Please set your exam date
Mobility
Study Questions
Practice Exercise 1
A patient performs rehabilitative exercises with resistance after a knee injury. The nurse interprets this type of exercise as which of the following?
Explanation
Different types of muscle contractions and exercise modalities are used in rehabilitation. Isotonic exercises change muscle length while moving a joint against a fixed load; isometric exercises create tension without movement; isokinetic exercises use machines that control movement speed and adjust resistance so muscle works maximally through the whole range - making them particularly useful for targeted rehab.
Rationale for correct answer:
2. Isokinetic exercise uses specialized equipment that provides resistance so that the muscle contracts at a constant speed throughout the range of motion. Isokinetic training is commonly used in rehabilitation (especially for knee injuries) because it allows controlled, measurable strengthening while protecting the joint.
Rationale for incorrect answers:
1. Isotonic exercises produce movement of a joint while the muscle changes length (concentric/eccentric contractions) against a constant load (e.g., lifting free weights, doing squats). They build strength and endurance but the resistance is typically a fixed weight.
3. Isometric exercise involves muscle contraction without joint movement (no change in muscle length) - for example, pushing the palms together or holding a static quad set. It increases muscle tension and can maintain strength but does not produce the joint motion typical of many rehab programs.
4. Aerobic exercise is rhythmic, uses large muscle groups, and increases oxygen consumption and cardiovascular endurance (e.g., walking, cycling). It is not primarily focused on resisted, controlled strengthening of a single joint with a rehab device.
Take home points
- Isokinetic - rehab machines that keep contraction speed constant and automatically adjust resistance
- Excellent for controlled strengthening after joint injury.
- Isotonic- joint movement against set weights
- Isometric- tension without movement; aerobic -cardiovascular-focused.
Which of the following would the nurse expect to assess when a patient experiences a greater breakdown of protein than that which is manufactured?
Explanation
Protein contains nitrogen; the body’s nitrogen balance reflects whether it is building (positive balance) or breaking down (negative balance) lean tissue. Situations with increased catabolism (severe illness, injury, starvation) or insufficient dietary protein produce negative nitrogen balance - a clinical sign that the patient is losing lean body mass and needs nutritional and medical intervention.
Rationale for correct answer:
4. Negative nitrogen balance: Nitrogen balance compares nitrogen (protein) intake with nitrogen loss. When protein catabolism exceeds synthesis, more nitrogen is excreted than ingested, producing a negative nitrogen balance.
Rationale for incorrect answers:
1. Fluid volume excess describes too much body water (edema, weight gain, bounding pulses) and is not a direct marker of protein catabolism versus synthesis.
2. A contracture is a permanent shortening of muscle or connective tissue around a joint from immobilization or fibrosis; it’s not the direct result of whole-body negative protein balance.
3. Osteoporosis is loss of bone mass and microarchitectural deterioration; while nutrition and protein affect bone health, the immediate physiologic shorthand for more protein breakdown than synthesis is not osteoporosis.
Take home points
- Negative nitrogen balance- more protein breakdown than synthesis.
- It signals catabolism and need for nutritional/clinical intervention.
- Monitor high-risk patients (trauma, burns, sepsis, prolonged immobility) for negative nitrogen balance.
When explaining the cause of frequent urinary tract infections related to immobility, the nurse understands that immobility may result in which of the following?
Explanation
Lack of movement can lead to incomplete bladder emptying and decreased frequency of voiding - called urinary stasis - which allows bacteria to multiply and increases the risk of UTIs. Immobility also contributes to other urinary problems (e.g., increased urinary calcium from bone breakdown).
Rationale for correct answer:
2. Urinary stasis: When a patient is immobile, they may not void frequently or completely (because of decreased mobility to toileting, decreased abdominal and pelvic muscle tone, or dependency), causing urine to remain in the bladder. Urinary stasis provides a medium for bacterial growth and is a major risk factor for urinary tract infections (UTIs).
Rationale for incorrect answers:
1. Improved renal blood supply to the kidneys: Immobility does not improve renal blood flow. If anything, prolonged bed rest can reduce overall circulation and predispose to complications; improved renal perfusion is not a consequence of immobility.
3. Decreased urinary calcium: Immobility typically increases bone resorption, releasing calcium into the bloodstream and urine (hypercalciuria). So urinary calcium usually rises, not decreases.
4. Acidic urine formation: Urinary pH can vary with diet, medications, and infection; immobility itself does not reliably cause acidic urine. It’s urinary stasis and bacterial overgrowth that more directly increase UTI risk.
Take home points
- Urinary stasis from immobility is the main reason immobile patients have higher UTI risk.
- Encourage frequent voiding, timed toileting, appropriate hydration, and use of mechanical aids (bedpans/commodes) or catheter protocols to reduce UTI risk in immobile patients.
Isotonic exercises such as walking are intended to achieve which of the following? Select all that apply.
Explanation
Isotonic activities involve concentric and eccentric muscle contractions with joint movement (walking, cycling, swimming). They improve muscle tone, endurance, circulation, and joint mobility; with appropriate intensity they also increase muscle strength and mass. Acute cardiovascular responses include increased heart rate and cardiac output, while chronic adaptations improve resting cardiovascular efficiency.
Rationale for correct answer:
1. Increase muscle tone and improve circulation: Isotonic exercises (muscle contraction with joint movement, e.g., walking) promote muscle conditioning and enhance venous return and overall circulation.
3. Increase muscle mass and strength: Repeated isotonic contractions against resistance or body weight can increase muscle strength and, depending on intensity, muscle mass. Walking primarily improves endurance and tone, but isotonic activities overall can enhance muscle strength.
5. Maintain joint range of motion: Because isotonic exercises involve movement through joint ranges, they help maintain or improve joint mobility and prevent stiffness.
Rationale for incorrect answers:
2. Increase blood pressure: Blood pressure rises during exercise acutely, but the intended therapeutic effect of regular isotonic exercise is to improve cardiovascular fitness and typically lower resting blood pressure over time. Increasing BP is not a desired long-term goal.
5. Decrease heart rate and cardiac output: During isotonic exercise heart rate and cardiac output increase to meet metabolic demands. Regular training can decrease resting heart rate and improve stroke volume (so exercise improves efficiency), but the immediate effect is an increase.
Take home points
- Isotonic exercises (like walking) improve muscle tone, circulation, endurance, and help maintain joint range of motion.
- Expect increased heart rate and cardiac output during activity, but regular isotonic exercise improves resting cardiovascular fitness and can lower resting blood pressure and heart rate over time.
A patient has been on bed rest for over 5 days. Which of these findings during the nurse’s assessment may indicate a complication of immobility?
Explanation
Prolonged bed rest can affect multiple systems—musculoskeletal, cardiovascular, respiratory, urinary, and gastrointestinal. Nurses must recognize early signs such as decreased peristalsis to prevent further complications through interventions like mobilization, hydration, and dietary management.
Rationale for correct answer:
1. Decreased peristalsis: Prolonged immobility slows gastrointestinal motility, leading to decreased peristalsis. This may cause constipation, fecal impaction, and discomfort—common complications of inactivity and reduced muscle tone in the abdomen. Encouraging fluids, fiber intake, and ambulation helps prevent this.
Rationale for incorrect answers:
2. Decreased heart rate: Although resting heart rate may slightly decrease with bed rest, it is not a typical complication of immobility. The more significant cardiovascular effects include orthostatic hypotension and venous stasis, not bradycardia.
3. Increased blood pressure: Immobility is more commonly associated with orthostatic hypotension due to blood pooling in the lower extremities and decreased cardiac workload, not hypertension.
4. Increased urinary output: Inactivity tends to decrease urinary output and promote urinary stasis, which increases the risk for urinary tract infection (UTI) and renal calculi. Increased output would not indicate a complication of immobility.
Take-home points
- Decreased peristalsis is a hallmark complication of prolonged immobility, often leading to constipation and discomfort.
- Regular mobility and repositioning are essential to maintain body system function and prevent complications during extended bed rest.
Practice Exercise 2
Mr. Brown is experiencing some difficulty breathing. The nurse most appropriately assists him into which position?
Explanation
Upright positions (Fowler’s) facilitate lung expansion by allowing the diaphragm to move more freely and reducing abdominal pressure on the chest, which improves oxygenation and comfort in dyspneic patients.
Rationale for correct answer:
3. Fowler’s position: Fowler’s (sitting upright at 45–90°) promotes maximal chest expansion and diaphragmatic descent, reduces abdominal pressure on the thorax, and improves ventilation and oxygenation. It’s the most appropriate immediate position for a patient experiencing difficulty breathing.
Rationale for incorrect answers:
1. Dorsal recumbent position: Dorsal recumbent (supine with knees bent) lies the patient flat on their back. This position reduces diaphragmatic excursion and is not optimal for someone who is short of breath.
2. Lateral position: Side-lying (lateral) may be useful for airway protection, certain respiratory conditions, or to improve ventilation of a dependent lung in unilateral disease, but it is not the standard first choice for general dyspnea.
4. Sims’ position: Sims’ (semi-prone, used commonly for rectal procedures or enema administration) is not used to relieve dyspnea and may compromise respiratory mechanics.
Take home points
- Place dyspneic patients in Fowler’s position to improve ventilation and ease breathing.
- Positioning is a simple, immediate nursing intervention that can significantly improve respiratory status while further assessment and treatments proceed.
A bedridden patient who is blind is admitted to a healthcare facility from his or her home with pressure ulcers on the sacral area. Which nursing diagnosis would be a priority?
Explanation
Nursing priorities focus first on actual, immediate threats to health and safety - here, an existing skin breakdown that can rapidly worsen or become infected. Effective care simultaneously treats the acute problem and addresses underlying contributors (immobility, nutrition, incontinence, sensory deficits) to prevent recurrence.
Rationale for correct answer:
2. Impaired Skin Integrity related to immobility: The patient already has actual pressure ulcers on the sacrum. Impaired skin integrity directly addresses the existing wound problem and its cause (immobility). Actual problems that threaten tissue viability, infection risk, pain, and further deterioration take priority over potential/risk problems.
Rationale for incorrect answers:
1. Risk for Imbalanced Body Temperature related to stage 2 pressure ulcer: A risk diagnosis describes a potential future problem. Although severe infections or large wounds can affect temperature regulation, a stage 2 sacral pressure ulcer in a single area is unlikely to cause an immediate body-temperature imbalance.
3. Feeding Self-Care Deficit related to blindness: Blindness may impair independent feeding, but it is not inherently as immediately threatening as an existing pressure ulcer that risks infection and further tissue loss. This is an important problem to assess and plan for assistive strategies, but not the highest priority given the current wounds.
4. Activity Intolerance related to prolonged bed rest: Activity intolerance is likely present and contributes to immobility, but it is more of a contributing/related condition. The immediate problem requiring nursing action on admission is the impaired skin integrity.
Take home points
- Actual problems that threaten tissue viability or life take priority over potential/risk diagnoses.
- Treat the wound promptly and address contributing factors (immobility, moisture, nutrition, sensory impairment) to prevent progression and complications.
Five minutes after the client’s first postoperative exercise, the client’s vital signs have not yet returned to baseline. Which is an appropriate nursing diagnosis?
Explanation
When a client shows measurable signs (e.g., abnormal vital signs, symptoms) after activity, choose an actual nursing diagnosis that reflects current physiologic intolerance. Reserve “risk for…” diagnoses for situations where hazards exist but no current manifestations are present.
Rationale for correct answer:
1. Activity Intolerance: This diagnosis is used when a client demonstrates actual inadequate physiological or psychological energy to endure or complete required or desired daily activities. The objective finding (vital signs not returning to baseline 5 minutes after activity) is evidence that the client is not tolerating the activity at this time.
Rationale for incorrect answers:
2. Risk for Activity Intolerance: “Risk for…” is used when no current evidence exists but risk factors are present. In this scenario there is current, measurable evidence (vital signs not back to baseline), so an actual diagnosis is appropriate rather than a risk diagnosis.
3. Impaired Physical Mobility: This focuses on limitation in independent physical movement (ambulation, range of motion). While the client may have limited tolerance, the key problem reported here is the inability to physiologically tolerate activity, not necessarily a limitation of movement itself.
4. Risk for Disuse Syndrome: This is a risk diagnosis referring to consequences of inactivity (muscle atrophy, bone demineralization, etc.). The client’s immediate problem is demonstrated intolerance to activity, not the future risk of disuse complications.
Take home points
- Use an actual nursing diagnosis (e.g., Activity Intolerance) when there is current, observable evidence of a problem.
- Choose a risk diagnosis only when risk factors exist but no current signs or symptoms are present.
When assessing a client’s gait, which does the nurse look for and encourage?
