Proctored Exam 4: Gastrointestinal System
Proctored Exam 4: Gastrointestinal System
Total Questions : 21
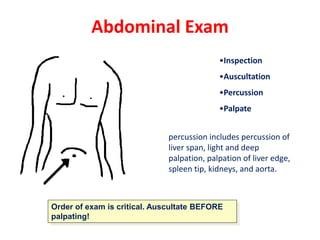
Showing 10 questions Sign up for moreA nurse performs an abdominal assessment on 4 patients. Which of the following would be considered a normal abdominal assessment?
Explanation
A. abdomen nondistended, soft, with active bowel sounds in all four quadrants.
A normal abdominal assessment would involve an abdomen that is not distended (not bloated or swollen), it feels soft to the touch, and there are active bowel sounds heard in all four quadrants. Bowel sounds refer to the sounds produced by the movement of the intestines and are typically described as gurgling or rumbling noises.
Option A describes a normal assessment because the abdomen is not distended, it feels soft, and there are active bowel sounds in all four quadrants.
Option B is incorrect because a distended abdomen and hypoactive bowel sounds (decreased or absent bowel sounds) are not normal findings.
Option C is also incorrect because a distended abdomen with hyperactive bowel sounds (increased and loud bowel sounds) is not normal.
Option D is incorrect because a nondistended abdomen that feels firm and has hypoactive bowel sounds is also not a normal finding.
A nurse is monitoring bowel elimination of a patient who has a history of constipation. The nurse implements measures to assist with bowel elimination if the patient has not had a bowel movement - what would be the BEST option to try first?
Explanation
Stool softeners, also known as emollient laxatives, work by helping to moisten and soften the stool, making it easier to pass. They are typically taken orally and act by promoting water absorption into the stool, thereby making it softer and easier to pass. This option is often recommended as a first-line treatment for constipation, especially for patients with a history of constipation.
Soap suds enema (option B) is not recommendable as the best option to try first because it involves introducing a solution of soap and water into the rectum to stimulate bowel movement. It is usually used for immediate relief of constipation and is not recommended as the first option.
Suppositories (option C) is not recommendable as the best option to try first because they are medications that are inserted into the rectum to stimulate bowel movement. They work by irritating the lining of the rectum and promoting peristalsis. Suppositories are generally considered to be more invasive than stool softeners and are typically used if other methods have not been successful.
Mineral oil enema (option D) is not recommendable as the best option to try first because it involves introducing mineral oil into the rectum to lubricate the stool and facilitate its passage. This option is also considered more aggressive and is usually used when other methods have failed.
A nurse is preparing a cleansing enema for an adult patient who is constipated and has not responded to laxative use. Before giving the enema, the nurse should
Explanation
The nurse should warm the solution to body temperature before giving the enema to the adult patient. It is important for the solution to be at a comfortable and safe temperature for the patient to avoid any discomfort or injury. This can be achieved by using a thermometer to ensure the solution is warmed to approximately body temperature, which is around 98.6 degrees Fahrenheit (37 degrees Celsius). Microwaving the solution or using boiling water can lead to temperature extremes that could harm the patient. Cooling the solution to 65 degrees Fahrenheit may be too cool and uncomfortable for the patient. Therefore, warming the solution to body temperature is the most appropriate choice.
In option A, cooling the solution to 65 degrees F (option A) may be too cold and uncomfortable for the patient.
In option B, boiling the solution and letting it cool down (option B) is not necessary and may result in a solution that is too hot and potentially harmful to the patient. Boiling the solution is not recommended, as it can alter the composition of the enema and make it less effective.
In option D, warming the solution in the microwave (option D) is not recommended, as it can lead to uneven heating and potentially create hot spots in the solution. Microwaving enema solutions can also cause the solution to become too hot and pose a risk of injury to the patient.
It is important for the nurse to follow the manufacturer's instructions for preparing the cleansing enema solution, ensuring it is warmed to body temperature to provide optimal patient comfort and safety during the procedure.

There is an order to administer a large volume, cleansing enema to an adult patient. The enema bag is filled with how many milliliters of fluid for this procedure?
