A nurse on a medical-surgical unit is performing an admission assessment of a client who has COPD with emphysema. The client reports that he has a frequent productive cough and is short of breath. The nurse should anticipate which of the following assessment findings for this client?
Oxygen saturation level 96%
Respiratory alkalosis
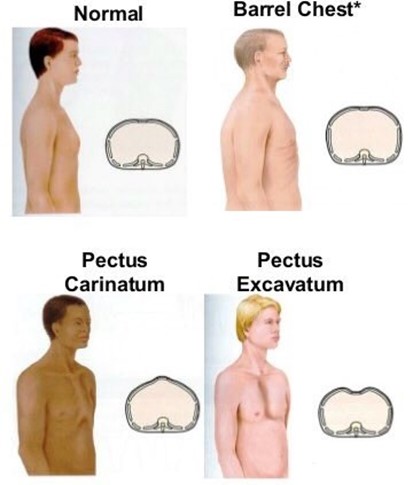
Increased anteroposterior diameter of the chest
Petechiae on chest
The Correct Answer is C
Increased anteroposterior diameter of the chest, also known as barrel chest, is a common finding in clients who have COPD with emphysema. It is caused by chronic air trapping and hyperinflation of the lungs, which results in fattening of the diaphragm and widening of the rib cage.
a) Oxygen saturation level 96% is within the normal range of 95% to 100% and does not indicate hypoxemia or impaired gas exchange. Clients who have COPD with emphysema typically have lower oxygen saturation levels, ranging from 88% to 92%.
b) Respiratory alkalosis is a condition in which the blood pH is elevated due to decreased carbon dioxide levels. It is caused by hyperventilation, which can occur in response to hypoxia, anxiety, or pain. Clients who have COPD with emphysema usually have respiratory acidosis, which is a condition in which the blood pH is lowered due to increased carbon dioxide levels. It is caused by hypoventilation, which results from impaired lung function and airway obstruction.
d) Petechiae on chest are small red or purple spots on the skin caused by bleeding from capillaries. They are not a typical finding in clients who have COPD with emphysema, unless they have severe coughing episodes or coagulation disorders. They can indicate infection, inflammation, trauma, or vascular disease.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
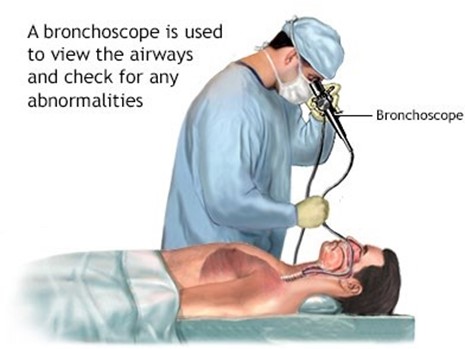
Hyperextended position, or backward bending of the neck, is the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position allows the provider to insert the scope through the mouth and into the trachea and bronchi, while avoiding injury to the teeth, tongue, or larynx. It also facilitates visualization of the airways and removal of foreign bodies or secretions.
b) Neutral position, or alignment of the head and neck with the spine, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may interfere with the insertion of the scope and cause damage to the oral structures or airways.
c) Extended position, or forward bending of the neck, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may obstruct the airway and make it difficult for the provider to insert the scope and access the bronchi.
d) Flexed position, or downward bending of the neck, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may compress the airway and prevent adequate ventilation and oxygenation of the client.
Correct Answer is A
Explanation
Answer: A
Rationale:
A) Administering a nebulized beta-adrenergic:
In the case of an acute asthma exacerbation, administering a nebulized beta-adrenergic agonist (such as albuterol) is the highest priority. These medications act quickly to relax bronchial smooth muscle, dilate airways, and improve airflow. This intervention directly addresses the underlying bronchospasm and helps to alleviate the acute symptoms of asthma.
B) Providing immediate rest for the client:
While rest is important in managing an acute asthma exacerbation, it is not the immediate priority. Addressing the airway obstruction with appropriate medications is crucial for stabilizing the client's condition before focusing on comfort measures such as rest.
C) Positioning the client in high-Fowler's:
Positioning the client in a high-Fowler's position can help improve lung expansion and facilitate breathing. However, this action is secondary to administering medication that can relieve the acute symptoms of bronchoconstriction. The medication should be administered first to rapidly address the exacerbation.
D) Initiating oxygen therapy:
Oxygen therapy might be necessary if the client shows signs of hypoxemia or severe respiratory distress. However, the immediate priority is to address the bronchospasm with a nebulized beta-adrenergic agonist to improve airflow. Once the acute bronchospasm is managed, oxygen therapy can be implemented if needed to support oxygen saturation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
