Please set your exam date
Health and Physical Assessment of the Adult Client
Study Questions
Practice Exercise 1
Which of the following would be most important for a nurse to do to ensure the accuracy of inspection during assessment?
Explanation
Inspection is the first step in physical assessment and involves the systematic observation of the client’s body for normal and abnormal findings. It provides critical visual information about the client's health status, including posture, skin integrity, symmetry, and movement.
Rationale for correct answer:
1. Compare bilateral body parts: Comparing bilateral (left and right) body parts is essential in inspection because it helps identify asymmetry, which may indicate abnormalities such as swelling, muscle atrophy, or joint deformities.
Rationale for incorrect answers:
2.Have 20/20 vision: While good vision aids in assessment, having perfect 20/20 vision is not a requirement for accurate inspection. Nurses may wear corrective lenses if needed. The key factor is observational skill, not visual acuity alone.
3. Focus on selected body systems: Focusing only on selected body systems may limit the scope of the assessment and result in missed findings. Inspection should be systematic and comprehensive, even when targeting a specific complaint.
4. Use touch judiciously: Touch is part of palpation, not inspection. While it is important to use touch appropriately in later phases of assessment, it does not enhance visual inspection itself.
Take home points:
- Comparing bilateral body parts allows the nurse to recognize asymmetry and detect subtle abnormalities during inspection.
- Accurate inspection relies on systematic observation and proper technique, not just on personal physical traits like vision.
Percussion over the stomach reveals a loud, drum-like sound. The nurse would document this finding as which of the following?
Explanation
Percussion is a physical assessment technique used by nurses and other healthcare providers to evaluate the underlying structures of the body by tapping on the surface and interpreting the resulting sound. Each type of tissue (air-filled, fluid-filled, or solid) produces a distinct sound.
Rationale for correct answer:
3. Tympany is a loud, high-pitched, drum-like sound typically heard over air-filled structures, such as the stomach or intestines. It is a normal finding when percussing the abdomen, especially over the gastric bubble or bowel loops.
Rationale for incorrect answers:
1. Dullness is a soft, thud-like sound heard over dense organs, such as the liver or a full bladder, or areas with fluid accumulation or masses.
2. Flatness is a very soft and high-pitched sound heard over bones or muscle, where there is no air.
4. Resonance is a low-pitched, hollow sound heard over normal lung tissue. While it indicates air, it is not as loud or drum-like as tympany.
Take home points:
- Tympany is the expected percussion sound over air-filled organs like the stomach and intestines and should be documented accordingly.
- Understanding different percussion tones (tympany, resonance, dullness, flatness) helps nurses distinguish normal from abnormal findings in various body systems.
When palpating body structures, the nurse uses which sense?
Explanation
Palpation is one of the four basic physical assessment techniques used by nurses and healthcare providers (alongside inspection, percussion, and auscultation). It involves the use of hands and fingers to gather information about the body by feeling for texture, temperature, moisture, tenderness, size, shape, and consistency of body structures.
Rationale for correct answer:
4. Touch is the primary sense used during palpation. The nurse uses the hands to detect changes in the body’s texture, temperature, moisture, masses, pulsations, tenderness, or pain.
Rationale for incorrect answers:
1.Intuition may help guide clinical decision-making based on experience, but it is not a sense and cannot replace the physical act of palpating with the hands.
2. Vision is used in inspection, not palpation. While both are assessment techniques, palpation is based on physical contact, not visual observation.
3. Hearing is used during auscultation, such as when listening to heart, lung, or bowel sounds. It plays no role in palpation, which relies on tactile input.
Take home points:
- Palpation relies on the sense of touch to gather data about the client’s physical state, such as tenderness, temperature, or lumps.
- Each physical assessment technique engages a different sensory pathway-touch for palpation, sight for inspection, hearing for auscultation, and so on.
While conducting a physical assessment, the nurse uses the bell of the stethoscope to hear which type of sounds?
Explanation
Auscultation is a key component of the physical examination that involves listening to internal body sounds using a stethoscope. The stethoscope has two main parts for auscultation: the diaphragm, which detects high-pitched sounds, and the bell, which detects low-pitched sounds.
Rationale for correct answer:
4. Heart sounds: The bell of the stethoscope is designed to pick up low-pitched sounds, such as certain heart sounds-specifically S3, S4, and murmurs, particularly those associated with mitral stenosis.
Rationale for incorrect answers:
1.Tympanic sounds are percussion sounds, not auscultated sounds. They are heard when percussing air-filled areas like the stomach.
2. Bowel sounds are high-pitched, gurgling noises heard best with the diaphragm, not the bell, of the stethoscope.
3. Lung sounds, including breath sounds like crackles or wheezes, are high-pitched and are also best heard using the diaphragm of the stethoscope.
Take home points:
- The bell of the stethoscope is used to auscultate low-pitched heart sounds such as S3, S4, and murmurs.
- Proper stethoscope technique-knowing when to use the bell versus the diaphragm-ensures accurate detection of normal and abnormal findings during auscultation.
Practice Exercise 2
When assessing a patient’s eyes, which instrument would the nurse use to visualize the retina?
Explanation
During a physical examination, accurate assessment of the eyes is essential for detecting abnormalities in vision and underlying health conditions. Choosing the correct instrument for visualization of the retina ensures effective clinical assessment, early detection of eye disease, and appropriate referral.
Rationale for correct answer:
2. Ophthalmoscope: The ophthalmoscope is a handheld instrument used to examine the interior of the eye, particularly the retina, optic disc, blood vessels, and macula.
Rationale for incorrect answers:
1.Otoscope: This instrument is used to inspect the ear canal and tympanic membrane (eardrum). It has a light and magnifying lens, but it is not designed to examine the eye.
3.Stethoscope: A stethoscope is used to auscultate sounds in the body, such as heart, lung, and bowel sounds. It plays no role in eye assessment.
4.Tuning fork: A tuning fork is typically used for hearing and vibration tests, such as the Rinne or Weber test, or to assess peripheral neuropathy. It has no function in examining the eye.
Take home points:
- The ophthalmoscope is the correct tool used to examine internal structures of the eye, especially the retina.
- Understanding the function of each assessment tool is essential to perform accurate and appropriate physical examinations and ensure proper clinical decision-making.
Which technique would a nurse use to assess skin turgor?
Explanation
Skin turgor is a clinical indicator used during a physical assessment to evaluate a client’s hydration status. It reflects the skin’s elasticity and ability to return to its normal position after being pinched.
Rationale for correct answer:
4. Lightly pinch a fold of skin: To assess skin turgor, the nurse gently pinches a fold of skin, usually on the forearm, sternum, or abdomen, and then releases it. If the skin quickly returns to its normal position, turgor is normal.
Rationale for incorrect answers:
1.Indent area with fingertips: This technique is used to assess for pitting edema, not skin turgor. The nurse presses the skin (often over the shin or ankle) to observe if an indentation remains.
2. Use a special type of lighting: Special lighting, like tangential or oblique lighting, may help visualize skin lesions, rashes, or color changes, but it does not assess elasticity or turgor.
3. Touch the area to detect moisture: Touching the skin helps assess temperature or moisture (e.g., dry, clammy, diaphoretic skin) but not elasticity.
Take home points:
- Pinching and releasing a fold of skin is the correct method for assessing turgor, which helps evaluate hydration status.
- Each skin assessment technique serves a different purpose-turgor for hydration, indentation for edema, moisture for temperature/fluid balance.
A patient’s visual acuity is assessed as 20/40 in both eyes using the Snellen chart. The nurse interprets this finding as which of the following?
Explanation
The Snellen chart is a standardized tool used during physical assessments to evaluate visual acuity. The results are recorded as a fraction (e.g., 20/20 or 20/40), where the top number represents the distance at which the patient is standing from the chart (usually 20 feet), and the bottom number represents the distance at which a person with normal vision can read the same line.
Rationale for correct answer:
3. The patient has less than normal vision: A 20/40 Snellen result means the patient can see at 20 feet what a person with normal vision can see at 40 feet. This indicates reduced visual acuity, or less than normal vision. It may warrant further evaluation or correction (e.g., glasses).
Rationale for incorrect answers:
1. The patient can see twice as well as normal: This is the opposite of what 20/40 means. The patient sees less clearly, not better.
2. The patient has double vision: Double vision is known as diplopia, which refers to seeing two images of one object. It is a separate issue and not measured by the Snellen chart.
4. The patient has normal vision: Normal visual acuity is defined as 20/20. A 20/40 result is below normal and may affect tasks like reading small print or driving.
Take home points:
- A 20/40 vision score means the patient sees at 20 feet what a person with normal vision sees at 40 feet-indicating less than normal visual acuity.
- The Snellen chart helps identify the need for vision correction or referral.
When using an otoscope to assess the tympanic membrane of an adult, the nurse straightens the ear canal by gently pulling the pinna in which direction?
Explanation
The otoscope is an essential tool used in physical assessments to examine the external auditory canal and tympanic membrane (eardrum). To obtain a clear view of the tympanic membrane in an adult, the nurse must properly straighten the ear canal, which has a natural curve.
Rationale for correct answer:
1. Up and back: In adults, the ear canal curves upward and backward, so the nurse should gently pull the pinna up and back to straighten the canal for optimal visualization of the tympanic membrane. This allows the otoscope to pass easily and prevents trauma or discomfort.
Rationale for incorrect answers:
2. Down and forward: This method is used for infants and children under age 3, whose ear canals angle more downward and are shorter.
3. Away from the examiner: Pulling the ear "away" is vague and not clinically specific. It does not refer to the anatomical direction required to straighten the canal.
4. In any direction: This is unsafe and inaccurate. Improper manipulation can cause pain or injury and obstruct the view of the tympanic membrane.
Take home points:
- When examining an adult ear, always pull the pinna up and back to straighten the auditory canal and visualize the tympanic membrane.
- The technique for otoscopic examination differs by age: pull down and back for infants and up and back for adults to accommodate anatomical differences.
