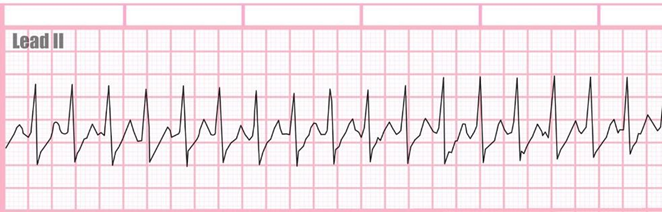
Mr Jones came to the ER complaining of chest palpitations. He states his heart feels like it is "racing". The nurse found the following rhythm on the monitor. What is the next step would the nurse expect to take first?
Defibrillate
Ask him to blow into a syringe
Draw troponins
Give amiodarone
The Correct Answer is B
B This maneuver, called the Valsalva maneuver, can sometimes help to restore normal heart rhythm in cases of SVT. It involves blowing forcefully into a syringe or performing a similar action that increases intra-abdominal pressure, which can stimulate the vagus nerve and help to slow down the heart rate.
A Defibrillation is a treatment used for life-threatening cardiac arrhythmias, particularly ventricular fibrillation or pulseless ventricular tachycardia. It involves delivering a therapeutic dose of electrical energy to the heart with a device called a defibrillator.
C Drawing troponin levels may be appropriate if there is suspicion of myocardial infarction as the cause of chest palpitations or if there are other symptoms suggestive of acute coronary syndrome. However, in the context of SVT presenting with chest palpitations and a racing heart, the priority is to address the arrhythmia first
D Amiodarone is an antiarrhythmic medication used to treat various types of cardiac arrhythmias, including ventricular and supraventricular arrhythmias. While it can be effective in certain cases of SVT, it is not typically the first-line treatment or the immediate next step in managing SVT in the emergency department.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["C","D","E","F"]
Explanation
A. Administering antibiotics helps target the suspected infection and prevent its spread. Broad-spectrum antibiotics are typically initiated until the specific pathogen is identified through cultures. This action should be completed as soon as possible within the first hour.
D. Lactate measurement is important in assessing tissue perfusion and the severity of sepsis. Elevated lactate levels indicate tissue hypoperfusion and can help identify patients at higher risk of mortality. Monitoring lactate levels guides resuscitation efforts and helps in assessing the response to treatment.
E. Fluid resuscitation is a cornerstone in the management of sepsis. Administering a large volume of intravenous fluids helps restore intravascular volume, improve tissue perfusion, and prevent further organ dysfunction. The recommended initial fluid bolus is 30 ml/kg of crystalloid solution, such as normal saline, administered rapidly within the first few hours of recognition of sepsis.
F. Blood cultures help identify the causative organism(s) responsible for the sepsis. This information is crucial for guiding antibiotic therapy, especially in cases of severe sepsis or septic shock. Blood cultures should be obtained before initiating antibiotic therapy to maximize their sensitivity and specificity.
B. Type and cross-match for packed red blood cells (PRBCs) are indicated in situations where blood transfusion may be required, such as severe anemia or active bleeding. While sepsis can lead to various complications, such as disseminated intravascular coagulation (DIC), the priority in the first hour is resuscitation and antibiotic administration.
G. Obtaining a urine specimen may be indicated to assess for urinary tract infection (UTI), which can be a potential source of sepsis. However, in the initial management of sepsis, obtaining blood cultures (option F) takes precedence as blood cultures provide more critical information for guiding antibiotic therapy.
H. Obtaining a wound culture may help identify the specific pathogens present in the wound and guide antibiotic therapy if the wound is suspected to be the source of sepsis. However, in the first hour of managing sepsis, the priority is to initiate broad-spectrum antibiotics and obtain blood cultures, as these interventions are more urgent in preventing further complications from sepsis.
Correct Answer is A
Explanation
A. A heart murmur typically indicates turbulent blood flow through a heart valve. This turbulence can occur due to various reasons, such as valve stenosis (narrowing), regurgitation (leakage), or structural abnormalities of the valves. The turbulent flow produces audible sounds that can be heard with a stethoscope during cardiac auscultation.
B. A heart murmur is not caused by blood entering an inflexible chamber. Instead, it is caused by turbulent blood flow through the heart valves. The sound produced by this turbulent flow may vary depending on the underlying pathology of the valve.
C. While heart murmurs can be described based on their characteristics (such as high-pitched or low- pitched), the presence of a heart murmur does not necessarily indicate a narrow valve. Murmurs can occur due to various valve abnormalities, including stenosis (narrowing) or regurgitation (leakage). The pitch and quality of the murmur may vary depending on the underlying pathology and the location of the abnormality.
D. A heart murmur is not typically associated with inflammation around the heart. While inflammation of the heart (such as myocarditis or pericarditis) can cause symptoms and abnormal sounds, these conditions would not be described specifically as a "heart murmur."
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
