Ati advanced med surg exam 3
Ati advanced med surg exam 3
Total Questions : 60
Showing 10 questions Sign up for moreA nurse is caring for a 73-year-old client in the emergency department (ED)
Explanation
A. Administering antibiotics helps target the suspected infection and prevent its spread. Broad-spectrum antibiotics are typically initiated until the specific pathogen is identified through cultures. This action should be completed as soon as possible within the first hour.
D. Lactate measurement is important in assessing tissue perfusion and the severity of sepsis. Elevated lactate levels indicate tissue hypoperfusion and can help identify patients at higher risk of mortality. Monitoring lactate levels guides resuscitation efforts and helps in assessing the response to treatment.
E. Fluid resuscitation is a cornerstone in the management of sepsis. Administering a large volume of intravenous fluids helps restore intravascular volume, improve tissue perfusion, and prevent further organ dysfunction. The recommended initial fluid bolus is 30 ml/kg of crystalloid solution, such as normal saline, administered rapidly within the first few hours of recognition of sepsis.
F. Blood cultures help identify the causative organism(s) responsible for the sepsis. This information is crucial for guiding antibiotic therapy, especially in cases of severe sepsis or septic shock. Blood cultures should be obtained before initiating antibiotic therapy to maximize their sensitivity and specificity.
B. Type and cross-match for packed red blood cells (PRBCs) are indicated in situations where blood transfusion may be required, such as severe anemia or active bleeding. While sepsis can lead to various complications, such as disseminated intravascular coagulation (DIC), the priority in the first hour is resuscitation and antibiotic administration.
G. Obtaining a urine specimen may be indicated to assess for urinary tract infection (UTI), which can be a potential source of sepsis. However, in the initial management of sepsis, obtaining blood cultures (option F) takes precedence as blood cultures provide more critical information for guiding antibiotic therapy.
H. Obtaining a wound culture may help identify the specific pathogens present in the wound and guide antibiotic therapy if the wound is suspected to be the source of sepsis. However, in the first hour of managing sepsis, the priority is to initiate broad-spectrum antibiotics and obtain blood cultures, as these interventions are more urgent in preventing further complications from sepsis.
A nurse is collecting a medication history from a client who is scheduled to have a cardiac catheterization. Which of the following medications taken by the client interacts with contrast material and places the client at risk for acute kidney injury?
Explanation
B Metformin is an oral antidiabetic medication commonly used to treat type 2 diabetes. There is a potential risk of lactic acidosis when metformin is used in conjunction with contrast material, particularly in patients with underlying renal impairment. Contrast-induced nephropathy can exacerbate renal dysfunction, leading to increased levels of metformin and potentially increasing the risk of lactic acidosis. Therefore, metformin use before or after contrast administration should be carefully monitored, and in some cases, temporarily discontinued to reduce the risk of lactic acidosis.
A Atorvastatin is a statin medication commonly used to lower cholesterol levels. It does not have a direct interaction with contrast material used in cardiac catheterization. Therefore, it does not place the client at risk for acute kidney injury related to contrast-induced nephropathy (CIN).
C Carvedilol is a beta-blocker medication used to treat high blood pressure and heart failure. It does not have a direct interaction with contrast material used in cardiac catheterization. Therefore, it does not place the client at risk for acute kidney injury related to contrast-induced nephropathy (CIN).
D Nitroglycerin is a medication commonly used to relieve chest pain (angina) in patients with coronary artery disease. It does not have a direct interaction with contrast material used in cardiac catheterization. Therefore, it does not place the client at risk for acute kidney injury related to contrast- induced nephropathy (CIN).
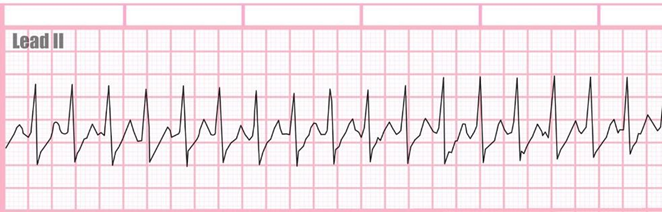
A nurse in an urgent care center is assessing a client who reports a sudden onset of irregular palpitations, fatigue, and dizziness. The nurse finds a rapid and irregular heart rate with a significant pulse deficit. Which of the following dysrhythmias should the nurse expect to find on the ECG?
Explanation
C Atrial fibrillation (AF) is characterized by rapid, irregular electrical activity in the atria, leading to an irregularly irregular ventricular response. AF often results in palpitations, fatigue, and dizziness due to the irregular heart rhythm and inefficient cardiac output. A significant pulse deficit may also be present due to the irregularity of the ventricular response compared to the atrial activity. Given the sudden onset of irregular palpitations, fatigue, dizziness, and a significant pulse deficit, atrial fibrillation is a likely dysrhythmia in this scenario.