Practice Exercise 3
Percussion of the thorax reveals a dull sound. The nurse interprets this to indicate which of the following?
Explanation
Percussion is a valuable technique during a physical assessment, especially of the thorax, to determine the underlying structures’ density and composition. Each type of tissue-air-filled, fluid-filled, solid, or bony-produces a distinct percussion sound.
Rationale for correct answer:
4. Fluid or a solid mass: A dull sound on thoracic percussion indicates the presence of fluid (e.g., pleural effusion) or a solid mass (e.g., tumor, consolidated lung as in pneumonia).
Rationale for incorrect answers:
1. An air-filled structure: Air-filled lung tissue produces a resonant sound, which is low-pitched and hollow-not dull.
2. A bony structure: Bone produces a flat sound-very soft and high-pitched-because it is extremely dense and lacks air.
3. Emphysematous tissue: Emphysema causes hyperresonance due to trapped air and overdistended alveoli. This is a loud, lower-pitched sound-not dull.
Take home points:
- A dull sound during thoracic percussion often signals the presence of fluid or solid tissue, such as in pneumonia, tumors, or pleural effusion.
- Knowing the characteristic percussion sounds-resonance (air), dullness (fluid/solid), flatness (bone), tympany (gas)-helps nurses detect underlying thoracic abnormalities early.
The nurse auscultates the thorax and lungs and hears coarse gurgling sounds on expiration. The nurse would describe these sounds as:
Explanation
Auscultation of the lungs is a vital component of respiratory assessment. Breath sounds are classified as normal (e.g., vesicular, bronchial, bronchovesicular) or abnormal (adventitious).
Rationale for correct answer:
1. Adventitious breath sounds are abnormal lung sounds that include crackles (rales), wheezes, rhonchi, and pleural friction rubs. Coarse gurgling sounds heard on expiration are typically rhonchi.
Rationale for incorrect answers:
2. Bronchovesicular breath sounds: These are normal breath sounds heard over the mainstem bronchi. They are moderate in pitch and intensity, with equal inspiration and expiration.
3. Vesicular breath sounds: These are soft, low-pitched normal sounds heard over most of the lung fields. Inspiration is longer than expiration, and no gurgling or harshness is present.
4. Bronchial sounds: These are harsh, high-pitched normal sounds heard over the trachea. Expiration is longer than inspiration.
Take home points:
- Adventitious breath sounds are abnormal and include rhonchi, which sound like coarse gurgling or snoring and often indicate secretions in the airways.
- Differentiating normal from abnormal lung sounds is essential for identifying respiratory problems and guiding timely interventions.
When assessing heart sounds, the nurse understands that the sounds heard reflect which of the following?
Explanation
Cardiac auscultation is a fundamental part of the physical assessment and allows nurses to evaluate the mechanical function of the heart through sound. Heart sounds are primarily generated by the closure of valves in the heart, not the flow of blood or muscle contraction directly.
Rationale for correct answer:
3. Closure of the heart valves: The first heart sound (S1, “lub”) occurs with closure of the mitral and tricuspid valves at the beginning of ventricular systole. The second heart sound (S2, “dub”) corresponds to closure of the aortic and pulmonic valves at the end of systole.
Rationale for incorrect answers:
1. Blood flow through the heart: While blood flow is a continuous and essential process in cardiac function, it is generally silent under normal conditions.
2. Blood moving into the heart from the aorta: Blood does not move from the aorta into the heart; instead, it flows out of the left ventricle into the aorta during systole.
4. Contraction of the cardiac muscle: Although cardiac contraction (systole) is an integral part of the cardiac cycle, it does not directly produce the heart sounds heard during auscultation.
Take home points:
- Heart sounds are primarily caused by the closure of cardiac valves.
- S1 and S2 are the two main heart sounds: S1 is from atrioventricular (AV) valve closure, and S2 is from semilunar valve closure.
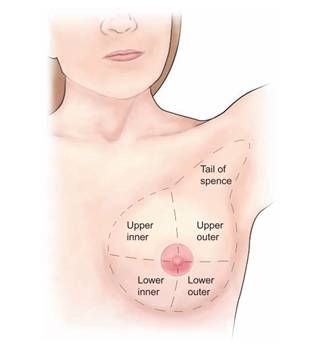
When palpating the breast of a woman during an assessment, the nurse would divide the breast into which of the following?
Explanation
Breast assessment is an essential part of a comprehensive physical examination, especially for early detection of abnormalities such as lumps, cysts, or signs of breast cancer.
Rationale for correct answer:
1. Quadrants: The breast is commonly divided into four quadrants (upper outer, upper inner, lower outer, lower inner) and the tail of Spence (which extends into the axilla) during physical examination. This division facilitates a systematic approach to palpation.
Rationale for incorrect answers:
2. Halves: Dividing the breast into halves (e.g., right/left or top/bottom) is not standard practice. This method is too vague and lacks clinical specificity when locating findings.
3. Entire breast tissue: While it is essential to palpate the entire breast, this option does not describe how the breast is divided during palpation.
4. Bilateral comparison: While comparing one breast to the other is important to assess symmetry or detect abnormalities, this is not how a single breast is divided during palpation.
Take home points:
- Dividing the breast into quadrants and assessing the tail of Spence ensures a systematic and thorough breast exam.
- Precise anatomical terminology in assessments supports early detection and treatment of breast abnormalities.
Practice Exercise 4
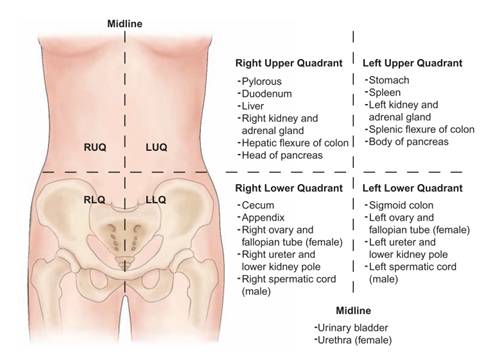
After inspecting a patient’s abdomen, which technique would the nurse do next?
Explanation
During a physical assessment of the abdomen, the nurse must follow a specific sequence to ensure accurate findings and avoid altering bowel sounds. The four primary techniques used in abdominal assessment are inspection, auscultation, percussion, and palpation.
Rationale for correct answer:
3. Auscultation is done first (before touching the abdomen) to listen to bowel sounds in their natural state, assessing frequency, intensity, and presence.
Rationale for incorrect answers:
1. Percussion: While percussion is part of the abdominal assessment, it follows auscultation. Performing percussion too early may alter the natural bowel sounds or cause discomfort.
2. Palpation: Palpation should be performed last because it can stimulate peristalsis, thereby falsely increasing bowel sound frequency. Early palpation can lead to misinterpretation of bowel activity or mask underlying tenderness.
4. Whichever the patient agrees to: Although patient comfort and consent are always prioritized, the assessment technique order is based on clinical guidelines to avoid compromising assessment accuracy.
Take home points:
- The correct sequence for abdominal assessment is: inspection → auscultation → percussion → palpation.
- This order ensures that bowel sounds are assessed accurately before any manipulation of the abdomen occurs.
When assessing a patient’s mental status, which of the following would the nurse be least likely to include when evaluating level of awareness?
Explanation
When assessing a patient’s mental status, evaluating level of awareness is essential in determining the client’s cognitive function and neurological integrity.
Rationale for correct answer:
4. Level of consciousness: While closely related to mental status, level of consciousness refers to how awake, alert, and responsive a patient is (e.g., alert, lethargic, stuporous, comatose). It is assessed before orientation but is a separate parameter from awareness.
Rationale for incorrect answers:
1. Orientation to time: This assesses whether the patient knows the current day, date, or time of day (e.g., morning or evening). It is a component of the mental status exam and helps determine whether the patient is oriented.
2. Ability to state where he is: This checks for orientation to place, another critical component of awareness. It shows whether the patient recognizes their environment (e.g., home, hospital, city).
3. Ability to state name: This checks for orientation to person. A patient’s ability to recall their name is a basic aspect of awareness and identity.
Take home points:
- Orientation to person, place, and time is used to assess a client’s level of awareness during a mental status exam.
- Level of consciousness is distinct from orientation- it is evaluated separately as it reflects arousal and responsiveness, not cognitive orientation.
A nurse is conducting an assessment of a patient’s cranial nerves. The nurse asks the patient to raise the eyebrows, smile, and show the teeth to assess which cranial nerve?
Explanation
Assessment of cranial nerves is an essential part of the neurological examination. Each cranial nerve has a specific function, including sensory (e.g., smell, vision), motor (e.g., facial movement, tongue movement), or both.
Rationale for correct answer:
3. Facial: The facial nerve (cranial nerve VII) controls the muscles of facial expression. Asking the patient to raise eyebrows, smile, frown, and show teeth tests the motor function of this nerve.
Rationale for incorrect answers:
1. Olfactory: The olfactory nerve (cranial nerve I) is responsible for the sense of smell. Testing it involves identifying familiar odors with the eyes closed. It is not involved in facial movement or expression.
2. Optic: The optic nerve (cranial nerve II) is responsible for vision, including visual acuity and visual fields. It is tested using visual charts or confrontation testing.
4. Vagus: The vagus nerve (cranial nerve X) is involved in functions such as voice, swallowing, and parasympathetic control of the heart and digestive tract. Testing it involves evaluating the gag reflex and palate movement.
Take-home points:
- The facial nerve (cranial nerve VII) is tested by assessing facial expressions such as smiling, frowning, and raising eyebrows.
- Understanding the function of each cranial nerve is key to correctly assessing neurological integrity and identifying potential areas of dysfunction.
Comprehensive Questions
Which is a normal finding on auscultation of the lungs?
Explanation
Lung assessment is a key component of a comprehensive physical examination. Nurses and healthcare providers use percussion and auscultation to evaluate lung structure and function.
