RN Pharmacology 2023
ATI RN Pharmacology 2023
Total Questions : 65
Showing 10 questions Sign up for moreA nurse is administering medications to a client who weighs 132 lb. The prescription reads chloramphenicol, 50mg/kg/day in 4 divided doses. Available is chloramphenicol 100 mg/mL. How many mL should the nurse give with each dose? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
Convert the client's weight from pounds to kilograms. We can use the formula 1 kg = 2.2 lb. So, 132 lb / 2.2 = 60 kg.
Calculate the total daily dose of chloramphenicol for the client. We can use the formula Dose (mg) = Weight (kg) x Dosage (mg/kg). So, 60 kg x 50 mg/kg = 3000 mg.
Divide the total daily dose by 4 to get the dose for each administration. So, 3000 mg / 4 = 750 mg.
Calculate the volume of chloramphenicol solution needed for each dose. We can use the formula Volume (mL) = Dose (mg) / Concentration (mg/mL). So, 750 mg / 100 mg/mL =
7.5 mL.
Round the answer to the nearest tenth. So, the nurse should give 7.5 mL of chloramphenicol solution with each dose.
A nurse is planning to administer medications to a client who weighs 198 lb. The prescription reads, "filgrastim 5 mcg/kg, subcutaneous, daily." Available is filgrastim 300 mcg/mL. How many mL should the nurse plan to give with each dose? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
Convert the client's weight from pounds to kilograms by dividing by 2.2. 198 lb / 2.2 = 90 kg
Calculate the dose of filgrastim in micrograms by multiplying the client's weight in kilograms by the prescribed dose per kilogram. 90 kg x 5 mcg/kg = 450 mcg
Calculate the volume of filgrastim in milliliters by dividing the dose in micrograms by the concentration of the available solution. 450 mcg / 300 mcg/mL = 1.5 mL
Round the answer to the nearest tenth. The nurse should plan to give 1.5 mL of filgrastim with each dose.
A nurse is preparing to administer the initial dose of penicillin G IM to a client. The nurse should monitor for which of the following as an indication of an allergic reaction following the injection?
Explanation
A. Pallor: Pallor refers to paleness of the skin and is not typically associated with an allergic reaction to penicillin G IM.
B. Dyspepsia: Dyspepsia refers to indigestion or discomfort in the upper abdomen and is not typically associated with an allergic reaction to penicillin G IM.
C. Bradycardia: Bradycardia refers to a slow heart rate and is not typically associated with an allergic reaction to penicillin G IM.
D. Urticaria: Urticaria, commonly known as hives, is a characteristic manifestation of an allergic reaction to penicillin G IM. It presents as raised, red, itchy welts on the skin.

A nurse is caring for a client who is taking lithium and reports starting a new exercise program. The nurse should assess the client for which of the following electrolyte imbalances?
Explanation
A. Hypomagnesemia: While lithium can affect magnesium levels, starting a new exercise program is not typically associated with hypomagnesemia. Hypomagnesemia may result in muscle weakness, tremors, and cardiac dysrhythmias.
B. Hypocalcemia: Starting a new exercise program is not typically associated with hypocalcemia. Hypocalcemia may present with muscle cramps, tetany, and seizures.
C. Hyponatremia: Starting a new exercise program may lead to dehydration and electrolyte imbalances, including hyponatremia (low sodium levels). This can have profound effects on patients taking lithium. Symptoms of hyponatremia include weakness, confusion, and seizures.
D. Hypokalemia is not a common occurrence among individuals doing exercise.
A nurse is providing teaching to a client who is receiving intermittent parenteral metronidazole. Which of the following conditions should the nurse recognize as an indication for this medication?
Explanation
A. Endocarditis: Metronidazole is an antibiotic commonly used to treat infections caused by anaerobic bacteria, including certain types of endocarditis.
B. Kidney transplant: Metronidazole is not typically indicated for kidney transplant. Other antibiotics may be used in post-transplant care to prevent or treat infections.
C. Seizures: Metronidazole is not indicated for seizures. In fact, it may rarely cause neurological side effects such as seizures, but it is not typically used to treat seizures.
D. Hypokalemia: Metronidazole is not indicated for hypokalemia. It is an antibiotic and does not directly affect potassium levels.
A nurse is caring for a client with gingivitis in the clinic.
Which of the following client statements indicates to the nurse the teaching was effective?
Explanation
A nurse is caring for a client who has diabetes insipidus and is receiving desmopressin by intermittent IV bolus. Which of the following manifestations should the nurse identify as an indication of a therapeutic response to the medication?
Explanation
A. Increase in serum sodium: Desmopressin, a synthetic form of vasopressin, works to decrease urine output and increase water reabsorption in the kidneys. Therefore, a therapeutic response to desmopressin would not result in an increase in serum sodium; rather, it would aim to normalize serum sodium levels by reducing excessive urine output.
