Please set your exam date
Bowel elimination
Study Questions
Practice Exercise 1
Clients should be taught that repeatedly ignoring the sensation of needing to defecate could result in which of the following?
Explanation
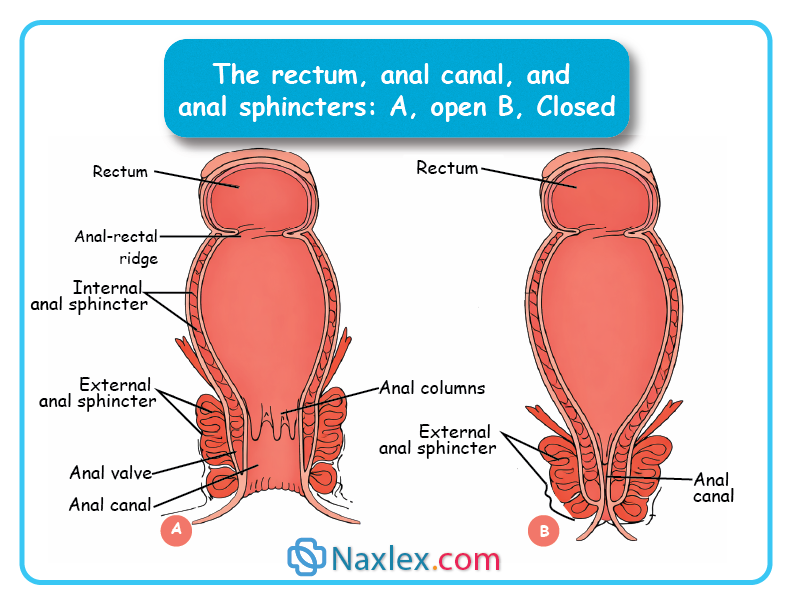
The defecation reflex is an involuntary response that controls the elimination of feces. When the rectum becomes distended by the accumulation of stool, stretch receptors in its walls are activated, sending signals to the spinal cord. This triggers contraction of the rectal muscles and relaxation of the internal anal sphincter, while the external anal sphincter remains under voluntary control. If conditions are appropriate, voluntary relaxation of the external sphincter and contraction of abdominal muscles allow defecation to occur.
Rationale for correct answer:
1. Constipation: If a person repeatedly ignores this urge, the stool remains in the colon longer than intended. Because one of the primary functions of the colon is to reabsorb water, the stool becomes increasingly dry, hard, and difficult to pass. Over time, the rectum can become desensitized to the presence of stool, leading to chronic constipation.
Rationale for incorrect answers:
2. Diarrhea: This is characterized by rapid movement of fecal contents through the large intestine, resulting in liquid stools. Ignoring the urge to defecate has the opposite effect - it slows transit time.
3. Incontinence: Fecal incontinence is the involuntary loss of bowel control. While chronic constipation can eventually lead to overflow incontinence (where liquid stool leaks around a hard mass), the direct, immediate result of ignoring the urge is the retention of stool, not the loss of control.
4. Hemorrhoids: While hemorrhoids are often a secondary result of constipation (due to straining to pass hard stool), the physiological process initiated by ignoring the urge is the hardening of stool, which is the definition of constipation. Constipation is the direct result; hemorrhoids are a potential complication of that result.
Test taking strategy:
- When a question asks for a result of a specific behavior, look for the most direct physiological consequence.
- While several options might seem related (like hemorrhoids), ask yourself: “What happens first inside the body?” The immediate internal change is the drying of the stool, which defines constipation.
Take home points:
- The longer stool sits in the large intestine, the more water is removed.
- Voluntary suppression of the urge to defecate is a leading behavioral cause of hard, dry stools.
A nurse is assessing a client with epigastric pain. Which of the following is most likely to validate that the client is experiencing intestinal bleeding?
Explanation
Gastrointestinal (GI) bleeding refers to any bleeding that occurs within the digestive tract, ranging from the esophagus to the rectum. It can present as hematemesis, hematochezia or melena, or be occult and detected only through testing. Causes include peptic ulcers, gastritis, esophageal varices, diverticulosis, hemorrhoids, inflammatory bowel disease, and malignancies.
Rationale for correct answer:
3. Semisoft black-colored stools: Black, tarry stools known as melena indicate bleeding from the upper GI tract (esophagus, stomach, or duodenum). The dark color results from the hemoglobin being partially digested by stomach acid and enzymes as it travels through the intestines.
Rationale for incorrect answers:
1. Large quantities of fat mixed with pale yellow liquid stool: This describes steatorrhea, which is associated with malabsorption syndromes like celiac disease or cystic fibrosis or gallbladder or pancreatic issues, but not typically active bleeding.
2. Brown, formed stools: This is the description of normal, healthy stool. The brown color comes from stercobilin, a bile derivative, and indicates no significant bleeding in the tract.
4. Narrow, pencil-shaped stool: Pencil-shaped stools are a red flag for a physical obstruction in the lower colon or rectum, such as a tumor or stricture, but they do not specifically validate active bleeding.
Test taking strategy:
- In nursing assessments, color changes in stool are highly specific.
- Associate black/tarry with upper GI bleed and clay/pale with bile obstruction.
- Since the question mentions epigastric pain (pain in the upper middle abdomen), you should look for the stool type associated with the upper tract: Melena.
Take home points:
- Melena (black/tarry): Usually indicates upper GI bleeding.
- Hematochezia (bright red): Usually indicates lower GI bleeding.
A nurse is conducting a staff education program on bowel elimination. Which of the following is a true statement about the effects of medication on bowel elimination?
Explanation
Medications can significantly influence bowel elimination, often leading to either constipation or diarrhea depending on their action. Drugs such as opioids, antidepressants, antihistamines, iron supplements, and certain blood pressure medications commonly slow intestinal motility, reduce fluid in the stool, and cause constipation. In contrast, antibiotics, laxatives, and some chemotherapy agents may irritate the bowel or alter gut flora, resulting in diarrhea.
Rationale for correct answer:
1. Diarrhea commonly occurs with amoxicillin clavulanate use: Antibiotics, particularly broad-spectrum ones like amoxicillin-clavulanate, disrupt the normal bacterial flora of the gut. This imbalance often leads to diarrhea and increases the risk for Clostridioides difficile infection.
Rationale for incorrect answers:
2. Anticoagulants cause a white discoloration of the stool: Anticoagulants like warfarin or heparin increase the risk of GI bleeding, which would cause the stool to appear pink, red, or tarry. White or clay-colored stools are caused by antacids or a lack of bile (biliary obstruction).
3. Narcotic analgesics increase gastrointestinal motility: Opioids/narcotics are notorious for decreasing motility by binding to receptors in the gut, leading to significant constipation.
4. Iron salts impair digestion and cause a green stool: While iron can cause GI upset, it characteristically causes the stool to turn black and tarry (which can be mistaken for melena) and often causes constipation.
Test taking strategy:
- Match the medication to its most well-known GI effect.
- Eliminate options with incorrect cause–effect relationships.
- Choose the option that reflects a common, expected side effect, not a rare one.
Take home points:
- Antibiotic-associated diarrhea is a primary safety concern for nurses because it can lead to dehydration and secondary infections.
- Drug-induced color changes:
- Iron/Bismuth – Black
- Antacids - White/Speckled
- Antibiotics - Green/Grey
- Anticoagulants - Red/Pink.
A client complains of excessive flatulence. When reviewing the client’s dietary intake, which food, if eaten regularly, would you identify as possibly responsible?
Explanation
Excessive flatulence refers to the frequent passage of gas from the digestive tract, often caused by swallowing air, consuming gas-producing foods, or underlying gastrointestinal issues. Common dietary triggers include beans, lentils, cabbage, onions, carbonated drinks, and high-fiber foods, which increase fermentation in the intestines. It can also result from lactose intolerance, irritable bowel syndrome, or imbalances in gut bacteria.
Rationale for correct answer:
2. Cauliflower: Cauliflower is a cruciferous vegetable. These vegetables contain a complex sugar called raffinose and high levels of fiber that the human body cannot fully digest. When bacteria in the large intestine break down these components, they produce gas - hydrogen, carbon dioxide, and methane as a byproduct.
Rationale for incorrect answers:
1. Meat: Protein-rich foods like meat are generally digested in the stomach and small intestine and are not primary triggers for gas, although they can contribute to the odor of gas due to sulfur content.
3. Potatoes: While potatoes contain starch, they are generally considered gas-friendly compared to other carbohydrates. Most of the starch in potatoes is digested easily, leaving little for the gas-producing bacteria in the colon.
4. Ice cream: While dairy can cause gas in individuals with lactose intolerance, it is not a universal gas-producer for the general population in the same way that high-fiber cruciferous vegetables are.
Test taking strategy:
When a question asks about gas or flatulence, look for cruciferous vegetables or legumes/beans. These are the classic gas-producers tested in nursing exams.
Take home points:
- Cruciferous vegetables (broccoli, cabbage, cauliflower), legumes (beans), and highly carbonated beverages are the most common dietary sources of flatulence.
- Flatulence is a normal byproduct of healthy bacteria fermenting undigested carbohydrates in the colon.
Practice Exercise 2
A client is scheduled for a colonoscopy. The nurse will provide information to the client about which type of enema?
Explanation
A colonoscopy is a diagnostic and sometimes therapeutic procedure used to examine the interior lining of the large intestine with a flexible, lighted tube called a colonoscope. It is commonly performed to investigate symptoms such as rectal bleeding, chronic diarrhea, abdominal pain, or changes in bowel habits, and is also used for routine screening for colorectal cancer. Preparation involves cleansing the bowel with special solutions to ensure clear visibility.
Rationale for correct answer:
4. Low, small-volume enemas often commercially prepared, e.g., Fleet enema are commonly prescribed before diagnostic procedures like colonoscopy to cleanse the bowel effectively and safely.
Rationale for incorrect answers:
1. Oil retention: These are used specifically to lubricate and soften a fecal impaction. They do not provide the washing action needed to clear the entire colon wall for a clear camera view.
2. Return flow: Also known as a Harris flush, these move 100–200 mL of fluid in and out of the rectum to stimulate the passing of gas (flatus). It is a localized treatment for distension, not a cleansing prep.
3. High, large-volume enemas are cleansing enemas but are not typically used before colonoscopy because they can be uncomfortable and less practical. Because of the risk of loss of fluid and electrolytes, high, large-volume enemas are seldom used
Test taking strategy:
- Identify the goal of care, not the most aggressive option. Colonoscopy prep - bowel cleansing with safety.
- Eliminate options with different purposes: Oil retention- stool softening, Return flow - gas relief
- Apply safety principles: High, large-volume enemas increase risk for fluid & electrolyte imbalance.
- Choose the option commonly used with bowel prep regimens- Low, small-volume enemas.
Take home points:
- Low, small-volume enemas are commonly used as part of colonoscopy preparation due to lower risk of fluid and electrolyte imbalance.
- High, large-volume enemas are rarely used today because of safety concerns, especially in older or medically vulnerable clients.
A client with a new stoma who has not had a bowel movement since surgery last week reports feeling nauseous. What is the appropriate nursing action?
Explanation
Complications of stomas can include both physical and psychosocial issues. Physically, clients may experience skin irritation or breakdown around the stoma due to leakage or poor appliance fit, as well as infection, bleeding, or ulceration. Mechanical problems such as stoma prolapse (protrusion), retraction (pulling inward), stenosis (narrowing), or parastomal hernia can interfere with normal function and appliance management.
Rationale for correct answer:
2. After assessing the stoma and surrounding skin, notify the surgeon: A client who is one-week post-op with no bowel movement and nausea is exhibiting classic signs of a postoperative ileus or a bowel obstruction. This is a potential surgical complication. The nurse must first perform a focused assessment (looking for stoma color and skin integrity) and then immediately notify the surgeon of the possible obstruction.
Rationale for incorrect answers:
1. Prepare to irrigate the colostomy: Irrigation is a procedure used to train a sigmoid colostomy or to treat constipation. It should never be done on a brand-new stoma without a specific surgeon's order, as it could cause trauma or perforation to the fresh surgical site.
3. Assess bowel sounds and administer antiemetic: While assessing bowel sounds is good, simply giving an antiemetic mask the symptoms of a serious complication (obstruction). You cannot treat the nausea without addressing the reason why the patient is nauseous.
4. Administer a bulk-forming laxative: Giving a laxative to a patient with a suspected bowel obstruction is dangerous. If there is a physical blockage, adding bulk and stimulating the gut can lead to increased pressure, pain, and potential bowel rupture.
Test taking strategy:
- If a patient is post-operative and presents with absent expected findings (no bowel movement) and new distressing symptoms (nausea), the answer usually involves assessing and then notifying the surgical team.
- Avoid independent interventions like laxatives or irrigation that could cause harm to a fresh surgical site.
Take home points:
- No stool output combined with nausea or vomiting in a post-surgical patient is a red flag for an ileus or obstruction.
- Always assess the stoma before calling the provider, so you can provide a complete SBAR report (color, swelling, skin condition).
A nurse is caring for a client with intestinal obstruction. During removal of a fecal impaction, which of the following could occur because of vagal stimulation?
Explanation
Fecal impaction is a severe form of constipation in which a large, hardened mass of stool becomes lodged in the rectum or colon, making natural elimination difficult or impossible. It often results from chronic constipation, prolonged laxative use, immobility, dehydration, or neurological conditions that impair bowel function.
Rationale for correct answer:
1. Bradycardia: The rectum is richly supplied with parasympathetic nerve endings. Digital stimulation during the removal of a fecal impaction can stimulate the vagus nerve. Because the vagus nerve exerts an inhibitory effect on the heart, overstimulation results in a sudden drop-in heart rate and potentially a drop in blood pressure (syncope).
Rationale for incorrect answers:
2. Atelectasis: This refers to the collapse of alveoli in the lungs. While it is a common postoperative complication due to shallow breathing, it is not physiologically linked to the stimulation of the vagus nerve in the rectum.
3. Tachycardia: This is an increased heart rate. Vagal stimulation produces the opposite effect (the parasympathetic response), which slows the heart rate down rather than speeding it up.
4. Cardiac tamponade: This is a life-threatening condition where fluid builds up in the pericardial sac, compressing the heart. It is typically caused by trauma or disease, not by digital rectal stimulation.
Test taking strategy:
Whenever you see vagal stimulation or Vagus nerve, remember its job is to slow things down. Look for the answer choice that describes a slowing of a vital sign-in this case, bradycardia.
Take home points:
- If a client becomes pale, diaphoretic, or complains of feeling faint during digital impaction removal, the procedure must be stopped immediately to assess the heart rate.
