Which of the following is a common cause of cardiogenic shock?
Anaphylaxis
Hypovolemia
Pulmonary embolism
Myocardial infarction
The Correct Answer is D
D. Myocardial infarction (heart attack) is a common cause of cardiogenic shock. In myocardial infarction, part of the heart muscle becomes ischemic or necrotic due to occlusion of a coronary artery. This leads to impaired cardiac function and reduced cardiac output, resulting in cardiogenic shock. Prompt recognition and treatment of myocardial infarction are crucial to prevent or manage cardiogenic shock.
A. Anaphylaxis is a severe allergic reaction that can lead to systemic vasodilation and distributive shock, but it is not a common cause of cardiogenic shock. In anaphylaxis, the primary mechanism of shock is typically related to widespread vasodilation and increased vascular permeability rather than impaired cardiac function.
B. Hypovolemic shock occurs due to a decrease in intravascular volume, leading to inadequate tissue perfusion. It is not a common cause of cardiogenic shock, as the underlying mechanism is different. In hypovolemic shock, the primary issue is the loss of circulating blood volume, whereas cardiogenic shock involves impaired cardiac function.
C. Pulmonary embolism can lead to acute right heart strain or failure, which may result in hemodynamic instability and shock. However, pulmonary embolism typically causes obstructive shock rather than cardiogenic shock. Obstructive shock occurs when blood flow is obstructed, such as by a pulmonary embolism, leading to reduced cardiac output.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
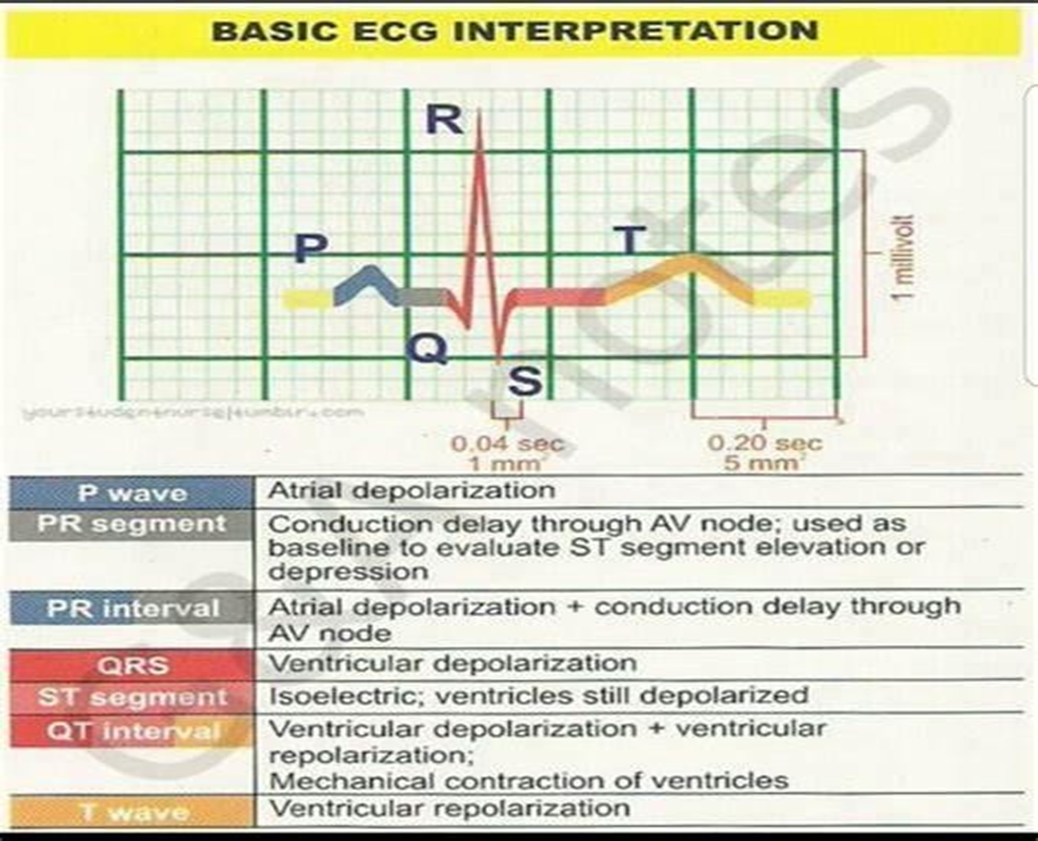
B. The QT interval represents ventricular depolarization and repolarization. It starts at the beginning of the QRS complex and ends at the end of the T wave. The QT interval reflects the total time it takes for both ventricular depolarization and repolarization to occur. Prolongation of the QT interval can be associated with an increased risk of arrhythmias, including torsades de pointes.
A. The QRS complex represents ventricular depolarization, which is the electrical activation of the ventricles. The duration of the QRS complex provides information about the time it takes for ventricular depolarization to occur. A prolonged QRS complex can indicate abnormalities in ventricular conduction, such as bundle branch blocks or ventricular hypertrophy.
C. The ST segment represents the early part of ventricular repolarization. It starts at the end of the QRS complex and ends at the beginning of the T wave. Changes in the ST segment, such as elevation or depression, can indicate myocardial ischemia or injury.
D. The PR interval represents the time it takes for the electrical impulse to travel from the atria to the ventricles. It includes atrial depolarization, atrial contraction, and the delay at the atrioventricular node. The PR interval does not specifically provide information about ventricular depolarization and repolarization.
Correct Answer is D
Explanation
D Sedatives are typically administered alongside neuromuscular blockers to ensure the patient's comfort and prevent awareness during mechanical ventilation.
A The absence of a cough reflex when suctioned is expected in a patient receiving cisatracurium (Nimbex) because it is a neuromuscular blocking agent that induces paralysis. Cisatracurium inhibits skeletal muscle movement, including the muscles involved in coughing.
B An oxygen saturation between 90% to 93% is within an acceptable range for a patient in this condition.
C The lack of response to voice may indicate that the patient is sedated or experiencing effects from the neuromuscular blocking agent. However, since the patient is receiving cisatracurium to prevent asynchronous breathing with the positive pressure ventilator, it's expected that the patient will not respond to voice due to the medication-induced paralysis.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