B. Decrease in urine output: The primary therapeutic goal of desmopressin in the treatment of diabetes insipidus is to decrease urine output by increasing water reabsorption in the kidneys. Therefore, a decrease in urine output would indicate a positive response to the medication.
C. Increase in heart rate: Desmopressin primarily affects kidney function by increasing water reabsorption and does not typically have a direct effect on heart rate. Therefore, an increase in heart rate would not be a manifestation of a therapeutic response to desmopressin.
D. Decrease in blood pressure: Desmopressin works to increase water reabsorption in the kidneys and does not typically cause significant changes in blood pressure. Therefore, a decrease in blood pressure would not be a manifestation of a therapeutic response to desmopressin.
A nurse in a provider's office is caring for a client.
Nurses' Notes
3 months ago:
Client seen in provider's office for routine physical. Today:
Client reports dizziness and light-headedness upon standing. Client reports waking up at night to void.
What actions should the nurse take? Select all that apply.
Explanation
A. Advise the client to change positions slowly: The client's symptoms of dizziness and light- headedness upon standing suggest orthostatic hypotension, which can be managed by advising the client to change positions slowly to minimize blood pressure drops upon standing.
B. Check the client for orthostatic hypotension. Monitor the client for dysrhythmias: The client's symptoms, along with the report of waking up at night to void, are suggestive of orthostatic hypotension, a drop in blood pressure upon standing. Checking for orthostatic hypotension and monitoring for dysrhythmias are appropriate nursing actions to assess and manage this condition.
C. Advise the client to restrict potassium intake: Restricting potassium intake is not indicated based on the client's symptoms of dizziness and light-headedness. This action is not relevant to the situation described.
D. Advise the client to take the medication before bedtime: There is no indication in the scenario provided that medication timing is related to the client's symptoms. This action is not relevant to addressing the client's reported symptoms.
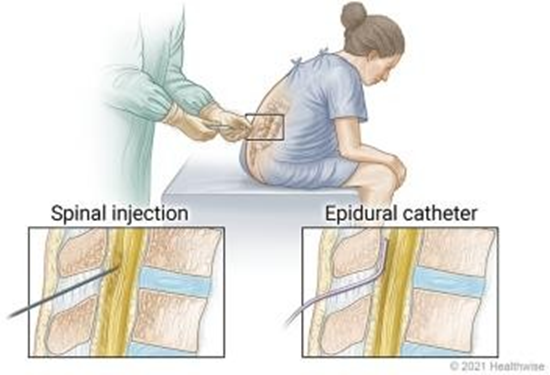
A nurse is assessing a client who is in labor and is receiving epidural anesthesia. Which of the following findings should the nurse identify as the priority?
Explanation
A. Urinary retention: While urinary retention can be a complication of epidural anesthesia, it is not the priority finding in this scenario. The priority is to address potential complications that can lead to maternal or fetal compromise.
B. Leg weakness: Leg weakness can occur as a side effect of epidural anesthesia but is not the priority finding in this scenario unless it is severe and compromises the client's ability to
mobilize or push during labor.
C. Hypotension: Hypotension is a common complication of epidural anesthesia due to sympathetic blockade, which can lead to decreased venous return and subsequent maternal
hypotension. Maternal hypotension can compromise uteroplacental perfusion, leading to fetal distress. Therefore, addressing hypotension promptly is the priority to prevent adverse maternal and fetal outcomes.
D. Temperature 39°C (102.2°F): While fever should be monitored and addressed, it is not the priority finding in this scenario unless it indicates an infection, which would require further assessment and intervention. However, maternal hypotension poses a more immediate risk to both the mother and the fetus during labor.
A nurse is caring for a client in a provider's office.
Which of the following statements should the nurse include when teaching the client about the prescribed LEVODPA? Select all that apply.
Explanation
A. "Consumption of a high protein meal can reduce the effectiveness of the medication."
High-protein meals can interfere with levodopa absorption in the intestine, reducing its effectiveness. Clients should consume protein in moderate amounts and distribute intake throughout the day.
B. "You may notice your urine becomes lighter in color."
Levodopa can cause urine, sweat, and saliva to become darker (brown, red, or black), not lighter. This is a harmless side effect but should be discussed with the client.
C. "You may initially notice an increase in involuntary movements."
Levodopa can cause dyskinesia (involuntary movements), especially with prolonged use or at higher doses. These movements can include facial twitching, jerking, or head bobbing.
D. "The medication can cause nausea, so take with a meal."
Levodopa can cause nausea, particularly when first starting the medication. Taking it with food can help reduce gastrointestinal discomfort, but avoiding high-protein meals is important.
E. "This medication can make you light-headed if you stand up too quickly from a seated or lying position."
Levodopa can cause orthostatic hypotension, leading to dizziness or light-headedness when changing positions. Clients should be advised to rise slowly to prevent falls.
You just viewed 10 questions out of the 65 questions on the ATI RN Pharmacology 2023 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



