Hesi rn medical surgical proctored exam (cardiac)
Total Questions : 58
Showing 10 questions, Sign in for moreA 57-year-old male client is brought to the emergency department (ED) by emergency medical services (EMS) with reports of chest pain. Client was mowing his lawn and noticed chest pain presenting as tightness and pressure. The pain continued to increase over about 30 minutes when the client decided to rest. The client's wife called emergency medical services (EMS) when the pain was unrelieved after 20 minutes of rest. Client reports no other incidents of experiencing this pain. His medical history includes hypertension, obesity, and a 20 year history of smoking, having quit about 5 years ago. Takes metoprolol succinate ER 25 mg PO.
1230:
The client presents to the emergency department (ED) after arrival via emergency medical services (EMS) with reports on increasing chest pain.
Neurological: Alert and oriented to person, place, time, and situation. Agitated. Denies headaches.
Cardiovascular: Reported chest pain described as pressure and tightness that is unrelieved with rest. Rapid regular rhythm. Normal heart tones. Radial and pedal pulses 2+. Capillary refill 2 seconds.
Respiratory: Rapid and shallow breaths. Clear breath sounds throughout bilateral lungs.
Gastrointestinal: Within normal limits (WNL).
Genitourinary: WNL.
Musculoskeletal: WNL
Pain: Reported 7 on a 0 to 10 scale, tightness and pressure in chest. Started approximately 2 hours ago and got progressively worse, unrelieved by rest.
1230:
- Temperature: 98.1° F (36.7° C) orally
- Heart rate: 121 beats/minute
- Respirations: 21 breaths/minute
- Blood pressure: 162/98 mm Hg
- Oxygen saturation: 92% on room air
- Body mass index (BMI): 32 Kg/m2 (normal 18 to 24.9 kg/m2)
- Pain: 7 on a 0 to 10 scale, tightness and pressure in chest
Click to highlight the findings that require follow up.
Neurological: Alert and oriented person, place, time, and situation Agitated. Denies headaches.
Cardiovascular: Reported chest pain described as pressure and tightness that is unrelieved with rest. Rapid regular rhythm. Normal heart tones. Radial and pedal pulses 2+. Capillary refill 2 seconds.
Respiratory: Rapid and shallow breaths. Clear breath sounds throughout bilateral lungs.
Gastrointestinal: Within normal limits (WNL).
Genitourinary: WNL.
Musculoskeletal M/MIL
Pain: Reported 7 on a 0 to 10 scale, tightness and pressure in chest. Started approximately 2 hours ago and got progressively worse, unrelieved by rest.
Explanation
- Agitation: Agitation may indicate hypoxia or reduced cerebral perfusion due to cardiac compromise. In a patient with chest pain and borderline hypoxia, it can be an early warning sign of clinical deterioration that requires follow-up.
- Chest pain described as pressure tightness unrelieved by rest: Unrelieved chest pain lasting longer than 20 minutes is strongly suggestive of myocardial infarction rather than stable angina. Immediate cardiac workup and intervention are needed to prevent myocardial damage.
- Pain rated 7/10: A moderate to severe pain rating in the chest warrants urgent evaluation, especially when consistent with cardiac characteristics like tightness and pressure. High pain intensity is often correlated with worsening ischemia.
1230:
The client presents to the emergency department (ED) after arrival via emergency medical services (EMS) with reports on increasing chest pain.
Neurological: Alert and oriented to person, place, time, and situation. Agitated. Denies headaches.
Cardiovascular: Reported chest pain described as pressure and tightness that is unrelieved with rest. Rapid regular rhythm. Normal heart tones. Radial and pedal pulses 2+. Capillary refill 2 seconds.
Respiratory: Rapid and shallow breaths. Clear breath sounds throughout bilateral lungs.
Gastrointestinal: Within normal limits (WNL).
Genitourinary: WNL.
Musculoskeletal: WNL
Pain: Reported 7 on a 0 to 10 scale, tightness and pressure in chest. Started approximately 2 hours ago and got progressively worse, unrelieved by rest.