- Always check the client's baseline pulse and cardiac history before performing digital removal, as those with pre-existing heart conditions are at higher risk for vagal responses.
A nurse is caring for a client with fecal incontinence. Which nursing diagnoses are most applicable? Select all that apply
Explanation
Fecal incontinence is the involuntary loss of stool, ranging from occasional leakage to complete inability to control bowel movements. It often results from weakened anal sphincter muscles, nerve damage, or conditions that affect bowel function such as chronic diarrhea, constipation, or rectal surgery. Clients may experience embarrassment, social withdrawal, and skin irritation due to frequent soiling.
Rationale for correct answers:
1. Bowel Incontinence: This is the primary problem. Fecal incontinence is defined as the involuntary passage of stool, which directly supports this nursing diagnosis as the priority.
3. Disturbed Body Image: Incontinence is often viewed as a loss of a basic adult function. Clients may feel unclean or ashamed of their body's inability to control elimination, which significantly impacts their self-perception and body image.
4. Social Isolation: The fear of having an accident in public, combined with concerns about odors, often leads clients to stay home and avoid social gatherings, resulting in withdrawal and isolation.
5. Risk for Impaired Skin Integrity: Fecal matter contains enzymes and bacteria that are highly irritating to the skin. Constant or frequent exposure to moisture and stool leads to skin breakdown, maceration, and incontinence-associated dermatitis (IAD).
Rationale for incorrect answer:
2. Risk for Deficient Fluid Volume: While diarrhea can lead to fluid loss, fecal incontinence itself is a matter of control, not necessarily high-volume output. Unless the client has severe, watery diarrhea causing the incontinence, they are generally not at high risk for systemic fluid volume deficit.
Test taking strategy:
- Treat each option as a True/False statement.
- Start with the obvious, direct diagnosis. What problem is clearly present? Bowel incontinence
- Think in nursing domains
- Physical (skin integrity)
- Psychosocial (body image, social interaction)
Take home points:
- Nursing diagnoses for elimination issues must address both the physical (skin integrity) and the psychosocial (body image, social isolation) impacts on the client.
- Always identify the actual problem first (bowel incontinence) before moving to the potential complications or risks.
Practice Exercise 3
The nurse assesses a client’s abdomen several days after abdominal surgery. It is firm, distended, and painful to palpate. The client reports feeling “bloated.” The nurse consults with the surgeon, who orders an enema. The nurse prepares to give what kind of enema?
Explanation
Postoperative bloating and distension are common gastrointestinal complications that occur after surgery, often due to slowed peristalsis, accumulation of gas, or temporary impairment of bowel function from anesthesia, opioid use, or surgical manipulation of the intestines. Clients may experience abdominal fullness, discomfort, pain, and reduced appetite, sometimes accompanied by nausea or decreased passage of stool and flatus.
Rationale for correct answer:
3. Return flow: Also known as a Harris Flush, the return flow enema is specifically designed to help a patient expel flatus. It involves the repeated instillation of 100–200 mL of fluid followed by lowering the container to allow the fluid to flow back out. This sloshing motion stimulates the movement of gas bubbles out of the colon, relieving distension and the bloated feeling.
Rationale for incorrect answers:
1. Soapsuds enemas act by irritating the intestinal mucosa to stimulate peristalsis and defecation. While they help with constipation, they are not the primary choice for relieving simple gas-related distension and bloating in a post-op patient.
2. Retention: A general retention enema (like a medicated or nutrient enema) is intended to be held in the bowel for a long period. This would likely increase the patient's feeling of fullness and discomfort rather than relieving it.
4. Oil retention: Oil retention enemas are used to lubricate the rectum and soften hard stool (fecal impaction). They do not address the accumulation of gas in the intestinal tract.
Test taking strategy:
- Look for the keyword “bloated” or “distended.” In a post-abdominal surgery context, these words are classic indicators of trapped gas.
- Once you identify gas as the problem, look for the only enema on the list designed to remove it: the return flow.
Take home points:
- Distinguish between distension caused by stool (requires cleansing enemas) and distension caused by gas (requires return-flow enemas).
- The return flow enema is unique because it is a closed-loop style of irrigation that focuses on flatus removal through the use of hydrostatic pressure.
As the nurse prepares to assist a client with her newly created ileostomy, they are aware of which of the following?
Explanation
An ileostomy is a surgical procedure that creates an opening (stoma) in the abdominal wall by bringing the end of the small intestine to the surface, allowing waste to bypass the colon, rectum, and anus and exit into an external pouch. It is performed when the large intestine cannot function properly due to conditions like Crohn’s disease, ulcerative colitis, or cancer.
Rationale for correct answer:
4. Fecal drainage will be liquid: An ileostomy is created from the ileum. Since the waste bypasses the large intestine-where the majority of water reabsorption occurs-the output remains liquid or very loose.
Rationale for incorrect answers:
1. An appliance will not be required on a continual basis: Unlike a sigmoid colostomy, which may sometimes be managed with irrigation and a small cap, an ileostomy drains continuously from the small intestine. Because there is no sphincter to control the flow, an appliance must be worn at all times to collect the constant drainage.
2. The size of the stoma stabilizes within 2 weeks: A new stoma is typically swollen immediately following surgery. It generally takes 6 to 8 weeks for the edema to subside and for the stoma to reach its permanent, stable size.
3. Irrigation is necessary for regulation: Irrigation is used for distal colostomies (like a sigmoidostomy) to train the bowel. It is not performed on ileostomies because the drainage is constant and liquid; you cannot regulate the small intestine through irrigation.
Test taking strategy:
Since the small intestine is responsible for nutrient absorption but the colon is responsible for water absorption, anything exiting the small intestine must still be liquid.
Take home points:
- Because an ileostomy bypasses the colon entirely, the effluent will always be liquid and high in electrolytes.
- As ileostomy drainage is liquid and contains digestive enzymes, it is highly caustic. Maintaining a secure appliance seal is critical to prevent skin breakdown.
Comprehensive Questions
A nurse is caring for an older adult who is prone to constipation. Which statement provides evidence that the client is in need of further teaching?
Explanation
Constipation is a condition characterized by infrequent, difficult, or painful bowel movements, often resulting in the passage of hard, dry stools. It occurs when stool moves too slowly through the intestines or remains in the colon for prolonged periods, allowing excessive water absorption. Common causes include inadequate fluid or fiber intake, lack of physical activity, ignoring the urge to defecate, certain medications, and medical conditions that affect bowel function.
Rationale for correct answer:
2. “I need to take a laxative such as Milk of Magnesia if I don’t have a BM every day.” Normal bowel frequency varies from person to person ranging from three times a day to three times a week. Overuse of laxatives can lead to laxative dependency, where the bowel loses its natural ability to contract.
Rationale for incorrect answers:
1. “I need to drink one and a half to two quarts of liquid each day.” Adequate hydration, roughly 1,500–2,000 Ml, is essential for keeping stool soft. Since the client understands this, no further teaching is required.
3. “If my bowel pattern changes on its own, I should call you.” A sudden, unexplained change in bowel habits-especially in older adults-can be a warning sign of underlying issues like colorectal cancer or bowel obstructions. The client demonstrates good judgment here.
4. “Eating my meals at regular times is likely to result in regular bowel movements.” The gastrocolic reflex is stimulated by eating. Consistent meal times help establish a predictable rhythm for the bowels, encouraging regularity.
Test taking strategy:
- This is a false response question (indicated by the phrase “need for further teaching”). You are looking for the incorrect clinical statement.
- When you see “need for further teaching,” the right answer is the wrong medical advice.
Take home points:
- Regularity is defined by the individual's established pattern, not a 24-hour clock. Educating patients on this prevents the laxative cycle.
- Chronic use of stimulant or osmotic laxatives can damage the myenteric plexus (the nerves in the gut wall), making the constipation worse in the long run.
The nurse is most likely to report which finding to the primary care provider for a client who has an established colostomy?
Explanation
A colostomy is a surgical procedure that creates an opening (stoma) in the colon through the abdominal wall, diverting feces to an external pouch, typically due to disease, injury, or blockage, and can be temporary to allow healing or permanent. Waste exits the body through the stoma into a colostomy bag, bypassing the anus, as there's no sphincter control at the stoma. Reasons include cancer, diverticulitis, or Crohn's disease, and after surgery.
Rationale for correct answer:
3. The stoma color is a deep red-purple: This indicates ischemia -inadequate blood supply. A healthy stoma should be “beefy red” or pink. Purple, blue, or black indicates the tissue is dying and requires immediate surgical intervention.
Rationale for incorrect answers:
1. The stoma extends 1/2 in. above the abdomen: This is a normal, healthy finding. A “budded” stoma ensures that effluent (waste) empties directly into the pouch rather than sitting on the skin.
2. The skin looks red briefly after removing the appliance: This is normal reactive hyperemia. Just like taking off a band-aid, the skin may be pink for a few minutes. As long as the skin isn't broken or persistently painful, it is not an emergency.
4. The ascending colostomy delivers liquid feces: This is physiologically normal. In the ascending colon, the stool hasn't reached the parts of the bowel that reabsorb water, so the output is expected to be liquid.
Test taking strategy:
- When a nursing question asks what to report to the provider, it is looking for a sign of a complication. Options 1, 2, and 4 describe expected findings.
- Option 3 describes a circulatory failure. Always prioritize circulation issues.
Take home points:
- In ostomy care, the color of the stoma is the most critical indicator of viability.
- The higher the ostomy in the GI tract (ascending), the more liquid the stool. The lower it is (Sigmoid), the more formed the stool.
A nurse is aware that which goal is the most appropriate for clients with diarrhea related to ingestion of an antibiotic for an upper respiratory infection?
Explanation
Diarrhea related to the ingestion of an antibiotic occurs when the medication disrupts the normal balance of intestinal flora, reducing beneficial bacteria and allowing harmful organisms to proliferate. This imbalance can lead to increased intestinal motility and reduced absorption of water, resulting in loose, frequent stools. Antibiotic-associated diarrhea can sometimes be severe, particularly if caused by Clostridium difficile infection, which produces toxins that inflame and damage the intestinal lining.
Rationale for correct answer:
2. The client will return to his or her previous fecal elimination pattern: In the nursing process, a goal or expected outcome should directly resolve the nursing diagnosis. If the problem is diarrhea, the most appropriate and measurable goal is for the client to return to their baseline (normal) bowel habits once the underlying cause is addressed.
Rationale for incorrect answers:
1. The client will wear a medical alert bracelet: Diarrhea is a common side effect of antibiotics due to the disruption of normal intestinal flora, not necessarily an allergic reaction. Unless the client shows signs of an allergy, a medical alert bracelet is inappropriate and unnecessary.
3. The client will verbalize the need to take an antidiarrheal medication prn: Antidiarrheal medications are often contraindicated in antibiotic-associated diarrhea (such as C. diff), as they can slow down the clearance of toxins from the gut.
4. The client will increase intake of insoluble fiber: Insoluble fiber like bran or raw veggies acts as a laxative and speeds up GI transit time, which would likely worsen diarrhea. While soluble fiber like rice or bananas can help bulk up stool, increasing insoluble fiber is the wrong dietary intervention for this client.
Test taking strategy:
- When asked for the most appropriate goal, use the mirror technique. Look at the problem (diarrhea) and look for the answer that reflects the solution.
- Choices 1, 3, and 4 are interventions or actions, whereas Choice 2 is an actual outcome.
Take home points:
- Distinguishing between a side effect (diarrhea) and a true allergy (hives, angioedema) is critical for determining nursing interventions and client safety.
- An effective nursing goal is patient-centered and describes the desired change in the patient’s status-in this case, restoring normal bowel function.
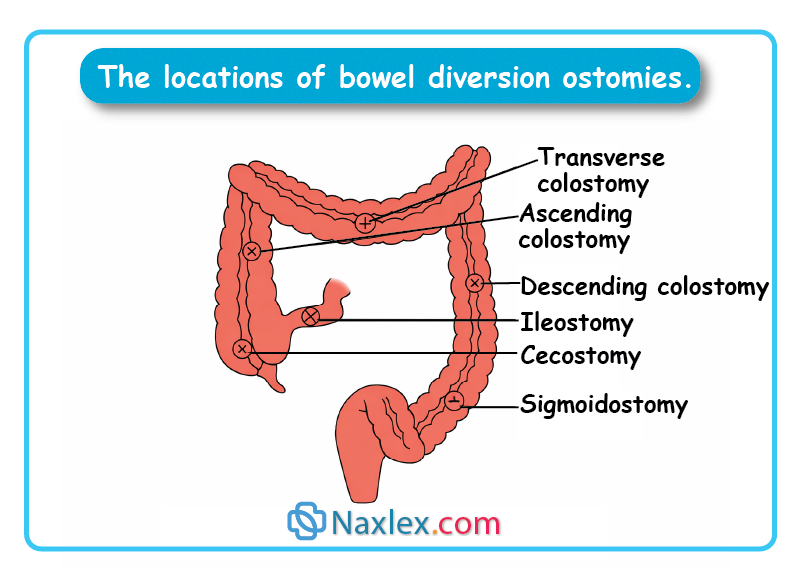
A student nurse is assigned to care for a client with a sigmoidostomy. The student will assess which ostomy site?
