OB Pediatric Cumulative Exam Test 4 V 1 2023 Proctored Exam
OB Pediatric Cumulative Exam Test 4 V 1 2023 Proctored Exam
Total Questions : 46
Showing 10 questions Sign up for moreMagnesium sulfate is given to women with preeclampsia and eclampsia to:
Explanation
Magnesium sulfate is given to women with preeclampsia and eclampsia to prevent and treat convulsions.
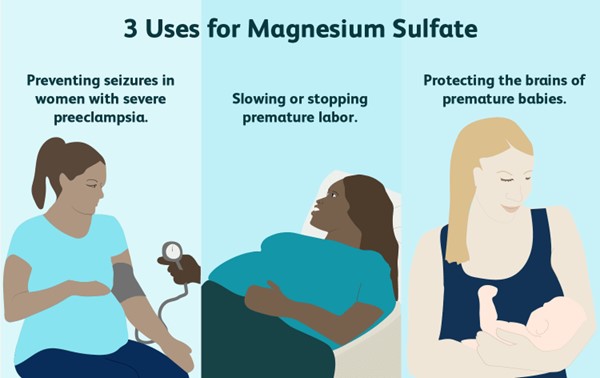
Magnesium sulfate is a mineral that reduces seizure risks in women with preeclampsia. A healthcare provider will give the medication intravenously. Sometimes, it’s also used to prolong pregnancy for up to two days. This allows drugs that speed up your baby’s lung development to be administered.
Choice A is wrong because magnesium sulfate does not improve patellar reflexes or increase respiratory efficiency. In fact, it may cause decreased or absent deep tendon reflexes and respiratory depression as side effects.
Choice B is wrong because magnesium sulfate does not shorten the duration of labor. It may actually prolong labor by inhibiting uterine contractions.
Choice D is wrong because magnesium sulfate does not prevent a boggy uterus or lessen the lochial flow. It has no effect on uterine tone or bleeding after delivery.
A pregnant woman has been receiving a magnesium sulfate infusion for the treatment of severe preeclampsia for 24 hours.
On assessment, the nurse finds the following vital signs: temperature of 37.3° C, pulse rate of 88 beats/min, respiratory rate of 10 breaths/min, blood pressure (BP) of 148/90 mm Hg, absent deep tendon reflexes, and no ankle clonus.
The patient complains, “I’m so thirsty and warm.” The nurse:
Explanation
The patient is showing signs of magnesium toxicity, such as respiratory depression, hyporeflexia, and flushing.
Magnesium sulfate is a high-alert medication that can cause serious adverse effects if not monitored closely.
The nurse should stop the infusion immediately and notify the provider.
Choice A is wrong because calling for a stat magnesium sulfate level will not address the immediate problem of toxicity.
The nurse should act quickly to prevent further complications.
Choice B is wrong because administering oxygen will not reverse the effects of magnesium toxicity.
Oxygen may be helpful for respiratory distress, but it will not correct the underlying cause.
Choice D is wrong because hydralazine is an antihypertensive medication that lowers blood pressure.
The patient’s blood pressure is already within the normal range for a pregnant woman with preeclampsia (140-160/90-110 mm Hg).
Hydralazine may cause hypotension and fetal distress.
A woman is in her seventh month of pregnancy.
She has been reporting nasal congestion and occasional epistaxis. The nurse suspects that:
Explanation
This is a normal respiratory change in pregnancy caused by elevated levels of estrogen. Estrogen increases blood flow and causes the nasal mucosa to swell, leading to congestion and nosebleeds. This condition is called pregnancy rhinitis and affects up to 20% of pregnant women.
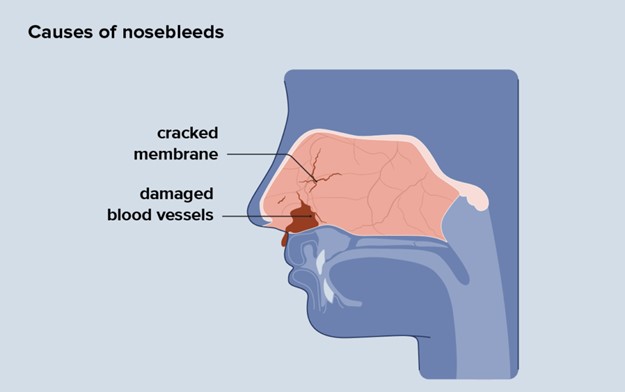
Choice B is wrong because this is not an abnormal cardiovascular change, and the nosebleeds are not an ominous sign. They are usually harmless and do not affect the pregnancy outcome.
Choice C is wrong because there is no evidence that the woman is a victim of domestic violence.
This is a serious accusation that should not be made without proper assessment and screening.
