Wgu Hesi RN Foundation of Nursing
Wgu Hesi RN Foundation of Nursing
Total Questions : 51
Showing 10 questions Sign up for moreA client tells the nurse about starting an aerobic workout program to lose weight and help with insomnia. The client states that it still takes over an hour to fall asleep at night. Which action should the nurse implement?
Explanation
D. The most appropriate action for the nurse to take is to gather more information about the client's exercise schedule. This will help the nurse assess whether the client's exercise regimen may be contributing to or exacerbating the insomnia. Understanding the timing, intensity, and duration of the client's aerobic workouts can provide insights into potential factors affecting sleep patterns.
A. Advising the client that lifestyle changes often take several weeks to be effective is a valid point. However, it does not directly address the potential impact of exercise timing on sleep.
B. Determining the amount of weight the client has lost since increasing activity may provide useful information about the client's progress with weight loss but does not directly address the issue of difficulty falling asleep.
C. Encouraging the client to exercise every day to eliminate bedtime wakefulness is not necessarily appropriate, as excessive or late-night exercise may exacerbate rather than alleviate bedtime wakefulness in some individuals.
A client is admitted with reports of shortness of breath, dyspnea on exertion, and chest pressure. The healthcare provider prescribes a medication that is unfamiliar to the nurse. When checking the drug handbook, the nurse reads that the prescribed amount is an unusually large dose. Which action should the nurse take?
Explanation
D. When encountering a medication dosage that appears unusually large or different from what is expected, the nurse should always verify the prescription with the healthcare provider before administering the medication. This step ensures patient safety and helps prevent medication errors.
A. Giving the dosage recommended in the drug handbook may not be appropriate if the prescribed dosage differs significantly from the usual or recommended dosage due to patient- specific factors or other considerations.
B. In situations where the prescribed dosage seems unusually large or different from the usual guidelines, it is essential to confirm with the healthcare provider who wrote the prescription to ensure accuracy and appropriateness for the specific patient.
C. Administering the medication as prescribed without further clarification could potentially lead to harm if the prescribed dosage is incorrect or inappropriate for the patient's condition.
When providing health teaching to older adult clients, which action is most important for the nurse to implement?
Explanation
C. When providing health teaching to older adult clients, using everyday language is crucial. Older adults may have varying levels of health literacy and cognitive abilities, so using simple, clear language facilitates better understanding and comprehension of the information being provided.
A. Underlining key words on the written information may be helpful for emphasizing important points, but it is not as critical as using everyday language to enhance understanding
B. Speaking loudly and facing the client may not be necessary for all older adult clients and could even be perceived as patronizing or disrespectful.
D. Providing a very well-lit meeting space is important for optimizing visual acuity, especially for older adults who may have age-related changes in vision. However, while adequate lighting is beneficial, it is not as critical
The nurse notices a client grimacing while moving from the bed to a chair, but when asked about the pain the client denies having any pain. Which intervention should the nurse implement first?
Explanation
A. Administering pain medication solely based on nonverbal cues without further assessment and confirmation of pain may lead to unnecessary medication administration and potential adverse effects.
B.Monitoring the client's nonverbal behavior is crucial in this situation because it can provide valuable insight into the client's pain experience. However, this shoudl come after listening to the client first.
C. Directly asking the client about the grimacing is a very reasonable approach. Since the client denies pain but is exhibiting nonverbal signs of discomfort, the nurse could ask specific questions to explore whether there is another underlying cause.
D. Reviewing the pain medications prescribed is important to ensure that the client is receiving appropriate pain management, but it may not be the most immediate intervention in this scenario.
The nurse is inserting a urinary catheter that has been prescribed for the client. When the tip of the catheter reemerges from the insertion site, which action should the nurse take next?
Explanation
B. If the tip of the urinary catheter reemerges from the insertion site during insertion, it means that the catheter has become contaminated with microorganisms from the urethra or surrounding area. Continuing to insert the same catheter can introduce these microorganisms into the urinary tract, increasing the risk of urinary tract infection (UTI).
A. Increasing the lighting in the room allows for optimal visualization during the procedure, but it is not the priority action when the catheter has become contaminated.
C. Cleaning the catheter with providone-iodine is not sufficient to sterilize the catheter and eliminate the risk of introducing pathogens into the urinary tract.
D. Repositioning the legs before reinsertion does not address the contamination of the catheter and does not mitigate the risk of introducing pathogens into the urinary tract.
When assuming care of a client at 1900, the nurse learns in report that a client with a urinary tract infection had an indwelling urinary catheter removed during the previous shift. Which information is most important for the nurse to obtain?
Explanation
A. Delayed or inability to void after catheter removal could indicate urinary retention, which may require further intervention such as bladder scanning, straight catheterization, or reinsertion of a urinary catheter.
B. This is important for assessing the timing of antibiotic therapy but may not be directly related to the client's ability to void after catheter removal.
C. Color of the urine during catheter removal may provide information about the client's urinary status, but it does not confirm whether the client was able to void effectively after catheter removal.