Explanation
Components of a normal gait pattern include: head posture and gaze, heel-to-toe foot contact, reciprocal arm swing, and trunk/pelvic rotation. Nurses observe gait to identify impairments - balance, coordination, strength, neurologic problems- and to teach or encourage safer, more efficient walking mechanics that reduce fall risk and conserve energy.
Rationale for correct answer:
1. The spine rotates, initiating locomotion: Normal gait includes coordinated rotation of the pelvis and trunk (spine) that contributes to stride length and balance. Trunk/pelvic rotation is part of normal locomotion and helps conserve energy and promote smooth, efficient movement - something the nurse observes and may encourage if limited.
Rationale for incorrect answers:
2. Gaze is slightly downward: A normal, safe gait is associated with the head up and gaze forward (looking ahead to navigate). A persistently downward gaze can impair balance and increase fall risk.
3. Toes strike the ground before the heel: Normal walking has a heel-strike (heel contacts first) followed by foot flat and toe-off. Toe-first contact is abnormal and suggests gait deviation.
4. Arm on the same side as the swing-through foot moves forward at the same time: Normal gait shows reciprocal arm swing: the arm opposite the swing leg moves forward (e.g., right leg forward - left arm forward). Same-side forward movement is abnormal and indicates poor coordination.
Take home points
- Normal gait - head up/gaze forward, heel-strike then toe-off, reciprocal arm swing (opposite arm to leg), and pelvic/trunk rotation for efficiency.
- Deviations from these patterns may signal mobility problems that need assessment or intervention.
The nurse is performing an assessment of an immobilized client. Which assessment causes the nurse to take action?
Explanation
Immobilized clients are at high risk for pressure injuries, pulmonary complications- atelectasis, deep-vein thrombosis, and urinary issues. Early skin changes are actionable findings requiring immediate preventive measures to avoid progression to ulceration.
Rationale for correct answer:
2. Reddened area on sacrum: New persistent redness over a pressure point (sacrum) suggests early pressure injury (stage I) from prolonged pressure. This requires immediate nursing action: relieve pressure- reposition, inspect skin closely, implement pressure-relief measures (turning schedule, specialty mattress), and document/monitor.
Rationale for incorrect answers:
1. Heart rate 86 beats/min: A heart rate of 86 bpm is within normal adult range and does not alone indicate an urgent problem in an immobilized client.
3. Nonproductive cough: A nonproductive cough may be an early sign of atelectasis or developing pulmonary issue in an immobilized client and should be monitored and managed (incentive spirometry, deep-breathing exercises), but a reddened sacrum is more urgent for preventing tissue breakdown.
4. Urine output of 50 mL/h: Output of 50 mL/hour is above the commonly used minimum adequate threshold (≥30 mL/hour) and is acceptable. It does not by itself require immediate corrective action.
Take home points
- Early pressure-area redness is an urgent finding in an immobile client - reposition and institute pressure-relief measures immediately.
- Monitor respiratory and urinary status in immobilized patients, but prioritize skin breakdown prevention because pressure injuries can develop quickly and are largely preventable.
Practice Exercise 3
Why are mechanical aids necessary for patient handling and movement?
Explanation
Mechanical aids-such as hoists, slide sheets, and transfer boards-play a critical role in preventing workplace injuries among healthcare workers, especially back injuries, which are common with manual lifting. While proper body mechanics, teamwork, and physical fitness can contribute to safer handling, they are not sufficient by themselves. The introduction of mechanical aids aligns with occupational safety standards and promotes both staff well-being and patient comfort, ensuring safe and efficient transfers.
Rationale for correct answer:
2. Manual lifting techniques are not sufficient to protect nurses from injury: Research shows that manual lifting places excessive stress on the musculoskeletal system, particularly the back and shoulders. Even when using correct posture and teamwork, the physical demands can exceed safe limits.
Rationale for incorrect answers:
1. Nurses do not have sufficient training using proper body mechanics to be safe: Nurses are taught proper body mechanics (e.g., wide base of support, bending knees, keeping load close). However, even with correct technique, manual lifting alone is not enough to prevent musculoskeletal injury, especially with heavier or immobile patients.
3. They reduce the time and number of staff needed to move the patient: Mechanical aids can indeed improve efficiency by reducing the number of staff required to transfer or reposition a patient. However, the primary rationale is staff safety and injury prevention.
4. Nurses are not as physically fit as they should be: Physical fitness does not guarantee protection from injury during lifting. Even a strong, fit nurse can suffer back injury when manually handling patients, since human lifting capacity is lower than many patient weights. Mechanical aids are necessary regardless of nurse fitness.
Take home points
- Manual lifting alone is unsafe-mechanical aids are essential to prevent musculoskeletal injuries in nurses.
- Mechanical aids not only protect staff but also improve efficiency and patient safety during handling and transfers.
While doing range-of-motion exercises with a patient who is bedridden, the nurse is aware of which of the following considerations?
Explanation
Safe principles of range-of-motion therapy: preserve joint mobility and prevent contractures by performing controlled movements within a patient’s comfortable range. ROM can be active (patient moves), active-assistive, or passive (nurse moves joint). Important principles are to support the joint, move smoothly, avoid forcing or jerking, stop at resistance (not pain), monitor for signs of intolerance (swelling, increased pain, increased respirations, pallor), and document what was done.
Rationale for correct answer:
4. Each joint is exercised to the point of resistance but not pain: Standard ROM technique is to move each joint until you feel firm resistance (end of available range) but never force beyond that point or into pain. This prevents overstretching, tissue damage, and discouragement from painful practice.
Rationale for incorrect answers:
1. Neck hyperextension should be encouraged, particularly in older people: Neck hyperextension can be harmful (risking cervical strain, vertebral artery compromise, or discomfort) and is not routinely encouraged-especially in older adults with cervical spondylosis. Neutral alignment and gentle, controlled movement are preferred.
2. Exercises should be continued until the patient is fatigued: Exercises that cause fatigue increase risk of injury and discourage participation. ROM is intended to maintain mobility, prevent contractures, and preserve joint health; stop before marked fatigue and allow rest between sets.
3. Exercises should be done frequently to lessen pain for the patient: Regular movement can reduce stiffness and pain over time, but frequency must be balanced with rest and tolerance. The statement is overly broad and could be unsafe if it encourages doing too many repetitions or exercising into pain.
Take home points
- Never force ROM beyond the patient’s tolerance.
- Regular ROM prevents stiffness, but avoid causing fatigue or injury; always support the joint and watch for adverse signs.
When a patient is using a cane for maximal support, the nurse is aware that the patient should do which of the following?
Explanation
Proper cane use includes holding it in the hand opposite the weaker leg (strong side), using the cane to share weight and improve balance, keeping the elbow slightly flexed, and coordinating the sequence of cane and leg movements so that the cane provides support when the weaker limb bears weight. Correct technique reduces fall risk and promotes efficient, safer ambulation.
Rationale for correct answer:
2. Distribute weight evenly between the feet and the cane: When using a cane for maximal support, the user should place some of their body weight through the cane while walking so that the load is shared between the cane and the legs. This decreases the force that must be borne by the weaker limb and improves balance and safety.
Rationale for incorrect answers:
1. Hold the cane on the weaker side: The cane should be held in the stronger (unaffected) hand - that is, on the side opposite the weaker leg. Holding it on the stronger side lets the cane provide support and off-load weight from the weaker limb. Holding it on the weak side reduces stability.
3. Keep the elbow that is holding the cane straight and stiff: The elbow should be slightly flexed (about 20–30°) for proper leverage and comfort. A locked, stiff elbow transmits forces awkwardly and increases risk of discomfort or injury.
4. Advance the weaker foot ahead of the cane: The safe technique is to move the cane forward (about one small step’s length) and then advance the weaker (affected) leg toward or to the level of the cane; the stronger leg then steps past. Advancing the weaker foot ahead of the cane increases instability and fall risk.
Take home points
- Hold the cane on the stronger side (opposite the weak leg) and use it to share weight - don’t hold it on the weak side.
- Keep the elbow slightly flexed and advance the cane first, then the weaker leg - coordinate movements for stability.
To increase stability during client transfer, the nurse increases the base of support by performing which action?
Explanation
Basic principles of body mechanics and safe patient handling include how the base of support, center of gravity, and leverage affect stability. For safe transfers, nurses should widen their base of support, lower their center of gravity (bend knees), keep the load close to the body, and use leg muscles rather than the back.
Rationale for correct answer:
2. Spacing the feet farther apart: Widening the stance increases the base of support (BOS). A larger BOS makes it easier to keep the center of gravity (COG) within the BOS during movement, which improves overall stability during transfers.
Rationale for incorrect answers:
1. Leaning slightly backward: Leaning backward shifts the nurse’s center of gravity posteriorly and can actually reduce balance or place the nurse at risk of falling backward. It does not widen the base of support; it merely shifts weight and may make the transfer less stable.
3. Tensing the abdominal muscles: Tensing core muscles improves trunk stability and protects the back, which helps safe body mechanics, but it does not increase the base of support. It’s supportive, not a method of enlarging the BOS.
4. Bending the knees: Bending the knees lowers the center of gravity and uses leg muscles rather than the back (good body mechanics), which improves stability and reduces injury risk - however it does not increase the width of the base of support.
Take home points
- Widen your stance (feet farther apart) to increase the base of support and improve stability during transfers.
- Combine a wider base with bending the knees and keeping the patient close to your body to maximize safety and reduce back injury risk.
Comprehensive Questions
What term would the nurse use to identify the strong, flexible, inelastic fibrous bands and flattened sheets of connective tissue that attach muscle to bone?
Explanation
Tendons (including aponeuroses) connect muscle to bone and are built for high tensile strength so muscle force is efficiently transmitted to the skeleton; ligaments connect bones and stabilize joints; cartilage cushions and provides smooth surfaces and structural form; and joints are the anatomical sites of bone articulation. Clinically, recognizing these differences helps distinguish injury types (e.g., strain involves muscle/tendon, sprain involves ligament, cartilage damage leads to joint pain/degeneration).
Rationale for correct answer:
1. Tendons are dense, regularly arranged fibrous connective tissue made mostly of parallel collagen fibers (type I). They attach muscle to bone, transmit the force of muscle contraction to produce movement, and are strong and relatively inelastic. Flattened sheets of tendon tissue are called aponeuroses.
Rationale for incorrect answers:
2. Ligaments are also fibrous connective tissue but they connect bone to bone (or bone to cartilage) at joints. Their fiber arrangement and elastic content allow them to stabilize joints and limit excessive movement. They are functionally and anatomically distinct from tendons.
3. Cartilage is a firm but flexible avascular connective tissue (types: hyaline, elastic, fibrocartilage). It provides cushioning, smooth articular surfaces, and structural support (e.g., intervertebral discs, articular surfaces, ear). It does not attach muscle to bone.
4. Joints are the site where two or more bones meet. Joints are structures composed of bone ends plus associated cartilage, ligaments, synovial membranes (in synovial joints), etc.—they are not connective-tissue bands that attach muscle to bone.
Take home points:
- Tendons attach muscle to bone (strong, mostly inelastic collagen bundles; aponeuroses are flattened tendons).
- Ligaments attach bone to bone (stabilize joints).
The nurse is assisting a patient with conditioning exercises to prepare for ambulation. The nurse correctly instructs the patient to do what?
Explanation
Conditioning prepares muscles for weight-bearing and improves confidence with transfers and walking. Interventions should be individualized, start gently, avoid Valsalva, monitor vital signs and symptoms, and progressively increase intensity and duration as tolerated.
Rationale for correct answer:
2. Breathe in and out smoothly during quadriceps drills: Proper breathing during conditioning and quad sets improves oxygenation, prevents undue intrathoracic/intra-abdominal pressure, and lowers cardiovascular strain. Quadriceps drills are commonly used to build strength for standing and ambulation, and breathing smoothly is essential.
Rationale for incorrect answers:
1. Do full-body pushups in bed six to eight times daily: Bed push-ups can strengthen upper body muscles used for transfers, but prescribing “full-body pushups six to eight times daily” as a blanket instruction is unrealistic and may cause fatigue or be unsafe for some patients. Exercise prescription must be individualized.
3. Dangle on the side of the bed for 30 to 60 minutes: “Dangling” (sitting on the side of the bed) is used to assess tolerance and help orthostatic adaptation, but starting with 30–60 minutes is excessive and may precipitate orthostatic hypotension, dizziness, or nausea. Begin with short intervals, then gradually increase.
4. Allow the nurse to bathe the patient completely to prevent fatigue: While conserving energy is appropriate at times, encouraging independence and graded activity (having the patient perform as much as safely possible) helps conditioning. Full assistance for all ADLs impedes strengthening needed for ambulation.
