A nurse in an urgent care center is assessing a client who reports a sudden onset of irregular palpitations, fatigue, and dizziness. The nurse finds a rapid and irregular heart rate with a significant pulse deficit. Which of the following dysrhythmias should the nurse expect to find on the ECG?
Sinus bradycardia
Sinus tachycardia
Atrial fibrillation
First-degree AV block
The Correct Answer is C
Choice A Reason: This is incorrect. Sinus bradycardia is a slow and regular heart rate that originates from the sinus node. It does not cause irregular palpitations, fatigue, or dizziness, unless the heart rate is very low or the client has underlying cardiac disease.
Choice B reason: This is incorrect. Sinus tachycardia is a fast and regular heart rate that originates from the sinus node. It may cause fatigue or dizziness, but not irregular palpitations or pulse deficit.
Choice C Reason: This is correct. Atrial fibrillation is a fast and irregular heart rate that originates from multiple foci in the atria. It causes irregular palpitations, fatigue, dizziness, and pulse deficit due to ineffective atrial contractions and variable ventricular response.
Choice D Reason: This is incorrect. First-degree AV block is a delay in the conduction of impulses from the atria to the ventricles. It does not affect the heart rate or rhythm, and does not cause any symptoms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","C","E"]
Explanation
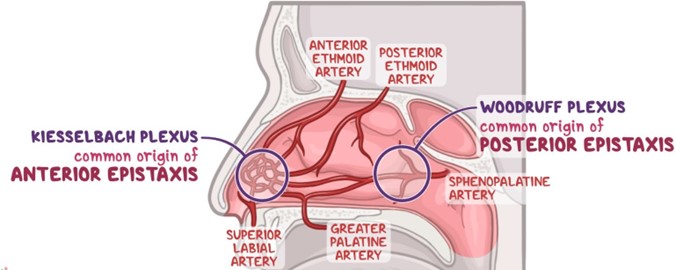
Choice A Reason: This is correct because placing ice to the bridge of the client’s nose can cause vasoconstriction and reduce blood flow to the nasal mucosa.
Choice B Reason: This is incorrect because tilting the client's head backward can cause blood to drain into the throat and increase the risk of aspiration, nausea, and vomiting.
Choice C Reason: This is correct because moving the client into high-Fowler position can lower the blood pressure in the head and neck and decrease bleeding.
Choice D reason Reason This is incorrect because instructing the client to blow his nose can dislodge any clots that have formed and worsen bleeding.
Choice E Reason: This is correct because applying pressure to the nares can compress the bleeding site and promote clotting.
Correct Answer is C
Explanation
Choice A Reason: This is incorrect. Sinus bradycardia is a slow and regular heart rate that originates from the sinus node. It does not cause irregular palpitations, fatigue, or dizziness, unless the heart rate is very low or the client has underlying cardiac disease.
Choice B reason: This is incorrect. Sinus tachycardia is a fast and regular heart rate that originates from the sinus node. It may cause fatigue or dizziness, but not irregular palpitations or pulse deficit.
Choice C Reason: This is correct. Atrial fibrillation is a fast and irregular heart rate that originates from multiple foci in the atria. It causes irregular palpitations, fatigue, dizziness, and pulse deficit due to ineffective atrial contractions and variable ventricular response.
Choice D Reason: This is incorrect. First-degree AV block is a delay in the conduction of impulses from the atria to the ventricles. It does not affect the heart rate or rhythm, and does not cause any symptoms.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
