A patient with respiratory failure has a respiratory rate of 26 breaths/min and an oxygen saturation (SpO2) of 80%. The patient is increasingly pale and restless but follows commands. Which intervention will the nurse anticipate?
Initiation of continuous positive pressure ventilation (CPAP)
Endotracheal intubation and positive pressure ventilation
Insertion of a mini-tracheostomy with frequent suctioning
Administration of 100% O2 by non-rebreather mask
The Correct Answer is B
B. Endotracheal intubation and positive pressure ventilation are indicated in patients with respiratory failure who are unable to maintain adequate oxygenation or ventilation with non-invasive interventions. Intubation allows for the delivery of positive pressure ventilation, oxygenation, and airway protection. It also facilitates the clearance of secretions and administration of medications. Given the patient's severe hypoxemia, impending respiratory distress, and deteriorating condition, endotracheal intubation and positive pressure ventilation are the most appropriate interventions to ensure adequate oxygenation and prevent further deterioration.
A. CPAP is a non-invasive ventilation modality that provides a continuous positive pressure to the airways throughout the respiratory cycle. While CPAP may be beneficial in certain cases of respiratory failure, it may not be sufficient for a patient with severe hypoxemia (SpO2 of 80%) and impending respiratory distress. CPAP is typically indicated for patients with conditions such as obstructive sleep apnea or mild to moderate respiratory failure.
C. Mini-tracheostomy may be considered in certain cases of upper airway obstruction or inadequate airway clearance. However, in this scenario, the patient's hypoxemia is likely due to severe respiratory failure rather than upper airway obstruction. While suctioning may be necessary to clear secretions, it does not address the underlying cause of hypoxemia or provide ventilatory support.
D. While administration of supplemental oxygen is important in the management of hypoxemia, a non- rebreather mask may not be sufficient for a patient with severe hypoxemia and impending respiratory distress. Non-rebreather masks can deliver high concentrations of oxygen but may not provide adequate positive pressure support or airway protection. In this case, endotracheal intubation and positive pressure ventilation are more appropriate to ensure adequate oxygenation and ventilation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. Prone positioning involves turning the patient onto their abdomen to improve ventilation-perfusion matching by redistributing ventilation to the dorsal lung regions, where perfusion is typically better in ARDS patients.
B. Semi-recumbent positioning may be used to prevent aspiration and reduce the risk of VAP but is not as effective as prone positioning for improving V/Q matching.
C. Albumin infusion is not specific interventions for improving ventilation-perfusion matching in ARDS and should be considered based on other clinical indications.
D. Transfusion of packed red blood cells (PRBC) may be indicated in cases of severe anemia or hypoxemia due to inadequate oxygen-carrying capacity. However, it is not a primary intervention for improving ventilation-perfusion matching in ARDS
Correct Answer is B
Explanation
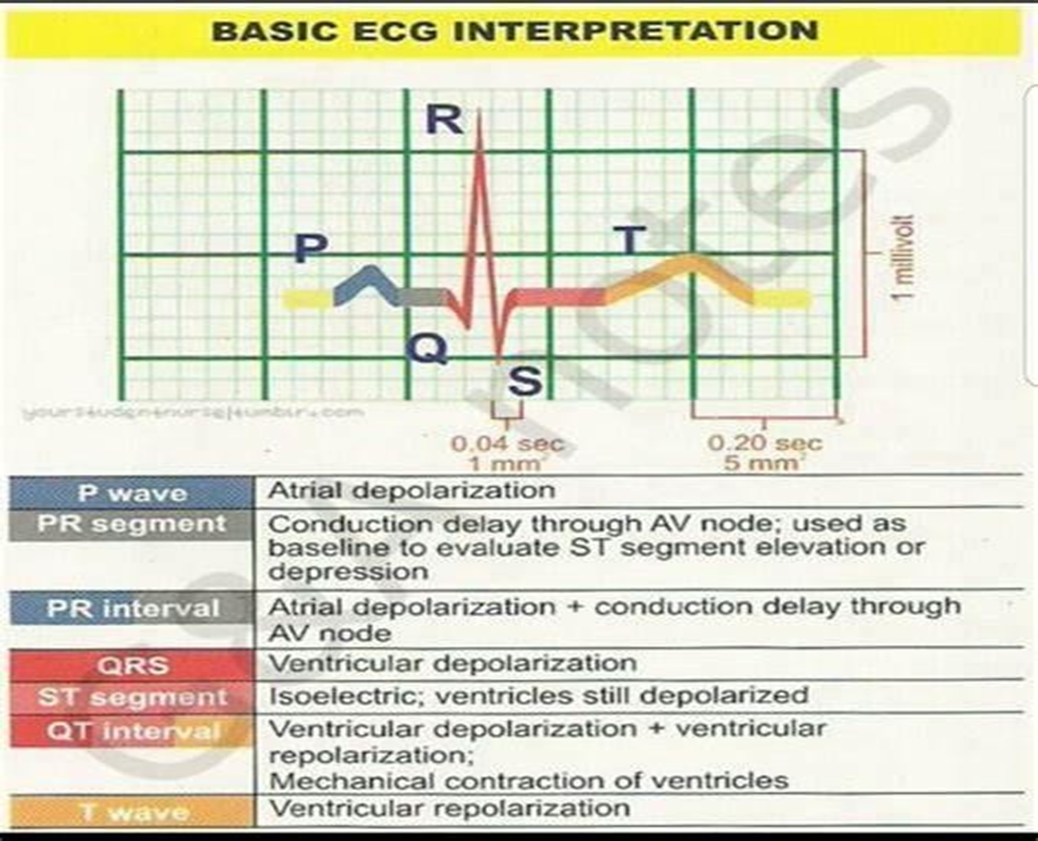
B. The QT interval represents ventricular depolarization and repolarization. It starts at the beginning of the QRS complex and ends at the end of the T wave. The QT interval reflects the total time it takes for both ventricular depolarization and repolarization to occur. Prolongation of the QT interval can be associated with an increased risk of arrhythmias, including torsades de pointes.
A. The QRS complex represents ventricular depolarization, which is the electrical activation of the ventricles. The duration of the QRS complex provides information about the time it takes for ventricular depolarization to occur. A prolonged QRS complex can indicate abnormalities in ventricular conduction, such as bundle branch blocks or ventricular hypertrophy.
C. The ST segment represents the early part of ventricular repolarization. It starts at the end of the QRS complex and ends at the beginning of the T wave. Changes in the ST segment, such as elevation or depression, can indicate myocardial ischemia or injury.
D. The PR interval represents the time it takes for the electrical impulse to travel from the atria to the ventricles. It includes atrial depolarization, atrial contraction, and the delay at the atrioventricular node. The PR interval does not specifically provide information about ventricular depolarization and repolarization.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