Rationale for correct answer:
2. Resonance over the left upper lobe: Resonance is the expected normal percussion sound over healthy lung tissue, including the left upper lobe. It indicates the presence of air within the alveoli and suggests that the lung is well-aerated.
Rationale for incorrect answers:
1. Tympany over the right upper lobe: Tympany is a high-pitched, drum-like sound typically heard over air-filled organs like the stomach or in cases of a large pneumothorax. It is not normal over lung tissue, including the right upper lobe.
3. Hyperresonance over the left lower lobe: Hyperresonance is louder and lower-pitched than normal resonance and often suggests excess air, as seen in emphysema or a pneumothorax. It is not a normal finding over any lung area and should prompt further evaluation.
4. Dullness above the left 10th intercostal space: Dullness on percussion indicates increased density, such as fluid (pleural effusion) or consolidation (pneumonia). This is not a normal finding and may signal underlying pathology in the lung or pleural space.
Take-home points
- Resonance is the normal percussion sound over healthy, aerated lung fields.
- Any deviation-such as dullness, tympany, or hyperresonance-may indicate underlying pathology.
The nurse positions the client sitting upright during palpation of which area?
Explanation
In physical assessment, client positioning is crucial for accurate inspection, palpation, percussion, and auscultation. The nurse selects positions that provide the best access to anatomical areas while maintaining client comfort and dignity.
Rationale for correct answer:
3. Breast: Palpation of the breasts is commonly performed with the client in multiple positions, including sitting upright, particularly during inspection and palpation of the axillary (underarm) area and lymph nodes.
Rationale for incorrect answers:
1. Abdomen: The abdomen is best palpated with the client in the supine position, lying flat with knees slightly flexed. This relaxes the abdominal muscles and provides optimal access to all four quadrants for light and deep palpation.
2. Genitals: Genital examination typically requires the lithotomy position for females (lying on back with legs elevated and supported) or standing or supine for males, depending on the purpose (e.g., hernia exam or testicular palpation).
4. Head and neck: While inspection of the head and neck is commonly done with the client sitting upright, palpation (e.g., of lymph nodes, thyroid gland) is often performed with the client sitting but with the head slightly tilted or extended, not strictly upright.
Take home points
- The sitting upright position is used during breast palpation, especially when assessing axillary tissue and lymph nodes.
- Proper positioning varies by assessment area.
After auscultating the abdomen, the nurse should report which finding to the primary care provider?
Explanation
Auscultation of the abdomen is a vital step in assessing gastrointestinal and vascular function. It helps detect bowel motility, vascular abnormalities, and potential obstructions. Normally, bowel sounds are present and irregular, occurring every 5-15 seconds.
Rationale for correct answer:
1. Bruit over the aorta: A bruit is a swishing or whooshing sound heard over an artery, indicating turbulent blood flow-often due to aneurysm or arterial stenosis. A bruit over the abdominal aorta can signal an abdominal aortic aneurysm (AAA), a potentially life-threatening condition.
Rationale for incorrect answers:
2.Absence of bowel sounds for 60 seconds: Bowel sounds can be irregular, and 60 seconds is not enough time to confirm absence. To declare absent bowel sounds, the nurse must listen in all four quadrants for a full 5 minutes.
3. Continuous bowel sounds over the ileocecal valve: The ileocecal valve, located in the right lower quadrant, is often the most active region of the abdomen. Continuous or frequent bowel sounds here may be normal, especially after eating.
4. A completely irregular pattern of bowel sounds: Bowel sounds are normally irregular in rhythm and timing. They can vary in pitch and frequency, and this irregularity is a normal finding.
Take home points
- A bruit over the abdominal aorta is an abnormal vascular sound and may indicate a serious condition like an abdominal aortic aneurysm. It should be reported immediately.
- Bowel sounds are naturally irregular-their absence must be confirmed by listening for a full 5 minutes before reporting.
If unable to locate the client’s popliteal pulse during a routine examination, what should the nurse do next?
Explanation
Peripheral pulse assessment is a critical component of the circulatory examination. Nurses evaluate the strength, rate, rhythm, and presence of pulses to determine adequate blood flow to the extremities.
Rationale for correct answer:
1. Check for a pedal pulse: If the popliteal pulse is absent or difficult to palpate, the nurse should immediately check distal pulses, such as the dorsalis pedis or posterior tibial pulses, to assess whether circulation is intact below the knee.
Rationale for incorrect answers:
2. Check for a femoral pulse: While checking the proximal (femoral) pulse might be appropriate after distal pulses are absent or diminished, it is not the immediate next step. First, the nurse should assess whether blood flow continues beyond the popliteal area by checking distal pulses.
3. Take the client’s blood pressure on that thigh: Thigh blood pressure is not typically indicated for routine peripheral pulse evaluation and may be technically difficult or inaccurate without specialized equipment (e.g., thigh cuff, Doppler).
4. Ask another nurse to try to locate the pulse: While collaboration can be helpful, the nurse should first complete their own assessment, starting with other distal pulses. Asking for help is secondary unless there's uncertainty or need for confirmation after following proper protocol.
Take-home points
- If a peripheral pulse is not palpable, always check a more distal pulse next to evaluate if blood flow continues beyond the affected site.
- The presence of distal pulses (e.g., dorsalis pedis or posterior tibial) indicates that circulation is adequate, even if the popliteal pulse cannot be felt.
Which of the following is an expected finding during assessment of the older adult?
Explanation
Aging brings about predictable and progressive physiological changes in all body systems. These changes are not necessarily indicative of disease but represent a normal part of the aging process.
Rationale for correct answer:
2. Decreased peripheral, color, and night vision: Older adults commonly experience: Decreased peripheral vision (due to retinal changes), Reduced color discrimination (particularly blues and greens), Poorer night vision (due to reduced pupil size and lens transparency).
Rationale for incorrect answers:
1.Facial hair that becomes finer and softer: In older adults, especially women, facial hair may actually become coarser and more noticeable due to hormonal changes, particularly decreased estrogen and relative androgen excess.
3. Increased sensitivity to odors: Olfactory sensitivity declines with age due to loss of olfactory neurons and decreased mucosal receptors. Older adults often have reduced ability to detect and distinguish smells, which can affect appetite and safety (e.g., detecting gas leaks or spoiled food).
4. An irregular respiratory rate and rhythm at rest: While the respiratory system ages (e.g., decreased lung elasticity and vital capacity), a regular rate and rhythm is still expected at rest.
Take home points
- Decreased peripheral, color, and night vision are expected in older adults due to physiological changes in the eye (e.g., presbyopia, retinal thinning, and lens clouding).
- Unexpected changes in respiratory rhythm or heightened smell sensitivity are not normal with aging and should prompt further clinical evaluation.
If the client reports loss of short-term memory, the nurse would assess this using which one of the following?
Explanation
Short-term memory, which refers to the ability to retain and recall information recently acquired-typically within minutes. Short-term memory is often the first type affected in conditions such as delirium, dementia, or following brain injury.
Rationale for correct answer:
3. Ask the client to describe how he or she arrived at this location: Asking the client how they arrived (e.g., which route they took or who brought them) is an effective way to assess short-term memory, as it involves recalling recent events.
Rationale for incorrect answers:
1. Have the client repeat a series of three numbers, increasing to eight if possible: This test assesses attention span and immediate recall, not short-term memory. It is often used to evaluate concentration and the ability to retain and repeat information in the moment.
2. Have the client describe his or her childhood illnesses: This evaluates long-term (remote) memory, not short-term memory. Questions about childhood events, past jobs, or places lived help assess whether distant memories remain intact.
4. Ask the client to count backward from 100 subtracting seven each time: This is known as the serial sevens test, and it assesses concentration, attention, and executive function, not short-term memory.
Take home points
- Short-term memory is best evaluated by asking the client to recall recent events.
- Different cognitive functions are assessed with different techniques, so choosing the right method ensures accurate evaluation.
To palpate lymph nodes, the nurse uses which technique?
Explanation
Lymph node palpation is a vital part of the head-to-toe physical exam, especially during head, neck, axillary, and inguinal assessments. It helps identify signs of infection, inflammation, or malignancy.
Rationale for correct answer:
3. Use the pads of two fingers in a circular motion: This is the recommended technique for palpating lymph nodes. The nurse uses the pads of the index and middle fingers, applying gentle pressure in a circular motion to detect superficial nodes.
Rationale for incorrect answers:
1. Use the flat of all four fingers in a vertical and then side-to-side motion: This technique is more appropriate for assessing the chest wall or abdominal structures, not for palpating lymph nodes.
2. Use the back of the hand and feel for temperature variation between the right and left sides: While the back of the hand (dorsal surface) is used to assess temperature, it is not used for palpating lymph nodes.
4. Compress the nodes between the index fingers of both hands: Compressing lymph nodes between fingers may not allow for an accurate assessment and could miss deeper nodes or fail to detect subtle changes in consistency.
Take home points
- The correct method to palpate lymph nodes is using the pads of two fingers in a circular motion, allowing for precise assessment of node size, texture, and mobility.
- Avoid using broad surfaces like the flat of the hand or non-sensitive areas like the back of the hand-these are not appropriate for lymph node evaluation.
A patient has been admitted from the emergency department (ED) with a primary problem of abdominal pain. Diagnostic tests performed in the ED are pending. The nurse focuses an examination on the abdomen and uses the following techniques. Which technique is correct?
Explanation
When assessing a client with abdominal pain, the nurse must follow a specific order of physical assessment techniques: inspection, auscultation, percussion, and palpation-unlike in other systems where palpation may follow auscultation.
Rationale for correct answer:
1. Perform auscultation first: In abdominal assessment, auscultation is performed before percussion and palpation to prevent disturbing the bowel sounds
Rationale for incorrect answers:
2. Have patient place folded arms under the head: Folding arms behind the head tightens the abdominal wall, making it more difficult to palpate or inspect. The correct position is supine with arms at the sides or across the chest to promote relaxation of the abdominal muscles.
