Med Surg Exam 1
ATI Med Surg Exam 1
Total Questions : 41
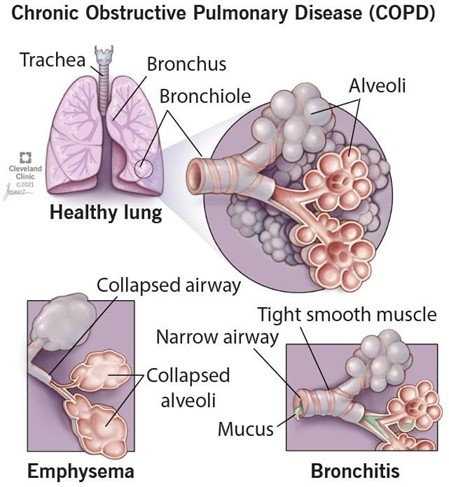
Showing 10 questions Sign up for moreA nurse is developing a plan of care for a client who has COPD. The nurse should include which of the
following interventions in the plan?
Explanation
Pursed-lip breathing is a technique that helps clients with COPD to exhale more effectively and prevent air trapping in the lungs. It also reduces dyspnea and improves oxygenation.
a) A low protein diet is not recommended for clients with COPD, as they need adequate protein intake to maintain muscle mass and prevent malnutrition.
c) Fluid restriction is not necessary for clients with COPD, unless they have signs of fluid overload or heart failure. Adequate hydration helps to thin secretions and facilitate expectoration.
d) Early-morning hours are not the best time for exercise and activity for clients with COPD, as they may experience more shortness of breath and fatigue due to diurnal variations in lung function. A better time would be mid-morning or afternoon, after taking bronchodilators and clearing secretions.
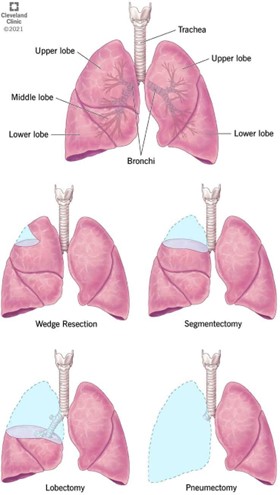
A nurse is assessing a client who is to undergo a left lobectomy to treat lung cancer. The client tells the nurse that she is scared and wishes she had never smoked. Which of the following responses should the nurse make?
Explanation
This response is empathetic and therapeutic, as it acknowledges the client's feelings and invites her to express her concerns. It also shows respect and interest in the client's perspective.
a) This response is false reassurance and nontherapeutic, as it dismisses the client's feelings and implies
that the surgery will solve everything.
b) This response is self-disclosure and nontherapeutic, as it shifts the focus from the client to the nurse and
does not address the client's fears.
d) This response is minimizing and nontherapeutic, as it tells the client how to feel and does not acknowledge the client's regret or anxiety.
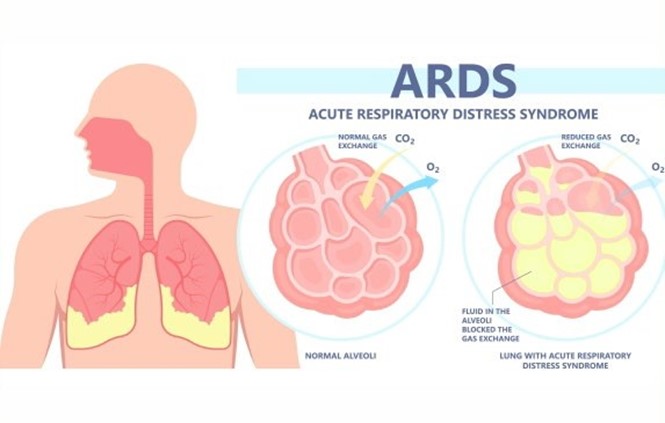
A nurse is planning care for a client who has acute respiratory distress syndrome (ARDS). Which of the following interventions should the nurse include in the plan?
