affect.
Rationale for incorrect answers
1. Laughter at tragic news reflects inappropriate affect, not flat affect. It shows emotional response, though mismatched.
2. Isolation may suggest withdrawal but does not confirm lack of emotional expression.
4. Feelings may still exist internally; flat affect refers to outward expression, not internal emotional experience.
Take Home Points
- Flat affect is a negative symptom marked by lack of emotional expression.
- It differs from inappropriate affect, which involves mismatched emotional responses.
- Clients may feel emotions internally but show no outward signs.
- Social withdrawal is not equivalent to flat affect.
Practice Exercise 2
A client is brought to the emergency department after being found wandering the streets and talking to unseen others. Which situation is further evidence of a diagnosis of schizophrenia for this client?
Explanation
Schizophrenia is a chronic psychiatric disorder characterized by psychosis, including hallucinations, delusions, and disorganized thinking. For diagnosis, symptoms must persist for at least six months, with one month of active-phase features. It impairs social and occupational functioning and must be differentiated from mood disorders, substance-induced psychosis, and developmental conditions. Negative symptoms like avolition and flat affect often persist beyond acute episodes.
Rationale for correct answer
4. Duration of symptoms is a core diagnostic criterion. The DSM-5 requires continuous signs of disturbance for at least 6 months, including one month of active symptoms such as hallucinations or delusions. This timeframe distinguishes schizophrenia from brief psychotic disorder and schizophreniform disorder. The wandering and hallucinations described in the stem meet active-phase criteria, and persistence for 6 months confirms diagnostic threshold.
Rationale for incorrect answers
1. Autism spectrum disorder may present with social withdrawal or communication deficits, but hallucinations are not typical. If psychotic symptoms occur in autism, schizophrenia can only be diagnosed if prominent hallucinations or delusions persist for a month. Autism alone does not confirm schizophrenia.
2. Medical conditions like temporal lobe epilepsy or encephalitis can cause hallucinations. If symptoms are attributable to a medical etiology, schizophrenia cannot be diagnosed. Rule-out of organic causes is mandatory before confirming a psychiatric diagnosis.
3. Manic or depressive symptoms suggest schizoaffective or bipolar disorder with psychotic features. Schizophrenia requires that mood symptoms are not predominant. If mood episodes are concurrent and substantial, another diagnosis is more appropriate.
Take Home Points
- Schizophrenia requires continuous symptoms for at least 6 months, including 1 month of active-phase psychosis.
- Rule out substance use and medical conditions before confirming schizophrenia.
- Mood symptoms must be secondary or absent; otherwise consider schizoaffective or bipolar disorder.
- Autism may coexist with schizophrenia only if psychotic symptoms are prominent and persistent.
A 21-year-old client, being treated for asthma with steroid medication, has been experiencing delusions of persecution and disorganized thinking for the past 6 months. Which factor may rule out a diagnosis of schizophrenia?
Explanation
Schizophrenia diagnostic criteria Schizophrenia requires continuous symptoms for at least 6 months, including at least 1 month of active-phase symptoms such as delusions, hallucinations, or disorganized speech. The remaining time may include residual or prodromal symptoms. Functional impairment must be evident in work, relationships, or self-care. Diagnosis excludes conditions caused by substances or medical disorders.
Rationale for correct answer
4. Duration of symptoms for 6 months meets the DSM criteria for schizophrenia. This includes active and residual phases with impaired functioning.
Rationale for incorrect answers
1. Autism may coexist with schizophrenia, but its presence alone does not confirm schizophrenia unless hallucinations or delusions are present.
2. Medical conditions must be ruled out before diagnosing schizophrenia. If symptoms are due to illness, schizophrenia is not diagnosed.
3. Mood symptoms suggest schizoaffective or mood disorders with psychosis, not schizophrenia unless psychotic symptoms dominate.
Take Home Points
- Schizophrenia diagnosis requires 6 months of continuous symptoms including 1 month of active psychosis.
- Medical and substance-induced causes must be excluded before confirming schizophrenia.
- Mood symptoms may indicate schizoaffective disorder, not schizophrenia.
- Autism alone does not confirm schizophrenia unless psychotic symptoms are present.
The nurse is assessing a client diagnosed with disorganized schizophrenia. Which symptoms should the nurse expect the client to exhibit?
Explanation
Steroid-induced psychosis Corticosteroids can cause psychiatric symptoms including delusions, hallucinations, and disorganized thinking, especially at high doses. These effects typically emerge within days to weeks of initiation and may resolve after discontinuation. Steroid-induced psychosis must be differentiated from primary psychotic disorders, as it is substance-related and reversible.
Rationale for correct answer
4. Medication effects must be ruled out before diagnosing schizophrenia. Steroids can cause psychosis, making schizophrenia diagnosis inappropriate.
Rationale for incorrect answers
1. Six months is the minimum duration required, but if symptoms are due to steroids, schizophrenia is not diagnosed.
2. Auditory hallucinations are common but not mandatory. Delusions and disorganized speech alone can meet criteria.
3. Age 21 is within the typical onset range for schizophrenia, which usually begins between ages 16 and 30.
Take Home Points
- Steroid-induced psychosis must be ruled out before diagnosing schizophrenia.
- Auditory hallucinations are not required for schizophrenia diagnosis.
- Age 21 is typical for schizophrenia onset.
- Duration alone does not confirm schizophrenia if symptoms are substance-induced.
On an in-patient unit, the nurse is caring for a client who is assuming bizarre positions for long periods of time. To which diagnostic category of schizophrenia would this client most likely be assigned?
Explanation
Schizophrenia is a chronic psychiatric disorder marked by psychosis, disorganized thinking, and impaired social functioning. Though DSM-5 removed formal subtypes, classical categories like catatonic, paranoid, and disorganized remain useful for clinical description. Catatonia involves motor immobility, rigidity, and posturing, often with mutism or echolalia. It may occur in schizophrenia, mood disorders, or medical conditions. Catatonic features include waxy flexibility, negativism, and purposeless agitation. Diagnosis requires at least three of twelve catatonic symptoms.
Rationale for correct answer
2. The client’s prolonged bizarre posturing is a hallmark of motor immobility and waxy flexibility, defining features of catatonic schizophrenia. These behaviors reflect a disruption in voluntary movement and responsiveness, consistent with catatonia.
Rationale for incorrect answers
1. Disorganized schizophrenia presents with disorganized speech, flat affect, and erratic behavior, not sustained posturing. Clients may laugh inappropriately or show poor hygiene, but motor rigidity is absent.
3. Paranoid schizophrenia is dominated by delusions and auditory hallucinations, often involving persecution or conspiracy. Posturing is not typical; behavior is more reactive to perceived threats.
4. Undifferentiated schizophrenia is diagnosed when symptoms do not clearly fit other subtypes. However, bizarre posturing is specific enough to classify under catatonic, making undifferentiated inappropriate here.
Take Home Points
- Catatonic schizophrenia involves motor immobility, waxy flexibility, and bizarre postures, often with mutism or echolalia.
- Disorganized schizophrenia features incoherent speech, flat affect, and erratic behavior, not motor symptoms.
- Paranoid schizophrenia centers on delusions and hallucinations, with preserved motor function.
- DSM-5 removed formal subtypes, but classical categories remain useful for describing symptom clusters.
A client on an in-patient psychiatric unit refuses to take medications because, “The pill has a special code written on it that will make it poisonous.” What kind of delusion is this client experiencing?
Explanation
Persecutory delusion involves false beliefs that one is being harmed, conspired against, or targeted by others. It reflects paranoia, often with themes of poisoning, surveillance, or sabotage. Clients may misinterpret benign actions as threats and resist treatment due to fear. These delusions are fixed and not amenable to logic or reassurance, and they are among the most common in schizophrenia.
Rationale for correct answer
3. Poisoning fear reflects a persecutory delusion, where the client believes others intend harm. The belief is fixed and irrational, despite evidence to the contrary.
Rationale for incorrect answers
1. Erotomania involves belief that someone, often of higher status, is in love with the client. It does not include fear of harm.
2. Grandiosity includes exaggerated self-worth or power, not fear of being poisoned or targeted.
4. Somatic delusions involve false beliefs about bodily functions or disease, not external threats or sabotage.
Take Home Points
- Persecutory delusions involve irrational beliefs of being harmed or conspired against.
- These delusions are common in schizophrenia and often lead to treatment refusal.
- Grandiose and erotomanic delusions reflect inflated self-perception or romantic beliefs.
- Somatic delusions focus on false physical illness or dysfunction, not external threats.
The nurse is interviewing a client who states, “The dentist put a filling in my tooth; I now receive transmissions that control what I think and do.” The nurse accurately documents this symptom with which charting entry?
Explanation
Delusion of influence is a psychotic symptom where the client believes their thoughts, actions, or feelings are being controlled by external forces. It reflects a loss of autonomy and distorted perception of reality, often involving bizarre mechanisms like implants or transmissions. This type of delusion is common in schizophrenia and may be accompanied by hallucinations or disorganized thinking.
Rationale for correct answer
4. The belief that transmissions from a dental filling control thoughts and actions is a classic external control delusion. It reflects thought manipulation, a hallmark of delusion of influence.
Rationale for incorrect answers
1. Delusion of persecution involves beliefs of being targeted or harmed by others. This scenario lacks a threat or victimization component.
2. Delusion of grandeur involves exaggerated self-importance or power. The client does not claim superiority or special status.
3. Somatic delusions involve false beliefs about bodily functions or health. While the tooth is mentioned, the focus is on external control, not physical illness.
Take Home Points
- Delusion of influence involves belief that thoughts or actions are controlled by external forces.
- It differs from persecutory delusions, which involve harm or targeting.
- Somatic delusions focus on bodily dysfunction, not external manipulation.
- Accurate documentation supports diagnosis and guides antipsychotic treatment.
Practice Exercise 3
A nurse is evaluating a client diagnosed with paranoid schizophrenia who reports hearing a voice that says, “Do not remove your hat because they will be able to read your mind.” Which response by the nurse is the most therapeutic?