3. Palpate the patient’s painful area first: Palpating the painful site first could lead to guarding, involuntary muscle contraction, or missed findings elsewhere.
4. Observe the contour of the abdomen while asking the patient to take a deep breath and hold it. While observing the abdominal contour is appropriate, asking the patient to take a deep breath and hold it is not part of standard abdominal inspection.
Take home points
- Always auscultate the abdomen before palpation or percussion to avoid altering bowel sounds and ensure accurate assessment.
- Palpate tender areas last and keep the client’s arms at their sides to promote relaxation and allow for a more effective abdominal examination.
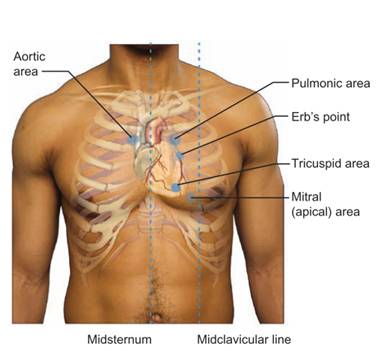
Which number corresponds to the area of the chest where you would auscultate for the tricuspid valve?
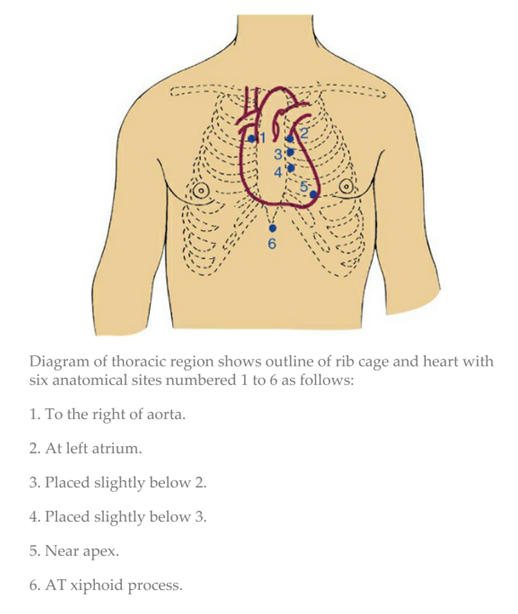
Explanation
Auscultation of the heart involves listening to specific valve areas over the chest to assess the function and detect abnormalities in heart sounds. These valve areas do not correspond precisely to the anatomical position of the valves, but rather to where the sounds are best heard.
Rationale for correct answer:
4. Placed slightly below 3 (Lower Left Sternal Border): Number 4 represents the 4th or 5th left intercostal space at the lower left sternal border, the traditional location for auscultating the tricuspid valve.
Rationale for incorrect answers:
1. To the right of aorta: This is the 2nd right intercostal space, where the aortic valve is auscultated.
2. At left atrium (2nd left intercostal space): This is the pulmonic valve area, not the tricuspid. Located at the 2nd left intercostal space, this site is used for auscultating pulmonic valve sounds.
3. Placed slightly below 2: This is near Erb’s point (3rd left intercostal space), where both aortic and pulmonic murmurs may be heard equally well-but it's not specific to the tricuspid valve.
5. Near apex: This is the mitral valve area, located at the 5th intercostal space at the midclavicular line, where mitral valve sounds are best heard (especially mitral regurgitation or stenosis murmurs).
6. At xiphoid process: It may be useful for detecting certain low-frequency heart sounds in children but is not used for valve assessment in adults.
Take home points:
- The tricuspid valve is best auscultated at the lower left sternal border in the 4th or 5th intercostal space.
- Knowing the auscultation sites for all four heart valves (aortic, pulmonic, tricuspid, and mitral) helps identify specific murmurs and cardiac abnormalities more accurately.
The nurse is teaching a patient to prevent heart disease. Which information should the nurse include? Select all that apply
Explanation
Heart disease remains the leading cause of death worldwide, but many cases are preventable through lifestyle modifications and early risk-factor management. Nurses play a critical role in educating patients about strategies to reduce their risk of cardiovascular disease.
Rationale for correct answer:
2. Talk with your health care provider about taking a daily low dose of aspirin: Daily low-dose aspirin therapy may be beneficial for certain individuals at high risk for heart disease (e.g., those with a history of heart attack or stroke).
3. Work with your health care provider to develop a regular exercise program: Regular physical activity helps reduce blood pressure, control weight, improve cholesterol levels, and boost cardiovascular fitness.
4. Limit saturated and trans fats, sodium, red meats, sweets, and sugar-sweetened beverages: A heart-healthy diet includes reducing intake of saturated and trans fats (which raise LDL cholesterol), processed foods high in sodium, red meat, and added sugars.
5. Review strategies to encourage the patient to quit smoking: Smoking is a major modifiable risk factor for heart disease. Nurses should assess readiness to quit, provide resources such as counseling or nicotine replacement, and refer to cessation programs.
Rationale for incorrect answer:
1.Add salt to every meal: Excessive sodium intake is associated with high blood pressure, a major risk factor for heart disease and stroke. Rather than adding salt, patients should be encouraged to limit sodium intake to <2,300 mg/day (or lower if hypertensive).
Take home points
- Heart disease prevention focuses on lifestyle changes, such as diet, exercise, smoking cessation, and individualized risk assessments (e.g., aspirin use).
- Patient education should emphasize what to limit (e.g., sodium, fats, smoking) and what to increase (e.g., activity, healthy food choices) to promote cardiovascular health.
The nurse is assessing the cranial nerves. Match the cranial nerve with its related function.
Explanation
The cranial nerves (CN I–XII) emerge directly from the brain and brainstem and control various motor, sensory, and parasympathetic functions of the head, neck, and some thoracic organs. During a comprehensive neurological assessment, the nurse must test these nerves to identify signs of neurologic dysfunction.
Rationale for correct answers:
1.XII Hypoglossal -e. Position of the tongue
The hypoglossal nerve controls the motor movement of the tongue. During assessment, the client is asked to stick out the tongue, and deviation or weakness indicates impairment of CN XII.
2. V Trigeminal -a. Motor innervation to the jaw
The trigeminal nerve has both motor and sensory components. Motor function includes muscles of mastication (chewing). The nurse assesses jaw movement and strength.
3. VI Abducens -b. Lateral movement of the eyeballs
The abducens nerve controls the lateral rectus muscle, which moves the eye laterally (abduction). Inability to look outward may suggest CN VI palsy.
4. IV Trochlear -d. Downward, inward eye movements
The trochlear nerve controls the superior oblique muscle, responsible for downward and inward eye movement. Difficulty with this motion may lead to vertical diplopia (double vision).
5. X Vagus -c. Sensation of the pharynx
The vagus nerve provides sensory innervation to the pharynx and larynx, and also has motor and parasympathetic functions. It plays a role in swallowing, speech, and the gag reflex.
Take home points
Each cranial nerve has specific motor, sensory, or both functions, and testing them individually helps identify the location and extent of neurological impairment.
- Cranial nerves IV (Trochlear), VI (Abducens), and III (Oculomotor) are especially important for eye movement coordination.
- CN V (Trigeminal) and XII (Hypoglossal) focus on facial sensation/mastication and tongue movement, respectively.
The nurse is observing the patient for general appearance and behavior. What assessments might indicate that the patient is in pain? Select all that apply
Explanation
Pain is a subjective experience, but nurses can often detect pain through careful observation of a patient’s general appearance and behavior. Nonverbal cues such as posture, facial expressions, guarding behaviors, respiratory patterns, and general responsiveness are important indicators.
Rationale for correct answers:
1. Is slumped in the bed: A slumped posture can indicate discomfort or fatigue related to pain. Patients in pain often avoid repositioning themselves due to the fear of aggravating pain.
3. Is short of breath and breathing rapidly: Pain can activate the sympathetic nervous system, leading to increased respiratory rate and shallow breathing. This is especially common with acute or severe pain.
4. Protects and splints the left arm: Guarding or splinting a body part is a classic nonverbal sign of pain. It reflects an attempt to minimize movement and protect the area from further discomfort.
Rationale for incorrect answers:
2. Responds to questions by making eye contact: Making eye contact and appropriately responding to questions suggest the patient is engaged and cooperative.
5. Is alert and oriented: Being alert and oriented indicates intact cognition and neurological function. While pain does not rule out alertness, this finding is not directly associated with signs of discomfort or distress.
Take home points:
- Nonverbal cues such as guarding, altered posture, and increased respiratory rate can signal that a patient is experiencing pain, especially if the patient is unable to verbalize it.
- Objective observation during general assessment plays a key role in identifying pain and initiating timely interventions to promote comfort and prevent complications.
A patient has undergone surgery for a femoral artery bypass. The surgeon’s orders include assessment of dorsalis pedis pulses. The nurse will use which of the following techniques to assess the pulses? Select all that apply
Explanation
After a femoral artery bypass, careful monitoring of distal perfusion is critical to detect signs of occlusion or ischemia early. One of the most important parameters is the assessment of distal pulses, such as the dorsalis pedis pulse, which provides information about blood flow to the lower extremities.
Rationale for correct answers:
2. Have the patient slightly flex the knee with the foot resting on the bed: Slightly flexing the knee and allowing the foot to rest on the bed relaxes the muscles of the lower leg and foot, making it easier to palpate the dorsalis pedis pulse on the dorsum (top) of the foot.
3. Have the patient relax the foot while lying supine: The dorsalis pedis pulse is best palpated when the client is in a supine position with the foot relaxed. This ensures muscles are not contracted, which could make the pulse more difficult to detect.
Rationale for incorrect answers:
1. Place the fingers behind and below the medial malleolus: This technique is used to palpate the posterior tibial pulse, not the dorsalis pedis pulse. The posterior tibial artery runs behind the medial malleolus (inner ankle), while the dorsalis pedis artery is located on the top of the foot.
4. Palpate the groove lateral to the flexor tendon of the wrist: This describes the technique for assessing the radial pulse, which is located on the wrist. It is unrelated to the dorsalis pedis pulse or assessing lower extremity circulation.