Choice D is wrong because there is no indication that the woman has been using cocaine intranasally. Cocaine use can cause nasal damage and bleeding, but it can also have other signs and symptoms such as agitation, euphoria, dilated pupils, increased heart rate and blood pressure, and risk of miscarriage or preterm labor.
Which infant would be more likely to have Rh incompatibility?
Explanation
choice A.
Infant of an Rh-negative mother and a father who is Rh-positive and homozygous for the Rh factor.
Rh incompatibility occurs when a woman is Rh-negative and her baby is Rh-positive. This can cause hemolytic disease of the neonate (HDN), a condition where the mother’s antibodies destroy the baby’s red blood cells.
Choice B is wrong because if both the mother and the baby are Rh-negative, there is no risk of Rh incompatibility.
Choice C is wrong because if the father is heterozygous for the Rh factor, there is a 50% chance that the baby will be Rh-negative and not affected by Rh incompatibility.
Choice D is wrong because if both the mother and the baby are Rh-positive, there is no risk of Rh incompatibility.
Human immunodeficiency virus (HIV) may be perinatally transmitted:
Explanation
The correct answer is choice D. Perinatal transmission of HIV is when HIV is passed from a woman with HIV to her child during pregnancy, childbirth, or breastfeeding.
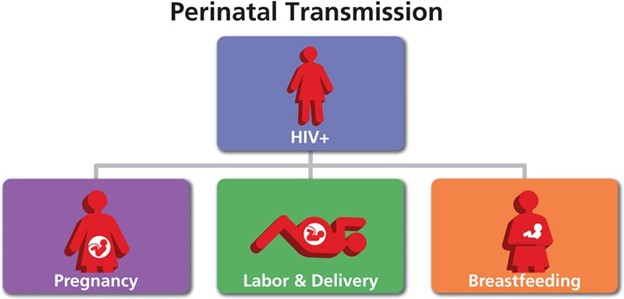
Breast milk from an infected mother can contain HIV and infect the baby.
Choice A is wrong because HIV can be transmitted at any stage of pregnancy, not only in the third trimester.
Choice B is wrong because needlestick injury is not a common mode of perinatal transmission of HIV. It is more likely to occur among health care workers who are exposed to contaminated needles or sharp objects.
Choice C is wrong because HIV can also be transmitted through the ingestion of amniotic fluid, but it is not the only way. Amniotic fluid is the fluid that surrounds and protects the baby in the womb.
A premature infant with respiratory distress syndrome receives artificial surfactant. How would the nurse explain surfactant therapy to the parents?
Explanation
choice A. Surfactant improves the ability of your baby’s lungs to exchange oxygen and carbon dioxide.
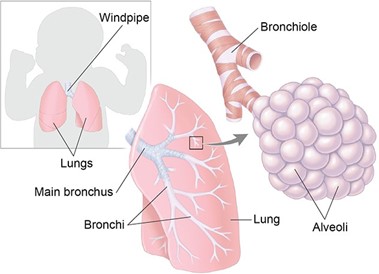
Surfactant is a substance that coats the inner surface of the alveoli, the tiny air sacs in the lungs.
It reduces the surface tension of the alveoli and prevents them from collapsing during exhalation.
Premature infants often lack enough surfactant, which leads to respiratory distress syndrome (RDS).
Artificial surfactant is given to these infants to help them breathe more easily. Choice B is wrong because surfactant has nothing to do with sedation.
Sedation is a state of reduced consciousness induced by drugs. Surfactant does not affect the level of consciousness of the infant.
Choice C is wrong because surfactant is not used to reduce episodes of periodic apnea.
Periodic apnea is a condition where the infant stops breathing for a short time, usually due to immature brainstem function.
Surfactant does not affect the brainstem or the control of breathing.
Choice D is wrong because surfactant is not used to fight a possible respiratory tract infection. Surfactant does not have any antibacterial or antiviral properties.
Surfactant is used to treat RDS, which is caused by a lack of surfactant, not by an infection.
A macrosomic infant is born after a difficult forceps-assisted delivery.
After stabilization, the infant is weighed, and the birth weight is 4550 g (9 lbs, 6 ounces). The nurse’s most appropriate action is to:
Explanation
choice D. Monitor blood glucose levels frequently and observe closely for signs of hypoglycemia. This is because a macrosomic infant (a newborn who’s much larger than average) is at risk of developing low blood sugar levels after birth, especially if the mother has diabetes. Hypoglycemia can cause neurological damage in the newborn, so it is important to detect and treat it promptly.
Choice A is wrong because leaving the infant in the room with the mother without monitoring the blood glucose levels may miss signs of hypoglycemia and delay treatment.
Choice B is wrong because taking the infant immediately to the nursery may separate the infant from the mother and interfere with breastfeeding, which can help prevent hypoglycemia.