Take home points
- Breathe smoothly during strengthening exercises to avoid Valsalva and undue cardiopulmonary strain.
- Progress activity gradually and promote patient participation rather than excessive passive care that prevents conditioning.
In many situations, a patient has sufficient strength to walk if he or she can do which of the following?
Explanation
Functional assessment of mobility - specifically which simple bedside observation best predicts whether a patient has the strength and endurance to walk. Walking requires coordinated lower-extremity strength, trunk stability, balance and some cardiovascular endurance; a patient who can sit unsupported for a prolonged period demonstrates many of these capabilities and is more likely to tolerate standing and ambulation than someone who can only perform minimal isolated movements.
Rationale for correct answer:
3. Raise the foot off the bed 1 inch: Being able to lift the foot slightly against gravity indicates sufficient quadriceps and hip flexor strength, which are critical muscle groups for initiating steps and supporting body weight during walking. This simple bedside test directly assesses lower-limb strength needed for ambulation.
Rationale for incorrect answers:
1. Lie prone for 1 hour: Tolerating a prone position only shows postural tolerance, not active lower-limb strength or coordination needed for ambulation.
2. Bathe him- or herself: Self-bathing demonstrates independence in activities of daily living (ADLs) but may be performed sitting down. It doesn’t reliably test lower-extremity strength for ambulation.
4. Sit up in bed for 1 hour: Sitting up tests trunk stability and endurance, but it does not directly confirm that the leg muscles are strong enough to support walking.
Take home points
- Raising the foot off the bed = direct sign of lower-limb strength needed for ambulation.
- Other activities (sitting up, bathing, lying prone) show endurance or independence but do not confirm walking strength.
Mrs. Eden tells the nurse she feels faint while walking in the corridor with the nurse. What should the nurse do?
Explanation
For a patient experiencing presyncope or syncope while ambulating, the nurse’s priority is fall prevention and restoring cerebral perfusion - achieved by stopping ambulation, supporting the patient, and getting them into a seated or supine position quickly and gently. After stabilizing, the nurse should assess vitals, check for symptoms (chest pain, diaphoresis, paleness), review medications, and arrange further evaluation as indicated.
Rationale for correct answer:
4. Guide her to a nearby chair, easing her onto it to rest: Helping the patient to sit immediately lowers the center of gravity, reduces orthostatic strain, and prevents a fall. Once seated or supine, the nurse should assess airway/breathing/circulation, loosen tight clothing, measure vital signs, and be prepared to place the patient supine with legs elevated if symptoms worsen.
Rationale for incorrect answers:
1. Instruct the patient to quicken her pace so they can return to her room: Speeding up increases metabolic and cardiovascular demand and raises the risk of collapse or falling. Do not accelerate a patient who feels faint.
2. Leave her momentarily to find another nurse to help: Leaving a patient who is feeling faint removes immediate support and increases risk of injury if she collapses. The nurse should stay with and support the patient.
3. Advise her to look down at her feet to help maintain her balance: Looking down is not a reliable safety maneuver for syncope and may actually worsen dizziness or compromise balance. The priority is to reduce orthostatic stress and get the patient into a safe sitting/lying position.
Take home points
- If a patient feels faint while walking, stop immediately and assist the patient to sit or lie down - do not leave them or make them walk faster.
- Preventing a fall is the first priority; after the patient is safe, assess vital signs and consider causes such as orthostatic hypotension, medications, hypovolemia, or cardiac issues.
The use of patient care ergonomics is associated with which of the following patient outcomes?
Explanation
Ergonomic practices (use of lifts, transfer devices, proper body mechanics, and team approaches) are implemented to protect caregivers from injury and to improve patient safety and comfort during movement. When used correctly, ergonomics promote safer transfers, preserve patient skin integrity, maintain dignity, and often facilitate earlier mobilization and rehabilitation.
Rationale for correct answer:
1. Increased patient comfort, security, and dignity during lifts and transfers: Patient-centered ergonomics are designed to protect both patients and caregivers. Proper ergonomics reduce painful manual handling, minimize jarring or sliding, and support safe, dignified transfers - improving comfort, security, and dignity.
Rationale for incorrect answers:
2. Increased patient falls, skin tears, and abrasions: The opposite is true: when ergonomics are applied correctly, the incidence of falls, skin tears, and abrasions generally decreases because movements are controlled, and friction/shear are minimized.
3. Decreased patient movement and independence: Ergonomic interventions are intended to enable safer mobility and independence where possible. While some mechanical aids require staff assistance initially, the goal is to preserve or restore safe movement, not reduce it.
4. Increased friction and shearing: Good ergonomics aim to reduce friction and shear (for example, by using slide sheets, repositioning aids, or lifts), thereby lowering risk of skin breakdown.
Take home points
- Patient-care ergonomics improve safety and dignity - they make lifts/transfers more comfortable and secure for patients.
- Proper ergonomics reduce risks (falls, skin injury) and support safer mobility; they are implemented to protect both patients and staff.
Which of the following should the nurse do when assisting the patient to ambulate?
Explanation
Safe ambulation principles: assessing readiness, using proper assistive devices and techniques (gait belt use, side/behind positioning), preventing fatigue, and promoting independence while minimizing fall risk. The gait belt is a simple, effective tool that gives the nurse control and reduces the need to use awkward lifting postures. Safe ambulation also requires good footwear, clear environment, appropriate pacing, and monitoring for signs of intolerance.
Rationale for correct answer:
3. Use a gait belt to provide support: A properly applied gait belt gives the nurse secure, ergonomic handholds to assist, steady, and catch the patient if they stumble. It reduces fall risk and protects both patient and caregiver when used correctly.
Rationale for incorrect answers:
1. Place a hand under the axilla to provide support: Placing a hand under the axilla can be uncomfortable or painful for the patient and risks injury to the caregiver (or the patient’s brachial plexus). It also gives poor leverage and less control than using a gait belt or holding the patient at the trunk/hips.
2. Ensure the patient walks as far as possible for as long as possible: Pushing a patient to walk farther/longer than tolerated increases the risk of fatigue, dizziness, falls, and cardiac or respiratory compromise. Ambulation should be progressed gradually and individualized to the patient’s endurance and safety.
4. Encourage the patient to watch their feet to ensure a steady gait: Looking down limits visual input about the environment, can throw off balance, and often worsens gait stability. Patients should be encouraged to look forward, scan the path, and use assistive devices correctly.
Take home points
- Use a gait belt for support - it provides the safest, most controlled way to steady and assist a patient during ambulation.
- Progress ambulation gradually and keep the patient looking forward - avoid overexertion and discourage looking down at the feet which can destabilize gait.
When working with an older patient to develop an exercise program, the nurse would recommend which of the following?
Explanation
Key principles of safe exercise prescription for older adults include individualizing frequency/intensity, using the talk test to gauge exertion, correctly calculating target heart rates if used, and obtaining medical clearance when indicated. A comprehensive program for older adults should incorporate aerobic activity, strength training, balance, and flexibility, start gradually, and progress as tolerated under clinical guidance.
Rationale for correct answer:
4. Obtaining medical clearance before beginning the program: Older adults - particularly those with chronic conditions, sedentary lifestyle, or multiple risk factors - should have medical clearance or assessment before starting a new exercise program. This reduces the risk of adverse cardiac or musculoskeletal events and helps tailor the safe intensity and types of activity.
Rationale for incorrect answers:
1. A frequency of six times a week: Exercise programs should be individualized, include rest days, and consider current fitness, comorbidities, and tolerance. General recommendations are usually expressed as minutes per week (e.g., 150 min moderate activity) with strength and balance sessions included.
2. Exercising to the point of breathlessness when trying to speak: The “talk test” is used clinically: during moderate-intensity activity a person should be able to talk but not sing. If someone becomes breathless to the point they cannot speak, intensity is too high and should be reduced.
3. Maintaining a target heart rate of 220 plus age: The common maximal heart-rate estimate is 220 − age (not plus age), and target exercise HR is a percentage of that maximum. Heart-rate targets should be individualized and determined after appropriate assessment.
Take-home points
- Get medical clearance when appropriate - especially for older or sedentary patients or those with chronic conditions.
- Use the talk test and start low-go slow - avoid working to the point where the patient cannot speak;
A client weighs 250 pounds and needs to be transferred from the bed to a chair. Which instruction by the nurse to the unlicensed assistive personnel (UAP) is most appropriate?
Explanation
For heavy or non-assisting clients, nurses should prioritize mechanical lifts and team transfers rather than manual lifting, and UAPs should be given clear instructions that follow facility policy and evidence-based safe-handling practices.
Rationale for correct answer:
3. “Use the mechanical lift and another person to transfer the client from the bed to the chair.” This gives a clear, evidence-based instruction: use a mechanical lift (or other safe patient-handling device) plus an assistant as needed. Mechanical lifts reduce injury risk to staff and are the recommended method for transferring patients above manual-lift weight thresholds or when the patient cannot assist.
Rationale for incorrect answers:
1. “Using proper body mechanics will prevent you from injuring yourself.” Teaching proper body mechanics is important, but this statement overpromises: even when using correct technique, manually lifting very heavy patients still places staff at high risk of injury.
2. “You are physically fit and at lesser risk for injury when transferring the client.” This assumes the UAP’s fitness protects them-an unsafe assumption. Staff fitness does not eliminate the risk of musculoskeletal injury from manual transfers of heavy clients and is not an acceptable reason to forgo mechanical aids or additional help.
4. “Use the back belt to avoid hurting your back.” Back belts have not been shown to reliably prevent injury and are not a substitute for safe patient-handling equipment and team assistance. Relying on a back belt may give false security and is not the safest instruction.
Take home points
- For heavy or non-assisting patients, use mechanical lifts and assistance-don’t rely on manual lifts even if staff feel “fit.”
- Clear, safety-focused instructions to UAPs protect both staff and patients; belts or promises of “proper mechanics” alone are insufficient.
A nurse is teaching a client about active range-of-motion (ROM) exercises. The nurse then watches the client demonstrate these principles. The nurse would evaluate that teaching was successful when the client does which of the following?
Explanation
Principles of teaching and performing active ROM: safety (do not force movement or go past resistance), adequacy (multiple repetitions and appropriate frequency), and consistency (use a regular sequence so exercises are complete and measurable). The nurse should teach pain-free movement through the available range, an appropriate number of repetitions and sessions per day, and a consistent order so the client performs a complete, safe program.
Rationale for correct answer:
4. Uses the same sequence during each exercise session: Using a consistent sequence helps ensure all joints/muscle groups are exercised, reinforces correct technique, and reduces the chance of forgetting or skipping movements. Consistency also helps the nurse evaluate progress and identify problems.
Rationale for incorrect answers:
1. Exercises past the point of resistance: Pushing past resistance risks injury, pain, and joint damage. Active ROM should be performed only through the available, pain-free range; resistance indicates the limit of safe motion.
2. Performs each exercise one time: One repetition is insufficient to maintain or improve mobility. ROM programs normally call for multiple repetitions (often several sets of 8–10, or as prescribed) to be effective.
3. Performs each series of exercises once a day: Once-daily may be inadequate for many clients; ROM exercises are commonly done multiple times per day depending on the condition and goals. The point being tested is correct technique and consistency, not minimal frequency.
Take home points
- Never push a joint past its point of resistance or into pain - active ROM must be pain-limited.
- Consistency matters: perform a complete, repeated program in a consistent sequence so progress and problems are easy to monitor.
Performance of activities of daily living (ADLs) and active range of-motion (ROM) exercises can be accomplished simultaneously as illustrated by which of the following? Select all that apply
Explanation
Functional ROM- how routine ADLs and mobility tasks can simultaneously serve as therapeutic active range-of-motion exercises. Therapists and nurses often incorporate ROM training into meaningful activities (like eating, grooming, ambulation) so patients practice needed motions in context, improving adherence and functional gains.
Rationale for correct answer:
1. Elbow flexion with eating and bathing: Both eating (bringing a utensil to the mouth) and many bathing tasks (washing face, hair, underarms) use repeated elbow flexion. Encouraging ADLs provides functional repetitions of elbow flexion as active ROM.
4. Thumb ROM with eating and writing: Eating (grasping utensils) and writing (holding a pen/pencil) require thumb opposition and fine thumb movement-excellent opportunities for active ROM of the thumb.
5. Hip flexion with walking: Walking involves repeated hip flexion during the swing phase. Ambulation is a primary functional activity that provides active ROM for the hip.
Rationale for incorrect answers:
2. Elbow extension with shaving and eating: Shaving and eating primarily involve elbow flexion (bringing hand to face/mouth), not elbow extension. Elbow extension is used to reach away from the body, which is not the main movement in these ADLs.