1250:
A 12-lead electrocardiogram (ECG) is completed. A peripheral IV (PIV) catheter is placed in the left forearm. Laboratory specimens are collected. Applied 2 L/minute oxygen via nasal cannula to maintain oxygen saturation greater than 94%.
12-lead electrocardiogram (ECG)
Prothrombin time (PT), international normalized ratio (INR), troponin T, troponin I, C-reactive protein, cholesterol, triglycerides, high-density lipoproteins (HDL), low-density lipoproteins (LDL)
Titrate oxygen via nasal cannula to maintain oxygen saturation greater than 94%
Insert peripheral IV (PIV) access device and maintain per unit protocol
A 57-year-old male client is brought to the emergency department (ED) by emergency medical services (EMS) with reports of chest pain. Client was mowing his lawn and noticed chest pain presenting as tightness and pressure. The pain continued to increase over about 30 minutes when the client decided to rest. The client's wife called emergency medical services (EMS) when the pain was unrelieved after 20 minutes of rest. Client reports no other incidents of experiencing this pain. His medical history includes hypertension, obesity, and a 20 year history of smoking, having quit about 5 years ago. Takes metoprolol succinate ER 25 mg PO.
For each assessment finding, click to specify if the finding is consistent with angina or myocardial infarction, or both. Each column must have at least one response option selected.
Explanation
- Epigastric distress: Epigastric discomfort can occur in both angina and myocardial infarction due to referred pain or visceral irritation from ischemia. Clients may confuse this with indigestion, particularly in atypical presentations.
- Occurring without cause: Myocardial infarction pain often occurs suddenly and unpredictably, including during rest or sleep. It is not always precipitated by physical exertion or emotional stress, unlike classic stable angina.
- Pain only relieved by opioids: Myocardial infarction pain is severe and typically not responsive to nitroglycerin alone. Relief often requires opioid analgesics like morphine, which also help reduce cardiac workload.
- Feelings of fear: A sense of impending doom or intense anxiety is commonly reported in both angina and myocardial infarction, likely due to sympathetic nervous system activation during cardiac distress.
- Chest pain radiating down arm: Radiation of pain, especially to the left arm, is classic in both angina and myocardial infarction. It reflects the shared neural pathways between the heart and upper extremity.
- Pain relieved by nitroglycerin: Angina is typically responsive to rest and nitroglycerin, which dilates coronary arteries and reduces oxygen demand. In contrast, MI pain often persists despite nitroglycerin.
A 57-year-old male client is brought to the emergency department (ED) by emergency medical services (EMS) with reports of chest pain. Client was mowing his lawn and noticed chest pain presenting as tightness and pressure. The pain continued to increase over about 30 minutes when the client decided to rest. The client's wife called emergency medical services (EMS) when the pain was unrelieved after 20 minutes of rest. Client reports no other incidents of experiencing this pain. His medical history includes hypertension, obesity, and a 20 year history of smoking, having quit about 5 years ago. Takes metoprolol succinate ER 25 mg PO.
1230:
The client presents to the emergency department (ED) after arrival via emergency medical services (EMS) with reports on increasing chest pain.
Neurological: Alert and oriented to person, place, time, and situation. Agitated. Denies headaches.
Cardiovascular: Reported chest pain described as pressure and tightness that is unrelieved with rest. Rapid regular rhythm. Normal heart tones. Radial and pedal pulses 2+. Capillary refill 2 seconds.
Respiratory: Rapid and shallow breaths. Clear breath sounds throughout bilateral lungs.
Gastrointestinal: Within normal limits (WNL).
Genitourinary: WNL.
Musculoskeletal: WNL
Pain: Reported 7 on a 0 to 10 scale, tightness and pressure in chest. Started approximately 2 hours ago and got progressively worse, unrelieved by rest.
1250:
A 12-lead electrocardiogram (ECG) is completed. A peripheral IV (PIV) catheter is placed in the left forearm. Laboratory specimens are collected. Applied 2 L/minute oxygen via nasal cannula to maintain oxygen saturation greater than 94%.
