Endocrinology Midterm Exam
Endocrinology Midterm Exam
Total Questions : 42
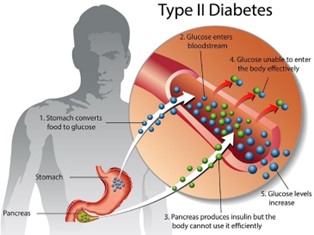
Showing 10 questions Sign up for moreMary, a 63-year-old patient is newly diagnosed with type 2 diabetes. When determining an education plan, the nurse’s first action should be to?
Explanation
The first step in the education plan should be to assess their understanding and perception of the disease. This will help the nurse to identify any misconceptions or knowledge gaps that the patient may have and tailor the education plan accordingly. Understanding the patient's perceptions will also help the nurse to establish a trusting relationship with the patient and increase their engagement in diabetes self-management.
Options b, c, and d are important components of the diabetes education plan, but they should be implemented after the initial assessment of the patient's perception and understanding of their diagnosis.
A client has been taught to restrict dietary sodium. Which food selection by the client indicates to the nurse that teaching has been effective?
Explanation
This meal choice is low in sodium as it contains fresh ingredients and does not include processed or pre-packaged foods that are typically high in sodium. Chicken, bread, and carrots are naturally low in sodium, and the client can control the amount of added salt or seasoning. In contrast, the other food choices are likely to be high in sodium due to added salt, cheese, or processed ingredients.
Therefore, the nurse should encourage the client to choose fresh, low-sodium foods and avoid processed or pre-packaged meals.

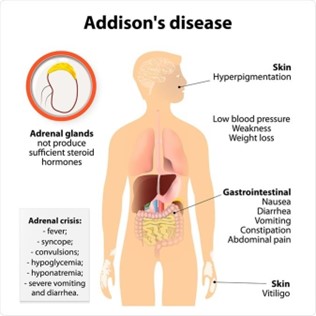
A patient is admitted to the hospital in Addisonian Crisis a month after a diagnosis of Addison’s disease. The nurse identifies the nursing diagnosis of ineffective therapeutic regimen management related to lack of knowledge of management of the condition when the patient says:
Explanation
The statement "I had the stomach flu earlier this week and couldn't take the hydrocortisone" indicates that the patient may not be adhering to their prescribed medication regimen, which can lead to an Addisonian crisis. Therefore, the nursing diagnosis of ineffective therapeutic regimen management related to lack of knowledge of management of the condition is appropriate.
Addison’s disease is a condition in which the adrenal glands do not produce enough cortisol and aldosterone. Hydrocortisone is a glucocorticoid medication that is often used to replace the cortisol that the adrenal glands are not producing. In the Addisonian crisis, the body is unable to produce the necessary levels of cortisol and aldosterone, which can lead to potentially life-threatening complications such as hypotension, dehydration, and electrolyte imbalances.
The other statements may indicate areas where patient education is needed, but they do not directly relate to the immediate risk of an Addisonian crisis.
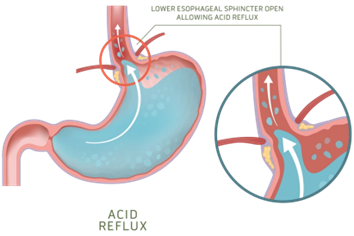
When admitting a patient with a stroke who is unconscious and unresponsive to stimuli. The nurse learns from the patient’s family that the patient has a history of GERD, the nurse will plan to do frequent assessment of the patient’s:
Explanation
GERD can increase the risk of aspiration (inhalation of stomach contents into the lungs), which can cause respiratory issues, including abnormal breath sounds. In these cases, monitoring of breath sounds may be more appropriate than monitoring of bowel sounds.
Bowel sounds are not typically monitored for GERD patients as GERD is a condition that affects the esophagus and the stomach, not the intestines. GERD is caused by the reflux of stomach contents into the esophagus, which can cause symptoms such as heartburn and regurgitation.