Explanation
Therapeutic response to paranoid delusions Clients with paranoid schizophrenia often experience persecutory delusions involving threats or surveillance. These beliefs are fixed, resistant to logic, and emotionally distressing. Therapeutic communication must prioritize validation of feelings without reinforcing the delusion. Empathy reduces defensiveness and builds trust, allowing gradual cognitive restructuring. Avoiding confrontation or challenging the delusion directly is essential to prevent escalation or withdrawal.
Rationale for correct answer
4. Empathy and emotional validation help reduce distress and build rapport. The nurse acknowledges the fear without reinforcing the delusion.
Rationale for incorrect answers
1. Questioning the delusion’s content may feel intrusive or accusatory, increasing paranoia and mistrust.
2. Challenging the logic of the delusion provokes defensiveness and does not support therapeutic engagement.
3. Denial of the belief invalidates the client’s experience and may escalate agitation or withdrawal.
Take Home Points
- Therapeutic responses to delusions should validate emotions without reinforcing false beliefs.
- Empathy builds trust and reduces defensiveness in paranoid schizophrenia.
- Avoid challenging or denying delusional content directly.
- Open-ended, nonjudgmental communication supports cognitive restructuring over time.
A nurse is developing a plan of care for a client prescribed the traditional antipsychotic drug haloperidol (Haldol®) for the treatment of schizophrenia. Which medication should the nurse expect to administer if extrapyramidal side effects develop?
Explanation
Haloperidol is a high-potency typical antipsychotic that blocks dopamine D2 receptors, often leading to extrapyramidal symptoms (EPS). These include dystonia, akathisia, parkinsonism, and tardive dyskinesia. EPS can emerge within hours to days of treatment. Management includes anticholinergic agents like benztropine, which reduce muscular rigidity and tremors by restoring dopamine-acetylcholine balance.
Rationale for correct answer
2. Benztropine is an anticholinergic that effectively treats EPS by reducing muscle stiffness and tremors associated with dopamine blockade.
Rationale for incorrect answers
1. Olanzapine is an atypical antipsychotic, not used to treat EPS; it may cause EPS at high doses.
3. Chlorpromazine is another typical antipsychotic and may worsen EPS due to similar dopamine antagonism.
4. Escitalopram is an SSRI used for depression and has no role in managing extrapyramidal symptoms.
Take Home Points
- Haloperidol commonly causes extrapyramidal symptoms due to dopamine blockade.
- Benztropine is the first-line treatment for EPS.
- Atypical antipsychotics may cause EPS but are not used to treat it.
- SSRIs do not address EPS and may complicate symptom management.
A client, who is experiencing both positive and negative symptoms of schizophrenia, is prescribed an atypical antipsychotic, risperidone (Risperdal®). The client asks the nurse to explain the common side effects of this medication. Which side effects should the nurse state to the client? Select all that apply.
Explanation
Risperidone side effects Risperidone is an atypical antipsychotic that blocks dopamine D2 and serotonin 5-HT2A receptors. It treats both positive and negative symptoms of schizophrenia. Common side effects include drowsiness, dizziness, weight gain, hypotension, and constipation. It may also elevate prolactin levels. Dystonia is less common with atypicals but can occur at higher doses or in sensitive individuals.
Rationale for correct answers
1. Dizziness results from orthostatic hypotension due to alpha-adrenergic blockade, especially during early treatment.
3. Drowsiness is common due to central nervous system sedation and histamine receptor antagonism.
4. Weight gain occurs from metabolic changes and increased appetite, particularly with long-term use.
5. Constipation is due to mild anticholinergic effects and reduced gastrointestinal motility.
6. Hypotension results from peripheral vasodilation via alpha-1 adrenergic blockade, especially in early dosing.
Rationale for incorrect answers
2. Dystonia is rare with risperidone and more typical of high-potency first-generation antipsychotics like haloperidol.
Take Home Points
- Risperidone treats both positive and negative symptoms of schizophrenia.
- Common side effects include sedation, dizziness, weight gain, hypotension, and constipation.
- Dystonia is uncommon with atypical antipsychotics.
- Monitoring for metabolic and cardiovascular effects is essential during risperidone therapy.
A client with schizophrenia is taking the atypical antipsychotic medication clozapine (Clozaril). Which signs and symptoms indicate the presence of adverse effects associated with this medication? Select all that apply.
Explanation
Clozapine adverse effects Clozapine is an atypical antipsychotic used for treatment-resistant schizophrenia. It can cause agranulocytosis, myocarditis, and orthostatic hypotension. Early signs of hematologic toxicity include fever, sore throat, and flu-like symptoms. Regular ANC monitoring is mandatory. It also causes dose-dependent seizures and cardiovascular effects. Contraindicated in uncontrolled epilepsy, severe cardiac disease, and history of clozapine-induced myocarditis.
Rationale for correct answers
1. Sore throat is a warning sign of neutropenia, a serious hematologic adverse effect requiring immediate blood count monitoring.
4. Fever reflects systemic infection and may indicate agranulocytosis or myocarditis, both serious clozapine-related complications.
5. Flulike symptoms often precede neutropenia or myocarditis, requiring urgent evaluation and possible discontinuation of clozapine.
6. Orthostatic hypotension is common during initial titration due to clozapine’s alpha-adrenergic blockade and cardiovascular effects.
Rationale for incorrect answers
2. Extrapyramidal symptoms like pill-rolling are rare with clozapine due to its low D2 receptor affinity.
3. Polyuria is not a recognized adverse effect of clozapine; it may suggest diabetes insipidus or hyperglycemia from other causes.
Take Home Points
- Clozapine requires strict monitoring due to risk of agranulocytosis, myocarditis, and seizures.
- Early signs of neutropenia include sore throat, fever, and flu-like symptoms.
- Orthostatic hypotension is common during dose initiation and titration.
- Clozapine has low risk of extrapyramidal symptoms compared to typical antipsychotics.
Which client is most likely to benefit from group therapy?
Explanation
Group therapy in schizophrenia Group therapy benefits clients with stable symptoms, insight, and social engagement. It enhances interpersonal skills, reduces isolation, and fosters peer support. It is contraindicated during acute psychosis or noncompliance. Outpatient clients with stable medication adherence and insight are ideal candidates.
Rationale for correct answer
1. Outpatient clients with schizophrenia are typically stabilized, making them receptive to group dynamics and therapeutic engagement.
Rationale for incorrect answers
2. Stabilization phase requires individualized care; group therapy may overwhelm or confuse newly admitted clients.
3. Exacerbation of symptoms impairs reality testing and social functioning, limiting benefit from group interaction.
4. Noncompliance with medication undermines therapeutic engagement and may disrupt group cohesion or safety.
Take Home Points
- Group therapy suits clients with stable schizophrenia and good insight.
- Acute psychosis or noncompliance limits group therapy effectiveness.
- Peer support and social skill development are key benefits.
- Individual therapy is preferred during symptom exacerbation or early stabilization.
A client diagnosed with paranoid schizophrenia tells the nurse about three previous suicide attempts. Which nursing diagnosis would take priority and reflect this client’s problem?
Explanation
Risk for suicide is the most urgent concern when a client reports previous attempts, especially in the context of paranoid schizophrenia, where delusions and hallucinations may drive self-harm. Suicidal ideation in schizophrenia is often linked to command hallucinations, hopelessness, or persecutory beliefs. Immediate safety and suicide prevention take precedence over other psychiatric symptoms.
Rationale for correct answer
2. Prior suicide attempts indicate elevated lethality and intent, making suicide risk the top priority. In schizophrenia, this risk is compounded by impaired judgment and psychotic symptoms that may distort reality and increase impulsivity.
Rationale for incorrect answers
1. Disturbed thought processes are characteristic of schizophrenia but do not pose an immediate life-threatening risk. Safety concerns override cognitive symptoms in prioritization.
3. Violence toward others is not indicated in this scenario. The client’s history centers on self-harm, not aggression or threats to others.
4. Altered sensory perception, such as hallucinations, contributes to suicide risk but is a secondary concern. The priority is preventing harm, not managing perceptual distortions.
Take Home Points
- Suicide risk takes precedence when a client reports prior attempts, regardless of diagnosis.
- Paranoid schizophrenia may involve command hallucinations that increase self-harm risk.
- Thought disturbances and hallucinations are important but secondary to immediate safety.
- Nursing interventions must focus on suicide prevention before addressing other psychiatric symptoms.
A client’s family is having a difficult time accepting the client’s diagnosis of schizophrenia, and this has led to family conflict. Which nursing diagnosis reflects this problem?
Explanation
Interrupted family processes refers to a disruption in the family’s ability to manage emotional support, communication, and role responsibilities due to a health crisis. In schizophrenia, families often struggle with denial, stigma, and adjustment to the chronic nature of the illness. This can lead to conflict, impaired coping, and breakdown in relational dynamics.
Rationale for correct answer
2. Family conflict due to difficulty accepting the diagnosis reflects disrupted roles and emotional strain, which are central to interrupted family processes. The diagnosis alters expectations, routines, and emotional equilibrium within the family unit.
Rationale for incorrect answers
1. Impaired home maintenance involves inability to perform household tasks, often due to physical or cognitive limitations. It does not address relational or emotional conflict.
3. Social isolation refers to withdrawal from broader social networks, not internal family discord. It is more applicable to the client than the family.
4. Disturbed thought processes describe cognitive disorganization in the client, not the family’s reaction. It does not reflect interpersonal or systemic family issues.
Take Home Points
- Interrupted family processes involve emotional and role disruption due to illness in a family member.
- Schizophrenia often causes relational strain and denial within families.
- Nursing interventions should support education, communication, and coping strategies for families.
- Other diagnoses like impaired home maintenance or social isolation target different domains of functioning.
Comprehensive Questions
A nurse is discussing discharge plans with a homeless client diagnosed with paranoid schizophrenia. What is the primary factor that will affect the formulation of the discharge plan for this client?