Take home points:
- The dorsalis pedis pulse is located on the top of the foot, lateral to the extensor hallucis longus tendon.
- It is best assessed with the patient lying supine and the foot relaxed.
- Post-femoral artery bypass, monitoring distal pulses like the dorsalis pedis is essential to ensure graft patency and detect early signs of limb ischemia.
Which of the following are normal findings you should find during a physical exam? Select all that apply
Explanation
Recognizing normal versus abnormal findings is critical in identifying early signs of illness, ensuring accurate documentation, and promoting prompt interventions when needed.
Rationale for correct answers:
1. Jugular vein flattens when a patient sits up: This is a normal finding. When a patient is sitting upright, gravity reduces venous return, causing the jugular vein to flatten or become non-distended.
4. Normal sitting posture involves some degree of rounding of the shoulders: Slight rounding of the shoulders is a normal postural variation, especially in older adults. However, marked kyphosis (extreme curvature) would be abnormal.
5. Normally there is no bulging within the intercostal spaces during breathing: In a healthy individual, intercostal spaces remain flat or slightly retracted during normal breathing. Bulging of the intercostal spaces may indicate air trapping, increased intrathoracic pressure, or respiratory distress.
Rationale for incorrect answers:
2. A swooshing sound is normally heard when auscultating a carotid artery: A swooshing sound, known as a bruit, is abnormal. It suggests turbulent blood flow, often caused by atherosclerosis or narrowing of the artery. A normal carotid auscultation should be silent, without bruit.
3. Upon palpation, a lymph node is normally tender: Normal lymph nodes are usually non-tender, soft, movable, and small. Tender lymph nodes suggest infection or inflammation, while hard or fixed nodes may raise concern for malignancy.
Take home points:
- Silence is normal when auscultating carotid arteries; a bruit signals vascular abnormality.
- Understanding subtle normal variations, such as minor postural changes or lymph node characteristics, helps distinguish pathology from healthy findings.
The nurse is assessing a patient who returned 1 hour ago from surgery for an abdominal hysterectomy. Which assessment finding would require immediate follow-up?
Explanation
After surgery, especially major abdominal procedures like a hysterectomy, patients are closely monitored for signs of postoperative complications. Nurses play a critical role in identifying early signs of respiratory depression, hemorrhage, infection, or impaired circulation.
Rationale for correct answers:
3. Respiratory rate of 8 breaths/min is below the normal range (12-20 breaths/min) and may indicate respiratory depression, which is a serious and potentially life-threatening complication, particularly after receiving opioids for postoperative pain control.
Rationale for incorrect answers:
1. Auscultation of an apical heart rate of 76 is within the normal adult range (60-100 bpm) and is expected postoperatively, especially when the patient is resting and under pain control.
2. Absence of bowel sounds on abdominal assessment: It is expected for bowel sounds to be absent or hypoactive immediately after abdominal surgery due to the effects of anesthesia and surgical manipulation of the intestines.
4. Palpation of dorsalis pedis pulses with strength of +2: A pulse strength of +2 is normal and indicates adequate peripheral circulation. There is no indication of vascular compromise, and this finding is reassuring, not alarming.
Take home points:
- Always assess respiratory rate and depth closely after surgery, especially within the first few hours when opioid analgesics can depress respiratory drive.
- Not all abnormal findings require urgent intervention postoperatively-learn to distinguish expected effects of surgery (like decreased bowel sounds) from dangerous signs (like respiratory depression).
Exams on Health and Physical Assessment of the Adult Client
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Health Assessment
- The Health History
- Components Of A Health History
- Physical Assessment
- Practice Exercise 1
- General Survey
- Assessing The Integument
- Assessing The Head And Neck
- Practice Exercise 2
- Assessing The Thorax And Lungs
- Assessing The Cardiovascular And Peripheral Vascular Systems
- Assessing The Breasts And Axillae
- Practice Exercise 3
- Assessing The Abdomen
- Assessing The Muscular System
- Assessment Of Female Genitals And Inguinal Area
- Assessment Of Male Genitals And Inguinal Area
- Assessing The Neurologic System
- Practice Exercise 4
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Explain the purposes and types of health assessment.
- Follow guidelines for conducting a health history.
- Prepare the patient and the environment for a health assessment.
- Identify the equipment and positions used during a physical assessment.
- Use the techniques of inspection, palpation, percussion, and auscultation appropriately during a physical assessment.
- Conduct a physical assessment in a systematic manner.
- Document health assessment findings in a concise, descriptive, and legally appropriate manner.
- Describe nursing responsibilities before, during, and after diagnostic procedures.
Introduction
Conducting a health assessment involves collecting, validating, and analyzing subjective data (also called symptoms) and objective data (also called signs) to determine the overall level of physical, psychological, sociocultural, developmental, and spiritual health of a patient.
- Subjective data are experienced or known only by the patient (e.g., pain and nausea), and are gathered by verbal report during the health history.
- Objective data are directly observed or elicited through physical examination techniques.
Health Assessment
3.1 Types of health assessment:
Health assessment is an integral component of nursing care and is the foundation of the nursing process.
A health assessment may be comprehensive, ongoing partial, focused, or emergency.
- A comprehensive assessment with a health history and complete physical examination is usually conducted when a patient first enters a healthcare setting, with information providing a baseline for comparing later assessments.
- An ongoing partial assessment is one that is conducted at regular intervals (e.g., at the beginning of each home health visit or each hospital shift) during care of the patient.
- A focused assessment is conducted to assess a specific problem.
- An emergency assessment is a type of rapid focused assessment conducted to determine potentially fatal situations.
Assessments are used to plan, implement, and evaluate teaching and care to promote an optimal level of health through interventions to prevent illness, restore health, and facilitate coping with disabilities or death.
3.2 Preparing the patient:
When conducting a nursing health assessment, it is important to consider and remain sensitive to the patient’s physiologic needs and psychological needs.
- Explain that the first part of the assessment will involve questions about the patient’s health concerns, health habits, and lifestyle.
- Inform the patient that after the health history is completed, body structures will be examined.
- Explain that drapes (covers) will be used during the examination, and only the area being assessed will be exposed and that the assessments should not be painful.
- Ask the patient to empty the bladder before the examination to both promote patient comfort.
- Nurses must consider patients within the context of family, culture, and community.
3.3 Preparing the environment:
Clinics, offices, and hospitals may have a special examination room that provides a quiet, private space for assessment.
- If such a room is available, the examination table is prepared, a gown and drape for the patient are provided, and instruments and special supplies needed for the assessment are gathered.
- If the area is open to others, an enclosure with a curtain or screen is essential.
- The room should be warm enough to prevent chilling, and the area or room should be adequately lighted, either by sunlight or overhead lighting.
The Health History
A health history is a collection of subjective data that provides a detailed profile of the patient’s health status. The health history helps the nurse identify risk factors for alterations in health.
Components Of A Health History
1. Biographical Data
Biographical information is often collected during admission to a healthcare facility or agency and documented on a specific form. Biographical data include:
- Name
- Address
- Gender
- Marital status
- Occupation
- Religious preference
- Healthcare financing
- Primary healthcare provider
2. Reason for Seeking Healthcare:
The patient’s reason for seeking care helps to focus the rest of the assessment.
Ask an open-ended question, such as, “Tell me why you are here today.” Be sure to document in the patient’s own words.
3. History of Present Health Concern
When taking the patient’s history of present health concern, be sure to explore the symptoms thoroughly.
4. Medical History:
A patient’s medical history may provide insight to causes of current symptoms. It also alerts the nurse to certain risk factors.
Medical history includes past illnesses, chronic health problems and treatment, and previous surgeries or hospitalizations.
5. Family History
Certain disorders have genetic links.
6. Lifestyle:
A patient’s lifestyle contributes to his or her overall health and well-being- smoking, sleep, feeding, exercise.
Physical Assessment
The physical assessment is usually conducted in a head-to-toe sequence or a system sequence but can be adapted to meet the needs of the patient.
It is often necessary to modify the sequence, positions, and specific assessments based on the patient’s age, energy level, cognitive and physical state, as well as time constraints.
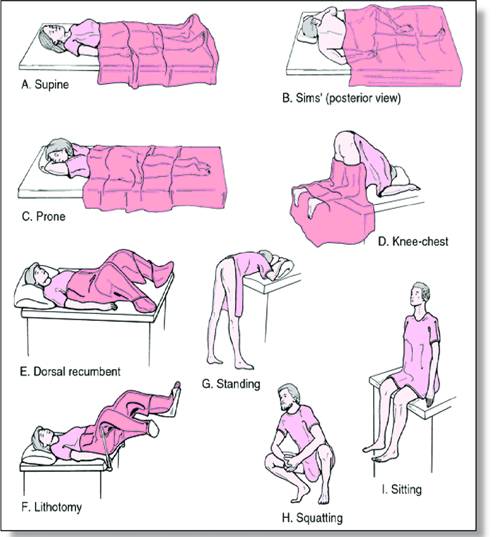
Positioning during a physical assessment:
During positioning, it is important to consider the patient’s age, culture, health status, mobility, physical condition, energy level, and privacy.
Uncomfortable or embarrassing positions should not be maintained for long periods.
|
Positioning |
Purpose |
|
Standing |
It is used to assess posture, balance, and gait (while walking upright). |
|
Sitting |
It allows visualization of the upper body, facilitates full lung expansion, and is used to assess vital signs and the head, neck, anterior and posterior thorax, lungs, heart, breasts, and upper extremities. |
|
Supine |
It facilitates abdominal muscle relaxation and is used to assess vital signs and the head, neck, anterior thorax, lungs, heart, breasts, abdomen, extremities, and peripheral pulses. |
|
Prone |
It is used to assess the hip joint and the posterior thorax. |
|
Dorsal Recumbent |
It is used to assess the head, neck, anterior thorax, lungs, heart, breasts, extremities, and peripheral pulses. It should not be used for abdominal assessment because it causes contraction of the abdominal muscles. |
|
Sims Position |
It is used to assess the rectum or vagina. |
|
Lithotomy |
It is used to assess female genitalia and rectum. |
|
Knee-chest |
It is used to assess the anus and rectum. |
Draping:
Draping prevents unnecessary exposure, provides privacy, and keeps the patient warm during the physical assessment.