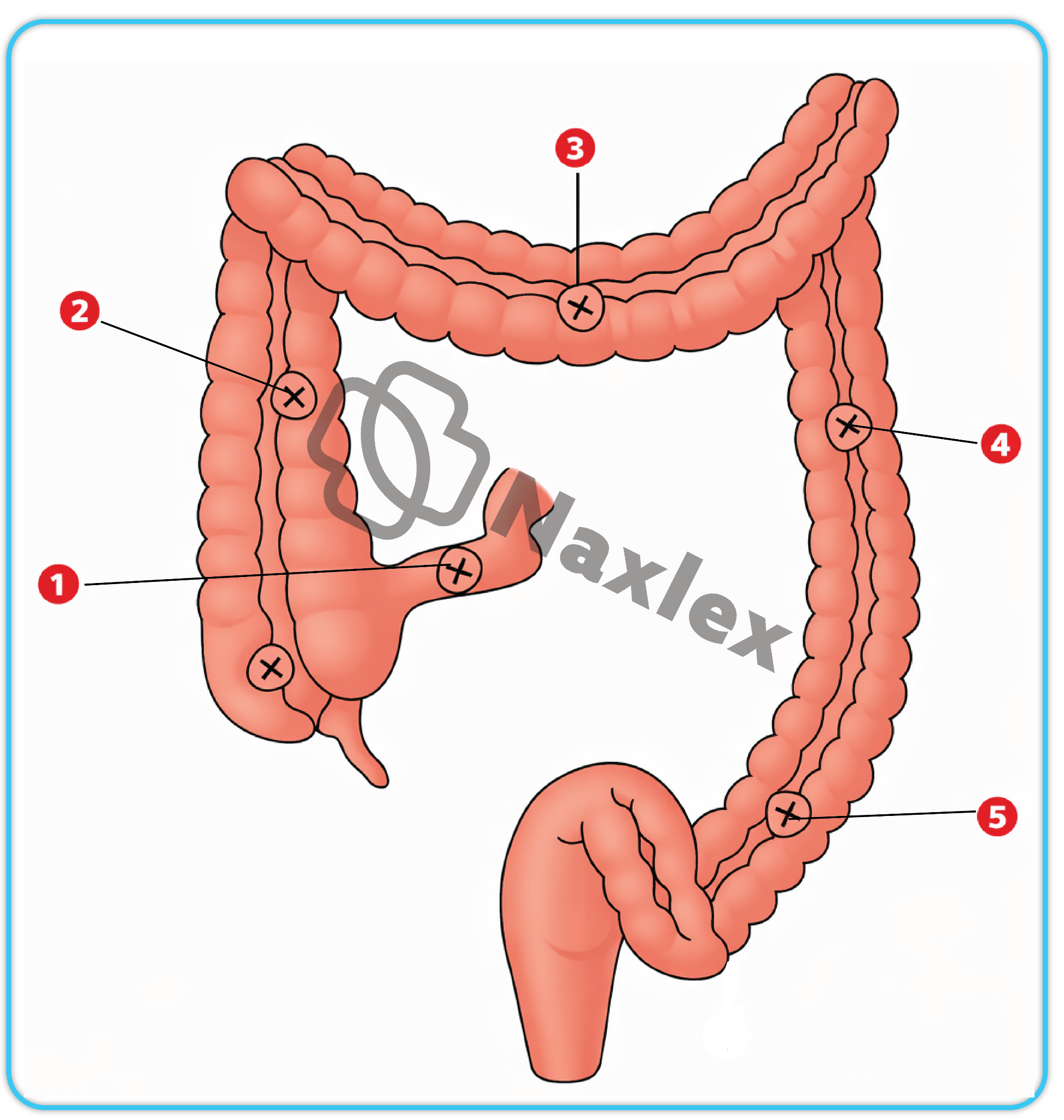
Explanation
A sigmoidostomy is a type of colostomy in which the surgical opening (stoma) is created from the sigmoid colon, the final portion of the large intestine, and brought through the abdominal wall to divert stool into an external pouch.
Rationale for correct answer:
5. Sigmoidostomy: The sigmoid colon is the S-shaped final segment of the colon before the rectum. A sigmoidostomy (Site 5) is located in the lower-left quadrant. Because the stool has traveled the entire length of the colon, it is well-formed and most similar to normal bowel movements.
Rationale for incorrect answers:
1. Ileostomy (Site 1): This site is located at the end of the small intestine (ileum). It typically produces constant, liquid, and highly acidic drainage.
2. Ascending Colostomy (Site 2): Located in the ascending colon on the right side of the abdomen. The output here is liquid to semi-liquid because water has not yet been reabsorbed.
3. Transverse Colostomy (Site 3): Located in the transverse colon across the upper abdomen. This usually results in malodorous, mushy, or semi-formed stool.
4. Descending Colostomy (Site 4): Located in the descending colon on the left side of the abdomen. The stool is becoming more solid as it moves toward the rectum.
Test taking strategy:
- Visualize the path of digestion. It starts on the patient's lower right (Ileum/Ascending) and ends on the patient's lower left (Sigmoid).
- Since sigmoid is the very last part of the colon before the rectum, look for the marker furthest along the left side of the diagram.
Take home points:
- The names of ostomies correspond to the section of the bowel used.
- The further down the tract the ostomy is (like a sigmoidostomy), the more formed the stool will be, as the colon has had maximum time to absorb water.
If a client was instructed to avoid foods that may have a laxative effect, the nurse would advise the client to avoid which of the following foods?
Explanation
Foods with natural laxative effects are typically rich in fiber, water, and certain compounds that stimulate bowel movements. Common examples include prunes, figs, pears, papaya, apples, and kiwifruit, which soften stool and improve intestinal transit. Leafy greens, whole grains, flaxseeds, and chia seeds add bulk to stool, while legumes and beans enhance gut motility.
Rationale for correct answer:
2. Alcohol is a known GI irritant and can have a laxative effect. It can increase gut motility and interfere with water absorption in the intestines, often leading to looser stools. Other foods with similar effects include spicy foods, coffee, and chocolate.
Rationale for incorrect answers:
1. Cheese: This food is generally known to have a constipating effect. Dairy products like cheese can slow down intestinal motility in many individuals.
3. Eggs: Like cheese, eggs are low-fiber, high-protein foods that are more likely to cause constipation or have a neutralizing effect on bowel patterns rather than a laxative one.
4. Pasta: Refined carbohydrates such as white pasta are low in fiber and are traditionally associated with constipation or binding the stool, making them inappropriate for a client trying to avoid laxative effects.
Test taking strategy:
- Group the options by their physical properties.
- Cheese, eggs, and pasta are all solid, low-fiber foods that typically slow digestion.
- Alcohol is the odd one out as a liquid irritant.
Take home points:
- Alcohol and caffeine act as chemical irritants that speed up the gut, while heavy proteins and refined starches act as binders that slow it down.
- When teaching a client about diarrhea management, the BRAT diet (Bananas, Rice, Applesauce, Toast) is often used to provide binding effects, while alcohol is strictly avoided.
A client has a fecal impaction. The nurse correctly administers an oil-retention enema by doing which of the following?
Explanation
An oil-retention enema involves introducing a small volume of mineral or vegetable oil into the rectum, where it is held for 30 minutes to several hours to soften hardened stool and ease elimination. The oil lubricates the intestinal walls and penetrates fecal matter, making it easier to pass, especially in cases of constipation or fecal impaction.
Rationale for correct answer:
3. Instructing the client to retain the enema for at least 30 minutes: The goal of an oil-retention enema is to lubricate the rectum and soften the hard fecal mass (impaction). For the oil to effectively penetrate the stool, it must remain in the rectum for an extended period, typically 30 to 60 minutes.
Rationale for incorrect answers:
1. Administering a large volume of solution (500–1,000 mL): These are small-volume enemas (usually 90–120 mL). Large volumes (500–1,000 mL) are used for cleansing enemas to distend the bowel.
2. Mixing milk and molasses in equal parts: A milk and molasses enema is a specific type of carminative enema used to help expel gas. Oil-retention enemas use mineral or vegetable oil.
4. Administering the enema while the client is sitting on the toilet: Enemas should be administered in the left Sims' position (lying on the left side with the right knee flexed). Sitting on a toilet makes it difficult for the fluid to flow into the sigmoid colon and increases the risk of immediate expulsion before the oil can work.
Test taking strategy:
- Ask yourself: “What is the purpose of an oil-retention enema?”
- The purpose is to soften stool. To soften something, it needs to soak.
- Therefore, the answer that provides the longest soak time (retaining for 30 minutes) is the most logically correct nursing action for this specific type of enema.
Take home points:
- The name retention enema tells you the priority intervention: the patient must keep the fluid inside for it to be therapeutic.
- Positioning: Proper positioning (Left Sims') uses the natural anatomy of the descending and sigmoid colon to allow the fluid to flow by gravity and stay in place.
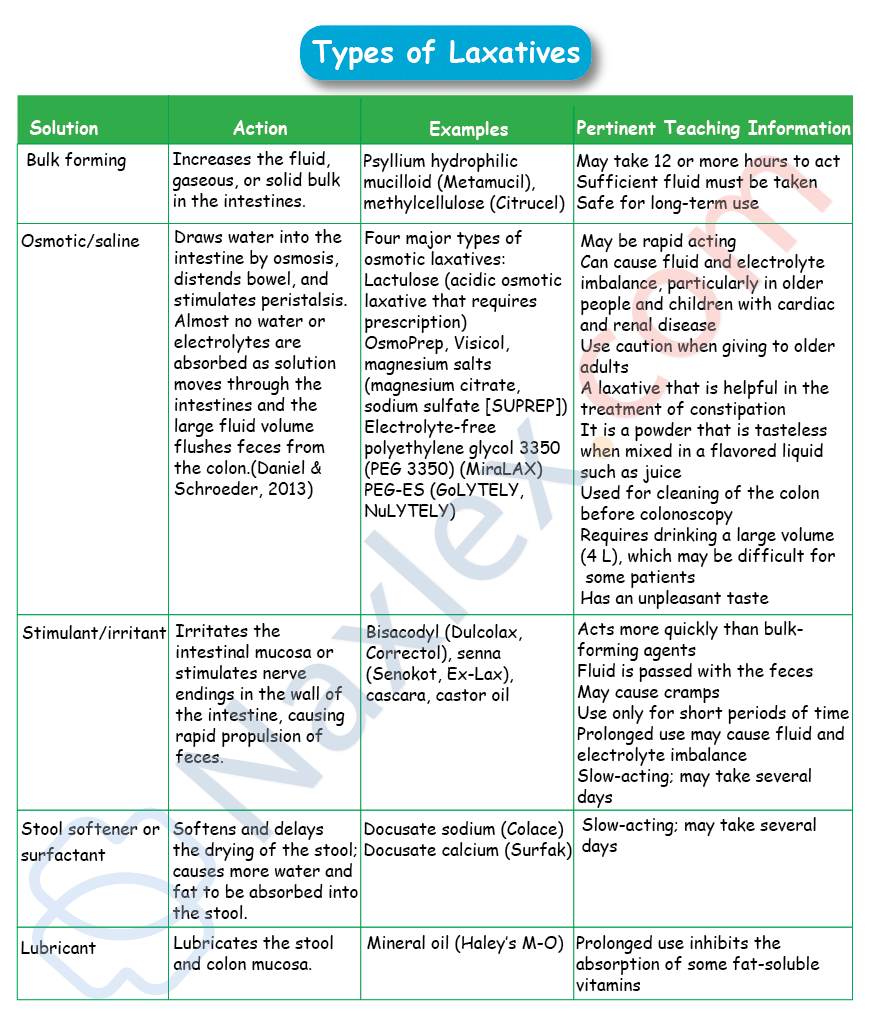
A nurse is educating student nurses about laxatives. Which class of laxative acts by causing the stool to absorb water and swell?
Explanation
Laxatives are classified into several groups based on how they promote bowel elimination. Bulk-forming agents increase stool size and stimulate peristalsis. Stool softeners allow water and fats to penetrate stool, making it easier to pass. Osmotic laxatives draw water into the intestines to soften stool and speed transit. Stimulant laxatives directly trigger intestinal contractions. Lubricant laxatives coat stool and intestinal walls to ease passage.
Rationale for correct answer:
1. Bulk-forming such as psyllium or methylcellulose consist of high-fiber content. They work by absorbing water into the intestine, which causes the stool to swell. This increased bulk stretches the intestinal wall, stimulating natural peristalsis.
Rationale for incorrect answers:
2. Emollient: Also known as stool softeners like docusate sodium, these work by lowering the surface tension of the stool, allowing water and fats to penetrate the fecal mass. They make the stool slippery rather than making it swell.
3. Lubricant: Lubricant laxatives like mineral oil coat the surface of the stool and the intestinal tract. This prevents water from being absorbed out of the stool and allows the mass to slide through the colon more easily.
4. Stimulant: Stimulant laxatives like senna or bisacodyl work by chemically irritating the intestinal mucosa or stimulating the nerve endings in the gut wall to force contractions. They do not work by changing the volume of the stool through water absorption.
Test taking strategy:
- The question uses the words “absorb water” and “swell.” Look for the answer that implies getting bigger.
- The word “Bulk” in bulk-forming is a direct synonym for swelling or increasing size, making it the most logical choice.
Take home points:
- Because bulk-forming laxatives work by absorbing water, they must be taken with a full glass of water.
- Bulk-forming laxatives are generally considered the safest for long-term use because they most closely mimic the body's natural physiological stimulus for a bowel movement.
A client is nervous about a colonoscopy scheduled for tomorrow. The nurse describes the test by explaining that it allows which of the following?
Explanation
A colonoscopy is a medical procedure that uses a flexible tube with a camera (colonoscope) to examine the inside of the colon and rectum, helping detect abnormalities such as polyps, inflamed tissue, bleeding, or signs of colorectal cancer.
Rationale for correct answer:
2. Visual examination of the large intestine: A colonoscopy involves the insertion of a flexible fiber-optic scope - colonoscope - through the anus to provide a direct visual examination of the entire length of the colon and often the distal ileum.
Rationale for incorrect answers:
1. Visual examination of the esophagus and stomach: This describes an Esophagogastroduodenoscopy (EGD) or Upper Endoscopy. While it uses a similar camera tool, it focuses on the upper GI tract, not the colon.
3. Radiographic examination of the large intestine: This describes a barium enema. This is an X-ray (radiographic) procedure where contrast dye is inserted into the rectum to visualize the colon on a screen; it does not involve a camera for a direct visual view.
4. Fluoroscopic examination of the small intestine: This describes a small bowel follow-through. It involves swallowing contrast and using real-time X-rays (fluoroscopy) to watch the material move through the small intestine.
Test taking strategy:
Break the word down: “Colon” refers to the large intestine, and “scopy” means to look at or view. Therefore, a “colonoscopy” is viewing the large intestine.
Take home points:
- Any medical term ending in “-oscopy” refers to a visual examination using a scope/camera. Terms ending in “-graphy” or “-gram” usually refer to imaging like X-rays.
- Colonoscopies are the gold standard for colorectal cancer screening because they allow the provider to both see abnormalities and take biopsies or remove polyps simultaneously.
A nurse is aware that a bowel training program includes which of the following?
Explanation
A bowel training program is a structured routine designed to help individuals establish regular bowel movements and manage issues such as constipation or fecal incontinence. It typically involves scheduling toileting at consistent times, often after meals to take advantage of the body’s natural gastrocolic reflex, combined with dietary adjustments like increasing fiber and fluid intake.
Rationale for correct answer:
4. Allowing ample time for evacuation: Consistency and patience are the foundations of bowel training. Clients should be encouraged to attempt defecation at the same time each day usually 30–60 minutes after a meal to utilize the gastrocolic reflex. Providing a relaxed, private environment with enough time, usually 15–20 minutes, ensures the client does not strain or feel rushed.
Rationale for incorrect answers:
1. Using a diet that is low in bulk: A successful bowel training program requires a high-fiber (high-bulk) diet. Fiber adds weight and volume to the stool, which stretches the colon wall and stimulates the necessary peristalsis for a bowel movement.