Explanation
A large volume enema is usually administered with 500 to 1000 mL of fluid. This amount of fluid helps to promote a thorough cleansing of the colon and facilitate the removal of fecal material. However, it's important to note that the specific volume may vary depending on the patient's individual needs, clinical situation, and healthcare provider's instructions.
300 to 500 mL in option (A) is incorrect because its wont help to promote a thorough cleansing of the colon.
200 to 100 mL in option (C) is incorrect because it will not facilitate the removal of fecal material.
50 to 150 ml in option (D) is incorrect because it describes smaller volumes of fluid that would be more suitable for other types of enemas, such as small volume enemas or retention enemas, which have different purposes and indications.
A patient who is constipated has just received a mineral oil-retention enema. The nurse encourages this patient to hold this enema for a minimum of how long?
Explanation
When a patient receives a mineral oil-retention enema for constipation, it is important for them to hold the enema for at least 15 minutes to allow the mineral oil to soften the stool and facilitate its passage. During this time, the patient should try to resist the urge to defecate and retain the enema solution in the rectum for the desired effect.
Holding the enema for just 5 minutes (option A) may not provide sufficient time for the mineral oil to have an optimal effect on softening the stool.
Holding the enema for 60 minutes (option B) is incorrect because is not typically necessary and may cause discomfort or inconvenience to the patient. Most mineral oil-retention enemas do not require such a long duration of retention.
Holding the enema for just 1 minute (option C) is incorrect because is too short a duration for the mineral oil to have any significant effect on softening the stool.
It is important for the nurse to provide specific instructions to the patient regarding the duration of enema retention and ensure the patient understands the importance of following these instructions.
A nurse is digitally removing stool that is impacted from a patient. The nurse should stop the procedure immediately and take corrective action if the patient's
Explanation
During the digital removal of impacted stool, if the patient's pulse rate decreases significantly, it is an indication of a potentially serious condition and the nurse should stop the procedure immediately. A sudden decrease in pulse rate may indicate vagal stimulation, which can lead to a vasovagal response or a more severe cardiovascular event. The nurse should assess the patient's condition, provide appropriate interventions, and notify the healthcare provider as necessary. The other options presented in the question are within normal ranges or do not indicate an immediate need for corrective action.
An increase in blood pressure from 110/84 to 118/88 mm Hg (option A) may not necessarily require immediate action, as it falls within a normal range and may be attributed to factors such as anxiety or pain.
A small increase in temperature from 98.8°F to 99.0°F (option B) may not be alarming on its own and may be within normal fluctuations.
An increase in respiratory rate from 16 to 24 breaths/min (option D) may indicate increased effort or anxiety during the procedure but is not typically a cause for immediate concern unless accompanied by other significant symptoms.

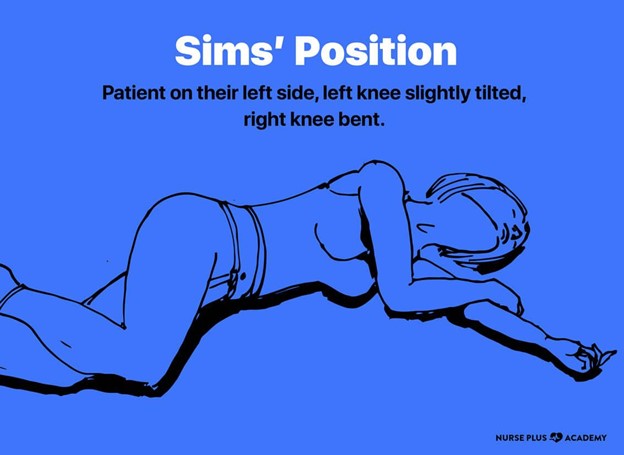
A nurse is preparing her patient to receive a Fleet enema. What position is best for the procedure?
Explanation
When preparing a patient to receive a Fleet enema, the left, lateral side-lying position (also known as the Sims position) is typically the most suitable. This position allows for better access to the rectum, making the administration of the enema easier and more effective. In the Sims position, the patient lies on their left side with the upper knee flexed, which helps to expose the rectal area for the enema administration. It also facilitates the retention of the enema solution, allowing it to flow toward the descending colon.
