Custom Maternity Final 23D Proctored Exam
ATI Custom Maternity Final 23D Proctored Exam
Total Questions : 69
Showing 10 questions Sign up for moreWhich of these is a characteristic of a preterm infant?
Explanation
Choice A reason:
Hypertonia is not a characteristic of a preterm infant, but rather of a post-term infant. Hypertonia means increased muscle tone or stiffness, which is more common in infants who are overdue. Preterm infants have poor muscle tone and less subcutaneous fat.
Choice B reason:
Long toenails are also not a characteristic of a preterm infant but of a post-term infant. Long toenails indicate that the infant has grown beyond the expected gestational age. Preterm infants have short and brittle nails.
Choice C reason:
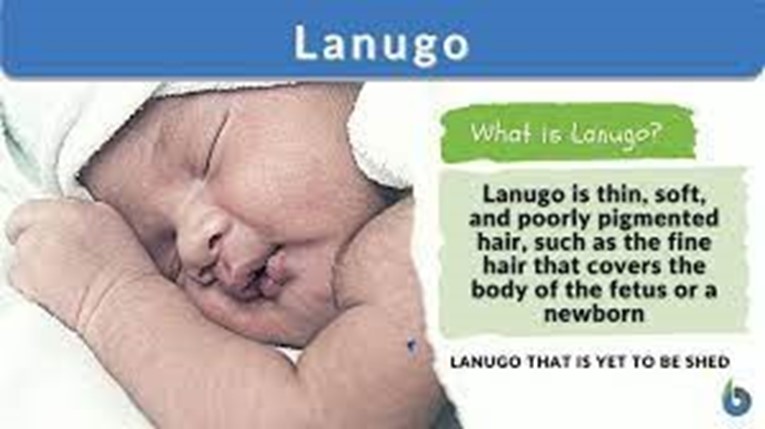
Lanugo is a characteristic of a preterm infant. Lanugo is fine, downy hair that covers the body of the fetus. It usually disappears by the 36th week of gestation, but preterm infants may still have it at birth.
Choice D reason:
Dry skin is not a characteristic of a preterm infant but of a post-term infant. Dry skin indicates that the infant has lost moisture and subcutaneous fat due to prolonged exposure to the amniotic fluid. Preterm infants have thin and transparent skin that may be covered by vernix caseosa, a white, cheesy substance that protects the skin from the amniotic fluid.
What are the signs and symptoms of Thalassemia? Select all that apply.
Explanation
Choice A reason:
Slow growth is a common symptom of thalassemia, especially in children. It is caused by the reduced production of hemoglobin and red blood cells, which leads to anemia and poor oxygen delivery to the tissues. Slow growth can also affect the development of facial bones and cause deformities.
Choice B reason:
Fatigue is another common symptom of thalassemia, also related to anemia and low oxygen levels in the body. People with thalassemia may feel tired, weak, and short of breath even after mild physical activity. Fatigue can also affect their mood, concentration, and quality of life.
Choice C reason:
Hematoma is not a typical symptom of thalassemia. Hematoma is a collection of blood under the skin or in an organ, usually caused by trauma, injury, or bleeding disorders. People with thalassemia may have a higher risk of bleeding due to low platelet counts or frequent blood transfusions, but this does not necessarily result in hematoma.
Choice D reason:
Pruritus is not a typical symptom of thalassemia. Pruritus is a sensation of itching that can affect any part of the body. It can have many causes, such as dry skin, allergies, infections, or liver problems. People with thalassemia may experience pruritus as a side effect of iron overload or iron chelation therapy, but it is not a direct consequence of the condition.
Choice E reason:
Ecchymoses are not typical symptoms of thalassemia. Ecchymoses are large bruises that appear on the skin due to bleeding under the surface. They can be caused by trauma, injury, or bleeding disorders. People with thalassemia may have a higher risk of bleeding due to low platelet counts or frequent blood transfusions, but this does not necessarily result in ecchymoses.
A nurse is caring for a newborn immediately following delivery. After assuring a patent airway, which of the following actions should be the nurse's priority?
Explanation
Choice A reason:

Drying the newborn's skin thoroughly is the nurse's priority after assuring a patent airway because it reduces evaporative heat loss by the newborn and prevents cold stress. Cold stress can lead to hypoxia, hypoglycemia, acidosis, and increased bilirubin levels. Drying the newborn also stimulates breathing and crying, which are signs of a healthy newborn.
Choice B reason:
Administering phytonadione IM is not the nurse's priority because it is not an immediate life-saving intervention. Phytonadione is given to prevent hemorrhagic disease of the newborn, which is caused by vitamin K deficiency. However, this condition usually occurs after the first day of life, so administering phytonadione can be delayed until after the initial assessment and stabilization of the newborn.