12-lead electrocardiogram (ECG)
Prothrombin time (PT), international normalized ratio (INR), troponin T, troponin 1, C-reactive protein, cholesterol, triglycerides, high-density lipoproteins (HDL), low-density lipoproteins (LDL)
Titrate oxygen via nasal cannula to maintain oxygen saturation greater than 94%
Insert peripheral IV (PIV) access device and maintain per unit protocol
|
Test |
Result |
Range |
|
Prothrombin time |
12 seconds |
11 to 12.5 seconds |
|
International Normalized ratio |
1.0 |
0.8 to 1.1 |
|
Troponin T |
0.01 ng/mL(0.01 μg/L) |
Less than 0.1 ng/Ml (Less than 0.1 μg/L) |
Initial testing is complete, and the nurse is reviewing the results.
Choose the most likely options for the information missing from the statement by selecting from the lists of options provided.
The nurse determines that the client has
Explanation
• New onset angina: The client’s chest pain is unrelieved by rest and associated with ST depression on ECG. These features indicate myocardial ischemia without infarction, consistent with unstable angina. Since this is the client’s first episode, it is classified as new onset angina, which requires urgent evaluation and treatment.
• Troponin: Troponin is a specific cardiac biomarker that rises in response to myocardial cell injury or infarction. A normal troponin level in the setting of ST depression and chest pain suggests ischemia without necrosis, confirming the diagnosis of angina rather than myocardial infarction.
• ST elevation myocardial infarction: STEMI is diagnosed when there is ST elevation in two or more contiguous ECG leads, accompanied by elevated cardiac markers. The client’s ECG shows ST depression, not elevation, and his troponin is normal, making STEMI unlikely.
• Chronic stable angina: Chronic stable angina occurs with predictable exertion and is typically relieved by rest or nitroglycerin. This client’s pain worsened over 30 minutes and was not relieved by rest, indicating unstable rather than stable angina.
• prothrombin: Prothrombin time reflects clotting ability, not cardiac ischemia. While important in evaluating bleeding risks or anticoagulation status, it is not relevant in diagnosing angina or MI.
• INR: INR is used to monitor anticoagulation therapy, especially in clients on warfarin. It does not indicate myocardial injury or help confirm ischemia or infarction. The client’s INR is normal and unrelated to the chest pain evaluation.
A 57-year-old male client is brought to the emergency department (ED) by emergency medical services (EMS) with reports of chest pain. Client was mowing his lawn and noticed chest pain presenting as tightness and pressure. The pain continued to increase over about 30 minutes when the client decided to rest. The client's wife called emergency medical services (EMS) when the pain was unrelieved after 20 minutes of rest. Client reports no other incidents of experiencing this pain. His medical history includes hypertension, obesity, and a 20 year history of smoking, having quit about 5 years ago. Takes metoprolol succinate ER 25 mg PO.
1230:
The client presents to the emergency department (ED) after arrival via emergency medical services (EMS) with reports on increasing chest pain.
Neurological: Alert and oriented to person, place, time, and situation. Agitated. Denies headaches.
Cardiovascular: Reported chest pain described as pressure and tightness that is unrelieved with rest. Rapid regular rhythm. Normal heart tones. Radial and pedal pulses 2+. Capillary refill 2 seconds.
Respiratory: Rapid and shallow breaths. Clear breath sounds throughout bilateral lungs.
Gastrointestinal: Within normal limits (WNL).
Genitourinary: WNL.
Musculoskeletal: WNL
Pain: Reported 7 on a 0 to 10 scale, tightness and pressure in chest. Started approximately 2 hours ago and got progressively worse, unrelieved by rest.
1250:
A 12-lead electrocardiogram (ECG) is completed. A peripheral IV (PIV) catheter is placed in the left forearm. Laboratory specimens are collected. Applied 2 L/minute oxygen via nasal cannula to maintain oxygen saturation greater than 94%.
