A nurse is assessing a client who has postoperative atelectasis and is hypoxic. Which of the following manifestations should the nurse expect?
Lethargy
Bradycardia
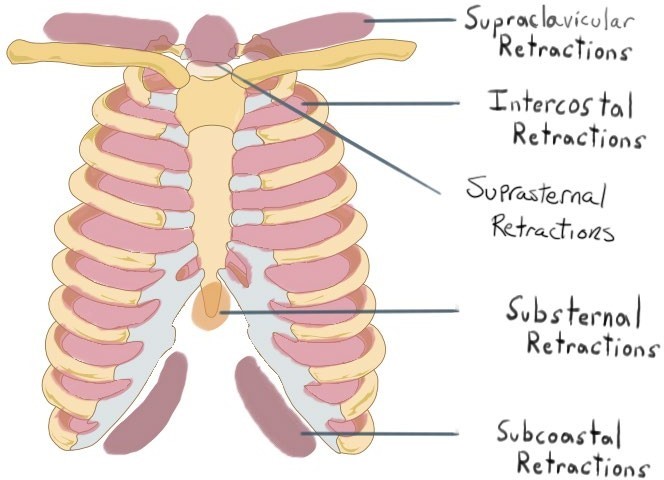
Intercostal retractions
Bradypnea
The Correct Answer is C
Intercostal retractions, or the inward movement of the chest wall between the ribs, are a sign of respiratory distress and hypoxia. They indicate increased work of breathing and reduced lung expansion, which are common in clients who have postoperative atelectasis. Atelectasis is a collapse of alveoli in a part of the lung, which impairs gas exchange and oxygenation.
a) Lethargy, or a state of reduced mental alertness and energy, is not a typical manifestation of hypoxia. It can be caused by other factors, such as pain, medication, infection, or electrolyte imbalance. Hypoxia usually causes restlessness, anxiety, or confusion.
b) Bradycardia, or a slow heart rate, is not a typical manifestation of hypoxia. It can be caused by other factors, such as medication, vagal stimulation, or heart block. Hypoxia usually causes tachycardia, or a fast heart rate, as the body tries to compensate for the low oxygen level.
d) Bradypnea, or a slow respiratory rate, is not a typical manifestation of hypoxia. It can be caused by other factors, such as medication, brain injury, or metabolic alkalosis. Hypoxia usually causes tachypnea, or a fast respiratory rate, as the body tries to increase oxygen intake and carbon dioxide elimination.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
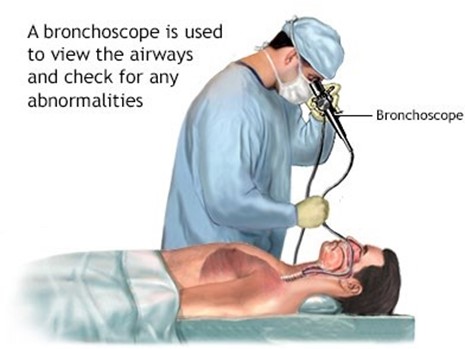
Hyperextended position, or backward bending of the neck, is the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position allows the provider to insert the scope through the mouth and into the trachea and bronchi, while avoiding injury to the teeth, tongue, or larynx. It also facilitates visualization of the airways and removal of foreign bodies or secretions.
b) Neutral position, or alignment of the head and neck with the spine, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may interfere with the insertion of the scope and cause damage to the oral structures or airways.
c) Extended position, or forward bending of the neck, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may obstruct the airway and make it difficult for the provider to insert the scope and access the bronchi.
d) Flexed position, or downward bending of the neck, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may compress the airway and prevent adequate ventilation and oxygenation of the client.
Correct Answer is ["A","C","E"]
Explanation
These clients have impaired swallowing, gag reflex, or level of consciousness, which increase their risk of aspiration while eating.
The other options are not correct because:
b. A client who has had prolonged diarrhea does not have a direct risk factor for aspiration, as diarrhea affects the lower gastrointestinal tract and not the upper airway or esophagus.
d. A client who has lactose intolerance does not have a risk factor for aspiration, as lactose intolerance causes abdominal cramps, bloating, gas, or diarrhea when consuming dairy products, but does not affect the ability to swallow or protect the airway.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