Explanation
Placing the client in a prone position improves oxygenation and ventilation by reducing lung compression, increasing lung expansion, and redistributing blood flow to better match ventilation.
a) Administering low-flow oxygen via nasal cannula is not sufficient for a client with ARDS, who requires
high levels of oxygenation and positive pressure ventilation to prevent alveolar collapse and hypoxemia.
b) Offering high-protein and high-carbohydrate foods frequently is beneficial for a client with ARDS, as it provides adequate nutrition and energy to support lung healing and prevent muscle wasting. However, it is not the priority intervention for improving respiratory function.
d) Encouraging oral intake of at least 3,000 mL of fluids per day is contraindicated for a client with ARDS, who is at risk of fluid overload and pulmonary edema. Fluid intake should be restricted and diuretics should be administered as prescribed to reduce fluid accumulation in the lungs.
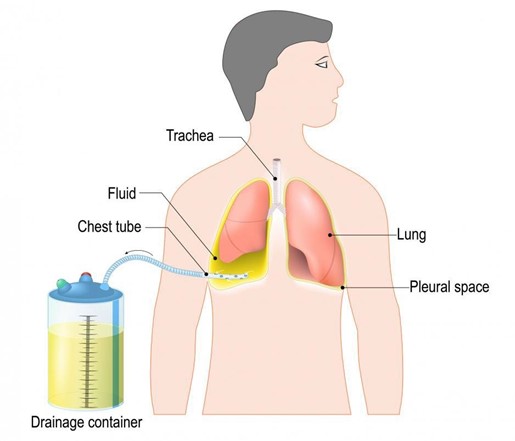
A nurse is caring for a client who has a chest tube connected to a closed drainage system and needs to be transported to the x-ray department. Which of the following actions should the nurse take?
Explanation
Keeping the drainage system below the level of the client's chest prevents backflow of fluid or air into the
pleural space and maintains negative pressure in the system.
a) Disconnecting the chest tube from the drainage system during transport is dangerous and can cause pneumothorax, infection, or bleeding. The chest tube should remain connected to the drainage system at all times unless ordered by the provider.
b) Emptying the collection chamber prior to transport is unnecessary and can interfere with accurate measurement of drainage. The collection chamber should be emptied only when it is full or at the end of each shift.
c) Clamping the chest tube prior to transferring the client to a wheelchair is contraindicated and can cause tension pneumothorax, as it prevents air from escaping the pleural space. The chest tube should only be clamped for a brief period when changing the drainage system or checking for air leaks, and only with a provider's order.
A nurse is providing dietary teaching for a client who has chronic obstructive pulmonary disease. Which of the following instructions should the nurse include?
Explanation
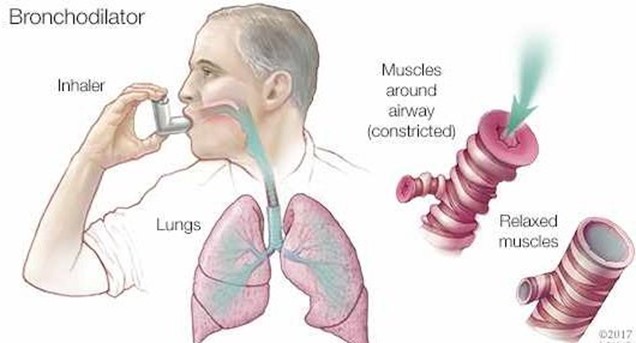
Using a bronchodilator 1 hour before eating can help reduce dyspnea and improve appetite for a client who has COPD. It can also facilitate oxygen delivery to the tissues and prevent hypoxia.
b) Eating 3 large meals each day is not recommended for a client who has COPD, as it can cause abdominal distension and increase pressure on the diaphragm, leading to dyspnea and fatigue. A better option is to eat 5 to 6 small meals throughout the day.
c) Limiting water intake with meals is not advisable for a client who has COPD, as it can cause dehydration and increase the viscosity of secretions, making them harder to expectorate. A better option is to drink at least 2 L of fluids per day, preferably between meals.
d) Reducing protein intake is not beneficial for a client who has COPD, as protein is essential for maintaining muscle mass and strength, especially of the respiratory muscles. A better option is to increase protein intake to at least 1.2 g/kg of body weight per day.
A nurse is caring for a client who has a chest tube connected to a closed drainage system and needs to be transported to the x-ray department. Which of the following actions should the nurse take?