2. Decreasing fluid intake to 1,000 mL: Adequate hydration is essential for bowel training; typically, 2,000–3,000 mL of fluid per day is recommended. Low fluid intake leads to hard, dry stools that are difficult to pass, defeating the purpose of the program.
3. Administering an enema once a day: While a suppository may be used to initiate a schedule, daily enemas are avoided in training programs because they can lead to dependency and can cause fluid and electrolyte imbalances.
Test taking strategy:
- Bowel training is a restorative process. Look for the option that mimics natural healthy habits.
- Options 1, 2, and 3 describe artificial or restrictive measures.
- Option 4 describes a supportive, natural behavioral intervention, which is the hallmark of nursing-led rehabilitation programs.
Take home points:
- Bowel training relies on establishing a predictable routine to take advantage of the body's natural reflexes.
- Fiber, fluids, and timing are the three essential physiological requirements for successful bowel rehabilitation.
The nurse is aware that a barium enema should be done before an upper gastrointestinal series because of which of the following?
Explanation
A barium enema is a diagnostic procedure used to examine the colon and rectum by introducing a liquid containing barium sulfate into the bowel through the rectum. The barium coats the lining of the intestine, making it visible on X-ray images and allowing doctors to detect abnormalities such as polyps, tumors, diverticula, or structural changes.
Rationale for correct answer:
1. Retained barium may cloud the colon: Barium is a thick, radiopaque contrast medium. If an upper GI series is done first, the barium must travel through the entire intestinal tract to be excreted. This process can take several days. If a barium enema (lower GI study) is attempted while that oral barium is still lingering in the colon, it will obscure the view and cloud the X-ray images, making the results of the enema study uninterpretable.
Rationale for incorrect answers:
2. Barium can cause lower gastrointestinal bleeding: This is incorrect. Barium is an inert substance and does not cause bleeding. Its primary risk is impaction/constipation if it is not flushed out of the system with fluids.
3. The physician’s orders are in that sequence: While orders are followed, this does not explain the rationale behind the sequencing. Nursing exams require you to understand the underlying physiological or diagnostic reason.
4. Barium is absorbed readily in the lower intestine: Barium is not absorbed by the body; it is meant to stay in the lumen of the gut to coat the walls for X-ray visualization and is eventually excreted in the stool.
Test taking strategy:
- Think about the direction of travel. Oral barium (Upper GI) moves downward and hangs around the exit. Rectal barium (Enema) is inserted and then expelled.
- If you put the barium in from the top first, it trashes the area you need to look at from the bottom. To keep the images clean, you start with the bottom-most test.
Take home points:
- When multiple barium studies are needed, always schedule the lower study (enema) before the upper study (swallow) to prevent interference.
- Because barium hardens as water is absorbed, the nurse must prioritize increased fluid intake and potentially a laxative after any barium study to prevent fecal impaction.
Nurses should recommend avoiding the habitual use of laxatives. Which of the following is the rationale for this?
Explanation
Habitual use of laxatives can lead to significant complications in bowel function and overall health. Over time, frequent use may cause the bowel to become dependent on stimulation, reducing its natural ability to contract and eliminate stool effectively. This can result in chronic constipation, electrolyte imbalances, dehydration, and even damage to the intestinal mucosa.
Rationale for correct answer:
2. They will cause chronic constipation: Habitual use of laxatives, particularly stimulants, leads to a loss of natural muscle tone in the colon and a decreased sensitivity to the defecation reflex. This creates a vicious cycle or laxative dependency where the client can no longer have a bowel movement without chemical assistance, ultimately resulting in chronic, long-term constipation.
Rationale for incorrect answers:
1. They will cause a fecal impaction: While untreated constipation can lead to impaction, laxatives are designed to prevent it. However, the overuse of laxatives makes the bowel less likely to function on its own, which may eventually lead to an impaction if the laxative is suddenly stopped.
3. They change the pH of the gastrointestinal tract: While some osmotic laxatives may slightly alter the local environment, the primary reason nurses discourage habitual use is the physiological loss of bowel function and muscle tone, not pH shifts.
4. They inhibit the intestinal enzymes: Laxatives generally work through irritation, osmosis, or lubrication; they do not typically interfere with the digestive enzymes responsible for breaking down food in the small intestine.
Test taking strategy:
- When a question asks for a rationale regarding habitual or chronic use, look for an answer that describes a long-term physiological change.
- Option 2 describes a chronic condition (chronic constipation) that results from a long-term habit, making it the most appropriate answer.
Take home points:
- Laxative Dependency: The “lazy bowel” syndrome occurs when the colon becomes dependent on external stimulation to contract, leading to chronic dysfunction.
- Natural Alternatives: Nurses should promote high-fiber diets, adequate hydration, and exercise as the primary methods for maintaining regularity rather than reaching for over-the-counter medications.
The nurse should incorporate which of the following as the basis for action when explaining the action of a hypertonic solution enema?
Explanation
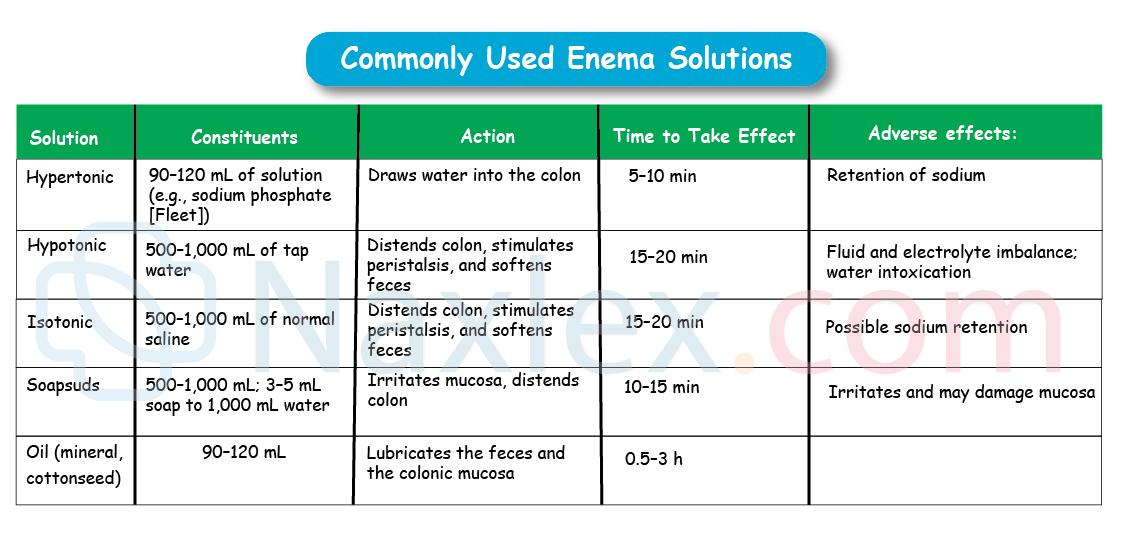
A hypertonic solution enema is a type of cleansing enema that uses a small volume of a concentrated solution, such as sodium phosphate, to draw water into the colon by osmosis. This influx of fluid stimulates peristalsis and softens stool, producing a rapid bowel movement, usually within 5–15 minutes. Because it works quickly and requires less liquid than other enemas, it is often used for acute relief of constipation.
Rationale for correct answer:
3. Osmosis of water into colon: A hypertonic solution has a higher concentration of solutes than the surrounding body fluids. Through osmosis, water is drawn from the interstitial spaces and vascular system into the colon. This increased volume of water distends the colon, which triggers the defecation reflex.
Rationale for incorrect answers:
1. Bowel mucosa irritation: While some enemas like soapsuds work through irritation to stimulate peristalsis, hypertonic enemas like Fleet enemas work primarily through fluid shift.
2. Diffusion of water out of colon: Diffusion out of the colon would dehydrate the stool and make it harder to pass. Hypertonic solutions pull water into the space they occupy.
4. Softening of fecal contents: This is a secondary effect. While the influx of water does soften the stool, the primary action that characterizes a hypertonic enema is the osmotic fluid shift.
Test taking strategy:
- Identify the type of solution mentioned. Hypertonic is a classic chemistry term related to osmosis.
- When you see hypertonic or isotonic in a nursing question about fluids, look for an answer choice that includes the word osmosis or describes a fluid shift between compartments.
Take home points:
- Concentration gradience: Water always follows the concentrated environment to try and balance it out.
- Because they pull water from the body into the bowel, hypertonic enemas use a very small volume (about 120 mL) but achieve significant distension.
A nurse is caring for a client with a nasogastric tube in place for gastric decompression. Which of the following are included in the nursing plan of care? Select all that apply
Explanation
Gastric decompression is a medical procedure used to relieve pressure and remove stomach contents by inserting a nasogastric (NG) or orogastric tube into the stomach. It is commonly performed in cases of bowel obstruction, severe vomiting, abdominal distension, or after surgery to prevent aspiration and reduce discomfort.
Rationale for correct answers:
2. Measure the length of the exposed tube: To ensure the tube has not migrated or been pulled out, the nurse should measure and record the length of the tube from the exit point (nares) to the end. Any change in length indicates potential displacement.
3. Measure the pH of the aspirated tube contents: Testing the pH of aspirated gastric contents (typically < 5.5) is a standard bedside method to help verify that the tube remains in the stomach and has not moved into the lungs or small intestine.
4. Administer frequent oral hygiene: Clients with NG tubes often breathe through their mouths and cannot drink fluids, leading to very dry mucous membranes. Frequent oral care (every 2-4 hours) prevents discomfort and oral infection.
5. Auscultate for bowel sounds every 4 hours: Since the tube is for gastric decompression, it is likely being used for an ileus or obstruction. Regular assessment of bowel sounds helps determine if GI motility is returning, which would indicate that the tube may soon be removed.
Rationale for incorrect answer:
1. Irrigate with Ringers’ lactate: NG tubes for decompression are typically irrigated with normal saline (0.9% NaCl), not Ringers’ lactate. Saline is used to prevent electrolyte depletion from the stomach during the irrigation and suction process.
Test taking strategy:
Focus on the purpose of the NG tube
- Gastric decompression - drainage, placement verification, comfort
Select interventions that directly support tube safety and function
- Position, patency, verification, oral care
Eliminate options with incorrect solutions or overly general assessments
Take home points:
- Correct placement of an NG tube must be verified not just after insertion, but at regular intervals through pH testing and external measurements.
- NG tubes are highly irritating; nursing care must prioritize local comfort.
A nurse is assessing a client with an ileostomy. Which of the following would be a common nursing diagnosis for this client?
Explanation
An ileostomy is a surgical procedure that creates an opening (stoma) in the abdominal wall by bringing the end of the small intestine (ileum) to the surface, allowing waste to bypass the colon, rectum, and anus and exit into an external pouch. It is performed when the large intestine cannot function properly due to conditions like Crohn’s disease, ulcerative colitis, or cancer.
Rationale for correct answer:
1. Disturbed Body Image: The creation of a stoma involves a significant change in physical appearance and a loss of control over a basic bodily function. Clients often struggle with the mutilation of their abdomen, the presence of a bag, and the fear of odors/leaking, all of which contribute to a disturbed body image.
Rationale for incorrect answers:
2. Constipation: This is almost never a diagnosis for an ileostomy. Because an ileostomy bypasses the entire large intestine where water is absorbed, the output is constant and liquid. Constipation is a concern for colostomies, not ileostomies.
3. Delayed Growth and Development: Unless the client is a child or adolescent whose physical or social milestones are being missed due to chronic illness, this is not a common or standard diagnosis for an adult with an ileostomy.
4. Excess Fluid Volume: The opposite is actually true. Because the colon is bypassed, the client loses large amounts of fluid and electrolytes in their liquid stool. They are at high risk for Deficient Fluid Volume, not excess.
Test taking strategy:
- Identify the location: "Ileo-" means small intestine. If the waste never hits the colon, it will be liquid. This eliminates constipation.
- Since they are losing liquid, Excess Fluid Volume is also incorrect.
- Choosing between the remaining options, Disturbed Body Image is a classic, universal nursing diagnosis for any permanent surgical alteration of the body.
Take home points:
- The nurse must address the emotional and identity shift of having an ostomy just as much as the physical care.
- Always associate ileostomy with fluid loss. Clients need to be monitored closely for signs of low blood pressure and electrolyte imbalances.
A nurse is preparing a staff education program on bowel elimination. Which of the following is an appropriate nursing action to include to promote regular bowel habits?
Explanation
Promoting regular bowel habits involves adopting healthy lifestyle practices that support normal digestive function and prevent constipation. Key strategies include maintaining a diet rich in fiber from fruits, vegetables, and whole grains, drinking adequate fluids to keep stools soft, and engaging in regular physical activity to stimulate intestinal motility. Establishing a consistent toileting schedule, especially after meals when the gastrocolic reflex is strongest, helps train the bowel to empty predictably.
Rationale for correct answer:
4. Assisting the client to as normal position as possible to defecate: Human anatomy is designed to defecate in a sitting or squatting position. This position uses gravity and increases intra-abdominal pressure to help evacuate the bowel. For a bedridden patient, this means raising the head of the bed to a high-Fowler’s position when using a bedpan.
Rationale for incorrect answers:
1. Encouraging the client to avoid moving his bowels until a certain time: Clients should be encouraged to heed the defecation reflex as soon as it occurs. Ignoring the urge leads to water reabsorption and constipation.
2. Encouraging the client to avoid excess fluid intake and fiber: To promote regularity, a nurse should encourage the opposite: an increase in fiber to add bulk and an increase in fluids (2,000–3,000 mL) to keep the stool soft.
3. Avoiding strenuous exercise: Physical activity and exercise like walking actually promote peristalsis and help move waste through the colon. Sedentary behavior is a leading cause of constipation.
Test taking strategy:
- In nursing education questions, the most appropriate action is usually the one that most closely mimics normal human physiology.
- Sitting up to go to the bathroom is the most natural and effective way to move bowels, making Option 4 the strongest clinical intervention.
Take home points:
- Simply sitting a patient up (if not contraindicated) is one of the most effective non-pharmacological interventions for bowel elimination.
- Education should focus on responding immediately to the body's signals to prevent the lazy bowel syndrome.
Exams on Bowel elimination
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
To:
- Describe the physiology of defecation.
- Distinguish normal from abnormal characteristics and constituents of feces.
- Identify factors that influence fecal elimination and patterns of defecation.
- Identify common causes and effects of selected fecal elimination problems.
- Describe methods used to assess fecal elimination.
- Identify examples of nursing diagnoses, outcomes, and interventions for clients with elimination problems.
- Identify measures that maintain normal fecal elimination patterns.
