custom Fluid and Electrolyte Exam Summer 2023 Proctored Exam
ATI custom Fluid and Electrolyte Exam Summer 2023 Proctored Exam
Total Questions : 45
Showing 10 questions Sign up for moreExplanation
Choice A rationale:
A phosphorus level of 4.5 mEq/L falls within the normal range, which is typically between 2.5 to 4.5 mEq/L. Although it's essential to monitor phosphorus levels, it is not the priority finding in this scenario.
Choice B rationale:
A potassium level of 2.9 mEq/L is the priority finding. The normal range for potassium is typically between 3.5 to 5.0 mEq/L. A potassium level of 2.9 mEq/L indicates severe hypokalemia, which can lead to life-threatening cardiac arrhythmias and muscle weakness. Immediate intervention is necessary to address the potassium imbalance.
Choice C rationale:
A calcium level of 8.2 mg/dL falls within the normal range (typically 8.5 to 10.2 mg/dL). While calcium levels are essential to monitor, they do not take precedence over the critically low potassium level in this situation.
Choice D rationale:
A sodium level of 145 mEq/L falls within the normal range, which is usually around 135 to 145 mEq/L. Although monitoring sodium levels is important, it is not the priority finding when compared to the critically low potassium level.
A nurse is caring for four hospitalized clients. Which of the following clients should the nurse identify as being at risk for fluid volume deficit?
Explanation
The correct answer is choice D. The client who has gastroenteritis and is febrile.
Choice A rationale:
The client with end-stage renal failure scheduled for dialysis would not be at risk for fluid volume deficit because dialysis is a treatment that removes waste, salt, and extra water to prevent them from building up in the body, keeping a safe level of certain chemicals in the blood, and controlling blood pressure.
Choice B rationale:
Being NPO (nothing by mouth) since midnight for endoscopy typically involves a short period of fasting. While it could potentially contribute to a mild fluid volume deficit, it is not as significant as other causes like vomiting or diarrhea, which can lead to more substantial fluid losses.
Choice C rationale:
A client with left-sided heart failure and an elevated BNP level is more likely to experience fluid volume overload rather than a deficit. BNP is released in response to ventricular volume expansion and pressure overload, which are indicative of heart failure, not fluid volume deficit.
Choice D rationale:
The client with gastroenteritis and a fever is at risk for fluid volume deficit due to increased fluid losses from vomiting, diarrhea, and fever-induced perspiration. These symptoms align with the common risk factors for fluid volume deficit, which include vomiting, diarrhea, and sweating.
The nurse is caring for a patient diagnosed with hypocalcemia. What additional assessments should the nurse include when caring for this patient?
Explanation
Other electrolyte disturbances.
Choice A rationale:
Drug toxicity is not directly related to hypocalcemia. The main concern in hypocalcemia is the calcium imbalance itself, not drug toxicity.
Choice B rationale:
Other electrolyte disturbances should be assessed because imbalances in other electrolytes, such as potassium and magnesium, are often associated with hypocalcemia. Electrolyte imbalances can interact and exacerbate each other, potentially leading to more severe complications.
Choice C rationale:
Hypertension is not a typical assessment finding in hypocalcemia. Hypertension is not directly related to calcium levels but may have other underlying causes.
Choice D rationale:
Visual disturbances are not commonly associated with hypocalcemia. Hypocalcemia is more likely to present with neuromuscular and cardiovascular symptoms, rather than visual disturbances.
A postoperative patient is diagnosed with fluid volume overload. What should the nurse expect to assess in this patient?
Explanation
Choice A rationale:
Fluid volume overload is an excess of fluid in the intravascular and/or interstitial spaces. One of the hallmark signs of fluid volume overload is distended neck veins, which indicates increased venous pressure due to the accumulation of fluid. The neck veins become more visible and prominent, especially when the patient is in a semi-Fowler's position.
Choice B rationale:
Poor skin turgor is a sign of dehydration, not fluid volume overload. It is characterized by the skin's inability to return to its normal position after being gently pinched. In fluid volume overload, the skin may become edematous and puffy, but it does not exhibit poor turgor.