3. Wrist hyperextension with writing: Writing uses a functional amount of wrist extension (and fine finger movement), but hyperextension (excessive extension beyond normal ROM) is neither necessary nor desirable and could cause strain. The activity provides normal wrist ROM, not hyperextension.
Take home points
- Use everyday activities (self-care and mobility) as opportunities for active ROM-this makes exercise purposeful and more likely to be repeated.
- Match the joint/movement needed in the ADL to the ROM goal.
The client is ambulating for the first time after surgery. The client tells the nurse, “I feel faint.” Which is the best action by the nurse?
Explanation
The immediate priority actions for a patient reporting presyncope/dizziness during ambulation - fall prevention and rapid safe positioning. The nurse’s first responsibility is to protect the client from falling (assist to a chair or floor), then assess (vital signs, skin color, bleeding), provide interventions (oxygen, fluids, medication review) and call for help if needed.
Rationale for correct answer:
4. Assist the client to a nearby chair: The priority is immediate safety: support the client and help her sit (or, if no chair is available, help her to the floor while protecting her head). This prevents a fall, allows measurement of vital signs, and lets you assess for orthostatic hypotension, blood loss, pain, medication effects, or other causes.
Rationale for incorrect answers:
1. Find another nurse for help: Getting help may be appropriate after the client is safe, but the immediate priority is preventing a fall or injury. Searching for help first delays immediate protection of the client.
2. Return the client to her room as quickly as possible: Rapid movement (walking the client back) risks the client fainting and falling. Move her safely and steadily to the nearest stable surface rather than hurriedly trying to get to the room.
3. Tell the client to take rapid, shallow breaths: Rapid, shallow breathing is not helpful and may increase dizziness. If anxiety or hyperventilation were present, breathing techniques would be considered, but the immediate action for faintness is to get the client safely to a chair or to the floor.
Take home points
- Immediately support and seat a patient who feels faint to prevent falls; don’t delay looking for help.
- After the client is safe, assess vital signs and possible causes (orthostatic hypotension, blood loss, medication effects) before further movement.
Before transferring a patient from the bed to a stretcher, which assessment data does the nurse need to gather? Select all that apply
Explanation
The nurse must perform a pre-transfer risk assessment (weight, mobility, activity tolerance) and follow a safe-mobility algorithm or facility policy to choose the correct equipment and number of staff. The goal is to protect both patient and caregivers by preventing falls and musculoskeletal injury.
Rationale for correct answer:
1. Patient’s weight: Knowing the patient’s weight is essential to decide whether manual transfer is safe or whether a mechanical lift or additional staff are required (many safe-handling algorithms and lift manufacturers set weight limits). Weight helps determine the number of caregivers and the type of equipment (full-body sling, sit-to-stand lift, etc.).
2. Patient’s activity tolerance: Activity tolerance (how long/what intensity the patient can tolerate without significant symptoms) indicates whether the patient can assist or needs rest breaks, and helps predict cardiopulmonary responses during transfer. This affects how you plan and pace the transfer and whether extra monitoring is needed.
3. Patient’s level of mobility: Assessing mobility (ability to bear weight, to pivot, to follow commands, to assist) directly determines whether a one-person transfer is safe, or if two people or a mechanical device must be used. Mobility screening tools and bedside mobility assessments are standard before any transfer.
Rationale for incorrect answers:
4. Recent laboratory values: Labs can be relevant in special situations (e.g., severe anemia, coagulopathy, electrolyte abnormalities causing weakness or orthostatic symptoms), but they are not a standard part of the transfer safety checklist unless there is a specific clinical reason to suspect a lab-related risk. Assess functional status first and request labs selectively.
5. Nutritional intake: Nutritional intake is important for overall care planning (wound healing, long-term recovery), but it generally does not determine the immediate safety of a bed-to-stretcher transfer. It would not normally change the equipment or number of staff required for the transfer.
6. Safe mobility algorithm: Using a facility or evidence-based safe mobility algorithm (or mobility assessment tool) integrates weight, mobility, ability to assist, and other risk factors and guides the nurse to the correct device, number of caregivers, or whether a lift is required. Algorithms reduce guesswork and staff injuries.
Take home points
- Always assess weight, mobility level, and activity tolerance before a transfer.
- These facts determine whether mechanical lifts or extra staff are needed.
A 51-year-old adult comes to a medical clinic for an annual physical exam. The patient is found to be slightly overweight and reports being inactive, walking only 2 to 3 times a week with his wife after work. He has good muscle strength and coordination of lower extremities. Which of the following recommendations from the Physical Activity Guidelines for Americans should the nurse suggest? Select all that apply
Explanation
The Physical Activity Guidelines for Americans provide evidence-based recommendations to promote health, prevent chronic disease, and improve quality of life through regular physical activity. Nurses play a vital role in educating and motivating clients to incorporate aerobic and muscle-strengthening activities safely and effectively into their daily lives.
Rationale for correct answers:
1. Move more and sit less throughout the day: According to the Physical Activity Guidelines for Americans, adults should reduce sedentary behavior by moving more throughout the day. Any amount of movement is beneficial compared to sitting still, especially for individuals with sedentary lifestyles.
3. Perform muscle-strengthening activities using light weights on 2 or more days a week: The guidelines recommend that adults perform muscle-strengthening activities of moderate or greater intensity on 2 or more days per week, targeting all major muscle groups. Using light weights with proper resistance is appropriate for beginners.
4. Walk at a vigorous pace with wife at least 150 minutes over five days a week: Adults should perform at least 150 minutes of moderate-intensity aerobic activity (e.g., brisk walking) or 75 minutes of vigorous-intensity activity weekly. Spreading the activity over five days promotes consistency and improves cardiovascular health, weight management, and endurance.
Rationale for incorrect answers:
2. Participate in at least 90 minutes a week of moderate-intensity aerobic physical activity:
This amount is below the recommended minimum. Adults should engage in at least 150 minutes per week of moderate-intensity aerobic activity (such as brisk walking). Ninety minutes weekly is insufficient to achieve meaningful health benefits or meet guideline recommendations.
5. Focus on balance training: Balance training is mainly recommended for older adults (≥65 years) or those at risk of falls. This patient is 51 years old, has good coordination and muscle strength, and does not currently need specific balance training interventions.
Take-home points
- Adults should perform at least 150 minutes of moderate-intensity aerobic activity per week plus muscle-strengthening exercises on 2 or more days weekly.
- Encouraging clients to move more and sit less throughout the day can greatly enhance overall health, especially for those with sedentary lifestyles.
Family members have asked for a meeting with the nursing staff of an assisted living residential center to discuss the feasibility of their mother using a walker. The family is worried that her health is declining; they wonder whether she can use the walker safely. Which of the following instructions should the nurse give the family after assessing that it is safe for the woman to use a walker? Select all that apply
Explanation
Nurses must assess each client’s strength, balance, and coordination before recommending an appropriate assistive device. Proper education on walker use promotes independence, safety, and confidence during ambulation while minimizing the risk of injury.
Rationale for correct answers:
1. A walker is useful for patients who have impaired balance: Walkers provide a broad base of support, helping individuals with impaired balance or weakness to maintain stability while ambulating. They are particularly useful for older adults or clients recovering from illness or surgery, as they reduce the risk of falls and promote safe mobility.
4. Walkers should not be used on stairs: Walkers are not designed for use on stairs due to stability and balance limitations. Attempting to use one on stairs poses a serious fall hazard. For clients who must use stairs, other assistive devices like handrails or canes should be used instead.
5. If the patient has difficulty advancing the walker, a walker with wheels is an option: For clients who have difficulty lifting a standard walker, a wheeled walker (rolling walker) is safer and easier to maneuver. It allows smoother movement and reduces upper-body strain, especially for clients with limited arm strength.
Rationale for incorrect answers:
2. The patient uses a walker by pushing the device forward: Walkers should not be pushed forward forcefully. Instead, the patient should lift and place the walker about one step ahead (unless it has wheels). Pushing a standard walker may cause it to tip or roll uncontrollably, increasing the risk of falls.
3. Leaning over the walker improves the patient’s balance: Leaning over the walker is unsafe and promotes poor posture. It shifts the center of gravity forward, increasing fall risk and leading to back strain. The correct position is to stand upright inside the walker, keeping the elbows slightly flexed and the body aligned.
Take-home points
- Walkers enhance stability for clients with impaired balance but should never be used on stairs or leaned on excessively.
- Education on proper technique and device selection (standard vs. wheeled walker) is crucial for promoting safety and maintaining functional mobility in older adults.
A patient has an order for application of compression stockings. Place the following steps for application of the compression stockings in the correct order:
Explanation
Compression stocking application,is an important nursing intervention used to prevent venous thromboembolism (VTE) and reduce venous stasis in immobile patients. Proper sizing, correct technique, and smooth application are essential to maintain circulation and prevent complications such as skin breakdown or constriction.
Rationale for correct answers:
Step 1-- 2. Use tape measure to measure patient’s leg for proper stocking size.
Accurate measurement ensures the stockings fit correctly. Ill-fitting stockings can cause impaired circulation or fail to provide adequate compression.
Step 2-- 4. Turn elastic stocking inside out, keeping hand inside holding heel. Take other hand and pull stocking inside out until reaching the heel.
This step prepares the stocking for easier and smoother application, ensuring the heel and toe portions are properly aligned.
Step 3—1. Place patient’s toes into foot of stocking up to the heel; keep smooth.
Starting at the toes ensures proper fit and alignment. The fabric should remain smooth to prevent skin irritation or pressure injury.
Step 4—5. Slide remaining portion of stocking over patient’s foot, covering toes. Be sure foot fits into toe and heel of stocking.
This step ensures the stocking conforms to the foot’s shape and provides even pressure distribution.
Step 5-- 3: Slide stocking up over patient’s calf until sock is completely extended.
Pulling the stocking smoothly up the leg completes the process and ensures proper compression without folds or wrinkles that may impede circulation.
Take-home points
- Compression stockings prevent venous stasis and thrombus formation in clients with limited mobility or at risk for DVT.
- Proper sizing and smooth application technique are vital to ensure therapeutic effectiveness and prevent circulatory impairment.
Exams on Mobility
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Identify Variables that influence body alignment and mobility.
- Differentiate isotonic, isometric, and isokinetic exercise.
- Describe the effects of exercise and immobility on major body systems.
- Assess body alignment, mobility, and activity tolerance, using appropriate interview and physical assessment skills.
- Develop nursing diagnoses that correctly identify mobility problems amenable to nursing interventions.
- Utilize principles of body mechanics when appropriate.
- Use safe patient handling and movement techniques and equipment when positioning, moving, lifting, and ambulating patients.
- Plan, implement, and evaluate nursing care related to select nursing diagnoses involving mobility problems.
Introduction
A strong, well-developed body of research evidence supports the role of exercise in improving the health status of individuals with cardiovascular disease, pulmonary dysfunction, disabilities of aging, and depression.
A growing body of research supports the preventive and therapeutic effects of exercise for individuals with hypertension, osteoporosis, coronary heart disease, mental health disorders, diabetes, cancer, arthritis, chronic fatigue syndrome.
An activity-exercise pattern refers to a person’s routine of exercise, activity, leisure, and recreation. It includes:
- activities of daily living (ADLs) that require energy expenditure such as hygiene, dressing, cooking, shopping, eating, working, and home maintenance.
- the type, quality, and quantity of exercise, including sports.
Mobility, the ability to move freely, easily, rhythmically, and purposefully in the environment, is an essential part of living. People must move to protect themselves from trauma and to meet their basic needs
Movement
3.1 NORMAL MOVEMENT
Normal movement and stability are the result of an intact musculoskeletal system, an intact nervous system, and intact inner ear structures responsible for equilibrium.
It involves four basic elements: body alignment (posture), joint mobility, balance, and coordinated movement.
- Alignment and Posture
Proper body alignment and posture bring body parts into position in a manner that promotes optimal balance and maximal body function whether the client is standing, sitting, or lying down.
A person maintains balance as long as the line of gravity (an imaginary vertical line drawn through the body’s center of gravity) passes through the center of gravity (the point at which all of the body’s mass is centered) and the base of support (the foundation on which the body rests).
Abdominal and skeletal muscles function almost continuously, making tiny adjustments that enable an erect or seated posture despite the endless downward pull of gravity. The extensor muscles, often referred to as the antigravity muscles, carry the major load as they keep the body upright.
- Joint mobility:
The bones of the skeleton articulate at the joints, and most of the skeletal muscles attach to the two bones at the joint.