- Describe essentials of fecal stoma care for clients with an ostomy.
- Verbalize the steps used in: a. Administering an enema. b. Changing a bowel diversion ostomy appliance.
Introduction
Regular elimination of bowel waste products is essential for normal body functioning. Alterations in bowel elimination are often early signs or symptoms of problems within either the gastrointestinal (GI) tract or other body systems. Because bowel function depends on the interaction among several different factors, elimination patterns and habits vary among individuals.
Understanding normal bowel elimination and factors that promote, slow down, or cause alterations in elimination help you manage patients’ elimination problems.
Physiology & Pathophysiology of Defecation
Anatomy of the large intestine
The adult colon is approximately 125–150 cm (50–60 in.) long and consists of seven distinct parts:
- Cecum: The beginning of the large intestine.
- Ascending Colon
- Transverse Colon
- Descending Colon
- Sigmoid Colon: Connects to the rectum.
- Rectum: 10–15 cm long; contains vertical folds (with arteries/veins) to help retain feces.
- Anus: The distal outlet.
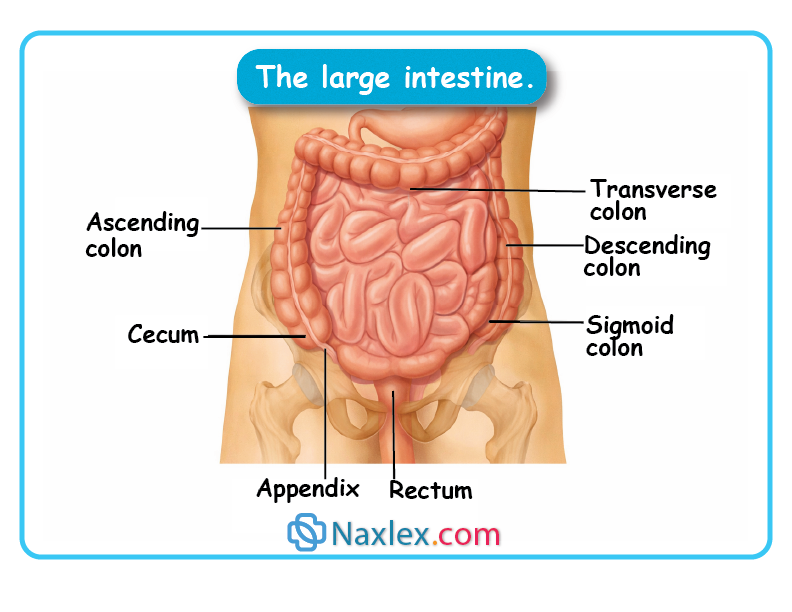
Key structural features:
- Ileocecal valve: Regulates chyme flow from the small intestine to the large intestine and prevents backflow.
- Haustra: Pouches formed because the longitudinal muscles are shorter than the colon itself.
- Anal sphincters:
- Internal: Involuntary control (autonomic nervous system).
- External: Voluntary control (somatic nervous system).
Functions of the colon
- Absorption: Absorbs water and nutrients. Of the 1,500 mL of chyme entering daily, all but 100 mL is reabsorbed.
- Protection: Secretes mucus (high in bicarbonate) to protect the wall from bacterial activity and fecal acids, and to act as an adherent for feces.
- Elimination: Transports and expels feces (solid waste) and flatus (air and digestion by-products).
Intestinal motility (Movements)
To move waste forward, the colon utilizes three types of movement:
- Haustral churning: Back-and-forth movement within the haustra. Mixes contents and aids water absorption.
- Colon peristalsis: Sluggish, wavelike movements that propel contents forward slowly.
- Mass peristalsis: Powerful muscular contractions covering large areas. Occurs only a few times a day, usually triggered by eating (gastrocolic reflex).
The process of defecation
Defecation is the expulsion of feces from the anus and rectum.
- Trigger: Peristalsis moves feces into the sigmoid colon and rectum.
- Sensation: Sensory nerves in the rectum are stimulated, creating the urge.
- Internal reflex: The internal anal sphincter relaxes involuntarily, and feces move into the anal canal.
- Voluntary control: The external anal sphincter is relaxed voluntarily (usually when seated).
- Assistance: Abdominal muscles, the diaphragm, and pelvic floor muscles contract to increase pressure.
- Note: Thigh flexion and a sitting position facilitate the process.
Ignoring the Urge: If the defecation reflex is repeatedly inhibited, the rectum expands to accommodate waste, leading to a loss of sensitivity and eventually constipation.
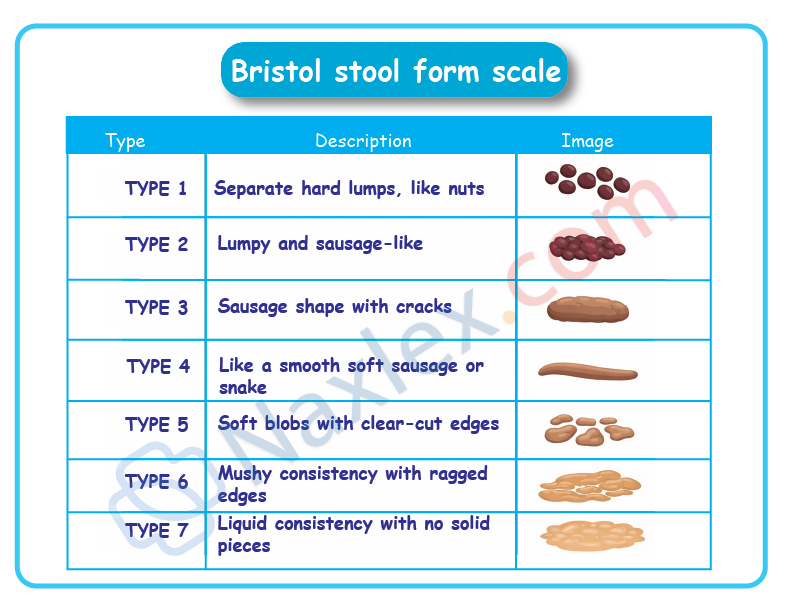
Characteristics of Feces
Feces are typically composed of 75% water and 25% solid materials.
|
Characteristic |
Normal Findings |
Notes |
|
Color |
Brown |
Due to stercobilin and urobilin (derived from bilirubin). |
|
Consistency |
Soft but formed |
Affected by transit time; faster transit = more fluid (diarrhea). |
|
Odor |
Pungent |
Caused by bacterial action on chyme. |
|
Water Content |
~75% |
Decreased water intake leads to hard, difficult-to-pass stools. |
1.1 FACTORS AFFECTING DEFECATION
1. Developmental considerations
Elimination patterns change significantly across the lifespan as the nervous and muscular systems mature and eventually age.
Infants and Children
- Newborns: Pass meconium (black, tarry, odorless) within 24 hours.
- Infants: Frequent, soft stools due to immature intestines. Breast-fed stools are light yellow/golden; formula-fed stools are dark yellow/tan.
- Toddlers: Bowel control typically begins at 1.5 to 2 years. Daytime control is usually achieved by age 2.5 after toilet training.
- School-Age/Adolescents: Habits similar to adults, though play may cause them to delay defecation.
Older adults
- Constipation: Affects up to 50% of older adults due to reduced activity, low fiber/fluid, and muscle weakness.
- The regularity myth: Many believe a daily BM is required; however, normal patterns vary (e.g., every other day).
- Laxative dependency: Habitual use weakens natural reflexes and can cause electrolyte imbalances.
- Intervention: Increase fiber (20–35g), fluids (6–8 glasses), and exercise. Toileting 30 minutes after meals capitalizes on the gastrocolic reflex.
2. Lifestyle Factors
Diet
- Fiber (Bulk): Essential for fecal volume.
- Insoluble: (Whole wheat, veggies) Increases bulk and movement.
- Soluble: (Oats, beans, apples) Forms a gel; lowers cholesterol/glucose.
- Recommended Fiber: Men (~30–38g), Women (~21–25g).
- Food Effects:
- Gas-producing: Cabbage, onions, bananas.
- Laxative-effect: Prunes, bran, alcohol.
- Constipating: Cheese, pasta, lean meats.
Fluid Intake
- Requirement: Healthy elimination requires 2,000 to 3,000 mL of fluid daily.
- Mechanism: If intake is low, the colon reabsorbs more water from chyme, resulting in hard, dry feces.
Activity & Psychology
- Activity: Stimulates peristalsis. Weak abdominal/pelvic muscles or immobility (bed rest) lead to constipation.
- Psychological Factors:
- Anxiety/Anger: Can increase peristalsis (diarrhea/nausea).
- Depression: Can slow intestinal motility (constipation).
3. Habits and Medications
Defecation habits
- Ignoring the urge to defecate (due to work, lack of privacy, or embarrassment) causes the rectum to reabsorb more water, making stool harder and eventually weakening the defecation reflex.
Medications and stool appearance
- Opioids (Morphine/Codeine): Cause constipation by decreasing GI activity.
- Iron Supplements: Can cause constipation or diarrhea; turns stool black.
- Aspirin: May cause GI bleeding, resulting in red or black stool.
- Antibiotics: May cause gray-green discoloration.
- Antacids: May cause whitish discoloration or specks.
- Pepto-Bismol: Turns stool black.
4. Clinical and pathological factors
Surgery and anesthesia
- General anesthesia: Blocks parasympathetic stimulation, slowing or stopping colonic movements.
- Ileus: Temporary cessation of intestinal movement (24–48 hours) following direct handling of intestines during surgery.
- Nursing priority: Listening for bowel sounds post-operatively.
Pathologic conditions and pain
- Neurological: Spinal cord or head injuries can impair sensory stimulation or sphincter control (incontinence).
- Pain: Patients may suppress the urge to defecate to avoid pain (e.g., post-hemorrhoidectomy), leading to constipation.
1.2 FECAL ELIMINATION PROBLEMS
Effective nursing care requires an understanding of the pathophysiology, causes, and clinical implications of altered bowel elimination.
1. Constipation: Fewer than three bowel movements per week, characterized by the passage of dry, hard stool or no stool at all.
- Pathophysiology: Slow movement of feces through the large intestine, leading to excessive water reabsorption.
- Key characteristics:
- Straining during defecation.
- Feeling of incomplete evacuation.
- Decreased frequency relative to the person's normal pattern.
- Common causes:
- Lifestyle: Low fiber/fluid intake, immobility, lack of privacy, ignoring the urge.
- Medical/Psychological: IBS, pelvic floor dysfunction, depression, neurological conditions (Parkinson’s, Stroke).
- Medications: Opioids, iron supplements, antacids, antidepressants.
- Major risk: The Valsalva maneuver
- Straining while holding the breath increases intrathoracic pressure and vagal tone.
- Danger: Can cause a sudden drop-in pulse rate; extremely risky for patients with heart disease, brain injuries, or respiratory disease.
2. Fecal impaction: A hardened mass of feces wedged in the rectum, resulting from prolonged retention.
- Classic sign: Liquid fecal seepage (diarrhea) with no normal stool. The liquid portion of feces bypasses the hard mass.
- Symptoms: Rectal pain, frequent but nonproductive urge to defecate, anorexia, abdominal distention, and vomiting.
- Clinical alert (Older adults): Sudden changes in mental status or delirium can be a sign of fecal impaction.
- Management:
- Digital rectal examination (may require a provider’s order).
- Oil retention enemas followed by cleansing enemas.
- Manual removal if other methods fail.
3. Diarrhea: Passage of liquid feces and increased frequency of defecation.
- Pathophysiology: Rapid movement of chyme through the large intestine, preventing adequate water and electrolyte reabsorption.
- Complications: Fluid and electrolyte imbalances (high risk for infants and older adults).
- Skin breakdown (perineal irritation).
- C. Difficile (Clostridium difficile):
- Symptoms: Foul-smelling, mucoid diarrhea.
- Risk factors: Recent antibiotic use (fluoroquinolones), chemotherapy, immunosuppression.
- Nursing Priority: Alcohol-based gels do not kill spores; must use soap and water and bleach-based cleaners.
- Intervention: Keep skin clean/dry; use zinc oxide or fecal collectors to prevent breakdown.
4. Bowel incontinence: Loss of voluntary control over fecal and gaseous discharges.
- Types:
- Partial: Inability to control flatus or minor soiling.
- Major: Inability to control feces of normal consistency.
- Causes: Impaired anal sphincter function, spinal cord trauma, neuromuscular diseases, or tumors.
- Psychosocial impact: High risk for social isolation and embarrassment. Over 50% of nursing home residents experience some form of incontinence.
5. Flatulence: Excessive gas (flatus) in the intestines, leading to distention.
- Sources: Swallowed air, bacterial action on chyme, or gas diffusion from the bloodstream.
- Causes: Certain foods (cabbage, onions), narcotics, or abdominal surgery.
- Management: Eructation (belching) for gastric gas.
- Absorption into the bloodstream.
- If gas cannot be expelled naturally, a rectal tube may be necessary to relieve distention.
|
Problem |
Primary characteristic |
Key nursing risk |
|
Constipation |
Hard, dry stool; < 3x/week |
Valsalva maneuver (cardiac risk) |
|
Impaction |
Liquid seepage; mass in rectum |
Delirium in older adults |
|
Diarrhea |
Liquid feces; high frequency |
Dehydration/Skin breakdown |
|
Incontinence |
Loss of voluntary control |
Social isolation |
|
Flatulence |
Intestinal distention/gas |
Discomfort; may need rectal tube |
1.3 BOWEL DIVERSION OSTOMIES
An ostomy is a surgically created opening that connects an internal organ (gastrointestinal, urinary, or respiratory) to the skin. In bowel diversions, this opening is called a stoma.
Types of intestinal ostomies
Ostomies are named based on their anatomical location. While some provide nutrition, others are designed for waste elimination.
Feeding ostomies
- Gastrostomy: Opening into the stomach.
- Jejunostomy: Opening into the jejunum (mid-section of the small intestine).
- Purpose: Primarily used to provide an alternative route for enteral feeding.
Bowel diversion ostomies
- Ileostomy: Opening into the ileum (distal small intestine).
- Colostomy: Opening into the colon (large intestine).
- Purpose: To divert and drain fecal material.
The Stoma: Appearance and sensation
- Normal Appearance: Red, fleshy, and moist (similar to the inside of the cheek).
- Bleeding: Slight bleeding is normal when touched, especially initially.
- Sensation: The stoma has no nerve endings; the patient cannot feel the stoma itself.
Classification of bowel ostomies
A. Permanence
- Temporary: Often performed for traumatic injuries or inflammatory conditions to allow the distal bowel to rest and heal. The surgical reconnection of a temporary ostomy is called a take-down.
