Gastro Urinary Systems Medication Proctored Exam
Gastro Urinary Systems Medication Proctored Exam
Total Questions : 44
Showing 10 questions Sign up for moreA nurse is reinforcing teaching about cimetidine with a client who has peptic ulcer disease. Which of the following information should the nurse include in the teaching?
Explanation
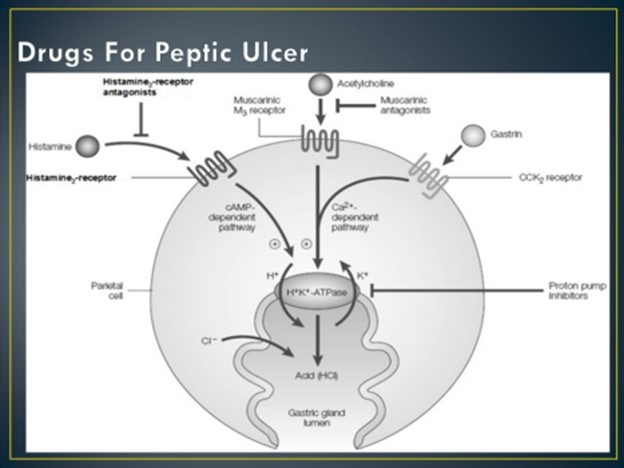
Cimetidine is a medication known as a histamine H2 receptor antagonist, commonly used in the treatment of peptic ulcer disease. It works by reducing the production of stomach acid. When teaching a client about cimetidine, it is important to inform them about the timing of taking other medications, specifically antacids.
Antacids, which are used to neutralize stomach acid, can interfere with the absorption of cimetidine if taken simultaneously. Therefore, it is generally recommended to wait at least 1 hour after taking cimetidine before taking an antacid. This allows sufficient time for the cimetidine to be absorbed and start working effectively before neutralizing stomach acid with an antacid.
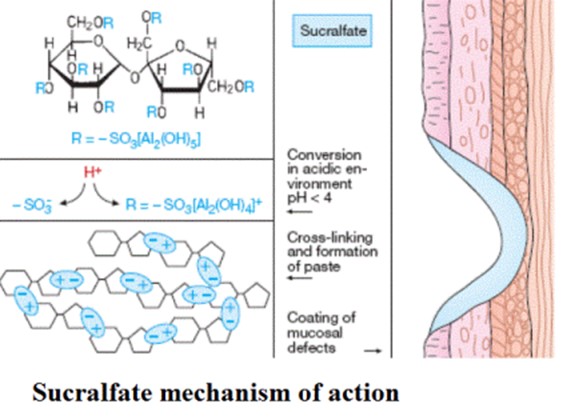
A nurse is reinforcing teaching a client who has peptic ulcer disease and is starting therapy with sucralfate. Which of the following instructions should the nurse include in the teaching?
Explanation
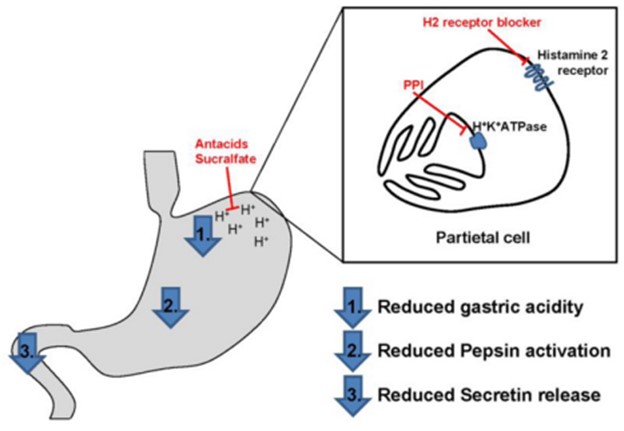
Sucralfate is a medication commonly used in the treatment of peptic ulcer disease. It works by forming a protective barrier over the ulcer site, providing a physical barrier against gastric acid, and promoting the healing process. When teaching a client about sucralfate, it is important to provide instructions regarding its proper administration.
