A nurse is educating a client with systemic lupus erythematosus about the use of prednisone. Which piece of information should be prioritized?
Prednisone should never be discontinued abruptly.
Long-term effects of prednisone include redistribution of fat.
Prednisone can lead to sodium and fluid retention.
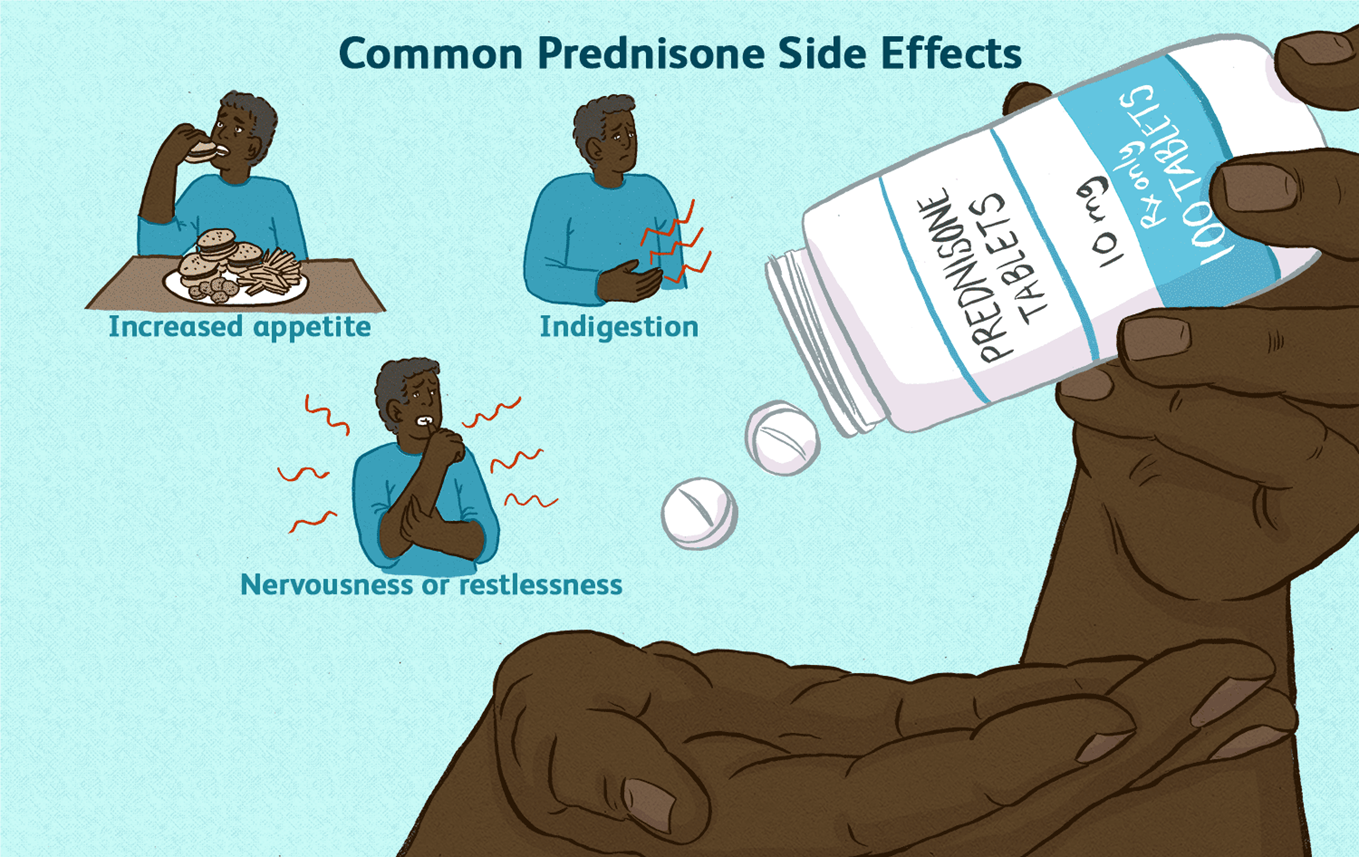
Prednisone might cause the client to feel jittery or nervous.
The Correct Answer is A
Choice A rationale:
Prednisone is a corticosteroid that suppresses the body's natural production of cortisol. Cortisol is a hormone that is essential for life, and it plays a role in many important bodily functions, including:
Regulating blood sugar levels Maintaining blood pressure Reducing inflammation Responding to stress
When a person takes prednisone for a long period of time, their body begins to rely on the medication to provide cortisol. If the medication is stopped suddenly, the body cannot produce enough cortisol on its own, which can lead to a life-threatening condition called adrenal insufficiency.
Adrenal insufficiency can cause a variety of symptoms, including: Extreme fatigue
Weakness Dizziness Nausea Vomiting Abdominal pain Confusion
Loss of consciousness
To prevent adrenal insufficiency, it is important to taper off prednisone slowly over a period of time. This allows the body to gradually adjust to producing cortisol on its own.
Here are some additional details about why prednisone should never be discontinued abruptly: The risk of adrenal insufficiency is highest when prednisone has been taken for more than 3 weeks. The longer a person has been taking prednisone, the slower the taper should be.
It is important to follow the tapering instructions provided by the healthcare provider.
If a person experiences any symptoms of adrenal insufficiency, they should seek medical attention immediately.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
The correct answer is Choice B.
Choice A rationale: Massaging the site with scented oils is not recommended as it may further irritate the inflamed tissue. Additionally, scented oils can cause allergic reactions or skin irritation, worsening the client's discomfort.
Choice B rationale: Applying warm compresses to the site increases blood flow, reduces inflammation, and provides pain relief. Warm compresses also promote healing by improving circulation and reducing edema, making them an appropriate intervention for phlebitis.
Choice C rationale: Administering topical lidocaine to the site is generally not recommended without a prescription. Although it may provide localized pain relief, it can mask underlying issues and delay appropriate medical assessment and treatment.
Choice D rationale: Administering prescribed oral pain medication can provide systemic pain relief. However, it may not be as effective as a localized treatment for reducing inflammation and discomfort at the site of the peripheral vascular access device.
Correct Answer is C
Explanation
Choice A rationale:
While it's true that dehydration can lead to incontinence, simply stating this fact to the patient doesn't directly address the issue of dehydration. It doesn't provide actionable steps to correct the dehydration.
Incontinence can be a result of dehydration, but addressing the dehydration is the primary concern to prevent further complications.
Providing information about incontinence might be helpful in other contexts, but it's not the most effective advice to address mild dehydration in this specific scenario.
Choice B rationale:
Diuretics promote fluid loss through urination, which can worsen dehydration.
Advising the patient to take a diuretic in the morning would be counterproductive in this case. The goal is to increase fluid intake, not further deplete fluid levels.
It's important to consider the patient's medications and potential interactions before suggesting any changes to their medication regimen.
Choice C rationale:
Regular fluid intake is essential for maintaining hydration and replenishing lost fluids.
This advice directly addresses the issue of dehydration by encouraging the patient to consume fluids consistently. Drinking fluids every 1 to 2 hours can help restore fluid balance and prevent further complications.
It's a simple, actionable, and effective measure to address mild dehydration.
Choice D rationale:
While reducing sodium intake can be beneficial for some individuals with hypertension or other conditions, it's not the most relevant advice for addressing mild dehydration.
Sodium restriction might be appropriate in certain cases, but it doesn't directly address the immediate need to increase fluid intake.
The primary focus in this situation should be on replenishing fluids, not restricting sodium.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
