A nurse is collecting data from a client who has peptic ulcer disease. Which of the following findings is a manifestation of gastrointestinal perforation?
Bradycardia
Hyperactive bowel sounds
Report of epigastric fullness
Severe upper abdominal pain
The Correct Answer is D
Choice A: Bradycardia. This is not a manifestation of gastrointestinal perforation, but rather a sign of vagal stimulation, which can occur in response to gastric distension, vomiting, or suctioning. Vagal stimulation can slow down the heart rate and lower the blood pressure.
Choice B: Hyperactive bowel sounds. This is not a manifestation of gastrointestinal perforation, but rather a sign of increased intestinal motility, which can occur in response to inflammation, infection, or irritation of the gastrointestinal tract. Hyperactive bowel sounds are loud, high-pitched, and frequent.
Choice C: Report of epigastric fullness. This is not a manifestation of gastrointestinal perforation, but rather a sign of delayed gastric emptying, which can occur in response to gastric outlet obstruction, gastroparesis, or pyloric stenosis. Epigastric fullness is a feeling of pressure or discomfort in the upper abdomen after eating.
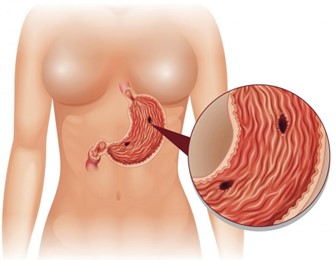
Choice D: Severe upper abdominal pain. This is a manifestation of gastrointestinal perforation, which is a life-threatening complication of peptic ulcer disease. Peptic ulcer disease is a condition that causes erosion and ulceration of the mucosal lining of the stomach or duodenum. If the ulcer penetrates through the wall of the gastrointestinal tract, it can cause perforation, which is a hole that allows gastric contents to leak into the peritoneal cavity. This can cause peritonitis, which is an inflammation and infection of the peritoneum. Peritonitis can cause severe upper abdominal pain, which may radiate to the shoulder or back. The pain may be sudden, sharp, and constant.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A: Docusate. This is not a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis. Docusate is a stool softener that can prevent constipation and straining, but it is not indicated for ulcerative colitis.
Choice B: A corticosteroid medication. This is a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis, which is a chronic inflammatory bowel disease that causes ulcers and inflammation in the colon and rectum. A corticosteroid medication, such as prednisone, can reduce inflammation, suppress the immune system, and relieve symptoms such as diarrhea, bleeding, and pain.
Choice C: Aspirin. This is not a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis. Aspirin is a nonsteroidal anti-inflammatory drug (NSAID) that can relieve pain and inflammation, but it can also irritate the gastrointestinal mucosa and worsen ulcerative colitis.
Choice D: A bowel cathartic medication. This is not a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis. A bowel cathartic medication, such as bisacodyl, can stimulate bowel movements and cleanse the colon, but it can also cause dehydration, electrolyte imbalance, and aggravate ulcerative colitis.
Correct Answer is C
Explanation
Choice A: Hypernatremia. This is not a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease. Hypernatremia is a high level of sodium in the blood, which can be caused by dehydration, excessive sodium intake, or kidney dysfunction. It is not related to Addison’s disease or cortisol and aldosterone levels.
Choice B: Bradycardia. This is not a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease. Bradycardia is a slow heart rate, which can be caused by vagal stimulation, medication side effects, or cardiac disorders. It is not related to Addison’s disease or cortisol and aldosterone levels.
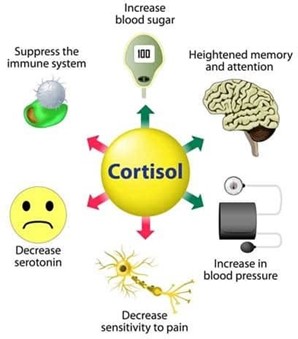
Choice C: Hypotension. This is a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease, which is a condition that occurs when the adrenal glands do not produce enough cortisol and aldosterone. Cortisol is a hormone that regulates the metabolism of carbohydrates, proteins, and fats, and helps the body cope with stress. Aldosterone is a hormone that regulates the balance of sodium and potassium in the blood and fluid volume. Addison’s disease can cause hypotension, which is a low blood pressure, due to decreased aldosterone production and fluid loss.
Choice D: Hypokalemia. This is not a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease. Hypokalemia is a low level of potassium in the blood, which can be caused by diuretics, vomiting, diarrhea, or alkalosis. It is not related to Addison’s disease or cortisol and aldosterone levels.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