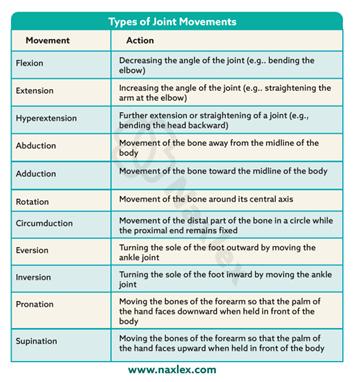
These muscles are categorized according to the type of joint movement they produce on contraction. Muscles are therefore called flexors, extensors, internal rotators, and the like.
The flexor muscles are stronger than the extensor muscles. Thus, when a person is inactive, the joints are pulled into a flexed (bent) position. If this tendency is not counteracted with exercise and position changes, the muscles permanently shorten, and the joint becomes fixed in a flexed position (contracture).
The range of motion (ROM) of a joint is the maximum movement that is possible for that joint. Joint range of motion varies from individual to individual and is determined by genetic makeup, developmental patterns, the presence or absence of disease, and the amount of physical activity in which the person normally engages.
- Balance:
The mechanisms involved in maintaining balance and posture are complex and involve informational inputs from the labyrinth (inner ear), from vision (vestibulo-ocular input), and from stretch receptors of muscles and tendons (vestibulospinal input).
Mechanisms of equilibrium (sense of balance) respond, frequently without our awareness, to various head movements.
Proprioception is the term used to describe awareness of posture, movement, and changes in equilibrium and the knowledge of position, weight, and resistance of objects in relation to the body.
- Coordinated movement:
Balanced, smooth, purposeful movement is the result of proper functioning of the cerebral cortex, cerebellum, and basal ganglia.
The cerebral cortex initiates voluntary motor activity, the cerebellum coordinates the motor activities of movement, and the basal ganglia maintain posture.
Factors Affecting Body Alignment and Activity
Body alignment, mobility, and daily activity are influenced by multiple factors: growth and development, nutrition, personal values/attitudes, external factors, and prescribed limitations.
1. Growth and Development
- Infants/Children: Movements initially reflexive - progress to controlled motor skills. Gross motor skills develop head-to-toe (head control - crawling - walking). Fine motor refinement (drawing, dressing, brushing teeth) occurs by preschool age. Immobility in children delays social/motor development.
- School-age (6–12 yrs): Motor skills refine further; PE and sports shape lifelong exercise patterns. Posture usually excellent.
- Adolescents: Growth spurts may cause postural issues (e.g., heavy bags, screen use). Habits may persist into adulthood.
- Adults (20–40 yrs): Few mobility issues except pregnancy, which alters balance. Moderate exercise is encouraged during pregnancy (with medical clearance). Benefits: prevents gestational diabetes, controls weight, reduces long-term obesity risk.
- Older Adults: Age-related changes: decreased muscle tone, bone density, flexibility, reaction time. Osteoporosis (common in women) - brittle bones, fractures, stooped posture, shuffling gait. Regular activity maintains strength, flexibility, bone health, reduces falls, obesity, diabetes, and improves mood.
2. Nutrition
Undernutrition: Weakness, fatigue, poor muscle development. Deficiencies: Vitamin D - bone deformities and Calcium & Vitamin D - osteoporosis risk.
Overnutrition (obesity): Alters posture, stresses joints, affects balance and movement.
3. Personal Values and Attitudes
Family influence shapes exercise habits. Sedentary lifestyle often passed on to children. Appearance, cultural roles, and location influence activity choices. Motivation can be enhanced through:
-
- Fun/social activities, music, goal-setting, progress tracking.
- Framing exercise as recreation, well-being, or self-care.
FIT model (Frequency, Intensity, Time) used for exercise prescription. Nurses should tailor exercise plans to client’s health, fitness, motivation, and safety.
4. External Factors
- Environment: Extreme heat/humidity - discourage activity. Safe, pleasant environments - encourage activity.
- Hydration: Short activity - 1–2 cups of water. Endurance events - hydration before, during, and after (water + sports drinks with sodium).
- Resources: Lack of money, facilities, or safe neighborhoods limits opportunities for activity.
- Technology: TV, computers, video games increase sedentary behavior (esp. in adolescents).
5. Prescribed Limitations
- Medical restrictions: Casts, splints, braces, traction limit movement to promote healing. Dyspnea - avoid exertion. Bed rest used for edema, pain relief, tissue repair, reducing oxygen needs.
- Types of bed rest vary: Strict confinement vs. bathroom privileges.
3.2 EXERCISE
People participate in exercise programs to decrease risk factors for chronic diseases and to increase their health and well-being.
Functional strength is another goal of exercise, and is defined as the ability of the body to perform work.
Activity tolerance is the type and amount of exercise or ADLs an individual is able to perform without experiencing adverse effects.
Types of exercise:
Exercise involves the active contraction and relaxation of muscles. Exercises can be classified according to the type of muscle contraction (isotonic, isometric, or isokinetic) and according to the source of energy (aerobic or anaerobic).
According to the type of muscle contraction:
- Isotonic (dynamic) exercises are those in which the muscle shortens to produce muscle contraction and active movement. Most physical conditioning exercises—running, walking, swimming, cycling.
Isotonic exercises increase muscle tone, mass, and strength and maintain joint flexibility and circulation. During isotonic exercise, both heart rate and cardiac output quicken to increase blood flow to all parts of the body.
- Isometric (static or setting) exercises are those in which muscle contraction occurs without moving the joint (muscle length does not change).
These exercises involve exerting pressure against a solid object and are useful for strengthening abdominal, gluteal, and quadriceps muscles used in ambulation; for maintaining strength in immobilized muscles in casts or traction; and for endurance training.
- Isokinetic (resistive) exercises involve muscle contraction or tension against resistance. During isokinetic exercises, the person tenses (isometric) against resistance. These exercises are used in physical conditioning and are often done to build up certain muscle groups.
According to the source of energy
- Aerobic exercise is activity during which the amount of oxygen taken into the body is greater than that used to perform the activity. Aerobic exercises use large muscle groups that move repetitively. Aerobic exercises improve cardiovascular conditioning and physical fitness.
- Anaerobic exercise involves activity in which the muscles cannot draw out enough oxygen from the bloodstream, and anaerobic pathways are used to provide additional energy for a short time. This type of exercise is used in endurance training for athletes such as weight lifting and sprinting.
Intensity of exercise can be measured in three ways:
1. Target heart rate. The goal is to work up to and sustain a target heart rate during exercise, based on the person’s age. To determine target heart rate, first calculate the person’s maximum heart rate by subtracting his or her current age in years from 220. Then obtain the target heart rate by taking 60% to 85% of the maximum. Because heart rates vary among individuals, the tests that follow are replacing this measure.
2. Talk test. This test is easier to implement and keeps most people at 60% of maximum heart rate or more. When exercising, the person should experience labored breathing, yet still be able to carry on a conversation.
3. Borg scale of perceived exertion: This scale measures “how difficult” the exercise feels to the person in terms of heart and lung exertion. The scale progresses from 1 to 20 with the following markers: 7 = very, very light; 9 = very light; 11 = fairly light; 13 = somewhat hard; 15 = hard; 17 = very hard; and 19 = very, very hard.
Nursing insights: Guidelines and Minimal Requirements for Physical Activity
FREQUENCY AND DURATION
- Aerobic: Cumulative 30 minutes or more daily (can be divided throughout the day) of “moderate intensity” movement as measured by talk test and perceived exertion scale.
- Stretching: Should be added onto that minimum requirement so that all parts of the body are stretched each day.
- Strength training: Should be added onto these minimum requirements so that all muscle groups are addressed at least three times a week, with a day of rest after training.
TYPE OF EXERCISE
- Aerobic: Elliptical exercisers, walking, biking, gardening, dancing, and swimming are recommended for all individuals including beginners and older adults. Activities that are more strenuous include jogging, running, Spinning, power yoga, bouncing, boxing, and jumping rope.
- Stretching: Yoga, Pilates, qigong, and many other flexibility programs are effective.
- Strength training: Resistance can be provided with weights, bands, balls, apparatus, and body weight.
SAFETY
- Stress the importance of balance and prevention of falls, proper clothing to ensure thermal safety, checking equipment for proper function, wearing a helmet and other protective gear, using reflective devices at night, and carrying identification and emergency information.
Benefits of Exercise
Regular exercise is essential for mental and physical health, supporting multiple body systems.
1. Musculoskeletal System
- Maintains/increases muscle size, tone, strength (hypertrophy with strenuous exercise).
- Improves efficiency of muscle contraction.
- Joints: exercise provides nourishment, increased flexibility, stability, ROM.
- Bones: weight-bearing exercise strengthens bones; prevents osteoporosis.
- Reduces weakness, frailty, depression, falls in older adults.
2. Cardiovascular System
- AHA: 150 min/week moderate OR 75 min/week vigorous exercise.
- Benefits:
- increased HR and contraction strength.
- increased cardiac output and circulation.
- Stress reduction.
- Aerobic exercises (walking, cycling, yoga) improve BP, HR variability, circulation, and lower stress.
3. Respiratory System
- Improves ventilation, gas exchange, oxygenation.
- Enhances toxin elimination and brain oxygenation - better problem solving, stability.
- Prevents pooling of secretions, reduces infection risk.
- Helps in management of COPD (walking, cycling, strength training).
- Yoga breathing aids asthma control.
4. Gastrointestinal System
- Improves appetite, GI tone, and peristalsis.
- Relieves constipation (rowing, swimming, walking, sit-ups).
- Helps in IBS and digestive disorders.
5. Metabolic/Endocrine System
- Increases metabolic rate (up to 20x during strenuous exercise).
- Continued increased metabolism after activity.
- Uses triglycerides and fatty acids - decreases cholesterol, triglycerides, HbA1C.
- Promotes weight loss and insulin sensitivity.
6. Urinary System
- increased blood flow - better waste excretion.
- Prevents urinary stasis, reducing UTI risk.
7. Immune System
- Exercise aids lymphatic circulation - improved pathogen destruction.
- Moderate exercise enhances immunity.
- Excessive strenuous exercise may temporarily Decreased immunity - need rest for recovery.
8. Psychoneurologic System
- Depression/stress can reduce activity - slumped posture, fatigue.
- Regular exercise:
- improves mood, decreases anxiety and stress.
- increases neurotransmitters (serotonin, norepinephrine), increases endorphins.
- Improves sleep quality.
- Excessive exercise sometimes linked to eating disorders.
9. Cognitive Function
- Improves decision-making, problem solving, planning, attention.
- Strengthens neuronal connections.
- Cross-lateral movements (e.g., Brain Gym) aid ADD/ADHD, learning, mood disorders.
10. Spiritual Health
- Yoga and meditative movement - improve mind–body–spirit balance.
- Promote relaxation response (RR) - decrease HR, BP, RR, stress.
- Techniques:
- Progressive muscle relaxation.
- Labyrinth walking or finger-tracing mandalas - induce calm, reduce insomnia.
3.3 EFFECTS OF IMMOBILITY
Immobility negatively impacts multiple body systems. The severity depends on duration of inactivity, health status, and sensory awareness. Early ambulation is key to preventing complications.
1. Musculoskeletal System
- Disuse osteoporosis - bone demineralization (risk of fractures).
- Disuse atrophy - muscle wasting, Decreased strength and function.
- Contractures - permanent muscle shortening, deformities (foot drop, wrist drop, hip rotation).
- Joint stiffness/pain - immobility of collagen tissue and calcium deposits in joints.
2. Cardiovascular System
- Diminished cardiac reserve - tachycardia with minimal exertion.
- Valsalva maneuver (breath-holding during straining) - Decreased venous return, possible arrhythmias.
- Orthostatic hypotension - dizziness, fainting, Increased HR on standing due to poor vasoconstriction reflex.
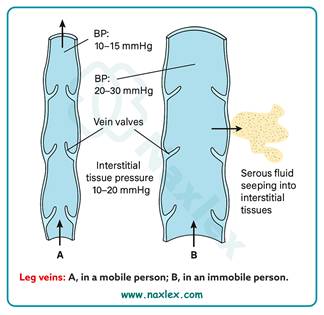
- Venous vasodilation/stasis - pooling of blood in legs, incompetent valves.
- Dependent edema - fluid accumulation in sacrum, heels, legs.
- Thrombus formation – DVT (deep venous thrombosis) risk, possible embolism (lungs, heart, brain).
3. Respiratory System
- Decreased lung expansion - shallow breathing, Decreased vital capacity.
- Pooling of secretions - risk of respiratory acidosis, infection.
- Atelectasis - collapse of alveoli from mucus blockages and Decreased surfactant.
- Hypostatic pneumonia - pooled secretions promote bacterial growth, serious infection risk.
4. Metabolic System
- Decreased Metabolic rate - reduced energy needs.
- Negative nitrogen balance - protein breakdown > synthesis, poor wound healing.