Explanation
Keeping the drainage system below the level of the client's chest prevents backflow of fluid or air into the pleural space and maintains negative pressure in the system.
a) Disconnecting the chest tube from the drainage system during transport is dangerous and can cause pneumothorax, infection, or bleeding. The chest tube should remain connected to the drainage system at all times unless ordered by the provider.
b) Emptying the collection chamber prior to transport is unnecessary and can interfere with accurate measurement of drainage. The collection chamber should be emptied only when it is full or at the end of each shift.
c) Clamping the chest tube prior to transferring the client to a wheelchair is contraindicated and can cause tension pneumothorax, as it prevents air from escaping the pleural space. The chest tube should only be clamped for a brief period when changing the drainage system or checking for air leaks, and only with a provider's order.
A nurse on a medical-surgical unit is performing an admission assessment of a client who has COPD with emphysema. The client reports that he has a frequent productive cough and is short of breath. The nurse should anticipate which of the following assessment findings for this client?
Explanation
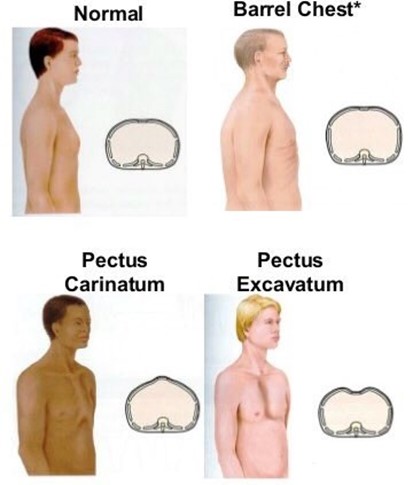
Increased anteroposterior diameter of the chest, also known as barrel chest, is a common finding in clients who have COPD with emphysema. It is caused by chronic air trapping and hyperinflation of the lungs, which results in fattening of the diaphragm and widening of the rib cage.
a) Oxygen saturation level 96% is within the normal range of 95% to 100% and does not indicate hypoxemia or impaired gas exchange. Clients who have COPD with emphysema typically have lower oxygen saturation levels, ranging from 88% to 92%.
b) Respiratory alkalosis is a condition in which the blood pH is elevated due to decreased carbon dioxide levels. It is caused by hyperventilation, which can occur in response to hypoxia, anxiety, or pain. Clients who have COPD with emphysema usually have respiratory acidosis, which is a condition in which the blood pH is lowered due to increased carbon dioxide levels. It is caused by hypoventilation, which results from impaired lung function and airway obstruction.
d) Petechiae on chest are small red or purple spots on the skin caused by bleeding from capillaries. They are not a typical finding in clients who have COPD with emphysema, unless they have severe coughing episodes or coagulation disorders. They can indicate infection, inflammation, trauma, or vascular disease.
A nurse is caring for a client who has asthma and is taking fluticasone. The nurse should monitor the client
for which of the following adverse effects?
Explanation
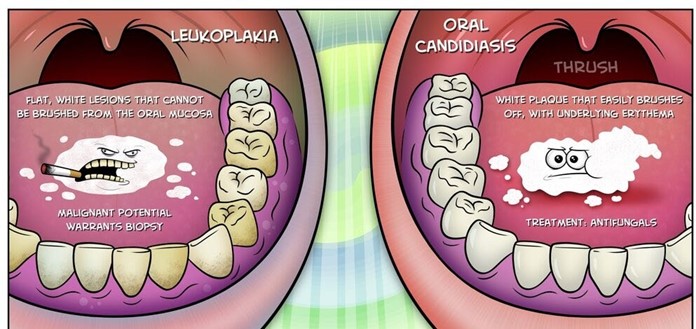
Oral candidiasis, also known as thrush, is a fungal infection of the mouth caused by Candida albicans. It is a common adverse effect of inhaled corticosteroids, such as fluticasone, which can suppress the normal flora of the oral cavity and create a favorable environment for fungal growth. It manifests as white patches or plaques on the tongue, palate, or cheeks that can be scraped off.
a) Polyuria, or excessive urination, is not an adverse effect of fluticasone. It can be caused by diabetes mellitus, diabetes insipidus, diuretics, or kidney disease.
b) Hypoglycemia, or low blood glucose level, is not an adverse effect of fluticasone. It can be caused by
insulin overdose, oral hypoglycemic agents, alcohol intake, or prolonged fasting.
c) Hypertension, or high blood pressure, is not an adverse effect of fluticasone. It can be caused by stress, obesity, smoking, salt intake, or kidney disease.
