ICHS (Florida International College of Health Sciences) Med Surg 1 Proctored Exam
ICHS (Florida International College of Health Sciences) Med Surg 1 Proctored Exam
Total Questions : 53
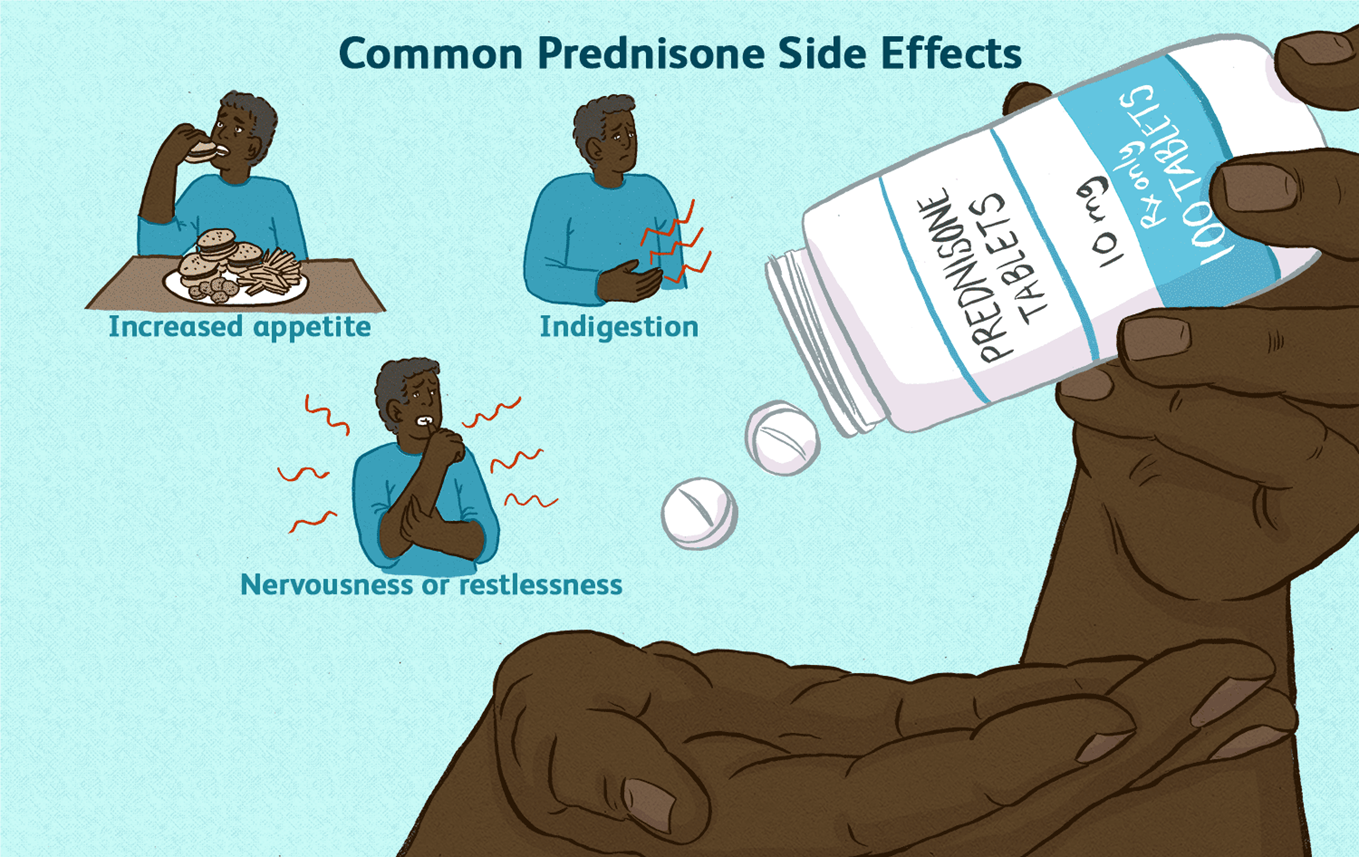
Showing 10 questions Sign up for moreA nurse is educating a client with systemic lupus erythematosus about the use of prednisone. Which piece of information should be prioritized?
Explanation
Choice A rationale:
Prednisone is a corticosteroid that suppresses the body's natural production of cortisol. Cortisol is a hormone that is essential for life, and it plays a role in many important bodily functions, including:
Regulating blood sugar levels Maintaining blood pressure Reducing inflammation Responding to stress
When a person takes prednisone for a long period of time, their body begins to rely on the medication to provide cortisol. If the medication is stopped suddenly, the body cannot produce enough cortisol on its own, which can lead to a life-threatening condition called adrenal insufficiency.