Abdominal girth is not routinely monitored for GERD patients as it is not typically related to the condition. GERD is a disorder that affects the esophagus and stomach and does not typically cause significant changes in abdominal size or girth. In rare cases, GERD can be complicated by a condition known as a para oesophageal hernia, which can cause a visible bulge in the abdomen. In these cases, monitoring of abdominal size and shape may be necessary.
The apical pulse is not routinely monitored for GERD patients as it is not directly related to the condition. GERD is a disorder that affects the digestive system, specifically the esophagus and stomach and does not typically have an impact on heart rate or rhythm.
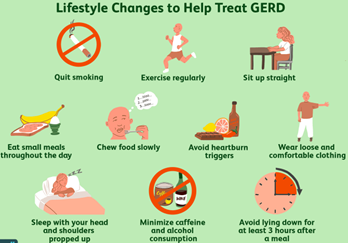
Which information will the nurse include when teaching a patient with newly diagnosed GERD?
Explanation
When teaching a patient with newly diagnosed GERD, the nurse will include that they will need to keep the head of their bed elevated on blocks. This helps prevent stomach acid from flowing back into the esophagus while sleeping.
Peppermint tea might not be helpful in reducing GERD symptoms as it can relax the lower esophageal sphincter and worsen reflux.
Eating between meals is not recommended as it can increase acid secretion. Vigorous physical activities may increase the incidence of reflux.
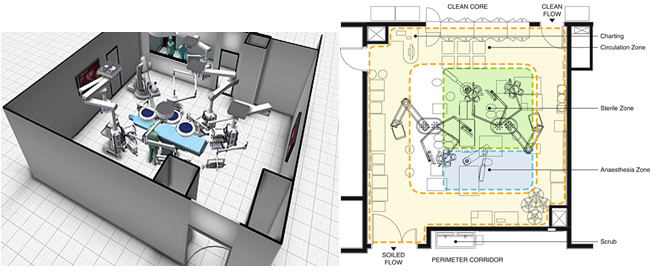
The physical environment and traffic control measures of the operating room are designed primarily to:
Explanation
The operating room is a sterile environment, and it is critical to maintain a clean and controlled environment to reduce the risk of infection to the patient. The measures taken include maintaining positive air pressure, controlling temperature and humidity, filtering the air, using sterile surgical instruments, and limiting traffic in and out of the operating room. These measures help to prevent the spread of infectious agents that may be present in the operating room. While the other options (a, b, and d) may also be important considerations in the design of the operating room, preventing transmission of infection is the primary goal.
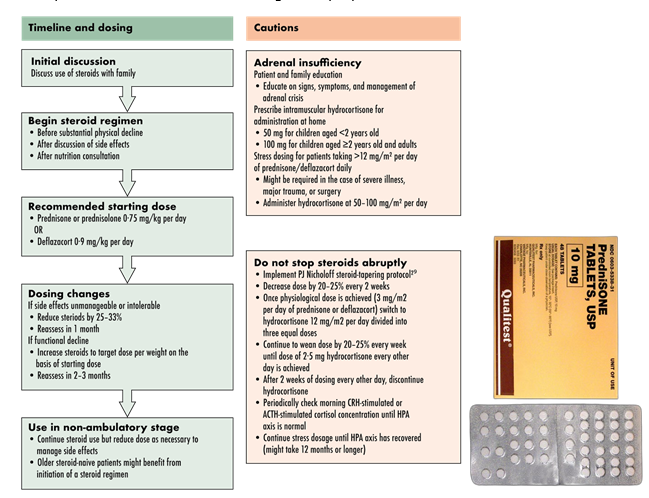
A patient is taking high doses of prednisone to control the symptoms of acute exacerbation of systemic lupus erythematosus. When teaching the patient about the use of prednisone, which information is important for the nurse to include?
Explanation
Sudden discontinuation of prednisone can result in adrenal insufficiency and can lead to life-threatening complications. The nurse should also instruct the patient to report any symptoms of an infection, such as fever, to the doctor promptly, as prednisone can mask signs of an infection.