One of the key instructions is to take sucralfate 1 hour before meals. This timing allows the medication to form a protective coating in the stomach before food is ingested. Taking sucralfate on an empty stomach enhances its effectiveness in protecting the ulcer and promoting healing.
"Take the medication with an antacid" - Sucralfate should not be taken with an antacid. Antacids can interfere with the protective mechanism of sucralfate by neutralizing stomach acid, which is necessary for sucralfate to bind and form a protective coating. It is recommended to wait at least 30 minutes to 1 hour after taking sucralfate before taking an antacid.
"Take as needed for pain relief" - Sucralfate is not typically used for immediate pain relief in peptic ulcer disease. It is primarily used for its protective and healing properties. Pain relief is
usually addressed with other medications, such as antacids, acid-reducing medications, or pain medications as prescribed by a healthcare provider.
"Store the medication in the refrigerator" - Sucralfate does not require refrigeration. It should be stored at room temperature, away from excessive heat or moisture, as per the specific instructions provided by the manufacturer or healthcare provider.
A nurse is collecting data from a client who has peptic ulcer disease. Which of the following findings is a manifestation of gastrointestinal perforation?
Explanation
The manifestation of gastrointestinal perforation includes severe upper abdominal pain. This can be a significant symptom indicating a potential perforation in the gastrointestinal tract. It is important to note that gastrointestinal perforation is a medical emergency that requires immediate attention and intervention.
Hyperactive bowel sounds: This finding is more commonly associated with conditions like bowel obstruction or gastroenteritis rather than gastrointestinal perforation.

Bradycardia: Bradycardia (slower than normal heart rate) is not a typical manifestation of gastrointestinal perforation. It may be associated with other conditions or factors.
Report of epigastric fullness: Epigastric fullness can be a symptom of various gastrointestinal conditions, including peptic ulcer disease itself. However, it is not a specific manifestation of gastrointestinal perforation.
A nurse is caring for a client who has cirrhosis and a prescription for lactulose. Following administration, the nurse should monitor the client for which of the following adverse effects?
Explanation
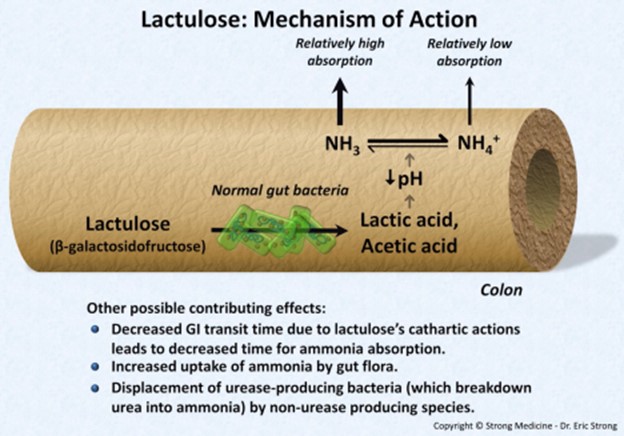
After administering lactulose to a client with cirrhosis, the nurse should monitor for the adverse effects of diarrhea. Lactulose is a laxative commonly used in the treatment of hepatic encephalopathy, which can occur in individuals with cirrhosis. One of the intended effects of lactulose is to promote bowel movements and reduce the absorption of ammonia in the gut, thus helping to manage hepatic encephalopathy.
While lactulose can cause adverse effects such as diarrhea, it is not typically associated with peripheral edema. Peripheral edema is often seen in cirrhosis due to fluid retention caused by liver dysfunction.
Dry mouth and headache are less commonly associated with lactulose use and are not typically the primary adverse effects to monitor for in this scenario.
A nurse is planning care for a client who has a peptic ulcer and a new prescription for sucralfate 2 gm administered twice daily. Which of the following times should the nurse plan to administer the medication?
Explanation
Sucralfate is a medication used to treat peptic ulcers by forming a protective coating on the stomach lining. It should be taken on an empty stomach, as food can interfere with its absorption and effectiveness. One hour before breakfast and the evening meal is the correct timing for administering sucralfate, allowing for an empty stomach before meals.