Choice C reason:
Documenting the Apgar score is not the nurse's priority because it is not an action that directly affects the newborn's well-being. The Apgar score is a tool to assess the newborn's condition at 1 and 5 minutes after birth based on five criteria: heart rate, respiratory effort, muscle tone, reflex irritability, and color. The Apgar score can help guide the nurse's interventions, but it is not more important than providing care to the newborn.
Choice D reason:
Applying identification bands is not the nurse's priority because it is not an urgent or essential action. Identification bands are used to ensure the safety and security of the newborn and prevent errors or mix-ups. However, applying identification bands can be done after the newborn is dried, warmed, and assessed for any problems.
A nurse is collecting data from a newborn who has respiratory distress syndrome and is experiencing respiratory acidosis. Which of the following risk factors predisposes the newborn to respiratory difficulties?
Explanation
Choice A reason:
Small for gestational age (SGA) newborns are at risk for respiratory distress syndrome (RDS) and respiratory acidosis because they have immature lungs that produce less surfactant, which is needed to keep the alveoli open and prevent atelectasis. SGA newborns also have less glycogen stores, which can lead to hypoglycemia and impaired oxygen delivery to the tissues.
Choice B reason:
Maternal history of asthma is not a risk factor for RDS or respiratory acidosis in the newborn. Asthma is a chronic inflammatory disorder of the airways that affects the mother, not the fetus. Maternal asthma can cause complications such as preterm labor, preeclampsia, or intrauterine growth restriction, but it does not directly affect the fetal lung development or function.
Choice C reason:
Ventricular septal defect (VSD) is a congenital heart defect that causes a hole in the wall between the ventricles of the heart. This can result in increased pulmonary blood flow and pressure, which can lead to pulmonary edema and heart failure in the newborn. However, VSD does not cause RDS or respiratory acidosis, which are related to lung maturity and surfactant production.
Choice D reason:
Cesarean birth is not a risk factor for RDS or respiratory acidosis in the newborn. Cesarean birth can increase the risk of transient tachypnea of the newborn (TTN), which is caused by delayed absorption of fetal lung fluid. TTN usually resolves within 24 to 48 hours and does not cause a significant acid-base imbalance in the newborn.
A nurse is caring for a client who is postpartum. The nurse should recognize which of the following statements by the client as a possible indicator of inhibition of parental attachment?
Explanation
Choice A reason:
This statement does not indicate inhibition of parental attachment. The client may have prior experience or knowledge of bathing a newborn and may not need the demonstration. The nurse should respect the client's autonomy and confidence in this skill.
Choice B reason:
This statement does not indicate inhibition of parental attachment. The client may be exhausted from the labor and delivery process and may need some rest to recover. The nurse should support the client's request and ensure that the newborn is well cared for in the nursery.
Choice C reason:
This statement indicates inhibition of parental attachment. The client expresses dissatisfaction with the newborn's appearance and implies that the newborn is not attractive enough. The nurse should explore the client's feelings and expectations about the newborn and provide reassurance and education about normal variations in newborn features.
Choice D reason:
This statement does not indicate inhibition of parental attachment. The client recognizes a family resemblance in the newborn and expresses a positive connection with the newborn and the partner. The nurse should acknowledge the client's observation and encourage further bonding with the newborn.
What is the most significant risk factor for clubfoot?
Explanation
Choice A reason:

Smoking is the most significant risk factor for clubfoot, according to several studies that have found a strong association between maternal smoking during pregnancy and the occurrence of clubfoot in the offspring. Smoking may affect the development of the muscles and tendons in the fetus, leading to abnormal positioning of the foot.
Choice B reason:
Trauma during pregnancy is not a significant risk factor for clubfoot, as there is no evidence that physical injury to the mother or the fetus can cause this deformity. Clubfoot is a congenital condition that is present at birth and usually detected by prenatal ultrasound.
Choice C reason:
Hypertension is not a significant risk factor for clubfoot, as there is no evidence that high blood pressure in the mother or the fetus can cause this deformity. Clubfoot is a congenital condition that is present at birth and usually detected by prenatal ultrasound.
Choice D reason:
Decreased circulation is not a significant risk factor for clubfoot, as there is no evidence that poor blood flow to the mother or the fetus can cause this deformity. Clubfoot is a congenital condition that is present at birth and usually detected by prenatal ultrasound.
A nurse is assisting in the care of a newborn who is 72 hr old and is receiving treatment for neonatal abstinence syndrome.
Which of the following data collection findings should the nurse identify as requiring immediate follow- up? (Select all that apply.).
Explanation
Choice A reason
Blood pressure is not a priority finding for a newborn with neonatal abstinence syndrome (NAS). Blood pressure is usually normal or slightly elevated in NAS, and it is not a reliable indicator of the severity of withdrawal symptoms.