Adrenal insufficiency can cause a variety of symptoms, including: Extreme fatigue
Weakness Dizziness Nausea Vomiting Abdominal pain Confusion
Loss of consciousness
To prevent adrenal insufficiency, it is important to taper off prednisone slowly over a period of time. This allows the body to gradually adjust to producing cortisol on its own.
Here are some additional details about why prednisone should never be discontinued abruptly: The risk of adrenal insufficiency is highest when prednisone has been taken for more than 3 weeks. The longer a person has been taking prednisone, the slower the taper should be.
It is important to follow the tapering instructions provided by the healthcare provider.
If a person experiences any symptoms of adrenal insufficiency, they should seek medical attention immediately.
A nurse has conducted an educational session for a community group on Lyme disease. Which statement by a participant indicates a need for further review of the material?
Explanation
Choice A rationale:
This statement is accurate. Early Lyme disease (Stage I) is typically treated with oral antibiotics for 14 to 21 days. This is often effective in clearing the infection and preventing further complications.
Choice B rationale:
This statement is also accurate. A red rash that may resemble a bull's eye is a common early symptom of Lyme disease. It often appears at the site of the tick bite, typically within 3 to 30 days after the bite.
Choice C rationale:
This statement is incorrect. While Lyme disease can be serious if not treated, it is rarely fatal. Most people who are treated for Lyme disease recover fully. However, if left untreated, it can lead to chronic health problems, such as arthritis, neurological problems, and heart issues.
Choice D rationale:
This statement is accurate. Taking precautions against tick bites is essential for preventing Lyme disease. Ticks are most active during the warmer months, so it's crucial to be vigilant about tick prevention during the spring, summer, and fall.
A nursing manager is worried about the number of infections in the hospital unit. What action by the manager would be most effective in preventing these infections?
Explanation
Choice A rationale:
While promptly removing urinary catheters can reduce the risk of catheter-associated urinary tract infections (CAUTIs), it addresses only one specific type of infection. It doesn't comprehensively address other common healthcare-associated infections (HAIs) like central line-associated bloodstream infections (CLABSIs), surgical site infections (SSIs), ventilator-associated pneumonia (VAP), and Clostridium difficile infections (CDI).
Education about infection control methods, however, encompasses a broader range of preventive measures that can be applied to various HAIs, making it a more effective strategy for overall infection prevention.
Choice C rationale:
Placing patients in appropriate isolation can prevent the spread of infections, but it's a reactive measure that's implemented after an infection has already occurred. It doesn't address the root causes of infections or prevent their occurrence in the first place.
Education about infection control methods, on the other hand, is a proactive approach that aims to prevent infections from happening in the first place by teaching staff about proper hygiene practices, aseptic techniques, and other infection prevention strategies.
Choice D rationale:
Monitoring hand hygiene practices is crucial for infection prevention, but it's only one aspect of a comprehensive infection control program. Education about infection control methods goes beyond hand hygiene and covers various other preventive measures, such as:
Proper use of personal protective equipment (PPE) Aseptic technique during invasive procedures
Proper cleaning and disinfection of equipment and surfaces Proper handling of patient waste
Recognition of signs and symptoms of infection Prompt reporting of potential outbreaks
Therefore, educating staff members about infection control methods is the most effective action the nursing manager can take to prevent infections in the hospital unit because it provides a comprehensive approach to infection prevention, addressing various aspects of HAI prevention and promoting a culture of safety among healthcare staff.
A nurse is caring for an older patient admitted with mild dehydration. What advice should the nurse give to best address this issue?
Explanation
Choice A rationale:
While it's true that dehydration can lead to incontinence, simply stating this fact to the patient doesn't directly address the issue of dehydration. It doesn't provide actionable steps to correct the dehydration.
Incontinence can be a result of dehydration, but addressing the dehydration is the primary concern to prevent further complications.
Providing information about incontinence might be helpful in other contexts, but it's not the most effective advice to address mild dehydration in this specific scenario.
Choice B rationale:
Diuretics promote fluid loss through urination, which can worsen dehydration.
Advising the patient to take a diuretic in the morning would be counterproductive in this case. The goal is to increase fluid intake, not further deplete fluid levels.
It's important to consider the patient's medications and potential interactions before suggesting any changes to their medication regimen.
Choice C rationale:
Regular fluid intake is essential for maintaining hydration and replenishing lost fluids.
This advice directly addresses the issue of dehydration by encouraging the patient to consume fluids consistently. Drinking fluids every 1 to 2 hours can help restore fluid balance and prevent further complications.
It's a simple, actionable, and effective measure to address mild dehydration.
Choice D rationale:
While reducing sodium intake can be beneficial for some individuals with hypertension or other conditions, it's not the most relevant advice for addressing mild dehydration.
Sodium restriction might be appropriate in certain cases, but it doesn't directly address the immediate need to increase fluid intake.