Drapes may be paper, cloth, or bed linens.
When conducting an assessment, expose only the body parts being assessed to maintain the patient’s modesty and comfort.
Techniques of physical assessment:
The four primary assessment techniques are inspection, palpation, percussion, and auscultation.
Bilateral body parts are always compared.
1. Inspection:
Is the process of performing deliberate, purposeful observations in a systematic manner.
Each area of the body is inspected for size, color, shape, position, and symmetry, noting normal findings and any deviations from normal.
2. Palpation:
The hands and fingers are sensitive tools and can assess skin temperature, turgor, texture, and moisture, as well as vibrations within the body and shape or structures within the body.

3. Percussion:
Percussion is the act of striking one object against another to produce sound. The sound waves produced by the striking action over body tissues are known as percussion tones.
Percussion is used to assess the location, shape, size, and density of tissues.
4. Auscultation:
Auscultation is the act of listening with a stethoscope to sounds produced within the body.
Four characteristics of sound are assessed by auscultation:
- pitch (ranging from high to low)
- loudness (ranging from soft to loud)
- quality (e.g., gurgling or swishing)
- duration (short, medium, or long).
Equipment used during physical examination:
General Survey
The general survey is the first component of the physical assessment.
It includes observing the patient’s overall appearance and behavior, taking vital signs, and measuring height and weight.
1. Appearance and behavior:
- Inspect the patient’s body build, posture, and gait.
- Note signs of illness, such as changes in posture, skin color, and respirations; nonverbal communication of pain or distress; and short attention span.
- Observe hygiene and grooming.
- Clues to mood and mental health are provided by speech, facial expressions, ability to relax, eye contact, and behavior.
2.Vital signs:
Vital signs are measured to establish a baseline for the database and to detect actual or potential health problems.
3. Height and weight:
The ratio of height to weight is an assessment of overall health and overnutrition or undernutrition. Height and weight should be measured using accurate scales and measuring devices.
Assessing The Integument
The integument is comprised of the skin, nails, hair, and scalp.
7.1 Health history:
• History of rashes, lesions, change in color, or itching
• History of bruising or bleeding in the skin
• History of allergies to medications, plants, foods, or other substances
• Exposure to the sun and sunburn history
• Presence of lesions (wounds, bruises, abrasions, or burns)
• Change in the color, size, or shape of a mole
• Recent chemotherapy or radiation therapy
• Exposure to chemicals that may be harmful to the skin, hair, or nails
• Degree of mobility
• Types of food eaten and liquids consumed each day
7.2 Physical assessment:
1. Skin colour: Changes in skin color include erythema, cyanosis, jaundice, and pallor
2. Skin vascularity: The skin is inspected for vascularity, bleeding, or bruising; these signs might relate to a cardiovascular, hematologic, or liver dysfunction.
- Ecchymosis is a collection of blood in the subcutaneous tissues, causing purplish discoloration.
- Petechiae are small hemorrhagic spots caused by capillary bleeding.
3. Lesions are areas of diseased or injured tissue. Lesions are categorized as primary or secondary.
- Primary lesions are those that may arise from previously normal skin
- Secondary lesions result from changes in primary lesions.
4. Skin temperature, texture, moisture, and turgor:
- The skin is normally warm and dry. An increase in skin temperature and moisture can indicate an elevated body temperature.
- An excessive amount of perspiration, such as when the entire skin is moist, is called diaphoresis.
- Turgor is the fullness or elasticity of the skin. It is usually assessed on the sternum or under the clavicle by lifting a fold of skin with the thumb and first finger
- Difficulty in lifting a skin fold may indicate edema (excess fluid in the tissues).
Edema may be graded as 0 (none), +1 (trace, 2 mm), +2 (moderate, 4 mm), +3 (deep, 6 mm), or +4 (very deep, 8 mm).
5. Nails:
The nails are inspected for shape, angle, texture, and color.
6. Hair and scalp:
Hair is found on all body surfaces except the palms of the hands, the soles of the feet, and parts of the genitalia.
Abnormal findings include unusual balding (alopecia) and excessive amounts of hair on the face and body (hirsutism).
Assessing The Head And Neck
Assessment of the head and neck includes the skull, face, eyes, ears, nose and sinuses, mouth and pharynx, trachea, thyroid gland, and lymph nodes.
8.1 Health history:
Changes in vision or hearing with aging
- History of use of corrective lenses or hearing aids
- Loss of an eye (use of artificial eye)
- History of allergies
- History of disturbances in vision or hearing
- History of chronic illnesses such as hypertension, diabetes mellitus, or thyroid disease
- Exposure to harmful substances or loud noises
- Exposure to ultraviolet light
- History of smoking (how long, how many packs/day), chewing tobacco, or cocaine use
- History of eye or ear infections
- History of head trauma
- History of persistent hoarseness
- Oral and dental care practices
8.2 Physical assessment:
Head and face:
- Abnormal findings include lack of symmetry or unusual size or contour of the skull (either may be the result of trauma or diseases affecting the growth of bone) and tenderness.
- Measuring head circumference is a normal part of infant assessment to the age of 2 years and should be conducted at each health-related visit.
- Edema of the face, especially around the eye (periorbital edema), and involuntary facial movements (e.g., tics, fasciculations, tremors) are abnormal findings
Eyes:
Assessment includes the external and internal eye structures, visual acuity, extraocular movements, and peripheral vision.
1. External eye structures:
The eyes, eyebrows, eyelids, eyelashes, lacrimal glands, pupils, and iris are inspected for position and alignment.
Asymmetry of position and alignment of the eyes may be caused by muscle weakness or a congenital abnormality.
Abnormal findings include:
- drooping of the upper lids (ptosis)- damage to the oculomotor nerve, myasthenia gravis, or a congenital disorder
- inward turning of the lower lid and lashes (entropion)
- outward turning of the lower lid and lashes (ectropion)
- redness or drainage (from infection of the lid margins, conjunctivae, or hair follicles)
Inspect and palpate the lacrimal glands for edema and pain.
The pupils are normally black, equal in size, round, and smooth.
- The pupils may be pale and cloudy if the patient has cataracts (loss of opacity of the lens).
- Injury to the eye, glaucoma, and certain medications may cause the pupil to dilate (mydriasis); certain drugs can cause constriction (miosis)
Assess the pupils for reaction to light and accommodation and for convergence.
2. Internal eye structures:
The internal eye is examined with the ophthalmoscope to assess the fundus, including the retina, optic nerve disc, macula, fovea centralis, and retinal vessels.
3. Visual Acuity, Extraocular Movements, and Peripheral Vision:
- Visual acuity is assessed with the Snellen chart.
- The numerator is 20, representing the distance from which a person with normal vision (recorded as 20/20) can read the letters. The denominator represents the smallest line read accurately by the patient.
- Test extraocular movements by assessing the cardinal fields of vision for coordination and alignment.
- Tests for peripheral vision (or visual fields) are used to assess retinal function and optic nerve function.
4. Ears:
Inspect the external ear for shape, size, and lesions.
Abnormal findings include unequal height and size, uneven color, and lesions.
The otoscope is used to examine the ear canal and the tympanic membrane.
- Straighten the ear canal of the adult by gently pulling the pinna up and back.
- In children younger than 3 years of age, straighten the ear canal by pulling the pinna down and back.
5. Hearing and sound conduction:
Tuning fork tests, such as the Weber and Rinne tests, help assess the type of hearing loss:
- conductive (the result of a problem with the transmission of sound waves through the outer and middle ear)
- sensorineural (from inner ear damage)
- a combination of both.
The Weber test is used to assess for bone conduction of sound. With this test, the sound is normally heard in both ears or is localized at the center of the head. Patients with conductive hearing loss hear the sound better in the affected ear. If the sound is heard better in the ear without a problem, it indicates damage to the inner ear or a nerve disorder.
The Rinne test is used to compare bone and air conduction of sound. With this test, hearing of air-conducted sound is normally greater than bone-conducted sound (documented as AC > BC). If the hearing loss is conductive, sound of bone conduction will be the same or greater than air conduction.
6. Nose:
Assessment of the nose involves examining the external nose, the nares, and the turbinates.
Assess the nose for patency by occluding one nostril at a time and asking the patient to inhale and exhale through the nose.
Inspect each nostril using an otoscope with a short, wide tip or using a nasal speculum and penlight.
Abnormal findings are:
- swelling of the mucosa
- bleeding or discharge (indicating allergies with inflammation or infection)
- perforation or deviation of the nasal septum (cocaine use may cause perforation
- a deviated septum may be congenital or from trauma)
- polyps (often seen with chronic allergies).
7. Thyroid gland:
Assess the thyroid gland using palpation, keeping in mind that the gland is not palpable in all patients.
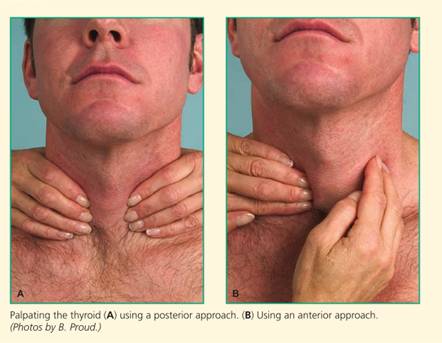
Posterior Approach
• Standing behind the patient, place your hands around the patient's neck, with the fingertips over the lower half of the neck and trachea.
• Ask the patient to swallow, and feel for enlargement of the gland as it rises.
• Palpate each lobe of the thyroid by having the patient turn the head slightly toward the side to be examined; then gently displace the trachea with one hand.