12-lead electrocardiogram (ECG)
Prothrombin time (PT), international normalized ratio (INR), troponin T, troponin 1, C-reactive protein, cholesterol, triglycerides, high-density lipoproteins (HDL), low-density lipoproteins (LDL)
Titrate oxygen via nasal cannula to maintain oxygen saturation greater than 94%
Insert peripheral IV (PIV) access device and maintain per unit protocol
|
Test |
Result |
Range |
|
Prothrombin time |
12 seconds |
11 to 12.5 seconds |
|
International Normalized ratio |
1.0 |
0.8 to 1.1 |
|
Troponin T |
0.01 ng/mL(0.01 μg/L) |
Less than 0.1 ng/Ml (Less than 0.1 μg/L) |
Drag and drop word choices to complete the sentence.
If healthcare providers (HCPs) see a narrowed heart vessel while performing a percutaneous coronary intervention (PCI), they may perform a balloon angioplasty to compress the plaque against the vessel wall and hold it there with a stent, which will lessen
Explanation
- Pain from myocardial ischemia occurs when narrowed coronary arteries restrict blood flow to the heart muscle. PCI with balloon angioplasty and stent placement reopens the blocked artery, restoring oxygen-rich blood and thereby relieving ischemic chest pain symptoms that were previously unrelieved by rest.
- Dysrhythmias often develop as a result of decreased perfusion to the heart’s conduction system during ischemia. By improving blood flow through PCI, the myocardium becomes more electrically stable, reducing the risk of ventricular or atrial dysrhythmias related to oxygen deprivation and myocardial irritability.
- Heart blocks occur when electrical conduction through the heart is delayed or interrupted, often due to damage in the conduction pathways. PCI does not reverse scarring or fibrosis of these pathways and is not a treatment for conduction system abnormalities like AV block unless directly caused by ischemia.
- Palpitations are often caused by a range of factors including anxiety, stimulants, or electrolyte imbalances, in addition to arrhythmias. While some ischemic-related arrhythmias may improve after PCI, palpitations due to non-cardiac or unrelated causes would likely persist despite successful revascularization.
- Shortness of breath can be due to myocardial ischemia, but also stems from pulmonary conditions or left-sided heart failure. Although PCI improves cardiac perfusion, it does not directly resolve fluid overload or pulmonary congestion, which may still contribute to dyspnea even after the intervention.
A 57-year-old male client is brought to the emergency department (ED) by emergency medical services (EMS) with reports of chest pain. Client was mowing his lawn and noticed chest pain presenting as tightness and pressure. The pain continued to increase over about 30 minutes when the client decided to rest. The client's wife called emergency medical services (EMS) when the pain was unrelieved after 20 minutes of rest. Client reports no other incidents of experiencing this pain. His medical history includes hypertension, obesity, and a 20 year history of smoking, having quit about 5 years ago. Takes metoprolol succinate ER 25 mg PO.
1230:
The client presents to the emergency department (ED) after arrival via emergency medical services (EMS) with reports on increasing chest pain.
Neurological: Alert and oriented to person, place, time, and situation. Agitated. Denies headaches.
Cardiovascular: Reported chest pain described as pressure and tightness that is unrelieved with rest. Rapid regular rhythm. Normal heart tones. Radial and pedal pulses 2+. Capillary refill 2 seconds.
Respiratory: Rapid and shallow breaths. Clear breath sounds throughout bilateral lungs.
Gastrointestinal: Within normal limits (WNL).
Genitourinary: WNL.
Musculoskeletal: WNL
Pain: Reported 7 on a 0 to 10 scale, tightness and pressure in chest. Started approximately 2 hours ago and got progressively worse, unrelieved by rest.
1250:
A 12-lead electrocardiogram (ECG) is completed. A peripheral IV (PIV) catheter is placed in the left forearm. Laboratory specimens are collected. Applied 2 L/minute oxygen via nasal cannula to maintain oxygen saturation greater than 94%.