At the time the client takes a proton pump inhibitor: Proton pump inhibitors are a different class of medications used to reduce stomach acid production. It is recommended to administer sucralfate separately, as it works differently and has different administration requirements.
Thirty minutes after breakfast and the evening meal: Administering sucralfate after meals is not ideal, as it may not provide the desired therapeutic effect on an empty stomach.
The time the client takes an antacid: Antacids are also different from sucralfate, and they can interfere with its absorption. It is generally recommended to administer sucralfate separately from antacids.
A nurse is caring for a client who receives intermittent enteral feedings through an NG tube. Before administering a feeding, the nurse should measure the gastric residual for which of the following purposes?
Explanation
The nurse should measure the gastric residual before administering a feeding to identify delayed gastric emptying. Gastric residual refers to the volume of formula or contents remaining in the stomach from the previous feeding. Measuring gastric residual helps assess how well the client's stomach is emptying and can indicate if there is delayed gastric emptying.
By measuring gastric residual, the nurse can:
● Determine if the stomach has adequately emptied from the previous feeding. ● Assess the client's tolerance to enteral feedings.
● Detect signs of delayed gastric emptying, which can be indicative of gastrointestinal motility issues or other complications.
● Adjust the feeding rate or make other modifications to the enteral feeding plan based on the amount of residual volume.
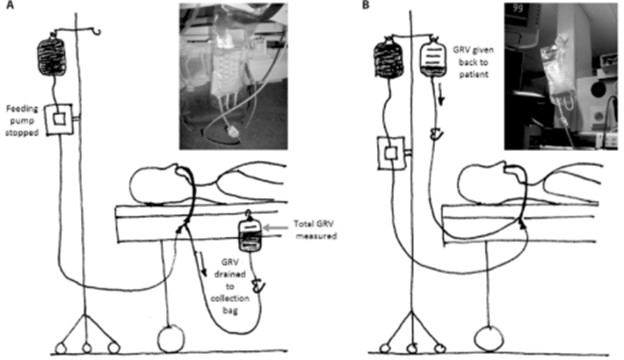
Confirming the placement of the NG tube is typically done using other methods, such as an X-ray, pH testing, or auscultation of air insufflation. Gastric residual measurement primarily serves the purpose of assessing gastric emptying, rather than confirming tube placement.
While electrolyte imbalances can be monitored in the overall care of a client receiving enteral feedings, measuring gastric residual specifically focuses on assessing gastric emptying and feeding tolerance, rather than determining the client's electrolyte balance.
Removing gastric acid that might cause dyspepsia is not the primary purpose of measuring gastric residual. Gastric residual measurement aims to evaluate the volume of the previous feeding and assess gastric emptying, rather than focusing on dyspepsia specifically.
A nurse is collecting data from a client in the health clinic who is reporting epigastric pain. Which of the following statements made by the client should the nurse identify as being consistent with peptic ulcer disease?
Explanation
A. "I feel so much better after eating."This is most consistent with a duodenal ulcer, where pain is relieved by food (but often returns 2–3 hours later). Gastric ulcers, on the other hand, may worsen with eating.
B. "The pain is worse after I eat a meal high in fat."Fatty food intolerance and postprandial pain are more characteristic of gallbladder disease (cholelithiasis/cholecystitis), not PUD.
C. "The pain radiates down to my lower back."Pain radiating to the back is more typical of pancreatitis, not PUD.
D. "My pain is relieved by having a bowel movement."Relief of abdominal pain with a bowel movement suggests irritable bowel syndrome (IBS), not PUD.
A nurse is reinforcing teaching with a client who reports taking bisacodyl daily. Which of the following information should the nurse include?
Explanation
Bisacodyl is a stimulant laxative commonly used to treat constipation. However, it is important to educate the client about the potential risks associated with chronic laxative use. The statement regarding electrolyte imbalance is important because excessive or prolonged use of laxatives can lead to electrolyte disturbances, such as low potassium levels (hypokalemia), which can have adverse effects on various body functions.
