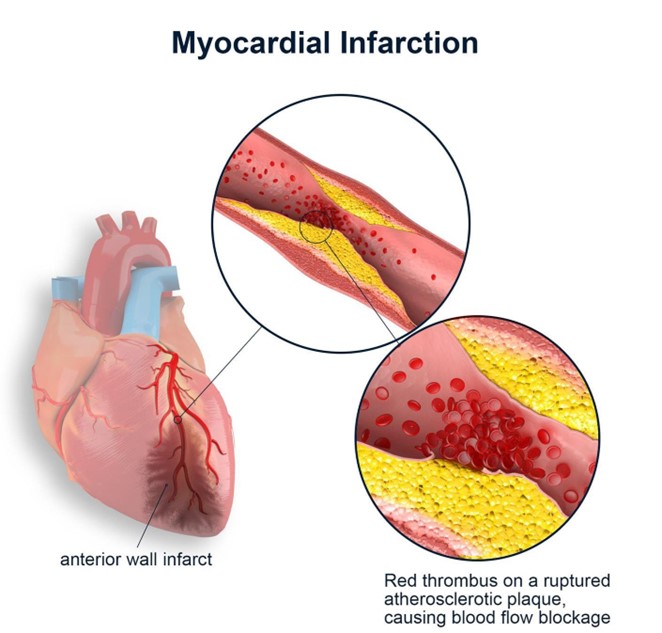
A nurse is admitting a client who has acute heart failure following myocardial infarction (MI). The nurse recognizes that which of the following prescriptions by the provider requires clarification?
Laboratory testing of serum potassium upon admission
Bumetanide 1 mg IV bolus every 12 hr
0.9% normal saline IV at 50 mL/hr continuous
Morphine sulfate 2 mg IV bolus every 2 hr PRN pain
The Correct Answer is C
Choice A Reason: This choice is incorrect because laboratory testing of serum potassium upon admission is an appropriate prescription for a client who has acute heart failure following MI. Serum potassium is an electrolyte that affects the cardiac function and rhythm. A normal serum potassium range is 3.5 to 5 mEq/L, and an abnormal level can indicate hypokalemia or hyperkalemia, which can cause arrhythmias, muscle weakness, or paralysis. Therefore, monitoring serum potassium is important to detect and correct any electrolyte imbalance and prevent complications.
Choice B Reason: This choice is incorrect because bumetanide 1 mg IV bolus every 12 hr is an appropriate prescription for a client who has acute heart failure following MI. Bumetanide is a loop diuretic that helps to reduce fluid retention and edema by increasing the urine output and sodium excretion. It may be used for clients who have heart failure, hypertension, or renal impairment, but it can cause hypokalemia, hypotension, or dehydration.
Therefore, administering bumetanide as prescribed can help to improve the cardiac output and reduce the preload and afterload.
Choice C Reason: This choice is correct because 0.9% normal saline IV at 50 mL/hr continuous is an inappropriate prescription for a client who has acute heart failure following MI. 0.9% normal saline is an isotonic solution that contains the same concentration of solutes as blood plasma. It may be used for clients who have fluid loss, dehydration, or shock, but it can worsen fluid overload and pulmonary edema in clients who have acute heart failure. Therefore, clarifying this prescription with the provider is necessary to prevent further deterioration of the client's condition.
Choice D Reason: This choice is incorrect because morphine sulfate 2 mg IV bolus every 2 hr PRN pain is an appropriate prescription for a client who has acute heart failure following MI. Morphine sulfate is an opioid analgesic that helps to relieve pain and anxiety by binding to the opioid receptors in the brain and spinal cord. It may be used for clients who have moderate to severe pain, dyspnea, or chest discomfort, but it can cause respiratory depression, hypotension, or nausea. Therefore, administering morphine sulfate as prescribed can help to reduce the oxygen demand and improve the cardiac function.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["24"]
Explanation
- To find the concentration of heparin in the solution, divide the amount of heparin by the volume of D5W: 25,000 units / 500 mL = 50 units/mL
- To find the infusion rate, divide the prescribed dose by the concentration: 1,200 units/hr / 50 units/mL = 24 mL/hr
- Round the answer to the nearest tenth/whole number: 24 mL/hr
Correct Answer is A
Explanation
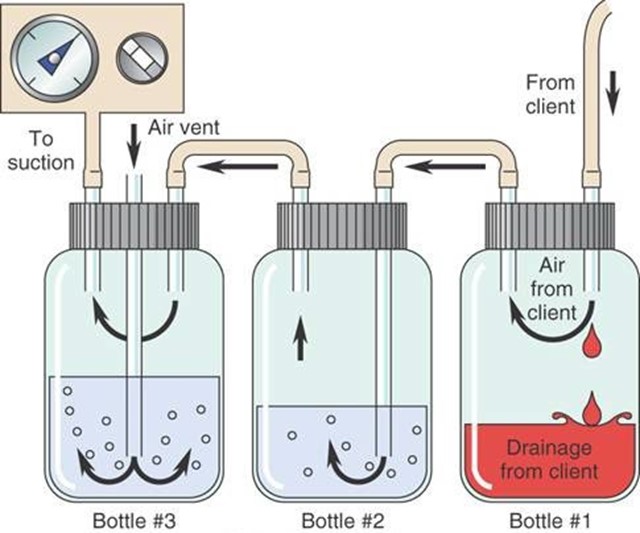
Choice A Reason: Continuous bubbling in the water-seal chamber indicates an air leak in the chest tube system, which can compromise the drainage of air and fluid from the pleural space and impair lung expansion.
Choice B Reason: Occasional bubbling in the water-seal chamber is normal and expected, as it indicates that air is being removed from the pleural space.
Choice C Reason: Fluctuations in the fluid level in the water-seal chamber are normal and expected, as they reflect changes in intrathoracic pressure during inspiration and expiration.
Choice D Reason: Constant bubbling in the suction-control chamber is normal and expected, as it indicates that suction is being applied to the chest tube system.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