D. Intake and output reports for the previous shift is relevant for assessing fluid balance and urinary output trends but does not specifically address the client's ability to void after catheter removal.
The nurse is caring for a client with a history of neuropathy who reports increasing numbness and tingling in the lower extremities. Which problem should the nurse determine is the priority for promoting foot care at this time?
Explanation
D. Neuropathy, especially when associated with numbness and tingling in the lower extremities, poses a significant risk for impaired skin integrity. The loss of sensation can lead to decreased awareness of pressure, friction, or trauma to the feet, making the client more susceptible to skin breakdown, ulcers, and injuries.
A. Increasing numbness and tingling in the lower extremities, which primarily suggests neuropathic symptoms rather than impaired mobility.
B. A self-care deficit may arise if the client's neuropathy significantly affects their ability to perform foot care tasks independently. However, self-care deficit becomes a priority concern.
C. Neuropathy can increase the risk of foot injuries due to decreased sensation, which in turn can lead to infections if not promptly addressed. However, while infection is a potential complication, the immediate concern in this scenario is preventing the development of skin breakdown and ulcers.
The nurse is demonstrating three-point gait crutch walking to an older adult client who broke a foot while playing soccer with the grandchildren. Which behavior indicates that the client understands proper crutch walking?
Explanation
B. In three-point gait crutch walking, the client should progress to foot touchdown and weight bearing of the affected leg. This means that the client is able to advance the crutches forward, followed by the affected leg, and then the unaffected leg. The weight should be borne primarily by the hands and arms on the crutches while the affected leg supports some weight as tolerated.
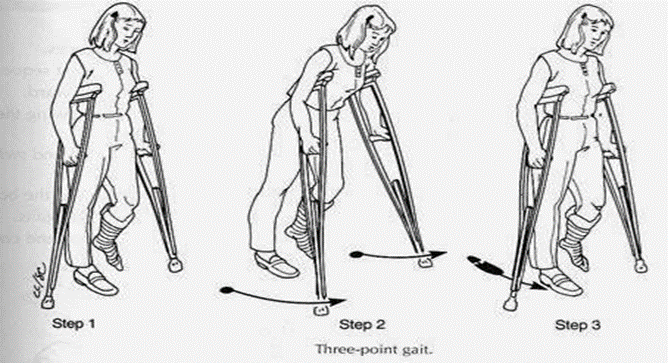
A. Bearing body weight on the palms of hands during the crutch gait describes the correct distribution of weight on the crutches, which is important for proper technique, but it does not specifically address the coordination of crutch and leg movements in three-point gait.
C. Practices bicep and triceps isometric exercises is not directly related to proper crutch walking technique but may be beneficial for strengthening the upper extremities, which are involved in using crutches.
D. Inspects crutches to ensure rubber tips are intact is important for safety but does not specifically indicate understanding of proper crutch walking technique.
An older adult female client tells the clinic nurse about frequently awakening during the night and not being able to go back to sleep. Which action(s) should the nurse suggest to the client to help improve sleep? Select all that apply.
Explanation
B. Caffeine can interfere with sleep, especially if consumed close to bedtime. Opt for decaffeinated options in the evening. Avoiding caffeinated beverages late in the day can help promote better sleep by reducing the stimulant effects of caffeine, which can interfere with falling asleep or staying asleep.
C. Establish a regular time for going to bed and getting up. Consistency helps regulate your
body’s internal clock. Try to maintain the same sleep schedule even on weekends.
A. Taking an afternoon nap to make up for missed sleep is not recommended, as napping during the day can disrupt nighttime sleep patterns and make it harder to fall asleep or stay asleep at night, especially for older adults.
D. Asking the healthcare provider for a mild sedative for bedtime may not be the first-line recommendation, as sedatives can have side effects and potential risks, especially for older adults. Non-pharmacological interventions are typically preferred for improving sleep quality.
E. Alcohol consumption before bedtime can disrupt sleep patterns and interfere with restorative sleep, particularly when combined with other substances like caffeine or sugar.
A client is in contact isolation due to a stage IV coccyx wound infected with methicillin resistant Staphylococcus aureus (MRSA). The nurse plans interventions to prevent multiple re-entries to the client's room. In which order should the nurse perform the interventions?
Explanation
Restarting the IV line first ensures that the client has immediate access to intravenous fluids and medications, which is critical for maintaining hydration and treatment continuity. This is especially important if the client is receiving antibiotics or other medications that need to be administered continuously or urgently.
Following the IV line, performing tracheostomy care ensures that the airway is maintained and free from obstructions. This is essential, especially in clients with compromised respiratory function. By addressing the airway next, the nurse ensures that the client can breathe effectively and is stable.
Changing the coccyx dressing is important for wound management, especially with an infected wound. Performing this last minimizes the risk of contaminating the sterile field or the dressing while the nurse is managing other tasks. This also reduces the number of times the nurse enters and exits the room, adhering to contact isolation protocols.
You just viewed 10 questions out of the 51 questions on the Wgu Hesi RN Foundation of Nursing Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



