A patient diagnosed with HIV-II is admitted to the hospital presenting symptoms of fever, night sweats, and a severe cough.
The laboratory results show a CD4+ cell count of 180/mm and a negative tuberculosis (TB) skin test conducted 4 days prior.
What is the first action the nurse should take?
Inform the primary health care provider about the CD4+ results.
Implement Airborne Precautions for the patient.
Initiate Droplet Precautions for the patient.
Provide care using Standard Precautions.
The Correct Answer is D
Rationale for Choice A:
While it's important for the primary healthcare provider to be informed about the CD4+ results, it's not the first action the nurse should take. The priority is to implement appropriate infection control measures to protect the patient, other patients, and healthcare staff.
CD4+ cell count is a crucial indicator of the patient's immune status. A count of 180/mm is significantly low, suggesting a weakened immune system and increased vulnerability to infections. However, informing the provider alone doesn't directly address the immediate need for infection control.
Rationale for Choice B:
Airborne Precautions are specifically used for patients with known or suspected airborne infections, such as tuberculosis, measles, or varicella. These precautions involve the use of negative pressure rooms and N95 respirators.
In this case, the patient's TB skin test was negative, indicating no evidence of active tuberculosis infection. Implementing Airborne Precautions unnecessarily could lead to excessive resource utilization and potential stigmatization of the patient.
Rationale for Choice C:
Droplet Precautions are used for patients with infections that can be spread through large respiratory droplets, such as influenza, pertussis, or meningococcal meningitis. These precautions involve the use of masks and eye protection.
While the patient's symptoms of fever, night sweats, and severe cough could be consistent with a droplet-spread infection, there's no definitive evidence to support this at the present time. Initiating Droplet Precautions without a clear indication could also lead to unnecessary resource use and potential anxiety for the patient.
Rationale for Choice D:
Standard Precautions are the foundation of infection control and should be used for all patients, regardless of their known or suspected infection status. These precautions include hand hygiene, use of personal protective equipment (PPE) when indicated, and safe handling of sharps and bodily fluids.
By implementing Standard Precautions, the nurse can effectively minimize the risk of transmission of pathogens, protecting both the patient and other individuals in the healthcare setting. This is the most appropriate first action to ensure a safe and appropriate level of care.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale:
Skin and mucous membranes are the most effective and crucial barriers to infection. They provide a continuous physical barrier that prevents pathogens from entering the body. Here's a detailed explanation of their protective mechanisms:
1. Physical Barrier:
Skin: The outermost layer of skin, the epidermis, is composed of tightly packed cells that are difficult for pathogens to penetrate. It's also covered in a layer of sebum, an oily substance that helps to repel water and microorganisms.
Mucous membranes: These moist linings cover the openings of the body, such as the nose, mouth, eyes, and digestive, respiratory, and urogenital tracts. They produce mucus, a sticky substance that traps pathogens and prevents them from entering the body. Mucus also contains enzymes and antibodies that can kill certain pathogens.
2. Chemical Barrier:
Skin and mucous membranes secrete a variety of substances that have antimicrobial properties. These include: Sebum: Contains fatty acids that can kill bacteria and fungi.
Sweat: Contains salt and lysozyme, an enzyme that can break down bacterial cell walls. Saliva: Contains enzymes that can break down food and kill bacteria.
Gastric acid: The highly acidic environment of the stomach kills most pathogens that are ingested.
3. Immune Barrier:
Skin and mucous membranes are home to a diverse community of microbes, known as the microbiome. These microbes play an important role in protecting against infection by competing with pathogens for resources and space.
Mucous membranes contain specialized immune cells, such as M cells and dendritic cells, that can recognize pathogens and initiate an immune response.
In contrast, the other choices are less effective barriers to infection:
Choice B: Gastrointestinal secretions, such as gastric acid, do play a role in preventing infection, but they are not as effective as skin and mucous membranes. Pathogens can still enter the body through the digestive tract, even in the presence of gastric acid.
Choice C: Colonization by host bacteria can actually help to protect against infection by competing with pathogens. However, it is not a primary barrier to infection.
Choice D: Inflammatory processes are a response to infection, not a barrier to it. They occur after pathogens have already entered the body.