- Permanent: Performed when the rectum or anus is nonfunctional due to birth defects or diseases like cancer.
B. Anatomic location & Drainage characteristics
The location of the ostomy determines the consistency of the stool. The further along the bowel the ostomy is, the more formed the stool becomes.
|
Location |
Stool Consistency |
Regulation |
Nursing Considerations |
|
Ileostomy |
Liquid |
None (Constant) |
High enzymes (damaging to skin); minimal odor; must wear appliance 24/7. |
|
Ascending colostomy |
Liquid |
None |
High enzymes; odorous; requires skin protection. |
|
Transverse colostomy |
Mushy |
None |
Malodorous; "mushy" because some water is reabsorbed. |
|
Descending colostomy |
Semi-solid |
Increasing |
More formed as water is reabsorbed. |
|
Sigmoid colostomy |
Formed/Normal |
Possible |
May not require an appliance at all times; odors are easily controlled. |
Note: Over time, the remaining colon compensates by absorbing more water, which may cause stool to become more formed even in transverse ostomies.
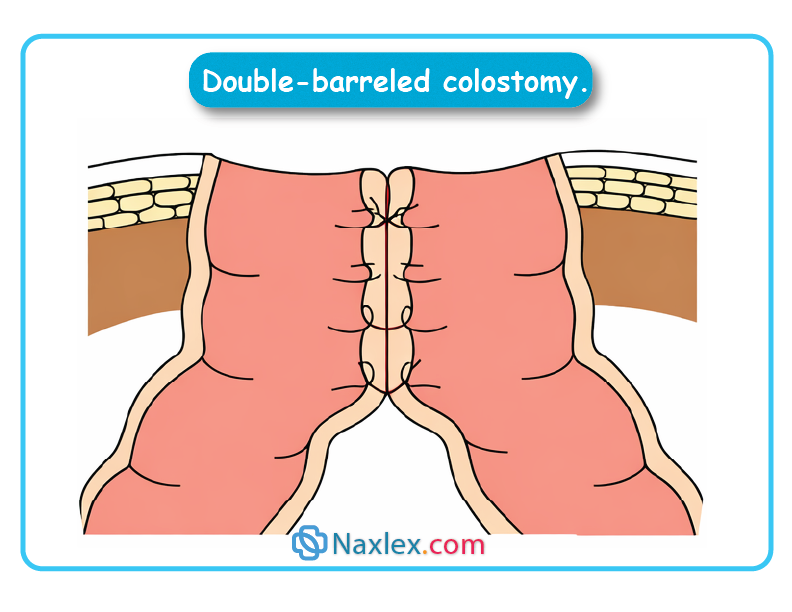
Surgical construction of the stoma
- Single (End/Terminal) Stoma: One end of the bowel is brought to the surface. Usually permanent.
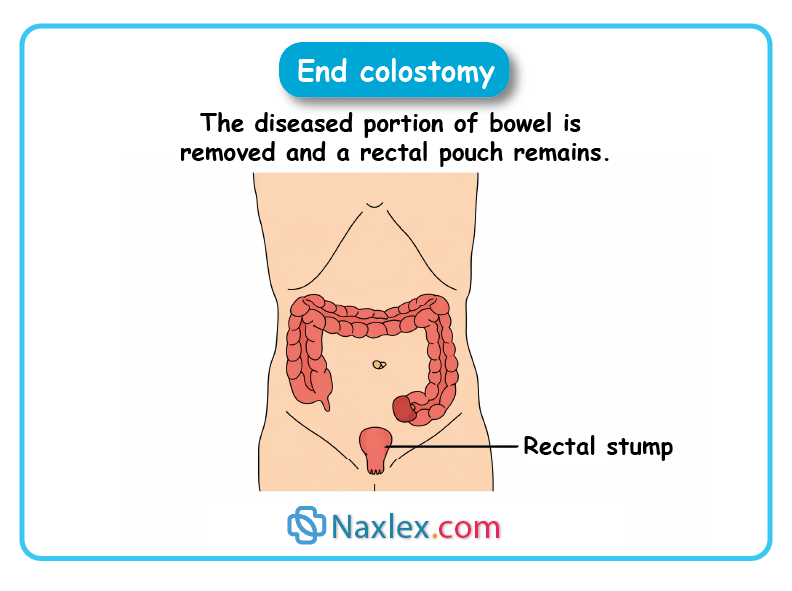
- Loop Stoma: A loop of bowel is pulled out and supported by a bridge/tube.
- Proximal (Afferent) end: Active (drains feces).
- Distal (Efferent) end: Inactive.
- Often an emergency procedure; bulky and harder to manage.
- Divided Colostomy: Two separate stomas are created.
- Proximal end: Drains feces.
- Distal end (Mucous Fistula): Secretes only mucus. Prevents feces from entering the distal bowel.
- Double-Barreled Colostomy: Proximal and distal loops are sutured together for ~10 cm, and both ends are brought to the surface, resembling a double-barreled shotgun.
Nursing insight: Skin Integrity
Because Ileostomy and Ascending Colostomy drainage contains digestive enzymes, these patients are at the highest risk for peristomal skin breakdown. Maintaining a secure seal and using skin barriers is a priority nursing intervention.
Nursing management of fecal elimination
1.1. Nursing Assessment
Assessment is a multi-step process involving the collection of subjective and objective data.
1. Nursing history
The goal is to determine the client's normal pattern and identify changes.
- Key areas: Usual feces description, recent changes, past/current problems, presence of an ostomy, and factors influencing elimination.
- Influencing factors:
- Diet: Fiber intake, regular meal times, and trigger foods.
- Fluid: Amount and type of daily intake.
- Exercise: Daily activity patterns (affects peristalsis).
- Medications: Use of iron, antibiotics, or laxatives.
- Stress: Impact on defecation frequency or consistency.
2. Physical examination
- Abdomen: Follow a specific sequence: inspection, auscultation, percussion and palpation.
- Note: Auscultation must precede palpation because touching the abdomen can alter bowel sounds (peristalsis).
- Rectum/Anus: Inspection and palpation for abnormalities.
3. Fecal Inspection
Observe for:
- Color, Consistency, and Shape.
- Amount and Odor.
- Abnormal constituents: Blood, pus, excessive mucus, or parasites.
1.2. Nursing Diagnosis (NANDA-I)
Common diagnostic labels include:
- Bowel Incontinence
- Constipation / Risk for Constipation / Perceived Constipation
- Diarrhea
- Dysfunctional Gastrointestinal Motility
Related diagnoses (Etiologies):
- Skin integrity: Risk for breakdown due to diarrhea or incontinence.
- Fluid/electrolytes: Risk for imbalance due to prolonged diarrhea or ostomy loss.
- Psychosocial: Situational Low Self-Esteem or Disturbed Body Image (often related to ostomies).
1.3. Planning and Goals
The primary objectives for the client are:
- Maintain or restore normal bowel patterns.
- Maintain/regain normal stool consistency.
- Prevent risks: Fluid/electrolyte imbalance, skin breakdown, and pain.
1.4. Nursing Implementation
1. Promoting regular defecation
- Privacy: Essential for relaxation; stay only if the client is a fall risk.
- Timing: Encourage defecation when the urge is felt (often after meals due to the gastrocolic reflex).
- Positioning: Squatting or leaning forward is best. For bedbound clients, use a bedpan (regular or slipper/fracture pan).
- Exercise: Use isometric abdominal and thigh-strengthening exercises for weak/immobile clients.
2. Dietary interventions
|
Condition |
Intervention |
|
Constipation |
Increase fiber (bran, whole grains, fruit) and hot/warm fluids (lemon water, prune juice). |
|
Diarrhea |
Bland foods, small frequent meals; avoid excessively hot/cold fluids and high-fiber/spiced foods. |
|
Flatulence |
Avoid gas-forming foods (cabbage, beans, onions), straws, and carbonated drinks. |
3. Medications
- Cathartics/laxatives: Induce defecation. Warning: Chronic use weakens natural reflexes.
- Antidiarrheals: Slow motility or absorb excess fluid.
- Antiflatulents: (e.g., Simethicone) Coalesce gas bubbles to ease passage.
4. Enemas
Solutions introduced into the rectum to increase peristalsis.
- Cleansing: Removes feces (High: cleanses entire colon; Low: cleanses rectum/sigmoid).
- Carminative: Used to expel flatus (60–80 mL).
- Retention: Oil or medication retained for 1–3 hours to soften stool or treat infection.
- Return-Flow (Harris Flush): Alternating flow to expel gas.
5. Digital removal of fecal impaction
Digital removal is the manual breaking up and extraction of hardened stool. It is a sensitive procedure with significant physiological risks.
i. Clinical precautions
- Vagal response: Rectal stimulation can trigger the vagus nerve, causing a sudden drop in heart rate (bradycardia) or cardiac arrhythmias.
- Contraindications: Use extreme caution or consult a provider for clients with a history of cardiac disease or dysrhythmias.
- Tissue Integrity: The bowel mucosa is fragile; digital removal can cause injury or bleeding.
ii. Procedure highlights
- Pre-treatment: Administer an oil retention enema 30 minutes prior to soften the mass.
- Pain Management: If permitted, apply 1–2 mL of lidocaine (Xylocaine) gel 5 minutes before the procedure.
- Positioning: Left or Right side-lying with knees flexed. (Right side uses gravity; Left side offers direct access to the sigmoid colon).
- Technique: Use a lubricated, gloved index finger. Move stool downward in small portions.
- Monitoring: Periodically check for signs of fatigue, pallor, diaphoresis (sweating), or pulse changes.
6. Bowel training programs
Designed for clients with chronic constipation, frequent impaction, or fecal incontinence to establish a predictable defecation pattern.
1. The plan (Lifestyle adjustments)
- Fluids: 2,500 to 3,000 mL per day.
- Nutrition: High-fiber diet and hot drinks before usual defecation time.
- Exercise: Increased physical activity.
2. Daily routine (Lasting 2–3 Weeks)
- Stimulation: Administer a cathartic suppository (e.g., Dulcolax) 30 minutes before the target time.
- Privacy: Provide 30–40 minutes of uninterrupted time.
- Positioning: Teach the client to lean forward and apply abdominal pressure (avoiding excessive straining/Valsalva).
7. Fecal incontinence management
a. Incontinence pouch
Used for large volumes of liquid stool to prevent skin breakdown (excoriation).
- Advantage: Replaces the use of rectal Foley catheters, which can damage the anal sphincter.
- Maintenance: Change every 72 hours or sooner if leaking.

b. Artificial Bowel Sphincter
A surgical implant consisting of a cuff, a pressure-regulating balloon, and a pump.
- Function: The cuff remains inflated to maintain continence and is manually deflated to allow defecation. It automatically reinflates after 10 minutes.
- Nursing Alert: Enemas and rectal meds may be contraindicated; always check the manufacturer's guide.
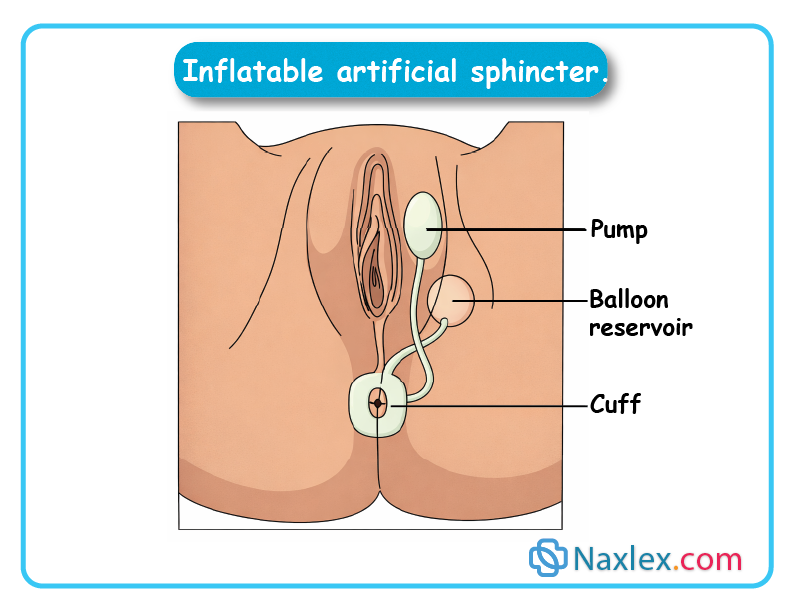
8. Ostomy management
Nursing care focuses on skin integrity, odor control, and psychological support.
a. Stoma and skin care
- Stoma Appearance: Should be moist and reddish-pink.
- Peristomal Skin: Must be assessed for irritation, especially with ileostomies (liquid output contains caustic digestive enzymes).
- Application: The skin barrier (wafer) is cut to fit the stoma size to prevent stool-to-skin contact.
- Pouches can be closed or drainable
- A drainable pouch usually has a clip where the end of the pouch is folded over the clamp and clipped. Newer drainable pouches have an integrated closure system instead of a clamp. The client folds up the end of the pouch three times and presses firmly to seal the pouch. Drainable pouches are usually used by people who need to empty the pouch more than twice a day.
- Closed pouches are often used by people who have a regular stoma discharge (e.g., sigmoid colostomy) and only have to empty the pouch 1 or 2 times a day. Some people find it easier to change a closed pouch than emptying a drainable pouch, which requires some dexterity.
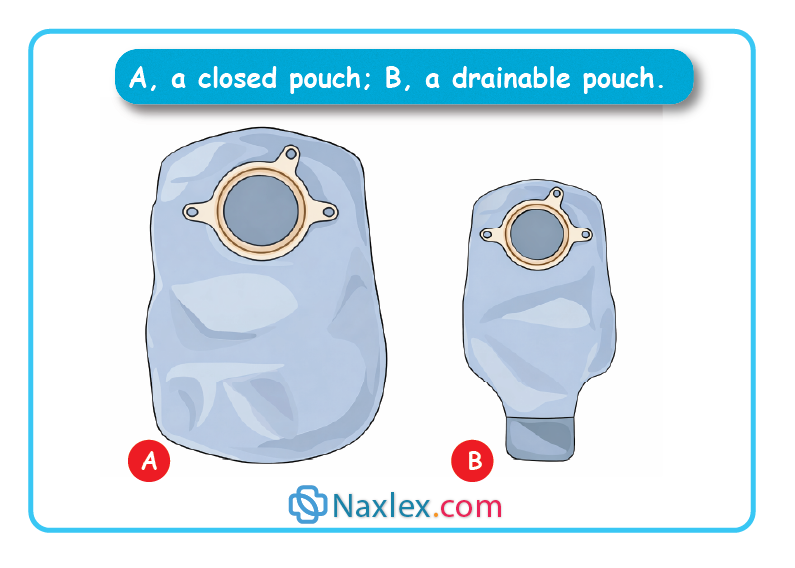
b. Appliance management
- Emptying: Drain when the pouch is 1/3 to 1/2 full to prevent the weight from pulling the seal off the skin.
