FUNDAMENTALS QUIZ
ATI FUNDAMENTALS QUIZ
Total Questions : 29
Showing 10 questions Sign up for moreA nurse is conducting an interview with a client. Which example best demonstrates use of open-ended questions in an interview?
Explanation
A. "Do you smoke?" This is a closed-ended question that can be answered with a simple "yes" or "no." It doesn't encourage elaboration or detailed responses.
B. "How are you feeling?" This is an open-ended question that encourages the client to provide more detailed and descriptive responses about their current state or feelings. It allows the client to share more information and gives the nurse a better understanding of their condition.
C. "Are you feeling well?" Similar to option A, this is a closed-ended question. It prompts a "yes" or "no" answer without inviting further discussion or detailed explanation.
D. "Do you use any illicit drugs?" This is another closed-ended question that requires a "yes" or "no" answer. It does not provide the opportunity for the client to discuss their drug use in detail.
A school nurse is concerned about the almost skeletal appearance of one of the high school students. Although all of the following nutritional problems can occur in adolescents, which one is most often associated with a negative self-concept?
Explanation
A. Obesity: While obesity can be linked to a negative self-concept, it is not as closely associated with a "skeletal appearance" as anorexia nervosa.
B. Fad dieting: Fad dieting may indicate concerns about body image, but it does not typically lead to a skeletal appearance and may not necessarily be tied to a deeply negative self-concept.
C. Anorexia nervosa: Anorexia nervosa is characterized by extreme weight loss and a skeletal appearance. It is often associated with a severely negative self-concept and distorted body image, where individuals see themselves as overweight even when they are underweight.
D. Eating fast foods: While this can lead to poor nutritional habits and weight issues, it does not typically lead to a skeletal appearance and is not directly associated with a negative self-concept.
Which type of play is most typical of the toddler stage?
Explanation
A. Parallel play: Parallel play is typical of toddlers, where they play alongside each other but do not interact or play directly with each other. This is a key stage in social development where they start to notice peers but prefer independent activities.
B. Cooperative play: Cooperative play involves children playing together with a common goal or activity. This type of play is more typical of older preschoolers and school-age children.
C. Solitary play: Solitary play is common in infants and very young toddlers where they play alone and are not engaged with others. By the toddler stage, children often progress to parallel play.
D. Associative play: Associative play involves children interacting and playing together, but not with a structured goal or organization. This typically develops after parallel play, around the preschool age.

A nurse is educating a group of middle adults about health promotion. What statement by one of the participants indicates the need for additional education?
Explanation
A. "I will make exercise a part of my daily activities." This is a positive and correct statement. Regular exercise is an important component of a healthy lifestyle and should be encouraged.
B. "I should eat a diet high in fats but low in fiber." This statement is incorrect and indicates a misunderstanding of healthy dietary guidelines. A diet high in fats and low in fiber is not recommended for maintaining health and can lead to various health issues like obesity, heart disease, and digestive problems.
C. "I only have one glass of wine a day with dinner." This statement aligns with moderate alcohol consumption guidelines, which suggest that up to one glass of wine per day for women and two for men can be part of a healthy lifestyle.
D. "I will begin a smoking cessation program this week." This statement reflects a positive health choice. Quitting smoking is one of the most beneficial actions a person can take for their health, reducing risks for many diseases.
You're assessing a 4-month-old infant. Which finding below is a normal milestone that should be reached by this infant at this age?
Explanation
A. Pincer grasp: The pincer grasp, which involves using the thumb and forefinger to pick up small objects, typically develops around 8 to 12 months of age, not at 4 months.
B. Rolls from tummy to back: At 4 months, many infants start to develop the ability to roll from their tummy to their back. This is a typical milestone for this age and reflects developing motor skills.
C. Walks with support: Walking with support usually begins around 9 to 12 months of age, much later than 4 months.
D. Rolls from back to tummy: Rolling from back to tummy typically occurs a bit later, often around 5 to 6 months. At 4 months, rolling from tummy to back is the more expected milestone.
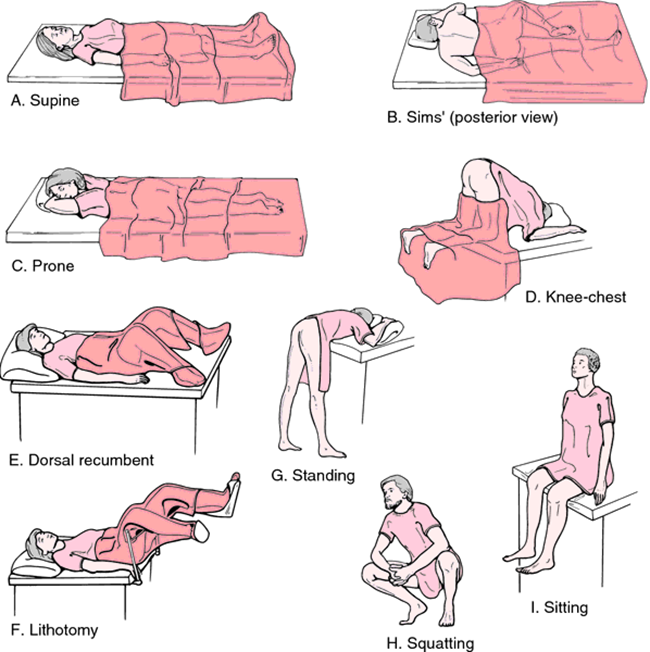
A nurse is preparing to examine the breasts of a client. In what position should the nurse place the client?