12-lead electrocardiogram (ECG)
Prothrombin time (PT), international normalized ratio (INR), troponin T, troponin 1, C-reactive protein, cholesterol, triglycerides, high-density lipoproteins (HDL), low-density lipoproteins (LDL)
Titrate oxygen via nasal cannula to maintain oxygen saturation greater than 94%
Insert peripheral IV (PIV) access device and maintain per unit protocol
Aspirin 325 mg PO daily
Nitroglycerin 0.3 mg sublingual (SL) every
5 minutes up to 3 times PRN for chest pain
Titrate oxygen via nasal cannula to maintain oxygen saturation greater than94%
1500:
Admit to observation unit
2000:
Lisinopril 40 mg PO daily
|
Test |
Result |
Range |
|
Prothrombin time |
12 seconds |
11 to 12.5 seconds |
|
International Normalized ratio |
1.0 |
0.8 to 1.1 |
|
Troponin T |
0.01 ng/mL(0.01 μg/L) |
Less than 0.1 ng/Ml (Less than 0.1 μg/L) |
For each medication, choose the drug classification and medication action.
Explanation
- Amlodipine: Amlodipine inhibits the influx of calcium ions into vascular smooth muscle and cardiac muscle, leading to vasodilation and reduced blood pressure. It’s used primarily for hypertension and angina.
- Aspirin: Aspirin irreversibly inhibits cyclooxygenase (COX), thereby reducing thromboxane A2 production and platelet aggregation. It lowers the risk of clot formation in clients with suspected myocardial infarction.
- Lisinopril: Lisinopril blocks the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. It lowers blood pressure and reduces afterload, which helps reduce cardiac workload in clients with hypertension or heart failure.
- Nitroglycerin: Nitroglycerin dilates both veins and arteries, particularly the coronary arteries, reducing myocardial oxygen demand and improving oxygen delivery. It’s used to relieve angina and manage acute chest pain.
A 57-year-old male client is brought to the emergency department (ED) by emergency medical services (EMS) with reports of chest pain. Client was mowing his lawn and noticed chest pain presenting as tightness and pressure. The pain continued to increase over about 30 minutes when the client decided to rest. The client's wife called emergency medical services (EMS) when the pain was unrelieved after 20 minutes of rest. Client reports no other incidents of experiencing this pain. His medical history includes hypertension, obesity, and a 20 year history of smoking, having quit about 5 years ago. Takes metoprolol succinate ER 25 mg PO.
1230:
The client presents to the emergency department (ED) after arrival via emergency medical services (EMS) with reports on increasing chest pain.
Neurological: Alert and oriented to person, place, time, and situation. Agitated. Denies headaches.
Cardiovascular: Reported chest pain described as pressure and tightness that is unrelieved with rest. Rapid regular rhythm. Normal heart tones. Radial and pedal pulses 2+. Capillary refill 2 seconds.
Respiratory: Rapid and shallow breaths. Clear breath sounds throughout bilateral lungs.
Gastrointestinal: Within normal limits (WNL).
Genitourinary: WNL.
Musculoskeletal: WNL
Pain: Reported 7 on a 0 to 10 scale, tightness and pressure in chest. Started approximately 2 hours ago and got progressively worse, unrelieved by rest.
1250:
A 12-lead electrocardiogram (ECG) is completed. A peripheral IV (PIV) catheter is placed in the left forearm. Laboratory specimens are collected. Applied 2 L/minute oxygen via nasal cannula to maintain oxygen saturation greater than 94%.
12-lead electrocardiogram (ECG)
Prothrombin time (PT), international normalized ratio (INR), troponin T, troponin 1, C-reactive protein, cholesterol, triglycerides, high-density lipoproteins (HDL), low-density lipoproteins (LDL)
Titrate oxygen via nasal cannula to maintain oxygen saturation greater than 94%
Insert peripheral IV (PIV) access device and maintain per unit protocol
Aspirin 325 mg PO daily
Nitroglycerin 0.3 mg sublingual (SL) every
5 minutes up to 3 times PRN for chest pain
Titrate oxygen via nasal cannula to maintain oxygen saturation greater than94%
1500:
Admit to observation unit
2000:
Lisinopril 40 mg PO daily
|
Test |
Result |
Range |
|
Prothrombin time |
12 seconds |
11 to 12.5 seconds |
|
International Normalized ratio |
1.0 |
0.8 to 1.1 |
|
Troponin T |
0.01 ng/mL(0.01 μg/L) |
Less than 0.1 ng/Ml (Less than 0.1 μg/L) |
Which 2 statements from the client should the nurse recognize as a need for further education?