- Changing: Usually every 3 to 7 days.
- Odor Control: Use odor-barrier pouches or internal charcoal filters.
c. Colostomy irrigation
- Indications: Only for sigmoid or descending colostomies.
- Goal: To stimulate peristalsis so the client can eventually stop wearing a pouch between irrigations.
- Requirements: Requires 300–1,000 mL of fluid, a specialized irrigation cone, and approximately 60 minutes of time.
9. Psychosocial Considerations
- Sensitivity: Nurses must maintain a matter-of-fact facial expression to avoid conveying disgust, which can trigger shame or trauma in the client.
- Support: Refer clients to Wound Ostomy Continence Nurses (WOCN) or support groups like the United Ostomy Associations of America.
1.5. Evaluating
The goals established during the planning phase are evaluated according to specific desired outcomes, also established in that phase. If outcomes are not achieved, the nurse should explore the reasons. The nurse might consider some or all of the following questions:
-
- Were the client’s fluid intake and diet appropriate?
- Was the client’s activity level appropriate?
- Are prescribed medications or other factors affecting the gastrointestinal function?
- Do the client and family understand the provided instructions well enough to comply with the required therapy?
- Were sufficient physical and emotional support provided?
Skills
1.1 SKILL I: Administering an Enema
1. Purpose and types of enemas
Enemas are used to instill fluid into the rectum and sigmoid colon to achieve specific clinical outcomes.
|
Type |
Primary purpose |
Key characteristics |
|
Cleansing |
Remove feces |
Stimulates peristalsis through volume and irritants. |
|
Carminative |
Expel flatus (gas) |
Instills 60–80 mL to distend the rectum and trigger gas release. |
|
Retention |
Soften stool/Medicate |
Liquid is held for 1–3 hours. Oil softens feces; antibiotics treat local infection. |
|
Return-Flow (Harris Flush) |
Expel flatus |
Alternates 100–200 mL of fluid in and out (5–6 times) to stimulate peristalsis. |
2. Assessment & planning
Pre-procedure assessment
- Bowel history: Last BM, amount, color, and consistency.
- Physical: Presence of abdominal distention.
- Functional: Sphincter control and mobility (toilet vs. bedpan).
- Medical history: Check for kidney or cardiac disease (contraindicates certain hypertonic/hypotonic solutions).
Holistic considerations
- Privacy & trauma: Procedures involving body orifices can trigger memories of past abuse. Monitor for emotional responses.
- Cultural sensitivity: Consider gender preferences of the caregiver and personal space.
- Delegation: UAPs can perform some enemas, but the nurse must interpret abnormal findings (e.g., resistance, inability to retain).
3. Implementation: Step-by-Step
Preparation
- Lubricate: Apply water-soluble lubricant to about 5 cm (2 in.) of the tube.
- Prime Tubing: Run solution through to expel air (prevents unnecessary distention).
- Identify & Explain: Verify identity, explain the feeling of "fullness," and the need to retain fluid.
Performance
- Positioning: Place client in Left Lateral (Sims') position with the right leg acutely flexed.
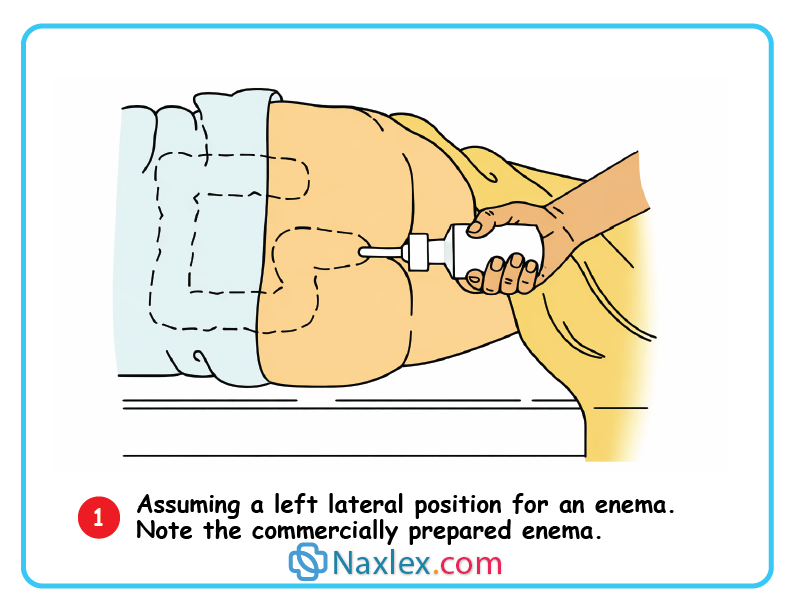
- Insertion:
- Lift the upper buttock for visualization.
- Insert tube smoothly toward the umbilicus (belly button).
- Length: 7–10 cm (3–4 in.) for adults.
- Clinical Tip: If resistance is met, ask the client to deep breathe and run a small amount of fluid to relax the sphincter. Never force.
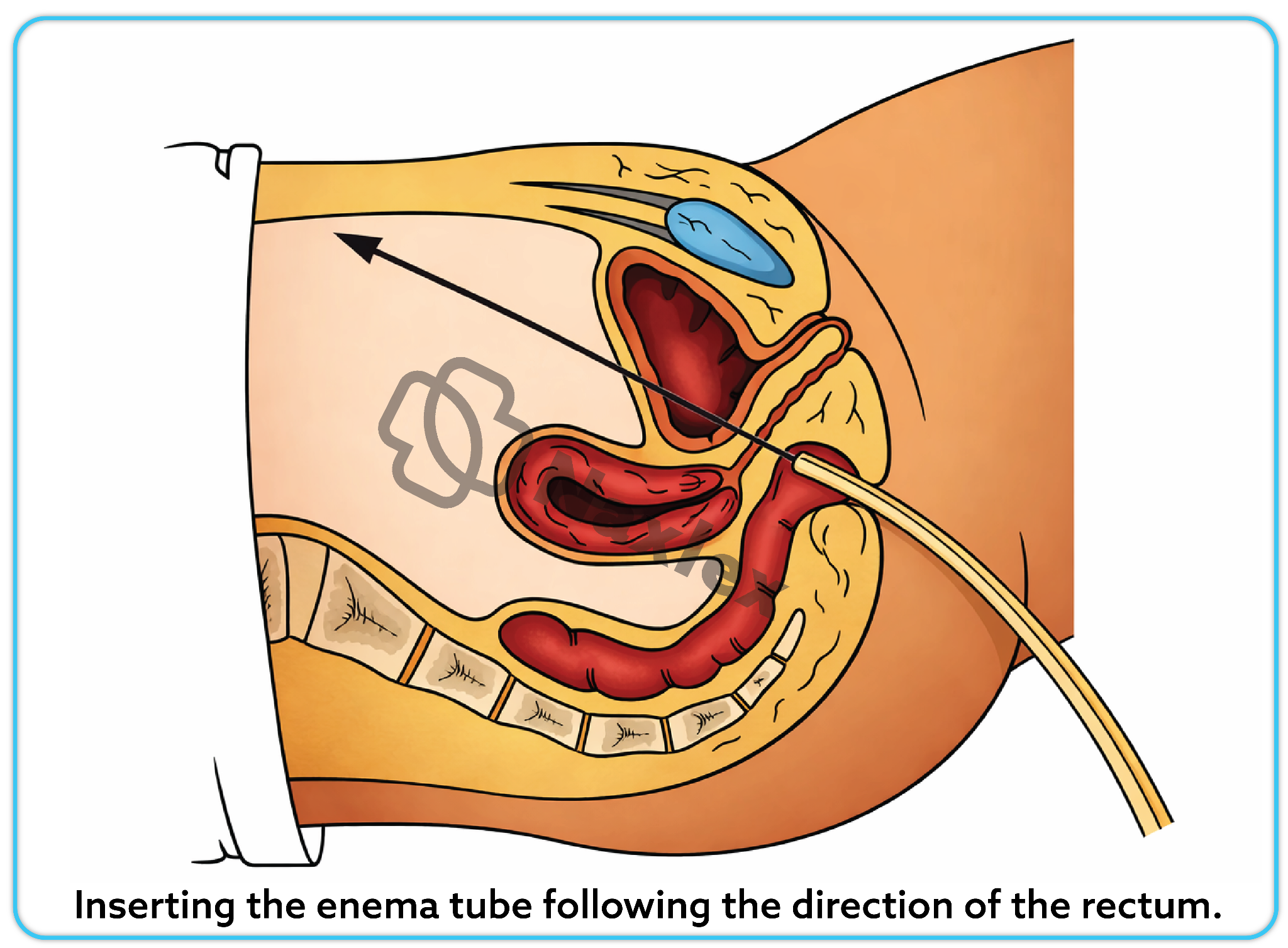
- Administration:
- Height: Hold large-volume bags 30 cm (12 in.) above the rectum for low enemas; 30–49 cm (12–18 in.) for high enemas.
- Flow Rate: If pain/cramping occurs, lower the bag or clamp for 30 seconds, then restart slower.
- Small-Volume: Roll up the plastic container as it empties to prevent suctioning back fluid.
- Completion:
- Withdraw the tube into a paper towel once the container is empty or the client cannot hold more.
- Encourage the client to remain lying down to help retain the fluid.
4. Evaluation and documentation
- Defecation: Assist to a sitting position (facilitates bowel movement).
- Observation: Inspect the results (color, consistency, amount) before the toilet is flushed.
- Documentation: Record the type of enema, volume used, client tolerance, and the character of the return.
Clinical alert
Some clients may prefer to self-administer. The nurse should validate the client’s technique and provide assistance as necessary.
1.2 SKILL II: Changing a Bowel diversion ostomy appliance
1. Purpose of care
- Skin Integrity: To assess and protect the peristomal skin from irritation.
- Assessment: To monitor the amount and type of fecal output.
- Psychosocial: To minimize odors and support the client's body image and self-esteem.
2. Assessment
Stoma assessment
- Color: Should be red and moist (like the inside of a cheek).
- Warning: Pale, dusky, blue, or purple hues indicate impaired circulation. Notify the surgeon immediately.
- Size/shape: New stomas are swollen for 2–6 weeks. Persistent swelling may indicate a blockage.
- Bleeding: Slight bleeding when touched is normal; significant bleeding is not.
Peristomal skin & output
- Skin: Check the 5–13 cm (2–5 in.) area around the stoma for redness or ulceration. A burning sensation often signals skin breakdown.
- Feces: Note the color, consistency, and odor. Watch for pus or blood.
- Emotional Status: Evaluate how the client is coping with body image changes and their readiness to learn self-care.
3. Planning & delegation
- Timing: Change the appliance when the bowel is least active:
- First thing in the morning.
- 2 to 4 hours after meals.
- Avoid: Meal times or immediately after medications that stimulate the bowel.
- Delegation: New ostomies: Must be cared for by a Registered Nurse.
- Established ostomies: In some agencies, UAPs may replace well-established appliances.
4. Implementation (Performance steps)
Removal and cleaning
- Positioning: Sitting or standing is preferred to avoid skin wrinkles during application.
- Empty first: Empty the pouch before removal to prevent spillage. Save the clamp if it is reusable.
- Removal: Push the skin away from the barrier slowly, working from the top down.
- Cleaning: Use warm water and a washcloth. Avoid moisturizing or deodorant soaps, as they interfere with adhesive.
- Preparation: Place a gauze pad over the stoma to absorb seepage while the skin dries.