Explanation
A. Lithotomy: The lithotomy position is primarily used for gynecological exams and procedures, where the client is lying on their back with legs elevated and supported. It is not appropriate for breast examination.
B. Sims: The Sims position, where the client is lying on their side with one knee bent, is typically used for rectal exams and certain types of enemas. It is not suitable for breast examination.
C. Supine: The supine position, where the client lies flat on their back, is the most appropriate for breast examination. This position allows for better palpation and inspection of the breasts and facilitates a thorough examination.
D. Prone: The prone position involves lying face down. This position does not provide access to the breasts and is not used for breast examination.
A nurse is assessing a 12-month-old infant who is brought to the clinic by the parents for a well-child visit. The nurse reviews the infant's health history and notes that the infant weighed 8 lb at birth. When assessing the infant's weight at this visit, the nurse would anticipate that the infant would weigh approximately how much at this time?
Explanation
A. 20 lbs: This is a plausible estimate. By 12 months, an infant's birth weight typically triples. Therefore, an 8 lb birth weight would approximately translate to 24 lbs at 12 months.
B. 32 lbs: This estimate is too high. If an infant's birth weight triples by 12 months, an 8 lb birth weight would not be expected to reach 32 lbs.
C. 24 lbs: An infant's weight usually triples by their first birthday. Therefore, an infant born weighing 8 lbs would be expected to weigh about 24 lbs at 12 months.
D. 16 lbs: This is an underestimate. An 8 lb infant would double their birth weight by about 4 to 6 months, and by 12 months, they would typically have tripled their birth weight to around 24 lbs.
When assessing the abdomen, which assessment technique is used last?
Explanation
A. Percussion: Percussion is typically performed before palpation. It helps to detect differences in density of abdominal contents, fluid presence, and gas patterns.
B. Auscultation: Auscultation is performed before any palpation or percussion to prevent altering bowel sounds. It is typically the second step after inspection.
C. Palpation: Palpation is used last during an abdominal assessment to prevent altering the characteristics of bowel sounds and to ensure that any tenderness or abnormal masses are identified after a thorough initial assessment. Palpation can cause changes in bowel sounds and tenderness.
D. Inspection: Inspection is always the first step in any physical examination. It allows for a visual assessment of the abdomen, looking for distension, asymmetry, and skin changes.
A nurse is caring for a client who has returned to the unit following a surgical procedure. The client's oxygen saturation is 85%. Which of the following actions should the nurse take first?
Explanation
A. Administer oxygen at 2 L/min: Administering oxygen is important but should be done after positioning the client to improve natural ventilation.
B. Raise the head of the bed: Raising the head of the bed is the first action to take as it facilitates better lung expansion and improves ventilation. This can help increase the oxygen saturation more immediately and effectively.
C. Encourage coughing and deep breathing: Encouraging coughing and deep breathing is also beneficial to help clear secretions and improve lung function, but positioning the client for optimal breathing should be prioritized first.
D. Administer prescribed analgesic medication. Administering analgesics may be necessary for pain management, but it does not directly address the immediate need to improve oxygen saturation.
Upon entering the client's room at the beginning of a shift and throughout the shift, the nurse assesses the client. The nurse considers the client's plan of care and response to nursing interventions during the assessments. What type of assessment is the nurse performing?
Explanation
A. Ongoing assessment: Ongoing assessments are continuous evaluations performed throughout the nurse's shift to monitor the client's status, response to interventions, and to adjust the care plan as needed.
B. Focused assessment: A focused assessment is targeted on a specific problem or area of concern, rather than a general or comprehensive evaluation.
C. Emergency assessment: An emergency assessment is rapid and focuses on identifying life-threatening conditions or urgent needs. It is not a routine, ongoing assessment.
D. Comprehensive assessment: A comprehensive assessment is an in-depth evaluation of the client's overall health status, usually performed upon admission or during initial evaluation. It is not typically repeated throughout the shift.
You just viewed 10 questions out of the 29 questions on the ATI FUNDAMENTALS QUIZ Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