Choice C rationale:
Concentrated hemoglobin and hematocrit levels are seen in conditions of dehydration or hemoconcentration, not in fluid volume overload. In fluid volume overload, there is excess fluid, which may lead to dilutional effects, resulting in decreased concentration of blood components.
Choice D rationale:
Decreased urine output is associated with fluid volume deficit (dehydration) rather than fluid volume overload. In fluid volume overload, there is often an increase in urine output as the body tries to eliminate the excess fluid.
A client is admitted to the emergency room with a respiratory rate of 7/min. Arterial blood gases (ABG) reveal the following values. Which of the following is an appropriate analysis of the ABGs? pH 7.22, PacO₂ 68 mm Hg, Base excess -2, PaO₂ 78 mm Hg, Saturation 80%, Bicarbonate 26 mEq/L.
Explanation
Respiratory acidosis.
Choice A rationale:
Metabolic alkalosis occurs when there is an increase in pH and bicarbonate (HCO₃⁻) levels, which is not the case here. The pH value in this scenario is 7.22, indicating acidosis.
Choice B rationale:
Respiratory acidosis results from the retention of carbon dioxide (PaCO₂) in the blood, leading to a decrease in pH. In this case, the pH is low (7.22), and the PacO₂ is elevated (68 mm Hg), supporting the diagnosis of respiratory acidosis.
Choice C rationale:
Metabolic acidosis is characterized by a decrease in pH and bicarbonate levels, along with a possible negative base excess. However, in this scenario, the base excess is -2, which does not indicate metabolic acidosis.
Choice D rationale:
Respiratory alkalosis occurs when there is a decrease in PaCO₂, leading to an increase in blood pH. The ABG values provided (pH 7.22, PacO₂ 68 mm Hg) are not consistent with respiratory alkalosis.
A nurse is reviewing the arterial blood gas results for a client in the ICU who has kidney failure and determines the client has respiratory acidosis. Which of the following findings should the nurse expect?
Explanation
Widened QRS Complexes.
Choice A rationale:
Hyperactive deep tendon reflexes are not typical findings in respiratory acidosis. They are more commonly associated with conditions like hypocalcemia or hypercalcemia.
Choice B rationale:
Warm, flushed skin is not directly related to respiratory acidosis. It is not a typical manifestation of this acid-base imbalance.
Choice C rationale:
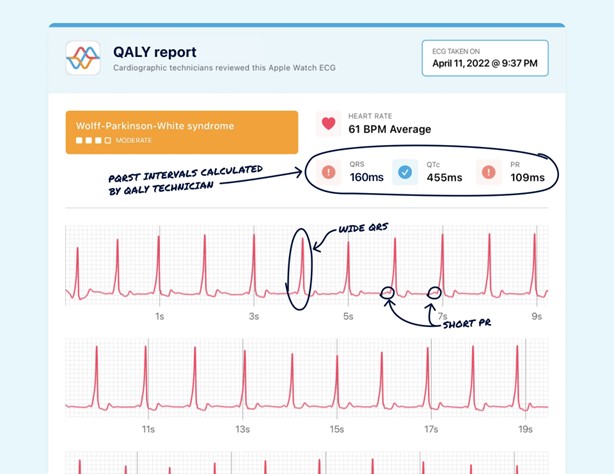
Widened QRS complexes on an ECG are characteristic findings in respiratory acidosis. Acidosis can lead to changes in the electrical conduction of the heart, resulting in QRS complex widening.
Choice D rationale:
Bounding peripheral pulses are not directly associated with respiratory acidosis. They may be seen in conditions like hyperthyroidism or anemia but are not specific to respiratory acidosis. Remember, always interpret lab results and clinical findings in the context of the patient's overall condition, medical history, and other relevant factors to provide the best care possible.
The nurse is planning care for a patient with severe burns. What health problem should the nurse realize that this patient could develop?
Explanation
Extracellular fluid deficit.
Choice A rationale:
Intracellular fluid deficit is a decrease in the fluid inside the cells, which may occur in conditions such as diabetic ketoacidosis. Severe burns are more likely to cause extracellular fluid shifts rather than intracellular fluid deficits.