- Anorexia - decreased appetite, risk of malnutrition.
- Negative calcium balance - bone calcium loss due to lack of weight-bearing.
5. Urinary System
- Urinary stasis - incomplete emptying in supine position.
- Renal calculi - excess calcium in urine forms stones.
- Urinary retention - bladder distention, overflow incontinence.
- Urinary infections (UTIs) - stagnant urine supports bacterial growth, reflux may infect kidneys.
6. Gastrointestinal System
- Constipation/impaction - Decreased peristalsis, weak abdominal muscles, uncomfortable bedpan use.
- Straining (Valsalva) - Increased intra-abdominal pressure, risk to cardiovascular system.
7. Integumentary System
- Reduced skin turgor - skin atrophy, loss of elasticity.
- Skin breakdown/pressure ulcers - impaired circulation and nutrition supply to skin.
8. Psychoneurologic System
- Decreased Endorphins - poor mood regulation.
- Low self-esteem from dependency and loss of role.
- Emotional changes - apathy, withdrawal, regression, anger, aggression.
- Decreased Intellectual stimulation - poor concentration, problem-solving, decision-making.
- Time perception changes - altered awareness of intervals.
- Anxiety due to loss of control.
Nursing Management
4.1 ASSESSING
Assessment relative to a client’s activity and exercise should be routinely addressed and includes a nursing history and a physical examination of:
- body alignment
- gait
- appearance and movement of joints
- capabilities and limitations for movement
- muscle mass and strength
- activity tolerance
- problems related to immobility
- physical fitness.
NURSING HISTORY
An activity and exercise history is usually part of the comprehensive nursing history.
Daily activity level
• What activities do you carry out during a routine day?
• Are you able to carry out the following tasks independently?
- Eating
- Dressing and grooming
- Bathing d. Toileting
- Ambulating
- Using a wheelchair
- Transferring in and out of bed, bath, and car
- Cooking
- House cleaning
- Shopping
• Where problems exist in your ability to carry out such tasks:
- Would you rate yourself as partially or totally dependent?
- How is the task achieved (by family, friend, agency, or use of specialized equipment)?
Activity tolerance
• What types of activities make you tired?
• Do you ever experience dizziness, shortness of breath, marked increase in respiratory rate, or other problems following mild or moderate activity?
Exercise
• What type of exercise do you carry out to enhance your physical fitness?
• What is the frequency and length of this exercise session?
• Do you believe exercise is beneficial to your health? Explain.
Factors affecting mobility
• Environmental factors: Do stairs, lack of railings or other assistive devices, or an unsafe neighborhood impede your mobility or exercise regimen?
• Health problems: Do any of the following health problems affect your muscle strength or endurance: heart disease, lung disease, stroke, cancer, neuromuscular problems, musculoskeletal problems, visual or mental impairments, trauma, or pain?
• Financial factors: Are your finances adequate to obtain equipment or other aids that you require to enhance your mobility?
PHYSICAL EXAMINATION
Conduct the physical examination focusing on activity and exercise patterns
1. Body Alignment
Identify posture variations, learning needs, and factors causing poor posture.
Assessment:
- Inspect client standing from anterior, posterior, and lateral views.
- Normal findings:
- Shoulders and hips level
- Toes point forward
- Spine straight
- Abnormal findings:
- Slumped posture- neck flexed forward, abdomen protruding, pelvis thrust forward (lordosis), hyperextended knees - leads to fatigue and low back pain.
Contributing Factors: Fatigue, pain, compression fractures, muscle weakness, poor self-esteem.
2. Gait
Determine mobility and fall risk.
Normal Gait:
- Two phases: Stance (weight-bearing) and Swing (leg moves forward).
- Features:
- Chin level, gaze straight ahead
- Heel strikes ground before toe
- Feet dorsiflexed during swing phase
- Arms move opposite to legs
- Movement smooth, rhythmic, and coordinated
Normal pace:
- Adults: 70–100 steps/minute
- Older adults: ~40 steps/minute
Assess with/without assistive devices (e.g., cane, walker).
3. Appearance and Movement of Joints
Examine: Inspection, palpation, active/passive range of motion (ROM).
Assess for:
- Swelling, redness - inflammation/injury
- Deformities (bony enlargement, contractures)
- Symmetry of involvement and muscle development
- Tenderness or crepitation (crackling sound)
- Increased temperature (compare bilaterally)
- Degree of movement (use goniometer if indicated)
Precautions:
- Move joints smoothly, slowly, and rhythmically—never force.
4. Capabilities and Limitations for Movement
Assess for:
- Effects of illness or devices (IV lines, casts)
- Mental alertness, ability to follow directions
- Medication effects (narcotics, sedatives, antihistamines)
- Balance and coordination
- Orthostatic hypotension: Dizziness, BP drop, tachycardia on standing
- Pain (may need analgesic before movement)
- Vision (adequacy for safe ambulation)
Evaluate assistance needs for:
- Turning in bed
- Moving from supine - sitting or standing
- Rising from chair
- Maintaining balance and posture while walking or standing
5. Muscle Mass and Strength
Determine readiness for movement or ambulation and prevent injury.
Assess:
- Upper and lower extremity strength (important for using crutches/walkers)
- Compare muscle size and tone bilaterally
Nursing Consideration: Provide assistance as needed to prevent strain or falls.
6. Activity Tolerance
Determine client’s strength and endurance for daily activities.
Assess in clients who are:
- Cardiopulmonary compromised
- Immobilized long-term
- Experiencing muscle wasting, pain, fatigue, or depression
Monitor:
- Heart rate, respiratory rate, rhythm, blood pressure
- At four intervals:
- Before activity (baseline)
- During activity
- Immediately after
- 3 minutes post-activity (recovery)
Stop activity if:
- Facial pallor, dizziness, weakness
- Change in consciousness
- Marked increase in HR or RR
- Irregular rhythm
- Dyspnea or chest pain
- Diastolic BP change ≥ 10 mmHg
Normal recovery: HR returns to baseline within 5 minutes.
7. Problems Related to Immobility
Assessment Methods: Inspection, palpation, auscultation, lab results, body weight, fluid intake/output.
Importance:
- Establish baseline data early for comparison.
- Identify at-risk clients early to prevent complications.
At-Risk Clients:
- Poorly nourished
- Decreased pain/pressure sensation
- Cardiovascular, pulmonary, or neuromuscular issues
- Altered level of consciousness
Common Complications: Pressure injuries, contractures, DVT, pneumonia, constipation, urinary stasis.
4.2 DIAGNOSING
NANDA International includes the following nursing diagnostic labels for activity and exercise problems:
• Activity Intolerance: insufficient physiological or psychological energy to endure or complete required or desired daily activities. Wilkinson suggests specifying the level of endurance. Levels include:
Level I: Walks regular pace on level ground but becomes more short of breath than normal when climbing one or more flights of stairs.
Level II: Walks one city block or 500 feet on level ground or climbs one flight of stairs slowly without stopping.
Level III: Walks no more than 50 feet on level ground without stopping and is unable to climb one flight of stairs without stopping.
Level IV: Dyspnea and fatigue at rest.
• Risk for Activity Intolerance: vulnerable to experiencing insufficient physiological or psychological energy to endure or complete required or desired daily activities, which may compromise health.
• Impaired Physical Mobility: limitation in independent, purposeful physical movement of the body or of one or more extremities. More specific versions of this diagnosis are
- Impaired Bed Mobility
- Impaired Transfer Ability
- Impaired Walking Impaired
- Wheelchair Mobility
- Impaired Sitting
• Sedentary Lifestyle: reports a habit of life that is characterized by a low physical activity level.
• Risk for Disuse Syndrome: vulnerable to deterioration of body systems as the result of prescribed or unavoidable musculoskeletal inactivity, which may compromise health
Depending on the data obtained, problems with mobility often affect other areas of human functioning and indicate other diagnoses. In these instances, the mobility problem becomes the etiology. The etiology needs to be described more explicitly in terms such as reduced ROM, neuromuscular impairment or musculoskeletal impairment of upper and lower extremities, or joint pain. Examples in which Impaired Physical Mobility is the etiology follow:
- Fear (of falling)
- Ineffective Coping
- Situational Low Self-Esteem
- Powerlessness
- Risk for Falls.
When problems associated with prolonged immobility arise, many other diagnoses may be necessary. Examples include, but are not limited to, the following:
• Ineffective Airway Clearance if there is stasis of pulmonary secretions
• Risk for Infection if there is stasis of urinary or pulmonary secretions
• Risk for Injury if orthostatic hypotension is present
• Disturbed Sleep Pattern if there is a lack of daytime physical activity
• Risk for Situational Low Self-Esteem if there is functional impairment and/or role disturbance.
4.3 PLANNING
To promote safe mobility, maintain independence, and prevent complications of immobility through individualized nursing goals and interventions.
Nursing Outcomes Classification (NOC)
Helpful NOC labels for planning care include:
- Activity tolerance
- Ambulation
- Balance
- Body positioning
- Coordinated movement
- Endurance
- Fall prevention behavior
- Fatigue level
- Immobility consequences (physiological & psycho-cognitive)
- Joint movement
- Mobility
- Physical fitness
- Play participation
- Self-care
Nursing Responsibilities
- Positioning, transferring, and ambulating clients are usually independent nursing functions.
- Primary care practitioner prescribes activity restrictions or specific positions after surgery, anesthesia, or musculoskeletal/neurologic trauma.
- Every client must have a written activity order upon admission.
Nursing Considerations in Planning
- Identify clients needing assistance with body alignment or movement.
- Determine the degree of assistance required.
- Encourage maximum independence while ensuring safety.
- Provide guidance and education on proper body mechanics and safe movement.
Overall Client Goals
The client will:
- Demonstrate increased tolerance for physical activity.
- Have restored or improved ambulation and ability to perform ADLs.
- Remain free from injury related to falls or improper body mechanics.
- Show enhanced physical fitness.
- Remain free from complications associated with immobility.
Planning for Home Care
For clients discharged with mobility or activity problems:
Nurse should:
- Assess actual and potential health problems, strengths, and available resources.
- Conduct a Home Care Assessment to identify environmental and physical barriers.
- Develop a discharge plan addressing:
- Mobility limitations
- Required assistive devices
- Support systems
- Instructional needs for client and family (safe ambulation, transfers, exercises).
Teaching focus: Safe movement, prevention of falls, maintaining mobility, and proper body mechanics.
4.4 IMPLEMENTING
Nurses can initiate and apply a wide variety of exercise and activity interventions as needed to address a multitude of client concerns.
Nursing strategies to maintain or promote body alignment and mobility involve:
- positioning clients appropriately
- moving and turning clients in bed
- transferring clients
- providing ROM exercises
- ambulating clients with or without mechanical aids
- strategies to prevent the complications of immobility
Whenever positioning, moving, and ambulating clients, nurses must use proper body mechanics and assistive lifting/moving equipment to avoid musculoskeletal strain and injury.
Using Body Mechanics
Body mechanics is the term used to describe the efficient, coordinated, and safe use of the body to move objects and carry out the ADLs.
When a person moves, the center of gravity shifts continuously in the direction of the moving body parts. Balance depends on the interrelationship of the center of gravity, the line of gravity, and the base of support.
The closer the line of gravity is to the center of the base of support, the greater the person’s stability.
Conversely, the closer the line of gravity is to the edge of the base of support, the more precarious the balance. If the line of gravity falls outside the base of support, the person falls.
Body balance, therefore, can be greatly enhanced by
-
- widening the base of support
- lowering the center of gravity, bringing it closer to the base of support.
The base of support is easily widened by spreading the feet farther apart. The center of gravity is readily lowered by flexing the hips and knees until a squatting position is achieved.
Manually moving and lifting clients often cause musculoskeletal disorders (MSDs).
This limit should be further reduced if the health care worker is lifting in a restricted space, sitting or kneeling, twisting, one-handed, or with arms extended; if working longer than 8 hours; or if the client is combative, cannot follow direction, or has physical or medical conditions that impact his or her being lifted or moved.
If the weight to be lifted exceeds 35 pounds or the other conditions exist, assistive devices should be used.
Lifting: It is important to remember that nurses should not lift more than 35 pounds without assistance from proper equipment and/or other individuals.
Types of assistive equipment include mobile-powered or mechanical lifts, ceiling-mounted lifts, sit-to-stand powered lifts, friction-reducing devices, and transfer chairs.
Pulling and Pushing: When pulling or pushing an object, a person maintains balance with least effort when the base of support is increased in the direction in which the movement is to be produced or opposed.
When pulling an object, a person can enlarge the base of support by
(a) moving the rear leg back if the person is facing the object
(b) moving the front foot forward if the person is facing away from the object
Preventing Back Injury
Nurses provide clients with the opportunity to change positions, expand their lungs, or change their environments as appropriate.