Choice B reason
Gastrointestinal disturbances are a common and serious finding for a newborn with NAS. Vomiting and diarrhea can lead to dehydration, electrolyte imbalance, and poor weight gain. Projectile vomiting can also increase the risk of aspiration. This finding requires immediate follow-up and intervention.
Choice C reason
Skin color is not a priority finding for a newborn with NAS. Acrocyanosis (bluish color of the hands and feet) is a normal finding in newborns and does not indicate hypoxia or poor circulation. It usually resolves within the first few days of life.
Choice D reason
NAS score is not a priority finding for a newborn with NAS. NAS score is a tool used to assess the severity of withdrawal symptoms and the need for pharmacological treatment. It is based on a set of clinical signs and symptoms that are scored at regular intervals. However, it is not a substitute for clinical judgment and individualized care. The NAS score alone does not determine the urgency of follow-up.
Choice E reason
Temperature is not a priority finding for a newborn with NAS. Temperature may be slightly elevated or normal in NAS, and it is not a specific sign of infection or withdrawal. Temperature regulation is important for newborns, but it is not an immediate concern in this case.
Choice F reason
Oxygen saturation is a priority finding for a newborn with NAS. Tachypnea (rapid breathing) and retractions (inward movement of the chest wall) are signs of respiratory distress, which can compromise oxygen delivery to the tissues and organs. Hypoxia (low oxygen level) can cause brain damage, organ failure, and death if not corrected promptly. This finding requires immediate follow-up and intervention.
Choice G reason
Central nervous system disturbances are a priority finding for a newborn with NAS. Increased muscle tone, tremors, high-pitched cry, and seizures are signs of neurological dysfunction,which can indicate brain injury, bleeding, or infection. Seizures can also worsen hypoxia and metabolic acidosis. This finding requires immediate follow-up and intervention.
Choice H reason
Respiratory rate is not a priority finding for a newborn with NAS. Respiratory rate may be increased or normal in NAS, and it is not a specific sign of respiratory distress or infection. Respiratory rate should be monitored along with other vital signs.
A nurse is assisting in the care of a newborn who is 72 hr old and is receiving treatment for neonatal abstinence syndrome.
Which of the following data collection findings should the nurse identify as requiring immediate follow-up? (Select all that apply.).
Explanation
Choice A reason:
Blood pressure is not a priority finding for a newborn with neonatal abstinence syndrome (NAS). Blood pressure is usually normal or slightly elevated in NAS, and it is not a reliable indicator of the severity of withdrawal symptoms.
Choice B reason:
Gastrointestinal disturbances are a common and serious finding for a newborn with NAS. Vomiting and diarrhea can lead to dehydration, electrolyte imbalance, and poor weight gain. Projectile vomiting can also increase the risk of aspiration. This finding requires immediate follow-up and intervention.
Choice C reason:
Skin color is not a priority finding for a newborn with NAS. Acrocyanosis (bluish color of the hands and feet) is a normal finding in newborns and does not indicate hypoxia or poor circulation. It usually resolves within the first few days of life.
Choice D reason:
NAS score is not a priority finding for a newborn with NAS. NAS score is a tool used to assess the severity of withdrawal symptoms and the need for pharmacological treatment. It is based on a set of clinical signs and symptoms that are scored at regular intervals. However, it is not a substitute for clinical judgment and individualized care. The NAS score alone does not determine the urgency of follow-up.
Choice E reason:
Temperature is not a priority finding for a newborn with NAS. The temperature may be slightly elevated or normal in NAS, and it is not a specific sign of infection or withdrawal. Temperature regulation is important for newborns, but it is not an immediate concern in this case.
Choice F reason:
Oxygen saturation is a priority finding for a newborn with NAS. Tachypnea (rapid breathing) and retractions (inward movement of the chest wall) are signs of respiratory distress, which can compromise oxygen delivery to the tissues and organs. Hypoxia (low oxygen level) can cause brain damage, organ failure, and death if not corrected promptly. This finding requires immediate follow-up and intervention.
Choice G reason:
Central nervous system disturbances are a priority finding for a newborn with NAS. Increased muscle tone, tremors, high-pitched cries, and seizures are signs of neurological dysfunction, which can indicate brain injury, bleeding, or infection. Seizures can also worsen hypoxia and metabolic acidosis. This finding requires immediate follow-up and intervention.
Choice H reason:
Respiratory rate is not a priority finding for a newborn with NAS. Respiratory rate may be increased or normal in NAS, and it is not a specific sign of respiratory distress or infection. Respiratory rate should be monitored along with other vital signs, but.
A nurse is assisting in the care of a newborn who is 72 hours old and is receiving treatment for neonatal abstinence syndrome.
Which of the following data collection findings should the nurse identify as requiring immediate follow-up? (Select all that apply.).