Choice B rationale:
Interstitial fluid deficit involves a decrease in fluid in the interstitial spaces between cells. While burns can lead to fluid shifts, the primary concern is fluid loss from the vascular space (extracellular fluid).
Choice C rationale:
Intracellular fluid overload is not a typical health problem associated with severe burns. Burn injuries are more likely to cause fluid loss and shifts out of the intracellular space.
Choice D rationale:
Severe burns can result in significant loss of plasma and extracellular fluid, leading to hypovolemia and extracellular fluid deficit. This fluid loss can lead to hypovolemic shock and other complications if not adequately managed.
A nurse is caring for a client who has metabolic alkalosis. For which of the following clinical manifestations should the nurse monitor? (Select all that apply.).
Explanation
The correct answer is choice A, C, and D.
Choice A rationale:
Lethargy is a common symptom of metabolic alkalosis due to the body’s attempt to compensate for the altered pH balance, leading to decreased energy levels and fatigue.
Choice B rationale:
Kussmaul’s respirations are typically associated with metabolic acidosis, not alkalosis. These deep, labored breaths are the body’s way of trying to expel excess carbon dioxide to correct acidosis.
Choice C rationale:
Circumoral paresthesia, or tingling around the mouth, is a symptom of metabolic alkalosis. This occurs due to changes in calcium ion concentration affecting nerve function.
Choice D rationale:
Bicarbonate excess is a direct cause of metabolic alkalosis. Elevated bicarbonate levels in the blood lead to an increased pH, resulting in alkalosis.
Choice E rationale:
Flushing is not a typical symptom of metabolic alkalosis. It is more commonly associated with conditions that cause vasodilation or increased blood flow to the skin.
A patient newly diagnosed with diabetes mellitus is admitted to the emergency department with nausea, vomiting, and abdominal pain. ABG results reveal a pH of 7.2 and a bicarbonate level of 20 mEq/L. What other assessment findings should the nurse anticipate in this patient? Select all that apply.
Explanation
Choice A rationale:
Dysrhythmias are not a direct consequence of diabetic ketoacidosis (DKA) or the acid-base imbalance indicated by the patient's pH of 7.2 and bicarbonate level of 20 mEq/L. DKA primarily affects the respiratory system, leading to Kussmaul respirations, not dysrhythmias.
Choice B rationale:
Kussmaul respirations are an expected finding in a patient with diabetic ketoacidosis (DKA) and metabolic acidosis. These deep, rapid breaths are the body's attempt to compensate for the acidosis by eliminating excess CO2.
Choice C rationale:
Weakness is a common symptom of DKA. The hyperglycemia and acidosis result in intracellular dehydration and impaired cellular function, leading to weakness and fatigue.
Choice D rationale:
Cold, clammy skin is not typically associated with DKA. Instead, patients with DKA may have warm, dry skin due to dehydration and impaired thermoregulation.
Choice E rationale:
Tachycardia is an expected finding in a patient with DKA. The metabolic acidosis and dehydration lead to an increase in heart rate as the body attempts to maintain perfusion.
A patient has a serum phosphate level of 2.0 mg/dL. Which treatments should the nurse expect to be prescribed for this patient? Select all that apply.
Explanation
The correct answers are Choices B, C, and D.
Choice A rationale: Normal saline is not typically used to treat low phosphate levels. It is often used to treat dehydration and electrolyte imbalances that do not include hypophosphatemia.
Choice B rationale: Potassium phosphate is used to treat low phosphate levels. It directly supplements phosphate levels in the body, making it an appropriate treatment for hypophosphatemia.
Choice C rationale: Additional milk intake can help increase phosphate levels, as milk is a good source of phosphate. This is a suitable recommendation for a patient with low phosphate levels.
Choice D rationale: Increased Vitamin D intake can enhance phosphate absorption from the gastrointestinal tract, making it a beneficial treatment for a patient with low phosphate levels.
You just viewed 10 questions out of the 45 questions on the ATI custom Fluid and Electrolyte Exam Summer 2023 Proctored Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