Two movements to avoid because of their potential for causing back injury are twisting (rotation) of the thoracolumbar spine and acute flexion of the back with hips and knees straight (stooping).
- Understand that the use of body mechanics will not necessarily prevent injury if manually handling a load greater than 35 pounds without the use of assistive devices.
- Avoid lifting anything greater than 35 pounds. Use assistive equipment, get help from coworkers, and participate in the purchasing/ordering process of appropriate assistive equipment for your work setting.
- Become consciously aware of your posture and body mechanics.
- When standing for a period of time, periodically move legs and hips, and flex one hip and knee and rest your foot on an object if possible.
- When sitting, keep your knees slightly higher than your hips.
- Use a firm mattress and soft pillow that provide good body support at natural body curvatures.
- Exercise regularly to maintain overall physical condition and regulate weight; include exercises that strengthen the pelvic, abdominal, and spinal muscles.
- Avoid movements that cause pain or require spinal flexion with straight legs (e.g., toe-touching and sit-ups) or spinal rotation (twisting).
- When moving an object, spread your feet apart to provide a wide base of support.
- Wear comfortable low-heeled shoes that provide good foot support and reduce the risk of slipping, stumbling, or turning your ankle.
Positioning clients
Purpose of Positioning
- To maintain good body alignment, comfort, and safety.
- To prevent complications such as:
- Pressure ulcers
- Contractures
- Nerve and vessel damage
- Muscle discomfort
- To promote circulation, muscle tone, and postural reflexes.
Frequency of Position Changes
- Clients should be repositioned at least every 2 hours, day and night.
- More frequent repositioning is required if there is a risk of skin breakdown.
Clients Requiring Assistance
- Independent clients: Reposition themselves; need minimal guidance.
- Dependent clients: Weak, frail, paralyzed, in pain, or unconscious — rely entirely on nurses for repositioning.
- Best practice: Use two or more nurses and assistive devices to prevent injury and maintain client dignity.
Key Nursing Responsibilities
Before and After Positioning
Assess skin for redness, breakdown, or irritation. Provide skin care and ensure dryness. Check for comfort and adjust support as needed.
During Positioning
Maintain proper alignment and joint support. Ensure mattress is firm and supportive: Avoid sagging or overly soft surfaces and use bed boards for clients with back issues. Keep bed linens clean, dry, and wrinkle-free. Ensure freedom of movement (loosen top bedclothes). Use support devices (pillows, wedges, trochanter rolls) only as needed to: Maintain alignment, Relieve pressure and Prevent strain or deformity.
Avoid:
-
- Placing bony prominences directly over each other
- Pressure on areas like the popliteal space
- Friction (rubbing between skin and sheets)
- Shearing forces (skin stationary while deep tissues slide, especially when semi-sitting)
Preventing Friction and Shearing
- Friction: Caused by rubbing of sheets or rough surfaces - skin abrasion.
- Shearing: Combination of friction and pressure; occurs when the client slides downward in bed - damages deep tissues, especially over the sacrum.
- Prevention:
- Lift, don’t drag, during repositioning.
- Use draw sheets or sliding boards.
- Keep head of bed at lowest elevation possible to prevent sliding.
Client-Centered Positioning
Always ask the client which position feels most comfortable. Combine visual alignment with client feedback to ensure both comfort and correct positioning. Document preferred positions and effectiveness of alignment techniques.
|
Position |
Description |
Angle of Elevation / Body Alignment |
Uses / Indications |
Precautions / Disadvantages |
|
Fowler’s Position
|
Semisitting position with head and trunk raised. |
Head and trunk raised 45°–60°; knees may or may not be flexed. |
- Facilitates breathing and chest expansion. - Beneficial for clients with respiratory or cardiac problems. |
- Avoid excessive pillows behind the head (risk of neck flexion contractures). - Encourage occasional rest without pillow to maintain neck extension. |
|
Semi-Fowler’s (Low Fowler’s) |
Mild elevation of head and trunk. |
15°–45°, typically 30°. |
- Common resting position. - Used in tube feeding and for postoperative comfort. |
- May still allow some risk of aspiration if head not elevated adequately. |
|
High-Fowler’s |
Nearly upright sitting position. |
60°–90° (often 90°). |
- Promotes maximum lung expansion. - Used for severe respiratory distress, swallowing, and eating. |
- May cause pressure on sacrum and buttocks; use pillows or cushions. |
|
Orthopneic Position
|
Client sits upright, leaning forward on an overbed table. |
Sitting upright with overbed table supporting arms. |
- Facilitates maximum chest expansion. - Used for clients with difficulty exhaling (e.g., COPD, asthma). |
- May not be tolerated for long; requires good trunk strength to maintain. |
|
Dorsal Recumbent (Back-Lying)
|
Head and shoulders slightly elevated. |
Supine with small pillow under head and shoulders. |
- Provides comfort and relaxation. - Used post-surgery (esp. spinal or after anesthesia). |
- Risk of pressure on sacrum and heels if maintained long.- Not same as flat supine position. |
|
Prone Position
|
Client lies on abdomen, head to one side. |
Flat, hips not flexed. |
- Promotes hip and knee extension. - Prevents flexion contractures. - Promotes oral drainage (e.g., post mouth/throat surgery). |
- Not suitable for spinal, cardiac, or respiratory problems. - May cause lordosis, neck strain, and plantar flexion. - Use for short periods only. |
|
Lateral (Side-Lying) Position
|
Client lies on one side with top leg flexed and in front. |
One side of body; top hip and knee flexed. |
- Relieves pressure on sacrum and heels. - Promotes good spinal alignment.- Comfortable for sleeping and resting. |
- Requires frequent turning to prevent pressure injuries. - Support pillows may be needed for alignment. |
|
Sims’ (Semiprone) Position
|
Halfway between lateral and prone. |
Lower arm behind body; upper arm flexed; both legs flexed (upper leg more). |
- Facilitates oral drainage and prevents aspiration. - Used for unconscious or paralyzed clients, enemas, rectal exams, and pregnancy comfort. |
- May cause pressure on humerus and clavicle on dependent side. - Must ensure proper limb support. |
4.4 IMPLEMENTING (CONTINUED)
Moving and Turning Clients in Bed
Ill or immobile clients often need assistance to move in bed. Nurses must balance client independence with safety, maintain correct body alignment, and use proper techniques and assistive devices to prevent injury to both client and caregiver.
- Assess the client’s ability to move and assist before performing any repositioning.
- Maintain proper body alignment to prevent strain on the musculoskeletal system.
- Use assistive devices and adequate staff to ensure safety.
- Promote client comfort, privacy, and dignity during all movements.
- Follow agency policy on the use of mechanical lifts and assistance requirements.
Assistive Equipment
- Hydraulic lifts: Used for transfers between bed, wheelchair, stretcher, or bathtub.
- Friction-reducing devices: Minimize skin shear during repositioning.
- Overhead trapeze: Allows partially mobile clients to assist in movement.
- Pillows and rolls: Maintain alignment and prevent pressure injuries.
Assessment Before Moving
Evaluate:
- Physical ability (muscle strength, paralysis)
- Cognitive ability and understanding of instructions
- Willingness to participate
- Degree of discomfort or pain (administer analgesia if needed)
- Weight and body size
- Effects of medications (e.g., those causing drowsiness or hypotension)
- Presence of lines, catheters, or drains
- Risk of orthostatic hypotension
Planning
- Review previous records for mobility limitations.
- Gather assistive devices and required personnel.
- Explain the procedure clearly to the client and family.
- Provide privacy and perform hand hygiene.
- Adjust bed height and lock wheels before starting.
Body Mechanics for Nurses
- Face the direction of movement to avoid twisting.
- Use a wide stance for stability.
- Flex hips, knees, and ankles to lower center of gravity.
- Engage core muscles before movement.
- Rock body weight (front to back or back to front) to move smoothly.
SKILL: Moving a Client Up in Bed
Purpose: Reposition clients who have slid down in bed or to promote comfort and alignment.
Implementation:
- Flatten the bed as tolerated and remove pillows.
- Protect the head with a pillow against the bed frame.
- Use appropriate devices and assistance based on client’s weight:
- <200 lb: Friction-reducing sheet + 2 assistants.
- 201–300 lb: Slide sheet + 4 assistants or air transfer + 2 assistants.
- 300 lb: Air transfer system or total lift.
- Encourage client to flex knees, push with feet, and assist as able.
- Move client smoothly on count of three using proper body mechanics.
- Reposition and support client comfortably, raise head of bed if indicated.
Documentation:
- Time and new position
- Pressure areas noted
- Devices used
- Client’s ability to assist
- Client response (comfort, dizziness, anxiety)
SKILL: Turning a Client (Lateral or Prone Position)
Purpose: For repositioning, pressure relief, linen changes, or procedures (e.g., placing a bedpan).
Preparation:
- Check for IV lines, catheters, and mobility aids.
- Use assistive devices or mechanical lifts if needed.
- Ensure two or more caregivers for safety.
Performance Steps:
- Explain procedure, perform hand hygiene, and ensure privacy.
- Flatten bed, lock wheels, and raise bed to working height.
- Move client toward opposite edge of bed to prevent falling off after turning.
- Cross client’s near leg over the far leg and position near arm across the chest.
- Slightly abduct far shoulder to prevent it from being trapped.
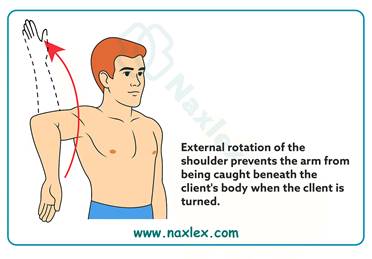
- With one hand on shoulder and the other on hip, roll client toward you.
- Support head and limbs with pillows.
- For prone position, keep the far arm alongside the body before turning.
- Avoid pulling client once prone to prevent injury to breasts or genitals.
Documentation:
- Positions changed from/to
- Skin condition and pressure areas
- Client’s ability to assist
- Response to repositioning
- Use of support devices
Delegation
- Moving and turning clients can be delegated to Unlicensed Assistive Personnel (UAP) if the nurse:
- Assesses the client first.
- Ensures necessary equipment and assistance are available.
- Instructs UAP to report changes in condition (e.g., pain, dizziness, weakness).
Evaluation
After moving:
- Assess comfort, pain, dizziness, anxiety
- Check body alignment and vital signs (if needed)
- Verify safety measures (side rails up, call light within reach)
Safety Tips
- Never lift more than 35 lb of a client’s weight—use assistive devices.
- Always lock wheels on the bed and equipment.
- Maintain client privacy and dignity.
- Avoid twisting the spine or overreaching.
- Ensure communication and coordination among assisting personnel.
NURSING INSIGHTS: Positioning, Moving, and Turning Clients
INFANTS
• Position infants on their back for sleep, even after feeding. There is little risk of regurgitation and choking, and the rate of sudden infant death syndrome (SIDS) is significantly lower in infants who sleep on their backs.
• The skin of newborns can be fragile and may be abraded or torn (sheared) if the infant is pulled across a bed.
CHILDREN
• Carefully inspect the dependent skin surfaces of all infants and children confined to bed at least three times in each 24-hour period.
OLDER ADULTS
• In clients who have had cerebrovascular accidents (strokes), there is a risk of shoulder displacement on the paralyzed side from improper moving or repositioning techniques. Use care when moving, positioning in bed, and transferring. Pillows or foam devices are helpful to support the affected arm and shoulder and prevent injury.
• Decreased subcutaneous fat and thinning of the skin place older adults at risk for skin breakdown. Repositioning approximately every 2 hours (more or less, depending on the unique needs of the individual client) helps reduce pressure on bony prominences and avoid tissue trauma.
Using Mechanical Aids for Walking
Mechanical aids for ambulation include canes, walkers, and crutches. These devices help clients with impaired mobility maintain balance, stability, and independence.
1. Canes
Types
- Standard cane: Single straight leg.
- Tripod cane: Three feet for increased support.
- Quad cane: Four feet; provides the greatest stability.
Features:
Rubber tips prevent slipping. Standard cane length ≈ 91 cm (36 in); adjustable aluminum canes: 56–97 cm (22–38 in). Elbow should be slightly flexed when the cane is in use.
How to Use a Cane
- Hold the cane on the stronger side of the body.
- Place the cane tip 15 cm (6 in) to the side and in front of the near foot.
When maximum support is required:
- Move cane forward about 30 cm (1 ft).
- Move weaker leg forward to the cane (weight on cane + strong leg).
- Move stronger leg forward past cane and weak leg.
- Repeat sequence.
When less support is needed:
- Move cane and weak leg together.