The primary focus in this situation should be on replenishing fluids, not restricting sodium.
A patient is scheduled to receive 2000 ml of Normal Saline over 24 hours. How much fluid should be administered per hour?
Explanation
Rationale:
Step 1: Divide the total volume of fluid (2000 ml) by the total time in hours (24 hours). Step 2: Perform the calculation: 2000 ml ÷ 24 hours = 83.33 ml/hour.
Step 3: Round the answer to the nearest whole number, as fluid administration is typically measured in whole milliliters.
The correct answer is 83 ml/hour.
A nurse is discussing with a colleague who is relocating to a new state and needs to find a new job there. What is the best advice the nurse can give?
Explanation
Choice A rationale:
While working in a facility affiliated with a medical or nursing school can offer opportunities for professional development and collaboration, it is not the most important factor to consider when choosing a new job.
Affiliation with a school does not guarantee a positive work environment, strong nursing leadership, or a commitment to quality patient care, which are all hallmarks of Magnet hospitals.
It's essential to consider other factors that directly impact job satisfaction, patient outcomes, and overall nursing excellence.
Choice B rationale:
Having the latest technology can be beneficial, but it does not ensure a supportive work environment or a high standard of nursing care.
Technology is only one aspect of a hospital's operations, and it should not be the primary focus when making a career decision. It's crucial to prioritize factors that directly influence the quality of nursing practice and patient outcomes.
Choice C rationale:
Inquiring about nurse-client ratios is important, as it can provide insight into the workload and staffing levels at a hospital. However, it's not the most comprehensive indicator of a hospital's commitment to nursing excellence.
Magnet status, in contrast, signifies a broader commitment to quality nursing care, professional development, and positive work environments.
Choice D rationale:
Magnet status is a prestigious designation awarded by the American Nurses Credentialing Center (ANCC) to hospitals that demonstrate excellence in nursing care, leadership, and innovation.
Magnet hospitals are known for:
Attracting and retaining highly qualified nurses Fostering a culture of collaboration and teamwork Investing in professional development and growth
Promoting evidence-based practice and quality improvement Demonstrating outstanding patient outcomes
Seeking employment at a Magnet hospital is strongly recommended for nurses who prioritize professional growth, job satisfaction, and the delivery of exceptional patient care.
A patient diagnosed with HIV-II is admitted to the hospital presenting symptoms of fever, night sweats, and a severe cough.
The laboratory results show a CD4+ cell count of 180/mm and a negative tuberculosis (TB) skin test conducted 4 days prior.
What is the first action the nurse should take?
Explanation
Rationale for Choice A:
While it's important for the primary healthcare provider to be informed about the CD4+ results, it's not the first action the nurse should take. The priority is to implement appropriate infection control measures to protect the patient, other patients, and healthcare staff.
CD4+ cell count is a crucial indicator of the patient's immune status. A count of 180/mm is significantly low, suggesting a weakened immune system and increased vulnerability to infections. However, informing the provider alone doesn't directly address the immediate need for infection control.
Rationale for Choice B:
Airborne Precautions are specifically used for patients with known or suspected airborne infections, such as tuberculosis, measles, or varicella. These precautions involve the use of negative pressure rooms and N95 respirators.
In this case, the patient's TB skin test was negative, indicating no evidence of active tuberculosis infection. Implementing Airborne Precautions unnecessarily could lead to excessive resource utilization and potential stigmatization of the patient.
Rationale for Choice C:
Droplet Precautions are used for patients with infections that can be spread through large respiratory droplets, such as influenza, pertussis, or meningococcal meningitis. These precautions involve the use of masks and eye protection.
While the patient's symptoms of fever, night sweats, and severe cough could be consistent with a droplet-spread infection, there's no definitive evidence to support this at the present time. Initiating Droplet Precautions without a clear indication could also lead to unnecessary resource use and potential anxiety for the patient.
Rationale for Choice D:
Standard Precautions are the foundation of infection control and should be used for all patients, regardless of their known or suspected infection status. These precautions include hand hygiene, use of personal protective equipment (PPE) when indicated, and safe handling of sharps and bodily fluids.
By implementing Standard Precautions, the nurse can effectively minimize the risk of transmission of pathogens, protecting both the patient and other individuals in the healthcare setting. This is the most appropriate first action to ensure a safe and appropriate level of care.
A nurse is providing care for a patient who has a methicillin-resistant Staphylococcus aureus (MRSA) infection, which was cultured from the urine. What is the most appropriate action for the nurse to take?
Explanation
Choice A rationale:
Utilizing a respirator when handling urine output is not the most appropriate action for a nurse caring for a patient with MRSA.
MRSA is not typically transmitted through the air, but rather through direct contact with infected wounds or contaminated surfaces.
