A nurse is reinforcing teaching a client who has peptic ulcer disease and is starting therapy with sucralfate. Which of the following instructions should the nurse include in the teaching?
Take the medication with an antacid
Take the medication 1 hr before meals
Take as needed for pain relief
Store the medication in the refrigerator
The Correct Answer is B
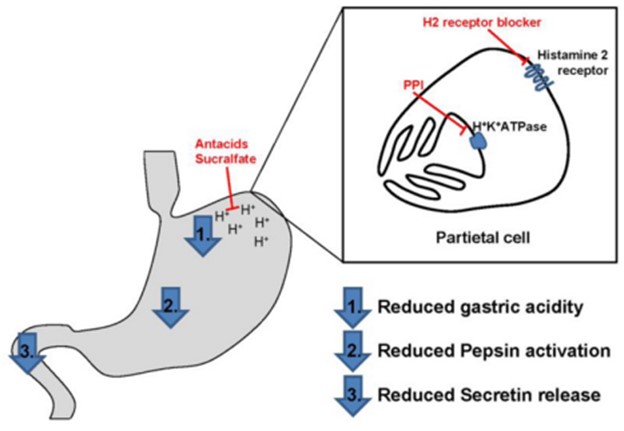
Sucralfate is a medication commonly used in the treatment of peptic ulcer disease. It works by forming a protective barrier over the ulcer site, providing a physical barrier against gastric acid, and promoting the healing process. When teaching a client about sucralfate, it is important to provide instructions regarding its proper administration.
One of the key instructions is to take sucralfate 1 hour before meals. This timing allows the medication to form a protective coating in the stomach before food is ingested. Taking sucralfate on an empty stomach enhances its effectiveness in protecting the ulcer and promoting healing.
"Take the medication with an antacid" - Sucralfate should not be taken with an antacid. Antacids can interfere with the protective mechanism of sucralfate by neutralizing stomach acid, which is necessary for sucralfate to bind and form a protective coating. It is recommended to wait at least 30 minutes to 1 hour after taking sucralfate before taking an antacid.
"Take as needed for pain relief" - Sucralfate is not typically used for immediate pain relief in peptic ulcer disease. It is primarily used for its protective and healing properties. Pain relief is
usually addressed with other medications, such as antacids, acid-reducing medications, or pain medications as prescribed by a healthcare provider.
"Store the medication in the refrigerator" - Sucralfate does not require refrigeration. It should be stored at room temperature, away from excessive heat or moisture, as per the specific instructions provided by the manufacturer or healthcare provider.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Bisacodyl is a stimulant laxative commonly used to treat constipation. However, it is important to educate the client about the potential risks associated with chronic laxative use. The statement regarding electrolyte imbalance is important because excessive or prolonged use of laxatives can lead to electrolyte disturbances, such as low potassium levels (hypokalemia), which can have adverse effects on various body functions.
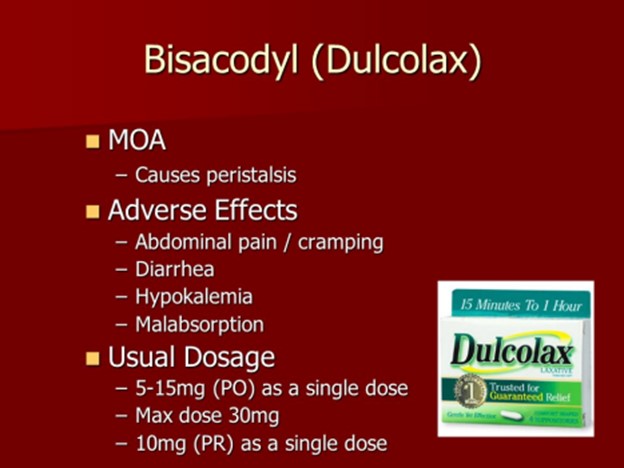
"Daily bowel movements are necessary for good intestinal health": While regular bowel movements are generally desirable, stating that daily bowel movements are necessary for good intestinal health is an overgeneralization. Bowel movement frequency can vary among individuals, and it is important to consider other factors such as diet, hydration, and overall health.
"Chronic use of laxatives can lead to a tear in the rectal mucosa": While chronic use of laxatives can lead to complications such as dependence and potential damage to the digestive system, specifically mentioning a tear in the rectal mucosa (rectal mucosal injury) is not the most commonly associated concern.
"Decrease your intake of high-fiber foods": It is generally recommended to increase fiber intake for individuals with constipation. Decreasing high-fiber foods would counteract the benefits of dietary fiber in promoting regular bowel movements and alleviating constipation.
Correct Answer is B
Explanation
Measuring the output from an indwelling urinary catheter is within the scope of practice for an assistive personnel (AP). It involves a straightforward task that does not require specialized nursing knowledge or judgment.
The other tasks mentioned should not be delegated to an AP:
Administer an enteral feeding to a client who has a new gastrostomy tube: Administering enteral feedings requires specialized knowledge and training to ensure proper placement and administration. This task should be performed by a licensed nurse.
Evaluate a client's pain level 30 min after receiving an oral analgesic: Evaluating pain level and the effectiveness of pain management requires nursing assessment and judgment. This task should be performed by a licensed nurse.
Reinforce foot care to a client who has a new diagnosis of diabetes mellitus: Providing education and reinforcing foot care to a client with a new diagnosis of diabetes requires
specialized knowledge about the disease and its management. This task should be performed by a licensed nurse.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