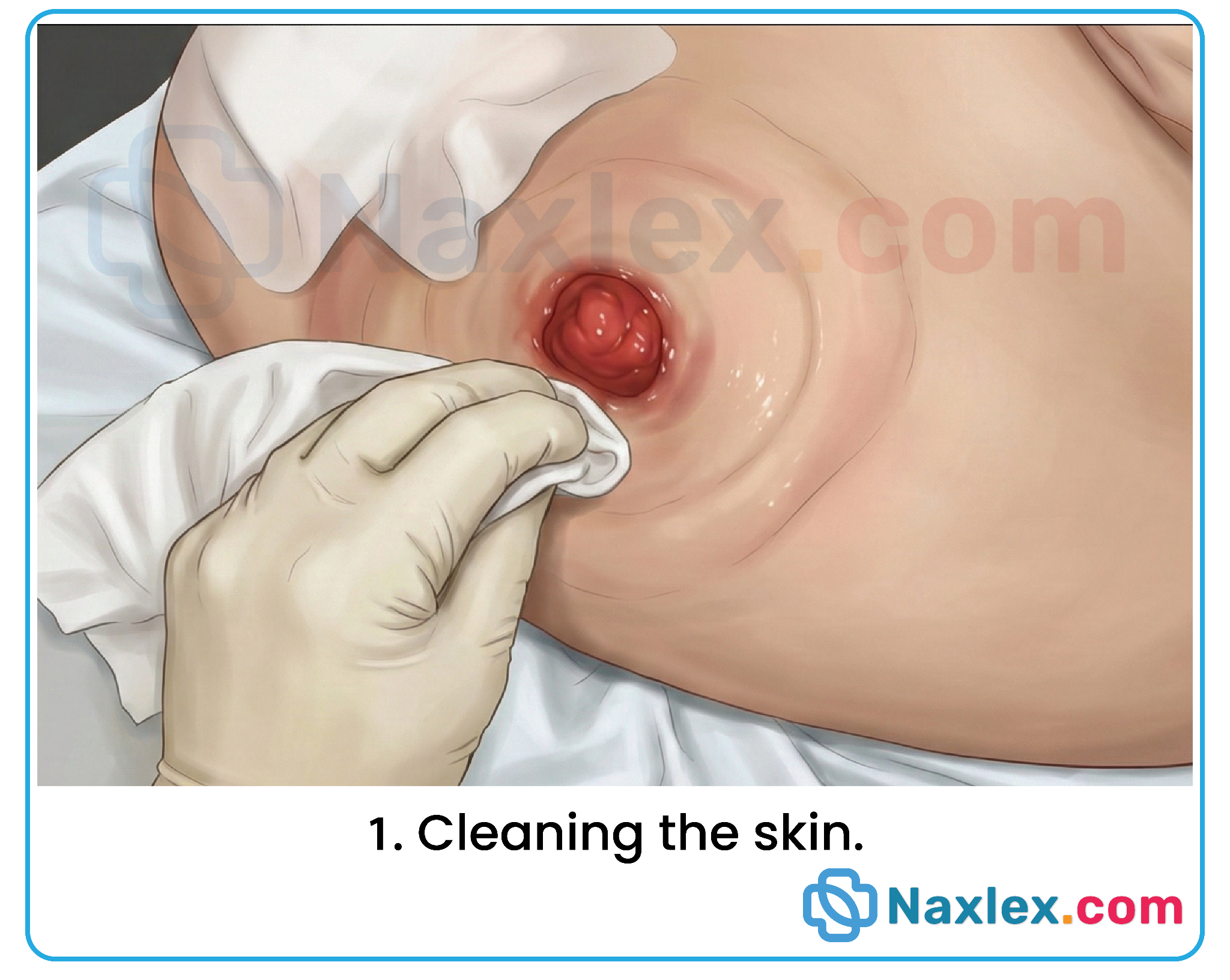
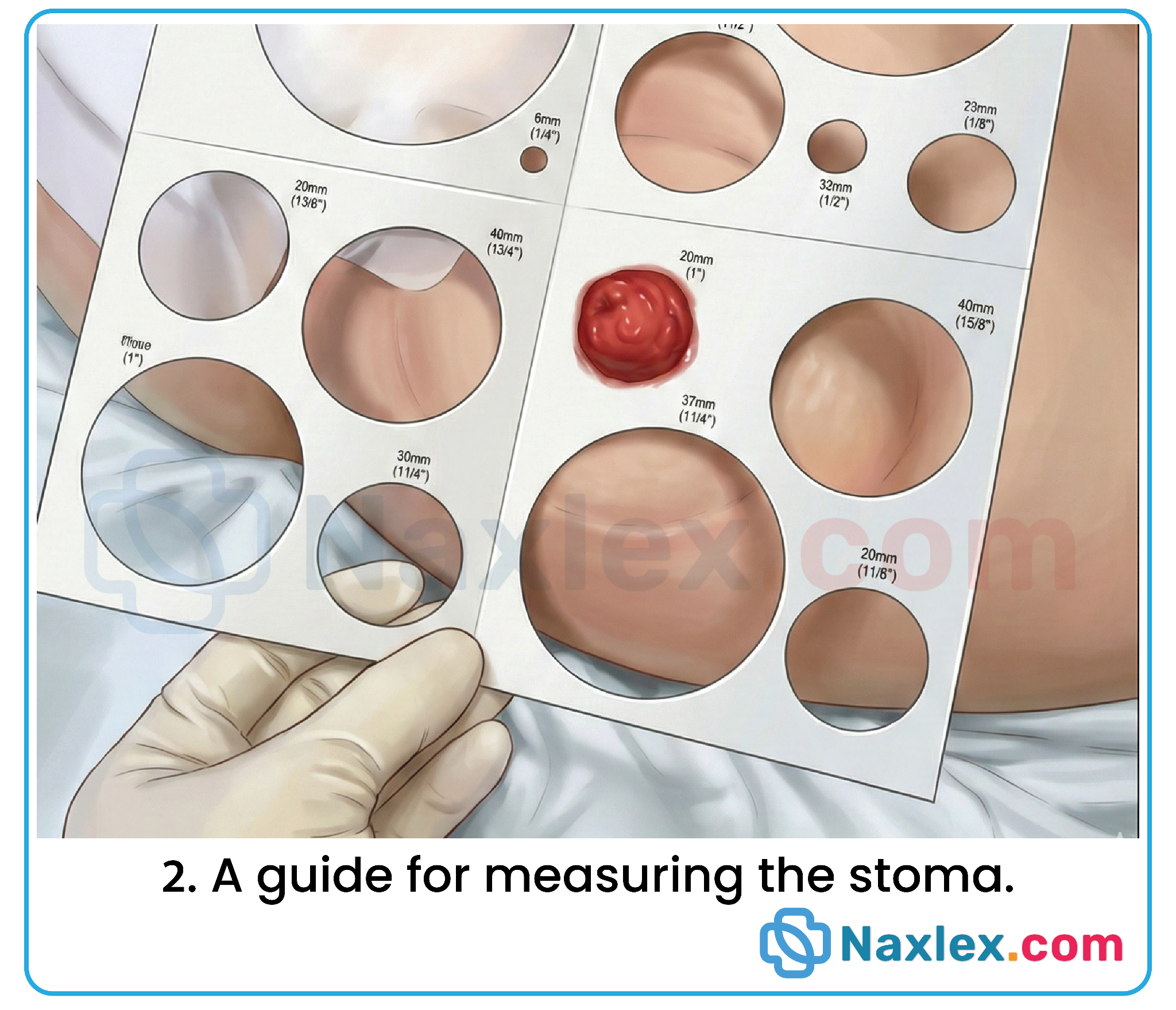
Applying the new appliance
- Measure: Use a measuring guide. The opening should be no more than 1/8 inch larger than the stoma. This prevents stool from touching the skin while allowing the stoma to expand.
- Apply barrier: Trace the size on the backing, cut, and remove the adhesive cover.
- Secure: One-piece: Center over the stoma and press for 30 seconds.
- Two-piece: Apply the skin barrier (wafer) first, then snap the pouch onto the flange. Heat and pressure from your hand activate the adhesive.
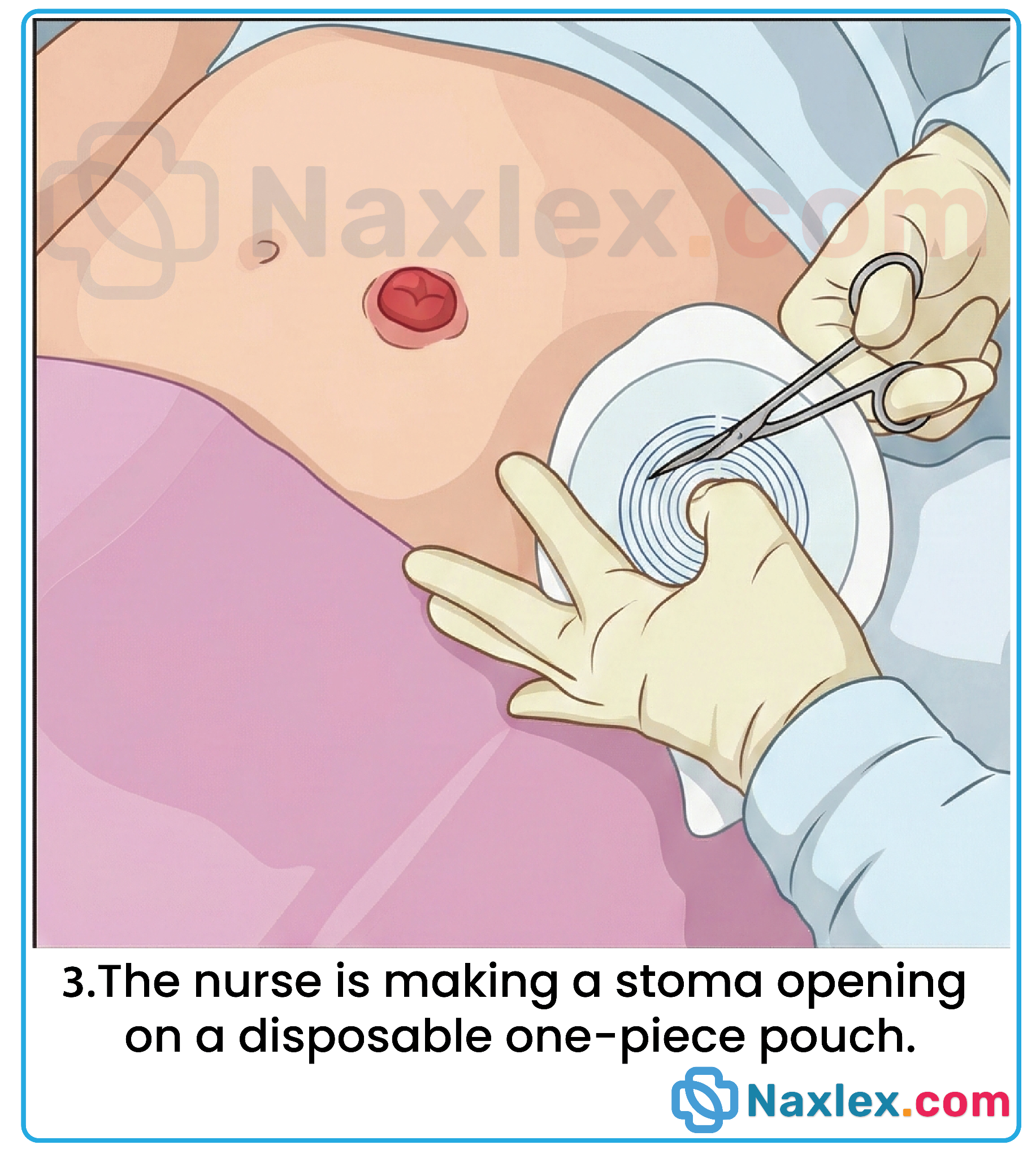
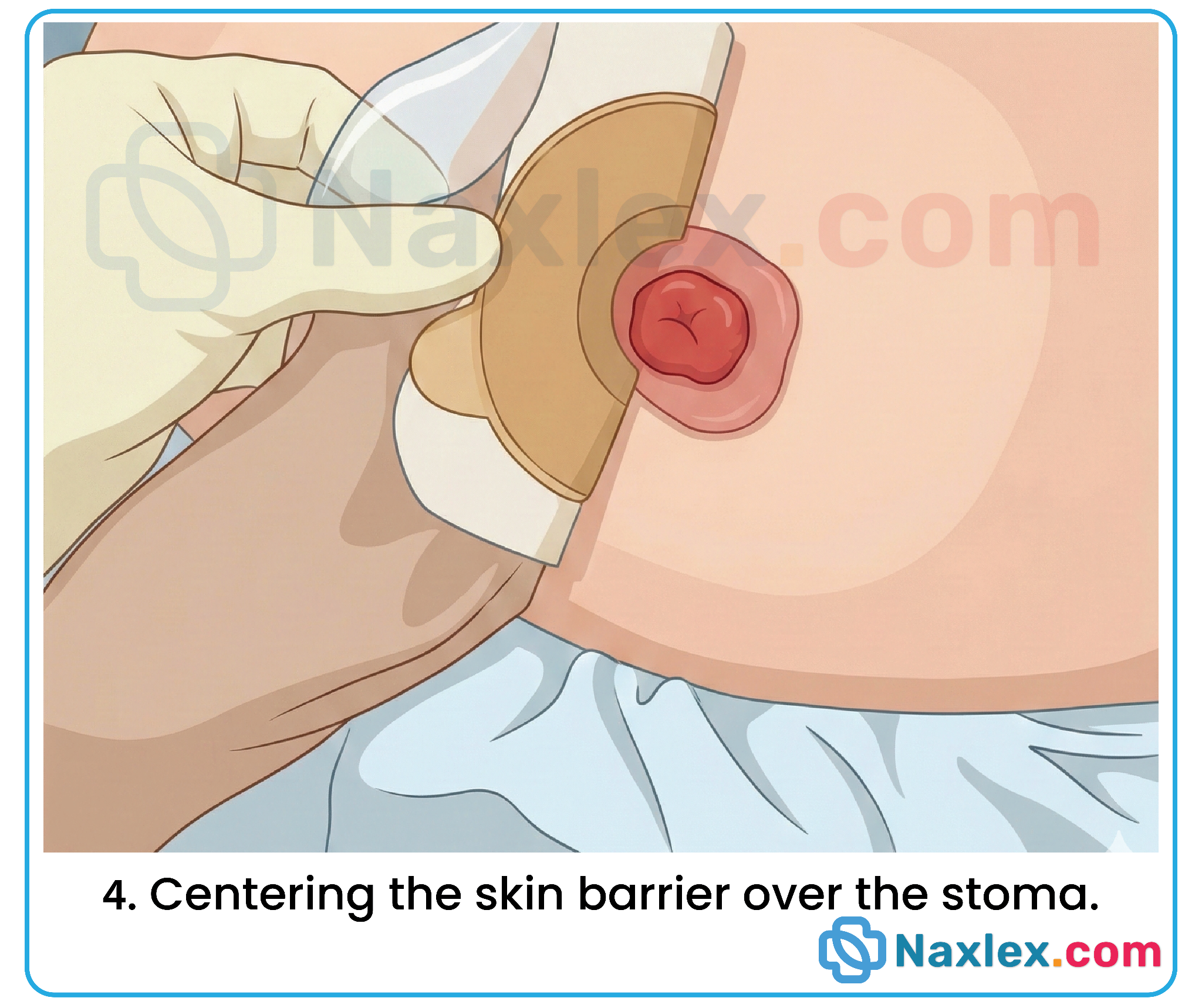

5. Maintenance: Emptying a drainable pouch
- When: Empty when 1/3 to 1/2 full of stool or gas to prevent the weight from breaking the seal.
- Cleaning: After draining, wipe the inside of the pouch tail with tissue before re-clamping to maintain cleanliness and odor control.
6. Documentation
Always record:
- Stoma appearance (color/size) and peristomal skin condition.
- Characteristics of the stool (amount, color, consistency).
- The client's reaction and any self-care skills they demonstrated.
Summary
- Primary functions of the large intestine are the absorption of water and nutrients, the mucoid protection of the intestinal wall, and fecal elimination.
- Patterns of fecal elimination vary greatly among people, but a regular pattern of fecal elimination with formed, soft stools is essential to health and a sense of well-being. to health and a sense of well-being.
- Various factors affect defecation: developmental level, diet, fluid intake, activity and exercise, psychological factors, defecation habits, medications, diagnostic and medical procedures, pathologic conditions, and pain.
- Common fecal elimination problems include constipation, diarrhea, bowel incontinence, and flatulence. Each has specific defining characteristics and contributing causes that often relate to or are identical to the factors that affect defecation.
- Normal defecation is often facilitated in both well and ill clients by providing privacy, teaching clients to attend to defecation urges promptly, assisting clients to normal sitting positions whenever possible, encouraging appropriate food and fluid intake, and scheduling regular exercise.
- Nursing strategies include administering cathartics and antidiarrheals; administering cleansing, carminative, retention, or return flow enemas; applying protective skin agents; monitoring fluid and electrolyte balance; and instructing clients in ways to promote normal defecation.
- The purpose of an enema is to increase peristalsis and the excretion of feces and flatus. Enemas are classified into four groups: cleansing, carminative, retention, and return-flow enemas.
- Digital removal of an impaction should be carried out gently because of vagal nerve stimulation and subsequent depressed cardiac rate. A primary care provider’s order is often necessary.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Bowel elimination
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