Explanation
Choice A:
Blood pressure is not a priority finding for a newborn with neonatal abstinence syndrome (NAS). Blood pressure may be slightly elevated or normal in NAS, but it is not a sign of severe withdrawal or a risk for complications. •
Choice B:
Gastrointestinal disturbances are common and serious symptoms of NAS. They include poor feeding, vomiting, diarrhea, dehydration and poor weight gain. These can lead to electrolyte imbalance, malnutrition and failure to thrive. This choice requires immediate follow-up. •
Choice C:
Skin color is not a priority finding for a newborn with NAS. Skin color may be normal or slightly pale in NAS, but it is not a sign of severe withdrawal or risk for complications. •
Choice D:
NAS score is a priority finding for a newborn with NAS. NAS score is a tool used to assess the severity of withdrawal symptoms and the need for pharmacological treatment. A high NAS score indicates that the newborn needs medication to manage the withdrawal and prevent complications such as seizures. This choice requires immediate follow-up. •
Choice E:
Temperature is not a priority finding for a newborn with NAS. The temperature may be slightly elevated or normal in NAS, but it is not a sign of severe withdrawal or risk for complications. •
Choice F:
Oxygen saturation is a priority finding for a newborn with NAS. Oxygen saturation measures the amount of oxygen in the blood. Low oxygen saturation can indicate respiratory distress, which is a common and serious symptom of NAS. Respiratory distress can lead to hypoxia, acidosis, and brain damage. This choice requires immediate follow-up. •
Choice G:
Central nervous system disturbances are common and serious symptoms of NAS. They include tremors, irritability, excessive crying, hyperactivity, increased muscle tone, seizures, and sleep problems. These can indicate severe withdrawal and risk for neurological damage. This choice requires immediate follow-up.
Choice H:
Respiratory rate is a priority finding for a newborn with NAS. The respiratory rate measures the number of breaths per minute. A high respiratory rate can indicate respiratory distress, which is a common and serious symptom of NAS. Respiratory distress can lead to hypoxia, acidosis, and brain damage. This choice requires immediate follow-up.
A nurse is assisting in the care of a newborn who is 72 hours old and is receiving treatment for neonatal abstinence syndrome.
Which of the following data collection findings should the nurse identify as requiring immediate follow-up? (Select all that apply.).
Explanation
Choice A:
Blood pressure. The normal blood pressure range for a newborn is 60 to 80 mm Hg systolic and 40 to 50 mm Hg diastolic. The baby's blood pressure is low, which could indicate shock, dehydration, infection, or heart failure. This requires immediate follow-up to identify and treat the cause.
Choice B:
Gastrointestinal disturbances. Gastrointestinal disturbances such as vomiting and diarrhea are common symptoms of neonatal abstinence syndrome (NAS), which is a withdrawal syndrome of infants after birth caused by in-utero exposure to drugs of dependence, most commonly opioids. These symptoms are not life-threatening and can be managed with supportive care such as hydration, nutrition, and comfort measures.
Choice C:
Skin color. Skin color is not a reliable indicator of NAS, as it can vary depending on the baby's ethnicity, temperature, oxygenation, and circulation. Skin color alone does not require immediate follow-up unless it is accompanied by other signs of distress such as cyanosis, pallor, or jaundice.
Choice D:
NAS score. NAS score is a tool used to assess the severity of withdrawal symptoms in infants with NAS. It includes items such as tremors, irritability, sleep problems, muscle tone, reflexes, seizures, yawning, sneezing, feeding, vomiting, stooling and temperature. A high NAS score indicates that the baby needs more intensive treatment such as medication to ease the withdrawal process. A low NAS score indicates that the baby is coping well and may not need medication. The NAS score should be monitored frequently and adjusted according to the baby's response.
Choice E:
Temperature. The normal temperature range for a newborn is 36.5 to 37.5°C (97.7 to 99.5°F). The baby's temperature is high, which could indicate infection, dehydration or hyperthermia. This requires immediate follow-up to identify and treat the cause.
Choice F:
Oxygen saturation. The normal oxygen saturation range for a newborn is 95 to 100%. The baby's oxygen saturation is within the normal range and does not require immediate follow- up unless it drops below 90% or rises above 100%, which could indicate hypoxia or hyperoxia respectively.
Choice G:
Central nervous system disturbances. Central nervous system disturbances such as seizures, tremors, irritability, and overactive reflexes are common symptoms of NAS. These symptoms are not life-threatening and can be managed with supportive care such as swaddling, rocking, dimming lights, and reducing noise.
Choice H:
Respiratory rate. The normal respiratory rate range for a newborn is 40 to 60 breaths per minute. The baby's respiratory rate is high, which could indicate respiratory distress, infection, pain, or anxiety. This requires immediate follow-up to identify and treat the cause.
You just viewed 10 questions out of the 69 questions on the ATI Custom Maternity Final 23D Proctored Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