Explanation
Discharge planning for clients with paranoid schizophrenia who are homeless must prioritize community resources. Without access to shelters, food, and outpatient care, continuity of treatment is compromised. Coordination with shelters and outreach teams is essential to prevent relapse and rehospitalization.
Rationale for correct answer
4. Community resources like shelters determine the feasibility of discharge. Without housing, medication adherence and follow-up care are unlikely.
Rationale for incorrect answers
1. Support systems are important but secondary to basic needs like shelter, which must be secured first.
2. Ability of the nurse to work with the client is valuable but does not directly affect discharge logistics.
3. Compliance depends on stable housing and access to care, which cannot be assumed in homelessness.
Take Home Points
- Homeless clients with schizophrenia require coordinated discharge planning with shelter and outreach services.
- Community resources are foundational before psychosocial interventions can be effective.
- Medication adherence is unlikely without stable housing and follow-up care.
- Discharge plans must address physiological needs before therapeutic goals.
A nurse is educating a client diagnosed with schizophrenia on appropriate measures to help prevent the relapse of schizophrenic symptoms. Which interventions should the nurse encourage the client to use to help prevent symptom relapse? Select all that apply.
Explanation
Relapse prevention in schizophrenia Relapse in schizophrenia is often triggered by stress, poor sleep, and substance use. Preventive strategies include lifestyle regulation, early symptom reporting, and psychoeducation. Physical activity improves mood and cognition. Alcohol worsens psychosis and interferes with medication metabolism.
Rationale for correct answers
2. Regular exercise improves neurocognitive function, reduces stress, and enhances overall mental health stability.
3. Sleep disturbances often precede relapse; reporting changes allows early intervention and medication adjustment.
4. Stress management reduces cortisol levels and prevents exacerbation of psychotic symptoms.
5. Alcohol disrupts neurotransmitter balance and increases risk of noncompliance and relapse.
Rationale for incorrect answers
1. Ignoring hallucinations may worsen distress and delay reporting; clients should be taught coping strategies instead.
6. Employment should be individualized; avoiding all demanding jobs may hinder recovery and autonomy.
Take Home Points
- Relapse prevention includes sleep regulation, stress management, and substance avoidance.
- Physical activity supports cognitive and emotional stability in schizophrenia.
- Early reporting of symptom changes enables timely intervention.
- Employment should be tailored, not universally avoided.
A nurse is reviewing with the client’s father the discharge plan of a client recently diagnosed with paranoid schizophrenia. Which of the father’s statements indicates to the nurse that he understands the diagnoses and prognosis of paranoid schizophrenia?
Explanation
Paranoid schizophrenia has a variable course. With medication adherence, symptoms can stabilize, but relapses are common. Long-term management includes psychosocial support and monitoring. Prognosis improves with insight, support, and early intervention. Hospitalization may recur despite treatment.
Rationale for correct answer
2. Continued medication use reduces symptom recurrence and improves functional outcomes, though not guaranteeing full remission.
Rationale for incorrect answers
1. Depression is not a hallmark of paranoid subtype; vigilance should focus on psychotic symptoms and medication adherence.
3. Hospitalization may recur due to stress, noncompliance, or environmental triggers; one episode is rarely definitive.
4. Home monitoring is helpful but not always feasible or necessary; outpatient follow-up is often sufficient.
Take Home Points
- Medication adherence is critical to symptom control in paranoid schizophrenia.
- Relapse is common even with treatment; prognosis varies.
- Paranoid subtype focuses on delusions and hallucinations, not mood symptoms.
- Family education should emphasize long-term management, not unrealistic expectations.
The mother of a client diagnosed with paranoid schizophrenia visiting her son 2 days after his admission to the psychiatric unit approaches a nurse and states, “He is still talking about how the government is controlling his thoughts.” What is the most accurate nursing appraisal of the mother’s statement?
Explanation
Paranoid schizophrenia is a subtype of schizophrenia marked by persistent delusions, often of persecution or grandeur, and auditory hallucinations. Clients may believe external forces control their thoughts or behaviors. Insight is typically poor, and symptoms may persist despite early treatment. Antipsychotic medications require time—often 1 to 2 weeks—to show therapeutic effects. Family education is essential to align expectations and reduce distress caused by misinterpretation of symptoms.
Rationale for correct answer
4. The mother’s misunderstanding reflects a lack of insight into the illness. Education helps her interpret delusional content as part of the disorder and not a sign of treatment failure.
Rationale for incorrect answers
1. Unrealistic expectations are evident; believing delusions should resolve within two days ignores the pharmacodynamics of antipsychotics and the chronic nature of schizophrenia.
2. Misguided concern arises from assuming persistence of delusions indicates worsening or ineffective care, rather than recognizing the expected course of symptom resolution.
3. Premature medication adjustment is not warranted; antipsychotics require time to reach therapeutic levels, and changes should be based on clinical evaluation, not family perception.
Take Home Points
- Paranoid schizophrenia involves persistent delusions and auditory hallucinations, often with poor insight.
- Antipsychotic medications typically take 1–2 weeks to show clinical improvement.
- Family education is crucial to manage expectations and support therapeutic goals.
- Misinterpretation of symptoms by family can lead to unnecessary concern or pressure on clinical decisions.
A client admitted to a behavioral medicine unit with a diagnosis of catatonic schizophrenia is constantly rearranging furniture and appears to be responding to internal stimuli. In addition to being free of physical injury during phases of hyperactivity, which short-term goal is appropriate for this client?
Explanation
Catatonic schizophrenia is marked by extreme motor disturbances, ranging from stupor to excessive hyperactivity, often without purpose. Clients may exhibit repetitive movements, echolalia, or posturing. During hyperactive phases, basic needs like nutrition and hydration are frequently neglected, increasing risk for dehydration, malnutrition, and exhaustion. These clients may also respond to internal stimuli, making redirection difficult. Safety and physiological stability are prioritized before psychosocial goals.
Rationale for correct answer
2. Ensuring nutrition and hydration supports physiological stability, which is critical during hyperactivity when clients may ignore basic needs due to internal preoccupation.
Rationale for incorrect answers
1. Sleep is important but not the most immediate concern during hyperactivity; clients may be unable to settle due to psychomotor agitation.
3. Interaction is unrealistic during acute phases; clients are often internally preoccupied and socially withdrawn, making engagement unlikely.
4. Activity reduction within 24 hours is not a reliable goal; antipsychotic effects may take longer, and hyperactivity may persist unpredictably.
Take Home Points
- Catatonic schizophrenia includes extremes of motor behavior, from stupor to purposeless hyperactivity.
- During hyperactivity, clients may neglect food, fluids, and sleep, risking physiological compromise.
- Short-term goals should prioritize safety and basic physiological needs over social or behavioral changes.
- Psychosocial goals are more appropriate once stabilization is achieved and internal stimuli are reduced.
A nurse includes the nursing diagnosis of disturbed thought processes secondary to paranoia in the care plan for a newly admitted client diagnosed with schizophrenia. Which approach is most appropriate for this client?
Explanation
Paranoia in schizophrenia involves persistent delusions of persecution, mistrust, and hypervigilance. Clients may misinterpret benign actions as threatening, leading to defensive or aggressive behavior. They often perceive others as plotting against them or controlling their thoughts. Nonverbal cues like whispering or laughing can be misconstrued as ridicule or conspiracy. Therapeutic communication must be clear, direct, and non-threatening to reduce anxiety and build trust.
Rationale for correct answer
1. Avoiding nonverbal triggers like whispering or laughing prevents misinterpretation and escalation of paranoid ideation, fostering a safer therapeutic environment.
Rationale for incorrect answers
2. Premature focus on community supports overlooks the acute phase needs; paranoia impairs trust, making external planning ineffective initially.
3. Unrealistic expectation; clients with paranoia often isolate due to mistrust and fear, making peer interaction unlikely and potentially distressing.
4. Inappropriate timing; obtaining consent requires trust and cognitive clarity, which may be compromised during acute paranoid episodes.
Take Home Points
- Paranoid schizophrenia involves mistrust, delusions of persecution, and misinterpretation of social cues.
- Nonverbal behaviors like whispering or laughing can intensify paranoid ideation.
- Initial care should focus on safety, trust-building, and minimizing perceived threats.
- Social and legal interventions should be deferred until paranoia subsides and insight improves.
A nurse is discussing the importance of taking medication as prescribed with a client diagnosed with paranoid schizophrenia. Which response demonstrates that the nurse understands the importance of relapse prevention?
Explanation
Relapse in paranoid schizophrenia leads to worsening of psychotic symptoms, impaired functioning, and reduced responsiveness to treatment. Each episode of relapse increases the risk of cognitive decline, hospitalization, and social withdrawal. Long-term outcomes deteriorate with repeated episodes, making adherence to antipsychotic therapy critical. Relapse prevention involves psychoeducation, medication compliance, and early recognition of warning signs. Even brief lapses in adherence can precipitate symptom recurrence.
Rationale for correct answer
2. Emphasizing the cumulative impact of relapse reinforces the importance of consistent medication use and helps the client understand long-term consequences of nonadherence.
Rationale for incorrect answers
1. Oversimplified assurance ignores the complexity of schizophrenia; relapse can occur despite adherence due to stressors or medication resistance.
3. Minimizing side effects may reduce trust; clients need honest information to make informed decisions and report adverse effects promptly.
4. Reactive advice lacks proactive education; while contacting providers is important, it doesn’t address the broader issue of relapse prevention.
Take Home Points
- Relapse in schizophrenia worsens long-term prognosis and increases risk of cognitive and functional decline.
- Medication adherence is essential to prevent relapse and maintain stability.
- Clients should be educated on the consequences of relapse and the importance of early symptom recognition.
- Communication should be honest, supportive, and focused on long-term health outcomes.
A nurse is reviewing with the family the discharge plan of a client diagnosed with paranoid schizophrenia. A family member asks, “What should I do if the voices come back again?” Which nurse response is most appropriate when advising the family member of what to do during a relapse of paranoid schizophrenia?
