A nurse is providing dietary teaching for a client who has chronic obstructive pulmonary disease. Which of the following instructions should the nurse include?
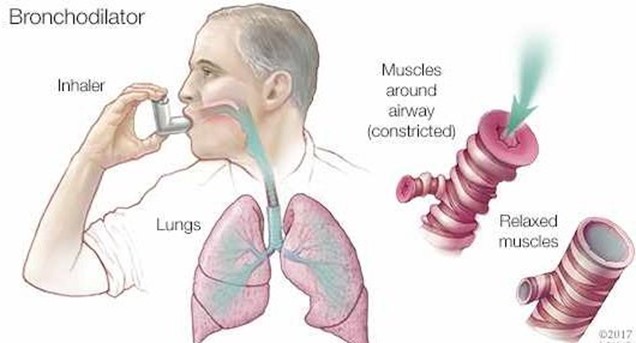
"Use a bronchodilator 1 hour before eating."
"Eat 3 large meals each day."
"Limit water intake with meals."
"Reduce protein intake."
None
None
The Correct Answer is A
Using a bronchodilator 1 hour before eating can help reduce dyspnea and improve appetite for a client who has COPD. It can also facilitate oxygen delivery to the tissues and prevent hypoxia.
b) Eating 3 large meals each day is not recommended for a client who has COPD, as it can cause abdominal distension and increase pressure on the diaphragm, leading to dyspnea and fatigue. A better option is to eat 5 to 6 small meals throughout the day.
c) Limiting water intake with meals is not advisable for a client who has COPD, as it can cause dehydration and increase the viscosity of secretions, making them harder to expectorate. A better option is to drink at least 2 L of fluids per day, preferably between meals.
d) Reducing protein intake is not beneficial for a client who has COPD, as protein is essential for maintaining muscle mass and strength, especially of the respiratory muscles. A better option is to increase protein intake to at least 1.2 g/kg of body weight per day.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Montelukast is an oral leukotriene receptor antagonist that prevents inflammation and bronchoconstriction in asthma. It is taken once daily in the evening to prevent nocturnal symptoms and improve morning lung function.
- "I rinse my mouth after taking this medication." This is not necessary, as montelukast is not associated with oral thrush or dysgeusia, unlike some inhaled corticosteroids.
- "I use a spacer device when I inhale this medication." This is not applicable, as montelukast is not an inhaler, but a tablet or chewable form.
- "I take this medication when I get an asthma attack." This is not appropriate, as montelukast is not a rescue medication, but a maintenance medication that should be taken regularly to prevent asthma exacerbations. A short-acting beta2 agonist such as albuterol should be used for acute relief of symptoms.
Correct Answer is D
Explanation
Answer: D. Cheyne-Stokes respirations
Rationale:
A) Stridor: Stridor is a high-pitched, wheezing sound resulting from disrupted airflow in the upper airway. It is not characterized by alternating periods of hyperventilation and apnea, making this choice incorrect.
B) Kussmaul respirations: Kussmaul respirations are deep, labored breaths typically associated with metabolic acidosis, such as diabetic ketoacidosis. These respirations do not exhibit alternating periods of hyperventilation and apnea, so this option is not applicable.
C) Apneustic respirations: Apneustic respirations are characterized by prolonged inhalation followed by a prolonged pause before exhalation. This pattern does not align with the alternating hyperventilation and apnea described, making it an incorrect choice.
D) Cheyne-Stokes respirations: Cheyne-Stokes respirations are characterized by a cyclical pattern of increasing depth and rate of breathing followed by a gradual decrease in depth and a period of apnea. This description matches the client's breathing pattern of alternating hyperventilation and apnea, making this the correct answer.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