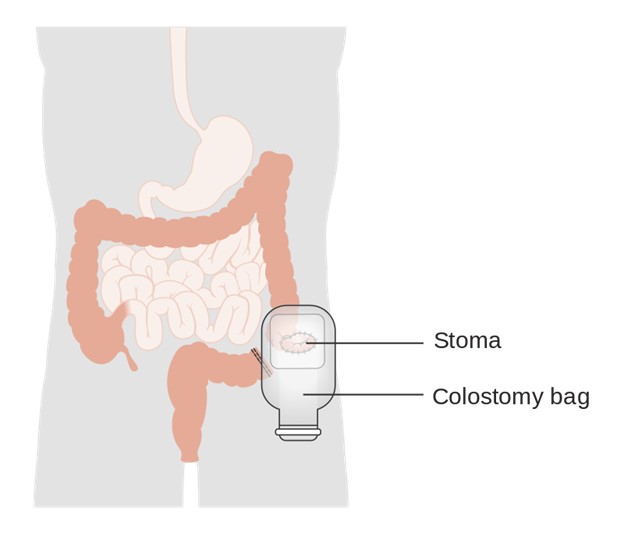
A patient with a colostomy asks how often the faceplate (wafer) of the ostomy appliance should be changed. The most appropriate response by the nurse is that it is usually changed every
Explanation
The faceplate, also known as the wafer or barrier, of an ostomy appliance should typically be changed every 3 to 5 days. This timeframe allows for regular maintenance of the stoma and surrounding skin, ensuring proper hygiene and minimizing the risk of skin irritation or infection. However, it's important to note that individual circumstances may vary, and the frequency of faceplate changes can be adjusted based on the patient's specific needs, the type of ostomy, and the condition of the skin. Regular assessment of the stoma and peristomal skin is essential to determine the optimal timing for faceplate changes.
A nurse is caring for a patient with a colostomy. The ostomy drainage bag should be emptied whenever it is
Explanation
A.Waiting until the bag is completely full before emptying can lead to leakage, discomfort, and potential damage to the stoma or skin surrounding it. It's generally best to empty the bag before it becomes completely full.
B.This is a good practice to prevent overfilling and reduce the risk of leaks or discomfort. Emptying the bag when it is about half full helps maintain the bag's functionality and ensures the stoma site remains clean and secure.
C. 1/4 full
While emptying the bag at this level could prevent overfilling, it may be more frequent than necessary and could be inconvenient for the patient.
D. % full The exact percentage is not typically used as a guideline for when to empty the bag. The general practice is based on visual assessment of how full the bag is.
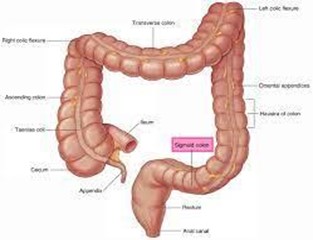
The nurse would expect the least formed stool to be present in which portion of the digestive tract?
Explanation
a. Sigmoid colon: By the time the stool reaches the sigmoid colon, it is typically well-formed and solid. The sigmoid colon is the last segment of the colon before the rectum, and at this point, most water has been absorbed from the stool.
b. Ascending colon: The ascending colon is where the least formed stool is found. As the contents move from the small intestine into the large intestine, they are still in a liquid state. The ascending colon is the first part of the large intestine where absorption of water and electrolytes begins, but the stool is not yet fully formed.
c. Descending colon: In the descending colon, the stool is more solid than in the ascending and transverse colon but not as fully formed as it will be in the sigmoid colon. Water absorption continues in this section, leading to the stool becoming more solid.
d. Transverse colon: The transverse colon lies between the ascending and descending colon. The stool here is more formed than in the ascending colon but still not as solid as it will be by the time it reaches the descending and sigmoid colon. The process of water absorption is ongoing in this section.
You just viewed 10 questions out of the 21 questions on the Proctored Exam 4: Gastrointestinal System Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