Explanation
Relapse in paranoid schizophrenia
Relapse in paranoid schizophrenia often presents with re-emergence of hallucinations, delusions, and social withdrawal. Auditory hallucinations—commonly voices—can be distressing and may provoke agitation or fear. During relapse, clients may lose insight and become suspicious of others. Immediate supportive interventions are critical to prevent escalation. Distraction techniques such as listening to music, engaging in conversation, or performing simple tasks can reduce the intensity of internal stimuli and promote safety until professional help is accessed.
Rationale for correct answer
3. Staying with the client and using distraction techniques provides emotional support and helps reduce the impact of hallucinations. It also ensures safety and prevents isolation during relapse.
Rationale for incorrect answers
1. Appointments are essential for long-term management but do not address acute symptoms. Voices may return between visits, requiring immediate action.
2. Crisis centers are helpful, but listing them during discharge lacks immediacy. Families need actionable steps to manage symptoms at home before escalation.
4. Phone numbers offer access to care but do not equip the family with practical strategies. Passive advice may delay intervention and increase distress.
Take Home Points
- Relapse in paranoid schizophrenia often involves auditory hallucinations and increased suspicion.
- Distraction techniques help reduce the emotional impact of hallucinations and promote safety.
- Family members should be trained in supportive strategies to manage symptoms during relapse.
- Emergency contacts are important but should be paired with active symptom management approaches.
Which specific client outcome best reflects the primary goal of crisis intervention for a client diagnosed with schizophrenia who is experiencing an alcohol-induced crisis?
Explanation
Crisis intervention aims to stabilize acute symptoms, reduce distress, and restore functional coping. In schizophrenia complicated by alcohol use, clients often experience exacerbated psychosis, impaired judgment, and poor insight. The immediate goal is not long-term recovery but short-term stabilization and development of adaptive strategies. Teaching coping mechanisms helps clients manage triggers, reduce relapse risk, and engage in treatment. Insight and skill-building are prioritized over detox timelines or occupational goals.
Rationale for correct answer
3. Identifying coping strategies reflects internalization of skills that support emotional regulation and relapse prevention, aligning with the short-term goals of crisis stabilization.
Rationale for incorrect answers
1. Detoxification is a medical process, not a behavioral goal; success in detox does not guarantee psychological stabilization or coping development.
2. Employment is unrealistic during crisis; returning to work requires sustained stability, insight, and functional capacity beyond the scope of immediate intervention.
4. Medication knowledge is important but secondary; during crisis, clients may lack cognitive clarity, making skill acquisition more feasible than detailed pharmacologic understanding.
Take Home Points
- Crisis intervention focuses on short-term stabilization and development of adaptive coping skills.
- Alcohol use worsens psychotic symptoms and impairs insight in schizophrenia.
- Teaching coping mechanisms supports relapse prevention and emotional regulation.
- Occupational and pharmacologic goals are more appropriate in post-crisis rehabilitation phases.
A client diagnosed with schizophrenia is refusing to take a prescribed psychotropic medication. A nurse attempts to persuade the client to comply with the physician’s orders. Under which circumstance could the client be forced to take medication?
Explanation
Involuntary administration of psychotropic medication is legally and ethically restricted to situations where the client poses an imminent danger to self or others. Schizophrenia may involve delusions, hallucinations, and impaired judgment, but refusal alone does not justify forced treatment. Threats of violence, especially with intent and target specificity, meet criteria for emergency intervention. Legal standards require clear documentation of risk, and interventions must be the least restrictive necessary to ensure safety.
Rationale for correct answer
2. A direct threat to harm a nurse indicates imminent risk, justifying emergency medication to prevent violence and protect others.
Rationale for incorrect answers
1. Delusions of grandeur, such as claiming to be God, are common in schizophrenia but do not imply danger or justify forced medication.
3. Leaving the hospital may breach treatment plans but does not meet criteria for involuntary medication unless accompanied by risk behaviors.
4. Past suicide attempts indicate vulnerability but do not justify forced medication unless current suicidal ideation or intent is present.
Take Home Points
- Involuntary medication requires evidence of imminent danger to self or others.
- Delusional content alone does not justify forced treatment unless linked to risk.
- Threats of violence with intent and specificity meet emergency intervention criteria.
- Legal and ethical standards prioritize least restrictive measures and client rights.
A client with schizophrenia has a history of nonadherence to the prescribed medication regimen and requires hospitalization for exacerbation of schizophrenic symptoms. Injectable antipsychotic agents are being considered for long-term use to better stabilize the client’s symptoms. Which medications, if prescribed by the health-care provider, should the nurse question? Select all that apply.
Explanation
Long-acting injectable (LAI) antipsychotics are used to improve adherence in schizophrenia, especially in clients with noncompliance history. These formulations maintain therapeutic levels over weeks, reducing relapse risk. Only specific agents are available in depot form. Olanzapine and ziprasidone are not routinely used as LAIs due to safety concerns or lack of approved long-acting formulations. Olanzapine LAI requires post-injection monitoring due to risk of sedation syndrome, making it unsuitable for nonadherent clients.
Rationale for correct answers
2. Olanzapine LAI carries risk of post-injection delirium/sedation syndrome, requiring 3-hour monitoring, which is impractical for clients with poor adherence.
5. Ziprasidone lacks an approved long-acting injectable formulation for maintenance therapy, making it unsuitable for long-term stabilization.
Rationale for incorrect answers
1. Risperidone consta is a long-acting atypical antipsychotic administered biweekly, effective for improving adherence and symptom control.
3. Haloperidol decanoate is a first-generation depot antipsychotic with monthly dosing, suitable for clients with chronic nonadherence.
4. Fluphenazine decanoate is another first-generation depot agent, effective for long-term symptom control in schizophrenia.
6. Aripiprazole is available in LAI form (e.g., Abilify Maintena), offering monthly dosing and good tolerability for maintenance therapy.
Take Home Points
- Long-acting injectables improve adherence and reduce relapse in schizophrenia.
- Olanzapine LAI requires post-injection monitoring due to sedation risk.
- Ziprasidone lacks an approved long-acting injectable formulation.
Risperidone, haloperidol, fluphenazine, and aripiprazole are suitable LAI options for nonadherent clients.
A client with schizophrenia is being prepared for discharge. He tells the nurse that he has no home or family and has been living on the street. Which response by the nurse is most appropriate?
Explanation
Schizophrenia is a chronic psychiatric disorder marked by psychosis, impaired reality testing, and functional decline. Discharge planning must address housing, medication adherence, and psychosocial support. Homelessness exacerbates relapse risk and impairs access to care. Coordinated services, including social work, are essential for continuity and safety.
Rationale for correct answer
3. A referral to social services ensures continuity of care and addresses basic needs such as housing, food, and safety. This aligns with discharge planning protocols for vulnerable psychiatric clients, especially those without stable shelter.
Rationale for incorrect answers
1. Providing shelter contacts without assessing broader needs lacks a comprehensive approach. It does not ensure follow-through or address underlying barriers to care.
2. Exploring feelings may offer insight but delays intervention. The priority is securing housing and services, not emotional processing at discharge.
4. Informing the charge nurse and documenting is procedural, not therapeutic. It fails to initiate the necessary support systems for safe discharge.
Take Home Points
- Discharge planning for schizophrenia must include housing, medication, and psychosocial support.
- Homelessness increases risk of relapse, hospitalization, and poor treatment adherence.
- Social services are critical in coordinating care for clients with no support system.
Emotional support is important but secondary to meeting physiological and safety needs
A nurse is preparing to care for a client diagnosed with catatonic schizophrenia. In anticipation of this client’s arrival, what should the nurse do?
Explanation
Catatonic schizophrenia is a subtype of schizophrenia marked by motor immobility, mutism, and extreme negativism. Clients may exhibit waxy flexibility, posturing, or stupor. Risk of pressure injuries, dehydration, and nutritional deficits is high due to prolonged immobility and refusal to eat or speak.
Rationale for correct answer
3. A specialty mattress overlay prevents pressure ulcers and supports skin integrity in clients with prolonged immobility. It is a proactive intervention for catatonic states where movement is severely restricted.
Rationale for incorrect answers
1. Notifying security implies a risk of violence, which is not characteristic of catatonic schizophrenia. These clients are typically withdrawn and non-aggressive.
2. Magnesium sulfate is used for eclampsia, not schizophrenia. It has no therapeutic role in catatonia and may cause unnecessary complications.
4. NPO status is not universally indicated in catatonia. Unless aspiration risk is confirmed, nutrition should be supported, not withheld.
Take Home Points
- Catatonic schizophrenia involves motor immobility, mutism, and posturing, increasing risk for pressure injuries.
- Specialty mattresses help prevent skin breakdown in immobile psychiatric clients.
- Catatonia is non-aggressive; security measures are rarely necessary.
- Nutritional support should be individualized; NPO status is not routine in catatonia.
A nurse is caring for a client who has schizophrenia. What’s the first-line treatment for this client?
Explanation
Schizophrenia is a chronic psychiatric disorder characterized by delusions, hallucinations, and disorganized thinking. It results from dysregulation of dopamine pathways, particularly in the mesolimbic system. First-line treatment targets neurotransmitter imbalance using antipsychotic medications to reduce positive symptoms and prevent relapse. Long-term management includes psychosocial interventions but pharmacologic therapy is foundational.
Rationale for correct answer
4. Antipsychotics are the primary treatment for schizophrenia, targeting dopamine dysregulation to reduce hallucinations and delusions. They are essential for symptom control and preventing acute psychotic episodes.
Rationale for incorrect answers
1. Group therapy may support social skills but is not effective during acute psychosis. It is adjunctive, not first-line.
2. Thyroid therapy is used for hypothyroidism, not schizophrenia. There is no direct link between thyroid dysfunction and primary psychotic disorders.
3. Milieu therapy provides a structured environment but lacks pharmacologic impact. It supports safety and routine but does not treat core symptoms.
Take Home Points
- Antipsychotics are the cornerstone of schizophrenia treatment, especially for positive symptoms.
- Dopamine dysregulation in the mesolimbic pathway underlies hallucinations and delusions.