A nurse is caring for a client who has just developed a pulmonary embolism. Which of the following medications should the nurse anticipate administering?
Explanation
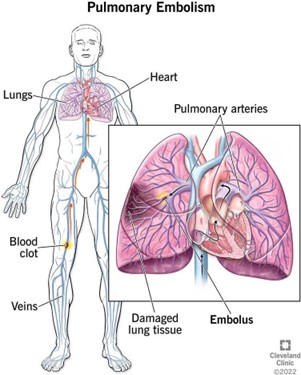
Heparin is an anticoagulant that prevents the formation of new clots and the extension of existing clots. It is the drug of choice for treating acute pulmonary embolism, which is a life-threatening condition caused by a blood clot that travels to the lungs and blocks a pulmonary artery.
a) Dexamethasone is a corticosteroid that reduces inflammation and suppresses immune response. It is not indicated for treating pulmonary embolism, but it may be used for other pulmonary conditions, such as asthma or COPD.
b) Atropine is an anticholinergic that blocks the action of acetylcholine and increases heart rate and cardiac output. It is not indicated for treating pulmonary embolism, but it may be used for bradycardia or asystole.
d) Furosemide is a loop diuretic that increases urine output and reduces fluid volume and blood pressure. It is not indicated for treating pulmonary embolism, but it may be used for heart failure or edema.
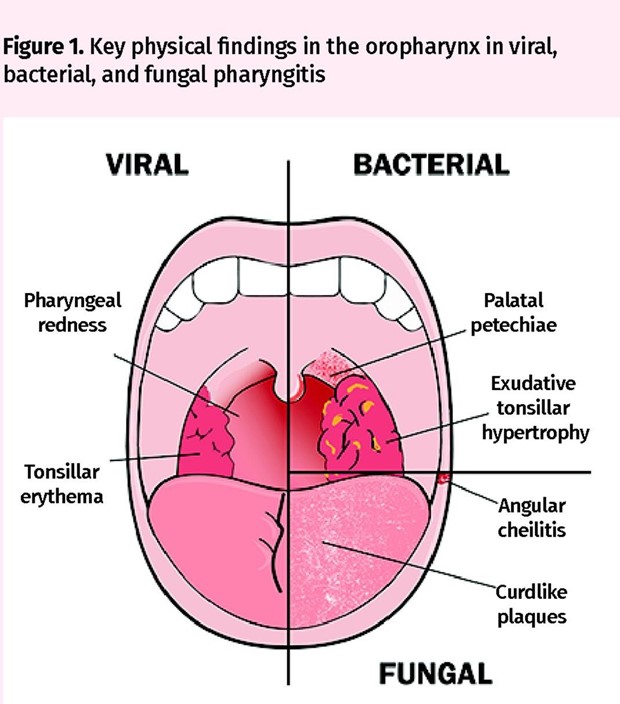
A nurse is providing teaching to the parents of a child who has streptococcal pharyngitis about ways to prevent disease transmission. Which of the following responses by the parents indicates an understanding of the teaching?
Explanation
Discarding the toothbrush and buying another is a way to prevent disease transmission, as the toothbrush can harbor bacteria and reinfect the child or spread the infection to others. The toothbrush should be discarded after 24 hours of antibiotic therapy.
a) Encouraging the child to drink lots of fluids is a way to promote hydration and soothe the throat, but it does not prevent disease transmission. The child should avoid sharing cups or utensils with others and use disposable tissues or paper towels.
b) Taking the child's temperature every 4 hours is a way to monitor fever, but it does not prevent disease transmission. The thermometer should be cleaned and disinfected after each use and not shared with others.
d) Giving the child Tylenol for the pain is a way to relieve discomfort, but it does not prevent disease transmission. The medication should be administered according to the label instructions and not shared with others.
You just viewed 10 questions out of the 41 questions on the ATI Med Surg Exam 1 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



