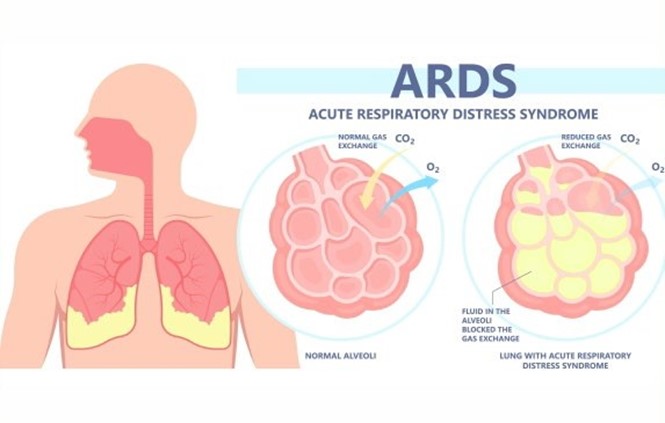
A nurse is planning care for a client who has acute respiratory distress syndrome (ARDS). Which of the following interventions should the nurse include in the plan?
Administer low-flow oxygen continuously via nasal cannula.
Offer high-protein and high-carbohydrate foods frequently.
Place in a prone position.
Encourage oral intake of at least 3,000 mL of fluids per day.
The Correct Answer is C
Placing the client in a prone position improves oxygenation and ventilation by reducing lung compression, increasing lung expansion, and redistributing blood flow to better match ventilation.
a) Administering low-flow oxygen via nasal cannula is not sufficient for a client with ARDS, who requires
high levels of oxygenation and positive pressure ventilation to prevent alveolar collapse and hypoxemia.
b) Offering high-protein and high-carbohydrate foods frequently is beneficial for a client with ARDS, as it provides adequate nutrition and energy to support lung healing and prevent muscle wasting. However, it is not the priority intervention for improving respiratory function.
d) Encouraging oral intake of at least 3,000 mL of fluids per day is contraindicated for a client with ARDS, who is at risk of fluid overload and pulmonary edema. Fluid intake should be restricted and diuretics should be administered as prescribed to reduce fluid accumulation in the lungs.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A humidifier bottle adds moisture to the oxygen, which prevents drying and irritation of the nasal mucosa
and enhances gas exchange.
a. Remove the nasal cannula while the client eats. This is not advisable, as the client may become hypoxic during eating, especially if they have pneumonia and impaired lung function. The nurse should monitor the client's oxygen saturation and respiratory status during meals and adjust the oxygen delivery device as needed.
c. Secure the oxygen tubing to the bed sheet near the client's head. This is not safe, as it can cause entanglement, dislodgement, or kinking of the tubing, which can compromise oxygen delivery and cause injury to the client.
d. Apply petroleum jelly to the nares as needed to soothe mucous membranes. This is not recommended, as petroleum products can ignite in the presence of oxygen and cause burns or fire. A water-based lubricant should be used instead.

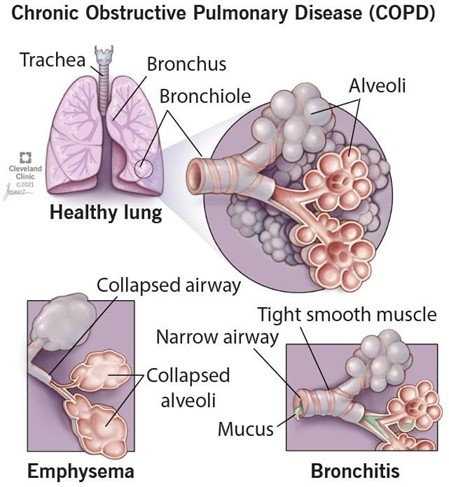
Correct Answer is B
Explanation
Pursed-lip breathing is a technique that helps clients with COPD to exhale more effectively and prevent air trapping in the lungs. It also reduces dyspnea and improves oxygenation.
a) A low protein diet is not recommended for clients with COPD, as they need adequate protein intake to maintain muscle mass and prevent malnutrition.
c) Fluid restriction is not necessary for clients with COPD, unless they have signs of fluid overload or heart failure. Adequate hydration helps to thin secretions and facilitate expectoration.
d) Early-morning hours are not the best time for exercise and activity for clients with COPD, as they may experience more shortness of breath and fatigue due to diurnal variations in lung function. A better time would be mid-morning or afternoon, after taking bronchodilators and clearing secretions.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