- Psychosocial therapies are adjunctive and used after stabilization.
- Thyroid dysfunction is not a primary cause of schizophrenia and does not guide treatment.
On the treatment plan for a client diagnosed with schizophrenia, one of the goals is to discuss issues that reinforce reality. Which intervention should the nurse use to assist the client to meet this goal?
Explanation
Reality orientation is a therapeutic approach used in schizophrenia to help clients reconnect with the external environment, reduce hallucinations, and improve insight. It involves structured interventions that clarify time, place, and person, and link symptoms to identifiable triggers. Teaching clients to recognize how stressors influence psychotic symptoms enhances coping and supports recovery.
Rationale for correct answer
2. Teaching the link between external stressors and hallucinations promotes insight and reality testing. It helps the client understand that symptoms are not rooted in reality but are responses to internal or environmental triggers.
Rationale for incorrect answers
1. Asking the client to find discrepancies between thoughts and feelings assumes intact cognition, which may be impaired in schizophrenia. This abstract task may increase confusion rather than reinforce reality.
3. Limiting relationships may worsen isolation and reduce opportunities for reality-based interactions. Social engagement is therapeutic when structured and monitored.
4. Discouraging substance use is important, but it does not directly reinforce reality orientation. It addresses contributing factors, not the core goal of reconnecting with the real world.
Take Home Points
- Reality orientation helps clients with schizophrenia distinguish internal distortions from external reality.
- Stress management education supports insight and reduces hallucinations.
- Social interaction, when structured, enhances reality testing and reduces isolation.
- Substance use may worsen psychosis but is not the primary focus of reality reinforcement strategies.
A nurse is caring for a schizophrenic client who’s well managed on medications. He reveals that he’s doing so well, he doesn’t think he needs to take medication anymore. What response indicates the nurse best understands the client’s diagnosis?
Explanation
Medication adherence in schizophrenia is critical to prevent relapse, maintain functional stability, and reduce hospitalization. Antipsychotics control positive symptoms like hallucinations and delusions, but discontinuation—even when symptoms improve—can lead to rapid decompensation. Insight into illness is often impaired, making psychoeducation essential.
Rationale for correct answer
1. This response reinforces the importance of adherence and explains the risk of relapse. It acknowledges the client’s progress while educating about the chronic nature of schizophrenia and the need for continued pharmacologic support.
Rationale for incorrect answers
2. Deferring to the physician without educating the client misses an opportunity for psychoeducation. It may reinforce denial and reduce the client’s engagement in treatment.
3. Suggesting medication for “several months” implies a temporary need, which is inaccurate. Schizophrenia requires long-term, often lifelong, pharmacologic management.
4. Telling the client to comply because of a doctor’s order is authoritarian and lacks therapeutic value. It does not foster understanding or autonomy in managing a chronic condition.
Take Home Points
- Schizophrenia requires long-term antipsychotic treatment to prevent relapse and maintain stability.
- Insight into illness is often impaired; psychoeducation is key to promoting adherence.
- Relapse risk increases significantly after abrupt medication discontinuation.
- Therapeutic communication should be informative, respectful, and support client autonomy.
A client diagnosed with schizophrenia is about to be discharged and is facing the stressor of acquiring independent employment. For the nurse using a behavioral approach, which nursing intervention is most appropriate in meeting this client’s needs?
Explanation
Behavioral therapy in schizophrenia focuses on skill-building, reinforcement, and structured interventions to improve functioning. It uses modeling, rehearsal, and feedback to help clients adapt to real-world challenges. Employment stress requires practical preparation, and behavioral strategies like role-play enhance confidence, reduce anxiety, and improve performance in social tasks.
Rationale for correct answer
2. Role-playing simulates real-life scenarios and builds adaptive behavior through repetition and feedback. It helps the client rehearse responses, reduce anxiety, and improve social competence, which are essential for successful employment.
Rationale for incorrect answers
1. Thought blocking is a cognitive strategy, not behavioral. It targets internal symptom control, not external skill development relevant to employment.
3. Housing advocacy is a case management task, not a behavioral intervention. It addresses environmental needs but does not build employment-related skills.
4. PRN medication use is a pharmacologic approach. It may reduce anxiety but does not equip the client with behavioral tools for job readiness.
Take Home Points
- Behavioral therapy emphasizes skill-building through modeling, rehearsal, and reinforcement.
- Role-playing is effective for preparing clients with schizophrenia for employment and social tasks.
- Cognitive and pharmacologic strategies support symptom control but do not build functional skills.
- Case management addresses environmental needs but is not part of behavioral intervention.
A nurse is admitting a client to the in-patient unit who is exhibiting bizarre delusions, auditory hallucinations, and incoherent speech. The client is experiencing suicidal ideations and rates mood at 2/10. Based on this clinical picture, the client is manifesting symptoms in what diagnostic category?
Explanation
Schizoaffective disorder is a psychiatric condition marked by psychotic symptoms such as hallucinations and delusions, occurring alongside a mood episode—either depressive or manic. Diagnosis requires the presence of psychosis for at least two weeks without mood symptoms, followed by periods where both occur together. Clients often present with suicidal ideation, affective instability, and disorganized thought processes.
Rationale for correct answer
3. The presence of mood disturbance (rated 2/10) alongside psychotic features like hallucinations and delusions supports schizoaffective disorder. Suicidal ideation further confirms the depressive component, distinguishing it from pure schizophrenia.
Rationale for incorrect answers
1. Paranoid schizophrenia involves persecutory delusions and auditory hallucinations but lacks prominent mood symptoms. The low mood rating and suicidal ideation are inconsistent with this subtype.
2. Brief psychotic disorder lasts less than one month and typically follows a severe stressor. The presence of mood symptoms and suicidal ideation suggests a more complex, enduring condition.
4. Schizophreniform disorder mimics schizophrenia but lasts less than six months. It does not require mood symptoms, making it less likely given the depressive features in this case.
Take Home Points
- Schizoaffective disorder combines psychotic symptoms with a major mood episode.
- Diagnosis requires psychosis alone for at least two weeks, followed by concurrent mood and psychotic symptoms.
- Suicidal ideation and low mood ratings point toward a depressive component.
- Differentiation from schizophrenia and schizophreniform depends on duration and presence of mood symptoms.
A new graduate nurse is assessing a 20-year-old client in the emergency department. The client is seeing and hearing things that others do not see or hear. The nurse tells the supervisor, “I believe the client has schizophrenia.” Which of the following supervisor responses is the most appropriate? Select all that apply.
Explanation
Psychotic symptom assessment requires a structured approach to determine duration, etiology, and associated features. Hallucinations and delusions may occur in schizophrenia, substance-induced psychosis, mood disorders, or brief reactive states. A comprehensive evaluation includes substance use history, mood symptoms, social functioning, and timeline of symptom onset.
Rationale for correct answers
1. Duration helps differentiate between brief psychotic disorder, schizophreniform, and schizophrenia. Symptoms lasting over six months suggest schizophrenia; under one month may indicate a transient psychotic episode.
2. Substance use can trigger drug-induced psychosis, especially with stimulants, hallucinogens, or withdrawal states. Ruling out pharmacologic causes is essential before diagnosing a primary psychotic disorder.
4. Mood symptoms help identify schizoaffective disorder or mood disorders with psychotic features. Depression or mania co-occurring with hallucinations alters the diagnostic pathway.
5. Social relationships reflect functional decline, a core criterion in schizophrenia. Poor interpersonal connections may support the diagnosis or indicate other psychiatric conditions.
Rationale for incorrect answers
3. The nurse’s role includes clinical observation and reporting findings. While diagnosis is physician-led, nurses contribute essential data through assessment and documentation.
Take Home Points
- Duration of psychotic symptoms is key in differentiating schizophrenia from other disorders.
- Substance-induced psychosis must be ruled out before confirming a primary diagnosis.
- Mood symptoms guide diagnosis toward schizoaffective or mood disorders with psychosis.
- Functional decline, especially in relationships, supports schizophrenia diagnosis.
The nurse is performing an admission assessment on a client diagnosed with paranoid schizophrenia. To receive the most accurate assessment information, which should the nurse consider?
Explanation
Paranoid schizophrenia is a subtype of schizophrenia marked by delusions, suspiciousness, and intact cognitive functioning. Clients may be guarded, mistrustful, and reluctant to share personal information. Although they often retain higher functioning than other subtypes, their paranoia can significantly impair communication and limit the reliability of self-reported data.
Rationale for correct answer
2. Due to mistrust and guardedness, clients with paranoid schizophrenia may withhold or distort information. Reviewing past records and speaking with family provides a more accurate and comprehensive clinical picture.
Rationale for incorrect answers
1. While cognitive function may be preserved, paranoia interferes with openness. The client may be unwilling or unable to contribute meaningfully to history-taking.
3. Schizophrenia is heterogeneous and complex. Paranoid subtype presents unique challenges, especially in building rapport and gathering reliable data.
4. The global assessment of functioning score offers a snapshot, not detailed history. It cannot replace thorough data collection from multiple sources.
Take Home Points
- Paranoid schizophrenia involves delusions and mistrust, which impair communication during assessment.
- Collateral information from records and family is essential for accurate evaluation.
- Cognitive functioning may be intact, but guardedness limits reliability of self-report.
- GAF scores are useful but insufficient for comprehensive nursing assessment.
Clients diagnosed with schizophrenia may have difficulty knowing where their ego boundaries end and others’ begin. Which client behavior reflects this deficit?
Explanation
Ego boundary disturbance in schizophrenia refers to impaired differentiation between self and others, leading to identity confusion and imitative behaviors. Clients may mimic others’ actions, feel thoughts are being inserted or controlled, or struggle to distinguish internal experiences from external reality. This deficit contributes to disorganized behavior and poor interpersonal functioning.
Rationale for correct answer
4. Imitating others’ movements reflects blurred boundaries and impaired self-other differentiation. It indicates the client cannot clearly separate their own identity from external influences, a hallmark of ego boundary disturbance.