A First-degree AV block is characterized by a prolonged PR interval on the electrocardiogram (ECG), indicating delayed conduction between the atria and ventricles. While it can indicate conduction system abnormalities, it typically does not result in rapid or irregular palpitations, fatigue, or dizziness.
Therefore, it is less likely to be the cause of the client's symptoms.
B Sinus tachycardia is characterized by a rapid heart rate originating from the sinus node, typically with a regular rhythm. While sinus tachycardia can cause palpitations and fatigue, it is less likely to result in an irregular heart rate with a significant pulse deficit. Therefore, it is less likely to be the cause of the client's symptoms.
D Sinus bradycardia is characterized by a slow heart rate originating from the sinus node. While sinus bradycardia can cause fatigue and dizziness, it typically does not result in a rapid or irregular heart rate. Therefore, it is less likely to be the cause of the client's symptoms.
Norepinephrine has been prescribed for a patient who was admitted with dehydration and hypotension. Which data indicate that the nurse should consult with the health care provider before starting the norepinephrine?
Explanation
A Adequate fluid administration is essential before giving vasopressors to patients with hypovolemic shock. The patient’s low central venous pressure indicates a need for more volume replacement. The other patient data are not contraindications to norepinephrine administration.
B Low dose dopamine is not a contraindication to epinephrine administration.
C A sinus tachycardia is not a contraindication to epinephrine administration
D Lack of urine output is not a contraindication to epinephrine administration
Mr Jones came to the ER complaining of chest palpitations. He states his heart feels like it is "racing". The nurse found the following rhythm on the monitor. What is the next step would the nurse expect to take first?
Explanation
B This maneuver, called the Valsalva maneuver, can sometimes help to restore normal heart rhythm in cases of SVT. It involves blowing forcefully into a syringe or performing a similar action that increases intra-abdominal pressure, which can stimulate the vagus nerve and help to slow down the heart rate.
A Defibrillation is a treatment used for life-threatening cardiac arrhythmias, particularly ventricular fibrillation or pulseless ventricular tachycardia. It involves delivering a therapeutic dose of electrical energy to the heart with a device called a defibrillator.
C Drawing troponin levels may be appropriate if there is suspicion of myocardial infarction as the cause of chest palpitations or if there are other symptoms suggestive of acute coronary syndrome. However, in the context of SVT presenting with chest palpitations and a racing heart, the priority is to address the arrhythmia first
D Amiodarone is an antiarrhythmic medication used to treat various types of cardiac arrhythmias, including ventricular and supraventricular arrhythmias. While it can be effective in certain cases of SVT, it is not typically the first-line treatment or the immediate next step in managing SVT in the emergency department.
A nurse is monitoring a client who is receiving a unit of packed RBCs following surgery. Which of the following assessments is an indication that the client might be experiencing circulatory overload?
Explanation
C Dyspnea, or difficulty breathing, is a classic symptom of circulatory overload. When the circulatory system is overloaded with excess fluid, it can lead to pulmonary congestion and impaired gas exchange, resulting in dyspnea. Patients experiencing circulatory overload may exhibit signs such as shortness of breath, increased respiratory rate, and crackles on lung auscultation.
A Flushing, or the sudden reddening of the skin, is not typically associated with circulatory overload. Instead, it can be a symptom of various conditions such as fever, allergic reactions, or hormonal changes. While circulatory overload may lead to fluid retention and increased blood volume, flushing is not a characteristic symptom.
B Vomiting is also not a typical symptom of circulatory overload. Vomiting can be caused by various factors such as anesthesia, pain medications, or postoperative ileus. While fluid overload can result in gastrointestinal symptoms like nausea and abdominal discomfort, vomiting is not a specific indicator of circulatory overload.
D Bradycardia, or a slow heart rate, is not typically associated with circulatory overload. Instead, it can be caused by factors such as medications (e.g., opioids, beta-blockers), vagal stimulation, or underlying cardiac conditions. In circulatory overload, the body's compensatory response is often tachycardia (increased heart rate) rather than bradycardia.
A nurse is assessing a client who has atrial fibrillation. Which of the following pulse characteristics should the nurse expect?
Explanation
A In atrial fibrillation (AF), the electrical activity in the atria is chaotic, leading to an irregularly irregular ventricular response. As a result, the pulse felt at the radial artery will be irregular, with no discernible pattern. The irregularity is a hallmark feature of AF and is often described as "irregularly irregular."
B Bounding pulses are characterized by a strong and forceful pulsation felt at the arterial pulse sites. In atrial fibrillation, the irregular and rapid ventricular response can lead to an increased stroke volume and forceful contraction of the left ventricle during diastole, resulting in bounding pulses. However, bounding pulses are not typically associated with atrial fibrillation; they are more commonly seen in conditions such as aortic regurgitation or hyperdynamic circulation.
