A nurse is providing discharge teaching to a client who has asthma and a new prescription for fluticasone/salmeterol. For which of the following adverse effects should the nurse instruct the client to report to the provider?
Dry oral mucous membranes
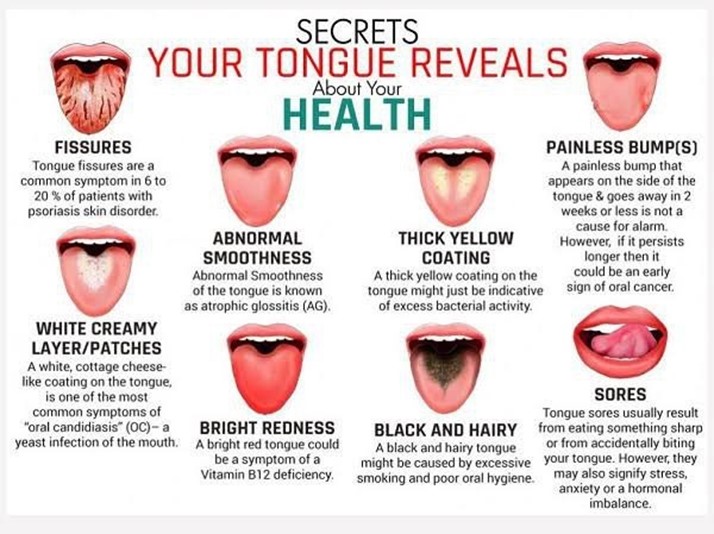
White coating in the mouth
Sedation
Increased appetite
The Correct Answer is B
White coating in the mouth, also known as oral candidiasis or thrush, is a serious adverse effect of fluticasone/salmeterol, which is a combination of an inhaled corticosteroid and a long-acting beta2 agonist. It is caused by fungal infection of the oral cavity due to suppression of the normal flora by the corticosteroid component. The client should report this symptom to the provider, as it may require antifungal treatment and discontinuation of the medication.
a) Dry oral mucous membranes is a common and mild adverse effect of fluticasone/salmeterol, which can be relieved by drinking water, chewing sugarless gum, or using artificial saliva. It does not require reporting to the provider or stopping the medication.
c) Sedation is not an adverse effect of fluticasone/salmeterol, but it may be caused by other medications, such as antihistamines, opioids, or benzodiazepines. The client should avoid driving or operating machinery if sedated and consult with the provider about possible drug interactions.
d) Increased appetite is not an adverse effect of fluticasone/salmeterol, but it may be caused by other factors, such as stress, boredom, or hormonal changes. The client should maintain a balanced diet and exercise regularly to prevent weight gain and promote health.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Increasing fluid intake helps to hydrate the mucous membranes and thin the respiratory secretions, which facilitates expectoration and improves gas exchange.
- Encourage coughing and deep breathing. This is beneficial for clearing the airways and preventing atelectasis, but it does not directly affect the viscosity of the secretions.
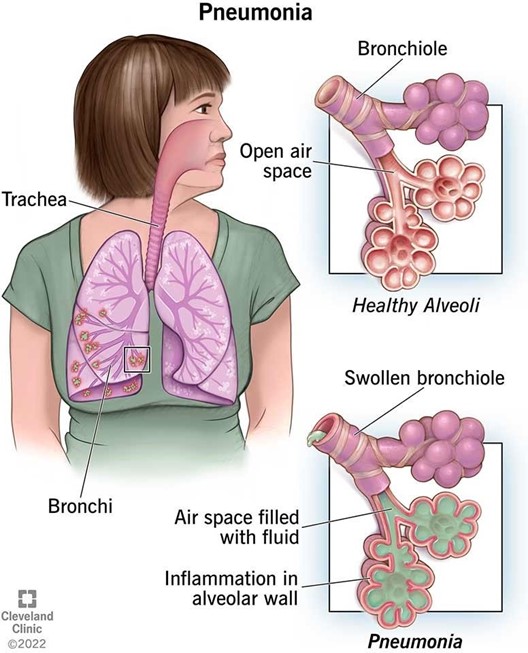
- Encourage regular use of the incentive spirometer. This is helpful for expanding the lungs and preventing complications such as pneumonia or pleural effusion, but it does not influence the consistency of the secretions.
- Encourage the client to ambulate frequently. This is important for promoting circulation and mobility, but it does not have a significant effect on the thinning of the secretions.
Correct Answer is B
Explanation
Answer: B
Rationale:
A) "Expect your sputum cultures to be negative after 6 months of therapy":
While sputum cultures may become negative after a period of effective therapy, it is not always guaranteed to happen within exactly 6 months. Tuberculosis (TB) treatment usually involves several months of medication, and sputum cultures are monitored periodically to assess treatment efficacy, not solely at the 6-month mark.
B) "Drink at least 8 ounces of water when you take the pyrazinamide tablet":
Drinking plenty of water with pyrazinamide is important to prevent dehydration and to help minimize potential side effects, such as hyperuricemia or gout. Adequate hydration can also aid in the effective elimination of the medication from the body, thus reducing the risk of adverse effects.
C) "Provide a sputum specimen every 2 weeks to the clinic for testing":
Sputum specimens are typically provided less frequently than every 2 weeks, usually monthly, to monitor the progress of TB treatment. Testing frequency may vary depending on the client's condition and the healthcare provider's recommendations.
D) "Take isoniazid with an antacid":
Isoniazid should not be taken with antacids, as antacids can interfere with the absorption of isoniazid. It is usually advised to take isoniazid on an empty stomach, and clients should be instructed to wait at least 1 hour after taking isoniazid before consuming antacids.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