Rationale for incorrect answers
1. Eating only prepackaged food suggests paranoia or fear of contamination, not ego boundary disturbance. The behavior is protective, not identity-related.
2. Believing others are poisoning food is a persecutory delusion, focused on harm and mistrust. It does not reflect confusion about self versus others.
3. Interpreting idioms literally is concrete thinking, common in schizophrenia but unrelated to ego boundaries. It reflects cognitive rigidity, not identity confusion.
Take Home Points
- Ego boundary disturbance involves impaired self-other differentiation and identity confusion.
- Imitative behaviors like echopraxia reflect blurred boundaries in schizophrenia.
- Paranoia and concrete thinking are distinct symptoms not linked to ego boundary deficits.
- Accurate assessment of ego boundaries informs therapeutic strategies and interpersonal interventions.
The children’s saying, “Step on a crack and you break your mother’s back,” is an example of which type of thinking?
Explanation
Magical thinking is a cognitive distortion where individuals believe their thoughts, words, or actions can cause events in a way that defies logical causality. It is common in early childhood development and certain psychiatric conditions like schizophrenia or obsessive-compulsive disorder. This type of thinking reflects a belief in supernatural or irrational connections between unrelated events.
Rationale for correct answer
3. The belief that stepping on a crack could harm someone reflects irrational causality and superstitious thinking, which are hallmarks of magical thinking. It assumes a mystical link between an action and an unrelated consequence.
Rationale for incorrect answers
1. Concrete thinking involves literal interpretation of language and difficulty with abstraction, but it does not imply belief in supernatural causation.
2. Neologisms are invented words with idiosyncratic meanings, often seen in disorganized speech. This saying uses real words, not fabricated ones.
4. Clang associations involve speech driven by sound patterns like rhyming or alliteration, not content. The phrase is meaningful and not based on phonetic similarity.
Take Home Points
- Magical thinking involves belief in irrational or supernatural connections between actions and outcomes.
- It is developmentally normal in children but pathological in adults with psychosis or OCD.
- Concrete thinking is literal and lacks abstraction but does not involve mystical beliefs.
- Clang associations are sound-driven and reflect disorganized thought, not magical causality.
The nurse is assessing a client diagnosed with schizophrenia. The client states, “We wanted to take the bus, but the airport took all the traffic.” Which charting entry accurately documents this symptom?
Explanation
Associative looseness is a formal thought disorder seen in schizophrenia where ideas shift from one to another with little or no logical connection. Speech may appear coherent superficially but lacks internal consistency. The client’s statements may be grammatically correct yet conceptually fragmented, making communication difficult and disorganized.
Rationale for correct answer
1. The statement reflects disorganized thought with loosely connected ideas. The mention of a bus and airport lacks logical flow, indicating associative looseness—a hallmark of schizophrenia’s thought disorder.
Rationale for incorrect answers
2. Word salad involves incoherent and jumbled speech with no grammatical structure. This client’s sentence, though illogical, is grammatically intact.
3. Delusional thinking involves fixed false beliefs, often with themes of persecution or grandeur. The statement lacks a clear belief system or conviction.
4. Illusions are misinterpretations of real external stimuli. The statement does not describe a sensory misperception but rather a disorganized thought pattern.
Take Home Points
- Associative looseness presents as grammatically correct but illogically connected speech.
- Word salad is incoherent and lacks grammatical structure.
- Delusions are fixed false beliefs, not disorganized speech.
- Illusions involve misinterpreting real stimuli, not conceptual confusion.
The nurse reports that a client diagnosed with a thought disorder is experiencing religiosity. Which client statement would confirm this finding?
Explanation
Religiosity in thought disorders refers to an excessive or preoccupying focus on religious themes, rituals, or beliefs that dominate cognition and behavior. It may manifest as compulsive scripture reading, rigid spiritual routines, or interpreting all events through a religious lens. In schizophrenia, this symptom can be part of delusional or disorganized thinking, often interfering with daily functioning and insight.
Rationale for correct answer
2. Reading the Bible every hour to determine actions reflects preoccupation and compulsivity with religious content. It confirms religiosity as the client’s behavior is dominated by spiritual themes beyond normative practice.
Rationale for incorrect answers
1. Seeing Jesus is a hallucination, not religiosity. It involves sensory perception without external stimulus, not excessive religious focus.
3. Claiming to be dead and in heaven is a nihilistic or bizarre delusion, not centered on religious practice or belief systems.
4. Believing the CIA poisoned the Bible reflects paranoia, not religiosity. The focus is on persecution, not spiritual obsession.
Take Home Points
- Religiosity involves excessive religious focus that dominates thought and behavior.
- It differs from hallucinations, which are sensory distortions, and delusions, which are fixed false beliefs.
- Paranoid and nihilistic delusions may include religious content but are not classified as religiosity.
- Assessment must distinguish between normative spiritual beliefs and pathological preoccupation.
The nurse states, “It’s time for lunch.” A client diagnosed with schizophrenia responds, “It’s time for lunch, lunch, lunch.” Which type of communication process is the client using, and what is the underlying reason for its use?
Explanation
Echolalia is a speech disturbance where individuals repeat words or phrases spoken by others. It is common in schizophrenia, autism, and other neurodevelopmental disorders. In schizophrenia, echolalia reflects impaired ego boundaries and a disrupted sense of self, often serving as a primitive attempt to connect with others or stabilize identity through mimicry.
Rationale for correct answer
2. Repeating the nurse’s statement reflects echolalia, a symptom of disorganized speech. It serves as an effort to acquire identity and maintain connection when internal boundaries are blurred.
Rationale for incorrect answers
1. Echopraxia involves imitating movements, not speech. It reflects motor mimicry, not verbal repetition.
3. Unconscious identification is a defense mechanism, not a speech pattern. It does not explain the verbal repetition observed.
4. Depersonalization involves feeling detached from self or surroundings. It is an internal experience, not a communicative behavior.
Take Home Points
- Echolalia is verbal repetition of others’ speech, common in schizophrenia and autism.
- It reflects impaired ego boundaries and attempts to stabilize identity.
- Echopraxia is motor imitation, not speech-related.
- Depersonalization is a subjective detachment, not a speech disturbance.
Exams on Schizophrenia
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Pathophysiology And Neurobiology Of Schizophrenia
- Practice Exercise 1
- Assessment
- Diagnostic Criteria For Schizophrenia
- Practice Exercise 2
- Nursing Interventions
- Pharmacological Management
- Psychosocial And Therapeutic Nursing Interventions
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Understand the DSM-5 diagnostic criteria for schizophrenia
- Describe the pathophysiology and neurobiology underlying the disorder
- Recognize and assess key symptoms, including physical, motor, emotional, and cognitive features
- Distinguish the different types of delusions and perceptual distortions
- Identify approaches for assessing language and communication deficits
- Develop nursing interventions for managing hallucinations and delusions
- Differentiate pharmacological and non-pharmacological (psychosocial) treatments
- Apply knowledge through practice questions and concept summaries
Introduction
- Schizophrenia is a severe, chronic psychiatric disorder characterized by profound alterations in thought, perception, and behavior.
- It is typified by episodes of psychosis—meaning a significant loss of contact with reality—which can present with a variety of positive symptoms (such as hallucinations and delusions) and negative symptoms (such as affective flattening and avolition).
- The typical onset is in late adolescence to early adulthood, though it can occur at any age.
- Schizophrenia significantly impairs functional ability, including social and occupational domains, self-care, and quality of life.
- The disorder affects roughly 1% of the global population, with immense personal and societal costs in terms of morbidity, disability, healthcare utilization, and lost productivity.
- The etiology is multifactorial, with genetic, neurobiological, and environmental elements converging.
- Treatment is multidimensional, requiring psychopharmacology, therapeutic communication, psychosocial rehabilitation, and intensive nursing care.
- Nursing students must master not only the signs and symptoms but also assessment techniques, pharmacologic and non-pharmacologic strategies, and high-yield clinical insights to excel in exams and patient care settings.
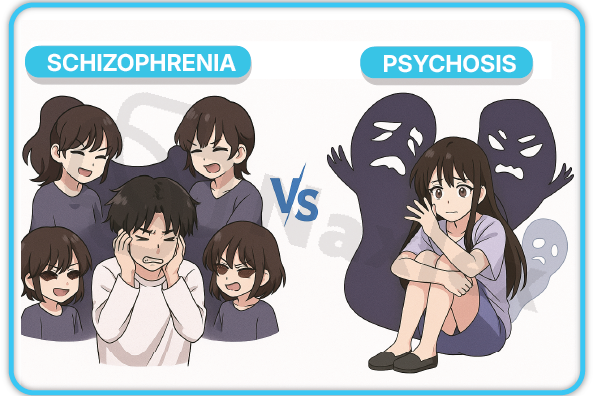
Pathophysiology And Neurobiology Of Schizophrenia
1.1 Structural and Neurochemical Changes
Schizophrenia is associated with distinct alterations in brain structure and neurochemistry:
- Structural brain changes include:
- Enlarged lateral, third, and fourth ventricles
- Reduced brain volume, particularly in the thalamus, medial temporal lobe, and prefrontal cortex
- Thinning of the cerebral cortex and reduced hippocampal volume
- Neurochemical changes:
- Dysregulation of dopamine, specifically in the mesolimbic (excess) and mesocortical (deficit) pathways
- Abnormalities in glutamatergic and serotonergic neurotransmission
- Reduced numbers of dendritic spines in the dorsolateral prefrontal cortex, affecting synaptic connectivity
1.2 Genetic and Environmental Risk Factors
- Genetics:
- Heritability estimates range from 60–80%. First-degree relatives of schizophrenic patients have five- to eleven-fold risk
- Monozygotic twins: 41–79% concordance
- Environmental/Developmental factors:
- Perinatal complications (e.g., hypoxia)
- Maternal infections (e.g., influenza), malnutrition, or severe prenatal stress
- Childhood trauma, neglect, social isolation, and urban upbringing
- Substance abuse, especially adolescent cannabis use
1.3 Dopaminergic and Glutamatergic Hypotheses
- Dopamine Hypothesis:
- Hyperactivity of dopamine in the mesolimbic pathway underpins positive symptoms (e.g., hallucinations, delusions)
- Hypoactivity in the mesocortical pathway leads to negative symptoms (avolition, alogia)
- Support: Amphetamines worsen psychosis; D2 antagonists (antipsychotics) ameliorate symptoms
- Glutamate Hypothesis:
- NMDA receptor dysfunction implicated, especially in negative and cognitive symptoms
Table: Major Dopaminergic Pathways and Their Clinical Associations
|
Pathway |
Brain Areas |
Effect in Schizophrenia |
Clinical Associations |
|
Mesolimbic |
VTA→Nucleus accumbens |
↑ DA → positive symptoms |
Hallucinations, Delusions |
|
Mesocortical |
VTA→Prefrontal cortex |
↓ DA → negative symptoms |
Avolition, Alogia, Affect blunting |
|
Nigrostriatal |
Substantia nigra→Striatum |
Antipsychotic-induced blockade |
Extrapyramidal side effects |
|
Tuberoinfundibular |
Hypothalamus→Pituitary |
Antipsychotic-induced blockade |
Hyperprolactinemia |
- These biochemical disruptions contribute to impaired salience attribution, cognitive deficits, and abnormal perceptions in schizophrenia.