C In some cases of atrial fibrillation, especially if the ventricular rate is very rapid or irregularly irregular, the pulse may not be palpable due to the inconsistent ventricular contractions.
However, in most cases of atrial fibrillation, a pulse is palpable, albeit irregular.
D Atrial fibrillation can result in a rapid ventricular response, leading to a fast heart rate. However, the pulse rate can vary widely among individuals with atrial fibrillation. While some may have a rapid heart rate (tachycardia), others may have a slower heart rate (bradycardia), depending on factors such as concomitant medications, autonomic tone, and the presence of underlying heart disease.
Which information about a patient who is receiving cisatracurium (Nimbex) to prevent asynchronous breathing with the positive pressure ventilator requires action by the nurse?
Explanation
D Sedatives are typically administered alongside neuromuscular blockers to ensure the patient's comfort and prevent awareness during mechanical ventilation.
A The absence of a cough reflex when suctioned is expected in a patient receiving cisatracurium (Nimbex) because it is a neuromuscular blocking agent that induces paralysis. Cisatracurium inhibits skeletal muscle movement, including the muscles involved in coughing.
B An oxygen saturation between 90% to 93% is within an acceptable range for a patient in this condition.
C The lack of response to voice may indicate that the patient is sedated or experiencing effects from the neuromuscular blocking agent. However, since the patient is receiving cisatracurium to prevent asynchronous breathing with the positive pressure ventilator, it's expected that the patient will not respond to voice due to the medication-induced paralysis.
The nurse is caring for a client who has heart failure with an EF of 40%. The client has a BP of 170/67 with an HR of 60. He currently is in normal sinus rhythm and has an amber urine output of 45ml in the last 3 hours. Which medication would the nurse expect to give first?
Explanation
D Normal saline bolus administration is indicated for hypovolemia or inadequate intravascular volume, which can lead to decreased cardiac output and hypotension. In this scenario, the client has an amber urine output of 45ml in the last 3 hours, indicating decreased urine output and potential hypovolemia. The elevated blood pressure (170/67 mmHg) suggests possible volume overload or fluid retention, but the decreased urine output raises concerns for inadequate intravascular volume. Therefore, administering a normal saline bolus may be the first priority to optimize intravascular volume and improve cardiac output.
A Isosorbide mononitrate is a vasodilator commonly used in the treatment of heart failure and angina. It helps reduce preload and afterload, thereby decreasing the workload on the heart. However, in this scenario, the client's blood pressure is elevated (170/67 mmHg), and there is no indication of acute decompensation or pulmonary congestion. Therefore, isosorbide PO may not be the first priority medication at this time.
B Nitroglycerin is a potent vasodilator commonly used to manage acute heart failure exacerbations and acute coronary syndromes. It helps reduce preload and afterload, improving cardiac output and relieving symptoms of heart failure. In this scenario, the client's blood pressure is elevated, but the heart rate is normal, and there are no signs of acute decompensation. Therefore, initiating a nitroglycerin drip may not be the first priority unless the client develops symptoms of acute decompensation or pulmonary congestion.
C Dopamine is a vasopressor medication that can be used to increase blood pressure and cardiac output in patients with hypotension or shock. However, in this scenario, the client's blood pressure is elevated (170/67 mmHg), and there is no evidence of hypotension. Therefore, initiating a dopamine drip may not be appropriate at this time and could potentially exacerbate hypertension.
A patient who has been involved in a motor vehicle crash arrives in the emergency department (ED) with cool, clammy skin; tachycardia; and hypotension. Which intervention prescribed by the health care provider should the nurse implement first?
Explanation
A The first intervention should be to ensure adequate oxygenation, as hypoxia can exacerbate shock. Therefore, providing oxygen at 100% via a non-rebreather mask is the most critical initial step. This intervention helps to maximize the amount of oxygen delivered to the patient's lungs and subsequently to the rest of the body, supporting vital organ function while further assessments and interventions are prepared.
B Continuous ECG monitoring allows for the assessment of the patient's heart rhythm, rate, and any signs of dysrhythmias or cardiac ischemia. This intervention is important for detecting any life- threatening arrhythmias, such as ventricular tachycardia or fibrillation, which may require immediate intervention. While ECG monitoring is important, it may not be the highest priority intervention.
C Drawing blood for type and crossmatch is important for preparing for potential blood transfusions if significant blood loss is suspected. However, this intervention may take some time to process, and immediate stabilization of the patient's condition is paramount.
D Large-bore IV catheters allow for rapid infusion of fluids to restore intravascular volume and improve tissue perfusion. This intervention is critical for stabilizing the patient's hemodynamic status and takes precedence in the management of shock. However, oxygenation should take priority.
You just viewed 10 questions out of the 60 questions on the Ati advanced med surg exam 3 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