• Ask the patient to swallow, and palpate the thyroid with the other hand.
• Repeat for the other side.
Anterior Approach
• Standing facing the patient, place the fingers of your left hand around the sternomastoid muscle.
• Ask the patient to swallow, and palpate (using the right hand) for enlargement.
• Repeat for the other side.
Assessing The Thorax And Lungs
The thorax comprises the lungs, rib cage, cartilage, and intercostal muscles.
10.1 Health History
Identify risk factors for altered health during the health history by asking about the following:
• History of trauma to the ribs or lung surgery
• Number of pillows used when sleeping
• History of chest pain with deep breathing
• History of persistent cough with or without producing sputum
• History of allergies
• Environmental exposure to chemicals, asbestos, or smoke
• History of smoking (how long, how many packs/day)
• History of lung disease in family members or self
• History of frequent or chronic respiratory infections
10.2 Physical assessment:
1. Inspection:
Observe the patient’s chest for color, shape or contour, breathing patterns, and muscle development.
The chest should be symmetric, with the transverse diameter greater than the anteroposterior diameter.
An increased anteroposterior diameter, as seen in chronic lung diseases, is described as barrel-chest.
Respirations should be smooth and even, ranging from 12 to 20 breaths/min.
2. Palpation:
Palpation is used to detect areas of sensitivity, chest expansion during respirations, and vibrations (fremitus).
Abnormal findings may be cool or excessively dry or moist skin, muscle asymmetry, tenderness, masses, and vibrations.
Chest expansion is determined by placing the hands over the posterior chest wall, with the fingers at the level of T9 or T10. Ask the patient to take a deep breath, and observe the movement of your thumbs
3. Auscultation
Auscultation is used to detect airflow within the respiratory tract.
- Bronchial sounds heard over the trachea are high-pitched, harsh sounds, with expiration being longer than inspiration.
- Bronchovesicular sounds are heard over the mainstem bronchus and are moderate “blowing” sounds, with inspiration equal to expiration.
- Vesicular breath sounds are soft, low-pitched sounds, heard best over the base of the lungs during inspiration, which is longer than expiration.
- Adventitious breath sounds are not normally heard in the lungs.
Nursing insights: Normal Age-Related Variations
INFANT/CHILD
Common thorax and lung variations in newborns and children include:
• Louder breath sounds on auscultation • More rapid respiratory rate (until 8 to 10 years of age) • Use of abdominal muscles during respiration
OLDER ADULT
Common thorax and lung variations in older adults include:
• Increased anteroposterior chest diameter • Increase in the dorsal spinal curve (kyphosis) • Decreased thoracic expansion • Use of accessory muscles to exhale
Assessing The Cardiovascular And Peripheral Vascular Systems
Cardiovascular and peripheral vascular assessment includes assessment of the heart and the extremities
11.1 Health history:
-
History of chest pain, palpitations, or dizziness
- Swelling in the ankles and feet
- Number of pillows used to sleep
- Type and amount of medications taken daily
- History of heart defect, rheumatic fever, or chest or heart surgery
- Personal and family history of hypertension (high blood pressure), myocardial infarction (heart attack), coronary artery disease, high blood cholesterol levels, or diabetes mellitus
- History of smoking (how long, how many packs/day)
- History of alcohol use
- Type and amount of exercise
- Usual foods eaten each day
11.2 Physical assessment:
1. Inspection:
Observe the neck and precordium for visible pulsations.
Inspect the epigastric area at the tip of the sternum for pulsation of the abdominal aorta.
Findings of neck vein distention (indicating heart disease) or visible pulsations in precordial areas other than the apical impulse (which may result from abnormalities of the ventricle) are considered abnormal.
2. Palpation:
Using the palmar surface of the hand with the four fingers held together, palpate the precordium gently for pulsations.
Palpate the apical impulse in the mitral area.
Normal findings include no pulsation palpable over the aortic and pulmonic areas, with a palpable apical impulse.
Abnormal findings include
- precordial thrills, which are fine, palpable, rushing vibrations over the right or left second intercostal space,
- lifts or heaves
3. Auscultations
Auscultation is used to determine the heart sounds caused by closure of the heart valves.
Use systematic auscultation, beginning at the aortic area, moving to the pulmonic area, then to Erb’s point, then to the tricuspid area, and finally to the mitral area.
Use the diaphragm of the stethoscope first to listen to high-pitched sounds. Then use the bell to listen to low pitched sounds.
Nursing insights: Normal Age-Related Variations
INFANT/CHILD
Common cardiovascular and peripheral vascular variations in newborns and children include:
- Visible cardiac pulsation if the chest wall is thin
- Sinus dysrhythmia (the rate increases with inspiration and decreases with expiration)
- Presence of S3 (in about one third of all children)
- More rapid heart rate (until about 8 years of age)
OLDER ADULT
Common cardiovascular and peripheral vascular variations in older adults include:
- Difficult-to-palpate apical pulse
- Difficult-to-palpate distal arteries
- Dilated proximal arteries
- More prominent and tortuous blood vessels; varicosities common
- Increased systolic and diastolic blood pressure
- Widening pulse pressure
Assessing The Breasts And Axillae
Physical assessment of the breasts and axilla are primarily conducted to identify any lumps in the breasts and/or enlargement or pain in axillary lymph nodes.
12.1 Health History
Identify risk factors for altered health during the health history by asking about the following:
- History of pain in one or both breasts, including relationship to menstrual period
- History of lumps or swelling, redness, change in size, or dimpling in the breasts
- History of discharge from the breast
- Family history of ovarian or breast cancer
- History of breast disease, biopsy, or surgery
- Menstrual and pregnancy history
- Use of hormones, oral contraceptives
- Exposure to radiation, benzene, or asbestos
- Usual dietary intake and alcohol consumption
- Knowledge and practice of breast self-examination
- Most recent clinical breast examination and mammogram
12.2 Physical assessment:
1. Inspection:
- Inspect the breasts for size, shape, symmetry, color, texture, and skin lesions.
- The shape of the breasts is round and smooth, and there should be no skin depressions (retraction) or puckering (dimpling).
- Inspect the areola and nipples for size and shape and the nipples for discharge, crusting, and inversion.
- Montgomery’s tubercles (sebaceous glands on the areolae of the breasts) are a normal component of the areola.
- The nipples are normally everted.
2. Palpation:
- Palpate the breasts in each of the four quadrants (the upper outer quadrant, the lower outer quadrant, the upper inner quadrant, and the lower inner quadrant) to detect any abnormal lumps.
- Palpate the nipple and areola and gently compress the nipple between the thumb and forefinger to assess for discharge.
- Palpate the axillary areas for lymph nodes.
Nursing insights: Normal Age-Related Variations
INFANT/CHILD
Common breast and axillae variations in newborns and children include:
- Breast enlargement and a white discharge from the nipples (up to 2 weeks of age)
- Female breast growth beginning at 10 or 11 years of age
- Temporary enlargement of one or both breasts (gynecomastia) in pubescent boys
OLDER ADULT
Common breast and axillae variations in older adults include:
• Granular, pendulous breasts in women
Assessing The Abdomen
14.1 Health history:
Identify risk factors for altered health during the health history by asking about the following:
- History of abdominal pain
- History of indigestion, nausea or vomiting, constipation or diarrhea
- History of food allergies or lactose intolerance
- Appetite and usual food and fluid intake
- Usual bowel and bladder elimination patterns
- History of gastrointestinal disorders, such as peptic ulcer disease, bowel disease, gallbladder disease, liver disease, or appendicitis
- History of urinary tract disorders such as infections, kidney stones, or kidney disease
- History of abdominal surgery or trauma
- Type and amount of prescribed and over-the-counter medications used
- Amount and type of alcohol ingestion
- For women, menstrual history
14.2 Physical assessment:
1. Inspection:
Inspect skin color and surface characteristics, including the umbilicus, contour, symmetry, peristalsis, pulsations, and visible masses.
Abnormal findings include swelling of the abdomen (indicating fluid retention called ascites) and abdominal masses or unusual pulsations.
2. Auscultation:
Auscultation is used to assess bowel sounds and vascular sounds.
Listen carefully for bowel sounds (gurgles and clicks, and note their frequency and character [usually occur every 5 to 34 seconds]). Before documenting bowel sounds as absent, the nurse must listen for 2 minutes or longer in each abdominal quadrant.
Abnormal findings include:
- increased bowel sounds (often heard with diarrhea or in early bowel obstruction)
- decreased bowel sounds (heard after abdominal surgery or late bowel obstruction)
- absent bowel sounds (indicating peritonitis or paralytic ileus)
- Bowel sounds of high-pitched tinkling or rushes of high-pitched sounds indicate a bowel obstruction.
Using the bell of the stethoscope, auscultate over the abdominal aorta, femoral arteries, and iliac arteries for bruits (abnormal sounds heard over a blood vessel as blood passes an obstruction).
3. Percussion:
- Percussion is useful in assessing a full bladder or changes in abdominal contents.
- Percuss the abdomen in all four quadrants in a systematic, clockwise manner to identify fluid, masses, or air.
- Normally, tympany, the dominant percussion tone, is heard over the abdomen while dullness is heard over the liver and a full bladder.
- Abnormal findings include decreased tympany and increased dullness, possibly caused by fluid or a mass.
4. Palpation:
Palpate each quadrant in a systematic manner, noting muscular resistance, tenderness, enlargement of the organs, or masses.
Abnormal findings include involuntary rigidity, spasm, and pain (which may indicate trauma, peritonitis, infection, tumors, or enlarged or diseased abdominal organs).
Nursing insights: Normal Age-Related Variations
INFANT/CHILD
Common abdominal variations in newborns and children include:
- Umbilical cord in newborns; dries and falls off within the first few weeks of life
- A “pot-belly” (under 5 years of age)
- Visible peristaltic waves
- Easily palpated liver and spleen
OLDER ADULT
Common abdominal variations in older adults include:
- Decreased bowel sounds
- Decreased abdominal tone
- Liver border palpated more easily
Assessing The Muscular System
MUSCLES:
Inspect the muscles for size.