Correct Answer is A
Explanation
Choice A rationale:
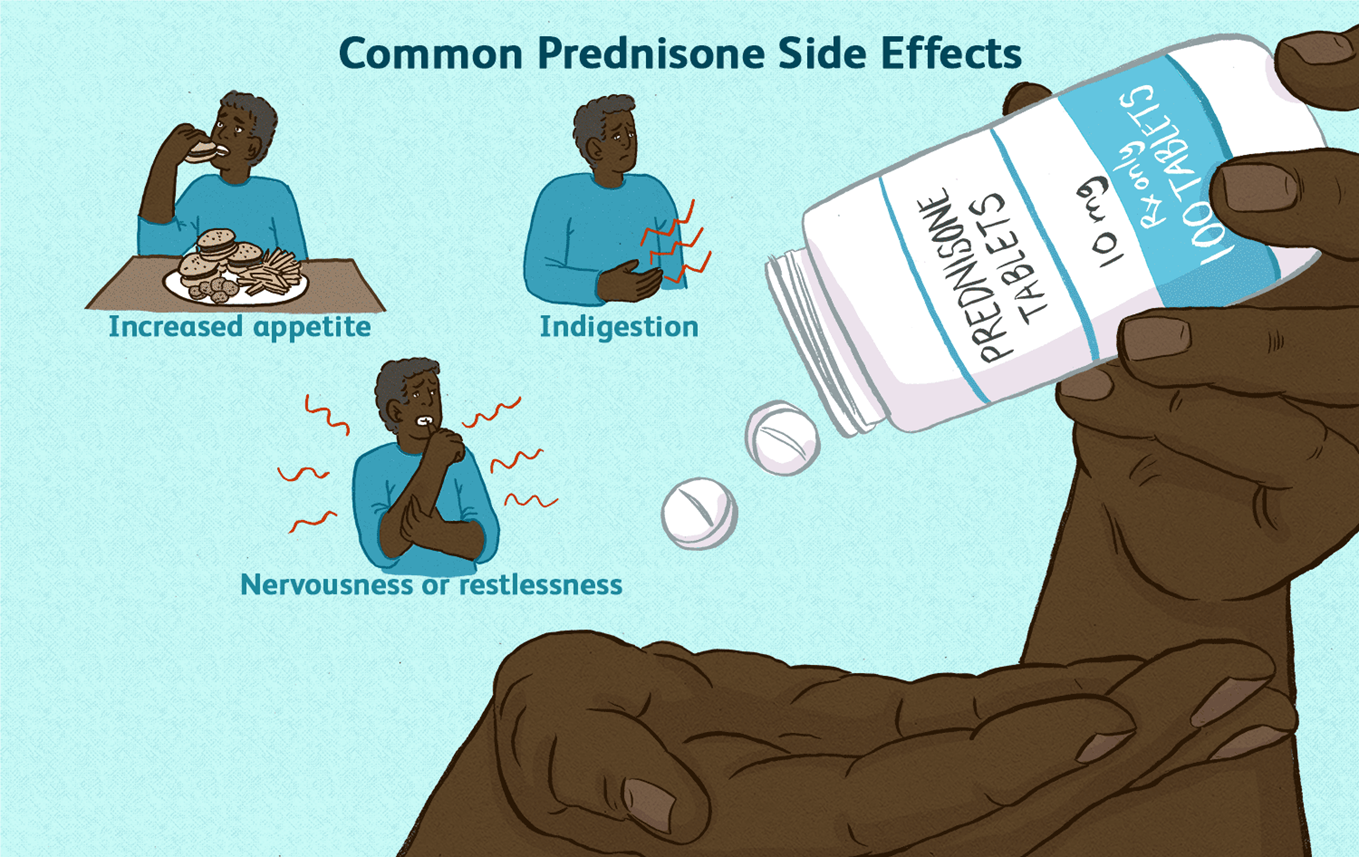
Prednisone is a corticosteroid that suppresses the body's natural production of cortisol. Cortisol is a hormone that is essential for life, and it plays a role in many important bodily functions, including:
Regulating blood sugar levels Maintaining blood pressure Reducing inflammation Responding to stress
When a person takes prednisone for a long period of time, their body begins to rely on the medication to provide cortisol. If the medication is stopped suddenly, the body cannot produce enough cortisol on its own, which can lead to a life-threatening condition called adrenal insufficiency.
Adrenal insufficiency can cause a variety of symptoms, including: Extreme fatigue
Weakness Dizziness Nausea Vomiting Abdominal pain Confusion
Loss of consciousness
To prevent adrenal insufficiency, it is important to taper off prednisone slowly over a period of time. This allows the body to gradually adjust to producing cortisol on its own.
Here are some additional details about why prednisone should never be discontinued abruptly: The risk of adrenal insufficiency is highest when prednisone has been taken for more than 3 weeks. The longer a person has been taking prednisone, the slower the taper should be.
It is important to follow the tapering instructions provided by the healthcare provider.
If a person experiences any symptoms of adrenal insufficiency, they should seek medical attention immediately.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
