A nurse is caring for a client who has emphysema. Which of the following findings should the nurse expect to assess in this client? (Select all that apply.)
Dyspnea
Barrel chest
Deep respirations
Clubbing of the fingers
Bradycardia
Correct Answer : A,B,D
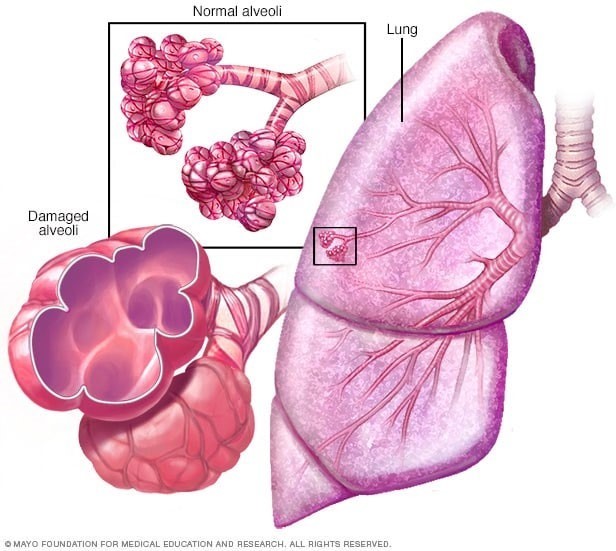
These findings are expected to be assessed in a client who has emphysema, which is a type of chronic obstructive pulmonary disease (COPD) characterized by destruction and enlargement of alveoli, loss of elastic recoil, and air trapping. These changes impair gas exchange and oxygenation, leading to chronic hypoxia and hypercapnia.
a) Dyspnea, or difficulty breathing, is a common symptom of emphysema, as the client has reduced lung capacity and increased work of breathing. Dyspnea may be worse with exertion, stress, or infection, and may cause anxiety and fatigue. The nurse should monitor the client's respiratory rate, rhythm, depth, and effort, and provide oxygen therapy as prescribed.
b) Barrel chest, or increased anteroposterior diameter of the chest, is a physical sign of emphysema, as the client has chronic air trapping and hyperinflation of the lungs. Barrel chest may also cause kyphosis, or curvature of the spine, and reduced chest wall movement. The nurse should measure the client's chest circumference and observe for any deformities or asymmetry.
d) Clubbing of the fingers, or enlargement and rounding of the nail beds, is a late sign of emphysema, as the client has chronic hypoxia and tissue ischemia. Clubbing may also affect the toes and ears, and may indicate pulmonary or cardiac disease. The nurse should inspect the client's nails for shape, color, angle, and capillary refill.
c) Deep respirations are not expected to be assessed in a client who has emphysema, as the client has shallow and rapid breathing due to air trapping and reduced lung compliance. Deep respirations may indicate other conditions, such as metabolic acidosis or anxiety. The nurse should assess the client's arterial blood gas levels and provide reassurance and relaxation techniques as needed.
e) Bradycardia, or slow heart rate, is not expected to be assessed in a client who has emphysema, as the client has tachycardia or normal heart rate due to hypoxia and increased sympathetic stimulation. Bradycardia may indicate other conditions, such as medication side effects, vagal stimulation, or heart block. The nurse should monitor the client's pulse rate, rhythm, quality, and electrocardiogram as indicated.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
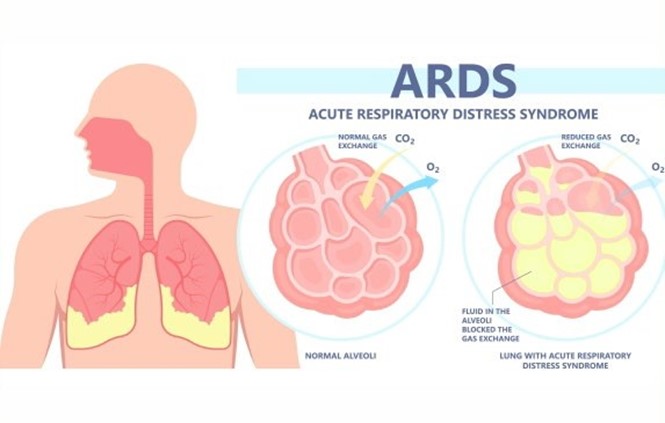
Placing the client in a prone position improves oxygenation and ventilation by reducing lung compression, increasing lung expansion, and redistributing blood flow to better match ventilation.
a) Administering low-flow oxygen via nasal cannula is not sufficient for a client with ARDS, who requires
high levels of oxygenation and positive pressure ventilation to prevent alveolar collapse and hypoxemia.
b) Offering high-protein and high-carbohydrate foods frequently is beneficial for a client with ARDS, as it provides adequate nutrition and energy to support lung healing and prevent muscle wasting. However, it is not the priority intervention for improving respiratory function.
d) Encouraging oral intake of at least 3,000 mL of fluids per day is contraindicated for a client with ARDS, who is at risk of fluid overload and pulmonary edema. Fluid intake should be restricted and diuretics should be administered as prescribed to reduce fluid accumulation in the lungs.
Correct Answer is ["B","C","E"]
Explanation
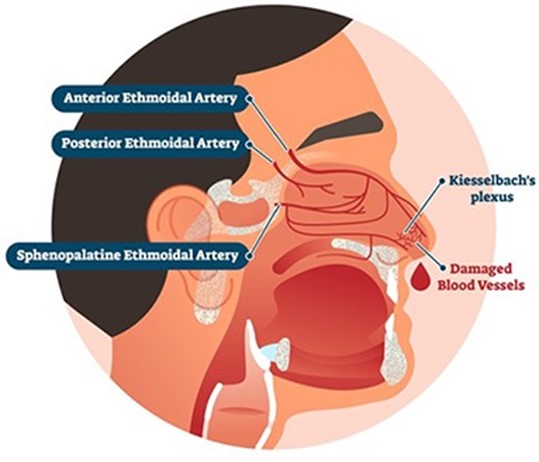
These actions help to control bleeding, reduce blood pressure, and promote clotting.
a. Tilt the client's head backward. This is not recommended, as it can cause blood to drain into the throat and increase the risk of aspiration, nausea, or vomiting.
d. Instruct the client to blow his nose. This is not advisable, as it can dislodge any clots that have formed and worsen bleeding.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