Choice C is wrong because performing a gestational age assessment to determine whether the infant is large for gestational age is not urgent and does not address the risk of hypoglycemia.
Normal ranges for blood glucose levels in term infants are 2.6 mmol/L or higher at any time. A blood glucose level of 2.5 mmol/L or less is considered hypoglycemic.
The nurse administers vitamin K to the newborn for which reason?
Explanation
Bacteria that synthesize vitamin K is not present in the newborn’s intestinal tract. Vitamin K is essential for blood clotting, and newborns are at risk of bleeding problems due to their lack of vitamin K. Therefore, vitamin K is given by injection to prevent hemorrhagic disease in the newborn.
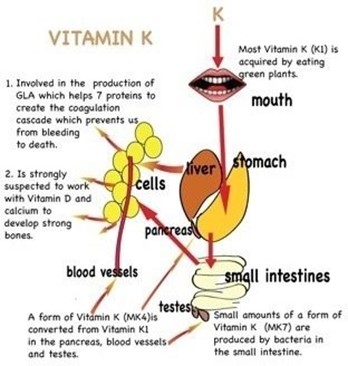
Choice A is wrong because most mothers do not have a diet deficient in vitamin K, and vitamin K deficiency in newborns is not related to the maternal diet.
Choice B is wrong because vitamin K does not prevent the synthesis of prothrombin in the liver, but rather enhances it. Prothrombin is a clotting factor that requires vitamin K for its production.
Choice D is wrong because the supply of vitamin K is not inadequate for at least 3 to 4 months, but rather for a few days until the newborn’s intestinal bacteria start producing it.
An Apgar score of 10 at 1 minute after birth would indicate a(n):
Explanation
An Apgar score of 10 at 1 minute after birth indicates that the infant is having no difficulty adjusting to extrauterine life but who should be assessed again at 5 minutes after birth. The Apgar score is a scoring system that evaluates the health of newborns at 1 and 5 minutes after birth based on five criteria: appearance, pulse, grimace, activity, and respiration. Each criterion is scored from 0 to 2, and the total score ranges from 0 to 10. A score of 7 to 10 is considered reassuring, a score of 4 to 6 is moderately abnormal, and a score of 0 to 3 is concerning.
Choice A is wrong because an Apgar score of 10 at 1 minute does not mean that the infant needs no further testing. The infant should still be assessed again at 5 minutes and monitored for any signs of distress or complications.
Choice B is wrong because an Apgar score of 10 at 1 minute does not indicate an infant in severe distress who needs resuscitation. An Apgar score of 0 to 3 would indicate a concerning condition that may require immediate intervention.
Choice C is wrong because an Apgar score of 10 at 1 minute does not predict a future free of neurologic problems. The Apgar score alone cannot be considered as evidence of, or a consequence of, asphyxia or brain injury; it does not predict individual neonatal mortality or neurologic outcome; and it should not be used for that purpose.
Normal ranges for each criterion are as follows:
- Appearance (color): pink all over (2 points), body pink but extremities blue (1 point), blue, bluish-gray, or pale all over (0 points)
- Pulse (heart rate): greater than 100 beats per minute (2 points), less than 100 beats per minute (1 point), absent (0 points)
- Grimace (response to stimulation): cough or sneeze, cry and withdrawal of foot with stimulation (2 points), facial movement/grimace with stimulation (1 point), absent (0 points)
- Activity (muscle tone): active movement (2 points), limbs flexed (1 point), limp or floppy (0 points)
- Respiration (breathing): good, strong cry (2 points), irregular, weak crying (1 point), absent (0 points)
A newborn is jaundiced and receivesphototherapy via ultraviolet bank lights.
An appropriate nursing intervention when caring for an infant with hyperbilirubinemia and receiving phototherapy by this method would be to:
Explanation
Placing eye shields over the newborn’s closed eyes. This is because phototherapy can cause eye damage and irritation to the newborn, so eye protection is essential.
Choice A is wrong because oil-based lotion can increase the absorption of heat and cause burns to the newborn’s skin.
Choice B is wrong because limiting the newborn’s intake of milk can cause dehydration and increase the risk of hyperbilirubinemia.
Choice D is wrong because changing the newborn’s position every 4 hours is not frequent enough to prevent pressure ulcers and ensure even exposure to the light.
Normal ranges for bilirubin levels in newborns are 1 to 12 mg/dL for term infants and 3 to 14 mg/dL for preterm infants. Phototherapy is usually indicated when the bilirubin level exceeds 15 mg/dL for term infants and 10 mg/dL for preterm infants.
You just viewed 10 questions out of the 46 questions on the OB Pediatric Cumulative Exam Test 4 V 1 2023 Proctored Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