Compare the muscles on one side of the body (e.g., of the arm, thigh, and calf) to the same muscle on the other side. For any discrepancies, measure the muscles with a tape.
Inspect the muscles and tendons for contractures (shortening).
Inspect the muscles for tremors, for example by having the client hold the arms out in front of the body.
Test muscle strength. Compare the right side with the left side. Sternocleidomastoid: Client turns the head to one side against the resistance of your hand. Repeat with the other side.
- Trapezius: Client shrugs the shoulders against the resistance of your hands.
- Deltoid: Client holds arm up and resists while you try to push it down.
- Biceps: Client fully extends each arm and tries to flex it while you attempt to hold arm in extension.
- Triceps: Client flexes each arm and then tries to extend it against your attempt to keep arm in flexion.
- Wrist and finger muscles: Client spreads the fingers and resists as you attempt to push the fingers together.
- Grip strength: Client grasps your index and middle fingers while you try to pull the fingers out.
- Hip muscles: Client is supine, both legs extended; client raises one leg at a time while you attempt to hold it down.
- Hip abduction: Client is supine, both legs extended. Place your hands on the lateral surface of each knee; client spreads the legs apart against your resistance.
- Hip adduction: Client is in same position as for hip abduction. Place your hands between the knees; client brings the legs together against your resistance.
- Hamstrings: Client is supine, both knees bent. Client resists while you attempt to straighten the legs.
- Quadriceps: Client is supine, knee partially extended; client resists while you attempt to flex the knee.
- Muscles of the ankles and feet: Client resists while you attempt to dorsiflex the foot and again resists while you attempt to flex the foot.
BONES:
- Inspect the skeleton for structure.
- Palpate the bones to locate any areas of edema or tenderness.
JOINTS
- Inspect the joint for swelling.
- Palpate each joint for tenderness, smoothness of movement, swelling, crepitation, and presence of nodules.
- Assess joint range of motion.
- For the types of joint movements- Ask the client to move selected body parts. The amount of joint movement can be measured by a goniometer, a device that measures the angle of a joint in degrees.
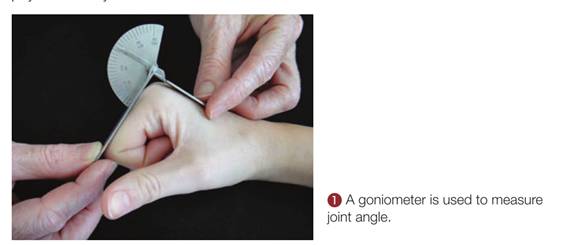
Assessment Of Female Genitals And Inguinal Area
|
Assessment |
Normal Findings |
Deviations from Normal |
|
Inspect the distribution, amount, and characteristics of pubic hair. |
There are wide variations; generally kinky in the menstruating adult, thinner and straighter after menopause Distributed in the shape of an inverse triangle |
Scant pubic hair (may indicate hormonal problem). Hair growth should not extend over the abdomen |
|
Inspect the skin of the pubic area for parasites, inflammation, swelling, and lesions. |
Pubic skin intact, no lesions Skin of vulva area slightly darker than the rest of the body Labia round, full, and relatively symmetric in adult females |
Lice, lesions, scars, fissures, swelling, erythema, excoriations, varicosities, or leukoplakia |
|
Inspect the clitoris, urethral orifice, and vaginal orifice when separating the labia minora. |
Clitoris does not exceed 1 cm (0.4 in.) in width and 2 cm (0.8 in.) in length Urethral orifice appears as a small slit and is the same color as surrounding tissues No inflammation, swelling, or discharge |
Presence of lesions. Presence of inflammation, swelling, or discharge |
|
Palpate the inguinal lymph nodes. Use the pads of the fingers in a rotary motion, noting any enlargement or tenderness |
No enlargement or tenderness |
Enlargement and tenderness |
Assessment Of Male Genitals And Inguinal Area
|
Assessment |
Normal Findings |
Deviations from Normal |
|
PUBIC HAIR: Inspect the distribution, amount, and characteristics of pubic hair. |
Triangular distribution, often spreading up the abdomen |
Scant amount or absence of hair |
|
PENIS Inspect the penile shaft and glans penis for lesions, nodules, swellings, and inflammation. Inspect the urethral meatus for swelling, inflammation, and discharge. |
Penile skin intact Appears slightly wrinkled and varies in color as widely as other body skin Foreskin easily retractable from the glans penis Small amount of thick white smegma between the glans and foreskin Pink and slitlike appearance Positioned at the tip of the penis |
Presence of lesions, nodules, swellings, or inflammation Foreskin not retractable Large amount, discolored, or malodorous substance
Inflammation; discharge Variation in meatal locations (e.g., hypospadias, on the underside of the penile shaft, and epispadias, on the upper side of the penile shaft) |
|
SCROTUM Inspect the scrotum for appearance, general size, and symmetry. Inspect all skin surfaces by spreading the rugated surface skin and lifting the scrotum as needed to observe posterior surfaces. |
Scrotal skin is darker in color than that of the rest of the body and is loose Size varies with temperature changes (the dartos muscles contract when the area is cold and relax when the area is warm) Scrotum appears asymmetric (left testis is usually lower than right testis) |
Discolorations; any tightening of skin (may indicate edema or mass) Marked asymmetry in size |
|
INGUINAL AREA Inspect both inguinal areas for bulges while the client is standing, if possible. First, have the client remain at rest. Next, have the client hold his breath and strain or bear down as though having a bowel movement. Bearing down may make the hernia more visible. |
No swelling or bulges |
Swelling or bulge (possible inguinal or femoral hernia) |
Assessing The Neurologic System
Neurologic assessment includes cerebral function, cranial nerve function, cerebellar function, motor and sensory function, and reflexes.
18.1 Health History
Identify risk factors for altered health during the health history by asking about the following:
- History of numbness, tingling, or tremors
- History of seizures
- History of headaches
- History of dizziness
- History of trauma to the head or spine
- History of infections of the brain
- History of stroke
- Changes in the ability to hear, see, taste, or smell
- Loss of ability to control bladder and bowel
- History of high blood pressure
- History of smoking (how long, how many packs/day)
- History of chronic alcohol use
- History of diabetes mellitus or heart disease
- Use of prescription and over-the-counter medications
- Family history of high blood pressure, Alzheimer’s disease, epilepsy, cancer, or Huntington’s chorea
- Frequency of blood cholesterol tests and results
- Exposure to environmental hazards (e.g., lead, insecticides)
18.2 Physical assessment:
1. Mental status:
Mental status assessment includes level of awareness,level of consciousness, behavior and appearance, memory, abstract reasoning, and language.
Level of consciousness is described as follows:
- Awake and alert: fully awake; oriented to person, place, and time; responds to all stimuli, including verbal commands
- Lethargic: appears drowsy or asleep most of the time but makes spontaneous movements; can be aroused by gentle shaking and saying patient’s name
- Stuporous: unconscious most of the time; has no spontaneous movement; must be shaken or shouted at to arouse; can make verbal responses, but these are less likely to be appropriate; responds to painful stimuli with purposeful movements
- Comatose: cannot be aroused, even with use of painful stimuli; may have some reflex activity (such as gag reflex); if no reflexes present, is in a deep coma
Assess awareness by evaluating orientation to time, place, and person.
The following questions may be used:
- Time: What is today’s date? What day of the week is it? What season of the year is this? What was the last holiday?
- Place: Where are you now? What is the name of this city? What state are we in?
- Person: What is your name? How old are you? Who came to visit you this morning?
Memory is assessed by asking questions that require answers demonstrating immediate recall and recall for past events.
Assessing Abstract Reasoning: Ask the patient to explain a proverb such as “the early bird catches the worm.” Be sure that the phrase is not culture specific.
2. Language
Injury to the cortex can cause aphasia, which is a disorder of language ability.
Aphasia may be expressive (the individual understands written and spoken words but cannot write or speak to communicate effectively) or receptive (the individual cannot understand written or spoken words). These aphasias may also be combined.
3. Cranial nerve function:
The function of the 12 cranial nerves is assessed primarily during the neurologic assessment, although parts of cranial nerve function are assessed with other body systems.
4. Motor and sensory function:
Motor ability is evaluated by assessing balance, gait, and coordination.
Sensory function is assessed by testing sensory discrimination of pain, light touch, and vibrations.
Nursing insights: Normal Age-Related Variations
INFANT/CHILD
Common neurologic variations for newborns and children include:
- Positive Babinski’s reflex (normal in children between 12 and 24 months)
- Grasp reflex (present at birth)
- Motor control develops in head, neck, trunk, and extremities sequence
OLDER ADULT
Common neurologic variations for older adults include:
- Slower thought processes and verbal responses
- Decreased sensory ability (hearing, sight, smell, taste, temperature, pain)
- Slower coordination and voluntary movements
- Decreased reflex responses
- Appearance of confusion in unfamiliar surroundings
- Slower gait, with a wider base and flexed hips and knees
- Diminished deep tendon reflexes
Summary
- The health examination is conducted to assess the function and integrity of the client’s body parts. Initial findings provide baseline data against which subsequent assessment findings are compared.
- The health examination may entail a complete head-to-toe assessment or individual assessment of a body system or body part.
- The health assessment is conducted in a systematic manner that requires the fewest position changes for the client.
- Aspects of the physical assessment procedures should be incorporated in the assessment, intervention, and evaluation phases of the nursing process.
- Skills in inspection, palpation, percussion, and auscultation are required for the physical health examination; these skills are used in that order throughout the examination except during abdominal assessment, when auscultation follows inspection and precedes percussion and palpation.
- Knowledge of the normal structure and function of body parts and systems is an essential requisite to conducting physical assessment.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Health and Physical Assessment of the Adult Client
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