1.4 Protective Factors
- Strong psychosocial support network
- Early diagnosis and effective antipsychotic therapy
- Well-developed coping and social skills
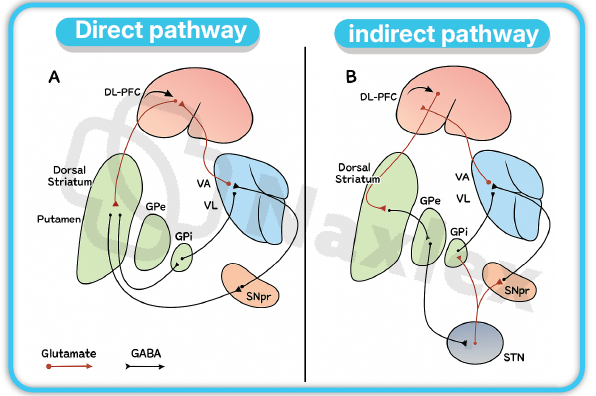
Assessment
- Recognizing and thoroughly assessing the multidimensional symptoms of schizophrenia is essential for nursing care.
1.1 Physical Characteristics
- Impaired personal hygiene and grooming
- Inappropriate or bizarre dress for the environment (e.g., wearing heavy clothing in summer)
1.2 Motor Activity
- Disorganized behavior: Unpredictable or inappropriate (e.g., childlike silliness, agitation)
- Catatonia: Rigid posture, resistance to movement, waxy flexibility, or stupor
- Psychomotor agitation: Restlessness, aimless pacing, inability to sit still
1.3 Emotional Characteristics
- Affective blunting or flattening: Expressionless face, poor eye contact
- Lack of emotional reciprocity
1.4 Compulsive Rituals
- Repetitive, ritualistic, and purposeless behaviors (e.g., counting, repetitive hand washing)
- May resemble obsessive-compulsive disorder but often lack insight
1.5 Overcompliance
- Excessive agreement, passivity, or compliance with instructions
- May mimic requests or follow bizarre rules obediently
1.6 Affective Disturbances
- Anhedonia: Inability to experience pleasure
- Avolition: Loss of motivation, apathy
- Asociality: Social withdrawal, lack of interest in interacting
1.7 Abnormal Thought Processes
Schizophrenia frequently manifests in abnormal thinking and reasoning (thought disorders):
- Disorganized thinking (formal thought disorder):
- Loosened associations: jumping from topic to topic
- Thought blocking: sudden interruption in speech or train of thought
- Incoherence: "word salad"
- Tangential speech: responses digress from topic and never return (never answer the question)
- Circumstantial speech: includes excessive detail before eventually returning to the main point
- Clanging: word choices driven by rhyme or sound, not meaning
- Neologisms: inventing new words or phrases
- Perseveration: persistent repetition of words or ideas
- Pressured speech: rapid and frenzied speech
1.8 Types of Delusions
- Persecutory (paranoid): Belief one is being plotted against or harmed
- Referential: Belief that neutral events, gestures, comments are directed at oneself (e.g., TV is sending special messages)
- Grandiose: Inflated sense of self-worth or power
- Nihilistic: Belief that the self, others, or the world does not exist (delusion of nonexistence)
- Somatic: Belief in abnormal bodily functions (e.g., one’s organs are rotting)
- Bizarre: Implausible beliefs (e.g., thoughts are being inserted or withdrawn)
- Erotomanic: False belief that another person is in love with the patient
Table: Types of Delusions in Schizophrenia
|
Type |
Description |
Example |
|
Persecutory |
Others intend harm or harassment |
"My neighbor has poisoned my food." |
|
Referential |
Neutral cues have personal significance |
"The TV host is talking about me." |
|
Grandiose |
Possesses great talent, importance, or special relationship |
"I am the President’s advisor." |
|
Nihilistic |
Nonexistence or impending catastrophe |
"I am dead; the world is ending." |
|
Somatic |
Abnormal body function or health |
"My liver is turning into stone." |
|
Bizarre |
Impossible, implausible beliefs |
"Aliens implanted electrodes in my brain." |
|
Erotomanic |
Another (often famous) person loves them |
"The movie star sends me secret signals." |
1.9 Perceptual Distortions
- Hallucinations:
- Most common: auditory (hearing voices)
- Others: visual, tactile, olfactory, gustatory
- Character: neutral, critical, commanding (command hallucinations), threatening
- Command hallucinations are particularly dangerous and must be assessed for content (risk to self or others).
- Illusions (misinterpretation of real external stimuli)
- Depersonalization (detachment from self) and derealization (perceiving environment as unreal)
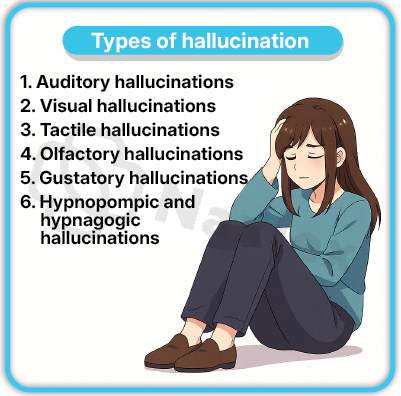
1.10 Language and Communication Disturbances
- Alogia: poverty of speech—brief, empty replies
- Poverty of speech content: adequate quantity but reduced meaningful information
- Speech disorganization: incoherence, neologisms, clanging, echolalia
NURSING INSIGHTS
- Auditory hallucinations (voices) are the most common perceptual disturbance in schizophrenia. Always assess for their content and risk.
- Negative symptoms (avolition, anhedonia, alogia, asociality, affective flattening) contribute most to chronic functional disability and poor quality of life.
- Early detection and intervention—symptom recognition and prompt treatment introduction—substantially improve long-term outcomes.
- Nurses must routinely assess for symptom fluctuations, medication effects, and risk for relapse.
- Flat affect may be mistaken for depression, but it represents a core deficit in emotional expression in schizophrenia, not mood.
Diagnostic Criteria For Schizophrenia
1.1 Key Symptoms and Duration
- Diagnosis of schizophrenia (DSM-5) is clinical and requires all of the following criteria:
- Characteristic symptoms: At least two of five key symptoms (delusions, hallucinations, disorganized speech, disorganized/catatonic behavior, negative symptoms) for a significant portion of a one-month period. At least one must be delusions, hallucinations, or disorganized speech.
- Functional impairment: Significant reduction in level of functioning in work, relationships, or self-care as compared to pre-morbid baseline.
- Duration: Continuous signs of disturbance persist for at least six months, including at least one month of active symptoms.
Table: Key Symptoms in Schizophrenia
|
Symptom |
Description |
|
Hallucinations |
Perceptions in the absence of external stimuli; most commonly auditory |
|
Delusions |
Fixed, false beliefs, not amenable to evidence |
|
Disorganized speech |
Incoherent, rambling, or tangential language; "word salad" |
|
Disorganized/catatonic behavior |
Bizarre or purpose-less motor activity, or complete lack of movement (catatonia) |
|
Negative symptoms |
Diminished emotional expression, avolition, alogia, asociality, anhedonia |
- For a diagnosis, clinicians must rule out mood disorders with psychosis, schizoaffective disorder, substance/medication-induced psychosis, and medical causes.