Monitoring for mood alterations and daily weight measurement are also important aspects of care, but they are not as crucial as the need to gradually taper off the medication.
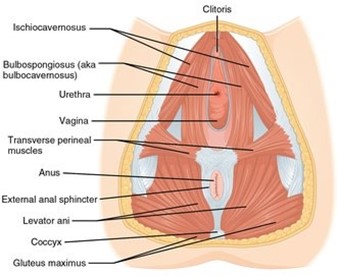
After her bath, a 62-year-old patient asks the nurse for a perineal pad saying that she uses them because sometimes she leaks urine when she laughs or coughs. Which intervention is most appropriate to include in the care plan for the patient?
Explanation
Kegel exercises are designed to strengthen the pelvic floor muscles, which can help improve urinary incontinence. By teaching the patient how to perform Kegel exercises, the nurse can provide a non-invasive, effective intervention that the patient can perform on her own to help manage her urinary incontinence.
Assisting the patient to the bathroom q3hr (b) may help reduce the frequency of incontinence episodes but it does not address the underlying issue of weakened pelvic floor muscles.
Demonstrating how to perform Crede’s maneuver (c) involves applying manual pressure to the bladder to assist with urination and is not appropriate for managing urinary incontinence related to laughing or coughing.
Placing a commode at the patient’s bedside (d) may be appropriate for patients who have difficulty with mobility or accessing the bathroom, but it does not address the underlying issue of weakened pelvic floor muscles causing urinary incontinence.

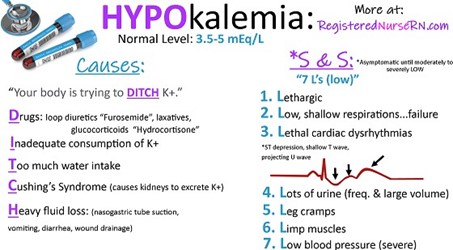
A client is taking furosemide (Lasix), a diuretic. and becomes confused. Which potassium level does the nurse correlate with this condition?
Explanation
Furosemide is a loop diuretic that works by blocking the reabsorption of sodium and chloride in the ascending loop of Henle in the kidney, leading to increased urine output. However, this medication can also cause potassium loss through increased urinary excretion, which can lead to hypokalemia (low potassium level). Hypokalemia can cause confusion, weakness, and other neurological symptoms.
The normal range for serum potassium is 3.5 to 5.0 mEq/L. A potassium level of 2.9 mEq/L is below the normal range and is considered hypokalemic. Therefore, the nurse should correlate the client's confusion with the low potassium level and notify the healthcare provider to adjust the medication or provide potassium supplements if indicated.

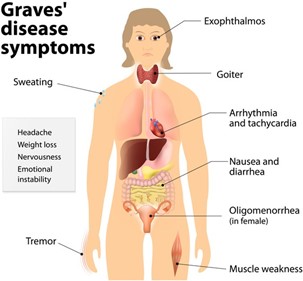
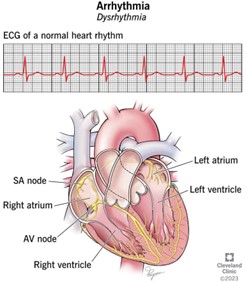
During the nursing assessment of a patient with Graves' disease. The nurse notes a bounding, rapid pulse and systolic hypertension. Based on these assessment data, which question is important for the nurse to ask the patient?
Explanation
The patient's bounding, rapid pulse and systolic hypertension may indicate cardiovascular complications associated with Graves' disease, such as tachycardia, atrial fibrillation, or congestive heart failure, which can cause chest pain. It is important for the nurse to assess for any symptoms of cardiovascular distress and report any abnormal findings to the healthcare provider for prompt intervention. Questions about appetite and constipation may be relevant to the patient's overall health status, but they are not the most important concern in this situation.
You just viewed 10 questions out of the 42 questions on the Endocrinology Midterm Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now