- Move strong leg forward (weight on cane and weak leg).
2. Walkers
Types
- Standard walker: Four rubber-tipped legs; must be lifted to move. The standard walker needs to be picked up to be used. The client therefore requires partial strength in both hands and wrists, strong elbow extensors, and strong shoulder depressors. The client also needs the ability to bear at least partial weight on both legs.
- Two-wheeled walker: Two legs with wheels and two without; offers more stability than four-wheeled models.
- Four-wheeled (roller) walker: Easier to move; includes hand brakes and often a seat; less stable.
Height Adjustment:
- Hand bar should be just below the waist, elbows slightly flexed (~30°).
- Too low leads to stooping; too high leads to shoulder strain.
How to Use a Walker
For maximum support:
- Move walker ahead ~15 cm (6 in).
- Move right foot up to walker (weight on left leg + arms).
- Move left foot up to meet right foot.
If one leg is weak:
- Move walker and weak leg together about 15 cm (6 in).
- Move stronger leg ahead (weight on arms + weak leg).
Note: When educating clients about the use of walkers, inform them that when transferring from chair or commode, they should back the walker to the chair or toilet seat and use arms of chair or commode to assist in sitting and standing. Teach clients to always use both hands when using a walker to transfer from standing to sitting
3. Crutches
Types
- Axillary (underarm) crutch: Most common; used for temporary needs.
- Lofstrand (forearm) crutch: Has a cuff around the forearm for wrist stability.
- Platform crutch: Allows forearm weight bearing for clients unable to bear weight on hands.
All crutches need rubber suction tips for traction.
Measuring for Crutches
- Supine method: Measure from anterior axillary fold to heel; add 2.5 cm (1 in).
- Standing method: Shoulder rest should be 2.5–5 cm (1–2 in) below axilla (≈ three finger widths).
- Handgrip height: When standing, elbows should flex about 30°.
- Body weight should be borne by hands, not the axillae, to prevent radial nerve injury (crutch palsy).
Crutch Gaits
|
Gait |
Description |
Requirements |
|
Four-point |
Right crutch → left foot → left crutch → right foot. Always 3 points of contact. |
Weight-bearing on both legs; safe and stable. |
|
Three-point |
Both crutches + weak leg → strong leg. |
Full weight-bearing on one leg only. |
|
Two-point |
Right crutch + left foot → left crutch + right foot. |
Partial weight-bearing on each foot; faster gait. |
|
Swing-to |
Move both crutches forward → swing body to crutches. |
Used by clients with leg paralysis. |
|
Swing-through |
Move both crutches forward → swing body past crutches. |
Requires strength and coordination. |
Tripod (Crutch) Stance
Crutches placed 15 cm (6 in.) in front and to the sides of feet. Feet slightly apart; head and back erect; weight on hands, not axillae. Provides wide base of support. Use a gait belt for safety during training.
Sitting and Standing with Crutches
Getting into a chair:
- Stand with back of unaffected leg centered against chair.
- Transfer both crutches to affected side and hold by hand bars.
- Hold chair arm with unaffected hand, lean forward, and sit down slowly.

Getting out of a chair:
- Move to edge; place unaffected leg under chair edge.
- Hold crutches in affected hand, chair arm with unaffected hand.
- Push up using both arms and unaffected leg, then assume tripod stance.
Using Crutches on Stairs
Going up stairs:
- Assume tripod position.
- Move strong leg up first.
- Move crutches and weak leg up to the same step.
- Repeat.
(Strong leg goes up first.)
Going down stairs:
- Assume tripod position.
- Move crutches and weak leg down first.
- Move strong leg down to the same step.
- Repeat.
(Weak leg goes down first.)
Transferring clients
Transferring clients means safely moving them between surfaces — such as from bed to chair, wheelchair, commode, or stretcher. The nurse must assess the client’s physical and mental ability, plan the transfer carefully, and ensure safety throughout the procedure.
Assistive devices include:
- Gait/transfer belts
- Sliding or transfer boards
- Friction-reducing devices (slide sheets, air transfer systems)
- Mechanical lifts
Key Assessment Before Transfer
Assess the client’s:
- Body size and weight
- Muscle strength and joint mobility
- Ability to bear weight and pivot
- Balance and activity tolerance
- Ability to follow instructions and cooperate
- Presence of pain, paralysis, or orthostatic hypotension
- Environment – available space, obstacles, and equipment condition
Planning
Review previous notes for client’s transfer ability. Administer pain medication before transfer if needed. Determine:
-
- The number of assistants required.
- Equipment needed (belt, slide sheet, lift, wheelchair, etc.).
- Client’s participation level.
Remove obstacles and ensure enough space. Assign one person to give commands during the transfer. Explain the procedure to both client and staff.
Gait/Transfer Belts
Used to control client movement during transfers or ambulation. Best for: Clients who can bear some weight and need minimal assistance.
Avoid using on:
-
- Clients requiring full lifting.
- Bariatric clients.
- Clients at high fall risk.
Do not use to lift clients from the floor.
- Belt should be snug around waist; use handles if available.
Sliding/Transfer Boards
Made of low-friction material; used between bed and chair. Suitable for clients who can sit upright and have upper-body strength. Client may self-transfer or be gently pushed/pulled using a slide sheet. Promotes independence and energy conservation for nurses.
General Transfer Guidelines
- Support the client, not the equipment.
- Provide privacy and use proper body mechanics (bend knees, straight back).
- Use step-by-step instructions to guide client movements.
- Lock wheels on beds, wheelchairs, and stretchers.
- Never leave clients unattended on stretchers or wheelchairs without brakes, straps, or side rails engaged.
- Always push a stretcher from the head end for safety.
SKILL: Transferring Between Bed and Chair/Wheelchair
Purpose
To assist clients in safely moving between bed, wheelchair, commode, or toilet.
Steps
- Preparation: Lock bed and wheelchair wheels. Place wheelchair parallel to the bed, on the client’s stronger side. Raise footplates and remove armrests if necessary.
- Assist Client: Help client sit on edge of bed; check for orthostatic hypotension. Ensure feet flat on floor and nonskid shoes/slippers worn. Place gait belt securely.
- Client Instructions: Lean forward slightly from hips. Strong leg under bed edge, weaker leg forward. Place hands on bed, not on nurse’s neck, for pushing.
- Nurse Positioning: Stand in front and slightly to weak side. Hold gait belt and support client’s shoulder. Flex knees and hips; keep a broad stance. Brace client’s knees/feet to prevent slipping.
- Standing and Pivoting: On cue (“1–2–3, stand”), client pushes down while nurse transfers weight and assists to standing. Allow time for stability, then pivot or take steps toward chair.
- Sitting: Have client feel chair with legs, then reach for armrests. Slowly lower client by bending knees and hips. Ensure client sits well back for stability. Replace footplates and remove belt.
Variations
- Two-nurse transfer: One on each side holding belt and elbows.
- Injured leg: Transfer toward strong side.
- Slide board: Use for clients unable to stand but able to use upper body.
Documentation
- Client’s ability to bear weight/pivot.
- Number of staff and devices used.
- Duration and tolerance of sitting up.
- Response to transfer and safety measures.
SKILL: Transferring Between Bed and Stretcher
Purpose
For moving supine clients between surfaces (e.g., bed to stretcher).
Assistive Devices
- Slide sheet, lateral transfer board, or air transfer system.
- Weight-based staffing recommendations:
- < 200 lb: 2 caregivers + friction-reducing device.
- 201–300 lb: 4 caregivers or air transfer system.
- 300 lb: 2 caregivers + ceiling lift or air system.
Steps
- Preparation: Lower bed head and adjust height slightly higher than stretcher. Place friction-reducing device under client. Position stretcher parallel to bed and lock wheels. Fill gap with blankets if needed.
- Transfer: If independent, let client lift or roll over. If dependent: Caregiver at bed pushes; others pull client using sheet or board. Client’s arms crossed and neck flexed to prevent injury. Use planned verbal cue to coordinate motion.
- After Transfer: Raise side rails and/or fasten safety straps. Unlock wheels and move stretcher away safely.
- Variation- Transfer Board: Smooth board (45–55 cm × 182 cm) with handholds. Roll client laterally, insert board, then slide across. Apply safety belts over chest, abdomen, and legs.
Documentation
- Equipment used.
- Number of staff.
- Safety measures (locked wheels, belts, side rails).
- Destination and reason for transfer.
Providing range of motion (ROM) exercises
Purpose: To maintain joint mobility, prevent contractures and stiffness, and promote circulation in clients with restricted activity or immobility. Helps preserve muscle tone and joint flexibility when clients cannot move independently.
Types of ROM Exercises
|
Type |
Description |
Who Performs It |
Purpose/Benefit |
|
Active ROM (AROM) |
Client independently moves each joint through full range |
Client |
Maintains muscle strength, endurance, and joint flexibility; promotes circulation and cardiorespiratory function |
|
Passive ROM (PROM) |
Another person moves the client’s joints through full range |
Nurse or caregiver |
Maintains joint flexibility and prevents contractures (does not build muscle strength) |
|
Active-Assistive ROM (AAROM) |
Client uses stronger limb to move weaker limb; nurse assists to complete motion |
Client + nurse |
Improves mobility and flexibility, especially useful for stroke or hemiplegic clients |
General Guidelines
- Perform ROM to the point of slight resistance, never pain.
- Movements should be smooth, slow, and rhythmic, avoiding jerky or forceful motion.
- Use the same sequence for every session to ensure consistency.
- Perform 3–5 repetitions for each movement, twice daily (e.g., during bathing).
- Support the joint above and below during movement to prevent strain or injury.
- Encourage client participation whenever possible.
For Active ROM
- Teach client the purpose and correct technique.
- Perform movements systematically in the same order each session.
- Each exercise should be done 3 times, twice daily.
- Stop if pain or discomfort occurs.
Older adults: Focus on maintaining ROM sufficient for Activities of Daily Living (ADLs) (e.g., dressing, bathing, walking). Full ROM in all joints is not necessary.
For Passive ROM
- Explain purpose and obtain cooperation.
- Ensure rings are removed to prevent swelling or injury.
- Client should wear a loose gown, covered with a bath blanket for warmth and privacy.
- Use correct body mechanics to avoid self-injury.
- Expose only the limb being exercised.
- Support joints with hands or forearms; never pull on a limb.
- If spasticity occurs: pause, apply gentle pressure until muscle relaxes, then continue.
- If rigidity occurs: apply slow, steady pressure and continue gently.
- Avoid hyperextension, especially in arthritic joints.
- Assess skin condition during exercises.
For Active-Assistive ROM
- Client uses stronger limb to assist weaker limb.
- Nurse completes movement to full range if client fatigues.
- Especially useful for clients recovering from stroke or hemiplegia.
- Enhances coordination, independence, and self-care ability.
Safety & Evaluation
- Monitor client’s tolerance, pain level, and muscle tone.
- Document:
- Type of ROM performed
- Client’s participation and tolerance
- Joints exercised
- Any discomfort or complications observed
4.5 EVALUATING
The goals established during the planning phase are evaluated according to specific desired outcomes, also established in that phase.
If outcomes are not achieved, the nurse, client, and support person if appropriate need to explore the reasons before modifying the care plan.
For example, the following questions may be considered if an immobilized client fails to maintain muscle mass and tone and joint mobility:
- Has the client’s physical or mental condition changed motivation to perform required exercise?
- Were appropriate range-of-motion exercises implemented?
- Was the client encouraged to participate in self-care activities as much as possible?
- Was the client encouraged to make as many decisions as possible when developing a daily activity plan and to express concerns?
- Did the nurse provide appropriate supervision and monitoring?
- Was the client’s diet adequate to provide appropriate nourishment for energy requirements?
Summary
- Exercise and activity are essential components for maintaining and regaining health and wellness.
- Purposeful coordinated movement of the body relies on the integrated functioning of the musculoskeletal system, the nervous system, and the vestibular apparatus of the inner ear.
- People maintain alignment and balance when the line of gravity passes through the center of gravity and the base of support.
- Exercise is classified as either isotonic, isometric, or isokinetic and as either aerobic or anaerobic.
- Immobility affects almost every body organ and system adversely.
- An activity and exercise history includes daily activity level, activity tolerance, type and frequency of exercise, and factors affecting mobility.
- Positioning a client in good body alignment and changing the position regularly and systematically are essential aspects of nursing practice.
- Before moving, turning, or transferring a client, the nurse must consider the client’s health status and degree of exertion permitted, physical ability to assist, ability to comprehend instruction, degree of discomfort, client’s weight, and whether to use assistive devices or another caregiver to assist.
- Clients need specific instructions about appropriate use of canes, walkers, and crutches.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Mobility
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now