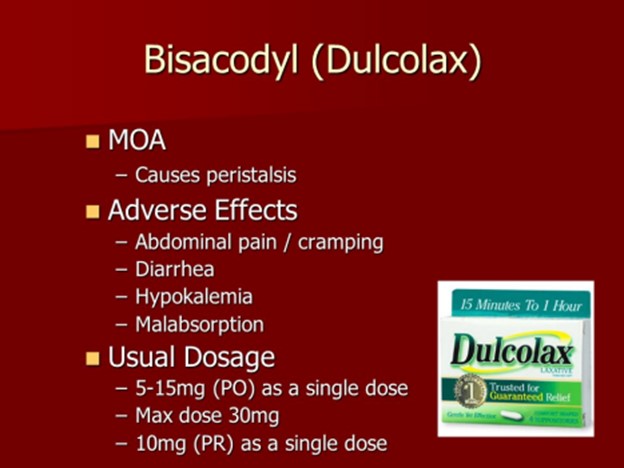
"Daily bowel movements are necessary for good intestinal health": While regular bowel movements are generally desirable, stating that daily bowel movements are necessary for good intestinal health is an overgeneralization. Bowel movement frequency can vary among individuals, and it is important to consider other factors such as diet, hydration, and overall health.
"Chronic use of laxatives can lead to a tear in the rectal mucosa": While chronic use of laxatives can lead to complications such as dependence and potential damage to the digestive system, specifically mentioning a tear in the rectal mucosa (rectal mucosal injury) is not the most commonly associated concern.
"Decrease your intake of high-fiber foods": It is generally recommended to increase fiber intake for individuals with constipation. Decreasing high-fiber foods would counteract the benefits of dietary fiber in promoting regular bowel movements and alleviating constipation.
A nurse is reinforcing teaching for a client who has a duodenal ulcer and a new prescription for sucralfate. The client asks the nurse how sucralfate works. Which of the following statements should the nurse make?
Explanation
Sucralfate works by forming a protective barrier or coating over the surface of the ulcer. It adheres to the ulcer site and provides a physical barrier that protects the ulcer from gastric acid, pepsin, and bile salts. This protective barrier allows the ulcer to heal by preventing further damage and irritation from the stomach acid.
A nurse is caring for a client who has gastroesophageal disease and a prescription for metoclopramide. For which of the following adverse effects should the monitor?
Explanation
Metoclopramide is a medication commonly used to treat gastrointestinal disorders such as gastroesophageal reflux disease (GERD). While it is generally well-tolerated, it can have some adverse effects. Sedation is one of the common side effects of metoclopramide. It can cause drowsiness, dizziness, and a feeling of tiredness in some individuals. Therefore, the nurse should monitor the client for any signs of sedation or excessive drowsiness, especially when the client starts taking the medication or when the dose is increased.
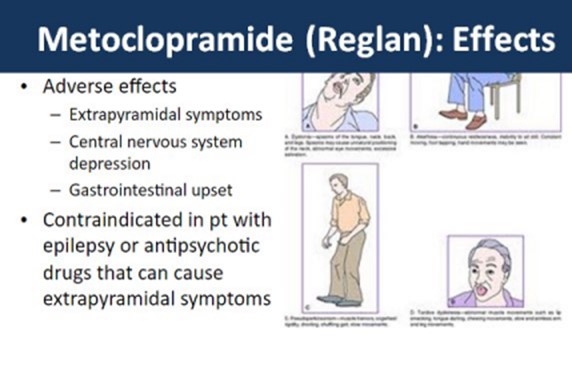
Hypertension: Metoclopramide is not known to cause hypertension (high blood pressure) as a common side effect. In fact, it may have a mild hypotensive (blood pressure-lowering) effect in some individuals.
Urinary retention: Metoclopramide does not typically cause urinary retention. Instead, it can enhance gastrointestinal motility and increase the frequency of bowel movements.
Blurred vision: While visual disturbances are rare adverse effects of metoclopramide, blurred vision is not a commonly reported side effect. However, other visual disturbances like oculogyric crisis (involuntary rolling back of the eyes) have been reported in rare cases. Nevertheless, monitoring for blurred vision specifically is not a priority when administering metoclopramide.
You just viewed 10 questions out of the 44 questions on the Gastro Urinary Systems Medication Proctored Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