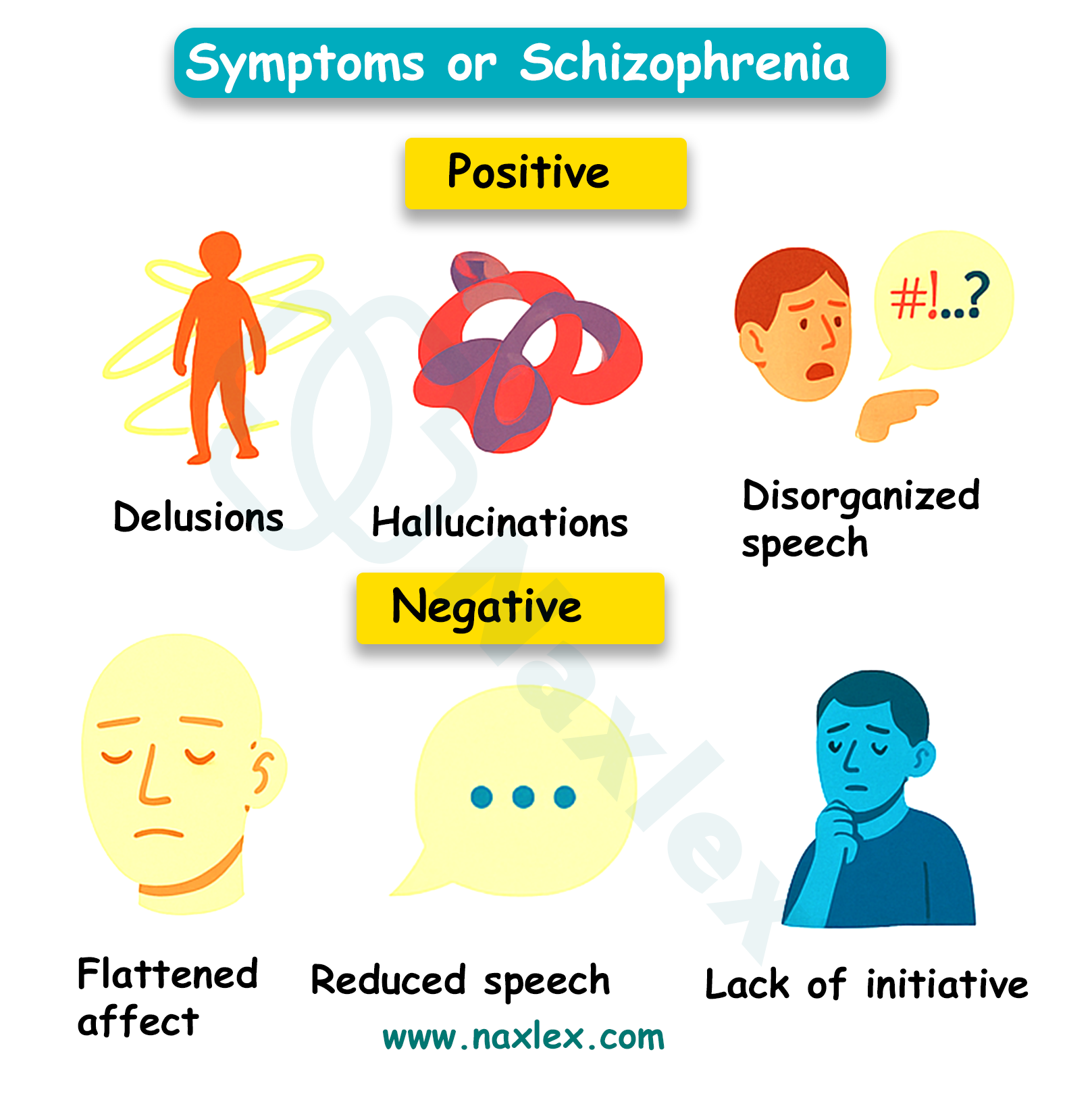
1.2 Functional Impairment and Exclusion Criteria
- Functional impairment in at least one major area—work, interpersonal relations, or self-care—must be evident.
- Exclusion criteria include ruling out schizoaffective disorder, mood disorders with psychotic features, and substance/medication-induced symptoms, as well as pervasive developmental disorders unless prominent delusions/hallucinations are present.
- DSM-5 subtype distinction (e.g. paranoid, disorganized, catatonic) was eliminated due to limited validity in diagnosis and treatment.
Nursing Interventions
1.1 Interventions for Active Hallucinations
- Maintain a calm, non-threatening, supportive environment
- Avoid reinforcing hallucinations (do not pretend to hear/see what they do)
- Acknowledge the patient’s feelings: “I understand you are hearing voices, and that must be frightening.”
- Encourage reality orientation: “I do not hear the voices, but I understand that you do.”
- Distract with reality-based activities (e.g. music, art, games)
- Monitor and document the content, intensity, and effect of hallucinations. Enquire about commands, especially those urging harm to self or others.
- Ensure a safe environment. Remove potential means for self-harm in case of dangerous command hallucinations
- Facilitate medication adherence
Key Table: Interventions for Hallucinations
|
Intervention |
Description |
|
Environment |
Quiet, minimize stimulation |
|
Safety |
1:1 supervision if at risk |
|
Distraction |
Music, drawing, verbal interruption |
|
Stress reduction |
Identify triggers, teach coping strategies |
1.2 Interventions for Delusions
- Build trust through honest, consistent, and non-judgmental interactions
- Do not challenge or argue about delusions; focus instead on feelings and reality orientation
- “That sounds very frightening for you. You are safe here.”
- Explore underlying feelings (fear, anxiety, loneliness)
- Encourage participation in structured, reality-based activities
- Monitor for risk of violence (persecutory/command delusions)
- Engage in cognitive-behavioral strategies to promote alternative explanations
- Maintain a calm tone to avoid escalating suspicion or agitation
1.3 Interventions for Overall Care in Schizophrenia
- Employ therapeutic communication techniques—short, concrete statements; validate emotions
- Support self-care and activities of daily living, often requiring step-by-step instructions
- Encourage medication adherence and psychoeducation
- Protect the patient from self-harm or harm to others (remove hazardous items, monitor for suicide risk)
- Promote social skills training and group therapy
- Facilitate family involvement for better monitoring and relapse prevention
Pharmacological Management
1.1 First-Generation and Second-Generation Antipsychotics
Antipsychotic medications remain the mainstay for the management of schizophrenia:
- First-generation antipsychotics (FGAs, typical):
- Examples: Haloperidol, chlorpromazine, fluphenazine
- Strong D2 blockade; high efficacy for positive symptoms
- Higher risk of extrapyramidal side effects (EPS) and tardive dyskinesia
- Second-generation antipsychotics (SGAs, atypical):
- Examples: Risperidone, olanzapine, quetiapine, clozapine
- Block D2 and 5-HT2A receptors
- Lower EPS risk, but higher risk of metabolic syndrome (weight gain, dyslipidemia, diabetes)
Special note:
- Clozapine is reserved for treatment-resistant schizophrenia. It requires regular blood monitoring due to risk of agranulocytosis (severe neutropenia).
- Long-acting injectable antipsychotics are indicated for patients with poor medication adherence.
1.2 Side Effect Profiles and Monitoring
Table: Side Effects of Antipsychotics
|
Drug Class |
Neurological |
Metabolic |
Rare but Severe |
|
FGAs |
EPS, tardive dyskinesia |
Mild |
Neuroleptic malignant syndrome |
|
SGAs |
Mild EPS (lower risk) |
Weight gain, diabetes, dyslipidemia |
Agranulocytosis (clozapine), myocarditis |
Nursing Role:
- Monitor for side effects (EPS: tremor, rigidity, akathisia; NMS: hyperthermia, rigidity, altered mental status)
- Educate patients and families regarding side effects and necessity of adherence
- Support metabolic health: monitor weight, blood pressure, glucose, lipids
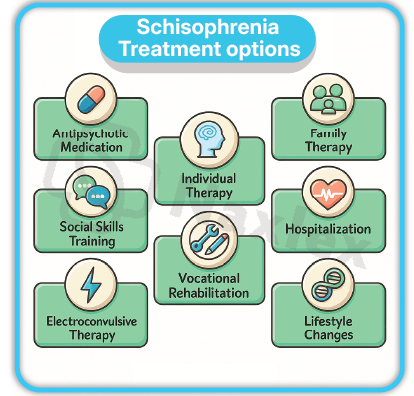
NURSING INSIGHTS
- Command hallucinations can instruct patients to harm themselves or others; safety assessment is always a priority.
- Persecutory delusions raise risk for aggression—prepare safety protocols and involve security if agitation escalates.
- Therapeutic communication: Always approach with empathy and non-confrontational language. Do not reinforce delusions but do not directly challenge them.
- Engage family and support systems to promote adherence and relapse prevention. Psychoeducation is protective.
Psychosocial And Therapeutic Nursing Interventions
- Psychoeducation: For patient and family, enhances medication adherence and relapse prevention
- Cognitive-behavioral therapy (CBT): Focus on reality testing, cope with hallucinations and delusions
- Social skills training: Enhances functioning, reduces isolation
- Occupational/vocational rehabilitation: Prepares for community integration
- Assertive community treatment (ACT): High-intensity, team-based, home/community care
- Substance use management: Address comorbidities (e.g., cannabis, alcohol)
- Support groups: Peer support improves adherence and helps reduce stigma
- Clozapine is the only antipsychotic with proven efficacy in treatment-resistant schizophrenia but carries the risk of agranulocytosis. Nurses must monitor for infections and ensure regular blood counts.
- Second-generation antipsychotics increase the risk of metabolic syndrome; nurses must routinely monitor weight, blood glucose, and lipid profiles.
- Long-acting injectable antipsychotics are particularly well-suited for patients who are non-adherent with oral regimens or frequently lose medications.
- Family psychoeducation and support reduce relapse rates and improve medication adherence. Involve families early and provide resources for community support groups.
Summary
- Schizophrenia is a complex, chronic psychotic disorder with a spectrum of positive, negative, and cognitive symptoms, all of which significantly impair daily functioning.
- Diagnosis is based on clinical assessment:
- At least two characteristic symptoms present for ≥1 month.
- Disturbance persisting for ≥6 months.
- Pathophysiology is rooted in structural abnormalities, and genetic factors.
- Neurochemical abnormalities, especially imbalances in dopamine and glutamate neurotransmission.
- Comprehensive nursing assessment covers physical, emotional, cognitive, and behavioral domains.
- Positive symptoms include auditory hallucinations and persecutory delusions.
- Negative → primary contributors to disability.
- Delusions: persecutory, referential, grandiose, nihilistic.
- Perceptual disturbances: most commonly auditory hallucinations.
- Nursing interventions prioritize safety, and reality orientation. Foster therapeutic alliances through empathetic, clear, and non-confrontational communication.
- Pharmacological treatment: Antipsychotics are the foundation.
- SGAs (second-generation antipsychotics) are most used.
- Clozapine for resistant cases.
- Ongoing side effect surveillance and metabolic monitoring.
- Patient/family psychoeducation.
- Rapid recognition and management of command hallucinations (safety priority).
- Education on medication adherence and side effect monitoring.
- Engagement of families for optimal outcomes.
- Practice questions reinforce applied knowledge for NCLEX and real-world care.
- Build strong understanding of schizophrenia to deliver evidence-based, patient-centered care, promote recovery, and reduce personal and societal burdens of the disease.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Schizophrenia
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