While a respirator may offer some protection against airborne particles, it is not necessary for routine care of a patient with MRSA.
It is more important to focus on hand hygiene and other infection control measures.
Choice B rationale:
Restricting visitors strictly to immediate family members only is not necessary for a patient with MRSA.
While it is important to limit the number of visitors to reduce the risk of spreading infection, there is no need to restrict visitors to immediate family members only.
Visitors should be instructed on proper hand hygiene and other infection control measures, and they should avoid contact with the patient's wounds or dressings.
Choice C rationale:
Washing hands only after removing gloves post-care is not sufficient for preventing the spread of MRSA. It is important to wash hands before and after any contact with the patient, even when wearing gloves.
This is because gloves can become contaminated with bacteria, and hand washing helps to remove any bacteria that may have gotten on the hands.
Choice D rationale:
Preparing to administer vancomycin is the most appropriate action for a nurse caring for a patient with MRSA. Vancomycin is an antibiotic that is effective against MRSA.
It is often used to treat MRSA infections, and it can help to prevent the infection from spreading.
An elderly patient, who is ambulatory and independent, is admitted to the hospital. What intervention by the nurse would be most effective in preventing falls for this patient?
Explanation
Rationale for Choice A:
Arranging for a bedside commode can be helpful for patients who have difficulty ambulating to the bathroom. However, it is not the most effective intervention for preventing falls in an ambulatory and independent patient. In fact, it could potentially increase the risk of falls if the patient attempts to use the commode without assistance or if they become disoriented in the dark.
Research has shown that bedside commodes are associated with an increased risk of falls in hospitalized patients. This is because patients may try to get out of bed to use the commode without assistance, or they may become disoriented in the dark and fall.
Additionally, bedside commodes can be a tripping hazard, especially for patients with impaired mobility.
Rationale for Choice B:
Ensuring the bathroom light is kept on during the night can help to reduce the risk of falls by making it easier for the patient to see. However, it is not the most effective intervention for preventing falls.
Patients may still fall even if the bathroom light is on, especially if they are weak, unsteady, or have impaired vision. Additionally, keeping the bathroom light on all night can disrupt the patient's sleep, which can also increase the risk of falls.
Rationale for Choice C:
Using side rails to keep the patient in bed is not an effective intervention for preventing falls. In fact, it can actually increase the risk of falls by making it more difficult for the patient to get out of bed safely.
Patients may try to climb over the side rails, which can lead to falls.
Additionally, side rails can restrict the patient's movement and make them feel trapped, which can lead to agitation and an increased risk of falls.
Rationale for Choice D:
Implementing a toileting schedule is the most effective intervention for preventing falls in an ambulatory and independent patient. This is because it helps to reduce the patient's need to get out of bed at night to use the bathroom.
When a patient has a scheduled time to toilet, they are less likely to try to get out of bed on their own and risk a fall. Additionally, a toileting schedule can help to prevent incontinence, which can also lead to falls.
The primary healthcare provider prescribes Hydroxychloroquine for a patient. What information should the nurse include when discussing this medication with the patient?
Explanation
Rationale for Choice A:
Hydroxychloroquine does not typically cause hair loss as a significant side effect. While some anecdotal reports have suggested hair thinning as a possibility, it's not a well-established or common occurrence in clinical studies.
If a patient experiences hair loss while on hydroxychloroquine, it's essential to rule out other potential causes, such as underlying medical conditions, stress, or nutritional deficiencies.
It's also important to note that some individuals may have a personal predisposition to hair loss, and medications can sometimes trigger or exacerbate this issue.
Rationale for Choice B:
Hydroxychloroquine is not known to cause a burst of energy. In fact, some patients may experience fatigue or drowsiness as a side effect.
It's crucial to inform patients about potential side effects to manage expectations and promote adherence to treatment.
If a patient experiences unexpected energy changes while taking hydroxychloroquine, it's essential to report this to their healthcare provider for further evaluation.
Rationale for Choice C:
Hydroxychloroquine is generally recommended to be taken with food or milk to reduce potential gastrointestinal side effects such as nausea and vomiting.
Taking it on an empty stomach could increase the risk of these side effects, which could impact medication adherence and effectiveness.
Rationale for Choice D:
Retinal damage is the most serious adverse effect of hydroxychloroquine. It can lead to irreversible vision loss if not detected and managed early.
Patients taking hydroxychloroquine must undergo regular eye examinations to monitor for any signs of retinal toxicity.
Early detection and prompt discontinuation of the medication can often prevent permanent vision loss.
It's crucial for nurses to educate patients about this potential risk and emphasize the importance of regular eye exams.
You just viewed 10 questions out of the 53 questions on the ICHS (Florida International College of Health Sciences) Med Surg 1 Proctored Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