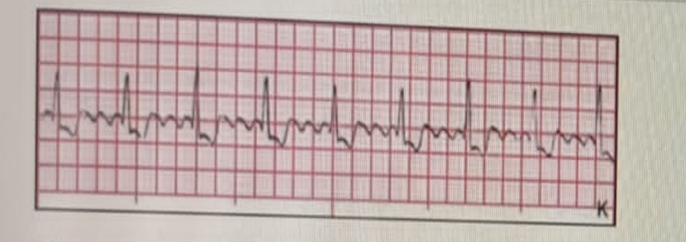
The nurse is monitoring the client's cardiac rhythm. Based on this strip, which is the correct interpretation of this rhythm?
A client collapses while ambulating in the hallway. The nurse calls for help after verifying that the client is not breathing and has no palpable pulse. Which intervention should the nurse implement?
When conducting discharge teaching for a client who has had a mechanical valve replacement, which information should the nurse plan to include?
Admit
Client was admitted to the hospital reporting chest pain. Describes the pain as sharp and rates the pain 8 on a 0 to 10 scale. Informs the location of the pain is in the middle of the chest and radiates down the left arm. 12-lead electrocardiogram (ECG) shows ST segment elevation.
- Temperature: 98.6° F (37° C) orally
- Heart rate: 88 beats/minute
- Respirations: 20 breaths/minute
- Blood pressure: 148/88 mm Hg
The nurse reviews chart data.
Complete the diagram by dragging from the choices area which potential condition the client is experiencing, two actions to take, and two parameters the nurse would monitor.
Explanation
- Myocardial infarction (MI): The client reports chest pain rated 8/10, radiating to the left arm, and has ST segment elevation on ECG. These findings are classic for ST-elevation myocardial infarction (STEMI), requiring immediate intervention.
- Draw laboratory cardiac markers: Troponin and other cardiac enzymes are critical for confirming myocardial injury. They help guide diagnosis, treatment, and monitoring of MI progression or resolution.
- Insert two peripheral IV (PIV) access devices: Dual IV access ensures reliable and rapid administration of emergency medications, fluids, or thrombolytics. This is vital for stabilizing the client during acute cardiac events.
- Pain level: Ongoing pain assessment is essential for monitoring myocardial ischemia, evaluating treatment response, and guiding further interventions to prevent cardiac tissue damage.
- 12-lead electrocardiogram (ECG): Continuous or repeated ECGs help detect changes in ST segments, arrhythmias, or infarct progression. It’s crucial in monitoring the effectiveness of interventions and early detection of complications.
- Reflux: While reflux may cause chest discomfort, it is not associated with ST elevation or arm radiation. These findings are cardiac in nature and point away from gastrointestinal causes.
- Costochondritis: This musculoskeletal condition causes localized chest pain but does not result in ECG changes or radiating pain. It is not supported by the client's data.
- Atrial fibrillation (A-fib): The client has a normal heart rate and regular rhythm. A-fib would show an irregular rhythm on ECG, not ST elevation, and is not the suspected diagnosis here.
- Insert nasogastric tube (NGT) for nutritional intake: An NGT is not a priority for a client with acute chest pain. The focus should be on stabilizing cardiac function rather than nutritional support.
- Consult nutritionist: Nutritional counseling may be relevant later, but it is not an acute intervention during a suspected myocardial infarction.
- Begin strict bedrest: While activity should be limited, “strict bedrest” is not always necessary and may lead to complications like DVT. The client’s mobility orders depend on cardiac stability.
- Intake and output: While important in general care, it is not as immediately critical in early MI management as pain and ECG monitoring.
- Nutritional intake: Nutritional monitoring is not an immediate priority during acute chest pain evaluation and cardiac stabilization.
- Peripheral edema: Edema may indicate chronic heart failure, but it is not a key indicator for acute myocardial infarction or urgent follow-up in this scenario.
Sign Up or Login to view all the 58 Questions on this Exam
Join over 100,000+ nursing students using Naxlex’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now